User login
Mitchel is a reporter for MDedge based in the Philadelphia area. He started with the company in 1992, when it was International Medical News Group (IMNG), and has since covered a range of medical specialties. Mitchel trained as a virologist at Roswell Park Memorial Institute in Buffalo, and then worked briefly as a researcher at Boston Children's Hospital before pivoting to journalism as a AAAS Mass Media Fellow in 1980. His first reporting job was with Science Digest magazine, and from the mid-1980s to early-1990s he was a reporter with Medical World News. @mitchelzoler
Congenital Heart Disease Screening Cuts Infant Mortality
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
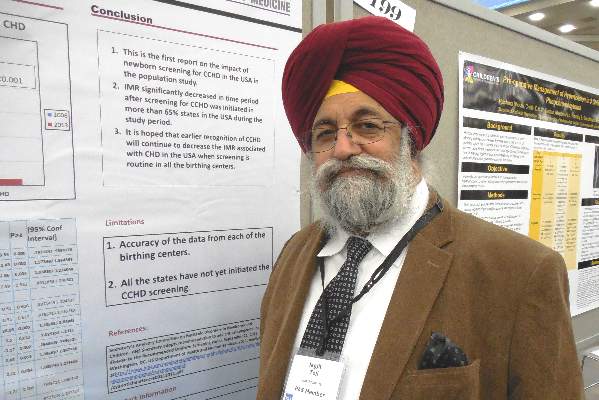
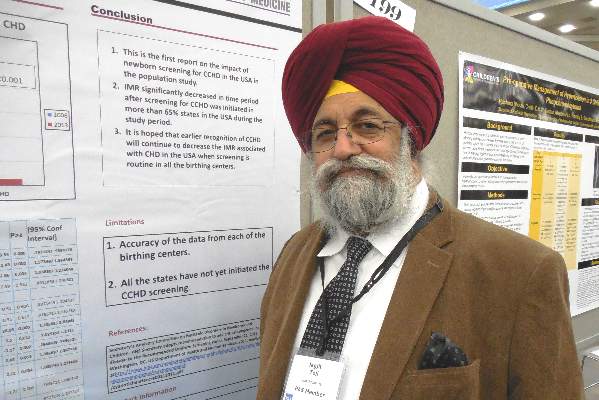
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
AT THE PAS ANNUAL MEETING
Congenital heart disease screening cuts infant mortality
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
On Twitter @mitchelzoler
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
On Twitter @mitchelzoler
BALTIMORE – The mandate to screen all U.S.-born neonates for critical congenital heart disease that started in 2011 has had an apparent effect on infant mortality.
By 2013, national U.S. data showed that the number of U.S. infants who died attributable to congenital heart disease had dropped by a small but statistically significant percentage, compared with a reference year prior to initiation of the mandate, 2006, Dr. Jagjit S. Teji reported in a poster at the annual meeting of the Pediatric Academic Societies.
“This is the first report on the impact of newborn screening for critical congenital heart disease,” said Dr. Teji, a neonatologist at Northwestern University in Chicago.
He analyzed birth and death records from the U.S. National Center for Health Statistics and calculated that infant mortality in 2013, compared with 2006, included roughly 100 fewer infants deaths attributable to congenital heart disease, a statistically significant difference, after adjusting for differences in variables between the 2 years that could affect mortality, including gestational ages at delivery, birth weight, maternal age, race, ethnicity, and marital status. The decrease occurred despite an overall increase in U.S. births of about 8% from 2006 to 2013.
In 2013, the rate of infant mortality was 0.027%, while in 2006 it was 0.032%, Dr. Teji reported. The decrease that appeared attributable to early screening for critical congenital heart disease was especially notable because by 2013 only two-thirds of states had a rule in place mandating newborn screening following the 2011 recommendation from the Department of Health & Human Services to U.S. clinicians to noninvasively measure blood oxygenation levels in the upper and lower limbs of newborns, using pulse oximetry, Dr. Teji said. By April 2016, this had grown to 48 states with mandates for newborn screening of critical congenital heart disease, usually performed just before newborns are discharged or after they are 24 hours old. Idaho and Wyoming are the exceptions.
Dr. Teji had no relevant financial disclosures.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Universal screening of U.S. neonates for critical congenital heart disease appeared to result in a significant reduction in infant mortality by 2013.
Major finding: U.S. infant mortality fell from an adjusted rate of 0.032% in 2006 to 0.027% in 2013, a statistically significant difference.
Data source: U.S. birth and death records from the National Center for Health Statistics.
Disclosures: Dr. Teji had no relevant financial disclosures.
Acid blockers boost infections in outpatient preemies
BALTIMORE – Treatment of premature infants with a drug that blocks gastroesophageal reflux once they are discharged home during the first year of life was associated with a significantly increased risk for development of pneumonia and gastroenteritis in a case-control study with 695 matched-pairs of infants.
Administering either a histamine2-receptor antagonist or proton pump inhibitor to these children was associated with an adjusted 75% increased risk for pneumonia and a 2.4-fold increased risk for gastroenteritis during the periods when the infants were on these acid-blocking drugs, Dr. Scott A. Lorch said at the annual meeting of the Pediatric Academic Societies. However, these medications did not appear to produce any lingering effects, with the rates of these infections falling to match control rates after acid-blocking treatment ceased.
The findings highlight that acid-blocking drugs “are not without consequences” and so should be “carefully considered before initiating therapy in this medically fragile population [premature infants], and if they are prescribed their continued need should be frequently assessed,” said Dr. Lorch, a neonatologist at the Children’s Hospital of Philadelphia.
In his experience, acid blockers “are being used like water, both in the hospital as well as after the infants go home. That is where there is concern. We see a fair number of kids on these medications for a much longer period of time than you’d expect. The average time on these medications is 6 months, and that is a long time to be on them,” Dr. Lorch said.
He noted that study results reported in 2015 by himself and his associates showed that in the 30-site primary care network affiliated with the Children’s Hospital of Philadelphia, three-quarters of the acid-blocking drug prescriptions written for infants who had been born prematurely came from primary care physicians once the infants had been discharged from the hospital.
The current study used data that had been collected on more than 2,000 infants who had been born at less than 36 weeks’ gestation during 2007-2009 and then discharged within 4 months of delivery into care by the primary care network and then followed until they were 3 years old. From this cohort, the researchers identified 695 infants who began treatment with either a histamine2-receptor antagonist or a proton pump inhibitor at some time during their first year and matched them by gestational age at birth and race with an equal number of infants from the cohort who never received an acid-blocking drug.
Dr. Lorch and his associates then analyzed the incidence rates of four different types of infections in the children during three time periods: while they were on the acid-blocking medication, and at 7 months and 13 months after the acid-blocking treatment stopped. Infection rates in the controls were tallied at ages that matched the periods studied in those who received the acid blockers.
The four infections they studied were pneumonia, gastroenteritis, bronchiolitis, and conjunctivitis. The last was included as a control as the researchers presumed that acid-blocker use should have no impact on the rates of conjunctivitis.
The results showed that during acid-blocker treatment, the incidence rate of pneumonia was 5% in those on an acid blocker and 3% in the controls, and the incidence of gastroenteritis was 19% in those on an acid blocker and 12% in the controls, Dr. Lorch reported. However, the rates of both infections were similar at 7 and 13 months after acid-blocker treatment stopped, and there was also no difference in the rates of both bronchiolitis and conjunctivitis during any period examined.
A multivariate analysis that controlled for a variety of clinical and demographic variables determined the 75% increased odds ratio for pneumonia and the 2.4-fold increased rate of gastroenteritis, compared with the controls, during periods of acid-blocker treatment. The analysis also showed that the presence of chronic lung disease appeared to have no impact on these infection rates.
Dr. Lorch had no relevant financial disclosures.
On Twitter @mitchelzoler
BALTIMORE – Treatment of premature infants with a drug that blocks gastroesophageal reflux once they are discharged home during the first year of life was associated with a significantly increased risk for development of pneumonia and gastroenteritis in a case-control study with 695 matched-pairs of infants.
Administering either a histamine2-receptor antagonist or proton pump inhibitor to these children was associated with an adjusted 75% increased risk for pneumonia and a 2.4-fold increased risk for gastroenteritis during the periods when the infants were on these acid-blocking drugs, Dr. Scott A. Lorch said at the annual meeting of the Pediatric Academic Societies. However, these medications did not appear to produce any lingering effects, with the rates of these infections falling to match control rates after acid-blocking treatment ceased.
The findings highlight that acid-blocking drugs “are not without consequences” and so should be “carefully considered before initiating therapy in this medically fragile population [premature infants], and if they are prescribed their continued need should be frequently assessed,” said Dr. Lorch, a neonatologist at the Children’s Hospital of Philadelphia.
In his experience, acid blockers “are being used like water, both in the hospital as well as after the infants go home. That is where there is concern. We see a fair number of kids on these medications for a much longer period of time than you’d expect. The average time on these medications is 6 months, and that is a long time to be on them,” Dr. Lorch said.
He noted that study results reported in 2015 by himself and his associates showed that in the 30-site primary care network affiliated with the Children’s Hospital of Philadelphia, three-quarters of the acid-blocking drug prescriptions written for infants who had been born prematurely came from primary care physicians once the infants had been discharged from the hospital.
The current study used data that had been collected on more than 2,000 infants who had been born at less than 36 weeks’ gestation during 2007-2009 and then discharged within 4 months of delivery into care by the primary care network and then followed until they were 3 years old. From this cohort, the researchers identified 695 infants who began treatment with either a histamine2-receptor antagonist or a proton pump inhibitor at some time during their first year and matched them by gestational age at birth and race with an equal number of infants from the cohort who never received an acid-blocking drug.
Dr. Lorch and his associates then analyzed the incidence rates of four different types of infections in the children during three time periods: while they were on the acid-blocking medication, and at 7 months and 13 months after the acid-blocking treatment stopped. Infection rates in the controls were tallied at ages that matched the periods studied in those who received the acid blockers.
The four infections they studied were pneumonia, gastroenteritis, bronchiolitis, and conjunctivitis. The last was included as a control as the researchers presumed that acid-blocker use should have no impact on the rates of conjunctivitis.
The results showed that during acid-blocker treatment, the incidence rate of pneumonia was 5% in those on an acid blocker and 3% in the controls, and the incidence of gastroenteritis was 19% in those on an acid blocker and 12% in the controls, Dr. Lorch reported. However, the rates of both infections were similar at 7 and 13 months after acid-blocker treatment stopped, and there was also no difference in the rates of both bronchiolitis and conjunctivitis during any period examined.
A multivariate analysis that controlled for a variety of clinical and demographic variables determined the 75% increased odds ratio for pneumonia and the 2.4-fold increased rate of gastroenteritis, compared with the controls, during periods of acid-blocker treatment. The analysis also showed that the presence of chronic lung disease appeared to have no impact on these infection rates.
Dr. Lorch had no relevant financial disclosures.
On Twitter @mitchelzoler
BALTIMORE – Treatment of premature infants with a drug that blocks gastroesophageal reflux once they are discharged home during the first year of life was associated with a significantly increased risk for development of pneumonia and gastroenteritis in a case-control study with 695 matched-pairs of infants.
Administering either a histamine2-receptor antagonist or proton pump inhibitor to these children was associated with an adjusted 75% increased risk for pneumonia and a 2.4-fold increased risk for gastroenteritis during the periods when the infants were on these acid-blocking drugs, Dr. Scott A. Lorch said at the annual meeting of the Pediatric Academic Societies. However, these medications did not appear to produce any lingering effects, with the rates of these infections falling to match control rates after acid-blocking treatment ceased.
The findings highlight that acid-blocking drugs “are not without consequences” and so should be “carefully considered before initiating therapy in this medically fragile population [premature infants], and if they are prescribed their continued need should be frequently assessed,” said Dr. Lorch, a neonatologist at the Children’s Hospital of Philadelphia.
In his experience, acid blockers “are being used like water, both in the hospital as well as after the infants go home. That is where there is concern. We see a fair number of kids on these medications for a much longer period of time than you’d expect. The average time on these medications is 6 months, and that is a long time to be on them,” Dr. Lorch said.
He noted that study results reported in 2015 by himself and his associates showed that in the 30-site primary care network affiliated with the Children’s Hospital of Philadelphia, three-quarters of the acid-blocking drug prescriptions written for infants who had been born prematurely came from primary care physicians once the infants had been discharged from the hospital.
The current study used data that had been collected on more than 2,000 infants who had been born at less than 36 weeks’ gestation during 2007-2009 and then discharged within 4 months of delivery into care by the primary care network and then followed until they were 3 years old. From this cohort, the researchers identified 695 infants who began treatment with either a histamine2-receptor antagonist or a proton pump inhibitor at some time during their first year and matched them by gestational age at birth and race with an equal number of infants from the cohort who never received an acid-blocking drug.
Dr. Lorch and his associates then analyzed the incidence rates of four different types of infections in the children during three time periods: while they were on the acid-blocking medication, and at 7 months and 13 months after the acid-blocking treatment stopped. Infection rates in the controls were tallied at ages that matched the periods studied in those who received the acid blockers.
The four infections they studied were pneumonia, gastroenteritis, bronchiolitis, and conjunctivitis. The last was included as a control as the researchers presumed that acid-blocker use should have no impact on the rates of conjunctivitis.
The results showed that during acid-blocker treatment, the incidence rate of pneumonia was 5% in those on an acid blocker and 3% in the controls, and the incidence of gastroenteritis was 19% in those on an acid blocker and 12% in the controls, Dr. Lorch reported. However, the rates of both infections were similar at 7 and 13 months after acid-blocker treatment stopped, and there was also no difference in the rates of both bronchiolitis and conjunctivitis during any period examined.
A multivariate analysis that controlled for a variety of clinical and demographic variables determined the 75% increased odds ratio for pneumonia and the 2.4-fold increased rate of gastroenteritis, compared with the controls, during periods of acid-blocker treatment. The analysis also showed that the presence of chronic lung disease appeared to have no impact on these infection rates.
Dr. Lorch had no relevant financial disclosures.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Premature infants who were discharged home and then received a drug to prevent gastroesophageal reflux during their first year had significantly increased rates of pneumonia and gastroenteritis during the periods when they were on the acid-blocking drugs.
Major finding: Treatment with an acid-blocking drug was associated with a 75% increased rate of pneumonia and a 2.4-fold higher rate of gastroenteritis.
Data source: Case-control study involving 695 matched pairs of infants from a single U.S. primary care network.
Disclosures: Dr. Lorch had no relevant financial disclosures.
Vitamin D Supplementation Cuts Dust Mite Atopy
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
AT THE PAS ANNUAL MEETING
Vitamin D supplementation cuts dust mite atopy
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
On Twitter @mitchelzoler
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
On Twitter @mitchelzoler
BALTIMORE – Three months of daily, oral treatment with a relatively high but safe dosage of a vitamin D supplement to pregnant mothers during late gestation followed by continued oral supplementation to their neonates during the first 6 months of life led to a significant reduction in the prevalence of dust-mite skin reactivity in those children once they reached 18 months old in a randomized, controlled trial with 259 mothers and infants.
And in a preliminary assessment that tallied the number of children who required primary care office visits for asthma through age 18 months, children who had received the highest vitamin D supplementation also showed a statistically significant reduction of these visits, compared with the placebo control children, Dr. Cameron C. Grant reported at the annual meeting of the Pediatric Academic Societies.
This suggestion that the vitamin D intervention could cut asthma development is not completely certain because in 18-month-old children, diagnosis of asthma is “very insecure,” noted Dr. Grant, a pediatrician at the University of Auckland, New Zealand and at Starship Children’s Hospital, also in Auckland. In addition, a limitation of the observed effect on dust mite atopy on skin-test challenge was that this follow-up occurred in only 186 (72%) of the 259 infants who participated in the study.
The study’s premise was that vitamin D is an immune system modulator, and that New Zealand provides an excellent setting to test the hypothesis that normalized vitamin D levels can help prevent development of atopy and asthma because many of the country’s residents are vitamin D deficient due to their diet and sun avoidance to prevent skin cancers. Results from prior studies had shown that 57% of New Zealand neonates have inadequate levels of vitamin D at birth, defined as a serum level of 25-hydroxyvitamin D of less than 20 ng/ml (less than 50 nmol/L), Dr. Grant noted.
“I think this intervention will only work in populations that are vitamin D deficient,” Dr. Grant said in an interview. In his study, the average serum level of 25-hydroxyvitamin D among control neonates was 38 nmol/L (about 15 ng/mL). In contrast, neonates born to mothers who had received a daily, higher-dose vitamin D supplement during the third trimester had serum measures that were roughly twice that level.
The study enrolled 260 pregnant women from the Auckland area with a single pregnancy at 26-30 weeks’ gestation; average gestational age at baseline was 27 weeks. Dr. Grant and his associates randomized the mothers to receive 1,000 IU oral vitamin D daily, 2,000 oral vitamin D daily, or placebo. The women delivered 259 infants. Infants born to women on the lower dosage supplement then received 400 IU vitamin daily for 6 months, those born to mothers on the higher level supplement received 800 IU vitamin D daily for 6 months, and those born to mothers in the placebo group received placebo supplements daily for 6 months.
Both supplement regimens led to statistically significant increases in serum levels of 25-hydroxyvitamin D in maternal serum at 36 weeks’ gestation, in cord blood at delivery, in the neonates’ serum at ages 2 months and 4 months, and in infant serum in the higher dosage group at 6 months of age, compared with similar measures taken at all these time points in the placebo group.
In addition, the neonates in the higher dosage group had significantly higher serum levels at 2, 4, and 6 months, compared with the lower dosage group. When measured a final time at 18-month follow-up, a year after the end of vitamin D supplementation, average serum levels of 25-hydroxyvitamin D in an three subgroups of children were virtually identical and similar to maternal serum levels at baseline. Dr. Grant and his associates had previously reported these findings and also had documented the safety of both the low and high levels of vitamin D supplements for both mothers and their children (Pediatrics. 2014 Jan;133[1]:e143-53).
The new findings reported by Dr. Grant focused on clinical outcomes at 18 months. He and his colleagues ran skin-prick testing on 186 of the 259 (72%) children in the study (the remaining children weren’t available for this follow-up assessment). They tested three aeroallergens: cat, pollen, and house dust mite. They saw no significant differences in the prevalence of positive skin-prick reactions among the three study groups to cat and pollen, but prevalence levels of positive reactions to dust mite were 9% in the controls, 3% of children in the low-dosage group, and none in the high dosage group. The difference between the controls and high dosage groups was statistically significant; the difference between the controls and the low dosage group was not significant, Dr. Grant said. Additional testing of specific IgE responses to four different dust mite antigens showed statistically significant reductions in responses to each of the four antigens among the high dosage children, compared with the controls and with the low dosage children.
The researchers also tallied the number of acute, primary care office visits during the first 18 months of life among the children in each of the three subgroups for a variety of respiratory diagnoses. The three groups showed no significant differences in total number of office visits for most of these diagnoses, including colds, otitis media, croup, and bronchitis. However, about 12% of children in the control group had been seen in a primary care office for a diagnosis of asthma, compared with none of the children in the low dosage group and about 4% in the high-dosage group. The differences between the two intervention groups and the control group were statistically significant. Dr. Grant cautioned that this finding is very preliminary and that any conclusions about the impact of vitamin D supplements on asthma incidence must await studies with larger numbers of children who are followed to an older age.
Dr. Grant had no disclosures.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Maternal treatment to achieve adequate vitamin D levels during late gestation followed by neonatal vitamin D supplementation significantly cut dust mite atopy at 18 months of age, along with a suggestion of reduced asthma incidence.
Major finding: Dust mite reactivity at 18 months occurred in no children treated with higher vitamin D supplementation and in 9% of controls.
Data source: A randomized, controlled, single-center study with 260 pregnant women who delivered 259 infants.
Disclosures: Dr. Grant had no disclosures.
Pediatric self-administration drives cough and cold drug mishaps
BALTIMORE – The vast majority of reported U.S. episodes of cough and cold medication serious adverse event episodes in young children occurred by an accidental, self-administration overdose, according to a review of all pediatric episodes collected by the designated national surveillance system during 2008-2014.
This pattern highlights the continued need for diligent education of families about the potential danger posed by these largely OTC products as well as a possible additional need for further improvement in protective packaging, Dr. G. Sam Wang said at the annual meeting of the Pediatric Academic Societies.
Although the manufacturers of these products voluntarily changed their labeling in 2007 to say “do not use” in children younger than 4 years old, the continued vulnerability of very young children and the high rate of self-administration suggests that labeling restrictions alone are “unlikely to have a significant impact” on the problem, he said. “What could be better is storage and [packaging] engineering controls to prevent the accidental ingestions that seem to represent the majority of cases,” Dr. Wang said in an interview.
The good news was that the 4,250 reported U.S. cases during 2008-2014 in children younger than age 12 years and judged by an expert review panel to be at least potentially related to cold and cough medications represents a significant decline, compared with earlier periods, and is also “quite low” when compared with the millions of units in annual U.S. sales.
“The overall adverse event rate compared with the volume sold is in the single digits per million of products sold, and the rate has been declining,” said Dr. Wang, a pediatric toxicologist at the University of Colorado in Denver and a consultant to the Rocky Mountain Poison & Drug Center, also in Denver, the group that maintains and reviews this registry, begun in January 2008. “I think we’re making progress,” but diligent education by physicians and other health care providers about the dangers posed by these drugs must continue, he said.
The analysis also identified that two drugs were by far the top culprits in causing pediatric adverse reactions to cough and cold medications, diphenhydramine and dextromethorphan. Diphenhydramine played a role in 53% of the 4,224 nonfatal adverse reaction cases and 54% of the 26 fatal cases identified by the registry panel as at least potentially related to a cough and cold medication, while dextromethorphan was responsible for 41% of the nonfatal and 19% of the fatal cases. In a majority of cases, these drugs were in products with a single active ingredient, although products with combined ingredients also played a role for some cases. Most often these drugs were in OTC formulations and in pediatric formulations.
Dr. Wang called it unlikely that manufacturers would formulate cold and cough medications without diphenhydramine or dextromethorphan because these drugs have the antitussive and sedative properties that consumers seek from cough and cold medications. He also noted that the addition of bittering agents to formulations have not had a history of reducing accidental self-administrations by children, but added “a good taste doesn’t help.”
During 2008-2014 U.S. surveillance by the registry review panel identified a total of 5,342 unique case reports of serious adverse events in children less than 12 years old and believed related to any of eight drugs commonly found in cold and cough medications. The reports came from any of five sources: the National Poison Data System, the Food and Drug Administration’s adverse event reporting system, safety reports to manufacturers, and through surveillance of the medical literature, and the news media. The panel winnowed these down to 4,250 cases at least potentially related to these drugs.
Among the 26 fatal cases, 16 (62%) occurred in children less than 2 years old and an additional four (15%) were in children aged 2 years to less than 4 years. Nine of these cases (35%) involved parental administration, with only two cases (8%) involving self-administration. An additional nine cases (35%) had no reported source of administration, and the remaining six (23%) cases involved other sources of administration. Seven of the 26 fatalities involved confirmed overdoses, with the dose unknown for the remaining 19 cases, Dr. Wang reported.
Among the 4,224 nonfatal cases, 15% occurred in children less than 2 years, 46% in children ages 2 years to less than 4 years, 19% in children 4 years to less than 6 years and 20% in children 6 years to less than 12 years. These cases involved a confirmed overdose in 73% of cases, a therapeutic range dose in 7%, with the remainder involving a dose of unknown size. Self-administration occurred 75% of the time.
On Twitter @mitchelzoler
BALTIMORE – The vast majority of reported U.S. episodes of cough and cold medication serious adverse event episodes in young children occurred by an accidental, self-administration overdose, according to a review of all pediatric episodes collected by the designated national surveillance system during 2008-2014.
This pattern highlights the continued need for diligent education of families about the potential danger posed by these largely OTC products as well as a possible additional need for further improvement in protective packaging, Dr. G. Sam Wang said at the annual meeting of the Pediatric Academic Societies.
Although the manufacturers of these products voluntarily changed their labeling in 2007 to say “do not use” in children younger than 4 years old, the continued vulnerability of very young children and the high rate of self-administration suggests that labeling restrictions alone are “unlikely to have a significant impact” on the problem, he said. “What could be better is storage and [packaging] engineering controls to prevent the accidental ingestions that seem to represent the majority of cases,” Dr. Wang said in an interview.
The good news was that the 4,250 reported U.S. cases during 2008-2014 in children younger than age 12 years and judged by an expert review panel to be at least potentially related to cold and cough medications represents a significant decline, compared with earlier periods, and is also “quite low” when compared with the millions of units in annual U.S. sales.
“The overall adverse event rate compared with the volume sold is in the single digits per million of products sold, and the rate has been declining,” said Dr. Wang, a pediatric toxicologist at the University of Colorado in Denver and a consultant to the Rocky Mountain Poison & Drug Center, also in Denver, the group that maintains and reviews this registry, begun in January 2008. “I think we’re making progress,” but diligent education by physicians and other health care providers about the dangers posed by these drugs must continue, he said.
The analysis also identified that two drugs were by far the top culprits in causing pediatric adverse reactions to cough and cold medications, diphenhydramine and dextromethorphan. Diphenhydramine played a role in 53% of the 4,224 nonfatal adverse reaction cases and 54% of the 26 fatal cases identified by the registry panel as at least potentially related to a cough and cold medication, while dextromethorphan was responsible for 41% of the nonfatal and 19% of the fatal cases. In a majority of cases, these drugs were in products with a single active ingredient, although products with combined ingredients also played a role for some cases. Most often these drugs were in OTC formulations and in pediatric formulations.
Dr. Wang called it unlikely that manufacturers would formulate cold and cough medications without diphenhydramine or dextromethorphan because these drugs have the antitussive and sedative properties that consumers seek from cough and cold medications. He also noted that the addition of bittering agents to formulations have not had a history of reducing accidental self-administrations by children, but added “a good taste doesn’t help.”
During 2008-2014 U.S. surveillance by the registry review panel identified a total of 5,342 unique case reports of serious adverse events in children less than 12 years old and believed related to any of eight drugs commonly found in cold and cough medications. The reports came from any of five sources: the National Poison Data System, the Food and Drug Administration’s adverse event reporting system, safety reports to manufacturers, and through surveillance of the medical literature, and the news media. The panel winnowed these down to 4,250 cases at least potentially related to these drugs.
Among the 26 fatal cases, 16 (62%) occurred in children less than 2 years old and an additional four (15%) were in children aged 2 years to less than 4 years. Nine of these cases (35%) involved parental administration, with only two cases (8%) involving self-administration. An additional nine cases (35%) had no reported source of administration, and the remaining six (23%) cases involved other sources of administration. Seven of the 26 fatalities involved confirmed overdoses, with the dose unknown for the remaining 19 cases, Dr. Wang reported.
Among the 4,224 nonfatal cases, 15% occurred in children less than 2 years, 46% in children ages 2 years to less than 4 years, 19% in children 4 years to less than 6 years and 20% in children 6 years to less than 12 years. These cases involved a confirmed overdose in 73% of cases, a therapeutic range dose in 7%, with the remainder involving a dose of unknown size. Self-administration occurred 75% of the time.
On Twitter @mitchelzoler
BALTIMORE – The vast majority of reported U.S. episodes of cough and cold medication serious adverse event episodes in young children occurred by an accidental, self-administration overdose, according to a review of all pediatric episodes collected by the designated national surveillance system during 2008-2014.
This pattern highlights the continued need for diligent education of families about the potential danger posed by these largely OTC products as well as a possible additional need for further improvement in protective packaging, Dr. G. Sam Wang said at the annual meeting of the Pediatric Academic Societies.
Although the manufacturers of these products voluntarily changed their labeling in 2007 to say “do not use” in children younger than 4 years old, the continued vulnerability of very young children and the high rate of self-administration suggests that labeling restrictions alone are “unlikely to have a significant impact” on the problem, he said. “What could be better is storage and [packaging] engineering controls to prevent the accidental ingestions that seem to represent the majority of cases,” Dr. Wang said in an interview.
The good news was that the 4,250 reported U.S. cases during 2008-2014 in children younger than age 12 years and judged by an expert review panel to be at least potentially related to cold and cough medications represents a significant decline, compared with earlier periods, and is also “quite low” when compared with the millions of units in annual U.S. sales.
“The overall adverse event rate compared with the volume sold is in the single digits per million of products sold, and the rate has been declining,” said Dr. Wang, a pediatric toxicologist at the University of Colorado in Denver and a consultant to the Rocky Mountain Poison & Drug Center, also in Denver, the group that maintains and reviews this registry, begun in January 2008. “I think we’re making progress,” but diligent education by physicians and other health care providers about the dangers posed by these drugs must continue, he said.
The analysis also identified that two drugs were by far the top culprits in causing pediatric adverse reactions to cough and cold medications, diphenhydramine and dextromethorphan. Diphenhydramine played a role in 53% of the 4,224 nonfatal adverse reaction cases and 54% of the 26 fatal cases identified by the registry panel as at least potentially related to a cough and cold medication, while dextromethorphan was responsible for 41% of the nonfatal and 19% of the fatal cases. In a majority of cases, these drugs were in products with a single active ingredient, although products with combined ingredients also played a role for some cases. Most often these drugs were in OTC formulations and in pediatric formulations.
Dr. Wang called it unlikely that manufacturers would formulate cold and cough medications without diphenhydramine or dextromethorphan because these drugs have the antitussive and sedative properties that consumers seek from cough and cold medications. He also noted that the addition of bittering agents to formulations have not had a history of reducing accidental self-administrations by children, but added “a good taste doesn’t help.”
During 2008-2014 U.S. surveillance by the registry review panel identified a total of 5,342 unique case reports of serious adverse events in children less than 12 years old and believed related to any of eight drugs commonly found in cold and cough medications. The reports came from any of five sources: the National Poison Data System, the Food and Drug Administration’s adverse event reporting system, safety reports to manufacturers, and through surveillance of the medical literature, and the news media. The panel winnowed these down to 4,250 cases at least potentially related to these drugs.
Among the 26 fatal cases, 16 (62%) occurred in children less than 2 years old and an additional four (15%) were in children aged 2 years to less than 4 years. Nine of these cases (35%) involved parental administration, with only two cases (8%) involving self-administration. An additional nine cases (35%) had no reported source of administration, and the remaining six (23%) cases involved other sources of administration. Seven of the 26 fatalities involved confirmed overdoses, with the dose unknown for the remaining 19 cases, Dr. Wang reported.
Among the 4,224 nonfatal cases, 15% occurred in children less than 2 years, 46% in children ages 2 years to less than 4 years, 19% in children 4 years to less than 6 years and 20% in children 6 years to less than 12 years. These cases involved a confirmed overdose in 73% of cases, a therapeutic range dose in 7%, with the remainder involving a dose of unknown size. Self-administration occurred 75% of the time.
On Twitter @mitchelzoler
AT THE PAS ANNUAL MEETING
Key clinical point: Serious adverse events in U.S. children caused by cough and cold medications most commonly occur from self-administration in children younger than 4 years old.
Major finding: Three-quarters of serious adverse events occurred by self-administration, with 61% of episodes in children younger than 4 years old.
Data source: Review of 5,342 reported U.S. cough and cold medication serious adverse event episodes in children during 2008-2014.
Disclosures: Dr. Wang had no disclosures.
ACCELERATE: Evacetrapib’s clinical failure sinks lipid-drug class
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Despite producing dramatically beneficially changes in lipid levels, treatment with evacetrapib failed to produce clinical benefit in its pivotal trial, adding to questions about benefits from the entire cholesterol ester transfer protein inhibitor class of drugs for cardiovascular disease prevention.
Major finding: During 25-month follow-up, cardiovascular disease events occurred in 13% of patients on evacetrapib and 13% of those on placebo.
Data source: ACCELERATE, a multicenter, international pivotal trial with 12,092 high-risk patients.
Disclosures: Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
PPI Cuts GI Events From Low- and High-dose Aspirin
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
AT ACC 2016
PPI cuts GI events from low- and high-dose aspirin
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for upper GI complications from aspirin (because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent), treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as high-dose aspirin. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups taking or not taking a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.*
*Changes were made to this story on 4/20/2016.
On Twitter @mitchelzoler
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for upper GI complications from aspirin (because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent), treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as high-dose aspirin. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups taking or not taking a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.*
*Changes were made to this story on 4/20/2016.
On Twitter @mitchelzoler
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for upper GI complications from aspirin (because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent), treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as high-dose aspirin. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups taking or not taking a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.*
*Changes were made to this story on 4/20/2016.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: In patients at high risk of cardiovascular disease on dual-antiplatelet therapy, concurrent proton pump inhibitor treatment cut gastrointestinal events, regardless of whether patients received a low or high aspirin dosage.
Major finding: Omeprazole cut the rate of upper-GI bleeds by more than half in patients taking low- or high-dose aspirin.
Data source: Post-hoc analysis of data in COGENT, a multicenter, randomized trial with 3,762 patients.
Disclosures: Cogent was sponsored by Cogentus Pharmaceuticals; however, the company went bankrupt and provided no support for the current analysis. Dr. Vaduganathan had no disclosures.
Ticagrelor Cuts Post-MI Events in Diabetes Patients
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
CHICAGO – The benefit from dual-antiplatelet therapy in high-risk patients following a myocardial infarction was especially apparent in post-MI patients with diabetes in a prespecified secondary analysis from a multicenter trial of ticagrelor with more than 21,000 patients.
Among post-MI patients with diabetes, treatment with ticagrelor plus aspirin led to an absolute 1.5% reduction in the rate of cardiovascular death, MI, or stroke during a median 33-month follow-up, compared with an absolute 1.1% cut in patients without diabetes, Dr. Deepak L. Bhatt said at the annual meeting of the American College of Cardiology. The relative risk reduction, compared with placebo was 16% in both the diabetes and no diabetes subgroups, statistically significant differences in both subgroups.
“Long-term treatment with ticagrelor reduced the composite of cardiovascular death, MI, or stroke in diabetic patients with a greater absolute risk reduction than in nondiabetic patients,” said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital in Boston. Treatment with ticagrelor plus aspirin in post-MI patients with diabetes also led to an increased number of major bleeding episodes, compared with patients on aspirin alone, but no excess of intracerebral hemorrhages or fatal bleeds, he noted.
This finding of a significant benefit from ticagrelor in post-MI patients with diabetes confirms similar, prior findings with other antiplatelet drugs (including clopidogrel, prasugrel, and vorapaxar) and prior findings with ticagrelor, Dr. Bhatt noted.
The new analysis used data collected in the Prevention of Cardiovascular Events in Patients With Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial. The primary results from PEGASUS-TIMI 54 had shown that adding ticagrelor to aspirin treatment of high-risk post-MI patients, including those who both had or did not have diabetes, significantly cut the composite rate of cardiovascular death, MI, and stroke, compared with aspirin alone (N Engl J Med. 2015 May 7;372[19]:1791-800). The study group included 6,806 patients with diabetes (type 2 diabetes in 99% of these patients), and 14,355 without diabetes. All patients had their MI 1-3 years before entering the study.
Dr. Bhatt and his associates examined the incidence of the various clinical endpoints measured in the study among only the patients with diabetes divided into those who received any dosage of ticagrelor (60 mg b.i.d. or 90 mg b.i.d.) or placebo, and also among the patients without diabetes. In addition to the primary endpoint, the new analysis showed that the rate of cardiovascular death during follow-up was 3.9% in the diabetes patients on dual therapy and 5.0% among the diabetes patients on aspirin only, a 22% relative risk reduction with ticagrelor added that was statistically significant. In contrast, among patients without diabetes the rates of cardiovascular death between those on and not on ticagrelor only differed by 0.2%, a 9% relative risk reduction that was not statistically significant. The same pattern occurred for the endpoint of death from coronary artery disease.
Concurrent with Dr. Bhatt’s report, the results appeared in an article published online (J Am Coll Cardiol. 2016 Apr; doi: 10.1016/S0735-1097[16]30023-7).
A new study, THEMIS, is examining the safety and efficacy of combined ticagrelor and aspirin treatment in a lower-risk group of patients with diabetes, those with coronary artery disease who have not had a prior MI. Those results may be available in 2018.
PEGASUS-TIMI 54 was sponsored by AstraZeneca, the company that markets ticagrelor (Brilinta). Dr. Bhatt has been an advisor to Cardax and Regado Biosciences and has received research support from AstraZeneca and several other companies.
AT ACC 2016