User login
Body mass index (BMI) is thought to be a predictor of body composition, with higher values indicating more adipose tissue. BMI is a measure of mass with respect to height. The World Health Organization1 has established health categories based on BMI measurements. Values from 18.5 to 24.9 kg/m2 are deemed to represent normal weight; those from 25 to 30 kg/m2, overweight; and those higher than 30 kg/m2, obesity. BMI is not a perfect tool, but it is the most widely used tool in clinical and research practice because of its relative reliability and ease of use.2 Being overweight or obese (according to BMI) is increasingly common among adults worldwide, and particularly in the United States. An estimated 39% of adults worldwide are overweight, and 13% are obese.1 An estimated 69% of US adults are overweight, including 35.1% who are obese.2
Various pathologies have been treated with reverse shoulder arthroplasty (RSA), and results have been promising,3-9 but little is known about patient demographic and clinical factors that may adversely affect outcomes. Recent work suggests younger age7 and failed prior arthroplasty may adversely affect RSA outcomes.10 Higher BMI has also been implicated as a cause of increased perioperative and immediate postoperative complications of RSA with minimum 90-day follow-up, but no one has examined shoulder function scores at minimum 2-year follow-up.11,12
We conducted a study to examine shoulder function scores, mobility, patient satisfaction, and complications at minimum 2-year follow-up in normal-weight, overweight, and obese patients who underwent RSA. We hypothesized that, compared with normal-weight patients, obese patients would have worse shoulder function scores, worse mobility, and more complications.
Materials and Methods
Inclusion Criteria and Demographics
After obtaining Institutional Review Board approval for this study, we used a prospective shoulder arthroplasty registry to identify patients (N = 77) who had rotator cuff tear arthropathy (RCTA) treated with primary RSA and then had minimum 2-year follow-up. The study period was 2004-2011. All patients had RCTA diagnosed with physical examination findings and anteroposterior, scapular Y, and axillary radiographs. RCTA was graded 1 to 5 using the classification system of Hamada and colleagues.13 Rotator cuff status was determined with preoperative computed tomography arthrogram (CTA) or magnetic resonance imaging (MRI) and confirmed at time of surgery. BMI calculations were based on height and weight measured at initial office visit. Thirty-four patients had normal weight (BMI <25 kg/m2), 21 were overweight (BMI 25-30 kg/m2), and 22 were obese (BMI >30 kg/m2). Patient demographic and clinical characteristics reviewed also included age, sex, follow-up duration, arm dominance, complications, prevalence of depression, and prevalence of diabetes. All RSAs were performed by the same surgeon (Dr. Edwards) at a single high-volume shoulder arthroplasty center.
Shoulder function scores evaluated before surgery and at final follow-up included Constant score,14 American Shoulder and Elbow Surgeons (ASES) score,15 Western Ontario Osteoarthritis Shoulder (WOOS) index,16 Single Assessment Numeric Evaluation (SANE),17 and mobility. Satisfaction was assessed by having patients describe themselves as very dissatisfied, dissatisfied, satisfied, or very satisfied. All intraoperative and postoperative complications were recorded.
Surgical Technique and Postoperative Rehabilitation
The Aequalis RSA system (Tornier) was used for all patients during the study period. The RSA technique used has been well described.18,19 A standard postoperative rehabilitation protocol was followed.19,20
Clinical and Radiographic Assessment
Patients were prospectively enrolled in a shoulder arthroplasty outcomes registry and followed clinically. Mean follow-up was 3.16 years (range, 2-8 years). Before surgery, patients were examined by the surgeon. Examinations were repeated 1 week, 6 weeks, 3 months, 6 months, and 12 months after surgery and annually thereafter. Mobility (active range of motion) was determined with a handheld goniometer. Strength of abduction was measured with a handheld digital dynamometer (Chatillon digital force gauge, 200 lbf; Ametek). Anteroposterior in plane of scapula, scapular Y, and axillary radiographs were obtained at each clinic appointment.
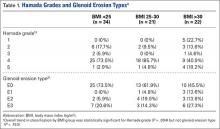
Before surgery, the surgeon reviewed all radiographs. Each RCTA was given a Hamada grade (1-5).13 Glenoid erosion in the coronal plane was classified (E0, E1, E2, E3) according to Sirveaux and colleagues.21 Hamada grades and glenoid erosion types are listed in Table 1. The overall trend in classification by BMI group was statistically significant for Hamada grade (P = .004) but not glenoid erosion type (P = .153).
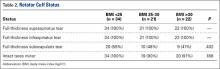
Before surgery, the surgeon also evaluated rotator cuff status using CTA or MRI. All patients had full-thickness tears of the supraspinatus and infraspinatus. The subscapularis was variably present, and subscapularis repair was performed when the subscapularis was intact. Rotator cuff status is listed in Table 2. There were no significant differences in the distribution of intact subscapularis (P = .402) or teres minor (P = .188) among the normal-weight, overweight, and obese groups. No patient had a latissimus dorsi transfer at time of RSA.
Statistical Analysis
Independent-samples t tests assuming unequal variances were used to compare the 3 BMI groups on age, follow-up duration, preoperative shoulder function scores, and mobility. Chi-square tests were used to identify any significant group differences in comorbidities (eg, complications, arm dominance, prevalence of depression, prevalence of diabetes) and patient satisfaction. Repeated-measures analysis of variance was used to evaluate main effects, changes from before surgery to final follow-up, and BMI group differences, as well as differences in changes from before surgery to final follow-up among the 3 BMI groups.
Results
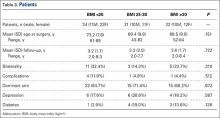
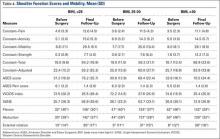
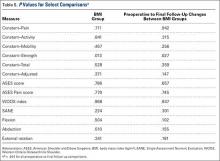
Among BMI groups (<25 kg/m2, 25-30 kg/m2, >30 kg/m2), there were no statistically significant preoperative differences in age, sex, follow-up duration, complications, arm dominance, prevalence of depression, or prevalence of diabetes (P >. 05) (Table 3). Table 4 lists the groups’ preoperative and final follow-up data (Constant score, ASES score, WOOS index, SANE, mobility). There were no statistically significant preoperative group differences in Constant score, ASES score, WOOS index, SANE, mobility, or patient satisfaction (P > .05) (Tables 5, 6).
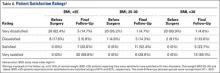
All groups’ shoulder function scores and mobility improved significantly from before surgery to final follow-up (P < .001) (Table 5). The groups’ magnitudes of change (improvement) from before surgery to final follow-up were almost identical, with no significant differences in shoulder function scores or mobility (Table 5). The only significant difference was in Constant–Strength, which was higher in the obese group (P = .017) (Table 5). Patient satisfaction ratings improved after surgery, with 79% of the normal-weight group reporting being satisfied or very satisfied with their shoulders (Table 6). The overweight and obese groups gave similar satisfied (81%) and very satisfied (82%) ratings. The small differences between group satisfaction scores were nonsignificant (P = .967).
Complications
The normal-weight group had 4 complications: periprosthetic infection (2 cases), intraoperative humeral fracture (1), and scapular spine stress fracture (1). The overweight group had 1 complication, an acromial stress fracture that was successfully treated with conservative measures. The obese group had 1 patient with 2 postoperative dislocations. The first dislocation was treated with closed reduction and bracing, and the second required revision surgery. There was no statistical difference in complications among the groups (P = .680).
Discussion
To our knowledge, this is the first study of the effects of varying BMI on functional outcomes of RSA with minimum 2-year follow-up. There appears to be minimal impact on shoulder function scores, complications, and patient satisfaction among normal-weight, overweight, and obese patients with RCTA treated by the same surgeon using similar techniques.
The relationship between obesity and increased perioperative risks or poorer surgical outcomes has been well established in orthopedic surgery. In a systematic review, Falagas and Kompoti22 found increased risk for perioperative and nosocomial infections in obese patients. Schoenfeld and colleagues23 and Jiang and colleagues24 reported increased risk for complications in spinal surgery. The total joint arthroplasty literature is rife with evidence suggesting higher BMI leads to increased risk for complications, including infection and deep venous thrombosis, as well as decreased functional outcome scores.25-29 Recent studies on shoulder surgery have shown worse outcomes in rotator cuff repair30 and a higher revision rate in hemiarthroplasy.31
Other RSA studies have examined short-term complications or perioperative risk factors associated with BMI. In a study using slightly different BMI groupings, Gupta and colleagues12 reported significantly higher complication rates for RSA patients with BMI higher than 35 kg/m2 compared to patients with BMI of 25 to 35 kg/m2 and compared to patients with BMI lower than 25 kg/m2. Their study highlighted medical and surgical complications and used a short follow-up period (minimum, 90 days). It did not assess shoulder function scores, and included multiple indications for RSA (eg, RCTA, proximal humerus fracture, inflammatory arthropathy). In another study, higher BMI was reported as a risk factor for early dislocation after RSA, but only 11 patients with a history of dislocation were assessed, and minimum follow-up was 6 months.32 We know of only one study that addressed RSA outcomes in obese patients and used minimum 2-year follow-up, but its primary endpoint was rate of complications, and it did not report shoulder function scores.11 Li and colleagues33 conducted a study similar to ours, but with primary total shoulder arthroplasty (TSA) patients, and reported similar results. Relative to normal BMI, higher BMI did not have a detrimental effect on short-term improvement in shoulder function after TSA.
Given the US obesity epidemic, our study results are encouraging. Depending on many factors, obesity remains a risk factor for poor outcomes in patients who undergo orthopedic surgery. As our results show, however, patients with higher BMI can obtain functional outcomes similar to those experienced by patients with normal-weight BMI after RSA for RCTA.
The primary limitation of this study was its retrospective design. Strengths of the study included its having a single surgeon and a single diagnosis: RCTA. In addition, each group was robust in size, a standard operative/postoperative protocol was used, and clinical results were measured with multiple validated shoulder function scores.
Conclusion
Improved shoulder function scores, mobility, and patient satisfaction can be expected after RSA for RCTA in patients with BMI higher than 30 kg/m2. These patients did not exhibit an increase in complications at short-term follow-up.
1. World Health Organization. Obesity and overweight [factsheet 311]. Updated January 2015. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed March 27, 2016.
2. National Center for Health Statistics, Centers for Disease Control and Prevention. Obesity and overweight. Updated February 25, 2016. http://www.cdc.gov/nchs/fastats/obesity-overweight.htm. Accessed March 27, 2016.
3. Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18(4):600-606.
4. Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468(6):1526-1533.
5. Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2009;17(5):284-289.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Muh SJ, Streit JJ, Wanner JP, et al. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95(20):1877-1883.
8. Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476-1485.
9. Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(20):1915-1923.
10. Boileau P, Melis B, Duperron D, Moineau G, Rumian AP, Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(10):1359-1370.
11. Beck JD, Irgit KS, Andreychik CM, Maloney PJ, Tang X, Harter GD. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013;38(5):965-970.
12. Gupta AK, Chalmers PN, Rahman Z, et al. Reverse total shoulder arthroplasty in patients of varying body mass index. J Shoulder Elbow Surg. 2014;23(1):35-42.
13. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
14. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
15. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
16. Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9(8):771-778.
17. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
18. Gartsman GM, Edwards TB. Shoulder Arthroplasty. Philadelpia, PA: Saunders Elsevier; 2008.
19. Liotard JP, Edwards TB, Padey A, Walch G, Boulahia A. Hydrotherapy rehabilitation after shoulder surgery. Tech Shoulder Elbow Surg. 2003;4:44-49.
20. Trappey GJ 4th, O’Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469(9):2505-2511.
21. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388-395.
22. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6(7):438-446.
23. Schoenfeld AJ, Carey PA, Cleveland AW 3rd, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J. 2013;13(10):1171-1179.
24. Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res. 2014;472(3):968-975.
25. Bozic KJ, Lau E, Kurtz S, et al. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Joint Surg Am. 2012;94(9):794-800.
26. Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466(11):2597-2604.
27. Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012;470(2):490-496.
28. Jämsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94(14):e101.
29. Naziri Q, Issa K, Malkani AL, Bonutti PM, Harwin SF, Mont MA. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop Relat Res. 2013;471(11):3523-3530.
30. Warrender WJ, Brown OL, Abboud JA. Outcomes of arthroscopic rotator cuff repairs in obese patients. J Shoulder Elbow Surg. 2011;20(6):961-967.
31. Singh JA, Sperling JW, Cofield RH. Risk factors for revision surgery after humeral head replacement: 1,431 shoulders over 3 decades. J Shoulder Elbow Surg. 2012;21(8):1039-1044.
32. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744.
33. Li X, Williams PN, Nguyen JT, Craig EV, Warren RF, Gulotta LV. Functional outcomes after total shoulder arthroplasty in obese patients. J Bone Joint Surg Am. 2013;95(21):e160.
Body mass index (BMI) is thought to be a predictor of body composition, with higher values indicating more adipose tissue. BMI is a measure of mass with respect to height. The World Health Organization1 has established health categories based on BMI measurements. Values from 18.5 to 24.9 kg/m2 are deemed to represent normal weight; those from 25 to 30 kg/m2, overweight; and those higher than 30 kg/m2, obesity. BMI is not a perfect tool, but it is the most widely used tool in clinical and research practice because of its relative reliability and ease of use.2 Being overweight or obese (according to BMI) is increasingly common among adults worldwide, and particularly in the United States. An estimated 39% of adults worldwide are overweight, and 13% are obese.1 An estimated 69% of US adults are overweight, including 35.1% who are obese.2
Various pathologies have been treated with reverse shoulder arthroplasty (RSA), and results have been promising,3-9 but little is known about patient demographic and clinical factors that may adversely affect outcomes. Recent work suggests younger age7 and failed prior arthroplasty may adversely affect RSA outcomes.10 Higher BMI has also been implicated as a cause of increased perioperative and immediate postoperative complications of RSA with minimum 90-day follow-up, but no one has examined shoulder function scores at minimum 2-year follow-up.11,12
We conducted a study to examine shoulder function scores, mobility, patient satisfaction, and complications at minimum 2-year follow-up in normal-weight, overweight, and obese patients who underwent RSA. We hypothesized that, compared with normal-weight patients, obese patients would have worse shoulder function scores, worse mobility, and more complications.
Materials and Methods
Inclusion Criteria and Demographics
After obtaining Institutional Review Board approval for this study, we used a prospective shoulder arthroplasty registry to identify patients (N = 77) who had rotator cuff tear arthropathy (RCTA) treated with primary RSA and then had minimum 2-year follow-up. The study period was 2004-2011. All patients had RCTA diagnosed with physical examination findings and anteroposterior, scapular Y, and axillary radiographs. RCTA was graded 1 to 5 using the classification system of Hamada and colleagues.13 Rotator cuff status was determined with preoperative computed tomography arthrogram (CTA) or magnetic resonance imaging (MRI) and confirmed at time of surgery. BMI calculations were based on height and weight measured at initial office visit. Thirty-four patients had normal weight (BMI <25 kg/m2), 21 were overweight (BMI 25-30 kg/m2), and 22 were obese (BMI >30 kg/m2). Patient demographic and clinical characteristics reviewed also included age, sex, follow-up duration, arm dominance, complications, prevalence of depression, and prevalence of diabetes. All RSAs were performed by the same surgeon (Dr. Edwards) at a single high-volume shoulder arthroplasty center.
Shoulder function scores evaluated before surgery and at final follow-up included Constant score,14 American Shoulder and Elbow Surgeons (ASES) score,15 Western Ontario Osteoarthritis Shoulder (WOOS) index,16 Single Assessment Numeric Evaluation (SANE),17 and mobility. Satisfaction was assessed by having patients describe themselves as very dissatisfied, dissatisfied, satisfied, or very satisfied. All intraoperative and postoperative complications were recorded.
Surgical Technique and Postoperative Rehabilitation
The Aequalis RSA system (Tornier) was used for all patients during the study period. The RSA technique used has been well described.18,19 A standard postoperative rehabilitation protocol was followed.19,20
Clinical and Radiographic Assessment
Patients were prospectively enrolled in a shoulder arthroplasty outcomes registry and followed clinically. Mean follow-up was 3.16 years (range, 2-8 years). Before surgery, patients were examined by the surgeon. Examinations were repeated 1 week, 6 weeks, 3 months, 6 months, and 12 months after surgery and annually thereafter. Mobility (active range of motion) was determined with a handheld goniometer. Strength of abduction was measured with a handheld digital dynamometer (Chatillon digital force gauge, 200 lbf; Ametek). Anteroposterior in plane of scapula, scapular Y, and axillary radiographs were obtained at each clinic appointment.
Before surgery, the surgeon reviewed all radiographs. Each RCTA was given a Hamada grade (1-5).13 Glenoid erosion in the coronal plane was classified (E0, E1, E2, E3) according to Sirveaux and colleagues.21 Hamada grades and glenoid erosion types are listed in Table 1. The overall trend in classification by BMI group was statistically significant for Hamada grade (P = .004) but not glenoid erosion type (P = .153).
Before surgery, the surgeon also evaluated rotator cuff status using CTA or MRI. All patients had full-thickness tears of the supraspinatus and infraspinatus. The subscapularis was variably present, and subscapularis repair was performed when the subscapularis was intact. Rotator cuff status is listed in Table 2. There were no significant differences in the distribution of intact subscapularis (P = .402) or teres minor (P = .188) among the normal-weight, overweight, and obese groups. No patient had a latissimus dorsi transfer at time of RSA.
Statistical Analysis
Independent-samples t tests assuming unequal variances were used to compare the 3 BMI groups on age, follow-up duration, preoperative shoulder function scores, and mobility. Chi-square tests were used to identify any significant group differences in comorbidities (eg, complications, arm dominance, prevalence of depression, prevalence of diabetes) and patient satisfaction. Repeated-measures analysis of variance was used to evaluate main effects, changes from before surgery to final follow-up, and BMI group differences, as well as differences in changes from before surgery to final follow-up among the 3 BMI groups.
Results
Among BMI groups (<25 kg/m2, 25-30 kg/m2, >30 kg/m2), there were no statistically significant preoperative differences in age, sex, follow-up duration, complications, arm dominance, prevalence of depression, or prevalence of diabetes (P >. 05) (Table 3). Table 4 lists the groups’ preoperative and final follow-up data (Constant score, ASES score, WOOS index, SANE, mobility). There were no statistically significant preoperative group differences in Constant score, ASES score, WOOS index, SANE, mobility, or patient satisfaction (P > .05) (Tables 5, 6).
All groups’ shoulder function scores and mobility improved significantly from before surgery to final follow-up (P < .001) (Table 5). The groups’ magnitudes of change (improvement) from before surgery to final follow-up were almost identical, with no significant differences in shoulder function scores or mobility (Table 5). The only significant difference was in Constant–Strength, which was higher in the obese group (P = .017) (Table 5). Patient satisfaction ratings improved after surgery, with 79% of the normal-weight group reporting being satisfied or very satisfied with their shoulders (Table 6). The overweight and obese groups gave similar satisfied (81%) and very satisfied (82%) ratings. The small differences between group satisfaction scores were nonsignificant (P = .967).
Complications
The normal-weight group had 4 complications: periprosthetic infection (2 cases), intraoperative humeral fracture (1), and scapular spine stress fracture (1). The overweight group had 1 complication, an acromial stress fracture that was successfully treated with conservative measures. The obese group had 1 patient with 2 postoperative dislocations. The first dislocation was treated with closed reduction and bracing, and the second required revision surgery. There was no statistical difference in complications among the groups (P = .680).
Discussion
To our knowledge, this is the first study of the effects of varying BMI on functional outcomes of RSA with minimum 2-year follow-up. There appears to be minimal impact on shoulder function scores, complications, and patient satisfaction among normal-weight, overweight, and obese patients with RCTA treated by the same surgeon using similar techniques.
The relationship between obesity and increased perioperative risks or poorer surgical outcomes has been well established in orthopedic surgery. In a systematic review, Falagas and Kompoti22 found increased risk for perioperative and nosocomial infections in obese patients. Schoenfeld and colleagues23 and Jiang and colleagues24 reported increased risk for complications in spinal surgery. The total joint arthroplasty literature is rife with evidence suggesting higher BMI leads to increased risk for complications, including infection and deep venous thrombosis, as well as decreased functional outcome scores.25-29 Recent studies on shoulder surgery have shown worse outcomes in rotator cuff repair30 and a higher revision rate in hemiarthroplasy.31
Other RSA studies have examined short-term complications or perioperative risk factors associated with BMI. In a study using slightly different BMI groupings, Gupta and colleagues12 reported significantly higher complication rates for RSA patients with BMI higher than 35 kg/m2 compared to patients with BMI of 25 to 35 kg/m2 and compared to patients with BMI lower than 25 kg/m2. Their study highlighted medical and surgical complications and used a short follow-up period (minimum, 90 days). It did not assess shoulder function scores, and included multiple indications for RSA (eg, RCTA, proximal humerus fracture, inflammatory arthropathy). In another study, higher BMI was reported as a risk factor for early dislocation after RSA, but only 11 patients with a history of dislocation were assessed, and minimum follow-up was 6 months.32 We know of only one study that addressed RSA outcomes in obese patients and used minimum 2-year follow-up, but its primary endpoint was rate of complications, and it did not report shoulder function scores.11 Li and colleagues33 conducted a study similar to ours, but with primary total shoulder arthroplasty (TSA) patients, and reported similar results. Relative to normal BMI, higher BMI did not have a detrimental effect on short-term improvement in shoulder function after TSA.
Given the US obesity epidemic, our study results are encouraging. Depending on many factors, obesity remains a risk factor for poor outcomes in patients who undergo orthopedic surgery. As our results show, however, patients with higher BMI can obtain functional outcomes similar to those experienced by patients with normal-weight BMI after RSA for RCTA.
The primary limitation of this study was its retrospective design. Strengths of the study included its having a single surgeon and a single diagnosis: RCTA. In addition, each group was robust in size, a standard operative/postoperative protocol was used, and clinical results were measured with multiple validated shoulder function scores.
Conclusion
Improved shoulder function scores, mobility, and patient satisfaction can be expected after RSA for RCTA in patients with BMI higher than 30 kg/m2. These patients did not exhibit an increase in complications at short-term follow-up.
Body mass index (BMI) is thought to be a predictor of body composition, with higher values indicating more adipose tissue. BMI is a measure of mass with respect to height. The World Health Organization1 has established health categories based on BMI measurements. Values from 18.5 to 24.9 kg/m2 are deemed to represent normal weight; those from 25 to 30 kg/m2, overweight; and those higher than 30 kg/m2, obesity. BMI is not a perfect tool, but it is the most widely used tool in clinical and research practice because of its relative reliability and ease of use.2 Being overweight or obese (according to BMI) is increasingly common among adults worldwide, and particularly in the United States. An estimated 39% of adults worldwide are overweight, and 13% are obese.1 An estimated 69% of US adults are overweight, including 35.1% who are obese.2
Various pathologies have been treated with reverse shoulder arthroplasty (RSA), and results have been promising,3-9 but little is known about patient demographic and clinical factors that may adversely affect outcomes. Recent work suggests younger age7 and failed prior arthroplasty may adversely affect RSA outcomes.10 Higher BMI has also been implicated as a cause of increased perioperative and immediate postoperative complications of RSA with minimum 90-day follow-up, but no one has examined shoulder function scores at minimum 2-year follow-up.11,12
We conducted a study to examine shoulder function scores, mobility, patient satisfaction, and complications at minimum 2-year follow-up in normal-weight, overweight, and obese patients who underwent RSA. We hypothesized that, compared with normal-weight patients, obese patients would have worse shoulder function scores, worse mobility, and more complications.
Materials and Methods
Inclusion Criteria and Demographics
After obtaining Institutional Review Board approval for this study, we used a prospective shoulder arthroplasty registry to identify patients (N = 77) who had rotator cuff tear arthropathy (RCTA) treated with primary RSA and then had minimum 2-year follow-up. The study period was 2004-2011. All patients had RCTA diagnosed with physical examination findings and anteroposterior, scapular Y, and axillary radiographs. RCTA was graded 1 to 5 using the classification system of Hamada and colleagues.13 Rotator cuff status was determined with preoperative computed tomography arthrogram (CTA) or magnetic resonance imaging (MRI) and confirmed at time of surgery. BMI calculations were based on height and weight measured at initial office visit. Thirty-four patients had normal weight (BMI <25 kg/m2), 21 were overweight (BMI 25-30 kg/m2), and 22 were obese (BMI >30 kg/m2). Patient demographic and clinical characteristics reviewed also included age, sex, follow-up duration, arm dominance, complications, prevalence of depression, and prevalence of diabetes. All RSAs were performed by the same surgeon (Dr. Edwards) at a single high-volume shoulder arthroplasty center.
Shoulder function scores evaluated before surgery and at final follow-up included Constant score,14 American Shoulder and Elbow Surgeons (ASES) score,15 Western Ontario Osteoarthritis Shoulder (WOOS) index,16 Single Assessment Numeric Evaluation (SANE),17 and mobility. Satisfaction was assessed by having patients describe themselves as very dissatisfied, dissatisfied, satisfied, or very satisfied. All intraoperative and postoperative complications were recorded.
Surgical Technique and Postoperative Rehabilitation
The Aequalis RSA system (Tornier) was used for all patients during the study period. The RSA technique used has been well described.18,19 A standard postoperative rehabilitation protocol was followed.19,20
Clinical and Radiographic Assessment
Patients were prospectively enrolled in a shoulder arthroplasty outcomes registry and followed clinically. Mean follow-up was 3.16 years (range, 2-8 years). Before surgery, patients were examined by the surgeon. Examinations were repeated 1 week, 6 weeks, 3 months, 6 months, and 12 months after surgery and annually thereafter. Mobility (active range of motion) was determined with a handheld goniometer. Strength of abduction was measured with a handheld digital dynamometer (Chatillon digital force gauge, 200 lbf; Ametek). Anteroposterior in plane of scapula, scapular Y, and axillary radiographs were obtained at each clinic appointment.
Before surgery, the surgeon reviewed all radiographs. Each RCTA was given a Hamada grade (1-5).13 Glenoid erosion in the coronal plane was classified (E0, E1, E2, E3) according to Sirveaux and colleagues.21 Hamada grades and glenoid erosion types are listed in Table 1. The overall trend in classification by BMI group was statistically significant for Hamada grade (P = .004) but not glenoid erosion type (P = .153).
Before surgery, the surgeon also evaluated rotator cuff status using CTA or MRI. All patients had full-thickness tears of the supraspinatus and infraspinatus. The subscapularis was variably present, and subscapularis repair was performed when the subscapularis was intact. Rotator cuff status is listed in Table 2. There were no significant differences in the distribution of intact subscapularis (P = .402) or teres minor (P = .188) among the normal-weight, overweight, and obese groups. No patient had a latissimus dorsi transfer at time of RSA.
Statistical Analysis
Independent-samples t tests assuming unequal variances were used to compare the 3 BMI groups on age, follow-up duration, preoperative shoulder function scores, and mobility. Chi-square tests were used to identify any significant group differences in comorbidities (eg, complications, arm dominance, prevalence of depression, prevalence of diabetes) and patient satisfaction. Repeated-measures analysis of variance was used to evaluate main effects, changes from before surgery to final follow-up, and BMI group differences, as well as differences in changes from before surgery to final follow-up among the 3 BMI groups.
Results
Among BMI groups (<25 kg/m2, 25-30 kg/m2, >30 kg/m2), there were no statistically significant preoperative differences in age, sex, follow-up duration, complications, arm dominance, prevalence of depression, or prevalence of diabetes (P >. 05) (Table 3). Table 4 lists the groups’ preoperative and final follow-up data (Constant score, ASES score, WOOS index, SANE, mobility). There were no statistically significant preoperative group differences in Constant score, ASES score, WOOS index, SANE, mobility, or patient satisfaction (P > .05) (Tables 5, 6).
All groups’ shoulder function scores and mobility improved significantly from before surgery to final follow-up (P < .001) (Table 5). The groups’ magnitudes of change (improvement) from before surgery to final follow-up were almost identical, with no significant differences in shoulder function scores or mobility (Table 5). The only significant difference was in Constant–Strength, which was higher in the obese group (P = .017) (Table 5). Patient satisfaction ratings improved after surgery, with 79% of the normal-weight group reporting being satisfied or very satisfied with their shoulders (Table 6). The overweight and obese groups gave similar satisfied (81%) and very satisfied (82%) ratings. The small differences between group satisfaction scores were nonsignificant (P = .967).
Complications
The normal-weight group had 4 complications: periprosthetic infection (2 cases), intraoperative humeral fracture (1), and scapular spine stress fracture (1). The overweight group had 1 complication, an acromial stress fracture that was successfully treated with conservative measures. The obese group had 1 patient with 2 postoperative dislocations. The first dislocation was treated with closed reduction and bracing, and the second required revision surgery. There was no statistical difference in complications among the groups (P = .680).
Discussion
To our knowledge, this is the first study of the effects of varying BMI on functional outcomes of RSA with minimum 2-year follow-up. There appears to be minimal impact on shoulder function scores, complications, and patient satisfaction among normal-weight, overweight, and obese patients with RCTA treated by the same surgeon using similar techniques.
The relationship between obesity and increased perioperative risks or poorer surgical outcomes has been well established in orthopedic surgery. In a systematic review, Falagas and Kompoti22 found increased risk for perioperative and nosocomial infections in obese patients. Schoenfeld and colleagues23 and Jiang and colleagues24 reported increased risk for complications in spinal surgery. The total joint arthroplasty literature is rife with evidence suggesting higher BMI leads to increased risk for complications, including infection and deep venous thrombosis, as well as decreased functional outcome scores.25-29 Recent studies on shoulder surgery have shown worse outcomes in rotator cuff repair30 and a higher revision rate in hemiarthroplasy.31
Other RSA studies have examined short-term complications or perioperative risk factors associated with BMI. In a study using slightly different BMI groupings, Gupta and colleagues12 reported significantly higher complication rates for RSA patients with BMI higher than 35 kg/m2 compared to patients with BMI of 25 to 35 kg/m2 and compared to patients with BMI lower than 25 kg/m2. Their study highlighted medical and surgical complications and used a short follow-up period (minimum, 90 days). It did not assess shoulder function scores, and included multiple indications for RSA (eg, RCTA, proximal humerus fracture, inflammatory arthropathy). In another study, higher BMI was reported as a risk factor for early dislocation after RSA, but only 11 patients with a history of dislocation were assessed, and minimum follow-up was 6 months.32 We know of only one study that addressed RSA outcomes in obese patients and used minimum 2-year follow-up, but its primary endpoint was rate of complications, and it did not report shoulder function scores.11 Li and colleagues33 conducted a study similar to ours, but with primary total shoulder arthroplasty (TSA) patients, and reported similar results. Relative to normal BMI, higher BMI did not have a detrimental effect on short-term improvement in shoulder function after TSA.
Given the US obesity epidemic, our study results are encouraging. Depending on many factors, obesity remains a risk factor for poor outcomes in patients who undergo orthopedic surgery. As our results show, however, patients with higher BMI can obtain functional outcomes similar to those experienced by patients with normal-weight BMI after RSA for RCTA.
The primary limitation of this study was its retrospective design. Strengths of the study included its having a single surgeon and a single diagnosis: RCTA. In addition, each group was robust in size, a standard operative/postoperative protocol was used, and clinical results were measured with multiple validated shoulder function scores.
Conclusion
Improved shoulder function scores, mobility, and patient satisfaction can be expected after RSA for RCTA in patients with BMI higher than 30 kg/m2. These patients did not exhibit an increase in complications at short-term follow-up.
1. World Health Organization. Obesity and overweight [factsheet 311]. Updated January 2015. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed March 27, 2016.
2. National Center for Health Statistics, Centers for Disease Control and Prevention. Obesity and overweight. Updated February 25, 2016. http://www.cdc.gov/nchs/fastats/obesity-overweight.htm. Accessed March 27, 2016.
3. Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18(4):600-606.
4. Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468(6):1526-1533.
5. Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2009;17(5):284-289.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Muh SJ, Streit JJ, Wanner JP, et al. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95(20):1877-1883.
8. Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476-1485.
9. Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(20):1915-1923.
10. Boileau P, Melis B, Duperron D, Moineau G, Rumian AP, Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(10):1359-1370.
11. Beck JD, Irgit KS, Andreychik CM, Maloney PJ, Tang X, Harter GD. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013;38(5):965-970.
12. Gupta AK, Chalmers PN, Rahman Z, et al. Reverse total shoulder arthroplasty in patients of varying body mass index. J Shoulder Elbow Surg. 2014;23(1):35-42.
13. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
14. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
15. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
16. Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9(8):771-778.
17. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
18. Gartsman GM, Edwards TB. Shoulder Arthroplasty. Philadelpia, PA: Saunders Elsevier; 2008.
19. Liotard JP, Edwards TB, Padey A, Walch G, Boulahia A. Hydrotherapy rehabilitation after shoulder surgery. Tech Shoulder Elbow Surg. 2003;4:44-49.
20. Trappey GJ 4th, O’Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469(9):2505-2511.
21. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388-395.
22. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6(7):438-446.
23. Schoenfeld AJ, Carey PA, Cleveland AW 3rd, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J. 2013;13(10):1171-1179.
24. Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res. 2014;472(3):968-975.
25. Bozic KJ, Lau E, Kurtz S, et al. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Joint Surg Am. 2012;94(9):794-800.
26. Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466(11):2597-2604.
27. Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012;470(2):490-496.
28. Jämsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94(14):e101.
29. Naziri Q, Issa K, Malkani AL, Bonutti PM, Harwin SF, Mont MA. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop Relat Res. 2013;471(11):3523-3530.
30. Warrender WJ, Brown OL, Abboud JA. Outcomes of arthroscopic rotator cuff repairs in obese patients. J Shoulder Elbow Surg. 2011;20(6):961-967.
31. Singh JA, Sperling JW, Cofield RH. Risk factors for revision surgery after humeral head replacement: 1,431 shoulders over 3 decades. J Shoulder Elbow Surg. 2012;21(8):1039-1044.
32. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744.
33. Li X, Williams PN, Nguyen JT, Craig EV, Warren RF, Gulotta LV. Functional outcomes after total shoulder arthroplasty in obese patients. J Bone Joint Surg Am. 2013;95(21):e160.
1. World Health Organization. Obesity and overweight [factsheet 311]. Updated January 2015. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed March 27, 2016.
2. National Center for Health Statistics, Centers for Disease Control and Prevention. Obesity and overweight. Updated February 25, 2016. http://www.cdc.gov/nchs/fastats/obesity-overweight.htm. Accessed March 27, 2016.
3. Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18(4):600-606.
4. Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468(6):1526-1533.
5. Gerber C, Pennington SD, Nyffeler RW. Reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2009;17(5):284-289.
6. Lenarz C, Shishani Y, McCrum C, Nowinski RJ, Edwards TB, Gobezie R. Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res. 2011;469(12):3324-3331.
7. Muh SJ, Streit JJ, Wanner JP, et al. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95(20):1877-1883.
8. Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476-1485.
9. Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(20):1915-1923.
10. Boileau P, Melis B, Duperron D, Moineau G, Rumian AP, Han Y. Revision surgery of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(10):1359-1370.
11. Beck JD, Irgit KS, Andreychik CM, Maloney PJ, Tang X, Harter GD. Reverse total shoulder arthroplasty in obese patients. J Hand Surg Am. 2013;38(5):965-970.
12. Gupta AK, Chalmers PN, Rahman Z, et al. Reverse total shoulder arthroplasty in patients of varying body mass index. J Shoulder Elbow Surg. 2014;23(1):35-42.
13. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
14. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
15. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
16. Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9(8):771-778.
17. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214-221.
18. Gartsman GM, Edwards TB. Shoulder Arthroplasty. Philadelpia, PA: Saunders Elsevier; 2008.
19. Liotard JP, Edwards TB, Padey A, Walch G, Boulahia A. Hydrotherapy rehabilitation after shoulder surgery. Tech Shoulder Elbow Surg. 2003;4:44-49.
20. Trappey GJ 4th, O’Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469(9):2505-2511.
21. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Molé D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388-395.
22. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6(7):438-446.
23. Schoenfeld AJ, Carey PA, Cleveland AW 3rd, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J. 2013;13(10):1171-1179.
24. Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res. 2014;472(3):968-975.
25. Bozic KJ, Lau E, Kurtz S, et al. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Joint Surg Am. 2012;94(9):794-800.
26. Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466(11):2597-2604.
27. Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012;470(2):490-496.
28. Jämsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012;94(14):e101.
29. Naziri Q, Issa K, Malkani AL, Bonutti PM, Harwin SF, Mont MA. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop Relat Res. 2013;471(11):3523-3530.
30. Warrender WJ, Brown OL, Abboud JA. Outcomes of arthroscopic rotator cuff repairs in obese patients. J Shoulder Elbow Surg. 2011;20(6):961-967.
31. Singh JA, Sperling JW, Cofield RH. Risk factors for revision surgery after humeral head replacement: 1,431 shoulders over 3 decades. J Shoulder Elbow Surg. 2012;21(8):1039-1044.
32. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744.
33. Li X, Williams PN, Nguyen JT, Craig EV, Warren RF, Gulotta LV. Functional outcomes after total shoulder arthroplasty in obese patients. J Bone Joint Surg Am. 2013;95(21):e160.