User login
A Surgical Surge
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Many or most specialties in medicine are adopting a hospitalist model, at least to a limited extent. In fact, hospital care of adult medical patients wasn’t even the first place the idea was adopted.
In talking with people from hundreds of institutions it seems clear the idea appeared earlier and grew more quickly in pediatrics than adult medicine. And in the past 10 to 15 years, fields like obstetrics (“laborists”), psychiatry, gastroenterology, and many others have slowly begun to adopt the hospitalist model.
One of the most recent disciplines to join the parade is general surgery. And when comparing the forces in play for hospitalists in the early 1990s to the current situation for surgical hospitalists, I think we may be close to a surge in surgical hospitalists similar to what we’ve seen with medical hospitalists in the past 10 years.
When I say surgical hospitalists, I’m referring to surgeons with a nearly exclusive inpatient practice. Other terms such as surgicalist, acute care surgeon, and traumatologist overlap to some degree but have ambiguous meanings.
Generalizations
For some months I have contacted all the surgical hospitalist practices I can find to learn what forces led to their creation and how they are structured. Several common themes are emerging:
Prevalence: There are probably no more than 20 to 40 surgical hospitalist practices, but many institutions are considering the idea. This is similar to the situation for medical hospitalists in the early to mid-1990s.
Driver to start program: In every program I’ve found, the main impetus to start it was to address the burden of emergency department (ED) call for existing general surgeons. Like primary care, ED call is regarded as unattractive because it is unpredictable (lots of night and weekend work), usually has a poor payer mix, and many general surgeons have seen the “center of gravity” of their practice move away from the hospital toward an ambulatory surgery center over the past 10 years or so. Additionally, many general surgeons are increasingly uncomfortable caring for trauma patients because of recent changes in that field. (For an excellent discussion of the changing nature of general surgery and trauma care see “The Acute Care Surgeon” in The Hospitalist, May 2006, p. 25.)
Case volume: General surgery case volume tends to go up at a hospital that puts a surgical hospitalist program in place. When existing surgeons are relieved of ED call they increase their volume of (mostly elective) surgery. The availability of surgical hospitalists may mean fewer emergency cases presenting to the ED are referred elsewhere (which may happen when non-hospitalist surgeons are required to take ED call). These changes in case volume and the timing of the operations (e.g., volume of night surgeries may go up) may require adjustments to operating room staffing and scheduling. Presumably this increased volume would not occur in an area oversupplied with surgeons.
Economics: Like nearly all medical hospitalist programs, surgical hospitalist practices are not viable without financial support in addition to collected professional fees. In all cases I am aware of, this support comes from the sponsoring hospital.
While the cost may be similar to what the hospital might have paid for existing surgeons to take ED call, hospitals seem to be getting a better return on that investment with surgical hospitalists. A small group of surgical hospitalists can handle the increased volume and all ED calls, improving clinical and service quality. Some institutions report that surgical hospitalists are much more attentive to billing for nonoperative work than their predecessors.
Structure: Programs should have an outpatient clinic where the surgical hospitalists can provide post-operative follow-up. In most cases, each surgeon spends only half a day a week in the clinic.
Scope of practice: All surgical hospitalist practices take most or all ED general surgery calls. In some institutions, the surgical hospitalist also leads the trauma team. Other duties at a few institutions include things like managing a wound-care clinic and being on-call to place lines.
Opinion of other surgeons: Community private practice surgeons tend to support these programs, but most institutions limit or prohibit surgical hospitalists from accepting elective referrals. Community surgeons are still offered the option of remaining on the ED call schedule—as might be the case for surgeons new to the community. At least one institution reported that the presence of surgical hospitalists improved recruitment of non-hospitalist general surgeons. However, I am also aware of one program put into place largely at the insistence of the existing surgeons. Those same surgeons later insisted it be dissolved because they saw it as unwanted competition.
Staff needs: Surgical hospitalist practices nearly always require fewer doctors than a medical hospitalist practice in the same institution. This can lead to a tension between having the right number of surgical hospitalists for the case volume (often just one or two doctors) and enough to provide for a reasonable call schedule. Existing groups have adopted a number of strategies.
Groups with only two doctors often have each work seven on/seven off. The doctor on-call for that week takes all night call him/herself. In some practices that have a medical hospitalist in-house all night, it could be reasonable to have routine calls on the surgical patients (e.g., sleeping pills, laxatives, low urine output, fever) first paged to the medical hospitalist, who refers the call to the surgical hospitalist only as needed.
At least one practice has hired enough surgeons so the call burden on each is reasonable. This might be more staff than required for the patient volume: Four surgical hospitalists each work 12-hour shifts in a seven on/seven off schedule. During the seven consecutive night shifts (worked by each surgeon one week in four), patient volume is low.
Some practices hire community surgeons as moonlighters or consider using nurse practitioners or physician’s assistants as first responders at night.
Demographics: Surgical hospitalists are usually midcareer doctors, not surgeons who have recently completed their training. Many say they have gotten burned out with the stress of operating a private practice and prefer hospital work to office work.
Where Will It All Lead?
In every institution I have made contact with, the medical and surgical hospitalists have a good working relationship. Each is available to the other for consults, and they work together so frequently that they can begin to build a greater sense of teamwork. It is important that both groups jointly develop guidelines, such as who admits which type of patients.
If, like primary care doctors, general surgeons and a handful of other specialties with significant hospital volume (such as obstetrics and gastroenterology) move largely to a hospitalist model, U.S. healthcare will have made a remarkable transformation. In the span of my career we will have gone from a system of most doctors seeing patients in and out of the hospital to a division of physician labor such that most doctors practice almost exclusively in only one setting or the other.
I can see how this could be a good thing for patients and medical professionals, but that isn’t a given. For it to turn out we must preserve the elements of the earlier system that worked well and mitigate new problems and complexities. We will need well-designed research to show the economic and quality effects of the hospitalist model on non-primary care fields such as general surgery. We face growing challenges in ensuring excellent communication between inpatient and outpatient caregivers—something that doesn’t work ideally in all medical hospitalist practices.
Let Me Hear From You
I’d like to hear about any surgical hospitalist program you know of so I can add it to my database of information about such programs. And if you’re thinking about becoming a surgical hospitalist or you’re an institution thinking about starting such a practice, feel free to contact me so we can compare notes. I can be reached at (425) 467-3316, or by e-mail: john@jnelson.net. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Haggle With the Hospital
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
A Unit-Based Approach
Would you want all your patients on the same nursing unit? Think about it—no more walking all over the building to see a few patients on each floor.
Because you would be physically present on “your” unit nearly all day, you could develop close working relationships with the nurses and other caregivers, which might improve everyone’s satisfaction with work. Everyone could better anticipate your work flow and communicate this to patients and families. You likely would be paged much less often because the nursing staff could keep track of whether you’re with a patient or off the floor to attend a conference; they could hold non-urgent issues until you get back.
All these things might make you and others more efficient—able to see the same number of patients you see today in less time, while maintaining or improving quality and cost effectiveness.
Sound familiar? The idea that working at only one site leads to efficiency and quality improvement is one of the underpinnings of the hospitalist concept. Instead of covering the outpatient office and hospital every day, doctors can focus on only the hospital or only the office. But what if you extended that idea to focusing your practice on only one unit within the hospital rather than the whole building? Would that be a good idea and lead to the benefits described above, or would that be taking the idea of “focused practice” too far?
Before answering, I should describe the approaches some practices have taken to pursue the benefits of concentrating patients in one part of the hospital. I’ll refer to this idea as “unit-based hospitalists,” the term current SHM President Rusty Holman uses when talking about this idea.
Locate most hospitalist patients in one unit. This is the most common form of unit-based hospitalists. Most institutions find the closest they can get to unit-based hospitalists is to have all hospitalist admissions go to the same floor when that floor has a bed available and the patient doesn’t require placement elsewhere. In such cases, the hospitalist practice might have something like 50% of patients on that floor and 50% dispersed throughout the hospital (telemetry, ICU, surgery floor). So the whole hospitalist practice has a primary “home” within the hospital, while each hospitalist spends part of each day caring for patients elsewhere. This is not very difficult for most hospitals to implement—and many are because most hospitalist patients end up on the “general medical” floor. This lets the hospitalist spend more time on that unit than any other. She can get to know the staff on that floor better, which might lead to many benefits, including improved satisfaction and efficiency.
Locate individual hospitalists on different hospital units. A more pure, but uncommon, form of unit-based hospitalists involves changing the way hospitalists are placed through the institution rather than changing patient placement. Each hospitalist in the group is assigned to a different nursing unit—or perhaps more than one unit—and sees whichever hospitalist patients are placed there. This system has the advantage of the hospitalist working all or most of the day on the same nursing unit, which can foster excellent teamwork. Instead of the nurse having to figure out which hospitalist to page for a particular patient, he simply needs to know, “Who is our hospitalist today?” and can contact that doctor for issues on most patients. Additionally, because the hospitalist will spend nearly the whole day physically on that unit, paging can be reduced significantly.
Despite its advantages, basing an individual hospitalist on a particular unit of the hospital is uncommon because in its purest form it can lead to terrible hospitalist-patient continuity. And, it’s hard to be confident that the disruptions in continuity are worth the benefits of the unit-based system. For example, the practice may have a patient to admit in the ED but can’t know which hospitalist should see the patient until a room is assigned. The fifth-floor hospitalist might go admit the patient in the ED, only to have the patient end up on the third floor, in which case the third-floor hospitalist would take over the next day. And each time the patient transferred to a new unit, either because of medical needs such as telemetry or simply because the hospital is full and needs to move patients, he would get a new hospitalist.
In addition to problems with continuity for patients who occupy more than one unit during their stay, this system would mean individual hospitalist workloads might get far out of balance. One floor might be very busy, while another is slow or limited by nurse staff shortages, and the respective hospitalists would have a correspondingly out-of-balance workload. A group could decide to address these problems by, for example, having the fifth-floor hospitalist see patients in other parts of the hospital in an effort to provide better hospitalist-patient continuity and address out-of-balance patient loads. But if this happens with any regularity it would mean the group has essentially moved back to a non-unit-based system.
In nearly all hospitals it would be unnecessary and unreasonable to assign a hospitalist to each nursing unit because some units tend to have few hospitalist patients. Yet when patients end up in those units because of medical necessity or bed space needs, one of the hospitalists will have to leave his/her unit to see this patient. If this happens often enough, it begins to dilute or negate the benefit of basing a hospitalist in one or two units.
Although one of the potential benefits of the unit-based model is enhanced relationships and integration among hospitalists and other unit-based clinical staff, it would be difficult to ensure that the same one or two hospitalists always work in a particular unit, and would limit scheduling flexibility dramatically. For example, if Dr. Starsky and Dr. Hutch are the unit-based hospitalists for Unit A, what happens if Dr. Starsky and Dr. Hutch are both scheduled to be off for the same block of days? What happens if both are scheduled to work the same block of days? To obtain the benefits of enhanced relationships and better unit integration, the practice would need to ensure that this scheduling overlap rarely happens—and that’s hard to do.
Where is the sweet spot in grouping patients and hospitalists by nursing unit? There is a wide range of opinion about whether unit-based hospital medicine in any form is worth pursuing. Some hospitalists are convinced that grouping all of their patients on the same unit could decrease efficiency because the doctor is nearly always working within view of patients and families and may be regularly interrupted. I am convinced that assigning each hospitalist to a particular unit in the hospital yields the greatest benefits. But I also think most institutions will find that the complexity and costs of this system are simply too high to justify. In that case, the next best approach might be to locate most hospitalist patients on the same unit unless that unit is full or the patient must be placed elsewhere. There is a good chance this is happening in your hospital—even if it isn’t written in the policy manual. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Would you want all your patients on the same nursing unit? Think about it—no more walking all over the building to see a few patients on each floor.
Because you would be physically present on “your” unit nearly all day, you could develop close working relationships with the nurses and other caregivers, which might improve everyone’s satisfaction with work. Everyone could better anticipate your work flow and communicate this to patients and families. You likely would be paged much less often because the nursing staff could keep track of whether you’re with a patient or off the floor to attend a conference; they could hold non-urgent issues until you get back.
All these things might make you and others more efficient—able to see the same number of patients you see today in less time, while maintaining or improving quality and cost effectiveness.
Sound familiar? The idea that working at only one site leads to efficiency and quality improvement is one of the underpinnings of the hospitalist concept. Instead of covering the outpatient office and hospital every day, doctors can focus on only the hospital or only the office. But what if you extended that idea to focusing your practice on only one unit within the hospital rather than the whole building? Would that be a good idea and lead to the benefits described above, or would that be taking the idea of “focused practice” too far?
Before answering, I should describe the approaches some practices have taken to pursue the benefits of concentrating patients in one part of the hospital. I’ll refer to this idea as “unit-based hospitalists,” the term current SHM President Rusty Holman uses when talking about this idea.
Locate most hospitalist patients in one unit. This is the most common form of unit-based hospitalists. Most institutions find the closest they can get to unit-based hospitalists is to have all hospitalist admissions go to the same floor when that floor has a bed available and the patient doesn’t require placement elsewhere. In such cases, the hospitalist practice might have something like 50% of patients on that floor and 50% dispersed throughout the hospital (telemetry, ICU, surgery floor). So the whole hospitalist practice has a primary “home” within the hospital, while each hospitalist spends part of each day caring for patients elsewhere. This is not very difficult for most hospitals to implement—and many are because most hospitalist patients end up on the “general medical” floor. This lets the hospitalist spend more time on that unit than any other. She can get to know the staff on that floor better, which might lead to many benefits, including improved satisfaction and efficiency.
Locate individual hospitalists on different hospital units. A more pure, but uncommon, form of unit-based hospitalists involves changing the way hospitalists are placed through the institution rather than changing patient placement. Each hospitalist in the group is assigned to a different nursing unit—or perhaps more than one unit—and sees whichever hospitalist patients are placed there. This system has the advantage of the hospitalist working all or most of the day on the same nursing unit, which can foster excellent teamwork. Instead of the nurse having to figure out which hospitalist to page for a particular patient, he simply needs to know, “Who is our hospitalist today?” and can contact that doctor for issues on most patients. Additionally, because the hospitalist will spend nearly the whole day physically on that unit, paging can be reduced significantly.
Despite its advantages, basing an individual hospitalist on a particular unit of the hospital is uncommon because in its purest form it can lead to terrible hospitalist-patient continuity. And, it’s hard to be confident that the disruptions in continuity are worth the benefits of the unit-based system. For example, the practice may have a patient to admit in the ED but can’t know which hospitalist should see the patient until a room is assigned. The fifth-floor hospitalist might go admit the patient in the ED, only to have the patient end up on the third floor, in which case the third-floor hospitalist would take over the next day. And each time the patient transferred to a new unit, either because of medical needs such as telemetry or simply because the hospital is full and needs to move patients, he would get a new hospitalist.
In addition to problems with continuity for patients who occupy more than one unit during their stay, this system would mean individual hospitalist workloads might get far out of balance. One floor might be very busy, while another is slow or limited by nurse staff shortages, and the respective hospitalists would have a correspondingly out-of-balance workload. A group could decide to address these problems by, for example, having the fifth-floor hospitalist see patients in other parts of the hospital in an effort to provide better hospitalist-patient continuity and address out-of-balance patient loads. But if this happens with any regularity it would mean the group has essentially moved back to a non-unit-based system.
In nearly all hospitals it would be unnecessary and unreasonable to assign a hospitalist to each nursing unit because some units tend to have few hospitalist patients. Yet when patients end up in those units because of medical necessity or bed space needs, one of the hospitalists will have to leave his/her unit to see this patient. If this happens often enough, it begins to dilute or negate the benefit of basing a hospitalist in one or two units.
Although one of the potential benefits of the unit-based model is enhanced relationships and integration among hospitalists and other unit-based clinical staff, it would be difficult to ensure that the same one or two hospitalists always work in a particular unit, and would limit scheduling flexibility dramatically. For example, if Dr. Starsky and Dr. Hutch are the unit-based hospitalists for Unit A, what happens if Dr. Starsky and Dr. Hutch are both scheduled to be off for the same block of days? What happens if both are scheduled to work the same block of days? To obtain the benefits of enhanced relationships and better unit integration, the practice would need to ensure that this scheduling overlap rarely happens—and that’s hard to do.
Where is the sweet spot in grouping patients and hospitalists by nursing unit? There is a wide range of opinion about whether unit-based hospital medicine in any form is worth pursuing. Some hospitalists are convinced that grouping all of their patients on the same unit could decrease efficiency because the doctor is nearly always working within view of patients and families and may be regularly interrupted. I am convinced that assigning each hospitalist to a particular unit in the hospital yields the greatest benefits. But I also think most institutions will find that the complexity and costs of this system are simply too high to justify. In that case, the next best approach might be to locate most hospitalist patients on the same unit unless that unit is full or the patient must be placed elsewhere. There is a good chance this is happening in your hospital—even if it isn’t written in the policy manual. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Would you want all your patients on the same nursing unit? Think about it—no more walking all over the building to see a few patients on each floor.
Because you would be physically present on “your” unit nearly all day, you could develop close working relationships with the nurses and other caregivers, which might improve everyone’s satisfaction with work. Everyone could better anticipate your work flow and communicate this to patients and families. You likely would be paged much less often because the nursing staff could keep track of whether you’re with a patient or off the floor to attend a conference; they could hold non-urgent issues until you get back.
All these things might make you and others more efficient—able to see the same number of patients you see today in less time, while maintaining or improving quality and cost effectiveness.
Sound familiar? The idea that working at only one site leads to efficiency and quality improvement is one of the underpinnings of the hospitalist concept. Instead of covering the outpatient office and hospital every day, doctors can focus on only the hospital or only the office. But what if you extended that idea to focusing your practice on only one unit within the hospital rather than the whole building? Would that be a good idea and lead to the benefits described above, or would that be taking the idea of “focused practice” too far?
Before answering, I should describe the approaches some practices have taken to pursue the benefits of concentrating patients in one part of the hospital. I’ll refer to this idea as “unit-based hospitalists,” the term current SHM President Rusty Holman uses when talking about this idea.
Locate most hospitalist patients in one unit. This is the most common form of unit-based hospitalists. Most institutions find the closest they can get to unit-based hospitalists is to have all hospitalist admissions go to the same floor when that floor has a bed available and the patient doesn’t require placement elsewhere. In such cases, the hospitalist practice might have something like 50% of patients on that floor and 50% dispersed throughout the hospital (telemetry, ICU, surgery floor). So the whole hospitalist practice has a primary “home” within the hospital, while each hospitalist spends part of each day caring for patients elsewhere. This is not very difficult for most hospitals to implement—and many are because most hospitalist patients end up on the “general medical” floor. This lets the hospitalist spend more time on that unit than any other. She can get to know the staff on that floor better, which might lead to many benefits, including improved satisfaction and efficiency.
Locate individual hospitalists on different hospital units. A more pure, but uncommon, form of unit-based hospitalists involves changing the way hospitalists are placed through the institution rather than changing patient placement. Each hospitalist in the group is assigned to a different nursing unit—or perhaps more than one unit—and sees whichever hospitalist patients are placed there. This system has the advantage of the hospitalist working all or most of the day on the same nursing unit, which can foster excellent teamwork. Instead of the nurse having to figure out which hospitalist to page for a particular patient, he simply needs to know, “Who is our hospitalist today?” and can contact that doctor for issues on most patients. Additionally, because the hospitalist will spend nearly the whole day physically on that unit, paging can be reduced significantly.
Despite its advantages, basing an individual hospitalist on a particular unit of the hospital is uncommon because in its purest form it can lead to terrible hospitalist-patient continuity. And, it’s hard to be confident that the disruptions in continuity are worth the benefits of the unit-based system. For example, the practice may have a patient to admit in the ED but can’t know which hospitalist should see the patient until a room is assigned. The fifth-floor hospitalist might go admit the patient in the ED, only to have the patient end up on the third floor, in which case the third-floor hospitalist would take over the next day. And each time the patient transferred to a new unit, either because of medical needs such as telemetry or simply because the hospital is full and needs to move patients, he would get a new hospitalist.
In addition to problems with continuity for patients who occupy more than one unit during their stay, this system would mean individual hospitalist workloads might get far out of balance. One floor might be very busy, while another is slow or limited by nurse staff shortages, and the respective hospitalists would have a correspondingly out-of-balance workload. A group could decide to address these problems by, for example, having the fifth-floor hospitalist see patients in other parts of the hospital in an effort to provide better hospitalist-patient continuity and address out-of-balance patient loads. But if this happens with any regularity it would mean the group has essentially moved back to a non-unit-based system.
In nearly all hospitals it would be unnecessary and unreasonable to assign a hospitalist to each nursing unit because some units tend to have few hospitalist patients. Yet when patients end up in those units because of medical necessity or bed space needs, one of the hospitalists will have to leave his/her unit to see this patient. If this happens often enough, it begins to dilute or negate the benefit of basing a hospitalist in one or two units.
Although one of the potential benefits of the unit-based model is enhanced relationships and integration among hospitalists and other unit-based clinical staff, it would be difficult to ensure that the same one or two hospitalists always work in a particular unit, and would limit scheduling flexibility dramatically. For example, if Dr. Starsky and Dr. Hutch are the unit-based hospitalists for Unit A, what happens if Dr. Starsky and Dr. Hutch are both scheduled to be off for the same block of days? What happens if both are scheduled to work the same block of days? To obtain the benefits of enhanced relationships and better unit integration, the practice would need to ensure that this scheduling overlap rarely happens—and that’s hard to do.
Where is the sweet spot in grouping patients and hospitalists by nursing unit? There is a wide range of opinion about whether unit-based hospital medicine in any form is worth pursuing. Some hospitalists are convinced that grouping all of their patients on the same unit could decrease efficiency because the doctor is nearly always working within view of patients and families and may be regularly interrupted. I am convinced that assigning each hospitalist to a particular unit in the hospital yields the greatest benefits. But I also think most institutions will find that the complexity and costs of this system are simply too high to justify. In that case, the next best approach might be to locate most hospitalist patients on the same unit unless that unit is full or the patient must be placed elsewhere. There is a good chance this is happening in your hospital—even if it isn’t written in the policy manual. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Promote Proper CPT Coding
Code nearly all visits at the highest level” was the entire orientation I got to CPT coding when I first started practice as a hospitalist in the 1980s.
I couldn’t believe this advice, which came from another physician, was sound—and it isn’t. So I tried to learn a little more about the subject on my own. After a year or so of somewhat futile self-education in coding, I decided I could never learn the very confusing rules and chose to do nearly the opposite of the “code all visits high” strategy: I coded nearly all visits at very low levels.
While some hospitalists are experts at proper CPT coding, I think a lot (the majority?) feel uneasy and do what I tended to do years ago: They “downcode” many visits, believing this will provide a margin of safety against being audited and accused of “upcoding.” The problem with this approach is that it can cost your practice significant professional fee revenue. And according to the letter of the law, downcoding is just as illegal as upcoding. (Though I haven’t seen any newspaper headlines about Medicare creating teams of auditors to stamp out illegal downcoding.)
Strategies to Improve
If you’re like many hospitalists and feel uneasy about how accurately you’re choosing CPT codes, I have a few suggestions.
First, SHM has a new course on CPT coding designed specifically for hospitalists. The next meetings are Oct. 3 in San Francisco and April 3, 2008, in San Diego as a precourse to SHM’s Annual Meeting 2008. The previous versions of the course have received high praise.
There are also a number of strategies your hospitalist group can use to help ensure proper coding stays on each doctor’s mind. Some organizations have an internal coding expert who might regularly review each doctor’s coding and provide education to address problem areas. Whether you have such an internal expert or not, you should probably have an annual audit by an external certified coder—someone who has no financial connection to your institution.
In addition to external resources, I think every group should create a monthly or quarterly report that allows each doctor to see his or her own pattern of coding compared with that of everyone else in the group. This will be most valuable if everyone’s name remains visible to everyone else. It should then be easy for me to tell that I code discharges at the low level far more often than the group average. I should be able to see that my partner Jane codes half of initial consult visits at the highest level and I code most of them much lower.
It would be unusual that this information would lead to strife and dissent within the group. If it does, you probably have significant cultural and interpersonal problems within your group. It will usually lead to the doctors talking about their patterns of documenting and coding among themselves—which goes a long way to keep the issue on everyone’s mind.
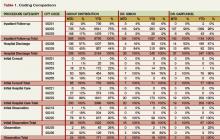
One format for such a report is on p. 61. CPT codes are grouped by category on the left side. The next set of columns is labeled “group distribution” and shows the month-to-date (MTD) and running 12-month (YTD) distribution of codes for all doctors in the group. Specific data for two doctors in the group is to the right of the group distribution. Note that there are more than 10 doctors in this hypothetical group, but I have shown only two of them because of space limitations.
When reviewing this table, Dr. Simon may get a little uncomfortable because she codes only 2% of follow-up visits at the highest level, but the group as a whole uses the highest code 17% of the time. And, she codes 88% of discharges at the high level, compared with 44% for the group as a whole. She is also out of step with her partners in highest initial consult and the middle initial observation codes. This information will probably make her receptive to peer-to-peer learning from her partners and may motivate her to review some of the coding rules.
Dr. Simon and Dr. Garfunkel are out of step with the group in how often they use the code for the middle level initial observation visit. This group needs to investigate whether these two doctors are coding these visits correctly, and everyone else is in error, or vice versa.
It is important to point out that the goal of the report isn’t to get each doctor to simply mirror the distribution of the group’s overall coding pattern. There might be cases in which the outlier doctor is coding correctly and everyone else is wrong. So the group average can’t be accepted as correct, and any significant discrepancies between one or two doctors and the group as a whole should be reviewed and discussed.
While a coding comparison table like this isn’t enough to ensure proper coding, it is a useful tool for highlighting the areas most in need of attention. I know of cases in which hospitalists who practiced together for several years had no idea their coding patterns were so dramatically different until they created a report like this. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Code nearly all visits at the highest level” was the entire orientation I got to CPT coding when I first started practice as a hospitalist in the 1980s.
I couldn’t believe this advice, which came from another physician, was sound—and it isn’t. So I tried to learn a little more about the subject on my own. After a year or so of somewhat futile self-education in coding, I decided I could never learn the very confusing rules and chose to do nearly the opposite of the “code all visits high” strategy: I coded nearly all visits at very low levels.
While some hospitalists are experts at proper CPT coding, I think a lot (the majority?) feel uneasy and do what I tended to do years ago: They “downcode” many visits, believing this will provide a margin of safety against being audited and accused of “upcoding.” The problem with this approach is that it can cost your practice significant professional fee revenue. And according to the letter of the law, downcoding is just as illegal as upcoding. (Though I haven’t seen any newspaper headlines about Medicare creating teams of auditors to stamp out illegal downcoding.)
Strategies to Improve
If you’re like many hospitalists and feel uneasy about how accurately you’re choosing CPT codes, I have a few suggestions.
First, SHM has a new course on CPT coding designed specifically for hospitalists. The next meetings are Oct. 3 in San Francisco and April 3, 2008, in San Diego as a precourse to SHM’s Annual Meeting 2008. The previous versions of the course have received high praise.
There are also a number of strategies your hospitalist group can use to help ensure proper coding stays on each doctor’s mind. Some organizations have an internal coding expert who might regularly review each doctor’s coding and provide education to address problem areas. Whether you have such an internal expert or not, you should probably have an annual audit by an external certified coder—someone who has no financial connection to your institution.
In addition to external resources, I think every group should create a monthly or quarterly report that allows each doctor to see his or her own pattern of coding compared with that of everyone else in the group. This will be most valuable if everyone’s name remains visible to everyone else. It should then be easy for me to tell that I code discharges at the low level far more often than the group average. I should be able to see that my partner Jane codes half of initial consult visits at the highest level and I code most of them much lower.
It would be unusual that this information would lead to strife and dissent within the group. If it does, you probably have significant cultural and interpersonal problems within your group. It will usually lead to the doctors talking about their patterns of documenting and coding among themselves—which goes a long way to keep the issue on everyone’s mind.
One format for such a report is on p. 61. CPT codes are grouped by category on the left side. The next set of columns is labeled “group distribution” and shows the month-to-date (MTD) and running 12-month (YTD) distribution of codes for all doctors in the group. Specific data for two doctors in the group is to the right of the group distribution. Note that there are more than 10 doctors in this hypothetical group, but I have shown only two of them because of space limitations.
When reviewing this table, Dr. Simon may get a little uncomfortable because she codes only 2% of follow-up visits at the highest level, but the group as a whole uses the highest code 17% of the time. And, she codes 88% of discharges at the high level, compared with 44% for the group as a whole. She is also out of step with her partners in highest initial consult and the middle initial observation codes. This information will probably make her receptive to peer-to-peer learning from her partners and may motivate her to review some of the coding rules.
Dr. Simon and Dr. Garfunkel are out of step with the group in how often they use the code for the middle level initial observation visit. This group needs to investigate whether these two doctors are coding these visits correctly, and everyone else is in error, or vice versa.
It is important to point out that the goal of the report isn’t to get each doctor to simply mirror the distribution of the group’s overall coding pattern. There might be cases in which the outlier doctor is coding correctly and everyone else is wrong. So the group average can’t be accepted as correct, and any significant discrepancies between one or two doctors and the group as a whole should be reviewed and discussed.
While a coding comparison table like this isn’t enough to ensure proper coding, it is a useful tool for highlighting the areas most in need of attention. I know of cases in which hospitalists who practiced together for several years had no idea their coding patterns were so dramatically different until they created a report like this. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Code nearly all visits at the highest level” was the entire orientation I got to CPT coding when I first started practice as a hospitalist in the 1980s.
I couldn’t believe this advice, which came from another physician, was sound—and it isn’t. So I tried to learn a little more about the subject on my own. After a year or so of somewhat futile self-education in coding, I decided I could never learn the very confusing rules and chose to do nearly the opposite of the “code all visits high” strategy: I coded nearly all visits at very low levels.
While some hospitalists are experts at proper CPT coding, I think a lot (the majority?) feel uneasy and do what I tended to do years ago: They “downcode” many visits, believing this will provide a margin of safety against being audited and accused of “upcoding.” The problem with this approach is that it can cost your practice significant professional fee revenue. And according to the letter of the law, downcoding is just as illegal as upcoding. (Though I haven’t seen any newspaper headlines about Medicare creating teams of auditors to stamp out illegal downcoding.)
Strategies to Improve
If you’re like many hospitalists and feel uneasy about how accurately you’re choosing CPT codes, I have a few suggestions.
First, SHM has a new course on CPT coding designed specifically for hospitalists. The next meetings are Oct. 3 in San Francisco and April 3, 2008, in San Diego as a precourse to SHM’s Annual Meeting 2008. The previous versions of the course have received high praise.
There are also a number of strategies your hospitalist group can use to help ensure proper coding stays on each doctor’s mind. Some organizations have an internal coding expert who might regularly review each doctor’s coding and provide education to address problem areas. Whether you have such an internal expert or not, you should probably have an annual audit by an external certified coder—someone who has no financial connection to your institution.
In addition to external resources, I think every group should create a monthly or quarterly report that allows each doctor to see his or her own pattern of coding compared with that of everyone else in the group. This will be most valuable if everyone’s name remains visible to everyone else. It should then be easy for me to tell that I code discharges at the low level far more often than the group average. I should be able to see that my partner Jane codes half of initial consult visits at the highest level and I code most of them much lower.
It would be unusual that this information would lead to strife and dissent within the group. If it does, you probably have significant cultural and interpersonal problems within your group. It will usually lead to the doctors talking about their patterns of documenting and coding among themselves—which goes a long way to keep the issue on everyone’s mind.
One format for such a report is on p. 61. CPT codes are grouped by category on the left side. The next set of columns is labeled “group distribution” and shows the month-to-date (MTD) and running 12-month (YTD) distribution of codes for all doctors in the group. Specific data for two doctors in the group is to the right of the group distribution. Note that there are more than 10 doctors in this hypothetical group, but I have shown only two of them because of space limitations.
When reviewing this table, Dr. Simon may get a little uncomfortable because she codes only 2% of follow-up visits at the highest level, but the group as a whole uses the highest code 17% of the time. And, she codes 88% of discharges at the high level, compared with 44% for the group as a whole. She is also out of step with her partners in highest initial consult and the middle initial observation codes. This information will probably make her receptive to peer-to-peer learning from her partners and may motivate her to review some of the coding rules.
Dr. Simon and Dr. Garfunkel are out of step with the group in how often they use the code for the middle level initial observation visit. This group needs to investigate whether these two doctors are coding these visits correctly, and everyone else is in error, or vice versa.
It is important to point out that the goal of the report isn’t to get each doctor to simply mirror the distribution of the group’s overall coding pattern. There might be cases in which the outlier doctor is coding correctly and everyone else is wrong. So the group average can’t be accepted as correct, and any significant discrepancies between one or two doctors and the group as a whole should be reviewed and discussed.
While a coding comparison table like this isn’t enough to ensure proper coding, it is a useful tool for highlighting the areas most in need of attention. I know of cases in which hospitalists who practiced together for several years had no idea their coding patterns were so dramatically different until they created a report like this. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Comp Close-Up
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
How hard do hospitalists work and how much are they paid? There are several sources of data to answer this question, and each has its strengths and weaknesses. Because these data influence contract negotiations and compliance with federal regulations, it is worth taking the time to understand the differences in each data set.
I’ll focus on the two most common sources of data: the biannual SHM survey of hospitalist productivity and compensation (officially titled “The Authoritative Source on the State of Hospital Medicine”), and the Medical Group Management Association’s (MGMA) annual “Physician Compensation and Production Survey.” There are many other surveys that report hospitalist data such as those by the American Medical Group Association (AMGA), Sullivan & Cotter, Hay Group, and others. Each July, Modern Healthcare magazine publishes the average compensation (but no other data) reported for hospitalists and other specialties by each of these organizations and several others (but not the SHM data). It should be easy to find a copy of Modern Healthcare in your hospital administration or library, or on the Internet.
The SHM and MGMA surveys are the most widely used sources of data for hospitalists, and some of their attributes are described in Table 1 (see below).
I should acknowledge my potential conflict of interest and potential for bias in comparing these surveys. This column is in an SHM publication. I’m very active in SHM, and I’m a past chairman and ongoing member of the Benchmarks Committee, which oversees the design and analysis of the SHM survey. And while I am familiar with and regularly review the MGMA survey, I have no other connection to that organization.
Much of the difference between the surveys is a result of the SHM survey being designed specifically for hospitalists in any type of practice setting (e.g., small hospitalist-only groups, as well as hospitalists with huge organizations like a university faculty group practice). In contrast, the MGMA survey is designed for all physician specialties, so a hospitalist answers the same questions as a traditional primary care doctor, plastic surgeon, and obstetrician.
MGMA data can be adversely affected by the inclusion of primary care office-based encounters. One of the principal ways the two surveys differ is how they address ambulatory visits. The MGMA survey reports inpatient and ambulatory visits separately, but “ambulatory” visits include any for a patient who is not a hospital inpatient. By this definition, hospitalists make ambulatory visits, most commonly to hospitalized patients who are on observation status, and also patients seen in an ED, skilled nursing facility, or pre-op clinic. Thus the MGMA survey doesn’t distinguish between ambulatory encounters a hospitalist would generate in the course of serving as a hospitalist, and those generated while that doctor might be serving in a non-hospitalist role such as office-based primary care or urgent care.
The SHM survey doesn’t include—and isn’t contaminated by—office-based primary care or urgent-care visits.
Of the 3,376 total encounters reported in the MGMA survey, 40% (1,351) are ambulatory encounters. Although the SHM survey does not distinguish between hospital and ambulatory encounters, my experience suggests few, if any, hospitalist practices make 40% of their total encounters with patients on observation status, or in an ED, SNF, or pre-op clinic. Thus, many of the ambulatory encounters reported by MGMA might have been office visits, not hospital-related visits.
Additionally, the median internal medicine hospitalist encounters (ambulatory and hospital combined) in the MGMA survey (3,376) is 42% higher than the median total encounters reported for internal medicine hospitalists in SHM’s survey (2,378). Yet the wRVUs reported in the MGMA survey (3,514) are only 8% higher than those reported in the SHM survey (3,256). Thus the calculated average wRVUs per encounter for the MGMA data is only 1.04, compared with 1.37 for the SHM data. An average of 1.04 wRVUs per encounter is very low for hospitalists, when almost all current procedural terminology (CPT) codes a hospitalist uses have a value of one or more wRVUs. Again, this suggests the MGMA data may be significantly influenced by the inclusion of office-based encounters, some of which have wRVUs of less than one. SHM has approached MGMA to discuss this data definition issue in their survey.
Why It Matters
You can use whichever data set best describes your situation. The MGMA has historically shown higher hospitalist salaries and higher workloads than the SHM data. But because the SHM data is the result of a survey customized for hospitalists and less likely than the MGMA data to be contaminated by non-hospital-related visits, the SHM data probably gives a more accurate picture.
Because the MGMA survey has been conducted for many years (far longer than the SHM survey) it has appropriately become one of the most authoritative sources of data on physician compensation for all specialties. Stark II regulations require hospitals to ensure they aren’t paying physicians above the fair market compensation (which could be seen as an inducement to refer patients to the hospital, among other concerns). And it specifically states that the MGMA survey is one of several approved sources of determining what fair market compensation is.
Even though the SHM data is most likely more representative and provides an important benchmark for hospitalists, the MGMA data has “pre-approved” status and thus is potentially safer to use for the specific purpose of determinations of fair market value.
With each iteration, the SHM survey will be adjusted to more specifically capture hospitalist activity; in many cases it is the best data for hospitalists to use in planning and benchmarking. But the MGMA data are still valuable and may be the most appropriate to refer to in contracts.
Note to readers: In May, SHM contacted MGMA regarding their concerns that MGMA survey data was not representative of hospitalists. MGMA responded with a willingness to discuss these issues with SHM. As this story goes to press, SHM and MGMA continue to have a dialogue about maximizing the accuracy of survey data. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
How to Hire and Use Clerical Staff
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
The Hospitalist-Patient Conundrum
Hospitalist-patient continuity is primarily a function of the number of consecutive days worked by a hospitalist, but the way new referrals are distributed can also affect continuity. This month, I will discuss both.
For my first few years as a hospitalist in the late 1980s and early 1990s, my one partner and I generally worked a schedule of 21 days on and seven days off. While I wouldn’t recommend that anyone try that today, it wasn’t as bad as you might think, because our patient volumes weren’t terribly high and, on about a third of the worked days, I was done shortly after lunch.
While working that schedule, I became aware of its benefit to hospitalist-patient continuity. I can remember many patients with hospital stays of more than two weeks whom I saw every day myself. As you might imagine, my partner and I talked periodically about working fewer than 21 days at a stretch and handing a service over to one another more frequently. But we were concerned that this would make us inefficient because more of our worked days would involve getting to know a new list of patients. In effect, we’d work more hours without an increase in income or patient volume.
While still working the 21-day schedule, I came to know another practice and was stunned that these doctors had taken essentially the opposite approach to scheduling. They worked 24-hour shifts on site and never worked more than one shift at a time. (If your shifts are 24-hours long, you probably can’t or shouldn’t work more than one at a time.) This schedule meant that a patient would see a different hospitalist each day. I couldn’t believe that either the patients or the hospitalists would think this was a reasonable thing to do, but the doctors were convinced it worked well. Later I learned that this group had been started by an emergency medicine practice, and it seems they had made the mistake of inserting an emergency department (ED) physician schedule into a hospitalist practice—and 24-hour shifts for ED doctors were more common then than now.
So, early in my career, the first two schedules I became acquainted with sat on opposite ends of a continuum that has since been filled in by many other options. Both the practice I was part of and the 24-hour-shift practice abandoned their original schedules within a few years and moved on to other alternatives. In fact, I have since worked nearly every schedule you can imagine, including the seven-on/seven-off schedule, which I think is a suboptimal choice for most groups. (See August 2006 “Career Management,” p. 9.) With each variation in my work schedule, I’ve thought a lot about its effect on continuity.
While there isn’t a great deal of research to prove it, improved continuity is probably associated with improvements in things like:
- Quality care and safety;
- Patient satisfaction (and probably hospitalist satisfaction also);
- Hospital resource utilization; and
- Hospitalist efficiency.
When hospitalists design a schedule, I recommend that the doctors think first about what will allow them a sustainable lifestyle while ensuring the necessary coverage—for some practices, this means keeping a doctor in the hospital around the clock. Ideally, they will come up with several options that satisfy these two metrics. In many cases, the option that results in the best continuity is the one they should choose.
While the number of consecutive days of work is the most important variable in determining continuity, the way a group distributes new referrals can also have an effect. If a hospitalist doesn’t take on any new referrals on the day before starting a series of days off, there will be fewer patients to hand over to the doctor who takes over the next day. If every member of the practice is exempted from taking on new patients on the day before rotating off, then fewer patients will have a new hospitalist, which means continuity is better. Another way to think of this is that new referrals are “frontloaded” into the earlier days a hospitalist works in each series, and no new patients are assigned on the last day—or maybe more—of a hospitalist’s consecutive days of work.
In my experience, most groups try to distribute patients equally to each doctor each day. This means that a doctor who will be off starting tomorrow takes the standard portion of new referrals to the practice today. The fact that all of those patients will be turned over to a new hospitalist tomorrow, however, adversely affects continuity.
Note that exempting a group member from taking on new patients on the last day of a rotation means that the doctors can’t all rotate on and off on the same day. For example, if a group has four doctors working each day, and all rotate off on the same day—a common practice—then of course it is impossible to exempt all the doctors from new referrals on the day before going off. Instead, it will work best if only one doctor rotates on or off at a time. That leaves all the other doctors available to accept new referrals, while exempting the one about to rotate off.
This approach has benefits that go beyond improving continuity. It means a hospitalist’s workload the day before rotating off will be lighter than on other days. This provides extra time to “tee the patient up” for the next hospitalist—maybe write a more detailed note or dictate a discharge summary in anticipation of the patient leaving the next day—and/or it means a shorter day of work, assuming the doctors can leave the hospital when their work is done and aren’t required to stay around until the end of a pre-defined shift. This shorter day can mean an opportunity to do things like scheduling a flight to vacation late on the last day of work rather than the next morning, which might mean an extra day out of town.
And if a doctor isn’t assigned any new patients on the day prior to rotating off, there will be fewer patients to get to know for the doctor coming in the next day. The first day back on service will be less stressful and, arguably, more efficient.
A principle benefit of having all hospitalists switch on the same day is that the system quickly becomes transparent to the hospital staff. They learn that every Monday—or whatever day is decided upon—all of the hospitalists are getting to know patients for the first time and will probably round much more slowly. Many important processes, such as discharges, may be delayed until later in the day. If only one hospitalist switches at a time, hospital staff will have a hard time keeping up. Any inefficiencies caused by the switch will be spread over many days, however, and this may make it easier to handle. And if patients are teed up better for the new hospitalist and there are fewer patients on the list, the inefficiency that is caused by a new doctor getting to know the patients can be offset by the smaller number of patients. That means, for example, that discharges are much less likely to be delayed because of the smaller patient load on the doctor’s first day on service.
Up to this point I’ve been discussing continuity during a single admission. What about continuity from one admission to the next? Nearly all groups assign patients based on when they are admitted, and the hospitalist who cared for the patient during a prior admission may have little influence on which hospitalist admits them this time. If a patient is readmitted within a week or two, and the previous attending hospitalist is working, some groups will try to pair them once again through a bounce-back system.
It’s worth thinking about whether your group could make an effort to always have the same hospitalist care for a patient unless that physician is off—even if the admissions are months apart. This system would mean that on first admission to the practice a patient would be assigned to the hospitalist who is up next. In this way, each hospitalist in the group would develop his or her own panel of patients. This would be particularly valuable for patients who are admitted frequently; however, it would be difficult for a doctor to control how labor-intensive his patient panel might become. One person might have the bad luck to collect far more medically and socially complex patients than others in the group, and workloads might become unbalanced, making the whole group less efficient. I’m hopeful that a group will come up with a way to overcome these problems and create a workable system of good continuity from one admission to the next, but, as far as I’m aware, no group is doing this now. If you have a workable system, please let me know.
One group I worked with years ago addressed continuity from one admission to the next by using a system that matched each hospitalist with a panel of referring doctors. For example, the same hospitalist would always admit the patients “belonging to” a cadre of primary care physicians (PCPs), and another hospitalist in the group would always admit patients from another set of PCPs. The patient would see the same hospitalist each admission, and the hospitalist could develop a close working relationship with the panel of PCPs. The hospitalist and the PCP became familiar with each other’s practice styles, schedules, and days off, and memorized one another’s phone and fax numbers, the names of office and support staff, and so on, making for a very smooth working relationship that could benefit patient care. If the assigned hospitalist was off when a particular PCP’s patient needed admission, then a partner would provide interim care and turn the patient over when that hospitalist returned.
As you can imagine, this can be a difficult system to implement because there are many days on which a patient might be hospitalized when the assigned hospitalist is not around. Additionally, it is nearly impossible to divide PCPs and their patients equitably so that each hospitalist has a reasonable workload and patient complexity. I can imagine this group meeting periodically to match hospitalists and PCPs in a fashion similar to a fantasy football draft: “I’ll take PCP Smith and Williams from you, if you take PCP Wilson off my hands.”
I’m interested in hearing any additional ideas groups have developed to facilitate good continuity. The number of consecutive days worked by each hospitalist and the way new patients are assigned are significant ways to influence continuity, but there may be others that we should all keep in mind. And remember, maximizing continuity is not only good for patients; it enables the hospitalist practice to function more efficiently because it minimizes the number of new patients each hospitalist will have to get to know. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Hospitalist-patient continuity is primarily a function of the number of consecutive days worked by a hospitalist, but the way new referrals are distributed can also affect continuity. This month, I will discuss both.
For my first few years as a hospitalist in the late 1980s and early 1990s, my one partner and I generally worked a schedule of 21 days on and seven days off. While I wouldn’t recommend that anyone try that today, it wasn’t as bad as you might think, because our patient volumes weren’t terribly high and, on about a third of the worked days, I was done shortly after lunch.
While working that schedule, I became aware of its benefit to hospitalist-patient continuity. I can remember many patients with hospital stays of more than two weeks whom I saw every day myself. As you might imagine, my partner and I talked periodically about working fewer than 21 days at a stretch and handing a service over to one another more frequently. But we were concerned that this would make us inefficient because more of our worked days would involve getting to know a new list of patients. In effect, we’d work more hours without an increase in income or patient volume.
While still working the 21-day schedule, I came to know another practice and was stunned that these doctors had taken essentially the opposite approach to scheduling. They worked 24-hour shifts on site and never worked more than one shift at a time. (If your shifts are 24-hours long, you probably can’t or shouldn’t work more than one at a time.) This schedule meant that a patient would see a different hospitalist each day. I couldn’t believe that either the patients or the hospitalists would think this was a reasonable thing to do, but the doctors were convinced it worked well. Later I learned that this group had been started by an emergency medicine practice, and it seems they had made the mistake of inserting an emergency department (ED) physician schedule into a hospitalist practice—and 24-hour shifts for ED doctors were more common then than now.
So, early in my career, the first two schedules I became acquainted with sat on opposite ends of a continuum that has since been filled in by many other options. Both the practice I was part of and the 24-hour-shift practice abandoned their original schedules within a few years and moved on to other alternatives. In fact, I have since worked nearly every schedule you can imagine, including the seven-on/seven-off schedule, which I think is a suboptimal choice for most groups. (See August 2006 “Career Management,” p. 9.) With each variation in my work schedule, I’ve thought a lot about its effect on continuity.
While there isn’t a great deal of research to prove it, improved continuity is probably associated with improvements in things like:
- Quality care and safety;
- Patient satisfaction (and probably hospitalist satisfaction also);
- Hospital resource utilization; and
- Hospitalist efficiency.
When hospitalists design a schedule, I recommend that the doctors think first about what will allow them a sustainable lifestyle while ensuring the necessary coverage—for some practices, this means keeping a doctor in the hospital around the clock. Ideally, they will come up with several options that satisfy these two metrics. In many cases, the option that results in the best continuity is the one they should choose.
While the number of consecutive days of work is the most important variable in determining continuity, the way a group distributes new referrals can also have an effect. If a hospitalist doesn’t take on any new referrals on the day before starting a series of days off, there will be fewer patients to hand over to the doctor who takes over the next day. If every member of the practice is exempted from taking on new patients on the day before rotating off, then fewer patients will have a new hospitalist, which means continuity is better. Another way to think of this is that new referrals are “frontloaded” into the earlier days a hospitalist works in each series, and no new patients are assigned on the last day—or maybe more—of a hospitalist’s consecutive days of work.
In my experience, most groups try to distribute patients equally to each doctor each day. This means that a doctor who will be off starting tomorrow takes the standard portion of new referrals to the practice today. The fact that all of those patients will be turned over to a new hospitalist tomorrow, however, adversely affects continuity.
Note that exempting a group member from taking on new patients on the last day of a rotation means that the doctors can’t all rotate on and off on the same day. For example, if a group has four doctors working each day, and all rotate off on the same day—a common practice—then of course it is impossible to exempt all the doctors from new referrals on the day before going off. Instead, it will work best if only one doctor rotates on or off at a time. That leaves all the other doctors available to accept new referrals, while exempting the one about to rotate off.
This approach has benefits that go beyond improving continuity. It means a hospitalist’s workload the day before rotating off will be lighter than on other days. This provides extra time to “tee the patient up” for the next hospitalist—maybe write a more detailed note or dictate a discharge summary in anticipation of the patient leaving the next day—and/or it means a shorter day of work, assuming the doctors can leave the hospital when their work is done and aren’t required to stay around until the end of a pre-defined shift. This shorter day can mean an opportunity to do things like scheduling a flight to vacation late on the last day of work rather than the next morning, which might mean an extra day out of town.
And if a doctor isn’t assigned any new patients on the day prior to rotating off, there will be fewer patients to get to know for the doctor coming in the next day. The first day back on service will be less stressful and, arguably, more efficient.
A principle benefit of having all hospitalists switch on the same day is that the system quickly becomes transparent to the hospital staff. They learn that every Monday—or whatever day is decided upon—all of the hospitalists are getting to know patients for the first time and will probably round much more slowly. Many important processes, such as discharges, may be delayed until later in the day. If only one hospitalist switches at a time, hospital staff will have a hard time keeping up. Any inefficiencies caused by the switch will be spread over many days, however, and this may make it easier to handle. And if patients are teed up better for the new hospitalist and there are fewer patients on the list, the inefficiency that is caused by a new doctor getting to know the patients can be offset by the smaller number of patients. That means, for example, that discharges are much less likely to be delayed because of the smaller patient load on the doctor’s first day on service.
Up to this point I’ve been discussing continuity during a single admission. What about continuity from one admission to the next? Nearly all groups assign patients based on when they are admitted, and the hospitalist who cared for the patient during a prior admission may have little influence on which hospitalist admits them this time. If a patient is readmitted within a week or two, and the previous attending hospitalist is working, some groups will try to pair them once again through a bounce-back system.
It’s worth thinking about whether your group could make an effort to always have the same hospitalist care for a patient unless that physician is off—even if the admissions are months apart. This system would mean that on first admission to the practice a patient would be assigned to the hospitalist who is up next. In this way, each hospitalist in the group would develop his or her own panel of patients. This would be particularly valuable for patients who are admitted frequently; however, it would be difficult for a doctor to control how labor-intensive his patient panel might become. One person might have the bad luck to collect far more medically and socially complex patients than others in the group, and workloads might become unbalanced, making the whole group less efficient. I’m hopeful that a group will come up with a way to overcome these problems and create a workable system of good continuity from one admission to the next, but, as far as I’m aware, no group is doing this now. If you have a workable system, please let me know.
One group I worked with years ago addressed continuity from one admission to the next by using a system that matched each hospitalist with a panel of referring doctors. For example, the same hospitalist would always admit the patients “belonging to” a cadre of primary care physicians (PCPs), and another hospitalist in the group would always admit patients from another set of PCPs. The patient would see the same hospitalist each admission, and the hospitalist could develop a close working relationship with the panel of PCPs. The hospitalist and the PCP became familiar with each other’s practice styles, schedules, and days off, and memorized one another’s phone and fax numbers, the names of office and support staff, and so on, making for a very smooth working relationship that could benefit patient care. If the assigned hospitalist was off when a particular PCP’s patient needed admission, then a partner would provide interim care and turn the patient over when that hospitalist returned.
As you can imagine, this can be a difficult system to implement because there are many days on which a patient might be hospitalized when the assigned hospitalist is not around. Additionally, it is nearly impossible to divide PCPs and their patients equitably so that each hospitalist has a reasonable workload and patient complexity. I can imagine this group meeting periodically to match hospitalists and PCPs in a fashion similar to a fantasy football draft: “I’ll take PCP Smith and Williams from you, if you take PCP Wilson off my hands.”
I’m interested in hearing any additional ideas groups have developed to facilitate good continuity. The number of consecutive days worked by each hospitalist and the way new patients are assigned are significant ways to influence continuity, but there may be others that we should all keep in mind. And remember, maximizing continuity is not only good for patients; it enables the hospitalist practice to function more efficiently because it minimizes the number of new patients each hospitalist will have to get to know. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Hospitalist-patient continuity is primarily a function of the number of consecutive days worked by a hospitalist, but the way new referrals are distributed can also affect continuity. This month, I will discuss both.
For my first few years as a hospitalist in the late 1980s and early 1990s, my one partner and I generally worked a schedule of 21 days on and seven days off. While I wouldn’t recommend that anyone try that today, it wasn’t as bad as you might think, because our patient volumes weren’t terribly high and, on about a third of the worked days, I was done shortly after lunch.
While working that schedule, I became aware of its benefit to hospitalist-patient continuity. I can remember many patients with hospital stays of more than two weeks whom I saw every day myself. As you might imagine, my partner and I talked periodically about working fewer than 21 days at a stretch and handing a service over to one another more frequently. But we were concerned that this would make us inefficient because more of our worked days would involve getting to know a new list of patients. In effect, we’d work more hours without an increase in income or patient volume.
While still working the 21-day schedule, I came to know another practice and was stunned that these doctors had taken essentially the opposite approach to scheduling. They worked 24-hour shifts on site and never worked more than one shift at a time. (If your shifts are 24-hours long, you probably can’t or shouldn’t work more than one at a time.) This schedule meant that a patient would see a different hospitalist each day. I couldn’t believe that either the patients or the hospitalists would think this was a reasonable thing to do, but the doctors were convinced it worked well. Later I learned that this group had been started by an emergency medicine practice, and it seems they had made the mistake of inserting an emergency department (ED) physician schedule into a hospitalist practice—and 24-hour shifts for ED doctors were more common then than now.
So, early in my career, the first two schedules I became acquainted with sat on opposite ends of a continuum that has since been filled in by many other options. Both the practice I was part of and the 24-hour-shift practice abandoned their original schedules within a few years and moved on to other alternatives. In fact, I have since worked nearly every schedule you can imagine, including the seven-on/seven-off schedule, which I think is a suboptimal choice for most groups. (See August 2006 “Career Management,” p. 9.) With each variation in my work schedule, I’ve thought a lot about its effect on continuity.
While there isn’t a great deal of research to prove it, improved continuity is probably associated with improvements in things like:
- Quality care and safety;
- Patient satisfaction (and probably hospitalist satisfaction also);
- Hospital resource utilization; and
- Hospitalist efficiency.
When hospitalists design a schedule, I recommend that the doctors think first about what will allow them a sustainable lifestyle while ensuring the necessary coverage—for some practices, this means keeping a doctor in the hospital around the clock. Ideally, they will come up with several options that satisfy these two metrics. In many cases, the option that results in the best continuity is the one they should choose.
While the number of consecutive days of work is the most important variable in determining continuity, the way a group distributes new referrals can also have an effect. If a hospitalist doesn’t take on any new referrals on the day before starting a series of days off, there will be fewer patients to hand over to the doctor who takes over the next day. If every member of the practice is exempted from taking on new patients on the day before rotating off, then fewer patients will have a new hospitalist, which means continuity is better. Another way to think of this is that new referrals are “frontloaded” into the earlier days a hospitalist works in each series, and no new patients are assigned on the last day—or maybe more—of a hospitalist’s consecutive days of work.
In my experience, most groups try to distribute patients equally to each doctor each day. This means that a doctor who will be off starting tomorrow takes the standard portion of new referrals to the practice today. The fact that all of those patients will be turned over to a new hospitalist tomorrow, however, adversely affects continuity.
Note that exempting a group member from taking on new patients on the last day of a rotation means that the doctors can’t all rotate on and off on the same day. For example, if a group has four doctors working each day, and all rotate off on the same day—a common practice—then of course it is impossible to exempt all the doctors from new referrals on the day before going off. Instead, it will work best if only one doctor rotates on or off at a time. That leaves all the other doctors available to accept new referrals, while exempting the one about to rotate off.
This approach has benefits that go beyond improving continuity. It means a hospitalist’s workload the day before rotating off will be lighter than on other days. This provides extra time to “tee the patient up” for the next hospitalist—maybe write a more detailed note or dictate a discharge summary in anticipation of the patient leaving the next day—and/or it means a shorter day of work, assuming the doctors can leave the hospital when their work is done and aren’t required to stay around until the end of a pre-defined shift. This shorter day can mean an opportunity to do things like scheduling a flight to vacation late on the last day of work rather than the next morning, which might mean an extra day out of town.
And if a doctor isn’t assigned any new patients on the day prior to rotating off, there will be fewer patients to get to know for the doctor coming in the next day. The first day back on service will be less stressful and, arguably, more efficient.
A principle benefit of having all hospitalists switch on the same day is that the system quickly becomes transparent to the hospital staff. They learn that every Monday—or whatever day is decided upon—all of the hospitalists are getting to know patients for the first time and will probably round much more slowly. Many important processes, such as discharges, may be delayed until later in the day. If only one hospitalist switches at a time, hospital staff will have a hard time keeping up. Any inefficiencies caused by the switch will be spread over many days, however, and this may make it easier to handle. And if patients are teed up better for the new hospitalist and there are fewer patients on the list, the inefficiency that is caused by a new doctor getting to know the patients can be offset by the smaller number of patients. That means, for example, that discharges are much less likely to be delayed because of the smaller patient load on the doctor’s first day on service.
Up to this point I’ve been discussing continuity during a single admission. What about continuity from one admission to the next? Nearly all groups assign patients based on when they are admitted, and the hospitalist who cared for the patient during a prior admission may have little influence on which hospitalist admits them this time. If a patient is readmitted within a week or two, and the previous attending hospitalist is working, some groups will try to pair them once again through a bounce-back system.
It’s worth thinking about whether your group could make an effort to always have the same hospitalist care for a patient unless that physician is off—even if the admissions are months apart. This system would mean that on first admission to the practice a patient would be assigned to the hospitalist who is up next. In this way, each hospitalist in the group would develop his or her own panel of patients. This would be particularly valuable for patients who are admitted frequently; however, it would be difficult for a doctor to control how labor-intensive his patient panel might become. One person might have the bad luck to collect far more medically and socially complex patients than others in the group, and workloads might become unbalanced, making the whole group less efficient. I’m hopeful that a group will come up with a way to overcome these problems and create a workable system of good continuity from one admission to the next, but, as far as I’m aware, no group is doing this now. If you have a workable system, please let me know.
One group I worked with years ago addressed continuity from one admission to the next by using a system that matched each hospitalist with a panel of referring doctors. For example, the same hospitalist would always admit the patients “belonging to” a cadre of primary care physicians (PCPs), and another hospitalist in the group would always admit patients from another set of PCPs. The patient would see the same hospitalist each admission, and the hospitalist could develop a close working relationship with the panel of PCPs. The hospitalist and the PCP became familiar with each other’s practice styles, schedules, and days off, and memorized one another’s phone and fax numbers, the names of office and support staff, and so on, making for a very smooth working relationship that could benefit patient care. If the assigned hospitalist was off when a particular PCP’s patient needed admission, then a partner would provide interim care and turn the patient over when that hospitalist returned.
As you can imagine, this can be a difficult system to implement because there are many days on which a patient might be hospitalized when the assigned hospitalist is not around. Additionally, it is nearly impossible to divide PCPs and their patients equitably so that each hospitalist has a reasonable workload and patient complexity. I can imagine this group meeting periodically to match hospitalists and PCPs in a fashion similar to a fantasy football draft: “I’ll take PCP Smith and Williams from you, if you take PCP Wilson off my hands.”
I’m interested in hearing any additional ideas groups have developed to facilitate good continuity. The number of consecutive days worked by each hospitalist and the way new patients are assigned are significant ways to influence continuity, but there may be others that we should all keep in mind. And remember, maximizing continuity is not only good for patients; it enables the hospitalist practice to function more efficiently because it minimizes the number of new patients each hospitalist will have to get to know. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Production-Based Compensation for Hospitalists Overlooked Too Often?
Should hospitalists, or doctors in general, be compensated based on their production? This question has received increased attention in the last few years. A major criticism of production-based compensation is that it is essentially a system that pays doctors for doing more, not for doing better. There is a growing interest in shifting at least some of physician (and hospital) compensation to a system based on the quality of care delivered.
At this point it isn’t entirely clear how all of this will play out in the coming years. What is clear is that for the time being the financial health of our practices is very dependent on our production (as well as other factors such as financial support from a hospital). So until Medicare and other payers change their system of physician reimbursement, I think it can be a good idea in many practices for at least some of a hospitalist’s income to be based on production because that helps connect him/her to the economic health of the practice.
In my May 2006 column (p. 50) I suggested that you consider production-based compensation because it can allow you and your partners to take more control of decisions about how hard you want to work and when you want to add additional doctors to your group. Most production-based compensation formulas allow doctors in the same group to work different amounts, such as working a different number of days on the schedule, and carrying different patient loads. In contrast, groups in which the hospitalists have a fixed salary (or one with a very small production-based component) usually require the doctors to work the same number of days on the schedule, and try to ensure all doctors have similar daily patient load.
When I discuss this idea with hospitalists around the country they often express concern that it would be too risky to go on a production-based salary system. They say things like, “I can’t go on production because I can’t control how many patients are referred to our practice.”
While it’s true that we have little control over patient volume from one day to the next, we have significant control over volume for any lengthy interval such as a year. If you provide good service to referring doctors and usually accept referrals graciously you will have a much higher volume than if you regularly resist referrals.
And I’ll bet that the majority of the other doctors at your hospital can’t precisely control their patient volume, but their compensation is based entirely on individual production. This is true of many emergency department and radiology practices, and some medical subspecialty groups. Why should hospitalist practice be different?
Another misconception about production-based compensation is that it is synonymous with foregoing any financial support from your hospital or other sponsoring institution. It isn’t. You can still pay individual doctors on productivity and include financial support from the hospital. For example, if the doctors are paid $55 for every wRVU generated, then $40 of that might come from professional fee collections, and $15 from the hospital (employer).
Others fear that a salary based on production will cause doctors to work at unreasonably high workloads, leading to poor patient care or patient satisfaction, or less efficient use of hospital resources (e.g., keep patients in the hospital longer). This is a potential risk, but not a common problem in my experience. There can also be concern that compensation based on productivity will cause the doctors within a group to compete with one another for patients (and income), leading to stress within the group. This is an uncommon problem, and—if it occurs within your group—it probably means that there are too many doctors in your practice (or that you should market the practice to attract more patients) rather than proving that productivity-based compensation is a bad idea.
But an explanation that clarifies objections to productivity-based compensation certainly isn’t enough of a reason to support it. You need to be convinced of some of its benefits. Hospitalists who aren’t used to being paid based in part or in whole on production tend to see it as a very stressful—or even oppressive—way to be paid. But I hope to convince you it is actually liberating.
In the absence of a production component, many groups try hard to ensure that every doctor works the same amount. For example, a group that pays a fixed annual salary to all doctors typically encourages or insists that each doctor must work almost the same amount. But when paid on production, each doctor in the group can, within reasonable boundaries, decide how much he or she wants to work. Of course all of the group’s work must be taken care of, but in nearly every group some doctors are probably willing to work a little more and others a little less than the average workload for the group.
Nearly 15 years ago, before I married and had children, I got hooked on the idea of learning to fly airplanes. Wow, did I enjoy it. But it is pretty time consuming to get a pilot’s license, to say nothing of the expense. There were a number of days that I was to be the admitting doctor for our practice, but great weather and an available plane and instructor would lure me away. On a number of occasions at 4 or 5 p.m. I called my partner who had gone home for the day and said, “Chuck, would you be willing to cover admissions so I can go flying?” He usually said “sure,” at which point I’d tell him that there were already two patients waiting in the ED.
This system made both of us happy. After nine months I was a licensed pilot and for that year my partner had a much higher income than I did. We both got what we wanted, and paying ourselves on production is what made this possible. If we were in a group with a fixed salary I can’t imagine he would have been willing to help me out so often (if ever), and I would have been limited to taking flying lessons only on my days off. Or I would have needed to pay my partner back by making up the evenings he covered for me.
My point in telling this story is that so many people think of paying hospitalists based entirely, or in part, on production is just a way to get them to maintain unreasonably high work loads. But I think it simply liberates the doctor to decide for himself what the right workload is, while owning the economic consequences of that choice. It allowed me the opportunity to work less.
A few hospitalists paid on production might choose badly and choose to work at an unreasonable (or unsafe) pace, but nearly all will make reasonable decisions. And members of a group can periodically adjust their workload up or down according to their need at the time; there is no requirement to work at the same load year after year. In fact, my partners and I in Florida didn’t even keep track of precisely how often each of us was on call over the year because there wasn’t any reason it needed to be the same for each person. (We did make some effort to distribute call evenly, but didn’t worry when it never worked out just right because each doctor could take more or less call and see a corresponding change in income).
I realize that there is no perfect compensation system, and one based on production can have shortcomings. But I think too many hospitalists assume the only reasonable system is one such as a fixed annual salary, or an hourly rate, or some method that intentionally avoids paying for productivity. You should think about how liberating productivity compensation can be. Basing a significant portion (say 40% or more—or even 100%) on productivity might be a good idea for you.
And there is nothing about productivity-based compensation that interferes with also providing financial reward for good quality of care. I’m a fan of both. If payers increasingly use quality of care as the basis for physician reimbursement in the future, individual physician compensation formulas should be based more on quality than production. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalists, or doctors in general, be compensated based on their production? This question has received increased attention in the last few years. A major criticism of production-based compensation is that it is essentially a system that pays doctors for doing more, not for doing better. There is a growing interest in shifting at least some of physician (and hospital) compensation to a system based on the quality of care delivered.
At this point it isn’t entirely clear how all of this will play out in the coming years. What is clear is that for the time being the financial health of our practices is very dependent on our production (as well as other factors such as financial support from a hospital). So until Medicare and other payers change their system of physician reimbursement, I think it can be a good idea in many practices for at least some of a hospitalist’s income to be based on production because that helps connect him/her to the economic health of the practice.
In my May 2006 column (p. 50) I suggested that you consider production-based compensation because it can allow you and your partners to take more control of decisions about how hard you want to work and when you want to add additional doctors to your group. Most production-based compensation formulas allow doctors in the same group to work different amounts, such as working a different number of days on the schedule, and carrying different patient loads. In contrast, groups in which the hospitalists have a fixed salary (or one with a very small production-based component) usually require the doctors to work the same number of days on the schedule, and try to ensure all doctors have similar daily patient load.
When I discuss this idea with hospitalists around the country they often express concern that it would be too risky to go on a production-based salary system. They say things like, “I can’t go on production because I can’t control how many patients are referred to our practice.”
While it’s true that we have little control over patient volume from one day to the next, we have significant control over volume for any lengthy interval such as a year. If you provide good service to referring doctors and usually accept referrals graciously you will have a much higher volume than if you regularly resist referrals.
And I’ll bet that the majority of the other doctors at your hospital can’t precisely control their patient volume, but their compensation is based entirely on individual production. This is true of many emergency department and radiology practices, and some medical subspecialty groups. Why should hospitalist practice be different?
Another misconception about production-based compensation is that it is synonymous with foregoing any financial support from your hospital or other sponsoring institution. It isn’t. You can still pay individual doctors on productivity and include financial support from the hospital. For example, if the doctors are paid $55 for every wRVU generated, then $40 of that might come from professional fee collections, and $15 from the hospital (employer).
Others fear that a salary based on production will cause doctors to work at unreasonably high workloads, leading to poor patient care or patient satisfaction, or less efficient use of hospital resources (e.g., keep patients in the hospital longer). This is a potential risk, but not a common problem in my experience. There can also be concern that compensation based on productivity will cause the doctors within a group to compete with one another for patients (and income), leading to stress within the group. This is an uncommon problem, and—if it occurs within your group—it probably means that there are too many doctors in your practice (or that you should market the practice to attract more patients) rather than proving that productivity-based compensation is a bad idea.
But an explanation that clarifies objections to productivity-based compensation certainly isn’t enough of a reason to support it. You need to be convinced of some of its benefits. Hospitalists who aren’t used to being paid based in part or in whole on production tend to see it as a very stressful—or even oppressive—way to be paid. But I hope to convince you it is actually liberating.
In the absence of a production component, many groups try hard to ensure that every doctor works the same amount. For example, a group that pays a fixed annual salary to all doctors typically encourages or insists that each doctor must work almost the same amount. But when paid on production, each doctor in the group can, within reasonable boundaries, decide how much he or she wants to work. Of course all of the group’s work must be taken care of, but in nearly every group some doctors are probably willing to work a little more and others a little less than the average workload for the group.
Nearly 15 years ago, before I married and had children, I got hooked on the idea of learning to fly airplanes. Wow, did I enjoy it. But it is pretty time consuming to get a pilot’s license, to say nothing of the expense. There were a number of days that I was to be the admitting doctor for our practice, but great weather and an available plane and instructor would lure me away. On a number of occasions at 4 or 5 p.m. I called my partner who had gone home for the day and said, “Chuck, would you be willing to cover admissions so I can go flying?” He usually said “sure,” at which point I’d tell him that there were already two patients waiting in the ED.
This system made both of us happy. After nine months I was a licensed pilot and for that year my partner had a much higher income than I did. We both got what we wanted, and paying ourselves on production is what made this possible. If we were in a group with a fixed salary I can’t imagine he would have been willing to help me out so often (if ever), and I would have been limited to taking flying lessons only on my days off. Or I would have needed to pay my partner back by making up the evenings he covered for me.
My point in telling this story is that so many people think of paying hospitalists based entirely, or in part, on production is just a way to get them to maintain unreasonably high work loads. But I think it simply liberates the doctor to decide for himself what the right workload is, while owning the economic consequences of that choice. It allowed me the opportunity to work less.
A few hospitalists paid on production might choose badly and choose to work at an unreasonable (or unsafe) pace, but nearly all will make reasonable decisions. And members of a group can periodically adjust their workload up or down according to their need at the time; there is no requirement to work at the same load year after year. In fact, my partners and I in Florida didn’t even keep track of precisely how often each of us was on call over the year because there wasn’t any reason it needed to be the same for each person. (We did make some effort to distribute call evenly, but didn’t worry when it never worked out just right because each doctor could take more or less call and see a corresponding change in income).
I realize that there is no perfect compensation system, and one based on production can have shortcomings. But I think too many hospitalists assume the only reasonable system is one such as a fixed annual salary, or an hourly rate, or some method that intentionally avoids paying for productivity. You should think about how liberating productivity compensation can be. Basing a significant portion (say 40% or more—or even 100%) on productivity might be a good idea for you.
And there is nothing about productivity-based compensation that interferes with also providing financial reward for good quality of care. I’m a fan of both. If payers increasingly use quality of care as the basis for physician reimbursement in the future, individual physician compensation formulas should be based more on quality than production. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Should hospitalists, or doctors in general, be compensated based on their production? This question has received increased attention in the last few years. A major criticism of production-based compensation is that it is essentially a system that pays doctors for doing more, not for doing better. There is a growing interest in shifting at least some of physician (and hospital) compensation to a system based on the quality of care delivered.
At this point it isn’t entirely clear how all of this will play out in the coming years. What is clear is that for the time being the financial health of our practices is very dependent on our production (as well as other factors such as financial support from a hospital). So until Medicare and other payers change their system of physician reimbursement, I think it can be a good idea in many practices for at least some of a hospitalist’s income to be based on production because that helps connect him/her to the economic health of the practice.
In my May 2006 column (p. 50) I suggested that you consider production-based compensation because it can allow you and your partners to take more control of decisions about how hard you want to work and when you want to add additional doctors to your group. Most production-based compensation formulas allow doctors in the same group to work different amounts, such as working a different number of days on the schedule, and carrying different patient loads. In contrast, groups in which the hospitalists have a fixed salary (or one with a very small production-based component) usually require the doctors to work the same number of days on the schedule, and try to ensure all doctors have similar daily patient load.
When I discuss this idea with hospitalists around the country they often express concern that it would be too risky to go on a production-based salary system. They say things like, “I can’t go on production because I can’t control how many patients are referred to our practice.”
While it’s true that we have little control over patient volume from one day to the next, we have significant control over volume for any lengthy interval such as a year. If you provide good service to referring doctors and usually accept referrals graciously you will have a much higher volume than if you regularly resist referrals.
And I’ll bet that the majority of the other doctors at your hospital can’t precisely control their patient volume, but their compensation is based entirely on individual production. This is true of many emergency department and radiology practices, and some medical subspecialty groups. Why should hospitalist practice be different?
Another misconception about production-based compensation is that it is synonymous with foregoing any financial support from your hospital or other sponsoring institution. It isn’t. You can still pay individual doctors on productivity and include financial support from the hospital. For example, if the doctors are paid $55 for every wRVU generated, then $40 of that might come from professional fee collections, and $15 from the hospital (employer).
Others fear that a salary based on production will cause doctors to work at unreasonably high workloads, leading to poor patient care or patient satisfaction, or less efficient use of hospital resources (e.g., keep patients in the hospital longer). This is a potential risk, but not a common problem in my experience. There can also be concern that compensation based on productivity will cause the doctors within a group to compete with one another for patients (and income), leading to stress within the group. This is an uncommon problem, and—if it occurs within your group—it probably means that there are too many doctors in your practice (or that you should market the practice to attract more patients) rather than proving that productivity-based compensation is a bad idea.
But an explanation that clarifies objections to productivity-based compensation certainly isn’t enough of a reason to support it. You need to be convinced of some of its benefits. Hospitalists who aren’t used to being paid based in part or in whole on production tend to see it as a very stressful—or even oppressive—way to be paid. But I hope to convince you it is actually liberating.
In the absence of a production component, many groups try hard to ensure that every doctor works the same amount. For example, a group that pays a fixed annual salary to all doctors typically encourages or insists that each doctor must work almost the same amount. But when paid on production, each doctor in the group can, within reasonable boundaries, decide how much he or she wants to work. Of course all of the group’s work must be taken care of, but in nearly every group some doctors are probably willing to work a little more and others a little less than the average workload for the group.
Nearly 15 years ago, before I married and had children, I got hooked on the idea of learning to fly airplanes. Wow, did I enjoy it. But it is pretty time consuming to get a pilot’s license, to say nothing of the expense. There were a number of days that I was to be the admitting doctor for our practice, but great weather and an available plane and instructor would lure me away. On a number of occasions at 4 or 5 p.m. I called my partner who had gone home for the day and said, “Chuck, would you be willing to cover admissions so I can go flying?” He usually said “sure,” at which point I’d tell him that there were already two patients waiting in the ED.
This system made both of us happy. After nine months I was a licensed pilot and for that year my partner had a much higher income than I did. We both got what we wanted, and paying ourselves on production is what made this possible. If we were in a group with a fixed salary I can’t imagine he would have been willing to help me out so often (if ever), and I would have been limited to taking flying lessons only on my days off. Or I would have needed to pay my partner back by making up the evenings he covered for me.
My point in telling this story is that so many people think of paying hospitalists based entirely, or in part, on production is just a way to get them to maintain unreasonably high work loads. But I think it simply liberates the doctor to decide for himself what the right workload is, while owning the economic consequences of that choice. It allowed me the opportunity to work less.
A few hospitalists paid on production might choose badly and choose to work at an unreasonable (or unsafe) pace, but nearly all will make reasonable decisions. And members of a group can periodically adjust their workload up or down according to their need at the time; there is no requirement to work at the same load year after year. In fact, my partners and I in Florida didn’t even keep track of precisely how often each of us was on call over the year because there wasn’t any reason it needed to be the same for each person. (We did make some effort to distribute call evenly, but didn’t worry when it never worked out just right because each doctor could take more or less call and see a corresponding change in income).
I realize that there is no perfect compensation system, and one based on production can have shortcomings. But I think too many hospitalists assume the only reasonable system is one such as a fixed annual salary, or an hourly rate, or some method that intentionally avoids paying for productivity. You should think about how liberating productivity compensation can be. Basing a significant portion (say 40% or more—or even 100%) on productivity might be a good idea for you.
And there is nothing about productivity-based compensation that interferes with also providing financial reward for good quality of care. I’m a fan of both. If payers increasingly use quality of care as the basis for physician reimbursement in the future, individual physician compensation formulas should be based more on quality than production. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.