User login
Aspirin for primary prevention? No clear guidance in 2015
ESTES PARK, COLO. – Physicians who choose not to recommend daily aspirin for primary prevention of cardiovascular disease have nothing to apologize for, even though their position is at odds with a current recommendation by the U.S. Preventive Services Task Force (USPSTF), Dr. David Tanaka declared at a conference on internal medicine sponsored by the University of Colorado.
Non-recommenders of aspirin for primary cardiovascular prevention have plenty of company, as highlighted in two recent large studies, noted Dr. Tanaka, a general internist at the university.
In one study, investigators analyzed National Health and Nutrition Examination Survey data for 2011-2012. They determined that while 87% of U.S. men aged 45-79 years were potentially eligible for aspirin for primary prevention of cardiovascular events under the USPSTF grade-A recommendation, a minority (34%) had received guidance from their physician to adopt this measure.
Further, 16% of women aged 55-79 years were eligible for aspirin for primary cardiovascular prevention under the USPSTF recommendation. As was the case for eligible men, the clinical recommendation rate for this practice was low: 42% of women had been advised to take a daily aspirin (J Gen Intern Med. 2015 Feb;30:155-60. doi: 10.1007/s11606-014-2985-8).
Dr. Tanaka noted that the task force is in the process of reassessing its current recommendations on aspirin for primary prevention, issued in 2009; the revision was slated to be published in 2014, according to the task force website.
The other highly revealing recent study was an analysis of 119 U.S. cardiology practices participating in the American College of Cardiology’s National Cardiovascular Disease Registry Practice Innovation and Clinical Excellence Registry (PINNACLE), a quality-improvement project.
The registry did not employ the USPSTF standard for eligibility for aspirin as primary prevention, opting instead to utilize an estimated 10-year cardiovascular disease risk of 6% or higher. Among 68,808 registry patients on aspirin for primary prevention, investigators determined that usage was inappropriate in 11.6% because their 10-year cardiovascular disease risk was below 6%. The most interesting finding, Dr. Tanaka said, was the huge disparity between practices in terms of inappropriate aspirin prescribing; some cardiology practices had zero inappropriate use of aspirin for primary prevention, while in other groups the rate was as high as 72% (J Am Coll Cardiol. 2015 Jan 20;65:111-21. doi: 10.1016/j.jacc.2014.10.035).
“I think these studies show that all of us – cardiologists, general internists, family physicians, everybody – we really don’t know exactly what to do,” Dr. Tanaka observed.
That’s understandable. Current guidelines don’t offer a clear consensus as to what’s best practice. The current 2010 joint ADA/AHA/ACCF scientific statement sings a different tune than those jointly issued in 2006, which remain much more widely known. The American College of Chest Physicians guidelines of 2012, the European Society of Cardiology Working Group on Thrombosis guidelines of 2014...none are in harmony, he said.
“It’s no wonder that there’s a wide variety of recommendations, since the risks and benefits of aspirin for primary prevention are actually very close,” Dr. Tanaka added.
He cited a metaanalysis of nine large randomized, placebo-controlled clinical trials of aspirin for primary prevention totaling more than 100,000 participants. The metaanalysis, conducted by investigators at St. George’s University of London, concluded aspirin did not reduce cardiovascular mortality or stroke, but it did result in a 20% reduction in the risk of nonfatal MI compared with placebo. This was offset by a 31% increase in the risk of nontrivial bleeding, defined as a fatal bleeding event, retinal bleeding, intracerebral bleeding, or GI bleeding requiring hospitalization and transfusion. The risk of hemorrhagic stroke was increased in aspirin users by roughly 1 event per 1,000 patients over 5 years (Arch Intern Med. 2012 Feb 13;172:209-16).
“If you really need good, solid proof in order to use a therapy, you can say ‘I’m not going to use aspirin for primary prevention because it’s not going to decrease my patients’ risk of dying,’ and that’s OK,” Dr. Tanaka said.
Many physicians will want to take a more nuanced approach, though, by individualizing the risk/benefit assessment and engaging in shared decision-making with at-risk patients, he continued.
At present, in Dr. Tanaka’s view, the best tools for this purpose are the AHA/ACC risk calculator, available online and as an app, and the Qbleed score, developed and validated in the U.K. in 753 general practices, with a massive derivation cohort of 4.4 million patients and 16.4 million person-years and validation cohort of 1.4 million patients. The Qbleed is by far the most precise tool available today for estimating bleeding risk.
Using the example of a 60-year-old woman with hypertension, diabetes, and no cardiovascular symptoms, Dr. Tanaka plugged the patient data into the AHA/ACC risk calculator and Qbleed and determined that her baseline 10-year risk of a cardiovascular event is 10%, with a 10-year risk of GI bleeding of 1% and a 0.4% risk of intracranial bleeding. Based upon the metaanalysis results, taking aspirin for primary prevention would reduce her 10-year risk of a nonfatal MI to roughly 8% while increasing her risk of a serious GI bleed from to 1.3%. Thus, her net benefit through taking aspirin would be one or two fewer nonfatal cardiovascular events versus a risk of 1.3 serious GI bleeds and roughly 0.5 intracranial bleeds.
“The discussion you have to have with your patient is which do you fear more: an MI or bleeding? You have to tell your patient that not all heart attacks or bleeds are the same. Maybe one-quarter or one-third of those bleeds are going to be intracerebral. And for me, an intracerebral bleed is a lot worse than a nonfatal heart attack, at least most of the time,” Dr. Tanaka continued.
In his own practice he finds himself recommending statins for primary prevention many times more frequently than aspirin.
“The people who qualify for aspirin will definitely quality for a statin, and statins are safer medicines with a proven cardiovascular mortality benefit. Statins have their own problems, but they don’t include GI and intracranial bleeding,” he said.
He emphasized that in contrast to primary prevention, aspirin for secondary cardiovascular prevention is unequivocally beneficial, with multiple studies showing a benefit-to-risk ratio of about 10-to-1.
Dr. Tanaka reported having no financial conflicts regarding his presentation.
ESTES PARK, COLO. – Physicians who choose not to recommend daily aspirin for primary prevention of cardiovascular disease have nothing to apologize for, even though their position is at odds with a current recommendation by the U.S. Preventive Services Task Force (USPSTF), Dr. David Tanaka declared at a conference on internal medicine sponsored by the University of Colorado.
Non-recommenders of aspirin for primary cardiovascular prevention have plenty of company, as highlighted in two recent large studies, noted Dr. Tanaka, a general internist at the university.
In one study, investigators analyzed National Health and Nutrition Examination Survey data for 2011-2012. They determined that while 87% of U.S. men aged 45-79 years were potentially eligible for aspirin for primary prevention of cardiovascular events under the USPSTF grade-A recommendation, a minority (34%) had received guidance from their physician to adopt this measure.
Further, 16% of women aged 55-79 years were eligible for aspirin for primary cardiovascular prevention under the USPSTF recommendation. As was the case for eligible men, the clinical recommendation rate for this practice was low: 42% of women had been advised to take a daily aspirin (J Gen Intern Med. 2015 Feb;30:155-60. doi: 10.1007/s11606-014-2985-8).
Dr. Tanaka noted that the task force is in the process of reassessing its current recommendations on aspirin for primary prevention, issued in 2009; the revision was slated to be published in 2014, according to the task force website.
The other highly revealing recent study was an analysis of 119 U.S. cardiology practices participating in the American College of Cardiology’s National Cardiovascular Disease Registry Practice Innovation and Clinical Excellence Registry (PINNACLE), a quality-improvement project.
The registry did not employ the USPSTF standard for eligibility for aspirin as primary prevention, opting instead to utilize an estimated 10-year cardiovascular disease risk of 6% or higher. Among 68,808 registry patients on aspirin for primary prevention, investigators determined that usage was inappropriate in 11.6% because their 10-year cardiovascular disease risk was below 6%. The most interesting finding, Dr. Tanaka said, was the huge disparity between practices in terms of inappropriate aspirin prescribing; some cardiology practices had zero inappropriate use of aspirin for primary prevention, while in other groups the rate was as high as 72% (J Am Coll Cardiol. 2015 Jan 20;65:111-21. doi: 10.1016/j.jacc.2014.10.035).
“I think these studies show that all of us – cardiologists, general internists, family physicians, everybody – we really don’t know exactly what to do,” Dr. Tanaka observed.
That’s understandable. Current guidelines don’t offer a clear consensus as to what’s best practice. The current 2010 joint ADA/AHA/ACCF scientific statement sings a different tune than those jointly issued in 2006, which remain much more widely known. The American College of Chest Physicians guidelines of 2012, the European Society of Cardiology Working Group on Thrombosis guidelines of 2014...none are in harmony, he said.
“It’s no wonder that there’s a wide variety of recommendations, since the risks and benefits of aspirin for primary prevention are actually very close,” Dr. Tanaka added.
He cited a metaanalysis of nine large randomized, placebo-controlled clinical trials of aspirin for primary prevention totaling more than 100,000 participants. The metaanalysis, conducted by investigators at St. George’s University of London, concluded aspirin did not reduce cardiovascular mortality or stroke, but it did result in a 20% reduction in the risk of nonfatal MI compared with placebo. This was offset by a 31% increase in the risk of nontrivial bleeding, defined as a fatal bleeding event, retinal bleeding, intracerebral bleeding, or GI bleeding requiring hospitalization and transfusion. The risk of hemorrhagic stroke was increased in aspirin users by roughly 1 event per 1,000 patients over 5 years (Arch Intern Med. 2012 Feb 13;172:209-16).
“If you really need good, solid proof in order to use a therapy, you can say ‘I’m not going to use aspirin for primary prevention because it’s not going to decrease my patients’ risk of dying,’ and that’s OK,” Dr. Tanaka said.
Many physicians will want to take a more nuanced approach, though, by individualizing the risk/benefit assessment and engaging in shared decision-making with at-risk patients, he continued.
At present, in Dr. Tanaka’s view, the best tools for this purpose are the AHA/ACC risk calculator, available online and as an app, and the Qbleed score, developed and validated in the U.K. in 753 general practices, with a massive derivation cohort of 4.4 million patients and 16.4 million person-years and validation cohort of 1.4 million patients. The Qbleed is by far the most precise tool available today for estimating bleeding risk.
Using the example of a 60-year-old woman with hypertension, diabetes, and no cardiovascular symptoms, Dr. Tanaka plugged the patient data into the AHA/ACC risk calculator and Qbleed and determined that her baseline 10-year risk of a cardiovascular event is 10%, with a 10-year risk of GI bleeding of 1% and a 0.4% risk of intracranial bleeding. Based upon the metaanalysis results, taking aspirin for primary prevention would reduce her 10-year risk of a nonfatal MI to roughly 8% while increasing her risk of a serious GI bleed from to 1.3%. Thus, her net benefit through taking aspirin would be one or two fewer nonfatal cardiovascular events versus a risk of 1.3 serious GI bleeds and roughly 0.5 intracranial bleeds.
“The discussion you have to have with your patient is which do you fear more: an MI or bleeding? You have to tell your patient that not all heart attacks or bleeds are the same. Maybe one-quarter or one-third of those bleeds are going to be intracerebral. And for me, an intracerebral bleed is a lot worse than a nonfatal heart attack, at least most of the time,” Dr. Tanaka continued.
In his own practice he finds himself recommending statins for primary prevention many times more frequently than aspirin.
“The people who qualify for aspirin will definitely quality for a statin, and statins are safer medicines with a proven cardiovascular mortality benefit. Statins have their own problems, but they don’t include GI and intracranial bleeding,” he said.
He emphasized that in contrast to primary prevention, aspirin for secondary cardiovascular prevention is unequivocally beneficial, with multiple studies showing a benefit-to-risk ratio of about 10-to-1.
Dr. Tanaka reported having no financial conflicts regarding his presentation.
ESTES PARK, COLO. – Physicians who choose not to recommend daily aspirin for primary prevention of cardiovascular disease have nothing to apologize for, even though their position is at odds with a current recommendation by the U.S. Preventive Services Task Force (USPSTF), Dr. David Tanaka declared at a conference on internal medicine sponsored by the University of Colorado.
Non-recommenders of aspirin for primary cardiovascular prevention have plenty of company, as highlighted in two recent large studies, noted Dr. Tanaka, a general internist at the university.
In one study, investigators analyzed National Health and Nutrition Examination Survey data for 2011-2012. They determined that while 87% of U.S. men aged 45-79 years were potentially eligible for aspirin for primary prevention of cardiovascular events under the USPSTF grade-A recommendation, a minority (34%) had received guidance from their physician to adopt this measure.
Further, 16% of women aged 55-79 years were eligible for aspirin for primary cardiovascular prevention under the USPSTF recommendation. As was the case for eligible men, the clinical recommendation rate for this practice was low: 42% of women had been advised to take a daily aspirin (J Gen Intern Med. 2015 Feb;30:155-60. doi: 10.1007/s11606-014-2985-8).
Dr. Tanaka noted that the task force is in the process of reassessing its current recommendations on aspirin for primary prevention, issued in 2009; the revision was slated to be published in 2014, according to the task force website.
The other highly revealing recent study was an analysis of 119 U.S. cardiology practices participating in the American College of Cardiology’s National Cardiovascular Disease Registry Practice Innovation and Clinical Excellence Registry (PINNACLE), a quality-improvement project.
The registry did not employ the USPSTF standard for eligibility for aspirin as primary prevention, opting instead to utilize an estimated 10-year cardiovascular disease risk of 6% or higher. Among 68,808 registry patients on aspirin for primary prevention, investigators determined that usage was inappropriate in 11.6% because their 10-year cardiovascular disease risk was below 6%. The most interesting finding, Dr. Tanaka said, was the huge disparity between practices in terms of inappropriate aspirin prescribing; some cardiology practices had zero inappropriate use of aspirin for primary prevention, while in other groups the rate was as high as 72% (J Am Coll Cardiol. 2015 Jan 20;65:111-21. doi: 10.1016/j.jacc.2014.10.035).
“I think these studies show that all of us – cardiologists, general internists, family physicians, everybody – we really don’t know exactly what to do,” Dr. Tanaka observed.
That’s understandable. Current guidelines don’t offer a clear consensus as to what’s best practice. The current 2010 joint ADA/AHA/ACCF scientific statement sings a different tune than those jointly issued in 2006, which remain much more widely known. The American College of Chest Physicians guidelines of 2012, the European Society of Cardiology Working Group on Thrombosis guidelines of 2014...none are in harmony, he said.
“It’s no wonder that there’s a wide variety of recommendations, since the risks and benefits of aspirin for primary prevention are actually very close,” Dr. Tanaka added.
He cited a metaanalysis of nine large randomized, placebo-controlled clinical trials of aspirin for primary prevention totaling more than 100,000 participants. The metaanalysis, conducted by investigators at St. George’s University of London, concluded aspirin did not reduce cardiovascular mortality or stroke, but it did result in a 20% reduction in the risk of nonfatal MI compared with placebo. This was offset by a 31% increase in the risk of nontrivial bleeding, defined as a fatal bleeding event, retinal bleeding, intracerebral bleeding, or GI bleeding requiring hospitalization and transfusion. The risk of hemorrhagic stroke was increased in aspirin users by roughly 1 event per 1,000 patients over 5 years (Arch Intern Med. 2012 Feb 13;172:209-16).
“If you really need good, solid proof in order to use a therapy, you can say ‘I’m not going to use aspirin for primary prevention because it’s not going to decrease my patients’ risk of dying,’ and that’s OK,” Dr. Tanaka said.
Many physicians will want to take a more nuanced approach, though, by individualizing the risk/benefit assessment and engaging in shared decision-making with at-risk patients, he continued.
At present, in Dr. Tanaka’s view, the best tools for this purpose are the AHA/ACC risk calculator, available online and as an app, and the Qbleed score, developed and validated in the U.K. in 753 general practices, with a massive derivation cohort of 4.4 million patients and 16.4 million person-years and validation cohort of 1.4 million patients. The Qbleed is by far the most precise tool available today for estimating bleeding risk.
Using the example of a 60-year-old woman with hypertension, diabetes, and no cardiovascular symptoms, Dr. Tanaka plugged the patient data into the AHA/ACC risk calculator and Qbleed and determined that her baseline 10-year risk of a cardiovascular event is 10%, with a 10-year risk of GI bleeding of 1% and a 0.4% risk of intracranial bleeding. Based upon the metaanalysis results, taking aspirin for primary prevention would reduce her 10-year risk of a nonfatal MI to roughly 8% while increasing her risk of a serious GI bleed from to 1.3%. Thus, her net benefit through taking aspirin would be one or two fewer nonfatal cardiovascular events versus a risk of 1.3 serious GI bleeds and roughly 0.5 intracranial bleeds.
“The discussion you have to have with your patient is which do you fear more: an MI or bleeding? You have to tell your patient that not all heart attacks or bleeds are the same. Maybe one-quarter or one-third of those bleeds are going to be intracerebral. And for me, an intracerebral bleed is a lot worse than a nonfatal heart attack, at least most of the time,” Dr. Tanaka continued.
In his own practice he finds himself recommending statins for primary prevention many times more frequently than aspirin.
“The people who qualify for aspirin will definitely quality for a statin, and statins are safer medicines with a proven cardiovascular mortality benefit. Statins have their own problems, but they don’t include GI and intracranial bleeding,” he said.
He emphasized that in contrast to primary prevention, aspirin for secondary cardiovascular prevention is unequivocally beneficial, with multiple studies showing a benefit-to-risk ratio of about 10-to-1.
Dr. Tanaka reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS From the ANNUAL INTERNAL MEDICINE PROGRAM
In refractory asthma, think vocal cord dysfunction
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
ESTES PARK, COLO. – Consider the possibility of comorbid vocal cord dysfunction in patients with asthma that doesn’t respond to aggressive therapy.
“Vocal cord dysfunction is an important diagnosis. It’s something to think about in your toughest-to-treat asthma patients. I think you’ll see a lot of it,” Dr. Robert L. Keith predicted at a conference on internal medicine sponsored by the University of Colorado.
Vocal cord dysfunction (VCD) is defined as adduction or closure of the vocal cords on inspiration or exhalation. VCD is a notorious mimicker of asthma. The two conditions share many signs and symptoms, including wheezing, shortness of breath, cough, chest tightness, stridor, and throat tightness, noted Dr. Keith, professor of medicine in the department of pulmonology and critical care medicine at the university.
In a classic study, investigators at National Jewish Health in Denver found that among patients referred to the tertiary center for asthma who had failed to respond to conventional therapies, 30% turned out to have asthma plus VCD and another 10% actually had VCD alone (Semin Respir Crit Care Med 1994;15(2):161-67).
The diagnosis of VCD is suggested by worsening symptoms upon bronchoprovocation during pulmonary function testing, with no change in forced expiratory volume in 1 second (FEV1) or PC20, which is the dose of the provocative inhalational agent required to produce a 20% drop in FEV1.
“You can think of VCD as extrathoracic obstruction,” Dr. Keith said.
Definitive diagnosis of VCD is made by direct fiber optic laryngoscopy carried out with no sedation, which would affect the vocal cords. Look for abnormal vocal cord movements during a variety of patient maneuvers, including panting and full inhalation and exhalation, Dr. Keith advised.
The cornerstone of VCD treatment is specific breathing exercises which were pioneered by and are still typically led by speech therapists. Hypnosis, biofeedback, and psychotherapy can be helpful. Patients experiencing a severe acute attack obtain benefit from inhaling a helium/oxygen mixture.
Injection of botulinum toxin or sectioning of the laryngeal nerve in order to affect vocal cord movement are other options, although Dr. Keith said he has never found it necessary to refer patients with VCD for those therapies.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Perioperative cardiovascular assessment guidelines pose new challenges
ESTES PARK, COLO. – The latest American College of Cardiology/American Heart Association guidelines on perioperative cardiovascular evaluation in patients undergoing noncardiac surgery create several major new responsibilities for physicians doing the evaluations.
Some primary care physicians will be uncomfortable with several of the new recommendations. Perhaps that shouldn’t come as a surprise, since not a single primary care physician was included among the 17 members of the writing committee or the 38-member review committee. Cardiologists of all subspecialties, surgeons, anesthesiologists, hospitalists, a patient representative – all had a voice. But not primary care, Dr. Robert E. Burke noted at a conference on internal medicine sponsored by the University of Colorado.
He was quick to add, however, that the document (Circulation. 2014 Dec 9;130[24]:e278-333) is an impressive, thoughtful piece of work built upon 490 reference citations, and it deserves to be incorporated into daily clinical practice, albeit with a few caveats.
“I think the writing panel did a really good job, but the recommendations are only as good as the evidence – and there are a couple of areas where the evidence is not very strong ... It’s up to you and your patient to decide what to do in the controversial areas,” said Dr. Burke, assistant chief of hospital medicine at the Denver VA Medical Center and an internist at the university.
A big change from the previous 2007 ACC/AHA guidelines that Dr. Burke fully supports is that it’s no longer sufficient for the evaluating physician to formally consider only the level of risk posed by the patient’s planned noncardiac surgery, which can vary from a low-risk operation such as cataract surgery to a far-higher-risk procedure addressing, for example, an expanding abdominal aortic aneurysm.
Under the 2014 guidelines, it’s also important to incorporate the surgical risk with an estimate of the individual’s personalized risk of perioperative major adverse cardiovascular events. If the estimated risk is less than 1%, it’s appropriate to proceed straightaway with surgery. In contrast, a 1% or greater perioperative risk is considered high, and it’s then recommended to continue along a lengthy management algorithm. This involves sending the patient for cardiac stress testing provided two conditions are met: the surgeon has to be unwilling to operate without the stress test results and the patient must be willing to undergo CABG before the noncardiac surgery, should the stress test and follow-up cardiac catheterization prove positive.
The guidelines recommend using either of two validated risk-prediction tools for calculating patient risk: the Revised Cardiac Risk Index (Circulation 1999 Sep 7;100[10]:1043-9) or the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP) predictor. Dr. Burke prefers the NSQIP tool. It predicts multiple cardiac and noncardiac outcomes, including all-cause mortality, within 30 days of surgery, and it has been validated in 525 U.S. hospitals with more than 1 million operations. It’s also quite user-friendly, according to Dr. Burke.
In his view, the guidelines contain two major areas of controvery. One involves the much more aggressive approach to revascularization prior to noncardiac surgery in high-cardiovascular-risk patients compared with the 2007 guidelines. The current guidelines give a class I recommendation to revascularization before noncardiac surgery in patients with left main or triple-vessel disease, as well as two-vessel disease that includes the left anterior descending coronary artery. He said this is a leap that’s not supported by the best available evidence, which comes from the older CARP (Coronary-Artery Revascularization before Elective Major Vascular Surgery) trial.
In CARP, 510 military veterans with documented coronary artery disease and planned vascular surgery were randomized to preoperative revascularization or not. The only exclusions were left main disease, severe aortic stenosis, or a left ventricular ejection fraction below 20%. After 2.8 years of follow-up post surgery, preoperative revascularization wasn’t associated with any mortality benefit in any patient subgroup (N Engl J Med. 2004 Dec 30;351[27]:2795-804).
“I want to restate that in this well-done randomized controlled trial, they could not find any benefit in any outcome in any group within this very-high-risk group of patients. This is really the main trial that exists in perioperative care, and I’m very impressed with the results. The guidelines extrapolate from studies in other areas. This is one area where I think the cardiologists are more interventional than I would like. If I had a patient in my office I could not tell him with a straight face that revascularization before their planned surgery is going to offer them any benefit during up to nearly 3 years of follow-up unless they have left main disease, which was an exclusion in CARP,” Dr. Burke said.
The other main controversy in his view is the ACC/AHA stance on postoperative troponin measurement. It gets a class III rating – meaning no benefit, don’t do it – for routine screening in unselected patients without signs or symptoms suggestive of myocardial ischemia. This recommendation is based upon the absence to date of a prospective trial showing that acting on an elevated postoperative troponin in such patients improves outcomes. True enough, Dr. Burke conceded, but he finds persuasive the results of VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), a prospective international study in which more than 15,000 patients undergoing noncardiac surgery underwent screening troponin measurements on the first 3 days after surgery.
Thirty-day mortality in the VISION study was 1% in those with a peak fourth-generation troponin of 0.01 ng/mL or less. Mortality was significantly increased in the nearly 12% of patients with a troponin of at least 0.02 ng/mL, climbing to a peak mortality rate of 16.9% in those with a postoperative troponin of 0.30 ng/mL or more (JAMA. 2012 Jun 6;307[21]:2295-304).
“I don’t know of any other test in the perioperative setting that’s as good as this in terms of risk-stratifying patients. We can’t just sit by and let this sort of 30-day mortality rate happen. We should do something. I think that if you treat these asymptomatic patients with an elevated postop troponin as if they had an MI – get them on optimal medical therapy and really push smoking cessation – it’s likely to have a benefit on outcomes,” said Dr. Burke.
He reported having no financial conflicts regarding his presentation.
ESTES PARK, COLO. – The latest American College of Cardiology/American Heart Association guidelines on perioperative cardiovascular evaluation in patients undergoing noncardiac surgery create several major new responsibilities for physicians doing the evaluations.
Some primary care physicians will be uncomfortable with several of the new recommendations. Perhaps that shouldn’t come as a surprise, since not a single primary care physician was included among the 17 members of the writing committee or the 38-member review committee. Cardiologists of all subspecialties, surgeons, anesthesiologists, hospitalists, a patient representative – all had a voice. But not primary care, Dr. Robert E. Burke noted at a conference on internal medicine sponsored by the University of Colorado.
He was quick to add, however, that the document (Circulation. 2014 Dec 9;130[24]:e278-333) is an impressive, thoughtful piece of work built upon 490 reference citations, and it deserves to be incorporated into daily clinical practice, albeit with a few caveats.
“I think the writing panel did a really good job, but the recommendations are only as good as the evidence – and there are a couple of areas where the evidence is not very strong ... It’s up to you and your patient to decide what to do in the controversial areas,” said Dr. Burke, assistant chief of hospital medicine at the Denver VA Medical Center and an internist at the university.
A big change from the previous 2007 ACC/AHA guidelines that Dr. Burke fully supports is that it’s no longer sufficient for the evaluating physician to formally consider only the level of risk posed by the patient’s planned noncardiac surgery, which can vary from a low-risk operation such as cataract surgery to a far-higher-risk procedure addressing, for example, an expanding abdominal aortic aneurysm.
Under the 2014 guidelines, it’s also important to incorporate the surgical risk with an estimate of the individual’s personalized risk of perioperative major adverse cardiovascular events. If the estimated risk is less than 1%, it’s appropriate to proceed straightaway with surgery. In contrast, a 1% or greater perioperative risk is considered high, and it’s then recommended to continue along a lengthy management algorithm. This involves sending the patient for cardiac stress testing provided two conditions are met: the surgeon has to be unwilling to operate without the stress test results and the patient must be willing to undergo CABG before the noncardiac surgery, should the stress test and follow-up cardiac catheterization prove positive.
The guidelines recommend using either of two validated risk-prediction tools for calculating patient risk: the Revised Cardiac Risk Index (Circulation 1999 Sep 7;100[10]:1043-9) or the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP) predictor. Dr. Burke prefers the NSQIP tool. It predicts multiple cardiac and noncardiac outcomes, including all-cause mortality, within 30 days of surgery, and it has been validated in 525 U.S. hospitals with more than 1 million operations. It’s also quite user-friendly, according to Dr. Burke.
In his view, the guidelines contain two major areas of controvery. One involves the much more aggressive approach to revascularization prior to noncardiac surgery in high-cardiovascular-risk patients compared with the 2007 guidelines. The current guidelines give a class I recommendation to revascularization before noncardiac surgery in patients with left main or triple-vessel disease, as well as two-vessel disease that includes the left anterior descending coronary artery. He said this is a leap that’s not supported by the best available evidence, which comes from the older CARP (Coronary-Artery Revascularization before Elective Major Vascular Surgery) trial.
In CARP, 510 military veterans with documented coronary artery disease and planned vascular surgery were randomized to preoperative revascularization or not. The only exclusions were left main disease, severe aortic stenosis, or a left ventricular ejection fraction below 20%. After 2.8 years of follow-up post surgery, preoperative revascularization wasn’t associated with any mortality benefit in any patient subgroup (N Engl J Med. 2004 Dec 30;351[27]:2795-804).
“I want to restate that in this well-done randomized controlled trial, they could not find any benefit in any outcome in any group within this very-high-risk group of patients. This is really the main trial that exists in perioperative care, and I’m very impressed with the results. The guidelines extrapolate from studies in other areas. This is one area where I think the cardiologists are more interventional than I would like. If I had a patient in my office I could not tell him with a straight face that revascularization before their planned surgery is going to offer them any benefit during up to nearly 3 years of follow-up unless they have left main disease, which was an exclusion in CARP,” Dr. Burke said.
The other main controversy in his view is the ACC/AHA stance on postoperative troponin measurement. It gets a class III rating – meaning no benefit, don’t do it – for routine screening in unselected patients without signs or symptoms suggestive of myocardial ischemia. This recommendation is based upon the absence to date of a prospective trial showing that acting on an elevated postoperative troponin in such patients improves outcomes. True enough, Dr. Burke conceded, but he finds persuasive the results of VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), a prospective international study in which more than 15,000 patients undergoing noncardiac surgery underwent screening troponin measurements on the first 3 days after surgery.
Thirty-day mortality in the VISION study was 1% in those with a peak fourth-generation troponin of 0.01 ng/mL or less. Mortality was significantly increased in the nearly 12% of patients with a troponin of at least 0.02 ng/mL, climbing to a peak mortality rate of 16.9% in those with a postoperative troponin of 0.30 ng/mL or more (JAMA. 2012 Jun 6;307[21]:2295-304).
“I don’t know of any other test in the perioperative setting that’s as good as this in terms of risk-stratifying patients. We can’t just sit by and let this sort of 30-day mortality rate happen. We should do something. I think that if you treat these asymptomatic patients with an elevated postop troponin as if they had an MI – get them on optimal medical therapy and really push smoking cessation – it’s likely to have a benefit on outcomes,” said Dr. Burke.
He reported having no financial conflicts regarding his presentation.
ESTES PARK, COLO. – The latest American College of Cardiology/American Heart Association guidelines on perioperative cardiovascular evaluation in patients undergoing noncardiac surgery create several major new responsibilities for physicians doing the evaluations.
Some primary care physicians will be uncomfortable with several of the new recommendations. Perhaps that shouldn’t come as a surprise, since not a single primary care physician was included among the 17 members of the writing committee or the 38-member review committee. Cardiologists of all subspecialties, surgeons, anesthesiologists, hospitalists, a patient representative – all had a voice. But not primary care, Dr. Robert E. Burke noted at a conference on internal medicine sponsored by the University of Colorado.
He was quick to add, however, that the document (Circulation. 2014 Dec 9;130[24]:e278-333) is an impressive, thoughtful piece of work built upon 490 reference citations, and it deserves to be incorporated into daily clinical practice, albeit with a few caveats.
“I think the writing panel did a really good job, but the recommendations are only as good as the evidence – and there are a couple of areas where the evidence is not very strong ... It’s up to you and your patient to decide what to do in the controversial areas,” said Dr. Burke, assistant chief of hospital medicine at the Denver VA Medical Center and an internist at the university.
A big change from the previous 2007 ACC/AHA guidelines that Dr. Burke fully supports is that it’s no longer sufficient for the evaluating physician to formally consider only the level of risk posed by the patient’s planned noncardiac surgery, which can vary from a low-risk operation such as cataract surgery to a far-higher-risk procedure addressing, for example, an expanding abdominal aortic aneurysm.
Under the 2014 guidelines, it’s also important to incorporate the surgical risk with an estimate of the individual’s personalized risk of perioperative major adverse cardiovascular events. If the estimated risk is less than 1%, it’s appropriate to proceed straightaway with surgery. In contrast, a 1% or greater perioperative risk is considered high, and it’s then recommended to continue along a lengthy management algorithm. This involves sending the patient for cardiac stress testing provided two conditions are met: the surgeon has to be unwilling to operate without the stress test results and the patient must be willing to undergo CABG before the noncardiac surgery, should the stress test and follow-up cardiac catheterization prove positive.
The guidelines recommend using either of two validated risk-prediction tools for calculating patient risk: the Revised Cardiac Risk Index (Circulation 1999 Sep 7;100[10]:1043-9) or the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP) predictor. Dr. Burke prefers the NSQIP tool. It predicts multiple cardiac and noncardiac outcomes, including all-cause mortality, within 30 days of surgery, and it has been validated in 525 U.S. hospitals with more than 1 million operations. It’s also quite user-friendly, according to Dr. Burke.
In his view, the guidelines contain two major areas of controvery. One involves the much more aggressive approach to revascularization prior to noncardiac surgery in high-cardiovascular-risk patients compared with the 2007 guidelines. The current guidelines give a class I recommendation to revascularization before noncardiac surgery in patients with left main or triple-vessel disease, as well as two-vessel disease that includes the left anterior descending coronary artery. He said this is a leap that’s not supported by the best available evidence, which comes from the older CARP (Coronary-Artery Revascularization before Elective Major Vascular Surgery) trial.
In CARP, 510 military veterans with documented coronary artery disease and planned vascular surgery were randomized to preoperative revascularization or not. The only exclusions were left main disease, severe aortic stenosis, or a left ventricular ejection fraction below 20%. After 2.8 years of follow-up post surgery, preoperative revascularization wasn’t associated with any mortality benefit in any patient subgroup (N Engl J Med. 2004 Dec 30;351[27]:2795-804).
“I want to restate that in this well-done randomized controlled trial, they could not find any benefit in any outcome in any group within this very-high-risk group of patients. This is really the main trial that exists in perioperative care, and I’m very impressed with the results. The guidelines extrapolate from studies in other areas. This is one area where I think the cardiologists are more interventional than I would like. If I had a patient in my office I could not tell him with a straight face that revascularization before their planned surgery is going to offer them any benefit during up to nearly 3 years of follow-up unless they have left main disease, which was an exclusion in CARP,” Dr. Burke said.
The other main controversy in his view is the ACC/AHA stance on postoperative troponin measurement. It gets a class III rating – meaning no benefit, don’t do it – for routine screening in unselected patients without signs or symptoms suggestive of myocardial ischemia. This recommendation is based upon the absence to date of a prospective trial showing that acting on an elevated postoperative troponin in such patients improves outcomes. True enough, Dr. Burke conceded, but he finds persuasive the results of VISION (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), a prospective international study in which more than 15,000 patients undergoing noncardiac surgery underwent screening troponin measurements on the first 3 days after surgery.
Thirty-day mortality in the VISION study was 1% in those with a peak fourth-generation troponin of 0.01 ng/mL or less. Mortality was significantly increased in the nearly 12% of patients with a troponin of at least 0.02 ng/mL, climbing to a peak mortality rate of 16.9% in those with a postoperative troponin of 0.30 ng/mL or more (JAMA. 2012 Jun 6;307[21]:2295-304).
“I don’t know of any other test in the perioperative setting that’s as good as this in terms of risk-stratifying patients. We can’t just sit by and let this sort of 30-day mortality rate happen. We should do something. I think that if you treat these asymptomatic patients with an elevated postop troponin as if they had an MI – get them on optimal medical therapy and really push smoking cessation – it’s likely to have a benefit on outcomes,” said Dr. Burke.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Remember ‘CURE’ indication for clopidogrel in ACS
ESTES PARK, COLO. – Clopidogrel is vastly underutilized in real-world medical management of patients with unstable angina or non–ST-segment elevation MI who don’t undergo coronary revascularization, Dr. Mel L. Anderson said at a conference on internal medicine sponsored by the University of Colorado.
Such patients fall under the umbrella of the so-called CURE indication for clopidogrel, named for the landmark Clopidogrel in Unstable Angina to Prevent Recurrent Events trial. CURE showed that adding clopidogrel to aspirin for an average of 9 months in patients with acute coronary syndrome without ST-segment elevation reduced the major adverse cardiovascular event rate from 11.4% to 9.3% (N Engl J Med. 2001;345[7]:494-502).
Clinical practice has changed enormously since CURE was published in 2001, so a group of investigators decided to see if discharging medically managed ACS patients on clopidogrel is still beneficial in the contemporary setting. They conducted a retrospective observational cohort study of 16,345 Kaiser Permanente Northern California patients with unstable angina or NSTEMI managed medically without percutaneous coronary intervention or coronary artery bypass graft, of whom only 36% were discharged on clopidogrel.
“It’s disappointing that fully two-thirds of patients did not get clopidogrel when they had an indication for it,” commented Dr. Anderson, chief of the hospital medicine section at the Denver VA Medical Center and an internist at the university.
Two-year all-cause mortality was 8.3% in the clopidogrel users, compared with 13% in propensity-matched controls not on clopidogrel, for an adjusted 37% relative risk reduction in favor of the antiplatelet agent (J Am Coll Cardiol. 2014 Jun 3;63[21]:2249-57).
“That’s a number-needed-to-treat of 20. It’s really quite a robust benefit for a drug that’s now generic and has a well-established safety profile,” Dr. Anderson continued.
The 2-year composite outcome of death or MI occurred in 13.5% of the clopidogrel group and 17.4% of controls, for a number-needed-to-treat of about 25. Clopidogrel’s benefit in terms of this composite endpoint achieved significance only among the 65% of participants with NSTEMI, not those with unstable angina.
“Don’t forget the CURE indication for clopidogrel,” the hospitalist concluded.
ESTES PARK, COLO. – Clopidogrel is vastly underutilized in real-world medical management of patients with unstable angina or non–ST-segment elevation MI who don’t undergo coronary revascularization, Dr. Mel L. Anderson said at a conference on internal medicine sponsored by the University of Colorado.
Such patients fall under the umbrella of the so-called CURE indication for clopidogrel, named for the landmark Clopidogrel in Unstable Angina to Prevent Recurrent Events trial. CURE showed that adding clopidogrel to aspirin for an average of 9 months in patients with acute coronary syndrome without ST-segment elevation reduced the major adverse cardiovascular event rate from 11.4% to 9.3% (N Engl J Med. 2001;345[7]:494-502).
Clinical practice has changed enormously since CURE was published in 2001, so a group of investigators decided to see if discharging medically managed ACS patients on clopidogrel is still beneficial in the contemporary setting. They conducted a retrospective observational cohort study of 16,345 Kaiser Permanente Northern California patients with unstable angina or NSTEMI managed medically without percutaneous coronary intervention or coronary artery bypass graft, of whom only 36% were discharged on clopidogrel.
“It’s disappointing that fully two-thirds of patients did not get clopidogrel when they had an indication for it,” commented Dr. Anderson, chief of the hospital medicine section at the Denver VA Medical Center and an internist at the university.
Two-year all-cause mortality was 8.3% in the clopidogrel users, compared with 13% in propensity-matched controls not on clopidogrel, for an adjusted 37% relative risk reduction in favor of the antiplatelet agent (J Am Coll Cardiol. 2014 Jun 3;63[21]:2249-57).
“That’s a number-needed-to-treat of 20. It’s really quite a robust benefit for a drug that’s now generic and has a well-established safety profile,” Dr. Anderson continued.
The 2-year composite outcome of death or MI occurred in 13.5% of the clopidogrel group and 17.4% of controls, for a number-needed-to-treat of about 25. Clopidogrel’s benefit in terms of this composite endpoint achieved significance only among the 65% of participants with NSTEMI, not those with unstable angina.
“Don’t forget the CURE indication for clopidogrel,” the hospitalist concluded.
ESTES PARK, COLO. – Clopidogrel is vastly underutilized in real-world medical management of patients with unstable angina or non–ST-segment elevation MI who don’t undergo coronary revascularization, Dr. Mel L. Anderson said at a conference on internal medicine sponsored by the University of Colorado.
Such patients fall under the umbrella of the so-called CURE indication for clopidogrel, named for the landmark Clopidogrel in Unstable Angina to Prevent Recurrent Events trial. CURE showed that adding clopidogrel to aspirin for an average of 9 months in patients with acute coronary syndrome without ST-segment elevation reduced the major adverse cardiovascular event rate from 11.4% to 9.3% (N Engl J Med. 2001;345[7]:494-502).
Clinical practice has changed enormously since CURE was published in 2001, so a group of investigators decided to see if discharging medically managed ACS patients on clopidogrel is still beneficial in the contemporary setting. They conducted a retrospective observational cohort study of 16,345 Kaiser Permanente Northern California patients with unstable angina or NSTEMI managed medically without percutaneous coronary intervention or coronary artery bypass graft, of whom only 36% were discharged on clopidogrel.
“It’s disappointing that fully two-thirds of patients did not get clopidogrel when they had an indication for it,” commented Dr. Anderson, chief of the hospital medicine section at the Denver VA Medical Center and an internist at the university.
Two-year all-cause mortality was 8.3% in the clopidogrel users, compared with 13% in propensity-matched controls not on clopidogrel, for an adjusted 37% relative risk reduction in favor of the antiplatelet agent (J Am Coll Cardiol. 2014 Jun 3;63[21]:2249-57).
“That’s a number-needed-to-treat of 20. It’s really quite a robust benefit for a drug that’s now generic and has a well-established safety profile,” Dr. Anderson continued.
The 2-year composite outcome of death or MI occurred in 13.5% of the clopidogrel group and 17.4% of controls, for a number-needed-to-treat of about 25. Clopidogrel’s benefit in terms of this composite endpoint achieved significance only among the 65% of participants with NSTEMI, not those with unstable angina.
“Don’t forget the CURE indication for clopidogrel,” the hospitalist concluded.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
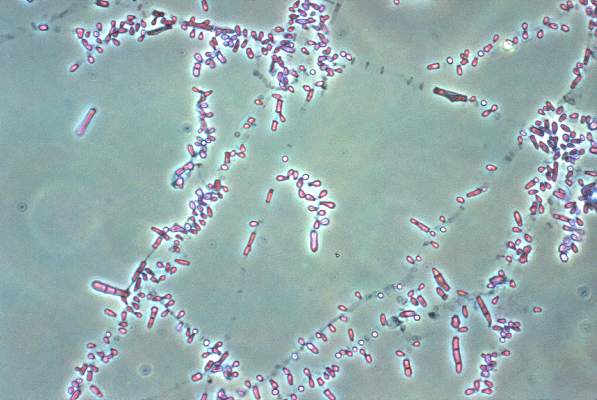
Fungal foot infections risk secondary infection in diabetic patients
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
VANCOUVER – Fungal foot infections in diabetic patients are often ignored and are far more than a cosmetic problem.
In patients with diabetes, tinea pedis and onychomycosis triple the likelihood of secondary bacterial infections including gram-negative intertrigo, cellulitis, and osteomyelitis. Further, they boost up to fivefold the risk of life- and limb-threatening gangrene, Dr. Manuela Papini said at the World Congress of Dermatology.
Her own work (G Ital Dermatol Venereol. 2013 Dec;148(6):603-8), as well as that of others, indicates tinea pedis and onychomycosis in diabetic patients often goes undiagnosed, ignored, or inadequately treated.
In her own experience, four out of five diabetic patients with a fungal foot infection are unaware of it, she said. Moreover, half of those with a diagnosed fungal foot infection remain untreated or insufficiently treated, added Dr. Papini, a dermatologist at the University of Perugia (Italy).
Fungal infections of the foot are three times more common among diabetic individuals than the general population. The reasons for this disparity included impaired peripheral circulation, an immunocompromised state, autonomic neuropathy, and the inability to maintain good foot hygiene because of obesity, impaired vision, or advanced age.
The causative organisms of fungal infections in diabetic patients are the same as those seen in the general population. So are the recommended first-line treatments. But treatment response is generally poor – much worse than in nondiabetics. Adherence to antifungal medication also is a real problem in diabetic patients, due in large part to the high prevalence of comorbid conditions and resultant polypharmacy.
“Most diabetic patients say their large pill burden is an issue, and they think onychomycosis is the least important of their problems,” she explained.
Photodynamic therapy and laser treatments show promise, but the supporting data aren’t yet sufficient to warrant their introduction into clinical practice, according to Dr. Papini.
As for contemporary therapy, she noted that the British Association of Dermatologists, in its current onychomycosis treatment guidelines, reserves its A-strength recommendations for two oral drugs given daily for 12 weeks: terbinafine and itraconazole, although itraconazole can alternatively be used as pulse therapy for 3-6 months. Topical therapies are advised only for superficial white onychomycosis and early distal lateral subungual onychomycosis (Br J Dermatol. 2014 Nov;171(5):937-58).
A systematic review of the published literature on treatment of diabetic fungal foot infections concluded that there is good evidence that oral terbinafine is as safe and effective as itraconazole for treating onychomycosis. The authors, however, found that there is no evidence to guide treatment of tinea pedis in the diabetic population (J Foot Ankle Res. 2011 Dec 4;4:26).
In the nondiabetic population, the first-line treatment for tinea pedis is typically a topical antifungal. A good option in diabetic patients is luliconazole (Luzu), which is active against Trichophyton rubrum – the most common causative organism – and has the advantage of simplicity: the regimen is once-daily treatment for 2 weeks, much shorter than for many other topical antifungals, Dr. Papini observed.
Until new and better treatments come along, she continued, the key to preventing relapse of fungal foot infections in diabetic patients is to choose the simplest and most effective therapy, stress to patients the importance of completing the treatment course, and provide instruction in self-inspection and disinfection of shoes and socks.
Dr. Papini reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
SVELT uses small amounts of fat for breast augmentation
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
VANCOUVER, B.C. – Serial small-volume fat transfer via liposuction is a novel, safe, and economical breast-augmentation procedure with high patient satisfaction, Dr. Barry A.S. Lycka said at the World Congress of Dermatology.
SVELT, an acronym for Serial Small-Volume Elective Lipo Transfer, offers women who are interested in breast augmentation but leery of silicone implants or other foreign materials the appealing prospect of removing unwanted fat from donor sites on their thighs, abdomen, and flanks and transferring it to their breasts, according to Dr. Lycka, a cosmetic dermatologist in private practice and at the University of Alberta, Edmonton.
He developed the office-based procedure together with Dr. Daryl K. Hoffman, a plastic surgeon at Stanford (Calif.) University.
The traditional criticisms of fat augmentation of the breasts are that it can result in fat necrosis, resorption, and/or calcification and that it makes mammographic detection of breast cancer more difficult. These complications, however, typically result from transfer of large quantities of fat, trauma inflicted upon the harvested cells, and imprecise placement of the transferred material.
SVELT sidesteps these issues by harvesting small volumes, typically 100 cc or less, under sterile tumescent anesthesia. The material is purified and then carefully injected into the dermal plane above the breast tissue. Downtime is brief. After several sessions spaced weeks apart, the result is a natural-looking and -feeling breast that is typically one cup size larger than pretreatment, according to the dermatologist.
Dr. Lycka reported on 130 patients who underwent SVELT performed by him or Dr. Hoffman. Fat resorption was minimal. Patients gave the procedure and its outcomes high marks. Complications were limited to three patients who developed small nodules that showed evidence of fat necrosis upon biopsy.
To dermatologists interested in adopting SVELT, Dr. Lycka emphasized that patient selection is critical: This is not a procedure for women who want to dramatically increase their breast size. Adequate viable fat at the donor sites is a must. Careful placement of the transferred material in the dermal plane above the breast tissue is essential. And the patient must always get a mammogram before undergoing SVELT.
EXPERT ANALYSIS FROM WCD 2015
Nail surgery: Top anesthesia tips
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
VANCOUVER – Achieving effective local anesthesia is the critical first step in successful nail surgery, Dr. Chris G. Adigun said at the World Congress of Dermatology.
“Always remember: Nail surgery hurts. Your patients will applaud you enthusiastically when they’re back home for your having used a long-acting anesthetic,” said Dr. Adigun, a dermatologist in group practice in Chapel Hill, N.C.
The three most widely used anesthetic agents in nail surgery are lidocaine (Xylocaine), bupivacaine (Marcaine), and ropivacaine (Naropin). Dr. Adigun said she strongly prefers ropivacaine. It combines the best features of the other two: lidocaine’s rapid onset along with a duration of action that’s even longer than bupivacaine’s, she noted. Ropivacaine’s duration of action is 8-12 hours – and it comes without bupivacaine’s potential for cardiotoxicity. Moreover, ropivacaine has a vasoconstrictive effect, which improves hemostasis and enhances visualization during the surgery.
She provided numerous additional tips on how to predictably achieve effective anesthesia for nail surgery:
• Buffer with sodium bicarbonate. The idea is to bring the anesthetic solution close to physiologic pH, which makes for a far less painful experience than injecting the acidic unbuffered solution.
• Warm it. Investigators have shown that warming anesthetic fluid reduces pain upon injection of both nonbuffered and buffered local anesthetics (Ann Emerg Med. 2011 Jul;58(1):86-98).
• Stick to a small-gauge needle. Dr. Adigan said she favors 30 gauge. It makes for a smaller, less painful puncture and limits the rate of flow of anesthetic fluid into the digital space.
• Inject in a perpendicular plane. This will disrupt fewer nerve endings than when going in at an angle.
“I think this is something that’s not frequently taught to residents in dermatology. I think we almost always go in at an angle, but if you go in at a perpendicular plane, you’re going to cause less pain,” according to Dr. Adigun.
• Inject just below the dermis. The dermis is nociceptor rich, and stretching those tissues by injecting a volume of fluid there will cause intense, continuous pain until the local anesthetic has time to take effect.
• Use distraction techniques liberally. Dr. Adigun said she likes to tell stories and jokes, which she calls “talkesthesia.” She also utilizes a battery-powered massager.
“Put the massager as close to your surgical field as you’re comfortable with. Under the gate theory of pain, you want to create as much sensory ‘noise’ as possible with your distraction techniques so that gate is filled with your sensory noise rather than pain,” the dermatologist explained.
There are three solid, time-tested completely acceptable techniques for getting the target digit numb: the wing block, the traditional digital block, and the transthecal digital block.
Dr. Adigun said she generally relies upon the wing block unless she is concerned that the associated blanching might cause her to lose her digital landmarks during surgery addressing a subtle abnormality. In that situation she turns mainly to the traditional digital block, which doesn’t interfere with digital landmarks and effectively anesthetizes both the paired digital and volar nerves.
The downside of the traditional digital block is it entails a 15- to 20-minute wait for the anesthetic to diffuse. So does the transthecal digital block, which has the additional shortcoming of achieving predictable results only when applied for surgery on the second, third, or fourth digits.
The wing block is an efficient infiltrative technique targeting the distal digit. It offers immediate anesthesia of the total nail unit. To achieve an excellent wing block, initially inject just 0.1-0.2 mL of anesthetic fluid subcutaneously into the proximal nail fold midway between the cuticle and the distal interphalangeal joint. Wait for a wheal to form; then wait an additional 45-60 seconds. At that point, inject obliquely along the lateral edge of the nail fold in the direction of the digital tip. The needle should be advanced while maintaining a gentle fluid bolus ahead of the needle tip in order to minimize the patient’s sensation of the moving needle. The process is then repeated on the opposite side of the digit.
“You want to keep that needle in the dermal plane and avoid filling the pulp with anesthetic fluid. If you do this correctly, only one prick is felt by the patient. I very rarely have to use a full cc of anesthetic fluid when I use a wing block,” Dr. Adigun said.
If any additional needle insertions are needed, make sure they’re placed into tissue that’s already been anesthetized, she added.
Dr. Adigun reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM WCD 2015
Beware of Skin Complications of Newer Antidiabetic Agents
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM WCD 2015
Beware of skin complications of newer antidiabetic agents
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
VANCOUVER, B.C. – Each of the newer classes of antidiabetic medications – the DPP-IV inhibitors, GLP-1 agonists, and SGLT2 inhibitors – has its own characteristic cutaneous side effects, Dr. Justin Endo said at the World Congress of Dermatology.
These drugs aren’t first-line agents for patients with type 2 diabetes, but they have gained solid standing as second-tier medications for the vast number of patients with inadequate glucose control or limiting side effects on first-line therapies, said Dr. Endo of the department of dermatology at the University of Wisconsin–Madison.
DPP-IV inhibitors
The dipeptidyl peptidase–IV inhibitors are the newer drugs linked to the most potentially serious side effects, namely, drug-induced bullous pemphigoid and angioedema.
Investigators at Western Michigan University, Kalamazoo, conducted a literature review and an analysis of the Food and Drug Administration’s Adverse Event Reporting System database and concluded there is a link between DPP-IV inhibitors and the development of bullous pemphigoid, a potentially fatal cutaneous autoimmune blistering disorder. The skin disease appeared after an average of 6 months on DPP-IV inhibitor therapy in their series. In most cases the bullous pemphigoid remitted in response to discontinuation of the drug, often in conjunction with a course of topical or less frequently, oral corticosteroid therapy (J Dermatol Case Rep. 2014 Mar 31;8[1]:24-8).
The mechanism for the development of bullous pemphigoid in patients on a DPP-IV inhibitor is unknown; however, the enzyme DPP-IV is expressed in skin and most other organs.
“I think a key take home is if patients in their 60s or 70s come in with pemphigoid, even though they’re in the usual age group for non–drug-induced pemphigoid, ask whether they are taking a DPP-IV inhibitor. And if they are, get it stopped,” Dr. Endo said.
An initial postmarketing flurry of case reports of angioedema in patients on the then-new DPP-IV inhibitors caused enormous concern until clarification was provided in a study by investigators at Vanderbilt University, Nashville, Tenn., and Novartis. They dove deep into the phase III randomized clinical trial data for one of these agents, vildagliptin (Galvus, manufactured by Novartis), and concluded there was no association between the drug and angioedema, except in patients simultaneously taking an ACE inhibitor, a known risk factor for angioedema. It seems that the dual therapy may cause a double hit, multiplying risk.
The bad news was that patients on an ACE inhibitor and vildagliptin had a 4.57-fold greater risk of angioedema than did those on a non–DPP-IV inhibitor comparator medication. The good news was that the absolute risk was very low: 14 confirmed cases in 2,754 subjects. And most cases of angioedema were of the non–life-threatening variety (Hypertension. 2009 Sep;54[3]:516-23).
“The evidence is really limited, but I have to agree with one expert who said, ‘Hey, if somebody comes into the hospital with angioedema, and they happen to be on a DPP-IV inhibitor and an ACE inhibitor, stop both.’ Whether or not patients can be safely rechallenged with a DPP-IV inhibitor isn’t yet known,” Dr. Endo said.
Another cutaneous side effect associated with DPP-IV inhibitor therapy is peripheral edema. It occurs in 1%-2% of treated patients and could contribute to the refractory nature of some diabetic foot ulcers, according to the dermatologist. Documented cases of photosensitivity, urticaria, and eosinophilic drug rashes have also been reported.
The DPP-IV inhibitors are oral drugs. Those approved in the United States are alogliptin (Nesina), linagliptin (Trajenta), saxagliptin (Onglyza), and sitagliptin (Januvia).
GLP-1 agonists
The chief cutaneous side effects of the glucagonlike peptide–1 receptor agonists are injection site reactions, reported in up to 20% of treated patients in some studies. These reactions are typically mild, itchy, erythematous, and transient.
The GLP-1 agonists are administered subcutaneously once or twice weekly. Those approved in the United States are albiglutide (Tanzeum), dulaglutide (Trulicity), exenatide (Byetta, Bydureon), and liraglutide (Saxenda, Victoza).
SGLT2 inhibitors
The sodium-glucose cotransporter–2 inhibitors are the newest of these three antidiabetic drug classes. They are oral agents. Their most common cutaneous side effect is candidiasis, occurring in about 10% of patients. Women and uncircumcized men are at greatest risk. Fortunately, most cases are mild, episodic, and successfully treated with topical or oral antimycotic therapy, Dr. Endo said.
The SGLT2 inhibitors approved in the United States are canagliflozin (Invokana), dapagliflozin (Farxiga), and enpagliflozin (Jardiance).
Dr. Endo reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM WCD 2015
Pushing policy makers to take skin diseases seriously
VANCOUVER – Dermatologic thought leaders worldwide have embarked upon a major international initiative aimed at making better skin health a strategic priority for politicians, health policy makers, and the general public.
The Grand Challenges in Global Skin Health Initiative, launched by the International League of Dermatological Societies, is aimed at proving the true value of dermatologic care. The impetus is a strong feeling within the dermatology community that skin diseases got a raw deal in the landmark Global Burden of Disease Study.
The Global Burden of Disease Study (Lancet. 2015 Jun 7. pii: S0140-6736(15)60692-4), funded by the Bill and Melinda Gates Foundation on behalf of the World Health Organization, ranked skin diseases far down on the list of conditions causing lost disability-adjusted life-years (DALYs) worldwide.
But DALYs as an indicator of disease burden tell only part of the story. They have a major limitation: “In the DALY concept, patients are never asked questions about the weight of their burden of disease; those questions are directed to health care professionals and the general public,” Dr. Matthias Augustin explained at the World Congress of Dermatology.
“We need to understand this because governments and other payers make use of these Global Burden of Disease data. We as dermatologists need to make sure that we are not underrepresented in the overall discussion,” said Dr. Augustin, professor of dermatology at the University of Hamburg-Eppendorf (Germany) and director of the Institute for Health Services Research in Dermatology and Nursing Professions at the university.
The true measure of value in health care needs to include patient-reported outcomes, and the Global Burden of Disease Study didn’t do that, he continued.
“There is a discrepancy between objective and subjective outcomes. Many papers have shown that the relationship between PASI scores representing severity of psoriasis and patient quality of life is very loose, if there’s any at all,” the dermatologist said.
Recently an international team of researchers analyzed the world’s published DALY data for psoriasis and concluded that this common skin disease ranked a mere 144th out of 176 conditions in this domain. The investigators argued that this metric vastly underestimates the true disease burden of psoriasis (Br J Dermatol. 2015 Jun;172(6):1665-8).
The investigators noted that the Global Burden of Disease Study treats psoriasis as a single entity consisting of psoriatic skin disease without taking into account the association with psoriatic arthritis, the increased risk of cardiovascular disease, or the enormous psychosocial sequelae of this disfiguring disease, which typically lasts for more than 40 years, or more than 60 years in individuals with childhood-onset psoriasis.
Dr. Augustin and the other founders of the Grand Challenges in Global Skin Initiative recently laid out the case for the project (Br J Dermatol. 2015 Jun;172(6):1469-72). The plan is to develop evidence-based proof of the added value of dermatologic care.
“Innovation in health care delivery has frequently ignored the needs of the whole patient and the populations in which they live. Skin disease has been a casualty in this respect,” the authors wrote. “However, perhaps the most powerful contribution to making skin health a realizable objective over the next 25 years is the recognition, among leaders of governments and nongovernmental organizations, that it is a realistic, affordable, and achievable goal, integral to future health and research strategies.”
The initial round of projects being undertaken through the initiative includes creation of a global psoriasis atlas, documentation of the adverse impact of UV exposure on outdoor workers on every continent, a centers-of-excellence program regarding aging skin, and a project addressing scabies – “a huge problem worldwide, and especially in developing countries,” Dr. Augustin noted.
“We intend to communicate our message to decision makers and let the patients speak; it’s in our common interest,” he said.
He reported having no relevant financial conflicts.
VANCOUVER – Dermatologic thought leaders worldwide have embarked upon a major international initiative aimed at making better skin health a strategic priority for politicians, health policy makers, and the general public.
The Grand Challenges in Global Skin Health Initiative, launched by the International League of Dermatological Societies, is aimed at proving the true value of dermatologic care. The impetus is a strong feeling within the dermatology community that skin diseases got a raw deal in the landmark Global Burden of Disease Study.
The Global Burden of Disease Study (Lancet. 2015 Jun 7. pii: S0140-6736(15)60692-4), funded by the Bill and Melinda Gates Foundation on behalf of the World Health Organization, ranked skin diseases far down on the list of conditions causing lost disability-adjusted life-years (DALYs) worldwide.
But DALYs as an indicator of disease burden tell only part of the story. They have a major limitation: “In the DALY concept, patients are never asked questions about the weight of their burden of disease; those questions are directed to health care professionals and the general public,” Dr. Matthias Augustin explained at the World Congress of Dermatology.
“We need to understand this because governments and other payers make use of these Global Burden of Disease data. We as dermatologists need to make sure that we are not underrepresented in the overall discussion,” said Dr. Augustin, professor of dermatology at the University of Hamburg-Eppendorf (Germany) and director of the Institute for Health Services Research in Dermatology and Nursing Professions at the university.
The true measure of value in health care needs to include patient-reported outcomes, and the Global Burden of Disease Study didn’t do that, he continued.
“There is a discrepancy between objective and subjective outcomes. Many papers have shown that the relationship between PASI scores representing severity of psoriasis and patient quality of life is very loose, if there’s any at all,” the dermatologist said.
Recently an international team of researchers analyzed the world’s published DALY data for psoriasis and concluded that this common skin disease ranked a mere 144th out of 176 conditions in this domain. The investigators argued that this metric vastly underestimates the true disease burden of psoriasis (Br J Dermatol. 2015 Jun;172(6):1665-8).
The investigators noted that the Global Burden of Disease Study treats psoriasis as a single entity consisting of psoriatic skin disease without taking into account the association with psoriatic arthritis, the increased risk of cardiovascular disease, or the enormous psychosocial sequelae of this disfiguring disease, which typically lasts for more than 40 years, or more than 60 years in individuals with childhood-onset psoriasis.
Dr. Augustin and the other founders of the Grand Challenges in Global Skin Initiative recently laid out the case for the project (Br J Dermatol. 2015 Jun;172(6):1469-72). The plan is to develop evidence-based proof of the added value of dermatologic care.
“Innovation in health care delivery has frequently ignored the needs of the whole patient and the populations in which they live. Skin disease has been a casualty in this respect,” the authors wrote. “However, perhaps the most powerful contribution to making skin health a realizable objective over the next 25 years is the recognition, among leaders of governments and nongovernmental organizations, that it is a realistic, affordable, and achievable goal, integral to future health and research strategies.”
The initial round of projects being undertaken through the initiative includes creation of a global psoriasis atlas, documentation of the adverse impact of UV exposure on outdoor workers on every continent, a centers-of-excellence program regarding aging skin, and a project addressing scabies – “a huge problem worldwide, and especially in developing countries,” Dr. Augustin noted.
“We intend to communicate our message to decision makers and let the patients speak; it’s in our common interest,” he said.
He reported having no relevant financial conflicts.
VANCOUVER – Dermatologic thought leaders worldwide have embarked upon a major international initiative aimed at making better skin health a strategic priority for politicians, health policy makers, and the general public.
The Grand Challenges in Global Skin Health Initiative, launched by the International League of Dermatological Societies, is aimed at proving the true value of dermatologic care. The impetus is a strong feeling within the dermatology community that skin diseases got a raw deal in the landmark Global Burden of Disease Study.
The Global Burden of Disease Study (Lancet. 2015 Jun 7. pii: S0140-6736(15)60692-4), funded by the Bill and Melinda Gates Foundation on behalf of the World Health Organization, ranked skin diseases far down on the list of conditions causing lost disability-adjusted life-years (DALYs) worldwide.
But DALYs as an indicator of disease burden tell only part of the story. They have a major limitation: “In the DALY concept, patients are never asked questions about the weight of their burden of disease; those questions are directed to health care professionals and the general public,” Dr. Matthias Augustin explained at the World Congress of Dermatology.
“We need to understand this because governments and other payers make use of these Global Burden of Disease data. We as dermatologists need to make sure that we are not underrepresented in the overall discussion,” said Dr. Augustin, professor of dermatology at the University of Hamburg-Eppendorf (Germany) and director of the Institute for Health Services Research in Dermatology and Nursing Professions at the university.
The true measure of value in health care needs to include patient-reported outcomes, and the Global Burden of Disease Study didn’t do that, he continued.
“There is a discrepancy between objective and subjective outcomes. Many papers have shown that the relationship between PASI scores representing severity of psoriasis and patient quality of life is very loose, if there’s any at all,” the dermatologist said.
Recently an international team of researchers analyzed the world’s published DALY data for psoriasis and concluded that this common skin disease ranked a mere 144th out of 176 conditions in this domain. The investigators argued that this metric vastly underestimates the true disease burden of psoriasis (Br J Dermatol. 2015 Jun;172(6):1665-8).
The investigators noted that the Global Burden of Disease Study treats psoriasis as a single entity consisting of psoriatic skin disease without taking into account the association with psoriatic arthritis, the increased risk of cardiovascular disease, or the enormous psychosocial sequelae of this disfiguring disease, which typically lasts for more than 40 years, or more than 60 years in individuals with childhood-onset psoriasis.
Dr. Augustin and the other founders of the Grand Challenges in Global Skin Initiative recently laid out the case for the project (Br J Dermatol. 2015 Jun;172(6):1469-72). The plan is to develop evidence-based proof of the added value of dermatologic care.
“Innovation in health care delivery has frequently ignored the needs of the whole patient and the populations in which they live. Skin disease has been a casualty in this respect,” the authors wrote. “However, perhaps the most powerful contribution to making skin health a realizable objective over the next 25 years is the recognition, among leaders of governments and nongovernmental organizations, that it is a realistic, affordable, and achievable goal, integral to future health and research strategies.”
The initial round of projects being undertaken through the initiative includes creation of a global psoriasis atlas, documentation of the adverse impact of UV exposure on outdoor workers on every continent, a centers-of-excellence program regarding aging skin, and a project addressing scabies – “a huge problem worldwide, and especially in developing countries,” Dr. Augustin noted.
“We intend to communicate our message to decision makers and let the patients speak; it’s in our common interest,” he said.
He reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM WCD 2015