User login
VIDEO: Penicillin skin testing improves inpatient antibiotic stewardship
HOUSTON– Dr. Megan S. Motosue of the Mayo Clinic in Rochester, Minn., discusses the value of penicillin skin testing as a potent tool for improving inpatient antibiotic stewardship. By routinely performing penicillin skin testing using standard methods in a consecutive series of inpatients with a self-reported history of penicillin allergy, roughly 80% were found to not in fact be allergic. And this information changed their physicians’ behavior: prior to testing, vancomycin was the most commonly used antibiotic in the inpatients, but its use was reduced by more than half based upon the skin test results, with a commensurate increase in prescriptions for semi-synthetic penicillins.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HOUSTON– Dr. Megan S. Motosue of the Mayo Clinic in Rochester, Minn., discusses the value of penicillin skin testing as a potent tool for improving inpatient antibiotic stewardship. By routinely performing penicillin skin testing using standard methods in a consecutive series of inpatients with a self-reported history of penicillin allergy, roughly 80% were found to not in fact be allergic. And this information changed their physicians’ behavior: prior to testing, vancomycin was the most commonly used antibiotic in the inpatients, but its use was reduced by more than half based upon the skin test results, with a commensurate increase in prescriptions for semi-synthetic penicillins.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HOUSTON– Dr. Megan S. Motosue of the Mayo Clinic in Rochester, Minn., discusses the value of penicillin skin testing as a potent tool for improving inpatient antibiotic stewardship. By routinely performing penicillin skin testing using standard methods in a consecutive series of inpatients with a self-reported history of penicillin allergy, roughly 80% were found to not in fact be allergic. And this information changed their physicians’ behavior: prior to testing, vancomycin was the most commonly used antibiotic in the inpatients, but its use was reduced by more than half based upon the skin test results, with a commensurate increase in prescriptions for semi-synthetic penicillins.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE 2015 AAAAI ANNUAL MEETING
Latest valvular disease guidelines bring big changes
SNOWMASS, COLO. – The 2014 American Heart Association/American College of Cardiology guidelines for the management of valvular heart disease break new ground in numerous ways, Dr. Rick A. Nishimura said at the Annual Cardiovascular Conference at Snowmass.
“We needed to do things differently. These guidelines were created in a different format from prior valvular heart disease guidelines. We wanted these guidelines to promote access to concise, relevant bytes of information at the point of care,” explained Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn., and cochair of the guidelines writing committee.
These guidelines – the first major revision in 8 years – introduce a new taxonomy and the first staging system for valvular heart disease. The guidelines also lower the threshold for intervention in asymptomatic patients, recommending surgical or catheter-based treatment at an earlier point in the disease process than ever before. And the guidelines introduce the concept of heart valve centers of excellence, offering a strong recommendation that patients be referred to those centers for procedures to be performed in the asymptomatic phase of disease (J. Am. Coll. Cardiol. 2014;63:2438-88).
These valvular heart disease guidelines place greater emphasis than before on the quality of the scientific evidence underlying recommendations. Since valvular heart disease is a field with a paucity of randomized trials, that meant cutting back.
“Our goal was, if there’s little evidence, don’t write a recommendation. So the number of recommendations went down, but at least the ones that were made were based on evidence,” the cardiologist noted.
Indeed, in the 2006 guidelines, more than 70% of the recommendations were Level of Evidence C and based solely upon expert opinion; in the new guidelines, that’s true for less than 50%. And the proportion of recommendations that are Level of Evidence B increased from 30% to 45%.
The 2014 update was prompted by huge changes in the field of valvular heart disease since 2006. For example, better data became available on the natural history of valvular heart disease. The old concept was not to operate on the asymptomatic patient with severe aortic stenosis and normal left ventricular function, but more recent natural history studies have shown that, left untreated, 72% of such patients will die or develop symptoms within 5 years.
So there has been a push to intervene earlier. Fortunately, that became doable, as recent years also brought improved noninvasive imaging, new catheter-based interventions, and refined surgical methods, enabling operators to safely lower the threshold for intervention in asymptomatic patients while at the same time extending procedural therapies to older, sicker populations.
Dr. Nishimura predicted that cardiologists and surgeons will find the new staging system clinically useful. The four stages, A-D, define the categories “at risk,” “progressive,” “asymptomatic severe,” and “symptomatic severe,” respectively. These categories are particularly helpful in determining how often to schedule patient follow-up and when to time intervention.
The guidelines recommend observation for patients who are Stage A or B and intervention when reasonable in patients who are Stage C2 or D. What bumps a patient with hemodynamically severe yet asymptomatic mitral regurgitation from Stage C1 to C2 is an left ventricular ejection fraction below 60% or a left ventricular end systolic dimension of 40 mm or more. In the setting of asymptomatic aortic stenosis, it’s a peak aortic valve velocity of 4.0 m/sec on Doppler echocardiography plus an LVEF of less than 50%.
The latest guidelines introduced the concept of heart valve centers of excellence in response to evidence of large variability across the country in terms of experience with valve operations. For example, the majority of centers perform fewer than 40 mitral valve repairs per year, and surgeons who perform mitral operations do a median of just five per year. The guideline committee, which included general and interventional cardiologists, surgeons, anesthesiologists, and imaging experts, was persuaded that those numbers are not sufficient to achieve optimal results in complex valve operations for asymptomatic patients.
The criteria for qualifying as a heart valve center of excellence, as defined in the guidelines, include having a multidisciplinary heart valve team, high patient volume, high-level surgical experience and expertise in complex valve procedures, and active participation in multicenter data registries and continuous quality improvement processes.
“The most important thing is you have to be very transparent with your data,” according to the cardiologist.
Ultimately, the most far-reaching change introduced in the current valvular heart disease guidelines is the switch from textbook format to what Dr. Nishimura calls structured data knowledge management.
“The AHA/ACC clinical practice guidelines are generally recognized as the flagship of U.S. cardiovascular medicine, but they’re like a library of old books. Clinically valuable knowledge is buried within documents that can be 200 pages long. What we need at the point of care is the gist: concise, relevant bytes of information that answer a specific clinical question, synthesized by experts,” Dr. Nishimura said.
The new approach is designed to counter the information overload that plagues contemporary medical practice. Each recommendation in the current valvular heart disease guidelines addresses a specific clinical question via a brief summary statement followed by a short explanatory paragraph, with accompanying references for those who seek additional details. This new format is designed to lead AHA/ACC clinical practice guidelines into the electronic information management future.
“In the future, you’ll go to your iPad or iPhone or whatever, type in search terms such as ‘anticoagulation for mechanical valves during pregnancy,’ and it will take you straight to the relevant knowledge byte. You can then click on ‘more’ and find out more and get to the supporting evidence tables. The knowledge chunks will be stored in a centralized knowledge management system. The nice thing about this is that it will be a living document that can easily be updated, instead of having to wait 8 years for a new version,” Dr. Nishimura explained.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – The 2014 American Heart Association/American College of Cardiology guidelines for the management of valvular heart disease break new ground in numerous ways, Dr. Rick A. Nishimura said at the Annual Cardiovascular Conference at Snowmass.
“We needed to do things differently. These guidelines were created in a different format from prior valvular heart disease guidelines. We wanted these guidelines to promote access to concise, relevant bytes of information at the point of care,” explained Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn., and cochair of the guidelines writing committee.
These guidelines – the first major revision in 8 years – introduce a new taxonomy and the first staging system for valvular heart disease. The guidelines also lower the threshold for intervention in asymptomatic patients, recommending surgical or catheter-based treatment at an earlier point in the disease process than ever before. And the guidelines introduce the concept of heart valve centers of excellence, offering a strong recommendation that patients be referred to those centers for procedures to be performed in the asymptomatic phase of disease (J. Am. Coll. Cardiol. 2014;63:2438-88).
These valvular heart disease guidelines place greater emphasis than before on the quality of the scientific evidence underlying recommendations. Since valvular heart disease is a field with a paucity of randomized trials, that meant cutting back.
“Our goal was, if there’s little evidence, don’t write a recommendation. So the number of recommendations went down, but at least the ones that were made were based on evidence,” the cardiologist noted.
Indeed, in the 2006 guidelines, more than 70% of the recommendations were Level of Evidence C and based solely upon expert opinion; in the new guidelines, that’s true for less than 50%. And the proportion of recommendations that are Level of Evidence B increased from 30% to 45%.
The 2014 update was prompted by huge changes in the field of valvular heart disease since 2006. For example, better data became available on the natural history of valvular heart disease. The old concept was not to operate on the asymptomatic patient with severe aortic stenosis and normal left ventricular function, but more recent natural history studies have shown that, left untreated, 72% of such patients will die or develop symptoms within 5 years.
So there has been a push to intervene earlier. Fortunately, that became doable, as recent years also brought improved noninvasive imaging, new catheter-based interventions, and refined surgical methods, enabling operators to safely lower the threshold for intervention in asymptomatic patients while at the same time extending procedural therapies to older, sicker populations.
Dr. Nishimura predicted that cardiologists and surgeons will find the new staging system clinically useful. The four stages, A-D, define the categories “at risk,” “progressive,” “asymptomatic severe,” and “symptomatic severe,” respectively. These categories are particularly helpful in determining how often to schedule patient follow-up and when to time intervention.
The guidelines recommend observation for patients who are Stage A or B and intervention when reasonable in patients who are Stage C2 or D. What bumps a patient with hemodynamically severe yet asymptomatic mitral regurgitation from Stage C1 to C2 is an left ventricular ejection fraction below 60% or a left ventricular end systolic dimension of 40 mm or more. In the setting of asymptomatic aortic stenosis, it’s a peak aortic valve velocity of 4.0 m/sec on Doppler echocardiography plus an LVEF of less than 50%.
The latest guidelines introduced the concept of heart valve centers of excellence in response to evidence of large variability across the country in terms of experience with valve operations. For example, the majority of centers perform fewer than 40 mitral valve repairs per year, and surgeons who perform mitral operations do a median of just five per year. The guideline committee, which included general and interventional cardiologists, surgeons, anesthesiologists, and imaging experts, was persuaded that those numbers are not sufficient to achieve optimal results in complex valve operations for asymptomatic patients.
The criteria for qualifying as a heart valve center of excellence, as defined in the guidelines, include having a multidisciplinary heart valve team, high patient volume, high-level surgical experience and expertise in complex valve procedures, and active participation in multicenter data registries and continuous quality improvement processes.
“The most important thing is you have to be very transparent with your data,” according to the cardiologist.
Ultimately, the most far-reaching change introduced in the current valvular heart disease guidelines is the switch from textbook format to what Dr. Nishimura calls structured data knowledge management.
“The AHA/ACC clinical practice guidelines are generally recognized as the flagship of U.S. cardiovascular medicine, but they’re like a library of old books. Clinically valuable knowledge is buried within documents that can be 200 pages long. What we need at the point of care is the gist: concise, relevant bytes of information that answer a specific clinical question, synthesized by experts,” Dr. Nishimura said.
The new approach is designed to counter the information overload that plagues contemporary medical practice. Each recommendation in the current valvular heart disease guidelines addresses a specific clinical question via a brief summary statement followed by a short explanatory paragraph, with accompanying references for those who seek additional details. This new format is designed to lead AHA/ACC clinical practice guidelines into the electronic information management future.
“In the future, you’ll go to your iPad or iPhone or whatever, type in search terms such as ‘anticoagulation for mechanical valves during pregnancy,’ and it will take you straight to the relevant knowledge byte. You can then click on ‘more’ and find out more and get to the supporting evidence tables. The knowledge chunks will be stored in a centralized knowledge management system. The nice thing about this is that it will be a living document that can easily be updated, instead of having to wait 8 years for a new version,” Dr. Nishimura explained.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – The 2014 American Heart Association/American College of Cardiology guidelines for the management of valvular heart disease break new ground in numerous ways, Dr. Rick A. Nishimura said at the Annual Cardiovascular Conference at Snowmass.
“We needed to do things differently. These guidelines were created in a different format from prior valvular heart disease guidelines. We wanted these guidelines to promote access to concise, relevant bytes of information at the point of care,” explained Dr. Nishimura, professor of medicine at the Mayo Clinic in Rochester, Minn., and cochair of the guidelines writing committee.
These guidelines – the first major revision in 8 years – introduce a new taxonomy and the first staging system for valvular heart disease. The guidelines also lower the threshold for intervention in asymptomatic patients, recommending surgical or catheter-based treatment at an earlier point in the disease process than ever before. And the guidelines introduce the concept of heart valve centers of excellence, offering a strong recommendation that patients be referred to those centers for procedures to be performed in the asymptomatic phase of disease (J. Am. Coll. Cardiol. 2014;63:2438-88).
These valvular heart disease guidelines place greater emphasis than before on the quality of the scientific evidence underlying recommendations. Since valvular heart disease is a field with a paucity of randomized trials, that meant cutting back.
“Our goal was, if there’s little evidence, don’t write a recommendation. So the number of recommendations went down, but at least the ones that were made were based on evidence,” the cardiologist noted.
Indeed, in the 2006 guidelines, more than 70% of the recommendations were Level of Evidence C and based solely upon expert opinion; in the new guidelines, that’s true for less than 50%. And the proportion of recommendations that are Level of Evidence B increased from 30% to 45%.
The 2014 update was prompted by huge changes in the field of valvular heart disease since 2006. For example, better data became available on the natural history of valvular heart disease. The old concept was not to operate on the asymptomatic patient with severe aortic stenosis and normal left ventricular function, but more recent natural history studies have shown that, left untreated, 72% of such patients will die or develop symptoms within 5 years.
So there has been a push to intervene earlier. Fortunately, that became doable, as recent years also brought improved noninvasive imaging, new catheter-based interventions, and refined surgical methods, enabling operators to safely lower the threshold for intervention in asymptomatic patients while at the same time extending procedural therapies to older, sicker populations.
Dr. Nishimura predicted that cardiologists and surgeons will find the new staging system clinically useful. The four stages, A-D, define the categories “at risk,” “progressive,” “asymptomatic severe,” and “symptomatic severe,” respectively. These categories are particularly helpful in determining how often to schedule patient follow-up and when to time intervention.
The guidelines recommend observation for patients who are Stage A or B and intervention when reasonable in patients who are Stage C2 or D. What bumps a patient with hemodynamically severe yet asymptomatic mitral regurgitation from Stage C1 to C2 is an left ventricular ejection fraction below 60% or a left ventricular end systolic dimension of 40 mm or more. In the setting of asymptomatic aortic stenosis, it’s a peak aortic valve velocity of 4.0 m/sec on Doppler echocardiography plus an LVEF of less than 50%.
The latest guidelines introduced the concept of heart valve centers of excellence in response to evidence of large variability across the country in terms of experience with valve operations. For example, the majority of centers perform fewer than 40 mitral valve repairs per year, and surgeons who perform mitral operations do a median of just five per year. The guideline committee, which included general and interventional cardiologists, surgeons, anesthesiologists, and imaging experts, was persuaded that those numbers are not sufficient to achieve optimal results in complex valve operations for asymptomatic patients.
The criteria for qualifying as a heart valve center of excellence, as defined in the guidelines, include having a multidisciplinary heart valve team, high patient volume, high-level surgical experience and expertise in complex valve procedures, and active participation in multicenter data registries and continuous quality improvement processes.
“The most important thing is you have to be very transparent with your data,” according to the cardiologist.
Ultimately, the most far-reaching change introduced in the current valvular heart disease guidelines is the switch from textbook format to what Dr. Nishimura calls structured data knowledge management.
“The AHA/ACC clinical practice guidelines are generally recognized as the flagship of U.S. cardiovascular medicine, but they’re like a library of old books. Clinically valuable knowledge is buried within documents that can be 200 pages long. What we need at the point of care is the gist: concise, relevant bytes of information that answer a specific clinical question, synthesized by experts,” Dr. Nishimura said.
The new approach is designed to counter the information overload that plagues contemporary medical practice. Each recommendation in the current valvular heart disease guidelines addresses a specific clinical question via a brief summary statement followed by a short explanatory paragraph, with accompanying references for those who seek additional details. This new format is designed to lead AHA/ACC clinical practice guidelines into the electronic information management future.
“In the future, you’ll go to your iPad or iPhone or whatever, type in search terms such as ‘anticoagulation for mechanical valves during pregnancy,’ and it will take you straight to the relevant knowledge byte. You can then click on ‘more’ and find out more and get to the supporting evidence tables. The knowledge chunks will be stored in a centralized knowledge management system. The nice thing about this is that it will be a living document that can easily be updated, instead of having to wait 8 years for a new version,” Dr. Nishimura explained.
He reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Tide turns in favor of multivessel PCI in STEMI
SNOWMASS, COLO. – Recent data seem to refute the 2013 American Heart Association/American College of Cardiology class III recommendation to avoid multivessel percutaneous coronary intervention at the time of primary PCI for ST-elevation MI, Dr. David R. Holmes Jr. observed at the Annual Cardiovascular Conference at Snowmass.
“The current AHA/ACC guidelines for STEMI should be and are being reevaluated regarding clarifications for the indications and timing of non–infarct artery revascularization,” according to Dr. Holmes, a cardiologist at the Mayo Clinic in Rochester, Minn., and an ACC past president.
Indeed, the ACC has already withdrawn from its ‘Choosing Wisely’ campaign its former recommendation discouraging multivessel revascularization at the time of primary PCI for STEMI. The college cited “new science showing that complete revascularization of all significant blocked arteries leads to better outcomes in some heart attack patients.”
Dr. Holmes was coauthor of a meta-analysis of 4 prospective and 14 retrospective studies involving more than 40,000 patients that concluded multivessel PCI for STEMI should be discouraged, and that significant nonculprit lesions should only be treated during staged procedures (J. Am. Coll. Cardiol. 2011;58:692-703). This meta-analysis was influential in the creation of the class III ‘don’t do it’ recommendation in the AHA/ACC guidelines. But Dr. Holmes said that in hindsight, the data included in the meta-analysis were something of a mishmash and “wound up being very hard to interpret.”
Greater clarity has been brought by two more recent randomized trials: PRAMI and CvLPRIT. Both were relatively small by cardiology standards, but they ended up showing similarly striking advantages in favor of using the STEMI hospitalization to perform preventive PCI of both the infarct-related artery and non–infarct arteries with major stenoses.
PRAMI included 465 acute STEMI patients who underwent infarct artery PCI and were then randomized to preventive PCI or infarct artery–only PCI. At a mean follow-up of 23 months, the preventive multivessel PCI group had a 65% reduction in the relative risk of the primary outcome, a composite of cardiac death, nonfatal MI, or refractory angina (N. Engl. J. Med. 2013;369:1115-23).
The yet-to-be-published CvLPRIT study was presented at the 2014 European Society of Cardiology meeting in Barcelona. The multicenter study included 296 STEMI patients with angiographically established significant multivessel disease who were randomized to primary PCI of the culprit vessel only or to complete revascularization. The primary outcome, the 12-month composite of all-cause mortality, recurrent MI, heart failure, or ischemia-driven revascularization, occurred in 10% of the complete revascularization group, compared with 21.2% of patients assigned to culprit artery–only PCI.
Also at the ESC conference, CvLPRIT investigator Dr. Anthony Gershlick of the University of Leicester (England) presented a meta-analysis combining the weighted results of PRAMI, CvLPRIT, and two earlier randomized trials: HELP AMI (Int. J. Cardiovasc. Intervent. 2004;6:128-33) and an Italian trial (Heart 2010;96:662-7). The results strongly favored multivessel PCI, with a 45% reduction in mortality and a 61% decrease in recurrent MI, compared with culprit vessel–only PCI at the time of admission for STEMI.
“Maybe there aren’t any innocent bystanders,” commented Dr. Holmes. “Maybe if you have somebody who has multivessel disease and you see something you think might be an innocent bystander but is a significant lesion, maybe it’s not so innocent. Maybe by treating them all at the time of the initial intervention the patient is going to do better.”
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Recent data seem to refute the 2013 American Heart Association/American College of Cardiology class III recommendation to avoid multivessel percutaneous coronary intervention at the time of primary PCI for ST-elevation MI, Dr. David R. Holmes Jr. observed at the Annual Cardiovascular Conference at Snowmass.
“The current AHA/ACC guidelines for STEMI should be and are being reevaluated regarding clarifications for the indications and timing of non–infarct artery revascularization,” according to Dr. Holmes, a cardiologist at the Mayo Clinic in Rochester, Minn., and an ACC past president.
Indeed, the ACC has already withdrawn from its ‘Choosing Wisely’ campaign its former recommendation discouraging multivessel revascularization at the time of primary PCI for STEMI. The college cited “new science showing that complete revascularization of all significant blocked arteries leads to better outcomes in some heart attack patients.”
Dr. Holmes was coauthor of a meta-analysis of 4 prospective and 14 retrospective studies involving more than 40,000 patients that concluded multivessel PCI for STEMI should be discouraged, and that significant nonculprit lesions should only be treated during staged procedures (J. Am. Coll. Cardiol. 2011;58:692-703). This meta-analysis was influential in the creation of the class III ‘don’t do it’ recommendation in the AHA/ACC guidelines. But Dr. Holmes said that in hindsight, the data included in the meta-analysis were something of a mishmash and “wound up being very hard to interpret.”
Greater clarity has been brought by two more recent randomized trials: PRAMI and CvLPRIT. Both were relatively small by cardiology standards, but they ended up showing similarly striking advantages in favor of using the STEMI hospitalization to perform preventive PCI of both the infarct-related artery and non–infarct arteries with major stenoses.
PRAMI included 465 acute STEMI patients who underwent infarct artery PCI and were then randomized to preventive PCI or infarct artery–only PCI. At a mean follow-up of 23 months, the preventive multivessel PCI group had a 65% reduction in the relative risk of the primary outcome, a composite of cardiac death, nonfatal MI, or refractory angina (N. Engl. J. Med. 2013;369:1115-23).
The yet-to-be-published CvLPRIT study was presented at the 2014 European Society of Cardiology meeting in Barcelona. The multicenter study included 296 STEMI patients with angiographically established significant multivessel disease who were randomized to primary PCI of the culprit vessel only or to complete revascularization. The primary outcome, the 12-month composite of all-cause mortality, recurrent MI, heart failure, or ischemia-driven revascularization, occurred in 10% of the complete revascularization group, compared with 21.2% of patients assigned to culprit artery–only PCI.
Also at the ESC conference, CvLPRIT investigator Dr. Anthony Gershlick of the University of Leicester (England) presented a meta-analysis combining the weighted results of PRAMI, CvLPRIT, and two earlier randomized trials: HELP AMI (Int. J. Cardiovasc. Intervent. 2004;6:128-33) and an Italian trial (Heart 2010;96:662-7). The results strongly favored multivessel PCI, with a 45% reduction in mortality and a 61% decrease in recurrent MI, compared with culprit vessel–only PCI at the time of admission for STEMI.
“Maybe there aren’t any innocent bystanders,” commented Dr. Holmes. “Maybe if you have somebody who has multivessel disease and you see something you think might be an innocent bystander but is a significant lesion, maybe it’s not so innocent. Maybe by treating them all at the time of the initial intervention the patient is going to do better.”
He reported having no financial conflicts of interest regarding his presentation.
SNOWMASS, COLO. – Recent data seem to refute the 2013 American Heart Association/American College of Cardiology class III recommendation to avoid multivessel percutaneous coronary intervention at the time of primary PCI for ST-elevation MI, Dr. David R. Holmes Jr. observed at the Annual Cardiovascular Conference at Snowmass.
“The current AHA/ACC guidelines for STEMI should be and are being reevaluated regarding clarifications for the indications and timing of non–infarct artery revascularization,” according to Dr. Holmes, a cardiologist at the Mayo Clinic in Rochester, Minn., and an ACC past president.
Indeed, the ACC has already withdrawn from its ‘Choosing Wisely’ campaign its former recommendation discouraging multivessel revascularization at the time of primary PCI for STEMI. The college cited “new science showing that complete revascularization of all significant blocked arteries leads to better outcomes in some heart attack patients.”
Dr. Holmes was coauthor of a meta-analysis of 4 prospective and 14 retrospective studies involving more than 40,000 patients that concluded multivessel PCI for STEMI should be discouraged, and that significant nonculprit lesions should only be treated during staged procedures (J. Am. Coll. Cardiol. 2011;58:692-703). This meta-analysis was influential in the creation of the class III ‘don’t do it’ recommendation in the AHA/ACC guidelines. But Dr. Holmes said that in hindsight, the data included in the meta-analysis were something of a mishmash and “wound up being very hard to interpret.”
Greater clarity has been brought by two more recent randomized trials: PRAMI and CvLPRIT. Both were relatively small by cardiology standards, but they ended up showing similarly striking advantages in favor of using the STEMI hospitalization to perform preventive PCI of both the infarct-related artery and non–infarct arteries with major stenoses.
PRAMI included 465 acute STEMI patients who underwent infarct artery PCI and were then randomized to preventive PCI or infarct artery–only PCI. At a mean follow-up of 23 months, the preventive multivessel PCI group had a 65% reduction in the relative risk of the primary outcome, a composite of cardiac death, nonfatal MI, or refractory angina (N. Engl. J. Med. 2013;369:1115-23).
The yet-to-be-published CvLPRIT study was presented at the 2014 European Society of Cardiology meeting in Barcelona. The multicenter study included 296 STEMI patients with angiographically established significant multivessel disease who were randomized to primary PCI of the culprit vessel only or to complete revascularization. The primary outcome, the 12-month composite of all-cause mortality, recurrent MI, heart failure, or ischemia-driven revascularization, occurred in 10% of the complete revascularization group, compared with 21.2% of patients assigned to culprit artery–only PCI.
Also at the ESC conference, CvLPRIT investigator Dr. Anthony Gershlick of the University of Leicester (England) presented a meta-analysis combining the weighted results of PRAMI, CvLPRIT, and two earlier randomized trials: HELP AMI (Int. J. Cardiovasc. Intervent. 2004;6:128-33) and an Italian trial (Heart 2010;96:662-7). The results strongly favored multivessel PCI, with a 45% reduction in mortality and a 61% decrease in recurrent MI, compared with culprit vessel–only PCI at the time of admission for STEMI.
“Maybe there aren’t any innocent bystanders,” commented Dr. Holmes. “Maybe if you have somebody who has multivessel disease and you see something you think might be an innocent bystander but is a significant lesion, maybe it’s not so innocent. Maybe by treating them all at the time of the initial intervention the patient is going to do better.”
He reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Hybrid revascularization remains a rare bird
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
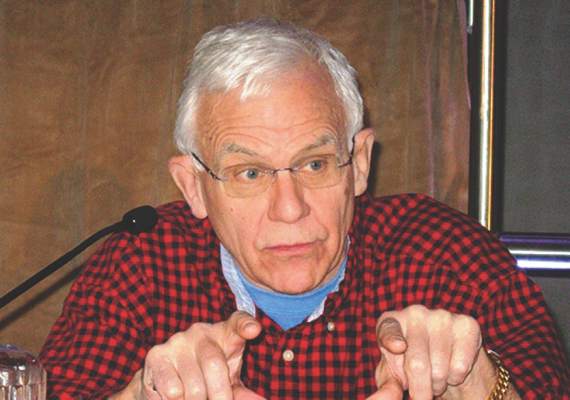
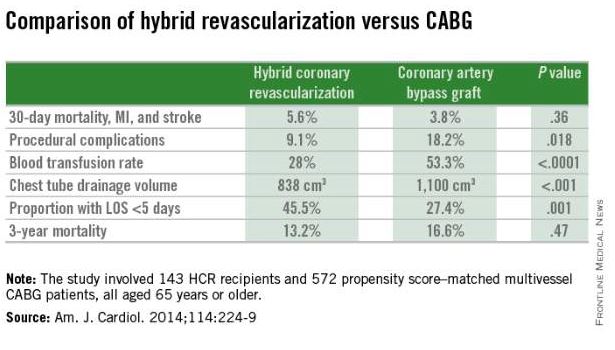
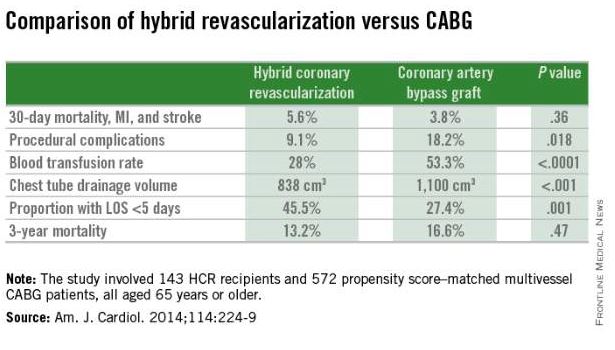
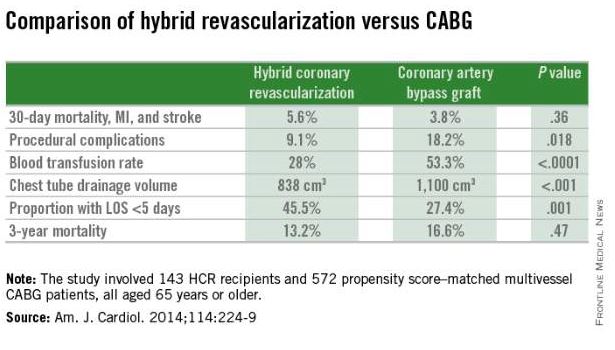
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
SNOWMASS, COLO. – For all the talk of embracing the heart team approach to coronary revascularization as the new standard, emphasizing interdisciplinary collaboration between cardiologists and surgeons, hybrid coronary revascularization remains a rarely employed strategy.
Hybrid coronary revascularization (HCR) is performed at one-third of U.S. centers providing coronary artery bypass graft (CABG) surgery, but that’s a misleading statistic. A mere handful of the centers have extensive experience with this strategy, according to the first nationwide assessment of HCR in patients with multivessel coronary artery disease.
“Only a very few centers – maybe 5 or 10 – do hybrid procedures as 8%-10% of their volume,” Dr. Vinod H. Thourani* said at the Annual Cardiovascular Conference at Snowmass.
He was a coinvestigator in the analysis of nearly 200,000 CABG procedures in the Society of Thoracic Surgeons (STS) national database for 2011-2013. Hybrid coronary revascularization – a combination of surgical and percutaneous techniques coupling minimally invasive bypass of the left anterior descending (LAD) coronary artery using an internal mammary artery graft along with drug-eluting stents for non-LAD lesions – accounted for just 0.48% of total CABG volume. And no trend for growth in the HCR approach was evident during the study period.
Moreover, even in the one-third of U.S. CABG centers that performed hybrid coronary revascularization, the strategy was used on average in less than 1% of all CABG procedures (Circulation 2014;130:872-9), noted Dr. Thourani, professor of cardiothoracic surgery and codirector of the Structural Heart and Valve Center at Emory University, Atlanta.
In contrast, he and his Emory colleagues have fully embraced HCR. At Emory, even as the annual number of primary isolated CABG procedures with sternotomy fell by 44% from 2005 to 2012, there was a compensatory increase in the number of HCRs.
“We’ve actually maintained our coronary bypass volume based on introducing HCR, unlike a lot of programs,” according to the surgeon.
The appeal of HCR is that it combines the durability of the internal mammary artery-to-LAD graft – long recognized as the main source of the survival advantage CABG holds over percutaneous interventions – with drug-eluting stents as a less invasive alternative to often-unreliable vein grafts in non-LAD target vessels.
The current American College of Cardiology/American Heart Association guidelines on coronary revascularization give HCR a favorable class IIa recommendation. However, since there are few data on clinical outcomes with HCR versus conventional CABG, Dr. Thourani and his coinvestigators compared in-hospital outcomes in the STS database. They found that after adjustment for the higher cardiovascular risk profiles present in patients undergoing HCR, the rates of in-hospital mortality and major morbidity in the two groups were similar, suggesting HCR may offer an equally safe alternative to CABG in selected patients.
Patients want less invasive alternatives to CABG with sternotomy. The three most common minimally invasive, sternal-sparing approaches are minimally invasive direct coronary artery bypass, or MIDCAB; robotic-assisted totally endoscopic coronary artery bypass, or TECAB; and robotic-assisted coronary artery bypass, a favored approach at Emory. In robotic-assisted coronary artery bypass, the harvest of the left internal mammary artery, pericardiotomy, and targeting of the LAD are accomplished with robotic assistance, but the anastomosis is hand sewn under direct vision, off pump, via a non–rib-spreading 3- to 4-cm minithoracotomy.
In a report on 307 consecutive patients who underwent robotic-assisted CABG at the university, including 159 who had HCR for multivessel disease, short-term clinical and angiographic outcomes were excellent (J. Thorac. Cardiovasc. Surg. 2014;147:179-85). Particularly striking, in Dr. Thourani’s view, was that only one postoperative stroke occurred, for a 0.3% incidence. That’s a far lower rate than typical with CABG with vein grafts.
In a more recent, as-yet-unpublished update including 477 consecutive HCR patients at Emory, the stroke rate remained extraordinarily low at 0.2%, he said.
“You can almost eliminate stroke with this procedure,” according to Dr. Thourani.
Thirty-day mortality was 0.8%, with an MI rate of 1.0%, a 3.8% incidence of conversion to sternotomy, and a 1.9% repeat revascularization rate. The rate of Fitzgibbon A patency was 96.2%, he noted.
“Return to work is really at the patient’s discretion. We tell them, ‘when you don’t hurt, you can go back.’ Some people go back 4-5 days after surgery. And there are really zero limitations for the patient – none whatsoever,” the surgeon said.
The HCR approach to multivessel revascularization appears to be particularly advantageous in diabetic patients and in older individuals. In a retrospective, nonrandomized single-center comparison of 143 HCR recipients who were propensity score matched to 572 patients who underwent multivessel CABG (Am. J. Cardiol. 2014;114:224-9), the HCR recipients had significantly fewer procedural complications, faster recovery, and similar 3-year mortality (see graphic).
Dr. Thourani said that because of the dirth of randomized trials data, it must be conceded that there is equipoise at present regarding the most effective treatment strategy in patients with multivessel coronary disease. The options are CABG with left internal mammary artery and vein grafts, HCR, medical management, multivessel percutaneous coronary intervention (PCI), and multiarterial CABG. But he added that the available evidence, while not definitive, does point the way forward.
“As we move into 2015 and the future, I think we should be doing less of the left intermal mammary artery with vein grafts, potentially less of the medical therapy, and I think we need to do a lot more multiarterial grafts if we think patients need to be opened up with a sternotomy. And if we don’t think they need to be opened up, we need to think very strongly about hybrid revascularization instead of multivessel PCI, especially in patients who are diabetic or old,” according to the surgeon.
Dr. Thourani reported serving as a consultant to Edwards Lifesciences and St. Jude Medical and receiving research grants from Abbott, Boston Scientific, Medtronic, and Sorin.
*Clarification, 4/20/2015: Dr. Vinod H. Thourani wishes to clarify that, as he stated in his presentation, the current work he reported on from Emory University was performed by Dr. Michael Halkos, who is the leader of hybrid revascularization at Emory, and that Dr. Halkos was lead author and researcher in several of the other studies reported upon.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Emergency department holds key to early readmissions for heart failure
SNOWMASS, COLO. – Under intense fiscal pressure to curb early hospital readmissions for heart failure, cardiologists and hospital administrators are taking a hard look at the traditional role of the emergency department as the point of triage for patients with decompensated heart failure.
“Alternatives to the emergency department for ambulatory triage and intervention are essential,” Dr. Akshay Desai said at the Annual Cardiovascular Conference at Snowmass.
“Traditionally, when our patients become decompensated, we send them from our office or clinic to the ED. And 80%-90% of those who present to the ED with the diagnosis of heart failure are admitted to the hospital. So this means that the ED is a pretty ineffective triage point for heart failure patients. Most ED staff are concerned about ambulatory follow-up and feel it’s safer to follow patients in the hospital. The message here is we need a more robust ambulatory framework to manage patients with milder decompensation so they don’t all need to come into the hospital,” said Dr. Desai of Brigham and Women’s Hospital and Harvard Medical School, Boston.
Hospital admission is of questionable value for a large fraction of decompensating heart failure patients. After all, not that much happens to them in the hospital that couldn’t take place in a less costly setting.
“For the most part, our patients in the hospital for decompensated heart failure get IV diuretics, with an average weight loss of about 4 kg. Surveillance is typically once- or twice-daily laboratory tests and a bedside clinical visit by a physician at 7:30 in the morning. Few patients get much else. There’s little diagnostic testing, few other therapies that require intensive monitoring, and most patients feel a little better by their first day in the hospital,” he said.
This suggests the need for what he called “an evolved model of heart failure care” in which the ED is replaced as the point of service by some form of ambulatory center that can serve as a buffer limiting the number of patients who need to come into the hospital.
“It could be a home-based strategy of IV diuretic administration, a clinic-based strategy of outpatient diuretic administration, or an observation unit based in the ED. All of these are now being tested in various models across the country as alternatives to help manage the readmission problem, and also to make life better for our patients, who’d prefer not to be in the hospital if they could be managed in other ways,” Dr. Desai continued.
Reducing 30-day readmission rates after a hospitalization for heart failure is seen by health policy makers as an opportunity to simultaneously improve care and reduce costs. But studies show only about half of readmissions in patients with heart failure are cardiovascular related, just half of those cardiovascular readmissions are heart failure related, and only about 30% of heart failure readmissions are truly preventable. However, wide variation exists across the country in risk-adjusted 30-day readmission rates, suggesting there is an opportunity for improvement in outlier hospitals.
Numerous factors have been linked to high heart failure readmission rates, including patient sociodemographic characteristics, comorbid conditions, and serum markers of heart failure severity. One underappreciated factor, in Dr. Desai’s view, is that readmission rates are significantly higher in hospitals that are financially and clinically resource poor, as shown in a Harvard School of Public Health analysis of Medicare claims data for more than 900,000 heart failure discharges. These resource-poor hospitals provide care for underserved populations, and they are experiencing a disproportionate burden of the financial penalties imposed for early readmission.
“As we seek to improve care for patients with heart failure, we should ensure that penalties for poor performance do not worsen disparities in quality of care,” according to the Harvard investigators (Circ. Cardiovasc. Qual. Outcomes 2011;4:53-9).
Dr. Desai reported serving as a consultant to 5AM Ventures, AtCor Medical, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – Under intense fiscal pressure to curb early hospital readmissions for heart failure, cardiologists and hospital administrators are taking a hard look at the traditional role of the emergency department as the point of triage for patients with decompensated heart failure.
“Alternatives to the emergency department for ambulatory triage and intervention are essential,” Dr. Akshay Desai said at the Annual Cardiovascular Conference at Snowmass.
“Traditionally, when our patients become decompensated, we send them from our office or clinic to the ED. And 80%-90% of those who present to the ED with the diagnosis of heart failure are admitted to the hospital. So this means that the ED is a pretty ineffective triage point for heart failure patients. Most ED staff are concerned about ambulatory follow-up and feel it’s safer to follow patients in the hospital. The message here is we need a more robust ambulatory framework to manage patients with milder decompensation so they don’t all need to come into the hospital,” said Dr. Desai of Brigham and Women’s Hospital and Harvard Medical School, Boston.
Hospital admission is of questionable value for a large fraction of decompensating heart failure patients. After all, not that much happens to them in the hospital that couldn’t take place in a less costly setting.
“For the most part, our patients in the hospital for decompensated heart failure get IV diuretics, with an average weight loss of about 4 kg. Surveillance is typically once- or twice-daily laboratory tests and a bedside clinical visit by a physician at 7:30 in the morning. Few patients get much else. There’s little diagnostic testing, few other therapies that require intensive monitoring, and most patients feel a little better by their first day in the hospital,” he said.
This suggests the need for what he called “an evolved model of heart failure care” in which the ED is replaced as the point of service by some form of ambulatory center that can serve as a buffer limiting the number of patients who need to come into the hospital.
“It could be a home-based strategy of IV diuretic administration, a clinic-based strategy of outpatient diuretic administration, or an observation unit based in the ED. All of these are now being tested in various models across the country as alternatives to help manage the readmission problem, and also to make life better for our patients, who’d prefer not to be in the hospital if they could be managed in other ways,” Dr. Desai continued.
Reducing 30-day readmission rates after a hospitalization for heart failure is seen by health policy makers as an opportunity to simultaneously improve care and reduce costs. But studies show only about half of readmissions in patients with heart failure are cardiovascular related, just half of those cardiovascular readmissions are heart failure related, and only about 30% of heart failure readmissions are truly preventable. However, wide variation exists across the country in risk-adjusted 30-day readmission rates, suggesting there is an opportunity for improvement in outlier hospitals.
Numerous factors have been linked to high heart failure readmission rates, including patient sociodemographic characteristics, comorbid conditions, and serum markers of heart failure severity. One underappreciated factor, in Dr. Desai’s view, is that readmission rates are significantly higher in hospitals that are financially and clinically resource poor, as shown in a Harvard School of Public Health analysis of Medicare claims data for more than 900,000 heart failure discharges. These resource-poor hospitals provide care for underserved populations, and they are experiencing a disproportionate burden of the financial penalties imposed for early readmission.
“As we seek to improve care for patients with heart failure, we should ensure that penalties for poor performance do not worsen disparities in quality of care,” according to the Harvard investigators (Circ. Cardiovasc. Qual. Outcomes 2011;4:53-9).
Dr. Desai reported serving as a consultant to 5AM Ventures, AtCor Medical, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – Under intense fiscal pressure to curb early hospital readmissions for heart failure, cardiologists and hospital administrators are taking a hard look at the traditional role of the emergency department as the point of triage for patients with decompensated heart failure.
“Alternatives to the emergency department for ambulatory triage and intervention are essential,” Dr. Akshay Desai said at the Annual Cardiovascular Conference at Snowmass.
“Traditionally, when our patients become decompensated, we send them from our office or clinic to the ED. And 80%-90% of those who present to the ED with the diagnosis of heart failure are admitted to the hospital. So this means that the ED is a pretty ineffective triage point for heart failure patients. Most ED staff are concerned about ambulatory follow-up and feel it’s safer to follow patients in the hospital. The message here is we need a more robust ambulatory framework to manage patients with milder decompensation so they don’t all need to come into the hospital,” said Dr. Desai of Brigham and Women’s Hospital and Harvard Medical School, Boston.
Hospital admission is of questionable value for a large fraction of decompensating heart failure patients. After all, not that much happens to them in the hospital that couldn’t take place in a less costly setting.
“For the most part, our patients in the hospital for decompensated heart failure get IV diuretics, with an average weight loss of about 4 kg. Surveillance is typically once- or twice-daily laboratory tests and a bedside clinical visit by a physician at 7:30 in the morning. Few patients get much else. There’s little diagnostic testing, few other therapies that require intensive monitoring, and most patients feel a little better by their first day in the hospital,” he said.
This suggests the need for what he called “an evolved model of heart failure care” in which the ED is replaced as the point of service by some form of ambulatory center that can serve as a buffer limiting the number of patients who need to come into the hospital.
“It could be a home-based strategy of IV diuretic administration, a clinic-based strategy of outpatient diuretic administration, or an observation unit based in the ED. All of these are now being tested in various models across the country as alternatives to help manage the readmission problem, and also to make life better for our patients, who’d prefer not to be in the hospital if they could be managed in other ways,” Dr. Desai continued.
Reducing 30-day readmission rates after a hospitalization for heart failure is seen by health policy makers as an opportunity to simultaneously improve care and reduce costs. But studies show only about half of readmissions in patients with heart failure are cardiovascular related, just half of those cardiovascular readmissions are heart failure related, and only about 30% of heart failure readmissions are truly preventable. However, wide variation exists across the country in risk-adjusted 30-day readmission rates, suggesting there is an opportunity for improvement in outlier hospitals.
Numerous factors have been linked to high heart failure readmission rates, including patient sociodemographic characteristics, comorbid conditions, and serum markers of heart failure severity. One underappreciated factor, in Dr. Desai’s view, is that readmission rates are significantly higher in hospitals that are financially and clinically resource poor, as shown in a Harvard School of Public Health analysis of Medicare claims data for more than 900,000 heart failure discharges. These resource-poor hospitals provide care for underserved populations, and they are experiencing a disproportionate burden of the financial penalties imposed for early readmission.
“As we seek to improve care for patients with heart failure, we should ensure that penalties for poor performance do not worsen disparities in quality of care,” according to the Harvard investigators (Circ. Cardiovasc. Qual. Outcomes 2011;4:53-9).
Dr. Desai reported serving as a consultant to 5AM Ventures, AtCor Medical, Novartis, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Acute anterior uveitis? Consider axial spondyloarthritis
SNOWMASS, COLO. – Ankylosing spondylitis, far and away, is the most common systemic disease in North America associated with uveitis, Dr. James T. Rosenbaum said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
The uveitis associated with ankylosing spondylitis and other HLA-B27-positive axial spondyloarthropathies is highly distinctive: It’s an anterior uveitis, meaning it occurs in front of the lens. It is sudden in onset, unilateral, often recurs in the opposite eye, and it resolves completely between attacks within several months. Also, it is associated with reduced intraocular pressure, according to Dr. Rosenbaum, professor of inflammatory diseases and chief of the division of arthritis and rheumatic diseases at Oregon Health & Science University and chief of ophthalmology at the Devers Eye Institute in Portland, Ore.
The differential diagnosis for a red eye is extensive. It includes conjunctivitis, scleritis, episcleritis, keratitis, and acute closed angle glaucoma, as well as anterior uveitis. But the only cause of a red eye that results in a constricted pupil is a sudden-onset acute anterior uveitis, he noted.
A patient with acute anterior uveitis has a 50% likelihood of being HLA-B27-positive. And a B27-positive patient with acute anterior uveitis and inflammatory back pain has nearly a 90% chance of having a spondyloarthropathy. Roughly half of these individuals meet diagnostic criteria for ankylosing spondylitis, and another 40% fulfill the Assessment of Spondyloarthritis International Society definition of spondyloarthritis, which doesn’t require definite evidence of inflammation of the sacroiliac joints on plain x-rays. An analysis of National Health and Nutrition Examination Survey data showed that 1% of U.S. adults have axial spondyloarthritis (Arthritis Care Res. 2012;64:905-10).
Yet in Dr. Rosenbaum’s experience, two-thirds of patients who present with HLA-B27-positive, unilateral, sudden-onset acute anterior uveitis have no idea that their inflammatory low back pain is a manifestation of ankylosing spondylitis or axial spondyloarthritis.
“Back pain is so endemic in our society that it’s rarely realized that the chronic back inflammation is related to the eye disease,” he observed.
Dr. Rosenbaum said that for most nonophthalmologists, uveitis flies under the radar.
“Most people don’t know what it is, but uveitis actually accounts for about 10% of all cases of blindness. And it’s a disease that often occurs in the prime of life, unlike macular degeneration or blindness due to diabetes,” he continued.
His uveitis treatment ladder starts with topical corticosteroids, which are often quite effective for anterior uveitis. Second-line therapy consists of periocular or intravitreal steroid injections, “just like you’d inject a shoulder or knee.” Oral corticosteroids are effective, but their long-term use is problematic, so Dr. Rosenbaum will quickly switch to an antimetabolite, with methotrexate his top choice.
“I would never use a TNF inhibitor to treat spondyloarthropathy-associated acute anterior uveitis per se, because this type of uveitis is typically short lived. As a practical matter, by the time I got approval from the third-party payer the uveitis would be gone. But if a patient is having recurrent severe episodes of uveitis, a TNF inhibitor will reduce the intensity and frequency of those flares. So will sulfasalazine. Methotrexate will, too, but it doesn’t affect the spondyloarthropathy,” he said.
Dr. Rosenbaum reported receiving consulting fees from a dozen pharmaceutical companies and research grants from AbbVie, Eyegate, Genentech, and Psivida.
SNOWMASS, COLO. – Ankylosing spondylitis, far and away, is the most common systemic disease in North America associated with uveitis, Dr. James T. Rosenbaum said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
The uveitis associated with ankylosing spondylitis and other HLA-B27-positive axial spondyloarthropathies is highly distinctive: It’s an anterior uveitis, meaning it occurs in front of the lens. It is sudden in onset, unilateral, often recurs in the opposite eye, and it resolves completely between attacks within several months. Also, it is associated with reduced intraocular pressure, according to Dr. Rosenbaum, professor of inflammatory diseases and chief of the division of arthritis and rheumatic diseases at Oregon Health & Science University and chief of ophthalmology at the Devers Eye Institute in Portland, Ore.
The differential diagnosis for a red eye is extensive. It includes conjunctivitis, scleritis, episcleritis, keratitis, and acute closed angle glaucoma, as well as anterior uveitis. But the only cause of a red eye that results in a constricted pupil is a sudden-onset acute anterior uveitis, he noted.
A patient with acute anterior uveitis has a 50% likelihood of being HLA-B27-positive. And a B27-positive patient with acute anterior uveitis and inflammatory back pain has nearly a 90% chance of having a spondyloarthropathy. Roughly half of these individuals meet diagnostic criteria for ankylosing spondylitis, and another 40% fulfill the Assessment of Spondyloarthritis International Society definition of spondyloarthritis, which doesn’t require definite evidence of inflammation of the sacroiliac joints on plain x-rays. An analysis of National Health and Nutrition Examination Survey data showed that 1% of U.S. adults have axial spondyloarthritis (Arthritis Care Res. 2012;64:905-10).
Yet in Dr. Rosenbaum’s experience, two-thirds of patients who present with HLA-B27-positive, unilateral, sudden-onset acute anterior uveitis have no idea that their inflammatory low back pain is a manifestation of ankylosing spondylitis or axial spondyloarthritis.
“Back pain is so endemic in our society that it’s rarely realized that the chronic back inflammation is related to the eye disease,” he observed.
Dr. Rosenbaum said that for most nonophthalmologists, uveitis flies under the radar.
“Most people don’t know what it is, but uveitis actually accounts for about 10% of all cases of blindness. And it’s a disease that often occurs in the prime of life, unlike macular degeneration or blindness due to diabetes,” he continued.
His uveitis treatment ladder starts with topical corticosteroids, which are often quite effective for anterior uveitis. Second-line therapy consists of periocular or intravitreal steroid injections, “just like you’d inject a shoulder or knee.” Oral corticosteroids are effective, but their long-term use is problematic, so Dr. Rosenbaum will quickly switch to an antimetabolite, with methotrexate his top choice.
“I would never use a TNF inhibitor to treat spondyloarthropathy-associated acute anterior uveitis per se, because this type of uveitis is typically short lived. As a practical matter, by the time I got approval from the third-party payer the uveitis would be gone. But if a patient is having recurrent severe episodes of uveitis, a TNF inhibitor will reduce the intensity and frequency of those flares. So will sulfasalazine. Methotrexate will, too, but it doesn’t affect the spondyloarthropathy,” he said.
Dr. Rosenbaum reported receiving consulting fees from a dozen pharmaceutical companies and research grants from AbbVie, Eyegate, Genentech, and Psivida.
SNOWMASS, COLO. – Ankylosing spondylitis, far and away, is the most common systemic disease in North America associated with uveitis, Dr. James T. Rosenbaum said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
The uveitis associated with ankylosing spondylitis and other HLA-B27-positive axial spondyloarthropathies is highly distinctive: It’s an anterior uveitis, meaning it occurs in front of the lens. It is sudden in onset, unilateral, often recurs in the opposite eye, and it resolves completely between attacks within several months. Also, it is associated with reduced intraocular pressure, according to Dr. Rosenbaum, professor of inflammatory diseases and chief of the division of arthritis and rheumatic diseases at Oregon Health & Science University and chief of ophthalmology at the Devers Eye Institute in Portland, Ore.
The differential diagnosis for a red eye is extensive. It includes conjunctivitis, scleritis, episcleritis, keratitis, and acute closed angle glaucoma, as well as anterior uveitis. But the only cause of a red eye that results in a constricted pupil is a sudden-onset acute anterior uveitis, he noted.
A patient with acute anterior uveitis has a 50% likelihood of being HLA-B27-positive. And a B27-positive patient with acute anterior uveitis and inflammatory back pain has nearly a 90% chance of having a spondyloarthropathy. Roughly half of these individuals meet diagnostic criteria for ankylosing spondylitis, and another 40% fulfill the Assessment of Spondyloarthritis International Society definition of spondyloarthritis, which doesn’t require definite evidence of inflammation of the sacroiliac joints on plain x-rays. An analysis of National Health and Nutrition Examination Survey data showed that 1% of U.S. adults have axial spondyloarthritis (Arthritis Care Res. 2012;64:905-10).
Yet in Dr. Rosenbaum’s experience, two-thirds of patients who present with HLA-B27-positive, unilateral, sudden-onset acute anterior uveitis have no idea that their inflammatory low back pain is a manifestation of ankylosing spondylitis or axial spondyloarthritis.
“Back pain is so endemic in our society that it’s rarely realized that the chronic back inflammation is related to the eye disease,” he observed.
Dr. Rosenbaum said that for most nonophthalmologists, uveitis flies under the radar.
“Most people don’t know what it is, but uveitis actually accounts for about 10% of all cases of blindness. And it’s a disease that often occurs in the prime of life, unlike macular degeneration or blindness due to diabetes,” he continued.
His uveitis treatment ladder starts with topical corticosteroids, which are often quite effective for anterior uveitis. Second-line therapy consists of periocular or intravitreal steroid injections, “just like you’d inject a shoulder or knee.” Oral corticosteroids are effective, but their long-term use is problematic, so Dr. Rosenbaum will quickly switch to an antimetabolite, with methotrexate his top choice.
“I would never use a TNF inhibitor to treat spondyloarthropathy-associated acute anterior uveitis per se, because this type of uveitis is typically short lived. As a practical matter, by the time I got approval from the third-party payer the uveitis would be gone. But if a patient is having recurrent severe episodes of uveitis, a TNF inhibitor will reduce the intensity and frequency of those flares. So will sulfasalazine. Methotrexate will, too, but it doesn’t affect the spondyloarthropathy,” he said.
Dr. Rosenbaum reported receiving consulting fees from a dozen pharmaceutical companies and research grants from AbbVie, Eyegate, Genentech, and Psivida.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Smart diet remains potent cardiovascular medicine
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
SNOWMASS, COLO. – Cutting dietary fat intake remains a highly effective strategy for reducing coronary heart disease risk – but only so long as the replacement nutrients aren’t even bigger offenders, Dr. Robert A. Vogel said at the Annual Cardiovascular Conference at Snowmass.
In the face of decades of public health admonitions to reduce saturated fat intake, most Americans have increased their consumption of trans fats and simple carbohydrates, especially sugar. And therein lies a problem. Trans fats are far more harmful than saturated fats in terms of cardiovascular risk. And excessive sugar consumption is a major contributor to abdominal obesity, metabolic syndrome, hypertension, and endothelial dysfunction.
“In the United States, sugar is a bigger source of hypertension than is salt,” asserted Dr. Vogel, a cardiologist at the University of Colorado, Denver.
The editors of Time magazine ignited a public controversy last year with a cover story arrestingly titled, “Eat Butter – Scientists labelled fat the enemy. Why they were wrong.” The editors were picking up on a British meta-analysis of 32 observational studies that concluded there is no clear evidence to support the notion that saturated fats are harmful to cardiovascular health and that swapping them out for consumption of polyunsaturated fatty acids (PUFAs) is beneficial (Ann. Intern. Med. 2014;160:398-406).
Dr. Vogel said those investigators are in fact correct: Many of the observational studies – going all the way back to the pioneering work by Dr. Ancel Keys in the 1950s – are flawed. They don’t convincingly prove the case for PUFAs as a healthier alternative. But there is persuasive evidence from well-conducted, randomized, controlled trials that this is indeed so, he added.
Several of these studies were done in an earlier era when it was possible to slip around the challenges and limitations of dietary studies in free-living populations. These trials wouldn’t be possible today for ethical reasons involving lack of informed consent.
For example, in the Finnish Mental Hospital Study conducted during 1959-1971, the food served at two mental institutions was altered. Patients at one hospital got 6 years of a diet high in PUFAs, then were crossed over to a typical Finnish diet. At the other mental hospital, patients were fed a normal Finnish diet for 6 years, then crossed over to the high-PUFA diet for 6 years. During the experimental-diet years, the coronary heart disease event rate was reduced by nearly 60% (Int. J. Epidemiol. 1979;8:99-118).
Similarly, in a prospective randomized trial conducted at a Los Angeles Veterans Affairs institution for older, cognitively impaired men, a no-choice shift to a diet high in PUFAs with reduced saturated fats resulted in roughly a 30% reduction in CHD events compared to the usual institutional diet (Lancet 1968;2:1060-2). A similar magnitude of CHD event reduction was seen with a high-PUFA dietary intervention in the Oslo Diet-Heart Study, a prospective secondary prevention trial (Circulation 1970;42:935-42).
In the contemporary era, the standout randomized dietary intervention trial is the Lyon Diet Heart Study, a 46-month prospective secondary prevention trial in which a Mediterranean diet low in saturated fat and high in alpha-linoleic acid, a PUFA, reduced the combined endpoint of cardiac death and nonfatal MI by 70%, compared with the usual post-MI prudent diet recommended at that time. Yet total cholesterol levels in the two study arms did not differ (Circulation 1999;99:779-85).
To put these results into context, Dr. Vogel noted that the Cholesterol Treatment Trialists Collaboration headquartered at the University of Oxford (England) has shown that for every 40 mg/dL of LDL-lowering achieved with statin therapy, the result is roughly a 20% reduction in CHD. In contrast, the classic nonpharmacologic diet studies resulted in 30%-70% relative risk reductions.
“Heart disease is a dietary disease,” the cardiologist emphasized. “When you compare diet intervention to LDL lowering with statins, you see that diet is very, very effective. But you have to know the details of the diet. You can’t take something out and put just anything in. It doesn’t work like that.”
For example, an analysis of data from the National Health and Nutrition Examination Survey concluded that individuals who consumed 25% of their calories from added sugar – that’s the equivalent of three 12-oz cans of a sugary cola per day – had a 175% increased risk of cardiovascular mortality during a median 14.6 years of follow-up, compared with those who got less than 10% of their calories from added sugar (JAMA Intern. Med. 2014;174:516-24).
And as for the impact of the trans fat that’s liberally present in many processed foods, the Nurses Health Study showed that for every 5% increase in energy intake from saturated fat – that’s equivalent to one 8-oz steak per day – the relative risk for CHD rose by a relatively modest 17%, while for a 5% increase in energy intake from trans fat – the equivalent of 4 oz of butter – CHD risk shot up by 382% (N. Engl. J. Med. 1997;337:1491-9).
Dr. Vogel reported serving as a paid consultant to the National Football League and the Pritikin Longevity Center and receiving a research grant from Sanofi.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Epinephrine use for anaphylaxis in schools: First national survey
HOUSTON – Fully 22% of the anaphylactic events occurring in students while attending U.S. schools, grades kindergarten through high school, are first episodes with no previous known allergy.
That was just one of several surprising findings in the first-ever national study of anaphylactic events and the use of epinephrine autoinjectors in U.S. schools.
“The big surprise for me was how frequently there was no known allergy. For those kids, having epinephrine stocked in the school was potentially life saving. And it underscores the importance that the teaching staff and aides and nurses know how to recognize anaphylaxis, because they wouldn’t know that that child was even at risk,” Dr. Martha V. White said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Dr. White, an allergist in private practice in Wheaton, Md., was lead investigator in the survey of schools participating in the national EPIPEN4SCHOOLS program. The program, conducted by Mylan, provides free EpiPen epinephrine autoinjectors to schools that can document that they have staff trained in their use. The epinephrine autoinjectors (EAIs) are stored at school for use in anyone experiencing anaphylaxis who doesn’t have their own.
The survey provides the clearest picture yet of anaphylaxis in school settings. It included all reported anaphylactic events occurring during the 2013-2014 school year at 6,019 responding U.S. schools. A total of 919 anaphylactic events were reported by 11% of the schools. Eighty-nine percent of the episodes occurred in students, the rest in school staff or visitors.
Twenty percent of anaphylactic events in students were associated with unknown triggers. When a trigger was identified, it was food in 62% of cases, an insect bite or sting in 10%, a medication or environmental trigger in 7%, and latex in 1%.
Among the surprising findings:
Epinephrine wasn’t used in 25% of anaphylactic events. Most of those events were treated with an oral antihistamine, a finding that caused Dr. White to bristle.
“That’s an educational opportunity, because antihistamines won’t stop allergic reactions,” she said in an interview. “They might make you feel like you’re doing something – they might help with the itching – but antihistamines aren’t going to actually stop an allergic reaction.”
Twenty percent of individuals with anaphylaxis weren’t sent to a hospital emergency department. “That’s another opportunity for education because you can have a recurrence of the anaphylaxis,” the allergist noted.
Indeed, roughly 20% of patients who experience anaphylaxis have a biphasic reaction, with recurrence of symptoms up to 38 hours after the first reaction. For this reason, the product labeling for EIAs states that emergency medical follow-up treatment is recommended after treatment of an anaphylactic event.
High school students appear to be at increased risk for in-school anaphylactic events. High schoolers accounted for 18% of the total K-12 student population, but they experienced 49% of all anaphylactic events.
School staff varied widely in their preparedness to recognize anaphylaxis and treat it with an EAI. At 36% of schools, only the school nurse and select staff were trained to recognize anaphylaxis. Twenty-nine percent of schools trained most staff, and 31% trained all staff, including coaches, athletic trainers, and office staff. More adults on campus were trained to recognize anaphylaxis than to actually administer epinephrine.
Mylan is continuing to operate the EPIPEN4SCHOOLS program. That’s good news, Dr. White said, because some major health insurance companies refuse to pay for two sets of EAIs – one for home and another for school – forcing parents to decide in which setting to leave their child unprotected.
“Remember, the autoinjector needs to be where the child is,” Dr. White said.
The survey was supported by Mylan. Dr. White reported serving on Mylan’s scientific advisory board and receiving research grants from most pharmaceutical companies with an interest in asthma medications.
HOUSTON – Fully 22% of the anaphylactic events occurring in students while attending U.S. schools, grades kindergarten through high school, are first episodes with no previous known allergy.
That was just one of several surprising findings in the first-ever national study of anaphylactic events and the use of epinephrine autoinjectors in U.S. schools.
“The big surprise for me was how frequently there was no known allergy. For those kids, having epinephrine stocked in the school was potentially life saving. And it underscores the importance that the teaching staff and aides and nurses know how to recognize anaphylaxis, because they wouldn’t know that that child was even at risk,” Dr. Martha V. White said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Dr. White, an allergist in private practice in Wheaton, Md., was lead investigator in the survey of schools participating in the national EPIPEN4SCHOOLS program. The program, conducted by Mylan, provides free EpiPen epinephrine autoinjectors to schools that can document that they have staff trained in their use. The epinephrine autoinjectors (EAIs) are stored at school for use in anyone experiencing anaphylaxis who doesn’t have their own.
The survey provides the clearest picture yet of anaphylaxis in school settings. It included all reported anaphylactic events occurring during the 2013-2014 school year at 6,019 responding U.S. schools. A total of 919 anaphylactic events were reported by 11% of the schools. Eighty-nine percent of the episodes occurred in students, the rest in school staff or visitors.
Twenty percent of anaphylactic events in students were associated with unknown triggers. When a trigger was identified, it was food in 62% of cases, an insect bite or sting in 10%, a medication or environmental trigger in 7%, and latex in 1%.
Among the surprising findings:
Epinephrine wasn’t used in 25% of anaphylactic events. Most of those events were treated with an oral antihistamine, a finding that caused Dr. White to bristle.
“That’s an educational opportunity, because antihistamines won’t stop allergic reactions,” she said in an interview. “They might make you feel like you’re doing something – they might help with the itching – but antihistamines aren’t going to actually stop an allergic reaction.”
Twenty percent of individuals with anaphylaxis weren’t sent to a hospital emergency department. “That’s another opportunity for education because you can have a recurrence of the anaphylaxis,” the allergist noted.
Indeed, roughly 20% of patients who experience anaphylaxis have a biphasic reaction, with recurrence of symptoms up to 38 hours after the first reaction. For this reason, the product labeling for EIAs states that emergency medical follow-up treatment is recommended after treatment of an anaphylactic event.
High school students appear to be at increased risk for in-school anaphylactic events. High schoolers accounted for 18% of the total K-12 student population, but they experienced 49% of all anaphylactic events.
School staff varied widely in their preparedness to recognize anaphylaxis and treat it with an EAI. At 36% of schools, only the school nurse and select staff were trained to recognize anaphylaxis. Twenty-nine percent of schools trained most staff, and 31% trained all staff, including coaches, athletic trainers, and office staff. More adults on campus were trained to recognize anaphylaxis than to actually administer epinephrine.
Mylan is continuing to operate the EPIPEN4SCHOOLS program. That’s good news, Dr. White said, because some major health insurance companies refuse to pay for two sets of EAIs – one for home and another for school – forcing parents to decide in which setting to leave their child unprotected.
“Remember, the autoinjector needs to be where the child is,” Dr. White said.
The survey was supported by Mylan. Dr. White reported serving on Mylan’s scientific advisory board and receiving research grants from most pharmaceutical companies with an interest in asthma medications.
HOUSTON – Fully 22% of the anaphylactic events occurring in students while attending U.S. schools, grades kindergarten through high school, are first episodes with no previous known allergy.
That was just one of several surprising findings in the first-ever national study of anaphylactic events and the use of epinephrine autoinjectors in U.S. schools.
“The big surprise for me was how frequently there was no known allergy. For those kids, having epinephrine stocked in the school was potentially life saving. And it underscores the importance that the teaching staff and aides and nurses know how to recognize anaphylaxis, because they wouldn’t know that that child was even at risk,” Dr. Martha V. White said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Dr. White, an allergist in private practice in Wheaton, Md., was lead investigator in the survey of schools participating in the national EPIPEN4SCHOOLS program. The program, conducted by Mylan, provides free EpiPen epinephrine autoinjectors to schools that can document that they have staff trained in their use. The epinephrine autoinjectors (EAIs) are stored at school for use in anyone experiencing anaphylaxis who doesn’t have their own.
The survey provides the clearest picture yet of anaphylaxis in school settings. It included all reported anaphylactic events occurring during the 2013-2014 school year at 6,019 responding U.S. schools. A total of 919 anaphylactic events were reported by 11% of the schools. Eighty-nine percent of the episodes occurred in students, the rest in school staff or visitors.
Twenty percent of anaphylactic events in students were associated with unknown triggers. When a trigger was identified, it was food in 62% of cases, an insect bite or sting in 10%, a medication or environmental trigger in 7%, and latex in 1%.
Among the surprising findings:
Epinephrine wasn’t used in 25% of anaphylactic events. Most of those events were treated with an oral antihistamine, a finding that caused Dr. White to bristle.
“That’s an educational opportunity, because antihistamines won’t stop allergic reactions,” she said in an interview. “They might make you feel like you’re doing something – they might help with the itching – but antihistamines aren’t going to actually stop an allergic reaction.”
Twenty percent of individuals with anaphylaxis weren’t sent to a hospital emergency department. “That’s another opportunity for education because you can have a recurrence of the anaphylaxis,” the allergist noted.
Indeed, roughly 20% of patients who experience anaphylaxis have a biphasic reaction, with recurrence of symptoms up to 38 hours after the first reaction. For this reason, the product labeling for EIAs states that emergency medical follow-up treatment is recommended after treatment of an anaphylactic event.
High school students appear to be at increased risk for in-school anaphylactic events. High schoolers accounted for 18% of the total K-12 student population, but they experienced 49% of all anaphylactic events.
School staff varied widely in their preparedness to recognize anaphylaxis and treat it with an EAI. At 36% of schools, only the school nurse and select staff were trained to recognize anaphylaxis. Twenty-nine percent of schools trained most staff, and 31% trained all staff, including coaches, athletic trainers, and office staff. More adults on campus were trained to recognize anaphylaxis than to actually administer epinephrine.
Mylan is continuing to operate the EPIPEN4SCHOOLS program. That’s good news, Dr. White said, because some major health insurance companies refuse to pay for two sets of EAIs – one for home and another for school – forcing parents to decide in which setting to leave their child unprotected.
“Remember, the autoinjector needs to be where the child is,” Dr. White said.
The survey was supported by Mylan. Dr. White reported serving on Mylan’s scientific advisory board and receiving research grants from most pharmaceutical companies with an interest in asthma medications.
AT 2015 AAAAI ANNUAL MEETING
Key clinical point: 11% of U.S. schools reported that one or more anaphylactic events occurred on site during the 2013-2014 school year.
Major finding: 20% of students treated with an epinephrine autoinjector while at school weren’t sent to the emergency department afterwards, even though the product labeling recommends doing so.
Data source: This national survey of anaphylactic episodes included 6,019 U.S. schools, kindergarten through high school.
Disclosures: The survey was funded by Mylan. The presenter reported serving on Mylan’s scientific advisory board and receiving research grants from most pharmaceutical companies with an interest in asthma medications.
Managing gymnasts’ wrist and back overuse injuries
SNOWMASS, COLO. – Overuse injuries in young gymnasts are extremely common, and they cluster at two vulnerable anatomic sites: the wrist and lower back.
“Gymnasts have to be one of the biggest parts of my sports medicine practice. Some of them are the toughest patients I see in terms of their workouts, consistency, and dedication to their sport. And they’ll work through the pain. Gymnastics is truly a sport where it’s been driven into them that no pain is no gain,” Dr. M. Timothy Hresko observed at the Winter Rheumaltogy Symposium sponsored by the American College of Rheumatology.
With a patient mindset like this, it’s little wonder that physicians have their work cut out for them when trying to help gymnasts heal and prevent future setbacks. Gymnasts are loathe to sit back and rest. Yet rest is central to successful treatment of overuse injuries. And therein lies the basis for a frequent locking of horns, added Dr. Hresko, an orthopedic surgeon at Harvard Medical School, Boston, and Boston Children’s Hospital.
“Quite often you need to reinforce to them the rest that’s necessary for this to work,” he said. “Young gymnasts will spend 20 hours a week in the gym: 4 hours, 5 days a week. We see a lot of overuse injuries associated with that. Is that pushing somebody too much? For skill sports, that’s what’s required if you want to develop the skill.”
Gymnast’s wrist: This is a stress fracture through the radial epiphyseal plate. It results from the tremendous weight-bearing loads imposed on the arms and wrists during many hours of repeated activities including tumbling, swinging, mounting, and vaulting.
Affected patients present with a complaint of pain with weight bearing on the wrist. Physical examination reveals tenderness over the distal radial growth plate and loss of range of motion in the wrist. An x-ray will show widening of the radial growth plate and perhaps irregular bone edges.
Treatment entails cessation of all impact activities for 2-3 months to permit the stress fracture to heal, along with wearing a wrist splint for protection during normal daily activities. The patient can return to gymnastics after that rest period, provided the distal radial physis is no longer tender. The return to the sport should be gradual, with resumption of vaulting reserved for last.
“Vaulting is probably the hardest activity to do and to return to,” according to Dr. Hresko.
Spondylolysis: this is a stress fracture of a lumbar vertebra, which, in gymnasts, results from repeated hyperextension. It’s the most common cause of low back pain in adolescent athletes.
“I must see 6-10 patients per week who have some phase of spondylolysis,” the surgeon said.
The diagnostic hallmark on physical examination is lumbar back pain that worsens with lumbar extension. A straight leg raise test is often positive. The stress fracture will show up on a plain film x-ray but therein lies a quandary.
“In a normal population of adolescents without symptoms, 6% will have evidence of spondylolysis on plain film x-ray. So if you see a positive x-ray in a patient with low back pain you have to ask yourself if this is really the cause of their pain,” Dr. Hresko said.
Herniated discs are “pretty rare” in youth, but the clues are the same as in adults: radicular symptoms, burning pain, and a positive straight leg raise test, he noted.
The treatment for spondylolysis is restricted activities, usually for 2-3 months or one season.
“I personally think it’s best to immobilize them with a brace. We use a custom-made, anterior-opening Boston overlap brace to limit extension. That way they can go back to activities sooner, but they’re usually out of their sport for one season, then we try to get them back for their second season, knowing that the injury isn’t going to heal anatomically,” the sports medicine specialist said.
Gymnasts who are hyperlordotic are at increased risk for spondylolysis. For injury prevention in such individuals, he emphasizes abdominal strengthening and pelvic tilting exercises to reduce the lumbar lordosis.
“We haven’t gone quite so far as to use anatomic body markers like lordosis to suggest somebody’s at such high risk that they should not go out for that sport – sort of an East German approach to athletics – but I do think that in gymnastics there are some patients whose bodies are just not up to the stress involved in that sport,” he concluded.
Dr. Hresko serves as a consultant to DePuy Spine.
SNOWMASS, COLO. – Overuse injuries in young gymnasts are extremely common, and they cluster at two vulnerable anatomic sites: the wrist and lower back.
“Gymnasts have to be one of the biggest parts of my sports medicine practice. Some of them are the toughest patients I see in terms of their workouts, consistency, and dedication to their sport. And they’ll work through the pain. Gymnastics is truly a sport where it’s been driven into them that no pain is no gain,” Dr. M. Timothy Hresko observed at the Winter Rheumaltogy Symposium sponsored by the American College of Rheumatology.
With a patient mindset like this, it’s little wonder that physicians have their work cut out for them when trying to help gymnasts heal and prevent future setbacks. Gymnasts are loathe to sit back and rest. Yet rest is central to successful treatment of overuse injuries. And therein lies the basis for a frequent locking of horns, added Dr. Hresko, an orthopedic surgeon at Harvard Medical School, Boston, and Boston Children’s Hospital.
“Quite often you need to reinforce to them the rest that’s necessary for this to work,” he said. “Young gymnasts will spend 20 hours a week in the gym: 4 hours, 5 days a week. We see a lot of overuse injuries associated with that. Is that pushing somebody too much? For skill sports, that’s what’s required if you want to develop the skill.”
Gymnast’s wrist: This is a stress fracture through the radial epiphyseal plate. It results from the tremendous weight-bearing loads imposed on the arms and wrists during many hours of repeated activities including tumbling, swinging, mounting, and vaulting.
Affected patients present with a complaint of pain with weight bearing on the wrist. Physical examination reveals tenderness over the distal radial growth plate and loss of range of motion in the wrist. An x-ray will show widening of the radial growth plate and perhaps irregular bone edges.
Treatment entails cessation of all impact activities for 2-3 months to permit the stress fracture to heal, along with wearing a wrist splint for protection during normal daily activities. The patient can return to gymnastics after that rest period, provided the distal radial physis is no longer tender. The return to the sport should be gradual, with resumption of vaulting reserved for last.
“Vaulting is probably the hardest activity to do and to return to,” according to Dr. Hresko.
Spondylolysis: this is a stress fracture of a lumbar vertebra, which, in gymnasts, results from repeated hyperextension. It’s the most common cause of low back pain in adolescent athletes.
“I must see 6-10 patients per week who have some phase of spondylolysis,” the surgeon said.
The diagnostic hallmark on physical examination is lumbar back pain that worsens with lumbar extension. A straight leg raise test is often positive. The stress fracture will show up on a plain film x-ray but therein lies a quandary.
“In a normal population of adolescents without symptoms, 6% will have evidence of spondylolysis on plain film x-ray. So if you see a positive x-ray in a patient with low back pain you have to ask yourself if this is really the cause of their pain,” Dr. Hresko said.
Herniated discs are “pretty rare” in youth, but the clues are the same as in adults: radicular symptoms, burning pain, and a positive straight leg raise test, he noted.
The treatment for spondylolysis is restricted activities, usually for 2-3 months or one season.
“I personally think it’s best to immobilize them with a brace. We use a custom-made, anterior-opening Boston overlap brace to limit extension. That way they can go back to activities sooner, but they’re usually out of their sport for one season, then we try to get them back for their second season, knowing that the injury isn’t going to heal anatomically,” the sports medicine specialist said.
Gymnasts who are hyperlordotic are at increased risk for spondylolysis. For injury prevention in such individuals, he emphasizes abdominal strengthening and pelvic tilting exercises to reduce the lumbar lordosis.
“We haven’t gone quite so far as to use anatomic body markers like lordosis to suggest somebody’s at such high risk that they should not go out for that sport – sort of an East German approach to athletics – but I do think that in gymnastics there are some patients whose bodies are just not up to the stress involved in that sport,” he concluded.
Dr. Hresko serves as a consultant to DePuy Spine.
SNOWMASS, COLO. – Overuse injuries in young gymnasts are extremely common, and they cluster at two vulnerable anatomic sites: the wrist and lower back.
“Gymnasts have to be one of the biggest parts of my sports medicine practice. Some of them are the toughest patients I see in terms of their workouts, consistency, and dedication to their sport. And they’ll work through the pain. Gymnastics is truly a sport where it’s been driven into them that no pain is no gain,” Dr. M. Timothy Hresko observed at the Winter Rheumaltogy Symposium sponsored by the American College of Rheumatology.
With a patient mindset like this, it’s little wonder that physicians have their work cut out for them when trying to help gymnasts heal and prevent future setbacks. Gymnasts are loathe to sit back and rest. Yet rest is central to successful treatment of overuse injuries. And therein lies the basis for a frequent locking of horns, added Dr. Hresko, an orthopedic surgeon at Harvard Medical School, Boston, and Boston Children’s Hospital.
“Quite often you need to reinforce to them the rest that’s necessary for this to work,” he said. “Young gymnasts will spend 20 hours a week in the gym: 4 hours, 5 days a week. We see a lot of overuse injuries associated with that. Is that pushing somebody too much? For skill sports, that’s what’s required if you want to develop the skill.”
Gymnast’s wrist: This is a stress fracture through the radial epiphyseal plate. It results from the tremendous weight-bearing loads imposed on the arms and wrists during many hours of repeated activities including tumbling, swinging, mounting, and vaulting.
Affected patients present with a complaint of pain with weight bearing on the wrist. Physical examination reveals tenderness over the distal radial growth plate and loss of range of motion in the wrist. An x-ray will show widening of the radial growth plate and perhaps irregular bone edges.
Treatment entails cessation of all impact activities for 2-3 months to permit the stress fracture to heal, along with wearing a wrist splint for protection during normal daily activities. The patient can return to gymnastics after that rest period, provided the distal radial physis is no longer tender. The return to the sport should be gradual, with resumption of vaulting reserved for last.
“Vaulting is probably the hardest activity to do and to return to,” according to Dr. Hresko.
Spondylolysis: this is a stress fracture of a lumbar vertebra, which, in gymnasts, results from repeated hyperextension. It’s the most common cause of low back pain in adolescent athletes.
“I must see 6-10 patients per week who have some phase of spondylolysis,” the surgeon said.
The diagnostic hallmark on physical examination is lumbar back pain that worsens with lumbar extension. A straight leg raise test is often positive. The stress fracture will show up on a plain film x-ray but therein lies a quandary.
“In a normal population of adolescents without symptoms, 6% will have evidence of spondylolysis on plain film x-ray. So if you see a positive x-ray in a patient with low back pain you have to ask yourself if this is really the cause of their pain,” Dr. Hresko said.
Herniated discs are “pretty rare” in youth, but the clues are the same as in adults: radicular symptoms, burning pain, and a positive straight leg raise test, he noted.
The treatment for spondylolysis is restricted activities, usually for 2-3 months or one season.
“I personally think it’s best to immobilize them with a brace. We use a custom-made, anterior-opening Boston overlap brace to limit extension. That way they can go back to activities sooner, but they’re usually out of their sport for one season, then we try to get them back for their second season, knowing that the injury isn’t going to heal anatomically,” the sports medicine specialist said.
Gymnasts who are hyperlordotic are at increased risk for spondylolysis. For injury prevention in such individuals, he emphasizes abdominal strengthening and pelvic tilting exercises to reduce the lumbar lordosis.
“We haven’t gone quite so far as to use anatomic body markers like lordosis to suggest somebody’s at such high risk that they should not go out for that sport – sort of an East German approach to athletics – but I do think that in gymnastics there are some patients whose bodies are just not up to the stress involved in that sport,” he concluded.
Dr. Hresko serves as a consultant to DePuy Spine.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Annual Recurrence Rate of Anaphylaxis in Kids Is Nearly 30%
HOUSTON – The annual incidence of recurrent anaphylaxis in children was 29% in the first prospective study to examine the issue.
“That rate is higher than previously reported in retrospective studies,” Dr. Andrew O’Keefe said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
He presented a study conducted as part of the Cross-Canada Anaphylaxis Registry (C-CARE). In the prospective study, the parents of 266 children who presented with anaphylaxis to two Montreal hospitals were contacted annually thereafter and asked about subsequent allergic reactions.
The parents of 96 children participated. Twenty-five of these 96 children experienced a total of 42 recurrent episodes of anaphylaxis, with an annual recurrence rate of 29%. Three-quarters of recurrences were categorized by investigators as moderate in severity, meaning they entailed crampy abdominal pain, recurrent vomiting, diarrhea, a barky cough, stridor, hoarseness, difficulty swallowing, shortness of breath, and/or moderate wheezing.
A striking study finding was that an epinephrine autoinjector was utilized prior to arrival at the hospital in only 52% of recurrences. That’s serious underutilization, commented Dr. O’Keefe, an allergist at Memorial University in St. Johns, Newfoundland.
“Physicians need to educate patients as to how to use the injectable epinephrine devices and encourage them to do so early during an episode of anaphylaxis, when they’re most effective,” he stressed in an interview.
Continue for principal triggers >>
Food was the principal trigger for 91% of recurrent episodes. Interestingly, children with recurrent anaphylaxis were 71% less likely to have peanut as a trigger, most likely because of extra vigilance regarding this notorious allergen, according to Dr. O’Keefe.
He noted a couple of significant study limitations. One is the small sample size. However, the study is being expanded to other academic medical centers across Canada, which will strengthen the findings.
The other limitation is the potential for bias introduced because parents whose child had severe anaphylaxis as the first episode were more than threefold more likely to participate in the prospective study. Still, the finding of a 29% annual recurrence rate among children in the Canadian study is not far afield from the results of some retrospective studies. For example, investigators at the Mayo Clinic reported as part of the Rochester Epidemiology Project a 21% incidence of a second anaphylactic event occurring at a median of 395 days after the first event in both child and adult residents of Olmsted County, Minn. (J. Allergy Clin. Immunol. 2008;122:1161-5).
That study and others also suggest that the incidence of anaphylaxis is increasing. In Olmsted County, the rate rose from 46.9 cases/100,000 persons in 1990 to 58.9 cases/100,000 in 2000.
Asked why the prehospital use of injectable epinephrine was so low in the Montreal children, Dr. O’Keefe said there are several possible reasons.
“We know that the rates among physicians as well as parents and children are lower than what they should be. Some of the reasons include failure to identify anaphylaxis, not having the device with you, and, finally, patients have to know how to use it and be willing to. There’s a psychological hurdle involving fear of misusing the device or hurting their child or using it inappropriately that prevents people from using it,” he said.
The study was supported by research grants from AllerGen, Health Canada, and Sanofi.
HOUSTON – The annual incidence of recurrent anaphylaxis in children was 29% in the first prospective study to examine the issue.
“That rate is higher than previously reported in retrospective studies,” Dr. Andrew O’Keefe said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
He presented a study conducted as part of the Cross-Canada Anaphylaxis Registry (C-CARE). In the prospective study, the parents of 266 children who presented with anaphylaxis to two Montreal hospitals were contacted annually thereafter and asked about subsequent allergic reactions.
The parents of 96 children participated. Twenty-five of these 96 children experienced a total of 42 recurrent episodes of anaphylaxis, with an annual recurrence rate of 29%. Three-quarters of recurrences were categorized by investigators as moderate in severity, meaning they entailed crampy abdominal pain, recurrent vomiting, diarrhea, a barky cough, stridor, hoarseness, difficulty swallowing, shortness of breath, and/or moderate wheezing.
A striking study finding was that an epinephrine autoinjector was utilized prior to arrival at the hospital in only 52% of recurrences. That’s serious underutilization, commented Dr. O’Keefe, an allergist at Memorial University in St. Johns, Newfoundland.
“Physicians need to educate patients as to how to use the injectable epinephrine devices and encourage them to do so early during an episode of anaphylaxis, when they’re most effective,” he stressed in an interview.
Continue for principal triggers >>
Food was the principal trigger for 91% of recurrent episodes. Interestingly, children with recurrent anaphylaxis were 71% less likely to have peanut as a trigger, most likely because of extra vigilance regarding this notorious allergen, according to Dr. O’Keefe.
He noted a couple of significant study limitations. One is the small sample size. However, the study is being expanded to other academic medical centers across Canada, which will strengthen the findings.
The other limitation is the potential for bias introduced because parents whose child had severe anaphylaxis as the first episode were more than threefold more likely to participate in the prospective study. Still, the finding of a 29% annual recurrence rate among children in the Canadian study is not far afield from the results of some retrospective studies. For example, investigators at the Mayo Clinic reported as part of the Rochester Epidemiology Project a 21% incidence of a second anaphylactic event occurring at a median of 395 days after the first event in both child and adult residents of Olmsted County, Minn. (J. Allergy Clin. Immunol. 2008;122:1161-5).
That study and others also suggest that the incidence of anaphylaxis is increasing. In Olmsted County, the rate rose from 46.9 cases/100,000 persons in 1990 to 58.9 cases/100,000 in 2000.
Asked why the prehospital use of injectable epinephrine was so low in the Montreal children, Dr. O’Keefe said there are several possible reasons.
“We know that the rates among physicians as well as parents and children are lower than what they should be. Some of the reasons include failure to identify anaphylaxis, not having the device with you, and, finally, patients have to know how to use it and be willing to. There’s a psychological hurdle involving fear of misusing the device or hurting their child or using it inappropriately that prevents people from using it,” he said.
The study was supported by research grants from AllerGen, Health Canada, and Sanofi.
HOUSTON – The annual incidence of recurrent anaphylaxis in children was 29% in the first prospective study to examine the issue.
“That rate is higher than previously reported in retrospective studies,” Dr. Andrew O’Keefe said at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
He presented a study conducted as part of the Cross-Canada Anaphylaxis Registry (C-CARE). In the prospective study, the parents of 266 children who presented with anaphylaxis to two Montreal hospitals were contacted annually thereafter and asked about subsequent allergic reactions.
The parents of 96 children participated. Twenty-five of these 96 children experienced a total of 42 recurrent episodes of anaphylaxis, with an annual recurrence rate of 29%. Three-quarters of recurrences were categorized by investigators as moderate in severity, meaning they entailed crampy abdominal pain, recurrent vomiting, diarrhea, a barky cough, stridor, hoarseness, difficulty swallowing, shortness of breath, and/or moderate wheezing.
A striking study finding was that an epinephrine autoinjector was utilized prior to arrival at the hospital in only 52% of recurrences. That’s serious underutilization, commented Dr. O’Keefe, an allergist at Memorial University in St. Johns, Newfoundland.
“Physicians need to educate patients as to how to use the injectable epinephrine devices and encourage them to do so early during an episode of anaphylaxis, when they’re most effective,” he stressed in an interview.
Continue for principal triggers >>
Food was the principal trigger for 91% of recurrent episodes. Interestingly, children with recurrent anaphylaxis were 71% less likely to have peanut as a trigger, most likely because of extra vigilance regarding this notorious allergen, according to Dr. O’Keefe.
He noted a couple of significant study limitations. One is the small sample size. However, the study is being expanded to other academic medical centers across Canada, which will strengthen the findings.
The other limitation is the potential for bias introduced because parents whose child had severe anaphylaxis as the first episode were more than threefold more likely to participate in the prospective study. Still, the finding of a 29% annual recurrence rate among children in the Canadian study is not far afield from the results of some retrospective studies. For example, investigators at the Mayo Clinic reported as part of the Rochester Epidemiology Project a 21% incidence of a second anaphylactic event occurring at a median of 395 days after the first event in both child and adult residents of Olmsted County, Minn. (J. Allergy Clin. Immunol. 2008;122:1161-5).
That study and others also suggest that the incidence of anaphylaxis is increasing. In Olmsted County, the rate rose from 46.9 cases/100,000 persons in 1990 to 58.9 cases/100,000 in 2000.
Asked why the prehospital use of injectable epinephrine was so low in the Montreal children, Dr. O’Keefe said there are several possible reasons.
“We know that the rates among physicians as well as parents and children are lower than what they should be. Some of the reasons include failure to identify anaphylaxis, not having the device with you, and, finally, patients have to know how to use it and be willing to. There’s a psychological hurdle involving fear of misusing the device or hurting their child or using it inappropriately that prevents people from using it,” he said.
The study was supported by research grants from AllerGen, Health Canada, and Sanofi.
AT 2015 AAAAI ANNUAL MEETING