User login
Team creates guidelines on CAR T-cell-related toxicity
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies. ![]()
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies. ![]()
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies. ![]()
Antibody shows early promise in AML/MDS trial
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year. ![]()
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year. ![]()
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year. ![]()
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.
New toolkit can help nurses use genomics in patient care
The National Human Genome Research Institute (NHGRI) has created an online toolkit to help nurses integrate genomics into patient care.
The Method for Introducing a New Competency Genomics (MINC) website provides resources for nursing leaders at all levels of genomics competency, ranging from basic knowledge about genomics to its practical impact on healthcare systems and policies.
The resources are intended to help practicing nurses care for patients undergoing genomic testing and treatments, build awareness in their communities, and understand how to prepare their workforce for emerging clinical applications.
“The MINC toolkit is a starting point for healthcare providers who want to promote genomic integration into practice to benefit their patients,” said Laura Lyman Rodriguez, PhD, director of the Division of Policy, Communication and Education at NHGRI.
“It was designed based on the efforts of magnet hospital nurses whose experiences were used in the design and foundation for the toolkit.”
The toolkit is structured in a question and answer format, allowing users to tailor their interventions based on the resources that will work best for them in their clinical setting.
A key feature of the toolkit is “Champion Stories.” These video testimonials from health administrators and educators describe how they overcame barriers as they developed the necessary genomics knowledge to offer personalized care to their patients. ![]()
The National Human Genome Research Institute (NHGRI) has created an online toolkit to help nurses integrate genomics into patient care.
The Method for Introducing a New Competency Genomics (MINC) website provides resources for nursing leaders at all levels of genomics competency, ranging from basic knowledge about genomics to its practical impact on healthcare systems and policies.
The resources are intended to help practicing nurses care for patients undergoing genomic testing and treatments, build awareness in their communities, and understand how to prepare their workforce for emerging clinical applications.
“The MINC toolkit is a starting point for healthcare providers who want to promote genomic integration into practice to benefit their patients,” said Laura Lyman Rodriguez, PhD, director of the Division of Policy, Communication and Education at NHGRI.
“It was designed based on the efforts of magnet hospital nurses whose experiences were used in the design and foundation for the toolkit.”
The toolkit is structured in a question and answer format, allowing users to tailor their interventions based on the resources that will work best for them in their clinical setting.
A key feature of the toolkit is “Champion Stories.” These video testimonials from health administrators and educators describe how they overcame barriers as they developed the necessary genomics knowledge to offer personalized care to their patients. ![]()
The National Human Genome Research Institute (NHGRI) has created an online toolkit to help nurses integrate genomics into patient care.
The Method for Introducing a New Competency Genomics (MINC) website provides resources for nursing leaders at all levels of genomics competency, ranging from basic knowledge about genomics to its practical impact on healthcare systems and policies.
The resources are intended to help practicing nurses care for patients undergoing genomic testing and treatments, build awareness in their communities, and understand how to prepare their workforce for emerging clinical applications.
“The MINC toolkit is a starting point for healthcare providers who want to promote genomic integration into practice to benefit their patients,” said Laura Lyman Rodriguez, PhD, director of the Division of Policy, Communication and Education at NHGRI.
“It was designed based on the efforts of magnet hospital nurses whose experiences were used in the design and foundation for the toolkit.”
The toolkit is structured in a question and answer format, allowing users to tailor their interventions based on the resources that will work best for them in their clinical setting.
A key feature of the toolkit is “Champion Stories.” These video testimonials from health administrators and educators describe how they overcame barriers as they developed the necessary genomics knowledge to offer personalized care to their patients. ![]()
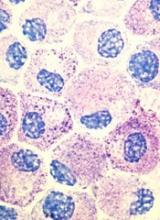
Murine study provides new insight into hematopoiesis
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Trials of atezolizumab placed on partial hold
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
EMA issues final opinion on FVIII products
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.
CHMP recommends approval of generic imatinib
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended granting marketing authorization for Imatinib Teva B.V., a generic of Glivec.
The recommendation is that Imatinib Teva B.V. be approved to treat chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), hypereosinophilic syndrome (HES), chronic eosinophilic leukemia (CEL), myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPNs), gastrointestinal stromal tumors (GIST), and dermatofibrosarcoma protuberans (DFSP).
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The European Commission’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
If approved, Imatinib Teva B.V. will be available as capsules and film-coated tablets (100 mg and 400 mg). And it will be authorized:
- As monotherapy for pediatric patients with newly diagnosed, Philadelphia-chromosome-positive (Ph+) CML for whom bone marrow transplant is not considered the first line of treatment.
- As monotherapy for pediatric patients with Ph+ CML in chronic phase after failure of interferon-alpha therapy or in accelerated phase or blast crisis.
- As monotherapy for adults with Ph+ CML in blast crisis.
- Integrated with chemotherapy to treat adult and pediatric patients with newly diagnosed, Ph+ ALL.
- As monotherapy for adults with relapsed or refractory Ph+ ALL.
- As monotherapy for adults with MDS/MPNs associated with platelet-derived growth factor receptor gene re-arrangements.
- As monotherapy for adults with advanced HES and/or CEL with FIP1L1-PDGFRα rearrangement.
- As monotherapy for adults with Kit- (CD117-) positive, unresectable and/or metastatic malignant GISTs.
- For the adjuvant treatment of adults who are at significant risk of relapse following resection of Kit-positive GIST. Patients who have a low or very low risk of recurrence should not receive adjuvant treatment.
- As monotherapy for adults with unresectable DFSP and adults with recurrent and/or metastatic DFSP who are not eligible for surgery.
The CHMP said studies have demonstrated the satisfactory quality of Imatinib Teva B.V. and its bioequivalence to the reference product, Glivec.
In adult and pediatric patients, the effectiveness of imatinib is based on:
- Overall hematologic and cytogenetic response rates and progression-free survival in CML
- Hematologic and cytogenetic response rates in Ph+ ALL and MDS/MPNs
- Hematologic response rates in HES/CEL
- Objective response rates in adults with unresectable and/or metastatic GIST and DFSP
- Recurrence-free survival in adjuvant GIST.
The experience with imatinib in patients with MDS/MPNs associated with PDGFR gene re-arrangements is very limited. There are no controlled trials demonstrating a clinical benefit or increased survival for these diseases.
CHMP advocates refusal of application for SM drug
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended refusal of the marketing authorization for masitinib (Masipro).
Masitinib is a tyrosine kinase inhibitor being developed by AB Science to treat adults with smoldering or indolent severe systemic mastocytosis (SM).
To support the application for masitinib, AB Science presented data from a study involving 135 SM patients who had severe symptoms, including at least one of the following: itching, hot flashes, depression, and tiredness.
Researchers compared masitinib to placebo in these patients, looking for improvements in any of the symptoms during the first 24 weeks of treatment.
The CHMP said it was concerned about the reliability of the study results because a routine good clinical practice inspection at the study sites revealed serious failings in the way the study had been conducted.
In addition, major changes were made to the study design while the study was underway, which made the results difficult to interpret.
Finally, data on the safety of masitinib were limited. And the CHMP was concerned about side effects, including neutropenia and harmful effects on the skin and liver, which were particularly relevant because masitinib was intended to be used long-term.
Therefore, the CHMP concluded the benefits of masitinib do not appear to outweigh the risks, and the committee recommended the drug be refused marketing authorization.
The CHMP informed AB Science of this negative opinion in May, and the company asked the committee to re-examine its opinion. However, the CHMP ultimately concluded that masitinib should be refused marketing authorization.
AB Science said this decision does not have any consequences for patients in clinical trials or compassionate use programs of masitinib.
The company also said it intends to initiate a confirmatory study in patients with smoldering or indolent severe SM that is unresponsive to optimal symptomatic treatment in order to confirm the results from the first pivotal study.
Application for pegfilgrastim biosimilar withdrawn
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017.
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017.
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017.
CHMP recommends approval of nilotinib for kids
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the authorized use for nilotinib (Tasigna) to include pediatric patients.
At present, nilotinib is approved for use in the European Economic Area to treat adults with chronic myeloid leukemia (CML).
The drug is used to treat adults with newly diagnosed, Philadelphia-chromosome-positive (Ph+), chronic phase CML and adults with chronic or accelerated phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
The CHMP has recommended expanding the marketing authorization of nilotinib to include pediatric patients with newly diagnosed, Ph+, chronic phase CML and pediatric patients with chronic phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
Detailed recommendations for the use of nilotinib will be described in the updated summary of product characteristics, which will be published in the revised European public assessment report. It will be available in all official European Union languages after a decision on this change to the marketing authorization has been granted by the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the authorized use for nilotinib (Tasigna) to include pediatric patients.
At present, nilotinib is approved for use in the European Economic Area to treat adults with chronic myeloid leukemia (CML).
The drug is used to treat adults with newly diagnosed, Philadelphia-chromosome-positive (Ph+), chronic phase CML and adults with chronic or accelerated phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
The CHMP has recommended expanding the marketing authorization of nilotinib to include pediatric patients with newly diagnosed, Ph+, chronic phase CML and pediatric patients with chronic phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
Detailed recommendations for the use of nilotinib will be described in the updated summary of product characteristics, which will be published in the revised European public assessment report. It will be available in all official European Union languages after a decision on this change to the marketing authorization has been granted by the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the authorized use for nilotinib (Tasigna) to include pediatric patients.
At present, nilotinib is approved for use in the European Economic Area to treat adults with chronic myeloid leukemia (CML).
The drug is used to treat adults with newly diagnosed, Philadelphia-chromosome-positive (Ph+), chronic phase CML and adults with chronic or accelerated phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
The CHMP has recommended expanding the marketing authorization of nilotinib to include pediatric patients with newly diagnosed, Ph+, chronic phase CML and pediatric patients with chronic phase, Ph+ CML with resistance or intolerance to prior therapy, including imatinib.
Detailed recommendations for the use of nilotinib will be described in the updated summary of product characteristics, which will be published in the revised European public assessment report. It will be available in all official European Union languages after a decision on this change to the marketing authorization has been granted by the European Commission (EC).
The EC typically adheres to the CHMP’s recommendations and delivers its final decision within 67 days of the CHMP’s recommendation.
The EC’s decision will be applicable to the entire European Economic Area—all member states of the European Union plus Iceland, Liechtenstein, and Norway.