User login
Immunotherapy may benefit relapsed HSCT recipients

Photo from Business Wire
Results of a phase 1 study suggest that repeated doses of the immunotherapy drug ipilimumab is a feasible treatment option for patients with hematologic diseases who relapse after allogeneic hematopoietic stem cell transplant (HSCT).
Seven of the 28 patients studied responded to the treatment, but immune-mediated toxic effects and graft-vs-host disease (GVHD) occurred as well.
These results were published in NEJM.
Ipilimumab, which is already approved to treat unresectable or metastatic melanoma, works by blocking the immune checkpoint CTLA-4. Blockade of CTLA-4 has been shown to augment T-cell activation and proliferation.
“We believe [,in the case of relapse after HSCT,] the donor immune cells are present but can’t recognize the tumor cells because of inhibitory signals that disguise them,” said study author Matthew Davids, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“By blocking the checkpoint, you allow the donor cells to see the cancer cells.”
Dr Davids and his colleagues tested this theory in 28 patients who had relapsed after allogeneic HSCT. The patients had acute myeloid leukemia (AML, n=12), Hodgkin lymphoma (n=7), non-Hodgkin lymphoma (n=4), myelodysplastic syndromes (MDS, n=2), multiple myeloma (n=1), myeloproliferative neoplasm (n=1), or acute lymphoblastic leukemia (n=1).
Patients had received a median of 3 prior treatment regimens, excluding HSCT (range, 1 to 14), and 20 patients (71%) had received treatment for relapse after transplant. Eight patients (29%) previously had grade 1/2 acute GVHD, and 16 (57%) previously had chronic GVHD.
The median time from transplant to initial treatment with ipilimumab was 675 days (range, 198 to 1830), and the median time from relapse to initial treatment with ipilimumab was 97 days (range, 0 to
1415).
Patients received induction therapy with ipilimumab at a dose of 3 mg/kg or 10 mg/kg every 3 weeks for a total of 4 doses. Those who had a clinical benefit received additional doses every 12 weeks for up to 60 weeks.
Safety
Five patients discontinued ipilimumab due to dose-limiting toxic effects. Four of these patients had GVHD, and 1 had severe immune-related adverse events.
Dose-limiting GVHD presented as chronic GVHD of the liver in 3 patients and acute GVHD of the gut in 1 patient.
Immune-related adverse events included death (n=1), pneumonitis (2 grade 2 events, 1 grade 4 event), colitis (1 grade 3 event), immune thrombocytopenia (1 grade 2 event), and diarrhea (1 grade 2 event).
Efficacy
There were no responses in patients who received ipilimumab at 3 mg/kg. Among the 22 patients who received ipilimumab at 10 mg/kg, 5 had a complete response, and 2 had a partial response.
Six other patients did not qualify as having responses but had a decrease in their tumor burden. Altogether, ipilimumab reduced tumor burden in 59% of patients.
The complete responses occurred in 4 patients with extramedullary AML and 1 patient with MDS developing into AML. Two of the AML patients remained in complete response at 12 and 15 months, and the patient with MDS remained in complete response at 16 months.
At a median follow-up of 15 months (range, 8 to 27), the median duration of response had not been reached. Responses were associated with in situ infiltration of cytotoxic CD8+ T cells, decreased activation of regulatory T cells, and expansion of subpopulations of effector T cells.
The 1-year overall survival rate was 49%.
The investigators said these encouraging results have set the stage for larger trials of checkpoint blockade in this patient population. Further research is planned to determine whether immunotherapy drugs could be given to high-risk patients to prevent relapse. ![]()

Photo from Business Wire
Results of a phase 1 study suggest that repeated doses of the immunotherapy drug ipilimumab is a feasible treatment option for patients with hematologic diseases who relapse after allogeneic hematopoietic stem cell transplant (HSCT).
Seven of the 28 patients studied responded to the treatment, but immune-mediated toxic effects and graft-vs-host disease (GVHD) occurred as well.
These results were published in NEJM.
Ipilimumab, which is already approved to treat unresectable or metastatic melanoma, works by blocking the immune checkpoint CTLA-4. Blockade of CTLA-4 has been shown to augment T-cell activation and proliferation.
“We believe [,in the case of relapse after HSCT,] the donor immune cells are present but can’t recognize the tumor cells because of inhibitory signals that disguise them,” said study author Matthew Davids, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“By blocking the checkpoint, you allow the donor cells to see the cancer cells.”
Dr Davids and his colleagues tested this theory in 28 patients who had relapsed after allogeneic HSCT. The patients had acute myeloid leukemia (AML, n=12), Hodgkin lymphoma (n=7), non-Hodgkin lymphoma (n=4), myelodysplastic syndromes (MDS, n=2), multiple myeloma (n=1), myeloproliferative neoplasm (n=1), or acute lymphoblastic leukemia (n=1).
Patients had received a median of 3 prior treatment regimens, excluding HSCT (range, 1 to 14), and 20 patients (71%) had received treatment for relapse after transplant. Eight patients (29%) previously had grade 1/2 acute GVHD, and 16 (57%) previously had chronic GVHD.
The median time from transplant to initial treatment with ipilimumab was 675 days (range, 198 to 1830), and the median time from relapse to initial treatment with ipilimumab was 97 days (range, 0 to
1415).
Patients received induction therapy with ipilimumab at a dose of 3 mg/kg or 10 mg/kg every 3 weeks for a total of 4 doses. Those who had a clinical benefit received additional doses every 12 weeks for up to 60 weeks.
Safety
Five patients discontinued ipilimumab due to dose-limiting toxic effects. Four of these patients had GVHD, and 1 had severe immune-related adverse events.
Dose-limiting GVHD presented as chronic GVHD of the liver in 3 patients and acute GVHD of the gut in 1 patient.
Immune-related adverse events included death (n=1), pneumonitis (2 grade 2 events, 1 grade 4 event), colitis (1 grade 3 event), immune thrombocytopenia (1 grade 2 event), and diarrhea (1 grade 2 event).
Efficacy
There were no responses in patients who received ipilimumab at 3 mg/kg. Among the 22 patients who received ipilimumab at 10 mg/kg, 5 had a complete response, and 2 had a partial response.
Six other patients did not qualify as having responses but had a decrease in their tumor burden. Altogether, ipilimumab reduced tumor burden in 59% of patients.
The complete responses occurred in 4 patients with extramedullary AML and 1 patient with MDS developing into AML. Two of the AML patients remained in complete response at 12 and 15 months, and the patient with MDS remained in complete response at 16 months.
At a median follow-up of 15 months (range, 8 to 27), the median duration of response had not been reached. Responses were associated with in situ infiltration of cytotoxic CD8+ T cells, decreased activation of regulatory T cells, and expansion of subpopulations of effector T cells.
The 1-year overall survival rate was 49%.
The investigators said these encouraging results have set the stage for larger trials of checkpoint blockade in this patient population. Further research is planned to determine whether immunotherapy drugs could be given to high-risk patients to prevent relapse. ![]()

Photo from Business Wire
Results of a phase 1 study suggest that repeated doses of the immunotherapy drug ipilimumab is a feasible treatment option for patients with hematologic diseases who relapse after allogeneic hematopoietic stem cell transplant (HSCT).
Seven of the 28 patients studied responded to the treatment, but immune-mediated toxic effects and graft-vs-host disease (GVHD) occurred as well.
These results were published in NEJM.
Ipilimumab, which is already approved to treat unresectable or metastatic melanoma, works by blocking the immune checkpoint CTLA-4. Blockade of CTLA-4 has been shown to augment T-cell activation and proliferation.
“We believe [,in the case of relapse after HSCT,] the donor immune cells are present but can’t recognize the tumor cells because of inhibitory signals that disguise them,” said study author Matthew Davids, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“By blocking the checkpoint, you allow the donor cells to see the cancer cells.”
Dr Davids and his colleagues tested this theory in 28 patients who had relapsed after allogeneic HSCT. The patients had acute myeloid leukemia (AML, n=12), Hodgkin lymphoma (n=7), non-Hodgkin lymphoma (n=4), myelodysplastic syndromes (MDS, n=2), multiple myeloma (n=1), myeloproliferative neoplasm (n=1), or acute lymphoblastic leukemia (n=1).
Patients had received a median of 3 prior treatment regimens, excluding HSCT (range, 1 to 14), and 20 patients (71%) had received treatment for relapse after transplant. Eight patients (29%) previously had grade 1/2 acute GVHD, and 16 (57%) previously had chronic GVHD.
The median time from transplant to initial treatment with ipilimumab was 675 days (range, 198 to 1830), and the median time from relapse to initial treatment with ipilimumab was 97 days (range, 0 to
1415).
Patients received induction therapy with ipilimumab at a dose of 3 mg/kg or 10 mg/kg every 3 weeks for a total of 4 doses. Those who had a clinical benefit received additional doses every 12 weeks for up to 60 weeks.
Safety
Five patients discontinued ipilimumab due to dose-limiting toxic effects. Four of these patients had GVHD, and 1 had severe immune-related adverse events.
Dose-limiting GVHD presented as chronic GVHD of the liver in 3 patients and acute GVHD of the gut in 1 patient.
Immune-related adverse events included death (n=1), pneumonitis (2 grade 2 events, 1 grade 4 event), colitis (1 grade 3 event), immune thrombocytopenia (1 grade 2 event), and diarrhea (1 grade 2 event).
Efficacy
There were no responses in patients who received ipilimumab at 3 mg/kg. Among the 22 patients who received ipilimumab at 10 mg/kg, 5 had a complete response, and 2 had a partial response.
Six other patients did not qualify as having responses but had a decrease in their tumor burden. Altogether, ipilimumab reduced tumor burden in 59% of patients.
The complete responses occurred in 4 patients with extramedullary AML and 1 patient with MDS developing into AML. Two of the AML patients remained in complete response at 12 and 15 months, and the patient with MDS remained in complete response at 16 months.
At a median follow-up of 15 months (range, 8 to 27), the median duration of response had not been reached. Responses were associated with in situ infiltration of cytotoxic CD8+ T cells, decreased activation of regulatory T cells, and expansion of subpopulations of effector T cells.
The 1-year overall survival rate was 49%.
The investigators said these encouraging results have set the stage for larger trials of checkpoint blockade in this patient population. Further research is planned to determine whether immunotherapy drugs could be given to high-risk patients to prevent relapse. ![]()
COMP recommends orphan status for drug to treat PNH

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()

The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) has issued a positive opinion recommending orphan designation for Coversin for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
Coversin is a second-generation complement inhibitor that acts on complement component-C5, preventing release of C5a and formation of C5b-9 (also known as the membrane attack complex).
Coversin is a recombinant small protein (16,740 Da) derived from a native protein found in the saliva of the Ornithodoros moubata tick.
The drug is being developed by Akari Therapeutics.
In vitro experiments have shown that Coversin inhibits red blood cell lysis in PNH, and the drug can achieve full complement inhibition in the blood of PNH patients who are resistant to the drug eculizumab.
In a phase 1a trial of healthy volunteers, Coversin completely inhibited complement C5 activity within 12 hours of administration.
Akari Therapeutics is currently conducting a phase 1b study of Coversin in healthy volunteers and is administering the drug to a patient with eculizumab-resistant PNH. Thus far, Coversin has prevented hemolytic episodes and improved disease symptoms in this patient. And the only drug-related adverse event has been occasional local and transient irritation at the injection site.
Coversin is also being studied in atypical hemolytic uremic syndrome and Guillain Barré syndrome.
About orphan designation
The COMP adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity in the European Union if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure. ![]()
Drug could be disease-modifying for SCD, team says
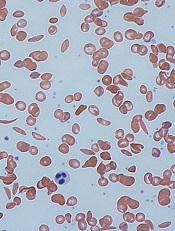
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
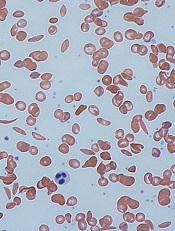
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
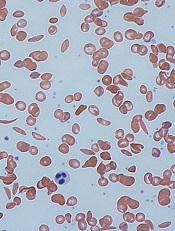
Image by Graham Beards
Researchers say the small molecule GBT440 could be a disease-modifying agent for patients with sickle cell disease (SCD).
Preclinical data showed that GBT440 can reduce sickling, extend the circulating half-life of red blood cells (RBCs), and decrease excessive erythropoiesis in SCD.
GBT440 binds specifically to hemoglobin and is designed to inhibit sickle hemoglobin (HbS) polymer formation.
“One promising strategy for preventing red blood cell sickling and subsequently modifying sickle cell disease over the long term involves inhibiting polymerization of HbS in red blood cells,” said David R. Archer, PhD, of Emory University School of Medicine in Atlanta, Georgia.
“This can be achieved by increasing the proportion of oxygenated HbS in those cells. We believe our preclinical results provide strong evidence that GBT440 inhibits HbS polymerization and red blood cell sickling, which is important because it addresses the underlying pathophysiology of sickle cell disease and has the potential to change its devastating clinical course.”
Dr Archer and his colleagues reported these results in the British Journal of Haematology. The research was supported by Global Blood Therapeutics, Inc., the company developing GBT440.
The researchers reported that, in vitro, GBT440 dose-dependently increased the affinity of HbS for oxygen, delayed polymerization of HbS, and reduced the number of sickled RBCs in whole blood from SCD patients.
In an animal model of SCD, GBT440 inhibited RBC sickling, prolonged the half-life of RBCs, and reduced reticulocyte counts.
The researchers said the drug also exhibited favorable pharmacokinetic properties in various animal species, suggesting the potential for once-daily oral dosing in SCD patients.
“Our preclinical work has developed a foundation of evidence that GBT440 is a potent inhibitor of the polymerization of HbS,” said Ted W. Love, MD, chief executive officer of Global Blood Therapeutics, Inc.
“We continue to build on these data with our ongoing phase 1/2 study, which has shown that GBT440 was well-tolerated over 90 days of dosing and that all SCD patients who received multiple doses of GBT440 exhibited improvements in one or more clinical markers of hemolysis and anemia. Our next step is to initiate a pivotal trial in adults with SCD later this year.” ![]()
Computer model shows how spleen filters blood

Researchers have created a computer model that shows how tiny slits in the spleen prevent old, diseased, or misshapen red blood cells from re-entering the bloodstream.
The team says the model can be used to study the spleen’s role in controlling diseases that affect the size and structure of red blood cells—such as sickle cell anemia, thalassemia, and malaria—and to develop new diagnostics and therapeutics for these diseases.
The researchers described the model in PNAS.
Previous studies have shown that part of the spleen’s filtration process relies on having red blood cells squeeze through tiny slits between the endothelial cells that line the spleen’s blood vessels. These “interendothelial slits” are no larger than 1.2 µm tall, 4 µm wide, and 1.9 µm deep.
More rigid and misshapen blood cells might not be able to pass through these narrow passages. And this process cannot be observed in vivo because of the minute size of the slits.
In order to “see” how the interendothelial slits regulate red blood cell circulation, the researchers created a computer simulation based on dissipative particle dynamics, a modeling method.
Their model allowed the team to determine the range of cell sizes and shapes that could fit through the slits. The range closely mirrored the range of sizes and shapes for healthy red blood cells, indicating that only healthy cells should be able to pass through the slits.
“The computational and analytical models from this work, along with a variety of experimental observations, point to a more detailed picture of how the physiology of the human spleen likely influences several key geometrical characteristics of red blood cells,” said study author Subra Suresh, ScD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“They also offer better understanding of how the circulatory bottleneck for the red blood cell in the spleen could affect a variety of acute and chronic disease states arising from hereditary disorders, human cancers, and infectious diseases, with implications for therapeutic interventions and drug efficacy assays.”
In addition to giving researchers a better picture of how the spleen functions, the findings provide new insights into drug treatments.
A class of drugs currently in development for treating malaria alters the shape of red blood cells infected with malaria, theoretically preventing them from passing through interendothelial slits. One such drug, spiroindoline KAE609, is in clinical trials.
The researchers’ results might also explain why artemisinin-based antimalarial drugs, which stiffen healthy and malaria-infected red blood cells, can lead to severe anemia. ![]()

Researchers have created a computer model that shows how tiny slits in the spleen prevent old, diseased, or misshapen red blood cells from re-entering the bloodstream.
The team says the model can be used to study the spleen’s role in controlling diseases that affect the size and structure of red blood cells—such as sickle cell anemia, thalassemia, and malaria—and to develop new diagnostics and therapeutics for these diseases.
The researchers described the model in PNAS.
Previous studies have shown that part of the spleen’s filtration process relies on having red blood cells squeeze through tiny slits between the endothelial cells that line the spleen’s blood vessels. These “interendothelial slits” are no larger than 1.2 µm tall, 4 µm wide, and 1.9 µm deep.
More rigid and misshapen blood cells might not be able to pass through these narrow passages. And this process cannot be observed in vivo because of the minute size of the slits.
In order to “see” how the interendothelial slits regulate red blood cell circulation, the researchers created a computer simulation based on dissipative particle dynamics, a modeling method.
Their model allowed the team to determine the range of cell sizes and shapes that could fit through the slits. The range closely mirrored the range of sizes and shapes for healthy red blood cells, indicating that only healthy cells should be able to pass through the slits.
“The computational and analytical models from this work, along with a variety of experimental observations, point to a more detailed picture of how the physiology of the human spleen likely influences several key geometrical characteristics of red blood cells,” said study author Subra Suresh, ScD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“They also offer better understanding of how the circulatory bottleneck for the red blood cell in the spleen could affect a variety of acute and chronic disease states arising from hereditary disorders, human cancers, and infectious diseases, with implications for therapeutic interventions and drug efficacy assays.”
In addition to giving researchers a better picture of how the spleen functions, the findings provide new insights into drug treatments.
A class of drugs currently in development for treating malaria alters the shape of red blood cells infected with malaria, theoretically preventing them from passing through interendothelial slits. One such drug, spiroindoline KAE609, is in clinical trials.
The researchers’ results might also explain why artemisinin-based antimalarial drugs, which stiffen healthy and malaria-infected red blood cells, can lead to severe anemia. ![]()

Researchers have created a computer model that shows how tiny slits in the spleen prevent old, diseased, or misshapen red blood cells from re-entering the bloodstream.
The team says the model can be used to study the spleen’s role in controlling diseases that affect the size and structure of red blood cells—such as sickle cell anemia, thalassemia, and malaria—and to develop new diagnostics and therapeutics for these diseases.
The researchers described the model in PNAS.
Previous studies have shown that part of the spleen’s filtration process relies on having red blood cells squeeze through tiny slits between the endothelial cells that line the spleen’s blood vessels. These “interendothelial slits” are no larger than 1.2 µm tall, 4 µm wide, and 1.9 µm deep.
More rigid and misshapen blood cells might not be able to pass through these narrow passages. And this process cannot be observed in vivo because of the minute size of the slits.
In order to “see” how the interendothelial slits regulate red blood cell circulation, the researchers created a computer simulation based on dissipative particle dynamics, a modeling method.
Their model allowed the team to determine the range of cell sizes and shapes that could fit through the slits. The range closely mirrored the range of sizes and shapes for healthy red blood cells, indicating that only healthy cells should be able to pass through the slits.
“The computational and analytical models from this work, along with a variety of experimental observations, point to a more detailed picture of how the physiology of the human spleen likely influences several key geometrical characteristics of red blood cells,” said study author Subra Suresh, ScD, of Carnegie Mellon University in Pittsburgh, Pennsylvania.
“They also offer better understanding of how the circulatory bottleneck for the red blood cell in the spleen could affect a variety of acute and chronic disease states arising from hereditary disorders, human cancers, and infectious diseases, with implications for therapeutic interventions and drug efficacy assays.”
In addition to giving researchers a better picture of how the spleen functions, the findings provide new insights into drug treatments.
A class of drugs currently in development for treating malaria alters the shape of red blood cells infected with malaria, theoretically preventing them from passing through interendothelial slits. One such drug, spiroindoline KAE609, is in clinical trials.
The researchers’ results might also explain why artemisinin-based antimalarial drugs, which stiffen healthy and malaria-infected red blood cells, can lead to severe anemia. ![]()
Study: CMV doesn’t lower risk of relapse, death
Small studies have suggested that early cytomegalovirus (CMV) reactivation may protect against leukemia relapse and even death after hematopoietic stem cell transplant.
However, a new study, based on data from about 9500 patients, suggests otherwise.
Results showed no association between CMV reactivation and relapse but suggested CMV reactivation increases the risk of non-relapse mortality.
Researchers reported these findings in Blood.
“The original purpose of the study was to confirm that CMV infection may prevent leukemia relapse, prevent death, and become a major therapeutic tool for improving patient survival rates,” said study author Pierre Teira, MD, of the University of Montreal in Quebec, Canada.
“However, we found the exact opposite. Our results clearly show that . . . the virus not only does not prevent leukemia relapse [it] also remains a major factor associated with the risk of death. Monitoring of CMV after transplantation remains a priority for patients.”
For this study, Dr Teira and his colleagues analyzed data from 9469 patients who received a transplant between 2003 and 2010.
The patients had acute myeloid leukemia (AML, n=5310), acute lymphoblastic leukemia (ALL, n=1883), chronic myeloid leukemia (CML, n=1079), or myelodysplastic syndromes (MDS, n=1197).
The median time to initial CMV reactivation was 41 days (range, 1-362 days).
The researchers found no significant association between CMV reactivation and disease relapse for AML (P=0.60), ALL (P=0.08), CML (P=0.94), or MDS (P=0.58).
However, CMV reactivation was associated with a significantly higher risk of nonrelapse mortality for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0004), and MDS (P=0.0002).
Therefore, CMV reactivation was associated with significantly lower overall survival for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0005), and MDS (P=0.003).
“Deaths due to uncontrolled CMV reactivation are virtually zero in this study, so uncontrolled CMV reactivation is not what reduces survival rates after transplantation,” Dr Teira noted. “The link between this common virus and increased risk of death remains a biological mystery.”
One possible explanation is that CMV decreases the ability of the patient’s immune system to fight against other types of infection. This is supported by the fact that death rates from infections other than CMV are higher in patients infected with CMV or patients whose donors were.
For researchers, the next step is therefore to verify whether the latest generation of anti-CMV treatments can prevent both reactivation of the virus and weakening of the patient’s immune system against other types of infection in the presence of CMV infection.
“CMV has a complex impact on the outcomes for transplant patients, and, each year, more than 30,000 patients around the world receive bone marrow transplants from donors,” Dr Teira said.
“It is therefore essential for future research to better understand the role played by CMV after bone marrow transplantation and improve the chances of success of the transplant. This will help to better choose the right donor for the right patient.” ![]()
Small studies have suggested that early cytomegalovirus (CMV) reactivation may protect against leukemia relapse and even death after hematopoietic stem cell transplant.
However, a new study, based on data from about 9500 patients, suggests otherwise.
Results showed no association between CMV reactivation and relapse but suggested CMV reactivation increases the risk of non-relapse mortality.
Researchers reported these findings in Blood.
“The original purpose of the study was to confirm that CMV infection may prevent leukemia relapse, prevent death, and become a major therapeutic tool for improving patient survival rates,” said study author Pierre Teira, MD, of the University of Montreal in Quebec, Canada.
“However, we found the exact opposite. Our results clearly show that . . . the virus not only does not prevent leukemia relapse [it] also remains a major factor associated with the risk of death. Monitoring of CMV after transplantation remains a priority for patients.”
For this study, Dr Teira and his colleagues analyzed data from 9469 patients who received a transplant between 2003 and 2010.
The patients had acute myeloid leukemia (AML, n=5310), acute lymphoblastic leukemia (ALL, n=1883), chronic myeloid leukemia (CML, n=1079), or myelodysplastic syndromes (MDS, n=1197).
The median time to initial CMV reactivation was 41 days (range, 1-362 days).
The researchers found no significant association between CMV reactivation and disease relapse for AML (P=0.60), ALL (P=0.08), CML (P=0.94), or MDS (P=0.58).
However, CMV reactivation was associated with a significantly higher risk of nonrelapse mortality for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0004), and MDS (P=0.0002).
Therefore, CMV reactivation was associated with significantly lower overall survival for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0005), and MDS (P=0.003).
“Deaths due to uncontrolled CMV reactivation are virtually zero in this study, so uncontrolled CMV reactivation is not what reduces survival rates after transplantation,” Dr Teira noted. “The link between this common virus and increased risk of death remains a biological mystery.”
One possible explanation is that CMV decreases the ability of the patient’s immune system to fight against other types of infection. This is supported by the fact that death rates from infections other than CMV are higher in patients infected with CMV or patients whose donors were.
For researchers, the next step is therefore to verify whether the latest generation of anti-CMV treatments can prevent both reactivation of the virus and weakening of the patient’s immune system against other types of infection in the presence of CMV infection.
“CMV has a complex impact on the outcomes for transplant patients, and, each year, more than 30,000 patients around the world receive bone marrow transplants from donors,” Dr Teira said.
“It is therefore essential for future research to better understand the role played by CMV after bone marrow transplantation and improve the chances of success of the transplant. This will help to better choose the right donor for the right patient.” ![]()
Small studies have suggested that early cytomegalovirus (CMV) reactivation may protect against leukemia relapse and even death after hematopoietic stem cell transplant.
However, a new study, based on data from about 9500 patients, suggests otherwise.
Results showed no association between CMV reactivation and relapse but suggested CMV reactivation increases the risk of non-relapse mortality.
Researchers reported these findings in Blood.
“The original purpose of the study was to confirm that CMV infection may prevent leukemia relapse, prevent death, and become a major therapeutic tool for improving patient survival rates,” said study author Pierre Teira, MD, of the University of Montreal in Quebec, Canada.
“However, we found the exact opposite. Our results clearly show that . . . the virus not only does not prevent leukemia relapse [it] also remains a major factor associated with the risk of death. Monitoring of CMV after transplantation remains a priority for patients.”
For this study, Dr Teira and his colleagues analyzed data from 9469 patients who received a transplant between 2003 and 2010.
The patients had acute myeloid leukemia (AML, n=5310), acute lymphoblastic leukemia (ALL, n=1883), chronic myeloid leukemia (CML, n=1079), or myelodysplastic syndromes (MDS, n=1197).
The median time to initial CMV reactivation was 41 days (range, 1-362 days).
The researchers found no significant association between CMV reactivation and disease relapse for AML (P=0.60), ALL (P=0.08), CML (P=0.94), or MDS (P=0.58).
However, CMV reactivation was associated with a significantly higher risk of nonrelapse mortality for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0004), and MDS (P=0.0002).
Therefore, CMV reactivation was associated with significantly lower overall survival for AML (P<0.0001), ALL (P<0.0001), CML (P=0.0005), and MDS (P=0.003).
“Deaths due to uncontrolled CMV reactivation are virtually zero in this study, so uncontrolled CMV reactivation is not what reduces survival rates after transplantation,” Dr Teira noted. “The link between this common virus and increased risk of death remains a biological mystery.”
One possible explanation is that CMV decreases the ability of the patient’s immune system to fight against other types of infection. This is supported by the fact that death rates from infections other than CMV are higher in patients infected with CMV or patients whose donors were.
For researchers, the next step is therefore to verify whether the latest generation of anti-CMV treatments can prevent both reactivation of the virus and weakening of the patient’s immune system against other types of infection in the presence of CMV infection.
“CMV has a complex impact on the outcomes for transplant patients, and, each year, more than 30,000 patients around the world receive bone marrow transplants from donors,” Dr Teira said.
“It is therefore essential for future research to better understand the role played by CMV after bone marrow transplantation and improve the chances of success of the transplant. This will help to better choose the right donor for the right patient.” ![]()
Drug enables transfusion independence in lower-risk MDS

COPENHAGEN—Results from a pair of phase 2 trials suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with lower-risk myelodysplastic syndromes (MDS).
In a 3-month base study, 51% of patients treated with luspatercept had an erythroid response, and 35% achieved transfusion independence.
In an ongoing extension study, 81% of luspatercept-treated patients have had an erythroid response, and 50% have achieved transfusion independence.
The majority of adverse events in both trials were grade 1 and 2.
Uwe Platzbecker, MD, of the University Hospital in Dresden, Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S131*). The studies were sponsored by Acceleron Pharma, Inc.
Luspatercept (formerly ACE-536) is a modified activin receptor type IIB fusion protein that increases red blood cell (RBC) levels by targeting molecules in the TGF-β superfamily. Acceleron and Celgene are developing luspatercept to treat anemia in patients with rare blood disorders.
The phase 2 base study was a dose-escalation trial in which MDS patients received luspatercept for 3 months. In the ongoing extension study, patients from the base study are receiving luspatercept for an additional 24 months.
In both studies, patients with high transfusion burden (≥4 RBC units/8 weeks) and those with low transfusion burden (<4 RBC units/8 weeks) received luspatercept once every 3 weeks.
Base study
This study included 58 patients with a median age of 71.5 (range, 27-90). Their median time since diagnosis was 2.4 years (range, 0-14). Seventeen percent of patients had prior lenalidomide treatment, and 66% had previously received erythropoiesis-stimulating agents (ESAs).
In patients with low transfusion burden (n=19), the median hemoglobin at baseline was 8.7 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=39), the median number of RBC units transfused per 8 weeks was 6 (range, 4-18).
Patients received luspatercept subcutaneously every 3 weeks for up to 5 doses. The study included 7 dose-escalation cohorts (n=27, 0.125 to 1.75 mg/kg) and an expansion cohort (n=31, 1.0 to 1.75 mg/kg).
The primary outcome measure was the proportion of patients who had an erythroid response. In non-transfusion-dependent patients, an erythroid response was defined as a hemoglobin increase of at least 1.5 g/dL from baseline for at least 14 days.
In transfusion-dependent patients, an erythroid response was defined as a reduction of at least 4 RBC units transfused or a reduction of at least 50% of RBC units transfused compared to pretreatment.
Fifty-one percent (25/49) of patients treated at the higher dose levels had an erythroid response. And 35% (14/40) of transfused patients treated at the higher dose levels were transfusion independent for at least 8 weeks.
Extension study
This study includes 32 patients with a median age of 71.5 (range, 29-90). Their median time since diagnosis was 2.9 years (range, 0-14). Nineteen percent of patients had prior lenalidomide treatment, and 59% had previously received ESAs.
In patients with low transfusion burden (n=13), the median hemoglobin at baseline was 8.5 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=19), the median number of RBC units transfused per 8 weeks was 6 (range, 4-14).
In this ongoing study, patients are receiving luspatercept (1.0 to 1.75 mg/kg) subcutaneously every 3 weeks for an additional 24 months.
At last follow-up (March 4, 2016), 81% (26/32) of patients had an erythroid response. And 50% (11/22) of patients who were transfused prior to study initiation achieved transfusion independence for at least 8 weeks (range, 9-80+ weeks).
Dr Platzbecker noted that, in both studies, erythroid responses were observed whether or not patients previously received ESAs and regardless of patients’ baseline erythropoietin levels.
Safety
There were three grade 3 adverse events that were possibly or probably related to luspatercept—an increase in blast cell count, myalgia, and worsening of general condition.
Adverse events that were possibly or probably related to luspatercept and occurred in at least 2 patients were fatigue (7%, n=4), bone pain (5%, n=3), diarrhea (5%, n=3), myalgia (5%, n=3), headache (3%, n=2), hypertension (3%, n=2), and injection site erythema (3%, n=2).
Dr Platzbecker said luspatercept was generally safe and well-tolerated in these studies. And the results of these trials supported the initiation of a phase 3 study (MEDALIST, NCT02631070) in patients with lower-risk MDS. ![]()
*Data in the abstract differ from data presented at the meeting.

COPENHAGEN—Results from a pair of phase 2 trials suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with lower-risk myelodysplastic syndromes (MDS).
In a 3-month base study, 51% of patients treated with luspatercept had an erythroid response, and 35% achieved transfusion independence.
In an ongoing extension study, 81% of luspatercept-treated patients have had an erythroid response, and 50% have achieved transfusion independence.
The majority of adverse events in both trials were grade 1 and 2.
Uwe Platzbecker, MD, of the University Hospital in Dresden, Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S131*). The studies were sponsored by Acceleron Pharma, Inc.
Luspatercept (formerly ACE-536) is a modified activin receptor type IIB fusion protein that increases red blood cell (RBC) levels by targeting molecules in the TGF-β superfamily. Acceleron and Celgene are developing luspatercept to treat anemia in patients with rare blood disorders.
The phase 2 base study was a dose-escalation trial in which MDS patients received luspatercept for 3 months. In the ongoing extension study, patients from the base study are receiving luspatercept for an additional 24 months.
In both studies, patients with high transfusion burden (≥4 RBC units/8 weeks) and those with low transfusion burden (<4 RBC units/8 weeks) received luspatercept once every 3 weeks.
Base study
This study included 58 patients with a median age of 71.5 (range, 27-90). Their median time since diagnosis was 2.4 years (range, 0-14). Seventeen percent of patients had prior lenalidomide treatment, and 66% had previously received erythropoiesis-stimulating agents (ESAs).
In patients with low transfusion burden (n=19), the median hemoglobin at baseline was 8.7 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=39), the median number of RBC units transfused per 8 weeks was 6 (range, 4-18).
Patients received luspatercept subcutaneously every 3 weeks for up to 5 doses. The study included 7 dose-escalation cohorts (n=27, 0.125 to 1.75 mg/kg) and an expansion cohort (n=31, 1.0 to 1.75 mg/kg).
The primary outcome measure was the proportion of patients who had an erythroid response. In non-transfusion-dependent patients, an erythroid response was defined as a hemoglobin increase of at least 1.5 g/dL from baseline for at least 14 days.
In transfusion-dependent patients, an erythroid response was defined as a reduction of at least 4 RBC units transfused or a reduction of at least 50% of RBC units transfused compared to pretreatment.
Fifty-one percent (25/49) of patients treated at the higher dose levels had an erythroid response. And 35% (14/40) of transfused patients treated at the higher dose levels were transfusion independent for at least 8 weeks.
Extension study
This study includes 32 patients with a median age of 71.5 (range, 29-90). Their median time since diagnosis was 2.9 years (range, 0-14). Nineteen percent of patients had prior lenalidomide treatment, and 59% had previously received ESAs.
In patients with low transfusion burden (n=13), the median hemoglobin at baseline was 8.5 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=19), the median number of RBC units transfused per 8 weeks was 6 (range, 4-14).
In this ongoing study, patients are receiving luspatercept (1.0 to 1.75 mg/kg) subcutaneously every 3 weeks for an additional 24 months.
At last follow-up (March 4, 2016), 81% (26/32) of patients had an erythroid response. And 50% (11/22) of patients who were transfused prior to study initiation achieved transfusion independence for at least 8 weeks (range, 9-80+ weeks).
Dr Platzbecker noted that, in both studies, erythroid responses were observed whether or not patients previously received ESAs and regardless of patients’ baseline erythropoietin levels.
Safety
There were three grade 3 adverse events that were possibly or probably related to luspatercept—an increase in blast cell count, myalgia, and worsening of general condition.
Adverse events that were possibly or probably related to luspatercept and occurred in at least 2 patients were fatigue (7%, n=4), bone pain (5%, n=3), diarrhea (5%, n=3), myalgia (5%, n=3), headache (3%, n=2), hypertension (3%, n=2), and injection site erythema (3%, n=2).
Dr Platzbecker said luspatercept was generally safe and well-tolerated in these studies. And the results of these trials supported the initiation of a phase 3 study (MEDALIST, NCT02631070) in patients with lower-risk MDS. ![]()
*Data in the abstract differ from data presented at the meeting.

COPENHAGEN—Results from a pair of phase 2 trials suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with lower-risk myelodysplastic syndromes (MDS).
In a 3-month base study, 51% of patients treated with luspatercept had an erythroid response, and 35% achieved transfusion independence.
In an ongoing extension study, 81% of luspatercept-treated patients have had an erythroid response, and 50% have achieved transfusion independence.
The majority of adverse events in both trials were grade 1 and 2.
Uwe Platzbecker, MD, of the University Hospital in Dresden, Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S131*). The studies were sponsored by Acceleron Pharma, Inc.
Luspatercept (formerly ACE-536) is a modified activin receptor type IIB fusion protein that increases red blood cell (RBC) levels by targeting molecules in the TGF-β superfamily. Acceleron and Celgene are developing luspatercept to treat anemia in patients with rare blood disorders.
The phase 2 base study was a dose-escalation trial in which MDS patients received luspatercept for 3 months. In the ongoing extension study, patients from the base study are receiving luspatercept for an additional 24 months.
In both studies, patients with high transfusion burden (≥4 RBC units/8 weeks) and those with low transfusion burden (<4 RBC units/8 weeks) received luspatercept once every 3 weeks.
Base study
This study included 58 patients with a median age of 71.5 (range, 27-90). Their median time since diagnosis was 2.4 years (range, 0-14). Seventeen percent of patients had prior lenalidomide treatment, and 66% had previously received erythropoiesis-stimulating agents (ESAs).
In patients with low transfusion burden (n=19), the median hemoglobin at baseline was 8.7 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=39), the median number of RBC units transfused per 8 weeks was 6 (range, 4-18).
Patients received luspatercept subcutaneously every 3 weeks for up to 5 doses. The study included 7 dose-escalation cohorts (n=27, 0.125 to 1.75 mg/kg) and an expansion cohort (n=31, 1.0 to 1.75 mg/kg).
The primary outcome measure was the proportion of patients who had an erythroid response. In non-transfusion-dependent patients, an erythroid response was defined as a hemoglobin increase of at least 1.5 g/dL from baseline for at least 14 days.
In transfusion-dependent patients, an erythroid response was defined as a reduction of at least 4 RBC units transfused or a reduction of at least 50% of RBC units transfused compared to pretreatment.
Fifty-one percent (25/49) of patients treated at the higher dose levels had an erythroid response. And 35% (14/40) of transfused patients treated at the higher dose levels were transfusion independent for at least 8 weeks.
Extension study
This study includes 32 patients with a median age of 71.5 (range, 29-90). Their median time since diagnosis was 2.9 years (range, 0-14). Nineteen percent of patients had prior lenalidomide treatment, and 59% had previously received ESAs.
In patients with low transfusion burden (n=13), the median hemoglobin at baseline was 8.5 g/dL (range, 6.4-10.1). In patients with high transfusion burden (n=19), the median number of RBC units transfused per 8 weeks was 6 (range, 4-14).
In this ongoing study, patients are receiving luspatercept (1.0 to 1.75 mg/kg) subcutaneously every 3 weeks for an additional 24 months.
At last follow-up (March 4, 2016), 81% (26/32) of patients had an erythroid response. And 50% (11/22) of patients who were transfused prior to study initiation achieved transfusion independence for at least 8 weeks (range, 9-80+ weeks).
Dr Platzbecker noted that, in both studies, erythroid responses were observed whether or not patients previously received ESAs and regardless of patients’ baseline erythropoietin levels.
Safety
There were three grade 3 adverse events that were possibly or probably related to luspatercept—an increase in blast cell count, myalgia, and worsening of general condition.
Adverse events that were possibly or probably related to luspatercept and occurred in at least 2 patients were fatigue (7%, n=4), bone pain (5%, n=3), diarrhea (5%, n=3), myalgia (5%, n=3), headache (3%, n=2), hypertension (3%, n=2), and injection site erythema (3%, n=2).
Dr Platzbecker said luspatercept was generally safe and well-tolerated in these studies. And the results of these trials supported the initiation of a phase 3 study (MEDALIST, NCT02631070) in patients with lower-risk MDS. ![]()
*Data in the abstract differ from data presented at the meeting.
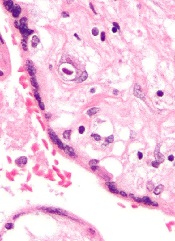
Long-term opioid use may not benefit SCD patients

and a normal one
Image by Betty Pace
Results of a small study suggest that long-term opioid treatment may not be the best option for pain management in adults with sickle cell disease (SCD).
The study showed that patients who received opioids long-term often fared worse in measures of pain, fatigue, and curtailed daily activities than patients who were not on long-term opioids.
Researchers reported these findings in the American Journal of Preventive Medicine.
“We need to be careful and skeptical about giving increasing doses of opioids to patients with sickle cell disease who are in chronic pain if it isn’t effective,” said study author C. Patrick Carroll, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“Too little is known about the effects of long-term opioid management of chronic pain.”
For this study, Dr Carroll and his colleagues enrolled 83 SCD patients—57 women and 26 men. All were 18 and older, and their average age was 39.
Twenty-nine of the patients had been prescribed daily, long-acting opioids to manage their pain. The remaining 54 patients weren’t on long-term opioids.
The patients filled out daily electronic pain diaries for 90 days. Self-reported levels of pain, physical activity, fatigue, and pain-related daily activity interference were recorded, along with self-reported levels of pain relief and medication satisfaction on a scale of 0 to 100.
Crises, pain, and fatigue
The proportion of days in vaso-occlusive crisis was significantly higher for patients who were on long-term opioid therapy than for those who were not—29% and 11.9%, respectively (P<0.01).
Patients on long-term opioids also reported significantly higher levels of crisis pain—60.6 and 41.0, respectively (P<0.001)—and non-crisis pain—34.5 and 10.3, respectively (P<0.001).
Patients on long-term opioid therapy had higher levels of pain-related activity interference, both on non-crisis days—24.9 and 7.4, respectively (P<0.001)—and crisis days—56.7 and 37.7, respectively (P<0.01).
And patients on long-term opioid therapy had higher levels of fatigue on non-crisis days—49.7 and 27.0, respectively (P<0.001)—and crisis days—66.1 and 53.0, respectively (P<0.05).
Central sensitization
The researchers also performed some standard measures of pain processing on the test subjects, which measured and averaged variables such as how intensely participants experienced unpleasant heat and pressure.
The team was particularly interested in the phenomenon of central sensitization, in which the central nervous system amplifies painful sensations.
Central sensitization may be one way that opioids can increase pain sensitivity, and it also may play a role in how SCD causes chronic pain, Dr Carroll said.
For example, one such measure of central sensitization uses repeated pokes from a mildly painful stimulus in succession. In people who have this hypersensitization, each poke is perceived as more intense than the last because the nervous system becomes progressively more sensitive to the pain.
Combining the data from several measures of central sensitization, the researchers used a scoring system that sets a normal measurement at 0 and rates how abnormal something is by how far the values move away from 0. They calculated a central sensitization index for patients on long-term opioids and those not taking them.
Overall, patients on long-term opioid therapy showed higher levels of central sensitization, with an index of 0.34, than those who were not on opioids, with an index of -0.10.
In patients who were not on long-term opioid therapy, the level of central sensitization correlated with the level of non-crisis pain. However, in patients who were taking long-term opioid therapy and also had higher levels of central sensitization and clinical pain, the correlation essentially vanished.
Dr Carroll said this was surprising and suggests the mechanisms of pain in SCD patients on long-term opioid therapy may be different from patients who don’t take daily opioids for pain.
Dr Carroll cautioned that this work is preliminary and should not lead to the discontinuation of long-term opioid therapy in SCD patients.
“We need to better understand how long-term opioid use affects pain sensitization and determine if certain people are more sensitive to these effects so we can prescribe the best treatment option for each individual patient,” Dr Carroll said. “We also need to learn more about how sickle cell disease may sensitize the nervous system.” ![]()

and a normal one
Image by Betty Pace
Results of a small study suggest that long-term opioid treatment may not be the best option for pain management in adults with sickle cell disease (SCD).
The study showed that patients who received opioids long-term often fared worse in measures of pain, fatigue, and curtailed daily activities than patients who were not on long-term opioids.
Researchers reported these findings in the American Journal of Preventive Medicine.
“We need to be careful and skeptical about giving increasing doses of opioids to patients with sickle cell disease who are in chronic pain if it isn’t effective,” said study author C. Patrick Carroll, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“Too little is known about the effects of long-term opioid management of chronic pain.”
For this study, Dr Carroll and his colleagues enrolled 83 SCD patients—57 women and 26 men. All were 18 and older, and their average age was 39.
Twenty-nine of the patients had been prescribed daily, long-acting opioids to manage their pain. The remaining 54 patients weren’t on long-term opioids.
The patients filled out daily electronic pain diaries for 90 days. Self-reported levels of pain, physical activity, fatigue, and pain-related daily activity interference were recorded, along with self-reported levels of pain relief and medication satisfaction on a scale of 0 to 100.
Crises, pain, and fatigue
The proportion of days in vaso-occlusive crisis was significantly higher for patients who were on long-term opioid therapy than for those who were not—29% and 11.9%, respectively (P<0.01).
Patients on long-term opioids also reported significantly higher levels of crisis pain—60.6 and 41.0, respectively (P<0.001)—and non-crisis pain—34.5 and 10.3, respectively (P<0.001).
Patients on long-term opioid therapy had higher levels of pain-related activity interference, both on non-crisis days—24.9 and 7.4, respectively (P<0.001)—and crisis days—56.7 and 37.7, respectively (P<0.01).
And patients on long-term opioid therapy had higher levels of fatigue on non-crisis days—49.7 and 27.0, respectively (P<0.001)—and crisis days—66.1 and 53.0, respectively (P<0.05).
Central sensitization
The researchers also performed some standard measures of pain processing on the test subjects, which measured and averaged variables such as how intensely participants experienced unpleasant heat and pressure.
The team was particularly interested in the phenomenon of central sensitization, in which the central nervous system amplifies painful sensations.
Central sensitization may be one way that opioids can increase pain sensitivity, and it also may play a role in how SCD causes chronic pain, Dr Carroll said.
For example, one such measure of central sensitization uses repeated pokes from a mildly painful stimulus in succession. In people who have this hypersensitization, each poke is perceived as more intense than the last because the nervous system becomes progressively more sensitive to the pain.
Combining the data from several measures of central sensitization, the researchers used a scoring system that sets a normal measurement at 0 and rates how abnormal something is by how far the values move away from 0. They calculated a central sensitization index for patients on long-term opioids and those not taking them.
Overall, patients on long-term opioid therapy showed higher levels of central sensitization, with an index of 0.34, than those who were not on opioids, with an index of -0.10.
In patients who were not on long-term opioid therapy, the level of central sensitization correlated with the level of non-crisis pain. However, in patients who were taking long-term opioid therapy and also had higher levels of central sensitization and clinical pain, the correlation essentially vanished.
Dr Carroll said this was surprising and suggests the mechanisms of pain in SCD patients on long-term opioid therapy may be different from patients who don’t take daily opioids for pain.
Dr Carroll cautioned that this work is preliminary and should not lead to the discontinuation of long-term opioid therapy in SCD patients.
“We need to better understand how long-term opioid use affects pain sensitization and determine if certain people are more sensitive to these effects so we can prescribe the best treatment option for each individual patient,” Dr Carroll said. “We also need to learn more about how sickle cell disease may sensitize the nervous system.” ![]()

and a normal one
Image by Betty Pace
Results of a small study suggest that long-term opioid treatment may not be the best option for pain management in adults with sickle cell disease (SCD).
The study showed that patients who received opioids long-term often fared worse in measures of pain, fatigue, and curtailed daily activities than patients who were not on long-term opioids.
Researchers reported these findings in the American Journal of Preventive Medicine.
“We need to be careful and skeptical about giving increasing doses of opioids to patients with sickle cell disease who are in chronic pain if it isn’t effective,” said study author C. Patrick Carroll, MD, of the Johns Hopkins University School of Medicine in Baltimore, Maryland.
“Too little is known about the effects of long-term opioid management of chronic pain.”
For this study, Dr Carroll and his colleagues enrolled 83 SCD patients—57 women and 26 men. All were 18 and older, and their average age was 39.
Twenty-nine of the patients had been prescribed daily, long-acting opioids to manage their pain. The remaining 54 patients weren’t on long-term opioids.
The patients filled out daily electronic pain diaries for 90 days. Self-reported levels of pain, physical activity, fatigue, and pain-related daily activity interference were recorded, along with self-reported levels of pain relief and medication satisfaction on a scale of 0 to 100.
Crises, pain, and fatigue
The proportion of days in vaso-occlusive crisis was significantly higher for patients who were on long-term opioid therapy than for those who were not—29% and 11.9%, respectively (P<0.01).
Patients on long-term opioids also reported significantly higher levels of crisis pain—60.6 and 41.0, respectively (P<0.001)—and non-crisis pain—34.5 and 10.3, respectively (P<0.001).
Patients on long-term opioid therapy had higher levels of pain-related activity interference, both on non-crisis days—24.9 and 7.4, respectively (P<0.001)—and crisis days—56.7 and 37.7, respectively (P<0.01).
And patients on long-term opioid therapy had higher levels of fatigue on non-crisis days—49.7 and 27.0, respectively (P<0.001)—and crisis days—66.1 and 53.0, respectively (P<0.05).
Central sensitization
The researchers also performed some standard measures of pain processing on the test subjects, which measured and averaged variables such as how intensely participants experienced unpleasant heat and pressure.
The team was particularly interested in the phenomenon of central sensitization, in which the central nervous system amplifies painful sensations.
Central sensitization may be one way that opioids can increase pain sensitivity, and it also may play a role in how SCD causes chronic pain, Dr Carroll said.
For example, one such measure of central sensitization uses repeated pokes from a mildly painful stimulus in succession. In people who have this hypersensitization, each poke is perceived as more intense than the last because the nervous system becomes progressively more sensitive to the pain.
Combining the data from several measures of central sensitization, the researchers used a scoring system that sets a normal measurement at 0 and rates how abnormal something is by how far the values move away from 0. They calculated a central sensitization index for patients on long-term opioids and those not taking them.
Overall, patients on long-term opioid therapy showed higher levels of central sensitization, with an index of 0.34, than those who were not on opioids, with an index of -0.10.
In patients who were not on long-term opioid therapy, the level of central sensitization correlated with the level of non-crisis pain. However, in patients who were taking long-term opioid therapy and also had higher levels of central sensitization and clinical pain, the correlation essentially vanished.
Dr Carroll said this was surprising and suggests the mechanisms of pain in SCD patients on long-term opioid therapy may be different from patients who don’t take daily opioids for pain.
Dr Carroll cautioned that this work is preliminary and should not lead to the discontinuation of long-term opioid therapy in SCD patients.
“We need to better understand how long-term opioid use affects pain sensitization and determine if certain people are more sensitive to these effects so we can prescribe the best treatment option for each individual patient,” Dr Carroll said. “We also need to learn more about how sickle cell disease may sensitize the nervous system.”
ESA benefits lower-risk MDS patients

COPENHAGEN—The erythropoiesis-stimulating agent (ESA) darbepoetin alfa can provide a clinical benefit in patients with lower-risk myelodysplastic syndromes (MDS), a phase 3 trial suggests.
In the ARCADE trial, darbepoetin alfa significantly reduced the incidence of red blood cell (RBC) transfusions in patients with low- and intermediate-1 risk myelodysplastic syndrome (MDS), when compared to placebo.
The ESA also significantly improved erythroid response.
In addition, researchers said adverse events (AEs) were generally balanced between the darbepoetin alfa and placebo arms.
Uwe Platzbecker, MD, of University Hospital Carl Gustav Carus Dresden in Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S128). The ARCADE trial was sponsored by Amgen.
Dr Platzbecker noted that, although ESAs are recommended in clinical guidelines to treat anemia in patients with lower-risk MDS, the drugs are not widely approved for this indication.
So, in the ARCADE trial, he and his colleagues assessed darbepoetin alfa in patients with low- or intermediate-1 risk MDS who had not previously taken ESAs or biologic response modifiers.
The patients had hemoglobin levels ≤10 g/dL, endogenous erythropoietin levels ≤500 mU/mL, and low transfusion burden (<4 RBC units in each of 2 consecutive 8-week periods prior to randomization).
During a 24-week period, 147 patients received either darbepoetin alfa at 500 μg (n=97) or placebo (n=49) every 3 weeks. The ESA dose was withheld if patients’ hemoglobin was >12.0 g/dL and decreased if hemoglobin increased by >1.5 g/dL in 3 weeks without transfusion.
At week 25, when the primary and key secondary endpoints were assessed, patients underwent an end-of-treatment period visit. They could then enter a 48-week active treatment period and cross over to receive darbepoetin alfa, with dose escalation allowed beginning on week 31. Treatment continued until week 72 or 73, and patients continue to be assessed every 26 weeks, for a minimum of 3 years.
Patient characteristics
Dr Platzbecker said baseline demographic and disease characteristics were generally similar between the treatment arms. All patients were Caucasian, and about 55% were male. The median age was 74 (range, 67-79). About half of patients in each treatment arm belonged to the low-risk IPSS category.
In both arms, most patients had refractory cytopenia with multilineage dysplasia (38.8% in the placebo arm and 46.4% in the darbepoetin alfa arm). Patients also had refractory anemia with excess blasts-1 (20.4% and 13.4%, respectively), refractory anemia (26.5% and 9.3%), refractory anemia with ring sideroblasts (8.2% and 17.5%), 5q deletion (4.1% and 11.3%), unclassifiable MDS (2.0% and 1.0%), and MDS of an unknown type (0% and 1.0%).
In the 16 weeks before randomization, 58.2% of all patients—53.1% in the placebo arm and 60.8% in the darbepoetin alfa arm—did not have any RBC transfusions. About 25% (24.7%)—22.4% in the placebo arm and 25.8% in the darbepoetin alfa arm—received 1 to 3 RBC units. And 17.1%—24.5% in the placebo arm and 13.4% in the darbepoetin alfa arm—received 4 or more RBC units.
Dosing
During the 24-week double-blind period of the study, 77% (37/48) of patients in the placebo arm and 79% (77/98) in the darbepoetin alfa arm received all 8 doses of treatment.
Sixteen percent (n=16) of patients in the darbepoetin alfa arm had a single dose reduction, and 2% (n=2) had 2 dose reductions. None of the patients in the placebo arm had a dose reduction.
Eleven percent of patients in the darbepoetin alfa arm had doses withheld due to increased hemoglobin. The dose was withheld once for 6 patients, twice for 4 patients, and 3 times for 1 patient. None of the placebo-treated patients had a dose withheld for this reason.
Ten percent (n=5) of placebo-treated patients and 2% (n=2) of darbepoetin alfa-treated patients had a dose withheld due to an AE. Two percent (n=1) and 3% (n=3) of patients, respectively, had a dose withheld for “other” reasons (noncompliance, investigator decision, and no investigational product on site).
During the 48-week open-label period of the study, 81% (102/126) of patients who received darbepoetin alfa increased their dose frequency from every 3 weeks to every 2 weeks. Dr Platzbecker said this suggests the optimal dose of the drug was not achieved during the 24-week double-blind period of the study.
Efficacy
During the 24-week double-blind period, there was a significant difference between the treatment arms with regard to RBC transfusions. The transfusion incidence was 59.2% (29/49) in the placebo arm and 36.1% (35/97) in the darbepoetin alfa arm (P=0.008).
During the 48-week open-label period, the incidence of RBC transfusion was 50.8% (64/126) among patients receiving darbepoetin alfa.
During the 24-week double-blind period, 11 patients (14.7%) in the darbepoetin alfa arm had an erythroid hematologic improvement (HI-E), but none of the patients in the placebo arm had such an improvement.
All 11 patients with HI-E had a baseline serum erythropoietin level less than 100 mU/mL, 1 of the patients had 2 RBC units transfused in the 16 weeks prior to randomization, but none had transfusions in the 8 weeks prior to randomization. Four of the patients had a dose withheld due to having hemoglobin levels greater than 12 g/dL.
During the 48-week open-label period, the HI-E rate was 34.7% (34/98) among patients receiving darbepoetin alfa.
Dr Platzbecker said the nature of the HI-E criteria likely underestimated the clinical benefit of darbepoetin alfa in this trial, and this was further complicated by the trial design. Specifically, hemoglobin was measured every 3 weeks, some patients may have had their doses reduced even if they were still anemic, and the optimal dose of darbepoetin alfa was likely not given during the double-blind period (as evidenced by the increase in doses during the open-label period).
For these reasons, Dr Platzbecker and his colleagues are exploring alternative response analyses to determine if there were additional patients who received a clinical benefit from darbepoetin alfa but did not meet HI-E criteria.
Safety
During the 24-week double-blind period, 4.2% (n=2) of patients in the placebo arm and 3.1% (n=3) in the darbepoetin alfa arm had AEs that led to treatment discontinuation. In the placebo arm, these events were pulmonary hypertension and renal failure. In the darbepoetin alfa arm, the events were pulmonary thrombosis, thrombocytopenia, and increased blast cell count.
The incidence of grade 3 or higher AEs was 27.1% (n=13) in the placebo arm and 15.3% (n=15) in the darbepoetin alfa arm. The incidence of grade 4 or higher AEs was 12.5% (n=6) and 5.1% (n=5), respectively. And the incidence of serious AEs was 16.7% (n=8) and 11.2% (n=11), respectively.
The incidence of fatal AEs was 4.2% (n=2) and 1% (n=1), respectively, but none of these were treatment-related. The deaths in the placebo arm were due to cardiac failure and cerebral hemorrhage, while the death in the darbepoetin alfa arm was due to hemorrhagic proctitis.
One patient in the darbepoetin alfa arm experienced a treatment-related serious AE.
AEs occurring at least 5% more frequently in the darbepoetin alfa arm than the placebo arm were fatigue (17.3% and 8.3%), pyrexia (9.2% and 2.1%), headache (7.1% and 2.1%), and myalgia (5.1% and 0%).
During the 48-week double-blind period, 7.9% (n=3) of patients formerly in the placebo arm and 3.4% (n=3) of patients formerly in the darbepoetin alfa arm had AEs that led to treatment discontinuation.
The incidence of grade 3 or higher AEs was 23.7% (n=9) and 31.0% (n=27), respectively. The incidence of grade 4 or higher AEs was 10.5% (n=4) and 10.3% (n=9), respectively. And the incidence of serious AEs was 18.4% (n=7) and 25.3% (n=22), respectively.
The incidence of fatal AEs was 2.6% (n=1) and 1.1% (n=1), respectively, but none of these were treatment-related. Two patients experienced a treatment-related serious AE—1 from each of the former treatment arms.

COPENHAGEN—The erythropoiesis-stimulating agent (ESA) darbepoetin alfa can provide a clinical benefit in patients with lower-risk myelodysplastic syndromes (MDS), a phase 3 trial suggests.
In the ARCADE trial, darbepoetin alfa significantly reduced the incidence of red blood cell (RBC) transfusions in patients with low- and intermediate-1 risk myelodysplastic syndrome (MDS), when compared to placebo.
The ESA also significantly improved erythroid response.
In addition, researchers said adverse events (AEs) were generally balanced between the darbepoetin alfa and placebo arms.
Uwe Platzbecker, MD, of University Hospital Carl Gustav Carus Dresden in Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S128). The ARCADE trial was sponsored by Amgen.
Dr Platzbecker noted that, although ESAs are recommended in clinical guidelines to treat anemia in patients with lower-risk MDS, the drugs are not widely approved for this indication.
So, in the ARCADE trial, he and his colleagues assessed darbepoetin alfa in patients with low- or intermediate-1 risk MDS who had not previously taken ESAs or biologic response modifiers.
The patients had hemoglobin levels ≤10 g/dL, endogenous erythropoietin levels ≤500 mU/mL, and low transfusion burden (<4 RBC units in each of 2 consecutive 8-week periods prior to randomization).
During a 24-week period, 147 patients received either darbepoetin alfa at 500 μg (n=97) or placebo (n=49) every 3 weeks. The ESA dose was withheld if patients’ hemoglobin was >12.0 g/dL and decreased if hemoglobin increased by >1.5 g/dL in 3 weeks without transfusion.
At week 25, when the primary and key secondary endpoints were assessed, patients underwent an end-of-treatment period visit. They could then enter a 48-week active treatment period and cross over to receive darbepoetin alfa, with dose escalation allowed beginning on week 31. Treatment continued until week 72 or 73, and patients continue to be assessed every 26 weeks, for a minimum of 3 years.
Patient characteristics
Dr Platzbecker said baseline demographic and disease characteristics were generally similar between the treatment arms. All patients were Caucasian, and about 55% were male. The median age was 74 (range, 67-79). About half of patients in each treatment arm belonged to the low-risk IPSS category.
In both arms, most patients had refractory cytopenia with multilineage dysplasia (38.8% in the placebo arm and 46.4% in the darbepoetin alfa arm). Patients also had refractory anemia with excess blasts-1 (20.4% and 13.4%, respectively), refractory anemia (26.5% and 9.3%), refractory anemia with ring sideroblasts (8.2% and 17.5%), 5q deletion (4.1% and 11.3%), unclassifiable MDS (2.0% and 1.0%), and MDS of an unknown type (0% and 1.0%).
In the 16 weeks before randomization, 58.2% of all patients—53.1% in the placebo arm and 60.8% in the darbepoetin alfa arm—did not have any RBC transfusions. About 25% (24.7%)—22.4% in the placebo arm and 25.8% in the darbepoetin alfa arm—received 1 to 3 RBC units. And 17.1%—24.5% in the placebo arm and 13.4% in the darbepoetin alfa arm—received 4 or more RBC units.
Dosing
During the 24-week double-blind period of the study, 77% (37/48) of patients in the placebo arm and 79% (77/98) in the darbepoetin alfa arm received all 8 doses of treatment.
Sixteen percent (n=16) of patients in the darbepoetin alfa arm had a single dose reduction, and 2% (n=2) had 2 dose reductions. None of the patients in the placebo arm had a dose reduction.
Eleven percent of patients in the darbepoetin alfa arm had doses withheld due to increased hemoglobin. The dose was withheld once for 6 patients, twice for 4 patients, and 3 times for 1 patient. None of the placebo-treated patients had a dose withheld for this reason.
Ten percent (n=5) of placebo-treated patients and 2% (n=2) of darbepoetin alfa-treated patients had a dose withheld due to an AE. Two percent (n=1) and 3% (n=3) of patients, respectively, had a dose withheld for “other” reasons (noncompliance, investigator decision, and no investigational product on site).
During the 48-week open-label period of the study, 81% (102/126) of patients who received darbepoetin alfa increased their dose frequency from every 3 weeks to every 2 weeks. Dr Platzbecker said this suggests the optimal dose of the drug was not achieved during the 24-week double-blind period of the study.
Efficacy
During the 24-week double-blind period, there was a significant difference between the treatment arms with regard to RBC transfusions. The transfusion incidence was 59.2% (29/49) in the placebo arm and 36.1% (35/97) in the darbepoetin alfa arm (P=0.008).
During the 48-week open-label period, the incidence of RBC transfusion was 50.8% (64/126) among patients receiving darbepoetin alfa.
During the 24-week double-blind period, 11 patients (14.7%) in the darbepoetin alfa arm had an erythroid hematologic improvement (HI-E), but none of the patients in the placebo arm had such an improvement.
All 11 patients with HI-E had a baseline serum erythropoietin level less than 100 mU/mL, 1 of the patients had 2 RBC units transfused in the 16 weeks prior to randomization, but none had transfusions in the 8 weeks prior to randomization. Four of the patients had a dose withheld due to having hemoglobin levels greater than 12 g/dL.
During the 48-week open-label period, the HI-E rate was 34.7% (34/98) among patients receiving darbepoetin alfa.
Dr Platzbecker said the nature of the HI-E criteria likely underestimated the clinical benefit of darbepoetin alfa in this trial, and this was further complicated by the trial design. Specifically, hemoglobin was measured every 3 weeks, some patients may have had their doses reduced even if they were still anemic, and the optimal dose of darbepoetin alfa was likely not given during the double-blind period (as evidenced by the increase in doses during the open-label period).
For these reasons, Dr Platzbecker and his colleagues are exploring alternative response analyses to determine if there were additional patients who received a clinical benefit from darbepoetin alfa but did not meet HI-E criteria.
Safety
During the 24-week double-blind period, 4.2% (n=2) of patients in the placebo arm and 3.1% (n=3) in the darbepoetin alfa arm had AEs that led to treatment discontinuation. In the placebo arm, these events were pulmonary hypertension and renal failure. In the darbepoetin alfa arm, the events were pulmonary thrombosis, thrombocytopenia, and increased blast cell count.
The incidence of grade 3 or higher AEs was 27.1% (n=13) in the placebo arm and 15.3% (n=15) in the darbepoetin alfa arm. The incidence of grade 4 or higher AEs was 12.5% (n=6) and 5.1% (n=5), respectively. And the incidence of serious AEs was 16.7% (n=8) and 11.2% (n=11), respectively.
The incidence of fatal AEs was 4.2% (n=2) and 1% (n=1), respectively, but none of these were treatment-related. The deaths in the placebo arm were due to cardiac failure and cerebral hemorrhage, while the death in the darbepoetin alfa arm was due to hemorrhagic proctitis.
One patient in the darbepoetin alfa arm experienced a treatment-related serious AE.
AEs occurring at least 5% more frequently in the darbepoetin alfa arm than the placebo arm were fatigue (17.3% and 8.3%), pyrexia (9.2% and 2.1%), headache (7.1% and 2.1%), and myalgia (5.1% and 0%).
During the 48-week double-blind period, 7.9% (n=3) of patients formerly in the placebo arm and 3.4% (n=3) of patients formerly in the darbepoetin alfa arm had AEs that led to treatment discontinuation.
The incidence of grade 3 or higher AEs was 23.7% (n=9) and 31.0% (n=27), respectively. The incidence of grade 4 or higher AEs was 10.5% (n=4) and 10.3% (n=9), respectively. And the incidence of serious AEs was 18.4% (n=7) and 25.3% (n=22), respectively.
The incidence of fatal AEs was 2.6% (n=1) and 1.1% (n=1), respectively, but none of these were treatment-related. Two patients experienced a treatment-related serious AE—1 from each of the former treatment arms.

COPENHAGEN—The erythropoiesis-stimulating agent (ESA) darbepoetin alfa can provide a clinical benefit in patients with lower-risk myelodysplastic syndromes (MDS), a phase 3 trial suggests.
In the ARCADE trial, darbepoetin alfa significantly reduced the incidence of red blood cell (RBC) transfusions in patients with low- and intermediate-1 risk myelodysplastic syndrome (MDS), when compared to placebo.
The ESA also significantly improved erythroid response.
In addition, researchers said adverse events (AEs) were generally balanced between the darbepoetin alfa and placebo arms.
Uwe Platzbecker, MD, of University Hospital Carl Gustav Carus Dresden in Germany, presented these results at the 21st Congress of the European Hematology Association (abstract S128). The ARCADE trial was sponsored by Amgen.
Dr Platzbecker noted that, although ESAs are recommended in clinical guidelines to treat anemia in patients with lower-risk MDS, the drugs are not widely approved for this indication.
So, in the ARCADE trial, he and his colleagues assessed darbepoetin alfa in patients with low- or intermediate-1 risk MDS who had not previously taken ESAs or biologic response modifiers.
The patients had hemoglobin levels ≤10 g/dL, endogenous erythropoietin levels ≤500 mU/mL, and low transfusion burden (<4 RBC units in each of 2 consecutive 8-week periods prior to randomization).
During a 24-week period, 147 patients received either darbepoetin alfa at 500 μg (n=97) or placebo (n=49) every 3 weeks. The ESA dose was withheld if patients’ hemoglobin was >12.0 g/dL and decreased if hemoglobin increased by >1.5 g/dL in 3 weeks without transfusion.
At week 25, when the primary and key secondary endpoints were assessed, patients underwent an end-of-treatment period visit. They could then enter a 48-week active treatment period and cross over to receive darbepoetin alfa, with dose escalation allowed beginning on week 31. Treatment continued until week 72 or 73, and patients continue to be assessed every 26 weeks, for a minimum of 3 years.
Patient characteristics
Dr Platzbecker said baseline demographic and disease characteristics were generally similar between the treatment arms. All patients were Caucasian, and about 55% were male. The median age was 74 (range, 67-79). About half of patients in each treatment arm belonged to the low-risk IPSS category.
In both arms, most patients had refractory cytopenia with multilineage dysplasia (38.8% in the placebo arm and 46.4% in the darbepoetin alfa arm). Patients also had refractory anemia with excess blasts-1 (20.4% and 13.4%, respectively), refractory anemia (26.5% and 9.3%), refractory anemia with ring sideroblasts (8.2% and 17.5%), 5q deletion (4.1% and 11.3%), unclassifiable MDS (2.0% and 1.0%), and MDS of an unknown type (0% and 1.0%).
In the 16 weeks before randomization, 58.2% of all patients—53.1% in the placebo arm and 60.8% in the darbepoetin alfa arm—did not have any RBC transfusions. About 25% (24.7%)—22.4% in the placebo arm and 25.8% in the darbepoetin alfa arm—received 1 to 3 RBC units. And 17.1%—24.5% in the placebo arm and 13.4% in the darbepoetin alfa arm—received 4 or more RBC units.
Dosing
During the 24-week double-blind period of the study, 77% (37/48) of patients in the placebo arm and 79% (77/98) in the darbepoetin alfa arm received all 8 doses of treatment.
Sixteen percent (n=16) of patients in the darbepoetin alfa arm had a single dose reduction, and 2% (n=2) had 2 dose reductions. None of the patients in the placebo arm had a dose reduction.
Eleven percent of patients in the darbepoetin alfa arm had doses withheld due to increased hemoglobin. The dose was withheld once for 6 patients, twice for 4 patients, and 3 times for 1 patient. None of the placebo-treated patients had a dose withheld for this reason.
Ten percent (n=5) of placebo-treated patients and 2% (n=2) of darbepoetin alfa-treated patients had a dose withheld due to an AE. Two percent (n=1) and 3% (n=3) of patients, respectively, had a dose withheld for “other” reasons (noncompliance, investigator decision, and no investigational product on site).
During the 48-week open-label period of the study, 81% (102/126) of patients who received darbepoetin alfa increased their dose frequency from every 3 weeks to every 2 weeks. Dr Platzbecker said this suggests the optimal dose of the drug was not achieved during the 24-week double-blind period of the study.
Efficacy
During the 24-week double-blind period, there was a significant difference between the treatment arms with regard to RBC transfusions. The transfusion incidence was 59.2% (29/49) in the placebo arm and 36.1% (35/97) in the darbepoetin alfa arm (P=0.008).
During the 48-week open-label period, the incidence of RBC transfusion was 50.8% (64/126) among patients receiving darbepoetin alfa.
During the 24-week double-blind period, 11 patients (14.7%) in the darbepoetin alfa arm had an erythroid hematologic improvement (HI-E), but none of the patients in the placebo arm had such an improvement.
All 11 patients with HI-E had a baseline serum erythropoietin level less than 100 mU/mL, 1 of the patients had 2 RBC units transfused in the 16 weeks prior to randomization, but none had transfusions in the 8 weeks prior to randomization. Four of the patients had a dose withheld due to having hemoglobin levels greater than 12 g/dL.
During the 48-week open-label period, the HI-E rate was 34.7% (34/98) among patients receiving darbepoetin alfa.
Dr Platzbecker said the nature of the HI-E criteria likely underestimated the clinical benefit of darbepoetin alfa in this trial, and this was further complicated by the trial design. Specifically, hemoglobin was measured every 3 weeks, some patients may have had their doses reduced even if they were still anemic, and the optimal dose of darbepoetin alfa was likely not given during the double-blind period (as evidenced by the increase in doses during the open-label period).
For these reasons, Dr Platzbecker and his colleagues are exploring alternative response analyses to determine if there were additional patients who received a clinical benefit from darbepoetin alfa but did not meet HI-E criteria.
Safety
During the 24-week double-blind period, 4.2% (n=2) of patients in the placebo arm and 3.1% (n=3) in the darbepoetin alfa arm had AEs that led to treatment discontinuation. In the placebo arm, these events were pulmonary hypertension and renal failure. In the darbepoetin alfa arm, the events were pulmonary thrombosis, thrombocytopenia, and increased blast cell count.
The incidence of grade 3 or higher AEs was 27.1% (n=13) in the placebo arm and 15.3% (n=15) in the darbepoetin alfa arm. The incidence of grade 4 or higher AEs was 12.5% (n=6) and 5.1% (n=5), respectively. And the incidence of serious AEs was 16.7% (n=8) and 11.2% (n=11), respectively.
The incidence of fatal AEs was 4.2% (n=2) and 1% (n=1), respectively, but none of these were treatment-related. The deaths in the placebo arm were due to cardiac failure and cerebral hemorrhage, while the death in the darbepoetin alfa arm was due to hemorrhagic proctitis.
One patient in the darbepoetin alfa arm experienced a treatment-related serious AE.
AEs occurring at least 5% more frequently in the darbepoetin alfa arm than the placebo arm were fatigue (17.3% and 8.3%), pyrexia (9.2% and 2.1%), headache (7.1% and 2.1%), and myalgia (5.1% and 0%).
During the 48-week double-blind period, 7.9% (n=3) of patients formerly in the placebo arm and 3.4% (n=3) of patients formerly in the darbepoetin alfa arm had AEs that led to treatment discontinuation.
The incidence of grade 3 or higher AEs was 23.7% (n=9) and 31.0% (n=27), respectively. The incidence of grade 4 or higher AEs was 10.5% (n=4) and 10.3% (n=9), respectively. And the incidence of serious AEs was 18.4% (n=7) and 25.3% (n=22), respectively.
The incidence of fatal AEs was 2.6% (n=1) and 1.1% (n=1), respectively, but none of these were treatment-related. Two patients experienced a treatment-related serious AE—1 from each of the former treatment arms.
Blood test may aid diagnosis of HELLP

Photo by Nina Matthews
A blood test developed to diagnose a rare genetic blood cell disorder, atypical hemolytic uremic syndrome (aHUS), may also aid in the diagnosis of HELLP syndrome, a life-threatening high blood pressure condition that affects 1% of all pregnant women.
The study, based on blood samples from a small number of women, suggests that aHUS has similar underlying biochemistry to HELLP, which affects hemolysis, elevates liver enzymes, and causes a low platelet count. Both conditions have over activation of the alternative pathway of complement.
At present, no diagnostic blood or biomarker test exists to diagnose HELLP, which is thought to be a severe form of preeclampsia. The condition is diagnosed only by its symptoms.
Senior study author Robert Brodsky, MD, of Johns Hopkins, and his team developed the modified Ham test to diagnose aHUS, a genetic disorder in which abnormal blood clots form in small blood vessels in the kidneys. They published that work last year in Blood.
The two conditions share a number of traits, such as hemolysis, elevated liver enzymes, a low platelet count, kidney dysfunction, high blood pressure, and seizures. This led the investigators to believe that the modified Ham test could also help identify women with HELLP syndrome.
"The clinical implications from an obstetric point of view are potentially huge," said lead study author Arthur Vaught, MD, also of Johns Hopkins. "If this works, we can reduce pre-term deliveries, stays in the neonatal intensive care unit, and other complications for mothers and their babies."
The team analyzed serum samples from 14 women with classic or atypical HELLP syndrome, 7 with severe preeclampsia, 11 women with normal pregnancies, and 8 healthy nonpregnant women. All pregnant women were at least 23 weeks’ gestation, the point at which HELLP symptoms start to arise.
The team evaluated patient sera using terminal product of complement activation (C5b-9). They observed that women with classic or atypical HELLP had increased complement activation compared to nonpregnant controls.
Women with classic HELLP had an average cell killing of 34.3% compared with 26% in women with atypical HELLP, 5% in women with normal pregnancies, and3.3% in women who were not pregnant.
The investigators then added eculizumab to HELLP sera to see whether the agent could inhibit complement activation. They found that mixing HELLP serum with eculizumab-containing serum significantly decreased cell killing compared with HELLP serum alone.
The kill rate in women with classic or atypical HELLP decreased from 34% to 5% with eculizumab.
Eculizumab (Soliris), manufactured by Alexion Pharmaceuticals, is a monoclonal antibody approved by the US Food and Drug Administration for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and aHUS.
Further investigation is required to confirm these findings, but thus far, the investigators believe the modified Ham assay may assist in diagnosing the HELLP syndrome and corroborate its relationship to aHUS.
The current study by Vaught et al is published in Experimental Hematology.

Photo by Nina Matthews
A blood test developed to diagnose a rare genetic blood cell disorder, atypical hemolytic uremic syndrome (aHUS), may also aid in the diagnosis of HELLP syndrome, a life-threatening high blood pressure condition that affects 1% of all pregnant women.
The study, based on blood samples from a small number of women, suggests that aHUS has similar underlying biochemistry to HELLP, which affects hemolysis, elevates liver enzymes, and causes a low platelet count. Both conditions have over activation of the alternative pathway of complement.
At present, no diagnostic blood or biomarker test exists to diagnose HELLP, which is thought to be a severe form of preeclampsia. The condition is diagnosed only by its symptoms.
Senior study author Robert Brodsky, MD, of Johns Hopkins, and his team developed the modified Ham test to diagnose aHUS, a genetic disorder in which abnormal blood clots form in small blood vessels in the kidneys. They published that work last year in Blood.
The two conditions share a number of traits, such as hemolysis, elevated liver enzymes, a low platelet count, kidney dysfunction, high blood pressure, and seizures. This led the investigators to believe that the modified Ham test could also help identify women with HELLP syndrome.
"The clinical implications from an obstetric point of view are potentially huge," said lead study author Arthur Vaught, MD, also of Johns Hopkins. "If this works, we can reduce pre-term deliveries, stays in the neonatal intensive care unit, and other complications for mothers and their babies."
The team analyzed serum samples from 14 women with classic or atypical HELLP syndrome, 7 with severe preeclampsia, 11 women with normal pregnancies, and 8 healthy nonpregnant women. All pregnant women were at least 23 weeks’ gestation, the point at which HELLP symptoms start to arise.
The team evaluated patient sera using terminal product of complement activation (C5b-9). They observed that women with classic or atypical HELLP had increased complement activation compared to nonpregnant controls.
Women with classic HELLP had an average cell killing of 34.3% compared with 26% in women with atypical HELLP, 5% in women with normal pregnancies, and3.3% in women who were not pregnant.
The investigators then added eculizumab to HELLP sera to see whether the agent could inhibit complement activation. They found that mixing HELLP serum with eculizumab-containing serum significantly decreased cell killing compared with HELLP serum alone.
The kill rate in women with classic or atypical HELLP decreased from 34% to 5% with eculizumab.
Eculizumab (Soliris), manufactured by Alexion Pharmaceuticals, is a monoclonal antibody approved by the US Food and Drug Administration for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and aHUS.
Further investigation is required to confirm these findings, but thus far, the investigators believe the modified Ham assay may assist in diagnosing the HELLP syndrome and corroborate its relationship to aHUS.
The current study by Vaught et al is published in Experimental Hematology.

Photo by Nina Matthews
A blood test developed to diagnose a rare genetic blood cell disorder, atypical hemolytic uremic syndrome (aHUS), may also aid in the diagnosis of HELLP syndrome, a life-threatening high blood pressure condition that affects 1% of all pregnant women.
The study, based on blood samples from a small number of women, suggests that aHUS has similar underlying biochemistry to HELLP, which affects hemolysis, elevates liver enzymes, and causes a low platelet count. Both conditions have over activation of the alternative pathway of complement.
At present, no diagnostic blood or biomarker test exists to diagnose HELLP, which is thought to be a severe form of preeclampsia. The condition is diagnosed only by its symptoms.
Senior study author Robert Brodsky, MD, of Johns Hopkins, and his team developed the modified Ham test to diagnose aHUS, a genetic disorder in which abnormal blood clots form in small blood vessels in the kidneys. They published that work last year in Blood.
The two conditions share a number of traits, such as hemolysis, elevated liver enzymes, a low platelet count, kidney dysfunction, high blood pressure, and seizures. This led the investigators to believe that the modified Ham test could also help identify women with HELLP syndrome.
"The clinical implications from an obstetric point of view are potentially huge," said lead study author Arthur Vaught, MD, also of Johns Hopkins. "If this works, we can reduce pre-term deliveries, stays in the neonatal intensive care unit, and other complications for mothers and their babies."
The team analyzed serum samples from 14 women with classic or atypical HELLP syndrome, 7 with severe preeclampsia, 11 women with normal pregnancies, and 8 healthy nonpregnant women. All pregnant women were at least 23 weeks’ gestation, the point at which HELLP symptoms start to arise.
The team evaluated patient sera using terminal product of complement activation (C5b-9). They observed that women with classic or atypical HELLP had increased complement activation compared to nonpregnant controls.
Women with classic HELLP had an average cell killing of 34.3% compared with 26% in women with atypical HELLP, 5% in women with normal pregnancies, and3.3% in women who were not pregnant.
The investigators then added eculizumab to HELLP sera to see whether the agent could inhibit complement activation. They found that mixing HELLP serum with eculizumab-containing serum significantly decreased cell killing compared with HELLP serum alone.
The kill rate in women with classic or atypical HELLP decreased from 34% to 5% with eculizumab.
Eculizumab (Soliris), manufactured by Alexion Pharmaceuticals, is a monoclonal antibody approved by the US Food and Drug Administration for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and aHUS.
Further investigation is required to confirm these findings, but thus far, the investigators believe the modified Ham assay may assist in diagnosing the HELLP syndrome and corroborate its relationship to aHUS.
The current study by Vaught et al is published in Experimental Hematology.
HU improves lung function in young SCD patients

Photo courtesy of St. Jude
Children’s Research Hospital
SAN FRANCISCO—A new study has shown that hydroxyurea (HU) can improve lung function in young patients with sickle cell disease (SCD).
“Persons with sickle cell disease experience an annual decline in lung function that starts in childhood,” said study investigator Anya McLaren, MD, of The Hospital for Sick Children in Toronto, Ontario, Canada.
“This study is the first of its kind to look at the effect of hydroxyurea on lung function. We found that hydroxyurea improves annual pulmonary function decline in children with sickle cell disease by more than one-third.”
The study was presented at the ATS 2016 International Conference as abstract 7225.
For this study, Dr McLaren and her colleagues evaluated the effects of HU in 94 SCD patients. The patients’ average age at baseline was 11 (range, 6 to 20), 96% of patients had HbSS genotype, and 47% were male.
The patients were followed for 4 years after HU initiation. The investigators assessed lung function before and after HU initiation in a few ways.
They used the forced expiratory volume (FEV) test, which measures how much air a person can exhale during a forced breath. The amount of air can be measured during the first second of the forced breath (FEV1) and at later time points.
Forced vital capacity (FVC) is the total amount of air exhaled during the FEV test. If the FEV1/FVC ratio is less than 80%, it indicates that an obstructive defect is present.
The investigators also assessed FEF25-75, or the forced expiratory flow at 25%–75% of FVC. This measurement helps determine if there is an obstruction in the airway.
In addition, the team measured total lung capacity.
Results
The investigators found no significant change in total lung capacity, FVC, or FEV1/FVC predicted measurements after patients began receiving HU.
However, there were significant improvements in both FEV1 and FEF25-75 after treatment.
The annual rate of decline in predicted FEV1 and FEF25-75 before patients started HU was -1.98%/year (95% CI -2.57 to -1.39) and -3.59%/year (95% CI -4.43 to -2.75), respectively.
After HU treatment began, there was a significant (P<0.05) improvement in the annual decline, to -1.28%/year (95% CI -1.79 to -0.76) and -2.88%/year (95% CI -3.49 to -2.28), respectively.
The investigators noted that changes in FEV1 and FEF25-75 were independent of a patient’s age at baseline and the time from HU therapy initiation.
Dr McLaren pointed out that HU is underused in SCD patients, likely because clinicians are concerned about patient non-compliance and afraid of potential side effects, particularly carcinogenesis. But some of those fears may be unfounded, she said.
“Long-term observational studies suggest beneficial effects [of HU] without excessive damage to bone marrow, deleterious effects on growth and development, altered fertility, accumulation of mutations, or increased carcinogenicity,” Dr McLaren said.
“Evidence that lung function may be better preserved while on hydroxyurea may encourage compliance and adherence to this medication for patients with sickle cell disease. In combination with the established safety data, it hopefully will promote physician recommendations for hydroxyurea initiation and encouragement of compliance.”

Photo courtesy of St. Jude
Children’s Research Hospital
SAN FRANCISCO—A new study has shown that hydroxyurea (HU) can improve lung function in young patients with sickle cell disease (SCD).
“Persons with sickle cell disease experience an annual decline in lung function that starts in childhood,” said study investigator Anya McLaren, MD, of The Hospital for Sick Children in Toronto, Ontario, Canada.
“This study is the first of its kind to look at the effect of hydroxyurea on lung function. We found that hydroxyurea improves annual pulmonary function decline in children with sickle cell disease by more than one-third.”
The study was presented at the ATS 2016 International Conference as abstract 7225.
For this study, Dr McLaren and her colleagues evaluated the effects of HU in 94 SCD patients. The patients’ average age at baseline was 11 (range, 6 to 20), 96% of patients had HbSS genotype, and 47% were male.
The patients were followed for 4 years after HU initiation. The investigators assessed lung function before and after HU initiation in a few ways.
They used the forced expiratory volume (FEV) test, which measures how much air a person can exhale during a forced breath. The amount of air can be measured during the first second of the forced breath (FEV1) and at later time points.
Forced vital capacity (FVC) is the total amount of air exhaled during the FEV test. If the FEV1/FVC ratio is less than 80%, it indicates that an obstructive defect is present.
The investigators also assessed FEF25-75, or the forced expiratory flow at 25%–75% of FVC. This measurement helps determine if there is an obstruction in the airway.
In addition, the team measured total lung capacity.
Results
The investigators found no significant change in total lung capacity, FVC, or FEV1/FVC predicted measurements after patients began receiving HU.
However, there were significant improvements in both FEV1 and FEF25-75 after treatment.
The annual rate of decline in predicted FEV1 and FEF25-75 before patients started HU was -1.98%/year (95% CI -2.57 to -1.39) and -3.59%/year (95% CI -4.43 to -2.75), respectively.
After HU treatment began, there was a significant (P<0.05) improvement in the annual decline, to -1.28%/year (95% CI -1.79 to -0.76) and -2.88%/year (95% CI -3.49 to -2.28), respectively.
The investigators noted that changes in FEV1 and FEF25-75 were independent of a patient’s age at baseline and the time from HU therapy initiation.
Dr McLaren pointed out that HU is underused in SCD patients, likely because clinicians are concerned about patient non-compliance and afraid of potential side effects, particularly carcinogenesis. But some of those fears may be unfounded, she said.
“Long-term observational studies suggest beneficial effects [of HU] without excessive damage to bone marrow, deleterious effects on growth and development, altered fertility, accumulation of mutations, or increased carcinogenicity,” Dr McLaren said.
“Evidence that lung function may be better preserved while on hydroxyurea may encourage compliance and adherence to this medication for patients with sickle cell disease. In combination with the established safety data, it hopefully will promote physician recommendations for hydroxyurea initiation and encouragement of compliance.”

Photo courtesy of St. Jude
Children’s Research Hospital
SAN FRANCISCO—A new study has shown that hydroxyurea (HU) can improve lung function in young patients with sickle cell disease (SCD).
“Persons with sickle cell disease experience an annual decline in lung function that starts in childhood,” said study investigator Anya McLaren, MD, of The Hospital for Sick Children in Toronto, Ontario, Canada.
“This study is the first of its kind to look at the effect of hydroxyurea on lung function. We found that hydroxyurea improves annual pulmonary function decline in children with sickle cell disease by more than one-third.”
The study was presented at the ATS 2016 International Conference as abstract 7225.
For this study, Dr McLaren and her colleagues evaluated the effects of HU in 94 SCD patients. The patients’ average age at baseline was 11 (range, 6 to 20), 96% of patients had HbSS genotype, and 47% were male.
The patients were followed for 4 years after HU initiation. The investigators assessed lung function before and after HU initiation in a few ways.
They used the forced expiratory volume (FEV) test, which measures how much air a person can exhale during a forced breath. The amount of air can be measured during the first second of the forced breath (FEV1) and at later time points.
Forced vital capacity (FVC) is the total amount of air exhaled during the FEV test. If the FEV1/FVC ratio is less than 80%, it indicates that an obstructive defect is present.
The investigators also assessed FEF25-75, or the forced expiratory flow at 25%–75% of FVC. This measurement helps determine if there is an obstruction in the airway.
In addition, the team measured total lung capacity.
Results
The investigators found no significant change in total lung capacity, FVC, or FEV1/FVC predicted measurements after patients began receiving HU.
However, there were significant improvements in both FEV1 and FEF25-75 after treatment.
The annual rate of decline in predicted FEV1 and FEF25-75 before patients started HU was -1.98%/year (95% CI -2.57 to -1.39) and -3.59%/year (95% CI -4.43 to -2.75), respectively.
After HU treatment began, there was a significant (P<0.05) improvement in the annual decline, to -1.28%/year (95% CI -1.79 to -0.76) and -2.88%/year (95% CI -3.49 to -2.28), respectively.
The investigators noted that changes in FEV1 and FEF25-75 were independent of a patient’s age at baseline and the time from HU therapy initiation.
Dr McLaren pointed out that HU is underused in SCD patients, likely because clinicians are concerned about patient non-compliance and afraid of potential side effects, particularly carcinogenesis. But some of those fears may be unfounded, she said.
“Long-term observational studies suggest beneficial effects [of HU] without excessive damage to bone marrow, deleterious effects on growth and development, altered fertility, accumulation of mutations, or increased carcinogenicity,” Dr McLaren said.
“Evidence that lung function may be better preserved while on hydroxyurea may encourage compliance and adherence to this medication for patients with sickle cell disease. In combination with the established safety data, it hopefully will promote physician recommendations for hydroxyurea initiation and encouragement of compliance.”