User login
ICD-10-CM code changes: What's new for 2018
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
2016 GYN coding changes to note for your maximized reimbursement
In the August 2016 issue of OBG
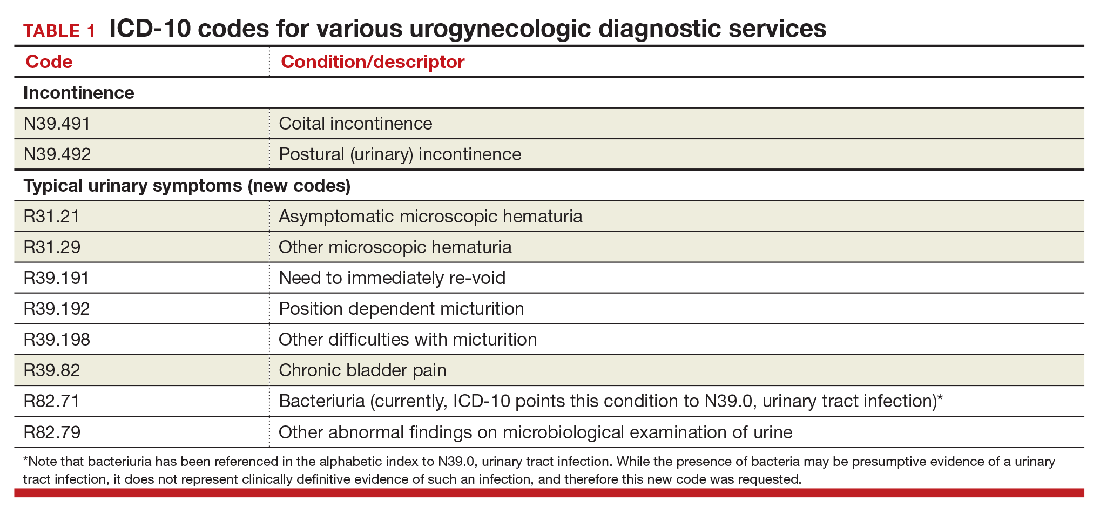
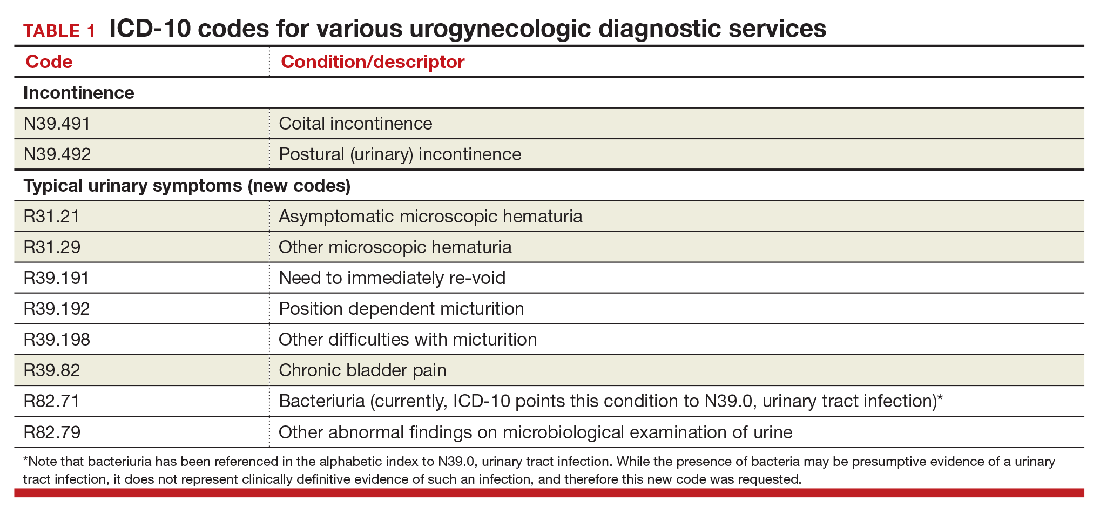
Urogynecology diagnostic codes
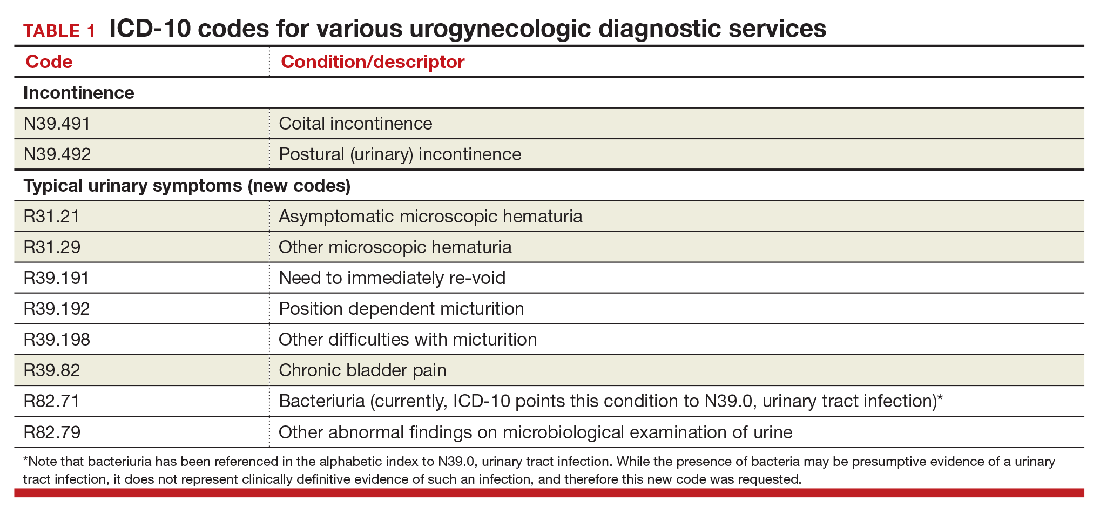
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
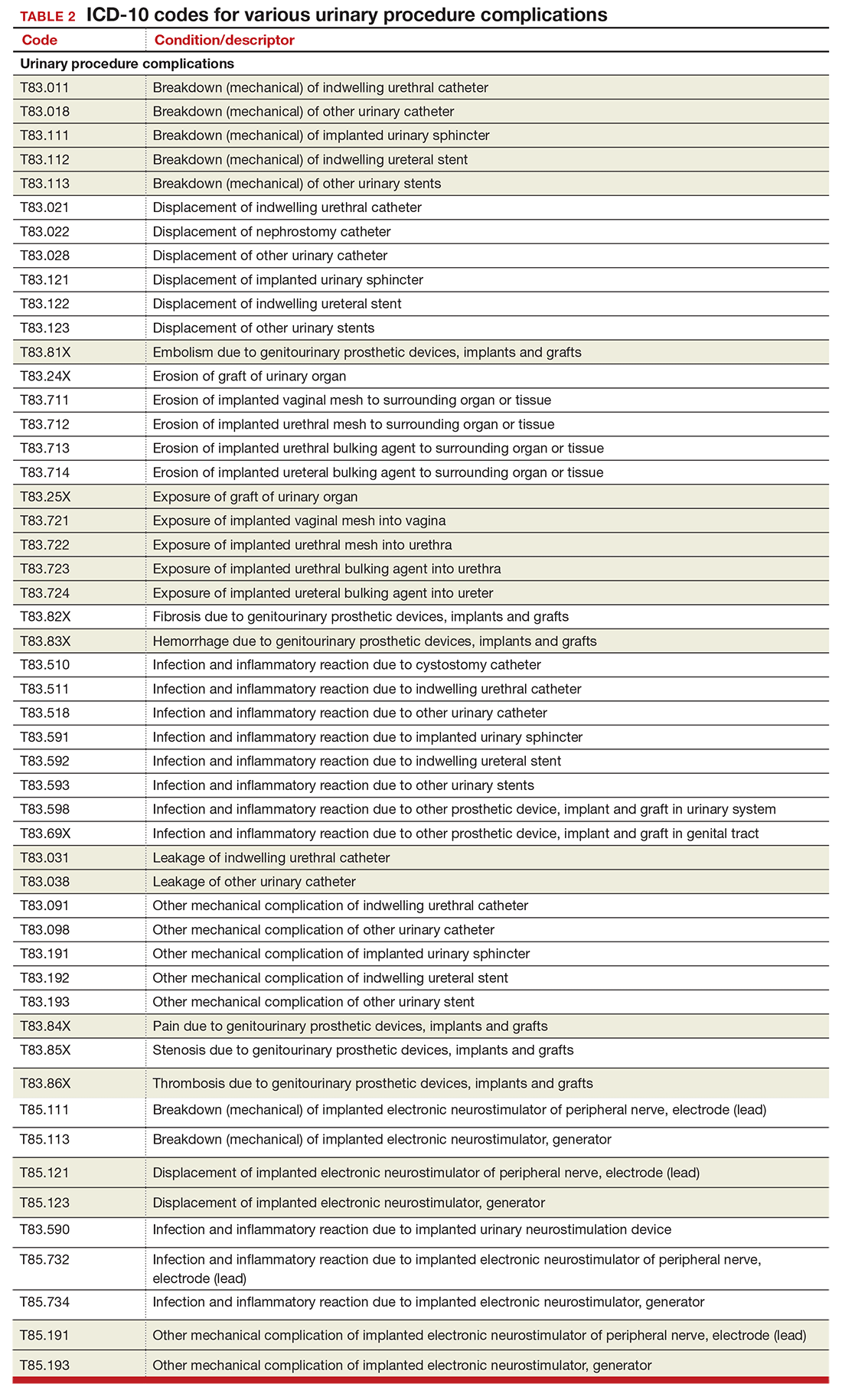
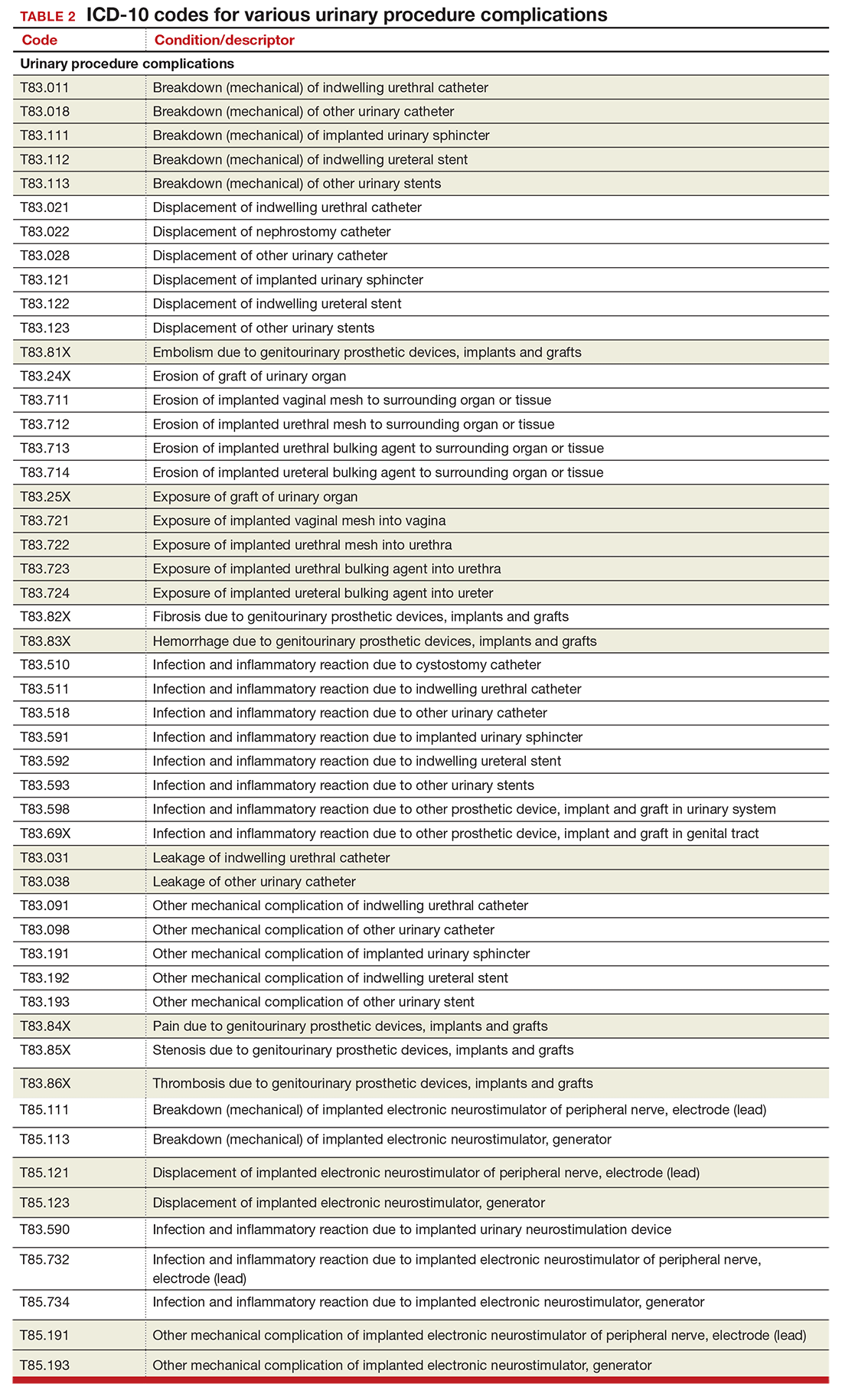
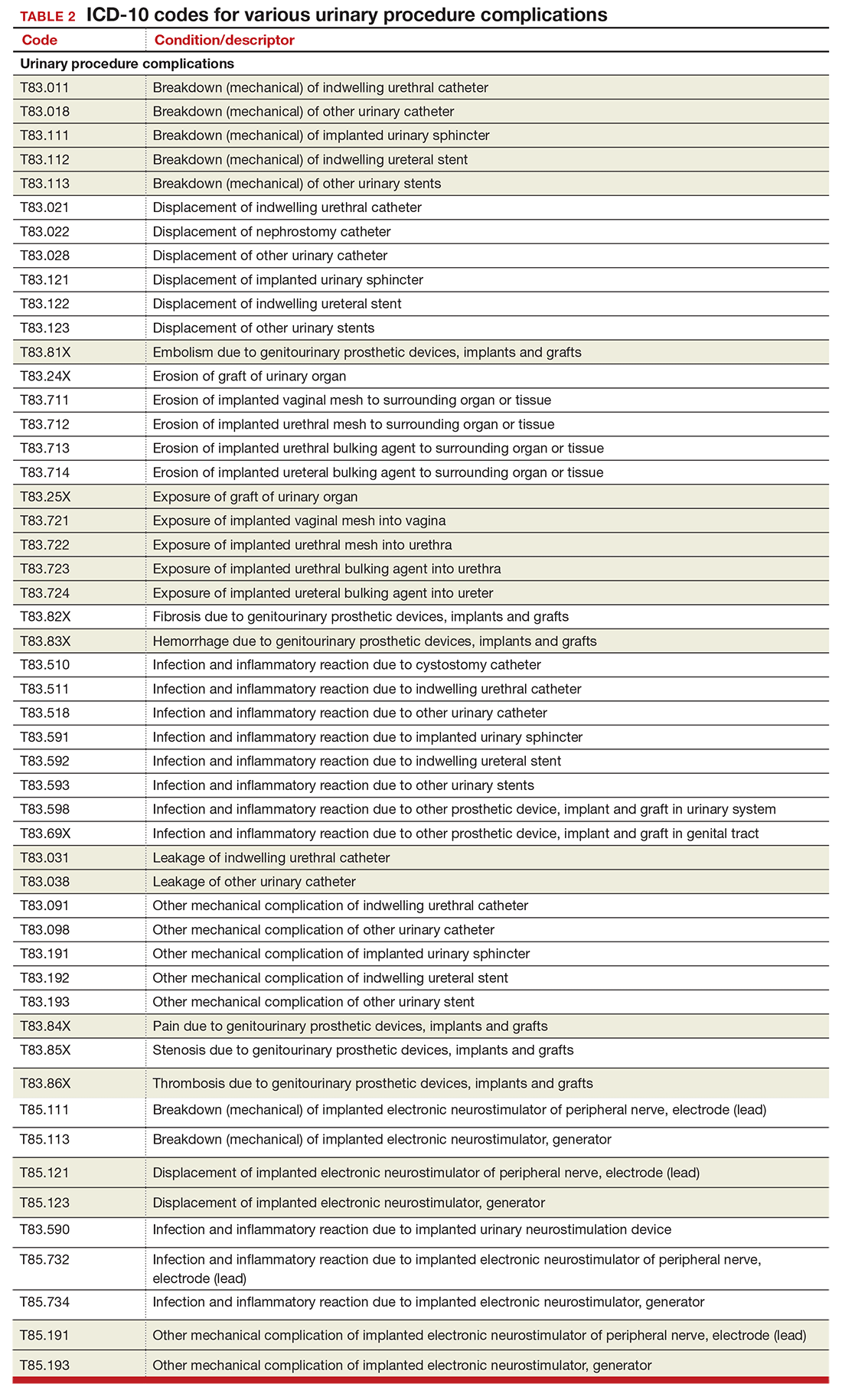
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
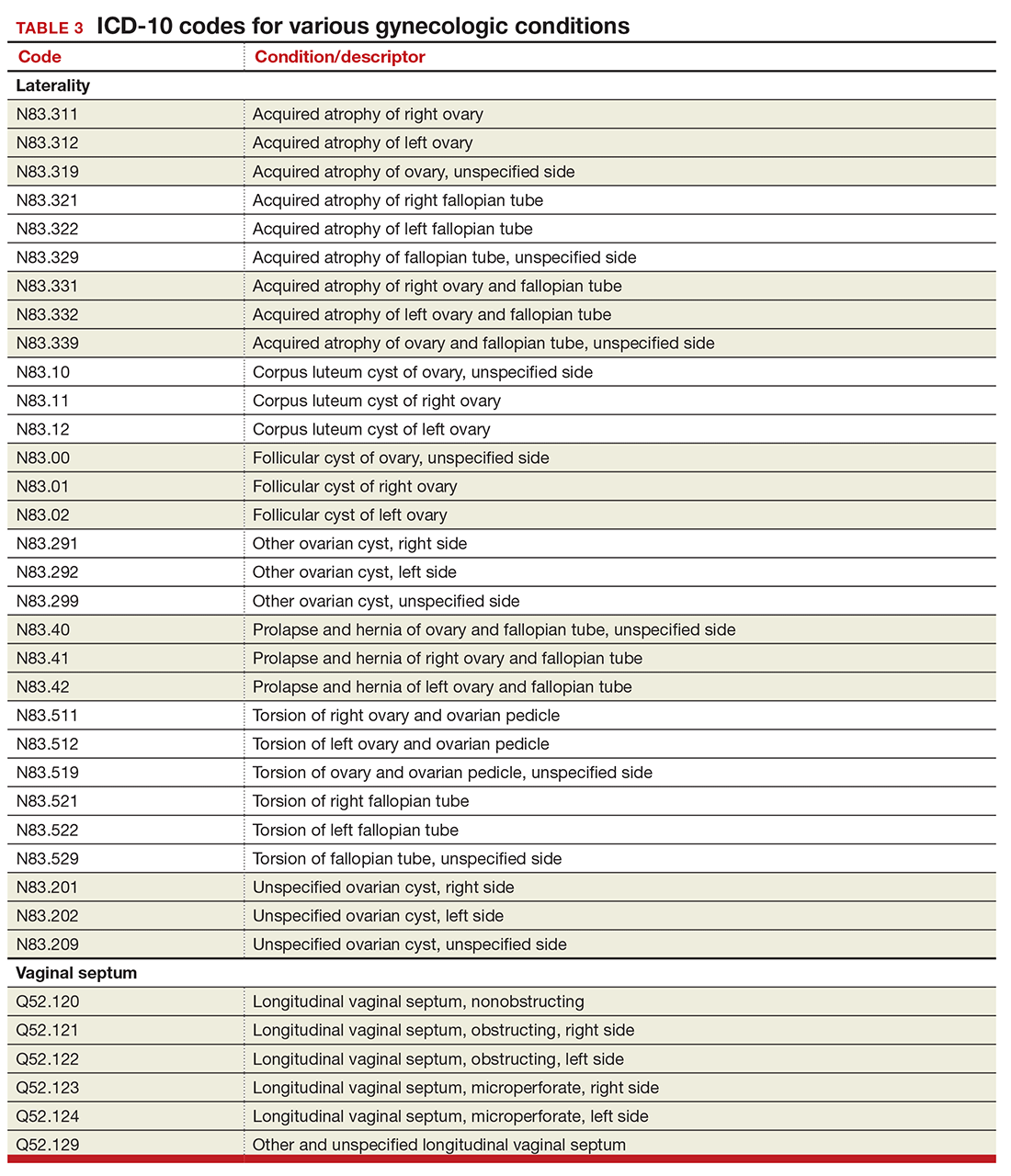
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
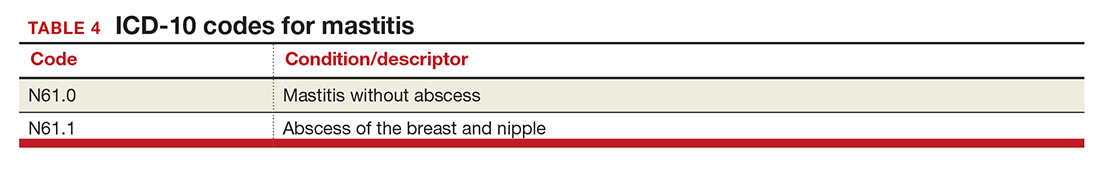
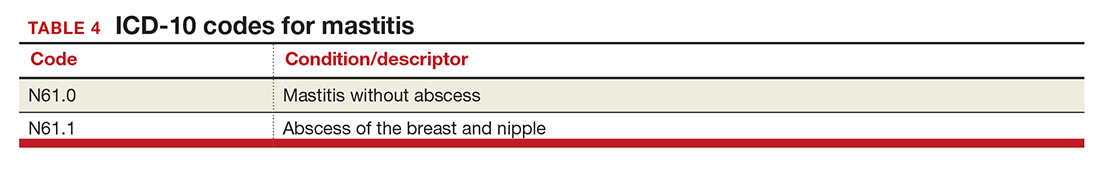
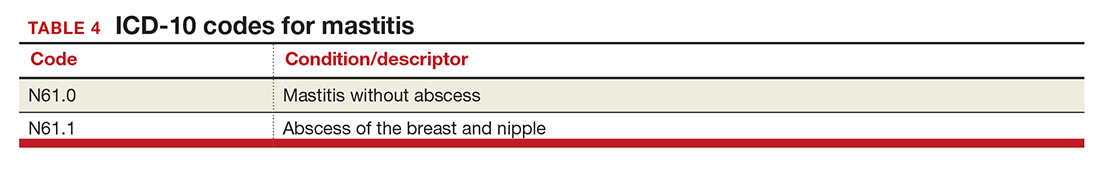
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
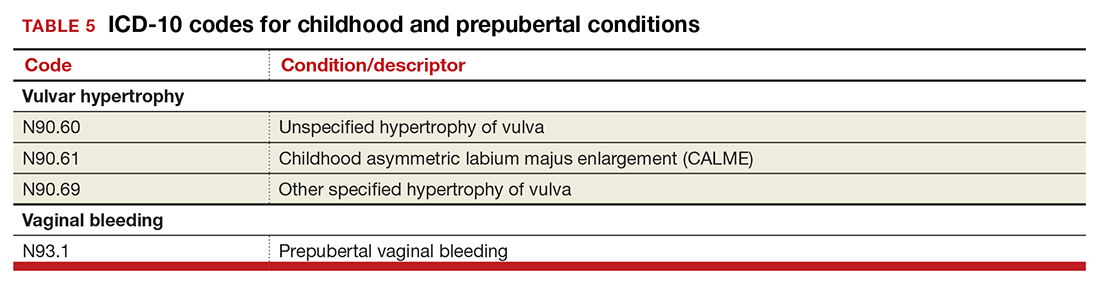
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
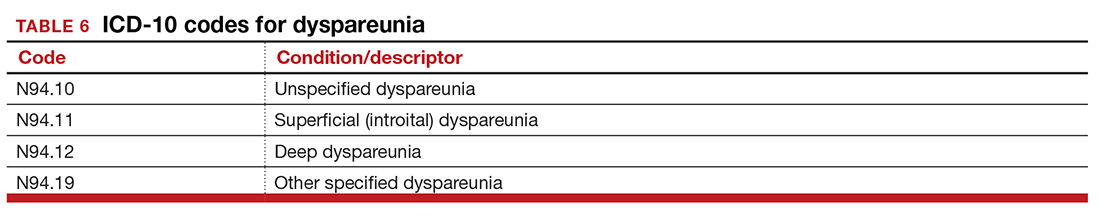
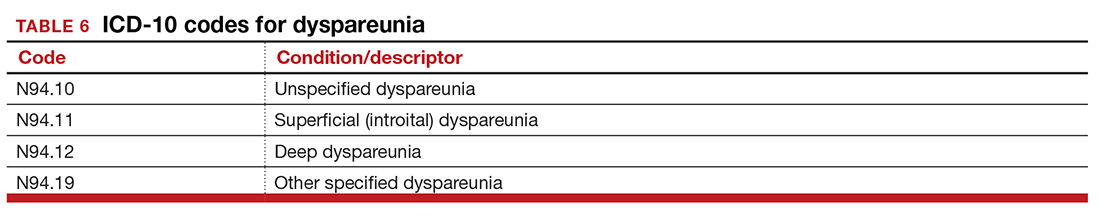
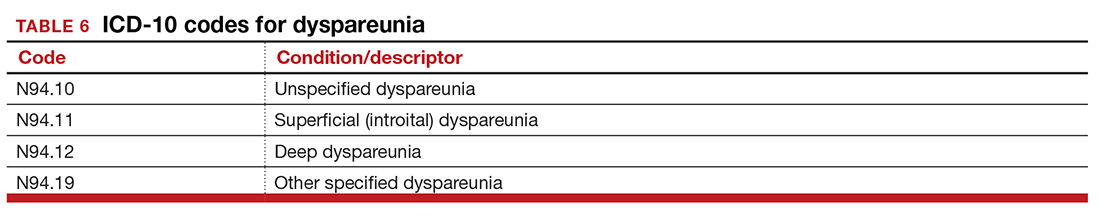
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
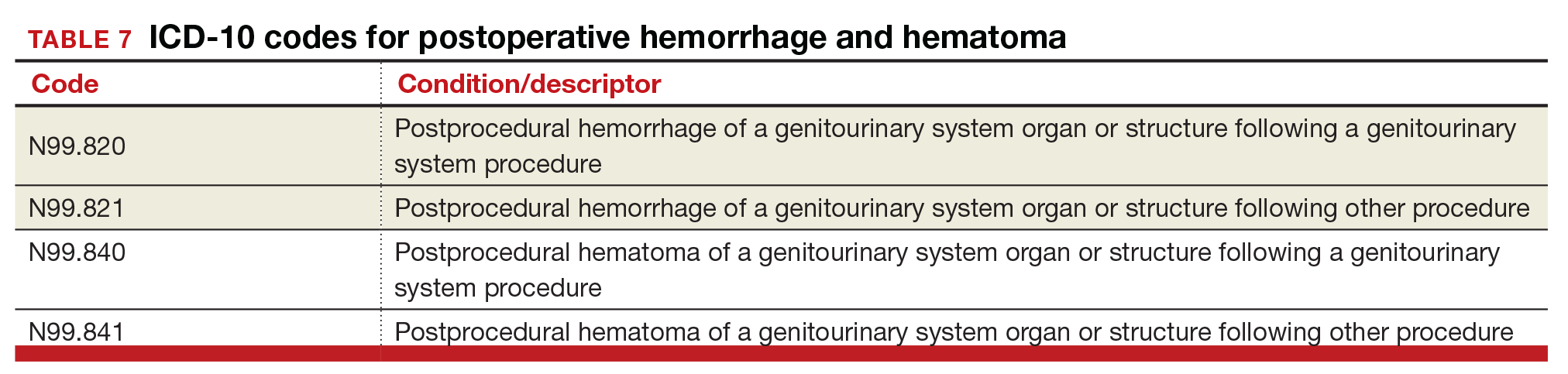
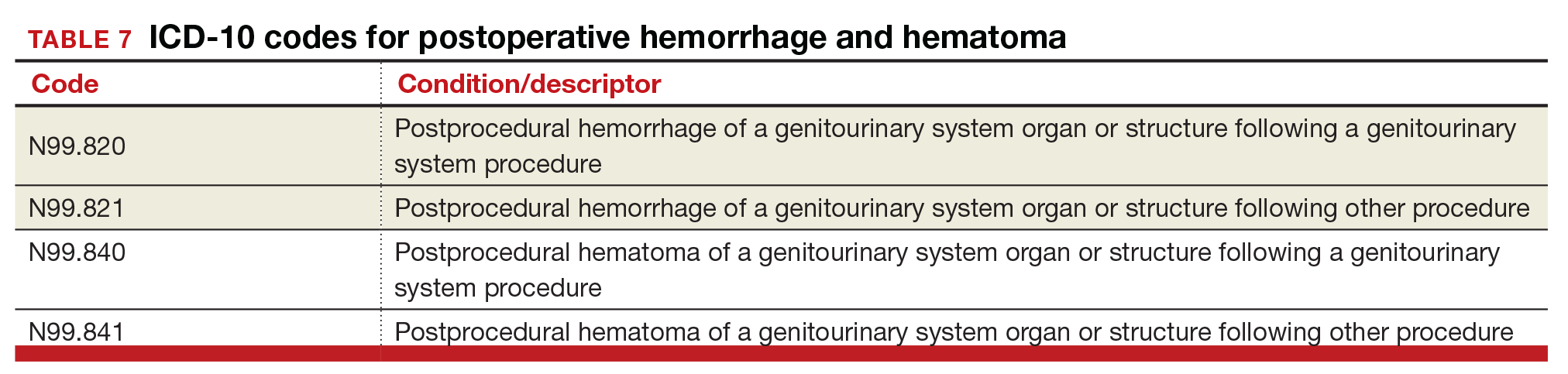
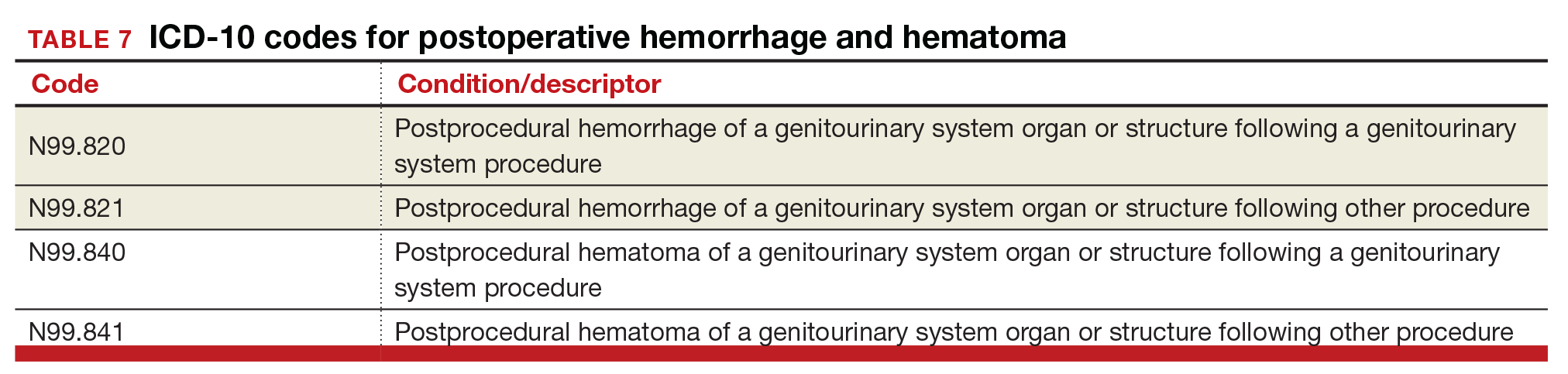
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
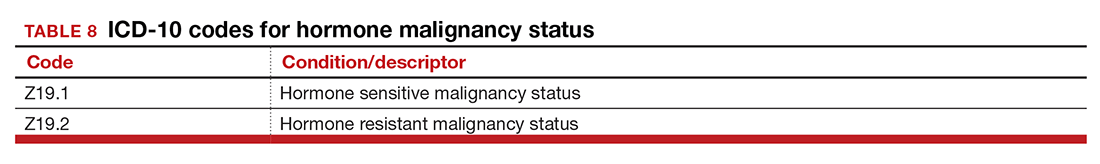
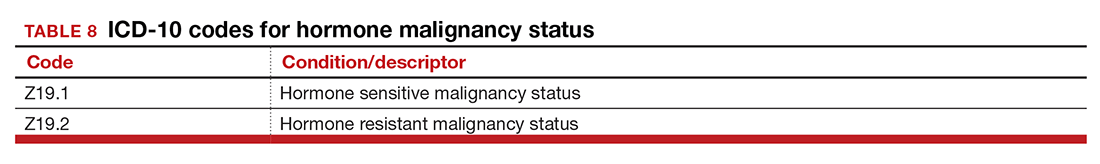
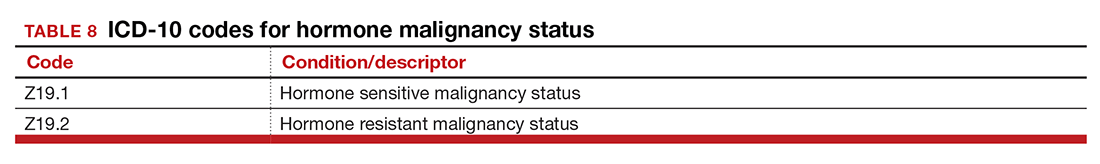
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
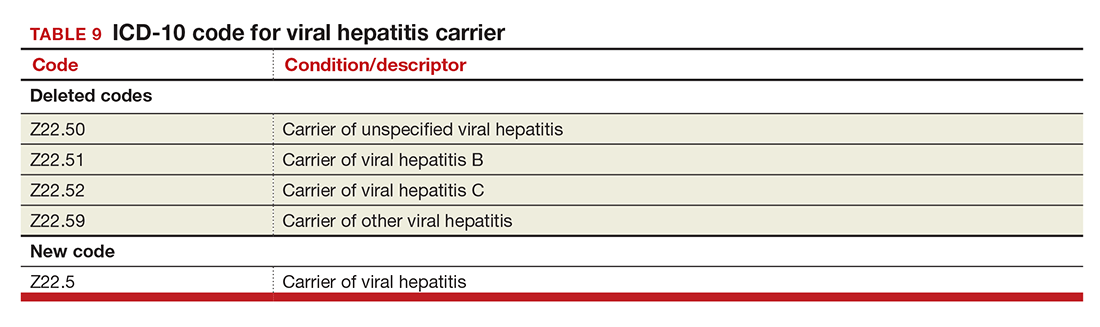
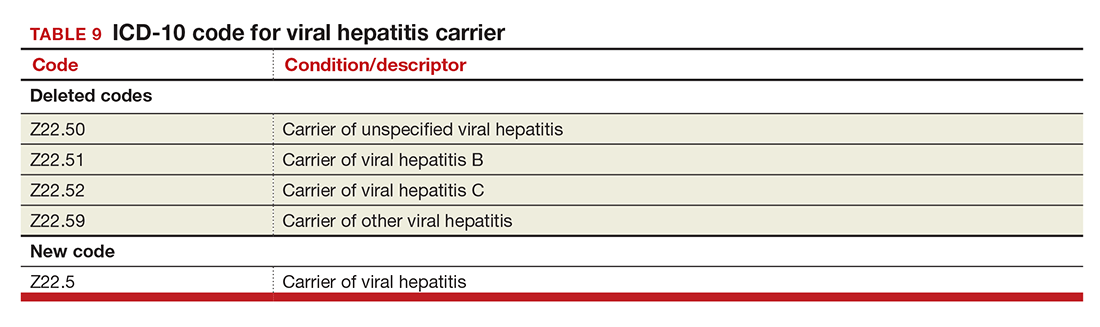
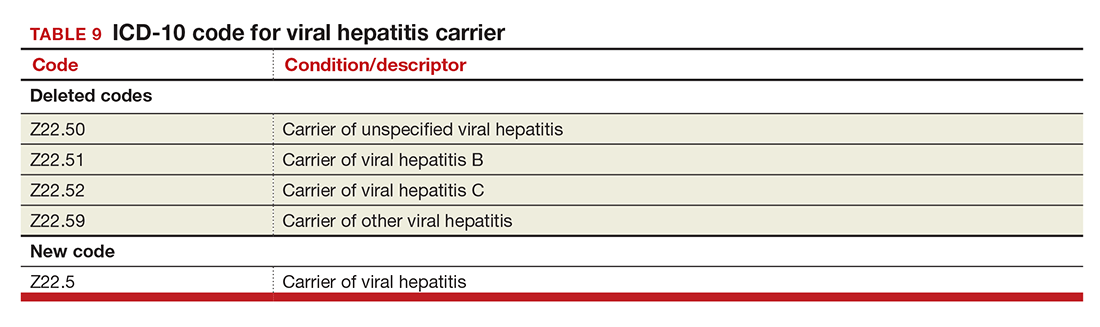
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
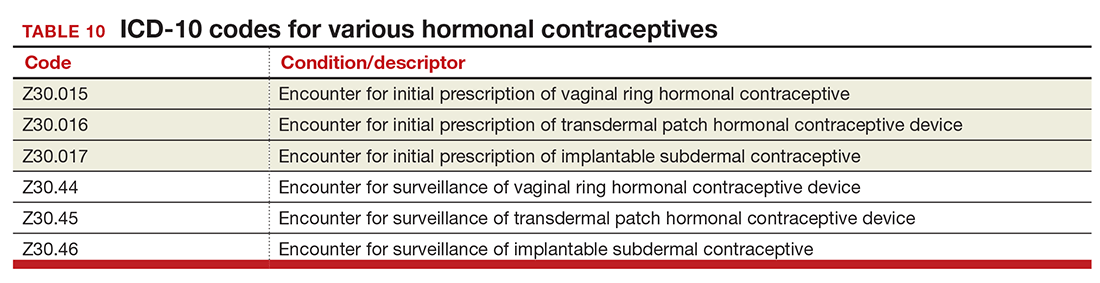
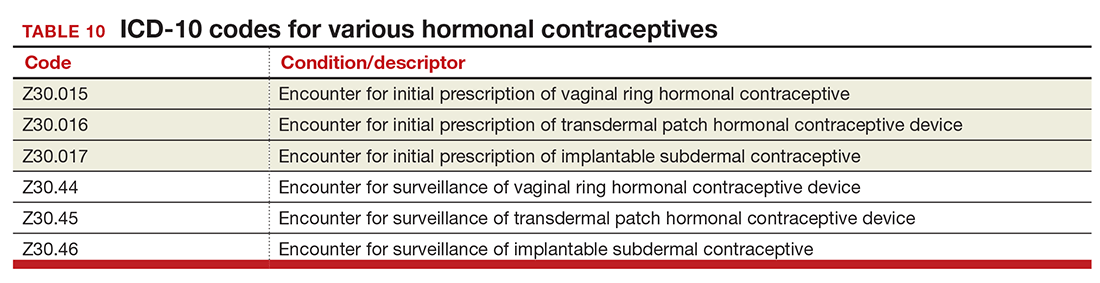
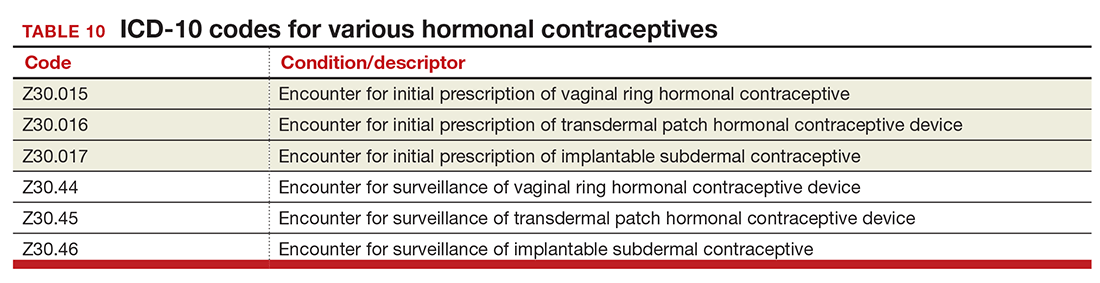
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
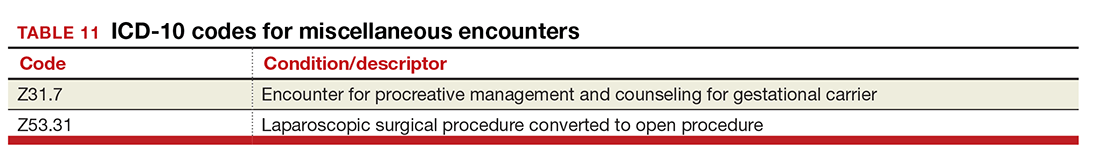
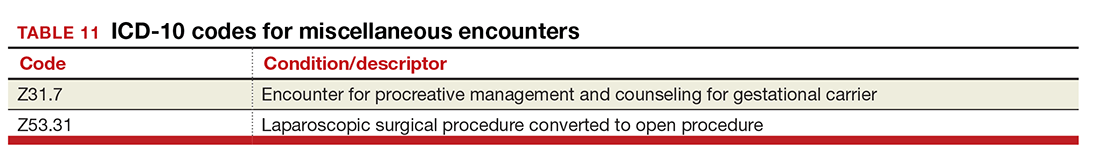
Miscellaneous code changes
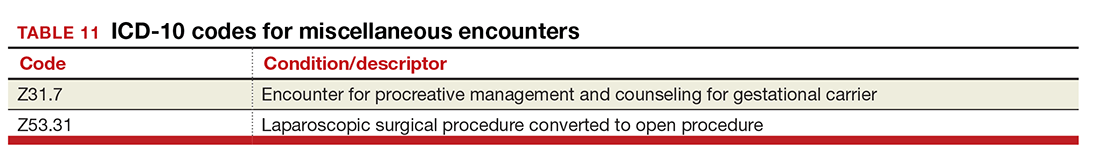
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
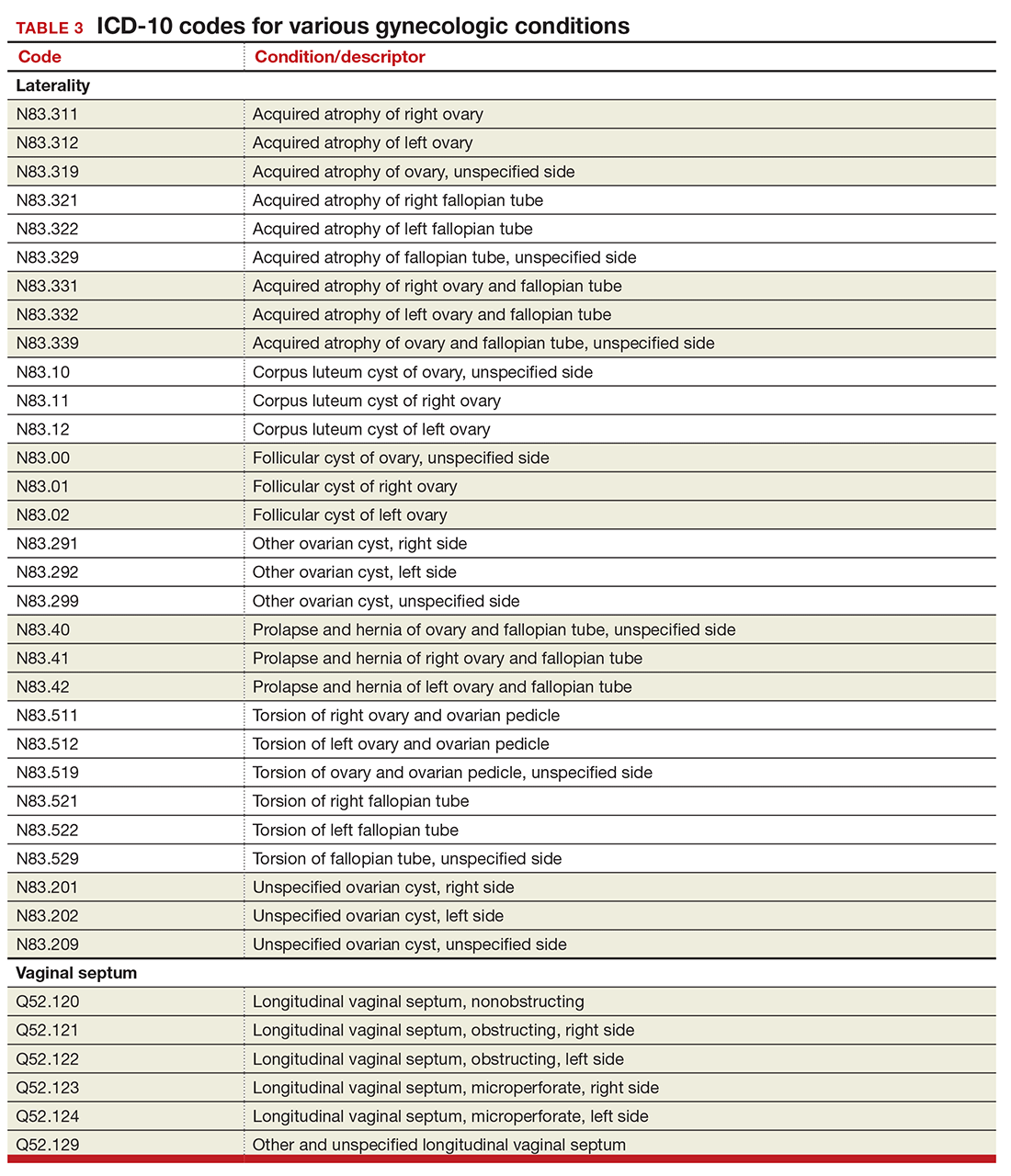
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
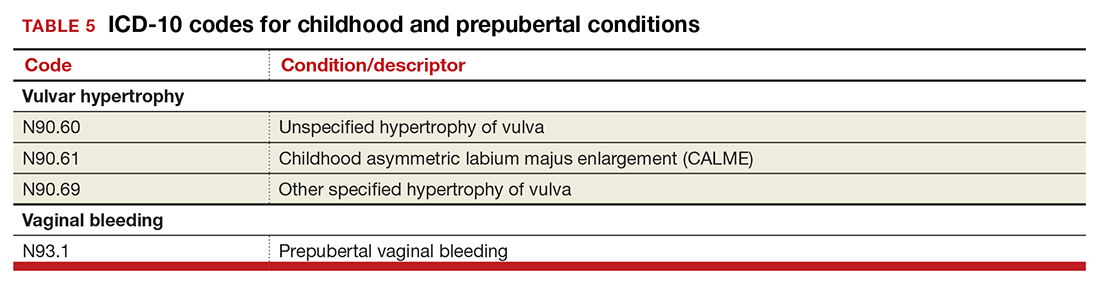
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In the August 2016 issue of OBG
Urogynecology diagnostic codes
Urogynecologists will find a large number of changes to codes they can select on October 1, 2016. While some codes improve reporting for conditions or symptoms related to urinary issues, many more concern postoperative complications following surgery for devices and grafts applied to the genitourinary system.
The American Urological Association requested new codes to align with a 2009 joint report on the terminology for female pelvic floor dysfunction.1 These codes, along with others, are listed in TABLE 1.
Urinary procedure complication codes
Not every urogynecologist will have an issue after surgery for incontinence, but if they do, there are tons of new and revised codes to address every possible complication the patient may have (TABLE 2). Each of these codes is reported based on whether the complication is being actively treated (initial encounter: final character is A), is being followed up after treatment (subsequent encounter: final character is D), or is caused by another condition (sequela: final character is S).
Gynecology-related diagnostic codes
Laterality
If there are 2 organs in the genitourinary system, the chances are good that there is now a right and a left designation code in ICD-10. Documentation should be clear, of course, and if the condition exists on both the right and the left side (even if only one side is being treated actively), list both codes, as there is no bilateral designation in the codes (TABLE 3). And while there is a code for “unspecified side,” providers normally do know which side, so use of this code should be avoided, if possible.
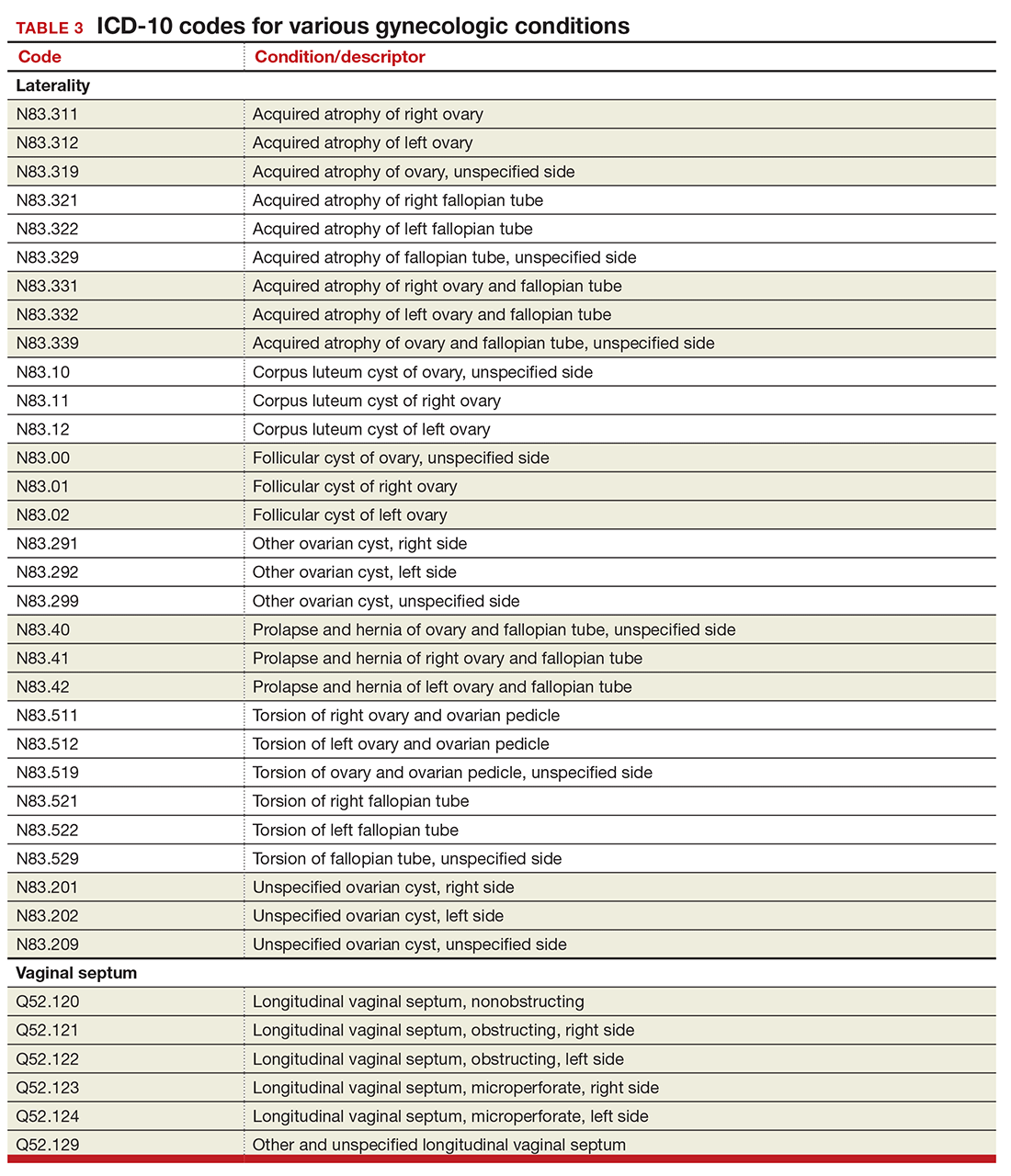
Vaginal septum
The right and left designations extend to the congenital codes for vaginal septum, but they go one step further. The American Congress of Obstetricians and Gynecologists (ACOG) requested that the codes for longitudinal vaginal septum be expanded to differentiate a nonobstructing vaginal septum from an obstructing vaginal septum, in addition to adding laterality to these codes (TABLE 3).2
Mastitis
There are now 2 new codes for inflammation of the breast; one describes mastitis without abscess, while the other code includes an abscess of the breast and nipple (TABLE 4). Once again, documentation will lead to the most specific code to describe the findings.
Childhood and prepubertal concerns
The single code for hypertrophy of the vulva has been expanded to include asymmetric labium majus enlargement. This code was requested by ACOG because this is a known clinical diagnosis and the currently available vulvar codes are inadequate for capturing this condition. The vulvar enlargement appears to be in response to hormonal surges during prepuberty and early puberty. Adult hypertrophy, either congenital or acquired from childbirth or as a late result of an old injury, would be reported by the “other specified” code (TABLE 5).
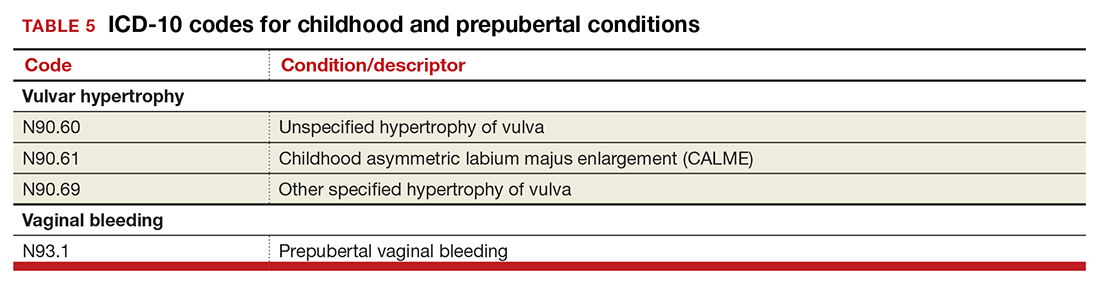
The causes of prepubertal bleeding vary and include the presence of a foreign object, tumors, or fluctuations in hormones, but prepubertal bleeding differs from the bleeding associated with normal menstruation. For that reason, ACOG requested a code that better captures the nature of the condition before a thorough work-up has pinpointed the cause (TABLE 5). Once the cause of the bleeding is known, a more specific diagnosis would then be reported (eg, D28.1, Benign neoplasm of vagina, or T19.2XXA, Foreign body in vulva and vagina, initial encounter).
Dypareunia
Additional documentation for dyspareunia will now be required to ensure that the most specific code is reported. In this case, the clinician should identify whether the pain is superficial or deep to better report on female pelvic floor dysfunction and to support the different treatments based on the location of the pain (TABLE 6). Deep dyspareunia would be felt in the mid or upper vagina.
Postoperative hemorrhage and hematoma
The codes for postprocedural hemorrhage and hematomas have received a face-lift: the single codes for these 2 complications will be split so that each can be reported separately (TABLE 7). Note that the new codes require that the condition be found following the initial surgery, and the code selected depends on whether the surgery involved the genitourinary system or another system.
Hormone malignancy status
The new Z19 codes will augment information known about a patient’s neoplasm (TABLE 8). The ICD-10 rule states that the type and location of the neoplasm are always coded first, followed by one of the new Z19 codes, if known.
Viral hepatitis carrier
The more specific code for type of viral hepatitis the patient is a carrier of has been bundled into a single code for viral hepatitis (TABLE 9). Carrier status in ICD-10 is defined as a person who harbors the specific organisms of a disease, does not currently have any symptoms, but is capable of transmitting the infection.
Contraception
The good news is that the ICD-9 code for contraceptive subdermal implants has been added to ICD-10 coding. In addition, the codes for contraceptive methods have been expanded to also include vaginal rings and transdermal patches (TABLE 10).
Miscellaneous code changes
Counseling a patient prior to pregnancy just got easier with the addition of a code for gestational carriers. Also, the old ICD-9 code that let a payer know that a procedure was converted from a laparoscopic to an open abdominal procedure is back (TABLE 11).
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. September 23–24, 2014;28–29. https://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed August 30, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee Meeting: diagnosis agenda. March 18–19, 2015. http://www.cdc.gov/nchs/data/icd/Tentative_Agenda_March%202015_Final.pdf. Accessed August 30, 2016.
In this Article
- Urogynecology dx codes
- Gynecology dx codes
- Codes for hormonal contraceptives
My go-to Web resources for quick ICD-10 coding questions
An OBG Management reader recently requested assistance finding an app or Web site that would be helpful for International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) coding, particularly for practicing ObGyns. It is not surprising that I have received this question, as we already are seeing a ton of smartphone apps that promise to search through the code descriptions quickly. None of these apps are ObGyn-specific but, given the vast amount, deciding which one is the best option to purchase and download can be a challenge.
Purchase considerations
Before you buy, decide what features you are looking for and make sure the app you have chosen can deliver what you need. Pay special attention to any reviews to learn the app’s pros and the cons. For instance, some apps offer code conversion from ICD-9 to ICD-10. Keep in mind, however, that not all conversions are accurate, and your search may just lead you to another unspecified code. Some apps will offer a decision tree, which is ideal. What you would like to avoid is an app that generates a list of 200 codes from a single search term.
A useful resource that I have found is this Buyers Guide to Mobile ICD-10 Apps from mHealthNews.1 This guide compares and contrasts the available apps (as of March 2014) for Android and Apple products. Some, you will note, are free; others are not. Try out a few before choosing. While several companies have developed products geared for ICD-10, many are not geared for mobile use and may have a substantial purchase price. Many of them also seem to be geared toward coders, not toward physician users.
My picks
ICD-10 Search was developed by e-MDs.2 It appears that this search program is part of a more extensive product that e-MDs sells, but for the time being, is free. This app deserves a look, especially because the decision tree format quickly gets you to the most specific code.
ICD-10 Code Lookup is the official offering from the Centers for Medicare & Medicaid Services (CMS).3 After you type in the term you are looking for, you get the search results in code order. The more specific your search terms, the closer you will get to the needed code. One caveat: the search mode is not set up to accept all clinical terms. For instance, I typed in "menorrhagia" and got 0 results; I typed in “menstruation, frequent” and I received 2 codes.
I hope this information is helpful, and I wish you an easy transition from ICD-9 to ICD-10.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
1. Schwartz E. Buyers guide to mobile ICD-10 apps. mHealthNews. http://www.mhealthnews.com/news/buyers-guide-mobile-icd-10-apps-smartphone-Apple-Android?page=0. Published March 24, 2014. Accessed September 16, 2015.
2. ICD-10 Search. e-MDs, Inc. http://app.icd10survivalkit.com/#tabDiagnosis. Accessed September 16, 2015.
3. Centers for Medicare & Medicaid Services. ICD-10 Code Lookup. https://www.cms.gov/medicare-coverage-database/staticpages/icd-10-code-lookup.aspx?KeyWord=follicular%20cyst&bc=AAAAAAAAAAACAA%3d%3d&. Accessed September 16, 2015.
An OBG Management reader recently requested assistance finding an app or Web site that would be helpful for International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) coding, particularly for practicing ObGyns. It is not surprising that I have received this question, as we already are seeing a ton of smartphone apps that promise to search through the code descriptions quickly. None of these apps are ObGyn-specific but, given the vast amount, deciding which one is the best option to purchase and download can be a challenge.
Purchase considerations
Before you buy, decide what features you are looking for and make sure the app you have chosen can deliver what you need. Pay special attention to any reviews to learn the app’s pros and the cons. For instance, some apps offer code conversion from ICD-9 to ICD-10. Keep in mind, however, that not all conversions are accurate, and your search may just lead you to another unspecified code. Some apps will offer a decision tree, which is ideal. What you would like to avoid is an app that generates a list of 200 codes from a single search term.
A useful resource that I have found is this Buyers Guide to Mobile ICD-10 Apps from mHealthNews.1 This guide compares and contrasts the available apps (as of March 2014) for Android and Apple products. Some, you will note, are free; others are not. Try out a few before choosing. While several companies have developed products geared for ICD-10, many are not geared for mobile use and may have a substantial purchase price. Many of them also seem to be geared toward coders, not toward physician users.
My picks
ICD-10 Search was developed by e-MDs.2 It appears that this search program is part of a more extensive product that e-MDs sells, but for the time being, is free. This app deserves a look, especially because the decision tree format quickly gets you to the most specific code.
ICD-10 Code Lookup is the official offering from the Centers for Medicare & Medicaid Services (CMS).3 After you type in the term you are looking for, you get the search results in code order. The more specific your search terms, the closer you will get to the needed code. One caveat: the search mode is not set up to accept all clinical terms. For instance, I typed in "menorrhagia" and got 0 results; I typed in “menstruation, frequent” and I received 2 codes.
I hope this information is helpful, and I wish you an easy transition from ICD-9 to ICD-10.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
An OBG Management reader recently requested assistance finding an app or Web site that would be helpful for International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) coding, particularly for practicing ObGyns. It is not surprising that I have received this question, as we already are seeing a ton of smartphone apps that promise to search through the code descriptions quickly. None of these apps are ObGyn-specific but, given the vast amount, deciding which one is the best option to purchase and download can be a challenge.
Purchase considerations
Before you buy, decide what features you are looking for and make sure the app you have chosen can deliver what you need. Pay special attention to any reviews to learn the app’s pros and the cons. For instance, some apps offer code conversion from ICD-9 to ICD-10. Keep in mind, however, that not all conversions are accurate, and your search may just lead you to another unspecified code. Some apps will offer a decision tree, which is ideal. What you would like to avoid is an app that generates a list of 200 codes from a single search term.
A useful resource that I have found is this Buyers Guide to Mobile ICD-10 Apps from mHealthNews.1 This guide compares and contrasts the available apps (as of March 2014) for Android and Apple products. Some, you will note, are free; others are not. Try out a few before choosing. While several companies have developed products geared for ICD-10, many are not geared for mobile use and may have a substantial purchase price. Many of them also seem to be geared toward coders, not toward physician users.
My picks
ICD-10 Search was developed by e-MDs.2 It appears that this search program is part of a more extensive product that e-MDs sells, but for the time being, is free. This app deserves a look, especially because the decision tree format quickly gets you to the most specific code.
ICD-10 Code Lookup is the official offering from the Centers for Medicare & Medicaid Services (CMS).3 After you type in the term you are looking for, you get the search results in code order. The more specific your search terms, the closer you will get to the needed code. One caveat: the search mode is not set up to accept all clinical terms. For instance, I typed in "menorrhagia" and got 0 results; I typed in “menstruation, frequent” and I received 2 codes.
I hope this information is helpful, and I wish you an easy transition from ICD-9 to ICD-10.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com
1. Schwartz E. Buyers guide to mobile ICD-10 apps. mHealthNews. http://www.mhealthnews.com/news/buyers-guide-mobile-icd-10-apps-smartphone-Apple-Android?page=0. Published March 24, 2014. Accessed September 16, 2015.
2. ICD-10 Search. e-MDs, Inc. http://app.icd10survivalkit.com/#tabDiagnosis. Accessed September 16, 2015.
3. Centers for Medicare & Medicaid Services. ICD-10 Code Lookup. https://www.cms.gov/medicare-coverage-database/staticpages/icd-10-code-lookup.aspx?KeyWord=follicular%20cyst&bc=AAAAAAAAAAACAA%3d%3d&. Accessed September 16, 2015.
1. Schwartz E. Buyers guide to mobile ICD-10 apps. mHealthNews. http://www.mhealthnews.com/news/buyers-guide-mobile-icd-10-apps-smartphone-Apple-Android?page=0. Published March 24, 2014. Accessed September 16, 2015.
2. ICD-10 Search. e-MDs, Inc. http://app.icd10survivalkit.com/#tabDiagnosis. Accessed September 16, 2015.
3. Centers for Medicare & Medicaid Services. ICD-10 Code Lookup. https://www.cms.gov/medicare-coverage-database/staticpages/icd-10-code-lookup.aspx?KeyWord=follicular%20cyst&bc=AAAAAAAAAAACAA%3d%3d&. Accessed September 16, 2015.
ICD-10-CM documentation and coding for obstetric procedures
The countdown is on for the big coding switch. Last month I wrote about changes in International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes that will occur in relation to gynecologic services, but now it’s time to tackle obstetric services. For obstetricians, the changes will be all about definitions. And documentation of obstetric conditions will be more complicated due to several factors, including the need to report trimester information and gestational age, use of a placeholder code, more complex guidelines for certain conditions, chorionicity for multiple gestations, and use of a 7th digit to identify the fetus with a problem.
No one is expecting clinicians to instantly be fluent in code-speak, but in order for the most specific diagnoses to be reported, the clinical documentation must be spot on. Think of it this way: ICD-10-CM is not requiring you to document more, it’s requiring you to document more precisely.
How to get started
Figuring out where you are now goes a long way toward knowing where you need to be when the calendar changes to October 1—and the best way to do it is to perform a gap analysis. This analysis can be carried out by the clinician or a qualified practice staff person.
To begin, run a report of the distinct obstetric codes you have billed in 2015 by frequency. Then sort them in numeric order so that each individual code category is captured for all of the 5th digits (and the code then will be counted as a single code). Finally, review 5 medical records for each of the top 10 reported diagnosis categories and determine whether you could have reported a more specific ICD-10-CM code.
The information you gain will go a long way toward identifying potential weaknesses in the documentation, or, if you are currently using an electronic health record (EHR) to look up a code, it will point up any weak points in searching for the right code, based on your specific documentation at the encounter. Remember, practice makes perfect…eventually.
Well-trained staff can help
Not only must you, the clinician, learn about the part your clinical documentation will play in providing the most specific information that will lead to a very specific code, but your coding and billing staff will need training as well. They are the ones who should be checking your claims for accuracy from October 1 forward, as they will know the basic rules about which codes can be billed together, code order, place codes, and so on. In other words, while you as a clinician should be responsible for picking the more specific code in ICD-10-CM, your staff is your backup when you don’t.
Feedback from your staff on how the claims are being processed and, perhaps, the overuse of unspecified codes will keep you moving toward the goal of complete and precise clinical documentation and the reporting of diagnoses at the highest level possible given the documentation.
Highlights of ICD-10-CM obstetric coding
Given the complexity of obstetric coding, this article deals only with the most important changes. It will be up to each clinician to learn the rules that surround the diagnostic codes that you report most frequently. Here again, a trained staff can help by preparing specific coding tools for the most frequently used diagnoses, including notes about what must be in the record to report the most specific code.
Trimester, gestational age, and timing definitions
The majority of obstetric complication codes (these are the codes that start with the letter “O”) and the “Z” codes for supervision of a normal pregnancy require trimester information to be valid. In the outpatient setting, the trimester will be based on the gestational age at the date of the encounter. For inpatient admissions, the trimester will be based on the age at the time of admission; if the patient is hospitalized over more than one trimester, it is the admission trimester that continues to be recorded, not the discharge trimester.
Although there are codes that indicate an unspecified trimester, they should be reported rarely if this information is, in fact, available. Trimesters are defined as:
- first: less than 14 weeks, 0 days
- second: 14 weeks, 0 days to less than 28 weeks, 0 days
- third: 28 weeks, 0 days until delivery.
Examples of trimester codes include:
- O25.11Malnutrition in pregnancy, first trimester
- O14.02 Mild to moderate preeclampsia, second trimester
- O24.013 Preexisting diabetes mellitus, type 1, in pregnancy, third trimester.
However, definitions in ICD-10-CM go beyond this, and these definitions will have to be taken into account to provide sufficient documentation to report the condition. In ICD-9-CM, a missed abortion and early hemorrhage in pregnancy occurred prior to 22 completed weeks, but in ICD-10-CM that definition changes to prior to 20 completed weeks.
Additional definitions that may impact coding:
- preterm labor or delivery: 20 completed weeks to less than 37 completed weeks
- full-term labor or delivery: 37 completed weeks to 40 completed weeks
- postterm pregnancy: more than 40 completed weeks to 42 completed weeks
- prolonged pregnancy: more than 42 completed weeks.
You also will be required to include a code for gestational age any time you report an obstetric complication. This and the trimester information will change as the pregnancy advances, so always be sure that the code selected matches the gestational age on the flow sheet at the time of the encounter. The gestational age code is Z3A.__, with the final 2 digits representing the weeks of gestation (for instance, from 27 weeks, 0 days to 27 weeks, 6 days, the final 2 digits will be “27”).
ICD-10-CM also has different conventions when it comes to timing as it relates to conditions that are present during the episode in which the patient delivers. When this is the case, an “in childbirth” code must be selected instead of assigning the diagnosis by trimester, if one is available. There also are codes that are specific to “in the puer-perium,” and these generally will be reported after the patient has been discharged after delivery but also would be reported if there is no “in childbirth” code available at the time of delivery. The code categories to which this concept will apply are:
- preexisting hypertension
- diabetes mellitus
- malnutrition
- liver and biliary tract disorders
- subluxation of symphysis (pubis)
- obstetric embolism
- maternal infectious and parasitic diseases classifiable elsewhere
- other maternal diseases classifiable elsewhere
- maternal malignant neoplasms, traumatic injuries, and abuse classifiable elsewhere.
Taking time to read a code description from a search program or drop-down menu also will be important because some codes refer to “of the puerperium” versus “complicating the puerperium” or “in the puerperium.” The first reference means that the condition develops after delivery, while the second and third terms mean that it developed prior to delivery. For example, code O90.81, Anemia of the puerperium, refers to anemia that develops following delivery, while code O99.03 Anemia complicating the puerperium, denotes preexisting anemia that is still present in the postpartum period.
Multiple gestation coding and the 7th digit
The first thing you will notice here is that several code categories require a 7th numeric character of 0 or 1 through 9. This rule will apply to the following categories:
- complications specific to multiple gestation
- maternal care for malpresentation of fetus
- maternal care for disproportion
- maternal care for known or suspected fetal abnormality and damage
- maternal care for other fetal problems
- polyhydramnios
- other disorders of amniotic fluid and membranes
- preterm labor with preterm delivery
- term delivery with preterm labor
- obstructed labor due to malposition and malpresentation of fetus
- labor and delivery with umbilical cord complications.
A 7th character of 0 will be reported if this is a singleton pregnancy, and the numbers 1 through 5 and 9 refer to which fetus of the multiple gestation has the problem. The number 9 would indicate any fetus that was not labeled as 1 to 5.
The trick in documentation will be identifying the fetus with the problem consistently while still recognizing that, in some cases, such as fetal position, twins may switch places. On the other hand, if one fetus is small for dates, chances are good that this fetus will remain so during pregnancy when twins are present.
A code will be denied as invalid without this 7th digit, so it will be good practice for the clinician to document this information at each visit.
Additional information in regard to multiple gestations will be the chorionicity of the pregnancy, if known, but there will also be an “unable to determine” and an “unspecified” code available if that better fits the documentation for the visit. Note, however, that there is no code for a trichorionic/ triamniotic pregnancy; therefore, only the unspecified code would be reported in that case. In addition, if there is a continuing pregnancy after fetal loss, the cause must be identified within the code (that is, fetal reduction, fetal demise [and retained], or spontaneous abortion).
Documentation requirements for certain conditions
If you plan on reporting any complication of pregnancy at the time of the encounter, information about that condition needs to be part of the antepartum flow sheet comments. If, at the time of the encounter, a condition the patient has is not addressed and the entire visit involves only routine care, you would report the code for routine supervision of preg- nancy rather than the complication code. If the complication is again addressed at a later visit, the complication code would be reported again for that visit. The routine supervision code and the complication code cannot be reported on the record for the same encounter under ICD-10-CM rules.
Hypertension. Documentation needs to state whether the hypertension is preexisting or gestational. If it is preexisting, it needs to be identified as essential or secondary. If the patient also has hypertensive heart disease or chronic kidney disease, this information should be included, as different codes must be selected.
Diabetes. The documentation needs to state whether it is preexisting or gestational. If preexisting, you must document whether it is type 1 or type 2. If it is type 2, you must report an additional code for long-term insulin use, if applicable. The assumption for a woman with type 1 diabetes is that she is always insulin-dependent, so long-term use is not reported separately. Note, however, that neither metformin nor glyburide is considered insulin and there is no mechanism for reporting control with these medications.
If diabetes is gestational, you must indicate whether the patient’s blood glucose level is controlled by diet or insulin. If both, report only the insulin. There is no code for the use of other medications for the control of gestational diabetes, so you would have to report an unspecified code in that case.
Also note that ICD-10-CM differentiates between an abnormal 1-hour glucose tolerance test (GTT) and gestational diabetes. Unless a 3-specimen or 4-specimen GTT has been performed and results are abnormal, a diagnosis of gestational diabetes should not be reported.
An additional code outside of the obstetric complication chapter is required to denote any manifestations of diabetes. If there are none, then a diabetes uncomplicated manifestation code must be reported.
Preterm labor and delivery. Your documentation must clearly indicate whether the patient has preterm labor with preterm delivery or whether the delivery is term in addition to the trimester. For instance, if you document that Mary presents with preterm labor at 27 weeks, 2 days and delivers a girl at 28 weeks, 6 days, your code will describe Preterm labor second trimester with preterm delivery third trimester. However, if Susan presents with preterm labor at 30 weeks, 2 days and is managed until 37 weeks, 1 day, when she delivers a baby boy, your code would describe Term delivery with preterm labor, third trimester.
New coding options
Among the new coding options under ICD-10-CM:
- Abnormal findings on antenatal screening. These would be reported when the antenatal test is abnormal but you have not yet determined a definitive diagnosis.
- Alcohol, drug, and tobacco use during pregnancy. If you report any of these codes, you must also report a manifestation code for the patient’s condition. If the use is uncomplicated, you would report that code instead.
- Abuse of the pregnant patient. You can report sexual, physical, or psychological abuse, but you also must report a code for any applicable injury to the patient and identify the abuser, if known.
- Pruritic urticarial papules and plaques of pregnancy
- Retained intrauterine contraceptive device in pregnancy
- Maternal care due to uterine scar from other previous surgery. This would mean a surgery other than a previous cesarean delivery.
- Maternal care for (suspected) damage to the fetus by other medical procedures
- Maternal care for hydrops fetalis
- Maternal care for viable fetus in abdominal pregnancy
- Malignant neoplasm complicating pregnancy
- Failed attempt at vaginal birth after previous cesarean delivery
- Supervision of high-risk pregnancy due to social problems (for instance, a homeless patient)
- Rh incompatibility status (when you lack confirmation of serum antibodies and are giving prophylactic Rho[D] immune globulin).
CMS takes steps to ease transition to ICD-10-CM
To help health care providers get “up to speed” on the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), which takes effect October 1, 2015, the Centers for Medicare and Medicaid Services (CMS) has launched a new series for specialists. A guide tailored to ObGyns is available at http://roadto10.org/example-practice-obgyn. The guide includes:
Parting words
ICD-10-CM may seem like the end of the world, but its difficulty is exaggerated. If you fail to prepare, you will fail, and money coming in the door may be affected. If you prepare with training and practice, you will have a short learning curve. I wish you all the best. If you have specific questions about your practice, don’t hesitate to let us know so they can be addressed early.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The countdown is on for the big coding switch. Last month I wrote about changes in International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes that will occur in relation to gynecologic services, but now it’s time to tackle obstetric services. For obstetricians, the changes will be all about definitions. And documentation of obstetric conditions will be more complicated due to several factors, including the need to report trimester information and gestational age, use of a placeholder code, more complex guidelines for certain conditions, chorionicity for multiple gestations, and use of a 7th digit to identify the fetus with a problem.
No one is expecting clinicians to instantly be fluent in code-speak, but in order for the most specific diagnoses to be reported, the clinical documentation must be spot on. Think of it this way: ICD-10-CM is not requiring you to document more, it’s requiring you to document more precisely.
How to get started
Figuring out where you are now goes a long way toward knowing where you need to be when the calendar changes to October 1—and the best way to do it is to perform a gap analysis. This analysis can be carried out by the clinician or a qualified practice staff person.
To begin, run a report of the distinct obstetric codes you have billed in 2015 by frequency. Then sort them in numeric order so that each individual code category is captured for all of the 5th digits (and the code then will be counted as a single code). Finally, review 5 medical records for each of the top 10 reported diagnosis categories and determine whether you could have reported a more specific ICD-10-CM code.
The information you gain will go a long way toward identifying potential weaknesses in the documentation, or, if you are currently using an electronic health record (EHR) to look up a code, it will point up any weak points in searching for the right code, based on your specific documentation at the encounter. Remember, practice makes perfect…eventually.
Well-trained staff can help
Not only must you, the clinician, learn about the part your clinical documentation will play in providing the most specific information that will lead to a very specific code, but your coding and billing staff will need training as well. They are the ones who should be checking your claims for accuracy from October 1 forward, as they will know the basic rules about which codes can be billed together, code order, place codes, and so on. In other words, while you as a clinician should be responsible for picking the more specific code in ICD-10-CM, your staff is your backup when you don’t.
Feedback from your staff on how the claims are being processed and, perhaps, the overuse of unspecified codes will keep you moving toward the goal of complete and precise clinical documentation and the reporting of diagnoses at the highest level possible given the documentation.
Highlights of ICD-10-CM obstetric coding
Given the complexity of obstetric coding, this article deals only with the most important changes. It will be up to each clinician to learn the rules that surround the diagnostic codes that you report most frequently. Here again, a trained staff can help by preparing specific coding tools for the most frequently used diagnoses, including notes about what must be in the record to report the most specific code.
Trimester, gestational age, and timing definitions
The majority of obstetric complication codes (these are the codes that start with the letter “O”) and the “Z” codes for supervision of a normal pregnancy require trimester information to be valid. In the outpatient setting, the trimester will be based on the gestational age at the date of the encounter. For inpatient admissions, the trimester will be based on the age at the time of admission; if the patient is hospitalized over more than one trimester, it is the admission trimester that continues to be recorded, not the discharge trimester.
Although there are codes that indicate an unspecified trimester, they should be reported rarely if this information is, in fact, available. Trimesters are defined as:
- first: less than 14 weeks, 0 days
- second: 14 weeks, 0 days to less than 28 weeks, 0 days
- third: 28 weeks, 0 days until delivery.
Examples of trimester codes include:
- O25.11Malnutrition in pregnancy, first trimester
- O14.02 Mild to moderate preeclampsia, second trimester
- O24.013 Preexisting diabetes mellitus, type 1, in pregnancy, third trimester.
However, definitions in ICD-10-CM go beyond this, and these definitions will have to be taken into account to provide sufficient documentation to report the condition. In ICD-9-CM, a missed abortion and early hemorrhage in pregnancy occurred prior to 22 completed weeks, but in ICD-10-CM that definition changes to prior to 20 completed weeks.
Additional definitions that may impact coding:
- preterm labor or delivery: 20 completed weeks to less than 37 completed weeks
- full-term labor or delivery: 37 completed weeks to 40 completed weeks
- postterm pregnancy: more than 40 completed weeks to 42 completed weeks
- prolonged pregnancy: more than 42 completed weeks.
You also will be required to include a code for gestational age any time you report an obstetric complication. This and the trimester information will change as the pregnancy advances, so always be sure that the code selected matches the gestational age on the flow sheet at the time of the encounter. The gestational age code is Z3A.__, with the final 2 digits representing the weeks of gestation (for instance, from 27 weeks, 0 days to 27 weeks, 6 days, the final 2 digits will be “27”).
ICD-10-CM also has different conventions when it comes to timing as it relates to conditions that are present during the episode in which the patient delivers. When this is the case, an “in childbirth” code must be selected instead of assigning the diagnosis by trimester, if one is available. There also are codes that are specific to “in the puer-perium,” and these generally will be reported after the patient has been discharged after delivery but also would be reported if there is no “in childbirth” code available at the time of delivery. The code categories to which this concept will apply are:
- preexisting hypertension
- diabetes mellitus
- malnutrition
- liver and biliary tract disorders
- subluxation of symphysis (pubis)
- obstetric embolism
- maternal infectious and parasitic diseases classifiable elsewhere
- other maternal diseases classifiable elsewhere
- maternal malignant neoplasms, traumatic injuries, and abuse classifiable elsewhere.
Taking time to read a code description from a search program or drop-down menu also will be important because some codes refer to “of the puerperium” versus “complicating the puerperium” or “in the puerperium.” The first reference means that the condition develops after delivery, while the second and third terms mean that it developed prior to delivery. For example, code O90.81, Anemia of the puerperium, refers to anemia that develops following delivery, while code O99.03 Anemia complicating the puerperium, denotes preexisting anemia that is still present in the postpartum period.
Multiple gestation coding and the 7th digit
The first thing you will notice here is that several code categories require a 7th numeric character of 0 or 1 through 9. This rule will apply to the following categories:
- complications specific to multiple gestation
- maternal care for malpresentation of fetus
- maternal care for disproportion
- maternal care for known or suspected fetal abnormality and damage
- maternal care for other fetal problems
- polyhydramnios
- other disorders of amniotic fluid and membranes
- preterm labor with preterm delivery
- term delivery with preterm labor
- obstructed labor due to malposition and malpresentation of fetus
- labor and delivery with umbilical cord complications.
A 7th character of 0 will be reported if this is a singleton pregnancy, and the numbers 1 through 5 and 9 refer to which fetus of the multiple gestation has the problem. The number 9 would indicate any fetus that was not labeled as 1 to 5.
The trick in documentation will be identifying the fetus with the problem consistently while still recognizing that, in some cases, such as fetal position, twins may switch places. On the other hand, if one fetus is small for dates, chances are good that this fetus will remain so during pregnancy when twins are present.
A code will be denied as invalid without this 7th digit, so it will be good practice for the clinician to document this information at each visit.
Additional information in regard to multiple gestations will be the chorionicity of the pregnancy, if known, but there will also be an “unable to determine” and an “unspecified” code available if that better fits the documentation for the visit. Note, however, that there is no code for a trichorionic/ triamniotic pregnancy; therefore, only the unspecified code would be reported in that case. In addition, if there is a continuing pregnancy after fetal loss, the cause must be identified within the code (that is, fetal reduction, fetal demise [and retained], or spontaneous abortion).
Documentation requirements for certain conditions
If you plan on reporting any complication of pregnancy at the time of the encounter, information about that condition needs to be part of the antepartum flow sheet comments. If, at the time of the encounter, a condition the patient has is not addressed and the entire visit involves only routine care, you would report the code for routine supervision of preg- nancy rather than the complication code. If the complication is again addressed at a later visit, the complication code would be reported again for that visit. The routine supervision code and the complication code cannot be reported on the record for the same encounter under ICD-10-CM rules.
Hypertension. Documentation needs to state whether the hypertension is preexisting or gestational. If it is preexisting, it needs to be identified as essential or secondary. If the patient also has hypertensive heart disease or chronic kidney disease, this information should be included, as different codes must be selected.
Diabetes. The documentation needs to state whether it is preexisting or gestational. If preexisting, you must document whether it is type 1 or type 2. If it is type 2, you must report an additional code for long-term insulin use, if applicable. The assumption for a woman with type 1 diabetes is that she is always insulin-dependent, so long-term use is not reported separately. Note, however, that neither metformin nor glyburide is considered insulin and there is no mechanism for reporting control with these medications.
If diabetes is gestational, you must indicate whether the patient’s blood glucose level is controlled by diet or insulin. If both, report only the insulin. There is no code for the use of other medications for the control of gestational diabetes, so you would have to report an unspecified code in that case.
Also note that ICD-10-CM differentiates between an abnormal 1-hour glucose tolerance test (GTT) and gestational diabetes. Unless a 3-specimen or 4-specimen GTT has been performed and results are abnormal, a diagnosis of gestational diabetes should not be reported.
An additional code outside of the obstetric complication chapter is required to denote any manifestations of diabetes. If there are none, then a diabetes uncomplicated manifestation code must be reported.
Preterm labor and delivery. Your documentation must clearly indicate whether the patient has preterm labor with preterm delivery or whether the delivery is term in addition to the trimester. For instance, if you document that Mary presents with preterm labor at 27 weeks, 2 days and delivers a girl at 28 weeks, 6 days, your code will describe Preterm labor second trimester with preterm delivery third trimester. However, if Susan presents with preterm labor at 30 weeks, 2 days and is managed until 37 weeks, 1 day, when she delivers a baby boy, your code would describe Term delivery with preterm labor, third trimester.
New coding options
Among the new coding options under ICD-10-CM:
- Abnormal findings on antenatal screening. These would be reported when the antenatal test is abnormal but you have not yet determined a definitive diagnosis.
- Alcohol, drug, and tobacco use during pregnancy. If you report any of these codes, you must also report a manifestation code for the patient’s condition. If the use is uncomplicated, you would report that code instead.
- Abuse of the pregnant patient. You can report sexual, physical, or psychological abuse, but you also must report a code for any applicable injury to the patient and identify the abuser, if known.
- Pruritic urticarial papules and plaques of pregnancy
- Retained intrauterine contraceptive device in pregnancy
- Maternal care due to uterine scar from other previous surgery. This would mean a surgery other than a previous cesarean delivery.
- Maternal care for (suspected) damage to the fetus by other medical procedures
- Maternal care for hydrops fetalis
- Maternal care for viable fetus in abdominal pregnancy
- Malignant neoplasm complicating pregnancy
- Failed attempt at vaginal birth after previous cesarean delivery
- Supervision of high-risk pregnancy due to social problems (for instance, a homeless patient)
- Rh incompatibility status (when you lack confirmation of serum antibodies and are giving prophylactic Rho[D] immune globulin).
CMS takes steps to ease transition to ICD-10-CM
To help health care providers get “up to speed” on the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), which takes effect October 1, 2015, the Centers for Medicare and Medicaid Services (CMS) has launched a new series for specialists. A guide tailored to ObGyns is available at http://roadto10.org/example-practice-obgyn. The guide includes:
Parting words
ICD-10-CM may seem like the end of the world, but its difficulty is exaggerated. If you fail to prepare, you will fail, and money coming in the door may be affected. If you prepare with training and practice, you will have a short learning curve. I wish you all the best. If you have specific questions about your practice, don’t hesitate to let us know so they can be addressed early.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The countdown is on for the big coding switch. Last month I wrote about changes in International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes that will occur in relation to gynecologic services, but now it’s time to tackle obstetric services. For obstetricians, the changes will be all about definitions. And documentation of obstetric conditions will be more complicated due to several factors, including the need to report trimester information and gestational age, use of a placeholder code, more complex guidelines for certain conditions, chorionicity for multiple gestations, and use of a 7th digit to identify the fetus with a problem.
No one is expecting clinicians to instantly be fluent in code-speak, but in order for the most specific diagnoses to be reported, the clinical documentation must be spot on. Think of it this way: ICD-10-CM is not requiring you to document more, it’s requiring you to document more precisely.
How to get started
Figuring out where you are now goes a long way toward knowing where you need to be when the calendar changes to October 1—and the best way to do it is to perform a gap analysis. This analysis can be carried out by the clinician or a qualified practice staff person.
To begin, run a report of the distinct obstetric codes you have billed in 2015 by frequency. Then sort them in numeric order so that each individual code category is captured for all of the 5th digits (and the code then will be counted as a single code). Finally, review 5 medical records for each of the top 10 reported diagnosis categories and determine whether you could have reported a more specific ICD-10-CM code.
The information you gain will go a long way toward identifying potential weaknesses in the documentation, or, if you are currently using an electronic health record (EHR) to look up a code, it will point up any weak points in searching for the right code, based on your specific documentation at the encounter. Remember, practice makes perfect…eventually.
Well-trained staff can help
Not only must you, the clinician, learn about the part your clinical documentation will play in providing the most specific information that will lead to a very specific code, but your coding and billing staff will need training as well. They are the ones who should be checking your claims for accuracy from October 1 forward, as they will know the basic rules about which codes can be billed together, code order, place codes, and so on. In other words, while you as a clinician should be responsible for picking the more specific code in ICD-10-CM, your staff is your backup when you don’t.
Feedback from your staff on how the claims are being processed and, perhaps, the overuse of unspecified codes will keep you moving toward the goal of complete and precise clinical documentation and the reporting of diagnoses at the highest level possible given the documentation.
Highlights of ICD-10-CM obstetric coding
Given the complexity of obstetric coding, this article deals only with the most important changes. It will be up to each clinician to learn the rules that surround the diagnostic codes that you report most frequently. Here again, a trained staff can help by preparing specific coding tools for the most frequently used diagnoses, including notes about what must be in the record to report the most specific code.
Trimester, gestational age, and timing definitions
The majority of obstetric complication codes (these are the codes that start with the letter “O”) and the “Z” codes for supervision of a normal pregnancy require trimester information to be valid. In the outpatient setting, the trimester will be based on the gestational age at the date of the encounter. For inpatient admissions, the trimester will be based on the age at the time of admission; if the patient is hospitalized over more than one trimester, it is the admission trimester that continues to be recorded, not the discharge trimester.
Although there are codes that indicate an unspecified trimester, they should be reported rarely if this information is, in fact, available. Trimesters are defined as:
- first: less than 14 weeks, 0 days
- second: 14 weeks, 0 days to less than 28 weeks, 0 days
- third: 28 weeks, 0 days until delivery.
Examples of trimester codes include:
- O25.11Malnutrition in pregnancy, first trimester
- O14.02 Mild to moderate preeclampsia, second trimester
- O24.013 Preexisting diabetes mellitus, type 1, in pregnancy, third trimester.
However, definitions in ICD-10-CM go beyond this, and these definitions will have to be taken into account to provide sufficient documentation to report the condition. In ICD-9-CM, a missed abortion and early hemorrhage in pregnancy occurred prior to 22 completed weeks, but in ICD-10-CM that definition changes to prior to 20 completed weeks.
Additional definitions that may impact coding:
- preterm labor or delivery: 20 completed weeks to less than 37 completed weeks
- full-term labor or delivery: 37 completed weeks to 40 completed weeks
- postterm pregnancy: more than 40 completed weeks to 42 completed weeks
- prolonged pregnancy: more than 42 completed weeks.
You also will be required to include a code for gestational age any time you report an obstetric complication. This and the trimester information will change as the pregnancy advances, so always be sure that the code selected matches the gestational age on the flow sheet at the time of the encounter. The gestational age code is Z3A.__, with the final 2 digits representing the weeks of gestation (for instance, from 27 weeks, 0 days to 27 weeks, 6 days, the final 2 digits will be “27”).
ICD-10-CM also has different conventions when it comes to timing as it relates to conditions that are present during the episode in which the patient delivers. When this is the case, an “in childbirth” code must be selected instead of assigning the diagnosis by trimester, if one is available. There also are codes that are specific to “in the puer-perium,” and these generally will be reported after the patient has been discharged after delivery but also would be reported if there is no “in childbirth” code available at the time of delivery. The code categories to which this concept will apply are:
- preexisting hypertension
- diabetes mellitus
- malnutrition
- liver and biliary tract disorders
- subluxation of symphysis (pubis)
- obstetric embolism
- maternal infectious and parasitic diseases classifiable elsewhere
- other maternal diseases classifiable elsewhere
- maternal malignant neoplasms, traumatic injuries, and abuse classifiable elsewhere.
Taking time to read a code description from a search program or drop-down menu also will be important because some codes refer to “of the puerperium” versus “complicating the puerperium” or “in the puerperium.” The first reference means that the condition develops after delivery, while the second and third terms mean that it developed prior to delivery. For example, code O90.81, Anemia of the puerperium, refers to anemia that develops following delivery, while code O99.03 Anemia complicating the puerperium, denotes preexisting anemia that is still present in the postpartum period.
Multiple gestation coding and the 7th digit
The first thing you will notice here is that several code categories require a 7th numeric character of 0 or 1 through 9. This rule will apply to the following categories:
- complications specific to multiple gestation
- maternal care for malpresentation of fetus
- maternal care for disproportion
- maternal care for known or suspected fetal abnormality and damage
- maternal care for other fetal problems
- polyhydramnios
- other disorders of amniotic fluid and membranes
- preterm labor with preterm delivery
- term delivery with preterm labor
- obstructed labor due to malposition and malpresentation of fetus
- labor and delivery with umbilical cord complications.
A 7th character of 0 will be reported if this is a singleton pregnancy, and the numbers 1 through 5 and 9 refer to which fetus of the multiple gestation has the problem. The number 9 would indicate any fetus that was not labeled as 1 to 5.
The trick in documentation will be identifying the fetus with the problem consistently while still recognizing that, in some cases, such as fetal position, twins may switch places. On the other hand, if one fetus is small for dates, chances are good that this fetus will remain so during pregnancy when twins are present.
A code will be denied as invalid without this 7th digit, so it will be good practice for the clinician to document this information at each visit.
Additional information in regard to multiple gestations will be the chorionicity of the pregnancy, if known, but there will also be an “unable to determine” and an “unspecified” code available if that better fits the documentation for the visit. Note, however, that there is no code for a trichorionic/ triamniotic pregnancy; therefore, only the unspecified code would be reported in that case. In addition, if there is a continuing pregnancy after fetal loss, the cause must be identified within the code (that is, fetal reduction, fetal demise [and retained], or spontaneous abortion).
Documentation requirements for certain conditions
If you plan on reporting any complication of pregnancy at the time of the encounter, information about that condition needs to be part of the antepartum flow sheet comments. If, at the time of the encounter, a condition the patient has is not addressed and the entire visit involves only routine care, you would report the code for routine supervision of preg- nancy rather than the complication code. If the complication is again addressed at a later visit, the complication code would be reported again for that visit. The routine supervision code and the complication code cannot be reported on the record for the same encounter under ICD-10-CM rules.
Hypertension. Documentation needs to state whether the hypertension is preexisting or gestational. If it is preexisting, it needs to be identified as essential or secondary. If the patient also has hypertensive heart disease or chronic kidney disease, this information should be included, as different codes must be selected.
Diabetes. The documentation needs to state whether it is preexisting or gestational. If preexisting, you must document whether it is type 1 or type 2. If it is type 2, you must report an additional code for long-term insulin use, if applicable. The assumption for a woman with type 1 diabetes is that she is always insulin-dependent, so long-term use is not reported separately. Note, however, that neither metformin nor glyburide is considered insulin and there is no mechanism for reporting control with these medications.
If diabetes is gestational, you must indicate whether the patient’s blood glucose level is controlled by diet or insulin. If both, report only the insulin. There is no code for the use of other medications for the control of gestational diabetes, so you would have to report an unspecified code in that case.
Also note that ICD-10-CM differentiates between an abnormal 1-hour glucose tolerance test (GTT) and gestational diabetes. Unless a 3-specimen or 4-specimen GTT has been performed and results are abnormal, a diagnosis of gestational diabetes should not be reported.
An additional code outside of the obstetric complication chapter is required to denote any manifestations of diabetes. If there are none, then a diabetes uncomplicated manifestation code must be reported.
Preterm labor and delivery. Your documentation must clearly indicate whether the patient has preterm labor with preterm delivery or whether the delivery is term in addition to the trimester. For instance, if you document that Mary presents with preterm labor at 27 weeks, 2 days and delivers a girl at 28 weeks, 6 days, your code will describe Preterm labor second trimester with preterm delivery third trimester. However, if Susan presents with preterm labor at 30 weeks, 2 days and is managed until 37 weeks, 1 day, when she delivers a baby boy, your code would describe Term delivery with preterm labor, third trimester.
New coding options
Among the new coding options under ICD-10-CM:
- Abnormal findings on antenatal screening. These would be reported when the antenatal test is abnormal but you have not yet determined a definitive diagnosis.
- Alcohol, drug, and tobacco use during pregnancy. If you report any of these codes, you must also report a manifestation code for the patient’s condition. If the use is uncomplicated, you would report that code instead.
- Abuse of the pregnant patient. You can report sexual, physical, or psychological abuse, but you also must report a code for any applicable injury to the patient and identify the abuser, if known.
- Pruritic urticarial papules and plaques of pregnancy
- Retained intrauterine contraceptive device in pregnancy
- Maternal care due to uterine scar from other previous surgery. This would mean a surgery other than a previous cesarean delivery.
- Maternal care for (suspected) damage to the fetus by other medical procedures
- Maternal care for hydrops fetalis
- Maternal care for viable fetus in abdominal pregnancy
- Malignant neoplasm complicating pregnancy
- Failed attempt at vaginal birth after previous cesarean delivery
- Supervision of high-risk pregnancy due to social problems (for instance, a homeless patient)
- Rh incompatibility status (when you lack confirmation of serum antibodies and are giving prophylactic Rho[D] immune globulin).
CMS takes steps to ease transition to ICD-10-CM
To help health care providers get “up to speed” on the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), which takes effect October 1, 2015, the Centers for Medicare and Medicaid Services (CMS) has launched a new series for specialists. A guide tailored to ObGyns is available at http://roadto10.org/example-practice-obgyn. The guide includes:
Parting words
ICD-10-CM may seem like the end of the world, but its difficulty is exaggerated. If you fail to prepare, you will fail, and money coming in the door may be affected. If you prepare with training and practice, you will have a short learning curve. I wish you all the best. If you have specific questions about your practice, don’t hesitate to let us know so they can be addressed early.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this Article
- How to do a gap analysis
- Highlights of OB coding
- Condition-specific coding notations
ICD-10-CM documentation and coding for GYN procedures
In 2 months, the new coding set will become the only accepted format for diagnostic coding on medical claims. By now, most clinicians and their staffs should have begun the training process, including the examination of current documentation patterns, to ensure that the more specific International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes can be reported.
In 2014, I informed you about the more general changes that are to come in the format and ideas for preparation.1 But now it is time to get down to the nitty-gritty (or granularity, if you prefer) of this coding format to ensure correct coding every time for your gynecology services. A separate article will appear in the September 2015 issue of OBG Management to describe diagnostic coding for obstetric care.
No wheel reinvention necessary
Many of the guidelines for ICD-9-CM will transfer over to ICD-10-CM, so it will not be necessary to reinvent the wheel—but there are important changes that will affect both your documentation and payers’ requirements for the highest level of specificity. There also will be some instructions in the tabular section of ICD-10-CM that will let you know whether a combination of codes can or cannot be reported together (called “excludes” notes). In the beginning, this process may require additional communication between practice staff and clinicians.
However, if your practice has prepared a teaching document that outlines currently used codes and compares them with ICD-10-CM code choices and provides comments in regard to issues such as code combinations, conversion to the new system should be almost seamless.
Remember, the documentation of the clinician drives the selection of the code. The less information provided, the less specificity—and the result may be increased denials due to medical necessity for procedures and treatments.
Most reported codes will begin with “N”
Although the format of the codes will change under ICD-10-CM, diagnostic reporting will remain the same for most of the gynecologic conditions reported, and clinicians should be aware that the codes they will be reporting mainly will come from those that begin with “N.” One advantage: None of these codes require a 7th character or utilize the “x” placeholder code. In fact, the majority of codes from this chapter will have a one-to-one counterpart in the ICD-9-CM codes. A few exceptions are outlined below.
In addition to the core of “N” codes, a handful of codes will come from other chapters to capture reasons for a gynecologic encounter or surgery. For instance, “Z” codes will be reported for encounters for reasons other than illness and include codes for contraceptive and procreative management, general counseling, history of diseases, preventive gynecologic examinations, and screening scenarios, to name just a few. “R” codes will be used most often for general signs and symptoms, such as abdominal pain or nausea and vomiting.
Your documentation will need to change in some important areas
When you see a patient for an injury to the urinary or pelvic organs that is not a complication of a procedure, or for a complication of a genitourinary prosthetic device, implant, or graft, you will need to document whether this is an initial or subsequent encounter or a sequela. This information is added as a 7th alpha character (a = initial, d = subsequent, s = sequela).
ICD-10-CM defines an initial encounter as the time period in which the patient is actively being treated. A subsequent encounter would be reported after the patient’s active treatment, while she is receiving routine care during the healing or recovery phase. For instance, you would report the encounter as subsequent when the patient is seen after her surgery for an injury to the ovary due to an automobile accident, but you would report an initial encounter for all visits through the surgical date of service when a patient presents with symptoms of mesh erosion requiring surgery. Sequela refers to a condition that developed as a result of another condition. For instance, if the patient’s intrauterine device (IUD) becomes embedded in the ostium due to an undetected uterine fibroid, that is a sequela.
The requirement to indicate laterality also will affect documentation, but this concept is limited to a few codes that might be reported by ObGyns. A designation of the right versus left organ will be required for reported cases of primary, secondary, borderline, or benign tumors of the breast, ovary, fallopian tube, broad ligament, and round ligament, as well as cancer in situ of the breast. However, the terms “bilateral” and “unilateral” are applied only to codes that describe hernias, acquired absence of the ovaries, and injuries to the ovaries and fallopian tubes that are not due to a surgical complication.
Unspecified codes still play a role
Unspecified ICD-10-CM codes still come into play when the clinician does not have enough information to assign a more specific code—that is, when, by the end of an encounter, no further information is available to assign a more specific diagnosis. For example, if a patient has signs of a fibroid upon examination, only the unspecified code can be reported until the clinician can discover whether it is intramural, submucosal, or subserosal. However, it would be equally incorrect to assign an unspecified code to an encounter once the nature of the fibroid has been determined.
Take note of these differences in coding
Here is a list of important new gynecologic coding requirements, which are presented in alphabetical order.
Amenorrhea, oligomenorrhea (N91.0–N91.5) and dysmenorrhea (N94.4–N94.5) will require documentation to indicate whether the condition is primary or secondary. Although an unspecified code is available, once treatment is begun the cause should be known and documented.
Artificial insemination problems will have a section:
- N98.0 Infection associated with artificial insemination
- N98.1 Hyperstimulation of ovaries
- N98.2 Complications of attempted introduction of fertilized ovum following in vitro fertilization
- N98.3 Complications of attempted introduction of embryo in embryo transfer
- N98.8 Other complications associated with artificial fertilization
- N98.9 Complication associated with artificial fertilization, unspecified.
Breast cancer codes will require documentation of which breast and what part of the breast is affected.
Contraceptive management highlights:
- Injectable contraceptives will have new codes for the initial prescription (Z30.013) and subsequent surveillance (Z30.42)
- IUD encounter for the prescription will have a new code (Z30.014), which is reported when the IUD is not being inserted on the same day
- Subdermal contraceptive implant surveillance will no longer have a specific code but will be included in the “other” contraceptive code Z30.49.
Conversion of a laparoscopic procedure to an open procedure will not have a code.
Cystocele, unspecified, will have code N81.10.
Dysplasia of vagina will be expanded into 3 codes based on mild, moderate, or unspecified: N89.0–N89.3.
Female genitourinary cancer codes:
- Documentation of right or left organs and which part of the uterus is affected will be required
- Cancer in situ of cervix will be expanded by site on the cervix: D06.0–D06.7
- Cancer in situ of the endometrium will have a specific code: D07.0.
Genuine stress urinary incontinence will only be referred to as stress incontinence (male or female). The code is now located in the urinary section of Chapter N: N39.3.
Genitourinary complications due to procedures and surgery will be organized in 1 section: N99
- Some conditions have more than 1 code based on cause:
- N99.2 Stricture of vagina due to surgical complication
- N89.5 Stricture of vagina not due to surgical complication
- N99.4 Pelvic adhesions due to surgical complication
- N73.6 Pelvic adhesions not due to surgical complication - Other codes will differentiate between intraoperative or postprocedure complications and whether the surgery is on the genitourinary system or a different surgery:
- N99.61 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating a genitourinary system procedure
- N99.62 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating other procedure
- N99.820 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following a genitourinary system procedure
- N99.821 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following other procedure.
Gynecologic examinations will have to include information on whether or not there were genitourinary abnormal findings on the exam. If so, an additional secondary code will be required to identify the abnormality: Z01.411 and finding code. (Without abnormal findings: Z01.419.) For instance, a diagnosis of bacterial vaginosis is made during the examination. The abnormal findings are not those from other areas such as the breast or thyroid.
Hematuria documentation must differentiate between gross: R31.0, benign essential:R31.1, or other forms: R31.2.
High-risk sexual behavior problems must be documented by heterosexual, bisexual, or homosexual behavior: Z72.51–Z72.53.
Hormonal contraceptives, long-term use, will have a specific code: Z79.3.
Hyperplasia without atypia (simple, complex, or benign) will be rolled into a single code: N85.01.
Immunizations, prophylactic, will not have specific codes as to type. An encounter for any type of immunization is Z23.
Pelvic pain will have its own symptom code: R10.2.
Personal history for cancer has been expanded:
- Personal history of cancer in situ:
- Z86.000 of breast
- Z86.001 of cervix uteri
- Z86.008 of other site - Personal history of benign neoplasm:
- Z86.012 of other benign neoplasm
- Z86.03 of uncertain behavior (borderline malignancies).
Procedures not carried out will be expanded in ICD-10 to include 2 new codes:
- Z53.01 Procedure contraindicated due to patient smoking
- Z53.21 Procedure not carried out because patient left before seeing physician.
Procreative management changes:
- Artificial insemination will not have a specific code
- New code for male factor infertility: Z31.81
- New code for Rh incompatibility: Z31.82. This code would be used when the patient presents for prophylactic rho(D) immune globulin in addition to the Z23 code for immunization. This code also would be reported for the patient being tested for isoimmunization with no test result at the time of the visit.
Uterine prolapse without vaginal wall prolapse (618.1) will not have a code replacement.
Vaginal conditions such as vaginal lacerations (old), leukorrhea not specified as infective, and vaginal hematoma will be represented by an “other” code: N89.8.
Vulvar cyst will have its own code: N90.7.
Vulvovaginitis has been expanded into category codes for acute, subacute/chronic conditions of both the vagina and the vulva, which changes the documentation requirements in order to code correctly: N76.0–N76.3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
1. Witt M. Moving forward with ICD-10: capitalize on this extra time. OBG Manag. 2014;26(7):17, 18, 20.
In 2 months, the new coding set will become the only accepted format for diagnostic coding on medical claims. By now, most clinicians and their staffs should have begun the training process, including the examination of current documentation patterns, to ensure that the more specific International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes can be reported.
In 2014, I informed you about the more general changes that are to come in the format and ideas for preparation.1 But now it is time to get down to the nitty-gritty (or granularity, if you prefer) of this coding format to ensure correct coding every time for your gynecology services. A separate article will appear in the September 2015 issue of OBG Management to describe diagnostic coding for obstetric care.
No wheel reinvention necessary
Many of the guidelines for ICD-9-CM will transfer over to ICD-10-CM, so it will not be necessary to reinvent the wheel—but there are important changes that will affect both your documentation and payers’ requirements for the highest level of specificity. There also will be some instructions in the tabular section of ICD-10-CM that will let you know whether a combination of codes can or cannot be reported together (called “excludes” notes). In the beginning, this process may require additional communication between practice staff and clinicians.
However, if your practice has prepared a teaching document that outlines currently used codes and compares them with ICD-10-CM code choices and provides comments in regard to issues such as code combinations, conversion to the new system should be almost seamless.
Remember, the documentation of the clinician drives the selection of the code. The less information provided, the less specificity—and the result may be increased denials due to medical necessity for procedures and treatments.
Most reported codes will begin with “N”
Although the format of the codes will change under ICD-10-CM, diagnostic reporting will remain the same for most of the gynecologic conditions reported, and clinicians should be aware that the codes they will be reporting mainly will come from those that begin with “N.” One advantage: None of these codes require a 7th character or utilize the “x” placeholder code. In fact, the majority of codes from this chapter will have a one-to-one counterpart in the ICD-9-CM codes. A few exceptions are outlined below.
In addition to the core of “N” codes, a handful of codes will come from other chapters to capture reasons for a gynecologic encounter or surgery. For instance, “Z” codes will be reported for encounters for reasons other than illness and include codes for contraceptive and procreative management, general counseling, history of diseases, preventive gynecologic examinations, and screening scenarios, to name just a few. “R” codes will be used most often for general signs and symptoms, such as abdominal pain or nausea and vomiting.
Your documentation will need to change in some important areas
When you see a patient for an injury to the urinary or pelvic organs that is not a complication of a procedure, or for a complication of a genitourinary prosthetic device, implant, or graft, you will need to document whether this is an initial or subsequent encounter or a sequela. This information is added as a 7th alpha character (a = initial, d = subsequent, s = sequela).
ICD-10-CM defines an initial encounter as the time period in which the patient is actively being treated. A subsequent encounter would be reported after the patient’s active treatment, while she is receiving routine care during the healing or recovery phase. For instance, you would report the encounter as subsequent when the patient is seen after her surgery for an injury to the ovary due to an automobile accident, but you would report an initial encounter for all visits through the surgical date of service when a patient presents with symptoms of mesh erosion requiring surgery. Sequela refers to a condition that developed as a result of another condition. For instance, if the patient’s intrauterine device (IUD) becomes embedded in the ostium due to an undetected uterine fibroid, that is a sequela.
The requirement to indicate laterality also will affect documentation, but this concept is limited to a few codes that might be reported by ObGyns. A designation of the right versus left organ will be required for reported cases of primary, secondary, borderline, or benign tumors of the breast, ovary, fallopian tube, broad ligament, and round ligament, as well as cancer in situ of the breast. However, the terms “bilateral” and “unilateral” are applied only to codes that describe hernias, acquired absence of the ovaries, and injuries to the ovaries and fallopian tubes that are not due to a surgical complication.
Unspecified codes still play a role
Unspecified ICD-10-CM codes still come into play when the clinician does not have enough information to assign a more specific code—that is, when, by the end of an encounter, no further information is available to assign a more specific diagnosis. For example, if a patient has signs of a fibroid upon examination, only the unspecified code can be reported until the clinician can discover whether it is intramural, submucosal, or subserosal. However, it would be equally incorrect to assign an unspecified code to an encounter once the nature of the fibroid has been determined.
Take note of these differences in coding
Here is a list of important new gynecologic coding requirements, which are presented in alphabetical order.
Amenorrhea, oligomenorrhea (N91.0–N91.5) and dysmenorrhea (N94.4–N94.5) will require documentation to indicate whether the condition is primary or secondary. Although an unspecified code is available, once treatment is begun the cause should be known and documented.
Artificial insemination problems will have a section:
- N98.0 Infection associated with artificial insemination
- N98.1 Hyperstimulation of ovaries
- N98.2 Complications of attempted introduction of fertilized ovum following in vitro fertilization
- N98.3 Complications of attempted introduction of embryo in embryo transfer
- N98.8 Other complications associated with artificial fertilization
- N98.9 Complication associated with artificial fertilization, unspecified.
Breast cancer codes will require documentation of which breast and what part of the breast is affected.
Contraceptive management highlights:
- Injectable contraceptives will have new codes for the initial prescription (Z30.013) and subsequent surveillance (Z30.42)
- IUD encounter for the prescription will have a new code (Z30.014), which is reported when the IUD is not being inserted on the same day
- Subdermal contraceptive implant surveillance will no longer have a specific code but will be included in the “other” contraceptive code Z30.49.
Conversion of a laparoscopic procedure to an open procedure will not have a code.
Cystocele, unspecified, will have code N81.10.
Dysplasia of vagina will be expanded into 3 codes based on mild, moderate, or unspecified: N89.0–N89.3.
Female genitourinary cancer codes:
- Documentation of right or left organs and which part of the uterus is affected will be required
- Cancer in situ of cervix will be expanded by site on the cervix: D06.0–D06.7
- Cancer in situ of the endometrium will have a specific code: D07.0.
Genuine stress urinary incontinence will only be referred to as stress incontinence (male or female). The code is now located in the urinary section of Chapter N: N39.3.
Genitourinary complications due to procedures and surgery will be organized in 1 section: N99
- Some conditions have more than 1 code based on cause:
- N99.2 Stricture of vagina due to surgical complication
- N89.5 Stricture of vagina not due to surgical complication
- N99.4 Pelvic adhesions due to surgical complication
- N73.6 Pelvic adhesions not due to surgical complication - Other codes will differentiate between intraoperative or postprocedure complications and whether the surgery is on the genitourinary system or a different surgery:
- N99.61 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating a genitourinary system procedure
- N99.62 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating other procedure
- N99.820 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following a genitourinary system procedure
- N99.821 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following other procedure.
Gynecologic examinations will have to include information on whether or not there were genitourinary abnormal findings on the exam. If so, an additional secondary code will be required to identify the abnormality: Z01.411 and finding code. (Without abnormal findings: Z01.419.) For instance, a diagnosis of bacterial vaginosis is made during the examination. The abnormal findings are not those from other areas such as the breast or thyroid.
Hematuria documentation must differentiate between gross: R31.0, benign essential:R31.1, or other forms: R31.2.
High-risk sexual behavior problems must be documented by heterosexual, bisexual, or homosexual behavior: Z72.51–Z72.53.
Hormonal contraceptives, long-term use, will have a specific code: Z79.3.
Hyperplasia without atypia (simple, complex, or benign) will be rolled into a single code: N85.01.
Immunizations, prophylactic, will not have specific codes as to type. An encounter for any type of immunization is Z23.
Pelvic pain will have its own symptom code: R10.2.
Personal history for cancer has been expanded:
- Personal history of cancer in situ:
- Z86.000 of breast
- Z86.001 of cervix uteri
- Z86.008 of other site - Personal history of benign neoplasm:
- Z86.012 of other benign neoplasm
- Z86.03 of uncertain behavior (borderline malignancies).
Procedures not carried out will be expanded in ICD-10 to include 2 new codes:
- Z53.01 Procedure contraindicated due to patient smoking
- Z53.21 Procedure not carried out because patient left before seeing physician.
Procreative management changes:
- Artificial insemination will not have a specific code
- New code for male factor infertility: Z31.81
- New code for Rh incompatibility: Z31.82. This code would be used when the patient presents for prophylactic rho(D) immune globulin in addition to the Z23 code for immunization. This code also would be reported for the patient being tested for isoimmunization with no test result at the time of the visit.
Uterine prolapse without vaginal wall prolapse (618.1) will not have a code replacement.
Vaginal conditions such as vaginal lacerations (old), leukorrhea not specified as infective, and vaginal hematoma will be represented by an “other” code: N89.8.
Vulvar cyst will have its own code: N90.7.
Vulvovaginitis has been expanded into category codes for acute, subacute/chronic conditions of both the vagina and the vulva, which changes the documentation requirements in order to code correctly: N76.0–N76.3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In 2 months, the new coding set will become the only accepted format for diagnostic coding on medical claims. By now, most clinicians and their staffs should have begun the training process, including the examination of current documentation patterns, to ensure that the more specific International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes can be reported.
In 2014, I informed you about the more general changes that are to come in the format and ideas for preparation.1 But now it is time to get down to the nitty-gritty (or granularity, if you prefer) of this coding format to ensure correct coding every time for your gynecology services. A separate article will appear in the September 2015 issue of OBG Management to describe diagnostic coding for obstetric care.
No wheel reinvention necessary
Many of the guidelines for ICD-9-CM will transfer over to ICD-10-CM, so it will not be necessary to reinvent the wheel—but there are important changes that will affect both your documentation and payers’ requirements for the highest level of specificity. There also will be some instructions in the tabular section of ICD-10-CM that will let you know whether a combination of codes can or cannot be reported together (called “excludes” notes). In the beginning, this process may require additional communication between practice staff and clinicians.
However, if your practice has prepared a teaching document that outlines currently used codes and compares them with ICD-10-CM code choices and provides comments in regard to issues such as code combinations, conversion to the new system should be almost seamless.
Remember, the documentation of the clinician drives the selection of the code. The less information provided, the less specificity—and the result may be increased denials due to medical necessity for procedures and treatments.
Most reported codes will begin with “N”
Although the format of the codes will change under ICD-10-CM, diagnostic reporting will remain the same for most of the gynecologic conditions reported, and clinicians should be aware that the codes they will be reporting mainly will come from those that begin with “N.” One advantage: None of these codes require a 7th character or utilize the “x” placeholder code. In fact, the majority of codes from this chapter will have a one-to-one counterpart in the ICD-9-CM codes. A few exceptions are outlined below.
In addition to the core of “N” codes, a handful of codes will come from other chapters to capture reasons for a gynecologic encounter or surgery. For instance, “Z” codes will be reported for encounters for reasons other than illness and include codes for contraceptive and procreative management, general counseling, history of diseases, preventive gynecologic examinations, and screening scenarios, to name just a few. “R” codes will be used most often for general signs and symptoms, such as abdominal pain or nausea and vomiting.
Your documentation will need to change in some important areas
When you see a patient for an injury to the urinary or pelvic organs that is not a complication of a procedure, or for a complication of a genitourinary prosthetic device, implant, or graft, you will need to document whether this is an initial or subsequent encounter or a sequela. This information is added as a 7th alpha character (a = initial, d = subsequent, s = sequela).
ICD-10-CM defines an initial encounter as the time period in which the patient is actively being treated. A subsequent encounter would be reported after the patient’s active treatment, while she is receiving routine care during the healing or recovery phase. For instance, you would report the encounter as subsequent when the patient is seen after her surgery for an injury to the ovary due to an automobile accident, but you would report an initial encounter for all visits through the surgical date of service when a patient presents with symptoms of mesh erosion requiring surgery. Sequela refers to a condition that developed as a result of another condition. For instance, if the patient’s intrauterine device (IUD) becomes embedded in the ostium due to an undetected uterine fibroid, that is a sequela.
The requirement to indicate laterality also will affect documentation, but this concept is limited to a few codes that might be reported by ObGyns. A designation of the right versus left organ will be required for reported cases of primary, secondary, borderline, or benign tumors of the breast, ovary, fallopian tube, broad ligament, and round ligament, as well as cancer in situ of the breast. However, the terms “bilateral” and “unilateral” are applied only to codes that describe hernias, acquired absence of the ovaries, and injuries to the ovaries and fallopian tubes that are not due to a surgical complication.
Unspecified codes still play a role
Unspecified ICD-10-CM codes still come into play when the clinician does not have enough information to assign a more specific code—that is, when, by the end of an encounter, no further information is available to assign a more specific diagnosis. For example, if a patient has signs of a fibroid upon examination, only the unspecified code can be reported until the clinician can discover whether it is intramural, submucosal, or subserosal. However, it would be equally incorrect to assign an unspecified code to an encounter once the nature of the fibroid has been determined.
Take note of these differences in coding
Here is a list of important new gynecologic coding requirements, which are presented in alphabetical order.
Amenorrhea, oligomenorrhea (N91.0–N91.5) and dysmenorrhea (N94.4–N94.5) will require documentation to indicate whether the condition is primary or secondary. Although an unspecified code is available, once treatment is begun the cause should be known and documented.
Artificial insemination problems will have a section:
- N98.0 Infection associated with artificial insemination
- N98.1 Hyperstimulation of ovaries
- N98.2 Complications of attempted introduction of fertilized ovum following in vitro fertilization
- N98.3 Complications of attempted introduction of embryo in embryo transfer
- N98.8 Other complications associated with artificial fertilization
- N98.9 Complication associated with artificial fertilization, unspecified.
Breast cancer codes will require documentation of which breast and what part of the breast is affected.
Contraceptive management highlights:
- Injectable contraceptives will have new codes for the initial prescription (Z30.013) and subsequent surveillance (Z30.42)
- IUD encounter for the prescription will have a new code (Z30.014), which is reported when the IUD is not being inserted on the same day
- Subdermal contraceptive implant surveillance will no longer have a specific code but will be included in the “other” contraceptive code Z30.49.
Conversion of a laparoscopic procedure to an open procedure will not have a code.
Cystocele, unspecified, will have code N81.10.
Dysplasia of vagina will be expanded into 3 codes based on mild, moderate, or unspecified: N89.0–N89.3.
Female genitourinary cancer codes:
- Documentation of right or left organs and which part of the uterus is affected will be required
- Cancer in situ of cervix will be expanded by site on the cervix: D06.0–D06.7
- Cancer in situ of the endometrium will have a specific code: D07.0.
Genuine stress urinary incontinence will only be referred to as stress incontinence (male or female). The code is now located in the urinary section of Chapter N: N39.3.
Genitourinary complications due to procedures and surgery will be organized in 1 section: N99
- Some conditions have more than 1 code based on cause:
- N99.2 Stricture of vagina due to surgical complication
- N89.5 Stricture of vagina not due to surgical complication
- N99.4 Pelvic adhesions due to surgical complication
- N73.6 Pelvic adhesions not due to surgical complication - Other codes will differentiate between intraoperative or postprocedure complications and whether the surgery is on the genitourinary system or a different surgery:
- N99.61 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating a genitourinary system procedure
- N99.62 Intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating other procedure
- N99.820 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following a genitourinary system procedure
- N99.821 Postprocedural hemorrhage and hematoma of a genitourinary system organ or structure following other procedure.
Gynecologic examinations will have to include information on whether or not there were genitourinary abnormal findings on the exam. If so, an additional secondary code will be required to identify the abnormality: Z01.411 and finding code. (Without abnormal findings: Z01.419.) For instance, a diagnosis of bacterial vaginosis is made during the examination. The abnormal findings are not those from other areas such as the breast or thyroid.
Hematuria documentation must differentiate between gross: R31.0, benign essential:R31.1, or other forms: R31.2.
High-risk sexual behavior problems must be documented by heterosexual, bisexual, or homosexual behavior: Z72.51–Z72.53.
Hormonal contraceptives, long-term use, will have a specific code: Z79.3.
Hyperplasia without atypia (simple, complex, or benign) will be rolled into a single code: N85.01.
Immunizations, prophylactic, will not have specific codes as to type. An encounter for any type of immunization is Z23.
Pelvic pain will have its own symptom code: R10.2.
Personal history for cancer has been expanded:
- Personal history of cancer in situ:
- Z86.000 of breast
- Z86.001 of cervix uteri
- Z86.008 of other site - Personal history of benign neoplasm:
- Z86.012 of other benign neoplasm
- Z86.03 of uncertain behavior (borderline malignancies).
Procedures not carried out will be expanded in ICD-10 to include 2 new codes:
- Z53.01 Procedure contraindicated due to patient smoking
- Z53.21 Procedure not carried out because patient left before seeing physician.
Procreative management changes:
- Artificial insemination will not have a specific code
- New code for male factor infertility: Z31.81
- New code for Rh incompatibility: Z31.82. This code would be used when the patient presents for prophylactic rho(D) immune globulin in addition to the Z23 code for immunization. This code also would be reported for the patient being tested for isoimmunization with no test result at the time of the visit.
Uterine prolapse without vaginal wall prolapse (618.1) will not have a code replacement.
Vaginal conditions such as vaginal lacerations (old), leukorrhea not specified as infective, and vaginal hematoma will be represented by an “other” code: N89.8.
Vulvar cyst will have its own code: N90.7.
Vulvovaginitis has been expanded into category codes for acute, subacute/chronic conditions of both the vagina and the vulva, which changes the documentation requirements in order to code correctly: N76.0–N76.3.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
1. Witt M. Moving forward with ICD-10: capitalize on this extra time. OBG Manag. 2014;26(7):17, 18, 20.
Reference
1. Witt M. Moving forward with ICD-10: capitalize on this extra time. OBG Manag. 2014;26(7):17, 18, 20.
ObGyn Medicare and CPT coding changes that could affect your income in 2015
At least one, if not many, of the coding changes highlighted below is likely to modify the incomes of ObGyns in the upcoming year. Here, I outline the 2015 changes that are most likely to affect your practice to some degree.
Medicare changes kick off a melancholy 2015
Surgical global periods: A move to eliminate them is underway
I begin this article not with a new or revised code, but with an active proposal, which, if implemented, could adversely affect your surgical income in a few short years.
Starting in 2017, the Centers for Medicare and Medicaid Services (CMS) has indicated that it will change all surgical codes to 0-day global periods. They plan on starting by converting 10-day global codes to 0-day codes in 2017, and then move on to the conversion of 90-day global codes in 2018. This is being proposed because of an Office of Inspector General (OIG) finding that many surgeons are not providing the evaluation and management (E/M) services included in the surgical code; therefore, Medicare is reimbursing for surgical procedures at a higher rate than warranted. In addition, the number of assigned visits may no longer reflect current care protocols, which again may mean that Medicare is not paying appropriately.
The immediate effect of this proposal—which has been adopted in the final rule published in the November 13, 2014, Federal Register—would be a reduction in payment for the converted codes due to a decrease in the assigned relative value units (RVUs). In addition, surgeons would need to document and provide the level of service for all preoperative and postoperative care, which may lead some payers to begin scrutinizing both levels of service billed and frequency of visits before and after surgical procedures.
CMS is still looking for any additional comments from physicians on this conversion process and such comments can be submitted electronically through a link at www.regulations.gov. Reference the final rule as CMS-1612-FC in your reply.
Medicare reimbursements poised to decrease in April
The calendar year 2015 conversion factor will remain at $35.80 from January 1 through March 31, 2015, as mandated by section 101 of the Protecting Access to Medicare Act of 2014. This represents the amount that will be multiplied by the geographically adjusted RVU for a code to determine the final Medicare allowable per procedure or service billed. Effective April 1, 2015, the conversion factor based on the sustainable growth rate (SGR) formula will be only $28.22—representing a 21.2% decrease—unless Congress acts to override this mandate.
Code bundling leads to lost Medicare compensation
Hysterectomy bundling. Effective October 1, 2014, CMS began permanently bundling anterior/posterior colporrhaphy and colpopexy procedures into all vaginal and laparoscopic-assisted hysterectomy codes. By permanently, CMS means that no modifier can be used to report Current Procedural Terminology (CPT) code 57260 (anterior and posterior [A&P] repair) or codes 57280, 57282, 57283 (abdominal, and vaginal approach colpopexy procedures) separately when performed with a vaginal or laparoscopic-assisted hysterectomy.
The American Congress of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) wrote to CMS in May with regard to these edits and objected to them strongly. These organizations will continue to work with CMS to get them removed. Until then, physicians who perform anterior/posterior colporrhaphy and colpopexy procedures with a vaginal or laparoscopic-assisted hysterectomy will need to clearly make a case in the operative report for the need to perform the additional procedures in order to add a modifier -22 (Increased procedural services) to the hysterectomy code for consideration of additional payment. If an A&P repair is performed, it would not be appropriate to bill only an anterior repair (CPT code 57240) or a posterior repair (CPT code 57250) to obtain some separate reimbursement as this would represent inaccurate coding.
Hysteroscopy bundling. Another edit that will affect ObGyns is the bundling of CPT code 58558 (Hysteroscopy, surgical; with sampling [biopsy] of endometrium and/or poly-pectomy, with or without D&C) into codes for hysteroscopic removal of a fibroid (58561) and the removal of an impacted foreign body (58562).
Previously, these codes could have been billed together, but now only the addition of a modifier -22 to the primary procedure (myomectomy or foreign body removal) presents any chance for additional reimbursement. In order to report the modifier, Medicare has indicated that the documentation must clearly support the additional work in accomplishing the primary procedure, including a statement of how much time it added to the normal procedure.
Awareness of new or revised CPT codes could benefit your earnings
The 2015 CPT code set includes several changes, including laboratory and vaccination codes, which may be of interest to your practice. Because of Health Insurance Portability and Accountability Act (HIPAA) requirements, insurers were required to accept new codes on January 1, 2015.
Added: Fetal chromosomal aneuploidy code for genomic sequencing
On January 1, 2014, CPT added a new code to report cell-free DNA to screen for fetal aneuploidy. This new code is 81507 (Fetal aneuploidy [trisomy 21, 18, and 13] DNA sequence analysis of selected regions using maternal plasma, algorithm reported as a risk score for each trisomy), and it was added to report the Harmony™ Prenatal Test.
For 2015, another new code, 81420 (Fetal chromosomal aneuploidy [eg, trisomy 21, monosomy X] genomic sequence analysis panel, circulating cell-free fetal DNA in maternal blood, must include analysis of chromosomes 13, 18, and 21), was added. This code represents a more comprehensive analysis and would therefore not be reported or ordered with code 81507. This new code requires a genomic sequence analysis panel.
HPV revisions extend beyond new codes
The codes for HPV testing have been redefined. These codes have been deleted: 87620-87622 (Infectious agent detection by nucleic acid [DNA or RNA]; papillomavirus, human, direct probe technique/amplified probe technique/quantification). In their place are three new codes to choose from:
- 87623, Human papillomavirus (HPV), low-risk types (eg, 6, 11, 42, 43, 44)
- 87624, Human papillomavirus (HPV), high-risk types (eg, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68)
- 87625, Human papillomavirus (HPV), types 16 and 18 only, includes type 45, if performed.
This coding change may be significant for payment as some payers will cover testing for high-risk HPV types only, so be sure your practice management team is aware of the latest rules for ordering HPV testing for your patients. Otherwise, patients could be faced with unexpected out-of-pocket expenses.
Egg freezing recognized as mainstream
- Infertility laboratories will be pleased to learn that CPT has changed the status of the code for cryopreservation of oocytes from a Category III to a Category I code. This means that this technology has now proven itself as a mainstream procedure, warranting a Category I CPT code. The new code is 89337 (Cryopreservation, mature oocyte[s]), which replaces the deleted code 0059T (Cryopreservation; oocyte[s]).
Vaccination codes for 2015
Almost every year new codes are added, and 2015 is no different. This year, you will see codes for:
- 90651, Human papillomavirus vaccine types 6, 11, 16, 18, 31, 33, 45, 52, 58, nonavalent (HPV), 3 dose schedule, for intramuscular use
- 90630, Influenza virus vaccine, quadrivalent (IIV4), split virus, preservative free, for intradermal use.
There is also a revision to the flu virus vaccine code 90654 to indicate that it represents a trivalent preservative-free vaccine. See the TABLE below for a complete list of all the vaccines by trade name and CPT/Medicare Healthcare Common Procedure Coding System (HCPCS) codes for the 2014−2015 flu season.
Keep in mind that reporting administration of the flu vaccine is different for Medicare than for private payers. Administration code G0008 and diagnosis code V04.81 (Need for prophylactic vaccination and inoculation against influenza) would be reported in conjunction with the appropriate vaccine code for Medicare, while CPT instructs you to report 90471 instead for the administration. When we switch to ICD-10 diagnostic coding on October 1, 2015, the code V04.81 becomes Z23 (Encounter for immunization).
Three new codes for anoscopy
The first two codes were formerly Category III codes representing new technology, but now have proven to be more mainstream.
- 46601, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, including collection of specimen(s) by brushing or washing, when performed
- 46607, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, with biopsy, single or multiple
- 0377T, Anoscopy with directed submucosal injection of bulking agent for fecal incontinence.
Replacement codes for vertebral fracture assessments
If your practice is performing or ordering vertebral assessments for patients, there are two new codes to report. The old code, 77082 (Dual-energy X-ray absorptiometry [DXA], bone density study, 1 or more sites; vertebral fracture assessment) for vertebral fracture assessment has been deleted and replaced with:
- 77085, Dual-energy X-ray absorptiometry (DXA), bone density study, 1 or more sites; axial skeleton (eg, hips, pelvis, spine), including vertebral fracture assessment
- 77086, Vertebral fracture assessment via dual-energy X-ray absorptiometry (DXA).
Coding for breast ultrasound and tomosynthesis get more descriptive—at least for private insurance
The CPT Editorial Panel created three codes to describe digital breast tomosynthesis services and two new codes for a breast ultrasound.
- 77061, Digital breast tomosynthesis; unilateral
- 77062, Digital breast tomosynthesis; bilateral
- 77063, Screening digital breast tomosynthesis, bilateral (List separately in addition to the code for the primary procedure.)
- 76641, Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete
- 76642, Ultrasound, breast, unilateral, … ; limited.
Medicare, on the other hand, has decided to create a G code for tomosynthesis, which is the only code that will be accepted for payment if the patient meets her high-risk criteria for performance of this test.
Under Medicare rules you would report/order the following codes for mammographic services:
- Film (use CPT codes)
- 77056, Mammography; bilateral
- 77057, Screening mammography, bilateral (2-view film study of each breast)
- 2D digital (use G0202, G0204, and G0206)
- G0204, Diagnostic mammography, producing direct digital image, bilateral, all views
- G0206, Diagnostic mammography, producing direct digital image, unilateral, all views
- 3D screening (use G0202 for 2D digital plus the new CPT code 77063 for 3D)
procedure.)
- 3D diagnostic (use G0204 or G0206 for the 2D digital plus the new G code G0279 for 3D)
Modifier 59 becomes more specific
Another Medicare coding change that may affect ObGyns is the addition of new Medicare modifiers that are intended to eventually replace the modifier -59. This new list of modifiers will need to be appended to bundled procedures to more clearly explain why the secondary procedures should be paid separately. At the most recent American Medical Association (AMA) CPT symposium in Chicago, Illinois, CMS medical directors indicated that the new modifiers should be used only when the clinician is given instructions to do so by the carrier. Until then, the modifier -59 should continue to be used by most clinicians.
Here are the new modifiers, with an example of their use with currently bundled procedures that allow a modifier -59 to be used under certain circumstances:
- -XE: Separate encounter (A service that is distinct because it occurred during a separate encounter.) For instance, a patient presents to the office in the morning to have an abscess on her labia near her urethra incised and drained (56405). She returns in the afternoon to have a temporary catheter inserted because she states she cannot urinate and you decide to put in a temporary Foley catheter (51702) until the swelling has gone down. Add the modifier XE to 51702 to indicate it was performed at a different patient encounter.
- -XP: Separate practitioner (A service that is distinct because it was performed by a different practitioner.) Normally, Medicare will reimburse an unaffiliated clinician for performing a procedure that is bundled, since the bundling edits apply to the billing surgeon. But when two physicians from the same practice each are performing a different procedure at the same operative session that would otherwise be bundled, this new modifier will make that clear.
For example, Dr. Bates is performing a laparoscopic paravaginal defect repair (57423) and calls Dr. Clark, a urogynecologist in his practice, to remove severe adhesions from the ureters. The claim should go in under the same tax ID number, with the code 50715 listed first (as it has greater RVUs) and code 57423 reported with the -XP modifier.
- -XS: Separate structure (A service that is distinct because it was performed on a separate organ/structure.) Dr. Scott is performing the removal of endometrial implants around the left fallopian tube and in the cul-de-sac and notices that the right fallopian tube appears closed. He performs chromotubation on the right fallopian tube and notes that the right tube is blocked. Billing in this case would be 58662, 58350-XS.
- -XU: Unusual non-overlapping service (The use of a service that is distinct because it does not overlap usual components of the main service.) Mary has Medicare coverage and presents at 20 weeks 4 days gestation with bleeding and labor pains. Her examination shows bulging membranes that rupture when you attempt to remove the cerclage suture. You note a large rent in the cervix, but cannot get to the cerclage sutures as the patient is in active labor and beginning to bear down. The fetus and placenta are delivered a short time later through the rent in the cervix. You repair the rent in the cervix following delivery.
In this case, code 59400-52 (reduced services since the patient delivered at 20 weeks and there were reduced antepartum services), and 57720-XU because the repair of the cervix is not part of the usual services for a vaginal delivery.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
At least one, if not many, of the coding changes highlighted below is likely to modify the incomes of ObGyns in the upcoming year. Here, I outline the 2015 changes that are most likely to affect your practice to some degree.
Medicare changes kick off a melancholy 2015
Surgical global periods: A move to eliminate them is underway
I begin this article not with a new or revised code, but with an active proposal, which, if implemented, could adversely affect your surgical income in a few short years.
Starting in 2017, the Centers for Medicare and Medicaid Services (CMS) has indicated that it will change all surgical codes to 0-day global periods. They plan on starting by converting 10-day global codes to 0-day codes in 2017, and then move on to the conversion of 90-day global codes in 2018. This is being proposed because of an Office of Inspector General (OIG) finding that many surgeons are not providing the evaluation and management (E/M) services included in the surgical code; therefore, Medicare is reimbursing for surgical procedures at a higher rate than warranted. In addition, the number of assigned visits may no longer reflect current care protocols, which again may mean that Medicare is not paying appropriately.
The immediate effect of this proposal—which has been adopted in the final rule published in the November 13, 2014, Federal Register—would be a reduction in payment for the converted codes due to a decrease in the assigned relative value units (RVUs). In addition, surgeons would need to document and provide the level of service for all preoperative and postoperative care, which may lead some payers to begin scrutinizing both levels of service billed and frequency of visits before and after surgical procedures.
CMS is still looking for any additional comments from physicians on this conversion process and such comments can be submitted electronically through a link at www.regulations.gov. Reference the final rule as CMS-1612-FC in your reply.
Medicare reimbursements poised to decrease in April
The calendar year 2015 conversion factor will remain at $35.80 from January 1 through March 31, 2015, as mandated by section 101 of the Protecting Access to Medicare Act of 2014. This represents the amount that will be multiplied by the geographically adjusted RVU for a code to determine the final Medicare allowable per procedure or service billed. Effective April 1, 2015, the conversion factor based on the sustainable growth rate (SGR) formula will be only $28.22—representing a 21.2% decrease—unless Congress acts to override this mandate.
Code bundling leads to lost Medicare compensation
Hysterectomy bundling. Effective October 1, 2014, CMS began permanently bundling anterior/posterior colporrhaphy and colpopexy procedures into all vaginal and laparoscopic-assisted hysterectomy codes. By permanently, CMS means that no modifier can be used to report Current Procedural Terminology (CPT) code 57260 (anterior and posterior [A&P] repair) or codes 57280, 57282, 57283 (abdominal, and vaginal approach colpopexy procedures) separately when performed with a vaginal or laparoscopic-assisted hysterectomy.
The American Congress of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) wrote to CMS in May with regard to these edits and objected to them strongly. These organizations will continue to work with CMS to get them removed. Until then, physicians who perform anterior/posterior colporrhaphy and colpopexy procedures with a vaginal or laparoscopic-assisted hysterectomy will need to clearly make a case in the operative report for the need to perform the additional procedures in order to add a modifier -22 (Increased procedural services) to the hysterectomy code for consideration of additional payment. If an A&P repair is performed, it would not be appropriate to bill only an anterior repair (CPT code 57240) or a posterior repair (CPT code 57250) to obtain some separate reimbursement as this would represent inaccurate coding.
Hysteroscopy bundling. Another edit that will affect ObGyns is the bundling of CPT code 58558 (Hysteroscopy, surgical; with sampling [biopsy] of endometrium and/or poly-pectomy, with or without D&C) into codes for hysteroscopic removal of a fibroid (58561) and the removal of an impacted foreign body (58562).
Previously, these codes could have been billed together, but now only the addition of a modifier -22 to the primary procedure (myomectomy or foreign body removal) presents any chance for additional reimbursement. In order to report the modifier, Medicare has indicated that the documentation must clearly support the additional work in accomplishing the primary procedure, including a statement of how much time it added to the normal procedure.
Awareness of new or revised CPT codes could benefit your earnings
The 2015 CPT code set includes several changes, including laboratory and vaccination codes, which may be of interest to your practice. Because of Health Insurance Portability and Accountability Act (HIPAA) requirements, insurers were required to accept new codes on January 1, 2015.
Added: Fetal chromosomal aneuploidy code for genomic sequencing
On January 1, 2014, CPT added a new code to report cell-free DNA to screen for fetal aneuploidy. This new code is 81507 (Fetal aneuploidy [trisomy 21, 18, and 13] DNA sequence analysis of selected regions using maternal plasma, algorithm reported as a risk score for each trisomy), and it was added to report the Harmony™ Prenatal Test.
For 2015, another new code, 81420 (Fetal chromosomal aneuploidy [eg, trisomy 21, monosomy X] genomic sequence analysis panel, circulating cell-free fetal DNA in maternal blood, must include analysis of chromosomes 13, 18, and 21), was added. This code represents a more comprehensive analysis and would therefore not be reported or ordered with code 81507. This new code requires a genomic sequence analysis panel.
HPV revisions extend beyond new codes
The codes for HPV testing have been redefined. These codes have been deleted: 87620-87622 (Infectious agent detection by nucleic acid [DNA or RNA]; papillomavirus, human, direct probe technique/amplified probe technique/quantification). In their place are three new codes to choose from:
- 87623, Human papillomavirus (HPV), low-risk types (eg, 6, 11, 42, 43, 44)
- 87624, Human papillomavirus (HPV), high-risk types (eg, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68)
- 87625, Human papillomavirus (HPV), types 16 and 18 only, includes type 45, if performed.
This coding change may be significant for payment as some payers will cover testing for high-risk HPV types only, so be sure your practice management team is aware of the latest rules for ordering HPV testing for your patients. Otherwise, patients could be faced with unexpected out-of-pocket expenses.
Egg freezing recognized as mainstream
- Infertility laboratories will be pleased to learn that CPT has changed the status of the code for cryopreservation of oocytes from a Category III to a Category I code. This means that this technology has now proven itself as a mainstream procedure, warranting a Category I CPT code. The new code is 89337 (Cryopreservation, mature oocyte[s]), which replaces the deleted code 0059T (Cryopreservation; oocyte[s]).
Vaccination codes for 2015
Almost every year new codes are added, and 2015 is no different. This year, you will see codes for:
- 90651, Human papillomavirus vaccine types 6, 11, 16, 18, 31, 33, 45, 52, 58, nonavalent (HPV), 3 dose schedule, for intramuscular use
- 90630, Influenza virus vaccine, quadrivalent (IIV4), split virus, preservative free, for intradermal use.
There is also a revision to the flu virus vaccine code 90654 to indicate that it represents a trivalent preservative-free vaccine. See the TABLE below for a complete list of all the vaccines by trade name and CPT/Medicare Healthcare Common Procedure Coding System (HCPCS) codes for the 2014−2015 flu season.
Keep in mind that reporting administration of the flu vaccine is different for Medicare than for private payers. Administration code G0008 and diagnosis code V04.81 (Need for prophylactic vaccination and inoculation against influenza) would be reported in conjunction with the appropriate vaccine code for Medicare, while CPT instructs you to report 90471 instead for the administration. When we switch to ICD-10 diagnostic coding on October 1, 2015, the code V04.81 becomes Z23 (Encounter for immunization).
Three new codes for anoscopy
The first two codes were formerly Category III codes representing new technology, but now have proven to be more mainstream.
- 46601, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, including collection of specimen(s) by brushing or washing, when performed
- 46607, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, with biopsy, single or multiple
- 0377T, Anoscopy with directed submucosal injection of bulking agent for fecal incontinence.
Replacement codes for vertebral fracture assessments
If your practice is performing or ordering vertebral assessments for patients, there are two new codes to report. The old code, 77082 (Dual-energy X-ray absorptiometry [DXA], bone density study, 1 or more sites; vertebral fracture assessment) for vertebral fracture assessment has been deleted and replaced with:
- 77085, Dual-energy X-ray absorptiometry (DXA), bone density study, 1 or more sites; axial skeleton (eg, hips, pelvis, spine), including vertebral fracture assessment
- 77086, Vertebral fracture assessment via dual-energy X-ray absorptiometry (DXA).
Coding for breast ultrasound and tomosynthesis get more descriptive—at least for private insurance
The CPT Editorial Panel created three codes to describe digital breast tomosynthesis services and two new codes for a breast ultrasound.
- 77061, Digital breast tomosynthesis; unilateral
- 77062, Digital breast tomosynthesis; bilateral
- 77063, Screening digital breast tomosynthesis, bilateral (List separately in addition to the code for the primary procedure.)
- 76641, Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete
- 76642, Ultrasound, breast, unilateral, … ; limited.
Medicare, on the other hand, has decided to create a G code for tomosynthesis, which is the only code that will be accepted for payment if the patient meets her high-risk criteria for performance of this test.
Under Medicare rules you would report/order the following codes for mammographic services:
- Film (use CPT codes)
- 77056, Mammography; bilateral
- 77057, Screening mammography, bilateral (2-view film study of each breast)
- 2D digital (use G0202, G0204, and G0206)
- G0204, Diagnostic mammography, producing direct digital image, bilateral, all views
- G0206, Diagnostic mammography, producing direct digital image, unilateral, all views
- 3D screening (use G0202 for 2D digital plus the new CPT code 77063 for 3D)
procedure.)
- 3D diagnostic (use G0204 or G0206 for the 2D digital plus the new G code G0279 for 3D)
Modifier 59 becomes more specific
Another Medicare coding change that may affect ObGyns is the addition of new Medicare modifiers that are intended to eventually replace the modifier -59. This new list of modifiers will need to be appended to bundled procedures to more clearly explain why the secondary procedures should be paid separately. At the most recent American Medical Association (AMA) CPT symposium in Chicago, Illinois, CMS medical directors indicated that the new modifiers should be used only when the clinician is given instructions to do so by the carrier. Until then, the modifier -59 should continue to be used by most clinicians.
Here are the new modifiers, with an example of their use with currently bundled procedures that allow a modifier -59 to be used under certain circumstances:
- -XE: Separate encounter (A service that is distinct because it occurred during a separate encounter.) For instance, a patient presents to the office in the morning to have an abscess on her labia near her urethra incised and drained (56405). She returns in the afternoon to have a temporary catheter inserted because she states she cannot urinate and you decide to put in a temporary Foley catheter (51702) until the swelling has gone down. Add the modifier XE to 51702 to indicate it was performed at a different patient encounter.
- -XP: Separate practitioner (A service that is distinct because it was performed by a different practitioner.) Normally, Medicare will reimburse an unaffiliated clinician for performing a procedure that is bundled, since the bundling edits apply to the billing surgeon. But when two physicians from the same practice each are performing a different procedure at the same operative session that would otherwise be bundled, this new modifier will make that clear.
For example, Dr. Bates is performing a laparoscopic paravaginal defect repair (57423) and calls Dr. Clark, a urogynecologist in his practice, to remove severe adhesions from the ureters. The claim should go in under the same tax ID number, with the code 50715 listed first (as it has greater RVUs) and code 57423 reported with the -XP modifier.
- -XS: Separate structure (A service that is distinct because it was performed on a separate organ/structure.) Dr. Scott is performing the removal of endometrial implants around the left fallopian tube and in the cul-de-sac and notices that the right fallopian tube appears closed. He performs chromotubation on the right fallopian tube and notes that the right tube is blocked. Billing in this case would be 58662, 58350-XS.
- -XU: Unusual non-overlapping service (The use of a service that is distinct because it does not overlap usual components of the main service.) Mary has Medicare coverage and presents at 20 weeks 4 days gestation with bleeding and labor pains. Her examination shows bulging membranes that rupture when you attempt to remove the cerclage suture. You note a large rent in the cervix, but cannot get to the cerclage sutures as the patient is in active labor and beginning to bear down. The fetus and placenta are delivered a short time later through the rent in the cervix. You repair the rent in the cervix following delivery.
In this case, code 59400-52 (reduced services since the patient delivered at 20 weeks and there were reduced antepartum services), and 57720-XU because the repair of the cervix is not part of the usual services for a vaginal delivery.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
At least one, if not many, of the coding changes highlighted below is likely to modify the incomes of ObGyns in the upcoming year. Here, I outline the 2015 changes that are most likely to affect your practice to some degree.
Medicare changes kick off a melancholy 2015
Surgical global periods: A move to eliminate them is underway
I begin this article not with a new or revised code, but with an active proposal, which, if implemented, could adversely affect your surgical income in a few short years.
Starting in 2017, the Centers for Medicare and Medicaid Services (CMS) has indicated that it will change all surgical codes to 0-day global periods. They plan on starting by converting 10-day global codes to 0-day codes in 2017, and then move on to the conversion of 90-day global codes in 2018. This is being proposed because of an Office of Inspector General (OIG) finding that many surgeons are not providing the evaluation and management (E/M) services included in the surgical code; therefore, Medicare is reimbursing for surgical procedures at a higher rate than warranted. In addition, the number of assigned visits may no longer reflect current care protocols, which again may mean that Medicare is not paying appropriately.
The immediate effect of this proposal—which has been adopted in the final rule published in the November 13, 2014, Federal Register—would be a reduction in payment for the converted codes due to a decrease in the assigned relative value units (RVUs). In addition, surgeons would need to document and provide the level of service for all preoperative and postoperative care, which may lead some payers to begin scrutinizing both levels of service billed and frequency of visits before and after surgical procedures.
CMS is still looking for any additional comments from physicians on this conversion process and such comments can be submitted electronically through a link at www.regulations.gov. Reference the final rule as CMS-1612-FC in your reply.
Medicare reimbursements poised to decrease in April
The calendar year 2015 conversion factor will remain at $35.80 from January 1 through March 31, 2015, as mandated by section 101 of the Protecting Access to Medicare Act of 2014. This represents the amount that will be multiplied by the geographically adjusted RVU for a code to determine the final Medicare allowable per procedure or service billed. Effective April 1, 2015, the conversion factor based on the sustainable growth rate (SGR) formula will be only $28.22—representing a 21.2% decrease—unless Congress acts to override this mandate.
Code bundling leads to lost Medicare compensation
Hysterectomy bundling. Effective October 1, 2014, CMS began permanently bundling anterior/posterior colporrhaphy and colpopexy procedures into all vaginal and laparoscopic-assisted hysterectomy codes. By permanently, CMS means that no modifier can be used to report Current Procedural Terminology (CPT) code 57260 (anterior and posterior [A&P] repair) or codes 57280, 57282, 57283 (abdominal, and vaginal approach colpopexy procedures) separately when performed with a vaginal or laparoscopic-assisted hysterectomy.
The American Congress of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) wrote to CMS in May with regard to these edits and objected to them strongly. These organizations will continue to work with CMS to get them removed. Until then, physicians who perform anterior/posterior colporrhaphy and colpopexy procedures with a vaginal or laparoscopic-assisted hysterectomy will need to clearly make a case in the operative report for the need to perform the additional procedures in order to add a modifier -22 (Increased procedural services) to the hysterectomy code for consideration of additional payment. If an A&P repair is performed, it would not be appropriate to bill only an anterior repair (CPT code 57240) or a posterior repair (CPT code 57250) to obtain some separate reimbursement as this would represent inaccurate coding.
Hysteroscopy bundling. Another edit that will affect ObGyns is the bundling of CPT code 58558 (Hysteroscopy, surgical; with sampling [biopsy] of endometrium and/or poly-pectomy, with or without D&C) into codes for hysteroscopic removal of a fibroid (58561) and the removal of an impacted foreign body (58562).
Previously, these codes could have been billed together, but now only the addition of a modifier -22 to the primary procedure (myomectomy or foreign body removal) presents any chance for additional reimbursement. In order to report the modifier, Medicare has indicated that the documentation must clearly support the additional work in accomplishing the primary procedure, including a statement of how much time it added to the normal procedure.
Awareness of new or revised CPT codes could benefit your earnings
The 2015 CPT code set includes several changes, including laboratory and vaccination codes, which may be of interest to your practice. Because of Health Insurance Portability and Accountability Act (HIPAA) requirements, insurers were required to accept new codes on January 1, 2015.
Added: Fetal chromosomal aneuploidy code for genomic sequencing
On January 1, 2014, CPT added a new code to report cell-free DNA to screen for fetal aneuploidy. This new code is 81507 (Fetal aneuploidy [trisomy 21, 18, and 13] DNA sequence analysis of selected regions using maternal plasma, algorithm reported as a risk score for each trisomy), and it was added to report the Harmony™ Prenatal Test.
For 2015, another new code, 81420 (Fetal chromosomal aneuploidy [eg, trisomy 21, monosomy X] genomic sequence analysis panel, circulating cell-free fetal DNA in maternal blood, must include analysis of chromosomes 13, 18, and 21), was added. This code represents a more comprehensive analysis and would therefore not be reported or ordered with code 81507. This new code requires a genomic sequence analysis panel.
HPV revisions extend beyond new codes
The codes for HPV testing have been redefined. These codes have been deleted: 87620-87622 (Infectious agent detection by nucleic acid [DNA or RNA]; papillomavirus, human, direct probe technique/amplified probe technique/quantification). In their place are three new codes to choose from:
- 87623, Human papillomavirus (HPV), low-risk types (eg, 6, 11, 42, 43, 44)
- 87624, Human papillomavirus (HPV), high-risk types (eg, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68)
- 87625, Human papillomavirus (HPV), types 16 and 18 only, includes type 45, if performed.
This coding change may be significant for payment as some payers will cover testing for high-risk HPV types only, so be sure your practice management team is aware of the latest rules for ordering HPV testing for your patients. Otherwise, patients could be faced with unexpected out-of-pocket expenses.
Egg freezing recognized as mainstream
- Infertility laboratories will be pleased to learn that CPT has changed the status of the code for cryopreservation of oocytes from a Category III to a Category I code. This means that this technology has now proven itself as a mainstream procedure, warranting a Category I CPT code. The new code is 89337 (Cryopreservation, mature oocyte[s]), which replaces the deleted code 0059T (Cryopreservation; oocyte[s]).
Vaccination codes for 2015
Almost every year new codes are added, and 2015 is no different. This year, you will see codes for:
- 90651, Human papillomavirus vaccine types 6, 11, 16, 18, 31, 33, 45, 52, 58, nonavalent (HPV), 3 dose schedule, for intramuscular use
- 90630, Influenza virus vaccine, quadrivalent (IIV4), split virus, preservative free, for intradermal use.
There is also a revision to the flu virus vaccine code 90654 to indicate that it represents a trivalent preservative-free vaccine. See the TABLE below for a complete list of all the vaccines by trade name and CPT/Medicare Healthcare Common Procedure Coding System (HCPCS) codes for the 2014−2015 flu season.
Keep in mind that reporting administration of the flu vaccine is different for Medicare than for private payers. Administration code G0008 and diagnosis code V04.81 (Need for prophylactic vaccination and inoculation against influenza) would be reported in conjunction with the appropriate vaccine code for Medicare, while CPT instructs you to report 90471 instead for the administration. When we switch to ICD-10 diagnostic coding on October 1, 2015, the code V04.81 becomes Z23 (Encounter for immunization).
Three new codes for anoscopy
The first two codes were formerly Category III codes representing new technology, but now have proven to be more mainstream.
- 46601, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, including collection of specimen(s) by brushing or washing, when performed
- 46607, Anoscopy; diagnostic, with high-resolution magnification (HRA) (eg, colposcope, operating microscope) and chemical agent enhancement, with biopsy, single or multiple
- 0377T, Anoscopy with directed submucosal injection of bulking agent for fecal incontinence.
Replacement codes for vertebral fracture assessments
If your practice is performing or ordering vertebral assessments for patients, there are two new codes to report. The old code, 77082 (Dual-energy X-ray absorptiometry [DXA], bone density study, 1 or more sites; vertebral fracture assessment) for vertebral fracture assessment has been deleted and replaced with:
- 77085, Dual-energy X-ray absorptiometry (DXA), bone density study, 1 or more sites; axial skeleton (eg, hips, pelvis, spine), including vertebral fracture assessment
- 77086, Vertebral fracture assessment via dual-energy X-ray absorptiometry (DXA).
Coding for breast ultrasound and tomosynthesis get more descriptive—at least for private insurance
The CPT Editorial Panel created three codes to describe digital breast tomosynthesis services and two new codes for a breast ultrasound.
- 77061, Digital breast tomosynthesis; unilateral
- 77062, Digital breast tomosynthesis; bilateral
- 77063, Screening digital breast tomosynthesis, bilateral (List separately in addition to the code for the primary procedure.)
- 76641, Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete
- 76642, Ultrasound, breast, unilateral, … ; limited.
Medicare, on the other hand, has decided to create a G code for tomosynthesis, which is the only code that will be accepted for payment if the patient meets her high-risk criteria for performance of this test.
Under Medicare rules you would report/order the following codes for mammographic services:
- Film (use CPT codes)
- 77056, Mammography; bilateral
- 77057, Screening mammography, bilateral (2-view film study of each breast)
- 2D digital (use G0202, G0204, and G0206)
- G0204, Diagnostic mammography, producing direct digital image, bilateral, all views
- G0206, Diagnostic mammography, producing direct digital image, unilateral, all views
- 3D screening (use G0202 for 2D digital plus the new CPT code 77063 for 3D)
procedure.)
- 3D diagnostic (use G0204 or G0206 for the 2D digital plus the new G code G0279 for 3D)
Modifier 59 becomes more specific
Another Medicare coding change that may affect ObGyns is the addition of new Medicare modifiers that are intended to eventually replace the modifier -59. This new list of modifiers will need to be appended to bundled procedures to more clearly explain why the secondary procedures should be paid separately. At the most recent American Medical Association (AMA) CPT symposium in Chicago, Illinois, CMS medical directors indicated that the new modifiers should be used only when the clinician is given instructions to do so by the carrier. Until then, the modifier -59 should continue to be used by most clinicians.
Here are the new modifiers, with an example of their use with currently bundled procedures that allow a modifier -59 to be used under certain circumstances:
- -XE: Separate encounter (A service that is distinct because it occurred during a separate encounter.) For instance, a patient presents to the office in the morning to have an abscess on her labia near her urethra incised and drained (56405). She returns in the afternoon to have a temporary catheter inserted because she states she cannot urinate and you decide to put in a temporary Foley catheter (51702) until the swelling has gone down. Add the modifier XE to 51702 to indicate it was performed at a different patient encounter.
- -XP: Separate practitioner (A service that is distinct because it was performed by a different practitioner.) Normally, Medicare will reimburse an unaffiliated clinician for performing a procedure that is bundled, since the bundling edits apply to the billing surgeon. But when two physicians from the same practice each are performing a different procedure at the same operative session that would otherwise be bundled, this new modifier will make that clear.
For example, Dr. Bates is performing a laparoscopic paravaginal defect repair (57423) and calls Dr. Clark, a urogynecologist in his practice, to remove severe adhesions from the ureters. The claim should go in under the same tax ID number, with the code 50715 listed first (as it has greater RVUs) and code 57423 reported with the -XP modifier.
- -XS: Separate structure (A service that is distinct because it was performed on a separate organ/structure.) Dr. Scott is performing the removal of endometrial implants around the left fallopian tube and in the cul-de-sac and notices that the right fallopian tube appears closed. He performs chromotubation on the right fallopian tube and notes that the right tube is blocked. Billing in this case would be 58662, 58350-XS.
- -XU: Unusual non-overlapping service (The use of a service that is distinct because it does not overlap usual components of the main service.) Mary has Medicare coverage and presents at 20 weeks 4 days gestation with bleeding and labor pains. Her examination shows bulging membranes that rupture when you attempt to remove the cerclage suture. You note a large rent in the cervix, but cannot get to the cerclage sutures as the patient is in active labor and beginning to bear down. The fetus and placenta are delivered a short time later through the rent in the cervix. You repair the rent in the cervix following delivery.
In this case, code 59400-52 (reduced services since the patient delivered at 20 weeks and there were reduced antepartum services), and 57720-XU because the repair of the cervix is not part of the usual services for a vaginal delivery.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.