User login
Obesity-associated protein linked to AML
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
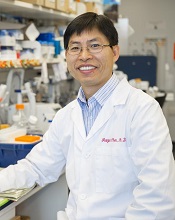
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
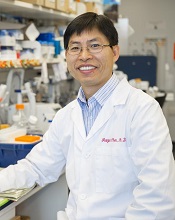
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
Syringes recalled due to infection risk
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at ProductRemovalInfo@nurseassist.com.
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
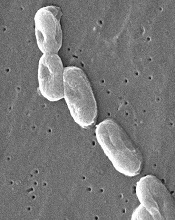
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at ProductRemovalInfo@nurseassist.com.
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
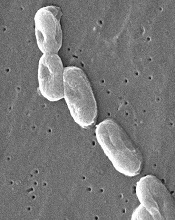
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at ProductRemovalInfo@nurseassist.com.
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
Antiplatelet agent may pose lower risk of bleeding

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()
GAP malaria vaccine shows early promise

Image from Margaret Shear
and Ute Frevert
A next-generation malaria vaccine that uses genetically attenuated parasites (GAPs) has demonstrated promise in a phase 1 trial and in experiments with mice, according to researchers.
The team generated a genetically attenuated Plasmodium falciparum parasite by knocking out 3 genes that are required for the parasite to cause malaria in humans.
Healthy volunteers infected with this parasite, Pf GAP3KO, exhibited strong antibody responses, according to researchers, and experienced only mild or moderate adverse events (AEs).
When antibodies from these patients were transferred to humanized mice, they inhibited malaria infection in the liver.
The researchers described this work in Science Translational Medicine.
“This most recent publication builds on our previous work,” said study author Sebastian Mikolajczak, PhD, of the Center for Infectious Disease Research in Seattle, Washington.
“We had already good indicators in preclinical studies that this new ‘triple knock-out’ GAP (GAP3KO), which has 3 genes removed, is completely attenuated. The clinical study now shows that the GAP3KO vaccine is completely attenuated in humans and also shows that, even after only a single administration, it elicits a robust immune response against the malaria parasite. Together, these findings are critical milestones for malaria vaccine development.”
Dr Mikolajczak and his colleagues created GAP3KO by knocking out 3 genes in P falciparum that are required for the parasite to successfully infect and cause disease in humans—Pf p52−/p36−/sap1−.
The researchers then tested Pf GAP3KO sporozoites in 10 healthy human volunteers. The sporozoites were delivered via bites from infected mosquitoes.
All subjects experienced grade 1 AEs, and 70% had grade 2 AEs. There were no grade 3 or higher AEs.
Grade 2 AEs included 1 case of fatigue and several cases of administration-site reactions, including erythema (n=6), pruritus (n=2), and swelling (n=3).
All 10 volunteers completed the 28-day study period without exhibiting any symptoms of malaria. They also remained negative for blood-stage parasitemia throughout the study period.
All subjects experienced antibody responses as well. The researchers collected sera from the volunteers on day 0, 7, 13, and 28 after immunization and analyzed it for anti-circumsporozoite protein (CSP) antibody responses.
The team measured anti-CSP immunoglobulin G (IgG) by enzyme-linked immunosorbent assay (ELISA) using full-length recombinant PfCSP protein.
At day 0, volunteers’ sera showed an average of 1436 ± 257.3 arbitrary units (AU) of anti-CSP titers by ELISA. However, 3 volunteers were slightly above the 2000 AU cutoff for positivity.
At day 7, 8 of the 10 volunteers were positive for anti-CSP IgG, with an average titer of 3821 ± 808.1 AU. At day 13, all volunteers were positive, with an average of 11,547 ± 2084 AU. Positivity was maintained through day 28, with an average of 5774± 840 AU.
To determine whether these antibodies could inhibit Pf sporozoite invasion in vivo, the researchers transferred them to FRG huHep liver chimeric humanized mice, which allow for complete development of liver-stage parasites.
The researchers chose 5 volunteers whose immune serum showed high levels of invasion inhibition in vitro and varying CSP IgG titers. The mice received purified IgG from these volunteers from day 0 and day 13 immune samples (5 mice per volunteer per time point).
The mice were then challenged with bites from mosquitoes infected with sporozoites of a green fluorescent protein–luciferase–expressing P falciparum strain.
The researchers calculated inhibition of infection by comparing the liver-stage burden of mice receiving day 13 IgG samples to the mean value of liver-stage burden in mice receiving day 0 IgG samples.
The day 13 IgG samples inhibited liver infection by an average of 23.18 ± 57%, 32.23 ± 29.16%, 69.38 ± 18.64%, 76.63 ± 19.98%, and 87.99 ± 15.56% (per volunteer).
The 3 volunteers whose serum exhibited the highest inhibition had the lowest Pf CSP titers of the 5 samples.
The researchers said these promising results in mice and humans pave the way to a phase 1b trial of the GAP3KO vaccine candidate using controlled human malaria infection. ![]()

Image from Margaret Shear
and Ute Frevert
A next-generation malaria vaccine that uses genetically attenuated parasites (GAPs) has demonstrated promise in a phase 1 trial and in experiments with mice, according to researchers.
The team generated a genetically attenuated Plasmodium falciparum parasite by knocking out 3 genes that are required for the parasite to cause malaria in humans.
Healthy volunteers infected with this parasite, Pf GAP3KO, exhibited strong antibody responses, according to researchers, and experienced only mild or moderate adverse events (AEs).
When antibodies from these patients were transferred to humanized mice, they inhibited malaria infection in the liver.
The researchers described this work in Science Translational Medicine.
“This most recent publication builds on our previous work,” said study author Sebastian Mikolajczak, PhD, of the Center for Infectious Disease Research in Seattle, Washington.
“We had already good indicators in preclinical studies that this new ‘triple knock-out’ GAP (GAP3KO), which has 3 genes removed, is completely attenuated. The clinical study now shows that the GAP3KO vaccine is completely attenuated in humans and also shows that, even after only a single administration, it elicits a robust immune response against the malaria parasite. Together, these findings are critical milestones for malaria vaccine development.”
Dr Mikolajczak and his colleagues created GAP3KO by knocking out 3 genes in P falciparum that are required for the parasite to successfully infect and cause disease in humans—Pf p52−/p36−/sap1−.
The researchers then tested Pf GAP3KO sporozoites in 10 healthy human volunteers. The sporozoites were delivered via bites from infected mosquitoes.
All subjects experienced grade 1 AEs, and 70% had grade 2 AEs. There were no grade 3 or higher AEs.
Grade 2 AEs included 1 case of fatigue and several cases of administration-site reactions, including erythema (n=6), pruritus (n=2), and swelling (n=3).
All 10 volunteers completed the 28-day study period without exhibiting any symptoms of malaria. They also remained negative for blood-stage parasitemia throughout the study period.
All subjects experienced antibody responses as well. The researchers collected sera from the volunteers on day 0, 7, 13, and 28 after immunization and analyzed it for anti-circumsporozoite protein (CSP) antibody responses.
The team measured anti-CSP immunoglobulin G (IgG) by enzyme-linked immunosorbent assay (ELISA) using full-length recombinant PfCSP protein.
At day 0, volunteers’ sera showed an average of 1436 ± 257.3 arbitrary units (AU) of anti-CSP titers by ELISA. However, 3 volunteers were slightly above the 2000 AU cutoff for positivity.
At day 7, 8 of the 10 volunteers were positive for anti-CSP IgG, with an average titer of 3821 ± 808.1 AU. At day 13, all volunteers were positive, with an average of 11,547 ± 2084 AU. Positivity was maintained through day 28, with an average of 5774± 840 AU.
To determine whether these antibodies could inhibit Pf sporozoite invasion in vivo, the researchers transferred them to FRG huHep liver chimeric humanized mice, which allow for complete development of liver-stage parasites.
The researchers chose 5 volunteers whose immune serum showed high levels of invasion inhibition in vitro and varying CSP IgG titers. The mice received purified IgG from these volunteers from day 0 and day 13 immune samples (5 mice per volunteer per time point).
The mice were then challenged with bites from mosquitoes infected with sporozoites of a green fluorescent protein–luciferase–expressing P falciparum strain.
The researchers calculated inhibition of infection by comparing the liver-stage burden of mice receiving day 13 IgG samples to the mean value of liver-stage burden in mice receiving day 0 IgG samples.
The day 13 IgG samples inhibited liver infection by an average of 23.18 ± 57%, 32.23 ± 29.16%, 69.38 ± 18.64%, 76.63 ± 19.98%, and 87.99 ± 15.56% (per volunteer).
The 3 volunteers whose serum exhibited the highest inhibition had the lowest Pf CSP titers of the 5 samples.
The researchers said these promising results in mice and humans pave the way to a phase 1b trial of the GAP3KO vaccine candidate using controlled human malaria infection. ![]()

Image from Margaret Shear
and Ute Frevert
A next-generation malaria vaccine that uses genetically attenuated parasites (GAPs) has demonstrated promise in a phase 1 trial and in experiments with mice, according to researchers.
The team generated a genetically attenuated Plasmodium falciparum parasite by knocking out 3 genes that are required for the parasite to cause malaria in humans.
Healthy volunteers infected with this parasite, Pf GAP3KO, exhibited strong antibody responses, according to researchers, and experienced only mild or moderate adverse events (AEs).
When antibodies from these patients were transferred to humanized mice, they inhibited malaria infection in the liver.
The researchers described this work in Science Translational Medicine.
“This most recent publication builds on our previous work,” said study author Sebastian Mikolajczak, PhD, of the Center for Infectious Disease Research in Seattle, Washington.
“We had already good indicators in preclinical studies that this new ‘triple knock-out’ GAP (GAP3KO), which has 3 genes removed, is completely attenuated. The clinical study now shows that the GAP3KO vaccine is completely attenuated in humans and also shows that, even after only a single administration, it elicits a robust immune response against the malaria parasite. Together, these findings are critical milestones for malaria vaccine development.”
Dr Mikolajczak and his colleagues created GAP3KO by knocking out 3 genes in P falciparum that are required for the parasite to successfully infect and cause disease in humans—Pf p52−/p36−/sap1−.
The researchers then tested Pf GAP3KO sporozoites in 10 healthy human volunteers. The sporozoites were delivered via bites from infected mosquitoes.
All subjects experienced grade 1 AEs, and 70% had grade 2 AEs. There were no grade 3 or higher AEs.
Grade 2 AEs included 1 case of fatigue and several cases of administration-site reactions, including erythema (n=6), pruritus (n=2), and swelling (n=3).
All 10 volunteers completed the 28-day study period without exhibiting any symptoms of malaria. They also remained negative for blood-stage parasitemia throughout the study period.
All subjects experienced antibody responses as well. The researchers collected sera from the volunteers on day 0, 7, 13, and 28 after immunization and analyzed it for anti-circumsporozoite protein (CSP) antibody responses.
The team measured anti-CSP immunoglobulin G (IgG) by enzyme-linked immunosorbent assay (ELISA) using full-length recombinant PfCSP protein.
At day 0, volunteers’ sera showed an average of 1436 ± 257.3 arbitrary units (AU) of anti-CSP titers by ELISA. However, 3 volunteers were slightly above the 2000 AU cutoff for positivity.
At day 7, 8 of the 10 volunteers were positive for anti-CSP IgG, with an average titer of 3821 ± 808.1 AU. At day 13, all volunteers were positive, with an average of 11,547 ± 2084 AU. Positivity was maintained through day 28, with an average of 5774± 840 AU.
To determine whether these antibodies could inhibit Pf sporozoite invasion in vivo, the researchers transferred them to FRG huHep liver chimeric humanized mice, which allow for complete development of liver-stage parasites.
The researchers chose 5 volunteers whose immune serum showed high levels of invasion inhibition in vitro and varying CSP IgG titers. The mice received purified IgG from these volunteers from day 0 and day 13 immune samples (5 mice per volunteer per time point).
The mice were then challenged with bites from mosquitoes infected with sporozoites of a green fluorescent protein–luciferase–expressing P falciparum strain.
The researchers calculated inhibition of infection by comparing the liver-stage burden of mice receiving day 13 IgG samples to the mean value of liver-stage burden in mice receiving day 0 IgG samples.
The day 13 IgG samples inhibited liver infection by an average of 23.18 ± 57%, 32.23 ± 29.16%, 69.38 ± 18.64%, 76.63 ± 19.98%, and 87.99 ± 15.56% (per volunteer).
The 3 volunteers whose serum exhibited the highest inhibition had the lowest Pf CSP titers of the 5 samples.
The researchers said these promising results in mice and humans pave the way to a phase 1b trial of the GAP3KO vaccine candidate using controlled human malaria infection. ![]()
Intervention relieves distress in cancer patients

chemotherapy
Photo by Rhoda Baer
Results of a small study suggest a single dose of the hallucinogenic drug psilocybin, when combined with counseling, can significantly lessen psychological distress in cancer patients for months at a time.
The study showed that psychological counseling and a single dose of psilocybin brought relief from distress that lasted for more than 6 months in a majority of the subjects monitored.
This was based on clinical evaluation scores for anxiety and depression.
“Our results represent the strongest evidence to date of a clinical benefit from psilocybin therapy, with the potential to transform care for patients with cancer-related psychological distress,” said study author Stephen Ross, MD, of New York University School of Medicine in New York, New York.
“If larger clinical trials prove successful, then we could ultimately have available a safe, effective, and inexpensive medication—dispensed under strict control—to alleviate the distress that increases suicide rates among cancer patients.”
Dr Ross and his colleagues reported the results of their study in the Journal of Psychopharmacology alongside a related study and 11 accompanying editorials.
Dr Ross’s study included 29 patients with cancer-related anxiety and depression. Their mean age was 56, and 62% were female. Ninety percent were Caucasian, and 10% were classified as “other” race.
Patients had breast cancer (31%), reproductive cancers (28%), digestive cancers (17%), leukemia/lymphoma (14%), and other cancers (10%).
All patients had been diagnosed as suffering from serious psychological distress related to their disease.
Treatment
Half of the patients were randomly assigned to receive a 0.3 mg/kg dose of psilocybin, and half received a vitamin placebo (250 mg of niacin) known to produce a “rush” that mimics a hallucinogenic drug experience.
Approximately half way through the study’s monitoring period (after 7 weeks), all patients switched treatments. Those who initially received psilocybin took a single dose of niacin, and vice-versa. Neither patients nor researchers knew who had first received psilocybin or placebo.
All patients were provided with tailored counseling from a psychiatrist, psychologist, nurse, or social worker. And the patients were monitored for side effects and improvements in their mental state.
Safety
The researchers said there were no serious adverse events (AEs), either medical or psychiatric, that were attributed to psilocybin.
The most common medical AEs that were attributable to psilocybin were non-clinically significant elevations in blood pressure and heart rate (76%), headaches/migraines (28%), and nausea (14%).
The most common psychiatric AEs attributable to psilocybin were transient anxiety (17%) and transient psychotic-like symptoms (7%; 1 case of transient paranoid ideation and 1 case of transient thought disorder).
Efficacy
The researchers said that, prior to the crossover, psilocybin produced immediate, substantial, and sustained improvements in anxiety and depression.
Specifically, patients who received psilocybin first had significant improvements in responses on the Hospital Anxiety and Depression Scale and the Beck Depression Inventory, when compared to patients who received niacin first.
The differences were significant 1 day after the patients’ first session and 7 weeks after the first session (P≤0.01 for all).
At the 6.5-month follow-up, 60% to 80% of participants continued with clinically significant reductions in depression or anxiety.
The researchers said a key finding of this study was that improvements in clinical evaluation scores for anxiety and depression lasted for the study’s extended monitoring period, which was 8 months for those who took psilocybin first.
Patients also reported post-psilocybin improvements in their quality of life, such as going out more, greater energy, getting along better with family members, and doing well at work. Some reported variations of spirituality, unusual peacefulness, and increased feelings of altruism.
“Our study showed that psilocybin facilitated experiences that drove reductions in psychological distress,” said study author Anthony Bossis, PhD, of New York University School of Medicine. “And if it’s true for cancer care, then it could apply to other stressful medical conditions.”
He cautioned that patients should not consume psilocybin on their own or without supervision from a physician and a trained counselor.
“Psilocybin therapy may not work for everyone,” he noted. “And some groups, such as people with schizophrenia, as well as adolescents, should not be treated with it.” ![]()

chemotherapy
Photo by Rhoda Baer
Results of a small study suggest a single dose of the hallucinogenic drug psilocybin, when combined with counseling, can significantly lessen psychological distress in cancer patients for months at a time.
The study showed that psychological counseling and a single dose of psilocybin brought relief from distress that lasted for more than 6 months in a majority of the subjects monitored.
This was based on clinical evaluation scores for anxiety and depression.
“Our results represent the strongest evidence to date of a clinical benefit from psilocybin therapy, with the potential to transform care for patients with cancer-related psychological distress,” said study author Stephen Ross, MD, of New York University School of Medicine in New York, New York.
“If larger clinical trials prove successful, then we could ultimately have available a safe, effective, and inexpensive medication—dispensed under strict control—to alleviate the distress that increases suicide rates among cancer patients.”
Dr Ross and his colleagues reported the results of their study in the Journal of Psychopharmacology alongside a related study and 11 accompanying editorials.
Dr Ross’s study included 29 patients with cancer-related anxiety and depression. Their mean age was 56, and 62% were female. Ninety percent were Caucasian, and 10% were classified as “other” race.
Patients had breast cancer (31%), reproductive cancers (28%), digestive cancers (17%), leukemia/lymphoma (14%), and other cancers (10%).
All patients had been diagnosed as suffering from serious psychological distress related to their disease.
Treatment
Half of the patients were randomly assigned to receive a 0.3 mg/kg dose of psilocybin, and half received a vitamin placebo (250 mg of niacin) known to produce a “rush” that mimics a hallucinogenic drug experience.
Approximately half way through the study’s monitoring period (after 7 weeks), all patients switched treatments. Those who initially received psilocybin took a single dose of niacin, and vice-versa. Neither patients nor researchers knew who had first received psilocybin or placebo.
All patients were provided with tailored counseling from a psychiatrist, psychologist, nurse, or social worker. And the patients were monitored for side effects and improvements in their mental state.
Safety
The researchers said there were no serious adverse events (AEs), either medical or psychiatric, that were attributed to psilocybin.
The most common medical AEs that were attributable to psilocybin were non-clinically significant elevations in blood pressure and heart rate (76%), headaches/migraines (28%), and nausea (14%).
The most common psychiatric AEs attributable to psilocybin were transient anxiety (17%) and transient psychotic-like symptoms (7%; 1 case of transient paranoid ideation and 1 case of transient thought disorder).
Efficacy
The researchers said that, prior to the crossover, psilocybin produced immediate, substantial, and sustained improvements in anxiety and depression.
Specifically, patients who received psilocybin first had significant improvements in responses on the Hospital Anxiety and Depression Scale and the Beck Depression Inventory, when compared to patients who received niacin first.
The differences were significant 1 day after the patients’ first session and 7 weeks after the first session (P≤0.01 for all).
At the 6.5-month follow-up, 60% to 80% of participants continued with clinically significant reductions in depression or anxiety.
The researchers said a key finding of this study was that improvements in clinical evaluation scores for anxiety and depression lasted for the study’s extended monitoring period, which was 8 months for those who took psilocybin first.
Patients also reported post-psilocybin improvements in their quality of life, such as going out more, greater energy, getting along better with family members, and doing well at work. Some reported variations of spirituality, unusual peacefulness, and increased feelings of altruism.
“Our study showed that psilocybin facilitated experiences that drove reductions in psychological distress,” said study author Anthony Bossis, PhD, of New York University School of Medicine. “And if it’s true for cancer care, then it could apply to other stressful medical conditions.”
He cautioned that patients should not consume psilocybin on their own or without supervision from a physician and a trained counselor.
“Psilocybin therapy may not work for everyone,” he noted. “And some groups, such as people with schizophrenia, as well as adolescents, should not be treated with it.” ![]()

chemotherapy
Photo by Rhoda Baer
Results of a small study suggest a single dose of the hallucinogenic drug psilocybin, when combined with counseling, can significantly lessen psychological distress in cancer patients for months at a time.
The study showed that psychological counseling and a single dose of psilocybin brought relief from distress that lasted for more than 6 months in a majority of the subjects monitored.
This was based on clinical evaluation scores for anxiety and depression.
“Our results represent the strongest evidence to date of a clinical benefit from psilocybin therapy, with the potential to transform care for patients with cancer-related psychological distress,” said study author Stephen Ross, MD, of New York University School of Medicine in New York, New York.
“If larger clinical trials prove successful, then we could ultimately have available a safe, effective, and inexpensive medication—dispensed under strict control—to alleviate the distress that increases suicide rates among cancer patients.”
Dr Ross and his colleagues reported the results of their study in the Journal of Psychopharmacology alongside a related study and 11 accompanying editorials.
Dr Ross’s study included 29 patients with cancer-related anxiety and depression. Their mean age was 56, and 62% were female. Ninety percent were Caucasian, and 10% were classified as “other” race.
Patients had breast cancer (31%), reproductive cancers (28%), digestive cancers (17%), leukemia/lymphoma (14%), and other cancers (10%).
All patients had been diagnosed as suffering from serious psychological distress related to their disease.
Treatment
Half of the patients were randomly assigned to receive a 0.3 mg/kg dose of psilocybin, and half received a vitamin placebo (250 mg of niacin) known to produce a “rush” that mimics a hallucinogenic drug experience.
Approximately half way through the study’s monitoring period (after 7 weeks), all patients switched treatments. Those who initially received psilocybin took a single dose of niacin, and vice-versa. Neither patients nor researchers knew who had first received psilocybin or placebo.
All patients were provided with tailored counseling from a psychiatrist, psychologist, nurse, or social worker. And the patients were monitored for side effects and improvements in their mental state.
Safety
The researchers said there were no serious adverse events (AEs), either medical or psychiatric, that were attributed to psilocybin.
The most common medical AEs that were attributable to psilocybin were non-clinically significant elevations in blood pressure and heart rate (76%), headaches/migraines (28%), and nausea (14%).
The most common psychiatric AEs attributable to psilocybin were transient anxiety (17%) and transient psychotic-like symptoms (7%; 1 case of transient paranoid ideation and 1 case of transient thought disorder).
Efficacy
The researchers said that, prior to the crossover, psilocybin produced immediate, substantial, and sustained improvements in anxiety and depression.
Specifically, patients who received psilocybin first had significant improvements in responses on the Hospital Anxiety and Depression Scale and the Beck Depression Inventory, when compared to patients who received niacin first.
The differences were significant 1 day after the patients’ first session and 7 weeks after the first session (P≤0.01 for all).
At the 6.5-month follow-up, 60% to 80% of participants continued with clinically significant reductions in depression or anxiety.
The researchers said a key finding of this study was that improvements in clinical evaluation scores for anxiety and depression lasted for the study’s extended monitoring period, which was 8 months for those who took psilocybin first.
Patients also reported post-psilocybin improvements in their quality of life, such as going out more, greater energy, getting along better with family members, and doing well at work. Some reported variations of spirituality, unusual peacefulness, and increased feelings of altruism.
“Our study showed that psilocybin facilitated experiences that drove reductions in psychological distress,” said study author Anthony Bossis, PhD, of New York University School of Medicine. “And if it’s true for cancer care, then it could apply to other stressful medical conditions.”
He cautioned that patients should not consume psilocybin on their own or without supervision from a physician and a trained counselor.
“Psilocybin therapy may not work for everyone,” he noted. “And some groups, such as people with schizophrenia, as well as adolescents, should not be treated with it.” ![]()
Infection in AML patient prompts discovery

Photo courtesy of
Janice Carr/CDC
The quest to understand a prolonged infection in an infant with acute myeloid leukemia (AML) has led to the discovery of a mutation that allows bacteria to tolerate antibiotic therapy.
Researchers described this discovery in the journal mBio.
“These findings detail a ‘perfect storm’ for development of antibiotic tolerance by bacteria that already pose a clinical challenge,” said study author Jason Rosch, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The same conditions may be present in other patients with immune systems that have been compromised by chemotherapy or disease,” added co-author Joshua Wolf, MBBS, also of St. Jude.
The “perfect storm” involved a patient who was 6 weeks old when she was diagnosed with AML. The treatment wiped out her white blood cells, and, despite infection-control measures, she developed a bloodstream infection with vancomycin-resistant Enterococcus faecium (VRE).
The infection persisted for 26 days and only resolved after her immune system recovered. She then successfully completed AML treatment.
In-depth DNA sequencing of 22 VRE samples collected during the patient’s infection helped researchers link the prolonged infection to a point mutation in the relA gene of VRE.
The mutation inappropriately activated the stringent response pathway, which bacteria use to survive under stress and to tolerate antibiotics.
The mutation resulted in elevated levels of the signaling molecule alarmone, and this likely primed the bacteria to survive exposure to multiple antibiotics, the researchers said.
The team also noted that relA-mutant VRE was susceptible to the antibiotics linezolid and daptomycin in minimum inhibitory concentration testing and during planktonic growth.
However, when growing in biofilm, relA-mutant VRE could tolerate high doses of both antibiotics.
“This mutation has particular clinical significance because the antibiotics involved, linezolid and daptomycin, are the last line of defense against VRE infection,” Dr Wolf said.
Among the compounds in development for the treatment of bacterial biofilms is the experimental antibiotic ADEP-4. In this study, ADEP-4 killed relA-mutant and non-mutant VRE growing in biofilm in the lab.
“In the future, compounds like ADEP-4 may provide a new approach to resolving persistent infections,” Dr Wolf said.
Dr Rosch noted that evidence gleaned from tracking the evolution of VRE throughout the infection suggested the patient’s immune-compromised state was essential to survival of the mutant VRE.
Gene transcription was altered significantly in relA-mutant VRE and produced biofilms that were less robust and possibly unlikely to otherwise survive.
“The case expands our understanding of the role of the stringent response in susceptibility and tolerance to a wide range of antibiotics, especially in biofilms,” Dr Rosch said. “It also demonstrates that these mutations can develop and gain a foothold during a human infection.” ![]()

Photo courtesy of
Janice Carr/CDC
The quest to understand a prolonged infection in an infant with acute myeloid leukemia (AML) has led to the discovery of a mutation that allows bacteria to tolerate antibiotic therapy.
Researchers described this discovery in the journal mBio.
“These findings detail a ‘perfect storm’ for development of antibiotic tolerance by bacteria that already pose a clinical challenge,” said study author Jason Rosch, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The same conditions may be present in other patients with immune systems that have been compromised by chemotherapy or disease,” added co-author Joshua Wolf, MBBS, also of St. Jude.
The “perfect storm” involved a patient who was 6 weeks old when she was diagnosed with AML. The treatment wiped out her white blood cells, and, despite infection-control measures, she developed a bloodstream infection with vancomycin-resistant Enterococcus faecium (VRE).
The infection persisted for 26 days and only resolved after her immune system recovered. She then successfully completed AML treatment.
In-depth DNA sequencing of 22 VRE samples collected during the patient’s infection helped researchers link the prolonged infection to a point mutation in the relA gene of VRE.
The mutation inappropriately activated the stringent response pathway, which bacteria use to survive under stress and to tolerate antibiotics.
The mutation resulted in elevated levels of the signaling molecule alarmone, and this likely primed the bacteria to survive exposure to multiple antibiotics, the researchers said.
The team also noted that relA-mutant VRE was susceptible to the antibiotics linezolid and daptomycin in minimum inhibitory concentration testing and during planktonic growth.
However, when growing in biofilm, relA-mutant VRE could tolerate high doses of both antibiotics.
“This mutation has particular clinical significance because the antibiotics involved, linezolid and daptomycin, are the last line of defense against VRE infection,” Dr Wolf said.
Among the compounds in development for the treatment of bacterial biofilms is the experimental antibiotic ADEP-4. In this study, ADEP-4 killed relA-mutant and non-mutant VRE growing in biofilm in the lab.
“In the future, compounds like ADEP-4 may provide a new approach to resolving persistent infections,” Dr Wolf said.
Dr Rosch noted that evidence gleaned from tracking the evolution of VRE throughout the infection suggested the patient’s immune-compromised state was essential to survival of the mutant VRE.
Gene transcription was altered significantly in relA-mutant VRE and produced biofilms that were less robust and possibly unlikely to otherwise survive.
“The case expands our understanding of the role of the stringent response in susceptibility and tolerance to a wide range of antibiotics, especially in biofilms,” Dr Rosch said. “It also demonstrates that these mutations can develop and gain a foothold during a human infection.” ![]()

Photo courtesy of
Janice Carr/CDC
The quest to understand a prolonged infection in an infant with acute myeloid leukemia (AML) has led to the discovery of a mutation that allows bacteria to tolerate antibiotic therapy.
Researchers described this discovery in the journal mBio.
“These findings detail a ‘perfect storm’ for development of antibiotic tolerance by bacteria that already pose a clinical challenge,” said study author Jason Rosch, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“The same conditions may be present in other patients with immune systems that have been compromised by chemotherapy or disease,” added co-author Joshua Wolf, MBBS, also of St. Jude.
The “perfect storm” involved a patient who was 6 weeks old when she was diagnosed with AML. The treatment wiped out her white blood cells, and, despite infection-control measures, she developed a bloodstream infection with vancomycin-resistant Enterococcus faecium (VRE).
The infection persisted for 26 days and only resolved after her immune system recovered. She then successfully completed AML treatment.
In-depth DNA sequencing of 22 VRE samples collected during the patient’s infection helped researchers link the prolonged infection to a point mutation in the relA gene of VRE.
The mutation inappropriately activated the stringent response pathway, which bacteria use to survive under stress and to tolerate antibiotics.
The mutation resulted in elevated levels of the signaling molecule alarmone, and this likely primed the bacteria to survive exposure to multiple antibiotics, the researchers said.
The team also noted that relA-mutant VRE was susceptible to the antibiotics linezolid and daptomycin in minimum inhibitory concentration testing and during planktonic growth.
However, when growing in biofilm, relA-mutant VRE could tolerate high doses of both antibiotics.
“This mutation has particular clinical significance because the antibiotics involved, linezolid and daptomycin, are the last line of defense against VRE infection,” Dr Wolf said.
Among the compounds in development for the treatment of bacterial biofilms is the experimental antibiotic ADEP-4. In this study, ADEP-4 killed relA-mutant and non-mutant VRE growing in biofilm in the lab.
“In the future, compounds like ADEP-4 may provide a new approach to resolving persistent infections,” Dr Wolf said.
Dr Rosch noted that evidence gleaned from tracking the evolution of VRE throughout the infection suggested the patient’s immune-compromised state was essential to survival of the mutant VRE.
Gene transcription was altered significantly in relA-mutant VRE and produced biofilms that were less robust and possibly unlikely to otherwise survive.
“The case expands our understanding of the role of the stringent response in susceptibility and tolerance to a wide range of antibiotics, especially in biofilms,” Dr Rosch said. “It also demonstrates that these mutations can develop and gain a foothold during a human infection.” ![]()
Drug eases existential anxiety in cancer patients

chemotherapy
Photo by Rhoda Baer
One-time treatment with the hallucinogenic drug psilocybin may provide long-term relief of existential anxiety in patients with life-threatening cancers, according to a small study.
After receiving a single high dose of the drug, most of the patients studied reported decreases in depression and anxiety as well as increases in quality of life and optimism.
These improvements were sustained at 6 months of follow-up.
“The most interesting and remarkable finding is that a single dose of psilocybin, which lasts 4 to 6 hours, produced enduring decreases in depression and anxiety symptoms, and this may represent a fascinating new model for treating some psychiatric conditions,” said study author Roland Griffiths, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Griffiths said this study grew out of a decade of research at Johns Hopkins on the effects of psilocybin in healthy volunteers, which showed that psilocybin can consistently produce positive changes in mood, behavior, and spirituality when administered to carefully screened and prepared participants.
The current study was designed to see if psilocybin could produce similar results in psychologically distressed cancer patients.
The results were published in the Journal of Psychopharmacology alongside a similar study and 11 accompanying editorials.
For their study, Dr Griffiths and his colleagues recruited 51 participants diagnosed with life-threatening cancers, most of which were recurrent or metastatic.
Types of cancer included breast (n=13), upper aerodigestive (n=7), gastrointestinal (n=4), genitourinary (n=18), and “other” cancers (n=1), as well as hematologic malignancies (n=8).
All participants had been given a formal psychiatric diagnosis, including an anxiety or depressive disorder.
Half of the participants were female, and they had an average age of 56. Ninety-two percent were white, 4% were black, and 2% were Asian.
Treatment
Each participant had 2 treatment sessions scheduled 5 weeks apart. In 1 session, they received a capsule containing a very low dose (1 or 3 mg per 70 kg) of psilocybin that was meant to act as a “control” because the dose was too low to produce effects.
In the other session, participants received a capsule with what is considered a moderate or high dose (22 or 30 mg per 70 kg).
To minimize expectancy effects, the participants and the staff members supervising the sessions were told that participants would receive psilocybin on both sessions, but they did not know that all participants would receive a high dose and a low dose.
Blood pressure and mood were monitored throughout the sessions.
Two monitors aided participants during each session, encouraging them to lie down, wear an eye mask, listen to music through headphones, and direct their attention on their inner experience. If anxiety or confusion arose, the monitors provided reassurance to the participants.
Participants, staff, and community observers rated participants’ moods, attitudes, and behaviors throughout the study.
The researchers assessed each participant via questionnaires and structured interviews before the first session, 7 hours after taking the psilocybin, 5 weeks after each session, and 6 months after the second session.
Adverse events
Thirty-four percent of participants had an episode of elevated systolic blood pressure (>160 mm Hg at 1 or more time-point) in the high-dose psilocybin session, and 17% of participants had such an episode in the low-dose session.
Thirteen percent and 2%, respectively, had an episode of elevated diastolic blood pressure (>100 mm Hg at 1 or more time-point). None of these episodes met criteria for medical intervention.
During the high-dose psilocybin session, 15% of patients experienced nausea or vomiting. There were no such events during the low-dose session.
Three participants reported mild to moderate headaches after the high-dose session.
Twenty-one percent of patients reported physical discomfort during the high-dose session, as did 8% of patients during the low-dose session.
Psychological discomfort occurred in 32% and 12% of participants, respectively. The researchers said there were no cases of hallucinogen persisting perception disorder or prolonged psychosis.
Efficacy outcomes
Most participants reported experiencing changes in visual perception, emotions, and thinking after taking high-dose psilocybin. They also reported experiences of psychological insight and profound, deeply meaningful experiences.
Six months after the final session of treatment, about 80% of participants continued to show clinically significant decreases in depressed mood and anxiety, according to clinician assessment.
According to the participants themselves, 83% had increases in well-being or life satisfaction at 6 months after treatment.
Sixty-seven percent of participants rated the experience as one of the top 5 meaningful experiences in their lives, and 70% rated the experience as one of their top 5 spiritually significant lifetime events.
“Before beginning the study, it wasn’t clear to me that this treatment would be helpful, since cancer patients may experience profound hopelessness in response to their diagnosis, which is often followed by multiple surgeries and prolonged chemotherapy,” Dr Griffiths said.
“I could imagine that cancer patients would receive psilocybin, look into the existential void, and come out even more fearful. However, the positive changes in attitudes, moods, and behavior that we documented in healthy volunteers were replicated in cancer patients.” ![]()

chemotherapy
Photo by Rhoda Baer
One-time treatment with the hallucinogenic drug psilocybin may provide long-term relief of existential anxiety in patients with life-threatening cancers, according to a small study.
After receiving a single high dose of the drug, most of the patients studied reported decreases in depression and anxiety as well as increases in quality of life and optimism.
These improvements were sustained at 6 months of follow-up.
“The most interesting and remarkable finding is that a single dose of psilocybin, which lasts 4 to 6 hours, produced enduring decreases in depression and anxiety symptoms, and this may represent a fascinating new model for treating some psychiatric conditions,” said study author Roland Griffiths, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Griffiths said this study grew out of a decade of research at Johns Hopkins on the effects of psilocybin in healthy volunteers, which showed that psilocybin can consistently produce positive changes in mood, behavior, and spirituality when administered to carefully screened and prepared participants.
The current study was designed to see if psilocybin could produce similar results in psychologically distressed cancer patients.
The results were published in the Journal of Psychopharmacology alongside a similar study and 11 accompanying editorials.
For their study, Dr Griffiths and his colleagues recruited 51 participants diagnosed with life-threatening cancers, most of which were recurrent or metastatic.
Types of cancer included breast (n=13), upper aerodigestive (n=7), gastrointestinal (n=4), genitourinary (n=18), and “other” cancers (n=1), as well as hematologic malignancies (n=8).
All participants had been given a formal psychiatric diagnosis, including an anxiety or depressive disorder.
Half of the participants were female, and they had an average age of 56. Ninety-two percent were white, 4% were black, and 2% were Asian.
Treatment
Each participant had 2 treatment sessions scheduled 5 weeks apart. In 1 session, they received a capsule containing a very low dose (1 or 3 mg per 70 kg) of psilocybin that was meant to act as a “control” because the dose was too low to produce effects.
In the other session, participants received a capsule with what is considered a moderate or high dose (22 or 30 mg per 70 kg).
To minimize expectancy effects, the participants and the staff members supervising the sessions were told that participants would receive psilocybin on both sessions, but they did not know that all participants would receive a high dose and a low dose.
Blood pressure and mood were monitored throughout the sessions.
Two monitors aided participants during each session, encouraging them to lie down, wear an eye mask, listen to music through headphones, and direct their attention on their inner experience. If anxiety or confusion arose, the monitors provided reassurance to the participants.
Participants, staff, and community observers rated participants’ moods, attitudes, and behaviors throughout the study.
The researchers assessed each participant via questionnaires and structured interviews before the first session, 7 hours after taking the psilocybin, 5 weeks after each session, and 6 months after the second session.
Adverse events
Thirty-four percent of participants had an episode of elevated systolic blood pressure (>160 mm Hg at 1 or more time-point) in the high-dose psilocybin session, and 17% of participants had such an episode in the low-dose session.
Thirteen percent and 2%, respectively, had an episode of elevated diastolic blood pressure (>100 mm Hg at 1 or more time-point). None of these episodes met criteria for medical intervention.
During the high-dose psilocybin session, 15% of patients experienced nausea or vomiting. There were no such events during the low-dose session.
Three participants reported mild to moderate headaches after the high-dose session.
Twenty-one percent of patients reported physical discomfort during the high-dose session, as did 8% of patients during the low-dose session.
Psychological discomfort occurred in 32% and 12% of participants, respectively. The researchers said there were no cases of hallucinogen persisting perception disorder or prolonged psychosis.
Efficacy outcomes
Most participants reported experiencing changes in visual perception, emotions, and thinking after taking high-dose psilocybin. They also reported experiences of psychological insight and profound, deeply meaningful experiences.
Six months after the final session of treatment, about 80% of participants continued to show clinically significant decreases in depressed mood and anxiety, according to clinician assessment.
According to the participants themselves, 83% had increases in well-being or life satisfaction at 6 months after treatment.
Sixty-seven percent of participants rated the experience as one of the top 5 meaningful experiences in their lives, and 70% rated the experience as one of their top 5 spiritually significant lifetime events.
“Before beginning the study, it wasn’t clear to me that this treatment would be helpful, since cancer patients may experience profound hopelessness in response to their diagnosis, which is often followed by multiple surgeries and prolonged chemotherapy,” Dr Griffiths said.
“I could imagine that cancer patients would receive psilocybin, look into the existential void, and come out even more fearful. However, the positive changes in attitudes, moods, and behavior that we documented in healthy volunteers were replicated in cancer patients.” ![]()

chemotherapy
Photo by Rhoda Baer
One-time treatment with the hallucinogenic drug psilocybin may provide long-term relief of existential anxiety in patients with life-threatening cancers, according to a small study.
After receiving a single high dose of the drug, most of the patients studied reported decreases in depression and anxiety as well as increases in quality of life and optimism.
These improvements were sustained at 6 months of follow-up.
“The most interesting and remarkable finding is that a single dose of psilocybin, which lasts 4 to 6 hours, produced enduring decreases in depression and anxiety symptoms, and this may represent a fascinating new model for treating some psychiatric conditions,” said study author Roland Griffiths, PhD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
Dr Griffiths said this study grew out of a decade of research at Johns Hopkins on the effects of psilocybin in healthy volunteers, which showed that psilocybin can consistently produce positive changes in mood, behavior, and spirituality when administered to carefully screened and prepared participants.
The current study was designed to see if psilocybin could produce similar results in psychologically distressed cancer patients.
The results were published in the Journal of Psychopharmacology alongside a similar study and 11 accompanying editorials.
For their study, Dr Griffiths and his colleagues recruited 51 participants diagnosed with life-threatening cancers, most of which were recurrent or metastatic.
Types of cancer included breast (n=13), upper aerodigestive (n=7), gastrointestinal (n=4), genitourinary (n=18), and “other” cancers (n=1), as well as hematologic malignancies (n=8).
All participants had been given a formal psychiatric diagnosis, including an anxiety or depressive disorder.
Half of the participants were female, and they had an average age of 56. Ninety-two percent were white, 4% were black, and 2% were Asian.
Treatment
Each participant had 2 treatment sessions scheduled 5 weeks apart. In 1 session, they received a capsule containing a very low dose (1 or 3 mg per 70 kg) of psilocybin that was meant to act as a “control” because the dose was too low to produce effects.
In the other session, participants received a capsule with what is considered a moderate or high dose (22 or 30 mg per 70 kg).
To minimize expectancy effects, the participants and the staff members supervising the sessions were told that participants would receive psilocybin on both sessions, but they did not know that all participants would receive a high dose and a low dose.
Blood pressure and mood were monitored throughout the sessions.
Two monitors aided participants during each session, encouraging them to lie down, wear an eye mask, listen to music through headphones, and direct their attention on their inner experience. If anxiety or confusion arose, the monitors provided reassurance to the participants.
Participants, staff, and community observers rated participants’ moods, attitudes, and behaviors throughout the study.
The researchers assessed each participant via questionnaires and structured interviews before the first session, 7 hours after taking the psilocybin, 5 weeks after each session, and 6 months after the second session.
Adverse events
Thirty-four percent of participants had an episode of elevated systolic blood pressure (>160 mm Hg at 1 or more time-point) in the high-dose psilocybin session, and 17% of participants had such an episode in the low-dose session.
Thirteen percent and 2%, respectively, had an episode of elevated diastolic blood pressure (>100 mm Hg at 1 or more time-point). None of these episodes met criteria for medical intervention.
During the high-dose psilocybin session, 15% of patients experienced nausea or vomiting. There were no such events during the low-dose session.
Three participants reported mild to moderate headaches after the high-dose session.
Twenty-one percent of patients reported physical discomfort during the high-dose session, as did 8% of patients during the low-dose session.
Psychological discomfort occurred in 32% and 12% of participants, respectively. The researchers said there were no cases of hallucinogen persisting perception disorder or prolonged psychosis.
Efficacy outcomes
Most participants reported experiencing changes in visual perception, emotions, and thinking after taking high-dose psilocybin. They also reported experiences of psychological insight and profound, deeply meaningful experiences.
Six months after the final session of treatment, about 80% of participants continued to show clinically significant decreases in depressed mood and anxiety, according to clinician assessment.
According to the participants themselves, 83% had increases in well-being or life satisfaction at 6 months after treatment.
Sixty-seven percent of participants rated the experience as one of the top 5 meaningful experiences in their lives, and 70% rated the experience as one of their top 5 spiritually significant lifetime events.
“Before beginning the study, it wasn’t clear to me that this treatment would be helpful, since cancer patients may experience profound hopelessness in response to their diagnosis, which is often followed by multiple surgeries and prolonged chemotherapy,” Dr Griffiths said.
“I could imagine that cancer patients would receive psilocybin, look into the existential void, and come out even more fearful. However, the positive changes in attitudes, moods, and behavior that we documented in healthy volunteers were replicated in cancer patients.”
Study reveals potential therapeutic targets for MDS

Preclinical research has revealed potential therapeutic targets for
myelodysplastic syndromes (MDS).
Investigators
found evidence to suggest that TRAF6, a toll-like receptor effector
with ubiquitin ligase activity, plays a key role in MDS.
So TRAF6 and
proteins regulated by TRAF6 may be therapeutic targets for MDS.
Daniel Starczynowski, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Nature Immunology.
The investigators first found that TRAF6 is overexpressed in hematopoietic stem/progenitor cells from MDS patients.
To more closely examine the role of TRAF6 in MDS, the team created mouse models in which the protein was overexpressed.
“We found that TRAF6 overexpression in mouse hematopoietic stem cells results in impaired blood cell formation and bone marrow failure,” Dr Starczynowski said.
Further investigation revealed that hnRNPA1, an RNA-binding protein and auxiliary splicing factor, is a substrate of TRAF6. And TRAF6 ubiquitination of hnRNPA1 regulates alternative splicing of Arhgap1.
This activates the GTP-binding Rho family protein Cdc42 and accounts for the defects observed in hematopoietic stem/progenitor cells that express TRAF6.
All of these proteins could be potential treatment targets for cases of MDS triggered by overexpression of TRAF6, according to Dr Starczynowski, who said future studies will test their therapeutic potential in mouse models of MDS.
“Based on our paper, a number of therapeutic approaches can be tested and directed against TRAF6 and other related proteins responsible for MDS,” he said.
Beyond the potential for new therapeutic approaches in MDS, this research revealed a new and critical immune-related function for TRAF6, according to the investigators.
TRAF6 regulates RNA isoform expression in response to various pathogens. In the context of the current study, TRAF6’s regulation of RNA isoform expression is important to the function of hematopoietic cells and reveals another dimension to how cells respond to infection, Dr Starczynowski said.

Preclinical research has revealed potential therapeutic targets for
myelodysplastic syndromes (MDS).
Investigators
found evidence to suggest that TRAF6, a toll-like receptor effector
with ubiquitin ligase activity, plays a key role in MDS.
So TRAF6 and
proteins regulated by TRAF6 may be therapeutic targets for MDS.
Daniel Starczynowski, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Nature Immunology.
The investigators first found that TRAF6 is overexpressed in hematopoietic stem/progenitor cells from MDS patients.
To more closely examine the role of TRAF6 in MDS, the team created mouse models in which the protein was overexpressed.
“We found that TRAF6 overexpression in mouse hematopoietic stem cells results in impaired blood cell formation and bone marrow failure,” Dr Starczynowski said.
Further investigation revealed that hnRNPA1, an RNA-binding protein and auxiliary splicing factor, is a substrate of TRAF6. And TRAF6 ubiquitination of hnRNPA1 regulates alternative splicing of Arhgap1.
This activates the GTP-binding Rho family protein Cdc42 and accounts for the defects observed in hematopoietic stem/progenitor cells that express TRAF6.
All of these proteins could be potential treatment targets for cases of MDS triggered by overexpression of TRAF6, according to Dr Starczynowski, who said future studies will test their therapeutic potential in mouse models of MDS.
“Based on our paper, a number of therapeutic approaches can be tested and directed against TRAF6 and other related proteins responsible for MDS,” he said.
Beyond the potential for new therapeutic approaches in MDS, this research revealed a new and critical immune-related function for TRAF6, according to the investigators.
TRAF6 regulates RNA isoform expression in response to various pathogens. In the context of the current study, TRAF6’s regulation of RNA isoform expression is important to the function of hematopoietic cells and reveals another dimension to how cells respond to infection, Dr Starczynowski said.

Preclinical research has revealed potential therapeutic targets for
myelodysplastic syndromes (MDS).
Investigators
found evidence to suggest that TRAF6, a toll-like receptor effector
with ubiquitin ligase activity, plays a key role in MDS.
So TRAF6 and
proteins regulated by TRAF6 may be therapeutic targets for MDS.
Daniel Starczynowski, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio, and his colleagues reported these findings in Nature Immunology.
The investigators first found that TRAF6 is overexpressed in hematopoietic stem/progenitor cells from MDS patients.
To more closely examine the role of TRAF6 in MDS, the team created mouse models in which the protein was overexpressed.
“We found that TRAF6 overexpression in mouse hematopoietic stem cells results in impaired blood cell formation and bone marrow failure,” Dr Starczynowski said.
Further investigation revealed that hnRNPA1, an RNA-binding protein and auxiliary splicing factor, is a substrate of TRAF6. And TRAF6 ubiquitination of hnRNPA1 regulates alternative splicing of Arhgap1.
This activates the GTP-binding Rho family protein Cdc42 and accounts for the defects observed in hematopoietic stem/progenitor cells that express TRAF6.
All of these proteins could be potential treatment targets for cases of MDS triggered by overexpression of TRAF6, according to Dr Starczynowski, who said future studies will test their therapeutic potential in mouse models of MDS.
“Based on our paper, a number of therapeutic approaches can be tested and directed against TRAF6 and other related proteins responsible for MDS,” he said.
Beyond the potential for new therapeutic approaches in MDS, this research revealed a new and critical immune-related function for TRAF6, according to the investigators.
TRAF6 regulates RNA isoform expression in response to various pathogens. In the context of the current study, TRAF6’s regulation of RNA isoform expression is important to the function of hematopoietic cells and reveals another dimension to how cells respond to infection, Dr Starczynowski said.
Team characterizes therapy-resistant ALL cells

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.”

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.”

Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.”
Drugs may be effective against hematologic, other cancers

Image courtesy of PNAS
A diabetes medication and an antihypertensive drug may prove effective in the treatment of hematologic malignancies and other cancers, according to preclinical research published in Science Advances.
Past research has shown that metformin, a drug used to treat type 2 diabetes, has anticancer properties.
However, the usual therapeutic dose is too low to effectively fight cancer, and higher doses of metformin could be too toxic.
With the current study, researchers found that the antihypertensive drug syrosingopine enhances the anticancer efficacy of metformin without harming normal blood cells.
The team screened over a thousand drugs to find one that could boost metformin’s efficacy against cancers.
They identified syrosingopine and tested it in combination with metformin—at concentrations substantially below the drugs’ therapeutic thresholds—on a range of cancer cell lines and in mouse models of liver cancer.
Thirty-five of the 43 cell lines tested were susceptible to both syrosingopine and metformin. This included leukemia, lymphoma, and multiple myeloma cell lines.
In addition, the mice given a short course of syrosingopine and metformin experienced a reduction in the number of visible liver tumors.
The researchers also tested syrosingopine and metformin in peripheral blasts from 12 patients with acute myeloid leukemia and a patient with blast crisis chronic myeloid leukemia. All 13 samples responded to the treatment.
On the other hand, syrosingopine and metformin did not affect peripheral blood cells from healthy subjects.
“[A]lmost all tumor cells were killed by this cocktail and at doses that are actually not toxic to normal cells,” said study author Don Benjamin, of the University of Basel in Switzerland.
“And the effect was exclusively confined to cancer cells, as the blood cells from healthy donors were insensitive to the treatment.”
The researchers believe metformin functions by lowering blood glucose levels for cancer cells, starving them of essential nutrients needed for their survival. However, it is not clear how syrosingopine works in conjunction with metformin.
The team emphasized the need for more research evaluating the drugs in combination.
“We have been able to show that the 2 known drugs lead to more profound effects on cancer cell proliferation than each drug alone,” Dr Benjamin said. “The data from this study support the development of combination approaches for the treatment of cancer patients.”

Image courtesy of PNAS
A diabetes medication and an antihypertensive drug may prove effective in the treatment of hematologic malignancies and other cancers, according to preclinical research published in Science Advances.
Past research has shown that metformin, a drug used to treat type 2 diabetes, has anticancer properties.
However, the usual therapeutic dose is too low to effectively fight cancer, and higher doses of metformin could be too toxic.
With the current study, researchers found that the antihypertensive drug syrosingopine enhances the anticancer efficacy of metformin without harming normal blood cells.
The team screened over a thousand drugs to find one that could boost metformin’s efficacy against cancers.
They identified syrosingopine and tested it in combination with metformin—at concentrations substantially below the drugs’ therapeutic thresholds—on a range of cancer cell lines and in mouse models of liver cancer.
Thirty-five of the 43 cell lines tested were susceptible to both syrosingopine and metformin. This included leukemia, lymphoma, and multiple myeloma cell lines.
In addition, the mice given a short course of syrosingopine and metformin experienced a reduction in the number of visible liver tumors.
The researchers also tested syrosingopine and metformin in peripheral blasts from 12 patients with acute myeloid leukemia and a patient with blast crisis chronic myeloid leukemia. All 13 samples responded to the treatment.
On the other hand, syrosingopine and metformin did not affect peripheral blood cells from healthy subjects.
“[A]lmost all tumor cells were killed by this cocktail and at doses that are actually not toxic to normal cells,” said study author Don Benjamin, of the University of Basel in Switzerland.
“And the effect was exclusively confined to cancer cells, as the blood cells from healthy donors were insensitive to the treatment.”
The researchers believe metformin functions by lowering blood glucose levels for cancer cells, starving them of essential nutrients needed for their survival. However, it is not clear how syrosingopine works in conjunction with metformin.
The team emphasized the need for more research evaluating the drugs in combination.
“We have been able to show that the 2 known drugs lead to more profound effects on cancer cell proliferation than each drug alone,” Dr Benjamin said. “The data from this study support the development of combination approaches for the treatment of cancer patients.”

Image courtesy of PNAS
A diabetes medication and an antihypertensive drug may prove effective in the treatment of hematologic malignancies and other cancers, according to preclinical research published in Science Advances.
Past research has shown that metformin, a drug used to treat type 2 diabetes, has anticancer properties.
However, the usual therapeutic dose is too low to effectively fight cancer, and higher doses of metformin could be too toxic.
With the current study, researchers found that the antihypertensive drug syrosingopine enhances the anticancer efficacy of metformin without harming normal blood cells.
The team screened over a thousand drugs to find one that could boost metformin’s efficacy against cancers.
They identified syrosingopine and tested it in combination with metformin—at concentrations substantially below the drugs’ therapeutic thresholds—on a range of cancer cell lines and in mouse models of liver cancer.
Thirty-five of the 43 cell lines tested were susceptible to both syrosingopine and metformin. This included leukemia, lymphoma, and multiple myeloma cell lines.
In addition, the mice given a short course of syrosingopine and metformin experienced a reduction in the number of visible liver tumors.
The researchers also tested syrosingopine and metformin in peripheral blasts from 12 patients with acute myeloid leukemia and a patient with blast crisis chronic myeloid leukemia. All 13 samples responded to the treatment.
On the other hand, syrosingopine and metformin did not affect peripheral blood cells from healthy subjects.
“[A]lmost all tumor cells were killed by this cocktail and at doses that are actually not toxic to normal cells,” said study author Don Benjamin, of the University of Basel in Switzerland.
“And the effect was exclusively confined to cancer cells, as the blood cells from healthy donors were insensitive to the treatment.”
The researchers believe metformin functions by lowering blood glucose levels for cancer cells, starving them of essential nutrients needed for their survival. However, it is not clear how syrosingopine works in conjunction with metformin.
The team emphasized the need for more research evaluating the drugs in combination.
“We have been able to show that the 2 known drugs lead to more profound effects on cancer cell proliferation than each drug alone,” Dr Benjamin said. “The data from this study support the development of combination approaches for the treatment of cancer patients.”