User login
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
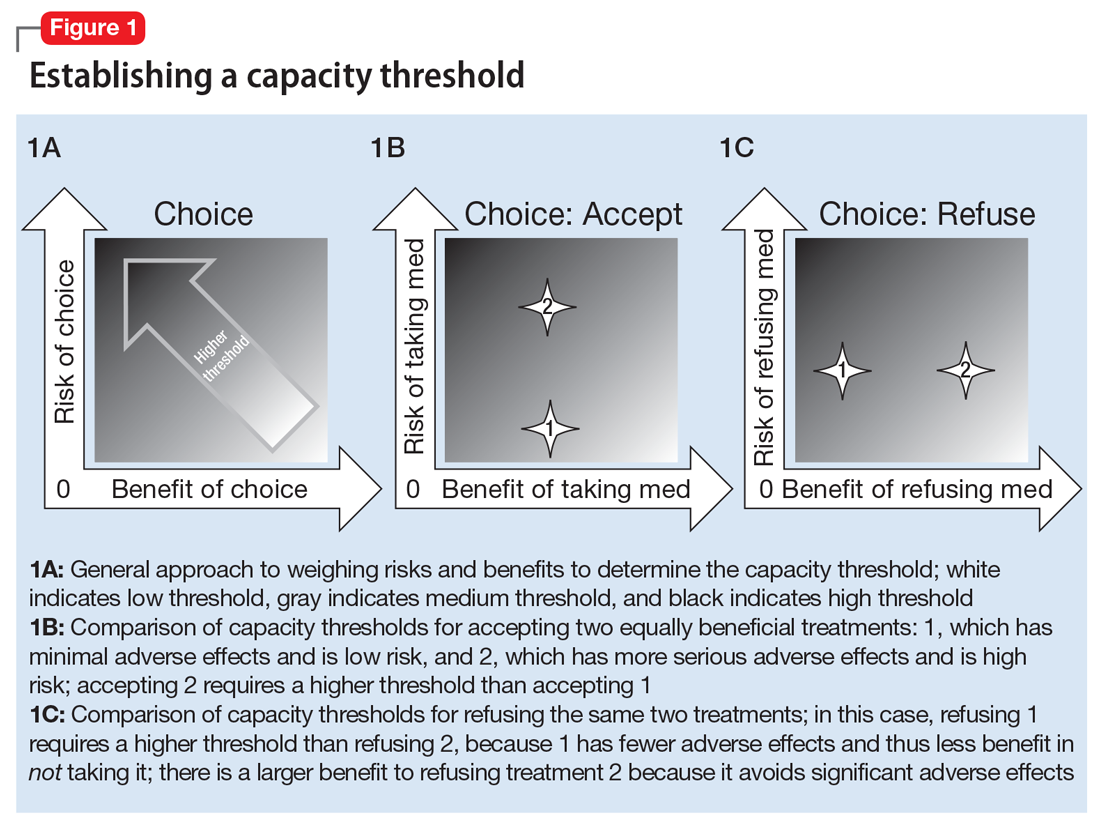
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
Leaving against medical advice
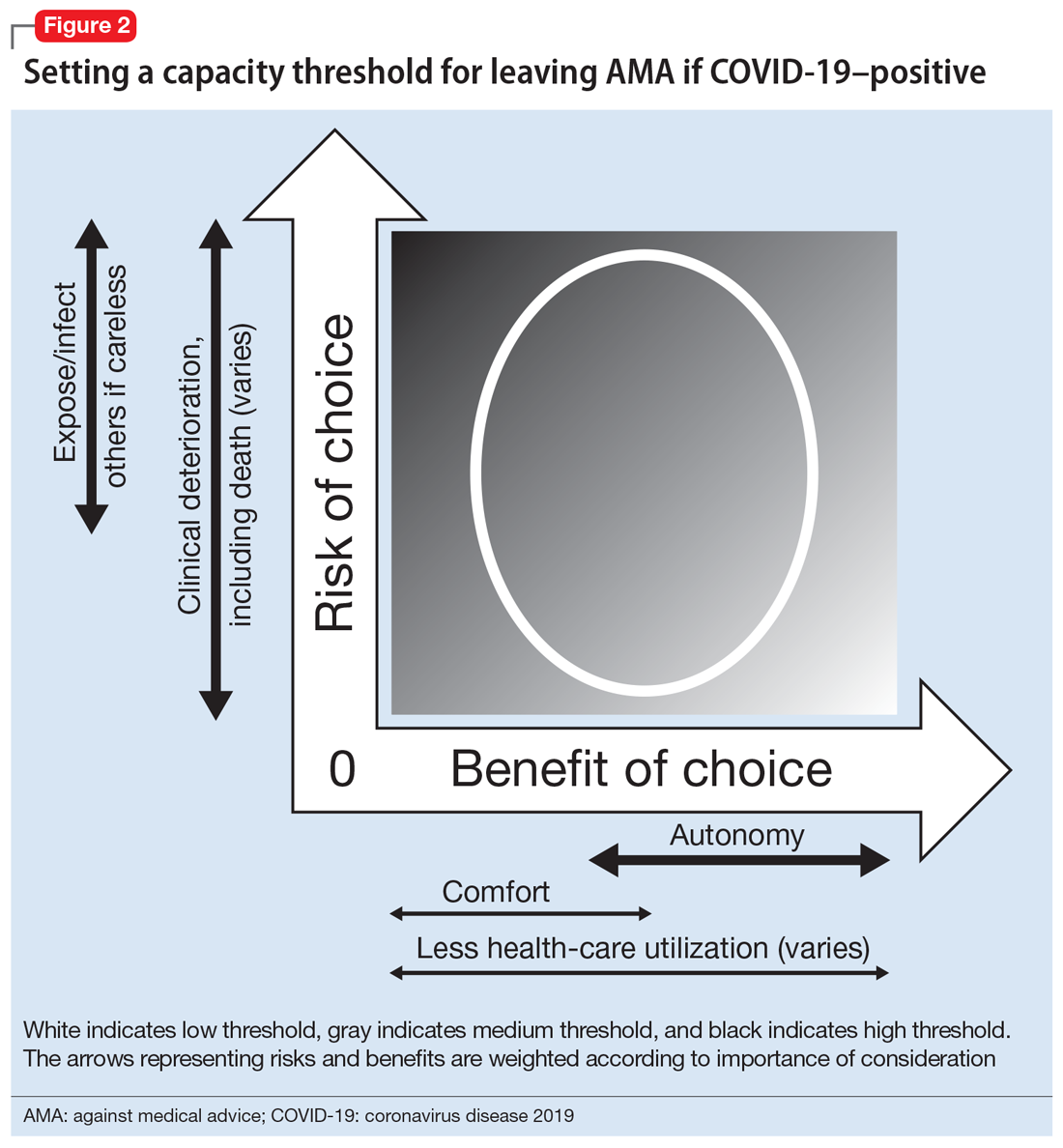
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
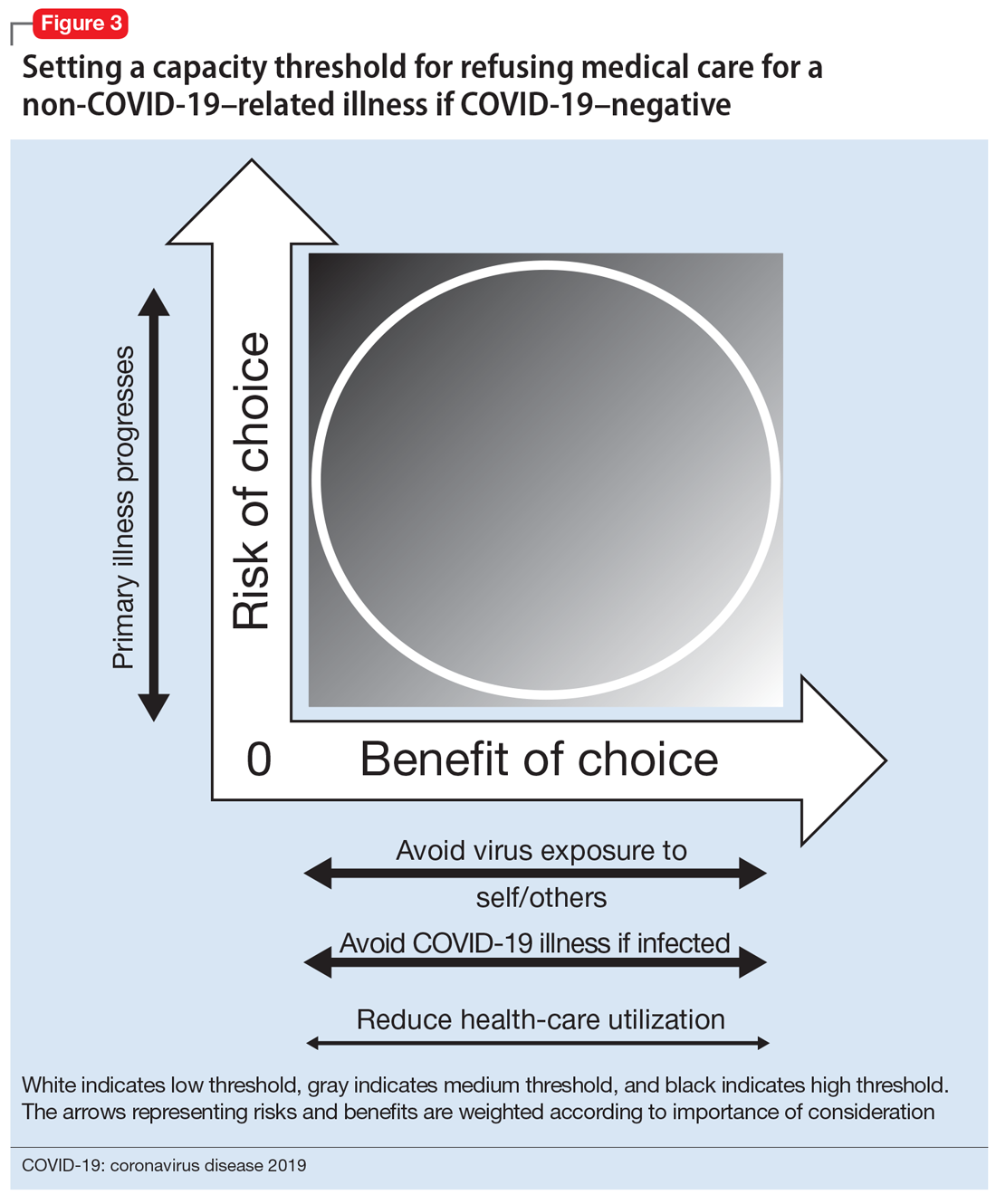
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
Leaving against medical advice
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
The coronavirus disease 2019 (COVID-19) pandemic has introduced many new clinical challenges. Consider the patient with fever and dyspnea who tests positive for COVID-19 but does not believe in COVID-19 and wants to leave the hospital against medical advice (AMA). Or the patient with numerous cardiovascular risk factors and crushing substernal chest pain who is too afraid of contracting COVID-19 to come to the emergency department. These challenging clinical scenarios can be addressed in the context of decision-making capacity (DMC), for which our medical colleagues often call upon psychiatrists to assist. This article reviews the framework for DMC assessment, describes how COVID-19 affects DMC assessment, and discusses approaches to these scenarios using the DMC framework.
Review of decision-making capacity
Assessment of DMC is a fundamental clinical skill. It allows a physician to balance autonomy with beneficence and non-maleficence. An autonomous decision is a decision that is made intentionally, with understanding, and without controlling influences (these are the elements of informed consent).1 However, if a patient cannot make a decision with intention and understanding, then beneficence and non-maleficence must prevail in order to protect the patient. Capacity assessments evaluate a patient’s ability to make an intentional and understood choice.
In order to prove capacity, a patient must demonstrate 4 functional abilities:
- choice refers to the ability to communicate a relatively stable choice2,3
- understanding refers to the ability to convey information about the illness, risks/benefits of the chosen intervention, and risks/benefits of alternative options.2,3 Understanding measures objective information about the medical situation
- appreciation refers to the patient’s ability to apply that information to his/her own life.2,3 Appreciation requires insight into having the illness and the ability to anticipate how one’s life would be impacted by one’s condition and choice. This is where life experiences and values come into play
- reasoning is intimately tied to appreciation. It refers to the ability to explain how the decision was made and which factors were most important.2,3
Most clinicians and ethicists endorse a “threshold” approach to decisional capacity, which specifies that the level of evidence required to prove capacity depends on the gravity of the medical situation (Figure 1A).1,4,5 The gravity of the situation is based on the risk/benefit analysis. Consider two treatments with equal benefit: one has minimal adverse effects (gastrointestinal upset) and the second has significant adverse effects (myelosuppression). Accepting the first treatment requires less intentionality and understanding than accepting the second because the risk is much lower and thus has a lower capacity threshold (Figure 1B). The capacity to refuse these treatments results in the opposite ranking (Figure 1C).
Establishing a threshold helps guide the physician in determining how robust the patient’s responses must be to have decisional capacity. For a high-threshold decision, the patient must have a well-developed and highly detailed level of understanding, appreciation, and reasoning.
How COVID-19 affects assessment of decision-making capacity
Three characteristics of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19 illness impact decision-making assessment:
- high level of contagiousness
- high health-care utilization
- the uncertainty about its clinical course and outcomes.
The high level of contagiousness stems from this virus’s estimated basic reproduction number (R0) of 2.2 to 5.7 (which indicates the expected number of cases from any single case), its long incubation period, and the potential for asymptomatic and pre-symptomatic shedding.6-9 Decision-making capacity assessments must therefore consider community-level effects in the risk/benefit analysis. Because SARS-CoV-2 is a new virus affecting humans, it can easily overwhelm existing hospital systems. This happened in Wuhan, China; Lombardy, Italy; and New York. In a stressed system, physicians will have to factor health-care utilization into the risk/benefit analysis. Finally, because this is a novel virus, there is still considerable uncertainty about the epidemiology, clinical course, and outcomes.10 The minimal dose of virus needed to cause illness is unknown. Patients can deteriorate quickly and unpredictably into needing ventilator support.11 Treatment options are limited, and many candidates are being investigated.12 This uncertainty hinders physicians’ ability to accurately estimate risks and benefits for an individual patient when discussing various medical decisions. As our understanding of SARS-CoV-2 improves, this uncertainty will lessen.
Continue to: Effects of the sociopolitical climate
Effects of the sociopolitical climate
In the United States, the COVID-19 pandemic emerged during a time of deep sociopolitical divide. Accordingly, beliefs about viral infectivity, severity of illness, and precautionary measures have varied. Some politicians, media outlets, and physicians have shared information that contradicts guidelines and recommendations from mainstream national and international medical and scientific organizations. Patients who subscribe to these reports and beliefs may not meet the threshold for understanding, appreciation, or reasoning. For example, if a patient’s beliefs about the virus depart from well-established medical evidence, they would technically lack understanding. The usual remedy for addressing misunderstanding is education and time. However, because of the divisiveness of the sociopolitical climate, the limited time physicians have with patients, and the fact that many DMC assessments will occur in acute-care settings, it may be difficult or near impossible to correct the misunderstanding.
The sociopolitical climate and its accompanying potentially erroneous or imbalanced narrative may thus directly impact patients’ understanding, appreciation, and reasoning. However, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. Additionally, some clinicians and ethicists might object to declaring incapacity in a patient with no underlying mental or neurologic dysfunction. The United States has a functional approach to capacity, based solely on meeting criteria for the 4 functional abilities.3,13 Mental or neurologic dysfunction is not legally required in the United States, but in practice, the consideration of incapacity is often closely linked to some form of cognitive impairment.14 Other countries do make dysfunction a specific criterion; for example, the United Kingdom dictates that mental incapacity can only occur in someone with “impairment of, or a disturbance in the functioning of, the mind or brain.”15
Leaving against medical advice
In the case of a patient who is COVID-19–positive, symptomatic, and wants to leave AMA, the threshold is automatically elevated because of societal-level risks (the risk of potential exposure or infection of others if a patient who is COVID-19–positive is not properly isolated). Furthermore, the individual risk of the patient leaving AMA depends on his/her age, comorbidities, and current clinical status; because of the uncertainty and rapid deterioration seen with COVID-19 illness, the calculated risk may actually be higher than for a non-COVID-19–related illness. Thus, in order to leave AMA, the patient’s responses must be fairly robust (Figure 2). Table 1 describes the information needed for robust understanding, appreciation, and reasoning.
For patients who do not meet this threshold, it is important to determine why. If a patient has a psychiatric condition that not only impacts DMC but also meets criteria for a psychiatric hold (ie, an imminent risk of harm to self or others), a psychiatric hold should be placed. If the patient does not meet the threshold because of altered mental status or some other neurologic or cognitive comorbidity, a medical hold should be placed. Most states do not have an explicit legal basis for a medical hold, although it does fall under the incapacity laws in the United States; in the absence of a surrogate, declaration of medical emergency can also be used if applicable.16,17 As a caveat, it can be difficult to detain someone on a medical hold because security officers may be afraid to physically detain someone without explicit legal paperwork.17
If a patient does not meet the capacity threshold but there does not seem to be a psychiatric, neurologic, or cognitive explanation, several options are possible. The first step would be to assess whether the patient is amenable to further discussion and compromise. A nonjudgmental and nonconfrontational approach that aims to further clarify the patient’s perspective and identify shared goals is key. Any plan that lowers the risks sufficiently would allow the patient to leave by lowering the capacity threshold. Enlisting the support of family and friends can be helpful. If this does not work, theoretically the patient should be detained in the hospital. Practically speaking, this may be difficult or unadvised. First, as described above, security officers may refuse to physically detain the patient.17 Second, the patient’s legally mandated surrogate may espouse similar COVID-related views as the patient; thus, this approach may not help keep the patient in the hospital. If the physician has serious concern about the risk of the patient leaving, he/she would have to consult the facility’s Ethics and Legal staff to determine capacity of the surrogate. Third, it can be problematic to declare incapacity in a patient whose understanding, appreciation, and reasoning arise from widely shared and relatively fixed sociopolitical values. In the current sociopolitical climate, involuntary detention may elicit a political backlash. Using medical detention for impending deterioration of clinical status would be more acceptable than using medical detention for isolation. Presently, there are no such laws for patients with COVID-19 (although this is not without precedent, as with active tuberculosis or Ebola18,19), but individual jurisdictions may have isolation or quarantine orders; the local health department could be contacted and may evaluate on a case-by-case basis.
Continue to: Refusing to seek medical care
Refusing to seek medical care
Anecdotally, many physicians have reported an increase in patients who are refusing clinic- or hospital-based treatment for a medical condition because they fear they may catch the virus. Although this is not strictly a capacity case—there is little recourse for action if a patient is refusing treatment from home (unless the patient requires a psychiatric hold or already has a guardian for medical decisions)—the same elements of thresholds apply and can be helpful in guiding conversations with the patient.
For the patient, the benefits of staying at home are to avoid potentially exposing themselves and the members of their household to the virus and COVID-19 illness. The risks of staying home include progression of the patient’s primary illness, which could lead to increased morbidity and mortality. Staying home has an ancillary benefit to the community of reducing health-care utilization, but at the risk of increasing utilization in the future.
The risk/benefit profile is shown on the thresholds graph in Figure 3. There is considerable variability. It is helpful to stratify the risk of progression of the primary condition as low (can be postponed indefinitely with minimal risk), medium (can be postponed for a short amount of time; risk of increased morbidity with ongoing delay and possibly increased mortality), or high (cannot be postponed; will have greater morbidity and/or higher risk of mortality). Because of the uncertainty about COVID-19, it is harder to quantify the benefits of refusing care and staying at home, although older patients and patients with underlying health issues are at higher risk of severe illness and death.20 However, by taking appropriate precautions when seeking care, viral exposure and risk of infection can be mitigated.
This risk/benefit analysis will help set the threshold for whether staying at home is reasonable or whether it would incur more risk of harm. If the latter, then the physician must elicit the patient’s understanding, appreciation, and reasoning related to their current medical condition and COVID-19. It is likely they are undervaluing the former and overvaluing the latter. Table 2 lists important points to cover during these discussions.
Although there is no legal recourse to force patients at home to come to the clinic or hospital for medical treatment, there are several possible strategies to motivate them to do so. One is to ask patients how likely (on a scale of 0 to 100) they think they are to contract COVID-19 if they came for evaluation/treatment, and how likely they feel they are to experience a bad outcome from their primary condition. Then, after providing psychoeducation about their primary medical condition and COVID-19–related precautions and risk, repeat this question. Another strategy is to empathize with the patient’s fears while also expressing concern about the primary medical condition and connecting with the patient on the shared desire to protect his/her health. A third is to draw a risk/benefit diagram (similar to Figure 3) or reassure the patient by describing the ways in which the clinic or hospital is minimizing exposure and infection risk. A final strategy is to enlist the help of the patient’s family or friends.
Continue to: Bottom Line
Bottom Line
In order to have decision-making capacity, a patient must demonstrate choice, understanding, appreciation, and reasoning. The degree of understanding, appreciation, and reasoning required depends on the capacity threshold, which is determined by a risk/benefit analysis. Conducting a risk/benefit analysis during the coronavirus disease 2019 (COVID-19) pandemic requires consideration of societallevel factors (such as contagiousness to others and health-care utilization) and is complicated by a wide range of uncertainties and divisive sociopolitical views regarding COVID-19.
Related Resources
- Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
- Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
Acknowledgments
The author thanks Drs. Awais Aftab, Zackary D. Berger, and R. Brett Lloyd for their helpful discussions on the topic.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.
1. Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2013.
2. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
3. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
4. Magid M, Dodd ML, Bostwick MJ, et al. Is your patient making the ‘wrong’ treatment choice? Current Psychiatry. 2006;5(3):13-20.
5. Ryznar E, Hamaoka D, Lloyd RB. Capacity evaluations. Association of Directors of Medical Student Education in Psychiatry. 2020. https://admsep.org/csi-emodules.php?c=capacity&v=y. Accessed March 30, 2020.
6. Sanche S, Lin YT, Xu C, et al. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477.
7. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207.
8. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469.
9. Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180.
10. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 — studies needed. N Engl J Med. 2020;382(13):1194-1196.
11. Goh KJ, Choong MC, Cheong EH, et al. Rapid progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore. 2020;49(3):108-118.
12. Asai A, Konno M, Ozaki M, et al. COVID-19 drug discovery using intensive approaches. Int J Mol Sci. 2020;21(8):2839.
13. Siegel AM, Barnwell AS, Sisti DA. Assessing decision-making capacity: a primer for the development of hospital practice guidelines. HEC Forum. 2014;26(2):159-168.
14. Karlawish J. Assessment of decision-making capacity in adults. UpToDate. https://www.uptodate.com/contents/assessment-of-decision-making-capacity-in-adults. Updated February 24, 2020. Accessed May 27, 2020.
15. Mental Capacity Act 2005. Chapter 9. http://www.legislation.gov.uk/ukpga/2005/9/part/1. Accessed May 27, 2020.
16. Kersten C. The doctor as jailer: medical detention of non-psychiatric patients. J Law Biosci. 2019;6(1):310-316.
17. Cheung EH, Heldt J, Strouse T, et al. The medical incapacity hold: a policy on the involuntary medical hospitalization of patients who lack decisional capacity. Psychosomatics. 2018;59(2):169-176.
18. Parmet WE, Sinha MS. Covid-19 - the law and limits of quarantine. N Engl J Med. 2020;382(15):e28.
19. Coker R, Thomas M, Lock K, et al. Detention and the evolving threat of tuberculosis: evidence, ethics, and law. J Law Med Ethics. 2007;35(4):609-615.
20. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458-464.