User login
Method may help MM patients avoid bone marrow biopsies
Engineers say they have devised a microfluidic technique to capture and count circulating plasma cells from small samples of blood.
They believe the technique, described in Scientific Reports, may allow patients with multiple myeloma (MM) to avoid bone marrow biopsies in favor of conventional blood draws.
“Procedures of the traditional tissue biopsy are painful, associated with complications such as potential infections, and often available only in central hospitals, which require patients to travel long distances,” said Mohammad Qasaimeh, PhD, of New York University Abu Dhabi in United Arab Emirates.
“Capturing plasma cells from blood samples can serve as a liquid biopsy, which can be performed in clinics as often as required, and serve as a diagnostic and prognostic test during and after chemotherapy treatment. Moreover, captured cells can be used for drug testing and, thus, serve as a tool for personalized medicine.”
About the technique
The current microfluidic technique builds on a design that was developed by George Whitesides, PhD, of Harvard University in Cambridge, Massachusetts.
Dr Whitesides and his colleagues fabricated a microchip, the channel of which they etched with repeating, V-shaped grooves, similar to a herringbone pattern.
The grooves cause any fluid flowing through the microchip to swirl about in eddies, rather passing straight through. The cells within the fluid therefore have a higher chance of making contact with the floor of the device.
Researchers have since reproduced this microfluidic design, coating the microchip’s floor with certain molecules to attract cells of interest.
Qasaimeh and colleagues used the microfluidic herringbone design to capture circulating plasma cells. They coated the channels of a microchip with CD138, an antibody expressed on the membranes of plasma cells.
The team then flowed 1 mL samples of blood through the device. The herringbone grooves circulated the blood in the microfluidic channels, where the antibodies grabbed onto any passing plasma cells and let the rest of the blood flow out of the device.
Once the cells were isolated in the microchip, the researchers could count the cells, as well as determine the kinds of antibodies each cell secretes.
Capturing cells
The researchers tested the device using blood samples from healthy donors as well as MM patients.
The team observed very low numbers of circulating plasma cells in healthy samples—2 to 5 cells per mL of blood—and substantially higher counts in MM patients—45 to 184 cells per mL.
The researchers noted that MM patients in remission also exhibited higher counts of circulating plasma cells—20 to 24 cells per mL—than healthy donors.
Rahit Karnik, PhD, of Massachusetts Institute of Technology in Cambridge, said this device may reveal more subtle information about a patient’s state, even in remission.
“When patients go into remission, their antibody levels can look normal,” Dr Karnik said. “But we detect a level of circulating plasma cells that is above the baseline. It’s hard to tell whether these cells are cancerous, but at least this technique is giving us more information. With the ease of a blood draw, this may enable us to track cancer in a much better way.”
Analyzing antibodies
The researchers also looked at antibodies produced by the plasma cells captured in the device.
The team determined the ratio of plasma cells producing kappa- and lambda-type antibodies and compared them to conventional blood tests for the same antibodies, for both healthy subjects and MM patients.
Both sets of results matched, which validates the microfluidic device’s accuracy.
Next steps
Dr Karnik said, in the future, researchers may use this design to perform genetic tests on the captured cells or look for mutations in the cells that may further characterize MM.
“We can capture and stain these cells in the device, which opens the possibility of studying whether there are new mutations in the cells,” Dr Karnik said.
“With cancers like multiple myeloma, even for patients in remission, cancer can recur. Detecting the level or mutation of plasma cells in blood might provide an early detection method for these patients.” ![]()
Engineers say they have devised a microfluidic technique to capture and count circulating plasma cells from small samples of blood.
They believe the technique, described in Scientific Reports, may allow patients with multiple myeloma (MM) to avoid bone marrow biopsies in favor of conventional blood draws.
“Procedures of the traditional tissue biopsy are painful, associated with complications such as potential infections, and often available only in central hospitals, which require patients to travel long distances,” said Mohammad Qasaimeh, PhD, of New York University Abu Dhabi in United Arab Emirates.
“Capturing plasma cells from blood samples can serve as a liquid biopsy, which can be performed in clinics as often as required, and serve as a diagnostic and prognostic test during and after chemotherapy treatment. Moreover, captured cells can be used for drug testing and, thus, serve as a tool for personalized medicine.”
About the technique
The current microfluidic technique builds on a design that was developed by George Whitesides, PhD, of Harvard University in Cambridge, Massachusetts.
Dr Whitesides and his colleagues fabricated a microchip, the channel of which they etched with repeating, V-shaped grooves, similar to a herringbone pattern.
The grooves cause any fluid flowing through the microchip to swirl about in eddies, rather passing straight through. The cells within the fluid therefore have a higher chance of making contact with the floor of the device.
Researchers have since reproduced this microfluidic design, coating the microchip’s floor with certain molecules to attract cells of interest.
Qasaimeh and colleagues used the microfluidic herringbone design to capture circulating plasma cells. They coated the channels of a microchip with CD138, an antibody expressed on the membranes of plasma cells.
The team then flowed 1 mL samples of blood through the device. The herringbone grooves circulated the blood in the microfluidic channels, where the antibodies grabbed onto any passing plasma cells and let the rest of the blood flow out of the device.
Once the cells were isolated in the microchip, the researchers could count the cells, as well as determine the kinds of antibodies each cell secretes.
Capturing cells
The researchers tested the device using blood samples from healthy donors as well as MM patients.
The team observed very low numbers of circulating plasma cells in healthy samples—2 to 5 cells per mL of blood—and substantially higher counts in MM patients—45 to 184 cells per mL.
The researchers noted that MM patients in remission also exhibited higher counts of circulating plasma cells—20 to 24 cells per mL—than healthy donors.
Rahit Karnik, PhD, of Massachusetts Institute of Technology in Cambridge, said this device may reveal more subtle information about a patient’s state, even in remission.
“When patients go into remission, their antibody levels can look normal,” Dr Karnik said. “But we detect a level of circulating plasma cells that is above the baseline. It’s hard to tell whether these cells are cancerous, but at least this technique is giving us more information. With the ease of a blood draw, this may enable us to track cancer in a much better way.”
Analyzing antibodies
The researchers also looked at antibodies produced by the plasma cells captured in the device.
The team determined the ratio of plasma cells producing kappa- and lambda-type antibodies and compared them to conventional blood tests for the same antibodies, for both healthy subjects and MM patients.
Both sets of results matched, which validates the microfluidic device’s accuracy.
Next steps
Dr Karnik said, in the future, researchers may use this design to perform genetic tests on the captured cells or look for mutations in the cells that may further characterize MM.
“We can capture and stain these cells in the device, which opens the possibility of studying whether there are new mutations in the cells,” Dr Karnik said.
“With cancers like multiple myeloma, even for patients in remission, cancer can recur. Detecting the level or mutation of plasma cells in blood might provide an early detection method for these patients.” ![]()
Engineers say they have devised a microfluidic technique to capture and count circulating plasma cells from small samples of blood.
They believe the technique, described in Scientific Reports, may allow patients with multiple myeloma (MM) to avoid bone marrow biopsies in favor of conventional blood draws.
“Procedures of the traditional tissue biopsy are painful, associated with complications such as potential infections, and often available only in central hospitals, which require patients to travel long distances,” said Mohammad Qasaimeh, PhD, of New York University Abu Dhabi in United Arab Emirates.
“Capturing plasma cells from blood samples can serve as a liquid biopsy, which can be performed in clinics as often as required, and serve as a diagnostic and prognostic test during and after chemotherapy treatment. Moreover, captured cells can be used for drug testing and, thus, serve as a tool for personalized medicine.”
About the technique
The current microfluidic technique builds on a design that was developed by George Whitesides, PhD, of Harvard University in Cambridge, Massachusetts.
Dr Whitesides and his colleagues fabricated a microchip, the channel of which they etched with repeating, V-shaped grooves, similar to a herringbone pattern.
The grooves cause any fluid flowing through the microchip to swirl about in eddies, rather passing straight through. The cells within the fluid therefore have a higher chance of making contact with the floor of the device.
Researchers have since reproduced this microfluidic design, coating the microchip’s floor with certain molecules to attract cells of interest.
Qasaimeh and colleagues used the microfluidic herringbone design to capture circulating plasma cells. They coated the channels of a microchip with CD138, an antibody expressed on the membranes of plasma cells.
The team then flowed 1 mL samples of blood through the device. The herringbone grooves circulated the blood in the microfluidic channels, where the antibodies grabbed onto any passing plasma cells and let the rest of the blood flow out of the device.
Once the cells were isolated in the microchip, the researchers could count the cells, as well as determine the kinds of antibodies each cell secretes.
Capturing cells
The researchers tested the device using blood samples from healthy donors as well as MM patients.
The team observed very low numbers of circulating plasma cells in healthy samples—2 to 5 cells per mL of blood—and substantially higher counts in MM patients—45 to 184 cells per mL.
The researchers noted that MM patients in remission also exhibited higher counts of circulating plasma cells—20 to 24 cells per mL—than healthy donors.
Rahit Karnik, PhD, of Massachusetts Institute of Technology in Cambridge, said this device may reveal more subtle information about a patient’s state, even in remission.
“When patients go into remission, their antibody levels can look normal,” Dr Karnik said. “But we detect a level of circulating plasma cells that is above the baseline. It’s hard to tell whether these cells are cancerous, but at least this technique is giving us more information. With the ease of a blood draw, this may enable us to track cancer in a much better way.”
Analyzing antibodies
The researchers also looked at antibodies produced by the plasma cells captured in the device.
The team determined the ratio of plasma cells producing kappa- and lambda-type antibodies and compared them to conventional blood tests for the same antibodies, for both healthy subjects and MM patients.
Both sets of results matched, which validates the microfluidic device’s accuracy.
Next steps
Dr Karnik said, in the future, researchers may use this design to perform genetic tests on the captured cells or look for mutations in the cells that may further characterize MM.
“We can capture and stain these cells in the device, which opens the possibility of studying whether there are new mutations in the cells,” Dr Karnik said.
“With cancers like multiple myeloma, even for patients in remission, cancer can recur. Detecting the level or mutation of plasma cells in blood might provide an early detection method for these patients.” ![]()
FDA approves drugs more quickly than EMA
The US Food and Drug Administration (FDA) reviews and approves new medicines in a shorter timeframe than the European Medicines Agency (EMA), according to an analysis published in NEJM.
The FDA has faced pressure from the public, politicians, and industry to accelerate review and approval of new medicines.
The FDA’s review process is currently being considered and reexamined as part of negotiations to reauthorize the law that directs funds to the agency—the Prescription Drug User Fee Act—which is due for reauthorization by October 2017.
To inform this debate, a group of researchers compared review times for new drugs approved by the FDA and the EMA between 2011 and 2015.
The results showed that the FDA approved more new drugs than the EMA—170 versus 144—during this time period.
The median review time was 306 days for FDA-approved drugs and 383 days for EMA-approved drugs (P<0.001).
Over the study period, the FDA approved 53 drugs intended to treat cancer/hematologic diseases, and the EMA approved 50. The median review times were 206 days and 379 days, respectively (P<0.001).
The FDA approved 74 orphan drugs, and the EMA approved 36. The median review times were 294 days and 403 days, respectively (P<0.001).
The current analysis is an update to a prior analysis, published in 2012, which showed the FDA approved new medicines more quickly than the EMA and Health Canada.
“The gap we had identified, where the FDA was 2 to 3 months faster, now it’s about 3 to 4 months faster,” said Joseph Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, an author of both studies.
“This is more information that should inform upcoming debates. The FDA is already making decisions quickly, and increasing its regulatory speed shouldn’t be our number-one priority.” ![]()
The US Food and Drug Administration (FDA) reviews and approves new medicines in a shorter timeframe than the European Medicines Agency (EMA), according to an analysis published in NEJM.
The FDA has faced pressure from the public, politicians, and industry to accelerate review and approval of new medicines.
The FDA’s review process is currently being considered and reexamined as part of negotiations to reauthorize the law that directs funds to the agency—the Prescription Drug User Fee Act—which is due for reauthorization by October 2017.
To inform this debate, a group of researchers compared review times for new drugs approved by the FDA and the EMA between 2011 and 2015.
The results showed that the FDA approved more new drugs than the EMA—170 versus 144—during this time period.
The median review time was 306 days for FDA-approved drugs and 383 days for EMA-approved drugs (P<0.001).
Over the study period, the FDA approved 53 drugs intended to treat cancer/hematologic diseases, and the EMA approved 50. The median review times were 206 days and 379 days, respectively (P<0.001).
The FDA approved 74 orphan drugs, and the EMA approved 36. The median review times were 294 days and 403 days, respectively (P<0.001).
The current analysis is an update to a prior analysis, published in 2012, which showed the FDA approved new medicines more quickly than the EMA and Health Canada.
“The gap we had identified, where the FDA was 2 to 3 months faster, now it’s about 3 to 4 months faster,” said Joseph Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, an author of both studies.
“This is more information that should inform upcoming debates. The FDA is already making decisions quickly, and increasing its regulatory speed shouldn’t be our number-one priority.” ![]()
The US Food and Drug Administration (FDA) reviews and approves new medicines in a shorter timeframe than the European Medicines Agency (EMA), according to an analysis published in NEJM.
The FDA has faced pressure from the public, politicians, and industry to accelerate review and approval of new medicines.
The FDA’s review process is currently being considered and reexamined as part of negotiations to reauthorize the law that directs funds to the agency—the Prescription Drug User Fee Act—which is due for reauthorization by October 2017.
To inform this debate, a group of researchers compared review times for new drugs approved by the FDA and the EMA between 2011 and 2015.
The results showed that the FDA approved more new drugs than the EMA—170 versus 144—during this time period.
The median review time was 306 days for FDA-approved drugs and 383 days for EMA-approved drugs (P<0.001).
Over the study period, the FDA approved 53 drugs intended to treat cancer/hematologic diseases, and the EMA approved 50. The median review times were 206 days and 379 days, respectively (P<0.001).
The FDA approved 74 orphan drugs, and the EMA approved 36. The median review times were 294 days and 403 days, respectively (P<0.001).
The current analysis is an update to a prior analysis, published in 2012, which showed the FDA approved new medicines more quickly than the EMA and Health Canada.
“The gap we had identified, where the FDA was 2 to 3 months faster, now it’s about 3 to 4 months faster,” said Joseph Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, an author of both studies.
“This is more information that should inform upcoming debates. The FDA is already making decisions quickly, and increasing its regulatory speed shouldn’t be our number-one priority.” ![]()
Inhibitor produces durable responses in rel/ref iNHL
WASHINGTON, DC—An investigational drug can produce durable responses and has a manageable safety profile in patients with relapsed or refractory indolent non-Hodgkin lymphoma (iNHL), according to researchers.
The drug is copanlisib, an intravenous pan-class I phosphatidylinositol-3-kinase (PI3K) inhibitor.
In the phase 2 CHRONOS-1 trial, copanlisib produced an objective response rate (ORR) of 59.2%, with a complete response (CR) rate of 12%, in patients with relapsed/refractory iNHL.
The median duration of response exceeded 98 weeks.
There were 3 deaths considered related to copanlisib, and the most common treatment-related adverse events (AEs) were transient hyperglycemia and hypertension.
These results were presented at the AACR Annual Meeting 2017 (abstract CT149). The study is supported by Bayer, the company developing copanlisib.
CHRONOS-1 included 141 patients with iNHL. Most (n=104) had follicular lymphoma (FL), 23 had marginal zone lymphoma (MZL), 8 had small lymphocytic lymphoma, and 6 had lymphoplasmacytoid/Waldenstrӧm’s macroglobulinemia.
All patients had relapsed after or were refractory to at least 2 prior lines of therapy, which included both rituximab and an alkylating agent.
For this study, the patients received 60 mg of intravenous copanlisib intermittently on days 1, 8, and 15 of a 28-day cycle.
At the time of analysis, the median duration of treatment was 22 weeks (range, 1-105), and 46 patients were still receiving copanlisib.
Efficacy
For the entire cohort, the ORR was 59.2%. Twelve percent of patients achieved a CR, 47.2% had a partial response (PR), 29.6% had stable disease, and 2.1% had progressive disease.
Among patients with FL, the ORR was 58.7%, the CR rate was 14.4%, and the PR rate was 44.2%.
Among patients with MZL, the ORR was 69.6%, with 8.7% of patients achieving a CR and 60.9% achieving a PR.
For the entire cohort, the estimated median duration of response was 687 days (range, 0-687). For patients with FL, it was 370 days (range, 0-687).
The estimated median progression-free survival was 340 days (range, 0-736), and the median overall survival had not been reached at the time of analysis.
Safety
The most common treatment-related AEs were transient hyperglycemia (all grades, 49%/grade 3+, 40%) and hypertension (all grades, 29%/grade 3+, 23%).
The researchers said other AEs of interest were neutropenia (all grades, 25%/grade 3+, 19%), diarrhea (all grades, 18%/grade 3+, 4%), lung infection (all grades, 14%/grade 3+, 11%), pneumonitis (all grades, 7%/grade 3+, 1.4%), and colitis (0.7%, all grade 3+).
Laboratory AEs of interest were alanine aminotransferase increase (all grades, 23%/grade 1, 19%) and aspartate aminotransferase increase (all grades, 28%/grade 1, 25%).
There were 2 non-fatal opportunistic infections.
There were 6 deaths, and 3 of them were considered related to copanlisib. These 3 deaths were due to lung infection, respiratory failure, and a thromboembolic event.
“[I]nhibition of the PI3K pathway has been shown to be an effective therapeutic strategy in treating indolent lymphomas . . .,” said study investigator Martin Dreyling, MD, of Klinikum der Universität München-Grosshadern in Munich, Germany.
“However, concerns exist about the safety of available oral PI3K inhibitors . . . . The results of CHRONOS-1 demonstrate that intermittent intravenous administration of copanlisib achieved durable efficacy with a manageable safety profile in this difficult-to-treat patient population.” ![]()
WASHINGTON, DC—An investigational drug can produce durable responses and has a manageable safety profile in patients with relapsed or refractory indolent non-Hodgkin lymphoma (iNHL), according to researchers.
The drug is copanlisib, an intravenous pan-class I phosphatidylinositol-3-kinase (PI3K) inhibitor.
In the phase 2 CHRONOS-1 trial, copanlisib produced an objective response rate (ORR) of 59.2%, with a complete response (CR) rate of 12%, in patients with relapsed/refractory iNHL.
The median duration of response exceeded 98 weeks.
There were 3 deaths considered related to copanlisib, and the most common treatment-related adverse events (AEs) were transient hyperglycemia and hypertension.
These results were presented at the AACR Annual Meeting 2017 (abstract CT149). The study is supported by Bayer, the company developing copanlisib.
CHRONOS-1 included 141 patients with iNHL. Most (n=104) had follicular lymphoma (FL), 23 had marginal zone lymphoma (MZL), 8 had small lymphocytic lymphoma, and 6 had lymphoplasmacytoid/Waldenstrӧm’s macroglobulinemia.
All patients had relapsed after or were refractory to at least 2 prior lines of therapy, which included both rituximab and an alkylating agent.
For this study, the patients received 60 mg of intravenous copanlisib intermittently on days 1, 8, and 15 of a 28-day cycle.
At the time of analysis, the median duration of treatment was 22 weeks (range, 1-105), and 46 patients were still receiving copanlisib.
Efficacy
For the entire cohort, the ORR was 59.2%. Twelve percent of patients achieved a CR, 47.2% had a partial response (PR), 29.6% had stable disease, and 2.1% had progressive disease.
Among patients with FL, the ORR was 58.7%, the CR rate was 14.4%, and the PR rate was 44.2%.
Among patients with MZL, the ORR was 69.6%, with 8.7% of patients achieving a CR and 60.9% achieving a PR.
For the entire cohort, the estimated median duration of response was 687 days (range, 0-687). For patients with FL, it was 370 days (range, 0-687).
The estimated median progression-free survival was 340 days (range, 0-736), and the median overall survival had not been reached at the time of analysis.
Safety
The most common treatment-related AEs were transient hyperglycemia (all grades, 49%/grade 3+, 40%) and hypertension (all grades, 29%/grade 3+, 23%).
The researchers said other AEs of interest were neutropenia (all grades, 25%/grade 3+, 19%), diarrhea (all grades, 18%/grade 3+, 4%), lung infection (all grades, 14%/grade 3+, 11%), pneumonitis (all grades, 7%/grade 3+, 1.4%), and colitis (0.7%, all grade 3+).
Laboratory AEs of interest were alanine aminotransferase increase (all grades, 23%/grade 1, 19%) and aspartate aminotransferase increase (all grades, 28%/grade 1, 25%).
There were 2 non-fatal opportunistic infections.
There were 6 deaths, and 3 of them were considered related to copanlisib. These 3 deaths were due to lung infection, respiratory failure, and a thromboembolic event.
“[I]nhibition of the PI3K pathway has been shown to be an effective therapeutic strategy in treating indolent lymphomas . . .,” said study investigator Martin Dreyling, MD, of Klinikum der Universität München-Grosshadern in Munich, Germany.
“However, concerns exist about the safety of available oral PI3K inhibitors . . . . The results of CHRONOS-1 demonstrate that intermittent intravenous administration of copanlisib achieved durable efficacy with a manageable safety profile in this difficult-to-treat patient population.” ![]()
WASHINGTON, DC—An investigational drug can produce durable responses and has a manageable safety profile in patients with relapsed or refractory indolent non-Hodgkin lymphoma (iNHL), according to researchers.
The drug is copanlisib, an intravenous pan-class I phosphatidylinositol-3-kinase (PI3K) inhibitor.
In the phase 2 CHRONOS-1 trial, copanlisib produced an objective response rate (ORR) of 59.2%, with a complete response (CR) rate of 12%, in patients with relapsed/refractory iNHL.
The median duration of response exceeded 98 weeks.
There were 3 deaths considered related to copanlisib, and the most common treatment-related adverse events (AEs) were transient hyperglycemia and hypertension.
These results were presented at the AACR Annual Meeting 2017 (abstract CT149). The study is supported by Bayer, the company developing copanlisib.
CHRONOS-1 included 141 patients with iNHL. Most (n=104) had follicular lymphoma (FL), 23 had marginal zone lymphoma (MZL), 8 had small lymphocytic lymphoma, and 6 had lymphoplasmacytoid/Waldenstrӧm’s macroglobulinemia.
All patients had relapsed after or were refractory to at least 2 prior lines of therapy, which included both rituximab and an alkylating agent.
For this study, the patients received 60 mg of intravenous copanlisib intermittently on days 1, 8, and 15 of a 28-day cycle.
At the time of analysis, the median duration of treatment was 22 weeks (range, 1-105), and 46 patients were still receiving copanlisib.
Efficacy
For the entire cohort, the ORR was 59.2%. Twelve percent of patients achieved a CR, 47.2% had a partial response (PR), 29.6% had stable disease, and 2.1% had progressive disease.
Among patients with FL, the ORR was 58.7%, the CR rate was 14.4%, and the PR rate was 44.2%.
Among patients with MZL, the ORR was 69.6%, with 8.7% of patients achieving a CR and 60.9% achieving a PR.
For the entire cohort, the estimated median duration of response was 687 days (range, 0-687). For patients with FL, it was 370 days (range, 0-687).
The estimated median progression-free survival was 340 days (range, 0-736), and the median overall survival had not been reached at the time of analysis.
Safety
The most common treatment-related AEs were transient hyperglycemia (all grades, 49%/grade 3+, 40%) and hypertension (all grades, 29%/grade 3+, 23%).
The researchers said other AEs of interest were neutropenia (all grades, 25%/grade 3+, 19%), diarrhea (all grades, 18%/grade 3+, 4%), lung infection (all grades, 14%/grade 3+, 11%), pneumonitis (all grades, 7%/grade 3+, 1.4%), and colitis (0.7%, all grade 3+).
Laboratory AEs of interest were alanine aminotransferase increase (all grades, 23%/grade 1, 19%) and aspartate aminotransferase increase (all grades, 28%/grade 1, 25%).
There were 2 non-fatal opportunistic infections.
There were 6 deaths, and 3 of them were considered related to copanlisib. These 3 deaths were due to lung infection, respiratory failure, and a thromboembolic event.
“[I]nhibition of the PI3K pathway has been shown to be an effective therapeutic strategy in treating indolent lymphomas . . .,” said study investigator Martin Dreyling, MD, of Klinikum der Universität München-Grosshadern in Munich, Germany.
“However, concerns exist about the safety of available oral PI3K inhibitors . . . . The results of CHRONOS-1 demonstrate that intermittent intravenous administration of copanlisib achieved durable efficacy with a manageable safety profile in this difficult-to-treat patient population.” ![]()
First fossilized mammalian RBCs, Babesia-type pathogens found
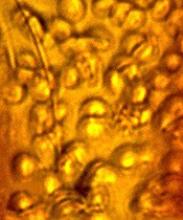
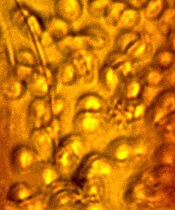
An amber specimen found in the Dominican Republic contained the first fossilized mammalian red blood cells (RBCs) and intraerythrocytic hemoparasites, according to an article published in the Journal of Medical Entomology.
The fossil contained an engorged tick and RBCs infected with parasites that resemble existing members of the Babesiidae and Theileriidae families of the order Piroplasmida.
It appears that 2 small holes in the back of the tick allowed blood to ooze out just as the tick became stuck in tree sap that later fossilized into amber.
“These 2 tiny holes indicate that something picked a tick off the mammal it was feeding on, puncturing it in the process and dropping it immediately into tree sap,” said study author George Poinar, Jr, PhD, of Oregon State University in Corvallis.
“This would be consistent with the grooming behavior of monkeys that we know lived at that time in this region. The fossilized blood cells, infected with these parasites, are simply amazing in their detail. This discovery provides the only known fossils of Babesia-type pathogens.”
Dr Poinar said the amber specimen came from mines located in the Cordillera Septentrional of the Dominican Republic. It may have originated anywhere from 15 to 45 million years ago.
The fossil contained an engorged nymphal tick of the genus Ambylomma. The parasites found in the RBCs were also found in the gut epithelial cells and body cavity of the tick.
“The life forms we find in amber can reveal so much about the history and evolution of diseases we still struggle with today,” Dr Poinar said. “This parasite, for instance, was clearly around millions of years before humans and appears to have evolved alongside primates, among other hosts.”
Part of what makes this fossil unique, Dr Poinar said, is the way in which the parasites and RBCs were preserved, almost as if they had been stained and otherwise treated in a lab.
The parasites were different enough in texture and density to stand out clearly within the RBCs during the natural embalming process for which amber is famous. ![]()
An amber specimen found in the Dominican Republic contained the first fossilized mammalian red blood cells (RBCs) and intraerythrocytic hemoparasites, according to an article published in the Journal of Medical Entomology.
The fossil contained an engorged tick and RBCs infected with parasites that resemble existing members of the Babesiidae and Theileriidae families of the order Piroplasmida.
It appears that 2 small holes in the back of the tick allowed blood to ooze out just as the tick became stuck in tree sap that later fossilized into amber.
“These 2 tiny holes indicate that something picked a tick off the mammal it was feeding on, puncturing it in the process and dropping it immediately into tree sap,” said study author George Poinar, Jr, PhD, of Oregon State University in Corvallis.
“This would be consistent with the grooming behavior of monkeys that we know lived at that time in this region. The fossilized blood cells, infected with these parasites, are simply amazing in their detail. This discovery provides the only known fossils of Babesia-type pathogens.”
Dr Poinar said the amber specimen came from mines located in the Cordillera Septentrional of the Dominican Republic. It may have originated anywhere from 15 to 45 million years ago.
The fossil contained an engorged nymphal tick of the genus Ambylomma. The parasites found in the RBCs were also found in the gut epithelial cells and body cavity of the tick.
“The life forms we find in amber can reveal so much about the history and evolution of diseases we still struggle with today,” Dr Poinar said. “This parasite, for instance, was clearly around millions of years before humans and appears to have evolved alongside primates, among other hosts.”
Part of what makes this fossil unique, Dr Poinar said, is the way in which the parasites and RBCs were preserved, almost as if they had been stained and otherwise treated in a lab.
The parasites were different enough in texture and density to stand out clearly within the RBCs during the natural embalming process for which amber is famous. ![]()
An amber specimen found in the Dominican Republic contained the first fossilized mammalian red blood cells (RBCs) and intraerythrocytic hemoparasites, according to an article published in the Journal of Medical Entomology.
The fossil contained an engorged tick and RBCs infected with parasites that resemble existing members of the Babesiidae and Theileriidae families of the order Piroplasmida.
It appears that 2 small holes in the back of the tick allowed blood to ooze out just as the tick became stuck in tree sap that later fossilized into amber.
“These 2 tiny holes indicate that something picked a tick off the mammal it was feeding on, puncturing it in the process and dropping it immediately into tree sap,” said study author George Poinar, Jr, PhD, of Oregon State University in Corvallis.
“This would be consistent with the grooming behavior of monkeys that we know lived at that time in this region. The fossilized blood cells, infected with these parasites, are simply amazing in their detail. This discovery provides the only known fossils of Babesia-type pathogens.”
Dr Poinar said the amber specimen came from mines located in the Cordillera Septentrional of the Dominican Republic. It may have originated anywhere from 15 to 45 million years ago.
The fossil contained an engorged nymphal tick of the genus Ambylomma. The parasites found in the RBCs were also found in the gut epithelial cells and body cavity of the tick.
“The life forms we find in amber can reveal so much about the history and evolution of diseases we still struggle with today,” Dr Poinar said. “This parasite, for instance, was clearly around millions of years before humans and appears to have evolved alongside primates, among other hosts.”
Part of what makes this fossil unique, Dr Poinar said, is the way in which the parasites and RBCs were preserved, almost as if they had been stained and otherwise treated in a lab.
The parasites were different enough in texture and density to stand out clearly within the RBCs during the natural embalming process for which amber is famous. ![]()
Rule identifies women at low risk of VTE recurrence
Results of the REVERSE-II study appear to validate the utility of the HERDOO2 rule to identify women who can safely stop taking anticoagulants after their first unprovoked venous thromboembolism (VTE).
Some women who were classified as low-risk according to HERDOO2 did experience VTE recurrence after they stopped taking anticoagulants.
However, their risk of recurrence was lower than that of women who were classified as high-risk and stopped taking anticoagulants.
These results were published in The BMJ.
“Patients can get very anxious trying to balance the risks of [anticoagulation] with the risks of another blood clot,” said study author Marc Rodger, MD, of Ottawa Hospital and University of Ottawa in Ontario, Canada.
“With this rule, we can confidently tell half of the women we see that they are at low risk of having another blood clot. This means they can stop taking blood thinners once their initial clot is treated, sparing them the cost, inconvenience, and risks of taking life-long medication.”
The HERDOO2 rule suggests a woman has a low risk of VTE if she has 1 or none of the following risk factors:
- HER=Hyperpigmentation, edema, or redness in either leg
- D=High levels of D-dimer in the blood
- O=Obesity (body mass index of 30 kg/m2 or more)
- O=Older age (65+).
To test the rule, Dr Rodgers and his colleagues evaluated 2785 men and women with a first, unprovoked VTE. The patients were recruited between 2008 and 2015 from 44 healthcare centers in 7 countries.
Patients who were found to be at low risk of VTE recurrence were told to stop taking anticoagulants after they completed the initial treatment for their first VTE.
For patients considered at high risk for VTE recurrence, the researchers left the decision of continuing anticoagulation to the patients and their doctors.
Low-risk patients
None of the men in this trial could be identified as low-risk using the HERDOO2 rule.
However, 631 women had a low risk of VTE recurrence according to HERDOO2. Most of these women (n=591) stopped anticoagulant therapy.
Twenty-seven low-risk women decided to continue anticoagulation, 1 patient’s physician decided she required continued anticoagulation, and 3 patients continued for “other” reasons.
Nine patients in this group were lost to follow-up.
High-risk patients
There were 2148 men and women considered at high risk for VTE recurrence. Most of these patients (n=1802) continued anticoagulation.
Of the 323 high-risk patients who stopped anticoagulation, 279 did so because of their own preference, 9 due to physician decision, 15 had a high risk of bleeding, and 20 stopped for “other” reasons.
Twenty-three patients in this group were lost to follow-up.
Results
The researchers followed the patients for a year after they had finished treatment for their first VTE.
The risk of recurrent major VTE per 100 patient-years was:
- 3.0% among low-risk women who discontinued anticoagulants
- 8.1% among men and high-risk women who discontinued anticoagulants
- 7.4% among high-risk women (only) who discontinued anticoagulants
- 1.6% among men and high-risk women who continued anticoagulants.
Among the low-risk women who continued to receive anticoagulants, there were no cases of recurrent, symptomatic VTE.
“We see 2 to 3 patients with unexplained blood clots every day at The Ottawa Hospital,” Dr Rodger said. “If this rule was applied across Canada, we estimate that over 10,000 women a year would be identified as low risk and be able to come off blood thinners.” ![]()
Results of the REVERSE-II study appear to validate the utility of the HERDOO2 rule to identify women who can safely stop taking anticoagulants after their first unprovoked venous thromboembolism (VTE).
Some women who were classified as low-risk according to HERDOO2 did experience VTE recurrence after they stopped taking anticoagulants.
However, their risk of recurrence was lower than that of women who were classified as high-risk and stopped taking anticoagulants.
These results were published in The BMJ.
“Patients can get very anxious trying to balance the risks of [anticoagulation] with the risks of another blood clot,” said study author Marc Rodger, MD, of Ottawa Hospital and University of Ottawa in Ontario, Canada.
“With this rule, we can confidently tell half of the women we see that they are at low risk of having another blood clot. This means they can stop taking blood thinners once their initial clot is treated, sparing them the cost, inconvenience, and risks of taking life-long medication.”
The HERDOO2 rule suggests a woman has a low risk of VTE if she has 1 or none of the following risk factors:
- HER=Hyperpigmentation, edema, or redness in either leg
- D=High levels of D-dimer in the blood
- O=Obesity (body mass index of 30 kg/m2 or more)
- O=Older age (65+).
To test the rule, Dr Rodgers and his colleagues evaluated 2785 men and women with a first, unprovoked VTE. The patients were recruited between 2008 and 2015 from 44 healthcare centers in 7 countries.
Patients who were found to be at low risk of VTE recurrence were told to stop taking anticoagulants after they completed the initial treatment for their first VTE.
For patients considered at high risk for VTE recurrence, the researchers left the decision of continuing anticoagulation to the patients and their doctors.
Low-risk patients
None of the men in this trial could be identified as low-risk using the HERDOO2 rule.
However, 631 women had a low risk of VTE recurrence according to HERDOO2. Most of these women (n=591) stopped anticoagulant therapy.
Twenty-seven low-risk women decided to continue anticoagulation, 1 patient’s physician decided she required continued anticoagulation, and 3 patients continued for “other” reasons.
Nine patients in this group were lost to follow-up.
High-risk patients
There were 2148 men and women considered at high risk for VTE recurrence. Most of these patients (n=1802) continued anticoagulation.
Of the 323 high-risk patients who stopped anticoagulation, 279 did so because of their own preference, 9 due to physician decision, 15 had a high risk of bleeding, and 20 stopped for “other” reasons.
Twenty-three patients in this group were lost to follow-up.
Results
The researchers followed the patients for a year after they had finished treatment for their first VTE.
The risk of recurrent major VTE per 100 patient-years was:
- 3.0% among low-risk women who discontinued anticoagulants
- 8.1% among men and high-risk women who discontinued anticoagulants
- 7.4% among high-risk women (only) who discontinued anticoagulants
- 1.6% among men and high-risk women who continued anticoagulants.
Among the low-risk women who continued to receive anticoagulants, there were no cases of recurrent, symptomatic VTE.
“We see 2 to 3 patients with unexplained blood clots every day at The Ottawa Hospital,” Dr Rodger said. “If this rule was applied across Canada, we estimate that over 10,000 women a year would be identified as low risk and be able to come off blood thinners.” ![]()
Results of the REVERSE-II study appear to validate the utility of the HERDOO2 rule to identify women who can safely stop taking anticoagulants after their first unprovoked venous thromboembolism (VTE).
Some women who were classified as low-risk according to HERDOO2 did experience VTE recurrence after they stopped taking anticoagulants.
However, their risk of recurrence was lower than that of women who were classified as high-risk and stopped taking anticoagulants.
These results were published in The BMJ.
“Patients can get very anxious trying to balance the risks of [anticoagulation] with the risks of another blood clot,” said study author Marc Rodger, MD, of Ottawa Hospital and University of Ottawa in Ontario, Canada.
“With this rule, we can confidently tell half of the women we see that they are at low risk of having another blood clot. This means they can stop taking blood thinners once their initial clot is treated, sparing them the cost, inconvenience, and risks of taking life-long medication.”
The HERDOO2 rule suggests a woman has a low risk of VTE if she has 1 or none of the following risk factors:
- HER=Hyperpigmentation, edema, or redness in either leg
- D=High levels of D-dimer in the blood
- O=Obesity (body mass index of 30 kg/m2 or more)
- O=Older age (65+).
To test the rule, Dr Rodgers and his colleagues evaluated 2785 men and women with a first, unprovoked VTE. The patients were recruited between 2008 and 2015 from 44 healthcare centers in 7 countries.
Patients who were found to be at low risk of VTE recurrence were told to stop taking anticoagulants after they completed the initial treatment for their first VTE.
For patients considered at high risk for VTE recurrence, the researchers left the decision of continuing anticoagulation to the patients and their doctors.
Low-risk patients
None of the men in this trial could be identified as low-risk using the HERDOO2 rule.
However, 631 women had a low risk of VTE recurrence according to HERDOO2. Most of these women (n=591) stopped anticoagulant therapy.
Twenty-seven low-risk women decided to continue anticoagulation, 1 patient’s physician decided she required continued anticoagulation, and 3 patients continued for “other” reasons.
Nine patients in this group were lost to follow-up.
High-risk patients
There were 2148 men and women considered at high risk for VTE recurrence. Most of these patients (n=1802) continued anticoagulation.
Of the 323 high-risk patients who stopped anticoagulation, 279 did so because of their own preference, 9 due to physician decision, 15 had a high risk of bleeding, and 20 stopped for “other” reasons.
Twenty-three patients in this group were lost to follow-up.
Results
The researchers followed the patients for a year after they had finished treatment for their first VTE.
The risk of recurrent major VTE per 100 patient-years was:
- 3.0% among low-risk women who discontinued anticoagulants
- 8.1% among men and high-risk women who discontinued anticoagulants
- 7.4% among high-risk women (only) who discontinued anticoagulants
- 1.6% among men and high-risk women who continued anticoagulants.
Among the low-risk women who continued to receive anticoagulants, there were no cases of recurrent, symptomatic VTE.
“We see 2 to 3 patients with unexplained blood clots every day at The Ottawa Hospital,” Dr Rodger said. “If this rule was applied across Canada, we estimate that over 10,000 women a year would be identified as low risk and be able to come off blood thinners.” ![]()
Half of patients retain response to CAR T-cell therapy
WASHINGTON, DC—Roughly half of patients who responded to chimeric antigen receptor (CAR) T-cell therapy in the ZUMA-1 trial have retained that response at a median follow-up exceeding 8 months.
The CAR T-cell therapy, axicabtagene ciloleucel (formerly KTE-C19), initially produced an objective response rate (ORR) of 82% in this trial of patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL).
At a median follow-up of 8.7 months, 44% of all patients (53% of responders) are still in response, and 39% are in complete response (CR).
Thirteen percent of patients had grade 3 or higher cytokine release syndrome (CRS), and 28% had neurologic events.
There were 2 deaths related to axicabtagene ciloleucel.
Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa, Florida, presented these updated results from ZUMA-1 at the AACR Annual Meeting 2017 (abstract CT019).
ZUMA-1 is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program.
Patients and treatment
The trial enrolled 111 patients, 101 of whom were successfully treated with axicabtagene ciloleucel. Seven patients could not be treated due to serious adverse events, 1 due to unavailable product, and 2 due to non-measurable disease.
Seventy-seven of the patients had diffuse large B-cell lymphoma (DLBCL), and 24 had transformed follicular lymphoma (TFL) or primary mediastinal B-cell lymphoma (PMBCL). Eighty-five percent of patients had stage III/IV disease.
Seventy-nine percent were refractory to chemotherapy and did not have a prior autologous stem cell transplant (auto-SCT). Twenty-one percent did undergo auto-SCT and relapsed within 12 months of the procedure.
Sixty-nine percent of patients had received 3 or more lines of prior therapy, and 54% were refractory to 2 consecutive lines of prior therapy.
For this study, the patients received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days.
Two days after the conditioning regimen was completed, patients received axicabtagene ciloleucel at a target dose of 2 × 106 CAR T cells/kg.
Efficacy
The following table shows overall response data, response data at 6 months, and ongoing responses at the primary analysis data cut-off.
| DLBCL (n=77) | TFL/PMBCL (n=24) | Combined (n=101) | ||||
| ORR (%) | CR (%) | ORR (%) | CR (%) | ORR (%) | CR (%) | |
| ORR | 82 | 49 | 83 | 71 | 82 | 54 |
| Month 6 | 36 | 31 | 54 | 50 | 41 | 36 |
| Ongoing | 36 | 31 | 67 | 63 | 44 | 39 |
The researchers said the ORR was generally consistent in key subgroups. The ORR was 83% in patients who were refractory to their second or greater line of therapy and 76% in patients who relapsed within 12 months of auto-SCT.
Overall, the median duration of response was 8.2 months. However, the median duration of response has not been reached for patients with a CR.
At a median follow-up of 8.7 months, the median overall survival has not been reached.
Safety
The most common grade 3 or higher adverse events included anemia (43%), neutropenia (39%), decreased neutrophil count (32%), febrile neutropenia (31%), decreased white blood cell count (29%), thrombocytopenia (24%), encephalopathy (21%), and decreased lymphocyte count (20%).
The incidence of grade 3 or higher CRS was 13%, and the incidence of neurologic events was 28%. These represent decreases from the interim analysis of ZUMA-1, when the rate of grade 3+ CRS was 18%, and the rate of neurological events was 34%.
“We believe the rates of CRS and neurologic events decreased over the course of the study as clinicians gained experience in the management of adverse events,” said Jeff Wiezorek, MD, senior vice-president of clinical development at Kite Pharma.
There were 3 deaths throughout the course of the trial that were not a result of disease progression.
Two deaths were deemed related to axicabtagene ciloleucel. One was a case of hemophagocytic lymphohistiocytosis. The other was cardiac arrest in the setting of CRS.
The third death was the result of a pulmonary embolism and was considered unrelated to axicabtagene ciloleucel. ![]()
WASHINGTON, DC—Roughly half of patients who responded to chimeric antigen receptor (CAR) T-cell therapy in the ZUMA-1 trial have retained that response at a median follow-up exceeding 8 months.
The CAR T-cell therapy, axicabtagene ciloleucel (formerly KTE-C19), initially produced an objective response rate (ORR) of 82% in this trial of patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL).
At a median follow-up of 8.7 months, 44% of all patients (53% of responders) are still in response, and 39% are in complete response (CR).
Thirteen percent of patients had grade 3 or higher cytokine release syndrome (CRS), and 28% had neurologic events.
There were 2 deaths related to axicabtagene ciloleucel.
Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa, Florida, presented these updated results from ZUMA-1 at the AACR Annual Meeting 2017 (abstract CT019).
ZUMA-1 is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program.
Patients and treatment
The trial enrolled 111 patients, 101 of whom were successfully treated with axicabtagene ciloleucel. Seven patients could not be treated due to serious adverse events, 1 due to unavailable product, and 2 due to non-measurable disease.
Seventy-seven of the patients had diffuse large B-cell lymphoma (DLBCL), and 24 had transformed follicular lymphoma (TFL) or primary mediastinal B-cell lymphoma (PMBCL). Eighty-five percent of patients had stage III/IV disease.
Seventy-nine percent were refractory to chemotherapy and did not have a prior autologous stem cell transplant (auto-SCT). Twenty-one percent did undergo auto-SCT and relapsed within 12 months of the procedure.
Sixty-nine percent of patients had received 3 or more lines of prior therapy, and 54% were refractory to 2 consecutive lines of prior therapy.
For this study, the patients received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days.
Two days after the conditioning regimen was completed, patients received axicabtagene ciloleucel at a target dose of 2 × 106 CAR T cells/kg.
Efficacy
The following table shows overall response data, response data at 6 months, and ongoing responses at the primary analysis data cut-off.
| DLBCL (n=77) | TFL/PMBCL (n=24) | Combined (n=101) | ||||
| ORR (%) | CR (%) | ORR (%) | CR (%) | ORR (%) | CR (%) | |
| ORR | 82 | 49 | 83 | 71 | 82 | 54 |
| Month 6 | 36 | 31 | 54 | 50 | 41 | 36 |
| Ongoing | 36 | 31 | 67 | 63 | 44 | 39 |
The researchers said the ORR was generally consistent in key subgroups. The ORR was 83% in patients who were refractory to their second or greater line of therapy and 76% in patients who relapsed within 12 months of auto-SCT.
Overall, the median duration of response was 8.2 months. However, the median duration of response has not been reached for patients with a CR.
At a median follow-up of 8.7 months, the median overall survival has not been reached.
Safety
The most common grade 3 or higher adverse events included anemia (43%), neutropenia (39%), decreased neutrophil count (32%), febrile neutropenia (31%), decreased white blood cell count (29%), thrombocytopenia (24%), encephalopathy (21%), and decreased lymphocyte count (20%).
The incidence of grade 3 or higher CRS was 13%, and the incidence of neurologic events was 28%. These represent decreases from the interim analysis of ZUMA-1, when the rate of grade 3+ CRS was 18%, and the rate of neurological events was 34%.
“We believe the rates of CRS and neurologic events decreased over the course of the study as clinicians gained experience in the management of adverse events,” said Jeff Wiezorek, MD, senior vice-president of clinical development at Kite Pharma.
There were 3 deaths throughout the course of the trial that were not a result of disease progression.
Two deaths were deemed related to axicabtagene ciloleucel. One was a case of hemophagocytic lymphohistiocytosis. The other was cardiac arrest in the setting of CRS.
The third death was the result of a pulmonary embolism and was considered unrelated to axicabtagene ciloleucel. ![]()
WASHINGTON, DC—Roughly half of patients who responded to chimeric antigen receptor (CAR) T-cell therapy in the ZUMA-1 trial have retained that response at a median follow-up exceeding 8 months.
The CAR T-cell therapy, axicabtagene ciloleucel (formerly KTE-C19), initially produced an objective response rate (ORR) of 82% in this trial of patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL).
At a median follow-up of 8.7 months, 44% of all patients (53% of responders) are still in response, and 39% are in complete response (CR).
Thirteen percent of patients had grade 3 or higher cytokine release syndrome (CRS), and 28% had neurologic events.
There were 2 deaths related to axicabtagene ciloleucel.
Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa, Florida, presented these updated results from ZUMA-1 at the AACR Annual Meeting 2017 (abstract CT019).
ZUMA-1 is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program.
Patients and treatment
The trial enrolled 111 patients, 101 of whom were successfully treated with axicabtagene ciloleucel. Seven patients could not be treated due to serious adverse events, 1 due to unavailable product, and 2 due to non-measurable disease.
Seventy-seven of the patients had diffuse large B-cell lymphoma (DLBCL), and 24 had transformed follicular lymphoma (TFL) or primary mediastinal B-cell lymphoma (PMBCL). Eighty-five percent of patients had stage III/IV disease.
Seventy-nine percent were refractory to chemotherapy and did not have a prior autologous stem cell transplant (auto-SCT). Twenty-one percent did undergo auto-SCT and relapsed within 12 months of the procedure.
Sixty-nine percent of patients had received 3 or more lines of prior therapy, and 54% were refractory to 2 consecutive lines of prior therapy.
For this study, the patients received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days.
Two days after the conditioning regimen was completed, patients received axicabtagene ciloleucel at a target dose of 2 × 106 CAR T cells/kg.
Efficacy
The following table shows overall response data, response data at 6 months, and ongoing responses at the primary analysis data cut-off.
| DLBCL (n=77) | TFL/PMBCL (n=24) | Combined (n=101) | ||||
| ORR (%) | CR (%) | ORR (%) | CR (%) | ORR (%) | CR (%) | |
| ORR | 82 | 49 | 83 | 71 | 82 | 54 |
| Month 6 | 36 | 31 | 54 | 50 | 41 | 36 |
| Ongoing | 36 | 31 | 67 | 63 | 44 | 39 |
The researchers said the ORR was generally consistent in key subgroups. The ORR was 83% in patients who were refractory to their second or greater line of therapy and 76% in patients who relapsed within 12 months of auto-SCT.
Overall, the median duration of response was 8.2 months. However, the median duration of response has not been reached for patients with a CR.
At a median follow-up of 8.7 months, the median overall survival has not been reached.
Safety
The most common grade 3 or higher adverse events included anemia (43%), neutropenia (39%), decreased neutrophil count (32%), febrile neutropenia (31%), decreased white blood cell count (29%), thrombocytopenia (24%), encephalopathy (21%), and decreased lymphocyte count (20%).
The incidence of grade 3 or higher CRS was 13%, and the incidence of neurologic events was 28%. These represent decreases from the interim analysis of ZUMA-1, when the rate of grade 3+ CRS was 18%, and the rate of neurological events was 34%.
“We believe the rates of CRS and neurologic events decreased over the course of the study as clinicians gained experience in the management of adverse events,” said Jeff Wiezorek, MD, senior vice-president of clinical development at Kite Pharma.
There were 3 deaths throughout the course of the trial that were not a result of disease progression.
Two deaths were deemed related to axicabtagene ciloleucel. One was a case of hemophagocytic lymphohistiocytosis. The other was cardiac arrest in the setting of CRS.
The third death was the result of a pulmonary embolism and was considered unrelated to axicabtagene ciloleucel. ![]()
Study provides new insight into RBC resilience
Researchers say they have developed a new system for studying the resilience of red blood cells (RBCs).
The team’s microfluidic system allowed them to look at how RBCs spring back into shape after deforming to pass through a narrow channel.
The researchers believe their findings could aid the diagnosis and treatment of blood-related diseases such as septic shock and malaria.
Hiroaki Ito, PhD, of Osaka University in Suita, Japan, and his colleagues detailed these findings in Scientific Reports.
To study RBCs, the researchers built a “catch-load-launch” microfluidic platform.
The setup included a microchannel in which a single RBC could be held in place for any desired length of time. The RBC was ultimately launched into a wider section using a robotic pump, which simulates the transition from a capillary into a larger vessel.
“The cell was precisely localized in the microchannel by the combination of pressure control and real-time visual feedback,” explained study author Makoto Kaneko, of Osaka University.
“This let us ‘catch’ an erythrocyte in front of the constriction, ‘load’ it inside for a desired time, and quickly ‘launch’ it from the constriction to monitor the shape recovery over time.”
The researchers found that, as the time the RBC was held in the constricted region was increased—from 5 seconds all the way to 5 minutes—the time it took the cell to recover its normal shape also increased.
For very short constriction times, the cells bounced back within 1/10 of a second. But it took approximately 10 seconds for cells to recover if they were held in the narrow segment longer than about 3 minutes.
The researchers also used their “catch-load-launch” system to study septic shock. This condition can occur when bacteria invade the bloodstream and release endotoxins.
Patients with septic shock may suffer from reduced circulation inside the narrow blood vessels as RBCs become too stiff. The same problem can be caused by the malaria parasite Plasmodium falciparum.
The researchers exposed RBCs to endotoxin from the bacteria Salmonella minnesota and found the RBCs became stiffer and less resilient.
“There is a great deal of evidence that relates certain diseases, including sepsis and malaria, to a decrease in the deformability of red blood cells,” Dr Ito said.
“Such a stiffening can lead to a disturbance in microcirculation, and our ‘catch-load-launch’ platform has the potential to be applied to the mechanical diagnosis of these diseased blood cells.” ![]()
Researchers say they have developed a new system for studying the resilience of red blood cells (RBCs).
The team’s microfluidic system allowed them to look at how RBCs spring back into shape after deforming to pass through a narrow channel.
The researchers believe their findings could aid the diagnosis and treatment of blood-related diseases such as septic shock and malaria.
Hiroaki Ito, PhD, of Osaka University in Suita, Japan, and his colleagues detailed these findings in Scientific Reports.
To study RBCs, the researchers built a “catch-load-launch” microfluidic platform.
The setup included a microchannel in which a single RBC could be held in place for any desired length of time. The RBC was ultimately launched into a wider section using a robotic pump, which simulates the transition from a capillary into a larger vessel.
“The cell was precisely localized in the microchannel by the combination of pressure control and real-time visual feedback,” explained study author Makoto Kaneko, of Osaka University.
“This let us ‘catch’ an erythrocyte in front of the constriction, ‘load’ it inside for a desired time, and quickly ‘launch’ it from the constriction to monitor the shape recovery over time.”
The researchers found that, as the time the RBC was held in the constricted region was increased—from 5 seconds all the way to 5 minutes—the time it took the cell to recover its normal shape also increased.
For very short constriction times, the cells bounced back within 1/10 of a second. But it took approximately 10 seconds for cells to recover if they were held in the narrow segment longer than about 3 minutes.
The researchers also used their “catch-load-launch” system to study septic shock. This condition can occur when bacteria invade the bloodstream and release endotoxins.
Patients with septic shock may suffer from reduced circulation inside the narrow blood vessels as RBCs become too stiff. The same problem can be caused by the malaria parasite Plasmodium falciparum.
The researchers exposed RBCs to endotoxin from the bacteria Salmonella minnesota and found the RBCs became stiffer and less resilient.
“There is a great deal of evidence that relates certain diseases, including sepsis and malaria, to a decrease in the deformability of red blood cells,” Dr Ito said.
“Such a stiffening can lead to a disturbance in microcirculation, and our ‘catch-load-launch’ platform has the potential to be applied to the mechanical diagnosis of these diseased blood cells.” ![]()
Researchers say they have developed a new system for studying the resilience of red blood cells (RBCs).
The team’s microfluidic system allowed them to look at how RBCs spring back into shape after deforming to pass through a narrow channel.
The researchers believe their findings could aid the diagnosis and treatment of blood-related diseases such as septic shock and malaria.
Hiroaki Ito, PhD, of Osaka University in Suita, Japan, and his colleagues detailed these findings in Scientific Reports.
To study RBCs, the researchers built a “catch-load-launch” microfluidic platform.
The setup included a microchannel in which a single RBC could be held in place for any desired length of time. The RBC was ultimately launched into a wider section using a robotic pump, which simulates the transition from a capillary into a larger vessel.
“The cell was precisely localized in the microchannel by the combination of pressure control and real-time visual feedback,” explained study author Makoto Kaneko, of Osaka University.
“This let us ‘catch’ an erythrocyte in front of the constriction, ‘load’ it inside for a desired time, and quickly ‘launch’ it from the constriction to monitor the shape recovery over time.”
The researchers found that, as the time the RBC was held in the constricted region was increased—from 5 seconds all the way to 5 minutes—the time it took the cell to recover its normal shape also increased.
For very short constriction times, the cells bounced back within 1/10 of a second. But it took approximately 10 seconds for cells to recover if they were held in the narrow segment longer than about 3 minutes.
The researchers also used their “catch-load-launch” system to study septic shock. This condition can occur when bacteria invade the bloodstream and release endotoxins.
Patients with septic shock may suffer from reduced circulation inside the narrow blood vessels as RBCs become too stiff. The same problem can be caused by the malaria parasite Plasmodium falciparum.
The researchers exposed RBCs to endotoxin from the bacteria Salmonella minnesota and found the RBCs became stiffer and less resilient.
“There is a great deal of evidence that relates certain diseases, including sepsis and malaria, to a decrease in the deformability of red blood cells,” Dr Ito said.
“Such a stiffening can lead to a disturbance in microcirculation, and our ‘catch-load-launch’ platform has the potential to be applied to the mechanical diagnosis of these diseased blood cells.”
New BTK inhibitor may overcome resistance in CLL
WASHINGTON, DC—Preclinical research suggests a second-generation BTK inhibitor may overcome the acquired resistance observed with its predecessor in patients with chronic lymphocytic leukemia (CLL).
Investigators found the non-covalent BTK inhibitor SNS-062 was unaffected by the BTK C481S mutation, which confers resistance to the first-generation BTK inhibitor ibrutinib.
“[A] subset of patients acquire resistance to ibrutinib, the current standard-of-care BTK inhibitor,” said Amy Johnson, PhD, of The Ohio State University in Columbus.
“A key resistance mechanism to covalent BTK inhibitors is a point mutation in the BTK active site, converting cysteine 481 to serine, or C481S.”
“In this study, we demonstrate that SNS-062, which binds non-covalently to BTK, is a potent inhibitor of BTK unaffected by the presence of the C481S mutation. These findings support clinical investigation of SNS-062 to address acquired resistance to covalent BTK inhibitors in patients.”
Dr Johnson and her colleagues presented these findings at the AACR Annual Meeting 2017 (abstract 1207).
SNS-062 is being developed by Sunesis Pharmaceuticals, Inc., and company investigators were involved in this research. But the study was sponsored by The Ohio State University.
For this study, Dr Johnson and her colleagues tested SNS-062 in primary CLL cells and X-linked agammaglobulinemia human cell lines.
The investigators found that SNS-062 inhibited BTK, decreased the expression of B-cell activation markers, and reduced CLL cell viability in a dose-dependent manner. And these effects were comparable to those observed with ibrutinib.
SNS-062 and ibrutinib demonstrated comparable activity against wild-type BTK. However, ibrutinib and another BTK inhibitor, acalabrutinib, were hindered by the BTK C481S mutation, while SNS-062 was not.
The investigators said SNS-062 was 6 times more potent than ibrutinib against C481S BTK and more than 640 times more potent than acalabrutinib.
The team also noted that SNS-062 exhibited high specificity, affecting a limited number of kinases outside the TEC kinase family.
Finally, the investigators found that SNS-062 diminished stromal cell protection in CLL cells, suggesting the drug can hinder protection from the tumor microenvironment.
WASHINGTON, DC—Preclinical research suggests a second-generation BTK inhibitor may overcome the acquired resistance observed with its predecessor in patients with chronic lymphocytic leukemia (CLL).
Investigators found the non-covalent BTK inhibitor SNS-062 was unaffected by the BTK C481S mutation, which confers resistance to the first-generation BTK inhibitor ibrutinib.
“[A] subset of patients acquire resistance to ibrutinib, the current standard-of-care BTK inhibitor,” said Amy Johnson, PhD, of The Ohio State University in Columbus.
“A key resistance mechanism to covalent BTK inhibitors is a point mutation in the BTK active site, converting cysteine 481 to serine, or C481S.”
“In this study, we demonstrate that SNS-062, which binds non-covalently to BTK, is a potent inhibitor of BTK unaffected by the presence of the C481S mutation. These findings support clinical investigation of SNS-062 to address acquired resistance to covalent BTK inhibitors in patients.”
Dr Johnson and her colleagues presented these findings at the AACR Annual Meeting 2017 (abstract 1207).
SNS-062 is being developed by Sunesis Pharmaceuticals, Inc., and company investigators were involved in this research. But the study was sponsored by The Ohio State University.
For this study, Dr Johnson and her colleagues tested SNS-062 in primary CLL cells and X-linked agammaglobulinemia human cell lines.
The investigators found that SNS-062 inhibited BTK, decreased the expression of B-cell activation markers, and reduced CLL cell viability in a dose-dependent manner. And these effects were comparable to those observed with ibrutinib.
SNS-062 and ibrutinib demonstrated comparable activity against wild-type BTK. However, ibrutinib and another BTK inhibitor, acalabrutinib, were hindered by the BTK C481S mutation, while SNS-062 was not.
The investigators said SNS-062 was 6 times more potent than ibrutinib against C481S BTK and more than 640 times more potent than acalabrutinib.
The team also noted that SNS-062 exhibited high specificity, affecting a limited number of kinases outside the TEC kinase family.
Finally, the investigators found that SNS-062 diminished stromal cell protection in CLL cells, suggesting the drug can hinder protection from the tumor microenvironment.
WASHINGTON, DC—Preclinical research suggests a second-generation BTK inhibitor may overcome the acquired resistance observed with its predecessor in patients with chronic lymphocytic leukemia (CLL).
Investigators found the non-covalent BTK inhibitor SNS-062 was unaffected by the BTK C481S mutation, which confers resistance to the first-generation BTK inhibitor ibrutinib.
“[A] subset of patients acquire resistance to ibrutinib, the current standard-of-care BTK inhibitor,” said Amy Johnson, PhD, of The Ohio State University in Columbus.
“A key resistance mechanism to covalent BTK inhibitors is a point mutation in the BTK active site, converting cysteine 481 to serine, or C481S.”
“In this study, we demonstrate that SNS-062, which binds non-covalently to BTK, is a potent inhibitor of BTK unaffected by the presence of the C481S mutation. These findings support clinical investigation of SNS-062 to address acquired resistance to covalent BTK inhibitors in patients.”
Dr Johnson and her colleagues presented these findings at the AACR Annual Meeting 2017 (abstract 1207).
SNS-062 is being developed by Sunesis Pharmaceuticals, Inc., and company investigators were involved in this research. But the study was sponsored by The Ohio State University.
For this study, Dr Johnson and her colleagues tested SNS-062 in primary CLL cells and X-linked agammaglobulinemia human cell lines.
The investigators found that SNS-062 inhibited BTK, decreased the expression of B-cell activation markers, and reduced CLL cell viability in a dose-dependent manner. And these effects were comparable to those observed with ibrutinib.
SNS-062 and ibrutinib demonstrated comparable activity against wild-type BTK. However, ibrutinib and another BTK inhibitor, acalabrutinib, were hindered by the BTK C481S mutation, while SNS-062 was not.
The investigators said SNS-062 was 6 times more potent than ibrutinib against C481S BTK and more than 640 times more potent than acalabrutinib.
The team also noted that SNS-062 exhibited high specificity, affecting a limited number of kinases outside the TEC kinase family.
Finally, the investigators found that SNS-062 diminished stromal cell protection in CLL cells, suggesting the drug can hinder protection from the tumor microenvironment.
ASCO addresses needs of SGMs with cancer
The American Society of Clinical Oncology (ASCO) has issued recommendations addressing the needs of sexual and gender minority (SGM) populations with cancer.
The recommendations are designed to focus attention on the challenges facing the SGM community—including discrimination and greater risk of anxiety and depression, resulting in disparate care—and concrete steps that can help minimize health disparities among SGM individuals.
The recommendations were published in a policy statement in the Journal of Clinical Oncology.
“Sexual and gender minorities face unique challenges related to cancer risk, discrimination, and other psychosocial issues,” said ASCO President Daniel F. Hayes, MD.
“Compounding these challenges is the fact that providers may have a lack of knowledge and sensitivity about the health risks and health needs facing their SGM patients.”
SGMs include individuals who are lesbian, gay, bisexual, transgender, and intersex (also referred to as those with differences in sex development).
ASCO’s policy statement notes that SGM populations bear a disproportionate cancer burden stemming from several factors, including:
- Lower rates of cancer screening, in part due to lower rates of insurance coverage, exclusion from traditional screening campaigns, and previous experience of discrimination in the healthcare system
- A hesitancy on the part of SGM patients to disclose their sexual orientation to providers due to a fear of stigmatization, which can create additional barriers to care.
ASCO’s statement calls for a coordinated effort to address health disparities among SGM populations, including:
- Increased patient access to culturally competent support services
- Expanded cancer prevention education for SGM individuals
- Robust policies prohibiting discrimination
- Adequate insurance coverage to meet the needs of SGM individuals affected by cancer
- Inclusion of SGM status as a required data element in cancer registries and clinical trials
- Increased focus on SGM populations in cancer research.
“Our objective was to raise awareness among oncology providers, patients, policy makers, and other stakeholders about the cancer care needs of SGM populations and the barriers that SGM individuals face in getting the highest-quality care,” said Jennifer J. Griggs, MD, lead author of the policy statement and a professor at the University of Michigan in Ann Arbor.
“To address these barriers, a coordinated effort is needed to enhance education for patients and providers, to improve outreach and support, and to encourage productive policy and legislative action.”
The American Society of Clinical Oncology (ASCO) has issued recommendations addressing the needs of sexual and gender minority (SGM) populations with cancer.
The recommendations are designed to focus attention on the challenges facing the SGM community—including discrimination and greater risk of anxiety and depression, resulting in disparate care—and concrete steps that can help minimize health disparities among SGM individuals.
The recommendations were published in a policy statement in the Journal of Clinical Oncology.
“Sexual and gender minorities face unique challenges related to cancer risk, discrimination, and other psychosocial issues,” said ASCO President Daniel F. Hayes, MD.
“Compounding these challenges is the fact that providers may have a lack of knowledge and sensitivity about the health risks and health needs facing their SGM patients.”
SGMs include individuals who are lesbian, gay, bisexual, transgender, and intersex (also referred to as those with differences in sex development).
ASCO’s policy statement notes that SGM populations bear a disproportionate cancer burden stemming from several factors, including:
- Lower rates of cancer screening, in part due to lower rates of insurance coverage, exclusion from traditional screening campaigns, and previous experience of discrimination in the healthcare system
- A hesitancy on the part of SGM patients to disclose their sexual orientation to providers due to a fear of stigmatization, which can create additional barriers to care.
ASCO’s statement calls for a coordinated effort to address health disparities among SGM populations, including:
- Increased patient access to culturally competent support services
- Expanded cancer prevention education for SGM individuals
- Robust policies prohibiting discrimination
- Adequate insurance coverage to meet the needs of SGM individuals affected by cancer
- Inclusion of SGM status as a required data element in cancer registries and clinical trials
- Increased focus on SGM populations in cancer research.
“Our objective was to raise awareness among oncology providers, patients, policy makers, and other stakeholders about the cancer care needs of SGM populations and the barriers that SGM individuals face in getting the highest-quality care,” said Jennifer J. Griggs, MD, lead author of the policy statement and a professor at the University of Michigan in Ann Arbor.
“To address these barriers, a coordinated effort is needed to enhance education for patients and providers, to improve outreach and support, and to encourage productive policy and legislative action.”
The American Society of Clinical Oncology (ASCO) has issued recommendations addressing the needs of sexual and gender minority (SGM) populations with cancer.
The recommendations are designed to focus attention on the challenges facing the SGM community—including discrimination and greater risk of anxiety and depression, resulting in disparate care—and concrete steps that can help minimize health disparities among SGM individuals.
The recommendations were published in a policy statement in the Journal of Clinical Oncology.
“Sexual and gender minorities face unique challenges related to cancer risk, discrimination, and other psychosocial issues,” said ASCO President Daniel F. Hayes, MD.
“Compounding these challenges is the fact that providers may have a lack of knowledge and sensitivity about the health risks and health needs facing their SGM patients.”
SGMs include individuals who are lesbian, gay, bisexual, transgender, and intersex (also referred to as those with differences in sex development).
ASCO’s policy statement notes that SGM populations bear a disproportionate cancer burden stemming from several factors, including:
- Lower rates of cancer screening, in part due to lower rates of insurance coverage, exclusion from traditional screening campaigns, and previous experience of discrimination in the healthcare system
- A hesitancy on the part of SGM patients to disclose their sexual orientation to providers due to a fear of stigmatization, which can create additional barriers to care.
ASCO’s statement calls for a coordinated effort to address health disparities among SGM populations, including:
- Increased patient access to culturally competent support services
- Expanded cancer prevention education for SGM individuals
- Robust policies prohibiting discrimination
- Adequate insurance coverage to meet the needs of SGM individuals affected by cancer
- Inclusion of SGM status as a required data element in cancer registries and clinical trials
- Increased focus on SGM populations in cancer research.
“Our objective was to raise awareness among oncology providers, patients, policy makers, and other stakeholders about the cancer care needs of SGM populations and the barriers that SGM individuals face in getting the highest-quality care,” said Jennifer J. Griggs, MD, lead author of the policy statement and a professor at the University of Michigan in Ann Arbor.
“To address these barriers, a coordinated effort is needed to enhance education for patients and providers, to improve outreach and support, and to encourage productive policy and legislative action.”
Report shows increase in blood cancer incidence and survival
A report on cancer in the US suggests the incidence of leukemia and myeloma has been on the rise in recent years, but the incidence of non-Hodgkin lymphoma (NHL) has been on the decline.
Meanwhile, annual death rates for leukemia and NHL have decreased, and annual death rates for myeloma have decreased in men but not in women.
Furthermore, patients with leukemia, NHL, and myeloma have seen a substantial improvement in 5-year survival rates in recent years relative to patients in the late 1970s.
These findings are part of the Annual Report to the Nation on the Status of Cancer, 1975-2014, which has been published in the Journal of the National Cancer Institute.
This report is released each year, but the current edition includes a special section focused on survival.
“While trends in death rates are the most commonly used measure to assess progress against cancer, survival trends are also an important measure to evaluate progress in improvement of cancer outcomes,” said Ahmedin Jemal, DVM, PhD, of the American Cancer Society.
“We last included a special section on cancer survival in 2004, and, as we found then, survival improved over time for almost all cancers at every stage of diagnosis.”
For the current report, researchers calculated the 5-year average annual percent changes (AAPCs) for 2009 to 2013 for cancer incidence and for 2010 to 2014 for cancer mortality.
Cancer incidence (2009-2013)
In women, the AAPC increased 1.5% for leukemia (P<0.05), decreased 0.5% for NHL (P<0.05), and increased 2.2% for myeloma (P<0.05).
In men, the AAPC increased 1.7% for leukemia (P<0.05), decreased 0.2% for NHL, and increased 2.8% for myeloma (P<0.05).
Cancer mortality (2010-2014)
In women, the AAPC decreased 1.2% for leukemia (P<0.05), decreased 2.2% for NHL (P<0.05), and increased 0.5% for myeloma.
In men, the AAPC decreased 1.0% for leukemia (P<0.05), decreased 2.0% for NHL (P<0.05), and decreased 0.9% for myeloma (P<0.05).
5-year survival
The researchers compared 5-year relative survival for cancers diagnosed from 1975 to 1977 and those diagnosed from 2006 to 2012.
The absolute percentage change over time (for both sexes combined) was 26.1% for NHL, 25.7% for myeloma, and 28.5% for leukemia.
Five-year survival for patients diagnosed in 1975-1977 was 46.5% for NHL, 24.6% for myeloma, and 34.2% for leukemia.
Five-year survival for patients diagnosed in 2006-2012 was 72.6% for NHL, 50.2% for myeloma, and 62.7% for leukemia.
A report on cancer in the US suggests the incidence of leukemia and myeloma has been on the rise in recent years, but the incidence of non-Hodgkin lymphoma (NHL) has been on the decline.
Meanwhile, annual death rates for leukemia and NHL have decreased, and annual death rates for myeloma have decreased in men but not in women.
Furthermore, patients with leukemia, NHL, and myeloma have seen a substantial improvement in 5-year survival rates in recent years relative to patients in the late 1970s.
These findings are part of the Annual Report to the Nation on the Status of Cancer, 1975-2014, which has been published in the Journal of the National Cancer Institute.
This report is released each year, but the current edition includes a special section focused on survival.
“While trends in death rates are the most commonly used measure to assess progress against cancer, survival trends are also an important measure to evaluate progress in improvement of cancer outcomes,” said Ahmedin Jemal, DVM, PhD, of the American Cancer Society.
“We last included a special section on cancer survival in 2004, and, as we found then, survival improved over time for almost all cancers at every stage of diagnosis.”
For the current report, researchers calculated the 5-year average annual percent changes (AAPCs) for 2009 to 2013 for cancer incidence and for 2010 to 2014 for cancer mortality.
Cancer incidence (2009-2013)
In women, the AAPC increased 1.5% for leukemia (P<0.05), decreased 0.5% for NHL (P<0.05), and increased 2.2% for myeloma (P<0.05).
In men, the AAPC increased 1.7% for leukemia (P<0.05), decreased 0.2% for NHL, and increased 2.8% for myeloma (P<0.05).
Cancer mortality (2010-2014)
In women, the AAPC decreased 1.2% for leukemia (P<0.05), decreased 2.2% for NHL (P<0.05), and increased 0.5% for myeloma.
In men, the AAPC decreased 1.0% for leukemia (P<0.05), decreased 2.0% for NHL (P<0.05), and decreased 0.9% for myeloma (P<0.05).
5-year survival
The researchers compared 5-year relative survival for cancers diagnosed from 1975 to 1977 and those diagnosed from 2006 to 2012.
The absolute percentage change over time (for both sexes combined) was 26.1% for NHL, 25.7% for myeloma, and 28.5% for leukemia.
Five-year survival for patients diagnosed in 1975-1977 was 46.5% for NHL, 24.6% for myeloma, and 34.2% for leukemia.
Five-year survival for patients diagnosed in 2006-2012 was 72.6% for NHL, 50.2% for myeloma, and 62.7% for leukemia.
A report on cancer in the US suggests the incidence of leukemia and myeloma has been on the rise in recent years, but the incidence of non-Hodgkin lymphoma (NHL) has been on the decline.
Meanwhile, annual death rates for leukemia and NHL have decreased, and annual death rates for myeloma have decreased in men but not in women.
Furthermore, patients with leukemia, NHL, and myeloma have seen a substantial improvement in 5-year survival rates in recent years relative to patients in the late 1970s.
These findings are part of the Annual Report to the Nation on the Status of Cancer, 1975-2014, which has been published in the Journal of the National Cancer Institute.
This report is released each year, but the current edition includes a special section focused on survival.
“While trends in death rates are the most commonly used measure to assess progress against cancer, survival trends are also an important measure to evaluate progress in improvement of cancer outcomes,” said Ahmedin Jemal, DVM, PhD, of the American Cancer Society.
“We last included a special section on cancer survival in 2004, and, as we found then, survival improved over time for almost all cancers at every stage of diagnosis.”
For the current report, researchers calculated the 5-year average annual percent changes (AAPCs) for 2009 to 2013 for cancer incidence and for 2010 to 2014 for cancer mortality.
Cancer incidence (2009-2013)
In women, the AAPC increased 1.5% for leukemia (P<0.05), decreased 0.5% for NHL (P<0.05), and increased 2.2% for myeloma (P<0.05).
In men, the AAPC increased 1.7% for leukemia (P<0.05), decreased 0.2% for NHL, and increased 2.8% for myeloma (P<0.05).
Cancer mortality (2010-2014)
In women, the AAPC decreased 1.2% for leukemia (P<0.05), decreased 2.2% for NHL (P<0.05), and increased 0.5% for myeloma.
In men, the AAPC decreased 1.0% for leukemia (P<0.05), decreased 2.0% for NHL (P<0.05), and decreased 0.9% for myeloma (P<0.05).
5-year survival
The researchers compared 5-year relative survival for cancers diagnosed from 1975 to 1977 and those diagnosed from 2006 to 2012.
The absolute percentage change over time (for both sexes combined) was 26.1% for NHL, 25.7% for myeloma, and 28.5% for leukemia.
Five-year survival for patients diagnosed in 1975-1977 was 46.5% for NHL, 24.6% for myeloma, and 34.2% for leukemia.
Five-year survival for patients diagnosed in 2006-2012 was 72.6% for NHL, 50.2% for myeloma, and 62.7% for leukemia.