User login
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.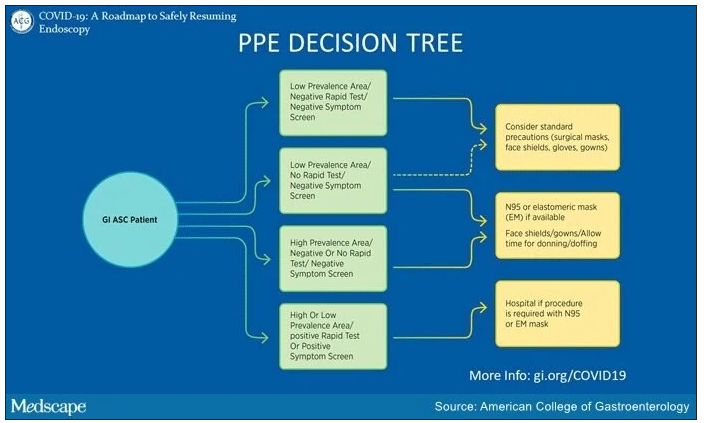
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.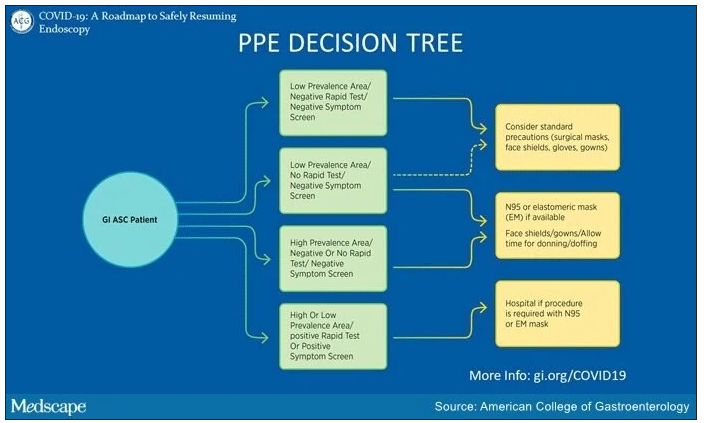
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.
Gastroenterologists can safely return to elective procedures when adequate personal protective equipment (PPE) is available, professional societies say.
Noting that some states have already lifted restrictions imposed to guard against COVID-19, the American Gastroenterological Association (AGA) and the Digestive Health Physicians Association (DHPA) on April 27 announced guidelines for resuming procedures delayed by the pandemic.
“Gastroenterologists are looking for some framework, however fluid it might be, to guide them in the next 2 to 4 weeks,” Paul Berggreen, MD, secretary of the DHPA, told Medscape Medical News.
The AGA and DHPA guidelines envision a return to elective procedures in areas where COVID-19 cases have been declining for at least 2 weeks and where they are permitted by government directives.
Decisions hinge on the availability of testing, Berggreen said. The guidelines recommend polymerase chain reaction (PCR) tests for COVID-19 infections prior to elective endoscopy. When these tests are not available, a daily temperature log for 10 days prior to the procedure may substitute, they say.
However, if no PCR test is done, the guidelines call on all procedure room personnel to use N95 masks or the equivalent. If these masks aren’t available, “consider delaying resumption of endoscopic procedures,” the guidelines say. The procedure should also be postponed or moved to an inpatient setting in the event of a positive test, according to the guidelines.
Only if the patient has a negative test result should the procedure go forward with the use of standard surgical masks rather than N95 masks or the equivalent, the guidelines say.
The mask recommendations differ slightly from a decision tree put forward during an American College of Gastroenterology (ACG) webinar on April 27, ACG President Mark Pochapin, MD, told Medscape Medical News.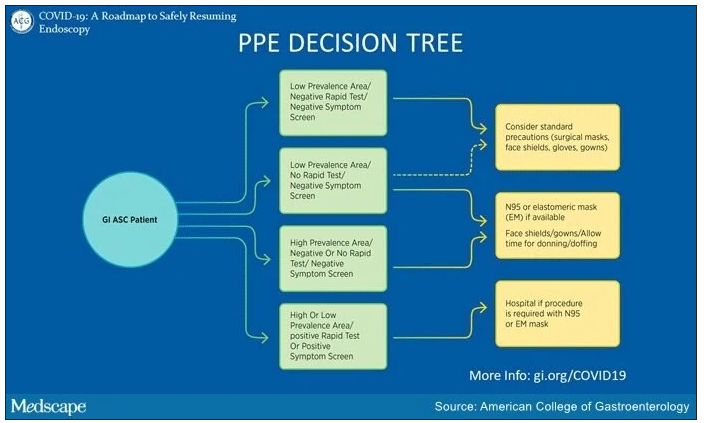
The ACG decision tree takes into consideration local prevalence of COVID-19. “In a low prevalence area if you have a negative test you can wear a regular surgical mask if the patient wears a surgical mask,” Pochapin said.
The ACG decision tree also envisions the possibility of endoscopy with surgical masks along with face shields in areas with low prevalence of COVID-19, even in the absence of testing, if a patient doesn’t have symptoms.
In contrast, the ACG decision tree calls for N95 or elastomeric masks in areas of high prevalence even with a negative test and a negative symptom screen. And it calls for a hospital procedure with an N95 or elastomeric mask in patients with either a positive symptom screen or a positive test.
In addition to masks, the AGA and DHPA guidelines recommend use of other PPE, such as water-resistant gowns, shoe covers, scrubs, double-gloving, and surgical head coverings.
They recommend daily screening of endoscopy center staff with temperature checks and surveys of COVID-19 symptoms and exposure.
Moreover, they call for social distancing of patients, visitors, and staff, and high-level disinfection of endoscopes. They recommend against endotracheal intubation of patients undergoing elective upper endoscopy.
The number of states allowing elective procedures is changing by the day, Berggreen said. In Arizona, where he practices, Gov. Doug Ducey removed all restrictions on elective procedures starting May 1. But other states, where caseloads have been higher, including New York and Massachusetts, have yet to follow suit.
“We are still in kind of a holding pattern,” Richard Hodin, MD, AGAF, chief of gastrointestinal surgery at Massachusetts General Hospital in Boston, told Medscape Medical News. Currently his facility is only doing procedures when a patient’s life is in danger.
The availability of testing also ranges widely from one practice to another. New York University, where Pochapin is director of gastroenterology, is able to do its own tests. Berggreen’s practice, Arizona Digestive Health in Phoenix, has assigned staff to swab patients in its parking lot and then send the samples to a lab by courier for analysis.
Berggreen said his practice has been essentially closed for the past month. In May, he expects his team will do about 30% of its normal volume. They will not start with purely elective procedures, such as following up on a polyp, but with semi-urgent cases, said Berggreen.
“Elective procedures can still be delayed a little bit longer,” he said. “But we’re trying to take care of our patients that are not purely elective: somebody with abdominal pain that you think is very likely a stomach ulcer, somebody with rectal bleeding or persistent diarrhea that›s really impacting their life and you›re thinking this could be an inflammatory condition of the colon.»
Berggreen said he is reassured by a recent survey of 968 healthcare workers in Northern Italy who conducted gastrointestinal endoscopy there during the COVID-19 outbreak. Only 4.3% of respondents tested positive for COVID-19, and 85.7% of these infections occurred before the introduction of PPE and measures to reduce cases. Results were similarly encouraging for patients.
Providing more endoscopy will relieve many patients, Berggreen said. “We all understand the need to limit the spread of the coronavirus but we also have patients who are going to start to have more struggles and potentially worse outcomes by sitting on a condition that requires endoscopy to diagnose and appropriately manage.”
Neither Berggreen, Pochapin, nor Hodin reported any relevant financial interests. The authors of the survey did not report a source of funding or any relevant financial interests.
This article first appeared on Medscape.com.