User login
Point-of-Care Ultrasound for Hospitalists: A Position Statement of the Society of Hospital Medicine
Many hospitalists incorporate point-of-care ultrasound (POCUS) into their daily practice because it adds value to their bedside evaluation of patients. However, standards for training and assessing hospitalists in POCUS have not yet been established. Other acute care specialties, including emergency medicine and critical care medicine, have already incorporated POCUS into their graduate medical education training programs, but most internal medicine residency programs are only beginning to provide POCUS training.1
Several features distinguish POCUS from comprehensive ultrasound examinations. First, POCUS is designed to answer focused questions, whereas comprehensive ultrasound examinations evaluate all organs in an anatomical region; for example, an abdominal POCUS exam may evaluate only for presence or absence of intraperitoneal free fluid, whereas a comprehensive examination of the right upper quadrant will evaluate the liver, gallbladder, and biliary ducts. Second, POCUS examinations are generally performed by the same clinician who generates the relevant clinical question to answer with POCUS and ultimately integrates the findings into the patient’s care.2 By contrast, comprehensive ultrasound examinations involve multiple providers and steps: a clinician generates a relevant clinical question and requests an ultrasound examination that is acquired by a sonographer, interpreted by a radiologist, and reported back to the requesting clinician. Third, POCUS is often used to evaluate multiple body systems. For example, to evaluate a patient with undifferentiated hypotension, a multisystem POCUS examination of the heart, inferior vena cava, lungs, abdomen, and lower extremity veins is typically performed. Finally, POCUS examinations can be performed serially to investigate changes in clinical status or evaluate response to therapy, such as monitoring the heart, lungs, and inferior vena cava during fluid resuscitation.
The purpose of this position statement is to inform a broad audience about how hospitalists are using diagnostic and procedural applications of POCUS. This position statement does not mandate that hospitalists use POCUS. Rather, it is intended to provide guidance on the safe and effective use of POCUS by the hospitalists who use it and the administrators who oversee its use. We discuss POCUS (1) applications, (2) training, (3) assessments, and (4) program management. This position statement was reviewed and approved by the Society of Hospital Medicine (SHM) Executive Committee in March 2018.
APPLICATIONS
As outlined in our earlier position statements,3,4 ultrasound guidance lowers complication rates and increases success rates of invasive bedside procedures. Diagnostic POCUS can guide clinical decision making prior to bedside procedures. For instance, hospitalists may use POCUS to assess the size and character of a pleural effusion to help determine the most appropriate management strategy: observation, medical treatment, thoracentesis, chest tube placement, or surgical therapy. Furthermore, diagnostic POCUS can be used to rapidly assess for immediate postprocedural complications, such as pneumothorax, or if the patient develops new symptoms.
TRAINING
Basic Knowledge
Basic knowledge includes fundamentals of ultrasound physics; safety;4 anatomy; physiology; and device operation, including maintenance and cleaning. Basic knowledge can be taught by multiple methods, including live or recorded lectures, online modules, or directed readings.
Image Acquisition
Training should occur across multiple types of patients (eg, obese, cachectic, postsurgical) and clinical settings (eg, intensive care unit, general medicine wards, emergency department) when available. Training is largely hands-on because the relevant skills involve integration of 3D anatomy with spatial manipulation, hand-eye coordination, and fine motor movements. Virtual reality ultrasound simulators may accelerate mastery, particularly for cardiac image acquisition, and expose learners to standardized sets of pathologic findings. Real-time bedside feedback on image acquisition is ideal because understanding how ultrasound probe manipulation affects the images acquired is essential to learning.
Image Interpretation
Training in image interpretation relies on visual pattern recognition of normal and abnormal findings. Therefore, the normal to abnormal spectrum should be broad, and learners should maintain a log of what abnormalities have been identified. Giving real-time feedback at the bedside is ideal because of the connection between image acquisition and interpretation. Image interpretation can be taught through didactic sessions, image review sessions, or review of teaching files with annotated images.
Clinical Integration
Learners must interpret and integrate image findings with other clinical data considering the image quality, patient characteristics, and changing physiology. Clinical integration should be taught by instructors that share similar clinical knowledge as learners. Although sonographers are well suited to teach image acquisition, they should not be the sole instructors to teach hospitalists how to integrate ultrasound findings in clinical decision making. Likewise, emphasis should be placed on the appropriate use of POCUS within a provider’s skill set. Learners must appreciate the clinical significance of POCUS findings, including recognition of incidental findings that may require further workup. Supplemental training in clinical integration can occur through didactics that include complex patient scenarios.
Pathways
Clinical competency can be achieved with training adherent to five criteria. First, the training environment should be similar to where the trainee will practice. Second, training and feedback should occur in real time. Third, specific applications should be taught rather than broad training in “hospitalist POCUS.” Each application requires unique skills and knowledge, including image acquisition pitfalls and artifacts. Fourth, clinical competence must be achieved and demonstrated; it is not necessarily gained through experience. Fifth, once competency is achieved, continued education and feedback are necessary to ensure it is maintained.
Residency-based POCUS training pathways can best fulfill these criteria. They may eventually become commonplace, but until then alternative pathways must exist for hospitalist providers who are already in practice. There are three important attributes of such pathways. First, administrators’ expectations about learners’ clinical productivity must be realistically, but only temporarily, relaxed; otherwise, competing demands on time will likely overwhelm learners and subvert training. Second, training should begin through a local or national hands-on training program. The SHM POCUS certificate program consolidates training for common diagnostic POCUS applications for hospitalists.6 Other medical societies offer training for their respective clinical specialties.7 Third, once basic POCUS training has begun, longitudinal training should continue ideally with a local hospitalist POCUS expert.
In some settings, a subgroup of hospitalists may not desire, or be able to achieve, competency in the manual skills of POCUS image acquisition. Nevertheless, hospitalists may still find value in understanding POCUS nomenclature, image pattern recognition, and the evidence and pitfalls behind clinical integration of specific POCUS findings. This subset of POCUS skills allows hospitalists to communicate effectively with and understand the clinical decisions made by their colleagues who are competent in POCUS use.
The minimal skills a hospitalist should possess to serve as a POCUS trainer include proficiency of basic knowledge, image acquisition, image interpretation, and clinical integration of the POCUS applications being taught; effectiveness as a hands-on instructor to teach image acquisition skills; and an in-depth understanding of common POCUS pitfalls and limitations.
ASSESSMENTS
Assessment methods for POCUS can include the following: knowledge-based questions, image acquisition using task-specific checklists on human or simulation models, image interpretation using a series of videos or still images with normal and abnormal findings, clinical integration using “next best step” in a multiple choice format with POCUS images, and simulation-based clinical scenarios. Assessment methods should be aligned with local availability of resources and trainers.
Basic Knowledge
Basic knowledge can be assessed via multiple choice questions assessing knowledge of ultrasound physics, image optimization, relevant anatomy, and limitations of POCUS imaging. Basic knowledge lies primarily in the cognitive domain and does not assess manual skills.
Image Acquisition
Image acquisition can be assessed by observation and rating of image quality. Where resources allow, assessment of image acquisition is likely best done through a combination of developing an image portfolio with a minimum number of high quality images, plus direct observation of image acquisition by an expert. Various programs have utilized minimum numbers of images acquired to help define competence with image acquisition skills.6–8 Although minimums may be a necessary step to gain competence, using them as a sole means to determine competence does not account for variable learning curves.9 As with other manual skills in hospital medicine, such as ultrasound-guided bedside procedures, minimum numbers are best used as a starting point for assessments.3,10 In this regard, portfolio development with meticulous attention to the gain, depth, and proper tomographic plane of images can monitor a hospitalist’s progress toward competence by providing objective assessments and feedback. Simulation may also be used as it allows assessment of image acquisition skills and an opportunity to provide real-time feedback, similar to direct observation but without actual patients.
Image Interpretation
Image interpretation is best assessed by an expert observing the learner at bedside; however, when bedside assessment is not possible, image interpretation skills may be assessed using multiple choice or free text interpretation of archived ultrasound images with normal and abnormal findings. This is often incorporated into the portfolio development portion of a training program, as learners can submit their image interpretation along with the video clip. Both normal and abnormal images can be used to assess anatomic recognition and interpretation. Emphasis should be placed on determining when an image is suboptimal for diagnosis (eg, incomplete exam or poor-quality images). Quality assurance programs should incorporate structured feedback sessions.
Clinical Integration
Assessment of clinical integration can be completed through case scenarios that assess knowledge, interpretation of images, and integration of findings into clinical decision making, which is often delivered via a computer-based assessment. Assessments should combine specific POCUS applications to evaluate common clinical problems in hospital medicine, such as undifferentiated hypotension and dyspnea. High-fidelity simulators can be used to blend clinical case scenarios with image acquisition, image interpretation, and clinical integration. When feasible, comprehensive feedback on how providers acquire, interpret, and apply ultrasound at the bedside is likely the best mechanism to assess clinical integration. This process can be done with a hospitalist’s own patients.
General Assessment
A general assessment that includes a summative knowledge and hands-on skills assessment using task-specific checklists can be performed upon completion of training. A high-fidelity simulator with dynamic or virtual anatomy can provide reproducible standardized assessments with variation in the type and difficulty of cases. When available, we encourage the use of dynamic assessments on actual patients that have both normal and abnormal ultrasound findings because simulated patient scenarios have limitations, even with the use of high-fidelity simulators. Programs are recommended to use formative and summative assessments for evaluation. Quantitative scoring systems using checklists are likely the best framework.11,12
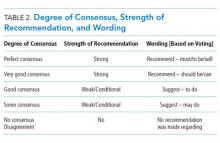
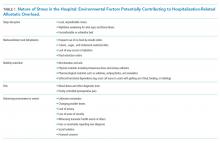
CERTIFICATES AND CERTIFICATION
A certificate of completion is proof of a provider’s participation in an educational activity; it does not equate with competency, though it may be a step toward it. Most POCUS training workshops and short courses provide certificates of completion. Certification of competency is an attestation of a hospitalist’s basic competence within a defined scope of practice (Table 2).13 However, without longitudinal supervision and feedback, skills can decay; therefore, we recommend a longitudinal training program that provides mentored feedback and incorporates periodic competency assessments. At present, no national board certification in POCUS is available to grant external certification of competency for hospitalists.
External Certificate
Certificates of completion can be external through a national organization. An external certificate of completion designed for hospitalists includes the POCUS Certificate of Completion offered by SHM in collaboration with CHEST.6 This certificate program provides regional training options and longitudinal portfolio development. Other external certificates are also available to hospitalists.7,14,15
Most hospitalists are boarded by the American Board of Internal Medicine or the American Board of Family Medicine. These boards do not yet include certification of competency in POCUS. Other specialty boards, such as emergency medicine, include competency in POCUS. For emergency medicine, completion of an accredited residency training program and certification by the national board includes POCUS competency.
Internal Certificate
There are a few examples of successful local institutional programs that have provided internal certificates of competency.12,14 Competency assessments require significant resources including investment by both faculty and learners. Ongoing evaluation of competency should be based on quality assurance processes.
Credentialing and Privileging
The American Medical Association (AMA) House of Delegates in 1999 passed a resolution (AMA HR. 802) recommending hospitals follow specialty-specific guidelines for privileging decisions related to POCUS use.17 The resolution included a statement that, “ultrasound imaging is within the scope of practice of appropriately trained physicians.”
Some institutions have begun to rely on a combination of internal and external certificate programs to grant privileges to hospitalists.10 Although specific privileges for POCUS may not be required in some hospitals, some institutions may require certification of training and assessments prior to granting permission to use POCUS.
Hospitalist programs are encouraged to evaluate ongoing POCUS use by their providers after granting initial permission. If privileging is instituted by a hospital, hospitalists must play a significant role in determining the requirements for privileging and ongoing maintenance of skills.
Maintenance of Skills
All medical skills can decay with disuse, including those associated with POCUS.12,18 Thus, POCUS users should continue using POCUS regularly in clinical practice and participate in POCUS continuing medical education activities, ideally with ongoing assessments. Maintenance of skills may be confirmed through routine participation in a quality assurance program.
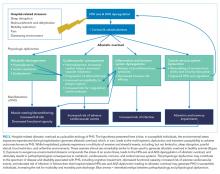
PROGRAM MANAGEMENT
Use of POCUS in hospital medicine has unique considerations, and hospitalists should be integrally involved in decision making surrounding institutional POCUS program management. Appointing a dedicated POCUS director can help a program succeed.8
Equipment and Image Archiving
Several factors are important to consider when selecting an ultrasound machine: portability, screen size, and ease of use; integration with the electronic medical record and options for image archiving; manufacturer’s service plan, including technical and clinical support; and compliance with local infection control policies. The ability to easily archive and retrieve images is essential for quality assurance, continuing education, institutional quality improvement, documentation, and reimbursement. In certain scenarios, image archiving may not be possible (such as with personal handheld devices or in emergency situations) or necessary (such as with frequent serial examinations during fluid resuscitation). An image archive is ideally linked to reports, orders, and billing software.10,19 If such linkages are not feasible, parallel external storage that complies with regulatory standards (ie, HIPAA compliance) may be suitable.20
Documentation and Billing
Components of documentation include the indication and type of ultrasound examination performed, date and time of the examination, patient identifying information, name of provider(s) acquiring and interpreting the images, specific scanning protocols used, patient position, probe used, and findings. Documentation can occur through a standalone note or as part of another note, such as a progress note. Whenever possible, documentation should be timely to facilitate communication with other providers.
Billing is supported through the AMA Current Procedural Terminology codes for “focused” or “limited” ultrasound examinations (Appendix 9). The following three criteria must be satisfied for billing. First, images must be permanently stored. Specific requirements vary by insurance policy, though current practice suggests a minimum of one image demonstrating relevant anatomy and pathology for the ultrasound examination coded. For ultrasound-guided procedures that require needle insertion, images should be captured at the point of interest, and a procedure note should reflect that the needle was guided and visualized under ultrasound.21 Second, proper documentation must be entered in the medical record. Third, local institutional privileges for POCUS must be considered. Although privileges are not required to bill, some hospitals or payers may require them.
Quality Assurance
Published guidelines on quality assurance in POCUS are available from different specialty organizations, including emergency medicine, pediatric emergency medicine, critical care, anesthesiology, obstetrics, and cardiology.8,22–28 Quality assurance is aimed at ensuring that physicians maintain basic competency in using POCUS to influence bedside decisions.
Quality assurance should be carried out by an individual or committee with expertise in POCUS. Multidisciplinary QA programs in which hospital medicine providers are working collaboratively with other POCUS providers have been demonstrated to be highly effective.10 Oversight includes ensuring that providers using POCUS are appropriately trained,10,22,28 using the equipment correctly,8,26,28 and documenting properly. Some programs have implemented mechanisms to review and provide feedback on image acquisition, interpretation, and clinical integration.8,10 Other programs have compared POCUS findings with referral studies, such as comprehensive ultrasound examinations.
CONCLUSIONS
Practicing hospitalists must continue to collaborate with their institutions to build POCUS capabilities. In particular, they must work with their local privileging body to determine what credentials are required. The distinction between certificates of completion and certificates of competency, including whether those certificates are internal or external, is important in the credentialing process.
External certificates of competency are currently unavailable for most practicing hospitalists because ABIM certification does not include POCUS-related competencies. As internal medicine residency training programs begin to adopt POCUS training and certification into their educational curricula, we foresee a need to update the ABIM Policies and Procedures for Certification. Until then, we recommend that certificates of competency be defined and granted internally by local hospitalist groups.
Given the many advantages of POCUS over traditional tools, we anticipate its increasing implementation among hospitalists in the future. As with all medical technology, its role in clinical care should be continuously reexamined and redefined through health services research. Such information will be useful in developing practice guidelines, educational curricula, and training standards.
Acknowledgments
The authors would like to thank all members that participated in the discussion and finalization of this position statement during the Point-of-care Ultrasound Faculty Retreat at the 2018 Society of Hospital Medicine Annual Conference: Saaid Abdel-Ghani, Brandon Boesch, Joel Cho, Ria Dancel, Renee Dversdal, Ricardo Franco-Sadud, Benjamin Galen, Trevor P. Jensen, Mohit Jindal, Gordon Johnson, Linda M. Kurian, Gigi Liu, Charles M. LoPresti, Brian P. Lucas, Venkat Kalidindi, Benji Matthews, Anna Maw, Gregory Mints, Kreegan Reierson, Gerard Salame, Richard Schildhouse, Daniel Schnobrich, Nilam Soni, Kirk Spencer, Hiromizu Takahashi, David M. Tierney, Tanping Wong, and Toru Yamada.
1. Schnobrich DJ, Mathews BK, Trappey BE, Muthyala BK, Olson APJ. Entrusting internal medicine residents to use point of care ultrasound: Towards improved assessment and supervision. Med Teach. 2018:1-6. doi:10.1080/0142159X.2018.1457210.
2. Soni NJ, Lucas BP. Diagnostic point-of-care ultrasound for hospitalists. J Hosp Med. 2015;10(2):120-124. doi:10.1002/jhm.2285.
3. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):117-125. doi:10.12788/jhm.2917.
4. Dancel R, Schnobrich D, Puri N, et al. Recommendations on the use of ultrasound guidance for adult thoracentesis: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):126-135. doi:10.12788/jhm.2940.
5. National Council on Radiation Protection and Measurements, The Council. Implementation of the Principle of as Low as Reasonably Achievable (ALARA) for Medical and Dental Personnel.; 1990.
6. Society of Hospital Medicine. Point of Care Ultrasound course: https://www.hospitalmedicine.org/clinical-topics/ultrasonography-cert/. Accessed February 6, 2018.
7. Critical Care Ultrasonography Certificate of Completion Program. CHEST. American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography. Accessed February 6, 2018.
8. American College of Emergency Physicians Policy Statement: Emergency Ultrasound Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/ACEP-Ultrasound-Guidelines/. Accessed February 6, 2018.
9. Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med. 2015;22(5):574-582. doi:10.1111/acem.12653.
10. Mathews BK, Zwank M. Hospital medicine point of care ultrasound credentialing: an example protocol. J Hosp Med. 2017;12(9):767-772. doi:10.12788/jhm.2809.
11. Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009;4(7):397-403. doi:10.1002/jhm.468.
12. Mathews BK, Reierson K, Vuong K, et al. The design and evaluation of the Comprehensive Hospitalist Assessment and Mentorship with Portfolios (CHAMP) ultrasound program. J Hosp Med. 2018;13(8):544-550. doi:10.12788/jhm.2938.
13. Soni NJ, Tierney DM, Jensen TP, Lucas BP. Certification of point-of-care ultrasound competency. J Hosp Med. 2017;12(9):775-776. doi:10.12788/jhm.2812.
14. Ultrasound Certification for Physicians. Alliance for Physician Certification and Advancement. APCA. https://apca.org/. Accessed February 6, 2018.
15. National Board of Echocardiography, Inc. https://www.echoboards.org/EchoBoards/News/2019_Adult_Critical_Care_Echocardiography_Exam.aspx. Accessed June 18, 2018.
16. Tierney DM. Internal Medicine Bedside Ultrasound Program (IMBUS). Abbott Northwestern. http://imbus.anwresidency.com/index.html. Accessed February 6, 2018.
17. American Medical Association House of Delegates Resolution H-230.960: Privileging for Ultrasound Imaging. Resolution 802. Policy Finder Website. http://search0.ama-assn.org/search/pfonline. Published 1999. Accessed February 18, 2018.
18. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi:10.4300/JGME-14-00284.1.
19. Flannigan MJ, Adhikari S. Point-of-care ultrasound work flow innovation: impact on documentation and billing. J Ultrasound Med. 2017;36(12):2467-2474. doi:10.1002/jum.14284.
20. Emergency Ultrasound: Workflow White Paper. https://www.acep.org/uploadedFiles/ACEP/memberCenter/SectionsofMembership/ultra/Workflow%20White%20Paper.pdf. Published 2013. Accessed February 18, 2018.
21. Ultrasound Coding and Reimbursement Document 2009. Emergency Ultrasound Section. American College of Emergency Physicians. http://emergencyultrasoundteaching.com/assets/2009_coding_update.pdf. Published 2009. Accessed February 18, 2018.
22. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest. 2009;135(4):1050-1060. doi:10.1378/chest.08-2305.
23. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part I: general ultrasonography. Crit Care Med. 2015;43(11):2479-2502. doi:10.1097/ccm.0000000000001216.
24. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part ii: cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. doi:10.1097/ccm.0000000000001847.
25. ACR–ACOG–AIUM–SRU Practice Parameter for the Performance of Obstetrical Ultrasound. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-ob.pdf. Published 2013. Accessed February 18, 2018.
26. AIUM practice guideline for documentation of an ultrasound examination. J Ultrasound Med. 2014;33(6):1098-1102. doi:10.7863/ultra.33.6.1098.
27. Marin JR, Lewiss RE. Point-of-care ultrasonography by pediatric emergency medicine physicians. Pediatrics. 2015;135(4):e1113-e1122. doi:10.1542/peds.2015-0343.
28. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26(6):567-581. doi:10.1016/j.echo.2013.04.001.
Many hospitalists incorporate point-of-care ultrasound (POCUS) into their daily practice because it adds value to their bedside evaluation of patients. However, standards for training and assessing hospitalists in POCUS have not yet been established. Other acute care specialties, including emergency medicine and critical care medicine, have already incorporated POCUS into their graduate medical education training programs, but most internal medicine residency programs are only beginning to provide POCUS training.1
Several features distinguish POCUS from comprehensive ultrasound examinations. First, POCUS is designed to answer focused questions, whereas comprehensive ultrasound examinations evaluate all organs in an anatomical region; for example, an abdominal POCUS exam may evaluate only for presence or absence of intraperitoneal free fluid, whereas a comprehensive examination of the right upper quadrant will evaluate the liver, gallbladder, and biliary ducts. Second, POCUS examinations are generally performed by the same clinician who generates the relevant clinical question to answer with POCUS and ultimately integrates the findings into the patient’s care.2 By contrast, comprehensive ultrasound examinations involve multiple providers and steps: a clinician generates a relevant clinical question and requests an ultrasound examination that is acquired by a sonographer, interpreted by a radiologist, and reported back to the requesting clinician. Third, POCUS is often used to evaluate multiple body systems. For example, to evaluate a patient with undifferentiated hypotension, a multisystem POCUS examination of the heart, inferior vena cava, lungs, abdomen, and lower extremity veins is typically performed. Finally, POCUS examinations can be performed serially to investigate changes in clinical status or evaluate response to therapy, such as monitoring the heart, lungs, and inferior vena cava during fluid resuscitation.
The purpose of this position statement is to inform a broad audience about how hospitalists are using diagnostic and procedural applications of POCUS. This position statement does not mandate that hospitalists use POCUS. Rather, it is intended to provide guidance on the safe and effective use of POCUS by the hospitalists who use it and the administrators who oversee its use. We discuss POCUS (1) applications, (2) training, (3) assessments, and (4) program management. This position statement was reviewed and approved by the Society of Hospital Medicine (SHM) Executive Committee in March 2018.
APPLICATIONS
As outlined in our earlier position statements,3,4 ultrasound guidance lowers complication rates and increases success rates of invasive bedside procedures. Diagnostic POCUS can guide clinical decision making prior to bedside procedures. For instance, hospitalists may use POCUS to assess the size and character of a pleural effusion to help determine the most appropriate management strategy: observation, medical treatment, thoracentesis, chest tube placement, or surgical therapy. Furthermore, diagnostic POCUS can be used to rapidly assess for immediate postprocedural complications, such as pneumothorax, or if the patient develops new symptoms.
TRAINING
Basic Knowledge
Basic knowledge includes fundamentals of ultrasound physics; safety;4 anatomy; physiology; and device operation, including maintenance and cleaning. Basic knowledge can be taught by multiple methods, including live or recorded lectures, online modules, or directed readings.
Image Acquisition
Training should occur across multiple types of patients (eg, obese, cachectic, postsurgical) and clinical settings (eg, intensive care unit, general medicine wards, emergency department) when available. Training is largely hands-on because the relevant skills involve integration of 3D anatomy with spatial manipulation, hand-eye coordination, and fine motor movements. Virtual reality ultrasound simulators may accelerate mastery, particularly for cardiac image acquisition, and expose learners to standardized sets of pathologic findings. Real-time bedside feedback on image acquisition is ideal because understanding how ultrasound probe manipulation affects the images acquired is essential to learning.
Image Interpretation
Training in image interpretation relies on visual pattern recognition of normal and abnormal findings. Therefore, the normal to abnormal spectrum should be broad, and learners should maintain a log of what abnormalities have been identified. Giving real-time feedback at the bedside is ideal because of the connection between image acquisition and interpretation. Image interpretation can be taught through didactic sessions, image review sessions, or review of teaching files with annotated images.
Clinical Integration
Learners must interpret and integrate image findings with other clinical data considering the image quality, patient characteristics, and changing physiology. Clinical integration should be taught by instructors that share similar clinical knowledge as learners. Although sonographers are well suited to teach image acquisition, they should not be the sole instructors to teach hospitalists how to integrate ultrasound findings in clinical decision making. Likewise, emphasis should be placed on the appropriate use of POCUS within a provider’s skill set. Learners must appreciate the clinical significance of POCUS findings, including recognition of incidental findings that may require further workup. Supplemental training in clinical integration can occur through didactics that include complex patient scenarios.
Pathways
Clinical competency can be achieved with training adherent to five criteria. First, the training environment should be similar to where the trainee will practice. Second, training and feedback should occur in real time. Third, specific applications should be taught rather than broad training in “hospitalist POCUS.” Each application requires unique skills and knowledge, including image acquisition pitfalls and artifacts. Fourth, clinical competence must be achieved and demonstrated; it is not necessarily gained through experience. Fifth, once competency is achieved, continued education and feedback are necessary to ensure it is maintained.
Residency-based POCUS training pathways can best fulfill these criteria. They may eventually become commonplace, but until then alternative pathways must exist for hospitalist providers who are already in practice. There are three important attributes of such pathways. First, administrators’ expectations about learners’ clinical productivity must be realistically, but only temporarily, relaxed; otherwise, competing demands on time will likely overwhelm learners and subvert training. Second, training should begin through a local or national hands-on training program. The SHM POCUS certificate program consolidates training for common diagnostic POCUS applications for hospitalists.6 Other medical societies offer training for their respective clinical specialties.7 Third, once basic POCUS training has begun, longitudinal training should continue ideally with a local hospitalist POCUS expert.
In some settings, a subgroup of hospitalists may not desire, or be able to achieve, competency in the manual skills of POCUS image acquisition. Nevertheless, hospitalists may still find value in understanding POCUS nomenclature, image pattern recognition, and the evidence and pitfalls behind clinical integration of specific POCUS findings. This subset of POCUS skills allows hospitalists to communicate effectively with and understand the clinical decisions made by their colleagues who are competent in POCUS use.
The minimal skills a hospitalist should possess to serve as a POCUS trainer include proficiency of basic knowledge, image acquisition, image interpretation, and clinical integration of the POCUS applications being taught; effectiveness as a hands-on instructor to teach image acquisition skills; and an in-depth understanding of common POCUS pitfalls and limitations.
ASSESSMENTS
Assessment methods for POCUS can include the following: knowledge-based questions, image acquisition using task-specific checklists on human or simulation models, image interpretation using a series of videos or still images with normal and abnormal findings, clinical integration using “next best step” in a multiple choice format with POCUS images, and simulation-based clinical scenarios. Assessment methods should be aligned with local availability of resources and trainers.
Basic Knowledge
Basic knowledge can be assessed via multiple choice questions assessing knowledge of ultrasound physics, image optimization, relevant anatomy, and limitations of POCUS imaging. Basic knowledge lies primarily in the cognitive domain and does not assess manual skills.
Image Acquisition
Image acquisition can be assessed by observation and rating of image quality. Where resources allow, assessment of image acquisition is likely best done through a combination of developing an image portfolio with a minimum number of high quality images, plus direct observation of image acquisition by an expert. Various programs have utilized minimum numbers of images acquired to help define competence with image acquisition skills.6–8 Although minimums may be a necessary step to gain competence, using them as a sole means to determine competence does not account for variable learning curves.9 As with other manual skills in hospital medicine, such as ultrasound-guided bedside procedures, minimum numbers are best used as a starting point for assessments.3,10 In this regard, portfolio development with meticulous attention to the gain, depth, and proper tomographic plane of images can monitor a hospitalist’s progress toward competence by providing objective assessments and feedback. Simulation may also be used as it allows assessment of image acquisition skills and an opportunity to provide real-time feedback, similar to direct observation but without actual patients.
Image Interpretation
Image interpretation is best assessed by an expert observing the learner at bedside; however, when bedside assessment is not possible, image interpretation skills may be assessed using multiple choice or free text interpretation of archived ultrasound images with normal and abnormal findings. This is often incorporated into the portfolio development portion of a training program, as learners can submit their image interpretation along with the video clip. Both normal and abnormal images can be used to assess anatomic recognition and interpretation. Emphasis should be placed on determining when an image is suboptimal for diagnosis (eg, incomplete exam or poor-quality images). Quality assurance programs should incorporate structured feedback sessions.
Clinical Integration
Assessment of clinical integration can be completed through case scenarios that assess knowledge, interpretation of images, and integration of findings into clinical decision making, which is often delivered via a computer-based assessment. Assessments should combine specific POCUS applications to evaluate common clinical problems in hospital medicine, such as undifferentiated hypotension and dyspnea. High-fidelity simulators can be used to blend clinical case scenarios with image acquisition, image interpretation, and clinical integration. When feasible, comprehensive feedback on how providers acquire, interpret, and apply ultrasound at the bedside is likely the best mechanism to assess clinical integration. This process can be done with a hospitalist’s own patients.
General Assessment
A general assessment that includes a summative knowledge and hands-on skills assessment using task-specific checklists can be performed upon completion of training. A high-fidelity simulator with dynamic or virtual anatomy can provide reproducible standardized assessments with variation in the type and difficulty of cases. When available, we encourage the use of dynamic assessments on actual patients that have both normal and abnormal ultrasound findings because simulated patient scenarios have limitations, even with the use of high-fidelity simulators. Programs are recommended to use formative and summative assessments for evaluation. Quantitative scoring systems using checklists are likely the best framework.11,12
CERTIFICATES AND CERTIFICATION
A certificate of completion is proof of a provider’s participation in an educational activity; it does not equate with competency, though it may be a step toward it. Most POCUS training workshops and short courses provide certificates of completion. Certification of competency is an attestation of a hospitalist’s basic competence within a defined scope of practice (Table 2).13 However, without longitudinal supervision and feedback, skills can decay; therefore, we recommend a longitudinal training program that provides mentored feedback and incorporates periodic competency assessments. At present, no national board certification in POCUS is available to grant external certification of competency for hospitalists.
External Certificate
Certificates of completion can be external through a national organization. An external certificate of completion designed for hospitalists includes the POCUS Certificate of Completion offered by SHM in collaboration with CHEST.6 This certificate program provides regional training options and longitudinal portfolio development. Other external certificates are also available to hospitalists.7,14,15
Most hospitalists are boarded by the American Board of Internal Medicine or the American Board of Family Medicine. These boards do not yet include certification of competency in POCUS. Other specialty boards, such as emergency medicine, include competency in POCUS. For emergency medicine, completion of an accredited residency training program and certification by the national board includes POCUS competency.
Internal Certificate
There are a few examples of successful local institutional programs that have provided internal certificates of competency.12,14 Competency assessments require significant resources including investment by both faculty and learners. Ongoing evaluation of competency should be based on quality assurance processes.
Credentialing and Privileging
The American Medical Association (AMA) House of Delegates in 1999 passed a resolution (AMA HR. 802) recommending hospitals follow specialty-specific guidelines for privileging decisions related to POCUS use.17 The resolution included a statement that, “ultrasound imaging is within the scope of practice of appropriately trained physicians.”
Some institutions have begun to rely on a combination of internal and external certificate programs to grant privileges to hospitalists.10 Although specific privileges for POCUS may not be required in some hospitals, some institutions may require certification of training and assessments prior to granting permission to use POCUS.
Hospitalist programs are encouraged to evaluate ongoing POCUS use by their providers after granting initial permission. If privileging is instituted by a hospital, hospitalists must play a significant role in determining the requirements for privileging and ongoing maintenance of skills.
Maintenance of Skills
All medical skills can decay with disuse, including those associated with POCUS.12,18 Thus, POCUS users should continue using POCUS regularly in clinical practice and participate in POCUS continuing medical education activities, ideally with ongoing assessments. Maintenance of skills may be confirmed through routine participation in a quality assurance program.
PROGRAM MANAGEMENT
Use of POCUS in hospital medicine has unique considerations, and hospitalists should be integrally involved in decision making surrounding institutional POCUS program management. Appointing a dedicated POCUS director can help a program succeed.8
Equipment and Image Archiving
Several factors are important to consider when selecting an ultrasound machine: portability, screen size, and ease of use; integration with the electronic medical record and options for image archiving; manufacturer’s service plan, including technical and clinical support; and compliance with local infection control policies. The ability to easily archive and retrieve images is essential for quality assurance, continuing education, institutional quality improvement, documentation, and reimbursement. In certain scenarios, image archiving may not be possible (such as with personal handheld devices or in emergency situations) or necessary (such as with frequent serial examinations during fluid resuscitation). An image archive is ideally linked to reports, orders, and billing software.10,19 If such linkages are not feasible, parallel external storage that complies with regulatory standards (ie, HIPAA compliance) may be suitable.20
Documentation and Billing
Components of documentation include the indication and type of ultrasound examination performed, date and time of the examination, patient identifying information, name of provider(s) acquiring and interpreting the images, specific scanning protocols used, patient position, probe used, and findings. Documentation can occur through a standalone note or as part of another note, such as a progress note. Whenever possible, documentation should be timely to facilitate communication with other providers.
Billing is supported through the AMA Current Procedural Terminology codes for “focused” or “limited” ultrasound examinations (Appendix 9). The following three criteria must be satisfied for billing. First, images must be permanently stored. Specific requirements vary by insurance policy, though current practice suggests a minimum of one image demonstrating relevant anatomy and pathology for the ultrasound examination coded. For ultrasound-guided procedures that require needle insertion, images should be captured at the point of interest, and a procedure note should reflect that the needle was guided and visualized under ultrasound.21 Second, proper documentation must be entered in the medical record. Third, local institutional privileges for POCUS must be considered. Although privileges are not required to bill, some hospitals or payers may require them.
Quality Assurance
Published guidelines on quality assurance in POCUS are available from different specialty organizations, including emergency medicine, pediatric emergency medicine, critical care, anesthesiology, obstetrics, and cardiology.8,22–28 Quality assurance is aimed at ensuring that physicians maintain basic competency in using POCUS to influence bedside decisions.
Quality assurance should be carried out by an individual or committee with expertise in POCUS. Multidisciplinary QA programs in which hospital medicine providers are working collaboratively with other POCUS providers have been demonstrated to be highly effective.10 Oversight includes ensuring that providers using POCUS are appropriately trained,10,22,28 using the equipment correctly,8,26,28 and documenting properly. Some programs have implemented mechanisms to review and provide feedback on image acquisition, interpretation, and clinical integration.8,10 Other programs have compared POCUS findings with referral studies, such as comprehensive ultrasound examinations.
CONCLUSIONS
Practicing hospitalists must continue to collaborate with their institutions to build POCUS capabilities. In particular, they must work with their local privileging body to determine what credentials are required. The distinction between certificates of completion and certificates of competency, including whether those certificates are internal or external, is important in the credentialing process.
External certificates of competency are currently unavailable for most practicing hospitalists because ABIM certification does not include POCUS-related competencies. As internal medicine residency training programs begin to adopt POCUS training and certification into their educational curricula, we foresee a need to update the ABIM Policies and Procedures for Certification. Until then, we recommend that certificates of competency be defined and granted internally by local hospitalist groups.
Given the many advantages of POCUS over traditional tools, we anticipate its increasing implementation among hospitalists in the future. As with all medical technology, its role in clinical care should be continuously reexamined and redefined through health services research. Such information will be useful in developing practice guidelines, educational curricula, and training standards.
Acknowledgments
The authors would like to thank all members that participated in the discussion and finalization of this position statement during the Point-of-care Ultrasound Faculty Retreat at the 2018 Society of Hospital Medicine Annual Conference: Saaid Abdel-Ghani, Brandon Boesch, Joel Cho, Ria Dancel, Renee Dversdal, Ricardo Franco-Sadud, Benjamin Galen, Trevor P. Jensen, Mohit Jindal, Gordon Johnson, Linda M. Kurian, Gigi Liu, Charles M. LoPresti, Brian P. Lucas, Venkat Kalidindi, Benji Matthews, Anna Maw, Gregory Mints, Kreegan Reierson, Gerard Salame, Richard Schildhouse, Daniel Schnobrich, Nilam Soni, Kirk Spencer, Hiromizu Takahashi, David M. Tierney, Tanping Wong, and Toru Yamada.
Many hospitalists incorporate point-of-care ultrasound (POCUS) into their daily practice because it adds value to their bedside evaluation of patients. However, standards for training and assessing hospitalists in POCUS have not yet been established. Other acute care specialties, including emergency medicine and critical care medicine, have already incorporated POCUS into their graduate medical education training programs, but most internal medicine residency programs are only beginning to provide POCUS training.1
Several features distinguish POCUS from comprehensive ultrasound examinations. First, POCUS is designed to answer focused questions, whereas comprehensive ultrasound examinations evaluate all organs in an anatomical region; for example, an abdominal POCUS exam may evaluate only for presence or absence of intraperitoneal free fluid, whereas a comprehensive examination of the right upper quadrant will evaluate the liver, gallbladder, and biliary ducts. Second, POCUS examinations are generally performed by the same clinician who generates the relevant clinical question to answer with POCUS and ultimately integrates the findings into the patient’s care.2 By contrast, comprehensive ultrasound examinations involve multiple providers and steps: a clinician generates a relevant clinical question and requests an ultrasound examination that is acquired by a sonographer, interpreted by a radiologist, and reported back to the requesting clinician. Third, POCUS is often used to evaluate multiple body systems. For example, to evaluate a patient with undifferentiated hypotension, a multisystem POCUS examination of the heart, inferior vena cava, lungs, abdomen, and lower extremity veins is typically performed. Finally, POCUS examinations can be performed serially to investigate changes in clinical status or evaluate response to therapy, such as monitoring the heart, lungs, and inferior vena cava during fluid resuscitation.
The purpose of this position statement is to inform a broad audience about how hospitalists are using diagnostic and procedural applications of POCUS. This position statement does not mandate that hospitalists use POCUS. Rather, it is intended to provide guidance on the safe and effective use of POCUS by the hospitalists who use it and the administrators who oversee its use. We discuss POCUS (1) applications, (2) training, (3) assessments, and (4) program management. This position statement was reviewed and approved by the Society of Hospital Medicine (SHM) Executive Committee in March 2018.
APPLICATIONS
As outlined in our earlier position statements,3,4 ultrasound guidance lowers complication rates and increases success rates of invasive bedside procedures. Diagnostic POCUS can guide clinical decision making prior to bedside procedures. For instance, hospitalists may use POCUS to assess the size and character of a pleural effusion to help determine the most appropriate management strategy: observation, medical treatment, thoracentesis, chest tube placement, or surgical therapy. Furthermore, diagnostic POCUS can be used to rapidly assess for immediate postprocedural complications, such as pneumothorax, or if the patient develops new symptoms.
TRAINING
Basic Knowledge
Basic knowledge includes fundamentals of ultrasound physics; safety;4 anatomy; physiology; and device operation, including maintenance and cleaning. Basic knowledge can be taught by multiple methods, including live or recorded lectures, online modules, or directed readings.
Image Acquisition
Training should occur across multiple types of patients (eg, obese, cachectic, postsurgical) and clinical settings (eg, intensive care unit, general medicine wards, emergency department) when available. Training is largely hands-on because the relevant skills involve integration of 3D anatomy with spatial manipulation, hand-eye coordination, and fine motor movements. Virtual reality ultrasound simulators may accelerate mastery, particularly for cardiac image acquisition, and expose learners to standardized sets of pathologic findings. Real-time bedside feedback on image acquisition is ideal because understanding how ultrasound probe manipulation affects the images acquired is essential to learning.
Image Interpretation
Training in image interpretation relies on visual pattern recognition of normal and abnormal findings. Therefore, the normal to abnormal spectrum should be broad, and learners should maintain a log of what abnormalities have been identified. Giving real-time feedback at the bedside is ideal because of the connection between image acquisition and interpretation. Image interpretation can be taught through didactic sessions, image review sessions, or review of teaching files with annotated images.
Clinical Integration
Learners must interpret and integrate image findings with other clinical data considering the image quality, patient characteristics, and changing physiology. Clinical integration should be taught by instructors that share similar clinical knowledge as learners. Although sonographers are well suited to teach image acquisition, they should not be the sole instructors to teach hospitalists how to integrate ultrasound findings in clinical decision making. Likewise, emphasis should be placed on the appropriate use of POCUS within a provider’s skill set. Learners must appreciate the clinical significance of POCUS findings, including recognition of incidental findings that may require further workup. Supplemental training in clinical integration can occur through didactics that include complex patient scenarios.
Pathways
Clinical competency can be achieved with training adherent to five criteria. First, the training environment should be similar to where the trainee will practice. Second, training and feedback should occur in real time. Third, specific applications should be taught rather than broad training in “hospitalist POCUS.” Each application requires unique skills and knowledge, including image acquisition pitfalls and artifacts. Fourth, clinical competence must be achieved and demonstrated; it is not necessarily gained through experience. Fifth, once competency is achieved, continued education and feedback are necessary to ensure it is maintained.
Residency-based POCUS training pathways can best fulfill these criteria. They may eventually become commonplace, but until then alternative pathways must exist for hospitalist providers who are already in practice. There are three important attributes of such pathways. First, administrators’ expectations about learners’ clinical productivity must be realistically, but only temporarily, relaxed; otherwise, competing demands on time will likely overwhelm learners and subvert training. Second, training should begin through a local or national hands-on training program. The SHM POCUS certificate program consolidates training for common diagnostic POCUS applications for hospitalists.6 Other medical societies offer training for their respective clinical specialties.7 Third, once basic POCUS training has begun, longitudinal training should continue ideally with a local hospitalist POCUS expert.
In some settings, a subgroup of hospitalists may not desire, or be able to achieve, competency in the manual skills of POCUS image acquisition. Nevertheless, hospitalists may still find value in understanding POCUS nomenclature, image pattern recognition, and the evidence and pitfalls behind clinical integration of specific POCUS findings. This subset of POCUS skills allows hospitalists to communicate effectively with and understand the clinical decisions made by their colleagues who are competent in POCUS use.
The minimal skills a hospitalist should possess to serve as a POCUS trainer include proficiency of basic knowledge, image acquisition, image interpretation, and clinical integration of the POCUS applications being taught; effectiveness as a hands-on instructor to teach image acquisition skills; and an in-depth understanding of common POCUS pitfalls and limitations.
ASSESSMENTS
Assessment methods for POCUS can include the following: knowledge-based questions, image acquisition using task-specific checklists on human or simulation models, image interpretation using a series of videos or still images with normal and abnormal findings, clinical integration using “next best step” in a multiple choice format with POCUS images, and simulation-based clinical scenarios. Assessment methods should be aligned with local availability of resources and trainers.
Basic Knowledge
Basic knowledge can be assessed via multiple choice questions assessing knowledge of ultrasound physics, image optimization, relevant anatomy, and limitations of POCUS imaging. Basic knowledge lies primarily in the cognitive domain and does not assess manual skills.
Image Acquisition
Image acquisition can be assessed by observation and rating of image quality. Where resources allow, assessment of image acquisition is likely best done through a combination of developing an image portfolio with a minimum number of high quality images, plus direct observation of image acquisition by an expert. Various programs have utilized minimum numbers of images acquired to help define competence with image acquisition skills.6–8 Although minimums may be a necessary step to gain competence, using them as a sole means to determine competence does not account for variable learning curves.9 As with other manual skills in hospital medicine, such as ultrasound-guided bedside procedures, minimum numbers are best used as a starting point for assessments.3,10 In this regard, portfolio development with meticulous attention to the gain, depth, and proper tomographic plane of images can monitor a hospitalist’s progress toward competence by providing objective assessments and feedback. Simulation may also be used as it allows assessment of image acquisition skills and an opportunity to provide real-time feedback, similar to direct observation but without actual patients.
Image Interpretation
Image interpretation is best assessed by an expert observing the learner at bedside; however, when bedside assessment is not possible, image interpretation skills may be assessed using multiple choice or free text interpretation of archived ultrasound images with normal and abnormal findings. This is often incorporated into the portfolio development portion of a training program, as learners can submit their image interpretation along with the video clip. Both normal and abnormal images can be used to assess anatomic recognition and interpretation. Emphasis should be placed on determining when an image is suboptimal for diagnosis (eg, incomplete exam or poor-quality images). Quality assurance programs should incorporate structured feedback sessions.
Clinical Integration
Assessment of clinical integration can be completed through case scenarios that assess knowledge, interpretation of images, and integration of findings into clinical decision making, which is often delivered via a computer-based assessment. Assessments should combine specific POCUS applications to evaluate common clinical problems in hospital medicine, such as undifferentiated hypotension and dyspnea. High-fidelity simulators can be used to blend clinical case scenarios with image acquisition, image interpretation, and clinical integration. When feasible, comprehensive feedback on how providers acquire, interpret, and apply ultrasound at the bedside is likely the best mechanism to assess clinical integration. This process can be done with a hospitalist’s own patients.
General Assessment
A general assessment that includes a summative knowledge and hands-on skills assessment using task-specific checklists can be performed upon completion of training. A high-fidelity simulator with dynamic or virtual anatomy can provide reproducible standardized assessments with variation in the type and difficulty of cases. When available, we encourage the use of dynamic assessments on actual patients that have both normal and abnormal ultrasound findings because simulated patient scenarios have limitations, even with the use of high-fidelity simulators. Programs are recommended to use formative and summative assessments for evaluation. Quantitative scoring systems using checklists are likely the best framework.11,12
CERTIFICATES AND CERTIFICATION
A certificate of completion is proof of a provider’s participation in an educational activity; it does not equate with competency, though it may be a step toward it. Most POCUS training workshops and short courses provide certificates of completion. Certification of competency is an attestation of a hospitalist’s basic competence within a defined scope of practice (Table 2).13 However, without longitudinal supervision and feedback, skills can decay; therefore, we recommend a longitudinal training program that provides mentored feedback and incorporates periodic competency assessments. At present, no national board certification in POCUS is available to grant external certification of competency for hospitalists.
External Certificate
Certificates of completion can be external through a national organization. An external certificate of completion designed for hospitalists includes the POCUS Certificate of Completion offered by SHM in collaboration with CHEST.6 This certificate program provides regional training options and longitudinal portfolio development. Other external certificates are also available to hospitalists.7,14,15
Most hospitalists are boarded by the American Board of Internal Medicine or the American Board of Family Medicine. These boards do not yet include certification of competency in POCUS. Other specialty boards, such as emergency medicine, include competency in POCUS. For emergency medicine, completion of an accredited residency training program and certification by the national board includes POCUS competency.
Internal Certificate
There are a few examples of successful local institutional programs that have provided internal certificates of competency.12,14 Competency assessments require significant resources including investment by both faculty and learners. Ongoing evaluation of competency should be based on quality assurance processes.
Credentialing and Privileging
The American Medical Association (AMA) House of Delegates in 1999 passed a resolution (AMA HR. 802) recommending hospitals follow specialty-specific guidelines for privileging decisions related to POCUS use.17 The resolution included a statement that, “ultrasound imaging is within the scope of practice of appropriately trained physicians.”
Some institutions have begun to rely on a combination of internal and external certificate programs to grant privileges to hospitalists.10 Although specific privileges for POCUS may not be required in some hospitals, some institutions may require certification of training and assessments prior to granting permission to use POCUS.
Hospitalist programs are encouraged to evaluate ongoing POCUS use by their providers after granting initial permission. If privileging is instituted by a hospital, hospitalists must play a significant role in determining the requirements for privileging and ongoing maintenance of skills.
Maintenance of Skills
All medical skills can decay with disuse, including those associated with POCUS.12,18 Thus, POCUS users should continue using POCUS regularly in clinical practice and participate in POCUS continuing medical education activities, ideally with ongoing assessments. Maintenance of skills may be confirmed through routine participation in a quality assurance program.
PROGRAM MANAGEMENT
Use of POCUS in hospital medicine has unique considerations, and hospitalists should be integrally involved in decision making surrounding institutional POCUS program management. Appointing a dedicated POCUS director can help a program succeed.8
Equipment and Image Archiving
Several factors are important to consider when selecting an ultrasound machine: portability, screen size, and ease of use; integration with the electronic medical record and options for image archiving; manufacturer’s service plan, including technical and clinical support; and compliance with local infection control policies. The ability to easily archive and retrieve images is essential for quality assurance, continuing education, institutional quality improvement, documentation, and reimbursement. In certain scenarios, image archiving may not be possible (such as with personal handheld devices or in emergency situations) or necessary (such as with frequent serial examinations during fluid resuscitation). An image archive is ideally linked to reports, orders, and billing software.10,19 If such linkages are not feasible, parallel external storage that complies with regulatory standards (ie, HIPAA compliance) may be suitable.20
Documentation and Billing
Components of documentation include the indication and type of ultrasound examination performed, date and time of the examination, patient identifying information, name of provider(s) acquiring and interpreting the images, specific scanning protocols used, patient position, probe used, and findings. Documentation can occur through a standalone note or as part of another note, such as a progress note. Whenever possible, documentation should be timely to facilitate communication with other providers.
Billing is supported through the AMA Current Procedural Terminology codes for “focused” or “limited” ultrasound examinations (Appendix 9). The following three criteria must be satisfied for billing. First, images must be permanently stored. Specific requirements vary by insurance policy, though current practice suggests a minimum of one image demonstrating relevant anatomy and pathology for the ultrasound examination coded. For ultrasound-guided procedures that require needle insertion, images should be captured at the point of interest, and a procedure note should reflect that the needle was guided and visualized under ultrasound.21 Second, proper documentation must be entered in the medical record. Third, local institutional privileges for POCUS must be considered. Although privileges are not required to bill, some hospitals or payers may require them.
Quality Assurance
Published guidelines on quality assurance in POCUS are available from different specialty organizations, including emergency medicine, pediatric emergency medicine, critical care, anesthesiology, obstetrics, and cardiology.8,22–28 Quality assurance is aimed at ensuring that physicians maintain basic competency in using POCUS to influence bedside decisions.
Quality assurance should be carried out by an individual or committee with expertise in POCUS. Multidisciplinary QA programs in which hospital medicine providers are working collaboratively with other POCUS providers have been demonstrated to be highly effective.10 Oversight includes ensuring that providers using POCUS are appropriately trained,10,22,28 using the equipment correctly,8,26,28 and documenting properly. Some programs have implemented mechanisms to review and provide feedback on image acquisition, interpretation, and clinical integration.8,10 Other programs have compared POCUS findings with referral studies, such as comprehensive ultrasound examinations.
CONCLUSIONS
Practicing hospitalists must continue to collaborate with their institutions to build POCUS capabilities. In particular, they must work with their local privileging body to determine what credentials are required. The distinction between certificates of completion and certificates of competency, including whether those certificates are internal or external, is important in the credentialing process.
External certificates of competency are currently unavailable for most practicing hospitalists because ABIM certification does not include POCUS-related competencies. As internal medicine residency training programs begin to adopt POCUS training and certification into their educational curricula, we foresee a need to update the ABIM Policies and Procedures for Certification. Until then, we recommend that certificates of competency be defined and granted internally by local hospitalist groups.
Given the many advantages of POCUS over traditional tools, we anticipate its increasing implementation among hospitalists in the future. As with all medical technology, its role in clinical care should be continuously reexamined and redefined through health services research. Such information will be useful in developing practice guidelines, educational curricula, and training standards.
Acknowledgments
The authors would like to thank all members that participated in the discussion and finalization of this position statement during the Point-of-care Ultrasound Faculty Retreat at the 2018 Society of Hospital Medicine Annual Conference: Saaid Abdel-Ghani, Brandon Boesch, Joel Cho, Ria Dancel, Renee Dversdal, Ricardo Franco-Sadud, Benjamin Galen, Trevor P. Jensen, Mohit Jindal, Gordon Johnson, Linda M. Kurian, Gigi Liu, Charles M. LoPresti, Brian P. Lucas, Venkat Kalidindi, Benji Matthews, Anna Maw, Gregory Mints, Kreegan Reierson, Gerard Salame, Richard Schildhouse, Daniel Schnobrich, Nilam Soni, Kirk Spencer, Hiromizu Takahashi, David M. Tierney, Tanping Wong, and Toru Yamada.
1. Schnobrich DJ, Mathews BK, Trappey BE, Muthyala BK, Olson APJ. Entrusting internal medicine residents to use point of care ultrasound: Towards improved assessment and supervision. Med Teach. 2018:1-6. doi:10.1080/0142159X.2018.1457210.
2. Soni NJ, Lucas BP. Diagnostic point-of-care ultrasound for hospitalists. J Hosp Med. 2015;10(2):120-124. doi:10.1002/jhm.2285.
3. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):117-125. doi:10.12788/jhm.2917.
4. Dancel R, Schnobrich D, Puri N, et al. Recommendations on the use of ultrasound guidance for adult thoracentesis: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):126-135. doi:10.12788/jhm.2940.
5. National Council on Radiation Protection and Measurements, The Council. Implementation of the Principle of as Low as Reasonably Achievable (ALARA) for Medical and Dental Personnel.; 1990.
6. Society of Hospital Medicine. Point of Care Ultrasound course: https://www.hospitalmedicine.org/clinical-topics/ultrasonography-cert/. Accessed February 6, 2018.
7. Critical Care Ultrasonography Certificate of Completion Program. CHEST. American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography. Accessed February 6, 2018.
8. American College of Emergency Physicians Policy Statement: Emergency Ultrasound Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/ACEP-Ultrasound-Guidelines/. Accessed February 6, 2018.
9. Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med. 2015;22(5):574-582. doi:10.1111/acem.12653.
10. Mathews BK, Zwank M. Hospital medicine point of care ultrasound credentialing: an example protocol. J Hosp Med. 2017;12(9):767-772. doi:10.12788/jhm.2809.
11. Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009;4(7):397-403. doi:10.1002/jhm.468.
12. Mathews BK, Reierson K, Vuong K, et al. The design and evaluation of the Comprehensive Hospitalist Assessment and Mentorship with Portfolios (CHAMP) ultrasound program. J Hosp Med. 2018;13(8):544-550. doi:10.12788/jhm.2938.
13. Soni NJ, Tierney DM, Jensen TP, Lucas BP. Certification of point-of-care ultrasound competency. J Hosp Med. 2017;12(9):775-776. doi:10.12788/jhm.2812.
14. Ultrasound Certification for Physicians. Alliance for Physician Certification and Advancement. APCA. https://apca.org/. Accessed February 6, 2018.
15. National Board of Echocardiography, Inc. https://www.echoboards.org/EchoBoards/News/2019_Adult_Critical_Care_Echocardiography_Exam.aspx. Accessed June 18, 2018.
16. Tierney DM. Internal Medicine Bedside Ultrasound Program (IMBUS). Abbott Northwestern. http://imbus.anwresidency.com/index.html. Accessed February 6, 2018.
17. American Medical Association House of Delegates Resolution H-230.960: Privileging for Ultrasound Imaging. Resolution 802. Policy Finder Website. http://search0.ama-assn.org/search/pfonline. Published 1999. Accessed February 18, 2018.
18. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi:10.4300/JGME-14-00284.1.
19. Flannigan MJ, Adhikari S. Point-of-care ultrasound work flow innovation: impact on documentation and billing. J Ultrasound Med. 2017;36(12):2467-2474. doi:10.1002/jum.14284.
20. Emergency Ultrasound: Workflow White Paper. https://www.acep.org/uploadedFiles/ACEP/memberCenter/SectionsofMembership/ultra/Workflow%20White%20Paper.pdf. Published 2013. Accessed February 18, 2018.
21. Ultrasound Coding and Reimbursement Document 2009. Emergency Ultrasound Section. American College of Emergency Physicians. http://emergencyultrasoundteaching.com/assets/2009_coding_update.pdf. Published 2009. Accessed February 18, 2018.
22. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest. 2009;135(4):1050-1060. doi:10.1378/chest.08-2305.
23. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part I: general ultrasonography. Crit Care Med. 2015;43(11):2479-2502. doi:10.1097/ccm.0000000000001216.
24. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part ii: cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. doi:10.1097/ccm.0000000000001847.
25. ACR–ACOG–AIUM–SRU Practice Parameter for the Performance of Obstetrical Ultrasound. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-ob.pdf. Published 2013. Accessed February 18, 2018.
26. AIUM practice guideline for documentation of an ultrasound examination. J Ultrasound Med. 2014;33(6):1098-1102. doi:10.7863/ultra.33.6.1098.
27. Marin JR, Lewiss RE. Point-of-care ultrasonography by pediatric emergency medicine physicians. Pediatrics. 2015;135(4):e1113-e1122. doi:10.1542/peds.2015-0343.
28. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26(6):567-581. doi:10.1016/j.echo.2013.04.001.
1. Schnobrich DJ, Mathews BK, Trappey BE, Muthyala BK, Olson APJ. Entrusting internal medicine residents to use point of care ultrasound: Towards improved assessment and supervision. Med Teach. 2018:1-6. doi:10.1080/0142159X.2018.1457210.
2. Soni NJ, Lucas BP. Diagnostic point-of-care ultrasound for hospitalists. J Hosp Med. 2015;10(2):120-124. doi:10.1002/jhm.2285.
3. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):117-125. doi:10.12788/jhm.2917.
4. Dancel R, Schnobrich D, Puri N, et al. Recommendations on the use of ultrasound guidance for adult thoracentesis: a position statement of the society of hospital medicine. J Hosp Med. 2018;13(2):126-135. doi:10.12788/jhm.2940.
5. National Council on Radiation Protection and Measurements, The Council. Implementation of the Principle of as Low as Reasonably Achievable (ALARA) for Medical and Dental Personnel.; 1990.
6. Society of Hospital Medicine. Point of Care Ultrasound course: https://www.hospitalmedicine.org/clinical-topics/ultrasonography-cert/. Accessed February 6, 2018.
7. Critical Care Ultrasonography Certificate of Completion Program. CHEST. American College of Chest Physicians. http://www.chestnet.org/Education/Advanced-Clinical-Training/Certificate-of-Completion-Program/Critical-Care-Ultrasonography. Accessed February 6, 2018.
8. American College of Emergency Physicians Policy Statement: Emergency Ultrasound Guidelines. 2016. https://www.acep.org/Clinical---Practice-Management/ACEP-Ultrasound-Guidelines/. Accessed February 6, 2018.
9. Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med. 2015;22(5):574-582. doi:10.1111/acem.12653.
10. Mathews BK, Zwank M. Hospital medicine point of care ultrasound credentialing: an example protocol. J Hosp Med. 2017;12(9):767-772. doi:10.12788/jhm.2809.
11. Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based mastery learning to improve the quality of central venous catheter placement in a medical intensive care unit. J Hosp Med. 2009;4(7):397-403. doi:10.1002/jhm.468.
12. Mathews BK, Reierson K, Vuong K, et al. The design and evaluation of the Comprehensive Hospitalist Assessment and Mentorship with Portfolios (CHAMP) ultrasound program. J Hosp Med. 2018;13(8):544-550. doi:10.12788/jhm.2938.
13. Soni NJ, Tierney DM, Jensen TP, Lucas BP. Certification of point-of-care ultrasound competency. J Hosp Med. 2017;12(9):775-776. doi:10.12788/jhm.2812.
14. Ultrasound Certification for Physicians. Alliance for Physician Certification and Advancement. APCA. https://apca.org/. Accessed February 6, 2018.
15. National Board of Echocardiography, Inc. https://www.echoboards.org/EchoBoards/News/2019_Adult_Critical_Care_Echocardiography_Exam.aspx. Accessed June 18, 2018.
16. Tierney DM. Internal Medicine Bedside Ultrasound Program (IMBUS). Abbott Northwestern. http://imbus.anwresidency.com/index.html. Accessed February 6, 2018.
17. American Medical Association House of Delegates Resolution H-230.960: Privileging for Ultrasound Imaging. Resolution 802. Policy Finder Website. http://search0.ama-assn.org/search/pfonline. Published 1999. Accessed February 18, 2018.
18. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi:10.4300/JGME-14-00284.1.
19. Flannigan MJ, Adhikari S. Point-of-care ultrasound work flow innovation: impact on documentation and billing. J Ultrasound Med. 2017;36(12):2467-2474. doi:10.1002/jum.14284.
20. Emergency Ultrasound: Workflow White Paper. https://www.acep.org/uploadedFiles/ACEP/memberCenter/SectionsofMembership/ultra/Workflow%20White%20Paper.pdf. Published 2013. Accessed February 18, 2018.
21. Ultrasound Coding and Reimbursement Document 2009. Emergency Ultrasound Section. American College of Emergency Physicians. http://emergencyultrasoundteaching.com/assets/2009_coding_update.pdf. Published 2009. Accessed February 18, 2018.
22. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest. 2009;135(4):1050-1060. doi:10.1378/chest.08-2305.
23. Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part I: general ultrasonography. Crit Care Med. 2015;43(11):2479-2502. doi:10.1097/ccm.0000000000001216.
24. Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part ii: cardiac ultrasonography. Crit Care Med. 2016;44(6):1206-1227. doi:10.1097/ccm.0000000000001847.
25. ACR–ACOG–AIUM–SRU Practice Parameter for the Performance of Obstetrical Ultrasound. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/us-ob.pdf. Published 2013. Accessed February 18, 2018.
26. AIUM practice guideline for documentation of an ultrasound examination. J Ultrasound Med. 2014;33(6):1098-1102. doi:10.7863/ultra.33.6.1098.
27. Marin JR, Lewiss RE. Point-of-care ultrasonography by pediatric emergency medicine physicians. Pediatrics. 2015;135(4):e1113-e1122. doi:10.1542/peds.2015-0343.
28. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26(6):567-581. doi:10.1016/j.echo.2013.04.001.
© 2019 Society of Hospital Medicine
Recommendations on the Use of Ultrasound Guidance for Adult Abdominal Paracentesis: A Position Statement of the Society of Hospital Medicine
Abdominal paracentesis is a common and increasingly performed procedure in the United States. According to Medicare Physician Supplier Procedure Summary Master Files, an estimated 150,000 paracenteses were performed on Medicare fee-for-service beneficiaries in 2008 alone; such a number represents more than a two-fold increase from the same service population in 1993.1 This increasing trend was again noted by the Nationwide Inpatient Sample data, which identified a 10% increase in hospitalized patients with a diagnosis of cirrhosis receiving paracentesis from 2004 (50%) to 2012 (61%; P < .0001).2
Although these data demonstrate that paracentesis is being performed frequently, paracentesis may be underutilized in hospitalized cirrhotics with ascites. In addition, in-hospital mortality of cirrhotics with ascites is higher among those who do not undergo paracentesis than among those who do (9% vs 6%; P = .03).3,4
While complications associated with paracentesis are rare, serious complications, including death, have been documented.5-10 The most common serious complication of paracentesis is bleeding, although puncture of the bowel and other abdominal organs has also been observed. Over the past few decades, ultrasound has been increasingly used with paracentesis due to the ability of ultrasound to improve detection of ascites11,12 and to avoid blood vessels10,13-15 and bowels.16
Three-quarters of all paracenteses are currently performed by interventional radiologists.1 However, paracenteses are often required off-hours,17 when interventional radiologists are less readily available. Weekend admissions have less frequent performance of early paracentesis than weekday admissions, and delaying paracentesis may increase mortality.3,18 High proficiency in ultrasound-guided paracentesis is achievable by nonradiologists19-28 with equal or better patient outcomes after appropriate training.29
The purpose of this guideline is to review the literature and present evidence-based recommendations on the performance of ultrasound-guided paracentesis at the bedside by practicing hospitalists.
METHODS
Detailed methods are described in Appendix 1. The Society of Hospital Medicine (SHM) Point-of-care Ultrasound (POCUS) Task Force was assembled to carry out this guideline development project under the direction of the SHM Board of Directors, Director of Education, and Education Committee. All expert panel members were physicians or advanced-practice providers with expertise in POCUS. Expert panel members were divided into working group members, external peer reviewers, and a methodologist, and all Task Force members were required to disclose any potential conflicts of interests (Appendix 2). The literature search was conducted in two independent phases. The first phase included literature searches conducted by the five working group members themselves. Key clinical questions and draft recommendations were then prepared, and a systematic literature search was conducted by a medical librarian based on the findings of the initial literature search and draft recommendations. The Medline, Embase, CINAHL, and Cochrane medical databases were initially searched from 1975 to October 2015. Google Scholar was also searched without limiters. An updated search was conducted from November 2015 to November 2017, search strings for which are included in Appendix 3. All article abstracts were first screened for relevance by at least two members of the working group. Full-text versions of screened articles were reviewed and articles on ultrasound guidance for paracentesis were selected. The following article types were excluded: non-English language, nonhuman, age <18 years, meeting abstracts, meeting posters, letters, and editorials. All relevant systematic reviews, meta-analyses, randomized controlled trials, and observational studies of ultrasound-guided paracentesis were screened and selected. Final article selection was based on working group consensus. The selected literature was incorporated into the draft recommendations.
We used the RAND Appropriateness Method that required panel judgment and consensus to establish recommendations.30 The voting members of the SHM POCUS Task Force reviewed and voted on the draft recommendations considering five transforming factors: (1) problem priority and importance; (2) level of quality of evidence; (3) benefit/harm balance; (4) benefit/burden balance; and (5) certainty/concerns about preferences/equity acceptability/feasibility. Panel members participated in two rounds of electronic voting using an internet-based electronic data collection tool (Redcap™) during February 2018 and April 2018 (Appendix 4) and voting on appropriateness was conducted using a 9-point Likert scale. The three zones based on the 9-point Likert scale were inappropriate (1-3 points), uncertain (4-6 points), and appropriate (7-9 points), and the degree of consensus was assessed using the RAND algorithm (Appendix 1, Figure 1, and Table 1). Establishing a recommendation required at least 70% agreement that a recommendation was “appropriate.” A strong recommendation required 80% of the votes within one integer of the median, following RAND rules, and disagreement was defined as >30% of panelists voting outside of the zone of the median.
Recommendations were classified as strong or weak/conditional based on preset rules defining the panel’s level of consensus, which determined the wording for each recommendation (Tables 1 and 2). The revised consensus-based recommendations underwent internal and external review by POCUS experts from different subspecialties, and a final review of the guideline document was performed by members of the SHM POCUS Task Force, SHM Education Committee, and SHM Board of Directors. The SHM Board of Directors endorsed the document prior to submission to the Journal of Hospital Medicine.
RESULTS
Literature search
A total of 794 references were pooled and screened from literature searches conducted by a certified medical librarian in October 2015 (604 citations) and updated in November 2017 (118 citations), and working group members’ personal bibliographies and searches (72 citations; Appendix 3, Figure 2). Final selection included 91 articles that were abstracted into a data table and incorporated into the draft recommendations.
RECOMMENDATIONS
Four domains (terminology, clinical outcomes, technique, and training) with 13 draft recommendations were generated based on the literature review by the paracentesis working group. After two rounds of panel voting, one recommendation did not achieve consensus based on the RAND rules, and 12 statements received final approval. The degree of consensus based on the median score and dispersion of voting around the median are shown in Appendix 5. All 12 statements achieved consensus as strong recommendations. The strength of each recommendation and degree of consensus are summarized in Table 3.
Terminology
Abdominal paracentesis is a procedure in which fluid is aspirated from the intraperitoneal space by percutaneous insertion of a needle with or without a catheter through the abdominal wall. Throughout this document, the term “paracentesis” refers to “abdominal paracentesis.”
In this document, ultrasound-guided paracentesis refers to the use of static ultrasound guidance to mark a needle insertion site immediately prior to performing the procedure. Real-time (dynamic) ultrasound guidance refers to tracking of the needle tip with ultrasound as it traverses the abdominal wall to enter the peritoneal cavity. Landmark-based paracentesis refers to paracentesis based on physical examination alone.
RECOMMENDATIONS
Clinical outcomes
1. We recommend that ultrasound guidance should be used for paracentesis to reduce the risk of serious complications, the most common being bleeding.
Rationale. The occurrence of both minor and serious life-threatening complications from paracentesis has been well described.5-10,31,32 A recent retrospective study that evaluated 515 landmark-guided paracenteses noted that the most common minor complication was persistent ascites leakage (5%) and that the most common serious complication was postprocedural bleeding (1%).8 Studies have shown that abdominal wall hematoma and hemoperitoneum are common hemorrhagic complications of paracentesis, although inferior epigastric artery pseudoaneurysm has also been described.9,33,34
Current literature suggests that ultrasound-guided paracentesis is a safe procedure, even with reduced platelet counts or elevated international normalized ratio.35-42 Most comparative studies have shown that ultrasound guidance reduces the risk of bleeding complications compared with the use of landmarks alone,7,31,32,43-45 although a few studies did not find a significant difference between techniques.20,36,46 One large retrospective observational study that analyzed the administrative data of 69,859 paracenteses from more than 600 hospitals demonstrated that ultrasound guidance reduced the odds of bleeding complications by 68% (OR, 0.32; 95% CI, 0.25–0.41). Bleeding complication rates with and without the use of ultrasound guidance were 0.27% (CI 0.26-0.29) versus 1.25% (CI 1.21-1.29; P < .0001), respectively. More importantly, in this study, paracentesis complicated by bleeding was associated with a higher in-hospital mortality rate
2. We recommend that ultrasound guidance should be used to avoid attempting paracentesis in patients with an insufficient volume of intraperitoneal free fluid to drain.
Rationale. Abdominal physical examination is not a reliable method for determining the presence or volume of intraperitoneal free fluid, as no specific physical examination finding has consistently shown both high sensitivity and specificity for detecting intraperitoneal free fluid.11,12,20,31,47-51 Patient factors limiting the diagnostic accuracy of physical examination include body habitus, abdominal wall edema, and gaseous bowel distention.
In comparative studies, ultrasound has been found to be significantly more sensitive and specific than physical examination in detecting peritoneal free fluid.11,12 Ultrasound can detect as little as 100 mL of peritoneal free fluid,52,53 and larger volumes of fluid have higher diagnostic accuracy.53-55 In one randomized trial of 100 patients suspected of having ascites, patients were randomized to landmark-based and ultrasound-guided paracentesis groups. Of the 56 patients in the ultrasound-guided group, 14 patients suspected of having ascites on physical examination were found to have no or an insufficient volume of ascites to attempt paracentesis.20 Another study with 41 ultrasound examinations on cancer patients suspected of having intraperitoneal free fluid by history and physical examination demonstrated that only 19 (46%) were considered to have a sufficient volume of ascites by ultrasound to attempt paracentesis.38
3. We recommend that ultrasound guidance should be used for paracentesis to improve the success rates of the overall procedure.
Rationale. In addition to avoiding drainage attempts in patients with an insufficient volume of intraperitoneal free fluid, ultrasound can increase the success rate of attempted procedures by localizing the largest fluid collection and guiding selection of an optimal needle insertion site. The success rates of landmark-based paracentesis in patients suspected of having intraperitoneal free fluid by physical examination are not well described in the literature, but multiple studies report success rates of 95%-100% for paracentesis when using ultrasound guidance to select a needle insertion site.20,38,56,57 In one randomized trial comparing ultrasound-guided versus landmark-based paracentesis, ultrasound-guided paracentesis revealed a significantly higher success rate (95% of procedures performed) compared with landmark-based parancentesis (61% of procedures performed). Moreover, 87% of the initial failures in the landmark-based group underwent subsequent successful paracentesis when ultrasound guidance was used. Ultrasound revealed that the rest of the patients (13%) did not have enough fluid to attempt ultrasound-guided paracentesis.20
Technique
4. We recommend that ultrasound should be used to assess the characteristics of intraperitoneal free fluid to guide clinical decision making of where paracentesis can be safely performed.
Rationale. The presence and characteristics of intraperitoneal fluid collections are important determinants of whether paracentesis, another procedure, or no procedure should be performed in a given clinical scenario. One study reported that the overall diagnostic accuracy of physical examination for detecting ascites was only 58%,50 and many providers are unable to detect ascites by physical examination until 1L of fluid has accumulated. One small study showed that at least 500 ml of fluid must accumulate before shifting dullness could be detected.58 By contrast, ultrasound has been shown to reliably detect as little as 100 mL of peritoneal free fluid 52,53 and has been proven to be superior to physical examination in several studies.11,12 Therefore, ultrasound can be used to qualitatively determine whether a sufficient volume of intraperitoneal free fluid is present to safely perform paracentesis.
Studies have shown that ultrasound can also be used to differentiate ascites from other pathologies (eg, matted bowel loops, metastases, abscesses) in patients with suspected ascites on history and physical examination.16 In addition, ultrasound can help to better understand the etiology and distribution of the ascites.59-61 Sonographic measurements allow semiquantitative assessment of the volume of intraperitoneal free fluid, which may correlate with the amount of fluid removed in therapeutic paracentesis procedures.62,63 Furthermore, depth of a fluid collection by ultrasound may be an independent risk factor for the presence of spontaneous bacterial peritonitis (SBP), with one small study showing a higher risk of SBP with larger fluid collections than with small ones.64
5. We recommend that ultrasound should be used to identify a needle insertion site based on size of the fluid collection, thickness of the abdominal wall, and proximity to abdominal organs.
Rationale. When providers perform paracentesis using ultrasound guidance, any fluid collection that is directly visualized and accessible may be considered for drainage. The presence of ascites using ultrasound is best detected using a low-frequency transducer, such as phased array or curvilinear transducer, which provides deep penetration into the abdomen and pelvis to assess peritoneal free fluid.13,14,45,51,65 An optimal needle insertion site should be determined based on a combination of visualization of largest fluid collection, avoidance of underlying abdominal organs, and thickness of abdominal wall.13,31,66,67
6. We recommend the needle insertion site should be evaluated using color flow Doppler ultrasound to identify and avoid abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. The anatomy of the superficial blood vessels of the abdominal wall, especially the lateral branches, varies greatly.68-70 Although uncommon, inadvertent laceration of an inferior epigastric artery or one of its large branches is associated with significant morbidity and mortality.10,15,69,71-73 A review of 126 cases of rectus sheath hematomas, which most likely occur due to laceration of the inferior or superior epigastric artery, at a single institution from 1992 to 2002 showed a mortality rate of 1.6%, even with aggressive intervention.74 Besides the inferior epigastric arteries, several other blood vessels are at risk of injury during paracentesis, including the inferior epigastric veins, thoracoepigastric veins, subcostal artery and vein branches, deep circumflex iliac artery and vein, and recanalized subumbilical vasculature.75-77 Laceration of any of the abdominal wall blood vessels could result in catastrophic bleeding.
Identification of abdominal wall blood vessels is most commonly performed with a high-frequency transducer using color flow Doppler ultrasound.10,13-15 A low-frequency transducer capable of color flow Doppler ultrasound may be utilized in patients with a thick abdominal wall.
Studies suggest that detection of abdominal wall blood vessels with ultrasound may reduce the risk of bleeding complications. One study showed that 43% of patients had a vascular structure present at one or more of the three traditional landmark paracentesis sites.78 Another study directly compared bleeding rates between an approach utilizing a low-frequency transducer to identify the largest collection of fluid only versus a two-transducer approach utilizing both low and high-frequency transducers to identify the largest collection of fluid and evaluate for any superficial blood vessels. In this study, which included 5,777 paracenteses, paracentesis-related minor bleeding rates were similar in both groups, but major bleeding rates were less in the group utilizing color flow Doppler to evaluate for superficial vessels (0.3% vs 0.08%); differences found between groups, however, did not reach statistical significance (P = .07).79
7. We recommend that a needle insertion site should be evaluated in multiple planes to ensure clearance from underlying abdominal organs and detect any abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. Most ultrasound machines have a slice thickness of <4 mm at the focal zone.80 Considering that an ultrasound beam represents a very thin 2-dimentional cross-section of the underlying tissues, visualization in only one plane could lead to inadvertent puncture of nearby critical structures such as loops of bowel or edges of solid organs. Therefore, it is important to evaluate the needle insertion site and surrounding areas in multiple planes by tilting the transducer and rotating the transducer to orthogonal planes.61 Additionally, evaluation with color flow Doppler could be performed in a similar fashion to ensure that no large blood vessels are along the anticipated needle trajectory.
8. We recommend that a needle insertion site should be marked with ultrasound immediately before performing the procedure, and the patient should remain in the same position between marking the site and performing the procedure.
Rationale. Free-flowing peritoneal fluid and abdominal organs, especially loops of small bowel, can easily shift when a patient changes position or takes a deep breath.13,16,53 Therefore, if the patient changes position or there is a delay between marking the needle insertion site and performing the procedure, the patient should be reevaluated with ultrasound to ensure that the marked needle insertion site is still safe for paracentesis.78 After marking the needle insertion site, the skin surface should be wiped completely clean of gel, and the probe should be removed from the area before sterilizing the skin surface.
9. We recommend that using real-time ultrasound guidance for paracentesis should be considered when the fluid collection is small or difficult to access.
Rationale. Use of real-time ultrasound guidance for paracentesis has been described to drain abdominal fluid collections.13,20,62 Several studies have commented that real-time ultrasound guidance for paracentesis may be necessary in obese patients, in patients with small fluid collections, or when performing the procedure near critical structures, such as loops of small bowel, liver, or spleen.57,81 Real-time ultrasound guidance for paracentesis requires additional training in needle tracking techniques and specialized equipment to maintain sterility.
Training
10. We recommend that dedicated training sessions, including didactics, supervised practice on patients, and simulation-based practice, should be used to teach novices how to perform ultrasound-guided paracentesis.
Rationale. Healthcare providers must gain multiple skills to safely perform ultrasound-guided paracentesis. Trainees must learn how to operate the ultrasound machine to identify the most appropriate needle insertion site based on the abdominal wall thickness, fluid collection size, proximity to nearby abdominal organs, and presence of blood vessels. Education regarding the use of ultrasound guidance for paracentesis is both desired 82,83 and being increasingly taught to health care providers who perform paracentesis.20,84-86
Several approaches have shown high uptake of essential skills to perform ultrasound-guided paracentesis after short training sessions. One study showed that first-year medical students can be taught to use POCUS to accurately diagnose ascites after three 30-minute teaching sessions.19 Another study showed that emergency medicine residents can achieve high levels of proficiency in the preprocedural ultrasound evaluation for paracentesis with only one hour of didactic training.20 Other studies also support the concept that adequate proficiency is achievable within brief, focused training sessions.21-28 However, these skills can decay significantly over time without ongoing education.87
11. We recommend that simulation-based practice should be used, when available, to facilitate acquisition of the required knowledge and skills to perform ultrasound-guided paracentesis.
Rationale. Simulation-based practice should be used when available, as it has been shown to increase competence in bedside diagnostic ultrasonography and procedural techniques for ultrasound-guided procedures, including paracentesis.22,25,29,88,89 One study showed that internal medicine residents were able to achieve a high level of proficiency to perform ultrasound-guided paracentesis after a three-hour simulation-based mastery learning session.88 A follow-up study suggested that, after sufficient simulation-based training, a nonradiologist can perform ultrasound-guided paracentesis as safely as an interventional radiologist.29
12. We recommend that competence in performing ultrasound-guided paracentesis should be demonstrated prior to independently performing the procedure on patients.
Rationale. Competence in ultrasound-guided paracentesis requires acquisition of clinical knowledge of paracentesis, skills in basic abdominal ultrasonography, and manual techniques to perform the procedure. Competence in ultrasound-guided paracentesis cannot be assumed for those graduating from internal medicine residency in the United States. While clinical knowledge of paracentesis remains a core competency of graduating internal medicine residents per the American Board of Internal Medicine, demonstration of competence in performing ultrasound-guided or landmark-based paracentesis is not currently mandated.90 A recent national survey of internal medicine residency program directors revealed that the curricula and resources available to train residents in bedside diagnostic ultrasound and ultrasound-guided procedures, including paracentesis, remain quite variable. 83
While it has not been well studied, competence in ultrasound for paracentesis, as with all other skills involved in bedside procedures, is likely best evaluated through direct observation on actual patients.91 As such, individualized systems to evaluate competency in ultrasound-guided paracentesis should be established for each site where it is performed. A list of consensus-derived ultrasound competencies for ultrasound-guided paracentesis has been proposed, and this list may serve as a guide for both training curriculum development and practitioner evaluation.86,91,92
KNOWLEDGE GAPS
In the process of developing these recommendations, we identified several important gaps in the literature regarding the use of ultrasound guidance for paracentesis.
First, while some data suggest that the use of ultrasound guidance for paracentesis may reduce the inpatient length of stay and overall costs, this suggestion has not been studied rigorously. In a retrospective review of 1,297 abdominal paracenteses by Patel et al., ultrasound-guided paracentesis was associated with a lower incidence of adverse events compared with landmark-based paracentesis (1.4% vs 4.7%; P = .01). The adjusted analysis from this study showed significant reductions in adverse events (OR 0.35; 95%CI 0.165-0.739; P = .006) and hospitalization costs ($8,761 ± $5,956 vs $9,848 ± $6,581; P < .001) for paracentesis with ultrasound guidance versus without such guidance. Additionally, the adjusted average length of stay was 0.2 days shorter for paracentesis with ultrasound guidance versus that without guidance (5.6 days vs 5.8 days; P < .0001).44 Similar conclusions were reached by Mercaldi et al., who conducted a retrospective study of 69,859 patients who underwent paracentesis. Fewer bleeding complications occurred when paracentesis was performed with ultrasound guidance (0.27%) versus without ultrasound guidance (1.27%). Hospitalization costs increased by $19,066 (P < .0001) and length of stay increased by 4.3 days (P < .0001) for patients when paracentesis was complicated by bleeding.43 Because both of these studies were retrospective reviews of administrative databases, associations between procedures, complications, and use of ultrasound may be limited by erroneous coding and documentation.
Second, regarding technique, it is unknown whether the use of real-time ultrasound guidance confers additional benefits compared with use of static ultrasound to mark a suitable needle insertion site. In clinical practice, real-time ultrasound guidance is used to sample small fluid collections, particularly when loops of bowel or a solid organ are nearby. It is possible that higher procedural success rates and lower complication rates may be demonstrated in these scenarios in future studies.
Third, the optimal approach to train providers to perform ultrasound-guided paracentesis is unknown. While short training sessions have shown high uptake of essential skills to perform ultrasound-guided paracentesis, data regarding the effectiveness of training using a comprehensive competency assessment are limited. Simulation-based mastery learning as a means to obtain competency for paracentesis has been described in one study,88 but the translation of competency demonstrated by simulation to actual patient outcomes has not been studied. Furthermore, the most effective method to train providers who are proficient in landmark-based paracentesis to achieve competency in ultrasound-guided paracentesis has not been well studied.
Fourth, the optimal technique for identifying blood vessels in the abdominal wall is unknown. We have proposed that color flow Doppler should be used to identify and avoid puncture of superficial vessels, but power Doppler is three times more sensitive at detecting blood vessels, especially at low velocities, such as in veins independent of direction or flow.93 Hence using power Doppler instead of color flow Doppler may further improve the ability to identify and avoid superficial vessels along the needle trajectory.92
Finally, the impact of ultrasound use on patient experience has yet to be studied. Some studies in the literature show high patient satisfaction with use of ultrasound at the bedside,94,95 but patient satisfaction with ultrasound-guided paracentesis has not been compared directly with the landmark-based technique.
CONCLUSIONS
The use of ultrasound guidance for paracentesis has been associated with higher success rates and lower complication rates. Ultrasound is superior to physical examination in assessing the presence and volume of ascites, and determining the optimal needle insertion site to avoid inadvertent injury to abdominal wall blood vessels. Hospitalists can attain competence in ultrasound-guided paracentesis through the use of various training methods, including lectures, simulation-based practice, and hands-on training. Ongoing use and training over time is necessary to maintain competence.
Acknowledgments
The authors thank all the members of the Society of Hospital Medicine Point-of-care Ultrasound Task Force and the Education Committee members for their time and dedication to develop these guidelines.
SHM Point-of-care Ultrasound Task Force: CHAIRS: Nilam Soni, Ricardo Franco Sadud, Jeff Bates. WORKING GROUPS: Thoracentesis Working Group: Ria Dancel (chair), Daniel Schnobrich, Nitin Puri. Vascular Access Working Group: Ricardo Franco (chair), Benji Matthews, Saaid Abdel-Ghani, Sophia Rodgers, Martin Perez, Daniel Schnobrich. Paracentesis Working Group: Joel Cho (chair), Benji Mathews, Kreegan Reierson, Anjali Bhagra, Trevor P. Jensen. Lumbar Puncture Working Group: Nilam J. Soni (chair), Ricardo Franco, Gerard Salame, Josh Lenchus, Venkat Kalidindi, Ketino Kobaidze. Credentialing Working Group: Brian P Lucas (chair), David Tierney, Trevor P. Jensen PEER REVIEWERS: Robert Arntfield, Michael Blaivas, Richard Hoppmann, Paul Mayo, Vicki Noble, Aliaksei Pustavoitau, Kirk Spencer, Vivek Tayal. METHODOLOGIST: Mahmoud El Barbary. LIBRARIAN: Loretta Grikis. SOCIETY OF HOSPITAL MEDICINE EDUCATION COMMITTEE: Daniel Brotman (past chair), Satyen Nichani (current chair), Susan Hunt. SOCIETY OF HOSPITAL MEDICINE STAFF: Nick Marzano.
Collaborators of the Society of Hospital Medicine Point-of-care Ultrasound Task Force
Saaid Abdel-Ghani, Robert Arntfield, Jeffrey Bates, Michael Blaivas, Dan Brotman, Carolina Candotti, Richard Hoppmann, Susan Hunt, Venkat Kalidindi, Ketino Kobaidze, Josh Lenchus, Paul Mayo, Satyen Nichani, Vicki Noble, Martin Perez, Nitin Puri, Aliaksei Pustavoitau, Sophia Rodgers, Gerard Salame, Daniel Schnobrich, Kirk Spencer, Vivek Tayal, David M. Tierney
Disclaimer
The contents of this publication do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
All 5 appendices are viewable online at https://www.journalofhospitalmedicine.com.
1. Duszak R, Jr., Chatterjee AR, Schneider DA. National fluid shifts: fifteen-year trends in paracentesis and thoracentesis procedures. J Am Coll Radiol. 2010;7(11):859-864. doi: 10.1016/j.jacr.2010.04.013.
2. O’Brien CR, Chang J, Campos RA, et al. Characterizing the safety of paracentesis in hospitalized patients with cirrhosis and ascites from 2004-2012 in the United States. Gastroenterology. 2016;150(4). https:/doi.org /10.1016/S0016-5085(16)32196-5.
3. Gaetano JN, Micic D, Aronsohn A, et al. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. J Gastroenterol Hepatol. 2016;31(5):1025-1030. doi: 10.1016/S0016-5085(16)32196-5
4. Orman ES, Hayashi PH, Bataller R, Barritt AS. Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites. Clin Gastroenterol Hepatol. 2014;12(3):496-503.e1. doi: 10.1016/j.cgh.2013.08.025.
5. Mallory A, Schaefer JW. Complications of diagnostic paracentesis in patients with liver disease. JAMA. 1978;239(7):628-630. doi: 10.1001/jama.1978.03280340048020.
6. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005;21(5):525-529. doi: 10.1111/j.1365-2036.2005.02387.x.
7. Shekhar C, Ramakrishnan A, Claridge LC. Paracentesis: UK trainees’ practice, experience and attitudes. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.096.
8. De Gottardi A, Thevenot T, Spahr L, et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7(8):906-909. doi: 10.1016/j.cgh.2009.05.004.
9. Sharzehi K, Jain V, Naveed A, Schreibman I. Hemorrhagic complications of paracentesis: a systematic review of the literature. Gastroenterol Res Pract. 2014;2014:985141. doi: 10.1155/2014/985141.
10. Sekiguchi H, Suzuki J, Daniels CE. Making paracentesis safer: a proposal for the use of bedside abdominal and vascular ultrasonography to prevent a fatal complication. Chest. 2013;143(4):1136-1139. doi: 10.1378/chest.12-0871.
11. Soyuncu S, Cete Y, Bozan H, Kartal M, Akyol AJ. Accuracy of physical and ultrasonographic examinations by emergency physicians for the early diagnosis of intraabdominal haemorrhage in blunt abdominal trauma. Injury. 2007;38(5):564-569. doi: 10.1016/j.injury.2007.01.010.
12. Chongtham DS, Singh MM, Kalantri SP, Pathak S, Jain AP. Accuracy of clinical manoeuvres in detection of minimal ascites. Indian J Med Sci. 1998;52(11):514-520.
13. Ennis J, Schultz G, Perera P, Williams S, Gharahbaghian L, Mandavia D. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293. doi: 10.4236/ijcm.2014.520163.
14. Szabo TL, Lewin PA. Ultrasound transducer selection in clinical imaging practice. J Ultrasound Med. 2013;32(4):573-582. doi: 10.7863/jum.2013.32.4.573.
15. Stone JC, Moak JH. Feasibility of sonographic localization of the inferior epigastric artery before ultrasound-guided paracentesis. Am J Emerg Med. 2015;33(12):1795-1798. doi: 10.1016/j.ajem.2015.06.067.
16. Yeh HC, Wolf BS. Ultrasonography in ascites. Radiology. 1977;124(3):783-790. doi: 10.1148/124.3.783.
17. Lucas BP, Asbury JK, Wang Y, et al. Impact of a bedside procedure service on general medicine inpatients: a firm-based trial. J Hosp Med. 2007;2(3):143-149. doi: 10.1002/jhm.159.
18. Kim JJ, Tsukamoto MM, Mathur AK, et al. Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis. Am J Gastroenterol. 2014;109(9):1436-1442. doi: 10.1038/ajg.2014.212.
19. Arora S, Cheung A, Tarique U, Agarwal A, Firdouse M, Ailon J. First-year medical students use of ultrasound or physical examination to diagnose hepatomegaly and ascites: a randomized controlled trial. J Ultrasound. 2017;20(3):199-204. doi: 10.1007/s40477-017-0261-6.
20. Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005;23(3):363-367. doi: 10.1016/j.ajem.2004.11.001.
21. Kotagal M, Quiroga E, Ruffatto BJ, et al. Impact of point-of-care ultrasound training on surgical residents’ confidence. J Surg Educ. 2015;72(4):e82-87. doi: 10.1016/j.jsurg.2015.01.021.
22. Martin R, Gannon D, Riggle J, et al. A comprehensive workshop using simulation to train internal medicine residents in bedside procedures performed by internists. Chest. 2012;142(4):545A. doi: 10.1378/chest.1390093.
23. Quddus A, Minami T, Summerhill E. Impact of a short 3-hour ultrasound training workshop for internal medicine residents. Chest. 2014;146(4): 509A. doi: 10.1378/chest.1989267.
24. Lanoix R, Leak LV, Gaeta T, Gernsheimer JR. A preliminary evaluation of emergency ultrasound in the setting of an emergency medicine training program. Am J Emerg Med. 2000;18(1):41-45. doi: 10.1016/S0735-6757(00)90046-9.
25. Dulohery MM, Eaton J, Tajouri T, Bhagra A. Ultrasound for internal medicine physicians: the future of physical exam. J Ultrasound Med. 2014;33(6):1005-1011. doi: 10.7863/ultra.33.6.1005
26. Lanoix R, Baker WE, Mele JM, Dharmarajan L. Evaluation of an instructional model for emergency ultrasonography. Acad Emerg Med. 1998;5(1):58-63. doi: 10.1111/j.1553-2712.1998.tb02576.x.
27. Terkamp C, Kirchner G, Wedemeyer J, et al. Simulation of abdomen sonography. Evaluation of a new ultrasound simulator. Ultraschall Med. 2003;24(4):239-234. doi: 10.1055/s-2003-41713.
28. Barsuk JH, Cohen ER, Potts S, et al. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23(9):749-756. doi: 10.1136/bmjqs-2013-002665.
29. Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126(4):349-356. doi: 10.1016/j.amjmed.2012.09.016.
30. Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User’s Manual. Santa Monica, CA: Rand Corp.; 2001.
31. Bard C, Lafortune M, Breton G. Ascites: ultrasound guidance or blind paracentesis? CMAJ. 1986;135(3):209-210. doi: 10.1016/0736-4679(87)90268-X.
32. Sudulagunta SR, Sodalagunta MB, Bangalore Raja SK, Khorram H, Sepehrar M, Noroozpour Z. Clinical profile and complications of paracentesis in refractory ascites patients with cirrhosis. Gastroenterol Res. 2015;8(3-4):228-233. doi: 10.14740/gr661w.
33. Lin S, Wang M, Zhu Y, et al. Hemorrhagic complications following abdominal paracentesis in acute on chronic liver failure: a propensity score analysis. Medicine (Baltimore). 2015;94(49):e2225. doi: 10.1097/MD.0000000000002225.
34. Lam EY, McLafferty RB, Taylor LM, Jr., et al. Inferior epigastric artery pseudoaneurysm: a complication of paracentesis. J Vasc Surg. 1998;28(3):566-569. doi: 10.1016/S0741-5214(98)70147-8.
35. Cervini P, Hesley GK, Thompson RL, Sampathkumar P, Knudsen JM. Incidence of infectious complications after an ultrasound-guided intervention. AJR Am J Roentgenol. 2010;195(4):846-850. doi: 10.2214/AJR.09.3168.
36. Wiese SS, Mortensen C, Bendtsen F. Few complications after paracentesis in patients with cirrhosis and refractory ascites. Dan Med Bull. 2011;58(1):A4212.
37. Jakobson DJ, Shemesh I. Merging ultrasound in the intensive care routine. Isr Med Assoc J. 2013;15(11):688-692.
38. Landers A, Ryan B. The use of bedside ultrasound and community-based paracentesis in a palliative care service. J Prim Health Care. 2014;6(2):148-151.
39. Lin CH, Shih FY, Ma MH, Chiang WC, Yang CW, Ko PC. Should bleeding tendency deter abdominal paracentesis? Dig Liver Dis. 2005;37(12):946-951. doi: 10.1016/j.dld.2005.07.009.
40. Kurup AN, Lekah A, Reardon ST, et al. Bleeding rate for ultrasound-guided paracentesis in thrombocytopenic patients. J Ultrasound Med. 2015;34(10):1833-1838. doi: 10.7863/ultra.14.10034.
41. Reardon S, Atwell TD, Lekah A. Major bleeding complication rate of ultrasound-guided paracentesis in thrombocytopenic patients. J Vasc Interv Radiol. 2013;24(4):S56. doi: 10.1016/j.jvir.2013.01.129.
42. Czul F, Prager M, Lenchus J. Intra-procedural risk of bleeding associated with ultrasound guided paracentesis in patients with abnormal coagulation studies: 1907. Hepatology. 2011;54(4):1259A.
43. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532-538. doi: 10.1378/chest.12-0447.
44. Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012;15(1):1-7. doi: 10.3111/13696998.2011.628723.
45. Nicolaou S, Talsky A, Khashoggi K, Venu V. Ultrasound-guided interventional radiology in critical care. Crit Care Med. 2007;35(5 Suppl):S186-197. doi: 10.1097/01.CCM.0000260630.68855.DF.
46. Conduit B, Wesley E, Christie J, Thalheimer U. PTU-002 Large volume paracentesis (LVP) can be safely performed by junior doctors without ultrasound guidance. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.095.
47. Williams JW, Jr., Simel DL. The rational clinical examination. Does this patient have ascites? How to divine fluid in the abdomen. JAMA. 1992;267(19):2645-2648. doi: 10.1001/jama.1992.03480190087038.
48. Rodriguez A, DuPriest RW, Jr., Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457-459.
49. McGibbon A, Chen GI, Peltekian KM, van Zanten SV. An evidence-based manual for abdominal paracentesis. Dig Dis Sci. 2007;52(12):3307-3315. doi: 10.1007/s10620-007-9805-5.
50. Cattau EL, Jr., Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247(8):1164-1166. doi: 10.1001/jama.1982.03320330060027.
51. Ali J, Rozycki GS, Campbell JP, Boulanger BR, Waddell JP, Gana TJ. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res. 1996;63(1):275-279. doi: 10.1006/jsre.1996.0260.
52. Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003;21(6):476-478. doi: 10.1016/S0735-6757(03)00162-1
53. Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22. doi: 10.1148/96.1.15.
54. Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39(2):375-380. doi: 10.1016/0736-4679(96)84805-0.
55. Paajanen H, Lahti P, Nordback I. Sensitivity of transabdominal ultrasonography in detection of intraperitoneal fluid in humans. Eur Radiol. 1999;9(7):1423-1425. doi: 10.1007/s003300050861.
56. Prabhakar A, Thabet A, Mueller P, Gee MS. Image-guided peritoneal access for fluid infusion in oncology patients: Indications, technique, and outcomes. J Vasc Interv Radiol. 2014;25(3):S41. doi: 10.1016/j.jvir.2013.12.100.
57. McGahan JP, Anderson MW, Walter JP. Portable real-time sonographic and needle guidance systems for aspiration and drainage. AJR Am J Roentgenol. 1986;147(6):1241-1246. doi: 10.2214/ajr.147.6.1241.
58. Moses WR. Shifting dullness in the abdomen. South Med J. 1946;39(12):985-987.
59. Edell SL, Gefter WB. Ultrasonic differentiation of types of ascitic fluid. AJR Am J Roentgenol. 1979;133(1):111-114. doi: 10.2214/ajr.133.1.111.
60. Doust BD, Thompson R. Ultrasonography of abdominal fluid collections. Gastrointest Radiol. 1978;3(3):273-279. doi: 10.1007/BF01887079.
61. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 2. Chest. 2005;128(3):1766-1781. doi: 10.1378/chest.128.3.1766.
62. Irshad A, Ackerman SJ, Anis M, Campbell AS, Hashmi A, Baker NL. Can the smallest depth of ascitic fluid on sonograms predict the amount of drainable fluid? J Clin Ultrasound. 2009;37(8):440-444. doi: 10.1002/jcu.20616.
63. Inadomi J, Cello JP, Koch J. Ultrasonographic determination of ascitic volume. Hepatology. 1996;24(3):549-551. doi: 10.1002/hep.510240314.
64. Sideris A, Patel P, Charles HW, Park J, Feldman D, Deipolyi AR. Imaging and clinical predictors of spontaneous bacterial peritonitis diagnosed by ultrasound-guided paracentesis. Proc (Bayl Univ Med Cent). 2017;30(3):262-264. https://doi.org/10.1080/08998280.2017.11929610
65. Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014;30(2):305-329. doi: 10.1016/j.ccc.2013.10.005.
66. Ross GJ, Kessler HB, Clair MR, Gatenby RA, Hartz WH, Ross LV. Sonographically guided paracentesis for palliation of symptomatic malignant ascites. AJR Am J Roentgenol. 1989;153(6):1309-1311. doi: 10.2214/ajr.153.6.1309.
67. Russell KW, Mone MC, Scaife CL. Umbilical paracentesis for acute hernia reduction in cirrhotic patients. BMJ Case Rep. 2013;2013. doi: 10.1136/bcr-2013-201304.
68. Epstein J, Arora A, Ellis H. Surface anatomy of the inferior epigastric artery in relation to laparoscopic injury. Clin Anat. 2004;17(5):400-408. doi: 10.1002/ca.10192.
69. Suzuki J, Sekiguchi H. Laceration of inferior epigastric artery resulting in abdominal compartment syndrome: a fatal complication of paracentesis. Am J Respir Crit Care Med. 2012;185:A5974. doi: 10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5974
70. Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg. 2004;239(2):182-185. doi: 10.1097/01.sla.0000109151.53296.07.
71. Webster ST, Brown KL, Lucey MR, Nostrant TT. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol. 1996;91(2):366-368.
72. Todd AW. Inadvertent puncture of the inferior epigastric artery during needle biopsy with fatal outcome. Clin Radiol. 2001;56(12):989-990. doi: 10.1053/crad.2001.0175.
73. Seidler M, Sayegh K, Roy A, Mesurolle B. A fatal complication of ultrasound-guided abdominal paracentesis. J Clin Ultrasound. 2013;41(7):457-460. doi: 10.1002/jcu.22050.
74. Cherry WB, Mueller PS. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore). 2006;85(2):105-110. doi: 10.1097/01.md.0000216818.13067.5a.
75. Oelsner DH, Caldwell SH, Coles M, Driscoll CJ. Subumbilical midline vascularity of the abdominal wall in portal hypertension observed at laparoscopy. Gastrointest Endosc. 1998;47(5):388-390. doi: 10.1016/S0016-5107(98)70224-X.
76. Krupski WC, Sumchai A, Effeney DJ, Ehrenfeld WK. The importance of abdominal wall collateral blood vessels. Planning incisions and obtaining arteriography. Arch Surg. 1984;119(7):854-857. doi: 10.1001/archsurg.1984.01390190092021.
77. Rozen WM, Ashton MW, Taylor GI. Reviewing the vascular supply of the anterior abdominal wall: redefining anatomy for increasingly refined surgery. Clin Anat. 2008;21(2):89-98. doi: 10.1002/ca.20585.
78. Adams A, Roggio A, Wilkerson RG. 368 Sonographic assessment of inadvertent vascular puncture during paracentesis using the traditional landmark approach. Ann Emerg Med. 2015;66:S132-S133. doi: 10.1016/j.annemergmed.2015.07.404
79. Barsuk JH, Rosen BT, Cohen ER, Feinglass J, Ault MJ. Vascular ultrasonography: a novel method to reduce paracentesis related major bleeding. J Hosp Med. 2018;13(1):30-33. doi: 10.12788/jhm.2863.
80. Skolnick ML. Estimation of ultrasound beam width in the elevation (section thickness) plane. Radiology. 1991;180(1):286-288. doi: 10.1148/radiology.180.1.2052713.
81. Keil-Rios D, Terrazas-Solis H, Gonzalez-Garay A, Sanchez-Avila JF, Garcia-Juarez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. doi: 10.1007/s11739-016-1406-x.
82. Kessler C, Bhandarkar S. Ultrasound training for medical students and internal medicine residents--a needs assessment. J Clin Ultrasound. 2010;38(8):401-408. doi: 10.1002/jcu.20719.
83. Schnobrich DJ, Gladding S, Olson AP, Duran-Nelson A. Point-of-care ultrasound in internal medicine: a national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. doi: 10.4300/JGME-D-12-00215.1.
84. Eisen LA, Leung S, Gallagher AE, Kvetan V. Barriers to ultrasound training in critical care medicine fellowships: a survey of program directors. Crit Care Med. 2010;38(10):1978-1983. doi: 10.1097/CCM.0b013e3181eeda53.
85. Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med. 2007;35(5 Suppl):S290-304. doi: 10.1097/01.CCM.0000260680.16213.26.
86. Ma I, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. doi: 10.1007/s11606-017-4071-5.
87. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi: 10.4300/JGME-14-00284.1.
88. Barsuk JH, Cohen ER, Vozenilek JA, O’Connor LM, McGaghie WC, Wayne DB. Simulation-based education with mastery learning improves paracentesis skills. J Grad Med Educ. 2012;4(1):23-27. doi: 10.4300/JGME-D-11-00161.1.
89. Lenchus JD. End of the “see one, do one, teach one” era: the next generation of invasive bedside procedural instruction. J Am Osteopath Assoc. 2010;110(6):340-346. doi: 10.7556/jaoa.2010.110.6.340.
90. American Board of Internal Medicine. Policies and Procedures for Certification. Philadelphia, PA: ABIM; 2006.
91. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. doi: 10.12788/jhm.2917.
92. Brown GM, Otremba M, Devine LA, Gray C, Millington SJ, Ma IW. Defining competencies for ultrasound-guided bedside procedures: consensus opinions from Canadian physicians. J Ultrasound Med. 2016;35(1):129-141. doi: 10.7863/ultra.15.01063.
93. Babcock DS, Patriquin H, LaFortune M, Dauzat M. Power doppler sonography: basic principles and clinical applications in children. Pediatr Radiol. 1996;26(2):109-115. doi: 10.1007/BF01372087.
94. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. doi: 10.1016/j.jemermed.2013.05.044.
95. Lindelius A, Torngren S, Nilsson L, Pettersson H, Adami J. Randomized clinical trial of bedside ultrasound among patients with abdominal pain in the emergency department: impact on patient satisfaction and health care consumption. Scand J Trauma Resusc Emerg Med. 2009;17:60. doi: 10.1186/1757-7241-17-60.
Abdominal paracentesis is a common and increasingly performed procedure in the United States. According to Medicare Physician Supplier Procedure Summary Master Files, an estimated 150,000 paracenteses were performed on Medicare fee-for-service beneficiaries in 2008 alone; such a number represents more than a two-fold increase from the same service population in 1993.1 This increasing trend was again noted by the Nationwide Inpatient Sample data, which identified a 10% increase in hospitalized patients with a diagnosis of cirrhosis receiving paracentesis from 2004 (50%) to 2012 (61%; P < .0001).2
Although these data demonstrate that paracentesis is being performed frequently, paracentesis may be underutilized in hospitalized cirrhotics with ascites. In addition, in-hospital mortality of cirrhotics with ascites is higher among those who do not undergo paracentesis than among those who do (9% vs 6%; P = .03).3,4
While complications associated with paracentesis are rare, serious complications, including death, have been documented.5-10 The most common serious complication of paracentesis is bleeding, although puncture of the bowel and other abdominal organs has also been observed. Over the past few decades, ultrasound has been increasingly used with paracentesis due to the ability of ultrasound to improve detection of ascites11,12 and to avoid blood vessels10,13-15 and bowels.16
Three-quarters of all paracenteses are currently performed by interventional radiologists.1 However, paracenteses are often required off-hours,17 when interventional radiologists are less readily available. Weekend admissions have less frequent performance of early paracentesis than weekday admissions, and delaying paracentesis may increase mortality.3,18 High proficiency in ultrasound-guided paracentesis is achievable by nonradiologists19-28 with equal or better patient outcomes after appropriate training.29
The purpose of this guideline is to review the literature and present evidence-based recommendations on the performance of ultrasound-guided paracentesis at the bedside by practicing hospitalists.
METHODS
Detailed methods are described in Appendix 1. The Society of Hospital Medicine (SHM) Point-of-care Ultrasound (POCUS) Task Force was assembled to carry out this guideline development project under the direction of the SHM Board of Directors, Director of Education, and Education Committee. All expert panel members were physicians or advanced-practice providers with expertise in POCUS. Expert panel members were divided into working group members, external peer reviewers, and a methodologist, and all Task Force members were required to disclose any potential conflicts of interests (Appendix 2). The literature search was conducted in two independent phases. The first phase included literature searches conducted by the five working group members themselves. Key clinical questions and draft recommendations were then prepared, and a systematic literature search was conducted by a medical librarian based on the findings of the initial literature search and draft recommendations. The Medline, Embase, CINAHL, and Cochrane medical databases were initially searched from 1975 to October 2015. Google Scholar was also searched without limiters. An updated search was conducted from November 2015 to November 2017, search strings for which are included in Appendix 3. All article abstracts were first screened for relevance by at least two members of the working group. Full-text versions of screened articles were reviewed and articles on ultrasound guidance for paracentesis were selected. The following article types were excluded: non-English language, nonhuman, age <18 years, meeting abstracts, meeting posters, letters, and editorials. All relevant systematic reviews, meta-analyses, randomized controlled trials, and observational studies of ultrasound-guided paracentesis were screened and selected. Final article selection was based on working group consensus. The selected literature was incorporated into the draft recommendations.
We used the RAND Appropriateness Method that required panel judgment and consensus to establish recommendations.30 The voting members of the SHM POCUS Task Force reviewed and voted on the draft recommendations considering five transforming factors: (1) problem priority and importance; (2) level of quality of evidence; (3) benefit/harm balance; (4) benefit/burden balance; and (5) certainty/concerns about preferences/equity acceptability/feasibility. Panel members participated in two rounds of electronic voting using an internet-based electronic data collection tool (Redcap™) during February 2018 and April 2018 (Appendix 4) and voting on appropriateness was conducted using a 9-point Likert scale. The three zones based on the 9-point Likert scale were inappropriate (1-3 points), uncertain (4-6 points), and appropriate (7-9 points), and the degree of consensus was assessed using the RAND algorithm (Appendix 1, Figure 1, and Table 1). Establishing a recommendation required at least 70% agreement that a recommendation was “appropriate.” A strong recommendation required 80% of the votes within one integer of the median, following RAND rules, and disagreement was defined as >30% of panelists voting outside of the zone of the median.
Recommendations were classified as strong or weak/conditional based on preset rules defining the panel’s level of consensus, which determined the wording for each recommendation (Tables 1 and 2). The revised consensus-based recommendations underwent internal and external review by POCUS experts from different subspecialties, and a final review of the guideline document was performed by members of the SHM POCUS Task Force, SHM Education Committee, and SHM Board of Directors. The SHM Board of Directors endorsed the document prior to submission to the Journal of Hospital Medicine.
RESULTS
Literature search
A total of 794 references were pooled and screened from literature searches conducted by a certified medical librarian in October 2015 (604 citations) and updated in November 2017 (118 citations), and working group members’ personal bibliographies and searches (72 citations; Appendix 3, Figure 2). Final selection included 91 articles that were abstracted into a data table and incorporated into the draft recommendations.
RECOMMENDATIONS
Four domains (terminology, clinical outcomes, technique, and training) with 13 draft recommendations were generated based on the literature review by the paracentesis working group. After two rounds of panel voting, one recommendation did not achieve consensus based on the RAND rules, and 12 statements received final approval. The degree of consensus based on the median score and dispersion of voting around the median are shown in Appendix 5. All 12 statements achieved consensus as strong recommendations. The strength of each recommendation and degree of consensus are summarized in Table 3.
Terminology
Abdominal paracentesis is a procedure in which fluid is aspirated from the intraperitoneal space by percutaneous insertion of a needle with or without a catheter through the abdominal wall. Throughout this document, the term “paracentesis” refers to “abdominal paracentesis.”
In this document, ultrasound-guided paracentesis refers to the use of static ultrasound guidance to mark a needle insertion site immediately prior to performing the procedure. Real-time (dynamic) ultrasound guidance refers to tracking of the needle tip with ultrasound as it traverses the abdominal wall to enter the peritoneal cavity. Landmark-based paracentesis refers to paracentesis based on physical examination alone.
RECOMMENDATIONS
Clinical outcomes
1. We recommend that ultrasound guidance should be used for paracentesis to reduce the risk of serious complications, the most common being bleeding.
Rationale. The occurrence of both minor and serious life-threatening complications from paracentesis has been well described.5-10,31,32 A recent retrospective study that evaluated 515 landmark-guided paracenteses noted that the most common minor complication was persistent ascites leakage (5%) and that the most common serious complication was postprocedural bleeding (1%).8 Studies have shown that abdominal wall hematoma and hemoperitoneum are common hemorrhagic complications of paracentesis, although inferior epigastric artery pseudoaneurysm has also been described.9,33,34
Current literature suggests that ultrasound-guided paracentesis is a safe procedure, even with reduced platelet counts or elevated international normalized ratio.35-42 Most comparative studies have shown that ultrasound guidance reduces the risk of bleeding complications compared with the use of landmarks alone,7,31,32,43-45 although a few studies did not find a significant difference between techniques.20,36,46 One large retrospective observational study that analyzed the administrative data of 69,859 paracenteses from more than 600 hospitals demonstrated that ultrasound guidance reduced the odds of bleeding complications by 68% (OR, 0.32; 95% CI, 0.25–0.41). Bleeding complication rates with and without the use of ultrasound guidance were 0.27% (CI 0.26-0.29) versus 1.25% (CI 1.21-1.29; P < .0001), respectively. More importantly, in this study, paracentesis complicated by bleeding was associated with a higher in-hospital mortality rate
2. We recommend that ultrasound guidance should be used to avoid attempting paracentesis in patients with an insufficient volume of intraperitoneal free fluid to drain.
Rationale. Abdominal physical examination is not a reliable method for determining the presence or volume of intraperitoneal free fluid, as no specific physical examination finding has consistently shown both high sensitivity and specificity for detecting intraperitoneal free fluid.11,12,20,31,47-51 Patient factors limiting the diagnostic accuracy of physical examination include body habitus, abdominal wall edema, and gaseous bowel distention.
In comparative studies, ultrasound has been found to be significantly more sensitive and specific than physical examination in detecting peritoneal free fluid.11,12 Ultrasound can detect as little as 100 mL of peritoneal free fluid,52,53 and larger volumes of fluid have higher diagnostic accuracy.53-55 In one randomized trial of 100 patients suspected of having ascites, patients were randomized to landmark-based and ultrasound-guided paracentesis groups. Of the 56 patients in the ultrasound-guided group, 14 patients suspected of having ascites on physical examination were found to have no or an insufficient volume of ascites to attempt paracentesis.20 Another study with 41 ultrasound examinations on cancer patients suspected of having intraperitoneal free fluid by history and physical examination demonstrated that only 19 (46%) were considered to have a sufficient volume of ascites by ultrasound to attempt paracentesis.38
3. We recommend that ultrasound guidance should be used for paracentesis to improve the success rates of the overall procedure.
Rationale. In addition to avoiding drainage attempts in patients with an insufficient volume of intraperitoneal free fluid, ultrasound can increase the success rate of attempted procedures by localizing the largest fluid collection and guiding selection of an optimal needle insertion site. The success rates of landmark-based paracentesis in patients suspected of having intraperitoneal free fluid by physical examination are not well described in the literature, but multiple studies report success rates of 95%-100% for paracentesis when using ultrasound guidance to select a needle insertion site.20,38,56,57 In one randomized trial comparing ultrasound-guided versus landmark-based paracentesis, ultrasound-guided paracentesis revealed a significantly higher success rate (95% of procedures performed) compared with landmark-based parancentesis (61% of procedures performed). Moreover, 87% of the initial failures in the landmark-based group underwent subsequent successful paracentesis when ultrasound guidance was used. Ultrasound revealed that the rest of the patients (13%) did not have enough fluid to attempt ultrasound-guided paracentesis.20
Technique
4. We recommend that ultrasound should be used to assess the characteristics of intraperitoneal free fluid to guide clinical decision making of where paracentesis can be safely performed.
Rationale. The presence and characteristics of intraperitoneal fluid collections are important determinants of whether paracentesis, another procedure, or no procedure should be performed in a given clinical scenario. One study reported that the overall diagnostic accuracy of physical examination for detecting ascites was only 58%,50 and many providers are unable to detect ascites by physical examination until 1L of fluid has accumulated. One small study showed that at least 500 ml of fluid must accumulate before shifting dullness could be detected.58 By contrast, ultrasound has been shown to reliably detect as little as 100 mL of peritoneal free fluid 52,53 and has been proven to be superior to physical examination in several studies.11,12 Therefore, ultrasound can be used to qualitatively determine whether a sufficient volume of intraperitoneal free fluid is present to safely perform paracentesis.
Studies have shown that ultrasound can also be used to differentiate ascites from other pathologies (eg, matted bowel loops, metastases, abscesses) in patients with suspected ascites on history and physical examination.16 In addition, ultrasound can help to better understand the etiology and distribution of the ascites.59-61 Sonographic measurements allow semiquantitative assessment of the volume of intraperitoneal free fluid, which may correlate with the amount of fluid removed in therapeutic paracentesis procedures.62,63 Furthermore, depth of a fluid collection by ultrasound may be an independent risk factor for the presence of spontaneous bacterial peritonitis (SBP), with one small study showing a higher risk of SBP with larger fluid collections than with small ones.64
5. We recommend that ultrasound should be used to identify a needle insertion site based on size of the fluid collection, thickness of the abdominal wall, and proximity to abdominal organs.
Rationale. When providers perform paracentesis using ultrasound guidance, any fluid collection that is directly visualized and accessible may be considered for drainage. The presence of ascites using ultrasound is best detected using a low-frequency transducer, such as phased array or curvilinear transducer, which provides deep penetration into the abdomen and pelvis to assess peritoneal free fluid.13,14,45,51,65 An optimal needle insertion site should be determined based on a combination of visualization of largest fluid collection, avoidance of underlying abdominal organs, and thickness of abdominal wall.13,31,66,67
6. We recommend the needle insertion site should be evaluated using color flow Doppler ultrasound to identify and avoid abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. The anatomy of the superficial blood vessels of the abdominal wall, especially the lateral branches, varies greatly.68-70 Although uncommon, inadvertent laceration of an inferior epigastric artery or one of its large branches is associated with significant morbidity and mortality.10,15,69,71-73 A review of 126 cases of rectus sheath hematomas, which most likely occur due to laceration of the inferior or superior epigastric artery, at a single institution from 1992 to 2002 showed a mortality rate of 1.6%, even with aggressive intervention.74 Besides the inferior epigastric arteries, several other blood vessels are at risk of injury during paracentesis, including the inferior epigastric veins, thoracoepigastric veins, subcostal artery and vein branches, deep circumflex iliac artery and vein, and recanalized subumbilical vasculature.75-77 Laceration of any of the abdominal wall blood vessels could result in catastrophic bleeding.
Identification of abdominal wall blood vessels is most commonly performed with a high-frequency transducer using color flow Doppler ultrasound.10,13-15 A low-frequency transducer capable of color flow Doppler ultrasound may be utilized in patients with a thick abdominal wall.
Studies suggest that detection of abdominal wall blood vessels with ultrasound may reduce the risk of bleeding complications. One study showed that 43% of patients had a vascular structure present at one or more of the three traditional landmark paracentesis sites.78 Another study directly compared bleeding rates between an approach utilizing a low-frequency transducer to identify the largest collection of fluid only versus a two-transducer approach utilizing both low and high-frequency transducers to identify the largest collection of fluid and evaluate for any superficial blood vessels. In this study, which included 5,777 paracenteses, paracentesis-related minor bleeding rates were similar in both groups, but major bleeding rates were less in the group utilizing color flow Doppler to evaluate for superficial vessels (0.3% vs 0.08%); differences found between groups, however, did not reach statistical significance (P = .07).79
7. We recommend that a needle insertion site should be evaluated in multiple planes to ensure clearance from underlying abdominal organs and detect any abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. Most ultrasound machines have a slice thickness of <4 mm at the focal zone.80 Considering that an ultrasound beam represents a very thin 2-dimentional cross-section of the underlying tissues, visualization in only one plane could lead to inadvertent puncture of nearby critical structures such as loops of bowel or edges of solid organs. Therefore, it is important to evaluate the needle insertion site and surrounding areas in multiple planes by tilting the transducer and rotating the transducer to orthogonal planes.61 Additionally, evaluation with color flow Doppler could be performed in a similar fashion to ensure that no large blood vessels are along the anticipated needle trajectory.
8. We recommend that a needle insertion site should be marked with ultrasound immediately before performing the procedure, and the patient should remain in the same position between marking the site and performing the procedure.
Rationale. Free-flowing peritoneal fluid and abdominal organs, especially loops of small bowel, can easily shift when a patient changes position or takes a deep breath.13,16,53 Therefore, if the patient changes position or there is a delay between marking the needle insertion site and performing the procedure, the patient should be reevaluated with ultrasound to ensure that the marked needle insertion site is still safe for paracentesis.78 After marking the needle insertion site, the skin surface should be wiped completely clean of gel, and the probe should be removed from the area before sterilizing the skin surface.
9. We recommend that using real-time ultrasound guidance for paracentesis should be considered when the fluid collection is small or difficult to access.
Rationale. Use of real-time ultrasound guidance for paracentesis has been described to drain abdominal fluid collections.13,20,62 Several studies have commented that real-time ultrasound guidance for paracentesis may be necessary in obese patients, in patients with small fluid collections, or when performing the procedure near critical structures, such as loops of small bowel, liver, or spleen.57,81 Real-time ultrasound guidance for paracentesis requires additional training in needle tracking techniques and specialized equipment to maintain sterility.
Training
10. We recommend that dedicated training sessions, including didactics, supervised practice on patients, and simulation-based practice, should be used to teach novices how to perform ultrasound-guided paracentesis.
Rationale. Healthcare providers must gain multiple skills to safely perform ultrasound-guided paracentesis. Trainees must learn how to operate the ultrasound machine to identify the most appropriate needle insertion site based on the abdominal wall thickness, fluid collection size, proximity to nearby abdominal organs, and presence of blood vessels. Education regarding the use of ultrasound guidance for paracentesis is both desired 82,83 and being increasingly taught to health care providers who perform paracentesis.20,84-86
Several approaches have shown high uptake of essential skills to perform ultrasound-guided paracentesis after short training sessions. One study showed that first-year medical students can be taught to use POCUS to accurately diagnose ascites after three 30-minute teaching sessions.19 Another study showed that emergency medicine residents can achieve high levels of proficiency in the preprocedural ultrasound evaluation for paracentesis with only one hour of didactic training.20 Other studies also support the concept that adequate proficiency is achievable within brief, focused training sessions.21-28 However, these skills can decay significantly over time without ongoing education.87
11. We recommend that simulation-based practice should be used, when available, to facilitate acquisition of the required knowledge and skills to perform ultrasound-guided paracentesis.
Rationale. Simulation-based practice should be used when available, as it has been shown to increase competence in bedside diagnostic ultrasonography and procedural techniques for ultrasound-guided procedures, including paracentesis.22,25,29,88,89 One study showed that internal medicine residents were able to achieve a high level of proficiency to perform ultrasound-guided paracentesis after a three-hour simulation-based mastery learning session.88 A follow-up study suggested that, after sufficient simulation-based training, a nonradiologist can perform ultrasound-guided paracentesis as safely as an interventional radiologist.29
12. We recommend that competence in performing ultrasound-guided paracentesis should be demonstrated prior to independently performing the procedure on patients.
Rationale. Competence in ultrasound-guided paracentesis requires acquisition of clinical knowledge of paracentesis, skills in basic abdominal ultrasonography, and manual techniques to perform the procedure. Competence in ultrasound-guided paracentesis cannot be assumed for those graduating from internal medicine residency in the United States. While clinical knowledge of paracentesis remains a core competency of graduating internal medicine residents per the American Board of Internal Medicine, demonstration of competence in performing ultrasound-guided or landmark-based paracentesis is not currently mandated.90 A recent national survey of internal medicine residency program directors revealed that the curricula and resources available to train residents in bedside diagnostic ultrasound and ultrasound-guided procedures, including paracentesis, remain quite variable. 83
While it has not been well studied, competence in ultrasound for paracentesis, as with all other skills involved in bedside procedures, is likely best evaluated through direct observation on actual patients.91 As such, individualized systems to evaluate competency in ultrasound-guided paracentesis should be established for each site where it is performed. A list of consensus-derived ultrasound competencies for ultrasound-guided paracentesis has been proposed, and this list may serve as a guide for both training curriculum development and practitioner evaluation.86,91,92
KNOWLEDGE GAPS
In the process of developing these recommendations, we identified several important gaps in the literature regarding the use of ultrasound guidance for paracentesis.
First, while some data suggest that the use of ultrasound guidance for paracentesis may reduce the inpatient length of stay and overall costs, this suggestion has not been studied rigorously. In a retrospective review of 1,297 abdominal paracenteses by Patel et al., ultrasound-guided paracentesis was associated with a lower incidence of adverse events compared with landmark-based paracentesis (1.4% vs 4.7%; P = .01). The adjusted analysis from this study showed significant reductions in adverse events (OR 0.35; 95%CI 0.165-0.739; P = .006) and hospitalization costs ($8,761 ± $5,956 vs $9,848 ± $6,581; P < .001) for paracentesis with ultrasound guidance versus without such guidance. Additionally, the adjusted average length of stay was 0.2 days shorter for paracentesis with ultrasound guidance versus that without guidance (5.6 days vs 5.8 days; P < .0001).44 Similar conclusions were reached by Mercaldi et al., who conducted a retrospective study of 69,859 patients who underwent paracentesis. Fewer bleeding complications occurred when paracentesis was performed with ultrasound guidance (0.27%) versus without ultrasound guidance (1.27%). Hospitalization costs increased by $19,066 (P < .0001) and length of stay increased by 4.3 days (P < .0001) for patients when paracentesis was complicated by bleeding.43 Because both of these studies were retrospective reviews of administrative databases, associations between procedures, complications, and use of ultrasound may be limited by erroneous coding and documentation.
Second, regarding technique, it is unknown whether the use of real-time ultrasound guidance confers additional benefits compared with use of static ultrasound to mark a suitable needle insertion site. In clinical practice, real-time ultrasound guidance is used to sample small fluid collections, particularly when loops of bowel or a solid organ are nearby. It is possible that higher procedural success rates and lower complication rates may be demonstrated in these scenarios in future studies.
Third, the optimal approach to train providers to perform ultrasound-guided paracentesis is unknown. While short training sessions have shown high uptake of essential skills to perform ultrasound-guided paracentesis, data regarding the effectiveness of training using a comprehensive competency assessment are limited. Simulation-based mastery learning as a means to obtain competency for paracentesis has been described in one study,88 but the translation of competency demonstrated by simulation to actual patient outcomes has not been studied. Furthermore, the most effective method to train providers who are proficient in landmark-based paracentesis to achieve competency in ultrasound-guided paracentesis has not been well studied.
Fourth, the optimal technique for identifying blood vessels in the abdominal wall is unknown. We have proposed that color flow Doppler should be used to identify and avoid puncture of superficial vessels, but power Doppler is three times more sensitive at detecting blood vessels, especially at low velocities, such as in veins independent of direction or flow.93 Hence using power Doppler instead of color flow Doppler may further improve the ability to identify and avoid superficial vessels along the needle trajectory.92
Finally, the impact of ultrasound use on patient experience has yet to be studied. Some studies in the literature show high patient satisfaction with use of ultrasound at the bedside,94,95 but patient satisfaction with ultrasound-guided paracentesis has not been compared directly with the landmark-based technique.
CONCLUSIONS
The use of ultrasound guidance for paracentesis has been associated with higher success rates and lower complication rates. Ultrasound is superior to physical examination in assessing the presence and volume of ascites, and determining the optimal needle insertion site to avoid inadvertent injury to abdominal wall blood vessels. Hospitalists can attain competence in ultrasound-guided paracentesis through the use of various training methods, including lectures, simulation-based practice, and hands-on training. Ongoing use and training over time is necessary to maintain competence.
Acknowledgments
The authors thank all the members of the Society of Hospital Medicine Point-of-care Ultrasound Task Force and the Education Committee members for their time and dedication to develop these guidelines.
SHM Point-of-care Ultrasound Task Force: CHAIRS: Nilam Soni, Ricardo Franco Sadud, Jeff Bates. WORKING GROUPS: Thoracentesis Working Group: Ria Dancel (chair), Daniel Schnobrich, Nitin Puri. Vascular Access Working Group: Ricardo Franco (chair), Benji Matthews, Saaid Abdel-Ghani, Sophia Rodgers, Martin Perez, Daniel Schnobrich. Paracentesis Working Group: Joel Cho (chair), Benji Mathews, Kreegan Reierson, Anjali Bhagra, Trevor P. Jensen. Lumbar Puncture Working Group: Nilam J. Soni (chair), Ricardo Franco, Gerard Salame, Josh Lenchus, Venkat Kalidindi, Ketino Kobaidze. Credentialing Working Group: Brian P Lucas (chair), David Tierney, Trevor P. Jensen PEER REVIEWERS: Robert Arntfield, Michael Blaivas, Richard Hoppmann, Paul Mayo, Vicki Noble, Aliaksei Pustavoitau, Kirk Spencer, Vivek Tayal. METHODOLOGIST: Mahmoud El Barbary. LIBRARIAN: Loretta Grikis. SOCIETY OF HOSPITAL MEDICINE EDUCATION COMMITTEE: Daniel Brotman (past chair), Satyen Nichani (current chair), Susan Hunt. SOCIETY OF HOSPITAL MEDICINE STAFF: Nick Marzano.
Collaborators of the Society of Hospital Medicine Point-of-care Ultrasound Task Force
Saaid Abdel-Ghani, Robert Arntfield, Jeffrey Bates, Michael Blaivas, Dan Brotman, Carolina Candotti, Richard Hoppmann, Susan Hunt, Venkat Kalidindi, Ketino Kobaidze, Josh Lenchus, Paul Mayo, Satyen Nichani, Vicki Noble, Martin Perez, Nitin Puri, Aliaksei Pustavoitau, Sophia Rodgers, Gerard Salame, Daniel Schnobrich, Kirk Spencer, Vivek Tayal, David M. Tierney
Disclaimer
The contents of this publication do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
All 5 appendices are viewable online at https://www.journalofhospitalmedicine.com.
Abdominal paracentesis is a common and increasingly performed procedure in the United States. According to Medicare Physician Supplier Procedure Summary Master Files, an estimated 150,000 paracenteses were performed on Medicare fee-for-service beneficiaries in 2008 alone; such a number represents more than a two-fold increase from the same service population in 1993.1 This increasing trend was again noted by the Nationwide Inpatient Sample data, which identified a 10% increase in hospitalized patients with a diagnosis of cirrhosis receiving paracentesis from 2004 (50%) to 2012 (61%; P < .0001).2
Although these data demonstrate that paracentesis is being performed frequently, paracentesis may be underutilized in hospitalized cirrhotics with ascites. In addition, in-hospital mortality of cirrhotics with ascites is higher among those who do not undergo paracentesis than among those who do (9% vs 6%; P = .03).3,4
While complications associated with paracentesis are rare, serious complications, including death, have been documented.5-10 The most common serious complication of paracentesis is bleeding, although puncture of the bowel and other abdominal organs has also been observed. Over the past few decades, ultrasound has been increasingly used with paracentesis due to the ability of ultrasound to improve detection of ascites11,12 and to avoid blood vessels10,13-15 and bowels.16
Three-quarters of all paracenteses are currently performed by interventional radiologists.1 However, paracenteses are often required off-hours,17 when interventional radiologists are less readily available. Weekend admissions have less frequent performance of early paracentesis than weekday admissions, and delaying paracentesis may increase mortality.3,18 High proficiency in ultrasound-guided paracentesis is achievable by nonradiologists19-28 with equal or better patient outcomes after appropriate training.29
The purpose of this guideline is to review the literature and present evidence-based recommendations on the performance of ultrasound-guided paracentesis at the bedside by practicing hospitalists.
METHODS
Detailed methods are described in Appendix 1. The Society of Hospital Medicine (SHM) Point-of-care Ultrasound (POCUS) Task Force was assembled to carry out this guideline development project under the direction of the SHM Board of Directors, Director of Education, and Education Committee. All expert panel members were physicians or advanced-practice providers with expertise in POCUS. Expert panel members were divided into working group members, external peer reviewers, and a methodologist, and all Task Force members were required to disclose any potential conflicts of interests (Appendix 2). The literature search was conducted in two independent phases. The first phase included literature searches conducted by the five working group members themselves. Key clinical questions and draft recommendations were then prepared, and a systematic literature search was conducted by a medical librarian based on the findings of the initial literature search and draft recommendations. The Medline, Embase, CINAHL, and Cochrane medical databases were initially searched from 1975 to October 2015. Google Scholar was also searched without limiters. An updated search was conducted from November 2015 to November 2017, search strings for which are included in Appendix 3. All article abstracts were first screened for relevance by at least two members of the working group. Full-text versions of screened articles were reviewed and articles on ultrasound guidance for paracentesis were selected. The following article types were excluded: non-English language, nonhuman, age <18 years, meeting abstracts, meeting posters, letters, and editorials. All relevant systematic reviews, meta-analyses, randomized controlled trials, and observational studies of ultrasound-guided paracentesis were screened and selected. Final article selection was based on working group consensus. The selected literature was incorporated into the draft recommendations.
We used the RAND Appropriateness Method that required panel judgment and consensus to establish recommendations.30 The voting members of the SHM POCUS Task Force reviewed and voted on the draft recommendations considering five transforming factors: (1) problem priority and importance; (2) level of quality of evidence; (3) benefit/harm balance; (4) benefit/burden balance; and (5) certainty/concerns about preferences/equity acceptability/feasibility. Panel members participated in two rounds of electronic voting using an internet-based electronic data collection tool (Redcap™) during February 2018 and April 2018 (Appendix 4) and voting on appropriateness was conducted using a 9-point Likert scale. The three zones based on the 9-point Likert scale were inappropriate (1-3 points), uncertain (4-6 points), and appropriate (7-9 points), and the degree of consensus was assessed using the RAND algorithm (Appendix 1, Figure 1, and Table 1). Establishing a recommendation required at least 70% agreement that a recommendation was “appropriate.” A strong recommendation required 80% of the votes within one integer of the median, following RAND rules, and disagreement was defined as >30% of panelists voting outside of the zone of the median.
Recommendations were classified as strong or weak/conditional based on preset rules defining the panel’s level of consensus, which determined the wording for each recommendation (Tables 1 and 2). The revised consensus-based recommendations underwent internal and external review by POCUS experts from different subspecialties, and a final review of the guideline document was performed by members of the SHM POCUS Task Force, SHM Education Committee, and SHM Board of Directors. The SHM Board of Directors endorsed the document prior to submission to the Journal of Hospital Medicine.
RESULTS
Literature search
A total of 794 references were pooled and screened from literature searches conducted by a certified medical librarian in October 2015 (604 citations) and updated in November 2017 (118 citations), and working group members’ personal bibliographies and searches (72 citations; Appendix 3, Figure 2). Final selection included 91 articles that were abstracted into a data table and incorporated into the draft recommendations.
RECOMMENDATIONS
Four domains (terminology, clinical outcomes, technique, and training) with 13 draft recommendations were generated based on the literature review by the paracentesis working group. After two rounds of panel voting, one recommendation did not achieve consensus based on the RAND rules, and 12 statements received final approval. The degree of consensus based on the median score and dispersion of voting around the median are shown in Appendix 5. All 12 statements achieved consensus as strong recommendations. The strength of each recommendation and degree of consensus are summarized in Table 3.
Terminology
Abdominal paracentesis is a procedure in which fluid is aspirated from the intraperitoneal space by percutaneous insertion of a needle with or without a catheter through the abdominal wall. Throughout this document, the term “paracentesis” refers to “abdominal paracentesis.”
In this document, ultrasound-guided paracentesis refers to the use of static ultrasound guidance to mark a needle insertion site immediately prior to performing the procedure. Real-time (dynamic) ultrasound guidance refers to tracking of the needle tip with ultrasound as it traverses the abdominal wall to enter the peritoneal cavity. Landmark-based paracentesis refers to paracentesis based on physical examination alone.
RECOMMENDATIONS
Clinical outcomes
1. We recommend that ultrasound guidance should be used for paracentesis to reduce the risk of serious complications, the most common being bleeding.
Rationale. The occurrence of both minor and serious life-threatening complications from paracentesis has been well described.5-10,31,32 A recent retrospective study that evaluated 515 landmark-guided paracenteses noted that the most common minor complication was persistent ascites leakage (5%) and that the most common serious complication was postprocedural bleeding (1%).8 Studies have shown that abdominal wall hematoma and hemoperitoneum are common hemorrhagic complications of paracentesis, although inferior epigastric artery pseudoaneurysm has also been described.9,33,34
Current literature suggests that ultrasound-guided paracentesis is a safe procedure, even with reduced platelet counts or elevated international normalized ratio.35-42 Most comparative studies have shown that ultrasound guidance reduces the risk of bleeding complications compared with the use of landmarks alone,7,31,32,43-45 although a few studies did not find a significant difference between techniques.20,36,46 One large retrospective observational study that analyzed the administrative data of 69,859 paracenteses from more than 600 hospitals demonstrated that ultrasound guidance reduced the odds of bleeding complications by 68% (OR, 0.32; 95% CI, 0.25–0.41). Bleeding complication rates with and without the use of ultrasound guidance were 0.27% (CI 0.26-0.29) versus 1.25% (CI 1.21-1.29; P < .0001), respectively. More importantly, in this study, paracentesis complicated by bleeding was associated with a higher in-hospital mortality rate
2. We recommend that ultrasound guidance should be used to avoid attempting paracentesis in patients with an insufficient volume of intraperitoneal free fluid to drain.
Rationale. Abdominal physical examination is not a reliable method for determining the presence or volume of intraperitoneal free fluid, as no specific physical examination finding has consistently shown both high sensitivity and specificity for detecting intraperitoneal free fluid.11,12,20,31,47-51 Patient factors limiting the diagnostic accuracy of physical examination include body habitus, abdominal wall edema, and gaseous bowel distention.
In comparative studies, ultrasound has been found to be significantly more sensitive and specific than physical examination in detecting peritoneal free fluid.11,12 Ultrasound can detect as little as 100 mL of peritoneal free fluid,52,53 and larger volumes of fluid have higher diagnostic accuracy.53-55 In one randomized trial of 100 patients suspected of having ascites, patients were randomized to landmark-based and ultrasound-guided paracentesis groups. Of the 56 patients in the ultrasound-guided group, 14 patients suspected of having ascites on physical examination were found to have no or an insufficient volume of ascites to attempt paracentesis.20 Another study with 41 ultrasound examinations on cancer patients suspected of having intraperitoneal free fluid by history and physical examination demonstrated that only 19 (46%) were considered to have a sufficient volume of ascites by ultrasound to attempt paracentesis.38
3. We recommend that ultrasound guidance should be used for paracentesis to improve the success rates of the overall procedure.
Rationale. In addition to avoiding drainage attempts in patients with an insufficient volume of intraperitoneal free fluid, ultrasound can increase the success rate of attempted procedures by localizing the largest fluid collection and guiding selection of an optimal needle insertion site. The success rates of landmark-based paracentesis in patients suspected of having intraperitoneal free fluid by physical examination are not well described in the literature, but multiple studies report success rates of 95%-100% for paracentesis when using ultrasound guidance to select a needle insertion site.20,38,56,57 In one randomized trial comparing ultrasound-guided versus landmark-based paracentesis, ultrasound-guided paracentesis revealed a significantly higher success rate (95% of procedures performed) compared with landmark-based parancentesis (61% of procedures performed). Moreover, 87% of the initial failures in the landmark-based group underwent subsequent successful paracentesis when ultrasound guidance was used. Ultrasound revealed that the rest of the patients (13%) did not have enough fluid to attempt ultrasound-guided paracentesis.20
Technique
4. We recommend that ultrasound should be used to assess the characteristics of intraperitoneal free fluid to guide clinical decision making of where paracentesis can be safely performed.
Rationale. The presence and characteristics of intraperitoneal fluid collections are important determinants of whether paracentesis, another procedure, or no procedure should be performed in a given clinical scenario. One study reported that the overall diagnostic accuracy of physical examination for detecting ascites was only 58%,50 and many providers are unable to detect ascites by physical examination until 1L of fluid has accumulated. One small study showed that at least 500 ml of fluid must accumulate before shifting dullness could be detected.58 By contrast, ultrasound has been shown to reliably detect as little as 100 mL of peritoneal free fluid 52,53 and has been proven to be superior to physical examination in several studies.11,12 Therefore, ultrasound can be used to qualitatively determine whether a sufficient volume of intraperitoneal free fluid is present to safely perform paracentesis.
Studies have shown that ultrasound can also be used to differentiate ascites from other pathologies (eg, matted bowel loops, metastases, abscesses) in patients with suspected ascites on history and physical examination.16 In addition, ultrasound can help to better understand the etiology and distribution of the ascites.59-61 Sonographic measurements allow semiquantitative assessment of the volume of intraperitoneal free fluid, which may correlate with the amount of fluid removed in therapeutic paracentesis procedures.62,63 Furthermore, depth of a fluid collection by ultrasound may be an independent risk factor for the presence of spontaneous bacterial peritonitis (SBP), with one small study showing a higher risk of SBP with larger fluid collections than with small ones.64
5. We recommend that ultrasound should be used to identify a needle insertion site based on size of the fluid collection, thickness of the abdominal wall, and proximity to abdominal organs.
Rationale. When providers perform paracentesis using ultrasound guidance, any fluid collection that is directly visualized and accessible may be considered for drainage. The presence of ascites using ultrasound is best detected using a low-frequency transducer, such as phased array or curvilinear transducer, which provides deep penetration into the abdomen and pelvis to assess peritoneal free fluid.13,14,45,51,65 An optimal needle insertion site should be determined based on a combination of visualization of largest fluid collection, avoidance of underlying abdominal organs, and thickness of abdominal wall.13,31,66,67
6. We recommend the needle insertion site should be evaluated using color flow Doppler ultrasound to identify and avoid abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. The anatomy of the superficial blood vessels of the abdominal wall, especially the lateral branches, varies greatly.68-70 Although uncommon, inadvertent laceration of an inferior epigastric artery or one of its large branches is associated with significant morbidity and mortality.10,15,69,71-73 A review of 126 cases of rectus sheath hematomas, which most likely occur due to laceration of the inferior or superior epigastric artery, at a single institution from 1992 to 2002 showed a mortality rate of 1.6%, even with aggressive intervention.74 Besides the inferior epigastric arteries, several other blood vessels are at risk of injury during paracentesis, including the inferior epigastric veins, thoracoepigastric veins, subcostal artery and vein branches, deep circumflex iliac artery and vein, and recanalized subumbilical vasculature.75-77 Laceration of any of the abdominal wall blood vessels could result in catastrophic bleeding.
Identification of abdominal wall blood vessels is most commonly performed with a high-frequency transducer using color flow Doppler ultrasound.10,13-15 A low-frequency transducer capable of color flow Doppler ultrasound may be utilized in patients with a thick abdominal wall.
Studies suggest that detection of abdominal wall blood vessels with ultrasound may reduce the risk of bleeding complications. One study showed that 43% of patients had a vascular structure present at one or more of the three traditional landmark paracentesis sites.78 Another study directly compared bleeding rates between an approach utilizing a low-frequency transducer to identify the largest collection of fluid only versus a two-transducer approach utilizing both low and high-frequency transducers to identify the largest collection of fluid and evaluate for any superficial blood vessels. In this study, which included 5,777 paracenteses, paracentesis-related minor bleeding rates were similar in both groups, but major bleeding rates were less in the group utilizing color flow Doppler to evaluate for superficial vessels (0.3% vs 0.08%); differences found between groups, however, did not reach statistical significance (P = .07).79
7. We recommend that a needle insertion site should be evaluated in multiple planes to ensure clearance from underlying abdominal organs and detect any abdominal wall blood vessels along the anticipated needle trajectory.
Rationale. Most ultrasound machines have a slice thickness of <4 mm at the focal zone.80 Considering that an ultrasound beam represents a very thin 2-dimentional cross-section of the underlying tissues, visualization in only one plane could lead to inadvertent puncture of nearby critical structures such as loops of bowel or edges of solid organs. Therefore, it is important to evaluate the needle insertion site and surrounding areas in multiple planes by tilting the transducer and rotating the transducer to orthogonal planes.61 Additionally, evaluation with color flow Doppler could be performed in a similar fashion to ensure that no large blood vessels are along the anticipated needle trajectory.
8. We recommend that a needle insertion site should be marked with ultrasound immediately before performing the procedure, and the patient should remain in the same position between marking the site and performing the procedure.
Rationale. Free-flowing peritoneal fluid and abdominal organs, especially loops of small bowel, can easily shift when a patient changes position or takes a deep breath.13,16,53 Therefore, if the patient changes position or there is a delay between marking the needle insertion site and performing the procedure, the patient should be reevaluated with ultrasound to ensure that the marked needle insertion site is still safe for paracentesis.78 After marking the needle insertion site, the skin surface should be wiped completely clean of gel, and the probe should be removed from the area before sterilizing the skin surface.
9. We recommend that using real-time ultrasound guidance for paracentesis should be considered when the fluid collection is small or difficult to access.
Rationale. Use of real-time ultrasound guidance for paracentesis has been described to drain abdominal fluid collections.13,20,62 Several studies have commented that real-time ultrasound guidance for paracentesis may be necessary in obese patients, in patients with small fluid collections, or when performing the procedure near critical structures, such as loops of small bowel, liver, or spleen.57,81 Real-time ultrasound guidance for paracentesis requires additional training in needle tracking techniques and specialized equipment to maintain sterility.
Training
10. We recommend that dedicated training sessions, including didactics, supervised practice on patients, and simulation-based practice, should be used to teach novices how to perform ultrasound-guided paracentesis.
Rationale. Healthcare providers must gain multiple skills to safely perform ultrasound-guided paracentesis. Trainees must learn how to operate the ultrasound machine to identify the most appropriate needle insertion site based on the abdominal wall thickness, fluid collection size, proximity to nearby abdominal organs, and presence of blood vessels. Education regarding the use of ultrasound guidance for paracentesis is both desired 82,83 and being increasingly taught to health care providers who perform paracentesis.20,84-86
Several approaches have shown high uptake of essential skills to perform ultrasound-guided paracentesis after short training sessions. One study showed that first-year medical students can be taught to use POCUS to accurately diagnose ascites after three 30-minute teaching sessions.19 Another study showed that emergency medicine residents can achieve high levels of proficiency in the preprocedural ultrasound evaluation for paracentesis with only one hour of didactic training.20 Other studies also support the concept that adequate proficiency is achievable within brief, focused training sessions.21-28 However, these skills can decay significantly over time without ongoing education.87
11. We recommend that simulation-based practice should be used, when available, to facilitate acquisition of the required knowledge and skills to perform ultrasound-guided paracentesis.
Rationale. Simulation-based practice should be used when available, as it has been shown to increase competence in bedside diagnostic ultrasonography and procedural techniques for ultrasound-guided procedures, including paracentesis.22,25,29,88,89 One study showed that internal medicine residents were able to achieve a high level of proficiency to perform ultrasound-guided paracentesis after a three-hour simulation-based mastery learning session.88 A follow-up study suggested that, after sufficient simulation-based training, a nonradiologist can perform ultrasound-guided paracentesis as safely as an interventional radiologist.29
12. We recommend that competence in performing ultrasound-guided paracentesis should be demonstrated prior to independently performing the procedure on patients.
Rationale. Competence in ultrasound-guided paracentesis requires acquisition of clinical knowledge of paracentesis, skills in basic abdominal ultrasonography, and manual techniques to perform the procedure. Competence in ultrasound-guided paracentesis cannot be assumed for those graduating from internal medicine residency in the United States. While clinical knowledge of paracentesis remains a core competency of graduating internal medicine residents per the American Board of Internal Medicine, demonstration of competence in performing ultrasound-guided or landmark-based paracentesis is not currently mandated.90 A recent national survey of internal medicine residency program directors revealed that the curricula and resources available to train residents in bedside diagnostic ultrasound and ultrasound-guided procedures, including paracentesis, remain quite variable. 83
While it has not been well studied, competence in ultrasound for paracentesis, as with all other skills involved in bedside procedures, is likely best evaluated through direct observation on actual patients.91 As such, individualized systems to evaluate competency in ultrasound-guided paracentesis should be established for each site where it is performed. A list of consensus-derived ultrasound competencies for ultrasound-guided paracentesis has been proposed, and this list may serve as a guide for both training curriculum development and practitioner evaluation.86,91,92
KNOWLEDGE GAPS
In the process of developing these recommendations, we identified several important gaps in the literature regarding the use of ultrasound guidance for paracentesis.
First, while some data suggest that the use of ultrasound guidance for paracentesis may reduce the inpatient length of stay and overall costs, this suggestion has not been studied rigorously. In a retrospective review of 1,297 abdominal paracenteses by Patel et al., ultrasound-guided paracentesis was associated with a lower incidence of adverse events compared with landmark-based paracentesis (1.4% vs 4.7%; P = .01). The adjusted analysis from this study showed significant reductions in adverse events (OR 0.35; 95%CI 0.165-0.739; P = .006) and hospitalization costs ($8,761 ± $5,956 vs $9,848 ± $6,581; P < .001) for paracentesis with ultrasound guidance versus without such guidance. Additionally, the adjusted average length of stay was 0.2 days shorter for paracentesis with ultrasound guidance versus that without guidance (5.6 days vs 5.8 days; P < .0001).44 Similar conclusions were reached by Mercaldi et al., who conducted a retrospective study of 69,859 patients who underwent paracentesis. Fewer bleeding complications occurred when paracentesis was performed with ultrasound guidance (0.27%) versus without ultrasound guidance (1.27%). Hospitalization costs increased by $19,066 (P < .0001) and length of stay increased by 4.3 days (P < .0001) for patients when paracentesis was complicated by bleeding.43 Because both of these studies were retrospective reviews of administrative databases, associations between procedures, complications, and use of ultrasound may be limited by erroneous coding and documentation.
Second, regarding technique, it is unknown whether the use of real-time ultrasound guidance confers additional benefits compared with use of static ultrasound to mark a suitable needle insertion site. In clinical practice, real-time ultrasound guidance is used to sample small fluid collections, particularly when loops of bowel or a solid organ are nearby. It is possible that higher procedural success rates and lower complication rates may be demonstrated in these scenarios in future studies.
Third, the optimal approach to train providers to perform ultrasound-guided paracentesis is unknown. While short training sessions have shown high uptake of essential skills to perform ultrasound-guided paracentesis, data regarding the effectiveness of training using a comprehensive competency assessment are limited. Simulation-based mastery learning as a means to obtain competency for paracentesis has been described in one study,88 but the translation of competency demonstrated by simulation to actual patient outcomes has not been studied. Furthermore, the most effective method to train providers who are proficient in landmark-based paracentesis to achieve competency in ultrasound-guided paracentesis has not been well studied.
Fourth, the optimal technique for identifying blood vessels in the abdominal wall is unknown. We have proposed that color flow Doppler should be used to identify and avoid puncture of superficial vessels, but power Doppler is three times more sensitive at detecting blood vessels, especially at low velocities, such as in veins independent of direction or flow.93 Hence using power Doppler instead of color flow Doppler may further improve the ability to identify and avoid superficial vessels along the needle trajectory.92
Finally, the impact of ultrasound use on patient experience has yet to be studied. Some studies in the literature show high patient satisfaction with use of ultrasound at the bedside,94,95 but patient satisfaction with ultrasound-guided paracentesis has not been compared directly with the landmark-based technique.
CONCLUSIONS
The use of ultrasound guidance for paracentesis has been associated with higher success rates and lower complication rates. Ultrasound is superior to physical examination in assessing the presence and volume of ascites, and determining the optimal needle insertion site to avoid inadvertent injury to abdominal wall blood vessels. Hospitalists can attain competence in ultrasound-guided paracentesis through the use of various training methods, including lectures, simulation-based practice, and hands-on training. Ongoing use and training over time is necessary to maintain competence.
Acknowledgments
The authors thank all the members of the Society of Hospital Medicine Point-of-care Ultrasound Task Force and the Education Committee members for their time and dedication to develop these guidelines.
SHM Point-of-care Ultrasound Task Force: CHAIRS: Nilam Soni, Ricardo Franco Sadud, Jeff Bates. WORKING GROUPS: Thoracentesis Working Group: Ria Dancel (chair), Daniel Schnobrich, Nitin Puri. Vascular Access Working Group: Ricardo Franco (chair), Benji Matthews, Saaid Abdel-Ghani, Sophia Rodgers, Martin Perez, Daniel Schnobrich. Paracentesis Working Group: Joel Cho (chair), Benji Mathews, Kreegan Reierson, Anjali Bhagra, Trevor P. Jensen. Lumbar Puncture Working Group: Nilam J. Soni (chair), Ricardo Franco, Gerard Salame, Josh Lenchus, Venkat Kalidindi, Ketino Kobaidze. Credentialing Working Group: Brian P Lucas (chair), David Tierney, Trevor P. Jensen PEER REVIEWERS: Robert Arntfield, Michael Blaivas, Richard Hoppmann, Paul Mayo, Vicki Noble, Aliaksei Pustavoitau, Kirk Spencer, Vivek Tayal. METHODOLOGIST: Mahmoud El Barbary. LIBRARIAN: Loretta Grikis. SOCIETY OF HOSPITAL MEDICINE EDUCATION COMMITTEE: Daniel Brotman (past chair), Satyen Nichani (current chair), Susan Hunt. SOCIETY OF HOSPITAL MEDICINE STAFF: Nick Marzano.
Collaborators of the Society of Hospital Medicine Point-of-care Ultrasound Task Force
Saaid Abdel-Ghani, Robert Arntfield, Jeffrey Bates, Michael Blaivas, Dan Brotman, Carolina Candotti, Richard Hoppmann, Susan Hunt, Venkat Kalidindi, Ketino Kobaidze, Josh Lenchus, Paul Mayo, Satyen Nichani, Vicki Noble, Martin Perez, Nitin Puri, Aliaksei Pustavoitau, Sophia Rodgers, Gerard Salame, Daniel Schnobrich, Kirk Spencer, Vivek Tayal, David M. Tierney
Disclaimer
The contents of this publication do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
All 5 appendices are viewable online at https://www.journalofhospitalmedicine.com.
1. Duszak R, Jr., Chatterjee AR, Schneider DA. National fluid shifts: fifteen-year trends in paracentesis and thoracentesis procedures. J Am Coll Radiol. 2010;7(11):859-864. doi: 10.1016/j.jacr.2010.04.013.
2. O’Brien CR, Chang J, Campos RA, et al. Characterizing the safety of paracentesis in hospitalized patients with cirrhosis and ascites from 2004-2012 in the United States. Gastroenterology. 2016;150(4). https:/doi.org /10.1016/S0016-5085(16)32196-5.
3. Gaetano JN, Micic D, Aronsohn A, et al. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. J Gastroenterol Hepatol. 2016;31(5):1025-1030. doi: 10.1016/S0016-5085(16)32196-5
4. Orman ES, Hayashi PH, Bataller R, Barritt AS. Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites. Clin Gastroenterol Hepatol. 2014;12(3):496-503.e1. doi: 10.1016/j.cgh.2013.08.025.
5. Mallory A, Schaefer JW. Complications of diagnostic paracentesis in patients with liver disease. JAMA. 1978;239(7):628-630. doi: 10.1001/jama.1978.03280340048020.
6. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005;21(5):525-529. doi: 10.1111/j.1365-2036.2005.02387.x.
7. Shekhar C, Ramakrishnan A, Claridge LC. Paracentesis: UK trainees’ practice, experience and attitudes. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.096.
8. De Gottardi A, Thevenot T, Spahr L, et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7(8):906-909. doi: 10.1016/j.cgh.2009.05.004.
9. Sharzehi K, Jain V, Naveed A, Schreibman I. Hemorrhagic complications of paracentesis: a systematic review of the literature. Gastroenterol Res Pract. 2014;2014:985141. doi: 10.1155/2014/985141.
10. Sekiguchi H, Suzuki J, Daniels CE. Making paracentesis safer: a proposal for the use of bedside abdominal and vascular ultrasonography to prevent a fatal complication. Chest. 2013;143(4):1136-1139. doi: 10.1378/chest.12-0871.
11. Soyuncu S, Cete Y, Bozan H, Kartal M, Akyol AJ. Accuracy of physical and ultrasonographic examinations by emergency physicians for the early diagnosis of intraabdominal haemorrhage in blunt abdominal trauma. Injury. 2007;38(5):564-569. doi: 10.1016/j.injury.2007.01.010.
12. Chongtham DS, Singh MM, Kalantri SP, Pathak S, Jain AP. Accuracy of clinical manoeuvres in detection of minimal ascites. Indian J Med Sci. 1998;52(11):514-520.
13. Ennis J, Schultz G, Perera P, Williams S, Gharahbaghian L, Mandavia D. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293. doi: 10.4236/ijcm.2014.520163.
14. Szabo TL, Lewin PA. Ultrasound transducer selection in clinical imaging practice. J Ultrasound Med. 2013;32(4):573-582. doi: 10.7863/jum.2013.32.4.573.
15. Stone JC, Moak JH. Feasibility of sonographic localization of the inferior epigastric artery before ultrasound-guided paracentesis. Am J Emerg Med. 2015;33(12):1795-1798. doi: 10.1016/j.ajem.2015.06.067.
16. Yeh HC, Wolf BS. Ultrasonography in ascites. Radiology. 1977;124(3):783-790. doi: 10.1148/124.3.783.
17. Lucas BP, Asbury JK, Wang Y, et al. Impact of a bedside procedure service on general medicine inpatients: a firm-based trial. J Hosp Med. 2007;2(3):143-149. doi: 10.1002/jhm.159.
18. Kim JJ, Tsukamoto MM, Mathur AK, et al. Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis. Am J Gastroenterol. 2014;109(9):1436-1442. doi: 10.1038/ajg.2014.212.
19. Arora S, Cheung A, Tarique U, Agarwal A, Firdouse M, Ailon J. First-year medical students use of ultrasound or physical examination to diagnose hepatomegaly and ascites: a randomized controlled trial. J Ultrasound. 2017;20(3):199-204. doi: 10.1007/s40477-017-0261-6.
20. Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005;23(3):363-367. doi: 10.1016/j.ajem.2004.11.001.
21. Kotagal M, Quiroga E, Ruffatto BJ, et al. Impact of point-of-care ultrasound training on surgical residents’ confidence. J Surg Educ. 2015;72(4):e82-87. doi: 10.1016/j.jsurg.2015.01.021.
22. Martin R, Gannon D, Riggle J, et al. A comprehensive workshop using simulation to train internal medicine residents in bedside procedures performed by internists. Chest. 2012;142(4):545A. doi: 10.1378/chest.1390093.
23. Quddus A, Minami T, Summerhill E. Impact of a short 3-hour ultrasound training workshop for internal medicine residents. Chest. 2014;146(4): 509A. doi: 10.1378/chest.1989267.
24. Lanoix R, Leak LV, Gaeta T, Gernsheimer JR. A preliminary evaluation of emergency ultrasound in the setting of an emergency medicine training program. Am J Emerg Med. 2000;18(1):41-45. doi: 10.1016/S0735-6757(00)90046-9.
25. Dulohery MM, Eaton J, Tajouri T, Bhagra A. Ultrasound for internal medicine physicians: the future of physical exam. J Ultrasound Med. 2014;33(6):1005-1011. doi: 10.7863/ultra.33.6.1005
26. Lanoix R, Baker WE, Mele JM, Dharmarajan L. Evaluation of an instructional model for emergency ultrasonography. Acad Emerg Med. 1998;5(1):58-63. doi: 10.1111/j.1553-2712.1998.tb02576.x.
27. Terkamp C, Kirchner G, Wedemeyer J, et al. Simulation of abdomen sonography. Evaluation of a new ultrasound simulator. Ultraschall Med. 2003;24(4):239-234. doi: 10.1055/s-2003-41713.
28. Barsuk JH, Cohen ER, Potts S, et al. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23(9):749-756. doi: 10.1136/bmjqs-2013-002665.
29. Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126(4):349-356. doi: 10.1016/j.amjmed.2012.09.016.
30. Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User’s Manual. Santa Monica, CA: Rand Corp.; 2001.
31. Bard C, Lafortune M, Breton G. Ascites: ultrasound guidance or blind paracentesis? CMAJ. 1986;135(3):209-210. doi: 10.1016/0736-4679(87)90268-X.
32. Sudulagunta SR, Sodalagunta MB, Bangalore Raja SK, Khorram H, Sepehrar M, Noroozpour Z. Clinical profile and complications of paracentesis in refractory ascites patients with cirrhosis. Gastroenterol Res. 2015;8(3-4):228-233. doi: 10.14740/gr661w.
33. Lin S, Wang M, Zhu Y, et al. Hemorrhagic complications following abdominal paracentesis in acute on chronic liver failure: a propensity score analysis. Medicine (Baltimore). 2015;94(49):e2225. doi: 10.1097/MD.0000000000002225.
34. Lam EY, McLafferty RB, Taylor LM, Jr., et al. Inferior epigastric artery pseudoaneurysm: a complication of paracentesis. J Vasc Surg. 1998;28(3):566-569. doi: 10.1016/S0741-5214(98)70147-8.
35. Cervini P, Hesley GK, Thompson RL, Sampathkumar P, Knudsen JM. Incidence of infectious complications after an ultrasound-guided intervention. AJR Am J Roentgenol. 2010;195(4):846-850. doi: 10.2214/AJR.09.3168.
36. Wiese SS, Mortensen C, Bendtsen F. Few complications after paracentesis in patients with cirrhosis and refractory ascites. Dan Med Bull. 2011;58(1):A4212.
37. Jakobson DJ, Shemesh I. Merging ultrasound in the intensive care routine. Isr Med Assoc J. 2013;15(11):688-692.
38. Landers A, Ryan B. The use of bedside ultrasound and community-based paracentesis in a palliative care service. J Prim Health Care. 2014;6(2):148-151.
39. Lin CH, Shih FY, Ma MH, Chiang WC, Yang CW, Ko PC. Should bleeding tendency deter abdominal paracentesis? Dig Liver Dis. 2005;37(12):946-951. doi: 10.1016/j.dld.2005.07.009.
40. Kurup AN, Lekah A, Reardon ST, et al. Bleeding rate for ultrasound-guided paracentesis in thrombocytopenic patients. J Ultrasound Med. 2015;34(10):1833-1838. doi: 10.7863/ultra.14.10034.
41. Reardon S, Atwell TD, Lekah A. Major bleeding complication rate of ultrasound-guided paracentesis in thrombocytopenic patients. J Vasc Interv Radiol. 2013;24(4):S56. doi: 10.1016/j.jvir.2013.01.129.
42. Czul F, Prager M, Lenchus J. Intra-procedural risk of bleeding associated with ultrasound guided paracentesis in patients with abnormal coagulation studies: 1907. Hepatology. 2011;54(4):1259A.
43. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532-538. doi: 10.1378/chest.12-0447.
44. Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012;15(1):1-7. doi: 10.3111/13696998.2011.628723.
45. Nicolaou S, Talsky A, Khashoggi K, Venu V. Ultrasound-guided interventional radiology in critical care. Crit Care Med. 2007;35(5 Suppl):S186-197. doi: 10.1097/01.CCM.0000260630.68855.DF.
46. Conduit B, Wesley E, Christie J, Thalheimer U. PTU-002 Large volume paracentesis (LVP) can be safely performed by junior doctors without ultrasound guidance. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.095.
47. Williams JW, Jr., Simel DL. The rational clinical examination. Does this patient have ascites? How to divine fluid in the abdomen. JAMA. 1992;267(19):2645-2648. doi: 10.1001/jama.1992.03480190087038.
48. Rodriguez A, DuPriest RW, Jr., Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457-459.
49. McGibbon A, Chen GI, Peltekian KM, van Zanten SV. An evidence-based manual for abdominal paracentesis. Dig Dis Sci. 2007;52(12):3307-3315. doi: 10.1007/s10620-007-9805-5.
50. Cattau EL, Jr., Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247(8):1164-1166. doi: 10.1001/jama.1982.03320330060027.
51. Ali J, Rozycki GS, Campbell JP, Boulanger BR, Waddell JP, Gana TJ. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res. 1996;63(1):275-279. doi: 10.1006/jsre.1996.0260.
52. Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003;21(6):476-478. doi: 10.1016/S0735-6757(03)00162-1
53. Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22. doi: 10.1148/96.1.15.
54. Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39(2):375-380. doi: 10.1016/0736-4679(96)84805-0.
55. Paajanen H, Lahti P, Nordback I. Sensitivity of transabdominal ultrasonography in detection of intraperitoneal fluid in humans. Eur Radiol. 1999;9(7):1423-1425. doi: 10.1007/s003300050861.
56. Prabhakar A, Thabet A, Mueller P, Gee MS. Image-guided peritoneal access for fluid infusion in oncology patients: Indications, technique, and outcomes. J Vasc Interv Radiol. 2014;25(3):S41. doi: 10.1016/j.jvir.2013.12.100.
57. McGahan JP, Anderson MW, Walter JP. Portable real-time sonographic and needle guidance systems for aspiration and drainage. AJR Am J Roentgenol. 1986;147(6):1241-1246. doi: 10.2214/ajr.147.6.1241.
58. Moses WR. Shifting dullness in the abdomen. South Med J. 1946;39(12):985-987.
59. Edell SL, Gefter WB. Ultrasonic differentiation of types of ascitic fluid. AJR Am J Roentgenol. 1979;133(1):111-114. doi: 10.2214/ajr.133.1.111.
60. Doust BD, Thompson R. Ultrasonography of abdominal fluid collections. Gastrointest Radiol. 1978;3(3):273-279. doi: 10.1007/BF01887079.
61. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 2. Chest. 2005;128(3):1766-1781. doi: 10.1378/chest.128.3.1766.
62. Irshad A, Ackerman SJ, Anis M, Campbell AS, Hashmi A, Baker NL. Can the smallest depth of ascitic fluid on sonograms predict the amount of drainable fluid? J Clin Ultrasound. 2009;37(8):440-444. doi: 10.1002/jcu.20616.
63. Inadomi J, Cello JP, Koch J. Ultrasonographic determination of ascitic volume. Hepatology. 1996;24(3):549-551. doi: 10.1002/hep.510240314.
64. Sideris A, Patel P, Charles HW, Park J, Feldman D, Deipolyi AR. Imaging and clinical predictors of spontaneous bacterial peritonitis diagnosed by ultrasound-guided paracentesis. Proc (Bayl Univ Med Cent). 2017;30(3):262-264. https://doi.org/10.1080/08998280.2017.11929610
65. Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014;30(2):305-329. doi: 10.1016/j.ccc.2013.10.005.
66. Ross GJ, Kessler HB, Clair MR, Gatenby RA, Hartz WH, Ross LV. Sonographically guided paracentesis for palliation of symptomatic malignant ascites. AJR Am J Roentgenol. 1989;153(6):1309-1311. doi: 10.2214/ajr.153.6.1309.
67. Russell KW, Mone MC, Scaife CL. Umbilical paracentesis for acute hernia reduction in cirrhotic patients. BMJ Case Rep. 2013;2013. doi: 10.1136/bcr-2013-201304.
68. Epstein J, Arora A, Ellis H. Surface anatomy of the inferior epigastric artery in relation to laparoscopic injury. Clin Anat. 2004;17(5):400-408. doi: 10.1002/ca.10192.
69. Suzuki J, Sekiguchi H. Laceration of inferior epigastric artery resulting in abdominal compartment syndrome: a fatal complication of paracentesis. Am J Respir Crit Care Med. 2012;185:A5974. doi: 10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5974
70. Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg. 2004;239(2):182-185. doi: 10.1097/01.sla.0000109151.53296.07.
71. Webster ST, Brown KL, Lucey MR, Nostrant TT. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol. 1996;91(2):366-368.
72. Todd AW. Inadvertent puncture of the inferior epigastric artery during needle biopsy with fatal outcome. Clin Radiol. 2001;56(12):989-990. doi: 10.1053/crad.2001.0175.
73. Seidler M, Sayegh K, Roy A, Mesurolle B. A fatal complication of ultrasound-guided abdominal paracentesis. J Clin Ultrasound. 2013;41(7):457-460. doi: 10.1002/jcu.22050.
74. Cherry WB, Mueller PS. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore). 2006;85(2):105-110. doi: 10.1097/01.md.0000216818.13067.5a.
75. Oelsner DH, Caldwell SH, Coles M, Driscoll CJ. Subumbilical midline vascularity of the abdominal wall in portal hypertension observed at laparoscopy. Gastrointest Endosc. 1998;47(5):388-390. doi: 10.1016/S0016-5107(98)70224-X.
76. Krupski WC, Sumchai A, Effeney DJ, Ehrenfeld WK. The importance of abdominal wall collateral blood vessels. Planning incisions and obtaining arteriography. Arch Surg. 1984;119(7):854-857. doi: 10.1001/archsurg.1984.01390190092021.
77. Rozen WM, Ashton MW, Taylor GI. Reviewing the vascular supply of the anterior abdominal wall: redefining anatomy for increasingly refined surgery. Clin Anat. 2008;21(2):89-98. doi: 10.1002/ca.20585.
78. Adams A, Roggio A, Wilkerson RG. 368 Sonographic assessment of inadvertent vascular puncture during paracentesis using the traditional landmark approach. Ann Emerg Med. 2015;66:S132-S133. doi: 10.1016/j.annemergmed.2015.07.404
79. Barsuk JH, Rosen BT, Cohen ER, Feinglass J, Ault MJ. Vascular ultrasonography: a novel method to reduce paracentesis related major bleeding. J Hosp Med. 2018;13(1):30-33. doi: 10.12788/jhm.2863.
80. Skolnick ML. Estimation of ultrasound beam width in the elevation (section thickness) plane. Radiology. 1991;180(1):286-288. doi: 10.1148/radiology.180.1.2052713.
81. Keil-Rios D, Terrazas-Solis H, Gonzalez-Garay A, Sanchez-Avila JF, Garcia-Juarez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. doi: 10.1007/s11739-016-1406-x.
82. Kessler C, Bhandarkar S. Ultrasound training for medical students and internal medicine residents--a needs assessment. J Clin Ultrasound. 2010;38(8):401-408. doi: 10.1002/jcu.20719.
83. Schnobrich DJ, Gladding S, Olson AP, Duran-Nelson A. Point-of-care ultrasound in internal medicine: a national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. doi: 10.4300/JGME-D-12-00215.1.
84. Eisen LA, Leung S, Gallagher AE, Kvetan V. Barriers to ultrasound training in critical care medicine fellowships: a survey of program directors. Crit Care Med. 2010;38(10):1978-1983. doi: 10.1097/CCM.0b013e3181eeda53.
85. Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med. 2007;35(5 Suppl):S290-304. doi: 10.1097/01.CCM.0000260680.16213.26.
86. Ma I, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. doi: 10.1007/s11606-017-4071-5.
87. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi: 10.4300/JGME-14-00284.1.
88. Barsuk JH, Cohen ER, Vozenilek JA, O’Connor LM, McGaghie WC, Wayne DB. Simulation-based education with mastery learning improves paracentesis skills. J Grad Med Educ. 2012;4(1):23-27. doi: 10.4300/JGME-D-11-00161.1.
89. Lenchus JD. End of the “see one, do one, teach one” era: the next generation of invasive bedside procedural instruction. J Am Osteopath Assoc. 2010;110(6):340-346. doi: 10.7556/jaoa.2010.110.6.340.
90. American Board of Internal Medicine. Policies and Procedures for Certification. Philadelphia, PA: ABIM; 2006.
91. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. doi: 10.12788/jhm.2917.
92. Brown GM, Otremba M, Devine LA, Gray C, Millington SJ, Ma IW. Defining competencies for ultrasound-guided bedside procedures: consensus opinions from Canadian physicians. J Ultrasound Med. 2016;35(1):129-141. doi: 10.7863/ultra.15.01063.
93. Babcock DS, Patriquin H, LaFortune M, Dauzat M. Power doppler sonography: basic principles and clinical applications in children. Pediatr Radiol. 1996;26(2):109-115. doi: 10.1007/BF01372087.
94. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. doi: 10.1016/j.jemermed.2013.05.044.
95. Lindelius A, Torngren S, Nilsson L, Pettersson H, Adami J. Randomized clinical trial of bedside ultrasound among patients with abdominal pain in the emergency department: impact on patient satisfaction and health care consumption. Scand J Trauma Resusc Emerg Med. 2009;17:60. doi: 10.1186/1757-7241-17-60.
1. Duszak R, Jr., Chatterjee AR, Schneider DA. National fluid shifts: fifteen-year trends in paracentesis and thoracentesis procedures. J Am Coll Radiol. 2010;7(11):859-864. doi: 10.1016/j.jacr.2010.04.013.
2. O’Brien CR, Chang J, Campos RA, et al. Characterizing the safety of paracentesis in hospitalized patients with cirrhosis and ascites from 2004-2012 in the United States. Gastroenterology. 2016;150(4). https:/doi.org /10.1016/S0016-5085(16)32196-5.
3. Gaetano JN, Micic D, Aronsohn A, et al. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. J Gastroenterol Hepatol. 2016;31(5):1025-1030. doi: 10.1016/S0016-5085(16)32196-5
4. Orman ES, Hayashi PH, Bataller R, Barritt AS. Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites. Clin Gastroenterol Hepatol. 2014;12(3):496-503.e1. doi: 10.1016/j.cgh.2013.08.025.
5. Mallory A, Schaefer JW. Complications of diagnostic paracentesis in patients with liver disease. JAMA. 1978;239(7):628-630. doi: 10.1001/jama.1978.03280340048020.
6. Pache I, Bilodeau M. Severe haemorrhage following abdominal paracentesis for ascites in patients with liver disease. Aliment Pharmacol Ther. 2005;21(5):525-529. doi: 10.1111/j.1365-2036.2005.02387.x.
7. Shekhar C, Ramakrishnan A, Claridge LC. Paracentesis: UK trainees’ practice, experience and attitudes. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.096.
8. De Gottardi A, Thevenot T, Spahr L, et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol. 2009;7(8):906-909. doi: 10.1016/j.cgh.2009.05.004.
9. Sharzehi K, Jain V, Naveed A, Schreibman I. Hemorrhagic complications of paracentesis: a systematic review of the literature. Gastroenterol Res Pract. 2014;2014:985141. doi: 10.1155/2014/985141.
10. Sekiguchi H, Suzuki J, Daniels CE. Making paracentesis safer: a proposal for the use of bedside abdominal and vascular ultrasonography to prevent a fatal complication. Chest. 2013;143(4):1136-1139. doi: 10.1378/chest.12-0871.
11. Soyuncu S, Cete Y, Bozan H, Kartal M, Akyol AJ. Accuracy of physical and ultrasonographic examinations by emergency physicians for the early diagnosis of intraabdominal haemorrhage in blunt abdominal trauma. Injury. 2007;38(5):564-569. doi: 10.1016/j.injury.2007.01.010.
12. Chongtham DS, Singh MM, Kalantri SP, Pathak S, Jain AP. Accuracy of clinical manoeuvres in detection of minimal ascites. Indian J Med Sci. 1998;52(11):514-520.
13. Ennis J, Schultz G, Perera P, Williams S, Gharahbaghian L, Mandavia D. Ultrasound for detection of ascites and for guidance of the paracentesis procedure: technique and review of the literature. Int J Clin Med. 2014;5:1277-1293. doi: 10.4236/ijcm.2014.520163.
14. Szabo TL, Lewin PA. Ultrasound transducer selection in clinical imaging practice. J Ultrasound Med. 2013;32(4):573-582. doi: 10.7863/jum.2013.32.4.573.
15. Stone JC, Moak JH. Feasibility of sonographic localization of the inferior epigastric artery before ultrasound-guided paracentesis. Am J Emerg Med. 2015;33(12):1795-1798. doi: 10.1016/j.ajem.2015.06.067.
16. Yeh HC, Wolf BS. Ultrasonography in ascites. Radiology. 1977;124(3):783-790. doi: 10.1148/124.3.783.
17. Lucas BP, Asbury JK, Wang Y, et al. Impact of a bedside procedure service on general medicine inpatients: a firm-based trial. J Hosp Med. 2007;2(3):143-149. doi: 10.1002/jhm.159.
18. Kim JJ, Tsukamoto MM, Mathur AK, et al. Delayed paracentesis is associated with increased in-hospital mortality in patients with spontaneous bacterial peritonitis. Am J Gastroenterol. 2014;109(9):1436-1442. doi: 10.1038/ajg.2014.212.
19. Arora S, Cheung A, Tarique U, Agarwal A, Firdouse M, Ailon J. First-year medical students use of ultrasound or physical examination to diagnose hepatomegaly and ascites: a randomized controlled trial. J Ultrasound. 2017;20(3):199-204. doi: 10.1007/s40477-017-0261-6.
20. Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med. 2005;23(3):363-367. doi: 10.1016/j.ajem.2004.11.001.
21. Kotagal M, Quiroga E, Ruffatto BJ, et al. Impact of point-of-care ultrasound training on surgical residents’ confidence. J Surg Educ. 2015;72(4):e82-87. doi: 10.1016/j.jsurg.2015.01.021.
22. Martin R, Gannon D, Riggle J, et al. A comprehensive workshop using simulation to train internal medicine residents in bedside procedures performed by internists. Chest. 2012;142(4):545A. doi: 10.1378/chest.1390093.
23. Quddus A, Minami T, Summerhill E. Impact of a short 3-hour ultrasound training workshop for internal medicine residents. Chest. 2014;146(4): 509A. doi: 10.1378/chest.1989267.
24. Lanoix R, Leak LV, Gaeta T, Gernsheimer JR. A preliminary evaluation of emergency ultrasound in the setting of an emergency medicine training program. Am J Emerg Med. 2000;18(1):41-45. doi: 10.1016/S0735-6757(00)90046-9.
25. Dulohery MM, Eaton J, Tajouri T, Bhagra A. Ultrasound for internal medicine physicians: the future of physical exam. J Ultrasound Med. 2014;33(6):1005-1011. doi: 10.7863/ultra.33.6.1005
26. Lanoix R, Baker WE, Mele JM, Dharmarajan L. Evaluation of an instructional model for emergency ultrasonography. Acad Emerg Med. 1998;5(1):58-63. doi: 10.1111/j.1553-2712.1998.tb02576.x.
27. Terkamp C, Kirchner G, Wedemeyer J, et al. Simulation of abdomen sonography. Evaluation of a new ultrasound simulator. Ultraschall Med. 2003;24(4):239-234. doi: 10.1055/s-2003-41713.
28. Barsuk JH, Cohen ER, Potts S, et al. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23(9):749-756. doi: 10.1136/bmjqs-2013-002665.
29. Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126(4):349-356. doi: 10.1016/j.amjmed.2012.09.016.
30. Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA Appropriateness Method User’s Manual. Santa Monica, CA: Rand Corp.; 2001.
31. Bard C, Lafortune M, Breton G. Ascites: ultrasound guidance or blind paracentesis? CMAJ. 1986;135(3):209-210. doi: 10.1016/0736-4679(87)90268-X.
32. Sudulagunta SR, Sodalagunta MB, Bangalore Raja SK, Khorram H, Sepehrar M, Noroozpour Z. Clinical profile and complications of paracentesis in refractory ascites patients with cirrhosis. Gastroenterol Res. 2015;8(3-4):228-233. doi: 10.14740/gr661w.
33. Lin S, Wang M, Zhu Y, et al. Hemorrhagic complications following abdominal paracentesis in acute on chronic liver failure: a propensity score analysis. Medicine (Baltimore). 2015;94(49):e2225. doi: 10.1097/MD.0000000000002225.
34. Lam EY, McLafferty RB, Taylor LM, Jr., et al. Inferior epigastric artery pseudoaneurysm: a complication of paracentesis. J Vasc Surg. 1998;28(3):566-569. doi: 10.1016/S0741-5214(98)70147-8.
35. Cervini P, Hesley GK, Thompson RL, Sampathkumar P, Knudsen JM. Incidence of infectious complications after an ultrasound-guided intervention. AJR Am J Roentgenol. 2010;195(4):846-850. doi: 10.2214/AJR.09.3168.
36. Wiese SS, Mortensen C, Bendtsen F. Few complications after paracentesis in patients with cirrhosis and refractory ascites. Dan Med Bull. 2011;58(1):A4212.
37. Jakobson DJ, Shemesh I. Merging ultrasound in the intensive care routine. Isr Med Assoc J. 2013;15(11):688-692.
38. Landers A, Ryan B. The use of bedside ultrasound and community-based paracentesis in a palliative care service. J Prim Health Care. 2014;6(2):148-151.
39. Lin CH, Shih FY, Ma MH, Chiang WC, Yang CW, Ko PC. Should bleeding tendency deter abdominal paracentesis? Dig Liver Dis. 2005;37(12):946-951. doi: 10.1016/j.dld.2005.07.009.
40. Kurup AN, Lekah A, Reardon ST, et al. Bleeding rate for ultrasound-guided paracentesis in thrombocytopenic patients. J Ultrasound Med. 2015;34(10):1833-1838. doi: 10.7863/ultra.14.10034.
41. Reardon S, Atwell TD, Lekah A. Major bleeding complication rate of ultrasound-guided paracentesis in thrombocytopenic patients. J Vasc Interv Radiol. 2013;24(4):S56. doi: 10.1016/j.jvir.2013.01.129.
42. Czul F, Prager M, Lenchus J. Intra-procedural risk of bleeding associated with ultrasound guided paracentesis in patients with abnormal coagulation studies: 1907. Hepatology. 2011;54(4):1259A.
43. Mercaldi CJ, Lanes SF. Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis. Chest. 2013;143(2):532-538. doi: 10.1378/chest.12-0447.
44. Patel PA, Ernst FR, Gunnarsson CL. Evaluation of hospital complications and costs associated with using ultrasound guidance during abdominal paracentesis procedures. J Med Econ. 2012;15(1):1-7. doi: 10.3111/13696998.2011.628723.
45. Nicolaou S, Talsky A, Khashoggi K, Venu V. Ultrasound-guided interventional radiology in critical care. Crit Care Med. 2007;35(5 Suppl):S186-197. doi: 10.1097/01.CCM.0000260630.68855.DF.
46. Conduit B, Wesley E, Christie J, Thalheimer U. PTU-002 Large volume paracentesis (LVP) can be safely performed by junior doctors without ultrasound guidance. Gut. 2013;62:A42. doi: 10.1136/gutjnl-2013-304907.095.
47. Williams JW, Jr., Simel DL. The rational clinical examination. Does this patient have ascites? How to divine fluid in the abdomen. JAMA. 1992;267(19):2645-2648. doi: 10.1001/jama.1992.03480190087038.
48. Rodriguez A, DuPriest RW, Jr., Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457-459.
49. McGibbon A, Chen GI, Peltekian KM, van Zanten SV. An evidence-based manual for abdominal paracentesis. Dig Dis Sci. 2007;52(12):3307-3315. doi: 10.1007/s10620-007-9805-5.
50. Cattau EL, Jr., Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982;247(8):1164-1166. doi: 10.1001/jama.1982.03320330060027.
51. Ali J, Rozycki GS, Campbell JP, Boulanger BR, Waddell JP, Gana TJ. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res. 1996;63(1):275-279. doi: 10.1006/jsre.1996.0260.
52. Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003;21(6):476-478. doi: 10.1016/S0735-6757(03)00162-1
53. Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22. doi: 10.1148/96.1.15.
54. Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39(2):375-380. doi: 10.1016/0736-4679(96)84805-0.
55. Paajanen H, Lahti P, Nordback I. Sensitivity of transabdominal ultrasonography in detection of intraperitoneal fluid in humans. Eur Radiol. 1999;9(7):1423-1425. doi: 10.1007/s003300050861.
56. Prabhakar A, Thabet A, Mueller P, Gee MS. Image-guided peritoneal access for fluid infusion in oncology patients: Indications, technique, and outcomes. J Vasc Interv Radiol. 2014;25(3):S41. doi: 10.1016/j.jvir.2013.12.100.
57. McGahan JP, Anderson MW, Walter JP. Portable real-time sonographic and needle guidance systems for aspiration and drainage. AJR Am J Roentgenol. 1986;147(6):1241-1246. doi: 10.2214/ajr.147.6.1241.
58. Moses WR. Shifting dullness in the abdomen. South Med J. 1946;39(12):985-987.
59. Edell SL, Gefter WB. Ultrasonic differentiation of types of ascitic fluid. AJR Am J Roentgenol. 1979;133(1):111-114. doi: 10.2214/ajr.133.1.111.
60. Doust BD, Thompson R. Ultrasonography of abdominal fluid collections. Gastrointest Radiol. 1978;3(3):273-279. doi: 10.1007/BF01887079.
61. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 2. Chest. 2005;128(3):1766-1781. doi: 10.1378/chest.128.3.1766.
62. Irshad A, Ackerman SJ, Anis M, Campbell AS, Hashmi A, Baker NL. Can the smallest depth of ascitic fluid on sonograms predict the amount of drainable fluid? J Clin Ultrasound. 2009;37(8):440-444. doi: 10.1002/jcu.20616.
63. Inadomi J, Cello JP, Koch J. Ultrasonographic determination of ascitic volume. Hepatology. 1996;24(3):549-551. doi: 10.1002/hep.510240314.
64. Sideris A, Patel P, Charles HW, Park J, Feldman D, Deipolyi AR. Imaging and clinical predictors of spontaneous bacterial peritonitis diagnosed by ultrasound-guided paracentesis. Proc (Bayl Univ Med Cent). 2017;30(3):262-264. https://doi.org/10.1080/08998280.2017.11929610
65. Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014;30(2):305-329. doi: 10.1016/j.ccc.2013.10.005.
66. Ross GJ, Kessler HB, Clair MR, Gatenby RA, Hartz WH, Ross LV. Sonographically guided paracentesis for palliation of symptomatic malignant ascites. AJR Am J Roentgenol. 1989;153(6):1309-1311. doi: 10.2214/ajr.153.6.1309.
67. Russell KW, Mone MC, Scaife CL. Umbilical paracentesis for acute hernia reduction in cirrhotic patients. BMJ Case Rep. 2013;2013. doi: 10.1136/bcr-2013-201304.
68. Epstein J, Arora A, Ellis H. Surface anatomy of the inferior epigastric artery in relation to laparoscopic injury. Clin Anat. 2004;17(5):400-408. doi: 10.1002/ca.10192.
69. Suzuki J, Sekiguchi H. Laceration of inferior epigastric artery resulting in abdominal compartment syndrome: a fatal complication of paracentesis. Am J Respir Crit Care Med. 2012;185:A5974. doi: 10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A5974
70. Saber AA, Meslemani AM, Davis R, Pimentel R. Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg. 2004;239(2):182-185. doi: 10.1097/01.sla.0000109151.53296.07.
71. Webster ST, Brown KL, Lucey MR, Nostrant TT. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol. 1996;91(2):366-368.
72. Todd AW. Inadvertent puncture of the inferior epigastric artery during needle biopsy with fatal outcome. Clin Radiol. 2001;56(12):989-990. doi: 10.1053/crad.2001.0175.
73. Seidler M, Sayegh K, Roy A, Mesurolle B. A fatal complication of ultrasound-guided abdominal paracentesis. J Clin Ultrasound. 2013;41(7):457-460. doi: 10.1002/jcu.22050.
74. Cherry WB, Mueller PS. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore). 2006;85(2):105-110. doi: 10.1097/01.md.0000216818.13067.5a.
75. Oelsner DH, Caldwell SH, Coles M, Driscoll CJ. Subumbilical midline vascularity of the abdominal wall in portal hypertension observed at laparoscopy. Gastrointest Endosc. 1998;47(5):388-390. doi: 10.1016/S0016-5107(98)70224-X.
76. Krupski WC, Sumchai A, Effeney DJ, Ehrenfeld WK. The importance of abdominal wall collateral blood vessels. Planning incisions and obtaining arteriography. Arch Surg. 1984;119(7):854-857. doi: 10.1001/archsurg.1984.01390190092021.
77. Rozen WM, Ashton MW, Taylor GI. Reviewing the vascular supply of the anterior abdominal wall: redefining anatomy for increasingly refined surgery. Clin Anat. 2008;21(2):89-98. doi: 10.1002/ca.20585.
78. Adams A, Roggio A, Wilkerson RG. 368 Sonographic assessment of inadvertent vascular puncture during paracentesis using the traditional landmark approach. Ann Emerg Med. 2015;66:S132-S133. doi: 10.1016/j.annemergmed.2015.07.404
79. Barsuk JH, Rosen BT, Cohen ER, Feinglass J, Ault MJ. Vascular ultrasonography: a novel method to reduce paracentesis related major bleeding. J Hosp Med. 2018;13(1):30-33. doi: 10.12788/jhm.2863.
80. Skolnick ML. Estimation of ultrasound beam width in the elevation (section thickness) plane. Radiology. 1991;180(1):286-288. doi: 10.1148/radiology.180.1.2052713.
81. Keil-Rios D, Terrazas-Solis H, Gonzalez-Garay A, Sanchez-Avila JF, Garcia-Juarez I. Pocket ultrasound device as a complement to physical examination for ascites evaluation and guided paracentesis. Intern Emerg Med. 2016;11(3):461-466. doi: 10.1007/s11739-016-1406-x.
82. Kessler C, Bhandarkar S. Ultrasound training for medical students and internal medicine residents--a needs assessment. J Clin Ultrasound. 2010;38(8):401-408. doi: 10.1002/jcu.20719.
83. Schnobrich DJ, Gladding S, Olson AP, Duran-Nelson A. Point-of-care ultrasound in internal medicine: a national survey of educational leadership. J Grad Med Educ. 2013;5(3):498-502. doi: 10.4300/JGME-D-12-00215.1.
84. Eisen LA, Leung S, Gallagher AE, Kvetan V. Barriers to ultrasound training in critical care medicine fellowships: a survey of program directors. Crit Care Med. 2010;38(10):1978-1983. doi: 10.1097/CCM.0b013e3181eeda53.
85. Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med. 2007;35(5 Suppl):S290-304. doi: 10.1097/01.CCM.0000260680.16213.26.
86. Ma I, Arishenkoff S, Wiseman J, et al. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32(9):1052-1057. doi: 10.1007/s11606-017-4071-5.
87. Kelm D, Ratelle J, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454-457. doi: 10.4300/JGME-14-00284.1.
88. Barsuk JH, Cohen ER, Vozenilek JA, O’Connor LM, McGaghie WC, Wayne DB. Simulation-based education with mastery learning improves paracentesis skills. J Grad Med Educ. 2012;4(1):23-27. doi: 10.4300/JGME-D-11-00161.1.
89. Lenchus JD. End of the “see one, do one, teach one” era: the next generation of invasive bedside procedural instruction. J Am Osteopath Assoc. 2010;110(6):340-346. doi: 10.7556/jaoa.2010.110.6.340.
90. American Board of Internal Medicine. Policies and Procedures for Certification. Philadelphia, PA: ABIM; 2006.
91. Lucas BP, Tierney DM, Jensen TP, et al. Credentialing of hospitalists in ultrasound-guided bedside procedures: a position statement of the Society of Hospital Medicine. J Hosp Med. 2018;13(2):117-125. doi: 10.12788/jhm.2917.
92. Brown GM, Otremba M, Devine LA, Gray C, Millington SJ, Ma IW. Defining competencies for ultrasound-guided bedside procedures: consensus opinions from Canadian physicians. J Ultrasound Med. 2016;35(1):129-141. doi: 10.7863/ultra.15.01063.
93. Babcock DS, Patriquin H, LaFortune M, Dauzat M. Power doppler sonography: basic principles and clinical applications in children. Pediatr Radiol. 1996;26(2):109-115. doi: 10.1007/BF01372087.
94. Howard ZD, Noble VE, Marill KA, et al. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46-53. doi: 10.1016/j.jemermed.2013.05.044.
95. Lindelius A, Torngren S, Nilsson L, Pettersson H, Adami J. Randomized clinical trial of bedside ultrasound among patients with abdominal pain in the emergency department: impact on patient satisfaction and health care consumption. Scand J Trauma Resusc Emerg Med. 2009;17:60. doi: 10.1186/1757-7241-17-60.
© 2019 Society of Hospital Medicine
The Role of the Medical Consultant in 2018: Putting It All Together
Whenever the principles of effective medical consultation are discussed, a classic article published in 1983 by Lee Goldman et al. is invariably referenced. In the “Ten Commandments for Effective Consultation,” Goldman argued that internists should “determine the question, establish urgency, look for yourself, be as brief as appropriate, be specific, provide contingency plans, honor thy turf, teach with tact, provide direct personal contact, and follow up.”1 If these Ten Commandments were followed, then the consultation would be more effective and satisfactory for both the consultant and the referring provider. However, with the advent of comanagement in 1994 where internists and surgeons have a “shared responsibility and accountability,”2 there has been a shift, and the once-concrete definitions of a specific reason for consult and the nature of “turf” have become blurred. Since 1994, the use of medical consultation and comanagement has skyrocketed, and today, more than 50% of surgical patients have a medical consultation or comanagement.3 This may be due to increased time pressures on surgeons and better outcomes of comanaged patients (eg, fewer postoperative complications, fewer transfers to an intensive care unit for acute medical deterioration, and increased likelihood to discharge to home).4
Medical management of surgical patients in the hospital involves a different skill set than that required to manage general medical patients. Accordingly, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) made medical consultation and perioperative care an End of Training Entrustable Professional Activities and ACGME subcompetency. Earlier this year, a nationwide perioperative curriculum for graduate medical education was consisting of eight objective and core topic modules and pretest/posttest questions selected from SHMConsults.com, including assessment and management of perioperative cardiac and pulmonary risk and management of diabetes, perioperative fever, and anticoagulants. Trainees were assessed using the multiple-choice questions, observed mini-cex, and written evaluation of a consultation report. Despite this encouraging development of curricula and competencies for trainees, there are still important gaps in our knowledge of basic patterns for consultation practices. For example, the type of patients and medical conditions currently encountered on our medical consultation and comanagement services had been previously unknown.
In the December issue of the Journal of Hospital Medicine, Wang et al. answer this question through the first cross-sectional multicenter prospective survey to examine medical consultation/comanagement practices since observational studies in the 1970-1990s.6 In a sample of 1,264 consultation requests from 11 academic medical centers over four two-week periods from July 2014 through July 2015, they found that the most common requests for consultation were medical management/comanagement, preoperative evaluation, blood pressure management, and other common postoperative complications, including postoperative atrial fibrillation, heart failure, renal failure, hyponatremia, anemia, hypoxia, and altered mental status.9 The majority of referrals were from orthopedic surgery and neurosurgery. They also found that medical consultants and comanagers provided comprehensive evaluations where more than a third of encounters addressed issues that were not stated in the initial reason for consult (RFC) and that consultants addressed more than two RFCs per encounter.9
These findings illustrate the paradigm shift of medical consultation focusing on a single specific question to addressing and optimizing the entire patient. This shift toward a broader, more open-ended reason for consultation may present some challenges such as “dumping” where referring surgeons and other specialists signoff their patients after surgery is completed, with internists processing the surgeons’ patients through the hospitalization. These challenges can be mitigated with predefined comanagement agreements with clearly defined roles and collaborative professional relationships.
Nonetheless, given the recent developments in curricula and training competencies mentioned above, internists are better equipped than ever before to put everything together and take care of the medical conditions of the increasingly complex and older surgical patient. For example, if one is consulted to see a patient for postoperative hypertension, it is difficult to not address the patient’s blood sugars in the 300s, lack of venous thromboembolism prophylaxis, delirium, acute renal failure, and acute blood loss anemia. The authors are correct to assert it is critically important to ensure that this input is desired by the referring physician either via verbal communication or comanagement agreements.
The findings of Wang et al. suggest some important future steps in medical consultation to ensure that our trainees and colleagues are prepared to take care of the entire patient regardless of whether the patient is on a consultant or comanagement agreement. This study shows that trainees are exposed to a diverse clinical experience on our medical consultation and comanagement services, which is in accordance with the objectives, assessment tools, and modules of the nationwide curriculum. It is likely that comanagement services will continue to expand as more of our medically complex patients will need either elective or emergency surgeries and surgeons have become less comfortable managing these patients on their own. We also may be asked to participate in quality improvement initiatives in the management of surgical patients, including the “perioperative surgical home programs,” where physicians work on a patient-centered approach to the surgical patient using evidence-based standard clinical care pathways and transitions from before surgery to postdischarge.7 We should share our experiences in quality improvement and the patient-centered medical home to ensure that our patients are optimized for surgery and beyond. As Lee Goldman et al. stated in the “Ten Commandments for Effective Consultations,1” consultative medicine is an important part of an internal medicine practice. Today, more than ever, the consultant or comanagement role or roles
1. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. PubMed
2. Macpherson DS, Parenti C, Nee J, et al. An internist joins the surgery service: does comanagement make a difference? J Gen Intern Med 1994;9:440-446. PubMed
3. Chen, LM, Wilk, AS, Thumma, JR et al. Use of medical consultants for hospitalized surgical patients. An observational cohort study. JAMA Intern Med. 2014;174(9):1470-1477. doi: 10.1001/jamainternmed.2014.3376. PubMed
4. Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service–a literature review comparing different models. Osteoporos Int. 2010;21(Suppl 4):S637-S646. doi: 10.1007/s00198-010-1396-x. PubMed
5. Fang M, O’Glasser A, Sahai S, Pfeifer K, Johnson KM, Kuperman E. Development of a nationwide consensus curriculum of perioperative medicine: a modified Delphi method. Periop Care Oper Room Manag. 2018;12:31-34. doi: 10.1016/j.pcorm.2018.09.002.
6. Wang ES, Moreland C, Shoffeitt M, Leykum LK. Who consults us and why? An evaluation of medicine consult/co-management services at academic medical centers. J Hosp Med. 2018;12(4):840-843. doi: 10.12788/jhm.3010. PubMed
7. Kain ZN, Vakharia S, Garson L, et al. The perioperative surgical home as a future perioperative practice model. Anesth Analg. 2014;118(5):1126-1130. doi: 10.1213/ANE.0000000000000190. PubMed
Whenever the principles of effective medical consultation are discussed, a classic article published in 1983 by Lee Goldman et al. is invariably referenced. In the “Ten Commandments for Effective Consultation,” Goldman argued that internists should “determine the question, establish urgency, look for yourself, be as brief as appropriate, be specific, provide contingency plans, honor thy turf, teach with tact, provide direct personal contact, and follow up.”1 If these Ten Commandments were followed, then the consultation would be more effective and satisfactory for both the consultant and the referring provider. However, with the advent of comanagement in 1994 where internists and surgeons have a “shared responsibility and accountability,”2 there has been a shift, and the once-concrete definitions of a specific reason for consult and the nature of “turf” have become blurred. Since 1994, the use of medical consultation and comanagement has skyrocketed, and today, more than 50% of surgical patients have a medical consultation or comanagement.3 This may be due to increased time pressures on surgeons and better outcomes of comanaged patients (eg, fewer postoperative complications, fewer transfers to an intensive care unit for acute medical deterioration, and increased likelihood to discharge to home).4
Medical management of surgical patients in the hospital involves a different skill set than that required to manage general medical patients. Accordingly, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) made medical consultation and perioperative care an End of Training Entrustable Professional Activities and ACGME subcompetency. Earlier this year, a nationwide perioperative curriculum for graduate medical education was consisting of eight objective and core topic modules and pretest/posttest questions selected from SHMConsults.com, including assessment and management of perioperative cardiac and pulmonary risk and management of diabetes, perioperative fever, and anticoagulants. Trainees were assessed using the multiple-choice questions, observed mini-cex, and written evaluation of a consultation report. Despite this encouraging development of curricula and competencies for trainees, there are still important gaps in our knowledge of basic patterns for consultation practices. For example, the type of patients and medical conditions currently encountered on our medical consultation and comanagement services had been previously unknown.
In the December issue of the Journal of Hospital Medicine, Wang et al. answer this question through the first cross-sectional multicenter prospective survey to examine medical consultation/comanagement practices since observational studies in the 1970-1990s.6 In a sample of 1,264 consultation requests from 11 academic medical centers over four two-week periods from July 2014 through July 2015, they found that the most common requests for consultation were medical management/comanagement, preoperative evaluation, blood pressure management, and other common postoperative complications, including postoperative atrial fibrillation, heart failure, renal failure, hyponatremia, anemia, hypoxia, and altered mental status.9 The majority of referrals were from orthopedic surgery and neurosurgery. They also found that medical consultants and comanagers provided comprehensive evaluations where more than a third of encounters addressed issues that were not stated in the initial reason for consult (RFC) and that consultants addressed more than two RFCs per encounter.9
These findings illustrate the paradigm shift of medical consultation focusing on a single specific question to addressing and optimizing the entire patient. This shift toward a broader, more open-ended reason for consultation may present some challenges such as “dumping” where referring surgeons and other specialists signoff their patients after surgery is completed, with internists processing the surgeons’ patients through the hospitalization. These challenges can be mitigated with predefined comanagement agreements with clearly defined roles and collaborative professional relationships.
Nonetheless, given the recent developments in curricula and training competencies mentioned above, internists are better equipped than ever before to put everything together and take care of the medical conditions of the increasingly complex and older surgical patient. For example, if one is consulted to see a patient for postoperative hypertension, it is difficult to not address the patient’s blood sugars in the 300s, lack of venous thromboembolism prophylaxis, delirium, acute renal failure, and acute blood loss anemia. The authors are correct to assert it is critically important to ensure that this input is desired by the referring physician either via verbal communication or comanagement agreements.
The findings of Wang et al. suggest some important future steps in medical consultation to ensure that our trainees and colleagues are prepared to take care of the entire patient regardless of whether the patient is on a consultant or comanagement agreement. This study shows that trainees are exposed to a diverse clinical experience on our medical consultation and comanagement services, which is in accordance with the objectives, assessment tools, and modules of the nationwide curriculum. It is likely that comanagement services will continue to expand as more of our medically complex patients will need either elective or emergency surgeries and surgeons have become less comfortable managing these patients on their own. We also may be asked to participate in quality improvement initiatives in the management of surgical patients, including the “perioperative surgical home programs,” where physicians work on a patient-centered approach to the surgical patient using evidence-based standard clinical care pathways and transitions from before surgery to postdischarge.7 We should share our experiences in quality improvement and the patient-centered medical home to ensure that our patients are optimized for surgery and beyond. As Lee Goldman et al. stated in the “Ten Commandments for Effective Consultations,1” consultative medicine is an important part of an internal medicine practice. Today, more than ever, the consultant or comanagement role or roles
Whenever the principles of effective medical consultation are discussed, a classic article published in 1983 by Lee Goldman et al. is invariably referenced. In the “Ten Commandments for Effective Consultation,” Goldman argued that internists should “determine the question, establish urgency, look for yourself, be as brief as appropriate, be specific, provide contingency plans, honor thy turf, teach with tact, provide direct personal contact, and follow up.”1 If these Ten Commandments were followed, then the consultation would be more effective and satisfactory for both the consultant and the referring provider. However, with the advent of comanagement in 1994 where internists and surgeons have a “shared responsibility and accountability,”2 there has been a shift, and the once-concrete definitions of a specific reason for consult and the nature of “turf” have become blurred. Since 1994, the use of medical consultation and comanagement has skyrocketed, and today, more than 50% of surgical patients have a medical consultation or comanagement.3 This may be due to increased time pressures on surgeons and better outcomes of comanaged patients (eg, fewer postoperative complications, fewer transfers to an intensive care unit for acute medical deterioration, and increased likelihood to discharge to home).4
Medical management of surgical patients in the hospital involves a different skill set than that required to manage general medical patients. Accordingly, in 2012, the Accreditation Council for Graduate Medical Education (ACGME) made medical consultation and perioperative care an End of Training Entrustable Professional Activities and ACGME subcompetency. Earlier this year, a nationwide perioperative curriculum for graduate medical education was consisting of eight objective and core topic modules and pretest/posttest questions selected from SHMConsults.com, including assessment and management of perioperative cardiac and pulmonary risk and management of diabetes, perioperative fever, and anticoagulants. Trainees were assessed using the multiple-choice questions, observed mini-cex, and written evaluation of a consultation report. Despite this encouraging development of curricula and competencies for trainees, there are still important gaps in our knowledge of basic patterns for consultation practices. For example, the type of patients and medical conditions currently encountered on our medical consultation and comanagement services had been previously unknown.
In the December issue of the Journal of Hospital Medicine, Wang et al. answer this question through the first cross-sectional multicenter prospective survey to examine medical consultation/comanagement practices since observational studies in the 1970-1990s.6 In a sample of 1,264 consultation requests from 11 academic medical centers over four two-week periods from July 2014 through July 2015, they found that the most common requests for consultation were medical management/comanagement, preoperative evaluation, blood pressure management, and other common postoperative complications, including postoperative atrial fibrillation, heart failure, renal failure, hyponatremia, anemia, hypoxia, and altered mental status.9 The majority of referrals were from orthopedic surgery and neurosurgery. They also found that medical consultants and comanagers provided comprehensive evaluations where more than a third of encounters addressed issues that were not stated in the initial reason for consult (RFC) and that consultants addressed more than two RFCs per encounter.9
These findings illustrate the paradigm shift of medical consultation focusing on a single specific question to addressing and optimizing the entire patient. This shift toward a broader, more open-ended reason for consultation may present some challenges such as “dumping” where referring surgeons and other specialists signoff their patients after surgery is completed, with internists processing the surgeons’ patients through the hospitalization. These challenges can be mitigated with predefined comanagement agreements with clearly defined roles and collaborative professional relationships.
Nonetheless, given the recent developments in curricula and training competencies mentioned above, internists are better equipped than ever before to put everything together and take care of the medical conditions of the increasingly complex and older surgical patient. For example, if one is consulted to see a patient for postoperative hypertension, it is difficult to not address the patient’s blood sugars in the 300s, lack of venous thromboembolism prophylaxis, delirium, acute renal failure, and acute blood loss anemia. The authors are correct to assert it is critically important to ensure that this input is desired by the referring physician either via verbal communication or comanagement agreements.
The findings of Wang et al. suggest some important future steps in medical consultation to ensure that our trainees and colleagues are prepared to take care of the entire patient regardless of whether the patient is on a consultant or comanagement agreement. This study shows that trainees are exposed to a diverse clinical experience on our medical consultation and comanagement services, which is in accordance with the objectives, assessment tools, and modules of the nationwide curriculum. It is likely that comanagement services will continue to expand as more of our medically complex patients will need either elective or emergency surgeries and surgeons have become less comfortable managing these patients on their own. We also may be asked to participate in quality improvement initiatives in the management of surgical patients, including the “perioperative surgical home programs,” where physicians work on a patient-centered approach to the surgical patient using evidence-based standard clinical care pathways and transitions from before surgery to postdischarge.7 We should share our experiences in quality improvement and the patient-centered medical home to ensure that our patients are optimized for surgery and beyond. As Lee Goldman et al. stated in the “Ten Commandments for Effective Consultations,1” consultative medicine is an important part of an internal medicine practice. Today, more than ever, the consultant or comanagement role or roles
1. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. PubMed
2. Macpherson DS, Parenti C, Nee J, et al. An internist joins the surgery service: does comanagement make a difference? J Gen Intern Med 1994;9:440-446. PubMed
3. Chen, LM, Wilk, AS, Thumma, JR et al. Use of medical consultants for hospitalized surgical patients. An observational cohort study. JAMA Intern Med. 2014;174(9):1470-1477. doi: 10.1001/jamainternmed.2014.3376. PubMed
4. Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service–a literature review comparing different models. Osteoporos Int. 2010;21(Suppl 4):S637-S646. doi: 10.1007/s00198-010-1396-x. PubMed
5. Fang M, O’Glasser A, Sahai S, Pfeifer K, Johnson KM, Kuperman E. Development of a nationwide consensus curriculum of perioperative medicine: a modified Delphi method. Periop Care Oper Room Manag. 2018;12:31-34. doi: 10.1016/j.pcorm.2018.09.002.
6. Wang ES, Moreland C, Shoffeitt M, Leykum LK. Who consults us and why? An evaluation of medicine consult/co-management services at academic medical centers. J Hosp Med. 2018;12(4):840-843. doi: 10.12788/jhm.3010. PubMed
7. Kain ZN, Vakharia S, Garson L, et al. The perioperative surgical home as a future perioperative practice model. Anesth Analg. 2014;118(5):1126-1130. doi: 10.1213/ANE.0000000000000190. PubMed
1. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753-1755. PubMed
2. Macpherson DS, Parenti C, Nee J, et al. An internist joins the surgery service: does comanagement make a difference? J Gen Intern Med 1994;9:440-446. PubMed
3. Chen, LM, Wilk, AS, Thumma, JR et al. Use of medical consultants for hospitalized surgical patients. An observational cohort study. JAMA Intern Med. 2014;174(9):1470-1477. doi: 10.1001/jamainternmed.2014.3376. PubMed
4. Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service–a literature review comparing different models. Osteoporos Int. 2010;21(Suppl 4):S637-S646. doi: 10.1007/s00198-010-1396-x. PubMed
5. Fang M, O’Glasser A, Sahai S, Pfeifer K, Johnson KM, Kuperman E. Development of a nationwide consensus curriculum of perioperative medicine: a modified Delphi method. Periop Care Oper Room Manag. 2018;12:31-34. doi: 10.1016/j.pcorm.2018.09.002.
6. Wang ES, Moreland C, Shoffeitt M, Leykum LK. Who consults us and why? An evaluation of medicine consult/co-management services at academic medical centers. J Hosp Med. 2018;12(4):840-843. doi: 10.12788/jhm.3010. PubMed
7. Kain ZN, Vakharia S, Garson L, et al. The perioperative surgical home as a future perioperative practice model. Anesth Analg. 2014;118(5):1126-1130. doi: 10.1213/ANE.0000000000000190. PubMed
© 2019 Society of Hospital Medicine
Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
The majority of hospitalized patients worldwide have at least one peripheral intravenous catheter (PIVC),1 making PIVC insertion one of the most common clinical procedures. In the United States, physicians, advanced practitioners, and nurses insert over 300 million of these devices in hospitalized patients annually.2 Despite their prevalence, PIVCs are associated with high rates of complications, including insertion difficulty, phlebitis, infiltration, occlusion, dislodgment, and catheter-associated bloodstream infection (CABSI), known to increase morbidity and mortality risk.2-9 Up to 90% of PIVCs are prematurely removed owing to failure before planned replacement or before intravenous (IV) therapy completion.3-6,10-12
PIVC complication and failure commonly triggers insertion of a replacement device and can entail significant costs.2-4 One example is PIVC-related CABSI, where treatment costs have been estimated to be between US$35,000 and US$56,000 per patient.6,13 Another important consideration is the pain and anxiety experienced by patients who need a replacement device, particularly those with difficult vascular access, who may require multiple cannulation attempts to replace a PIVC.12,14-16 In developing nations, serious adverse events related to PIVCs are even more concerning, because hospital acquired infection rates and associated mortality are nearly 20 times greater than in developed nations.17
A number of evidence-based interventions have been suggested to reduce PIVC failure rates. In addition to optimal hand hygiene when inserting or accessing a PIVC to prevent infection,18 recommended interventions include placement of the PIVC in an area of non-flexion such as the forearm to provide stability for the device and to reduce patient discomfort, securing the PIVC to reduce movement of the catheter at the insertion site and within the blood vessel, and use of occlusive dressings that reduce the risk of external contamination of the PIVC site.11,19,20 Best practice guidelines also recommend the prompt removal of devices that are symptomatic (when phlebitis or other complications are suspected) and when the catheter is no longer required.21,22
Recent evidence has demonstrated that catheter size can have an impact on device survival rates. In adults, large-bore catheters of 18 gauge (G) or higher were found to have an increased rate of thrombosis, and smaller-bore catheters of 22G or lower (in adults) were found to have higher rates of dislodgment and occlusion/infiltration. The catheter size recommended for adults based on the latest evidence for most clinical applications is 20G.3,20,23,24 In addition, the documentation of insertion, maintenance, and removal of PIVCs in the medical record is a requirement in most healthcare facilities worldwide and is recommended by best practice guidelines; however, adherence remains a challenge.1,19
The concerning prevalence of PIVC-related complications and the lack of comparative data internationally on organizational compliance with best practice guidelines formed the rationale for this study. Our study aim was to describe the insertion characteristics, management practices, and outcomes of PIVCs internationally and to compare these variables to recommended best practice.
MATERIALS AND METHODS
Study Design and Participants
In this international cross-sectional study, we recruited hospitals through professional networks, including vascular access, infection prevention, safety and quality, nursing, and hospital associations (Appendix 2). Healthcare organizations, government health departments, and intravascular device suppliers were informed of the study and requested to further disseminate information through their networks. A study website was developed,25 and social media outlets, including Twitter®, LinkedIn®, and Facebook®, were used to promote the study.
Approval was granted by the Griffith University Human Research Ethics Committee in Australia (reference number NRS/34/13/HREC). In addition, evidence of study site and local institutional review board/ethics committee approval was required prior to study commencement. Each participating site agreed to follow the study protocol and signed an authorship agreement form. No financial support was provided to any site.
Hospitalized adult and pediatric patients with a PIVC in situ on the day of the study were eligible for inclusion. Sample size was determined by local capacity. Hospitals were encouraged to audit their entire institution if possible; however, data were accepted from as little as one ward. Data collectors comprised nurses and doctors with experience in PIVC assessment. They were briefed on the study protocol and data collection forms by the local site coordinator, and they were supported by an overall global coordinator. Clinicians assessed the PIVC insertion site and accessed hospital records to collect data related to PIVC insertion, concurrent medications, and IV fluid orders. Further clarification of data was obtained if necessary by the clinicians from the patients and treating staff. No identifiable patient information was collected.
Data Collection
To assess whether clinical facilities were following best practice recommendations, the study team developed three data collection forms to collect information regarding site characteristics (site questionnaire), track participant recruitment (screening log), and collect data regarding PIVC characteristics and management practices (case report form [CRF]). All forms were internally and externally validated following a pilot study involving 14 sites in 13 countries.1
The CRF included variables used to assess best practice interventions, such as catheter insertion characteristics (date and time, reason, location, profession of inserter, anatomical site of placement), catheter type (gauge, brand, and product), insertion site assessment (adverse symptoms, dressing type and integrity), and information related to the IV therapy (types of IV fluids and medications, flushing solutions). Idle PIVCs were defined as not being used for blood sampling or IV therapy in the preceding 24 h.
Data collection forms were translated into 15 languages by professional translators and back-translated for validity. Translation of some languages included additional rigor. For example, Spanish-speaking members from the Spanish mainland as well as from South America were employed so that appropriate synonyms were used to capture local terms and practice. Three options were provided for data entry: directly into a purpose-developed electronic database (Lime Survey® Project, Hamburg, Germany); on paper, then transcribed into the survey database at a later time by the hospital site; or paper entry then sent (via email or post) to the coordinating center for data entry. Once cleaned and collated, all data were provided to each participating hospital to confirm accuracy and for site use in local quality improvement processes. Data were collected between June 1, 2014 and July 31, 2015.
Statistical Analysis
All data management was undertaken using SAS statistical software (SAS Institute Inc., Cary NC, USA). Results are presented for eight geographical regions using descriptive statistics (frequencies, percentages, and 95% CIs) for the variables of interest. To assess trends in catheter dwell time and rates of phlebitis, Poisson regression was used. All analyses were undertaken using the R language for statistical analysis (R Core Team, Vienna, Austria). The (STROBE (Strengthening the Reporting of Observational Studies in Epidemiology statement) guidelines for cross-sectional studies were followed, and results are presented according to these recommendations.26
RESULTS
Of the 415 hospitals that participated in this study, 406 had patients with PIVCs on the day of the study (the others being small rural centers). Thus, a total of 40,620 PIVCs in 38,161 patients from 406 hospitals in 51 countries were assessed, with no more than 5% missing data for any CRF question. There were 2459 patients (6.1%) with two or more PIVCs concurrently in situ. The median patient age was 59 y (interquartile range [IQR], 37–74 y), and just over half were male (n = 20,550, 51%). Hospital size ranged from fewer than 10 beds to over 1,000 beds, and hospitals were located in rural, regional, and metropolitan districts. The majority of countries (n = 31, 61%) contributed multiple sites, the highest being Australia with 79 hospitals. Countries with the most PIVCs studied were Spain (n = 5,553, 14%) and the United States (n = 5,048, 12%).
General surgical (n = 15,616, 39%) and medical (n = 15,448, 38%) patients represented most of the population observed. PIVCs were inserted primarily in general wards or clinics (n = 22,167, 55%) or in emergency departments (n = 7,388, 18%; Table) and for the administration of IV medication (n = 28,571, 70%) and IV fluids (n = 7,093, 18%; Table).
Globally, nurses were the primary PIVC inserters (n = 28,575, 71%); however, Australia/New Zealand had only 26% (n = 1,518) of PIVCs inserted by this group (Table). Only about one-third of PIVCs were placed in an area of non-flexion (forearm, n = 12,675, 31%, Table) the majority (n = 27,856, 69%) were placed in non-recommended anatomical sites (Figure 1). Most PIVCs were placed in the hand (n = 13,265, 32.7%) followed by the antecubital veins (n = 6176, 15.2%) and the wrist (n = 5,465, 13.5%). Site selection varied widely across the regions; 29% (n = 1686) of PIVCs in Australia/New Zealand were inserted into the antecubital veins, twice the study group average. Over half of the PIVCs inserted in the Middle East were placed in the hand (n = 295, 56%). This region also had the highest prevalence of devices placed in nonrecommended sites (n = 416, 79%; Figure 1).
The majority of PIVCs (n = 27,192, 67%; Table) were of recommended size (20–22G); however, some devices were observed to be large (14–18G; n = 6,802, 17%) or small (24-26g; n = 4,869, 12%) in adults. In Asia, 41% (n = 2,617) of devices inserted were 24-26G, more than three times the global rate. Half of all devices in Asia (n = 3,077, 48%) and the South Pacific (n = 67, 52%) were of a size not recommended for routine IV therapy (Figure 2).
The primary dressing material used was a transparent dressing (n = 31,596, 77.8%; Table); however, nearly 1 in 5 dressings used had either nonsterile tape alone (n = 5,169, 13%; Appendix 4), or a sterile gauze and tape (n = 2,592, 6%; Appendix 4.1). We found a wide variation in the use of nonsterile tape, including 1 in every 3 devices in South America dressed with nonsterile tape (n = 714, 30%) and a larger proportion in Africa (n = 543, 19%) and Europe (n = 3,056, 18%). Nonsterile tape was rarely used in North America and Australia/New Zealand. Although most PIVC dressings were clean, dry, and intact (n = 31,786, 79%; Table), one-fifth overall were compromised (moist, soiled, and/or lifting off the skin). Compromised dressings (Appendix 4.2) were more prevalent in Australia/New Zealand (n = 1,448; 25%) and in Africa (n = 707, 25%) than elsewhere.
Ten percent of PIVCs (n = 4,204) had signs and/or symptoms suggestive of phlebitis (characterized by pain, redness and/or swelling at the insertion site; Appendix 4.3). The highest prevalence of phlebitis occurred in Asia (n = 1,021, 16%), Africa (n = 360, 13%), and South America (n = 284, 12%). Pain and/or redness were the most common phlebitis symptoms. We found no association between dwell time of PIVCs and phlebitis rates (P = .085). Phlebitis rates were 12% (Days 1-3; n = 15,625), 16% (Days 4-7; n = 3,348), 10% (Days 8-21; n = 457), and 13% (Day21+; n = 174). Nearly 10% (n = 3,879) of catheters were observed to have signs of malfunction such as blood in the infusion tubing, leaking at the insertion site, or dislodgment (Appendix 4.4).
We observed 14% (n = 5,796) of PIVCs to be idle (Appendix 4.5), defined as not used in the preceding 24 h. Nearly one-fourth of all devices in North America (n = 1,230, 23%) and Australia/New Zealand (n = 1,335, 23%) were idle. PIVC documentation in hospital records was also poor, nearly half of all PIVCs (n = 19,768, 49%) had no documented date and time of insertion. The poorest compliance was in Australia/New Zealand (n = 3,428, 59%; Appendix 4.6). We also observed that 1 in 10 PIVCs had no documentation regarding who inserted the PIVC (n = 3,905). Thirty-six percent of PIVCs (n = 14,787) had no documented assessment of the PIVC site on the day of review (Appendix 4.7), including over half of all PIVCs in Asia (n = 3,364, 52%). Overall, the median dwell at the time of assessment for PIVCs with insertion date/time documented was 1.5 d (IQR, 1.0–2.5 d).
DISCUSSION
This international assessment of more than 40,000 PIVCs in 51 countries provides great insight into device characteristics and variation in management practices. Predominantly, PIVCs were inserted by nurses in the general ward environment for IV medication. One in ten PIVCs had at least one symptom of phlebitis, one in ten were dysfunctional, one in five PIVC dressings were compromised, and one in six PIVCs had not been used in the preceding 24 h. Nearly half of the PIVCs audited had the insertion date and time missing.
Regional variation was found in the professions inserting PIVCs, as well as in anatomical placement. In Australia/New Zealand, the proportion of nurses inserting PIVCs was much lower than the study group average (26% vs 71%). Because these countries contributed a substantial number of hospitals to the study, this seems a representative finding and suggests a need for education targeted at nurses for PIVC insertion in this region. The veins in the forearm are recommended as optimal for PIVC insertion in adults, rather than areas of high flexion, because the forearm provides a wide surface area to secure and dress PIVCs. Forearm placement can reduce pain during catheter dwell as well as decrease the risk of accidental removal or occlusion.3,19,27 We found only one-third of PIVCs were placed in the forearm, with most placed in the hand, antecubital veins, or wrist. This highlights an inconsistency with published recommendations and suggests that additional training and technology are required so that staff can better identify and insert PIVCs in the forearm for other than very short-term (procedural) PIVCp;s.19
Phlebitis triggering PIVC failure remains a global clinical challenge with numerous phlebitis definitions and varied assessment techniques.10 The prevalence of phlebitis has been difficult to approximate with varying estimates and definitions in the literature; however, it remains a key predictor of PIVC failure.6,10 Identification of this complication and prompt removal of the device is critical for patient comfort and reducing CABSI risk.5,28 The overall prevalence of phlebitis signs or symptoms (defined in this study as having one or more signs of redness, swelling, or pain surrounding the insertion site) was just over 10%, with pain and/or redness being most prevalent. These compromised PIVCs had not been removed as is recommended for such complications.19,28 Considering that our study was a snapshot at only one time point, the per-catheter incidence of phlebitis would be even higher; interestingly, among PIVCs with a documented insertion date and time, we observed that dwell time did not influence phlebitis rates.
Another concern is that nearly 10% (n = 3,879) of PIVCs were malfunctioning (eg, leaking) but were still in place. To bring these problems into context, around 2 billion PIVCs are used annually worldwide; as a consequence, millions of patients suffer from painful or malfunctioning PIVCs staff had not responded.1,29 The placement of large-bore catheters, and smaller-gauge ones in adults, is known to increase the incidence of malfunction that leads to failure. There are a number of sound clinical reasons for the use of large-bore (eg, resuscitation and rapid fluid replacement) or small-bore (eg, difficult venous access with small superficial veins only visible and palpable) catheters. However, it would be expected that only a small proportion of patients would require these devices, and not one in three devices as we identified. This finding suggests that some PIVCs were inappropriate in size for general IV therapy and may reflect antiquated hospital policies for some clinical cohorts.30,31
Overall, transparent dressings were used to cover the PIVC, but a number of patients were observed to have a sterile gauze and tape dressing (n = 2,592, 6%). Although the latter is less common, both dressing approaches are recommended in clinical practice guidelines because there is a lack of high-quality evidence regarding which is superior.21,22,32 Of concern was the use of nonsterile tape to dress the PIVC (n = 5,169, 12.7%). We found the prevalence of nonsterile tape use to be higher in lower-resourced countries in South America (n = 714, 30%), Africa (n = 543, 19%) and Europe (n = 3,056, 18%) and this was likely related to institutional cost reduction practices.
This finding illustrates an important issue regarding proper PIVC care and management practices in developing nations. It is widely known that access to safe health care in lower-resourced nations is challenging and that rates of mortality related to healthcare-associated infections are much higher. Thus, the differences we found in PIVC management practices in these countries are not surprising.33,34 International health networks such as the Infection Control Africa Network, the International Federation of Infection Control, and the Centers for Disease Control and Prevention can have great influence on ministries of health and clinicians in these countries to develop coordinated efforts for safe and sustainable IV practices to reduce the burden of hospital-acquired infections and related morbidity and mortality.
We found that 14% of all PIVCs had no documented IV medication or IV fluid administered in the previous 24 h, strongly indicating that they were no longer needed. Australia/New Zealand, Europe, and North America were observed to have a higher prevalence of idle catheters than the remaining regions. This suggests that an opportunity exists to develop surveillance systems that better identify idle devices for prompt removal to reduce infection risk and patient discomfort. Several randomized controlled trials, a Cochrane review, and clinical practice guidelines recommend prompt removal of PIVCs when not required, if there are any complications, or if the PIVC was inserted urgently without an aseptic insertion technique.21,28,35,36 Idle PIVCs have been implicated in adverse patient outcomes, including phlebitis and CABSI.13,27
The substantial proportion of patients with a PIVC in this study who had no clinical indication for a PIVC, a symptomatic insertion site, malfunctioning catheter, and suboptimal dressing quality suggests the need for physicians, advanced practitioners, and nurses to adopt evidence-based PIVC insertion and maintenance bundles and supporting checklists to reduce the prevalence of PIVC complications.19,21,38-40 Recommended strategies for inclusion in PIVC maintenance bundles are prompt removal of symptomatic and/or idle catheters, hand hygiene prior to accessing the catheter, regular assessment of the device, and replacement of suboptimal dressings.41,42 This approach should be implemented across all clinical specialties involved in PIVC insertion and care.
Our study findings need to be considered within the context of some limitations. The cross-sectional design prevented follow-up of PIVCs until removal to collect outcomes, including subsequent PIVC complications and/or failure, following the study observation. Ideally, data collection could have included patient-level preferences for PIVC insertion, history of PIVC use and/or failure, the number of PIVC insertion attempts, and the number of PIVCs used during that hospitalization. However, a cohort study of this magnitude was not feasible, particularly because all sites contributed staff time to complete the data collection. Only half of all initially registered sites eventually participated in the study; reasons for not participating were cited as local workload constraints and/or difficulties in applying for local approvals. Although efforts to enroll hospitals worldwide were exhaustive, our sample was not randomly selected but relied on self-selection and so is not representative, particularly for countries that contributed only one hospital site. Caution is also required when comparing inter regional differences, particularly developing regions, because better-resourced/academic sites were possibly over represented in the sample. Nevertheless, PIVC variables differed significantly between participating hospitals, suggesting that the data represent a reasonable reflection of hospital variability.
CONCLUSIONS
On the basis of this international investigation, we report variations in the characteristics, management practices, and outcomes of PIVCs inserted in hospital patients from 51 countries. Many PIVCs were idle, symptomatic, had substandard dressings, and were inserted in suboptimal anatomical sites. Despite international best practice guidelines, a large number of patients had PIVCs that were already failing or at risk of complications, including infection. A stronger focus is needed on compliance with PIVC insertion and management guidelines; better surveillance of PIVC sites; and improved assessment, decision-making, and documentation.
Acknowledgements
We are extremely grateful to colleagues from across the globe who committed their time and effort to this study (for full details of countries and team members see Appendix 1).
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
1. Alexandrou E, Ray-Barruel G, Carr PJ, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533. https:/doi.org/10.1002/jhm.2389
2. Zingg W, Pittet D. Peripheral venous catheters: an under-evaluated problem. Int J Antimicrob Agents. 2009;34(suppl 4):S38-S42. https:/ doi.org/10.1016/S0924-8579(09)70565-5
3. Wallis MC, McGrail MR, Webster J, Gowardman JR, Playford G, Rickard CM. Risk factors for PIV catheter failure: a multivariate analysis from a randomized control trial. Infect. Control Hosp Epidemiol. 2014;35(1):63-68. https:/doi.org/10.1086/674398.
4. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect. 2007;67(1):22-29.
5. Fakih MG, Jones K, Rey JE, et al. Sustained improvements in peripheral venous catheter care in non–intensive care units: a quasi-experimental controlled study of education and feedback. Infect. Control Hosp Epidemiol. 2012;33(5):449-455. https:/doi.org/10.1086/665322.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. J Infus Nurs. 2015;38(3):189-203. https:/ doi.org/10.1097/NAN.0000000000000100.
7. Austin ED, Sullivan SB, Whittier S, Lowy FD, Uhlemann AC. Peripheral intravenous catheter placement is an underrecognized source of Staphylococcus aureus bloodstream infection. Open Forum Infect Dis. 2016;3(2):ofw072. https:/ doi.org/10.1093/ofid/ofw072.
8. Stuart RL, Cameron D, Scott C, et al. Peripheral intravenous catheter-associated Staphylococcus aureus bacteraemia: more than 5 years of prospective data from two tertiary health services. Med J Aust. 2013;198(10):551-553.
9. Trinh TT, Chan PA, Edwards O, et al. Peripheral venous catheter-related Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2011;32(6):579-583. https:/doi.org/10.1086/660099.
10. Ray Barruel G, Polit DF, Murfield JE, Rickard CM. Infusion phlebitis assessment measures: a systematic review. J Eval Clin Pract. 2014;20(2):191-202. https:/ doi.org/ 10.1111/jep.12107
11. Marsh N, Webster J, Flynn J, et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access. 2015;16(3):237-244. https:/doi.org /10.5301/jva.5000348.
12. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851-858. https:/doi.org/ 10.12788/jhm.2836
13. Becerra MB, Shirley D, Safdar N. Prevalence, risk factors, and outcomes of idle intravenous catheters: An integrative review. Am J Infect Control. 2016;44(10):e167-e172. https:/ doi.org/10.1016/j.ajic.2016.03.073.
14. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Support Care Cancer. 2016;24(3):1181-1187. https:/ doi.org/10.1007/s00520-015-2900-9.
15. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-526. https:/doi.org/10.5301/jva.5000411
16. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16(1):64. https:/ doi.org/10.1186/s12912-017-0261-z
17. World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva2011. 9241501502.
18. Hirschmann H, Fux L, Podusel J, et al. The influence of hand hygiene prior to insertion of peripheral venous catheters on the frequency of complications. J Hosp Infect. 2001;49(3):199-203. https:/doi.org/10.1053/jhin.2001.1077
19. Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.
20. Abolfotouh MA, Salam M, Bani-Mustafa Aa, White D, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993. https://doi.org/10.2147/TCRM.S74685.
21. Loveday H, Wilson J, Pratt R, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014;86(suppl 1):S1-S70. https:/doi.org/10.1016/S0195-6701(13)60012-2.
22. O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. https:/doi.org/10.1093/cid/cir257
23. Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273. https:/doi.org/10.1111/j.1365-2648.2009.04980.x.
24. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83-89. https:/doi.org/10.12788/jhm.2867.
25. One Million Global Catheters PIVC Worldwide Prevalence study. OMG study website http://www.omgpivc.org/. Accessed 23 March, 2017.
26. Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. https:/doi.org/ 10.1136/bmj.39335.541782.AD
27. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134-1140. https:/doi.org/10.1016/j.ajem.2011.07.027.
28. Patel SA, Alebich MM, Feldman LS. Choosing wisely: things we do for no reason. Routine replacement of peripheral intravenous catheters. J Hosp Med. 2017;12(1):42-45.
29. Newswire. Global Peripheral I.V. Catheter Market 2014 - 2018. New York, PR Newswire Assoc; 2014.
30. Webster J, Larsen E, Booker C, Laws J, Marsh N. Prophylactic insertion of large bore peripheral intravenous catheters in maternity patients for postpartum haemorrhage: A cohort study. Aust N Z J Obstet Gynaecol. 2017.https:/doi.org/10.1111/ajo.12759.
31. Rivera A, Strauss K, van Zundert A, Mortier E. Matching the peripheral intravenous catheter to the individual patient. Acta Anaesthesiol Belg. 2006;58(1):19.
32. Webster J, Gillies D, O’Riordan E, Sherriff KL, Rickard CM. Gauze and tape and transparent polyurethane dressings for central venous catheters. Cochrane Database Syst Rev. 2011;11:CD003827. https:/doi.org/10.1002/14651858.CD003827.pub2
33. Dieleman JL, Templin T, Sadat N, et al. National spending on health by source for 184 countries between 2013 and 2040. Lancet. 2016;387(10037):2521-2535. https:/ doi.org/10.1016/S0140-6736(16)30167-2.
34. Allegranzi B, Nejad SB, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228-241. https:/ doi.org/10.1016/S0140-6736(10)61458-4.
35. Rickard CM, Webster J, Wallis MC, et al. Routine versus clinically indicated replacement of peripheral intravenous catheters: a randomised controlled equivalence trial. Lancet. 2012;380(9847):1066-1074. https:/doi.org/10.1016/S0140-6736(12)61082-4.
36. Webster J, Osborne S, Rickard CM, New K. Clinically indicated replacement versus routine replacement of peripheral venous catheters. Cochrane Database Syst Rev. 2015;8:CD007798. https://doi.org/10.1002/14651858.CD007798.pub4.
37. Yagnik L, Graves A, Thong K. Plastic in patient study: Prospective audit of adherence to peripheral intravenous cannula monitoring and documentation guidelines, with the aim of reducing future rates of intravenous cannula-related complications. Am J Infect Control. 2017;45(1):34-38. https:/doi.org/10.1016/j.ajic.2016.09.008.
38. Boyd S, Aggarwal I, Davey P, Logan M, Nathwani D. Peripheral intravenous catheters: the road to quality improvement and safer patient care. J Hosp Infect. 2011;77(1):37-41. https:/doi.org/10.1016/j.jhin.2010.09.011.
39. DeVries M, Valentine M, Mancos P. Protected clinical indication of peripheral intravenous lines: successful implementation. J Assoc Vasc Access. 2016;21(2):89-92. https://doi.org/10.1016/j.java.2016.03.001.
40. Rhodes D, Cheng A, McLellan S, et al. Reducing Staphylococcus aureus bloodstream infections associated with peripheral intravenous cannulae: successful implementation of a care bundle at a large Australian health service. J Hosp Infect. 2016;94(1):86-91. https:/doi.org/10.1016/j.jhin.2016.05.020.
41. Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatr. 2012;130(4):e996-e1004. https:/doi.org/10.1542/peds.2012-0295.
42. Marshall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 2014;35(suppl 2):S89-107. https:/doi.org/10.1086/676533.
© 2018 Society of Hospital Medicine
New South Wales 2751, Australia; Telephone: + 612 9685 9506; Fax: + 612 9685 9023; E-mail: E.Alexandrou@westernsydney.edu.au
Is Posthospital Syndrome a Result of Hospitalization-Induced Allostatic Overload?
After discharge from the hospital, patients have a significantly elevated risk for adverse events, including emergency department use, hospital readmission, and death. More than 1 in 3 patients discharged from the hospital require acute care in the month after hospital discharge, and more than 1 in 6 require readmission, with readmission diagnoses frequently differing from those of the preceding hospitalization.1-4 This heightened susceptibility to adverse events persists beyond 30 days but levels off by 7 weeks after discharge, suggesting that the period of increased risk is transient and dynamic.5
The term posthospital syndrome (PHS) describes this period of vulnerability to major adverse events following hospitalization.6 In addition to increased risk for readmission and mortality, patients in this period often show evidence of generalized dysfunction with new cognitive impairment, mobility disability, or functional decline.7-12 To date, the etiology of this vulnerability is neither well understood nor effectively addressed by transitional care interventions.13
One hypothesis to explain PHS is that stressors associated with the experience of hospitalization contribute to transient multisystem dysfunction that induces susceptibility to a broad range of medical maladies. These stressors include frequent sleep disruption, noxious sounds, painful stimuli, mobility restrictions, and poor nutrition.12 The stress hypothesis as a cause of PHS is therefore based, in large part, on evidence about allostasis and the deleterious effects of allostatic overload.
Allostasis defines a system functioning within normal stress-response parameters to promote adaptation and survival.14 In allostasis, the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic and parasympathetic branches of the autonomic nervous system (ANS) exist in homeostatic balance and respond to environmental stimuli within a range of healthy physiologic parameters. The hallmark of a system in allostasis is the ability to rapidly activate, then successfully deactivate, a stress response once the stressor (ie, threat) has resolved.14,15 To promote survival and potentiate “fight or flight” mechanisms, an appropriate stress response necessarily impacts multiple physiologic systems that result in hemodynamic augmentation and gluconeogenesis to support the anticipated action of large muscle groups, heightened vigilance and memory capabilities to improve rapid decision-making, and enhancement of innate and adaptive immune capabilities to prepare for wound repair and infection defense.14-16 The stress response is subsequently terminated by negative feedback mechanisms of glucocorticoids as well as a shift of the ANS from sympathetic to parasympathetic tone.17,18
Extended or repetitive stress exposure, however, leads to dysregulation of allostatic mechanisms responsible for stress adaptation and hinders an efficient and effective stress response. After extended stress exposure, baseline (ie, resting) HPA activity resets, causing a disruption of normal diurnal cortisol rhythm and an increase in total cortisol concentration. Moreover, in response to stress, HPA and ANS system excitation becomes impaired, and negative feedback properties are undermined.14,15 This maladaptive state, known as allostatic overload, disrupts the finely tuned mechanisms that are the foundation of mind-body balance and yields pathophysiologic consequences to multiple organ systems. Downstream ramifications of allostatic overload include cognitive deterioration, cardiovascular and immune system dysfunction, and functional decline.14,15,19
Although a stress response is an expected and necessary aspect of acute illness that promotes survival, the central thesis of this work is that additional environmental and social stressors inherent in hospitalization may unnecessarily compound stress and increase the risk of HPA axis dysfunction, allostatic overload, and subsequent multisystem dysfunction, predisposing individuals to adverse outcomes after hospital discharge. Based on data from both human subjects and animal models, we present a possible pathophysiologic mechanism for the postdischarge vulnerability of PHS, encourage critical contemplation of traditional hospitalization, and suggest interventions that might improve outcomes.
POSTHOSPITAL SYNDROME
Posthospital syndrome (PHS) describes a transient period of vulnerability after hospitalization during which patients are at elevated risk for adverse events from a broad range of conditions. In support of this characterization, epidemiologic data have demonstrated high rates of adverse outcomes following hospitalization. For example, data have shown that more than 1 in 6 older adults is readmitted to the hospital within 30 days of discharge.20 Death is also common in this first month, during which rates of postdischarge mortality may exceed initial inpatient mortality.21,22 Elevated vulnerability after hospitalization is not restricted to older adults, as readmission risk among younger patients 18 to 64 years of age may be even higher for selected conditions, such as heart failure.3,23
Vulnerability after hospitalization is broad. In patients over age 65 initially admitted for heart failure or acute myocardial infarction, only 35% and 10% of readmissions are for recurrent heart failure or reinfarction, respectively.1 Nearly half of readmissions are for noncardiovascular causes.1 Similarly, following hospitalization for pneumonia, more than 60 percent of readmissions are for nonpulmonary etiologies. Moreover, the risk for all these causes of readmission is much higher than baseline risk, indicating an extended period of lack of resilience to many types of illness.24 These patterns of broad susceptibility also extend to younger adults hospitalized with common medical conditions.3
Accumulating evidence suggests that hospitalized patients face functional decline, debility, and risk for adverse events despite resolution of the presenting illness, implying perhaps that the hospital environment itself is hazardous to patients’ health. In 1993, Creditor hypothesized that the “hazards of hospitalization,” including enforced bed-rest, sensory deprivation, social isolation, and malnutrition lead to a “cascade of dependency” in which a collection of small insults to multiple organ systems precipitates loss of function and debility despite cure or resolution of presenting illness.12 Covinsky (2011) later defined hospitalization-associated disability as an iatrogenic hospital-related “disorder” characterized by new impairments in abilities to perform basic activities of daily living such as bathing, feeding, toileting, dressing, transferring, and walking at the time of hospital discharge.11 Others have described a postintensive-care syndrome (PICS),25 characterized by cognitive, psychiatric, and physical impairments acquired during hospitalization for critical illness that persist postdischarge and increase the long-term risk for adverse outcomes, including elevated mortality rates,26,27 readmission rates,28 and physical disabilities.29 Similar to the “hazards of hospitalization,” PICS is thought to be related to common experiences of ICU stays, including mobility restriction, sensory deprivation, sleep disruption, sedation, malnutrition, and polypharmacy.30-33
Taken together, these data suggest that adverse health consequences attributable to hospitalization extend across the spectrum of age, presenting disease severity, and hospital treatment location. As detailed below, the PHS hypothesis is rooted in a mechanistic understanding of the role of exogenous stressors in producing physiologic dysregulation and subsequent adverse health effects across multiple organ systems.
Nature of Stress in the Hospital
Compounding the stress of acute illness, hospitalized patients are routinely and repetitively exposed to a wide variety of environmental stressors that may have downstream adverse consequences (Table 1). In the absence of overt clinical manifestations of harm, the possible subclinical physiologic dysfunction generated by the following stress exposures may increase patients’ susceptibility to the manifestations of PHS.
Sleep Disruption
Sleep disruptions trigger potent stress responses,34,35 yet they are common occurrences during hospitalization. In surveys, about half of patients report poor sleep quality during hospitalization that persists for many months after discharge.36 In a simulated hospital setting, test subjects exposed to typical hospital sounds (paging system, machine alarms, etc.) experienced significant sleep-wake cycle abnormalities.37 Although no work has yet focused specifically on the physiologic consequences of sleep disruption and stress in hospitalized patients, in healthy humans, mild sleep disruption has clear effects on allostasis by disrupting HPA activity, raising cortisol levels, diminishing parasympathetic tone, and impairing cognitive performance.18,34,35,38,39
Malnourishment
Malnourishment in hospitalized patients is common, with one-fifth of hospitalized patients receiving nothing per mouth or clear liquid diets for more than 3 continuous days,40 and one-fifth of hospitalized elderly patients receiving less than half of their calculated nutrition requirements.41 Although the relationship between food restriction, cortisol levels, and postdischarge outcomes has not been fully explored, in healthy humans, meal anticipation, meal withdrawal (withholding an expected meal), and self-reported dietary restraint are known to generate stress responses.42,43 Furthermore, malnourishment during hospitalization is associated with increased 90-day and 1-year mortality after discharge,44 adding malnourishment to the list of plausible components of hospital-related stress.
Mobility Restriction
Physical activity counterbalances stress responses and minimizes downstream consequences of allostatic load,15 yet mobility limitations via physical and chemical restraints are common in hospitalized patients, particularly among the elderly.45-47 Many patients are tethered to devices that make ambulation hazardous, such as urinary catheters and infusion pumps. Even without physical or chemical restraints or a limited mobility order, patients may be hesitant to leave the room so as not to miss transport to a diagnostic study or an unscheduled physician’s visit. Indeed, mobility limitations of hospitalized patients increase the risk for adverse events after discharge, while interventions designed to encourage mobility are associated with improved postdischarge outcomes.47,48
Other Stressors
Other hospital-related aversive stimuli are less commonly quantified, but clearly exist. According to surveys of hospitalized patients, sources of emotional stress include social isolation; loss of autonomy and privacy; fear of serious illness; lack of control over activities of daily living; lack of clear communication between treatment team and patients; and death of a patient roommate.49,50 Furthermore, consider the physical discomfort and emotional distress of patients with urinary incontinence awaiting assistance for a diaper or bedding change or the pain of repetitive blood draws or other invasive testing. Although individualized, the subjective discomfort and emotional distress associated with these experiences undoubtedly contribute to the stress of hospitalization.
IMPACT OF ALLOSTATIC OVERLOAD ON PHYSIOLOGIC FUNCTION
Animal Models of Stress
Laboratory techniques reminiscent of the numerous environmental stressors associated with hospitalization have been used to reliably trigger allostatic overload in healthy young animals.51 These techniques include sequential exposure to aversive stimuli, including food and water deprivation, continuous overnight illumination, paired housing with known and unknown cagemates, mobility restriction, soiled cage conditions, and continuous noise. All of these techniques have been shown to cause HPA axis and ANS dysfunction, allostatic overload, and subsequent stress-mediated consequences to multiple organ systems.19,52-54 Given the remarkable similarity of these protocols to common experiences during hospitalization, animal models of stress may be useful in understanding the spectrum of maladaptive consequences experienced by patients within the hospital (Figure 1).
These animal models of stress have resulted in a number of instructive findings. For example, in rodents, extended stress exposure induces structural and functional remodeling of neuronal networks that precipitate learning and memory, working memory, and attention impairments.55-57 These exposures also result in cardiovascular abnormalities, including dyslipidemia, progressive atherosclerosis,58,59 and enhanced inflammatory cytokine expression,60 all of which increase both atherosclerotic burden and susceptibility to plaque rupture, leading to elevated risk for major cardiovascular adverse events. Moreover, these extended stress exposures in animals increase susceptibility to both bacterial and viral infections and increase their severity.16,61 This outcome appears to be driven by a stress-induced elevation of glucocorticoid levels, decreased leukocyte proliferation, altered leukocyte trafficking, and a transition to a proinflammatory cytokine environment.16, 61 Allostatic overload has also been shown to contribute to metabolic dysregulation involving insulin resistance, persistence of hyperglycemia, dyslipidemia, catabolism of lean muscle, and visceral adipose tissue deposition.62-64 In addition to cardiovascular, immune, and metabolic consequences of allostatic overload, the spectrum of physiologic dysfunction in animal models is broad and includes mood disorder symptoms,65 intestinal barrier abnormalities,66 airway reactivity exacerbation,67 and enhanced tumor growth.68
Although the majority of this research highlights the multisystem effects of variable stress exposure in healthy animals, preliminary evidence suggests that aged or diseased animals subjected to additional stressors display a heightened inflammatory cytokine response that contributes to exaggerated sickness behavior and greater and prolonged cognitive deficits.69 Future studies exploring the consequences of extended stress exposure in animals with existing disease or debility may therefore more closely simulate the experience of hospitalized patients and perhaps further our understanding of PHS.
Hospitalized Patients
While no intervention studies have examined the effects of potential hospital stressors on the development of allostatic overload, there is evidence from small studies that dysregulated stress responses during hospitalization are associated with adverse events. For example, high serum cortisol, catecholamine, and proinflammatory cytokine levels during hospitalization have individually been associated with the development of cognitive dysfunction,70-72 increased risk of cardiovascular events such as myocardial infarction and stroke in the year following discharge,73-76 and the development of wound infections after discharge.77 Moreover, elevated plasma glucose during admission for myocardial infarction in patients with or without diabetes has been associated with greater in-hospital and 1-year mortality,78 with a similar relationship seen between elevated plasma glucose and survival after admission for stroke79 and pneumonia.80 Furthermore, in addition to atherothrombosis, stress may contribute to the risk for venous thromboembolism,81 resulting in readmissions for deep vein thrombosis or pulmonary embolism posthospitalization. Although potentially surrogate markers of illness acuity, a handful of studies have shown that these stress biomarkers are actually only weakly correlated with,82 or independent of,72,76 disease severity. As discussed in detail below, future studies utilizing a summative measure of multisystem physiologic dysfunction as opposed to individual biomarkers may more accurately reflect the cumulative stress effects of hospitalization and subsequent risk for adverse events.
Additional Considerations
Elderly patients, in particular, may have heightened susceptibility to the consequences of allostatic overload due to common geriatric issues such as multimorbidity and frailty. Patients with chronic diseases display both baseline HPA axis abnormalities as well as dysregulated stress responses and may therefore be more vulnerable to hospitalization-related stress. For example, when subjected to psychosocial stress, patients with chronic conditions such as diabetes, heart failure, or atherosclerosis demonstrate elevated cortisol levels, increased circulating markers of inflammation, as well as prolonged hemodynamic recovery after stress resolution compared with normal controls.83-85 Additionally, frailty may affect an individual’s susceptibility to exogenous stress. Indeed, frailty identified on hospital admission increases the risk for adverse outcomes during hospitalization and postdischarge.86 Although the specific etiology of this relationship is unclear, persons with frailty are known to have elevated levels of cortisol and other inflammatory markers,87,88 which may contribute to adverse outcomes in the face of additional stressors.
IMPLICATIONS AND NEXT STEPS
A large body of evidence stretching from bench to bedside suggests that environmental stressors associated with hospitalization are toxic. Understanding PHS within the context of hospital-induced allostatic overload presents a unifying theory for the interrelated multisystem dysfunction and increased susceptibility to adverse events that patients experience after discharge (Figure 2). Furthermore, it defines a potential pathophysiological mechanism for the cognitive impairment, elevated cardiovascular risk, immune system dysfunction, metabolic derangements, and functional decline associated with PHS. Additionally, this theory highlights environmental interventions to limit PHS development and suggests mechanisms to promote stress resilience. Although it is difficult to disentangle the consequences of the endogenous stress triggered by an acute illness from the exogenous stressors related to hospitalization, it is likely that the 2 simultaneous exposures compound risk for stress system dysregulation and allostatic overload. Moreover, hospitalized patients with preexisting HPA axis dysfunction at baseline from chronic disease or advancing age may be even more susceptible to these adverse outcomes. If this hypothesis is true, a reduction in PHS would require mitigation of the modifiable environmental stressors encountered by patients during hospitalization. Directed efforts to diminish ambient noise, limit nighttime disruptions, thoughtfully plan procedures, consider ongoing nutritional status, and promote opportunities for patients to exert some control over their environment may diminish the burden of extrinsic stressors encountered by all patients in the hospital and improve outcomes after discharge.
Hospitals are increasingly recognizing the importance of improving patients’ experience of hospitalization by reducing exposure to potential toxicities. For example, many hospitals are now attempting to reduce sleep disturbances and sleep latency through reduced nighttime noise and light levels, fewer nighttime interruptions for vital signs checks and medication administration, and commonsensical interventions like massages, herbal teas, and warm milk prior to bedtime.89 Likewise, intensive care units are targeting environmental and physical stressors with a multifaceted approach to decrease sedative use, promote healthy sleep cycles, and encourage exercise and ambulation even in those patients who are mechanically ventilated.30 Another promising development has been the increase of Hospital at Home programs. In these programs, patients who meet the criteria for inpatient admission are instead comprehensively managed at home for their acute illness through a multidisciplinary effort between physicians, nurses, social workers, physical therapists, and others. Patients hospitalized at home report higher levels of satisfaction and have modest functional gains, improved health-related quality of life, and decreased risk of mortality at 6 months compared with hospitalized patients.90,91 With some admitting diagnoses (eg, heart failure), hospitalization at home may be associated with decreased readmission risk.92 Although not yet investigated on a physiologic level, perhaps the benefits of hospital at home are partially due to the dramatic difference in exposure to environmental stressors.
A tool that quantifies hospital-associated stress may help health providers appreciate the experience of patients and better target interventions to aspects of their structure and process that contribute to allostatic overload. Importantly, allostatic overload cannot be identified by one biomarker of stress but instead requires evidence of dysregulation across inflammatory, neuroendocrine, hormonal, and cardiometabolic systems. Future studies to address the burden of stress faced by hospitalized patients should consider a summative measure of multisystem dysregulation as opposed to isolated assessments of individual biomarkers. Allostatic load has previously been operationalized as the summation of a variety of hemodynamic, hormonal, and metabolic factors, including blood pressure, lipid profile, glycosylated hemoglobin, cortisol, catecholamine levels, and inflammatory markers.93 To develop a hospital-associated allostatic load index, models should ideally be adjusted for acute illness severity, patient-reported stress, and capacity for stress resilience. This tool could then be used to quantify hospitalization-related allostatic load and identify those at greatest risk for adverse events after discharge, as well as measure the effectiveness of strategic environmental interventions (Table 2). A natural first experiment may be a comparison of the allostatic load of hospitalized patients versus those hospitalized at home.
The risk of adverse outcomes after discharge is likely a function of the vulnerability of the patient and the degree to which the patient’s healthcare team and social support network mitigates this vulnerability. That is, there is a risk that a person struggles in the postdischarge period and, in many circumstances, a strong healthcare team and social network can identify health problems early and prevent them from progressing to the point that they require hospitalization.13,94-96 There are also hospital occurrences, outside of allostatic load, that can lead to complications that lengthen the stay, weaken the patient, and directly contribute to subsequent vulnerability.94,97 Our contention is that the allostatic load of hospitalization, which may also vary by patient depending on the circumstances of hospitalization, is just one contributor, albeit potentially an important one, to vulnerability to medical problems after discharge.
In conclusion, a plausible etiology of PHS is the maladaptive mind-body consequences of common stressors during hospitalization that compound the stress of acute illness and produce allostatic overload. This stress-induced dysfunction potentially contributes to a spectrum of generalized disease susceptibility and risk of adverse outcomes after discharge. Focused efforts to diminish patient exposure to hospital-related stressors during and after hospitalization might diminish the presence or severity of PHS. Viewing PHS from this perspective enables the development of hypothesis-driven risk-prediction models, encourages critical contemplation of traditional hospitalization, and suggests that targeted environmental interventions may significantly reduce adverse outcomes.
1. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. http://dx.doi.org/10.1001/jama.2012.216476.
2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. http://dx.doi.org/10.1056/NEJMsa0803563.
3. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11(9):e1001737. http://dx.doi.org/10.1371/journal.pmed.1001737.
4. Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371. http://dx.doi.org/10.1001/jama.2012.216219.
5. Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411. http://dx.doi.org/10.1136/bmj.h411.
6. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. http://dx.doi.org/10.1056/NEJMp1212324.
7. Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175(4):523-529. http://dx.doi.org/10.1001/jamainternmed.2014.7889.
8. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115-2124. http://dx.doi.org/10.1001/jama.292.17.2115.
9. Inouye SK, Zhang Y, Han L, Leo-Summers L, Jones R, Marcantonio E. Recoverable cognitive dysfunction at hospital admission in older persons during acute illness. J Gen Intern Med. 2006;21(12):1276-1281. http://dx.doi.org/10.1111/j.1525-1497.2006.00613.x.
10. Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvements in cognition following hospital discharge of community dwelling seniors. J Gen Intern Med. 2011;26(7):765-770. http://dx.doi.org/10.1007/s11606-011-1681-1.
11. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. http://dx.doi.org/10.1001/jama.2011.1556.
12. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. http://dx.doi.org/10.7326/0003-4819-118-3-199302010-00011.
13. Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3(4):306-315. http://dx.doi.org/10.1007/s13670-014-0103-8.
14. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171-179. http://dx.doi.org/10.1056/NEJM199801153380307.
15. McEwen BS, Gianaros PJ. Stress- and allostasis-induced brain plasticity. Annu Rev Med. 2011;62:431-445. http://dx.doi.org/10.1146/annurev-med-052209-100430.
16. Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16(5):300-317. http://dx.doi.org/10.1159/000216188.
17. Thayer JF, Sternberg E. Beyond heart rate variability: vagal regulation of allostatic systems. Ann N Y Acad Sci. 2006;1088:361-372. http://dx.doi.org/10.1196/annals.1366.014.
18. Jacobson L, Akana SF, Cascio CS, Shinsako J, Dallman MF. Circadian variations in plasma corticosterone permit normal termination of adrenocorticotropin responses to stress. Endocrinology. 1988;122(4):1343-1348. http://dx.doi.org/10.1210/endo-122-4-1343.
19. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873-904. http://dx.doi.org/10.1152/physrev.00041.2006.
20. Medicare Hospital Quality Chartbook 2014: Performance Report on Outcome Measures. Prepared by Yale New Haven Health Services Corporation Center for Outcomes Research and Evaluation for Centers for Medicare & Medicaid Services. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/downloads/medicare-hospital-quality-chartbook-2014.pdf. Accessed February 26, 2018.
21. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303(21):2141-2147. http://dx.doi.org/10.1001/jama.2010.748.
22. Drye EE, Normand SL, Wang Y, et al. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1 Pt 1):19-26. http://dx.doi.org/10.7326/0003-4819-156-1-201201030-00004.
23. Dharmarajan K, Hsieh A, Dreyer RP, Welsh J, Qin L, Krumholz HM. Relationship between age and trajectories of rehospitalization risk in older adults. J Am Geriatr Soc. 2017;65(2):421-426. http://dx.doi.org/10.1111/jgs.14583.
24. Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One. 2016;11(10):e0160492. http://dx.doi.org/10.1371/journal.pone.0160492.
25. Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502-509. http://dx.doi.org/10.1097/CCM.0b013e318232da75.
26. Brinkman S, de Jonge E, Abu-Hanna A, Arbous MS, de Lange DW, de Keizer NF. Mortality after hospital discharge in ICU patients. Crit Care Med. 2013;41(5):1229-1236. http://dx.doi.org/10.1097/CCM.0b013e31827ca4e1.
27. Steenbergen S, Rijkenberg S, Adonis T, Kroeze G, van Stijn I, Endeman H. Long-term treated intensive care patients outcomes: the one-year mortality rate, quality of life, health care use and long-term complications as reported by general practitioners. BMC Anesthesiol. 2015;15:142. http://dx.doi.org/10.1186/s12871-015-0121-x.
28. Hill AD, Fowler RA, Pinto R, Herridge MS, Cuthbertson BH, Scales DC. Long-term outcomes and healthcare utilization following critical illness--a population-based study. Crit Care. 2016;20:76. http://dx.doi.org/10.1186/s13054-016-1248-y.
29. Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369-379. http://dx.doi.org/10.1016/S2213-2600(14)70051-7.
30. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(5):1024-1036. http://dx.doi.org/10.1097/CCM.0000000000000129.
31. Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626-1635. http://dx.doi.org/10.1056/NEJMra1209390.
32. Mendez-Tellez PA, Needham DM. Early physical rehabilitation in the ICU and ventilator liberation. Respir Care. 2012;57(10):1663-1669. http://dx.doi.org/10.4187/respcare.01931.
33. Schweickert WD, Hall J. ICU-acquired weakness. Chest. 2007;131(5):1541-1549. http://dx.doi.org/10.1378/chest.06-2065.
34. Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010;2010:759234. http://dx.doi.org/10.1155/2010/759234.
35. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. http://dx.doi.org/10.1016/S0140-6736(99)01376-8.
36. Orwelius L, Nordlund A, Nordlund P, Edell-Gustafsson U, Sjoberg F. Prevalence of sleep disturbances and long-term reduced health-related quality of life after critical care: a prospective multicenter cohort study. Crit Care. 2008;12(4):R97. http://dx.doi.org/10.1186/cc6973.
37. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. http://dx.doi.org/10.7326/0003-4819-157-3-201208070-00472.
38. Sunbul M, Kanar BG, Durmus E, Kivrak T, Sari I. Acute sleep deprivation is associated with increased arterial stiffness in healthy young adults. Sleep Breath. 2014;18(1):215-220. http://dx.doi.org/10.1007/s11325-013-0873-9.
39. Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117-126. http://dx.doi.org/10.1093/sleep/26.2.117.
40. Franklin GA, McClave SA, Hurt RT, et al. Physician-delivered malnutrition: why do patients receive nothing by mouth or a clear liquid diet in a university hospital setting? JPEN J Parenter Enteral Nutr. 2011;35(3):337-342. http://dx.doi.org/10.1177/0148607110374060.
41. Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA. 1999;281(21):2013-2019. http://dx.doi.org/10.1001/jama.281.21.2013.
42. Anderson DA, Shapiro JR, Lundgren JD, Spataro LE, Frye CA. Self-reported dietary restraint is associated with elevated levels of salivary cortisol. Appetite. 2002;38(1):13-17. http://dx.doi.org/10.1006/appe.2001.0459.
43. Ott V, Friedrich M, Prilop S, et al. Food anticipation and subsequent food withdrawal increase serum cortisol in healthy men. Physiol Behav. 2011;103(5):594-599. http://dx.doi.org/10.1016/j.physbeh.2011.04.020.
44. Covinsky KE, Martin GE, Beyth RJ, Justice AC, Sehgal AR, Landefeld CS. The relationship between clinical assessments of nutritional status and adverse outcomes in older hospitalized medical patients. J Am Geriatr Soc. 1999;47(5):532-538. http://dx.doi.org/10.1111/j.1532-5415.1999.tb02566.x.
45. Lazarus BA, Murphy JB, Coletta EM, McQuade WH, Culpepper L. The provision of physical activity to hospitalized elderly patients. Arch Intern Med. 1991;151(12):2452-2456.
46. Minnick AF, Mion LC, Johnson ME, Catrambone C, Leipzig R. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39(1):30-37. http://dx.doi.org/10.1111/j.1547-5069.2007.00140.x.
47. Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59(2):266-273. http://dx.doi.org/10.1111/j.1532-5415.2010.03276.x.
48. Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338-1344. http://dx.doi.org/10.1056/NEJM199505183322006.
49. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expectations: an international journal of public participation in health care and health policy. 2004;7(1):61-73. http://dx.doi.org/10.1046/j.1369-6513.2003.00251.x.
50. Volicer BJ. Hospital stress and patient reports of pain and physical status. Journal Human Stress. 1978;4(2):28-37. http://dx.doi.org/10.1080/0097840X.1978.9934984.
51. Willner P, Towell A, Sampson D, Sophokleous S, Muscat R. Reduction of sucrose preference by chronic unpredictable mild stress, and its restoration by a tricyclic antidepressant. Psychopharmacology (Berl). 1987;93(3):358-364. http://dx.doi.org/10.1007/BF00187257.
52. Grippo AJ, Francis J, Beltz TG, Felder RB, Johnson AK. Neuroendocrine and cytokine profile of chronic mild stress-induced anhedonia. Physiol Behav. 2005;84(5):697-706. http://dx.doi.org/10.1016/j.physbeh.2005.02.011.
53. Krishnan V, Nestler EJ. Animal models of depression: molecular perspectives. Curr Top Behav Neurosci. 2011;7:121-147. http://dx.doi.org/10.1007/7854_2010_108.
54. Magarinos AM, McEwen BS. Stress-induced atrophy of apical dendrites of hippocampal CA3c neurons: comparison of stressors. Neuroscience. 1995;69(1):83-88. http://dx.doi.org/10.1016/0306-4522(95)00256-I.
55. McEwen BS. Plasticity of the hippocampus: adaptation to chronic stress and allostatic load. Ann N Y Acad Sci. 2001;933:265-277. http://dx.doi.org/10.1111/j.1749-6632.2001.tb05830.x.
56. McEwen BS. The brain on stress: toward an integrative approach to brain, body, and behavior. Perspect Psychol Sci. 2013;8(6):673-675. http://dx.doi.org/10.1177/1745691613506907.
57. McEwen BS, Morrison JH. The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron. 2013;79(1):16-29. http://dx.doi.org/10.1016/j.neuron.2013.06.028.
58. Dutta P, Courties G, Wei Y, et al. Myocardial infarction accelerates atherosclerosis. Nature. 2012;487(7407):325-329. http://dx.doi.org/10.1038/nature11260.
59. Lu XT, Liu YF, Zhang L, et al. Unpredictable chronic mild stress promotes atherosclerosis in high cholesterol-fed rabbits. Psychosom Med. 2012;74(6):604-611. http://dx.doi.org/10.1097/PSY.0b013e31825d0b71.
60. Heidt T, Sager HB, Courties G, et al. Chronic variable stress activates hematopoietic stem cells. Nat Med. 2014;20(7):754-758. http://dx.doi.org/10.1038/nm.3589.
61. Sheridan JF, Feng NG, Bonneau RH, Allen CM, Huneycutt BS, Glaser R. Restraint stress differentially affects anti-viral cellular and humoral immune responses in mice. J Neuroimmunol. 1991;31(3):245-255. http://dx.doi.org/10.1016/0165-5728(91)90046-A.
62. Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009;9(6):787-793. http://dx.doi.org/10.1016/j.coph.2009.08.007.
63. Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30(1):1-10. http://dx.doi.org/10.1016/j.psyneuen.2004.05.007.
64. Tamashiro KL, Sakai RR, Shively CA, Karatsoreos IN, Reagan LP. Chronic stress, metabolism, and metabolic syndrome. Stress. 2011;14(5):468-474. http://dx.doi.org/10.3109/10253890.2011.606341.
65. McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54(3):200-207. http://dx.doi.org/10.1016/S0006-3223(03)00177-X.
66. Zareie M, Johnson-Henry K, Jury J, et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut. 2006;55(11):1553-1560. http://dx.doi.org/10.1136/gut.2005.080739.
67. Joachim RA, Quarcoo D, Arck PC, Herz U, Renz H, Klapp BF. Stress enhances airway reactivity and airway inflammation in an animal model of allergic bronchial asthma. Psychosom Med. 2003;65(5):811-815. http://dx.doi.org/10.1097/01.PSY.0000088582.50468.A3.
68. Thaker PH, Han LY, Kamat AA, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12(8):939-944. http://dx.doi.org/10.1038/nm1447.
69. Schreuder L, Eggen BJ, Biber K, Schoemaker RG, Laman JD, de Rooij SE. Pathophysiological and behavioral effects of systemic inflammation in aged and diseased rodents with relevance to delirium: A systematic review. Brain Behav Immun. 2017;62:362-381. http://dx.doi.org/10.1016/j.bbi.2017.01.010.
70. Mu DL, Li LH, Wang DX, et al. High postoperative serum cortisol level is associated with increased risk of cognitive dysfunction early after coronary artery bypass graft surgery: a prospective cohort study. PLoS One. 2013;8(10):e77637. http://dx.doi.org/10.1371/journal.pone.0077637.
71. Mu DL, Wang DX, Li LH, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. 2010;14(6):R238. http://dx.doi.org/10.1186/cc9393.
72. Nguyen DN, Huyghens L, Zhang H, Schiettecatte J, Smitz J, Vincent JL. Cortisol is an associated-risk factor of brain dysfunction in patients with severe sepsis and septic shock. Biomed Res Int. 2014;2014:712742. http://dx.doi.org/10.1155/2014/712742.
73. Elkind MS, Carty CL, O’Meara ES, et al. Hospitalization for infection and risk of acute ischemic stroke: the Cardiovascular Health Study. Stroke. 2011;42(7):1851-1856. http://dx.doi.org/10.1161/STROKEAHA.110.608588.
74. Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374-1376.
75. Jutla SK, Yuyun MF, Quinn PA, Ng LL. Plasma cortisol and prognosis of patients with acute myocardial infarction. J Cardiovasc Med (Hagerstown). 2014;15(1):33-41. http://dx.doi.org/10.2459/JCM.0b013e328364100b.
76. Yende S, D’Angelo G, Kellum JA, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242-1247. http://dx.doi.org/10.1164/rccm.200712-1777OC.
77. Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011;31(1):81-93. http://dx.doi.org/10.1016/j.iac.2010.09.010.
78. Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773-778. http://dx.doi.org/10.1016/S0140-6736(99)08415-9.
79. O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke. 1991;22(7):842-847. http://dx.doi.org/10.1161/01.STR.22.7.842.
80. Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169(8):910-914. http://dx.doi.org/10.1164/rccm.200310-1448OC.
81. Rosengren A, Freden M, Hansson PO, Wilhelmsen L, Wedel H, Eriksson H. Psychosocial factors and venous thromboembolism: a long-term follow-up study of Swedish men. J Thrombosis Haemostasis. 2008;6(4):558-564. http://dx.doi.org/10.1111/j.1538-7836.2007.02857.x.
82. Oswald GA, Smith CC, Betteridge DJ, Yudkin JS. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. BMJ. 1986;293(6552):917-922. http://dx.doi.org/10.1136/bmj.293.6552.917.
83. Middlekauff HR, Nguyen AH, Negrao CE, et al. Impact of acute mental stress on sympathetic nerve activity and regional blood flow in advanced heart failure: implications for ‘triggering’ adverse cardiac events. Circulation. 1997;96(6):1835-1842. http://dx.doi.org/10.1161/01.CIR.96.6.1835.
84. Nijm J, Jonasson L. Inflammation and cortisol response in coronary artery disease. Ann Med. 2009;41(3):224-233. http://dx.doi.org/10.1080/07853890802508934.
85. Steptoe A, Hackett RA, Lazzarino AI, et al. Disruption of multisystem responses to stress in type 2 diabetes: investigating the dynamics of allostatic load. Proc Natl Acad Sci U S A. 2014;111(44):15693-15698. http://dx.doi.org/10.1073/pnas.1410401111.
86. Sepehri A, Beggs T, Hassan A, et al. The impact of frailty on outcomes after cardiac surgery: a systematic review. J Thorac Cardiovasc Surg. 2014;148(6):3110-3117. http://dx.doi.org/10.1016/j.jtcvs.2014.07.087.
87. Johar H, Emeny RT, Bidlingmaier M, et al. Blunted diurnal cortisol pattern is associated with frailty: a cross-sectional study of 745 participants aged 65 to 90 years. J Clin Endocrinol Metab. 2014;99(3):E464-468. http://dx.doi.org/10.1210/jc.2013-3079.
88. Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med. 2011;27(1):79-87. http://dx.doi.org/10.1016/j.cger.2010.08.002.
89. Hospital Elder Life Program (HELP) for Prevention of Delirium. 2017; http://www.hospitalelderlifeprogram.org/. Accessed February 16, 2018.
90. Shepperd S, Doll H, Angus RM, et al. Admission avoidance hospital at home. Cochrane Database of System Rev. 2008;(4):CD007491. http://dx.doi.org/10.1002/14651858.CD007491.pub2’
91. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatrics Soc. 2009;57(2):273-278. http://dx.doi.org/10.1111/j.1532-5415.2008.02103.x.
92. Qaddoura A, Yazdan-Ashoori P, Kabali C, et al. Efficacy of hospital at home in patients with heart failure: a systematic review and meta-analysis. PloS One. 2015;10(6):e0129282. http://dx.doi.org/10.1371/journal.pone.0129282.
93. Seeman T, Gruenewald T, Karlamangla A, et al. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am J Hum Biol. 2010;22(4):463-472. http://dx.doi.org/10.1002/ajhb.21018.
94. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. http://dx.doi.org/10.1001/jamainternmed.2015.7863.
95. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00008.
96. Takahashi PY, Naessens JM, Peterson SM, et al. Short-term and long-term effectiveness of a post-hospital care transitions program in an older, medically complex population. Healthcare. 2016;4(1):30-35. http://dx.doi.org/10.1016/j.hjdsi.2015.06.006.
 97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
After discharge from the hospital, patients have a significantly elevated risk for adverse events, including emergency department use, hospital readmission, and death. More than 1 in 3 patients discharged from the hospital require acute care in the month after hospital discharge, and more than 1 in 6 require readmission, with readmission diagnoses frequently differing from those of the preceding hospitalization.1-4 This heightened susceptibility to adverse events persists beyond 30 days but levels off by 7 weeks after discharge, suggesting that the period of increased risk is transient and dynamic.5
The term posthospital syndrome (PHS) describes this period of vulnerability to major adverse events following hospitalization.6 In addition to increased risk for readmission and mortality, patients in this period often show evidence of generalized dysfunction with new cognitive impairment, mobility disability, or functional decline.7-12 To date, the etiology of this vulnerability is neither well understood nor effectively addressed by transitional care interventions.13
One hypothesis to explain PHS is that stressors associated with the experience of hospitalization contribute to transient multisystem dysfunction that induces susceptibility to a broad range of medical maladies. These stressors include frequent sleep disruption, noxious sounds, painful stimuli, mobility restrictions, and poor nutrition.12 The stress hypothesis as a cause of PHS is therefore based, in large part, on evidence about allostasis and the deleterious effects of allostatic overload.
Allostasis defines a system functioning within normal stress-response parameters to promote adaptation and survival.14 In allostasis, the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic and parasympathetic branches of the autonomic nervous system (ANS) exist in homeostatic balance and respond to environmental stimuli within a range of healthy physiologic parameters. The hallmark of a system in allostasis is the ability to rapidly activate, then successfully deactivate, a stress response once the stressor (ie, threat) has resolved.14,15 To promote survival and potentiate “fight or flight” mechanisms, an appropriate stress response necessarily impacts multiple physiologic systems that result in hemodynamic augmentation and gluconeogenesis to support the anticipated action of large muscle groups, heightened vigilance and memory capabilities to improve rapid decision-making, and enhancement of innate and adaptive immune capabilities to prepare for wound repair and infection defense.14-16 The stress response is subsequently terminated by negative feedback mechanisms of glucocorticoids as well as a shift of the ANS from sympathetic to parasympathetic tone.17,18
Extended or repetitive stress exposure, however, leads to dysregulation of allostatic mechanisms responsible for stress adaptation and hinders an efficient and effective stress response. After extended stress exposure, baseline (ie, resting) HPA activity resets, causing a disruption of normal diurnal cortisol rhythm and an increase in total cortisol concentration. Moreover, in response to stress, HPA and ANS system excitation becomes impaired, and negative feedback properties are undermined.14,15 This maladaptive state, known as allostatic overload, disrupts the finely tuned mechanisms that are the foundation of mind-body balance and yields pathophysiologic consequences to multiple organ systems. Downstream ramifications of allostatic overload include cognitive deterioration, cardiovascular and immune system dysfunction, and functional decline.14,15,19
Although a stress response is an expected and necessary aspect of acute illness that promotes survival, the central thesis of this work is that additional environmental and social stressors inherent in hospitalization may unnecessarily compound stress and increase the risk of HPA axis dysfunction, allostatic overload, and subsequent multisystem dysfunction, predisposing individuals to adverse outcomes after hospital discharge. Based on data from both human subjects and animal models, we present a possible pathophysiologic mechanism for the postdischarge vulnerability of PHS, encourage critical contemplation of traditional hospitalization, and suggest interventions that might improve outcomes.
POSTHOSPITAL SYNDROME
Posthospital syndrome (PHS) describes a transient period of vulnerability after hospitalization during which patients are at elevated risk for adverse events from a broad range of conditions. In support of this characterization, epidemiologic data have demonstrated high rates of adverse outcomes following hospitalization. For example, data have shown that more than 1 in 6 older adults is readmitted to the hospital within 30 days of discharge.20 Death is also common in this first month, during which rates of postdischarge mortality may exceed initial inpatient mortality.21,22 Elevated vulnerability after hospitalization is not restricted to older adults, as readmission risk among younger patients 18 to 64 years of age may be even higher for selected conditions, such as heart failure.3,23
Vulnerability after hospitalization is broad. In patients over age 65 initially admitted for heart failure or acute myocardial infarction, only 35% and 10% of readmissions are for recurrent heart failure or reinfarction, respectively.1 Nearly half of readmissions are for noncardiovascular causes.1 Similarly, following hospitalization for pneumonia, more than 60 percent of readmissions are for nonpulmonary etiologies. Moreover, the risk for all these causes of readmission is much higher than baseline risk, indicating an extended period of lack of resilience to many types of illness.24 These patterns of broad susceptibility also extend to younger adults hospitalized with common medical conditions.3
Accumulating evidence suggests that hospitalized patients face functional decline, debility, and risk for adverse events despite resolution of the presenting illness, implying perhaps that the hospital environment itself is hazardous to patients’ health. In 1993, Creditor hypothesized that the “hazards of hospitalization,” including enforced bed-rest, sensory deprivation, social isolation, and malnutrition lead to a “cascade of dependency” in which a collection of small insults to multiple organ systems precipitates loss of function and debility despite cure or resolution of presenting illness.12 Covinsky (2011) later defined hospitalization-associated disability as an iatrogenic hospital-related “disorder” characterized by new impairments in abilities to perform basic activities of daily living such as bathing, feeding, toileting, dressing, transferring, and walking at the time of hospital discharge.11 Others have described a postintensive-care syndrome (PICS),25 characterized by cognitive, psychiatric, and physical impairments acquired during hospitalization for critical illness that persist postdischarge and increase the long-term risk for adverse outcomes, including elevated mortality rates,26,27 readmission rates,28 and physical disabilities.29 Similar to the “hazards of hospitalization,” PICS is thought to be related to common experiences of ICU stays, including mobility restriction, sensory deprivation, sleep disruption, sedation, malnutrition, and polypharmacy.30-33
Taken together, these data suggest that adverse health consequences attributable to hospitalization extend across the spectrum of age, presenting disease severity, and hospital treatment location. As detailed below, the PHS hypothesis is rooted in a mechanistic understanding of the role of exogenous stressors in producing physiologic dysregulation and subsequent adverse health effects across multiple organ systems.
Nature of Stress in the Hospital
Compounding the stress of acute illness, hospitalized patients are routinely and repetitively exposed to a wide variety of environmental stressors that may have downstream adverse consequences (Table 1). In the absence of overt clinical manifestations of harm, the possible subclinical physiologic dysfunction generated by the following stress exposures may increase patients’ susceptibility to the manifestations of PHS.
Sleep Disruption
Sleep disruptions trigger potent stress responses,34,35 yet they are common occurrences during hospitalization. In surveys, about half of patients report poor sleep quality during hospitalization that persists for many months after discharge.36 In a simulated hospital setting, test subjects exposed to typical hospital sounds (paging system, machine alarms, etc.) experienced significant sleep-wake cycle abnormalities.37 Although no work has yet focused specifically on the physiologic consequences of sleep disruption and stress in hospitalized patients, in healthy humans, mild sleep disruption has clear effects on allostasis by disrupting HPA activity, raising cortisol levels, diminishing parasympathetic tone, and impairing cognitive performance.18,34,35,38,39
Malnourishment
Malnourishment in hospitalized patients is common, with one-fifth of hospitalized patients receiving nothing per mouth or clear liquid diets for more than 3 continuous days,40 and one-fifth of hospitalized elderly patients receiving less than half of their calculated nutrition requirements.41 Although the relationship between food restriction, cortisol levels, and postdischarge outcomes has not been fully explored, in healthy humans, meal anticipation, meal withdrawal (withholding an expected meal), and self-reported dietary restraint are known to generate stress responses.42,43 Furthermore, malnourishment during hospitalization is associated with increased 90-day and 1-year mortality after discharge,44 adding malnourishment to the list of plausible components of hospital-related stress.
Mobility Restriction
Physical activity counterbalances stress responses and minimizes downstream consequences of allostatic load,15 yet mobility limitations via physical and chemical restraints are common in hospitalized patients, particularly among the elderly.45-47 Many patients are tethered to devices that make ambulation hazardous, such as urinary catheters and infusion pumps. Even without physical or chemical restraints or a limited mobility order, patients may be hesitant to leave the room so as not to miss transport to a diagnostic study or an unscheduled physician’s visit. Indeed, mobility limitations of hospitalized patients increase the risk for adverse events after discharge, while interventions designed to encourage mobility are associated with improved postdischarge outcomes.47,48
Other Stressors
Other hospital-related aversive stimuli are less commonly quantified, but clearly exist. According to surveys of hospitalized patients, sources of emotional stress include social isolation; loss of autonomy and privacy; fear of serious illness; lack of control over activities of daily living; lack of clear communication between treatment team and patients; and death of a patient roommate.49,50 Furthermore, consider the physical discomfort and emotional distress of patients with urinary incontinence awaiting assistance for a diaper or bedding change or the pain of repetitive blood draws or other invasive testing. Although individualized, the subjective discomfort and emotional distress associated with these experiences undoubtedly contribute to the stress of hospitalization.
IMPACT OF ALLOSTATIC OVERLOAD ON PHYSIOLOGIC FUNCTION
Animal Models of Stress
Laboratory techniques reminiscent of the numerous environmental stressors associated with hospitalization have been used to reliably trigger allostatic overload in healthy young animals.51 These techniques include sequential exposure to aversive stimuli, including food and water deprivation, continuous overnight illumination, paired housing with known and unknown cagemates, mobility restriction, soiled cage conditions, and continuous noise. All of these techniques have been shown to cause HPA axis and ANS dysfunction, allostatic overload, and subsequent stress-mediated consequences to multiple organ systems.19,52-54 Given the remarkable similarity of these protocols to common experiences during hospitalization, animal models of stress may be useful in understanding the spectrum of maladaptive consequences experienced by patients within the hospital (Figure 1).
These animal models of stress have resulted in a number of instructive findings. For example, in rodents, extended stress exposure induces structural and functional remodeling of neuronal networks that precipitate learning and memory, working memory, and attention impairments.55-57 These exposures also result in cardiovascular abnormalities, including dyslipidemia, progressive atherosclerosis,58,59 and enhanced inflammatory cytokine expression,60 all of which increase both atherosclerotic burden and susceptibility to plaque rupture, leading to elevated risk for major cardiovascular adverse events. Moreover, these extended stress exposures in animals increase susceptibility to both bacterial and viral infections and increase their severity.16,61 This outcome appears to be driven by a stress-induced elevation of glucocorticoid levels, decreased leukocyte proliferation, altered leukocyte trafficking, and a transition to a proinflammatory cytokine environment.16, 61 Allostatic overload has also been shown to contribute to metabolic dysregulation involving insulin resistance, persistence of hyperglycemia, dyslipidemia, catabolism of lean muscle, and visceral adipose tissue deposition.62-64 In addition to cardiovascular, immune, and metabolic consequences of allostatic overload, the spectrum of physiologic dysfunction in animal models is broad and includes mood disorder symptoms,65 intestinal barrier abnormalities,66 airway reactivity exacerbation,67 and enhanced tumor growth.68
Although the majority of this research highlights the multisystem effects of variable stress exposure in healthy animals, preliminary evidence suggests that aged or diseased animals subjected to additional stressors display a heightened inflammatory cytokine response that contributes to exaggerated sickness behavior and greater and prolonged cognitive deficits.69 Future studies exploring the consequences of extended stress exposure in animals with existing disease or debility may therefore more closely simulate the experience of hospitalized patients and perhaps further our understanding of PHS.
Hospitalized Patients
While no intervention studies have examined the effects of potential hospital stressors on the development of allostatic overload, there is evidence from small studies that dysregulated stress responses during hospitalization are associated with adverse events. For example, high serum cortisol, catecholamine, and proinflammatory cytokine levels during hospitalization have individually been associated with the development of cognitive dysfunction,70-72 increased risk of cardiovascular events such as myocardial infarction and stroke in the year following discharge,73-76 and the development of wound infections after discharge.77 Moreover, elevated plasma glucose during admission for myocardial infarction in patients with or without diabetes has been associated with greater in-hospital and 1-year mortality,78 with a similar relationship seen between elevated plasma glucose and survival after admission for stroke79 and pneumonia.80 Furthermore, in addition to atherothrombosis, stress may contribute to the risk for venous thromboembolism,81 resulting in readmissions for deep vein thrombosis or pulmonary embolism posthospitalization. Although potentially surrogate markers of illness acuity, a handful of studies have shown that these stress biomarkers are actually only weakly correlated with,82 or independent of,72,76 disease severity. As discussed in detail below, future studies utilizing a summative measure of multisystem physiologic dysfunction as opposed to individual biomarkers may more accurately reflect the cumulative stress effects of hospitalization and subsequent risk for adverse events.
Additional Considerations
Elderly patients, in particular, may have heightened susceptibility to the consequences of allostatic overload due to common geriatric issues such as multimorbidity and frailty. Patients with chronic diseases display both baseline HPA axis abnormalities as well as dysregulated stress responses and may therefore be more vulnerable to hospitalization-related stress. For example, when subjected to psychosocial stress, patients with chronic conditions such as diabetes, heart failure, or atherosclerosis demonstrate elevated cortisol levels, increased circulating markers of inflammation, as well as prolonged hemodynamic recovery after stress resolution compared with normal controls.83-85 Additionally, frailty may affect an individual’s susceptibility to exogenous stress. Indeed, frailty identified on hospital admission increases the risk for adverse outcomes during hospitalization and postdischarge.86 Although the specific etiology of this relationship is unclear, persons with frailty are known to have elevated levels of cortisol and other inflammatory markers,87,88 which may contribute to adverse outcomes in the face of additional stressors.
IMPLICATIONS AND NEXT STEPS
A large body of evidence stretching from bench to bedside suggests that environmental stressors associated with hospitalization are toxic. Understanding PHS within the context of hospital-induced allostatic overload presents a unifying theory for the interrelated multisystem dysfunction and increased susceptibility to adverse events that patients experience after discharge (Figure 2). Furthermore, it defines a potential pathophysiological mechanism for the cognitive impairment, elevated cardiovascular risk, immune system dysfunction, metabolic derangements, and functional decline associated with PHS. Additionally, this theory highlights environmental interventions to limit PHS development and suggests mechanisms to promote stress resilience. Although it is difficult to disentangle the consequences of the endogenous stress triggered by an acute illness from the exogenous stressors related to hospitalization, it is likely that the 2 simultaneous exposures compound risk for stress system dysregulation and allostatic overload. Moreover, hospitalized patients with preexisting HPA axis dysfunction at baseline from chronic disease or advancing age may be even more susceptible to these adverse outcomes. If this hypothesis is true, a reduction in PHS would require mitigation of the modifiable environmental stressors encountered by patients during hospitalization. Directed efforts to diminish ambient noise, limit nighttime disruptions, thoughtfully plan procedures, consider ongoing nutritional status, and promote opportunities for patients to exert some control over their environment may diminish the burden of extrinsic stressors encountered by all patients in the hospital and improve outcomes after discharge.
Hospitals are increasingly recognizing the importance of improving patients’ experience of hospitalization by reducing exposure to potential toxicities. For example, many hospitals are now attempting to reduce sleep disturbances and sleep latency through reduced nighttime noise and light levels, fewer nighttime interruptions for vital signs checks and medication administration, and commonsensical interventions like massages, herbal teas, and warm milk prior to bedtime.89 Likewise, intensive care units are targeting environmental and physical stressors with a multifaceted approach to decrease sedative use, promote healthy sleep cycles, and encourage exercise and ambulation even in those patients who are mechanically ventilated.30 Another promising development has been the increase of Hospital at Home programs. In these programs, patients who meet the criteria for inpatient admission are instead comprehensively managed at home for their acute illness through a multidisciplinary effort between physicians, nurses, social workers, physical therapists, and others. Patients hospitalized at home report higher levels of satisfaction and have modest functional gains, improved health-related quality of life, and decreased risk of mortality at 6 months compared with hospitalized patients.90,91 With some admitting diagnoses (eg, heart failure), hospitalization at home may be associated with decreased readmission risk.92 Although not yet investigated on a physiologic level, perhaps the benefits of hospital at home are partially due to the dramatic difference in exposure to environmental stressors.
A tool that quantifies hospital-associated stress may help health providers appreciate the experience of patients and better target interventions to aspects of their structure and process that contribute to allostatic overload. Importantly, allostatic overload cannot be identified by one biomarker of stress but instead requires evidence of dysregulation across inflammatory, neuroendocrine, hormonal, and cardiometabolic systems. Future studies to address the burden of stress faced by hospitalized patients should consider a summative measure of multisystem dysregulation as opposed to isolated assessments of individual biomarkers. Allostatic load has previously been operationalized as the summation of a variety of hemodynamic, hormonal, and metabolic factors, including blood pressure, lipid profile, glycosylated hemoglobin, cortisol, catecholamine levels, and inflammatory markers.93 To develop a hospital-associated allostatic load index, models should ideally be adjusted for acute illness severity, patient-reported stress, and capacity for stress resilience. This tool could then be used to quantify hospitalization-related allostatic load and identify those at greatest risk for adverse events after discharge, as well as measure the effectiveness of strategic environmental interventions (Table 2). A natural first experiment may be a comparison of the allostatic load of hospitalized patients versus those hospitalized at home.
The risk of adverse outcomes after discharge is likely a function of the vulnerability of the patient and the degree to which the patient’s healthcare team and social support network mitigates this vulnerability. That is, there is a risk that a person struggles in the postdischarge period and, in many circumstances, a strong healthcare team and social network can identify health problems early and prevent them from progressing to the point that they require hospitalization.13,94-96 There are also hospital occurrences, outside of allostatic load, that can lead to complications that lengthen the stay, weaken the patient, and directly contribute to subsequent vulnerability.94,97 Our contention is that the allostatic load of hospitalization, which may also vary by patient depending on the circumstances of hospitalization, is just one contributor, albeit potentially an important one, to vulnerability to medical problems after discharge.
In conclusion, a plausible etiology of PHS is the maladaptive mind-body consequences of common stressors during hospitalization that compound the stress of acute illness and produce allostatic overload. This stress-induced dysfunction potentially contributes to a spectrum of generalized disease susceptibility and risk of adverse outcomes after discharge. Focused efforts to diminish patient exposure to hospital-related stressors during and after hospitalization might diminish the presence or severity of PHS. Viewing PHS from this perspective enables the development of hypothesis-driven risk-prediction models, encourages critical contemplation of traditional hospitalization, and suggests that targeted environmental interventions may significantly reduce adverse outcomes.
After discharge from the hospital, patients have a significantly elevated risk for adverse events, including emergency department use, hospital readmission, and death. More than 1 in 3 patients discharged from the hospital require acute care in the month after hospital discharge, and more than 1 in 6 require readmission, with readmission diagnoses frequently differing from those of the preceding hospitalization.1-4 This heightened susceptibility to adverse events persists beyond 30 days but levels off by 7 weeks after discharge, suggesting that the period of increased risk is transient and dynamic.5
The term posthospital syndrome (PHS) describes this period of vulnerability to major adverse events following hospitalization.6 In addition to increased risk for readmission and mortality, patients in this period often show evidence of generalized dysfunction with new cognitive impairment, mobility disability, or functional decline.7-12 To date, the etiology of this vulnerability is neither well understood nor effectively addressed by transitional care interventions.13
One hypothesis to explain PHS is that stressors associated with the experience of hospitalization contribute to transient multisystem dysfunction that induces susceptibility to a broad range of medical maladies. These stressors include frequent sleep disruption, noxious sounds, painful stimuli, mobility restrictions, and poor nutrition.12 The stress hypothesis as a cause of PHS is therefore based, in large part, on evidence about allostasis and the deleterious effects of allostatic overload.
Allostasis defines a system functioning within normal stress-response parameters to promote adaptation and survival.14 In allostasis, the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic and parasympathetic branches of the autonomic nervous system (ANS) exist in homeostatic balance and respond to environmental stimuli within a range of healthy physiologic parameters. The hallmark of a system in allostasis is the ability to rapidly activate, then successfully deactivate, a stress response once the stressor (ie, threat) has resolved.14,15 To promote survival and potentiate “fight or flight” mechanisms, an appropriate stress response necessarily impacts multiple physiologic systems that result in hemodynamic augmentation and gluconeogenesis to support the anticipated action of large muscle groups, heightened vigilance and memory capabilities to improve rapid decision-making, and enhancement of innate and adaptive immune capabilities to prepare for wound repair and infection defense.14-16 The stress response is subsequently terminated by negative feedback mechanisms of glucocorticoids as well as a shift of the ANS from sympathetic to parasympathetic tone.17,18
Extended or repetitive stress exposure, however, leads to dysregulation of allostatic mechanisms responsible for stress adaptation and hinders an efficient and effective stress response. After extended stress exposure, baseline (ie, resting) HPA activity resets, causing a disruption of normal diurnal cortisol rhythm and an increase in total cortisol concentration. Moreover, in response to stress, HPA and ANS system excitation becomes impaired, and negative feedback properties are undermined.14,15 This maladaptive state, known as allostatic overload, disrupts the finely tuned mechanisms that are the foundation of mind-body balance and yields pathophysiologic consequences to multiple organ systems. Downstream ramifications of allostatic overload include cognitive deterioration, cardiovascular and immune system dysfunction, and functional decline.14,15,19
Although a stress response is an expected and necessary aspect of acute illness that promotes survival, the central thesis of this work is that additional environmental and social stressors inherent in hospitalization may unnecessarily compound stress and increase the risk of HPA axis dysfunction, allostatic overload, and subsequent multisystem dysfunction, predisposing individuals to adverse outcomes after hospital discharge. Based on data from both human subjects and animal models, we present a possible pathophysiologic mechanism for the postdischarge vulnerability of PHS, encourage critical contemplation of traditional hospitalization, and suggest interventions that might improve outcomes.
POSTHOSPITAL SYNDROME
Posthospital syndrome (PHS) describes a transient period of vulnerability after hospitalization during which patients are at elevated risk for adverse events from a broad range of conditions. In support of this characterization, epidemiologic data have demonstrated high rates of adverse outcomes following hospitalization. For example, data have shown that more than 1 in 6 older adults is readmitted to the hospital within 30 days of discharge.20 Death is also common in this first month, during which rates of postdischarge mortality may exceed initial inpatient mortality.21,22 Elevated vulnerability after hospitalization is not restricted to older adults, as readmission risk among younger patients 18 to 64 years of age may be even higher for selected conditions, such as heart failure.3,23
Vulnerability after hospitalization is broad. In patients over age 65 initially admitted for heart failure or acute myocardial infarction, only 35% and 10% of readmissions are for recurrent heart failure or reinfarction, respectively.1 Nearly half of readmissions are for noncardiovascular causes.1 Similarly, following hospitalization for pneumonia, more than 60 percent of readmissions are for nonpulmonary etiologies. Moreover, the risk for all these causes of readmission is much higher than baseline risk, indicating an extended period of lack of resilience to many types of illness.24 These patterns of broad susceptibility also extend to younger adults hospitalized with common medical conditions.3
Accumulating evidence suggests that hospitalized patients face functional decline, debility, and risk for adverse events despite resolution of the presenting illness, implying perhaps that the hospital environment itself is hazardous to patients’ health. In 1993, Creditor hypothesized that the “hazards of hospitalization,” including enforced bed-rest, sensory deprivation, social isolation, and malnutrition lead to a “cascade of dependency” in which a collection of small insults to multiple organ systems precipitates loss of function and debility despite cure or resolution of presenting illness.12 Covinsky (2011) later defined hospitalization-associated disability as an iatrogenic hospital-related “disorder” characterized by new impairments in abilities to perform basic activities of daily living such as bathing, feeding, toileting, dressing, transferring, and walking at the time of hospital discharge.11 Others have described a postintensive-care syndrome (PICS),25 characterized by cognitive, psychiatric, and physical impairments acquired during hospitalization for critical illness that persist postdischarge and increase the long-term risk for adverse outcomes, including elevated mortality rates,26,27 readmission rates,28 and physical disabilities.29 Similar to the “hazards of hospitalization,” PICS is thought to be related to common experiences of ICU stays, including mobility restriction, sensory deprivation, sleep disruption, sedation, malnutrition, and polypharmacy.30-33
Taken together, these data suggest that adverse health consequences attributable to hospitalization extend across the spectrum of age, presenting disease severity, and hospital treatment location. As detailed below, the PHS hypothesis is rooted in a mechanistic understanding of the role of exogenous stressors in producing physiologic dysregulation and subsequent adverse health effects across multiple organ systems.
Nature of Stress in the Hospital
Compounding the stress of acute illness, hospitalized patients are routinely and repetitively exposed to a wide variety of environmental stressors that may have downstream adverse consequences (Table 1). In the absence of overt clinical manifestations of harm, the possible subclinical physiologic dysfunction generated by the following stress exposures may increase patients’ susceptibility to the manifestations of PHS.
Sleep Disruption
Sleep disruptions trigger potent stress responses,34,35 yet they are common occurrences during hospitalization. In surveys, about half of patients report poor sleep quality during hospitalization that persists for many months after discharge.36 In a simulated hospital setting, test subjects exposed to typical hospital sounds (paging system, machine alarms, etc.) experienced significant sleep-wake cycle abnormalities.37 Although no work has yet focused specifically on the physiologic consequences of sleep disruption and stress in hospitalized patients, in healthy humans, mild sleep disruption has clear effects on allostasis by disrupting HPA activity, raising cortisol levels, diminishing parasympathetic tone, and impairing cognitive performance.18,34,35,38,39
Malnourishment
Malnourishment in hospitalized patients is common, with one-fifth of hospitalized patients receiving nothing per mouth or clear liquid diets for more than 3 continuous days,40 and one-fifth of hospitalized elderly patients receiving less than half of their calculated nutrition requirements.41 Although the relationship between food restriction, cortisol levels, and postdischarge outcomes has not been fully explored, in healthy humans, meal anticipation, meal withdrawal (withholding an expected meal), and self-reported dietary restraint are known to generate stress responses.42,43 Furthermore, malnourishment during hospitalization is associated with increased 90-day and 1-year mortality after discharge,44 adding malnourishment to the list of plausible components of hospital-related stress.
Mobility Restriction
Physical activity counterbalances stress responses and minimizes downstream consequences of allostatic load,15 yet mobility limitations via physical and chemical restraints are common in hospitalized patients, particularly among the elderly.45-47 Many patients are tethered to devices that make ambulation hazardous, such as urinary catheters and infusion pumps. Even without physical or chemical restraints or a limited mobility order, patients may be hesitant to leave the room so as not to miss transport to a diagnostic study or an unscheduled physician’s visit. Indeed, mobility limitations of hospitalized patients increase the risk for adverse events after discharge, while interventions designed to encourage mobility are associated with improved postdischarge outcomes.47,48
Other Stressors
Other hospital-related aversive stimuli are less commonly quantified, but clearly exist. According to surveys of hospitalized patients, sources of emotional stress include social isolation; loss of autonomy and privacy; fear of serious illness; lack of control over activities of daily living; lack of clear communication between treatment team and patients; and death of a patient roommate.49,50 Furthermore, consider the physical discomfort and emotional distress of patients with urinary incontinence awaiting assistance for a diaper or bedding change or the pain of repetitive blood draws or other invasive testing. Although individualized, the subjective discomfort and emotional distress associated with these experiences undoubtedly contribute to the stress of hospitalization.
IMPACT OF ALLOSTATIC OVERLOAD ON PHYSIOLOGIC FUNCTION
Animal Models of Stress
Laboratory techniques reminiscent of the numerous environmental stressors associated with hospitalization have been used to reliably trigger allostatic overload in healthy young animals.51 These techniques include sequential exposure to aversive stimuli, including food and water deprivation, continuous overnight illumination, paired housing with known and unknown cagemates, mobility restriction, soiled cage conditions, and continuous noise. All of these techniques have been shown to cause HPA axis and ANS dysfunction, allostatic overload, and subsequent stress-mediated consequences to multiple organ systems.19,52-54 Given the remarkable similarity of these protocols to common experiences during hospitalization, animal models of stress may be useful in understanding the spectrum of maladaptive consequences experienced by patients within the hospital (Figure 1).
These animal models of stress have resulted in a number of instructive findings. For example, in rodents, extended stress exposure induces structural and functional remodeling of neuronal networks that precipitate learning and memory, working memory, and attention impairments.55-57 These exposures also result in cardiovascular abnormalities, including dyslipidemia, progressive atherosclerosis,58,59 and enhanced inflammatory cytokine expression,60 all of which increase both atherosclerotic burden and susceptibility to plaque rupture, leading to elevated risk for major cardiovascular adverse events. Moreover, these extended stress exposures in animals increase susceptibility to both bacterial and viral infections and increase their severity.16,61 This outcome appears to be driven by a stress-induced elevation of glucocorticoid levels, decreased leukocyte proliferation, altered leukocyte trafficking, and a transition to a proinflammatory cytokine environment.16, 61 Allostatic overload has also been shown to contribute to metabolic dysregulation involving insulin resistance, persistence of hyperglycemia, dyslipidemia, catabolism of lean muscle, and visceral adipose tissue deposition.62-64 In addition to cardiovascular, immune, and metabolic consequences of allostatic overload, the spectrum of physiologic dysfunction in animal models is broad and includes mood disorder symptoms,65 intestinal barrier abnormalities,66 airway reactivity exacerbation,67 and enhanced tumor growth.68
Although the majority of this research highlights the multisystem effects of variable stress exposure in healthy animals, preliminary evidence suggests that aged or diseased animals subjected to additional stressors display a heightened inflammatory cytokine response that contributes to exaggerated sickness behavior and greater and prolonged cognitive deficits.69 Future studies exploring the consequences of extended stress exposure in animals with existing disease or debility may therefore more closely simulate the experience of hospitalized patients and perhaps further our understanding of PHS.
Hospitalized Patients
While no intervention studies have examined the effects of potential hospital stressors on the development of allostatic overload, there is evidence from small studies that dysregulated stress responses during hospitalization are associated with adverse events. For example, high serum cortisol, catecholamine, and proinflammatory cytokine levels during hospitalization have individually been associated with the development of cognitive dysfunction,70-72 increased risk of cardiovascular events such as myocardial infarction and stroke in the year following discharge,73-76 and the development of wound infections after discharge.77 Moreover, elevated plasma glucose during admission for myocardial infarction in patients with or without diabetes has been associated with greater in-hospital and 1-year mortality,78 with a similar relationship seen between elevated plasma glucose and survival after admission for stroke79 and pneumonia.80 Furthermore, in addition to atherothrombosis, stress may contribute to the risk for venous thromboembolism,81 resulting in readmissions for deep vein thrombosis or pulmonary embolism posthospitalization. Although potentially surrogate markers of illness acuity, a handful of studies have shown that these stress biomarkers are actually only weakly correlated with,82 or independent of,72,76 disease severity. As discussed in detail below, future studies utilizing a summative measure of multisystem physiologic dysfunction as opposed to individual biomarkers may more accurately reflect the cumulative stress effects of hospitalization and subsequent risk for adverse events.
Additional Considerations
Elderly patients, in particular, may have heightened susceptibility to the consequences of allostatic overload due to common geriatric issues such as multimorbidity and frailty. Patients with chronic diseases display both baseline HPA axis abnormalities as well as dysregulated stress responses and may therefore be more vulnerable to hospitalization-related stress. For example, when subjected to psychosocial stress, patients with chronic conditions such as diabetes, heart failure, or atherosclerosis demonstrate elevated cortisol levels, increased circulating markers of inflammation, as well as prolonged hemodynamic recovery after stress resolution compared with normal controls.83-85 Additionally, frailty may affect an individual’s susceptibility to exogenous stress. Indeed, frailty identified on hospital admission increases the risk for adverse outcomes during hospitalization and postdischarge.86 Although the specific etiology of this relationship is unclear, persons with frailty are known to have elevated levels of cortisol and other inflammatory markers,87,88 which may contribute to adverse outcomes in the face of additional stressors.
IMPLICATIONS AND NEXT STEPS
A large body of evidence stretching from bench to bedside suggests that environmental stressors associated with hospitalization are toxic. Understanding PHS within the context of hospital-induced allostatic overload presents a unifying theory for the interrelated multisystem dysfunction and increased susceptibility to adverse events that patients experience after discharge (Figure 2). Furthermore, it defines a potential pathophysiological mechanism for the cognitive impairment, elevated cardiovascular risk, immune system dysfunction, metabolic derangements, and functional decline associated with PHS. Additionally, this theory highlights environmental interventions to limit PHS development and suggests mechanisms to promote stress resilience. Although it is difficult to disentangle the consequences of the endogenous stress triggered by an acute illness from the exogenous stressors related to hospitalization, it is likely that the 2 simultaneous exposures compound risk for stress system dysregulation and allostatic overload. Moreover, hospitalized patients with preexisting HPA axis dysfunction at baseline from chronic disease or advancing age may be even more susceptible to these adverse outcomes. If this hypothesis is true, a reduction in PHS would require mitigation of the modifiable environmental stressors encountered by patients during hospitalization. Directed efforts to diminish ambient noise, limit nighttime disruptions, thoughtfully plan procedures, consider ongoing nutritional status, and promote opportunities for patients to exert some control over their environment may diminish the burden of extrinsic stressors encountered by all patients in the hospital and improve outcomes after discharge.
Hospitals are increasingly recognizing the importance of improving patients’ experience of hospitalization by reducing exposure to potential toxicities. For example, many hospitals are now attempting to reduce sleep disturbances and sleep latency through reduced nighttime noise and light levels, fewer nighttime interruptions for vital signs checks and medication administration, and commonsensical interventions like massages, herbal teas, and warm milk prior to bedtime.89 Likewise, intensive care units are targeting environmental and physical stressors with a multifaceted approach to decrease sedative use, promote healthy sleep cycles, and encourage exercise and ambulation even in those patients who are mechanically ventilated.30 Another promising development has been the increase of Hospital at Home programs. In these programs, patients who meet the criteria for inpatient admission are instead comprehensively managed at home for their acute illness through a multidisciplinary effort between physicians, nurses, social workers, physical therapists, and others. Patients hospitalized at home report higher levels of satisfaction and have modest functional gains, improved health-related quality of life, and decreased risk of mortality at 6 months compared with hospitalized patients.90,91 With some admitting diagnoses (eg, heart failure), hospitalization at home may be associated with decreased readmission risk.92 Although not yet investigated on a physiologic level, perhaps the benefits of hospital at home are partially due to the dramatic difference in exposure to environmental stressors.
A tool that quantifies hospital-associated stress may help health providers appreciate the experience of patients and better target interventions to aspects of their structure and process that contribute to allostatic overload. Importantly, allostatic overload cannot be identified by one biomarker of stress but instead requires evidence of dysregulation across inflammatory, neuroendocrine, hormonal, and cardiometabolic systems. Future studies to address the burden of stress faced by hospitalized patients should consider a summative measure of multisystem dysregulation as opposed to isolated assessments of individual biomarkers. Allostatic load has previously been operationalized as the summation of a variety of hemodynamic, hormonal, and metabolic factors, including blood pressure, lipid profile, glycosylated hemoglobin, cortisol, catecholamine levels, and inflammatory markers.93 To develop a hospital-associated allostatic load index, models should ideally be adjusted for acute illness severity, patient-reported stress, and capacity for stress resilience. This tool could then be used to quantify hospitalization-related allostatic load and identify those at greatest risk for adverse events after discharge, as well as measure the effectiveness of strategic environmental interventions (Table 2). A natural first experiment may be a comparison of the allostatic load of hospitalized patients versus those hospitalized at home.
The risk of adverse outcomes after discharge is likely a function of the vulnerability of the patient and the degree to which the patient’s healthcare team and social support network mitigates this vulnerability. That is, there is a risk that a person struggles in the postdischarge period and, in many circumstances, a strong healthcare team and social network can identify health problems early and prevent them from progressing to the point that they require hospitalization.13,94-96 There are also hospital occurrences, outside of allostatic load, that can lead to complications that lengthen the stay, weaken the patient, and directly contribute to subsequent vulnerability.94,97 Our contention is that the allostatic load of hospitalization, which may also vary by patient depending on the circumstances of hospitalization, is just one contributor, albeit potentially an important one, to vulnerability to medical problems after discharge.
In conclusion, a plausible etiology of PHS is the maladaptive mind-body consequences of common stressors during hospitalization that compound the stress of acute illness and produce allostatic overload. This stress-induced dysfunction potentially contributes to a spectrum of generalized disease susceptibility and risk of adverse outcomes after discharge. Focused efforts to diminish patient exposure to hospital-related stressors during and after hospitalization might diminish the presence or severity of PHS. Viewing PHS from this perspective enables the development of hypothesis-driven risk-prediction models, encourages critical contemplation of traditional hospitalization, and suggests that targeted environmental interventions may significantly reduce adverse outcomes.
1. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. http://dx.doi.org/10.1001/jama.2012.216476.
2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. http://dx.doi.org/10.1056/NEJMsa0803563.
3. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11(9):e1001737. http://dx.doi.org/10.1371/journal.pmed.1001737.
4. Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371. http://dx.doi.org/10.1001/jama.2012.216219.
5. Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411. http://dx.doi.org/10.1136/bmj.h411.
6. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. http://dx.doi.org/10.1056/NEJMp1212324.
7. Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175(4):523-529. http://dx.doi.org/10.1001/jamainternmed.2014.7889.
8. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115-2124. http://dx.doi.org/10.1001/jama.292.17.2115.
9. Inouye SK, Zhang Y, Han L, Leo-Summers L, Jones R, Marcantonio E. Recoverable cognitive dysfunction at hospital admission in older persons during acute illness. J Gen Intern Med. 2006;21(12):1276-1281. http://dx.doi.org/10.1111/j.1525-1497.2006.00613.x.
10. Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvements in cognition following hospital discharge of community dwelling seniors. J Gen Intern Med. 2011;26(7):765-770. http://dx.doi.org/10.1007/s11606-011-1681-1.
11. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. http://dx.doi.org/10.1001/jama.2011.1556.
12. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. http://dx.doi.org/10.7326/0003-4819-118-3-199302010-00011.
13. Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3(4):306-315. http://dx.doi.org/10.1007/s13670-014-0103-8.
14. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171-179. http://dx.doi.org/10.1056/NEJM199801153380307.
15. McEwen BS, Gianaros PJ. Stress- and allostasis-induced brain plasticity. Annu Rev Med. 2011;62:431-445. http://dx.doi.org/10.1146/annurev-med-052209-100430.
16. Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16(5):300-317. http://dx.doi.org/10.1159/000216188.
17. Thayer JF, Sternberg E. Beyond heart rate variability: vagal regulation of allostatic systems. Ann N Y Acad Sci. 2006;1088:361-372. http://dx.doi.org/10.1196/annals.1366.014.
18. Jacobson L, Akana SF, Cascio CS, Shinsako J, Dallman MF. Circadian variations in plasma corticosterone permit normal termination of adrenocorticotropin responses to stress. Endocrinology. 1988;122(4):1343-1348. http://dx.doi.org/10.1210/endo-122-4-1343.
19. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873-904. http://dx.doi.org/10.1152/physrev.00041.2006.
20. Medicare Hospital Quality Chartbook 2014: Performance Report on Outcome Measures. Prepared by Yale New Haven Health Services Corporation Center for Outcomes Research and Evaluation for Centers for Medicare & Medicaid Services. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/downloads/medicare-hospital-quality-chartbook-2014.pdf. Accessed February 26, 2018.
21. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303(21):2141-2147. http://dx.doi.org/10.1001/jama.2010.748.
22. Drye EE, Normand SL, Wang Y, et al. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1 Pt 1):19-26. http://dx.doi.org/10.7326/0003-4819-156-1-201201030-00004.
23. Dharmarajan K, Hsieh A, Dreyer RP, Welsh J, Qin L, Krumholz HM. Relationship between age and trajectories of rehospitalization risk in older adults. J Am Geriatr Soc. 2017;65(2):421-426. http://dx.doi.org/10.1111/jgs.14583.
24. Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One. 2016;11(10):e0160492. http://dx.doi.org/10.1371/journal.pone.0160492.
25. Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502-509. http://dx.doi.org/10.1097/CCM.0b013e318232da75.
26. Brinkman S, de Jonge E, Abu-Hanna A, Arbous MS, de Lange DW, de Keizer NF. Mortality after hospital discharge in ICU patients. Crit Care Med. 2013;41(5):1229-1236. http://dx.doi.org/10.1097/CCM.0b013e31827ca4e1.
27. Steenbergen S, Rijkenberg S, Adonis T, Kroeze G, van Stijn I, Endeman H. Long-term treated intensive care patients outcomes: the one-year mortality rate, quality of life, health care use and long-term complications as reported by general practitioners. BMC Anesthesiol. 2015;15:142. http://dx.doi.org/10.1186/s12871-015-0121-x.
28. Hill AD, Fowler RA, Pinto R, Herridge MS, Cuthbertson BH, Scales DC. Long-term outcomes and healthcare utilization following critical illness--a population-based study. Crit Care. 2016;20:76. http://dx.doi.org/10.1186/s13054-016-1248-y.
29. Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369-379. http://dx.doi.org/10.1016/S2213-2600(14)70051-7.
30. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(5):1024-1036. http://dx.doi.org/10.1097/CCM.0000000000000129.
31. Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626-1635. http://dx.doi.org/10.1056/NEJMra1209390.
32. Mendez-Tellez PA, Needham DM. Early physical rehabilitation in the ICU and ventilator liberation. Respir Care. 2012;57(10):1663-1669. http://dx.doi.org/10.4187/respcare.01931.
33. Schweickert WD, Hall J. ICU-acquired weakness. Chest. 2007;131(5):1541-1549. http://dx.doi.org/10.1378/chest.06-2065.
34. Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010;2010:759234. http://dx.doi.org/10.1155/2010/759234.
35. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. http://dx.doi.org/10.1016/S0140-6736(99)01376-8.
36. Orwelius L, Nordlund A, Nordlund P, Edell-Gustafsson U, Sjoberg F. Prevalence of sleep disturbances and long-term reduced health-related quality of life after critical care: a prospective multicenter cohort study. Crit Care. 2008;12(4):R97. http://dx.doi.org/10.1186/cc6973.
37. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. http://dx.doi.org/10.7326/0003-4819-157-3-201208070-00472.
38. Sunbul M, Kanar BG, Durmus E, Kivrak T, Sari I. Acute sleep deprivation is associated with increased arterial stiffness in healthy young adults. Sleep Breath. 2014;18(1):215-220. http://dx.doi.org/10.1007/s11325-013-0873-9.
39. Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117-126. http://dx.doi.org/10.1093/sleep/26.2.117.
40. Franklin GA, McClave SA, Hurt RT, et al. Physician-delivered malnutrition: why do patients receive nothing by mouth or a clear liquid diet in a university hospital setting? JPEN J Parenter Enteral Nutr. 2011;35(3):337-342. http://dx.doi.org/10.1177/0148607110374060.
41. Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA. 1999;281(21):2013-2019. http://dx.doi.org/10.1001/jama.281.21.2013.
42. Anderson DA, Shapiro JR, Lundgren JD, Spataro LE, Frye CA. Self-reported dietary restraint is associated with elevated levels of salivary cortisol. Appetite. 2002;38(1):13-17. http://dx.doi.org/10.1006/appe.2001.0459.
43. Ott V, Friedrich M, Prilop S, et al. Food anticipation and subsequent food withdrawal increase serum cortisol in healthy men. Physiol Behav. 2011;103(5):594-599. http://dx.doi.org/10.1016/j.physbeh.2011.04.020.
44. Covinsky KE, Martin GE, Beyth RJ, Justice AC, Sehgal AR, Landefeld CS. The relationship between clinical assessments of nutritional status and adverse outcomes in older hospitalized medical patients. J Am Geriatr Soc. 1999;47(5):532-538. http://dx.doi.org/10.1111/j.1532-5415.1999.tb02566.x.
45. Lazarus BA, Murphy JB, Coletta EM, McQuade WH, Culpepper L. The provision of physical activity to hospitalized elderly patients. Arch Intern Med. 1991;151(12):2452-2456.
46. Minnick AF, Mion LC, Johnson ME, Catrambone C, Leipzig R. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39(1):30-37. http://dx.doi.org/10.1111/j.1547-5069.2007.00140.x.
47. Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59(2):266-273. http://dx.doi.org/10.1111/j.1532-5415.2010.03276.x.
48. Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338-1344. http://dx.doi.org/10.1056/NEJM199505183322006.
49. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expectations: an international journal of public participation in health care and health policy. 2004;7(1):61-73. http://dx.doi.org/10.1046/j.1369-6513.2003.00251.x.
50. Volicer BJ. Hospital stress and patient reports of pain and physical status. Journal Human Stress. 1978;4(2):28-37. http://dx.doi.org/10.1080/0097840X.1978.9934984.
51. Willner P, Towell A, Sampson D, Sophokleous S, Muscat R. Reduction of sucrose preference by chronic unpredictable mild stress, and its restoration by a tricyclic antidepressant. Psychopharmacology (Berl). 1987;93(3):358-364. http://dx.doi.org/10.1007/BF00187257.
52. Grippo AJ, Francis J, Beltz TG, Felder RB, Johnson AK. Neuroendocrine and cytokine profile of chronic mild stress-induced anhedonia. Physiol Behav. 2005;84(5):697-706. http://dx.doi.org/10.1016/j.physbeh.2005.02.011.
53. Krishnan V, Nestler EJ. Animal models of depression: molecular perspectives. Curr Top Behav Neurosci. 2011;7:121-147. http://dx.doi.org/10.1007/7854_2010_108.
54. Magarinos AM, McEwen BS. Stress-induced atrophy of apical dendrites of hippocampal CA3c neurons: comparison of stressors. Neuroscience. 1995;69(1):83-88. http://dx.doi.org/10.1016/0306-4522(95)00256-I.
55. McEwen BS. Plasticity of the hippocampus: adaptation to chronic stress and allostatic load. Ann N Y Acad Sci. 2001;933:265-277. http://dx.doi.org/10.1111/j.1749-6632.2001.tb05830.x.
56. McEwen BS. The brain on stress: toward an integrative approach to brain, body, and behavior. Perspect Psychol Sci. 2013;8(6):673-675. http://dx.doi.org/10.1177/1745691613506907.
57. McEwen BS, Morrison JH. The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron. 2013;79(1):16-29. http://dx.doi.org/10.1016/j.neuron.2013.06.028.
58. Dutta P, Courties G, Wei Y, et al. Myocardial infarction accelerates atherosclerosis. Nature. 2012;487(7407):325-329. http://dx.doi.org/10.1038/nature11260.
59. Lu XT, Liu YF, Zhang L, et al. Unpredictable chronic mild stress promotes atherosclerosis in high cholesterol-fed rabbits. Psychosom Med. 2012;74(6):604-611. http://dx.doi.org/10.1097/PSY.0b013e31825d0b71.
60. Heidt T, Sager HB, Courties G, et al. Chronic variable stress activates hematopoietic stem cells. Nat Med. 2014;20(7):754-758. http://dx.doi.org/10.1038/nm.3589.
61. Sheridan JF, Feng NG, Bonneau RH, Allen CM, Huneycutt BS, Glaser R. Restraint stress differentially affects anti-viral cellular and humoral immune responses in mice. J Neuroimmunol. 1991;31(3):245-255. http://dx.doi.org/10.1016/0165-5728(91)90046-A.
62. Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009;9(6):787-793. http://dx.doi.org/10.1016/j.coph.2009.08.007.
63. Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30(1):1-10. http://dx.doi.org/10.1016/j.psyneuen.2004.05.007.
64. Tamashiro KL, Sakai RR, Shively CA, Karatsoreos IN, Reagan LP. Chronic stress, metabolism, and metabolic syndrome. Stress. 2011;14(5):468-474. http://dx.doi.org/10.3109/10253890.2011.606341.
65. McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54(3):200-207. http://dx.doi.org/10.1016/S0006-3223(03)00177-X.
66. Zareie M, Johnson-Henry K, Jury J, et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut. 2006;55(11):1553-1560. http://dx.doi.org/10.1136/gut.2005.080739.
67. Joachim RA, Quarcoo D, Arck PC, Herz U, Renz H, Klapp BF. Stress enhances airway reactivity and airway inflammation in an animal model of allergic bronchial asthma. Psychosom Med. 2003;65(5):811-815. http://dx.doi.org/10.1097/01.PSY.0000088582.50468.A3.
68. Thaker PH, Han LY, Kamat AA, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12(8):939-944. http://dx.doi.org/10.1038/nm1447.
69. Schreuder L, Eggen BJ, Biber K, Schoemaker RG, Laman JD, de Rooij SE. Pathophysiological and behavioral effects of systemic inflammation in aged and diseased rodents with relevance to delirium: A systematic review. Brain Behav Immun. 2017;62:362-381. http://dx.doi.org/10.1016/j.bbi.2017.01.010.
70. Mu DL, Li LH, Wang DX, et al. High postoperative serum cortisol level is associated with increased risk of cognitive dysfunction early after coronary artery bypass graft surgery: a prospective cohort study. PLoS One. 2013;8(10):e77637. http://dx.doi.org/10.1371/journal.pone.0077637.
71. Mu DL, Wang DX, Li LH, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. 2010;14(6):R238. http://dx.doi.org/10.1186/cc9393.
72. Nguyen DN, Huyghens L, Zhang H, Schiettecatte J, Smitz J, Vincent JL. Cortisol is an associated-risk factor of brain dysfunction in patients with severe sepsis and septic shock. Biomed Res Int. 2014;2014:712742. http://dx.doi.org/10.1155/2014/712742.
73. Elkind MS, Carty CL, O’Meara ES, et al. Hospitalization for infection and risk of acute ischemic stroke: the Cardiovascular Health Study. Stroke. 2011;42(7):1851-1856. http://dx.doi.org/10.1161/STROKEAHA.110.608588.
74. Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374-1376.
75. Jutla SK, Yuyun MF, Quinn PA, Ng LL. Plasma cortisol and prognosis of patients with acute myocardial infarction. J Cardiovasc Med (Hagerstown). 2014;15(1):33-41. http://dx.doi.org/10.2459/JCM.0b013e328364100b.
76. Yende S, D’Angelo G, Kellum JA, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242-1247. http://dx.doi.org/10.1164/rccm.200712-1777OC.
77. Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011;31(1):81-93. http://dx.doi.org/10.1016/j.iac.2010.09.010.
78. Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773-778. http://dx.doi.org/10.1016/S0140-6736(99)08415-9.
79. O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke. 1991;22(7):842-847. http://dx.doi.org/10.1161/01.STR.22.7.842.
80. Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169(8):910-914. http://dx.doi.org/10.1164/rccm.200310-1448OC.
81. Rosengren A, Freden M, Hansson PO, Wilhelmsen L, Wedel H, Eriksson H. Psychosocial factors and venous thromboembolism: a long-term follow-up study of Swedish men. J Thrombosis Haemostasis. 2008;6(4):558-564. http://dx.doi.org/10.1111/j.1538-7836.2007.02857.x.
82. Oswald GA, Smith CC, Betteridge DJ, Yudkin JS. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. BMJ. 1986;293(6552):917-922. http://dx.doi.org/10.1136/bmj.293.6552.917.
83. Middlekauff HR, Nguyen AH, Negrao CE, et al. Impact of acute mental stress on sympathetic nerve activity and regional blood flow in advanced heart failure: implications for ‘triggering’ adverse cardiac events. Circulation. 1997;96(6):1835-1842. http://dx.doi.org/10.1161/01.CIR.96.6.1835.
84. Nijm J, Jonasson L. Inflammation and cortisol response in coronary artery disease. Ann Med. 2009;41(3):224-233. http://dx.doi.org/10.1080/07853890802508934.
85. Steptoe A, Hackett RA, Lazzarino AI, et al. Disruption of multisystem responses to stress in type 2 diabetes: investigating the dynamics of allostatic load. Proc Natl Acad Sci U S A. 2014;111(44):15693-15698. http://dx.doi.org/10.1073/pnas.1410401111.
86. Sepehri A, Beggs T, Hassan A, et al. The impact of frailty on outcomes after cardiac surgery: a systematic review. J Thorac Cardiovasc Surg. 2014;148(6):3110-3117. http://dx.doi.org/10.1016/j.jtcvs.2014.07.087.
87. Johar H, Emeny RT, Bidlingmaier M, et al. Blunted diurnal cortisol pattern is associated with frailty: a cross-sectional study of 745 participants aged 65 to 90 years. J Clin Endocrinol Metab. 2014;99(3):E464-468. http://dx.doi.org/10.1210/jc.2013-3079.
88. Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med. 2011;27(1):79-87. http://dx.doi.org/10.1016/j.cger.2010.08.002.
89. Hospital Elder Life Program (HELP) for Prevention of Delirium. 2017; http://www.hospitalelderlifeprogram.org/. Accessed February 16, 2018.
90. Shepperd S, Doll H, Angus RM, et al. Admission avoidance hospital at home. Cochrane Database of System Rev. 2008;(4):CD007491. http://dx.doi.org/10.1002/14651858.CD007491.pub2’
91. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatrics Soc. 2009;57(2):273-278. http://dx.doi.org/10.1111/j.1532-5415.2008.02103.x.
92. Qaddoura A, Yazdan-Ashoori P, Kabali C, et al. Efficacy of hospital at home in patients with heart failure: a systematic review and meta-analysis. PloS One. 2015;10(6):e0129282. http://dx.doi.org/10.1371/journal.pone.0129282.
93. Seeman T, Gruenewald T, Karlamangla A, et al. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am J Hum Biol. 2010;22(4):463-472. http://dx.doi.org/10.1002/ajhb.21018.
94. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. http://dx.doi.org/10.1001/jamainternmed.2015.7863.
95. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00008.
96. Takahashi PY, Naessens JM, Peterson SM, et al. Short-term and long-term effectiveness of a post-hospital care transitions program in an older, medically complex population. Healthcare. 2016;4(1):30-35. http://dx.doi.org/10.1016/j.hjdsi.2015.06.006.
 97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
1. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. http://dx.doi.org/10.1001/jama.2012.216476.
2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. http://dx.doi.org/10.1056/NEJMsa0803563.
3. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11(9):e1001737. http://dx.doi.org/10.1371/journal.pmed.1001737.
4. Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371. http://dx.doi.org/10.1001/jama.2012.216219.
5. Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411. http://dx.doi.org/10.1136/bmj.h411.
6. Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. http://dx.doi.org/10.1056/NEJMp1212324.
7. Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175(4):523-529. http://dx.doi.org/10.1001/jamainternmed.2014.7889.
8. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115-2124. http://dx.doi.org/10.1001/jama.292.17.2115.
9. Inouye SK, Zhang Y, Han L, Leo-Summers L, Jones R, Marcantonio E. Recoverable cognitive dysfunction at hospital admission in older persons during acute illness. J Gen Intern Med. 2006;21(12):1276-1281. http://dx.doi.org/10.1111/j.1525-1497.2006.00613.x.
10. Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvements in cognition following hospital discharge of community dwelling seniors. J Gen Intern Med. 2011;26(7):765-770. http://dx.doi.org/10.1007/s11606-011-1681-1.
11. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. http://dx.doi.org/10.1001/jama.2011.1556.
12. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. http://dx.doi.org/10.7326/0003-4819-118-3-199302010-00011.
13. Dharmarajan K, Krumholz HM. Strategies to reduce 30-day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3(4):306-315. http://dx.doi.org/10.1007/s13670-014-0103-8.
14. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171-179. http://dx.doi.org/10.1056/NEJM199801153380307.
15. McEwen BS, Gianaros PJ. Stress- and allostasis-induced brain plasticity. Annu Rev Med. 2011;62:431-445. http://dx.doi.org/10.1146/annurev-med-052209-100430.
16. Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. 2009;16(5):300-317. http://dx.doi.org/10.1159/000216188.
17. Thayer JF, Sternberg E. Beyond heart rate variability: vagal regulation of allostatic systems. Ann N Y Acad Sci. 2006;1088:361-372. http://dx.doi.org/10.1196/annals.1366.014.
18. Jacobson L, Akana SF, Cascio CS, Shinsako J, Dallman MF. Circadian variations in plasma corticosterone permit normal termination of adrenocorticotropin responses to stress. Endocrinology. 1988;122(4):1343-1348. http://dx.doi.org/10.1210/endo-122-4-1343.
19. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873-904. http://dx.doi.org/10.1152/physrev.00041.2006.
20. Medicare Hospital Quality Chartbook 2014: Performance Report on Outcome Measures. Prepared by Yale New Haven Health Services Corporation Center for Outcomes Research and Evaluation for Centers for Medicare & Medicaid Services. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/downloads/medicare-hospital-quality-chartbook-2014.pdf. Accessed February 26, 2018.
21. Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303(21):2141-2147. http://dx.doi.org/10.1001/jama.2010.748.
22. Drye EE, Normand SL, Wang Y, et al. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1 Pt 1):19-26. http://dx.doi.org/10.7326/0003-4819-156-1-201201030-00004.
23. Dharmarajan K, Hsieh A, Dreyer RP, Welsh J, Qin L, Krumholz HM. Relationship between age and trajectories of rehospitalization risk in older adults. J Am Geriatr Soc. 2017;65(2):421-426. http://dx.doi.org/10.1111/jgs.14583.
24. Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One. 2016;11(10):e0160492. http://dx.doi.org/10.1371/journal.pone.0160492.
25. Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502-509. http://dx.doi.org/10.1097/CCM.0b013e318232da75.
26. Brinkman S, de Jonge E, Abu-Hanna A, Arbous MS, de Lange DW, de Keizer NF. Mortality after hospital discharge in ICU patients. Crit Care Med. 2013;41(5):1229-1236. http://dx.doi.org/10.1097/CCM.0b013e31827ca4e1.
27. Steenbergen S, Rijkenberg S, Adonis T, Kroeze G, van Stijn I, Endeman H. Long-term treated intensive care patients outcomes: the one-year mortality rate, quality of life, health care use and long-term complications as reported by general practitioners. BMC Anesthesiol. 2015;15:142. http://dx.doi.org/10.1186/s12871-015-0121-x.
28. Hill AD, Fowler RA, Pinto R, Herridge MS, Cuthbertson BH, Scales DC. Long-term outcomes and healthcare utilization following critical illness--a population-based study. Crit Care. 2016;20:76. http://dx.doi.org/10.1186/s13054-016-1248-y.
29. Jackson JC, Pandharipande PP, Girard TD, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369-379. http://dx.doi.org/10.1016/S2213-2600(14)70051-7.
30. Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014;42(5):1024-1036. http://dx.doi.org/10.1097/CCM.0000000000000129.
31. Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(17):1626-1635. http://dx.doi.org/10.1056/NEJMra1209390.
32. Mendez-Tellez PA, Needham DM. Early physical rehabilitation in the ICU and ventilator liberation. Respir Care. 2012;57(10):1663-1669. http://dx.doi.org/10.4187/respcare.01931.
33. Schweickert WD, Hall J. ICU-acquired weakness. Chest. 2007;131(5):1541-1549. http://dx.doi.org/10.1378/chest.06-2065.
34. Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010;2010:759234. http://dx.doi.org/10.1155/2010/759234.
35. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. http://dx.doi.org/10.1016/S0140-6736(99)01376-8.
36. Orwelius L, Nordlund A, Nordlund P, Edell-Gustafsson U, Sjoberg F. Prevalence of sleep disturbances and long-term reduced health-related quality of life after critical care: a prospective multicenter cohort study. Crit Care. 2008;12(4):R97. http://dx.doi.org/10.1186/cc6973.
37. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. http://dx.doi.org/10.7326/0003-4819-157-3-201208070-00472.
38. Sunbul M, Kanar BG, Durmus E, Kivrak T, Sari I. Acute sleep deprivation is associated with increased arterial stiffness in healthy young adults. Sleep Breath. 2014;18(1):215-220. http://dx.doi.org/10.1007/s11325-013-0873-9.
39. Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117-126. http://dx.doi.org/10.1093/sleep/26.2.117.
40. Franklin GA, McClave SA, Hurt RT, et al. Physician-delivered malnutrition: why do patients receive nothing by mouth or a clear liquid diet in a university hospital setting? JPEN J Parenter Enteral Nutr. 2011;35(3):337-342. http://dx.doi.org/10.1177/0148607110374060.
41. Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA. 1999;281(21):2013-2019. http://dx.doi.org/10.1001/jama.281.21.2013.
42. Anderson DA, Shapiro JR, Lundgren JD, Spataro LE, Frye CA. Self-reported dietary restraint is associated with elevated levels of salivary cortisol. Appetite. 2002;38(1):13-17. http://dx.doi.org/10.1006/appe.2001.0459.
43. Ott V, Friedrich M, Prilop S, et al. Food anticipation and subsequent food withdrawal increase serum cortisol in healthy men. Physiol Behav. 2011;103(5):594-599. http://dx.doi.org/10.1016/j.physbeh.2011.04.020.
44. Covinsky KE, Martin GE, Beyth RJ, Justice AC, Sehgal AR, Landefeld CS. The relationship between clinical assessments of nutritional status and adverse outcomes in older hospitalized medical patients. J Am Geriatr Soc. 1999;47(5):532-538. http://dx.doi.org/10.1111/j.1532-5415.1999.tb02566.x.
45. Lazarus BA, Murphy JB, Coletta EM, McQuade WH, Culpepper L. The provision of physical activity to hospitalized elderly patients. Arch Intern Med. 1991;151(12):2452-2456.
46. Minnick AF, Mion LC, Johnson ME, Catrambone C, Leipzig R. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39(1):30-37. http://dx.doi.org/10.1111/j.1547-5069.2007.00140.x.
47. Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59(2):266-273. http://dx.doi.org/10.1111/j.1532-5415.2010.03276.x.
48. Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338-1344. http://dx.doi.org/10.1056/NEJM199505183322006.
49. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expectations: an international journal of public participation in health care and health policy. 2004;7(1):61-73. http://dx.doi.org/10.1046/j.1369-6513.2003.00251.x.
50. Volicer BJ. Hospital stress and patient reports of pain and physical status. Journal Human Stress. 1978;4(2):28-37. http://dx.doi.org/10.1080/0097840X.1978.9934984.
51. Willner P, Towell A, Sampson D, Sophokleous S, Muscat R. Reduction of sucrose preference by chronic unpredictable mild stress, and its restoration by a tricyclic antidepressant. Psychopharmacology (Berl). 1987;93(3):358-364. http://dx.doi.org/10.1007/BF00187257.
52. Grippo AJ, Francis J, Beltz TG, Felder RB, Johnson AK. Neuroendocrine and cytokine profile of chronic mild stress-induced anhedonia. Physiol Behav. 2005;84(5):697-706. http://dx.doi.org/10.1016/j.physbeh.2005.02.011.
53. Krishnan V, Nestler EJ. Animal models of depression: molecular perspectives. Curr Top Behav Neurosci. 2011;7:121-147. http://dx.doi.org/10.1007/7854_2010_108.
54. Magarinos AM, McEwen BS. Stress-induced atrophy of apical dendrites of hippocampal CA3c neurons: comparison of stressors. Neuroscience. 1995;69(1):83-88. http://dx.doi.org/10.1016/0306-4522(95)00256-I.
55. McEwen BS. Plasticity of the hippocampus: adaptation to chronic stress and allostatic load. Ann N Y Acad Sci. 2001;933:265-277. http://dx.doi.org/10.1111/j.1749-6632.2001.tb05830.x.
56. McEwen BS. The brain on stress: toward an integrative approach to brain, body, and behavior. Perspect Psychol Sci. 2013;8(6):673-675. http://dx.doi.org/10.1177/1745691613506907.
57. McEwen BS, Morrison JH. The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron. 2013;79(1):16-29. http://dx.doi.org/10.1016/j.neuron.2013.06.028.
58. Dutta P, Courties G, Wei Y, et al. Myocardial infarction accelerates atherosclerosis. Nature. 2012;487(7407):325-329. http://dx.doi.org/10.1038/nature11260.
59. Lu XT, Liu YF, Zhang L, et al. Unpredictable chronic mild stress promotes atherosclerosis in high cholesterol-fed rabbits. Psychosom Med. 2012;74(6):604-611. http://dx.doi.org/10.1097/PSY.0b013e31825d0b71.
60. Heidt T, Sager HB, Courties G, et al. Chronic variable stress activates hematopoietic stem cells. Nat Med. 2014;20(7):754-758. http://dx.doi.org/10.1038/nm.3589.
61. Sheridan JF, Feng NG, Bonneau RH, Allen CM, Huneycutt BS, Glaser R. Restraint stress differentially affects anti-viral cellular and humoral immune responses in mice. J Neuroimmunol. 1991;31(3):245-255. http://dx.doi.org/10.1016/0165-5728(91)90046-A.
62. Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009;9(6):787-793. http://dx.doi.org/10.1016/j.coph.2009.08.007.
63. Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30(1):1-10. http://dx.doi.org/10.1016/j.psyneuen.2004.05.007.
64. Tamashiro KL, Sakai RR, Shively CA, Karatsoreos IN, Reagan LP. Chronic stress, metabolism, and metabolic syndrome. Stress. 2011;14(5):468-474. http://dx.doi.org/10.3109/10253890.2011.606341.
65. McEwen BS. Mood disorders and allostatic load. Biol Psychiatry. 2003;54(3):200-207. http://dx.doi.org/10.1016/S0006-3223(03)00177-X.
66. Zareie M, Johnson-Henry K, Jury J, et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut. 2006;55(11):1553-1560. http://dx.doi.org/10.1136/gut.2005.080739.
67. Joachim RA, Quarcoo D, Arck PC, Herz U, Renz H, Klapp BF. Stress enhances airway reactivity and airway inflammation in an animal model of allergic bronchial asthma. Psychosom Med. 2003;65(5):811-815. http://dx.doi.org/10.1097/01.PSY.0000088582.50468.A3.
68. Thaker PH, Han LY, Kamat AA, et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12(8):939-944. http://dx.doi.org/10.1038/nm1447.
69. Schreuder L, Eggen BJ, Biber K, Schoemaker RG, Laman JD, de Rooij SE. Pathophysiological and behavioral effects of systemic inflammation in aged and diseased rodents with relevance to delirium: A systematic review. Brain Behav Immun. 2017;62:362-381. http://dx.doi.org/10.1016/j.bbi.2017.01.010.
70. Mu DL, Li LH, Wang DX, et al. High postoperative serum cortisol level is associated with increased risk of cognitive dysfunction early after coronary artery bypass graft surgery: a prospective cohort study. PLoS One. 2013;8(10):e77637. http://dx.doi.org/10.1371/journal.pone.0077637.
71. Mu DL, Wang DX, Li LH, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. 2010;14(6):R238. http://dx.doi.org/10.1186/cc9393.
72. Nguyen DN, Huyghens L, Zhang H, Schiettecatte J, Smitz J, Vincent JL. Cortisol is an associated-risk factor of brain dysfunction in patients with severe sepsis and septic shock. Biomed Res Int. 2014;2014:712742. http://dx.doi.org/10.1155/2014/712742.
73. Elkind MS, Carty CL, O’Meara ES, et al. Hospitalization for infection and risk of acute ischemic stroke: the Cardiovascular Health Study. Stroke. 2011;42(7):1851-1856. http://dx.doi.org/10.1161/STROKEAHA.110.608588.
74. Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374-1376.
75. Jutla SK, Yuyun MF, Quinn PA, Ng LL. Plasma cortisol and prognosis of patients with acute myocardial infarction. J Cardiovasc Med (Hagerstown). 2014;15(1):33-41. http://dx.doi.org/10.2459/JCM.0b013e328364100b.
76. Yende S, D’Angelo G, Kellum JA, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177(11):1242-1247. http://dx.doi.org/10.1164/rccm.200712-1777OC.
77. Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011;31(1):81-93. http://dx.doi.org/10.1016/j.iac.2010.09.010.
78. Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355(9206):773-778. http://dx.doi.org/10.1016/S0140-6736(99)08415-9.
79. O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke. 1991;22(7):842-847. http://dx.doi.org/10.1161/01.STR.22.7.842.
80. Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169(8):910-914. http://dx.doi.org/10.1164/rccm.200310-1448OC.
81. Rosengren A, Freden M, Hansson PO, Wilhelmsen L, Wedel H, Eriksson H. Psychosocial factors and venous thromboembolism: a long-term follow-up study of Swedish men. J Thrombosis Haemostasis. 2008;6(4):558-564. http://dx.doi.org/10.1111/j.1538-7836.2007.02857.x.
82. Oswald GA, Smith CC, Betteridge DJ, Yudkin JS. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. BMJ. 1986;293(6552):917-922. http://dx.doi.org/10.1136/bmj.293.6552.917.
83. Middlekauff HR, Nguyen AH, Negrao CE, et al. Impact of acute mental stress on sympathetic nerve activity and regional blood flow in advanced heart failure: implications for ‘triggering’ adverse cardiac events. Circulation. 1997;96(6):1835-1842. http://dx.doi.org/10.1161/01.CIR.96.6.1835.
84. Nijm J, Jonasson L. Inflammation and cortisol response in coronary artery disease. Ann Med. 2009;41(3):224-233. http://dx.doi.org/10.1080/07853890802508934.
85. Steptoe A, Hackett RA, Lazzarino AI, et al. Disruption of multisystem responses to stress in type 2 diabetes: investigating the dynamics of allostatic load. Proc Natl Acad Sci U S A. 2014;111(44):15693-15698. http://dx.doi.org/10.1073/pnas.1410401111.
86. Sepehri A, Beggs T, Hassan A, et al. The impact of frailty on outcomes after cardiac surgery: a systematic review. J Thorac Cardiovasc Surg. 2014;148(6):3110-3117. http://dx.doi.org/10.1016/j.jtcvs.2014.07.087.
87. Johar H, Emeny RT, Bidlingmaier M, et al. Blunted diurnal cortisol pattern is associated with frailty: a cross-sectional study of 745 participants aged 65 to 90 years. J Clin Endocrinol Metab. 2014;99(3):E464-468. http://dx.doi.org/10.1210/jc.2013-3079.
88. Yao X, Li H, Leng SX. Inflammation and immune system alterations in frailty. Clin Geriatr Med. 2011;27(1):79-87. http://dx.doi.org/10.1016/j.cger.2010.08.002.
89. Hospital Elder Life Program (HELP) for Prevention of Delirium. 2017; http://www.hospitalelderlifeprogram.org/. Accessed February 16, 2018.
90. Shepperd S, Doll H, Angus RM, et al. Admission avoidance hospital at home. Cochrane Database of System Rev. 2008;(4):CD007491. http://dx.doi.org/10.1002/14651858.CD007491.pub2’
91. Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatrics Soc. 2009;57(2):273-278. http://dx.doi.org/10.1111/j.1532-5415.2008.02103.x.
92. Qaddoura A, Yazdan-Ashoori P, Kabali C, et al. Efficacy of hospital at home in patients with heart failure: a systematic review and meta-analysis. PloS One. 2015;10(6):e0129282. http://dx.doi.org/10.1371/journal.pone.0129282.
93. Seeman T, Gruenewald T, Karlamangla A, et al. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am J Hum Biol. 2010;22(4):463-472. http://dx.doi.org/10.1002/ajhb.21018.
94. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176(4):484-493. http://dx.doi.org/10.1001/jamainternmed.2015.7863.
95. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520-528. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00008.
96. Takahashi PY, Naessens JM, Peterson SM, et al. Short-term and long-term effectiveness of a post-hospital care transitions program in an older, medically complex population. Healthcare. 2016;4(1):30-35. http://dx.doi.org/10.1016/j.hjdsi.2015.06.006.
 97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
97. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc. 2017;65(5):1026-1033. http://dx.doi.org/10.1111/jgs.14743.
© 2018 Society of Hospital Medicine