User login
Addressing quality improvement (QI) for the management of acute coronary syndrome (ACS) at the institutional level is essential for supporting hospitalists and other clinicians as they manage patients with ACS and achieve desired institutional outcomes. This systems approach may identify institution‐specific barriers to quality care, including those that affect the complex management of ACS. Having a firsthand view of patient care puts the hospitalist in a good position to assess the viability of existing processes and protocols that support care. Indeed, the hospitalist has a vested interest in improving systems of care as these systems directly affect the hospitalist's practice. This unique perspective gives the hospitalist an opportunity to facilitate systems change within the institution and to become an integral participant or leader in QI initiatives.
An increasing number of hospitalists are providing critical care at secondary and tertiary care facilities, driven by a shortage of intensivists in the United States. In a 20052006 survey about 75% of hospitalists reported they provide critical care services as part of their practice,1 and this would include care of patients with ACS. The Society of Hospital Medicine (SHM) has developed core competencies that recognize the important role of hospitalists in leading or participating in QI teams for ACS.2 Hospitalists must also be able to apply evidenced‐based outcomes data to support these initiatives.3 Hospitalist competencies for ACS include protocol development that supports the timely diagnosis and treatment of ACS, evaluation of resource utilization, staff education of secondary prevention measures, and implementation of measures to ensure institutional compliance with national quality standards (Table 1).2 Most hospital medicine groups will be expected to contribute to systems improvement, an area where hospitalists have already shown leadership for QI protocols related to glycemic control and venous thromboembolism prophylaxis. Hospitalists were prominent in targeting QI in these areas even though these QI initiatives could easily have been spearheaded by specialists.46
|
| Lead, coordinate, or participate in: |
| Protocol development to rapidly identify ACS, minimizing time to intervention |
| Protocol development for rapid identification and transfer of patients with ACS to a facility with an appropriate level of care |
| Multidisciplinary initiatives, including order sets for ACS and chest pain, that promote patient safety and optimize the use of resources |
| Staff education initiatives on the value of smoking cessation counseling and other prevention measures |
| Implement or integrate: |
| Systems to ensure hospitalwide adherence to national standards, documenting adherence as required by certifying organizations |
| Outcomes research, institution‐specific laboratory policies, and hospital formulary to create indicated and cost‐effective diagnostic and management strategies for patients with ACS |
QI Basics
QI at the institutional level addresses systems of care rather than individual performance, targeting both institutional performance and use of resources.3 QI is a continuous process in which practices and procedures related to patient management are regularly assessed to ascertain whether a quality gap exists. This in turn may lead to new processes, protocols, and algorithms that help the institution and clinicians meet benchmarks of quality care.
QI starts when an existing gap is recognizedthe gap between the scientific understanding of optimal care and actual patient care. The goal is to narrow or close this gap so that each patient receives optimal care. Underlying any QI initiative are 2 essential concepts. First, improvement requires systems changeany system will produce exactly what it is designed to produce. For example, if procedures are not in place to educate patients about smoking cessation while they are hospitalized, it is unlikely that the majority will routinely receive this counseling before they are discharged. Second, less is moreproductivity is not destroyed but often is enhanced by initiating simple and practical change. If a patient arrives in the emergency department (ED) with chest pain, instituting an order set that reminds clinicians to start antiplatelet therapy or a beta blocker can lessen the chance that these medications will be overlooked, especially when the patient transitions between providers or services within the hospital.
SHM has identified 7 essential elements of any QI initiative, and these are applicable to the care of the ACS patient (Table 2).7 These elements highlight the need for institutional support and teamwork that support standardized measures and tools specific to issues in ACS management. These issues include: (1) rapidly identifying a patient with ACS and initiating a care plan when the patient is admitted; (2) encouraging good communication between providers; (3) symptom management; (4) medication safety, polypharmacy, and medication reconciliation; (5) patient and caregiver education; (6) safe discharge and transitions in care; and (7) meeting Centers for Medicare and Medicaid Services (CMS) core measures.
| |
| Institutional support | Commitment of time, personnel, and tools to support the initiative |
| Multidisciplinary team | Team that focuses on quality of care for patients with ACS |
| Reliable metrics | Reflect CMS core and applicable PQRI measures; also reportable to inform team decision making |
| Identify the goal | Establish a measurable, achievable goal with an established timeline |
| Standard order sets | Defined clinical pathways that support evidence‐based treatment strategies, risk stratification, and safe transitions in care |
| Policies that support algorithms and protocols | Institution‐specific to support order sets |
| Education programs | Targeted to clinicians and patients; should cover items addressed in order sets, algorithms, and protocols |
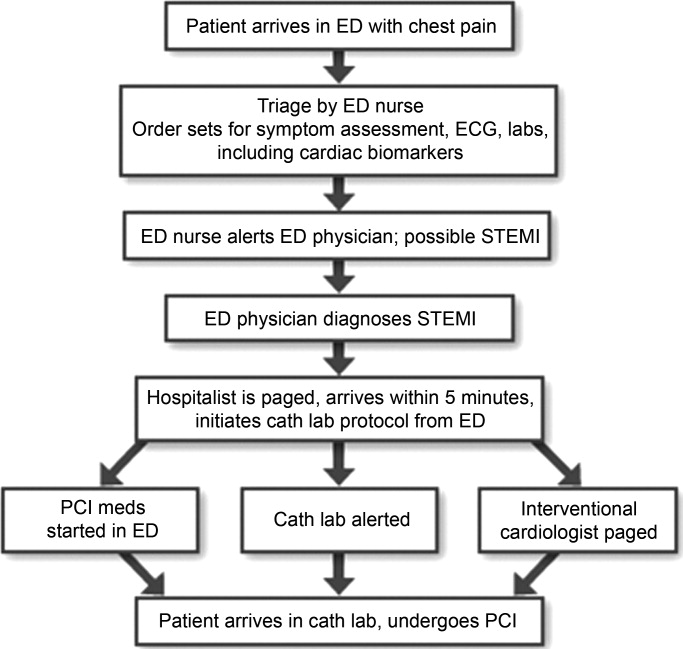
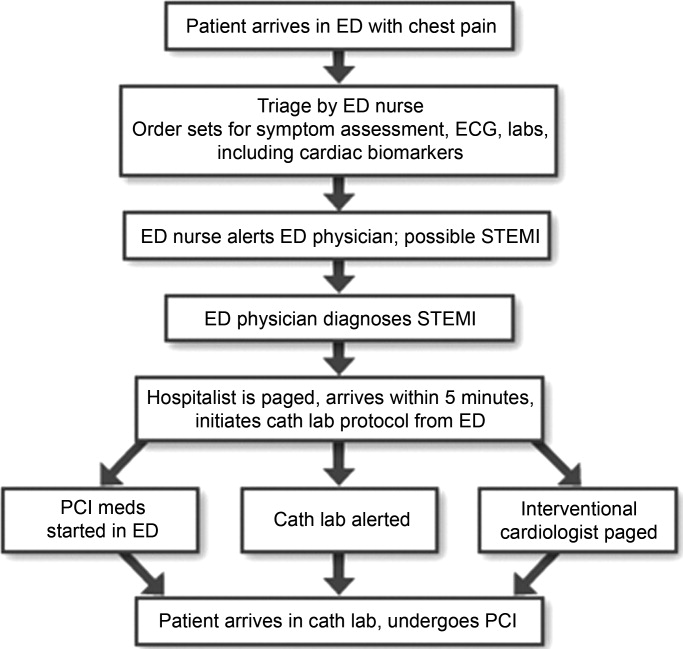
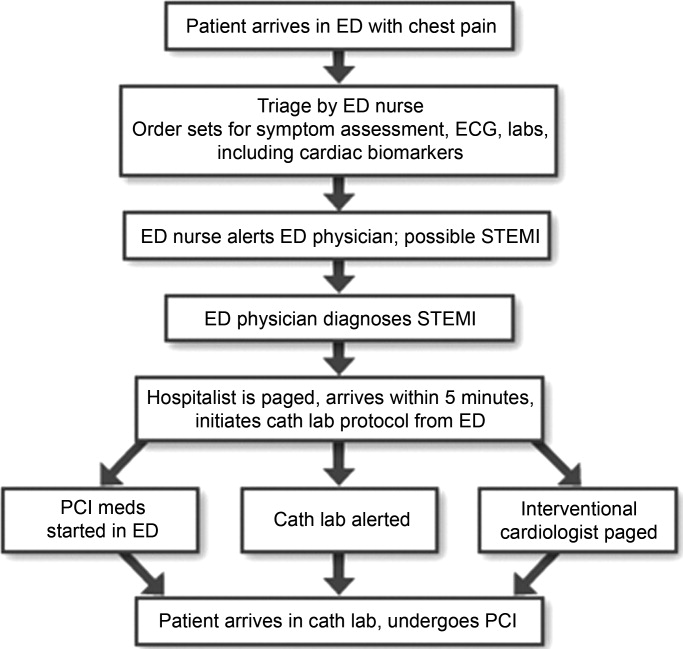
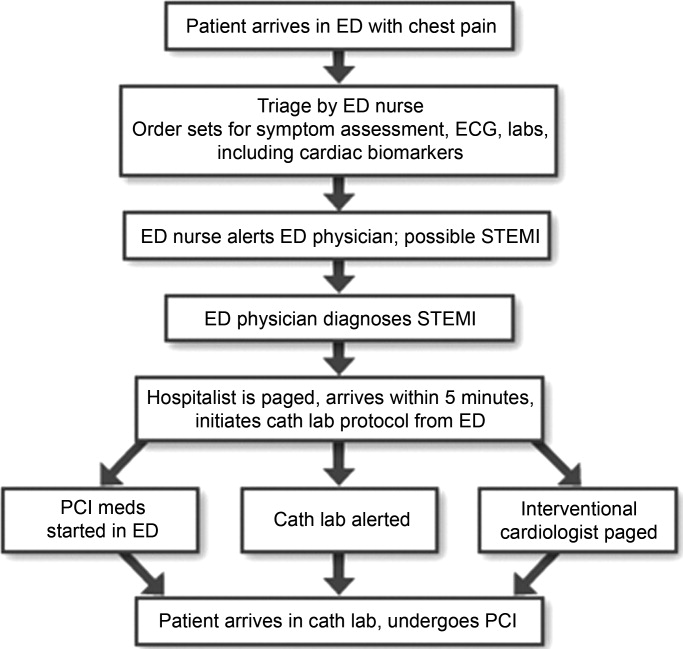
Tools such as process flow mapping and run charts can reveal quality gaps and indicate if process improvements are leading to stated objectives. Process flow mapping makes it possible to identify and visualize quality gaps that might otherwise be hidden and to identify their source or cause. Process mapping documents discrete steps within the flow and usually requires input from multiple disciplines; this information can guide a multidisciplinary QI team when formulating interventions for process improvement.7 Figure 1 shows process flow mapping for the early identification of ST‐segment elevation myocardial infarction (STEMI) when hospitalists have open access to activate the catheterization laboratory (cath lab). The time from door‐to‐balloon is a critical factor in reducing STEMI‐related morbidity8; processes that overcome delays to percutaneous coronary intervention (PCI) and improve communication can have a direct benefit on patient outcomes.
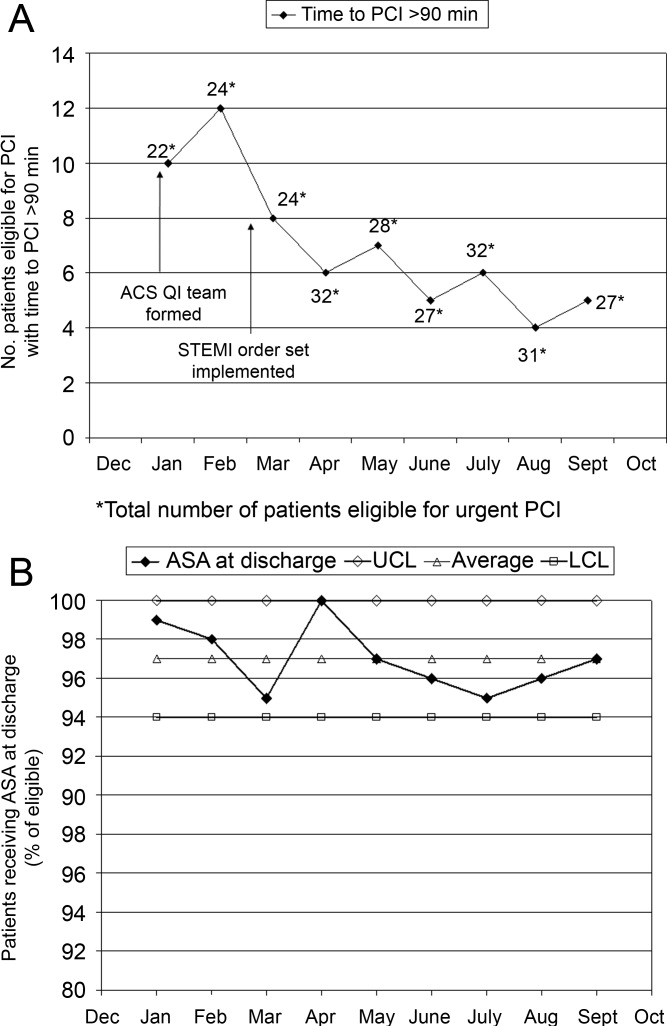
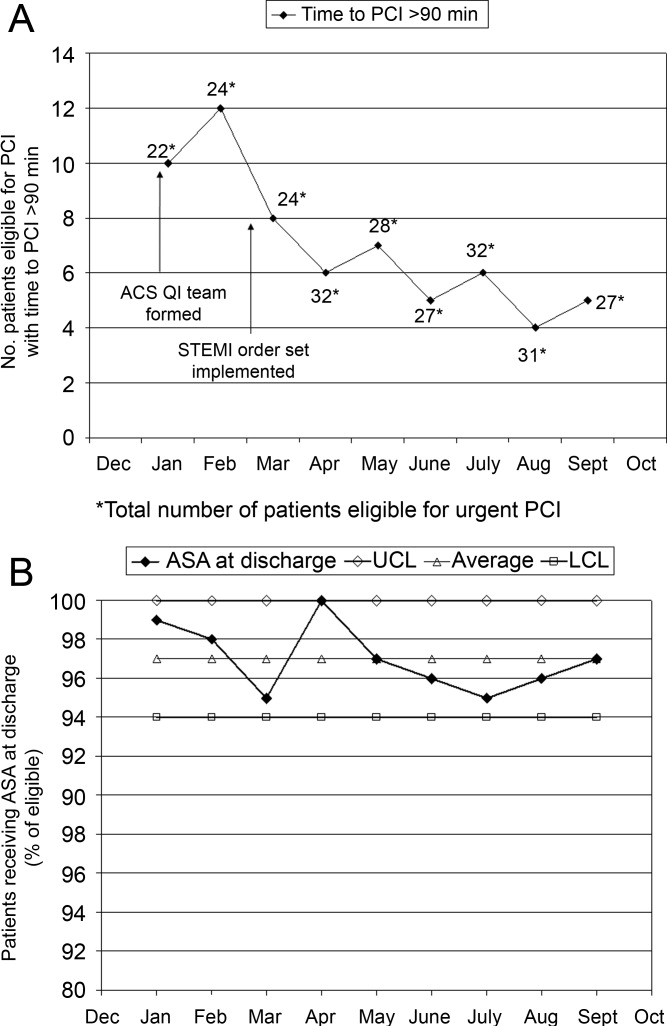
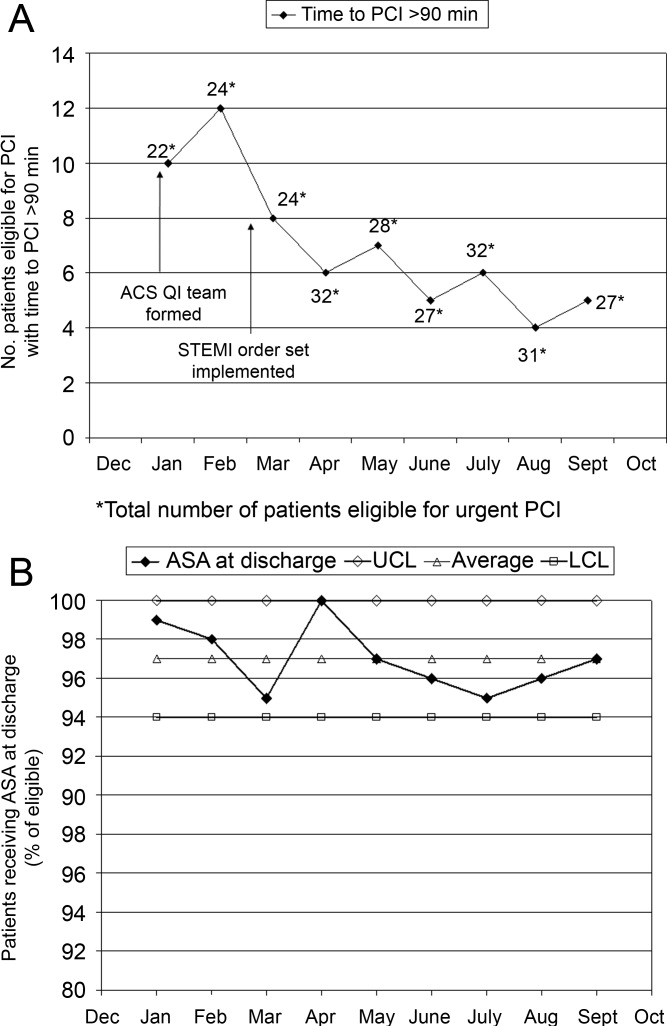
A run chart is a commonly used tool which graphically depicts progress in attaining a goal over time, before and after an intervention. Figure 2a is a run chart that shows the average time to PCI following implementation of an order set designed to support the use of a risk stratification tool for the early diagnosis of STEMI. In this case, the average time to PCI is observed to decrease over time, but still lags behind the desired goal of less than 90 minutes. This run chart indicates that further work is needed to improve the process of identifying patients with STEMI. Figure 2b shows the number of eligible STEMI patients who received aspirin at discharge following implementation of a discharge order set; here, the hospital has clearly made progress toward meeting this CMS core measure.
The following is a case study that illustrates how the implementation of standardized measures and tools can help hospitalists and other clinicians achieve quality measures in the care of a patient with ACS.
Case Study
Mary, a 68‐year‐old woman, presents to the ED with fatigue and some heartburn. She has a history of hypertension and may have had a mini stroke a few years ago. Her symptoms, which she has had on and off for the past few days, worsened considerably right before her arrival. She has been taking chewable antacids but is unsure if they have helped. Her physical exam is unremarkable. A stat electrocardiogram (ECG) shows inferior ST (part of an electrocardiogram between the QRS complex and the T wave) elevation in leads II and III, and augmented vector foot (aVF). Troponins are positive. This case can be approached from 2 perspectives.
Scenario 1
Mary arrives at a hospital that has few standardized systems or protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG, but fails to alert the ED physician. When the ED physician eventually sees the patient and reviews the ECG, she immediately administers nitroglycerin and pages the cardiologist on call and the hospitalist. The hospitalist arrives first and recognizes the STEMI, but hesitates to start unfractionated or low molecular weight heparin until the cardiologist determines whether the patient will undergo PCI. The cardiologist orders PCI, the cath lab is alerted, and the patient is started on the appropriate medications; the patient does not start an aspirin until after PCI. In this scenario, several short delays amount to a significant delay of about 2 hours before the patient reaches the cath lab. In addition, although aspirin is given on day 1, it is not done on arrival. Following PCI, the patient is transferred to the coronary care unit (CCU).
Scenario 2
Mary arrives at an institution with well‐defined, institution‐specific protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG; the results are immediately reviewed with the ED physician. STEMI is diagnosed and the cath lab protocol is activated; the patient receives aspirin as part of a standing order. The hospitalist meets the patient in the ED within 5 minutes and begins the protocol for unfractionated heparin and preparation for immediate PCI, allowing the ED physician to return to ED care. Simultaneously, the interventional cardiologist and cath lab are mobilized and the patient is transferred within 15 minutes. Additional appropriate medications are begun. The door‐to‐balloon time is 60 minutes, well within recommended timeframes. Following PCI, the patient is transferred to the CCU.
Measuring Performance Relative to ACS
Two agencies promulgating quality measures for hospital inpatient care are The Joint Commission (TJC) and the CMS. TJC and CMS jointly established core measures for patients with acute myocardial infarction (AMI) and these are considered key indicators of quality, evidence‐based care. As outlined in Table 3, the TJC/CMS recommendations promote, unless contraindicated, a minimum standard of care for patients with AMI.9, 10 Public reporting of institutional core measure performance has led to an intense focus on improving these metrics.
| Core Measure | Sample Metric |
|---|---|
| |
| Aspirin at arrival | Percentage of patients receiving aspirin within 24 hours before or after hospital arrival |
| Aspirin at discharge | Percentage of patients prescribed aspirin at hospital discharge |
| ACE inhibitor or ARB for LVSD | Percentage of patients with LVSD prescribed an ACEI or ARB at hospital discharge |
| Beta blocker | Percentage of patients prescribed a beta blocker at hospital discharge |
| Fibrinolytic medication given within 30 minutes of hospital arrival | Median time to fibrinolysis |
| Percentage of patients given fibrinolytic medication within 30 minutes of hospital arrival | |
| PCI received within 90 minutes of hospital arrival | Median time to PCI |
| Percentage of patients receiving primary PCI within 90 minutes of hospital arrival | |
| Smoking cessation counseling | Percentage of patients with a history of smoking cigarettes who are counseled about smoking cessation during hospitalization |
On a national level, TJC documented performance improvement from 2002 to 2008 for each of the core measures. Compliance with smoking cessation counseling improved the most, rising from 67% to almost 99%. In 2008, a combined measure of all individual core measures indicated that, overall, care of heart attack patients is of high quality. Hospitals delivered evidenced‐based care in 96.7% of the opportunities they had to provide this care. Compliance related to oral medications was also good (95%); however, a closer look at other individual measures shows that improvement is needed to reduce the time to fibrinolysis (52.4% compliance rate for 30 minutes or less) and time to primary PCI (81.6% compliance rate for 90 minutes or less).11
Financial incentives are tied to QI measures including those from CMS. At present, this system is in the pay‐for‐reporting phase, in which institutions are penalized for not reporting quality metrics for the CMS core measures. It is likely that, to further incentivize institutions to meet quality benchmarks, this will be expanded to a pay‐for‐performance system (eg, differential payments for readmissions or different payment scales based on prior performance). Public disclosure of institutional performance relative to ACS and other medical conditions is available through the HHS.gov website (www.hospitalcompare.hhs.gov), which compares performance between hospitals and provides a clear business motivation for institutions to improve and provide high quality care.
Two other reporting systems should be noted. The CMS Physician Quality Reporting Initiative (PQRI) includes physician‐related quality measures specific to ACS12 that overlap with institution‐level CMS core measures with regard to prescribing ACS medications. Payments associated with the PQRI are currently a small financial factor for hospitalists, but will likely grow as quality initiatives develop overall. The Hospital Care Quality Information From the Consumer Perspective (HCAHPS) initiative, also from CMS, strives to capture patients' perspectives on hospital care through a standardized survey. The goals are to collect data that can be used to compare hospital performance, create an incentive for QI through public disclosure of results, and increase transparency regarding the quality of hospital care.13 However, the focus is not ACS‐specific. Patients are queried about communication with hospital staff, communication about medications, and information about discharge, all areas of concern for the hospitalist in general that have been identified as areas for improvement relative to ACS.
Case Study (cont)
Scenario 1 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. The hospitalist and cardiologist see her separately on rounds and each assumes the other has a reason for not starting a beta blocker; therefore, a beta blocker is not prescribed. The nurse cannot tell who is in charge and does not anticipate the day of dischargeshe is just implementing the orders as they are written. The day of discharge arrives; the nurse learns from Mary that the hospitalist will discharge her that day. The hospitalist reviews the list of ACS medications and realizes that Mary still has not started a beta blocker. He cannot reach the cardiologist before Mary's ride home arrives, so he writes a note in the discharge summary alerting the primary care physician (PCP) to consider a beta blocker at follow‐up. Because of this lack of communication and systems for tracking the implementation of guideline‐recommended therapies, Mary is discharged without a CMS core measure medication, with no assurance that this will be addressed by the PCP.
Scenario 2 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. Standard post‐PCI/STEMI orders are in place according to institutional protocol. The hospitalist is able to confirm that all interventions required at admission (aspirin, beta blocker, assessment of smoking status) have occurred by reviewing a well‐structured checklist that includes easy‐to‐read visual cues. The checklist indicates that Mary was counseled about smoking cessation on day 1 of her stay in the CCU. Mary and her physicians and nurses are all aware of the target discharge date and the milestones that must be met prior to discharge (eg, echocardiogram, medication review, education, assessment of mobility, etc). Mary is instructed about each new medication and given educational materials.14 Follow‐up appointments postdischarge are made, and the discharge summary is sent electronically to the PCP. These institution‐specific protocols enhance communication overall and help the hospital meet high standards of patient care.
Special QI Issues in ACS Management for the Hospitalist
Coordination is especially important for patients with ACS because their care is so complex. Seamless transitions promote safe care as the patient moves from the ED, cath lab, recovery unit, medical floor, and discharge through the transition to primary care. Poor communication between clinicians during these transitions may result in delayed or overlooked treatment and other medical errors. Implementing an institutional system of care may overcome communication barriers and help ensure the institution meets its quality benchmarks, such as the CMS core measures. Standard order sets and protocols identify the steps and components needed to manage ACS. At admission, these measures promote early assessment of patient risk, triage to early intervention, medication reconciliation, and communication between stakeholders such as the hospitalist, cardiologist, and the cath lab.15, 16 During hospitalization, they help assure ongoing risk assessment and early consideration of discharge planning, culminating in discharge and the transition back to primary care.
A recent guideline update8 focused attention on the coordination of care between institutions and the critical importance of rapid triage for patients who need primary PCI and transfer from a non‐PCI to a PCI‐capable institution. The decision to transfer rests on multiple factors and requires rapid decision making on the part of clinicians. Time to reperfusion is shown to have a direct effect on patient outcomes. Established protocols within a non‐PCI facility can support timely transfer to a PCI‐capable facility if indicated. Factors such as the patient's mortality risk, the risk of bleeding from fibrinolytic therapy, duration of symptoms, and the time for transport to a PCI facility all must be considered. It is recognized that a regional system of STEMI care best supports collaborative efforts between institutions and community resources that support QI efforts.
Transitions in care, and particularly discharge, are areas with identified gaps in quality care17, 18 for which improvement has been pursued on an institutional level. Project BOOST (Better Outcomes for Older Adults Through Safe Transitions) seeks to improve the care of patients during the transition from inpatient to outpatient care, and focuses on elderly patients identified to be at high‐risk for adverse events during this transition.19 The goal is to improve outcomes related to 30‐day readmission rates, patient satisfaction, communication between inpatient and outpatient providers, identification of high‐risk patients who need intervention to reduce risk, and patient education about their risk for an adverse event. BOOST addresses these outcomes at an institutional level by offering resources related to project management, data collection, tools for clinicians and patients, and participating mentor institutions. These resources help an institution assess its readiness for change, identify quality gaps, promote teamwork, and guide the implementation and subsequent evaluation of process improvements. Specific tools for clinicians also support institutional goals for teamwork and communication, creating an environment for safe transitions. Both BOOST19 and the adaptable Transitions Tool from the SHM20 provide a framework for understanding processes that involve multiple departments and stakeholders, breaking complex processes into discrete parts for which quality gaps can be identified and change instituted to improve care. A checklist can also be a useful tool for ensuring specific issues are addressed during transitions in care. SHM developed a checklist for hospitalist use that lists elements of a discharge summary for patients with ACS (Table 4).21
| |
| Diagnoses | Elaborate on details of MI such as location, complications |
| Comorbidities | List, including diabetes, lipids, hypertension, renal disease |
| Medications | Note medication reconciliation, reason for not prescribing core measure medications, titration of any medications |
| Specific medications to address include ACE/ARB inhibitors, aspirin, beta blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) | |
| Procedures | Type of stent (bare‐metal stent, drug‐eluting stent) and stent location |
| Complications (hematoma, transfusion) | |
| If ECHO, note type, ejection fraction; provide copy of ECG | |
| Follow‐up appointment(s) | Primary care, cardiology, others such as cardiac rehabilitation |
| Follow‐up testing | ETT (type, timeframe); ECHO if indicated; laboratory assessments |
| Code status | |
| Activity | |
| Diet | |
| Wound care (eg, groin) | |
| Treatment course | Address cognitive level, discharge LDL, discharge creatinine, INR if on warfarin, LFTs if on statin |
| Copy all providers | |
Staff and patient education is also an area that can benefit from evaluation. Clinicians from multiple disciplines are stakeholders in QI and they should receive education about its purpose and goals. Usually institutions will have a QI methodology in place, and this should be conveyed to the members of the ACS team. Staff education about ACS should be tailored to each specialty, be institution‐specific, current, and comprehensive, and include methods for assessing the learner. Education should be easily available (eg, on the Internet or via an electronic format), interactive, case‐based, and mandatory. For patients, education should be available in languages other than English and identify community resources and opportunities for additional outpatient education. The value of any educational program should be assessed to measure learner participation, satisfaction, and comprehension.
Gathering metrics and generating objective evidence of change is critical to QI; quantifying improvement (or lack thereof) must be done to determine whether the changes implemented improve care and ultimately whether desired outcomes are met. Metrics should be meaningful, associated with standards of care (eg, CMS core measures), and carefully chosen to reflect current practice. CMS core measures are a good target for collecting metrics to assess an institution's performance relative to ACS (Table 3). The Specifications Manual for National and Hospital Inpatient Quality Measures10 from TJC and CMS identifies the data elements needed for reporting. Other metrics not specified as core measures are worthy of measurement because they are considered the standard of care for patients with ACS (Table 5). The metrics shown in Tables 3 and 5 assume that all patients are eligible for core‐measure or standard‐of‐care medications and procedures. Because some measures are contraindicated in some patients, it is more meaningful to measure the percentage of patients without a contraindication who receive the measure. If a measure is contraindicated, the patient's medical record must include supporting documentation indicating why a core measure was not met. To be objective and reduce bias regarding the effectiveness of QI measures, data collection is best done prospectively. If necessary, periodic assessments against performance measures (institutional, government, professional association) should be made to support timely intervention. Run charts can be particularly useful here, measuring change over time to identify trends or an intervention that supported, did not affect, or was a barrier to the desired change.
Case Study (cont)
Scenario 1 (cont)
Mary tells the hospitalist she felt the discharge process was rushed and confusing and that she was dissatisfied with her care overall. Recalling a recent review article on the process for public disclosure of patient ratings related to hospital stay, the hospitalist locates HospitalCompare.com on the Internet. He reviews results from patient satisfaction surveys that compare his institution with others in the geographic area and is surprised to discover that patients generally give his institution a poor rating as well as low marks for the quality of nursing and physicianpatient communication. He is interested in this information but is not aware of resources for further exploration.
Scenario 2 (cont)
At discharge, the hospitalist confirms with Mary that she has received smoking cessation counseling during her hospital stay; he documents this in her chart and discharge summary. The hospitalist was aware of this particular quality measure because the recent weekly score card of hospital performance, posted in the unit, reported that the hospital was not meeting its goal of 100% compliance for this CMS core measure. Among heart attack patients who were identified as smokers, only 80% of charts documented that the patient had been counseled about smoking cessation during the hospital stay. Mary says that she understands the importance of not smoking and says she will make an effort to stop.
| Standard of Care Measure | Sample Metric |
|---|---|
| |
| LDL‐cholesterol assessment | Percentage of patients who have LDL cholesterol measured during hospitalization |
| Lipid‐lowering therapy at discharge | Percentage of patients prescribed a statin at hospital discharge |
| Dietary consultation | Percentage of patients who receive a dietary consult during hospitalization |
| Time to receipt of high‐risk abnormal laboratory assessments | Median time to receipt of high‐risk laboratory results, eg, troponins |
| Cardiac risk assessment | Percentage of patients who receive a cardiac risk assessment during admission |
| Measurement of LVEF | Percentage of patients who receive a cardiac echocardiogram to measure of LVEF before discharge |
| Document communication with PCP | Percentage of patients whose communication with the PCP was documented at discharge |
| Completed medication reconciliation | Percentage of patients for whom medication reconciliation was documented by the time of discharge |
| Make 1‐week follow‐up appointment with PCP | Percentage of patients for whom a 1‐week follow‐up appointment with the PCP was documented at the time of discharge |
| Additional Measure | |
| Inpatient mortality | |
Conclusion
Each hospitalist can have an impact on ACS care systemwide. Hospitalists are on the front line of care and have a unique perspective on patients as they are transitioned through the hospital stay and on how an institution handles patient care overall. They experience firsthand the challenges presented by poor communication between providers, patients, and their families. They can offer breadth of experience and perspective when assessing processes linked to patient care and can be instrumental in ensuring each patient experiences safe transitions during the hospital stay. Hospitalists should participate in QI initiatives for ACS and should consider opportunities to take the lead on these initiatives within their institutions.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in the preparation of this manuscript.
- Hospitalists and intensivists: partners in caring for the critically ill—the time has come.J Hosp Med.2010;5:1–3.
- Society of Hospital Medicine. Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- Society of Hospital Medicine. Quality improvement.J Hosp Med.2006;1 (suppl):92.
- ,,, et al.Curriculum development: the venous thromboembolism quality improvement resource room.J Hosp Med.2006;1:124–132.
- ,,,,Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3:66–75.
- ,,,Effects of a subcutaneous insulin protocol, clinical education, and computerized order set on the quality of inpatient management of hyperglycemia: results of a clinical trial.J Hosp Med.2009;4:16–27.
- SHM Acute Coronary Syndrome Advisory Board. A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org. 2010. Accessed July 2010.
- ,,, et al.2009focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.year="2009"2009;54:2205–2241.
- The Joint Commission. Performance measure intiatives. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Acute+Myocardial+Infarction+Core+Measure+Set.htm. 2010. Accessed July 2010.
- The Joint Commission, Centers for Medicare and Medicare Services. Specifications manual for national hospital inpatient quality measures, version 2.5. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Current+NHQM+Manual.htm. 2009 November 6. Accessed July 2010.
- The Joint Commission. Improving America's hospitals: The Joint Commission's annual report on quality and safety 2009. Available at: http://www.jointcommission.org/Library/annual_report.2009. Accessed July 2010.
- Centers for Medicare and Medicare Services. Physician quality reporting initiative (PQRI). Available at: http://www.cms.hhs.gov/pqri. 2010. Accessed July 2010.
- Hospital Care Quality Information from the Consumer Perspective. CAHPS hospital survey. Available at: http://www.hcahpsonline.org. 2010. Accessed July 2010.
- ,,,.Discharge education improves clinical outcomes in patients with chronic heart failure.Circulation.2005;111:179–185.
- ,,, et al.National efforts to improve door‐to‐balloon time results from the Door‐to‐Balloon Alliance.J Am Coll Cardiol.2009;54:2423–2429.
- ,,, et al.Sustaining improvement in door‐to‐balloon time over 4 years: the Mayo clinic ST‐elevation myocardial infarction protocol.Circ Cardiovasc Qual Outcomes.2009;2:508–513.
- ,,,Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- Society of Hospital Medicine. Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. 2010. Accessed July 2010.
- SHM ACS Transitions Workgroup. SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm. 2010. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients‐‐development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
Addressing quality improvement (QI) for the management of acute coronary syndrome (ACS) at the institutional level is essential for supporting hospitalists and other clinicians as they manage patients with ACS and achieve desired institutional outcomes. This systems approach may identify institution‐specific barriers to quality care, including those that affect the complex management of ACS. Having a firsthand view of patient care puts the hospitalist in a good position to assess the viability of existing processes and protocols that support care. Indeed, the hospitalist has a vested interest in improving systems of care as these systems directly affect the hospitalist's practice. This unique perspective gives the hospitalist an opportunity to facilitate systems change within the institution and to become an integral participant or leader in QI initiatives.
An increasing number of hospitalists are providing critical care at secondary and tertiary care facilities, driven by a shortage of intensivists in the United States. In a 20052006 survey about 75% of hospitalists reported they provide critical care services as part of their practice,1 and this would include care of patients with ACS. The Society of Hospital Medicine (SHM) has developed core competencies that recognize the important role of hospitalists in leading or participating in QI teams for ACS.2 Hospitalists must also be able to apply evidenced‐based outcomes data to support these initiatives.3 Hospitalist competencies for ACS include protocol development that supports the timely diagnosis and treatment of ACS, evaluation of resource utilization, staff education of secondary prevention measures, and implementation of measures to ensure institutional compliance with national quality standards (Table 1).2 Most hospital medicine groups will be expected to contribute to systems improvement, an area where hospitalists have already shown leadership for QI protocols related to glycemic control and venous thromboembolism prophylaxis. Hospitalists were prominent in targeting QI in these areas even though these QI initiatives could easily have been spearheaded by specialists.46
|
| Lead, coordinate, or participate in: |
| Protocol development to rapidly identify ACS, minimizing time to intervention |
| Protocol development for rapid identification and transfer of patients with ACS to a facility with an appropriate level of care |
| Multidisciplinary initiatives, including order sets for ACS and chest pain, that promote patient safety and optimize the use of resources |
| Staff education initiatives on the value of smoking cessation counseling and other prevention measures |
| Implement or integrate: |
| Systems to ensure hospitalwide adherence to national standards, documenting adherence as required by certifying organizations |
| Outcomes research, institution‐specific laboratory policies, and hospital formulary to create indicated and cost‐effective diagnostic and management strategies for patients with ACS |
QI Basics
QI at the institutional level addresses systems of care rather than individual performance, targeting both institutional performance and use of resources.3 QI is a continuous process in which practices and procedures related to patient management are regularly assessed to ascertain whether a quality gap exists. This in turn may lead to new processes, protocols, and algorithms that help the institution and clinicians meet benchmarks of quality care.
QI starts when an existing gap is recognizedthe gap between the scientific understanding of optimal care and actual patient care. The goal is to narrow or close this gap so that each patient receives optimal care. Underlying any QI initiative are 2 essential concepts. First, improvement requires systems changeany system will produce exactly what it is designed to produce. For example, if procedures are not in place to educate patients about smoking cessation while they are hospitalized, it is unlikely that the majority will routinely receive this counseling before they are discharged. Second, less is moreproductivity is not destroyed but often is enhanced by initiating simple and practical change. If a patient arrives in the emergency department (ED) with chest pain, instituting an order set that reminds clinicians to start antiplatelet therapy or a beta blocker can lessen the chance that these medications will be overlooked, especially when the patient transitions between providers or services within the hospital.
SHM has identified 7 essential elements of any QI initiative, and these are applicable to the care of the ACS patient (Table 2).7 These elements highlight the need for institutional support and teamwork that support standardized measures and tools specific to issues in ACS management. These issues include: (1) rapidly identifying a patient with ACS and initiating a care plan when the patient is admitted; (2) encouraging good communication between providers; (3) symptom management; (4) medication safety, polypharmacy, and medication reconciliation; (5) patient and caregiver education; (6) safe discharge and transitions in care; and (7) meeting Centers for Medicare and Medicaid Services (CMS) core measures.
| |
| Institutional support | Commitment of time, personnel, and tools to support the initiative |
| Multidisciplinary team | Team that focuses on quality of care for patients with ACS |
| Reliable metrics | Reflect CMS core and applicable PQRI measures; also reportable to inform team decision making |
| Identify the goal | Establish a measurable, achievable goal with an established timeline |
| Standard order sets | Defined clinical pathways that support evidence‐based treatment strategies, risk stratification, and safe transitions in care |
| Policies that support algorithms and protocols | Institution‐specific to support order sets |
| Education programs | Targeted to clinicians and patients; should cover items addressed in order sets, algorithms, and protocols |
Tools such as process flow mapping and run charts can reveal quality gaps and indicate if process improvements are leading to stated objectives. Process flow mapping makes it possible to identify and visualize quality gaps that might otherwise be hidden and to identify their source or cause. Process mapping documents discrete steps within the flow and usually requires input from multiple disciplines; this information can guide a multidisciplinary QI team when formulating interventions for process improvement.7 Figure 1 shows process flow mapping for the early identification of ST‐segment elevation myocardial infarction (STEMI) when hospitalists have open access to activate the catheterization laboratory (cath lab). The time from door‐to‐balloon is a critical factor in reducing STEMI‐related morbidity8; processes that overcome delays to percutaneous coronary intervention (PCI) and improve communication can have a direct benefit on patient outcomes.
A run chart is a commonly used tool which graphically depicts progress in attaining a goal over time, before and after an intervention. Figure 2a is a run chart that shows the average time to PCI following implementation of an order set designed to support the use of a risk stratification tool for the early diagnosis of STEMI. In this case, the average time to PCI is observed to decrease over time, but still lags behind the desired goal of less than 90 minutes. This run chart indicates that further work is needed to improve the process of identifying patients with STEMI. Figure 2b shows the number of eligible STEMI patients who received aspirin at discharge following implementation of a discharge order set; here, the hospital has clearly made progress toward meeting this CMS core measure.
The following is a case study that illustrates how the implementation of standardized measures and tools can help hospitalists and other clinicians achieve quality measures in the care of a patient with ACS.
Case Study
Mary, a 68‐year‐old woman, presents to the ED with fatigue and some heartburn. She has a history of hypertension and may have had a mini stroke a few years ago. Her symptoms, which she has had on and off for the past few days, worsened considerably right before her arrival. She has been taking chewable antacids but is unsure if they have helped. Her physical exam is unremarkable. A stat electrocardiogram (ECG) shows inferior ST (part of an electrocardiogram between the QRS complex and the T wave) elevation in leads II and III, and augmented vector foot (aVF). Troponins are positive. This case can be approached from 2 perspectives.
Scenario 1
Mary arrives at a hospital that has few standardized systems or protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG, but fails to alert the ED physician. When the ED physician eventually sees the patient and reviews the ECG, she immediately administers nitroglycerin and pages the cardiologist on call and the hospitalist. The hospitalist arrives first and recognizes the STEMI, but hesitates to start unfractionated or low molecular weight heparin until the cardiologist determines whether the patient will undergo PCI. The cardiologist orders PCI, the cath lab is alerted, and the patient is started on the appropriate medications; the patient does not start an aspirin until after PCI. In this scenario, several short delays amount to a significant delay of about 2 hours before the patient reaches the cath lab. In addition, although aspirin is given on day 1, it is not done on arrival. Following PCI, the patient is transferred to the coronary care unit (CCU).
Scenario 2
Mary arrives at an institution with well‐defined, institution‐specific protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG; the results are immediately reviewed with the ED physician. STEMI is diagnosed and the cath lab protocol is activated; the patient receives aspirin as part of a standing order. The hospitalist meets the patient in the ED within 5 minutes and begins the protocol for unfractionated heparin and preparation for immediate PCI, allowing the ED physician to return to ED care. Simultaneously, the interventional cardiologist and cath lab are mobilized and the patient is transferred within 15 minutes. Additional appropriate medications are begun. The door‐to‐balloon time is 60 minutes, well within recommended timeframes. Following PCI, the patient is transferred to the CCU.
Measuring Performance Relative to ACS
Two agencies promulgating quality measures for hospital inpatient care are The Joint Commission (TJC) and the CMS. TJC and CMS jointly established core measures for patients with acute myocardial infarction (AMI) and these are considered key indicators of quality, evidence‐based care. As outlined in Table 3, the TJC/CMS recommendations promote, unless contraindicated, a minimum standard of care for patients with AMI.9, 10 Public reporting of institutional core measure performance has led to an intense focus on improving these metrics.
| Core Measure | Sample Metric |
|---|---|
| |
| Aspirin at arrival | Percentage of patients receiving aspirin within 24 hours before or after hospital arrival |
| Aspirin at discharge | Percentage of patients prescribed aspirin at hospital discharge |
| ACE inhibitor or ARB for LVSD | Percentage of patients with LVSD prescribed an ACEI or ARB at hospital discharge |
| Beta blocker | Percentage of patients prescribed a beta blocker at hospital discharge |
| Fibrinolytic medication given within 30 minutes of hospital arrival | Median time to fibrinolysis |
| Percentage of patients given fibrinolytic medication within 30 minutes of hospital arrival | |
| PCI received within 90 minutes of hospital arrival | Median time to PCI |
| Percentage of patients receiving primary PCI within 90 minutes of hospital arrival | |
| Smoking cessation counseling | Percentage of patients with a history of smoking cigarettes who are counseled about smoking cessation during hospitalization |
On a national level, TJC documented performance improvement from 2002 to 2008 for each of the core measures. Compliance with smoking cessation counseling improved the most, rising from 67% to almost 99%. In 2008, a combined measure of all individual core measures indicated that, overall, care of heart attack patients is of high quality. Hospitals delivered evidenced‐based care in 96.7% of the opportunities they had to provide this care. Compliance related to oral medications was also good (95%); however, a closer look at other individual measures shows that improvement is needed to reduce the time to fibrinolysis (52.4% compliance rate for 30 minutes or less) and time to primary PCI (81.6% compliance rate for 90 minutes or less).11
Financial incentives are tied to QI measures including those from CMS. At present, this system is in the pay‐for‐reporting phase, in which institutions are penalized for not reporting quality metrics for the CMS core measures. It is likely that, to further incentivize institutions to meet quality benchmarks, this will be expanded to a pay‐for‐performance system (eg, differential payments for readmissions or different payment scales based on prior performance). Public disclosure of institutional performance relative to ACS and other medical conditions is available through the HHS.gov website (www.hospitalcompare.hhs.gov), which compares performance between hospitals and provides a clear business motivation for institutions to improve and provide high quality care.
Two other reporting systems should be noted. The CMS Physician Quality Reporting Initiative (PQRI) includes physician‐related quality measures specific to ACS12 that overlap with institution‐level CMS core measures with regard to prescribing ACS medications. Payments associated with the PQRI are currently a small financial factor for hospitalists, but will likely grow as quality initiatives develop overall. The Hospital Care Quality Information From the Consumer Perspective (HCAHPS) initiative, also from CMS, strives to capture patients' perspectives on hospital care through a standardized survey. The goals are to collect data that can be used to compare hospital performance, create an incentive for QI through public disclosure of results, and increase transparency regarding the quality of hospital care.13 However, the focus is not ACS‐specific. Patients are queried about communication with hospital staff, communication about medications, and information about discharge, all areas of concern for the hospitalist in general that have been identified as areas for improvement relative to ACS.
Case Study (cont)
Scenario 1 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. The hospitalist and cardiologist see her separately on rounds and each assumes the other has a reason for not starting a beta blocker; therefore, a beta blocker is not prescribed. The nurse cannot tell who is in charge and does not anticipate the day of dischargeshe is just implementing the orders as they are written. The day of discharge arrives; the nurse learns from Mary that the hospitalist will discharge her that day. The hospitalist reviews the list of ACS medications and realizes that Mary still has not started a beta blocker. He cannot reach the cardiologist before Mary's ride home arrives, so he writes a note in the discharge summary alerting the primary care physician (PCP) to consider a beta blocker at follow‐up. Because of this lack of communication and systems for tracking the implementation of guideline‐recommended therapies, Mary is discharged without a CMS core measure medication, with no assurance that this will be addressed by the PCP.
Scenario 2 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. Standard post‐PCI/STEMI orders are in place according to institutional protocol. The hospitalist is able to confirm that all interventions required at admission (aspirin, beta blocker, assessment of smoking status) have occurred by reviewing a well‐structured checklist that includes easy‐to‐read visual cues. The checklist indicates that Mary was counseled about smoking cessation on day 1 of her stay in the CCU. Mary and her physicians and nurses are all aware of the target discharge date and the milestones that must be met prior to discharge (eg, echocardiogram, medication review, education, assessment of mobility, etc). Mary is instructed about each new medication and given educational materials.14 Follow‐up appointments postdischarge are made, and the discharge summary is sent electronically to the PCP. These institution‐specific protocols enhance communication overall and help the hospital meet high standards of patient care.
Special QI Issues in ACS Management for the Hospitalist
Coordination is especially important for patients with ACS because their care is so complex. Seamless transitions promote safe care as the patient moves from the ED, cath lab, recovery unit, medical floor, and discharge through the transition to primary care. Poor communication between clinicians during these transitions may result in delayed or overlooked treatment and other medical errors. Implementing an institutional system of care may overcome communication barriers and help ensure the institution meets its quality benchmarks, such as the CMS core measures. Standard order sets and protocols identify the steps and components needed to manage ACS. At admission, these measures promote early assessment of patient risk, triage to early intervention, medication reconciliation, and communication between stakeholders such as the hospitalist, cardiologist, and the cath lab.15, 16 During hospitalization, they help assure ongoing risk assessment and early consideration of discharge planning, culminating in discharge and the transition back to primary care.
A recent guideline update8 focused attention on the coordination of care between institutions and the critical importance of rapid triage for patients who need primary PCI and transfer from a non‐PCI to a PCI‐capable institution. The decision to transfer rests on multiple factors and requires rapid decision making on the part of clinicians. Time to reperfusion is shown to have a direct effect on patient outcomes. Established protocols within a non‐PCI facility can support timely transfer to a PCI‐capable facility if indicated. Factors such as the patient's mortality risk, the risk of bleeding from fibrinolytic therapy, duration of symptoms, and the time for transport to a PCI facility all must be considered. It is recognized that a regional system of STEMI care best supports collaborative efforts between institutions and community resources that support QI efforts.
Transitions in care, and particularly discharge, are areas with identified gaps in quality care17, 18 for which improvement has been pursued on an institutional level. Project BOOST (Better Outcomes for Older Adults Through Safe Transitions) seeks to improve the care of patients during the transition from inpatient to outpatient care, and focuses on elderly patients identified to be at high‐risk for adverse events during this transition.19 The goal is to improve outcomes related to 30‐day readmission rates, patient satisfaction, communication between inpatient and outpatient providers, identification of high‐risk patients who need intervention to reduce risk, and patient education about their risk for an adverse event. BOOST addresses these outcomes at an institutional level by offering resources related to project management, data collection, tools for clinicians and patients, and participating mentor institutions. These resources help an institution assess its readiness for change, identify quality gaps, promote teamwork, and guide the implementation and subsequent evaluation of process improvements. Specific tools for clinicians also support institutional goals for teamwork and communication, creating an environment for safe transitions. Both BOOST19 and the adaptable Transitions Tool from the SHM20 provide a framework for understanding processes that involve multiple departments and stakeholders, breaking complex processes into discrete parts for which quality gaps can be identified and change instituted to improve care. A checklist can also be a useful tool for ensuring specific issues are addressed during transitions in care. SHM developed a checklist for hospitalist use that lists elements of a discharge summary for patients with ACS (Table 4).21
| |
| Diagnoses | Elaborate on details of MI such as location, complications |
| Comorbidities | List, including diabetes, lipids, hypertension, renal disease |
| Medications | Note medication reconciliation, reason for not prescribing core measure medications, titration of any medications |
| Specific medications to address include ACE/ARB inhibitors, aspirin, beta blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) | |
| Procedures | Type of stent (bare‐metal stent, drug‐eluting stent) and stent location |
| Complications (hematoma, transfusion) | |
| If ECHO, note type, ejection fraction; provide copy of ECG | |
| Follow‐up appointment(s) | Primary care, cardiology, others such as cardiac rehabilitation |
| Follow‐up testing | ETT (type, timeframe); ECHO if indicated; laboratory assessments |
| Code status | |
| Activity | |
| Diet | |
| Wound care (eg, groin) | |
| Treatment course | Address cognitive level, discharge LDL, discharge creatinine, INR if on warfarin, LFTs if on statin |
| Copy all providers | |
Staff and patient education is also an area that can benefit from evaluation. Clinicians from multiple disciplines are stakeholders in QI and they should receive education about its purpose and goals. Usually institutions will have a QI methodology in place, and this should be conveyed to the members of the ACS team. Staff education about ACS should be tailored to each specialty, be institution‐specific, current, and comprehensive, and include methods for assessing the learner. Education should be easily available (eg, on the Internet or via an electronic format), interactive, case‐based, and mandatory. For patients, education should be available in languages other than English and identify community resources and opportunities for additional outpatient education. The value of any educational program should be assessed to measure learner participation, satisfaction, and comprehension.
Gathering metrics and generating objective evidence of change is critical to QI; quantifying improvement (or lack thereof) must be done to determine whether the changes implemented improve care and ultimately whether desired outcomes are met. Metrics should be meaningful, associated with standards of care (eg, CMS core measures), and carefully chosen to reflect current practice. CMS core measures are a good target for collecting metrics to assess an institution's performance relative to ACS (Table 3). The Specifications Manual for National and Hospital Inpatient Quality Measures10 from TJC and CMS identifies the data elements needed for reporting. Other metrics not specified as core measures are worthy of measurement because they are considered the standard of care for patients with ACS (Table 5). The metrics shown in Tables 3 and 5 assume that all patients are eligible for core‐measure or standard‐of‐care medications and procedures. Because some measures are contraindicated in some patients, it is more meaningful to measure the percentage of patients without a contraindication who receive the measure. If a measure is contraindicated, the patient's medical record must include supporting documentation indicating why a core measure was not met. To be objective and reduce bias regarding the effectiveness of QI measures, data collection is best done prospectively. If necessary, periodic assessments against performance measures (institutional, government, professional association) should be made to support timely intervention. Run charts can be particularly useful here, measuring change over time to identify trends or an intervention that supported, did not affect, or was a barrier to the desired change.
Case Study (cont)
Scenario 1 (cont)
Mary tells the hospitalist she felt the discharge process was rushed and confusing and that she was dissatisfied with her care overall. Recalling a recent review article on the process for public disclosure of patient ratings related to hospital stay, the hospitalist locates HospitalCompare.com on the Internet. He reviews results from patient satisfaction surveys that compare his institution with others in the geographic area and is surprised to discover that patients generally give his institution a poor rating as well as low marks for the quality of nursing and physicianpatient communication. He is interested in this information but is not aware of resources for further exploration.
Scenario 2 (cont)
At discharge, the hospitalist confirms with Mary that she has received smoking cessation counseling during her hospital stay; he documents this in her chart and discharge summary. The hospitalist was aware of this particular quality measure because the recent weekly score card of hospital performance, posted in the unit, reported that the hospital was not meeting its goal of 100% compliance for this CMS core measure. Among heart attack patients who were identified as smokers, only 80% of charts documented that the patient had been counseled about smoking cessation during the hospital stay. Mary says that she understands the importance of not smoking and says she will make an effort to stop.
| Standard of Care Measure | Sample Metric |
|---|---|
| |
| LDL‐cholesterol assessment | Percentage of patients who have LDL cholesterol measured during hospitalization |
| Lipid‐lowering therapy at discharge | Percentage of patients prescribed a statin at hospital discharge |
| Dietary consultation | Percentage of patients who receive a dietary consult during hospitalization |
| Time to receipt of high‐risk abnormal laboratory assessments | Median time to receipt of high‐risk laboratory results, eg, troponins |
| Cardiac risk assessment | Percentage of patients who receive a cardiac risk assessment during admission |
| Measurement of LVEF | Percentage of patients who receive a cardiac echocardiogram to measure of LVEF before discharge |
| Document communication with PCP | Percentage of patients whose communication with the PCP was documented at discharge |
| Completed medication reconciliation | Percentage of patients for whom medication reconciliation was documented by the time of discharge |
| Make 1‐week follow‐up appointment with PCP | Percentage of patients for whom a 1‐week follow‐up appointment with the PCP was documented at the time of discharge |
| Additional Measure | |
| Inpatient mortality | |
Conclusion
Each hospitalist can have an impact on ACS care systemwide. Hospitalists are on the front line of care and have a unique perspective on patients as they are transitioned through the hospital stay and on how an institution handles patient care overall. They experience firsthand the challenges presented by poor communication between providers, patients, and their families. They can offer breadth of experience and perspective when assessing processes linked to patient care and can be instrumental in ensuring each patient experiences safe transitions during the hospital stay. Hospitalists should participate in QI initiatives for ACS and should consider opportunities to take the lead on these initiatives within their institutions.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in the preparation of this manuscript.
Addressing quality improvement (QI) for the management of acute coronary syndrome (ACS) at the institutional level is essential for supporting hospitalists and other clinicians as they manage patients with ACS and achieve desired institutional outcomes. This systems approach may identify institution‐specific barriers to quality care, including those that affect the complex management of ACS. Having a firsthand view of patient care puts the hospitalist in a good position to assess the viability of existing processes and protocols that support care. Indeed, the hospitalist has a vested interest in improving systems of care as these systems directly affect the hospitalist's practice. This unique perspective gives the hospitalist an opportunity to facilitate systems change within the institution and to become an integral participant or leader in QI initiatives.
An increasing number of hospitalists are providing critical care at secondary and tertiary care facilities, driven by a shortage of intensivists in the United States. In a 20052006 survey about 75% of hospitalists reported they provide critical care services as part of their practice,1 and this would include care of patients with ACS. The Society of Hospital Medicine (SHM) has developed core competencies that recognize the important role of hospitalists in leading or participating in QI teams for ACS.2 Hospitalists must also be able to apply evidenced‐based outcomes data to support these initiatives.3 Hospitalist competencies for ACS include protocol development that supports the timely diagnosis and treatment of ACS, evaluation of resource utilization, staff education of secondary prevention measures, and implementation of measures to ensure institutional compliance with national quality standards (Table 1).2 Most hospital medicine groups will be expected to contribute to systems improvement, an area where hospitalists have already shown leadership for QI protocols related to glycemic control and venous thromboembolism prophylaxis. Hospitalists were prominent in targeting QI in these areas even though these QI initiatives could easily have been spearheaded by specialists.46
|
| Lead, coordinate, or participate in: |
| Protocol development to rapidly identify ACS, minimizing time to intervention |
| Protocol development for rapid identification and transfer of patients with ACS to a facility with an appropriate level of care |
| Multidisciplinary initiatives, including order sets for ACS and chest pain, that promote patient safety and optimize the use of resources |
| Staff education initiatives on the value of smoking cessation counseling and other prevention measures |
| Implement or integrate: |
| Systems to ensure hospitalwide adherence to national standards, documenting adherence as required by certifying organizations |
| Outcomes research, institution‐specific laboratory policies, and hospital formulary to create indicated and cost‐effective diagnostic and management strategies for patients with ACS |
QI Basics
QI at the institutional level addresses systems of care rather than individual performance, targeting both institutional performance and use of resources.3 QI is a continuous process in which practices and procedures related to patient management are regularly assessed to ascertain whether a quality gap exists. This in turn may lead to new processes, protocols, and algorithms that help the institution and clinicians meet benchmarks of quality care.
QI starts when an existing gap is recognizedthe gap between the scientific understanding of optimal care and actual patient care. The goal is to narrow or close this gap so that each patient receives optimal care. Underlying any QI initiative are 2 essential concepts. First, improvement requires systems changeany system will produce exactly what it is designed to produce. For example, if procedures are not in place to educate patients about smoking cessation while they are hospitalized, it is unlikely that the majority will routinely receive this counseling before they are discharged. Second, less is moreproductivity is not destroyed but often is enhanced by initiating simple and practical change. If a patient arrives in the emergency department (ED) with chest pain, instituting an order set that reminds clinicians to start antiplatelet therapy or a beta blocker can lessen the chance that these medications will be overlooked, especially when the patient transitions between providers or services within the hospital.
SHM has identified 7 essential elements of any QI initiative, and these are applicable to the care of the ACS patient (Table 2).7 These elements highlight the need for institutional support and teamwork that support standardized measures and tools specific to issues in ACS management. These issues include: (1) rapidly identifying a patient with ACS and initiating a care plan when the patient is admitted; (2) encouraging good communication between providers; (3) symptom management; (4) medication safety, polypharmacy, and medication reconciliation; (5) patient and caregiver education; (6) safe discharge and transitions in care; and (7) meeting Centers for Medicare and Medicaid Services (CMS) core measures.
| |
| Institutional support | Commitment of time, personnel, and tools to support the initiative |
| Multidisciplinary team | Team that focuses on quality of care for patients with ACS |
| Reliable metrics | Reflect CMS core and applicable PQRI measures; also reportable to inform team decision making |
| Identify the goal | Establish a measurable, achievable goal with an established timeline |
| Standard order sets | Defined clinical pathways that support evidence‐based treatment strategies, risk stratification, and safe transitions in care |
| Policies that support algorithms and protocols | Institution‐specific to support order sets |
| Education programs | Targeted to clinicians and patients; should cover items addressed in order sets, algorithms, and protocols |
Tools such as process flow mapping and run charts can reveal quality gaps and indicate if process improvements are leading to stated objectives. Process flow mapping makes it possible to identify and visualize quality gaps that might otherwise be hidden and to identify their source or cause. Process mapping documents discrete steps within the flow and usually requires input from multiple disciplines; this information can guide a multidisciplinary QI team when formulating interventions for process improvement.7 Figure 1 shows process flow mapping for the early identification of ST‐segment elevation myocardial infarction (STEMI) when hospitalists have open access to activate the catheterization laboratory (cath lab). The time from door‐to‐balloon is a critical factor in reducing STEMI‐related morbidity8; processes that overcome delays to percutaneous coronary intervention (PCI) and improve communication can have a direct benefit on patient outcomes.
A run chart is a commonly used tool which graphically depicts progress in attaining a goal over time, before and after an intervention. Figure 2a is a run chart that shows the average time to PCI following implementation of an order set designed to support the use of a risk stratification tool for the early diagnosis of STEMI. In this case, the average time to PCI is observed to decrease over time, but still lags behind the desired goal of less than 90 minutes. This run chart indicates that further work is needed to improve the process of identifying patients with STEMI. Figure 2b shows the number of eligible STEMI patients who received aspirin at discharge following implementation of a discharge order set; here, the hospital has clearly made progress toward meeting this CMS core measure.
The following is a case study that illustrates how the implementation of standardized measures and tools can help hospitalists and other clinicians achieve quality measures in the care of a patient with ACS.
Case Study
Mary, a 68‐year‐old woman, presents to the ED with fatigue and some heartburn. She has a history of hypertension and may have had a mini stroke a few years ago. Her symptoms, which she has had on and off for the past few days, worsened considerably right before her arrival. She has been taking chewable antacids but is unsure if they have helped. Her physical exam is unremarkable. A stat electrocardiogram (ECG) shows inferior ST (part of an electrocardiogram between the QRS complex and the T wave) elevation in leads II and III, and augmented vector foot (aVF). Troponins are positive. This case can be approached from 2 perspectives.
Scenario 1
Mary arrives at a hospital that has few standardized systems or protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG, but fails to alert the ED physician. When the ED physician eventually sees the patient and reviews the ECG, she immediately administers nitroglycerin and pages the cardiologist on call and the hospitalist. The hospitalist arrives first and recognizes the STEMI, but hesitates to start unfractionated or low molecular weight heparin until the cardiologist determines whether the patient will undergo PCI. The cardiologist orders PCI, the cath lab is alerted, and the patient is started on the appropriate medications; the patient does not start an aspirin until after PCI. In this scenario, several short delays amount to a significant delay of about 2 hours before the patient reaches the cath lab. In addition, although aspirin is given on day 1, it is not done on arrival. Following PCI, the patient is transferred to the coronary care unit (CCU).
Scenario 2
Mary arrives at an institution with well‐defined, institution‐specific protocols for triage and transitions in care. The triage nurse recognizes the need for and obtains an ECG; the results are immediately reviewed with the ED physician. STEMI is diagnosed and the cath lab protocol is activated; the patient receives aspirin as part of a standing order. The hospitalist meets the patient in the ED within 5 minutes and begins the protocol for unfractionated heparin and preparation for immediate PCI, allowing the ED physician to return to ED care. Simultaneously, the interventional cardiologist and cath lab are mobilized and the patient is transferred within 15 minutes. Additional appropriate medications are begun. The door‐to‐balloon time is 60 minutes, well within recommended timeframes. Following PCI, the patient is transferred to the CCU.
Measuring Performance Relative to ACS
Two agencies promulgating quality measures for hospital inpatient care are The Joint Commission (TJC) and the CMS. TJC and CMS jointly established core measures for patients with acute myocardial infarction (AMI) and these are considered key indicators of quality, evidence‐based care. As outlined in Table 3, the TJC/CMS recommendations promote, unless contraindicated, a minimum standard of care for patients with AMI.9, 10 Public reporting of institutional core measure performance has led to an intense focus on improving these metrics.
| Core Measure | Sample Metric |
|---|---|
| |
| Aspirin at arrival | Percentage of patients receiving aspirin within 24 hours before or after hospital arrival |
| Aspirin at discharge | Percentage of patients prescribed aspirin at hospital discharge |
| ACE inhibitor or ARB for LVSD | Percentage of patients with LVSD prescribed an ACEI or ARB at hospital discharge |
| Beta blocker | Percentage of patients prescribed a beta blocker at hospital discharge |
| Fibrinolytic medication given within 30 minutes of hospital arrival | Median time to fibrinolysis |
| Percentage of patients given fibrinolytic medication within 30 minutes of hospital arrival | |
| PCI received within 90 minutes of hospital arrival | Median time to PCI |
| Percentage of patients receiving primary PCI within 90 minutes of hospital arrival | |
| Smoking cessation counseling | Percentage of patients with a history of smoking cigarettes who are counseled about smoking cessation during hospitalization |
On a national level, TJC documented performance improvement from 2002 to 2008 for each of the core measures. Compliance with smoking cessation counseling improved the most, rising from 67% to almost 99%. In 2008, a combined measure of all individual core measures indicated that, overall, care of heart attack patients is of high quality. Hospitals delivered evidenced‐based care in 96.7% of the opportunities they had to provide this care. Compliance related to oral medications was also good (95%); however, a closer look at other individual measures shows that improvement is needed to reduce the time to fibrinolysis (52.4% compliance rate for 30 minutes or less) and time to primary PCI (81.6% compliance rate for 90 minutes or less).11
Financial incentives are tied to QI measures including those from CMS. At present, this system is in the pay‐for‐reporting phase, in which institutions are penalized for not reporting quality metrics for the CMS core measures. It is likely that, to further incentivize institutions to meet quality benchmarks, this will be expanded to a pay‐for‐performance system (eg, differential payments for readmissions or different payment scales based on prior performance). Public disclosure of institutional performance relative to ACS and other medical conditions is available through the HHS.gov website (www.hospitalcompare.hhs.gov), which compares performance between hospitals and provides a clear business motivation for institutions to improve and provide high quality care.
Two other reporting systems should be noted. The CMS Physician Quality Reporting Initiative (PQRI) includes physician‐related quality measures specific to ACS12 that overlap with institution‐level CMS core measures with regard to prescribing ACS medications. Payments associated with the PQRI are currently a small financial factor for hospitalists, but will likely grow as quality initiatives develop overall. The Hospital Care Quality Information From the Consumer Perspective (HCAHPS) initiative, also from CMS, strives to capture patients' perspectives on hospital care through a standardized survey. The goals are to collect data that can be used to compare hospital performance, create an incentive for QI through public disclosure of results, and increase transparency regarding the quality of hospital care.13 However, the focus is not ACS‐specific. Patients are queried about communication with hospital staff, communication about medications, and information about discharge, all areas of concern for the hospitalist in general that have been identified as areas for improvement relative to ACS.
Case Study (cont)
Scenario 1 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. The hospitalist and cardiologist see her separately on rounds and each assumes the other has a reason for not starting a beta blocker; therefore, a beta blocker is not prescribed. The nurse cannot tell who is in charge and does not anticipate the day of dischargeshe is just implementing the orders as they are written. The day of discharge arrives; the nurse learns from Mary that the hospitalist will discharge her that day. The hospitalist reviews the list of ACS medications and realizes that Mary still has not started a beta blocker. He cannot reach the cardiologist before Mary's ride home arrives, so he writes a note in the discharge summary alerting the primary care physician (PCP) to consider a beta blocker at follow‐up. Because of this lack of communication and systems for tracking the implementation of guideline‐recommended therapies, Mary is discharged without a CMS core measure medication, with no assurance that this will be addressed by the PCP.
Scenario 2 (cont)
Mary recuperates in the CCU and is transferred to the medical floor. Standard post‐PCI/STEMI orders are in place according to institutional protocol. The hospitalist is able to confirm that all interventions required at admission (aspirin, beta blocker, assessment of smoking status) have occurred by reviewing a well‐structured checklist that includes easy‐to‐read visual cues. The checklist indicates that Mary was counseled about smoking cessation on day 1 of her stay in the CCU. Mary and her physicians and nurses are all aware of the target discharge date and the milestones that must be met prior to discharge (eg, echocardiogram, medication review, education, assessment of mobility, etc). Mary is instructed about each new medication and given educational materials.14 Follow‐up appointments postdischarge are made, and the discharge summary is sent electronically to the PCP. These institution‐specific protocols enhance communication overall and help the hospital meet high standards of patient care.
Special QI Issues in ACS Management for the Hospitalist
Coordination is especially important for patients with ACS because their care is so complex. Seamless transitions promote safe care as the patient moves from the ED, cath lab, recovery unit, medical floor, and discharge through the transition to primary care. Poor communication between clinicians during these transitions may result in delayed or overlooked treatment and other medical errors. Implementing an institutional system of care may overcome communication barriers and help ensure the institution meets its quality benchmarks, such as the CMS core measures. Standard order sets and protocols identify the steps and components needed to manage ACS. At admission, these measures promote early assessment of patient risk, triage to early intervention, medication reconciliation, and communication between stakeholders such as the hospitalist, cardiologist, and the cath lab.15, 16 During hospitalization, they help assure ongoing risk assessment and early consideration of discharge planning, culminating in discharge and the transition back to primary care.
A recent guideline update8 focused attention on the coordination of care between institutions and the critical importance of rapid triage for patients who need primary PCI and transfer from a non‐PCI to a PCI‐capable institution. The decision to transfer rests on multiple factors and requires rapid decision making on the part of clinicians. Time to reperfusion is shown to have a direct effect on patient outcomes. Established protocols within a non‐PCI facility can support timely transfer to a PCI‐capable facility if indicated. Factors such as the patient's mortality risk, the risk of bleeding from fibrinolytic therapy, duration of symptoms, and the time for transport to a PCI facility all must be considered. It is recognized that a regional system of STEMI care best supports collaborative efforts between institutions and community resources that support QI efforts.
Transitions in care, and particularly discharge, are areas with identified gaps in quality care17, 18 for which improvement has been pursued on an institutional level. Project BOOST (Better Outcomes for Older Adults Through Safe Transitions) seeks to improve the care of patients during the transition from inpatient to outpatient care, and focuses on elderly patients identified to be at high‐risk for adverse events during this transition.19 The goal is to improve outcomes related to 30‐day readmission rates, patient satisfaction, communication between inpatient and outpatient providers, identification of high‐risk patients who need intervention to reduce risk, and patient education about their risk for an adverse event. BOOST addresses these outcomes at an institutional level by offering resources related to project management, data collection, tools for clinicians and patients, and participating mentor institutions. These resources help an institution assess its readiness for change, identify quality gaps, promote teamwork, and guide the implementation and subsequent evaluation of process improvements. Specific tools for clinicians also support institutional goals for teamwork and communication, creating an environment for safe transitions. Both BOOST19 and the adaptable Transitions Tool from the SHM20 provide a framework for understanding processes that involve multiple departments and stakeholders, breaking complex processes into discrete parts for which quality gaps can be identified and change instituted to improve care. A checklist can also be a useful tool for ensuring specific issues are addressed during transitions in care. SHM developed a checklist for hospitalist use that lists elements of a discharge summary for patients with ACS (Table 4).21
| |
| Diagnoses | Elaborate on details of MI such as location, complications |
| Comorbidities | List, including diabetes, lipids, hypertension, renal disease |
| Medications | Note medication reconciliation, reason for not prescribing core measure medications, titration of any medications |
| Specific medications to address include ACE/ARB inhibitors, aspirin, beta blockers, statin, sublingual NTG, clopidogrel (include duration of therapy) | |
| Procedures | Type of stent (bare‐metal stent, drug‐eluting stent) and stent location |
| Complications (hematoma, transfusion) | |
| If ECHO, note type, ejection fraction; provide copy of ECG | |
| Follow‐up appointment(s) | Primary care, cardiology, others such as cardiac rehabilitation |
| Follow‐up testing | ETT (type, timeframe); ECHO if indicated; laboratory assessments |
| Code status | |
| Activity | |
| Diet | |
| Wound care (eg, groin) | |
| Treatment course | Address cognitive level, discharge LDL, discharge creatinine, INR if on warfarin, LFTs if on statin |
| Copy all providers | |
Staff and patient education is also an area that can benefit from evaluation. Clinicians from multiple disciplines are stakeholders in QI and they should receive education about its purpose and goals. Usually institutions will have a QI methodology in place, and this should be conveyed to the members of the ACS team. Staff education about ACS should be tailored to each specialty, be institution‐specific, current, and comprehensive, and include methods for assessing the learner. Education should be easily available (eg, on the Internet or via an electronic format), interactive, case‐based, and mandatory. For patients, education should be available in languages other than English and identify community resources and opportunities for additional outpatient education. The value of any educational program should be assessed to measure learner participation, satisfaction, and comprehension.
Gathering metrics and generating objective evidence of change is critical to QI; quantifying improvement (or lack thereof) must be done to determine whether the changes implemented improve care and ultimately whether desired outcomes are met. Metrics should be meaningful, associated with standards of care (eg, CMS core measures), and carefully chosen to reflect current practice. CMS core measures are a good target for collecting metrics to assess an institution's performance relative to ACS (Table 3). The Specifications Manual for National and Hospital Inpatient Quality Measures10 from TJC and CMS identifies the data elements needed for reporting. Other metrics not specified as core measures are worthy of measurement because they are considered the standard of care for patients with ACS (Table 5). The metrics shown in Tables 3 and 5 assume that all patients are eligible for core‐measure or standard‐of‐care medications and procedures. Because some measures are contraindicated in some patients, it is more meaningful to measure the percentage of patients without a contraindication who receive the measure. If a measure is contraindicated, the patient's medical record must include supporting documentation indicating why a core measure was not met. To be objective and reduce bias regarding the effectiveness of QI measures, data collection is best done prospectively. If necessary, periodic assessments against performance measures (institutional, government, professional association) should be made to support timely intervention. Run charts can be particularly useful here, measuring change over time to identify trends or an intervention that supported, did not affect, or was a barrier to the desired change.
Case Study (cont)
Scenario 1 (cont)
Mary tells the hospitalist she felt the discharge process was rushed and confusing and that she was dissatisfied with her care overall. Recalling a recent review article on the process for public disclosure of patient ratings related to hospital stay, the hospitalist locates HospitalCompare.com on the Internet. He reviews results from patient satisfaction surveys that compare his institution with others in the geographic area and is surprised to discover that patients generally give his institution a poor rating as well as low marks for the quality of nursing and physicianpatient communication. He is interested in this information but is not aware of resources for further exploration.
Scenario 2 (cont)
At discharge, the hospitalist confirms with Mary that she has received smoking cessation counseling during her hospital stay; he documents this in her chart and discharge summary. The hospitalist was aware of this particular quality measure because the recent weekly score card of hospital performance, posted in the unit, reported that the hospital was not meeting its goal of 100% compliance for this CMS core measure. Among heart attack patients who were identified as smokers, only 80% of charts documented that the patient had been counseled about smoking cessation during the hospital stay. Mary says that she understands the importance of not smoking and says she will make an effort to stop.
| Standard of Care Measure | Sample Metric |
|---|---|
| |
| LDL‐cholesterol assessment | Percentage of patients who have LDL cholesterol measured during hospitalization |
| Lipid‐lowering therapy at discharge | Percentage of patients prescribed a statin at hospital discharge |
| Dietary consultation | Percentage of patients who receive a dietary consult during hospitalization |
| Time to receipt of high‐risk abnormal laboratory assessments | Median time to receipt of high‐risk laboratory results, eg, troponins |
| Cardiac risk assessment | Percentage of patients who receive a cardiac risk assessment during admission |
| Measurement of LVEF | Percentage of patients who receive a cardiac echocardiogram to measure of LVEF before discharge |
| Document communication with PCP | Percentage of patients whose communication with the PCP was documented at discharge |
| Completed medication reconciliation | Percentage of patients for whom medication reconciliation was documented by the time of discharge |
| Make 1‐week follow‐up appointment with PCP | Percentage of patients for whom a 1‐week follow‐up appointment with the PCP was documented at the time of discharge |
| Additional Measure | |
| Inpatient mortality | |
Conclusion
Each hospitalist can have an impact on ACS care systemwide. Hospitalists are on the front line of care and have a unique perspective on patients as they are transitioned through the hospital stay and on how an institution handles patient care overall. They experience firsthand the challenges presented by poor communication between providers, patients, and their families. They can offer breadth of experience and perspective when assessing processes linked to patient care and can be instrumental in ensuring each patient experiences safe transitions during the hospital stay. Hospitalists should participate in QI initiatives for ACS and should consider opportunities to take the lead on these initiatives within their institutions.
Acknowledgements
The author thanks Denise Erkkila, RPh for her editorial assistance in the preparation of this manuscript.
- Hospitalists and intensivists: partners in caring for the critically ill—the time has come.J Hosp Med.2010;5:1–3.
- Society of Hospital Medicine. Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- Society of Hospital Medicine. Quality improvement.J Hosp Med.2006;1 (suppl):92.
- ,,, et al.Curriculum development: the venous thromboembolism quality improvement resource room.J Hosp Med.2006;1:124–132.
- ,,,,Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3:66–75.
- ,,,Effects of a subcutaneous insulin protocol, clinical education, and computerized order set on the quality of inpatient management of hyperglycemia: results of a clinical trial.J Hosp Med.2009;4:16–27.
- SHM Acute Coronary Syndrome Advisory Board. A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org. 2010. Accessed July 2010.
- ,,, et al.2009focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.year="2009"2009;54:2205–2241.
- The Joint Commission. Performance measure intiatives. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Acute+Myocardial+Infarction+Core+Measure+Set.htm. 2010. Accessed July 2010.
- The Joint Commission, Centers for Medicare and Medicare Services. Specifications manual for national hospital inpatient quality measures, version 2.5. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Current+NHQM+Manual.htm. 2009 November 6. Accessed July 2010.
- The Joint Commission. Improving America's hospitals: The Joint Commission's annual report on quality and safety 2009. Available at: http://www.jointcommission.org/Library/annual_report.2009. Accessed July 2010.
- Centers for Medicare and Medicare Services. Physician quality reporting initiative (PQRI). Available at: http://www.cms.hhs.gov/pqri. 2010. Accessed July 2010.
- Hospital Care Quality Information from the Consumer Perspective. CAHPS hospital survey. Available at: http://www.hcahpsonline.org. 2010. Accessed July 2010.
- ,,,.Discharge education improves clinical outcomes in patients with chronic heart failure.Circulation.2005;111:179–185.
- ,,, et al.National efforts to improve door‐to‐balloon time results from the Door‐to‐Balloon Alliance.J Am Coll Cardiol.2009;54:2423–2429.
- ,,, et al.Sustaining improvement in door‐to‐balloon time over 4 years: the Mayo clinic ST‐elevation myocardial infarction protocol.Circ Cardiovasc Qual Outcomes.2009;2:508–513.
- ,,,Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- Society of Hospital Medicine. Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. 2010. Accessed July 2010.
- SHM ACS Transitions Workgroup. SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm. 2010. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients‐‐development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- Hospitalists and intensivists: partners in caring for the critically ill—the time has come.J Hosp Med.2010;5:1–3.
- Society of Hospital Medicine. Acute coronary syndrome.J Hosp Med.2006;1(suppl 1):2–3.
- Society of Hospital Medicine. Quality improvement.J Hosp Med.2006;1 (suppl):92.
- ,,, et al.Curriculum development: the venous thromboembolism quality improvement resource room.J Hosp Med.2006;1:124–132.
- ,,,,Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts.J Hosp Med.2008;3:66–75.
- ,,,Effects of a subcutaneous insulin protocol, clinical education, and computerized order set on the quality of inpatient management of hyperglycemia: results of a clinical trial.J Hosp Med.2009;4:16–27.
- SHM Acute Coronary Syndrome Advisory Board. A guide for effective quality improvement: improving acute coronary syndrome care for hospitalized patients. Available at: http://www.hospitalmedicine.org. 2010. Accessed July 2010.
- ,,, et al.2009focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol.year="2009"2009;54:2205–2241.
- The Joint Commission. Performance measure intiatives. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Acute+Myocardial+Infarction+Core+Measure+Set.htm. 2010. Accessed July 2010.
- The Joint Commission, Centers for Medicare and Medicare Services. Specifications manual for national hospital inpatient quality measures, version 2.5. Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Current+NHQM+Manual.htm. 2009 November 6. Accessed July 2010.
- The Joint Commission. Improving America's hospitals: The Joint Commission's annual report on quality and safety 2009. Available at: http://www.jointcommission.org/Library/annual_report.2009. Accessed July 2010.
- Centers for Medicare and Medicare Services. Physician quality reporting initiative (PQRI). Available at: http://www.cms.hhs.gov/pqri. 2010. Accessed July 2010.
- Hospital Care Quality Information from the Consumer Perspective. CAHPS hospital survey. Available at: http://www.hcahpsonline.org. 2010. Accessed July 2010.
- ,,,.Discharge education improves clinical outcomes in patients with chronic heart failure.Circulation.2005;111:179–185.
- ,,, et al.National efforts to improve door‐to‐balloon time results from the Door‐to‐Balloon Alliance.J Am Coll Cardiol.2009;54:2423–2429.
- ,,, et al.Sustaining improvement in door‐to‐balloon time over 4 years: the Mayo clinic ST‐elevation myocardial infarction protocol.Circ Cardiovasc Qual Outcomes.2009;2:508–513.
- ,,,Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,.Lost in transition: challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;141:533–536.
- Society of Hospital Medicine. Boosting Care Transitions Resource Room. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. 2010. Accessed July 2010.
- SHM ACS Transitions Workgroup. SHM ACS Transitions Tool. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_ACS/html_ACS/12ClinicalTools/05_Transitions.cfm. 2010. Accessed July 2010.
- ,,, et al.Transition of care for hospitalized elderly patients‐‐development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.