User login
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
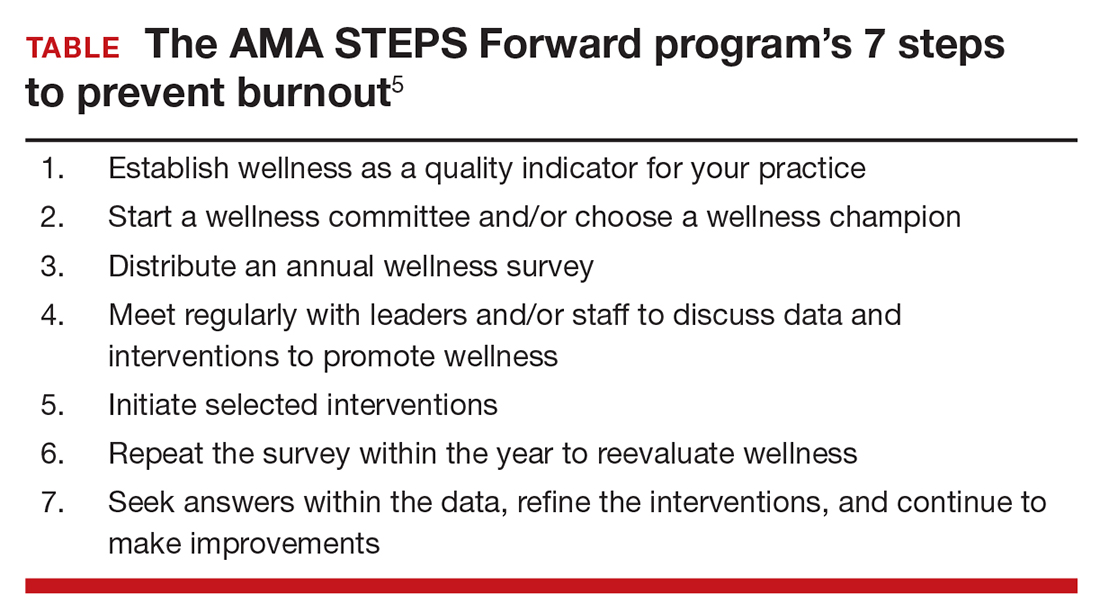
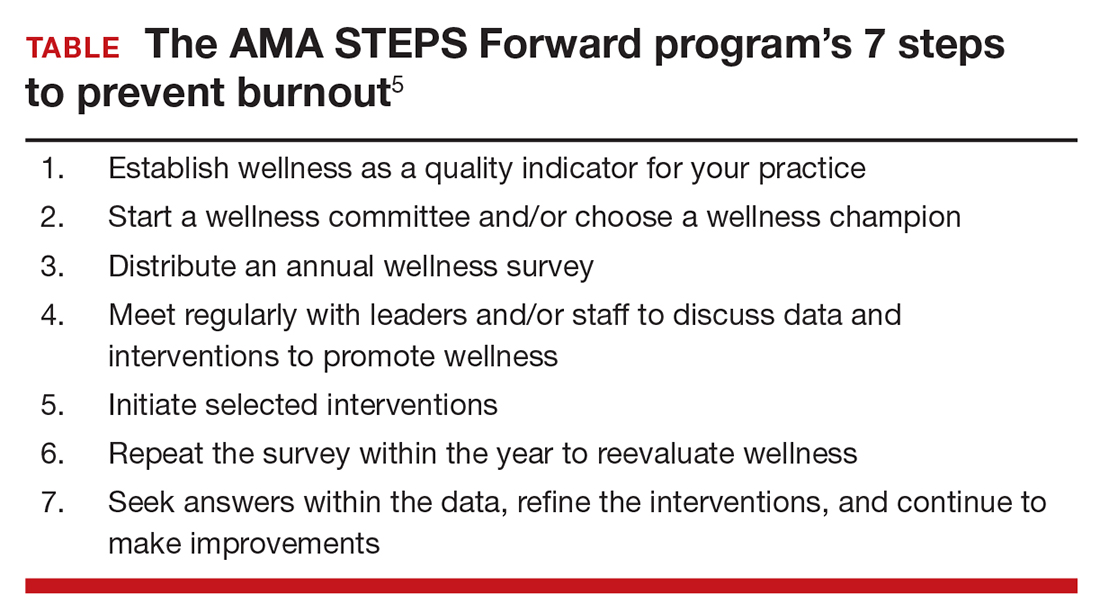
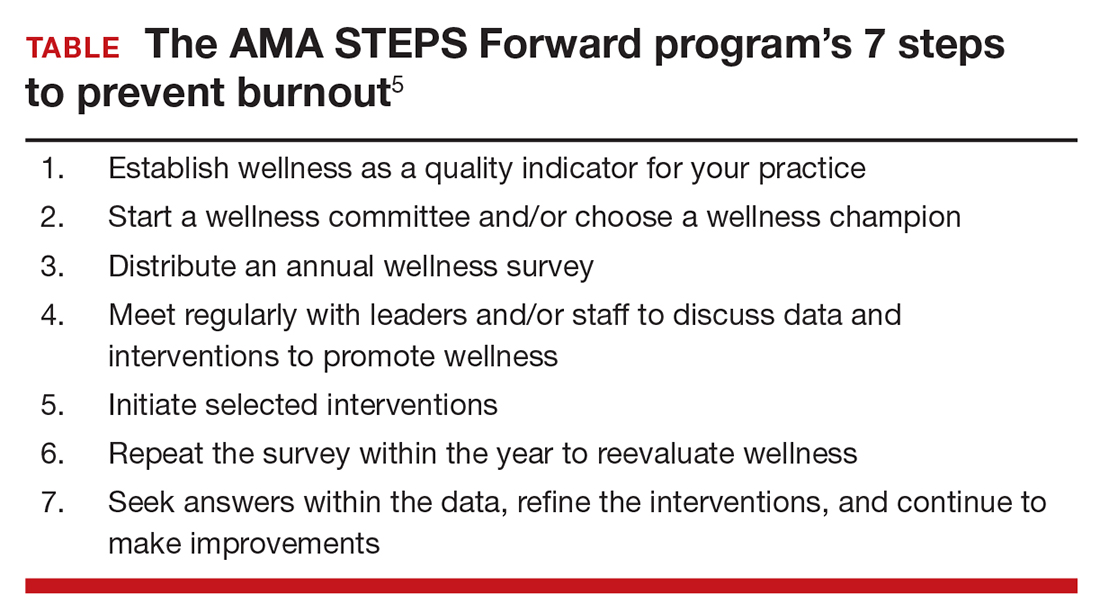
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Physician burnout is a serious issue, especially in the often high-pressure world of obstetrics and gynecology. In the July 2016 issue of OBG
Numerous studies show that burnout is associated with increased likelihood of physician suicide, decisions to leave the practice of medicine, and poorer health, including obesity. These statistics ring alarm bells that we cannot ignore, especially as they may signal real concern for patient care.
The top causes of physician burnout, according to a Medscape survey, are2:
- too many bureaucratic tasks
- spending too many hours at work
- increasing computerization of practice
- income not high enough.
Physician burnout is not a one-size-fits-all condition. Not everyone experiences it similarly. Likewise, there are many strategies you can use to prevent and overcome burnout.
Experts offer guidance on preventing burnout
The 3 ObGyn leaders profiled in this article offer insight, inspiration, and opportunities to help you regain the joy of practice. The American Medical Association (AMA) also offers an online practice-based initiative that includes strategies to help improve professional satisfaction.
Take burnout by the horns
As Assistant Dean for Graduate Medical Education and Professor of Clinical Biologic Sciences, Charles E. Schmidt College of Medicine, at Florida Atlantic University in Boca Raton, Florida, Roger P. Smith, MD, has developed an authoritative focus on the symptoms and effects of physician burnout. Recently, Dr. Smith taught a clinical seminar titled “Burnout: A constant threat” at the American College of Obstetricians and Gynecologists (ACOG) 2016 Annual Clinical and Scientific Meeting in Washington, DC, where he reviewed the causes and symptoms of burnout as well as strategies to minimize and avoid it. His work shows that burnout is pervasive and is becoming more so. Dr. Smith indicates that burnout is not any more common to one part of the country or one type of ObGyn care than any other, although it is becoming more commonly recognized among younger physicians.
As with other nonphysical ailments, symptoms of burnout may have affected ObGyns over many generations—symptoms that people did not discuss with their families or colleagues or that were easily dismissed.
Dr. Smith is opening the door for unreserved conversations about burnout in the physician community. He suggests ways for practices to focus on physician wellness and for individual ObGyns to recognize and take steps to overcome burnout signs. To hear Dr. Smith’s expert discussion on burnout, tune in to his audio interview, “Is burnout on the rise and what are the signs ObGyns should be on the lookout for?”
Develop a passion outside of medicine
Jeffrey M. Rothenberg, MD, MS, experienced serious burnout in 1997 after 3 infants in his high-risk obstetrical unit died in the same week. Like many ObGyns, he tries to not bring work-related issues home, but that week Dr. Rothenberg’s wife Joani, an accomplished art therapist, recognized her husband’s anguish. Soon, she enrolled him in a glass-blowing class to give him a needed break from the pressures of his practice. Dr. Rothenberg’s life was transformed. “Initially it was an escape,” he says about his venture into the art world. “Unlike the OR or in labor and delivery, no one could get hurt but me; it wasn’t life and death—it was something outside of what I do for a living and allowed me to disconnect from my chosen profession—if even for a little bit.”
Still a practicing ObGyn and currently the Designated Institutional Official at St. Vincent in Indianapolis, Dr. Rothenberg is now an accomplished glass artist with his work in public and private collections around the world. Because he feels so passionately that physicians should have a creative outlet, he helps medical students discover their own forms of self-expression through the Creative Arts Therapy Student Interest Group in the Office of Medical Student Service-Learning at Indiana University, where he serves as a mentor. There, he teaches medical students the importance of taking care of themselves as well as their patients. Dr. Rothenberg has made integrating the arts and humanities an integral part of the Indiana University School of Medicine curricula, and he helped establish the Visual Thinking Strategy program, which teaches nursing and medical students better communication skills using the power of observation gained through the arts. In honor of this work, Dr. Rothenberg received a 2015 Arnold P. Gold Foundation Humanism in Medicine Award.
For Dr. Rothenberg, glass has been the perfect medium. “It’s a very tactile art form, and I like doing things with my hands, as a surgeon—there’s a real affinity there—taking materials that are dangerous to touch and coaxing them into forms and shapes that are either artistic or functional is a challenge—but definitely stress reducing,” he says. He also found striking similarities between the operating room and the glass studio, which both involve teamwork, good communication skills, and repetition.
“I think that every healer needs an avocation in addition to his or her chosen vocation. Especially in medicine, both for patients and healers, we all deal with some amazingly complex and difficult situations—often at the intersection of life and death—that go beyond verbalizing and may have no right or wrong answer—just a bad and a worse choice. Given that backdrop, having another way to express yourself or an avenue for a kind of emotional catharsis... is very, very helpful. I think it’s important for our learners, in particular, to embrace the humanistic side of medicine. After all, medicine is so much more than just a science. It’s more of an art, and I think they can really bond with both patients and other providers alike if they have something else in common—something that they can talk about that is outside of medicine. We have very stressful jobs and we need to model to our trainees and to each other that it is important to take care of ourselves. It’s important for a healer to have a passion, a creative outlet,” he explains.
Be part of the solution
ACOG President Thomas Gellhaus, MD, has dedicated his life to advocating for his specialty and for patient care. His presidential initiatives hold great potential for preventing and overcoming burnout in ObGyns throughout the nation.
Join a mentoring program. Dr. Gellhaus encourages greater participation in mentoring—both as a mentor and a mentee—through an innovative mentor matching program created by Thomas Arnold, MD, and Tamara Helfer, MD, MBA, in ACOG District VI. This program allows physicians to share new ideas and aspirations, connect colleagues, and build lifelong bonds. Young ObGyns find an experienced and trusted advisor; more experienced ObGyns find satisfaction in helping others grow. Helping ObGyns avoid burnout is a key goal of this mentoring program, and Dr. Gellhaus is expanding the program to ACOG Fellows in all Districts.
The District VI mentoring program includes these goals:
- sharing skills, knowledge, and expertise
- demonstrating optimism and enthusiasm about the mentor-mentee relationship and the field of obstetrics and gynecology
- promoting ongoing learning and growth
- providing guidance and constructive feedback
- setting personal and professional goals
- celebrating accomplishments.
Dr. Arnold and Dr. Helfer point out that mentoring opportunities are also critical to help align practice with the future, especially working in collaborative groups, focusing on population health, and incorporating integrated learning. Learn more about bringing this mentorship program to your practice or ACOG section at http://www.acog.org/mentorshipprogram.
Consider going on a global health mission. Dr. Gellhaus and his family have participated in and led many medical missions over the years, braving oppressive heat and discomfort for the opportunity to bring health care to those who have none. He points out, “In areas where health care is out of reach, these missions help people return to economic productivity and retain their dignity.”
Under Dr. Gellhaus’ leadership, ACOG will help connect interested ObGyns with care needs across the globe through the organizations that need physician volunteers for short-term stays.
Already, ACOG is developing an ObGyn educational curriculum for Health Volunteers Overseas, a nonprofit organization that for 30 years has helped educate local health providers in villages in developing nations.
These short-term experiences not only can help physicians break out of their burnout ruts but also transform women’s lives and help build long-term relationships with physicians across the globe.
Become an advocate. Also under the leadership of Dr. Gellhaus, ACOG is investing in the imperative to help members thrive and lead health care into the next generation. Advocacy means getting politicians out of our exam rooms, reducing red tape, and improving payments and participation experiences for practicing ObGyns.
Dr. Gellhaus’ All-in for Advocacy program is designed to increase ACOG’s legislative power while expanding advocacy opportunities throughout the membership. Dr. Gellhaus said in his inaugural presidential address, “I’d like everyone to realize that caring for your patients does not end in the exam room or the surgical suite and everyone is affected by our legislative fights.”
All these initiatives offer alternatives to the pressure of day-to-day practice, and participation can bring back the joy of collegiality and making a difference.
AMA’s initiative to battle burnout
The AMA, too, has responded to physicians’ needs by developing its STEPS Forward interactive practice transformation series (www.stepsforward.org). A 2013 Rand study commissioned by the AMA found that “the satisfaction physicians derive from their work is eroding as they spend more time on grueling administrative rules, regulations and paperwork than caring for patients. The report noted that many physicians say that the bureaucratic obstacles to providing patients with high-quality care are major contributors to symptoms of burnout, including emotional fatigue, depersonalization, loss of enthusiasm and early retirement.”3,4
The STEPS Forward module Preventing Physician Burnout (www.stepsforward.org/modules/physician-burnout) can help identify if you are at risk for burnout and offers examples of how to implement changes that may restore your work satisfaction and work-life balance (TABLE).5 It details practice changes that can improve workflow and reduce administrative barriers, improving both patient and physician satisfaction.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613.
- Peckham C. Medscape lifestyle report 2016: Bias and burnout. http://www.medscape.com/features/slideshow/lifestyle/2016/public/overview#page=1. Published January 13, 2016. Accessed August 19, 2016.
- Friedberg MW, Chen PG, Van Busum KR, et al; RAND Corporation. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. 2013. http://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439 /RAND_RR439.pdf. Accessed August 19, 2016.
- American Medical Association. AMA launches STEPS Forward to address physician burnout [news release]. http://www.ama-assn.org/ama/pub/news/news/2015/2015-06-08-ama-launches-steps-forward.page. Published June 8, 2015. Accessed August 19, 2016.
- Linzer M, Guzman-Corrales L, Poplau S; American Medical Association. STEPS Forward. Preventing physician burnout. https://www.stepsforward.org/modules/physician-burnout. Accessed August 19, 2016.
In this Article
- Developing outside passions
- Thomas Gellhaus, MD, encourages mentorship
- 7 steps to prevent burnout

