User login
New mobile app assists clinicians in assessing menopausal patients
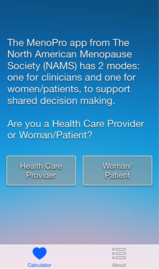
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.
 |
 |
 |
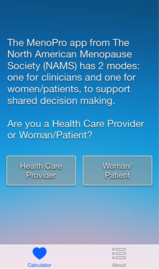
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
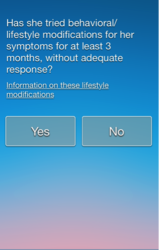
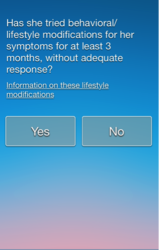
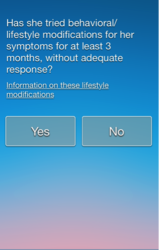
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.
 |
 |
 |
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
A new mobile app for iPhone and iPad enables both clinicians and patients to make decisions about menopausal therapies for moderate to severe hot flashes, night sweats, and/or genitourinary symptoms. The app also aids in assessing the patient’s risk of cardiovascular disease, breast cancer, and fracture.
 |
 |
 |
The MenoPro app, developed in association with the North American Menopause Society (NAMS), is available free of charge from Apple. The app is designed to aid in the assessment and management of bothersome menopausal symptoms in women aged 45 and older.
Designed for both clinician and patient
A novel feature of the app is its two modes—one for the clinician and another for the patient. The clinician mode enables risk assessment and decision-making to determine whether hormonal therapy might be indicated and to determine the formulation and dosage of the therapy selected. It also features assessment of the patient’s 10-year risk of cardiovascular disease, her risk of breast cancer using the Gail model, and her fracture risk using the FRAX tool. When hormonal therapies are not appropriate, the app steers the clinician to nonhormonal options.
The patient can make use of the app to learn about her different treatment options, including lifestyle modifications. The app guides her through a self-assessment to gauge how far along she is in the menopausal transition, the severity of her symptoms, and her interest in hormonal or nonhormonal therapy. The app begins by recommending lifestyle changes and behavioral factors that can reduce menopausal symptoms. After a 3-month trial of these modifications, the patient is prompted to visit her health-care provider if further relief is needed.
Only FDA-approved drugs are recommended
“The app is completely up to date in terms of information about the newest medications that have been approved by the US Food and Drug Administration,” says JoAnn E. Manson, MD, DrPH, current chair of the NAMS Scientific Program and a past president of NAMS. Dr. Manson is Chief of the Division of Preventive Medicine at Brigham and Women’s Hospital in Boston. She also is Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health at Harvard Medical School.
“The app focuses on FDA-approved medications, including off-label use of medications that may be commonly prescribed in practice to treat hot flashes, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs),” she says.
“I think another big advantage is that very often clinicians who are managing patients during the menopausal transition or in early menopause may not be thinking that much about cardiovascular risk or even know how to evaluate it or make use of a 10-year risk score. So the app really helps them to become very familiar with the evaluation of cardiovascular risk, breast cancer risk, and fracture risk, and provides them with the resources to make use of the information.”
An algorithm is available within the app
The app is based on an algorithm that can be accessed within the app by choosing the “About” button. Another feature: the clinician can email a summary of the patient’s assessment directly to her, along with links to resources on a variety of relevant topics.
“In the future, there is a plan to have the app available for other mobile phones and tablet devices in addition to the iPhone and iPad,” says Dr. Manson. “We also hope to have it incorporated into electronic health records, where it could be used for clinical decision-making within the record.”
The app is not intended to replace clinical judgment, she adds. “I think clinicians are really familiar with the concept that, when you’re using an app, clinical judgment remains paramount. The app is not going to replace the clinician’s own discernment of what is going on with the patient.”
For detailed information, see an article on the app in the journal Menopause, available at http://www.menopause.org/docs/default-source/professional/our-new-paper.pdf
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
First large study on the risk of cancer spread using power morcellation pinpoints risk of uterine malignancy
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Among women who undergo minimally invasive hysterectomy with electric power morcellation, the rate of uterine cancer is 27 cases per 10,000 women at the time of the procedure, according to a recent study published in the Journal of the American Medical Association.1 That figure translates into approximately one case of undetected uterine cancer in every 368 women undergoing hysterectomy. Earlier this year the US Food and Drug Administration (FDA) estimated the prevalence of uterine sarcoma at one case in every 352 women.2
Leading up to publication of this study in late July, there had been concern and considerable discussion—including a 2-day hearing convened by the FDA— about whether power morcellation may result in the spread of undetected malignancies and, if so, how often that may occur.
Although power morcellators have been available commercially for two decades, accurate estimates of the prevalence of malignancy at the time of power morcellation have been lacking.
Jason D. Wright, MD, and colleagues from Columbia University used the Perspective database, a large insurance database, to investigate the prevalence of underlying cancer in women who underwent uterine morcellation during minimally invasive hysterectomy from 2006 to 2012. This database is an “all-payer” database that includes more than 500 hospitals in the United States, many of them urban teaching centers.
The cohort included 232,882 women who underwent minimally invasive hysterectomy, including 36,470 (15.7%) who had uterine morcellation during the procedure. Among women who underwent morcellation, 99 cases of uterine cancer were identified, a prevalence of 27 cases per 10,000 women (95% confidence interval [CI], 22–32).
Among women who underwent power morcellation, the prevalence of underlying cancer and endometrial hyperplasia increased with age. For example, compared with women younger than 40 years, the prevalence ratio for uterine malignancy was:
- 4.97 (95% CI, 1.91–12.93) in women aged 50 to 54 years
- 19.37 (95% CI, 7.66–48.95) in those aged 55 to 59 years
- 21.36 (95% CI, 7.22–63.21) in women aged 60 to 64
- 35.97 (95% CI, 14.14–91.53) in women aged 65 or older.
“Prevalence information is the first step in determining the risk of spreading cancer with morcellation,” Wright and colleagues observe. “Patients considering morcellation should be adequately counseled about the prevalence of cancerous and precancerous conditions prior to undergoing the procedure.”
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
Reference
- Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation [published online ahead of print July 22, 2014]. JAMA. doi: 10.1001/jama.2014.9005.
- US Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. FDA Safety Communication. http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed July 28, 2014.
FDA, hospitals caution against laparoscopic power morcellation during hysterectomy and myomectomy
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy may be riskier than many have thought. That’s the conclusion reached by the US Food and Drug Administration (FDA) in a safety communication issued April 17, 2014. In its communication, the FDA “discouraged” use of power morcellation during hysterectomy and myomectomy. Shortly afterward, Brigham and Women’s and Massachusetts General hospitals in Boston banned power morcellation in all hysterectomy and myomectomy procedures. The hospitals may resume power morcellation at some future date using a containment system, pending guidance from the Institutional Review Board.
Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation [without a containment system] is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
The two Boston hospitals are not the only institutions reconsidering the use of power morcellation. Temple University Hospital in Philadelphia banned use of the procedure without a containment system in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, at the time of this writing, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also to dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
FDA STOPS SHORT OF A BAN
In laying out its concerns, the FDA stopped short of an outright ban on power morcellation. Instead, it stated that, “based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids.”4
It also noted that approximately 1 in 350 women “undergoing hysterectomy or myomectomy for the treatment of fibroids is found to have an unsuspected uterine sarcoma.”4
Among its recommendations for health-care providers:
- avoid laparoscopic uterine power morcellation in women with suspected or known uterine cancer
- carefully consider all available treatment options for women with symptomatic uterine fibroids
- thoroughly discuss the benefits and risks of all treatments with patients.4
The FDA also noted that “some clinicians and medical institutions now advocate using a specimen ‘bag’ during morcellation in an attempt to contain the uterine tissue and minimize the risk of spread in the abdomen and pelvis.”4
ACOG HAS YET TO WEIGH IN
At the time of this writing, the most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”5
FILLING THE TECHNOLOGY GAP
Now that power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation, which is demonstrated in a video at obgmanagement.com. Similarly, Ceana Nezhat, MD, and Erica Dun, MD, demonstrate enclosed vaginal morcellation of a large uterus. Click here to access these and other features in the Morcellation Topic Collection.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, and the city and state in which you practice.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy may be riskier than many have thought. That’s the conclusion reached by the US Food and Drug Administration (FDA) in a safety communication issued April 17, 2014. In its communication, the FDA “discouraged” use of power morcellation during hysterectomy and myomectomy. Shortly afterward, Brigham and Women’s and Massachusetts General hospitals in Boston banned power morcellation in all hysterectomy and myomectomy procedures. The hospitals may resume power morcellation at some future date using a containment system, pending guidance from the Institutional Review Board.
Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation [without a containment system] is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
The two Boston hospitals are not the only institutions reconsidering the use of power morcellation. Temple University Hospital in Philadelphia banned use of the procedure without a containment system in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, at the time of this writing, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also to dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
FDA STOPS SHORT OF A BAN
In laying out its concerns, the FDA stopped short of an outright ban on power morcellation. Instead, it stated that, “based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids.”4
It also noted that approximately 1 in 350 women “undergoing hysterectomy or myomectomy for the treatment of fibroids is found to have an unsuspected uterine sarcoma.”4
Among its recommendations for health-care providers:
- avoid laparoscopic uterine power morcellation in women with suspected or known uterine cancer
- carefully consider all available treatment options for women with symptomatic uterine fibroids
- thoroughly discuss the benefits and risks of all treatments with patients.4
The FDA also noted that “some clinicians and medical institutions now advocate using a specimen ‘bag’ during morcellation in an attempt to contain the uterine tissue and minimize the risk of spread in the abdomen and pelvis.”4
ACOG HAS YET TO WEIGH IN
At the time of this writing, the most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”5
FILLING THE TECHNOLOGY GAP
Now that power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation, which is demonstrated in a video at obgmanagement.com. Similarly, Ceana Nezhat, MD, and Erica Dun, MD, demonstrate enclosed vaginal morcellation of a large uterus. Click here to access these and other features in the Morcellation Topic Collection.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, and the city and state in which you practice.
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy may be riskier than many have thought. That’s the conclusion reached by the US Food and Drug Administration (FDA) in a safety communication issued April 17, 2014. In its communication, the FDA “discouraged” use of power morcellation during hysterectomy and myomectomy. Shortly afterward, Brigham and Women’s and Massachusetts General hospitals in Boston banned power morcellation in all hysterectomy and myomectomy procedures. The hospitals may resume power morcellation at some future date using a containment system, pending guidance from the Institutional Review Board.
Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation [without a containment system] is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
The two Boston hospitals are not the only institutions reconsidering the use of power morcellation. Temple University Hospital in Philadelphia banned use of the procedure without a containment system in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, at the time of this writing, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also to dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
FDA STOPS SHORT OF A BAN
In laying out its concerns, the FDA stopped short of an outright ban on power morcellation. Instead, it stated that, “based on currently available information, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids.”4
It also noted that approximately 1 in 350 women “undergoing hysterectomy or myomectomy for the treatment of fibroids is found to have an unsuspected uterine sarcoma.”4
Among its recommendations for health-care providers:
- avoid laparoscopic uterine power morcellation in women with suspected or known uterine cancer
- carefully consider all available treatment options for women with symptomatic uterine fibroids
- thoroughly discuss the benefits and risks of all treatments with patients.4
The FDA also noted that “some clinicians and medical institutions now advocate using a specimen ‘bag’ during morcellation in an attempt to contain the uterine tissue and minimize the risk of spread in the abdomen and pelvis.”4
ACOG HAS YET TO WEIGH IN
At the time of this writing, the most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”5
FILLING THE TECHNOLOGY GAP
Now that power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation, which is demonstrated in a video at obgmanagement.com. Similarly, Ceana Nezhat, MD, and Erica Dun, MD, demonstrate enclosed vaginal morcellation of a large uterus. Click here to access these and other features in the Morcellation Topic Collection.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, and the city and state in which you practice.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. April 17, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
To access articles, videos, and audiocasts in the Morcellation Topic Collection, click here.
Open power morcellation of uterine tumors during hysterectomy banned at two Boston hospitals
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy may be riskier than many have thought, especially when morcellation is performed in an “open” fashion (without use of a protective bag) in the peritoneal cavity. That’s the conclusion reached by two top Boston hospitals recently, when Brigham and Women’s and Massachusetts General both banned use of open power morcellation in gynecologic surgery.
Both hospitals assert that, when used outside of a containment system such as a morcellation bag, intraperitoneal open morcellation can spread tumor tissue throughout the peritoneal cavity. Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
Related article: Options for reducing the use of open power morcellation of uterine tumors Robert L. Barbieri, MD (Editorial, March 2014)
The two Boston hospitals are not the only institutions reconsidering the use of open power morcellation. Temple University Hospital in Philadelphia banned the procedure in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also of dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
The most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”4
FILLING THE TECHNOLOGY GAP
Now that open power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation. His strategy involves utilization of a large bowel isolation bag. For more on this approach, click here.
AAGL is in the process of formulating a policy on the use of open power morcellation. ACOG has not signaled its intent to weigh in on the issue.
Brigham and Women’s Hospital intends to carefully review requests for permission to utilize open power morcellation on a case-by-case basis, provided the surgeon presents all case details and a rationale for exemption from the new rule.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL. AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy may be riskier than many have thought, especially when morcellation is performed in an “open” fashion (without use of a protective bag) in the peritoneal cavity. That’s the conclusion reached by two top Boston hospitals recently, when Brigham and Women’s and Massachusetts General both banned use of open power morcellation in gynecologic surgery.
Both hospitals assert that, when used outside of a containment system such as a morcellation bag, intraperitoneal open morcellation can spread tumor tissue throughout the peritoneal cavity. Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
Related article: Options for reducing the use of open power morcellation of uterine tumors Robert L. Barbieri, MD (Editorial, March 2014)
The two Boston hospitals are not the only institutions reconsidering the use of open power morcellation. Temple University Hospital in Philadelphia banned the procedure in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also of dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
The most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”4
FILLING THE TECHNOLOGY GAP
Now that open power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation. His strategy involves utilization of a large bowel isolation bag. For more on this approach, click here.
AAGL is in the process of formulating a policy on the use of open power morcellation. ACOG has not signaled its intent to weigh in on the issue.
Brigham and Women’s Hospital intends to carefully review requests for permission to utilize open power morcellation on a case-by-case basis, provided the surgeon presents all case details and a rationale for exemption from the new rule.
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy may be riskier than many have thought, especially when morcellation is performed in an “open” fashion (without use of a protective bag) in the peritoneal cavity. That’s the conclusion reached by two top Boston hospitals recently, when Brigham and Women’s and Massachusetts General both banned use of open power morcellation in gynecologic surgery.
Both hospitals assert that, when used outside of a containment system such as a morcellation bag, intraperitoneal open morcellation can spread tumor tissue throughout the peritoneal cavity. Robert L. Barbieri, MD, who is chair of obstetrics and gynecology at Brigham and Women’s Hospital, recently wrote about this concern for OBG Management in his capacity as editor in chief of the journal.
“When used to treat tumors presumed to be fibroids, open power morcellation is associated with an increased risk of dispersing benign myoma tissue and occult malignant leiomyosarcoma tissue throughout the abdominal cavity,” he wrote.1 “Dispersion of benign myoma tissue may result in the growth of fibroids on the peritoneal surface, omentum, and bowel, causing abdominal and pelvic pain and necessitating reoperation. Dispersion of leiomyosarcoma tissue throughout the abdominal cavity may result in a Stage I cancer being upstaged to a Stage IV malignancy, requiring additional surgery and chemotherapy. In cases in which open power morcellation causes the upstaging of a leiomyosarcoma, the death rate is increased.”1
Related article: Options for reducing the use of open power morcellation of uterine tumors Robert L. Barbieri, MD (Editorial, March 2014)
The two Boston hospitals are not the only institutions reconsidering the use of open power morcellation. Temple University Hospital in Philadelphia banned the procedure in late February 2014.
And in December 2013, the Society of Gynecologic Oncology issued a position statement on the issue, which said, “power morcellation or other techniques that cut up the uterus in the abdomen have the potential to disseminate an otherwise contained malignancy throughout the abdominal cavity. For this reason, the Society of Gynecologic Oncology (SGO) asserts that it is generally contraindicated in the presence of documented or highly suspected malignancy, and may be inadvisable in premalignant conditions or risk-reducing surgery.”2
For its part, the AAGL, previously known as the American Association of Gynecologic Laparoscopists, “is reviewing the scientific evidence and best practices reported by our members,” stated an article in its Association News. “We recognize that, in rare cases, the use of power morcellators can lead to the dissemination of an occult malignancy of endometrial or myometrial origin, and also of dissemination of benign morcellated tissues. We encourage our members to fully research and understand the risks of power morcellation and to learn more about when alternative methods of tissue extraction may be appropriate.”3
The most recent committee opinion on choosing a hysterectomy route from the American College of Obstetricians and Gynecologists (ACOG) to touch on the issue states that, “the decision to perform a hysterectomy via [minimally invasive surgery] (with or without morcellation) is based on a patient evaluation, including the patient’s history and general health, tests, and procedures, such as pre-surgery biopsies. The evaluation and diagnostic process also provides an opportunity to identify any cautions or contraindications, such as finding a gynecological cancer.”4
FILLING THE TECHNOLOGY GAP
Now that open power morcellation appears to be receding as an option for minimally invasive gynecologic surgeons, what is the best approach?
In its position statement, the SGO recommends that, “Patients being considered for minimally invasive surgery performed by laparoscopic or robotic techniques who might require intracorporeal morcellation should be appropriately evaluated for the possibility of coexisting uterine or cervical malignancy. Other options to intracorporeal morcellation include removing the uterus through a mini-laparotomy or morcellating the uterus inside a laparoscopic bag.”2
K. Anthony Shibley, MD, a Minneapolis-area ObGyn, has developed a novel strategy to prevent tissue dissemination during open power morcellation. His strategy involves utilization of a large bowel isolation bag. For more on this approach, click here.
AAGL is in the process of formulating a policy on the use of open power morcellation. ACOG has not signaled its intent to weigh in on the issue.
Brigham and Women’s Hospital intends to carefully review requests for permission to utilize open power morcellation on a case-by-case basis, provided the surgeon presents all case details and a rationale for exemption from the new rule.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL. AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
- Barbieri RL. Options for reducing the use of open power morcellation of uterine tumors. OBG Manag. 2014;26(3):10,11,20.
- Society of Gynecologic Oncology. Position Statement: Morcellation. https://www.sgo.org/newsroom/position-statements-2/morcellation/. Published December 2013. Accessed April 8, 2014.
- AAGL. AAGL Member Update: Disseminated Leiomyosarcoma with Power Morcellation. http://www.aagl.org/aaglnews/aagl-member-update-disseminated-leiomyosarcoma-with-power-morcellation/. Accessed April 11, 2014.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114(5):1156–1158.
RELATED ARTICLES
![]()
![]()
Options for reducing the use of open power morcellation of uterine tumors Robert L. Barbieri, MD (Editorial, March 2014)
How I avoid open power morcellation
Morcellated leiomyosarcoma is a very real risk
(Comment & Controversy, March 2014)

![]()
Benefits and pitfalls of open power morcellation of uterine fibroids Robert L. Barbieri, MD (Editorial, February 2014)
Does screening mammography save lives?
When 25-year follow-up data from the Canadian National Breast Screening Study—published earlier this year—showed no benefit for annual mammography in women aged 40 to 59 years, the findings generated renewed debate about whether screening mammography actually saves lives.1
In that study, Miller and colleagues continued their follow-up of almost 90,000 women who had been randomly assigned to mammography (five annual screens) or no mammography from 1980 to 1985. Women aged 40 to 49 in the mammography arm and all women aged 50 to 69 underwent annual clinical breast examination (CBE). Women aged 40 to 49 in the control arm had a single CBE and continued usual care in the community. The main outcome measure was death from breast cancer.1
During the entire 25-year study, 3,250 women in the mammography arm were given a diagnosis of breast cancer, and 3,133 in the control arm received the same diagnosis. Of these, 500 and 505 women, respectively, died of the malignancy.
The overall hazard ratio for death from breast cancer in the mammography and control arms was 0.99 (95% confidence interval, 0.88–1.12). After 15 years of follow-up, 106 residual excess cancers (106/484; or 22%) were identified in the mammography arm and were attributed to “overdiagnosis.”1
During the screening period the mean size of breast cancers identified was 1.91 cm and 2.10 cm in the mammography and control arms, respectively (P = .01), and 30.6% and 32.4% of tumors, respectively, were associated with positive lymph nodes (P = .53).
PROFESSIONAL SOCIETIES STICK BY THEIR GUIDELINES
Following publication of the Canadian findings, the American College of Obstetricians and Gynecologists (ACOG) reaffirmed its recommendation for women at average risk for breast cancer to initiate annual screening at age 40. In an announcement issued February 14, 2014, ACOG noted that it had “a number of concerns” with the Canadian study.2
Similarly, the American Cancer Society reiterated its own recommendation that women aged 40 and older undergo annual mammography and CBE for as long as they remain healthy.3
The American College of Radiology went a few steps further, calling the Canadian study “incredibly flawed and misleading.”4 Its guidelines call for annual mammography beginning at age 40.
The US Preventive Services Task Force (USPSTF) 2009 guidelines on breast cancer screening also stand, with biennial mammography beginning at age 50 for women at average risk for breast cancer.5
The Canadian Cancer Society also reaffirmed its recommendations for breast cancer screening following publication of the Canadian trial 25-year follow-up data—although its recommendations call for screening to begin at age 50 and to be repeated thereafter at 2- to 3-year intervals.6,7
In short, nothing has changed…yet. But the Canadian trial raises a number of questions about breast cancer screening—and the answers aren’t as clear-cut as you might imagine.
IS THE CANADIAN TRIAL CREDIBLE?
Results from earlier randomized, controlled trials have indicated that screening mammography reduces death from breast cancer.
“The Canadian study is an outlier,” says Barbara Monsees, MD, Ronald and Hanna Evens Professor of Women’s Health in the department of radiology at Washington University in St. Louis, Missouri.
“There is an overwhelming amount of evidence that tells us that screening mammography saves lives,” says Dr. Monsees. “This evidence includes other randomized trials, case-control studies, results of organized screening programs, and downward trends in breast cancer deaths where screening is used.”
Mark D. Pearlman, MD, also believes the body of evidence shows that screening mammography is effective. Dr. Pearlman is vice chair and service chief in the division of obstetrics and gynecology and professor of surgery and director of the breast fellowship in obstetrics and gynecology at the University of Michigan Health System in Ann Arbor, Michigan. He has been on the surgical staff of the Breast Care Center there since 1990, with expertise in the management of women with breast disease and increased genetic risks for breast and ovarian cancer.
The Canadian trial is “a reasonably done study,” he says, “but there are some concerns. First, it’s not a new study—it was initially published 22 years ago. This latest publication is just a continuation of following these women.”
“This study, along with seven other randomized, controlled trials, was considered by the USPSTF in formulating its 2009 recommendations. In that meta-analysis, which included women in their 40s, screening mammography had benefit in every decade of life of interest.8 That is the basis on which ACOG made its recommendation for women at average risk to start annual screening at age 40 and continue at least until age 70,” Dr. Pearlman says. “When the USPSTF considered this negative study, it realized that there is benefit for mammography despite this single trial.”
Related article: Which women are most likely to die from breast cancer—those screened annually starting at age 40, biennially starting at age 50, or not at all? Mark D. Pearlman, MD (Examining the Evidence, November 2013)
James Dickinson, MBBS, PhD, a family physician and member of the Canadian Task Force on Preventive Health Care (a forerunner of the USPSTF), which has published its own set of guidelines on breast cancer screening, has a different perspective. Dr. Dickinson teaches at the University of Calgary in Alberta.
“One of the tendencies—particularly in medicine driven by commercial interests—is that as soon as there is even the slightest hint that something is worthwhile, there’s a rush to have everybody do it and make lots of profit from it. People don’t wait for the evidence. They jump to assume guilt or innocence without even looking for the evidence.”
“I give all credit to the Canadian trial investigators,” Dr. Dickinson says. “The world had jumped ahead of them and just assumed that breast screening worked. But they kept looking. They set up a good trial to start with and then followed it through and helped us understand that things aren’t as good as we would like them to be.”
Andrew M. Kaunitz, MD, professor and vice chair of obstetrics and gynecology at the University of Florida–Jacksonville also believes that the Canadian study’s findings are reliable. Dr. Kaunitz serves on the OBG Management Board of Editors.
“As pointed out in an editorial accompanying the Canadian trial, this study’s findings of a lack of efficacy of screening mammograms are ‘strikingly similar’ to other recent studies assessing breast cancer screening.”9–11
“Further, mammograms are costly and associated with a high rate of false-positive findings,” Dr. Kaunitz says.
“Too many weak links”
Among the main criticisms of the Canadian trial is a claim of flawed methodology.
“The Canadian trial is an update of a flawed study that was previously discredited for good reasons,” says Dr. Monsees. “In short, the quality of the mammograms was poor, and the overall study design did not reflect a true randomization process.”
“For example, true randomization requires eligible patients to be randomly divided into two or more groups, without any knowledge of their specific conditions that might bias trial results,” Dr. Monsees explains. “In the most valid randomized trials, this was accomplished by invitation. Without knowing anything about the women, investigators randomly assigned them to a group invited to be screened and a group not invited. In this manner, two equal groups were produced, with no way to corrupt the randomization process.”
“In the Canadian National Breast Screening Study, in contrast, once the women volunteered, they were given a clinical breast examination, and women with breast lumps and large lymph nodes in their underarms were identified. This information was provided to study coordinators, who assigned women on open lists to the mammography group or the control group,” Dr. Monsees says.
“Those of us in the imaging field know that the quality of mammography is only as good as the weakest link in the imaging chain. This study had far too many weak links. These criticisms are not new; they were raised during and after the trial and remain valid today.”
Dr. Pearlman does not believe that the Canadian trial reflects modern breast cancer screening.
“There are things in the Canadian trial that differ from what we see in modern mammography,” he says. “In the Canadian trial, in women diagnosed with breast cancer, they noted whether there was a palpable mass in the area of cancer. In the Canadian trial the percentage of palpable masses was approximately 66%, and that’s very very different from what we see with modern mammography. In current practice, about 15% of breast cancers diagnosed by mammography are palpable. And so it appears that, for some reason, they were seeing more advanced breast cancers when they were screening by mammography.”
Another concern focuses on the technology used in the trial.
“It appears that the Canadian investigators pulled old machines into service for the trial,” Dr. Pearlman says.
In addition, more recent advances, such as digital mammography and tomosynthesis, were not available at the time of the Canadian trial.
“Overall, the Canadian trial appears to be looking at a different group of women than what we typically see in the United States in women diagnosed with breast cancer,” says Dr. Pearlman. “And if they were, then it makes sense that there would be no benefit in mortality, since they were detecting more advanced breast cancers in that population.”
Dr. Pearlman also points to other studies of screening mammography that have produced findings contrasting those of the Canadian trial.
“At least eight large observational trials, case-control studies, and randomized, controlled trials of screening mammography have been published and were later evaluated by meta-analysis.8 That analysis showed a 50% reduction in mortality in women who had screening mammography. In both randomized, controlled trials, it showed a decrease of about 15% in mortality. In practice, looking at large populations of women who died of breast cancer and comparing them to women who had breast cancer but didn’t die, there is a 50% increased likelihood of dying if you don’t have screening mammography. So looking in both directions—both prospectively and retrospectively—there appears to be a substantial benefit to undergoing routine screening mammography in reducing breast cancer mortality,” Dr. Pearlman says.
Dr. Dickinson asserts that criticisms of the Canadian National Breast Screening Study were disproved long ago.
“Many of those accusations were brought out very early in the course of the Canadian trial and investigated in great detail and rejected. After all, this trial was funded by a major research funding body in Canada. And when it was informed that it had funded a ‘fraudulent’ trial, it investigated and found that the findings actually were legitimate,” says Dr. Dickinson.
“I think that the people who are still bringing up those accusations are doing it primarily because the results don’t fit what they wanted. It’s attacking the messenger because they don’t like the results.”
WEIGHING BENEFITS AND HARMS
When the Canadian Task Force on Preventive Health Care formulated its guidelines on screening mammography, it considered the same body of evidence assessed by the USPSTF for its 2009 guidelines. Dr. Dickinson, a member of the Canadian Task Force, notes that the Canadian approach differed from the American approach in several distinct areas.
“We used the USPSTF literature search up to 2008 and then we did an updated search, looking for papers published up to that time. But there were no new trials published from 2008 to 2011,” he says.
“So we looked at the same data but used the GRADE scheme, which carefully separates the strength of the evidence from the strength of the recommendations. It’s a ‘newish’ way of evaluating evidence,” Dr. Dickinson says. “It’s different from the USPSTF approach, which involves a different scale.”
“We used to assess preventive measures purely on the basis of efficacy—if they worked, we’d recommend them. Now we look at the balance of benefits and the potential for causing harm. So it’s not just about whether an intervention works, but about whether it works more than it causes harm,” he says.
“That means that you can have statistically significant benefits that are fairly small and are outweighed by harms. So, while screening mammography can significantly reduce the risk of death from breast cancer by a small amount, our recommendation for it is very weak because, to achieve that benefit, you also incur a lot of harm,” Dr. Dickinson says.
Dr. Pearlman agrees that “mammography is not a perfect test, by any means.”
“It’s inconvenient, people get worried, it’s uncomfortable, and it isn’t perfectly sensitive,” he says. “It’s also somewhat nonspecific, which means that about 10% of women who don’t have breast cancer will be called back for additional images, and about 10% of that group will get called back for a biopsy that is not due to cancer.”
HOW WE COUNSEL OUR PATIENTS
Dr. Kaunitz says he is less likely to recommend annual mammography screening in the wake of the Canadian trial and other findings.
“For decades, we have marched to the drumbeat of ‘mammograms save lives,’” he says. “Annual screens have become an easy recommendation for us to make and, for our patients, the reassurance that accompanies a normal mammogram is comforting. Many patients will be perplexed by this new information; others may view it with suspicion. While we await updated guidance from professional societies, my approach is to encourage patients to follow the 2009 USPSTF guidelines, which recommend that screening start at age 50 in average-risk women and be repeated every 2 years.”
Related articles:
Biennial vs annual mammograpy: How I manage my patients Andrew M. Kaunitz, MD (Commentary, June 2013)
Best age to begin screening mammograms: How I manage my patients Andrew M. Kaunitz, MD (Commentary, November 2013)
Dr. Dickinson takes a similar approach. “I recommend that people be cautious about having screening, but I listen to their stories. Someone may say, ‘My sister had breast cancer and I want a mammogram.’ Overall, I don’t encourage people to undergo mammography unless they have a strong reason for doing so. I try to follow the latest [Canadian] guidelines because I feel they’re based on the best available evidence.”
In contrast, Dr. Pearlman advises his patients according to ACOG guidelines (guidelines that he formulated on ACOG’s behalf), which call for annual screening to begin at age 40.
Dr. Monsees counsels her patients similarly.
“The scientific evidence clearly shows that screening saves the most lives if average-risk women begin annual screening at the age of 40,” she says. “For high-risk women, our recommendations are tailored to each woman’s individual case and made in conjunction with the referring physician. For example, we often begin screening earlier or perform supplemental screening with breast magnetic resonance imaging for women who are at high risk due to prior chest wall radiation or a strong family history.”
“Others have argued against screening average-risk women in their 40s,” Dr. Monsees notes. “But if diagnosed with breast cancer, women in their 40s have more years of life to lose. More than 40% of the years of life lost to breast cancer are among women diagnosed in their 40s. Others also have argued that only high-risk women should be screened in their 40s or yearly after 50. However, that is problematic because more than 75% of women diagnosed with breast cancer each year are not at elevated risk. If you screen only high-risk women you will miss most breast cancers.”13–15
“Mammography screening has been proven to save lives,” Dr. Monsees says. “It can’t find every cancer, and it can’t find every cancer early enough to save all women. Nevertheless, screening should not be abandoned while we are awaiting better screening tests, better pathological markers to differentiate which tumors should be treated more aggressively, and the development of better therapies. The bottom line: Mammography saves lives now, and we should embrace it.”
Dr. Dickinson is more cautious.
“There isn’t a perfect answer,” he says. “That’s the sad thing.”
Related audiocast: Dr. JoAnn V. Pinkerton discusses how she screens patients at increased risk for breast cancer
ACOG's stance
Current ACOG guidelines recommend that annual screening mammography begin at age 40 for women at average risk for breast cancer. Women with an elevated risk of breast cancer require a more complex assessment and thorough counseling and may begin screening even before age 40 in some cases.
We want to hear from you!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty-five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ. 2014;348:g366.
- ObGyns continue to recommend annual mammograms for women beginning at age 40. A look at the Canadian Trial Mammography Study. American College of Obstetricians and Gynecologists. https://www.acog.org/About_ACOG/News_Room/News_Releases/2011/Annual_Mammograms_Now_Recommended_for_Women_Beginning_at_Age_40. Published February 14, 2014. Accessed March 14, 2014.
- Simon S. Canadian study questions mammogram screening; findings unlike those of other studies. American Cancer Society. http://www.cancer.org/cancer/news/news/canadian -study-questions-mammogram-screening-findings-unlike-those-of-other-studies. Published February 12, 2014. Accessed March 14, 2014.
- BMJ article on breast cancer screening effectiveness incredibly flawed and misleading. American College of Radiology. http://www.acr.org/News-Publications/News/News-Articles/2014/ACR/BMJ-Article-on-Breast-Cancer-Screening-Effectiveness-Incredibly-Flawed-and-Misleading. Published February 12, 2014. Accessed March 14, 2014.
- US Preventive Services Task Force. Screening for breast cancer. http://www.uspreventiveservicestaskforce.org/uspstf /uspsbrca.htm. Published December 2009. Accessed March 14, 2014.
- Canadian Cancer Society’s perspective on new mammography study. Canadian Cancer Society. http://www.cancer.ca/en/about-us/for-media/media-releases/national/2014/mammography-study/?region=on. Published February 13, 2014. Accessed March 14, 2014.
- Canadian Task Force on Preventive Health Care. Recommendations on screening for breast cancer in average-risk women aged 40 to 74 years. CMAJ. 2011;183(17):1991–2001.
- Nickson C, Mason KE, English DR, Kavanagh AM. Mammographic screening and breast cancer mortality: a case-control study and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1479–1488.
- Kalager M, Adami H-O, Bretthauer M. Too much mammography. BMJ. 2014;348:g1403.
- Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast cancer mortality in Norway. N Engl J Med. 2010;363(13):1203–1210.
- Autier P, Boniol M, Gavin A, Vatten LJ. Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ. 2011;343:d4411.
- O’Donoghue C, Eklund M, Ozanne EM, Esserman LJ. Aggregate cost of mammography screening in the United States: comparison of current practice and advocated strategies. Ann Intern Med. 2014;160:145–153.
- American Cancer Society. What are the risk factors for breast cancer? January 31, 2014. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-risk-factors. Accessed March 21, 2014.
- National Breast Cancer Coalition: The Breast Cancer Deadline 2020. Myth #8: Most women with breast cancer have a family history of the disease. http://www.breastcancerdeadline2020.org/breast-cancer-information/myths-and-truths/myth-8-most-women-with-bc-have-family-history.html. Accessed March 21, 2014.
- Berg WA. Benefits of screening mammography. JAMA. 2010;303(2):168–169.
- Woodworth KA. Breast imaging through the ages: a historical review and future outlook. eradimaging. September 6, 2011. http://www.eradimaging.com/site/article.cfm?ID=769#.UzAv79ySuMM. Accessed March 24, 2014.
When 25-year follow-up data from the Canadian National Breast Screening Study—published earlier this year—showed no benefit for annual mammography in women aged 40 to 59 years, the findings generated renewed debate about whether screening mammography actually saves lives.1
In that study, Miller and colleagues continued their follow-up of almost 90,000 women who had been randomly assigned to mammography (five annual screens) or no mammography from 1980 to 1985. Women aged 40 to 49 in the mammography arm and all women aged 50 to 69 underwent annual clinical breast examination (CBE). Women aged 40 to 49 in the control arm had a single CBE and continued usual care in the community. The main outcome measure was death from breast cancer.1
During the entire 25-year study, 3,250 women in the mammography arm were given a diagnosis of breast cancer, and 3,133 in the control arm received the same diagnosis. Of these, 500 and 505 women, respectively, died of the malignancy.
The overall hazard ratio for death from breast cancer in the mammography and control arms was 0.99 (95% confidence interval, 0.88–1.12). After 15 years of follow-up, 106 residual excess cancers (106/484; or 22%) were identified in the mammography arm and were attributed to “overdiagnosis.”1
During the screening period the mean size of breast cancers identified was 1.91 cm and 2.10 cm in the mammography and control arms, respectively (P = .01), and 30.6% and 32.4% of tumors, respectively, were associated with positive lymph nodes (P = .53).
PROFESSIONAL SOCIETIES STICK BY THEIR GUIDELINES
Following publication of the Canadian findings, the American College of Obstetricians and Gynecologists (ACOG) reaffirmed its recommendation for women at average risk for breast cancer to initiate annual screening at age 40. In an announcement issued February 14, 2014, ACOG noted that it had “a number of concerns” with the Canadian study.2
Similarly, the American Cancer Society reiterated its own recommendation that women aged 40 and older undergo annual mammography and CBE for as long as they remain healthy.3
The American College of Radiology went a few steps further, calling the Canadian study “incredibly flawed and misleading.”4 Its guidelines call for annual mammography beginning at age 40.
The US Preventive Services Task Force (USPSTF) 2009 guidelines on breast cancer screening also stand, with biennial mammography beginning at age 50 for women at average risk for breast cancer.5
The Canadian Cancer Society also reaffirmed its recommendations for breast cancer screening following publication of the Canadian trial 25-year follow-up data—although its recommendations call for screening to begin at age 50 and to be repeated thereafter at 2- to 3-year intervals.6,7
In short, nothing has changed…yet. But the Canadian trial raises a number of questions about breast cancer screening—and the answers aren’t as clear-cut as you might imagine.
IS THE CANADIAN TRIAL CREDIBLE?
Results from earlier randomized, controlled trials have indicated that screening mammography reduces death from breast cancer.
“The Canadian study is an outlier,” says Barbara Monsees, MD, Ronald and Hanna Evens Professor of Women’s Health in the department of radiology at Washington University in St. Louis, Missouri.
“There is an overwhelming amount of evidence that tells us that screening mammography saves lives,” says Dr. Monsees. “This evidence includes other randomized trials, case-control studies, results of organized screening programs, and downward trends in breast cancer deaths where screening is used.”
Mark D. Pearlman, MD, also believes the body of evidence shows that screening mammography is effective. Dr. Pearlman is vice chair and service chief in the division of obstetrics and gynecology and professor of surgery and director of the breast fellowship in obstetrics and gynecology at the University of Michigan Health System in Ann Arbor, Michigan. He has been on the surgical staff of the Breast Care Center there since 1990, with expertise in the management of women with breast disease and increased genetic risks for breast and ovarian cancer.
The Canadian trial is “a reasonably done study,” he says, “but there are some concerns. First, it’s not a new study—it was initially published 22 years ago. This latest publication is just a continuation of following these women.”
“This study, along with seven other randomized, controlled trials, was considered by the USPSTF in formulating its 2009 recommendations. In that meta-analysis, which included women in their 40s, screening mammography had benefit in every decade of life of interest.8 That is the basis on which ACOG made its recommendation for women at average risk to start annual screening at age 40 and continue at least until age 70,” Dr. Pearlman says. “When the USPSTF considered this negative study, it realized that there is benefit for mammography despite this single trial.”
Related article: Which women are most likely to die from breast cancer—those screened annually starting at age 40, biennially starting at age 50, or not at all? Mark D. Pearlman, MD (Examining the Evidence, November 2013)
James Dickinson, MBBS, PhD, a family physician and member of the Canadian Task Force on Preventive Health Care (a forerunner of the USPSTF), which has published its own set of guidelines on breast cancer screening, has a different perspective. Dr. Dickinson teaches at the University of Calgary in Alberta.
“One of the tendencies—particularly in medicine driven by commercial interests—is that as soon as there is even the slightest hint that something is worthwhile, there’s a rush to have everybody do it and make lots of profit from it. People don’t wait for the evidence. They jump to assume guilt or innocence without even looking for the evidence.”
“I give all credit to the Canadian trial investigators,” Dr. Dickinson says. “The world had jumped ahead of them and just assumed that breast screening worked. But they kept looking. They set up a good trial to start with and then followed it through and helped us understand that things aren’t as good as we would like them to be.”
Andrew M. Kaunitz, MD, professor and vice chair of obstetrics and gynecology at the University of Florida–Jacksonville also believes that the Canadian study’s findings are reliable. Dr. Kaunitz serves on the OBG Management Board of Editors.
“As pointed out in an editorial accompanying the Canadian trial, this study’s findings of a lack of efficacy of screening mammograms are ‘strikingly similar’ to other recent studies assessing breast cancer screening.”9–11
“Further, mammograms are costly and associated with a high rate of false-positive findings,” Dr. Kaunitz says.
“Too many weak links”
Among the main criticisms of the Canadian trial is a claim of flawed methodology.
“The Canadian trial is an update of a flawed study that was previously discredited for good reasons,” says Dr. Monsees. “In short, the quality of the mammograms was poor, and the overall study design did not reflect a true randomization process.”
“For example, true randomization requires eligible patients to be randomly divided into two or more groups, without any knowledge of their specific conditions that might bias trial results,” Dr. Monsees explains. “In the most valid randomized trials, this was accomplished by invitation. Without knowing anything about the women, investigators randomly assigned them to a group invited to be screened and a group not invited. In this manner, two equal groups were produced, with no way to corrupt the randomization process.”
“In the Canadian National Breast Screening Study, in contrast, once the women volunteered, they were given a clinical breast examination, and women with breast lumps and large lymph nodes in their underarms were identified. This information was provided to study coordinators, who assigned women on open lists to the mammography group or the control group,” Dr. Monsees says.
“Those of us in the imaging field know that the quality of mammography is only as good as the weakest link in the imaging chain. This study had far too many weak links. These criticisms are not new; they were raised during and after the trial and remain valid today.”
Dr. Pearlman does not believe that the Canadian trial reflects modern breast cancer screening.
“There are things in the Canadian trial that differ from what we see in modern mammography,” he says. “In the Canadian trial, in women diagnosed with breast cancer, they noted whether there was a palpable mass in the area of cancer. In the Canadian trial the percentage of palpable masses was approximately 66%, and that’s very very different from what we see with modern mammography. In current practice, about 15% of breast cancers diagnosed by mammography are palpable. And so it appears that, for some reason, they were seeing more advanced breast cancers when they were screening by mammography.”
Another concern focuses on the technology used in the trial.
“It appears that the Canadian investigators pulled old machines into service for the trial,” Dr. Pearlman says.
In addition, more recent advances, such as digital mammography and tomosynthesis, were not available at the time of the Canadian trial.
“Overall, the Canadian trial appears to be looking at a different group of women than what we typically see in the United States in women diagnosed with breast cancer,” says Dr. Pearlman. “And if they were, then it makes sense that there would be no benefit in mortality, since they were detecting more advanced breast cancers in that population.”
Dr. Pearlman also points to other studies of screening mammography that have produced findings contrasting those of the Canadian trial.
“At least eight large observational trials, case-control studies, and randomized, controlled trials of screening mammography have been published and were later evaluated by meta-analysis.8 That analysis showed a 50% reduction in mortality in women who had screening mammography. In both randomized, controlled trials, it showed a decrease of about 15% in mortality. In practice, looking at large populations of women who died of breast cancer and comparing them to women who had breast cancer but didn’t die, there is a 50% increased likelihood of dying if you don’t have screening mammography. So looking in both directions—both prospectively and retrospectively—there appears to be a substantial benefit to undergoing routine screening mammography in reducing breast cancer mortality,” Dr. Pearlman says.
Dr. Dickinson asserts that criticisms of the Canadian National Breast Screening Study were disproved long ago.
“Many of those accusations were brought out very early in the course of the Canadian trial and investigated in great detail and rejected. After all, this trial was funded by a major research funding body in Canada. And when it was informed that it had funded a ‘fraudulent’ trial, it investigated and found that the findings actually were legitimate,” says Dr. Dickinson.
“I think that the people who are still bringing up those accusations are doing it primarily because the results don’t fit what they wanted. It’s attacking the messenger because they don’t like the results.”
WEIGHING BENEFITS AND HARMS
When the Canadian Task Force on Preventive Health Care formulated its guidelines on screening mammography, it considered the same body of evidence assessed by the USPSTF for its 2009 guidelines. Dr. Dickinson, a member of the Canadian Task Force, notes that the Canadian approach differed from the American approach in several distinct areas.
“We used the USPSTF literature search up to 2008 and then we did an updated search, looking for papers published up to that time. But there were no new trials published from 2008 to 2011,” he says.
“So we looked at the same data but used the GRADE scheme, which carefully separates the strength of the evidence from the strength of the recommendations. It’s a ‘newish’ way of evaluating evidence,” Dr. Dickinson says. “It’s different from the USPSTF approach, which involves a different scale.”
“We used to assess preventive measures purely on the basis of efficacy—if they worked, we’d recommend them. Now we look at the balance of benefits and the potential for causing harm. So it’s not just about whether an intervention works, but about whether it works more than it causes harm,” he says.
“That means that you can have statistically significant benefits that are fairly small and are outweighed by harms. So, while screening mammography can significantly reduce the risk of death from breast cancer by a small amount, our recommendation for it is very weak because, to achieve that benefit, you also incur a lot of harm,” Dr. Dickinson says.
Dr. Pearlman agrees that “mammography is not a perfect test, by any means.”
“It’s inconvenient, people get worried, it’s uncomfortable, and it isn’t perfectly sensitive,” he says. “It’s also somewhat nonspecific, which means that about 10% of women who don’t have breast cancer will be called back for additional images, and about 10% of that group will get called back for a biopsy that is not due to cancer.”
HOW WE COUNSEL OUR PATIENTS
Dr. Kaunitz says he is less likely to recommend annual mammography screening in the wake of the Canadian trial and other findings.
“For decades, we have marched to the drumbeat of ‘mammograms save lives,’” he says. “Annual screens have become an easy recommendation for us to make and, for our patients, the reassurance that accompanies a normal mammogram is comforting. Many patients will be perplexed by this new information; others may view it with suspicion. While we await updated guidance from professional societies, my approach is to encourage patients to follow the 2009 USPSTF guidelines, which recommend that screening start at age 50 in average-risk women and be repeated every 2 years.”
Related articles:
Biennial vs annual mammograpy: How I manage my patients Andrew M. Kaunitz, MD (Commentary, June 2013)
Best age to begin screening mammograms: How I manage my patients Andrew M. Kaunitz, MD (Commentary, November 2013)
Dr. Dickinson takes a similar approach. “I recommend that people be cautious about having screening, but I listen to their stories. Someone may say, ‘My sister had breast cancer and I want a mammogram.’ Overall, I don’t encourage people to undergo mammography unless they have a strong reason for doing so. I try to follow the latest [Canadian] guidelines because I feel they’re based on the best available evidence.”
In contrast, Dr. Pearlman advises his patients according to ACOG guidelines (guidelines that he formulated on ACOG’s behalf), which call for annual screening to begin at age 40.
Dr. Monsees counsels her patients similarly.
“The scientific evidence clearly shows that screening saves the most lives if average-risk women begin annual screening at the age of 40,” she says. “For high-risk women, our recommendations are tailored to each woman’s individual case and made in conjunction with the referring physician. For example, we often begin screening earlier or perform supplemental screening with breast magnetic resonance imaging for women who are at high risk due to prior chest wall radiation or a strong family history.”
“Others have argued against screening average-risk women in their 40s,” Dr. Monsees notes. “But if diagnosed with breast cancer, women in their 40s have more years of life to lose. More than 40% of the years of life lost to breast cancer are among women diagnosed in their 40s. Others also have argued that only high-risk women should be screened in their 40s or yearly after 50. However, that is problematic because more than 75% of women diagnosed with breast cancer each year are not at elevated risk. If you screen only high-risk women you will miss most breast cancers.”13–15
“Mammography screening has been proven to save lives,” Dr. Monsees says. “It can’t find every cancer, and it can’t find every cancer early enough to save all women. Nevertheless, screening should not be abandoned while we are awaiting better screening tests, better pathological markers to differentiate which tumors should be treated more aggressively, and the development of better therapies. The bottom line: Mammography saves lives now, and we should embrace it.”
Dr. Dickinson is more cautious.
“There isn’t a perfect answer,” he says. “That’s the sad thing.”
Related audiocast: Dr. JoAnn V. Pinkerton discusses how she screens patients at increased risk for breast cancer
ACOG's stance
Current ACOG guidelines recommend that annual screening mammography begin at age 40 for women at average risk for breast cancer. Women with an elevated risk of breast cancer require a more complex assessment and thorough counseling and may begin screening even before age 40 in some cases.
We want to hear from you!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
When 25-year follow-up data from the Canadian National Breast Screening Study—published earlier this year—showed no benefit for annual mammography in women aged 40 to 59 years, the findings generated renewed debate about whether screening mammography actually saves lives.1
In that study, Miller and colleagues continued their follow-up of almost 90,000 women who had been randomly assigned to mammography (five annual screens) or no mammography from 1980 to 1985. Women aged 40 to 49 in the mammography arm and all women aged 50 to 69 underwent annual clinical breast examination (CBE). Women aged 40 to 49 in the control arm had a single CBE and continued usual care in the community. The main outcome measure was death from breast cancer.1
During the entire 25-year study, 3,250 women in the mammography arm were given a diagnosis of breast cancer, and 3,133 in the control arm received the same diagnosis. Of these, 500 and 505 women, respectively, died of the malignancy.
The overall hazard ratio for death from breast cancer in the mammography and control arms was 0.99 (95% confidence interval, 0.88–1.12). After 15 years of follow-up, 106 residual excess cancers (106/484; or 22%) were identified in the mammography arm and were attributed to “overdiagnosis.”1
During the screening period the mean size of breast cancers identified was 1.91 cm and 2.10 cm in the mammography and control arms, respectively (P = .01), and 30.6% and 32.4% of tumors, respectively, were associated with positive lymph nodes (P = .53).
PROFESSIONAL SOCIETIES STICK BY THEIR GUIDELINES
Following publication of the Canadian findings, the American College of Obstetricians and Gynecologists (ACOG) reaffirmed its recommendation for women at average risk for breast cancer to initiate annual screening at age 40. In an announcement issued February 14, 2014, ACOG noted that it had “a number of concerns” with the Canadian study.2
Similarly, the American Cancer Society reiterated its own recommendation that women aged 40 and older undergo annual mammography and CBE for as long as they remain healthy.3
The American College of Radiology went a few steps further, calling the Canadian study “incredibly flawed and misleading.”4 Its guidelines call for annual mammography beginning at age 40.
The US Preventive Services Task Force (USPSTF) 2009 guidelines on breast cancer screening also stand, with biennial mammography beginning at age 50 for women at average risk for breast cancer.5
The Canadian Cancer Society also reaffirmed its recommendations for breast cancer screening following publication of the Canadian trial 25-year follow-up data—although its recommendations call for screening to begin at age 50 and to be repeated thereafter at 2- to 3-year intervals.6,7
In short, nothing has changed…yet. But the Canadian trial raises a number of questions about breast cancer screening—and the answers aren’t as clear-cut as you might imagine.
IS THE CANADIAN TRIAL CREDIBLE?
Results from earlier randomized, controlled trials have indicated that screening mammography reduces death from breast cancer.
“The Canadian study is an outlier,” says Barbara Monsees, MD, Ronald and Hanna Evens Professor of Women’s Health in the department of radiology at Washington University in St. Louis, Missouri.
“There is an overwhelming amount of evidence that tells us that screening mammography saves lives,” says Dr. Monsees. “This evidence includes other randomized trials, case-control studies, results of organized screening programs, and downward trends in breast cancer deaths where screening is used.”
Mark D. Pearlman, MD, also believes the body of evidence shows that screening mammography is effective. Dr. Pearlman is vice chair and service chief in the division of obstetrics and gynecology and professor of surgery and director of the breast fellowship in obstetrics and gynecology at the University of Michigan Health System in Ann Arbor, Michigan. He has been on the surgical staff of the Breast Care Center there since 1990, with expertise in the management of women with breast disease and increased genetic risks for breast and ovarian cancer.
The Canadian trial is “a reasonably done study,” he says, “but there are some concerns. First, it’s not a new study—it was initially published 22 years ago. This latest publication is just a continuation of following these women.”
“This study, along with seven other randomized, controlled trials, was considered by the USPSTF in formulating its 2009 recommendations. In that meta-analysis, which included women in their 40s, screening mammography had benefit in every decade of life of interest.8 That is the basis on which ACOG made its recommendation for women at average risk to start annual screening at age 40 and continue at least until age 70,” Dr. Pearlman says. “When the USPSTF considered this negative study, it realized that there is benefit for mammography despite this single trial.”
Related article: Which women are most likely to die from breast cancer—those screened annually starting at age 40, biennially starting at age 50, or not at all? Mark D. Pearlman, MD (Examining the Evidence, November 2013)
James Dickinson, MBBS, PhD, a family physician and member of the Canadian Task Force on Preventive Health Care (a forerunner of the USPSTF), which has published its own set of guidelines on breast cancer screening, has a different perspective. Dr. Dickinson teaches at the University of Calgary in Alberta.
“One of the tendencies—particularly in medicine driven by commercial interests—is that as soon as there is even the slightest hint that something is worthwhile, there’s a rush to have everybody do it and make lots of profit from it. People don’t wait for the evidence. They jump to assume guilt or innocence without even looking for the evidence.”
“I give all credit to the Canadian trial investigators,” Dr. Dickinson says. “The world had jumped ahead of them and just assumed that breast screening worked. But they kept looking. They set up a good trial to start with and then followed it through and helped us understand that things aren’t as good as we would like them to be.”
Andrew M. Kaunitz, MD, professor and vice chair of obstetrics and gynecology at the University of Florida–Jacksonville also believes that the Canadian study’s findings are reliable. Dr. Kaunitz serves on the OBG Management Board of Editors.
“As pointed out in an editorial accompanying the Canadian trial, this study’s findings of a lack of efficacy of screening mammograms are ‘strikingly similar’ to other recent studies assessing breast cancer screening.”9–11
“Further, mammograms are costly and associated with a high rate of false-positive findings,” Dr. Kaunitz says.
“Too many weak links”
Among the main criticisms of the Canadian trial is a claim of flawed methodology.
“The Canadian trial is an update of a flawed study that was previously discredited for good reasons,” says Dr. Monsees. “In short, the quality of the mammograms was poor, and the overall study design did not reflect a true randomization process.”
“For example, true randomization requires eligible patients to be randomly divided into two or more groups, without any knowledge of their specific conditions that might bias trial results,” Dr. Monsees explains. “In the most valid randomized trials, this was accomplished by invitation. Without knowing anything about the women, investigators randomly assigned them to a group invited to be screened and a group not invited. In this manner, two equal groups were produced, with no way to corrupt the randomization process.”
“In the Canadian National Breast Screening Study, in contrast, once the women volunteered, they were given a clinical breast examination, and women with breast lumps and large lymph nodes in their underarms were identified. This information was provided to study coordinators, who assigned women on open lists to the mammography group or the control group,” Dr. Monsees says.
“Those of us in the imaging field know that the quality of mammography is only as good as the weakest link in the imaging chain. This study had far too many weak links. These criticisms are not new; they were raised during and after the trial and remain valid today.”
Dr. Pearlman does not believe that the Canadian trial reflects modern breast cancer screening.
“There are things in the Canadian trial that differ from what we see in modern mammography,” he says. “In the Canadian trial, in women diagnosed with breast cancer, they noted whether there was a palpable mass in the area of cancer. In the Canadian trial the percentage of palpable masses was approximately 66%, and that’s very very different from what we see with modern mammography. In current practice, about 15% of breast cancers diagnosed by mammography are palpable. And so it appears that, for some reason, they were seeing more advanced breast cancers when they were screening by mammography.”
Another concern focuses on the technology used in the trial.
“It appears that the Canadian investigators pulled old machines into service for the trial,” Dr. Pearlman says.
In addition, more recent advances, such as digital mammography and tomosynthesis, were not available at the time of the Canadian trial.
“Overall, the Canadian trial appears to be looking at a different group of women than what we typically see in the United States in women diagnosed with breast cancer,” says Dr. Pearlman. “And if they were, then it makes sense that there would be no benefit in mortality, since they were detecting more advanced breast cancers in that population.”
Dr. Pearlman also points to other studies of screening mammography that have produced findings contrasting those of the Canadian trial.
“At least eight large observational trials, case-control studies, and randomized, controlled trials of screening mammography have been published and were later evaluated by meta-analysis.8 That analysis showed a 50% reduction in mortality in women who had screening mammography. In both randomized, controlled trials, it showed a decrease of about 15% in mortality. In practice, looking at large populations of women who died of breast cancer and comparing them to women who had breast cancer but didn’t die, there is a 50% increased likelihood of dying if you don’t have screening mammography. So looking in both directions—both prospectively and retrospectively—there appears to be a substantial benefit to undergoing routine screening mammography in reducing breast cancer mortality,” Dr. Pearlman says.
Dr. Dickinson asserts that criticisms of the Canadian National Breast Screening Study were disproved long ago.
“Many of those accusations were brought out very early in the course of the Canadian trial and investigated in great detail and rejected. After all, this trial was funded by a major research funding body in Canada. And when it was informed that it had funded a ‘fraudulent’ trial, it investigated and found that the findings actually were legitimate,” says Dr. Dickinson.
“I think that the people who are still bringing up those accusations are doing it primarily because the results don’t fit what they wanted. It’s attacking the messenger because they don’t like the results.”
WEIGHING BENEFITS AND HARMS
When the Canadian Task Force on Preventive Health Care formulated its guidelines on screening mammography, it considered the same body of evidence assessed by the USPSTF for its 2009 guidelines. Dr. Dickinson, a member of the Canadian Task Force, notes that the Canadian approach differed from the American approach in several distinct areas.
“We used the USPSTF literature search up to 2008 and then we did an updated search, looking for papers published up to that time. But there were no new trials published from 2008 to 2011,” he says.
“So we looked at the same data but used the GRADE scheme, which carefully separates the strength of the evidence from the strength of the recommendations. It’s a ‘newish’ way of evaluating evidence,” Dr. Dickinson says. “It’s different from the USPSTF approach, which involves a different scale.”
“We used to assess preventive measures purely on the basis of efficacy—if they worked, we’d recommend them. Now we look at the balance of benefits and the potential for causing harm. So it’s not just about whether an intervention works, but about whether it works more than it causes harm,” he says.
“That means that you can have statistically significant benefits that are fairly small and are outweighed by harms. So, while screening mammography can significantly reduce the risk of death from breast cancer by a small amount, our recommendation for it is very weak because, to achieve that benefit, you also incur a lot of harm,” Dr. Dickinson says.
Dr. Pearlman agrees that “mammography is not a perfect test, by any means.”
“It’s inconvenient, people get worried, it’s uncomfortable, and it isn’t perfectly sensitive,” he says. “It’s also somewhat nonspecific, which means that about 10% of women who don’t have breast cancer will be called back for additional images, and about 10% of that group will get called back for a biopsy that is not due to cancer.”
HOW WE COUNSEL OUR PATIENTS
Dr. Kaunitz says he is less likely to recommend annual mammography screening in the wake of the Canadian trial and other findings.
“For decades, we have marched to the drumbeat of ‘mammograms save lives,’” he says. “Annual screens have become an easy recommendation for us to make and, for our patients, the reassurance that accompanies a normal mammogram is comforting. Many patients will be perplexed by this new information; others may view it with suspicion. While we await updated guidance from professional societies, my approach is to encourage patients to follow the 2009 USPSTF guidelines, which recommend that screening start at age 50 in average-risk women and be repeated every 2 years.”
Related articles:
Biennial vs annual mammograpy: How I manage my patients Andrew M. Kaunitz, MD (Commentary, June 2013)
Best age to begin screening mammograms: How I manage my patients Andrew M. Kaunitz, MD (Commentary, November 2013)
Dr. Dickinson takes a similar approach. “I recommend that people be cautious about having screening, but I listen to their stories. Someone may say, ‘My sister had breast cancer and I want a mammogram.’ Overall, I don’t encourage people to undergo mammography unless they have a strong reason for doing so. I try to follow the latest [Canadian] guidelines because I feel they’re based on the best available evidence.”
In contrast, Dr. Pearlman advises his patients according to ACOG guidelines (guidelines that he formulated on ACOG’s behalf), which call for annual screening to begin at age 40.
Dr. Monsees counsels her patients similarly.
“The scientific evidence clearly shows that screening saves the most lives if average-risk women begin annual screening at the age of 40,” she says. “For high-risk women, our recommendations are tailored to each woman’s individual case and made in conjunction with the referring physician. For example, we often begin screening earlier or perform supplemental screening with breast magnetic resonance imaging for women who are at high risk due to prior chest wall radiation or a strong family history.”
“Others have argued against screening average-risk women in their 40s,” Dr. Monsees notes. “But if diagnosed with breast cancer, women in their 40s have more years of life to lose. More than 40% of the years of life lost to breast cancer are among women diagnosed in their 40s. Others also have argued that only high-risk women should be screened in their 40s or yearly after 50. However, that is problematic because more than 75% of women diagnosed with breast cancer each year are not at elevated risk. If you screen only high-risk women you will miss most breast cancers.”13–15
“Mammography screening has been proven to save lives,” Dr. Monsees says. “It can’t find every cancer, and it can’t find every cancer early enough to save all women. Nevertheless, screening should not be abandoned while we are awaiting better screening tests, better pathological markers to differentiate which tumors should be treated more aggressively, and the development of better therapies. The bottom line: Mammography saves lives now, and we should embrace it.”
Dr. Dickinson is more cautious.
“There isn’t a perfect answer,” he says. “That’s the sad thing.”
Related audiocast: Dr. JoAnn V. Pinkerton discusses how she screens patients at increased risk for breast cancer
ACOG's stance
Current ACOG guidelines recommend that annual screening mammography begin at age 40 for women at average risk for breast cancer. Women with an elevated risk of breast cancer require a more complex assessment and thorough counseling and may begin screening even before age 40 in some cases.
We want to hear from you!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue. Send your letter to: obg@frontlinemedcom.com Please include the city and state in which you practice. Stay in touch! Your feedback is important to us!
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty-five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ. 2014;348:g366.
- ObGyns continue to recommend annual mammograms for women beginning at age 40. A look at the Canadian Trial Mammography Study. American College of Obstetricians and Gynecologists. https://www.acog.org/About_ACOG/News_Room/News_Releases/2011/Annual_Mammograms_Now_Recommended_for_Women_Beginning_at_Age_40. Published February 14, 2014. Accessed March 14, 2014.
- Simon S. Canadian study questions mammogram screening; findings unlike those of other studies. American Cancer Society. http://www.cancer.org/cancer/news/news/canadian -study-questions-mammogram-screening-findings-unlike-those-of-other-studies. Published February 12, 2014. Accessed March 14, 2014.
- BMJ article on breast cancer screening effectiveness incredibly flawed and misleading. American College of Radiology. http://www.acr.org/News-Publications/News/News-Articles/2014/ACR/BMJ-Article-on-Breast-Cancer-Screening-Effectiveness-Incredibly-Flawed-and-Misleading. Published February 12, 2014. Accessed March 14, 2014.
- US Preventive Services Task Force. Screening for breast cancer. http://www.uspreventiveservicestaskforce.org/uspstf /uspsbrca.htm. Published December 2009. Accessed March 14, 2014.
- Canadian Cancer Society’s perspective on new mammography study. Canadian Cancer Society. http://www.cancer.ca/en/about-us/for-media/media-releases/national/2014/mammography-study/?region=on. Published February 13, 2014. Accessed March 14, 2014.
- Canadian Task Force on Preventive Health Care. Recommendations on screening for breast cancer in average-risk women aged 40 to 74 years. CMAJ. 2011;183(17):1991–2001.
- Nickson C, Mason KE, English DR, Kavanagh AM. Mammographic screening and breast cancer mortality: a case-control study and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1479–1488.
- Kalager M, Adami H-O, Bretthauer M. Too much mammography. BMJ. 2014;348:g1403.
- Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast cancer mortality in Norway. N Engl J Med. 2010;363(13):1203–1210.
- Autier P, Boniol M, Gavin A, Vatten LJ. Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ. 2011;343:d4411.
- O’Donoghue C, Eklund M, Ozanne EM, Esserman LJ. Aggregate cost of mammography screening in the United States: comparison of current practice and advocated strategies. Ann Intern Med. 2014;160:145–153.
- American Cancer Society. What are the risk factors for breast cancer? January 31, 2014. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-risk-factors. Accessed March 21, 2014.
- National Breast Cancer Coalition: The Breast Cancer Deadline 2020. Myth #8: Most women with breast cancer have a family history of the disease. http://www.breastcancerdeadline2020.org/breast-cancer-information/myths-and-truths/myth-8-most-women-with-bc-have-family-history.html. Accessed March 21, 2014.
- Berg WA. Benefits of screening mammography. JAMA. 2010;303(2):168–169.
- Woodworth KA. Breast imaging through the ages: a historical review and future outlook. eradimaging. September 6, 2011. http://www.eradimaging.com/site/article.cfm?ID=769#.UzAv79ySuMM. Accessed March 24, 2014.
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty-five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ. 2014;348:g366.
- ObGyns continue to recommend annual mammograms for women beginning at age 40. A look at the Canadian Trial Mammography Study. American College of Obstetricians and Gynecologists. https://www.acog.org/About_ACOG/News_Room/News_Releases/2011/Annual_Mammograms_Now_Recommended_for_Women_Beginning_at_Age_40. Published February 14, 2014. Accessed March 14, 2014.
- Simon S. Canadian study questions mammogram screening; findings unlike those of other studies. American Cancer Society. http://www.cancer.org/cancer/news/news/canadian -study-questions-mammogram-screening-findings-unlike-those-of-other-studies. Published February 12, 2014. Accessed March 14, 2014.
- BMJ article on breast cancer screening effectiveness incredibly flawed and misleading. American College of Radiology. http://www.acr.org/News-Publications/News/News-Articles/2014/ACR/BMJ-Article-on-Breast-Cancer-Screening-Effectiveness-Incredibly-Flawed-and-Misleading. Published February 12, 2014. Accessed March 14, 2014.
- US Preventive Services Task Force. Screening for breast cancer. http://www.uspreventiveservicestaskforce.org/uspstf /uspsbrca.htm. Published December 2009. Accessed March 14, 2014.
- Canadian Cancer Society’s perspective on new mammography study. Canadian Cancer Society. http://www.cancer.ca/en/about-us/for-media/media-releases/national/2014/mammography-study/?region=on. Published February 13, 2014. Accessed March 14, 2014.
- Canadian Task Force on Preventive Health Care. Recommendations on screening for breast cancer in average-risk women aged 40 to 74 years. CMAJ. 2011;183(17):1991–2001.
- Nickson C, Mason KE, English DR, Kavanagh AM. Mammographic screening and breast cancer mortality: a case-control study and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1479–1488.
- Kalager M, Adami H-O, Bretthauer M. Too much mammography. BMJ. 2014;348:g1403.
- Kalager M, Zelen M, Langmark F, Adami HO. Effect of screening mammography on breast cancer mortality in Norway. N Engl J Med. 2010;363(13):1203–1210.
- Autier P, Boniol M, Gavin A, Vatten LJ. Breast cancer mortality in neighbouring European countries with different levels of screening but similar access to treatment: trend analysis of WHO mortality database. BMJ. 2011;343:d4411.
- O’Donoghue C, Eklund M, Ozanne EM, Esserman LJ. Aggregate cost of mammography screening in the United States: comparison of current practice and advocated strategies. Ann Intern Med. 2014;160:145–153.
- American Cancer Society. What are the risk factors for breast cancer? January 31, 2014. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-risk-factors. Accessed March 21, 2014.
- National Breast Cancer Coalition: The Breast Cancer Deadline 2020. Myth #8: Most women with breast cancer have a family history of the disease. http://www.breastcancerdeadline2020.org/breast-cancer-information/myths-and-truths/myth-8-most-women-with-bc-have-family-history.html. Accessed March 21, 2014.
- Berg WA. Benefits of screening mammography. JAMA. 2010;303(2):168–169.
- Woodworth KA. Breast imaging through the ages: a historical review and future outlook. eradimaging. September 6, 2011. http://www.eradimaging.com/site/article.cfm?ID=769#.UzAv79ySuMM. Accessed March 24, 2014.
Risk of fetal death is increased in pregnant women with pre-existing diabetes
Women who enter pregnancy with diabetes are 4.5 times more likely to experience fetal death and almost twice as likely to lose their infant in the first year of life, compared with women without diabetes, a new study shows.1
Although previous investigations have explored the link between pre-existing maternal diabetes and fetal and infant death, they have not excluded congenital anomalies as a cause of death. In this newest study, Tennant and colleagues used data from several longstanding population-based registries in the north of England to explore the link in offspring without congenital anomalies.
Details of the study
Tennant and colleagues included all normally formed singleton offspring of women with pre-existing diabetes (1,206 with type 1 diabetes and 342 with type 2 diabetes) in the North of England from 1996 to 2008 in their study. Information on these pregnancies came from the Northern Diabetes in Pregnancy Survey. The relative risks (RR) of fetal death (death of a fetus at or after 20 weeks’ gestation) and infant death (death during the first year of life) were estimated by comparing these data with population data from the Northern Perinatal Morbidity and Mortality Survey.
The RR of fetal death in pregnancies marked by preexisting diabetes was 4.56, and it was 1.86 for infant death, compared with pregnancies without diabetes. These risks did not vary between women with type 1 diabetes and those with type 2 diabetes. Other variables associated with a higher risk of fetal or infant death were glycated hemoglobin levels greater than 6.6%, prepregnancy retinopathy, and a lack of folic acid supplementation.
The prevalence of fetal death was 3% in women with preexisting diabetes, and the prevalence of infant death was 0.7%, compared with 0.7% and 0.4%, respectively, in women without diabetes.
Tennant and colleagues found no evidence that the risk of fetal and infant death associated with preexisting maternal diabetes had decreased over time, or that the relative risk of stillbirth varied by gestational age.
The average glycated hemoglobin level in the study was 7.8%. The target for glycated hemoglobin is 7% according to the American Diabetes Association (ADA) and 6.1% according to England’s National Institute for Health and Care Excellence (NICE). Tennant and colleagues estimate that the prevalence of fetal and infant death would have been about 40% lower if the women in their study had achieved either the ADA or NICE target.
Related Article: Does myoinositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
Clinical recommendations
“It’s disappointing to see so little improvement because, with the right care, most women with diabetes can—and will—have a healthy baby,” the authors commented. “Stillbirths and infant deaths are thankfully not common, but they could be even less common if all women with diabetes can be helped to achieve the best possible control of their blood glucose levels.”
“We already know that folic acid reduces the risk of certain congenital anomalies, such as spina bifida or cleft lip, which is why women with diabetes are advised to take high-dose supplements of 5 mg daily. These are available on prescription and should be taken for at least 3 months before conceiving. Our results suggest this simple action may also help to reduce the risk of stillbirth or infant death, even in babies without these conditions.”
Related Article: Does folic acid supplementation have long-term benefit to offspring? Paul L. Ogburn, Jr, MD (Examining the Evidence, January 2012)
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Reference
- Tennant PW, Glinianaia SV, Bilous RW, Rankin J, Bell R. Pre-existing diabetes, maternal glycated haemoglobin, and the risks of fetal and infant death: a population-based study. Diabetologia. 2014;57(2):285–294.
Women who enter pregnancy with diabetes are 4.5 times more likely to experience fetal death and almost twice as likely to lose their infant in the first year of life, compared with women without diabetes, a new study shows.1
Although previous investigations have explored the link between pre-existing maternal diabetes and fetal and infant death, they have not excluded congenital anomalies as a cause of death. In this newest study, Tennant and colleagues used data from several longstanding population-based registries in the north of England to explore the link in offspring without congenital anomalies.
Details of the study
Tennant and colleagues included all normally formed singleton offspring of women with pre-existing diabetes (1,206 with type 1 diabetes and 342 with type 2 diabetes) in the North of England from 1996 to 2008 in their study. Information on these pregnancies came from the Northern Diabetes in Pregnancy Survey. The relative risks (RR) of fetal death (death of a fetus at or after 20 weeks’ gestation) and infant death (death during the first year of life) were estimated by comparing these data with population data from the Northern Perinatal Morbidity and Mortality Survey.
The RR of fetal death in pregnancies marked by preexisting diabetes was 4.56, and it was 1.86 for infant death, compared with pregnancies without diabetes. These risks did not vary between women with type 1 diabetes and those with type 2 diabetes. Other variables associated with a higher risk of fetal or infant death were glycated hemoglobin levels greater than 6.6%, prepregnancy retinopathy, and a lack of folic acid supplementation.
The prevalence of fetal death was 3% in women with preexisting diabetes, and the prevalence of infant death was 0.7%, compared with 0.7% and 0.4%, respectively, in women without diabetes.
Tennant and colleagues found no evidence that the risk of fetal and infant death associated with preexisting maternal diabetes had decreased over time, or that the relative risk of stillbirth varied by gestational age.
The average glycated hemoglobin level in the study was 7.8%. The target for glycated hemoglobin is 7% according to the American Diabetes Association (ADA) and 6.1% according to England’s National Institute for Health and Care Excellence (NICE). Tennant and colleagues estimate that the prevalence of fetal and infant death would have been about 40% lower if the women in their study had achieved either the ADA or NICE target.
Related Article: Does myoinositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
Clinical recommendations
“It’s disappointing to see so little improvement because, with the right care, most women with diabetes can—and will—have a healthy baby,” the authors commented. “Stillbirths and infant deaths are thankfully not common, but they could be even less common if all women with diabetes can be helped to achieve the best possible control of their blood glucose levels.”
“We already know that folic acid reduces the risk of certain congenital anomalies, such as spina bifida or cleft lip, which is why women with diabetes are advised to take high-dose supplements of 5 mg daily. These are available on prescription and should be taken for at least 3 months before conceiving. Our results suggest this simple action may also help to reduce the risk of stillbirth or infant death, even in babies without these conditions.”
Related Article: Does folic acid supplementation have long-term benefit to offspring? Paul L. Ogburn, Jr, MD (Examining the Evidence, January 2012)
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Women who enter pregnancy with diabetes are 4.5 times more likely to experience fetal death and almost twice as likely to lose their infant in the first year of life, compared with women without diabetes, a new study shows.1
Although previous investigations have explored the link between pre-existing maternal diabetes and fetal and infant death, they have not excluded congenital anomalies as a cause of death. In this newest study, Tennant and colleagues used data from several longstanding population-based registries in the north of England to explore the link in offspring without congenital anomalies.
Details of the study
Tennant and colleagues included all normally formed singleton offspring of women with pre-existing diabetes (1,206 with type 1 diabetes and 342 with type 2 diabetes) in the North of England from 1996 to 2008 in their study. Information on these pregnancies came from the Northern Diabetes in Pregnancy Survey. The relative risks (RR) of fetal death (death of a fetus at or after 20 weeks’ gestation) and infant death (death during the first year of life) were estimated by comparing these data with population data from the Northern Perinatal Morbidity and Mortality Survey.
The RR of fetal death in pregnancies marked by preexisting diabetes was 4.56, and it was 1.86 for infant death, compared with pregnancies without diabetes. These risks did not vary between women with type 1 diabetes and those with type 2 diabetes. Other variables associated with a higher risk of fetal or infant death were glycated hemoglobin levels greater than 6.6%, prepregnancy retinopathy, and a lack of folic acid supplementation.
The prevalence of fetal death was 3% in women with preexisting diabetes, and the prevalence of infant death was 0.7%, compared with 0.7% and 0.4%, respectively, in women without diabetes.
Tennant and colleagues found no evidence that the risk of fetal and infant death associated with preexisting maternal diabetes had decreased over time, or that the relative risk of stillbirth varied by gestational age.
The average glycated hemoglobin level in the study was 7.8%. The target for glycated hemoglobin is 7% according to the American Diabetes Association (ADA) and 6.1% according to England’s National Institute for Health and Care Excellence (NICE). Tennant and colleagues estimate that the prevalence of fetal and infant death would have been about 40% lower if the women in their study had achieved either the ADA or NICE target.
Related Article: Does myoinositol supplementation reduce the rate of gestational diabetes in pregnant women with a family history of type 2 diabetes? E. Albert Reece, MD, PhD, MBA (Examining the Evidence, June 2013)
Clinical recommendations
“It’s disappointing to see so little improvement because, with the right care, most women with diabetes can—and will—have a healthy baby,” the authors commented. “Stillbirths and infant deaths are thankfully not common, but they could be even less common if all women with diabetes can be helped to achieve the best possible control of their blood glucose levels.”
“We already know that folic acid reduces the risk of certain congenital anomalies, such as spina bifida or cleft lip, which is why women with diabetes are advised to take high-dose supplements of 5 mg daily. These are available on prescription and should be taken for at least 3 months before conceiving. Our results suggest this simple action may also help to reduce the risk of stillbirth or infant death, even in babies without these conditions.”
Related Article: Does folic acid supplementation have long-term benefit to offspring? Paul L. Ogburn, Jr, MD (Examining the Evidence, January 2012)
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Reference
- Tennant PW, Glinianaia SV, Bilous RW, Rankin J, Bell R. Pre-existing diabetes, maternal glycated haemoglobin, and the risks of fetal and infant death: a population-based study. Diabetologia. 2014;57(2):285–294.
Reference
- Tennant PW, Glinianaia SV, Bilous RW, Rankin J, Bell R. Pre-existing diabetes, maternal glycated haemoglobin, and the risks of fetal and infant death: a population-based study. Diabetologia. 2014;57(2):285–294.
Perinatal depression: what you can do to reduce its long-term effects
We’ve come a long way in our understanding of depression—and that’s a good thing. Consider the treatments popular in the late 18th and early 19th Centuries, for example, which included water immersion (short of drowning), spinning (to reorder the contents of the brain), and the induction of vomiting and administration of enemas, not to mention institutionalization.1 These modalities wouldn’t attract many patients (or clinicians) today.
And yet, even our distant forebears had some inkling of the potential for depression to continue from one generation to the next. As Trotula of Salerno noted around the 11th Century:
In other words, melancholy (aka depression) sometimes has its origins in the womb.
From our 21st Century vantage point, we understand this conclusion in more scientific terms. Data suggest than 14% to 23% of pregnant women will experience depressive symptoms during pregnancy,3 with the potential for long-term effects in the child. In the largest study to date on the effects of antenatal and postnatal parental depression on offspring, Pearson and colleagues found that children of mothers who are depressed during pregnancy are likely to experience depression themselves at age 18.4 Specifically, for each standard-deviation increase in the antenatal maternal depression score, offspring were 1.28 times more likely to have depression at age 18 (95% confidence interval [CI], 1.08–1.51; P = .003).4
Related Article: A talk about, then a plan for, antidepressants in pregnancy Danielle Carlin, MD, and Louann Brizendine, MD (May 2011)
Maternal depression in the postnatal period also was found to be a risk factor for depression in offspring, but only among mothers with “low education” (defined as either no education or compulsory education ending at or before age 16).4 For each standard-deviation increase in the postnatal maternal depression score in this population, offspring were 1.26 times more likely to have depression at age 18, compared with the children of nondepressed women (95% CI, 1.06–1.50; P = .01).4
Although antenatal depression in fathers was not associated with an increased incidence of depression in offspring, postnatal depression was—but only when the fathers had low education.4
As for the mechanism of transmission of depression from parent to child? Although Pearson and colleagues did not attempt to identify it, they did observe that the differential effects of maternal and paternal antenatal depression—with only maternal depression having an impact on offspring—suggest that, in pregnancy, maternal depression may be transmitted to her child “through the biological consequences of depression in utero.”4
Clearly, if it goes unchecked during pregnancy, maternal depression has the potential to ravage the life of both mother and child. In this article, I review guidance on the management of depression in pregnancy from the American College of Obstetricians and Gynecologists (ACOG) and the American Psychiatric Association (APA), and I offer insights from a perinatal psychiatrist on how ObGyns might adjust their practices to reduce the impact of depression on both mother and infant.
COMPLICATIONS OF PERINATAL DEPRESSION
In a joint report on depression and pregnancy from ACOG and the APA, Yonkers and colleagues noted that low birth weight, neonatal irritability, and diminished neonatal activity and attentiveness are among the adverse reproductive outcomes that have been associated with untreated maternal depression.3 Reproductive outcomes are more dire if maternal depression is severe or if the mother has bipolar disorder or postpartum psychosis, potentially including infanticide or death from suicide.5
Pregnancy complications such as vomiting, nausea, hyperemesis gravidarum, and preeclampsia appear to occur more frequently in depressed women than in nondepressed women, according to the ACOG/APA report,3 although this finding is based on limited data, notes Leena P. Mittal, MD, director of the Reproductive Psychiatry Consultation Service at Brigham and Women’s Hospital in Boston and instructor in psychiatry at Harvard Medical School.
“The trouble with those studies in general is the difficulty of controlling for both the severity of depression and the effects of treatment of depression—or the effects of treatment versus effects of the illness itself,” she says.
That difficulty is compounded by the likely use of multiple medications—
including nonpsychiatric agents—during pregnancy, “which makes it difficult to assess the impact of a single compound, such as an antidepressant, on maternal and fetal outcomes,” according to ACOG and the APA.3 (More than 80% of pregnant women take at least one dose of a medication.3)
HOW THE OBGYN CAN MAKE A DIFFERENCE
Because of the potential for adverse short- and long-term effects of perinatal depression, “there is a need to identify it and attempt to address it prior to the postpartum period,” Dr. Mittal says. “If a woman has depressive symptoms during pregnancy, it is important to try to direct her toward treatment—either by initiating treatment yourself or referring her to a psychiatrist or psychiatric care provider before she enters the postpartum period.” Once she’s postpartum, she will be exposed to additional variables that will influence the severity and duration of her depression, Dr. Mittal says.
Screen all pregnant women for depression
Dr. Mittal recommends routine screening of all perinatal women.
“The data are not entirely clear about the intervals at which these women should be screened,” she says, “but the recommendation would be screening at least once during pregnancy and then again postpartum. Some clinicians screen for depression during each trimester of pregnancy.”
At Dr. Mittal’s institution, such screening usually takes place at the patient’s first prenatal visit.
The screening tools with the most high-quality data backing them include the:
- Edinburgh Postnatal Depression Scale (EPDS). “Despite its name, this tool has been validated for use during pregnancy and for use in the nonperinatal woman as well,” Dr. Mittal notes. It also is in the public domain (http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf). “It’s particularly useful during pregnancy because it assesses the woman for symptoms of depression at the same time that it separates those symptoms from the physical symptoms of pregnancy—there can be some overlap.” The EPDS is self-administered, brief (10 questions), and easily assessed by the clinician, with a score of 10 or above indicating a likelihood of depression.6 It has been validated in more than a dozen languages, as well.
- Patient Health Questionnaire (PHQ-9).7 This is another public-domain tool validated for use during pregnancy (http://www.cqaimh.org/pdf/tool_phq9.pdf). It is utilized widely in primary care and closely associated with depression criteria listed in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders. Like the EPDS, it is self-administered, brief (9 questions), and easy to score. In general, PHQ-9 scores of 5, 10, 15, and 20 represent mild, moderate, moderately severe, and severe depression, respectively.8
Neither of these tools should override clinical judgment. Even with a positive score, clinical assessment is recommended. Nor are these tools designed to detect anxiety, personality disorders, and phobias.
Try to address the issue before conception
The best time to address perinatal depression, of course, with a conversation about prevention, is during the preconception period. Having time before pregnancy to determine the best perinatal management approach is especially valuable.
“What’s important for an ObGyn to consider when counseling someone who is contemplating pregnancy and who has a history of depression is the need to weigh the risks of treatment during pregnancy against the risks of nontreatment,” says Dr. Mittal. Two ways to do that are to assess the severity of her depressive symptoms—both currently and historically—and explore her response to treatment.
“Obviously, suicidality and psychosis suggest very severe illness, whether they are currently present or occurred in the past, and so does a history of psychiatric hospitalization,” says Dr. Mittal. “In such cases, the untreated illness itself carries significant risk, and when it is weighed against the perhaps smaller risk of antidepressant medication during pregnancy, the risk-benefit analysis likely is very different than it might be for someone with mild to moderate depression. I would definitely agree that addressing severity from the beginning is important.”
An understanding of the patient’s response to treatment also is beneficial. Has any treatment been helpful? If so, that information can guide the choice of treatment during pregnancy, says Dr. Mittal. Even knowing whether a woman has responded to nonpharmacologic therapy such as psychotherapy can help shape the treatment plan.
“It might mean that there’s a way to limit the risk of exposure to a variety of psychotropic medications,” Dr. Mittal says. “Or if the patient has had a good response to a particular medication, it might make sense to try that agent again—or, if she’s currently taking it, to stick with it.”
Even if preconception counseling is difficult to achieve, ObGyns see a large number of women of reproductive age during the course of routine gynecologic care.
“I do think it’s worth having a discussion about reproductive planning, especially in the context of their psychiatric illness or history, even if they aren’t currently planning a pregnancy,” says Dr. Mittal.
When to refer the patient to a psychiatrist
Again, the severity of symptoms comes into play.
“In severe mental illness—bipolar disorder, psychotic disorders, or a history of severe illness requiring psychiatric hospitalization—it is important to have a psychiatrist involved,” says Dr. Mittal.
“Even if the woman is stable during pregnancy, the postpartum risk—especially in bipolar disorder—is extremely high. The postpartum period is a vulnerable time, anyway, because obstetric care is coming to its end, and there’s a lot changing irrespective of mental illness. So a patient who’s at high risk for postpartum illness should have a psychiatrist on board as early as possible.”
Consultation with a psychiatrist is another option when managing women with severe depression, a significant psychiatric history, or refractory illness.
Should you prescribe antidepressant medication?
Dr. Mittal believes that ObGyns should feel fairly comfortable prescribing antidepressant medication to patients who have mild or moderate depression, provided that the initiation of such medication is the patient’s informed choice.
Once severe disease (including bipolar disorder and a history of suicidality or psychosis or psychiatric hospitalization) has been ruled out and a history indicates that the patient has mild to moderate symptoms and has responded to treatment, an ObGyn is well qualified to treat perinatal depression, says Dr. Mittal.
Typically, SSRIs are the first-line treatment for perinatal depression and generally have similar amounts of data about their risk in pregnancy. Paroxetine (Paxil) is the exception, as we have more data about the risk for cardiac defects in neonates exposed to it in utero, Dr. Mittal says.
SSRIs generally are found in low amounts in breast milk, although sertraline (Zoloft) generally is found in the smallest quantity, making it the most commonly used SSRI in pregnancy. Sertraline is followed by citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) in the respective amount of medication passed into breast milk.
The literature around the teratogenic risks of psychiatric medications is extremely diverse, she says. The “sum total” of the data suggests that SSRIs have relatively few teratogenic risks. “The overall story around SSRIs does not appear to suggest that they carry a risk of major malformations.”
Related Article: Antidepressants linked to pregnancy risks in infertility treatment (News for Your Practice, December 2012)
Dr. Mittal also recommends keeping in mind the possibility that psychotherapy alone is sometimes sufficient for a woman with mild to moderate depression.
“If she has a history of responding to psychotherapy alone and also has mild to moderate symptoms, I think a reasonable approach would be to try it again.”
“This is where preconception planning is especially useful,” she says. “If somebody with mild to moderate symptoms has never had a good trial of psychotherapy, the preconception period is a good time to determine whether it might be effective, to shape the optimal treatment plan.”
Two forms of psychotherapy have solid evidence of efficacy in perinatal depression:
- cognitive behavioral therapy (CBT) —an action-oriented approach that treats maladaptive thinking as the cause of pathologic behavior and “negative” emotions
- interpersonal psychotherapy (IPT)—a treatment in which the patient is educated about depression and its symptoms and her relation to the environment, especially social functioning. Unlike some other forms of therapy, IPT does not focus on underlying personality structures.
There are other forms of psychotherapy, but CBT and IPT have a large evidence base and are generally time-limited, rather than open-ended. They also are manualized and problem-focused, says Dr. Mittal.
How to prescribe an SSRI
SSRIs generally are initiated at a low dose and gradually titrated up (if necessary). A typical starting dose of sertraline, for example, would be 25 to 50 mg. The patient should be counseled about potential side effects, which include increased perspiration, somnolence or insomnia, nausea, diarrhea, headache, dizziness, and restlessness. These effects generally begin to subside the first week or two after initiation.
Sexual side effects such as reduced desire and difficulties with orgasm also may occur and generally do not diminish over time.
The patient also should be advised not to discontinue the SSRI abruptly, if at all possible, because of the risk that she might develop mild discontinuation syndrome. Although this syndrome is short-lived, self-limited, and non-life-threatening, it is uncomfortable. Symptoms include changes in mood or anxiety, shakiness, tremor, or gastrointestinal disturbance. If the patient elects to discontinue an SSRI, tapering over 4 to 7 days is preferable. However, in the event that the patient exhibits an adverse reaction or intolerance to antidepressant medication, immediate discontinuation may be appropriate, says Dr. Mittal.
After initiating SSRI therapy, follow-up in 2 weeks is appropriate, after which time oversight can be transferred to the patient’s primary care provider. In the United States, primary care physicians prescribe the bulk of SSRI medications.
It may take 6 to 8 weeks for the medication to begin to reduce depressive symptoms, although sleep and appetite sometimes improve within 1 or 2 weeks.
Avoid abrupt drug discontinuation in pregnancy
When asked to recommend one intervention that would have a big impact on reducing the burden of depression in pregnancy, Dr. Mittal zeroed in on the population of women who elect to discontinue antidepressant medication during pregnancy.
“I would suggest that ObGyns discourage these women against abrupt discontinuation,” she says. “There is a small body of literature that demonstrates that, in patients with significant illness—severe depression and bipolar disorder, certainly—abrupt discontinuation increases the likelihood of recurrence in the short period of time afterward. If medication is abruptly stopped when a woman discovers she’s pregnant, she’s likely to need to return to treatment during pregnancy because of recurrent symptoms. What happens in that case is that her pregnancy is exposed to both severe symptoms and the reinitiation of treatment, possibly including additional medications beyond the initial agent,” says Dr. Mittal.
Many women assume they should never get pregnant because of their mental health issues, their medications, or both, says Dr. Mittal. Or they believe they must stop their meds if they become pregnant. In fact, some patients report that they have been counseled to avoid medication in pregnancy by their psychiatrist or obstetrician!
“I have spoken to many psychiatrists who say they are not comfortable prescribing to pregnant women, so they either drop the patients or stop their meds!” she says.
When that happens, the patient should find another psychiatrist.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
- Nemade R, Reiss NS, Dombeck M. Historical understandings of depression. Mentalhelp.net. http://www.mentalhelp.net/poc/view_doc.php?type=doc&id=12995&cn=5. Published September 19, 2007. Accessed January 13, 2014.
- Brockington I. A historical perspective on the psychiatry of motherhood. In: Perinatal Stress, Mood, and Anxiety Disorders. Basel, Switzerland: S Karger AG; 2005.
- Yonkers KA, Wisner KL, Stewart DE, et al. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114(3):703–713.
- Pearson RM, Evans J, Kounali D, et al. Maternal depression during pregnancy and the postnatal period. Risks and possible mechanisms for offspring depression at age 18 years [published online ahead of print October 9, 2013]. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2013.2163.
- Hasser C, Brizendine L, Spielvogel A. SSRI use during pregnancy. Current Psychiatry. 2006;5(4):31–40.
- Edinburgh Postnatal Depression Scale. http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf. Accessed January 14, 2014.
- Patient Health Questionnaire (PHQ-9). http://www.cqaimh.org/pdf/tool_phq9.pdf. Accessed January 14, 2014.
- Kroenke K, Spitzer R, Williams W. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
We’ve come a long way in our understanding of depression—and that’s a good thing. Consider the treatments popular in the late 18th and early 19th Centuries, for example, which included water immersion (short of drowning), spinning (to reorder the contents of the brain), and the induction of vomiting and administration of enemas, not to mention institutionalization.1 These modalities wouldn’t attract many patients (or clinicians) today.
And yet, even our distant forebears had some inkling of the potential for depression to continue from one generation to the next. As Trotula of Salerno noted around the 11th Century:
In other words, melancholy (aka depression) sometimes has its origins in the womb.
From our 21st Century vantage point, we understand this conclusion in more scientific terms. Data suggest than 14% to 23% of pregnant women will experience depressive symptoms during pregnancy,3 with the potential for long-term effects in the child. In the largest study to date on the effects of antenatal and postnatal parental depression on offspring, Pearson and colleagues found that children of mothers who are depressed during pregnancy are likely to experience depression themselves at age 18.4 Specifically, for each standard-deviation increase in the antenatal maternal depression score, offspring were 1.28 times more likely to have depression at age 18 (95% confidence interval [CI], 1.08–1.51; P = .003).4
Related Article: A talk about, then a plan for, antidepressants in pregnancy Danielle Carlin, MD, and Louann Brizendine, MD (May 2011)
Maternal depression in the postnatal period also was found to be a risk factor for depression in offspring, but only among mothers with “low education” (defined as either no education or compulsory education ending at or before age 16).4 For each standard-deviation increase in the postnatal maternal depression score in this population, offspring were 1.26 times more likely to have depression at age 18, compared with the children of nondepressed women (95% CI, 1.06–1.50; P = .01).4
Although antenatal depression in fathers was not associated with an increased incidence of depression in offspring, postnatal depression was—but only when the fathers had low education.4
As for the mechanism of transmission of depression from parent to child? Although Pearson and colleagues did not attempt to identify it, they did observe that the differential effects of maternal and paternal antenatal depression—with only maternal depression having an impact on offspring—suggest that, in pregnancy, maternal depression may be transmitted to her child “through the biological consequences of depression in utero.”4
Clearly, if it goes unchecked during pregnancy, maternal depression has the potential to ravage the life of both mother and child. In this article, I review guidance on the management of depression in pregnancy from the American College of Obstetricians and Gynecologists (ACOG) and the American Psychiatric Association (APA), and I offer insights from a perinatal psychiatrist on how ObGyns might adjust their practices to reduce the impact of depression on both mother and infant.
COMPLICATIONS OF PERINATAL DEPRESSION
In a joint report on depression and pregnancy from ACOG and the APA, Yonkers and colleagues noted that low birth weight, neonatal irritability, and diminished neonatal activity and attentiveness are among the adverse reproductive outcomes that have been associated with untreated maternal depression.3 Reproductive outcomes are more dire if maternal depression is severe or if the mother has bipolar disorder or postpartum psychosis, potentially including infanticide or death from suicide.5
Pregnancy complications such as vomiting, nausea, hyperemesis gravidarum, and preeclampsia appear to occur more frequently in depressed women than in nondepressed women, according to the ACOG/APA report,3 although this finding is based on limited data, notes Leena P. Mittal, MD, director of the Reproductive Psychiatry Consultation Service at Brigham and Women’s Hospital in Boston and instructor in psychiatry at Harvard Medical School.
“The trouble with those studies in general is the difficulty of controlling for both the severity of depression and the effects of treatment of depression—or the effects of treatment versus effects of the illness itself,” she says.
That difficulty is compounded by the likely use of multiple medications—
including nonpsychiatric agents—during pregnancy, “which makes it difficult to assess the impact of a single compound, such as an antidepressant, on maternal and fetal outcomes,” according to ACOG and the APA.3 (More than 80% of pregnant women take at least one dose of a medication.3)
HOW THE OBGYN CAN MAKE A DIFFERENCE
Because of the potential for adverse short- and long-term effects of perinatal depression, “there is a need to identify it and attempt to address it prior to the postpartum period,” Dr. Mittal says. “If a woman has depressive symptoms during pregnancy, it is important to try to direct her toward treatment—either by initiating treatment yourself or referring her to a psychiatrist or psychiatric care provider before she enters the postpartum period.” Once she’s postpartum, she will be exposed to additional variables that will influence the severity and duration of her depression, Dr. Mittal says.
Screen all pregnant women for depression
Dr. Mittal recommends routine screening of all perinatal women.
“The data are not entirely clear about the intervals at which these women should be screened,” she says, “but the recommendation would be screening at least once during pregnancy and then again postpartum. Some clinicians screen for depression during each trimester of pregnancy.”
At Dr. Mittal’s institution, such screening usually takes place at the patient’s first prenatal visit.
The screening tools with the most high-quality data backing them include the:
- Edinburgh Postnatal Depression Scale (EPDS). “Despite its name, this tool has been validated for use during pregnancy and for use in the nonperinatal woman as well,” Dr. Mittal notes. It also is in the public domain (http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf). “It’s particularly useful during pregnancy because it assesses the woman for symptoms of depression at the same time that it separates those symptoms from the physical symptoms of pregnancy—there can be some overlap.” The EPDS is self-administered, brief (10 questions), and easily assessed by the clinician, with a score of 10 or above indicating a likelihood of depression.6 It has been validated in more than a dozen languages, as well.
- Patient Health Questionnaire (PHQ-9).7 This is another public-domain tool validated for use during pregnancy (http://www.cqaimh.org/pdf/tool_phq9.pdf). It is utilized widely in primary care and closely associated with depression criteria listed in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders. Like the EPDS, it is self-administered, brief (9 questions), and easy to score. In general, PHQ-9 scores of 5, 10, 15, and 20 represent mild, moderate, moderately severe, and severe depression, respectively.8
Neither of these tools should override clinical judgment. Even with a positive score, clinical assessment is recommended. Nor are these tools designed to detect anxiety, personality disorders, and phobias.
Try to address the issue before conception
The best time to address perinatal depression, of course, with a conversation about prevention, is during the preconception period. Having time before pregnancy to determine the best perinatal management approach is especially valuable.
“What’s important for an ObGyn to consider when counseling someone who is contemplating pregnancy and who has a history of depression is the need to weigh the risks of treatment during pregnancy against the risks of nontreatment,” says Dr. Mittal. Two ways to do that are to assess the severity of her depressive symptoms—both currently and historically—and explore her response to treatment.
“Obviously, suicidality and psychosis suggest very severe illness, whether they are currently present or occurred in the past, and so does a history of psychiatric hospitalization,” says Dr. Mittal. “In such cases, the untreated illness itself carries significant risk, and when it is weighed against the perhaps smaller risk of antidepressant medication during pregnancy, the risk-benefit analysis likely is very different than it might be for someone with mild to moderate depression. I would definitely agree that addressing severity from the beginning is important.”
An understanding of the patient’s response to treatment also is beneficial. Has any treatment been helpful? If so, that information can guide the choice of treatment during pregnancy, says Dr. Mittal. Even knowing whether a woman has responded to nonpharmacologic therapy such as psychotherapy can help shape the treatment plan.
“It might mean that there’s a way to limit the risk of exposure to a variety of psychotropic medications,” Dr. Mittal says. “Or if the patient has had a good response to a particular medication, it might make sense to try that agent again—or, if she’s currently taking it, to stick with it.”
Even if preconception counseling is difficult to achieve, ObGyns see a large number of women of reproductive age during the course of routine gynecologic care.
“I do think it’s worth having a discussion about reproductive planning, especially in the context of their psychiatric illness or history, even if they aren’t currently planning a pregnancy,” says Dr. Mittal.
When to refer the patient to a psychiatrist
Again, the severity of symptoms comes into play.
“In severe mental illness—bipolar disorder, psychotic disorders, or a history of severe illness requiring psychiatric hospitalization—it is important to have a psychiatrist involved,” says Dr. Mittal.
“Even if the woman is stable during pregnancy, the postpartum risk—especially in bipolar disorder—is extremely high. The postpartum period is a vulnerable time, anyway, because obstetric care is coming to its end, and there’s a lot changing irrespective of mental illness. So a patient who’s at high risk for postpartum illness should have a psychiatrist on board as early as possible.”
Consultation with a psychiatrist is another option when managing women with severe depression, a significant psychiatric history, or refractory illness.
Should you prescribe antidepressant medication?
Dr. Mittal believes that ObGyns should feel fairly comfortable prescribing antidepressant medication to patients who have mild or moderate depression, provided that the initiation of such medication is the patient’s informed choice.
Once severe disease (including bipolar disorder and a history of suicidality or psychosis or psychiatric hospitalization) has been ruled out and a history indicates that the patient has mild to moderate symptoms and has responded to treatment, an ObGyn is well qualified to treat perinatal depression, says Dr. Mittal.
Typically, SSRIs are the first-line treatment for perinatal depression and generally have similar amounts of data about their risk in pregnancy. Paroxetine (Paxil) is the exception, as we have more data about the risk for cardiac defects in neonates exposed to it in utero, Dr. Mittal says.
SSRIs generally are found in low amounts in breast milk, although sertraline (Zoloft) generally is found in the smallest quantity, making it the most commonly used SSRI in pregnancy. Sertraline is followed by citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) in the respective amount of medication passed into breast milk.
The literature around the teratogenic risks of psychiatric medications is extremely diverse, she says. The “sum total” of the data suggests that SSRIs have relatively few teratogenic risks. “The overall story around SSRIs does not appear to suggest that they carry a risk of major malformations.”
Related Article: Antidepressants linked to pregnancy risks in infertility treatment (News for Your Practice, December 2012)
Dr. Mittal also recommends keeping in mind the possibility that psychotherapy alone is sometimes sufficient for a woman with mild to moderate depression.
“If she has a history of responding to psychotherapy alone and also has mild to moderate symptoms, I think a reasonable approach would be to try it again.”
“This is where preconception planning is especially useful,” she says. “If somebody with mild to moderate symptoms has never had a good trial of psychotherapy, the preconception period is a good time to determine whether it might be effective, to shape the optimal treatment plan.”
Two forms of psychotherapy have solid evidence of efficacy in perinatal depression:
- cognitive behavioral therapy (CBT) —an action-oriented approach that treats maladaptive thinking as the cause of pathologic behavior and “negative” emotions
- interpersonal psychotherapy (IPT)—a treatment in which the patient is educated about depression and its symptoms and her relation to the environment, especially social functioning. Unlike some other forms of therapy, IPT does not focus on underlying personality structures.
There are other forms of psychotherapy, but CBT and IPT have a large evidence base and are generally time-limited, rather than open-ended. They also are manualized and problem-focused, says Dr. Mittal.
How to prescribe an SSRI
SSRIs generally are initiated at a low dose and gradually titrated up (if necessary). A typical starting dose of sertraline, for example, would be 25 to 50 mg. The patient should be counseled about potential side effects, which include increased perspiration, somnolence or insomnia, nausea, diarrhea, headache, dizziness, and restlessness. These effects generally begin to subside the first week or two after initiation.
Sexual side effects such as reduced desire and difficulties with orgasm also may occur and generally do not diminish over time.
The patient also should be advised not to discontinue the SSRI abruptly, if at all possible, because of the risk that she might develop mild discontinuation syndrome. Although this syndrome is short-lived, self-limited, and non-life-threatening, it is uncomfortable. Symptoms include changes in mood or anxiety, shakiness, tremor, or gastrointestinal disturbance. If the patient elects to discontinue an SSRI, tapering over 4 to 7 days is preferable. However, in the event that the patient exhibits an adverse reaction or intolerance to antidepressant medication, immediate discontinuation may be appropriate, says Dr. Mittal.
After initiating SSRI therapy, follow-up in 2 weeks is appropriate, after which time oversight can be transferred to the patient’s primary care provider. In the United States, primary care physicians prescribe the bulk of SSRI medications.
It may take 6 to 8 weeks for the medication to begin to reduce depressive symptoms, although sleep and appetite sometimes improve within 1 or 2 weeks.
Avoid abrupt drug discontinuation in pregnancy
When asked to recommend one intervention that would have a big impact on reducing the burden of depression in pregnancy, Dr. Mittal zeroed in on the population of women who elect to discontinue antidepressant medication during pregnancy.
“I would suggest that ObGyns discourage these women against abrupt discontinuation,” she says. “There is a small body of literature that demonstrates that, in patients with significant illness—severe depression and bipolar disorder, certainly—abrupt discontinuation increases the likelihood of recurrence in the short period of time afterward. If medication is abruptly stopped when a woman discovers she’s pregnant, she’s likely to need to return to treatment during pregnancy because of recurrent symptoms. What happens in that case is that her pregnancy is exposed to both severe symptoms and the reinitiation of treatment, possibly including additional medications beyond the initial agent,” says Dr. Mittal.
Many women assume they should never get pregnant because of their mental health issues, their medications, or both, says Dr. Mittal. Or they believe they must stop their meds if they become pregnant. In fact, some patients report that they have been counseled to avoid medication in pregnancy by their psychiatrist or obstetrician!
“I have spoken to many psychiatrists who say they are not comfortable prescribing to pregnant women, so they either drop the patients or stop their meds!” she says.
When that happens, the patient should find another psychiatrist.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
We’ve come a long way in our understanding of depression—and that’s a good thing. Consider the treatments popular in the late 18th and early 19th Centuries, for example, which included water immersion (short of drowning), spinning (to reorder the contents of the brain), and the induction of vomiting and administration of enemas, not to mention institutionalization.1 These modalities wouldn’t attract many patients (or clinicians) today.
And yet, even our distant forebears had some inkling of the potential for depression to continue from one generation to the next. As Trotula of Salerno noted around the 11th Century:
In other words, melancholy (aka depression) sometimes has its origins in the womb.
From our 21st Century vantage point, we understand this conclusion in more scientific terms. Data suggest than 14% to 23% of pregnant women will experience depressive symptoms during pregnancy,3 with the potential for long-term effects in the child. In the largest study to date on the effects of antenatal and postnatal parental depression on offspring, Pearson and colleagues found that children of mothers who are depressed during pregnancy are likely to experience depression themselves at age 18.4 Specifically, for each standard-deviation increase in the antenatal maternal depression score, offspring were 1.28 times more likely to have depression at age 18 (95% confidence interval [CI], 1.08–1.51; P = .003).4
Related Article: A talk about, then a plan for, antidepressants in pregnancy Danielle Carlin, MD, and Louann Brizendine, MD (May 2011)
Maternal depression in the postnatal period also was found to be a risk factor for depression in offspring, but only among mothers with “low education” (defined as either no education or compulsory education ending at or before age 16).4 For each standard-deviation increase in the postnatal maternal depression score in this population, offspring were 1.26 times more likely to have depression at age 18, compared with the children of nondepressed women (95% CI, 1.06–1.50; P = .01).4
Although antenatal depression in fathers was not associated with an increased incidence of depression in offspring, postnatal depression was—but only when the fathers had low education.4
As for the mechanism of transmission of depression from parent to child? Although Pearson and colleagues did not attempt to identify it, they did observe that the differential effects of maternal and paternal antenatal depression—with only maternal depression having an impact on offspring—suggest that, in pregnancy, maternal depression may be transmitted to her child “through the biological consequences of depression in utero.”4
Clearly, if it goes unchecked during pregnancy, maternal depression has the potential to ravage the life of both mother and child. In this article, I review guidance on the management of depression in pregnancy from the American College of Obstetricians and Gynecologists (ACOG) and the American Psychiatric Association (APA), and I offer insights from a perinatal psychiatrist on how ObGyns might adjust their practices to reduce the impact of depression on both mother and infant.
COMPLICATIONS OF PERINATAL DEPRESSION
In a joint report on depression and pregnancy from ACOG and the APA, Yonkers and colleagues noted that low birth weight, neonatal irritability, and diminished neonatal activity and attentiveness are among the adverse reproductive outcomes that have been associated with untreated maternal depression.3 Reproductive outcomes are more dire if maternal depression is severe or if the mother has bipolar disorder or postpartum psychosis, potentially including infanticide or death from suicide.5
Pregnancy complications such as vomiting, nausea, hyperemesis gravidarum, and preeclampsia appear to occur more frequently in depressed women than in nondepressed women, according to the ACOG/APA report,3 although this finding is based on limited data, notes Leena P. Mittal, MD, director of the Reproductive Psychiatry Consultation Service at Brigham and Women’s Hospital in Boston and instructor in psychiatry at Harvard Medical School.
“The trouble with those studies in general is the difficulty of controlling for both the severity of depression and the effects of treatment of depression—or the effects of treatment versus effects of the illness itself,” she says.
That difficulty is compounded by the likely use of multiple medications—
including nonpsychiatric agents—during pregnancy, “which makes it difficult to assess the impact of a single compound, such as an antidepressant, on maternal and fetal outcomes,” according to ACOG and the APA.3 (More than 80% of pregnant women take at least one dose of a medication.3)
HOW THE OBGYN CAN MAKE A DIFFERENCE
Because of the potential for adverse short- and long-term effects of perinatal depression, “there is a need to identify it and attempt to address it prior to the postpartum period,” Dr. Mittal says. “If a woman has depressive symptoms during pregnancy, it is important to try to direct her toward treatment—either by initiating treatment yourself or referring her to a psychiatrist or psychiatric care provider before she enters the postpartum period.” Once she’s postpartum, she will be exposed to additional variables that will influence the severity and duration of her depression, Dr. Mittal says.
Screen all pregnant women for depression
Dr. Mittal recommends routine screening of all perinatal women.
“The data are not entirely clear about the intervals at which these women should be screened,” she says, “but the recommendation would be screening at least once during pregnancy and then again postpartum. Some clinicians screen for depression during each trimester of pregnancy.”
At Dr. Mittal’s institution, such screening usually takes place at the patient’s first prenatal visit.
The screening tools with the most high-quality data backing them include the:
- Edinburgh Postnatal Depression Scale (EPDS). “Despite its name, this tool has been validated for use during pregnancy and for use in the nonperinatal woman as well,” Dr. Mittal notes. It also is in the public domain (http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf). “It’s particularly useful during pregnancy because it assesses the woman for symptoms of depression at the same time that it separates those symptoms from the physical symptoms of pregnancy—there can be some overlap.” The EPDS is self-administered, brief (10 questions), and easily assessed by the clinician, with a score of 10 or above indicating a likelihood of depression.6 It has been validated in more than a dozen languages, as well.
- Patient Health Questionnaire (PHQ-9).7 This is another public-domain tool validated for use during pregnancy (http://www.cqaimh.org/pdf/tool_phq9.pdf). It is utilized widely in primary care and closely associated with depression criteria listed in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders. Like the EPDS, it is self-administered, brief (9 questions), and easy to score. In general, PHQ-9 scores of 5, 10, 15, and 20 represent mild, moderate, moderately severe, and severe depression, respectively.8
Neither of these tools should override clinical judgment. Even with a positive score, clinical assessment is recommended. Nor are these tools designed to detect anxiety, personality disorders, and phobias.
Try to address the issue before conception
The best time to address perinatal depression, of course, with a conversation about prevention, is during the preconception period. Having time before pregnancy to determine the best perinatal management approach is especially valuable.
“What’s important for an ObGyn to consider when counseling someone who is contemplating pregnancy and who has a history of depression is the need to weigh the risks of treatment during pregnancy against the risks of nontreatment,” says Dr. Mittal. Two ways to do that are to assess the severity of her depressive symptoms—both currently and historically—and explore her response to treatment.
“Obviously, suicidality and psychosis suggest very severe illness, whether they are currently present or occurred in the past, and so does a history of psychiatric hospitalization,” says Dr. Mittal. “In such cases, the untreated illness itself carries significant risk, and when it is weighed against the perhaps smaller risk of antidepressant medication during pregnancy, the risk-benefit analysis likely is very different than it might be for someone with mild to moderate depression. I would definitely agree that addressing severity from the beginning is important.”
An understanding of the patient’s response to treatment also is beneficial. Has any treatment been helpful? If so, that information can guide the choice of treatment during pregnancy, says Dr. Mittal. Even knowing whether a woman has responded to nonpharmacologic therapy such as psychotherapy can help shape the treatment plan.
“It might mean that there’s a way to limit the risk of exposure to a variety of psychotropic medications,” Dr. Mittal says. “Or if the patient has had a good response to a particular medication, it might make sense to try that agent again—or, if she’s currently taking it, to stick with it.”
Even if preconception counseling is difficult to achieve, ObGyns see a large number of women of reproductive age during the course of routine gynecologic care.
“I do think it’s worth having a discussion about reproductive planning, especially in the context of their psychiatric illness or history, even if they aren’t currently planning a pregnancy,” says Dr. Mittal.
When to refer the patient to a psychiatrist
Again, the severity of symptoms comes into play.
“In severe mental illness—bipolar disorder, psychotic disorders, or a history of severe illness requiring psychiatric hospitalization—it is important to have a psychiatrist involved,” says Dr. Mittal.
“Even if the woman is stable during pregnancy, the postpartum risk—especially in bipolar disorder—is extremely high. The postpartum period is a vulnerable time, anyway, because obstetric care is coming to its end, and there’s a lot changing irrespective of mental illness. So a patient who’s at high risk for postpartum illness should have a psychiatrist on board as early as possible.”
Consultation with a psychiatrist is another option when managing women with severe depression, a significant psychiatric history, or refractory illness.
Should you prescribe antidepressant medication?
Dr. Mittal believes that ObGyns should feel fairly comfortable prescribing antidepressant medication to patients who have mild or moderate depression, provided that the initiation of such medication is the patient’s informed choice.
Once severe disease (including bipolar disorder and a history of suicidality or psychosis or psychiatric hospitalization) has been ruled out and a history indicates that the patient has mild to moderate symptoms and has responded to treatment, an ObGyn is well qualified to treat perinatal depression, says Dr. Mittal.
Typically, SSRIs are the first-line treatment for perinatal depression and generally have similar amounts of data about their risk in pregnancy. Paroxetine (Paxil) is the exception, as we have more data about the risk for cardiac defects in neonates exposed to it in utero, Dr. Mittal says.
SSRIs generally are found in low amounts in breast milk, although sertraline (Zoloft) generally is found in the smallest quantity, making it the most commonly used SSRI in pregnancy. Sertraline is followed by citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) in the respective amount of medication passed into breast milk.
The literature around the teratogenic risks of psychiatric medications is extremely diverse, she says. The “sum total” of the data suggests that SSRIs have relatively few teratogenic risks. “The overall story around SSRIs does not appear to suggest that they carry a risk of major malformations.”
Related Article: Antidepressants linked to pregnancy risks in infertility treatment (News for Your Practice, December 2012)
Dr. Mittal also recommends keeping in mind the possibility that psychotherapy alone is sometimes sufficient for a woman with mild to moderate depression.
“If she has a history of responding to psychotherapy alone and also has mild to moderate symptoms, I think a reasonable approach would be to try it again.”
“This is where preconception planning is especially useful,” she says. “If somebody with mild to moderate symptoms has never had a good trial of psychotherapy, the preconception period is a good time to determine whether it might be effective, to shape the optimal treatment plan.”
Two forms of psychotherapy have solid evidence of efficacy in perinatal depression:
- cognitive behavioral therapy (CBT) —an action-oriented approach that treats maladaptive thinking as the cause of pathologic behavior and “negative” emotions
- interpersonal psychotherapy (IPT)—a treatment in which the patient is educated about depression and its symptoms and her relation to the environment, especially social functioning. Unlike some other forms of therapy, IPT does not focus on underlying personality structures.
There are other forms of psychotherapy, but CBT and IPT have a large evidence base and are generally time-limited, rather than open-ended. They also are manualized and problem-focused, says Dr. Mittal.
How to prescribe an SSRI
SSRIs generally are initiated at a low dose and gradually titrated up (if necessary). A typical starting dose of sertraline, for example, would be 25 to 50 mg. The patient should be counseled about potential side effects, which include increased perspiration, somnolence or insomnia, nausea, diarrhea, headache, dizziness, and restlessness. These effects generally begin to subside the first week or two after initiation.
Sexual side effects such as reduced desire and difficulties with orgasm also may occur and generally do not diminish over time.
The patient also should be advised not to discontinue the SSRI abruptly, if at all possible, because of the risk that she might develop mild discontinuation syndrome. Although this syndrome is short-lived, self-limited, and non-life-threatening, it is uncomfortable. Symptoms include changes in mood or anxiety, shakiness, tremor, or gastrointestinal disturbance. If the patient elects to discontinue an SSRI, tapering over 4 to 7 days is preferable. However, in the event that the patient exhibits an adverse reaction or intolerance to antidepressant medication, immediate discontinuation may be appropriate, says Dr. Mittal.
After initiating SSRI therapy, follow-up in 2 weeks is appropriate, after which time oversight can be transferred to the patient’s primary care provider. In the United States, primary care physicians prescribe the bulk of SSRI medications.
It may take 6 to 8 weeks for the medication to begin to reduce depressive symptoms, although sleep and appetite sometimes improve within 1 or 2 weeks.
Avoid abrupt drug discontinuation in pregnancy
When asked to recommend one intervention that would have a big impact on reducing the burden of depression in pregnancy, Dr. Mittal zeroed in on the population of women who elect to discontinue antidepressant medication during pregnancy.
“I would suggest that ObGyns discourage these women against abrupt discontinuation,” she says. “There is a small body of literature that demonstrates that, in patients with significant illness—severe depression and bipolar disorder, certainly—abrupt discontinuation increases the likelihood of recurrence in the short period of time afterward. If medication is abruptly stopped when a woman discovers she’s pregnant, she’s likely to need to return to treatment during pregnancy because of recurrent symptoms. What happens in that case is that her pregnancy is exposed to both severe symptoms and the reinitiation of treatment, possibly including additional medications beyond the initial agent,” says Dr. Mittal.
Many women assume they should never get pregnant because of their mental health issues, their medications, or both, says Dr. Mittal. Or they believe they must stop their meds if they become pregnant. In fact, some patients report that they have been counseled to avoid medication in pregnancy by their psychiatrist or obstetrician!
“I have spoken to many psychiatrists who say they are not comfortable prescribing to pregnant women, so they either drop the patients or stop their meds!” she says.
When that happens, the patient should find another psychiatrist.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
- Nemade R, Reiss NS, Dombeck M. Historical understandings of depression. Mentalhelp.net. http://www.mentalhelp.net/poc/view_doc.php?type=doc&id=12995&cn=5. Published September 19, 2007. Accessed January 13, 2014.
- Brockington I. A historical perspective on the psychiatry of motherhood. In: Perinatal Stress, Mood, and Anxiety Disorders. Basel, Switzerland: S Karger AG; 2005.
- Yonkers KA, Wisner KL, Stewart DE, et al. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114(3):703–713.
- Pearson RM, Evans J, Kounali D, et al. Maternal depression during pregnancy and the postnatal period. Risks and possible mechanisms for offspring depression at age 18 years [published online ahead of print October 9, 2013]. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2013.2163.
- Hasser C, Brizendine L, Spielvogel A. SSRI use during pregnancy. Current Psychiatry. 2006;5(4):31–40.
- Edinburgh Postnatal Depression Scale. http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf. Accessed January 14, 2014.
- Patient Health Questionnaire (PHQ-9). http://www.cqaimh.org/pdf/tool_phq9.pdf. Accessed January 14, 2014.
- Kroenke K, Spitzer R, Williams W. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
- Nemade R, Reiss NS, Dombeck M. Historical understandings of depression. Mentalhelp.net. http://www.mentalhelp.net/poc/view_doc.php?type=doc&id=12995&cn=5. Published September 19, 2007. Accessed January 13, 2014.
- Brockington I. A historical perspective on the psychiatry of motherhood. In: Perinatal Stress, Mood, and Anxiety Disorders. Basel, Switzerland: S Karger AG; 2005.
- Yonkers KA, Wisner KL, Stewart DE, et al. The management of depression during pregnancy: A report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;114(3):703–713.
- Pearson RM, Evans J, Kounali D, et al. Maternal depression during pregnancy and the postnatal period. Risks and possible mechanisms for offspring depression at age 18 years [published online ahead of print October 9, 2013]. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2013.2163.
- Hasser C, Brizendine L, Spielvogel A. SSRI use during pregnancy. Current Psychiatry. 2006;5(4):31–40.
- Edinburgh Postnatal Depression Scale. http://www.fresno.ucsf.edu/pediatrics/downloads/edinburghscale.pdf. Accessed January 14, 2014.
- Patient Health Questionnaire (PHQ-9). http://www.cqaimh.org/pdf/tool_phq9.pdf. Accessed January 14, 2014.
- Kroenke K, Spitzer R, Williams W. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
Birth weight, not postterm delivery, puts a baby at risk for shoulder dystocia
Women who deliver a large infant before 40 weeks’ gestation have a higher risk of shoulder dystocia than those who deliver a large infant at 40 weeks’ gestation or later, according to a population-based study of all vaginal deliveries in Norway from 1969 to 2009 (n = 2,014,956).1 The increased risk of shoulder dystocia in deliveries before 40 weeks’ gestation was especially pronounced in pregnancies complicated by diabetes.
Large infants were defined as those weighing 3,500 g or more at delivery.
Related Article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial, May 2013)
DETAILS OF THE STUDY
Using the Medical Birth Registry of Norway, Overland and colleagues analyzed all vaginal deliveries of a singleton fetus in cephalic presentation over 30 years, calculating the incidence of shoulder dystocia by gestational age at delivery and estimating both crude and adjusted odds ratios.
Overall, the incidence of shoulder dystocia was 0.73%, and it increased along with gestational age at delivery. Using delivery at 40 to 41 weeks of gestation as the reference, Overland and colleagues found the following crude odds ratios (OR) for shoulder dystocia:
- delivery before 36 weeks: 0.27 (95% confidence interval [CI], 0.22–0.33)
- delivery at 42–43 weeks: 1.17 (95% CI, 1.11–1.22).
However, after adjustment for birth weight, the adjusted OR for shoulder dystocia was:
- delivery at 32–35 weeks: 2.92 (95% CI, 1.54–5.52)
- delivery at 42–43 weeks: 0.91 (95% CI, 0.50–1.66).
Among gestations affected by diabetes (n = 11,188), the incidence of shoulder dystocia was 3.95%.
Related Article: STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start, March 2013)
LONGER PREGNANCIES MAY BE BETTER “PRIMED” FOR DELIVERY
The surprising finding that the risk of shoulder dystocia is lower in postterm infants than in infants delivered prior to 40 weeks at a given birth weight “is not easily explained,” write Overland and colleagues.1 “A successful delivery depends on a complex interplay between the uterus, the pelvis (the pelvic girdle and the pelvic floor muscles) and the offspring…. The physiological changes that occur during pregnancy to prime the pregnant woman and the offspring for delivery are likely to be complete by the estimated term. Hence, the risk for delivery complications, such as shoulder dystocia, may be increased in deliveries before term,” the investigators theorize.1
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Reference
- Overland EA, Vatten, LJ, Eskild A. Pregnancy week at delivery and the risk of shoulder dystocia: a population study of 2,014,956 deliveries. BJOG. 2014;121:34–42.
Women who deliver a large infant before 40 weeks’ gestation have a higher risk of shoulder dystocia than those who deliver a large infant at 40 weeks’ gestation or later, according to a population-based study of all vaginal deliveries in Norway from 1969 to 2009 (n = 2,014,956).1 The increased risk of shoulder dystocia in deliveries before 40 weeks’ gestation was especially pronounced in pregnancies complicated by diabetes.
Large infants were defined as those weighing 3,500 g or more at delivery.
Related Article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial, May 2013)
DETAILS OF THE STUDY
Using the Medical Birth Registry of Norway, Overland and colleagues analyzed all vaginal deliveries of a singleton fetus in cephalic presentation over 30 years, calculating the incidence of shoulder dystocia by gestational age at delivery and estimating both crude and adjusted odds ratios.
Overall, the incidence of shoulder dystocia was 0.73%, and it increased along with gestational age at delivery. Using delivery at 40 to 41 weeks of gestation as the reference, Overland and colleagues found the following crude odds ratios (OR) for shoulder dystocia:
- delivery before 36 weeks: 0.27 (95% confidence interval [CI], 0.22–0.33)
- delivery at 42–43 weeks: 1.17 (95% CI, 1.11–1.22).
However, after adjustment for birth weight, the adjusted OR for shoulder dystocia was:
- delivery at 32–35 weeks: 2.92 (95% CI, 1.54–5.52)
- delivery at 42–43 weeks: 0.91 (95% CI, 0.50–1.66).
Among gestations affected by diabetes (n = 11,188), the incidence of shoulder dystocia was 3.95%.
Related Article: STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start, March 2013)
LONGER PREGNANCIES MAY BE BETTER “PRIMED” FOR DELIVERY
The surprising finding that the risk of shoulder dystocia is lower in postterm infants than in infants delivered prior to 40 weeks at a given birth weight “is not easily explained,” write Overland and colleagues.1 “A successful delivery depends on a complex interplay between the uterus, the pelvis (the pelvic girdle and the pelvic floor muscles) and the offspring…. The physiological changes that occur during pregnancy to prime the pregnant woman and the offspring for delivery are likely to be complete by the estimated term. Hence, the risk for delivery complications, such as shoulder dystocia, may be increased in deliveries before term,” the investigators theorize.1
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Women who deliver a large infant before 40 weeks’ gestation have a higher risk of shoulder dystocia than those who deliver a large infant at 40 weeks’ gestation or later, according to a population-based study of all vaginal deliveries in Norway from 1969 to 2009 (n = 2,014,956).1 The increased risk of shoulder dystocia in deliveries before 40 weeks’ gestation was especially pronounced in pregnancies complicated by diabetes.
Large infants were defined as those weighing 3,500 g or more at delivery.
Related Article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial, May 2013)
DETAILS OF THE STUDY
Using the Medical Birth Registry of Norway, Overland and colleagues analyzed all vaginal deliveries of a singleton fetus in cephalic presentation over 30 years, calculating the incidence of shoulder dystocia by gestational age at delivery and estimating both crude and adjusted odds ratios.
Overall, the incidence of shoulder dystocia was 0.73%, and it increased along with gestational age at delivery. Using delivery at 40 to 41 weeks of gestation as the reference, Overland and colleagues found the following crude odds ratios (OR) for shoulder dystocia:
- delivery before 36 weeks: 0.27 (95% confidence interval [CI], 0.22–0.33)
- delivery at 42–43 weeks: 1.17 (95% CI, 1.11–1.22).
However, after adjustment for birth weight, the adjusted OR for shoulder dystocia was:
- delivery at 32–35 weeks: 2.92 (95% CI, 1.54–5.52)
- delivery at 42–43 weeks: 0.91 (95% CI, 0.50–1.66).
Among gestations affected by diabetes (n = 11,188), the incidence of shoulder dystocia was 3.95%.
Related Article: STOP all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Ronald T. Burkman, MD (Stop/Start, March 2013)
LONGER PREGNANCIES MAY BE BETTER “PRIMED” FOR DELIVERY
The surprising finding that the risk of shoulder dystocia is lower in postterm infants than in infants delivered prior to 40 weeks at a given birth weight “is not easily explained,” write Overland and colleagues.1 “A successful delivery depends on a complex interplay between the uterus, the pelvis (the pelvic girdle and the pelvic floor muscles) and the offspring…. The physiological changes that occur during pregnancy to prime the pregnant woman and the offspring for delivery are likely to be complete by the estimated term. Hence, the risk for delivery complications, such as shoulder dystocia, may be increased in deliveries before term,” the investigators theorize.1
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
Reference
- Overland EA, Vatten, LJ, Eskild A. Pregnancy week at delivery and the risk of shoulder dystocia: a population study of 2,014,956 deliveries. BJOG. 2014;121:34–42.
Reference
- Overland EA, Vatten, LJ, Eskild A. Pregnancy week at delivery and the risk of shoulder dystocia: a population study of 2,014,956 deliveries. BJOG. 2014;121:34–42.
The robot is broadly accessible less than 10 years after its introduction to gynecologic surgery
Use of the robot has skyrocketed in recent years, with 84% of reproductive and gynecologic surgeons reporting access to the technology less than 10 years after its approval for gynecologic surgery by the US Food and Drug Administration. This and other findings from a survey of members of the American Society for Reproductive Medicine (ASRM) and AAGL were presented in a poster at the 42nd AAGL Global Congress in Washington, DC.1
Access to robotic assistance was highest among surgeons based in academic centers (93%) and lowest among those in private practice (77%), but remained high overall (84%).
Related article: The robot is gaining ground in gynecologic surgery.
Should you be using it? (An expert roundtable; April 2013)
Other findings of the survey:
- 85% of residents and fellows reported robotic training, with the greatest exposure to training reported in American Congress of Obstetricians and Gynecologists (ACOG) Districts IV (96%) and VI (100%) and less exposure in District I (72%). District IV comprises the District of Columbia, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Puerto Rico, and the West Indies. District VI comprises Illinois, Iowa, Minnesota, Nebraska, North Dakota, South Dakota, Wisconsin, Manitoba, and Saskatchewan. And District I comprises the Atlantic provinces (New Brunswick, Newfoundland, Nova Scotia, Prince Edward Island), Connecticut, Maine, Massachusetts, New Hampshire, Quebec, Rhode Island, and Vermont.
- Sixty-one percent of surgeons had earned or were planning to earn credentials in robotic surgery, with no difference between districts or types of practice. The figure did vary by subspecialty, however, with 100% of gynecologic oncologists reporting having earned or planning to earn credentials, compared with 79% of minimally invasive gynecologic surgeons, 77% of urogynecologists, 67% of ObGyns, 46% of gynecologists (no obstetric practice), and 44% of reproductive endocrinologists and infertility specialists.
- Some surgeons declined to use the robot. Surgeons who had access to a robot but who chose not to earn privileges gave the following reasons: high cost, 20%; increased time in the operating room (OR), 18%; need for additional training, 10%; additional OR time unavailable, 8%; cost of training, 4%; safety issues, 1%; and possible need for additional ports, 1%. There was greater concern about cost and increased operative time among private practitioners (24% and 25%, respectively) than academic physicians (13% and 15%, respectively).
A link to the online survey was emailed to all members of ASRM and AAGL in June 2012, with 561 practicing gynecologic laparoscopic surgeons and 138 residents and fellows responding, for a response rate of 15%.
Overall, investigators identified no single overriding barrier to use of the robot.
Most surgeons are satisfied with the energy sources they now use
The same survey included questions about surgeons’ attitudes toward various energy sources, including monopolar, bipolar, ultrasonic, laser, and other forms of energy. It found that 94% and 93% of respondents were satisfied or very satisfied with the primary energy source they currently used in the management of endometriosis and myomectomy, respectively. Seventy-nine percent reported having used a CO2 laser.
For the surgical management of endometriosis, practicing surgeons preferred:
- monopolar energy, 33%
- bipolar energy, 22%
- ultrasonic devices, 21%
- laser energy, 12%
- other energy source, 9%.
For myomectomy, practicing surgeons preferred:
- monopolar energy, 43%
- bipolar energy, 21%
- ultrasonic devices, 14%
- laser energy, 2%
- other energy source, 12%.
For colpotomy, practicing surgeons preferred:
- monopolar energy, 35%
- bipolar energy, 17%
- ultrasonic devices, 19%
- other energy source, 10%.
Among residents and fellows, the preference was greatest for monopolar energy for endometriosis, myomectomy, and colpotomy (44%, 41%, and 41%, respectively).
As for complications, practicing surgeons reported 78 related to endometriosis surgery and 73 related to myomectomy. The most common sites of complications were the bladder, ureter, and bowel. Unanticipated bleeding was also common.
Reference
- Bailey AP, Correia KF, Missmer SA, Gargiulo AR. Attitudes of minimally invasive reproductive and gynecologic surgeons toward robotic surgery. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
Use of the robot has skyrocketed in recent years, with 84% of reproductive and gynecologic surgeons reporting access to the technology less than 10 years after its approval for gynecologic surgery by the US Food and Drug Administration. This and other findings from a survey of members of the American Society for Reproductive Medicine (ASRM) and AAGL were presented in a poster at the 42nd AAGL Global Congress in Washington, DC.1
Access to robotic assistance was highest among surgeons based in academic centers (93%) and lowest among those in private practice (77%), but remained high overall (84%).
Related article: The robot is gaining ground in gynecologic surgery.
Should you be using it? (An expert roundtable; April 2013)
Other findings of the survey:
- 85% of residents and fellows reported robotic training, with the greatest exposure to training reported in American Congress of Obstetricians and Gynecologists (ACOG) Districts IV (96%) and VI (100%) and less exposure in District I (72%). District IV comprises the District of Columbia, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Puerto Rico, and the West Indies. District VI comprises Illinois, Iowa, Minnesota, Nebraska, North Dakota, South Dakota, Wisconsin, Manitoba, and Saskatchewan. And District I comprises the Atlantic provinces (New Brunswick, Newfoundland, Nova Scotia, Prince Edward Island), Connecticut, Maine, Massachusetts, New Hampshire, Quebec, Rhode Island, and Vermont.
- Sixty-one percent of surgeons had earned or were planning to earn credentials in robotic surgery, with no difference between districts or types of practice. The figure did vary by subspecialty, however, with 100% of gynecologic oncologists reporting having earned or planning to earn credentials, compared with 79% of minimally invasive gynecologic surgeons, 77% of urogynecologists, 67% of ObGyns, 46% of gynecologists (no obstetric practice), and 44% of reproductive endocrinologists and infertility specialists.
- Some surgeons declined to use the robot. Surgeons who had access to a robot but who chose not to earn privileges gave the following reasons: high cost, 20%; increased time in the operating room (OR), 18%; need for additional training, 10%; additional OR time unavailable, 8%; cost of training, 4%; safety issues, 1%; and possible need for additional ports, 1%. There was greater concern about cost and increased operative time among private practitioners (24% and 25%, respectively) than academic physicians (13% and 15%, respectively).
A link to the online survey was emailed to all members of ASRM and AAGL in June 2012, with 561 practicing gynecologic laparoscopic surgeons and 138 residents and fellows responding, for a response rate of 15%.
Overall, investigators identified no single overriding barrier to use of the robot.
Most surgeons are satisfied with the energy sources they now use
The same survey included questions about surgeons’ attitudes toward various energy sources, including monopolar, bipolar, ultrasonic, laser, and other forms of energy. It found that 94% and 93% of respondents were satisfied or very satisfied with the primary energy source they currently used in the management of endometriosis and myomectomy, respectively. Seventy-nine percent reported having used a CO2 laser.
For the surgical management of endometriosis, practicing surgeons preferred:
- monopolar energy, 33%
- bipolar energy, 22%
- ultrasonic devices, 21%
- laser energy, 12%
- other energy source, 9%.
For myomectomy, practicing surgeons preferred:
- monopolar energy, 43%
- bipolar energy, 21%
- ultrasonic devices, 14%
- laser energy, 2%
- other energy source, 12%.
For colpotomy, practicing surgeons preferred:
- monopolar energy, 35%
- bipolar energy, 17%
- ultrasonic devices, 19%
- other energy source, 10%.
Among residents and fellows, the preference was greatest for monopolar energy for endometriosis, myomectomy, and colpotomy (44%, 41%, and 41%, respectively).
As for complications, practicing surgeons reported 78 related to endometriosis surgery and 73 related to myomectomy. The most common sites of complications were the bladder, ureter, and bowel. Unanticipated bleeding was also common.
Use of the robot has skyrocketed in recent years, with 84% of reproductive and gynecologic surgeons reporting access to the technology less than 10 years after its approval for gynecologic surgery by the US Food and Drug Administration. This and other findings from a survey of members of the American Society for Reproductive Medicine (ASRM) and AAGL were presented in a poster at the 42nd AAGL Global Congress in Washington, DC.1
Access to robotic assistance was highest among surgeons based in academic centers (93%) and lowest among those in private practice (77%), but remained high overall (84%).
Related article: The robot is gaining ground in gynecologic surgery.
Should you be using it? (An expert roundtable; April 2013)
Other findings of the survey:
- 85% of residents and fellows reported robotic training, with the greatest exposure to training reported in American Congress of Obstetricians and Gynecologists (ACOG) Districts IV (96%) and VI (100%) and less exposure in District I (72%). District IV comprises the District of Columbia, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Puerto Rico, and the West Indies. District VI comprises Illinois, Iowa, Minnesota, Nebraska, North Dakota, South Dakota, Wisconsin, Manitoba, and Saskatchewan. And District I comprises the Atlantic provinces (New Brunswick, Newfoundland, Nova Scotia, Prince Edward Island), Connecticut, Maine, Massachusetts, New Hampshire, Quebec, Rhode Island, and Vermont.
- Sixty-one percent of surgeons had earned or were planning to earn credentials in robotic surgery, with no difference between districts or types of practice. The figure did vary by subspecialty, however, with 100% of gynecologic oncologists reporting having earned or planning to earn credentials, compared with 79% of minimally invasive gynecologic surgeons, 77% of urogynecologists, 67% of ObGyns, 46% of gynecologists (no obstetric practice), and 44% of reproductive endocrinologists and infertility specialists.
- Some surgeons declined to use the robot. Surgeons who had access to a robot but who chose not to earn privileges gave the following reasons: high cost, 20%; increased time in the operating room (OR), 18%; need for additional training, 10%; additional OR time unavailable, 8%; cost of training, 4%; safety issues, 1%; and possible need for additional ports, 1%. There was greater concern about cost and increased operative time among private practitioners (24% and 25%, respectively) than academic physicians (13% and 15%, respectively).
A link to the online survey was emailed to all members of ASRM and AAGL in June 2012, with 561 practicing gynecologic laparoscopic surgeons and 138 residents and fellows responding, for a response rate of 15%.
Overall, investigators identified no single overriding barrier to use of the robot.
Most surgeons are satisfied with the energy sources they now use
The same survey included questions about surgeons’ attitudes toward various energy sources, including monopolar, bipolar, ultrasonic, laser, and other forms of energy. It found that 94% and 93% of respondents were satisfied or very satisfied with the primary energy source they currently used in the management of endometriosis and myomectomy, respectively. Seventy-nine percent reported having used a CO2 laser.
For the surgical management of endometriosis, practicing surgeons preferred:
- monopolar energy, 33%
- bipolar energy, 22%
- ultrasonic devices, 21%
- laser energy, 12%
- other energy source, 9%.
For myomectomy, practicing surgeons preferred:
- monopolar energy, 43%
- bipolar energy, 21%
- ultrasonic devices, 14%
- laser energy, 2%
- other energy source, 12%.
For colpotomy, practicing surgeons preferred:
- monopolar energy, 35%
- bipolar energy, 17%
- ultrasonic devices, 19%
- other energy source, 10%.
Among residents and fellows, the preference was greatest for monopolar energy for endometriosis, myomectomy, and colpotomy (44%, 41%, and 41%, respectively).
As for complications, practicing surgeons reported 78 related to endometriosis surgery and 73 related to myomectomy. The most common sites of complications were the bladder, ureter, and bowel. Unanticipated bleeding was also common.
Reference
- Bailey AP, Correia KF, Missmer SA, Gargiulo AR. Attitudes of minimally invasive reproductive and gynecologic surgeons toward robotic surgery. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
Reference
- Bailey AP, Correia KF, Missmer SA, Gargiulo AR. Attitudes of minimally invasive reproductive and gynecologic surgeons toward robotic surgery. Poster presented at: 42nd AAGL Global Congress on Minimally Invasive Surgery; November 10–14, 2013; Washington, DC.
Private practice remains strong despite an increase in hospital employment
Although more physicians today are employed by hospitals than in the past, the overwhelming majority of doctors still work in private practices, according to 2012 data from the Physician Practice Benchmark Study (PPBS) conducted by the American Medical Association (AMA).1
The survey shows that 53.2% of physicians were self-employed in 2012, and 60% were operating in practices wholly owned by physicians. Only 23% of physicians worked in practices that were partially or fully owned by a hospital, and only 5.6% were directly employed by a hospital.1
The AMA estimates that 18.4% of physicians worked in solo practices in 2012, a decline of about 6% from the previous AMA survey in 2207/2008.1 In 1983, 40.5% of physicians were in solo practice.1
“To paraphrase Mark Twain, the reports of the death of private practice medicine have been greatly exaggerated,” said AMA President Ardis Dee Hoven, MD, in presenting the figures.1
And AMA investigators Carol C. Kane, PhD, and David W. Emmons, PhD, who authored the report, noted: “After a 5-year gap in physician-level data, the 2012 PPBS offers an update on the status of physician practice arrangements, and allows for a nationally representative response to the numerous articles of the past several years that have highlighted a surge in the employment of physicians by hospitals and the ‘death’ of private practice.”1
Details of the survey
Like earlier AMA surveys, the PPBS involved a nationally representative random sample of physicians who had completed residency, practiced at least 20 hours per week, and were not employed by the federal government.
Unlike earlier AMA surveys, which targeted AMA members, the 2012 PPBS utilized the Epocrates Honors market research panel rather than the AMA Masterfile. The reason for this switch: declining participation rates for surveys utilizing the Masterfile.
Another distinction: Earlier surveys failed to ask specifically whether the respondent’s practice was owned by its physician members or by a larger entity, such as a hospital. They also overlooked the organizational structure of practices. The 2012 survey addressed both issues.
The PPBS went to 14,750 physicians. Of these, 3,466 physicians responded, a response rate of 28%.1
FINDINGS ON THE STRUCTURE OF PRACTICE
Ownership status
In 2012, 53.2% of physicians fully or partly owned their practice (a decline of 8.0% since 2007/2008), 41.8% were employed, and 5.0% were independent contractors.1
Younger physicians were less likely to own their practice than older physicians were. Among physicians under age 40, the ownership rate was 43.3%, compared with 60.0% among doctors aged 55 years or older.1
Women, too, were less likely to own their practice (38.7% vs 59.6% for men).1
Type of practice
The most common type of practice setting was the single-specialty practice, reported by 45.5% of physicians. Women were less likely to report single-specialty practice than men (39.7% vs 48.0%).1
Among ObGyns, single-specialty practice was reported by 52.7% of respondents.1
Multispecialty practice was reported by 22.1% of respondents. Among ObGyns, that figure was 17.9%.1
Solo practice was reported by 18.4% of respondents but varied significantly by age. Among physicians under age 40, only 10% reported solo practice, compared with 25.3% of physicians aged 55 or older. Among women, solo practice was reported by 21.0%, compared with 17.3% among men. Among all ObGyns (men and women), 20.6% reported solo practice.1
Only 5.6% of physicians reported direct hospital employment. Among ObGyns, the figure was 2.3%.1
Size of the practice
Sixty percent of respondents (in all practice settings) reported working in a practice with fewer than 10 physicians. Sixteen percent reported working in a practice with 10 to 24 physicians, 7.1% in practices with 25 to 49 physicians, and 12.2% in practices with more than 50 physicians. Hospital employees were not asked about the number of physicians in their practice setting.
Among physicians in single-specialty practices, 39.0% reported that their practice included no more than four physicians, compared with 5.3% who reported a practice of at least 50 physicians.1
Among physicians in multispecialty practice, only 9.9% reported having no more than four physicians, compared with 35.5% reporting at least 50 physicians.1
Hospital ownership
Twenty-three percent of all respondents reported working in a practice that was at least partially owned by a hospital. Of these physicians, 14.7% worked in practices fully owned by a hospital.
Physicians who worked in a single-specialty practice were more likely to report physician ownership of that practice (71.8%) than were doctors in multi-specialty practice (36.9%). And physicians in small practices (single- or multispecialty) were more likely to report physician ownership than physicians in large practices: 72% of physicians in groups of two to four reported physician ownership, compared with 45.6% of physicians in groups of 50 or more. Physicians in large practices (≥50 members) also were more likely to report ownership by a not-for-profit foundation.1
After exploring the issue of hospital ownership from several different angles, Kane and Emmons found that the association between increasing practice size and hospital ownership did not persist. Rather, they found that the “wider scope of practice in multispecialty groups, not practice size, drives hospital ownership.” They theorized that hospitals are more likely to buy primary care practices to gain a strong referral base, and this theory was borne out by the data, which showed that primary care physicians are more likely to report hospital ownership.1
RELATED ARTICLE: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Two final comments
Kane and Emmons point out that their analysis doesn’t “capture relationships that are short of full employment” and, therefore, may underestimate “the degree of integration between physicians and hospitals.”1
Although the decline in solo practice may have been accelerated by reform measures in recent years, the shift was “already well underway in the early 1990s,” Kane and Emmons observed.1
Reference
- Kane CK, Emmons DW. Policy Research Perspectives: New Data on Physician Practice Arrangements: Private Practice Remains Strong Despite Shifts Toward Hospital Employment. American Medical Association. September 2013. http://www.ama-assn.org/resources/doc/health-policy/prp-physician-practice-arrangements.pdf. Accessed October 25, 2013.
Although more physicians today are employed by hospitals than in the past, the overwhelming majority of doctors still work in private practices, according to 2012 data from the Physician Practice Benchmark Study (PPBS) conducted by the American Medical Association (AMA).1
The survey shows that 53.2% of physicians were self-employed in 2012, and 60% were operating in practices wholly owned by physicians. Only 23% of physicians worked in practices that were partially or fully owned by a hospital, and only 5.6% were directly employed by a hospital.1
The AMA estimates that 18.4% of physicians worked in solo practices in 2012, a decline of about 6% from the previous AMA survey in 2207/2008.1 In 1983, 40.5% of physicians were in solo practice.1
“To paraphrase Mark Twain, the reports of the death of private practice medicine have been greatly exaggerated,” said AMA President Ardis Dee Hoven, MD, in presenting the figures.1
And AMA investigators Carol C. Kane, PhD, and David W. Emmons, PhD, who authored the report, noted: “After a 5-year gap in physician-level data, the 2012 PPBS offers an update on the status of physician practice arrangements, and allows for a nationally representative response to the numerous articles of the past several years that have highlighted a surge in the employment of physicians by hospitals and the ‘death’ of private practice.”1
Details of the survey
Like earlier AMA surveys, the PPBS involved a nationally representative random sample of physicians who had completed residency, practiced at least 20 hours per week, and were not employed by the federal government.
Unlike earlier AMA surveys, which targeted AMA members, the 2012 PPBS utilized the Epocrates Honors market research panel rather than the AMA Masterfile. The reason for this switch: declining participation rates for surveys utilizing the Masterfile.
Another distinction: Earlier surveys failed to ask specifically whether the respondent’s practice was owned by its physician members or by a larger entity, such as a hospital. They also overlooked the organizational structure of practices. The 2012 survey addressed both issues.
The PPBS went to 14,750 physicians. Of these, 3,466 physicians responded, a response rate of 28%.1
FINDINGS ON THE STRUCTURE OF PRACTICE
Ownership status
In 2012, 53.2% of physicians fully or partly owned their practice (a decline of 8.0% since 2007/2008), 41.8% were employed, and 5.0% were independent contractors.1
Younger physicians were less likely to own their practice than older physicians were. Among physicians under age 40, the ownership rate was 43.3%, compared with 60.0% among doctors aged 55 years or older.1
Women, too, were less likely to own their practice (38.7% vs 59.6% for men).1
Type of practice
The most common type of practice setting was the single-specialty practice, reported by 45.5% of physicians. Women were less likely to report single-specialty practice than men (39.7% vs 48.0%).1
Among ObGyns, single-specialty practice was reported by 52.7% of respondents.1
Multispecialty practice was reported by 22.1% of respondents. Among ObGyns, that figure was 17.9%.1
Solo practice was reported by 18.4% of respondents but varied significantly by age. Among physicians under age 40, only 10% reported solo practice, compared with 25.3% of physicians aged 55 or older. Among women, solo practice was reported by 21.0%, compared with 17.3% among men. Among all ObGyns (men and women), 20.6% reported solo practice.1
Only 5.6% of physicians reported direct hospital employment. Among ObGyns, the figure was 2.3%.1
Size of the practice
Sixty percent of respondents (in all practice settings) reported working in a practice with fewer than 10 physicians. Sixteen percent reported working in a practice with 10 to 24 physicians, 7.1% in practices with 25 to 49 physicians, and 12.2% in practices with more than 50 physicians. Hospital employees were not asked about the number of physicians in their practice setting.
Among physicians in single-specialty practices, 39.0% reported that their practice included no more than four physicians, compared with 5.3% who reported a practice of at least 50 physicians.1
Among physicians in multispecialty practice, only 9.9% reported having no more than four physicians, compared with 35.5% reporting at least 50 physicians.1
Hospital ownership
Twenty-three percent of all respondents reported working in a practice that was at least partially owned by a hospital. Of these physicians, 14.7% worked in practices fully owned by a hospital.
Physicians who worked in a single-specialty practice were more likely to report physician ownership of that practice (71.8%) than were doctors in multi-specialty practice (36.9%). And physicians in small practices (single- or multispecialty) were more likely to report physician ownership than physicians in large practices: 72% of physicians in groups of two to four reported physician ownership, compared with 45.6% of physicians in groups of 50 or more. Physicians in large practices (≥50 members) also were more likely to report ownership by a not-for-profit foundation.1
After exploring the issue of hospital ownership from several different angles, Kane and Emmons found that the association between increasing practice size and hospital ownership did not persist. Rather, they found that the “wider scope of practice in multispecialty groups, not practice size, drives hospital ownership.” They theorized that hospitals are more likely to buy primary care practices to gain a strong referral base, and this theory was borne out by the data, which showed that primary care physicians are more likely to report hospital ownership.1
RELATED ARTICLE: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Two final comments
Kane and Emmons point out that their analysis doesn’t “capture relationships that are short of full employment” and, therefore, may underestimate “the degree of integration between physicians and hospitals.”1
Although the decline in solo practice may have been accelerated by reform measures in recent years, the shift was “already well underway in the early 1990s,” Kane and Emmons observed.1
Although more physicians today are employed by hospitals than in the past, the overwhelming majority of doctors still work in private practices, according to 2012 data from the Physician Practice Benchmark Study (PPBS) conducted by the American Medical Association (AMA).1
The survey shows that 53.2% of physicians were self-employed in 2012, and 60% were operating in practices wholly owned by physicians. Only 23% of physicians worked in practices that were partially or fully owned by a hospital, and only 5.6% were directly employed by a hospital.1
The AMA estimates that 18.4% of physicians worked in solo practices in 2012, a decline of about 6% from the previous AMA survey in 2207/2008.1 In 1983, 40.5% of physicians were in solo practice.1
“To paraphrase Mark Twain, the reports of the death of private practice medicine have been greatly exaggerated,” said AMA President Ardis Dee Hoven, MD, in presenting the figures.1
And AMA investigators Carol C. Kane, PhD, and David W. Emmons, PhD, who authored the report, noted: “After a 5-year gap in physician-level data, the 2012 PPBS offers an update on the status of physician practice arrangements, and allows for a nationally representative response to the numerous articles of the past several years that have highlighted a surge in the employment of physicians by hospitals and the ‘death’ of private practice.”1
Details of the survey
Like earlier AMA surveys, the PPBS involved a nationally representative random sample of physicians who had completed residency, practiced at least 20 hours per week, and were not employed by the federal government.
Unlike earlier AMA surveys, which targeted AMA members, the 2012 PPBS utilized the Epocrates Honors market research panel rather than the AMA Masterfile. The reason for this switch: declining participation rates for surveys utilizing the Masterfile.
Another distinction: Earlier surveys failed to ask specifically whether the respondent’s practice was owned by its physician members or by a larger entity, such as a hospital. They also overlooked the organizational structure of practices. The 2012 survey addressed both issues.
The PPBS went to 14,750 physicians. Of these, 3,466 physicians responded, a response rate of 28%.1
FINDINGS ON THE STRUCTURE OF PRACTICE
Ownership status
In 2012, 53.2% of physicians fully or partly owned their practice (a decline of 8.0% since 2007/2008), 41.8% were employed, and 5.0% were independent contractors.1
Younger physicians were less likely to own their practice than older physicians were. Among physicians under age 40, the ownership rate was 43.3%, compared with 60.0% among doctors aged 55 years or older.1
Women, too, were less likely to own their practice (38.7% vs 59.6% for men).1
Type of practice
The most common type of practice setting was the single-specialty practice, reported by 45.5% of physicians. Women were less likely to report single-specialty practice than men (39.7% vs 48.0%).1
Among ObGyns, single-specialty practice was reported by 52.7% of respondents.1
Multispecialty practice was reported by 22.1% of respondents. Among ObGyns, that figure was 17.9%.1
Solo practice was reported by 18.4% of respondents but varied significantly by age. Among physicians under age 40, only 10% reported solo practice, compared with 25.3% of physicians aged 55 or older. Among women, solo practice was reported by 21.0%, compared with 17.3% among men. Among all ObGyns (men and women), 20.6% reported solo practice.1
Only 5.6% of physicians reported direct hospital employment. Among ObGyns, the figure was 2.3%.1
Size of the practice
Sixty percent of respondents (in all practice settings) reported working in a practice with fewer than 10 physicians. Sixteen percent reported working in a practice with 10 to 24 physicians, 7.1% in practices with 25 to 49 physicians, and 12.2% in practices with more than 50 physicians. Hospital employees were not asked about the number of physicians in their practice setting.
Among physicians in single-specialty practices, 39.0% reported that their practice included no more than four physicians, compared with 5.3% who reported a practice of at least 50 physicians.1
Among physicians in multispecialty practice, only 9.9% reported having no more than four physicians, compared with 35.5% reporting at least 50 physicians.1
Hospital ownership
Twenty-three percent of all respondents reported working in a practice that was at least partially owned by a hospital. Of these physicians, 14.7% worked in practices fully owned by a hospital.
Physicians who worked in a single-specialty practice were more likely to report physician ownership of that practice (71.8%) than were doctors in multi-specialty practice (36.9%). And physicians in small practices (single- or multispecialty) were more likely to report physician ownership than physicians in large practices: 72% of physicians in groups of two to four reported physician ownership, compared with 45.6% of physicians in groups of 50 or more. Physicians in large practices (≥50 members) also were more likely to report ownership by a not-for-profit foundation.1
After exploring the issue of hospital ownership from several different angles, Kane and Emmons found that the association between increasing practice size and hospital ownership did not persist. Rather, they found that the “wider scope of practice in multispecialty groups, not practice size, drives hospital ownership.” They theorized that hospitals are more likely to buy primary care practices to gain a strong referral base, and this theory was borne out by the data, which showed that primary care physicians are more likely to report hospital ownership.1
RELATED ARTICLE: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Two final comments
Kane and Emmons point out that their analysis doesn’t “capture relationships that are short of full employment” and, therefore, may underestimate “the degree of integration between physicians and hospitals.”1
Although the decline in solo practice may have been accelerated by reform measures in recent years, the shift was “already well underway in the early 1990s,” Kane and Emmons observed.1
Reference
- Kane CK, Emmons DW. Policy Research Perspectives: New Data on Physician Practice Arrangements: Private Practice Remains Strong Despite Shifts Toward Hospital Employment. American Medical Association. September 2013. http://www.ama-assn.org/resources/doc/health-policy/prp-physician-practice-arrangements.pdf. Accessed October 25, 2013.
Reference
- Kane CK, Emmons DW. Policy Research Perspectives: New Data on Physician Practice Arrangements: Private Practice Remains Strong Despite Shifts Toward Hospital Employment. American Medical Association. September 2013. http://www.ama-assn.org/resources/doc/health-policy/prp-physician-practice-arrangements.pdf. Accessed October 25, 2013.