User login
Distal radius fractures constitute 15% of all extremity fractures and are the most common upper extremity fractures.1-3 The incidence of distal radius fractures is continuing to escalate because of the expanding elderly population and concurrent increase in osteoporosis.3,4 In addition, open reduction and internal fixation with a volar locking plate for distal radius fractures are more commonly being performed by general orthopedists, who may not perform these surgeries frequently. Surgically treated patients experience less time immobilized and have a higher chance of regaining previous functional status.2 In a commonly used technique, volar fixed-angle plating is used to stabilize the distal radius. With the rising popularity of this method, more patients are having postoperative complications.1,3,5,6 Extensor tendon irritation and attritional rupture constitute up to 50% of all complications stemming from volar plating of the distal radius.1
Volar plate fixation of the distal radius was originally designed to decrease postoperative tendon complications by preventing the flexor and extensor tendons from coming into direct contact with the surgically placed plates and/or screws.1 This technique places the volar plate under the belly of the pronator quadratus muscle. Shielding the flexor tendons, the pronator quadratus can prevent the volar plate from causing flexor tendon attrition. This shielding does not occur on the dorsal side of the wrist because the extensor tendons are in full contact with the dorsal radius. As such, volar fixation gained in popularity on the premise of preventing extensor tendon complications by directly avoiding the dorsal compartment.1,7
The most common complication of volar plating ironically involves the dorsal compartment.1,7 The typical distal radius fracture occurs when a fall on an outstretched hand results in significant dorsal comminution. In these cases, it can be difficult to judge the appropriate screw length, as the depth gauge does not have an intact cortex to hook. There is the temptation to use intraoperative fluoroscopy and the depth gauge to estimate screw lengths at the distal radius, especially in cases in which a surgeon may not perform this type of surgery often. More specifically, use of a lateral image to gauge the appropriate length for screws may be tempting, but a false estimate is possible.
Screw prominence on the dorsal cortex may be caused by the complex geometry of the distal radius. This geometry is produced by the Lister tubercle and its adjacent groove for the extensor pollicis longus.7 The dorsal shape of the distal radius is a dome or dihedral with the thickest part at the Lister tubercle. The dihedral shape may hide possible dorsal screw prominence on a lateral radiograph, but screw prominence can be appreciated with computed tomography (CT) (Figures 1, 2).
We conducted a study to determine if and where screw prominence occurs, and in what amount, to establish general guidelines for screw depth based on lateral radiographs. We also wanted to be able to highlight the potential source of postoperative complications.
Materials and Methods
Twelve preserved cadaveric forearms were used for this study. Two sets of arms were paired, and the other arms came from different cadavers. In total, 5 male arms (3 left, 2 right) and 7 female arms (5 left, 2 right) were used.
The arms were harvested using a bone saw to cut through the humerus just proximal to the epicondyles, keeping the ulna and radius completely intact. Each arm was examined by the naked eye and by fluoroscopy to determine if any significant anatomical or traumatic variations in the distal radius were present. None showed any abnormal variation.
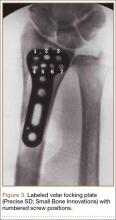
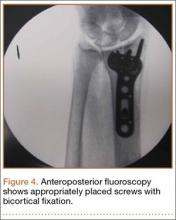
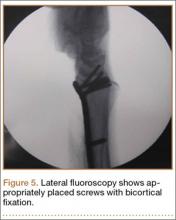
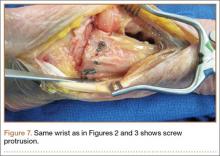
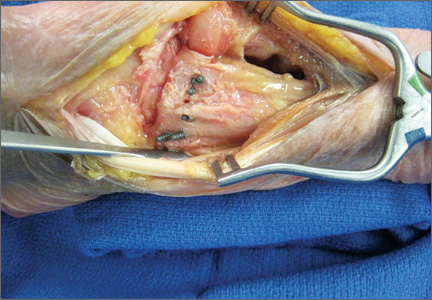
The flexor tendons and volar structures were removed to allow easy visualization and access to the distal radius. The volar locking plates (Precise SD; Small Bone Innovations) were positioned to the best anatomical and radiographic fit and secured with a proximal and distal Kirschner wire (Figure 3). A single cortical screw was placed through the shaft for compression. All 7 distal holes were drilled bicortically using an appropriately sized 2.0-mm drill and the standard block drill guide. A depth gauge was used in concordance with fluoroscopy to estimate the distance between cortices and appropriate screw lengths for each hole. A standard lateral view was used to determine the depth based on aligning the depth gauge at the dorsal cortex. The hook was not used to hook the dorsal cortex, as typically the dorsal cortex is severely comminuted and unavailable for measurement. Next, all 7 locking screws of premeasured length were secured into their respective holes. Anteroposterior, lateral, and oblique (forearm supinated and pronated 45°) radiographs were obtained to visualize screw placement and possible dorsal screw prominence (Figures 4-6).8 The extensor tendons and dorsal structures were then dissected away to expose any violation of the dorsal compartments, and calipers were used to measure absolute dorsal screw prominence and the depth of the Lister tubercle (Figure 7).
Mean (SD) dorsal prominence at each screw position was calculated. The screws were also categorized into radial (1,4), central (2,5), and ulnar (3,6,7) groups based on location within the plate (Figure 3). Equality of means testing was performed using a 1-way analysis of variance followed by a Bonferroni test.
Results
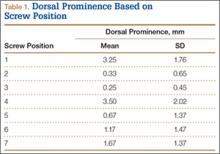
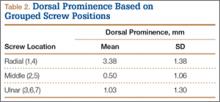
Mean (SD) dorsal prominence in millimeters is listed in Table 1. Positions 1 and 4 had significantly more dorsal prominence than the other 5 screw positions (P < .01 for all comparisons). Mean (SD) dorsal prominence based on grouped screw positions is listed in Table 2. There was significantly more dorsal prominence in the radial group that in the central group (P < .001) and ulnar group (P < .001). Mean depth of the Lister tubercle was 3.25 mm.
All prominent screws in the radial aspect of the radius were detected using a supinated 45° view. A 45° pronated view was not successful in demonstrating screw prominence on the ulnar side of the wrist because of overlap of the ulnar head.
Discussion
Extensor tendon irritation and extensor tendon rupture are frequent yet preventable complications of using volar plating systems to stabilize distal radius fractures. Many recent studies have investigated the intraoperative methodologies in order to identify real-time adjustments the surgeon can make to prevent negative outcomes. The first report of extensor tendon injury caused by volar plate fixation (published in 1989) was attributed to dorsal screw prominence.9,10 Even today, extensor tendon complications remain a challenge, as screw prominence is difficult to ascertain even with multiple intraoperative radiologic views.1,8
This study simulated real-time radiographic views to estimate if screws had extended into the dorsal compartment. These radiographic predictions were then correlated with the absolute dorsal screw prominence seen after dorsal compartment dissection. We determined that the supinated oblique view was the best imaging view for identifying radial styloid screw prominence.
Mean depth of the Lister tubercle was 3.25 mm (similar to previously reported 2 mm11). However, there was no correlation identified between depth of the Lister tubercle and amount of dorsal screw prominence.
We wanted to identify high-risk areas and estimate expected dorsal screw prominence in order to make appropriate intraoperative screw length adjustments. The radius is divided into radial, central, and ulnar columns. The central screw positions had the least dorsal screw prominence (mean, 0.50 mm). This central position was considered low-risk. Both the radial and the ulnar screw positions had more dorsal screw prominence (means, 3.38 mm and 1.03 mm, respectively). Only the radial screws had significantly more prominence. However, this study was not powered to detect a difference as small as that between the central and ulnar screw positions. Despite the lack of statistical significance, it is clear from the data that the ulnar screws trend toward more dorsal prominence, and, therefore, screw measurements at both the radial and ulnar screw locations (using the depth gauge) require adjustments.
Extensor tendon contact was difficult to determine based on any specific screw length, as the extensor tendon had to be dissected to determine prominence. Based on observations, a prominence of 2 mm seemed to present a risk for tendon irritation. The periosteum and the rounded end of the screw may obviate the risk with 1 mm of prominence. However, this observation may not hold true in an in vivo situation.
This study had several limitations. First, only a single brand of plate was used, making these findings specific to this system. However, concepts and conclusions can be extrapolated to all systems. The radial side had the highest risk for prominence, and this factor should be accounted for when selecting screw lengths. In addition, the ulnar column also poses some risk, but not to the degree of the radial column. Another limitation is that fractures were not created in these radii; therefore, dorsal comminution was not recreated. In some cases, the dorsal cortex may be displaced dorsally and be somewhat protective. This study is not meant to be an exhaustive study on all volar plates or provide absolute recommendations. It is meant to suggest caution to surgeons who may not be familiar with the complex anatomy of the dorsal radius and to identify areas where the risk for screw penetration is highest.
Shortening screw lengths at the positions described may trigger surgeons’ concerns about stabilizing distal radius fractures. In a 2012 biomechanical study, Wall and colleagues12 found no difference between unicortical screws (placed at 75% of the distance to the dorsal cortex) and bicortical screws in effectiveness in stabilizing distal radius fractures.12 The proposed reduction will result in the desired bicortical screw lengths but limit prominence. In addition, in the setting of dorsal comminution, the increased stability gained by bicortical fixation is minimal.
In fractures with an intact dorsal cortex, standard depth gauges will likely produce appropriate screw length measurements. However, even in this situation, and based on the results reported by Wall and colleagues,12 subtraction of 1 to 2 mm may prove prudent. In cases in which the dorsal cortex is comminuted and screw estimates based on fluoroscopy are used, the lateral image may provide estimates that lead to screw prominence. A 45° supinated view should be used to check screw length for the radial side, the column most at risk. However, comminution may also obscure this view. We cannot comment on that, as the present study did not create comminuted fractures of the distal radius. In addition, the ulnar column posed a lesser but real risk of screw prominence, which must also be accounted for, and typically is not appreciated with alternate views.
Last, use of live fluoroscopy instead of standard anteroposterior and lateral views may prove valuable in assessing hardware placement and screw length in the setting of a comminuted distal radius fracture. Through use of live fluoroscopy, prominent screws, especially those on the radial side, may be identified, and potential tendon injury may be avoided. Keeping in mind the shape of the dorsal aspect of the distal radius should assist surgeons in preventing screw prominence dorsally and limit complications.
1. Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand. 2007;2(3):144-150.
2. Nana AD, Joshi A, Lichtman DM. Plating of the distal radius. J Am Acad Orthop Surg. 2005;13(3):159-171.
3. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29(1):96-102.
4. Protopsaltis TS, Ruch DS. Volar approach to distal radius fractures. J Hand Surg. 2008;33(6):958-965.
5. Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90(9):1855-1861.
6. Gruber G, Zacherl M, Giessauf C, et al. Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am. 2010;92(5):1170-1178.
7. Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of Lister’s tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg. 2008;33(10):1716-1719.
8. Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg. 2012;37(5):963-967.
9. Perry DC, Machin DM, Casaletto JA, Brown DJ. Minimising the risk of extensor pollicis longus rupture following volar plate fixation of distal radius fractures: a cadaveric study. Ann R Coll Surg Engl. 2011;93(1):57-60.
10. Wong-Chung J, Quinlan W. Rupture of extensor pollicis longus following fixation of a distal radius fracture. Injury. 1989;20(6):375-376.
11. Park DH, Goldie BS. Volar plating for distal radius fractures—do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg. 2012;16(3):169-172.
12. Wall LB, Brodt MD, Silva MJ, Boyer MI, Calfee RP. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg. 2012;37(3):446-453.
Distal radius fractures constitute 15% of all extremity fractures and are the most common upper extremity fractures.1-3 The incidence of distal radius fractures is continuing to escalate because of the expanding elderly population and concurrent increase in osteoporosis.3,4 In addition, open reduction and internal fixation with a volar locking plate for distal radius fractures are more commonly being performed by general orthopedists, who may not perform these surgeries frequently. Surgically treated patients experience less time immobilized and have a higher chance of regaining previous functional status.2 In a commonly used technique, volar fixed-angle plating is used to stabilize the distal radius. With the rising popularity of this method, more patients are having postoperative complications.1,3,5,6 Extensor tendon irritation and attritional rupture constitute up to 50% of all complications stemming from volar plating of the distal radius.1
Volar plate fixation of the distal radius was originally designed to decrease postoperative tendon complications by preventing the flexor and extensor tendons from coming into direct contact with the surgically placed plates and/or screws.1 This technique places the volar plate under the belly of the pronator quadratus muscle. Shielding the flexor tendons, the pronator quadratus can prevent the volar plate from causing flexor tendon attrition. This shielding does not occur on the dorsal side of the wrist because the extensor tendons are in full contact with the dorsal radius. As such, volar fixation gained in popularity on the premise of preventing extensor tendon complications by directly avoiding the dorsal compartment.1,7
The most common complication of volar plating ironically involves the dorsal compartment.1,7 The typical distal radius fracture occurs when a fall on an outstretched hand results in significant dorsal comminution. In these cases, it can be difficult to judge the appropriate screw length, as the depth gauge does not have an intact cortex to hook. There is the temptation to use intraoperative fluoroscopy and the depth gauge to estimate screw lengths at the distal radius, especially in cases in which a surgeon may not perform this type of surgery often. More specifically, use of a lateral image to gauge the appropriate length for screws may be tempting, but a false estimate is possible.
Screw prominence on the dorsal cortex may be caused by the complex geometry of the distal radius. This geometry is produced by the Lister tubercle and its adjacent groove for the extensor pollicis longus.7 The dorsal shape of the distal radius is a dome or dihedral with the thickest part at the Lister tubercle. The dihedral shape may hide possible dorsal screw prominence on a lateral radiograph, but screw prominence can be appreciated with computed tomography (CT) (Figures 1, 2).
We conducted a study to determine if and where screw prominence occurs, and in what amount, to establish general guidelines for screw depth based on lateral radiographs. We also wanted to be able to highlight the potential source of postoperative complications.
Materials and Methods
Twelve preserved cadaveric forearms were used for this study. Two sets of arms were paired, and the other arms came from different cadavers. In total, 5 male arms (3 left, 2 right) and 7 female arms (5 left, 2 right) were used.
The arms were harvested using a bone saw to cut through the humerus just proximal to the epicondyles, keeping the ulna and radius completely intact. Each arm was examined by the naked eye and by fluoroscopy to determine if any significant anatomical or traumatic variations in the distal radius were present. None showed any abnormal variation.
The flexor tendons and volar structures were removed to allow easy visualization and access to the distal radius. The volar locking plates (Precise SD; Small Bone Innovations) were positioned to the best anatomical and radiographic fit and secured with a proximal and distal Kirschner wire (Figure 3). A single cortical screw was placed through the shaft for compression. All 7 distal holes were drilled bicortically using an appropriately sized 2.0-mm drill and the standard block drill guide. A depth gauge was used in concordance with fluoroscopy to estimate the distance between cortices and appropriate screw lengths for each hole. A standard lateral view was used to determine the depth based on aligning the depth gauge at the dorsal cortex. The hook was not used to hook the dorsal cortex, as typically the dorsal cortex is severely comminuted and unavailable for measurement. Next, all 7 locking screws of premeasured length were secured into their respective holes. Anteroposterior, lateral, and oblique (forearm supinated and pronated 45°) radiographs were obtained to visualize screw placement and possible dorsal screw prominence (Figures 4-6).8 The extensor tendons and dorsal structures were then dissected away to expose any violation of the dorsal compartments, and calipers were used to measure absolute dorsal screw prominence and the depth of the Lister tubercle (Figure 7).
Mean (SD) dorsal prominence at each screw position was calculated. The screws were also categorized into radial (1,4), central (2,5), and ulnar (3,6,7) groups based on location within the plate (Figure 3). Equality of means testing was performed using a 1-way analysis of variance followed by a Bonferroni test.
Results
Mean (SD) dorsal prominence in millimeters is listed in Table 1. Positions 1 and 4 had significantly more dorsal prominence than the other 5 screw positions (P < .01 for all comparisons). Mean (SD) dorsal prominence based on grouped screw positions is listed in Table 2. There was significantly more dorsal prominence in the radial group that in the central group (P < .001) and ulnar group (P < .001). Mean depth of the Lister tubercle was 3.25 mm.
All prominent screws in the radial aspect of the radius were detected using a supinated 45° view. A 45° pronated view was not successful in demonstrating screw prominence on the ulnar side of the wrist because of overlap of the ulnar head.
Discussion
Extensor tendon irritation and extensor tendon rupture are frequent yet preventable complications of using volar plating systems to stabilize distal radius fractures. Many recent studies have investigated the intraoperative methodologies in order to identify real-time adjustments the surgeon can make to prevent negative outcomes. The first report of extensor tendon injury caused by volar plate fixation (published in 1989) was attributed to dorsal screw prominence.9,10 Even today, extensor tendon complications remain a challenge, as screw prominence is difficult to ascertain even with multiple intraoperative radiologic views.1,8
This study simulated real-time radiographic views to estimate if screws had extended into the dorsal compartment. These radiographic predictions were then correlated with the absolute dorsal screw prominence seen after dorsal compartment dissection. We determined that the supinated oblique view was the best imaging view for identifying radial styloid screw prominence.
Mean depth of the Lister tubercle was 3.25 mm (similar to previously reported 2 mm11). However, there was no correlation identified between depth of the Lister tubercle and amount of dorsal screw prominence.
We wanted to identify high-risk areas and estimate expected dorsal screw prominence in order to make appropriate intraoperative screw length adjustments. The radius is divided into radial, central, and ulnar columns. The central screw positions had the least dorsal screw prominence (mean, 0.50 mm). This central position was considered low-risk. Both the radial and the ulnar screw positions had more dorsal screw prominence (means, 3.38 mm and 1.03 mm, respectively). Only the radial screws had significantly more prominence. However, this study was not powered to detect a difference as small as that between the central and ulnar screw positions. Despite the lack of statistical significance, it is clear from the data that the ulnar screws trend toward more dorsal prominence, and, therefore, screw measurements at both the radial and ulnar screw locations (using the depth gauge) require adjustments.
Extensor tendon contact was difficult to determine based on any specific screw length, as the extensor tendon had to be dissected to determine prominence. Based on observations, a prominence of 2 mm seemed to present a risk for tendon irritation. The periosteum and the rounded end of the screw may obviate the risk with 1 mm of prominence. However, this observation may not hold true in an in vivo situation.
This study had several limitations. First, only a single brand of plate was used, making these findings specific to this system. However, concepts and conclusions can be extrapolated to all systems. The radial side had the highest risk for prominence, and this factor should be accounted for when selecting screw lengths. In addition, the ulnar column also poses some risk, but not to the degree of the radial column. Another limitation is that fractures were not created in these radii; therefore, dorsal comminution was not recreated. In some cases, the dorsal cortex may be displaced dorsally and be somewhat protective. This study is not meant to be an exhaustive study on all volar plates or provide absolute recommendations. It is meant to suggest caution to surgeons who may not be familiar with the complex anatomy of the dorsal radius and to identify areas where the risk for screw penetration is highest.
Shortening screw lengths at the positions described may trigger surgeons’ concerns about stabilizing distal radius fractures. In a 2012 biomechanical study, Wall and colleagues12 found no difference between unicortical screws (placed at 75% of the distance to the dorsal cortex) and bicortical screws in effectiveness in stabilizing distal radius fractures.12 The proposed reduction will result in the desired bicortical screw lengths but limit prominence. In addition, in the setting of dorsal comminution, the increased stability gained by bicortical fixation is minimal.
In fractures with an intact dorsal cortex, standard depth gauges will likely produce appropriate screw length measurements. However, even in this situation, and based on the results reported by Wall and colleagues,12 subtraction of 1 to 2 mm may prove prudent. In cases in which the dorsal cortex is comminuted and screw estimates based on fluoroscopy are used, the lateral image may provide estimates that lead to screw prominence. A 45° supinated view should be used to check screw length for the radial side, the column most at risk. However, comminution may also obscure this view. We cannot comment on that, as the present study did not create comminuted fractures of the distal radius. In addition, the ulnar column posed a lesser but real risk of screw prominence, which must also be accounted for, and typically is not appreciated with alternate views.
Last, use of live fluoroscopy instead of standard anteroposterior and lateral views may prove valuable in assessing hardware placement and screw length in the setting of a comminuted distal radius fracture. Through use of live fluoroscopy, prominent screws, especially those on the radial side, may be identified, and potential tendon injury may be avoided. Keeping in mind the shape of the dorsal aspect of the distal radius should assist surgeons in preventing screw prominence dorsally and limit complications.
Distal radius fractures constitute 15% of all extremity fractures and are the most common upper extremity fractures.1-3 The incidence of distal radius fractures is continuing to escalate because of the expanding elderly population and concurrent increase in osteoporosis.3,4 In addition, open reduction and internal fixation with a volar locking plate for distal radius fractures are more commonly being performed by general orthopedists, who may not perform these surgeries frequently. Surgically treated patients experience less time immobilized and have a higher chance of regaining previous functional status.2 In a commonly used technique, volar fixed-angle plating is used to stabilize the distal radius. With the rising popularity of this method, more patients are having postoperative complications.1,3,5,6 Extensor tendon irritation and attritional rupture constitute up to 50% of all complications stemming from volar plating of the distal radius.1
Volar plate fixation of the distal radius was originally designed to decrease postoperative tendon complications by preventing the flexor and extensor tendons from coming into direct contact with the surgically placed plates and/or screws.1 This technique places the volar plate under the belly of the pronator quadratus muscle. Shielding the flexor tendons, the pronator quadratus can prevent the volar plate from causing flexor tendon attrition. This shielding does not occur on the dorsal side of the wrist because the extensor tendons are in full contact with the dorsal radius. As such, volar fixation gained in popularity on the premise of preventing extensor tendon complications by directly avoiding the dorsal compartment.1,7
The most common complication of volar plating ironically involves the dorsal compartment.1,7 The typical distal radius fracture occurs when a fall on an outstretched hand results in significant dorsal comminution. In these cases, it can be difficult to judge the appropriate screw length, as the depth gauge does not have an intact cortex to hook. There is the temptation to use intraoperative fluoroscopy and the depth gauge to estimate screw lengths at the distal radius, especially in cases in which a surgeon may not perform this type of surgery often. More specifically, use of a lateral image to gauge the appropriate length for screws may be tempting, but a false estimate is possible.
Screw prominence on the dorsal cortex may be caused by the complex geometry of the distal radius. This geometry is produced by the Lister tubercle and its adjacent groove for the extensor pollicis longus.7 The dorsal shape of the distal radius is a dome or dihedral with the thickest part at the Lister tubercle. The dihedral shape may hide possible dorsal screw prominence on a lateral radiograph, but screw prominence can be appreciated with computed tomography (CT) (Figures 1, 2).
We conducted a study to determine if and where screw prominence occurs, and in what amount, to establish general guidelines for screw depth based on lateral radiographs. We also wanted to be able to highlight the potential source of postoperative complications.
Materials and Methods
Twelve preserved cadaveric forearms were used for this study. Two sets of arms were paired, and the other arms came from different cadavers. In total, 5 male arms (3 left, 2 right) and 7 female arms (5 left, 2 right) were used.
The arms were harvested using a bone saw to cut through the humerus just proximal to the epicondyles, keeping the ulna and radius completely intact. Each arm was examined by the naked eye and by fluoroscopy to determine if any significant anatomical or traumatic variations in the distal radius were present. None showed any abnormal variation.
The flexor tendons and volar structures were removed to allow easy visualization and access to the distal radius. The volar locking plates (Precise SD; Small Bone Innovations) were positioned to the best anatomical and radiographic fit and secured with a proximal and distal Kirschner wire (Figure 3). A single cortical screw was placed through the shaft for compression. All 7 distal holes were drilled bicortically using an appropriately sized 2.0-mm drill and the standard block drill guide. A depth gauge was used in concordance with fluoroscopy to estimate the distance between cortices and appropriate screw lengths for each hole. A standard lateral view was used to determine the depth based on aligning the depth gauge at the dorsal cortex. The hook was not used to hook the dorsal cortex, as typically the dorsal cortex is severely comminuted and unavailable for measurement. Next, all 7 locking screws of premeasured length were secured into their respective holes. Anteroposterior, lateral, and oblique (forearm supinated and pronated 45°) radiographs were obtained to visualize screw placement and possible dorsal screw prominence (Figures 4-6).8 The extensor tendons and dorsal structures were then dissected away to expose any violation of the dorsal compartments, and calipers were used to measure absolute dorsal screw prominence and the depth of the Lister tubercle (Figure 7).
Mean (SD) dorsal prominence at each screw position was calculated. The screws were also categorized into radial (1,4), central (2,5), and ulnar (3,6,7) groups based on location within the plate (Figure 3). Equality of means testing was performed using a 1-way analysis of variance followed by a Bonferroni test.
Results
Mean (SD) dorsal prominence in millimeters is listed in Table 1. Positions 1 and 4 had significantly more dorsal prominence than the other 5 screw positions (P < .01 for all comparisons). Mean (SD) dorsal prominence based on grouped screw positions is listed in Table 2. There was significantly more dorsal prominence in the radial group that in the central group (P < .001) and ulnar group (P < .001). Mean depth of the Lister tubercle was 3.25 mm.
All prominent screws in the radial aspect of the radius were detected using a supinated 45° view. A 45° pronated view was not successful in demonstrating screw prominence on the ulnar side of the wrist because of overlap of the ulnar head.
Discussion
Extensor tendon irritation and extensor tendon rupture are frequent yet preventable complications of using volar plating systems to stabilize distal radius fractures. Many recent studies have investigated the intraoperative methodologies in order to identify real-time adjustments the surgeon can make to prevent negative outcomes. The first report of extensor tendon injury caused by volar plate fixation (published in 1989) was attributed to dorsal screw prominence.9,10 Even today, extensor tendon complications remain a challenge, as screw prominence is difficult to ascertain even with multiple intraoperative radiologic views.1,8
This study simulated real-time radiographic views to estimate if screws had extended into the dorsal compartment. These radiographic predictions were then correlated with the absolute dorsal screw prominence seen after dorsal compartment dissection. We determined that the supinated oblique view was the best imaging view for identifying radial styloid screw prominence.
Mean depth of the Lister tubercle was 3.25 mm (similar to previously reported 2 mm11). However, there was no correlation identified between depth of the Lister tubercle and amount of dorsal screw prominence.
We wanted to identify high-risk areas and estimate expected dorsal screw prominence in order to make appropriate intraoperative screw length adjustments. The radius is divided into radial, central, and ulnar columns. The central screw positions had the least dorsal screw prominence (mean, 0.50 mm). This central position was considered low-risk. Both the radial and the ulnar screw positions had more dorsal screw prominence (means, 3.38 mm and 1.03 mm, respectively). Only the radial screws had significantly more prominence. However, this study was not powered to detect a difference as small as that between the central and ulnar screw positions. Despite the lack of statistical significance, it is clear from the data that the ulnar screws trend toward more dorsal prominence, and, therefore, screw measurements at both the radial and ulnar screw locations (using the depth gauge) require adjustments.
Extensor tendon contact was difficult to determine based on any specific screw length, as the extensor tendon had to be dissected to determine prominence. Based on observations, a prominence of 2 mm seemed to present a risk for tendon irritation. The periosteum and the rounded end of the screw may obviate the risk with 1 mm of prominence. However, this observation may not hold true in an in vivo situation.
This study had several limitations. First, only a single brand of plate was used, making these findings specific to this system. However, concepts and conclusions can be extrapolated to all systems. The radial side had the highest risk for prominence, and this factor should be accounted for when selecting screw lengths. In addition, the ulnar column also poses some risk, but not to the degree of the radial column. Another limitation is that fractures were not created in these radii; therefore, dorsal comminution was not recreated. In some cases, the dorsal cortex may be displaced dorsally and be somewhat protective. This study is not meant to be an exhaustive study on all volar plates or provide absolute recommendations. It is meant to suggest caution to surgeons who may not be familiar with the complex anatomy of the dorsal radius and to identify areas where the risk for screw penetration is highest.
Shortening screw lengths at the positions described may trigger surgeons’ concerns about stabilizing distal radius fractures. In a 2012 biomechanical study, Wall and colleagues12 found no difference between unicortical screws (placed at 75% of the distance to the dorsal cortex) and bicortical screws in effectiveness in stabilizing distal radius fractures.12 The proposed reduction will result in the desired bicortical screw lengths but limit prominence. In addition, in the setting of dorsal comminution, the increased stability gained by bicortical fixation is minimal.
In fractures with an intact dorsal cortex, standard depth gauges will likely produce appropriate screw length measurements. However, even in this situation, and based on the results reported by Wall and colleagues,12 subtraction of 1 to 2 mm may prove prudent. In cases in which the dorsal cortex is comminuted and screw estimates based on fluoroscopy are used, the lateral image may provide estimates that lead to screw prominence. A 45° supinated view should be used to check screw length for the radial side, the column most at risk. However, comminution may also obscure this view. We cannot comment on that, as the present study did not create comminuted fractures of the distal radius. In addition, the ulnar column posed a lesser but real risk of screw prominence, which must also be accounted for, and typically is not appreciated with alternate views.
Last, use of live fluoroscopy instead of standard anteroposterior and lateral views may prove valuable in assessing hardware placement and screw length in the setting of a comminuted distal radius fracture. Through use of live fluoroscopy, prominent screws, especially those on the radial side, may be identified, and potential tendon injury may be avoided. Keeping in mind the shape of the dorsal aspect of the distal radius should assist surgeons in preventing screw prominence dorsally and limit complications.
1. Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand. 2007;2(3):144-150.
2. Nana AD, Joshi A, Lichtman DM. Plating of the distal radius. J Am Acad Orthop Surg. 2005;13(3):159-171.
3. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29(1):96-102.
4. Protopsaltis TS, Ruch DS. Volar approach to distal radius fractures. J Hand Surg. 2008;33(6):958-965.
5. Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90(9):1855-1861.
6. Gruber G, Zacherl M, Giessauf C, et al. Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am. 2010;92(5):1170-1178.
7. Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of Lister’s tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg. 2008;33(10):1716-1719.
8. Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg. 2012;37(5):963-967.
9. Perry DC, Machin DM, Casaletto JA, Brown DJ. Minimising the risk of extensor pollicis longus rupture following volar plate fixation of distal radius fractures: a cadaveric study. Ann R Coll Surg Engl. 2011;93(1):57-60.
10. Wong-Chung J, Quinlan W. Rupture of extensor pollicis longus following fixation of a distal radius fracture. Injury. 1989;20(6):375-376.
11. Park DH, Goldie BS. Volar plating for distal radius fractures—do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg. 2012;16(3):169-172.
12. Wall LB, Brodt MD, Silva MJ, Boyer MI, Calfee RP. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg. 2012;37(3):446-453.
1. Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand. 2007;2(3):144-150.
2. Nana AD, Joshi A, Lichtman DM. Plating of the distal radius. J Am Acad Orthop Surg. 2005;13(3):159-171.
3. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29(1):96-102.
4. Protopsaltis TS, Ruch DS. Volar approach to distal radius fractures. J Hand Surg. 2008;33(6):958-965.
5. Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90(9):1855-1861.
6. Gruber G, Zacherl M, Giessauf C, et al. Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am. 2010;92(5):1170-1178.
7. Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of Lister’s tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg. 2008;33(10):1716-1719.
8. Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg. 2012;37(5):963-967.
9. Perry DC, Machin DM, Casaletto JA, Brown DJ. Minimising the risk of extensor pollicis longus rupture following volar plate fixation of distal radius fractures: a cadaveric study. Ann R Coll Surg Engl. 2011;93(1):57-60.
10. Wong-Chung J, Quinlan W. Rupture of extensor pollicis longus following fixation of a distal radius fracture. Injury. 1989;20(6):375-376.
11. Park DH, Goldie BS. Volar plating for distal radius fractures—do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg. 2012;16(3):169-172.
12. Wall LB, Brodt MD, Silva MJ, Boyer MI, Calfee RP. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg. 2012;37(3):446-453.