User login
Uninsured population is big in Texas
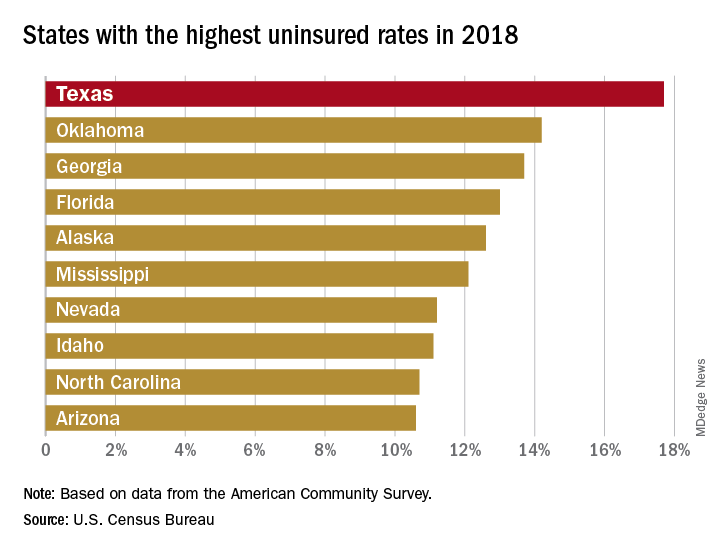
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.
There were just over 5 million uninsured people in the Lone Star State last year, representing an increase from 17.3% of the total population in 2017 to 17.7%, and that works out to an additional 186,000 residents with no health care coverage, the Census Bureau said in a recent report.
That 17.7% rate for 2018 gave Texas the highest proportion of uninsured population, putting it ahead of Oklahoma (14.2%), Georgia (13.7%), Florida (13.0%), Alaska (12.6%), and Mississippi (12.1%). Oklahoma had basically no change from 2017, while the other three each had a small but nonsignificant increase. Nationally, the rate of uninsured population went from 7.9% in 2017 to 8.5% in 2018, the Census Bureau investigators said.
On the other end of the coverage spectrum was Massachusetts, where only 2.8% of the population, or about 189,000 people, lacked health insurance in 2018. Washington, D.C., was next with an uninsured rate of 3.2%, followed by Vermont (4.0%), Hawaii (4.1%), Rhode Island (4.1%), and Minnesota (4.4%), they said, based on data from the American Community Survey.
A separate analysis of Census Bureau data by the personal finance website WalletHub showed that states that expanded Medicaid along with their Affordable Care Act implementation had an average uninsured rate of 7.0% in 2018, compared with 11.1% for states that did not expand eligibility.
All 50 states were in negative territory when changes in uninsured rates were calculated over a longer time period, 2010-2018, as the national rate fell by 6.6%. The largest drops among the states came in Nevada (–11.4%), California (–11.3%), Oregon (–10.1%), and New Mexico (–10.1%), while Massachusetts (–1.7%), Maine (–2.1%), and North Dakota (–2.5%) had the smallest declines, WalletHub reported.
Bringing focus to the issue: Dr. Elizabeth Loder on gender in medicine
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
koakes@mdedge.com
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
koakes@mdedge.com
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
koakes@mdedge.com
Court of Appeals to decide fate of Medicaid work requirements
The debate over whether states can impose work requirements on Medicaid recipients is now in the hands of a federal appeals court.
The U.S. Court of Appeals for the District of Columbia heard oral arguments Oct. 11, 2019, in two cases that challenge state waivers that require work as part of Medicaid eligibility.
In Stewart v. Azar, 16 patients from Kentucky are suing the Department of Health & Human Services over its approval of changes to Kentucky’s Medicaid program that include work requirements, premiums, and lockouts. In Gresham v. Azar, several Arkansas residents are challenging HHS over the approval of modifications to Arkansas’ Medicaid program that require work requirements and eliminate retroactive coverage.
The restrictive conditions in the Medicaid waivers would cause thousands of Medicaid enrollees to lose coverage, according to Jane Perkins, legal director for the National Health Law Program, an advocacy firm representing the plaintiffs.
“Section 1115 of the Social Security Act only allows the [HHS] Secretary to approve experimental projects that further Medicaid’s purpose of furnishing medical assistance to low-income people,” Ms. Perkins said in a statement. “These waiver projects do not further this objective. By the government’s own framing, they are intended to transform Medicaid and explode Medicaid expansion. Only Congress can rewrite a statute – not this administration. We hope the appellate court will uphold the well-reasoned opinions of the district court.”
HHS argues that it has the authority to allow any experimental, pilot, or demonstration project likely to promote the objectives of Medicaid, which in addition to medical assistance include rehabilitation services that help patients attain or retain independence or self-care. The waivers from Kentucky and Arkansas are consistent with these objectives, attorneys for HHS argued in court documents.
Kentucky’s waiver project promotes beneficiary health and financial independence, while Arkansas’ demonstration is likely to assist in improving health outcomes through strategies that promote community engagement and address health determinants, according to letters from the Centers for Medicare & Medicaid Service approving the projects.
Arkansas’ demonstration project, approved in March 2018, includes a requirement that adults aged 19-49 years complete 80 hours per month of community engagement activities, such as employment, education, job-skills training, or community service, as a condition of continued Medicaid eligibility. Kentucky’s proposal, approved in November 2018, requires Medicaid patients to spend at least 80 hours per month on qualified activities, including employment, job skills training, education, community services and/or participation in substance use disorder treatment.
Medicaid patients in both states sued HHS shortly after the waivers were approved, arguing that the work requirements were arbitrary and capricious and that the agency exceeded its statutory authority in approving the projects. The U.S. District Court for the District of Columbia ruled in favor of the patients in March 2019, finding that HHS failed to fully consider the impact of the Kentucky and Arkansas changes on current and future Medicaid beneficiaries. In a decision for Kentucky and a separate ruling for Arkansas, the court vacated HHS’ approval of the projects and remanded both waivers back to HHS for reconsideration. In the interim, officials in both Kentucky and Arkansas halted implementation of the work requirements. The Department of Justice appealed in both cases.
According to court documents, 18,000 Arkansans lost coverage for failure to comply with the work requirements before the regulations were halted. In Kentucky, the state estimates that 95,000 Kentuckians could lose coverage if the project goes into effect.
A decision by the appeals court is expected by December 2019.
The debate over whether states can impose work requirements on Medicaid recipients is now in the hands of a federal appeals court.
The U.S. Court of Appeals for the District of Columbia heard oral arguments Oct. 11, 2019, in two cases that challenge state waivers that require work as part of Medicaid eligibility.
In Stewart v. Azar, 16 patients from Kentucky are suing the Department of Health & Human Services over its approval of changes to Kentucky’s Medicaid program that include work requirements, premiums, and lockouts. In Gresham v. Azar, several Arkansas residents are challenging HHS over the approval of modifications to Arkansas’ Medicaid program that require work requirements and eliminate retroactive coverage.
The restrictive conditions in the Medicaid waivers would cause thousands of Medicaid enrollees to lose coverage, according to Jane Perkins, legal director for the National Health Law Program, an advocacy firm representing the plaintiffs.
“Section 1115 of the Social Security Act only allows the [HHS] Secretary to approve experimental projects that further Medicaid’s purpose of furnishing medical assistance to low-income people,” Ms. Perkins said in a statement. “These waiver projects do not further this objective. By the government’s own framing, they are intended to transform Medicaid and explode Medicaid expansion. Only Congress can rewrite a statute – not this administration. We hope the appellate court will uphold the well-reasoned opinions of the district court.”
HHS argues that it has the authority to allow any experimental, pilot, or demonstration project likely to promote the objectives of Medicaid, which in addition to medical assistance include rehabilitation services that help patients attain or retain independence or self-care. The waivers from Kentucky and Arkansas are consistent with these objectives, attorneys for HHS argued in court documents.
Kentucky’s waiver project promotes beneficiary health and financial independence, while Arkansas’ demonstration is likely to assist in improving health outcomes through strategies that promote community engagement and address health determinants, according to letters from the Centers for Medicare & Medicaid Service approving the projects.
Arkansas’ demonstration project, approved in March 2018, includes a requirement that adults aged 19-49 years complete 80 hours per month of community engagement activities, such as employment, education, job-skills training, or community service, as a condition of continued Medicaid eligibility. Kentucky’s proposal, approved in November 2018, requires Medicaid patients to spend at least 80 hours per month on qualified activities, including employment, job skills training, education, community services and/or participation in substance use disorder treatment.
Medicaid patients in both states sued HHS shortly after the waivers were approved, arguing that the work requirements were arbitrary and capricious and that the agency exceeded its statutory authority in approving the projects. The U.S. District Court for the District of Columbia ruled in favor of the patients in March 2019, finding that HHS failed to fully consider the impact of the Kentucky and Arkansas changes on current and future Medicaid beneficiaries. In a decision for Kentucky and a separate ruling for Arkansas, the court vacated HHS’ approval of the projects and remanded both waivers back to HHS for reconsideration. In the interim, officials in both Kentucky and Arkansas halted implementation of the work requirements. The Department of Justice appealed in both cases.
According to court documents, 18,000 Arkansans lost coverage for failure to comply with the work requirements before the regulations were halted. In Kentucky, the state estimates that 95,000 Kentuckians could lose coverage if the project goes into effect.
A decision by the appeals court is expected by December 2019.
The debate over whether states can impose work requirements on Medicaid recipients is now in the hands of a federal appeals court.
The U.S. Court of Appeals for the District of Columbia heard oral arguments Oct. 11, 2019, in two cases that challenge state waivers that require work as part of Medicaid eligibility.
In Stewart v. Azar, 16 patients from Kentucky are suing the Department of Health & Human Services over its approval of changes to Kentucky’s Medicaid program that include work requirements, premiums, and lockouts. In Gresham v. Azar, several Arkansas residents are challenging HHS over the approval of modifications to Arkansas’ Medicaid program that require work requirements and eliminate retroactive coverage.
The restrictive conditions in the Medicaid waivers would cause thousands of Medicaid enrollees to lose coverage, according to Jane Perkins, legal director for the National Health Law Program, an advocacy firm representing the plaintiffs.
“Section 1115 of the Social Security Act only allows the [HHS] Secretary to approve experimental projects that further Medicaid’s purpose of furnishing medical assistance to low-income people,” Ms. Perkins said in a statement. “These waiver projects do not further this objective. By the government’s own framing, they are intended to transform Medicaid and explode Medicaid expansion. Only Congress can rewrite a statute – not this administration. We hope the appellate court will uphold the well-reasoned opinions of the district court.”
HHS argues that it has the authority to allow any experimental, pilot, or demonstration project likely to promote the objectives of Medicaid, which in addition to medical assistance include rehabilitation services that help patients attain or retain independence or self-care. The waivers from Kentucky and Arkansas are consistent with these objectives, attorneys for HHS argued in court documents.
Kentucky’s waiver project promotes beneficiary health and financial independence, while Arkansas’ demonstration is likely to assist in improving health outcomes through strategies that promote community engagement and address health determinants, according to letters from the Centers for Medicare & Medicaid Service approving the projects.
Arkansas’ demonstration project, approved in March 2018, includes a requirement that adults aged 19-49 years complete 80 hours per month of community engagement activities, such as employment, education, job-skills training, or community service, as a condition of continued Medicaid eligibility. Kentucky’s proposal, approved in November 2018, requires Medicaid patients to spend at least 80 hours per month on qualified activities, including employment, job skills training, education, community services and/or participation in substance use disorder treatment.
Medicaid patients in both states sued HHS shortly after the waivers were approved, arguing that the work requirements were arbitrary and capricious and that the agency exceeded its statutory authority in approving the projects. The U.S. District Court for the District of Columbia ruled in favor of the patients in March 2019, finding that HHS failed to fully consider the impact of the Kentucky and Arkansas changes on current and future Medicaid beneficiaries. In a decision for Kentucky and a separate ruling for Arkansas, the court vacated HHS’ approval of the projects and remanded both waivers back to HHS for reconsideration. In the interim, officials in both Kentucky and Arkansas halted implementation of the work requirements. The Department of Justice appealed in both cases.
According to court documents, 18,000 Arkansans lost coverage for failure to comply with the work requirements before the regulations were halted. In Kentucky, the state estimates that 95,000 Kentuckians could lose coverage if the project goes into effect.
A decision by the appeals court is expected by December 2019.
#MyFirstNameIsDoctor: Why it matters, and what you can do
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
Changes to public charge rule blocked by courts
In three separate decisions, the U.S. District Court for the Southern District of New York, the U.S. District Court for the Northern District of California, and the U.S. District Court for the Eastern District of Washington temporarily barred the administration’s changes to the public charge rule from moving forward. The judges said lawsuits challenging the rule are likely to prevail in court.
The injunctions are much needed to protect patients and families, said R. Shawn Martin, senior vice president of advocacy, practice advancement, and policy for the American Academy of Family Physicians.
“The court decisions are important,” Mr. Martin said in an interview. “The AAFP believes that the public charge rule, as proposed by the administration, would have an immediate and negative impact on the health of thousands of people, including children. There is evidence that policies such as this create a culture where patients forgo interactions with the health care system out of fear. We should never be a country that compromises the health and well-being of individuals, especially those that are most vulnerable.”
White House Press Secretary Stephanie Grisham called the court rulings extremely disappointing and said the recent changes to the public charge rule restore integrity to the immigration system.
“The rulings today prevent our nation’s immigration officers from ensuring that immigrants seeking entry to the United States will be self-sufficient and instead allow noncitizens to continue taking advantage of our generous but limited public resources reserved for vulnerable Americans,” Ms. Graham said in a statement. “These injunctions are the latest inexplicable example of the administration being ordered to comply with the flawed or lawless guidance of a previous administration instead of the actual laws passed by Congress.”
Under the longstanding public charge rule, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation, which was scheduled to take effect on Oct. 15, 2019, would allow officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program, and several housing programs. The revised regulation would continue to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued in Washington state by 14 states. On Oct. 11, Judge Rosanna Malouf Peterson, U.S. district judge for the Eastern District of Washington, issued a nationwide ban of the revised public charge regulation, ruling that the plaintiff states will suffer irreparable harm if the rule moves forward.
“The plaintiff states have shown a significant threat of irreparable injury as a result of the impending enactment of the public charge rule by numerous individuals disenrolling from benefits for which they or their relatives were qualified, out of fear or confusion, that accepting those noncash public benefits will deprive them of an opportunity for legal permanent residency,” Judge Peterson wrote in her decision. “The plaintiff states have further demonstrated how that chilling effect predictably would cause irreparable injury by creating long-term costs to the plaintiff states from providing ongoing triage for residents who have missed opportunities for timely diagnoses, vaccinations, or building a strong foundation in childhood that will allow U.S. citizen children and future U.S. citizens to flourish and contribute to their communities as taxpaying adults.”
Judge Phyllis J. Hamilton, U.S. district judge for the Northern District of California, ruled similarly on Oct. 11, as did George Benjamin Daniels of the U.S. District Court for the Southern District of New York.
Physician associations previously voiced opposition to the administration’s changes to the public charge rule. In a joint statement, the AAFP, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the American College of Physicians, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
In three separate decisions, the U.S. District Court for the Southern District of New York, the U.S. District Court for the Northern District of California, and the U.S. District Court for the Eastern District of Washington temporarily barred the administration’s changes to the public charge rule from moving forward. The judges said lawsuits challenging the rule are likely to prevail in court.
The injunctions are much needed to protect patients and families, said R. Shawn Martin, senior vice president of advocacy, practice advancement, and policy for the American Academy of Family Physicians.
“The court decisions are important,” Mr. Martin said in an interview. “The AAFP believes that the public charge rule, as proposed by the administration, would have an immediate and negative impact on the health of thousands of people, including children. There is evidence that policies such as this create a culture where patients forgo interactions with the health care system out of fear. We should never be a country that compromises the health and well-being of individuals, especially those that are most vulnerable.”
White House Press Secretary Stephanie Grisham called the court rulings extremely disappointing and said the recent changes to the public charge rule restore integrity to the immigration system.
“The rulings today prevent our nation’s immigration officers from ensuring that immigrants seeking entry to the United States will be self-sufficient and instead allow noncitizens to continue taking advantage of our generous but limited public resources reserved for vulnerable Americans,” Ms. Graham said in a statement. “These injunctions are the latest inexplicable example of the administration being ordered to comply with the flawed or lawless guidance of a previous administration instead of the actual laws passed by Congress.”
Under the longstanding public charge rule, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation, which was scheduled to take effect on Oct. 15, 2019, would allow officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program, and several housing programs. The revised regulation would continue to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued in Washington state by 14 states. On Oct. 11, Judge Rosanna Malouf Peterson, U.S. district judge for the Eastern District of Washington, issued a nationwide ban of the revised public charge regulation, ruling that the plaintiff states will suffer irreparable harm if the rule moves forward.
“The plaintiff states have shown a significant threat of irreparable injury as a result of the impending enactment of the public charge rule by numerous individuals disenrolling from benefits for which they or their relatives were qualified, out of fear or confusion, that accepting those noncash public benefits will deprive them of an opportunity for legal permanent residency,” Judge Peterson wrote in her decision. “The plaintiff states have further demonstrated how that chilling effect predictably would cause irreparable injury by creating long-term costs to the plaintiff states from providing ongoing triage for residents who have missed opportunities for timely diagnoses, vaccinations, or building a strong foundation in childhood that will allow U.S. citizen children and future U.S. citizens to flourish and contribute to their communities as taxpaying adults.”
Judge Phyllis J. Hamilton, U.S. district judge for the Northern District of California, ruled similarly on Oct. 11, as did George Benjamin Daniels of the U.S. District Court for the Southern District of New York.
Physician associations previously voiced opposition to the administration’s changes to the public charge rule. In a joint statement, the AAFP, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the American College of Physicians, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
In three separate decisions, the U.S. District Court for the Southern District of New York, the U.S. District Court for the Northern District of California, and the U.S. District Court for the Eastern District of Washington temporarily barred the administration’s changes to the public charge rule from moving forward. The judges said lawsuits challenging the rule are likely to prevail in court.
The injunctions are much needed to protect patients and families, said R. Shawn Martin, senior vice president of advocacy, practice advancement, and policy for the American Academy of Family Physicians.
“The court decisions are important,” Mr. Martin said in an interview. “The AAFP believes that the public charge rule, as proposed by the administration, would have an immediate and negative impact on the health of thousands of people, including children. There is evidence that policies such as this create a culture where patients forgo interactions with the health care system out of fear. We should never be a country that compromises the health and well-being of individuals, especially those that are most vulnerable.”
White House Press Secretary Stephanie Grisham called the court rulings extremely disappointing and said the recent changes to the public charge rule restore integrity to the immigration system.
“The rulings today prevent our nation’s immigration officers from ensuring that immigrants seeking entry to the United States will be self-sufficient and instead allow noncitizens to continue taking advantage of our generous but limited public resources reserved for vulnerable Americans,” Ms. Graham said in a statement. “These injunctions are the latest inexplicable example of the administration being ordered to comply with the flawed or lawless guidance of a previous administration instead of the actual laws passed by Congress.”
Under the longstanding public charge rule, officials can refuse to admit immigrants into the United States – or to adjust their legal status – if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation, which was scheduled to take effect on Oct. 15, 2019, would allow officials to consider previously excluded programs in their determination, including nonemergency Medicaid for nonpregnant adults, the Supplemental Nutrition Assistance Program, and several housing programs. The revised regulation would continue to allow immigrants to access emergency medical care and disaster relief without public charge repercussions.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued in Washington state by 14 states. On Oct. 11, Judge Rosanna Malouf Peterson, U.S. district judge for the Eastern District of Washington, issued a nationwide ban of the revised public charge regulation, ruling that the plaintiff states will suffer irreparable harm if the rule moves forward.
“The plaintiff states have shown a significant threat of irreparable injury as a result of the impending enactment of the public charge rule by numerous individuals disenrolling from benefits for which they or their relatives were qualified, out of fear or confusion, that accepting those noncash public benefits will deprive them of an opportunity for legal permanent residency,” Judge Peterson wrote in her decision. “The plaintiff states have further demonstrated how that chilling effect predictably would cause irreparable injury by creating long-term costs to the plaintiff states from providing ongoing triage for residents who have missed opportunities for timely diagnoses, vaccinations, or building a strong foundation in childhood that will allow U.S. citizen children and future U.S. citizens to flourish and contribute to their communities as taxpaying adults.”
Judge Phyllis J. Hamilton, U.S. district judge for the Northern District of California, ruled similarly on Oct. 11, as did George Benjamin Daniels of the U.S. District Court for the Southern District of New York.
Physician associations previously voiced opposition to the administration’s changes to the public charge rule. In a joint statement, the AAFP, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the American College of Physicians, and the American Psychiatric Association expressed concern that the new regulation will discourage immigrants from seeking needed health care since such assistance may be used to deny green cards and visas, or even lead to deportations.
“Rather than face that threat, impacted patients currently served by our members almost certainly will avoid needed care from their trusted physicians, jeopardizing their own health and that of their communities,” the medical societies stated. “Many of our members have already witnessed this chilling effect among their own patient populations, with patients avoiding health services and programs out of fear.”
When can I retire?
Whenever Don McLean is asked what the lyrics to his iconic song “American Pie” mean, he answers: “They mean that I don’t have to work anymore.”
It would be nice if those of us who have never written an enigmatic hit tune could receive an unequivocal signal when it’s safe to retire. Unfortunately, the road to retirement is fraught with challenges, not least of which is locating the right off-ramp.
We tend to live longer than planned, so we run the risk of outliving our savings, which are often underfunded to begin with. And we don’t face facts about end-of-life care. Few of us have long-term care insurance, or the means to self-fund an extended long-term care situation, as I will discuss next month.
Many of us lack a clear idea of where our retirement income will come from, or if it will be there when we arrive. Doctors in particular are notorious for mismanaging their investments. Many try to self-manage retirement plans and personal savings without adequate time or knowledge to do it right. Involving a qualified financial professional is usually a far better strategy than going it alone.
So, As with everything else, it depends; but to arrive at any sort of reliable ballpark figure, you’ll need to know three things: how much you realistically expect to spend annually after retirement; how much principal will throw off that amount in interest and dividends each year; and how far your present savings are from that target.
An oft-quoted rule of thumb is that, in retirement, your expenses will be about 70% of what they are now. In my opinion, that’s nonsense. While a few bills, such as disability and malpractice insurance premiums, will go away, other costs, such as recreation and medical care, will increase. I suggest assuming that your spending will not diminish significantly in retirement. Those of us who love travel or fancy toys may need even more.
Once you have an estimate of your annual retirement expenses, you’ll need to determine how much principal you’ll need – usually in fixed pensions and invested assets – to generate that income. Most financial advisors use the 5% rule: Assume your nest egg will pay you a conservative 5% of its value each year in dividends and interest. That rule has worked well, on average, over the long term. So if you estimate your postretirement spending will be around $100,000 per year (in today’s dollars), you’ll need about $2 million in assets. For $200,000 annual spending, you’ll need $4 million. (Should you factor in Social Security? Yes, if you’re 50 years or older; if you’re younger, I wouldn’t count on receiving any entitlements, and be pleasantly surprised if you do.)
How do you accumulate that kind of money? Financial experts say too many physicians invest too aggressively. For retirement, safety is the key. The most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. $1,000 per month for 25 years with the market earning 10% (its historic long-term average) comes to almost $2 million, with the power of compounded interest working for you. And the earlier you start, the better.
It is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house or for college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your funds grow tax free until you withdraw them, presumably in a lower tax bracket.
At any age, it’s hard to motivate yourself to save, because it generally requires spending less money now. The way I do it is to pay myself first; that is, each month I make my regular savings contribution before considering any new purchases.
In the end, the strategy is very straightforward: Fill your retirement plan to its legal limit and let it grow, tax deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Whenever Don McLean is asked what the lyrics to his iconic song “American Pie” mean, he answers: “They mean that I don’t have to work anymore.”
It would be nice if those of us who have never written an enigmatic hit tune could receive an unequivocal signal when it’s safe to retire. Unfortunately, the road to retirement is fraught with challenges, not least of which is locating the right off-ramp.
We tend to live longer than planned, so we run the risk of outliving our savings, which are often underfunded to begin with. And we don’t face facts about end-of-life care. Few of us have long-term care insurance, or the means to self-fund an extended long-term care situation, as I will discuss next month.
Many of us lack a clear idea of where our retirement income will come from, or if it will be there when we arrive. Doctors in particular are notorious for mismanaging their investments. Many try to self-manage retirement plans and personal savings without adequate time or knowledge to do it right. Involving a qualified financial professional is usually a far better strategy than going it alone.
So, As with everything else, it depends; but to arrive at any sort of reliable ballpark figure, you’ll need to know three things: how much you realistically expect to spend annually after retirement; how much principal will throw off that amount in interest and dividends each year; and how far your present savings are from that target.
An oft-quoted rule of thumb is that, in retirement, your expenses will be about 70% of what they are now. In my opinion, that’s nonsense. While a few bills, such as disability and malpractice insurance premiums, will go away, other costs, such as recreation and medical care, will increase. I suggest assuming that your spending will not diminish significantly in retirement. Those of us who love travel or fancy toys may need even more.
Once you have an estimate of your annual retirement expenses, you’ll need to determine how much principal you’ll need – usually in fixed pensions and invested assets – to generate that income. Most financial advisors use the 5% rule: Assume your nest egg will pay you a conservative 5% of its value each year in dividends and interest. That rule has worked well, on average, over the long term. So if you estimate your postretirement spending will be around $100,000 per year (in today’s dollars), you’ll need about $2 million in assets. For $200,000 annual spending, you’ll need $4 million. (Should you factor in Social Security? Yes, if you’re 50 years or older; if you’re younger, I wouldn’t count on receiving any entitlements, and be pleasantly surprised if you do.)
How do you accumulate that kind of money? Financial experts say too many physicians invest too aggressively. For retirement, safety is the key. The most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. $1,000 per month for 25 years with the market earning 10% (its historic long-term average) comes to almost $2 million, with the power of compounded interest working for you. And the earlier you start, the better.
It is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house or for college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your funds grow tax free until you withdraw them, presumably in a lower tax bracket.
At any age, it’s hard to motivate yourself to save, because it generally requires spending less money now. The way I do it is to pay myself first; that is, each month I make my regular savings contribution before considering any new purchases.
In the end, the strategy is very straightforward: Fill your retirement plan to its legal limit and let it grow, tax deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Whenever Don McLean is asked what the lyrics to his iconic song “American Pie” mean, he answers: “They mean that I don’t have to work anymore.”
It would be nice if those of us who have never written an enigmatic hit tune could receive an unequivocal signal when it’s safe to retire. Unfortunately, the road to retirement is fraught with challenges, not least of which is locating the right off-ramp.
We tend to live longer than planned, so we run the risk of outliving our savings, which are often underfunded to begin with. And we don’t face facts about end-of-life care. Few of us have long-term care insurance, or the means to self-fund an extended long-term care situation, as I will discuss next month.
Many of us lack a clear idea of where our retirement income will come from, or if it will be there when we arrive. Doctors in particular are notorious for mismanaging their investments. Many try to self-manage retirement plans and personal savings without adequate time or knowledge to do it right. Involving a qualified financial professional is usually a far better strategy than going it alone.
So, As with everything else, it depends; but to arrive at any sort of reliable ballpark figure, you’ll need to know three things: how much you realistically expect to spend annually after retirement; how much principal will throw off that amount in interest and dividends each year; and how far your present savings are from that target.
An oft-quoted rule of thumb is that, in retirement, your expenses will be about 70% of what they are now. In my opinion, that’s nonsense. While a few bills, such as disability and malpractice insurance premiums, will go away, other costs, such as recreation and medical care, will increase. I suggest assuming that your spending will not diminish significantly in retirement. Those of us who love travel or fancy toys may need even more.
Once you have an estimate of your annual retirement expenses, you’ll need to determine how much principal you’ll need – usually in fixed pensions and invested assets – to generate that income. Most financial advisors use the 5% rule: Assume your nest egg will pay you a conservative 5% of its value each year in dividends and interest. That rule has worked well, on average, over the long term. So if you estimate your postretirement spending will be around $100,000 per year (in today’s dollars), you’ll need about $2 million in assets. For $200,000 annual spending, you’ll need $4 million. (Should you factor in Social Security? Yes, if you’re 50 years or older; if you’re younger, I wouldn’t count on receiving any entitlements, and be pleasantly surprised if you do.)
How do you accumulate that kind of money? Financial experts say too many physicians invest too aggressively. For retirement, safety is the key. The most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. $1,000 per month for 25 years with the market earning 10% (its historic long-term average) comes to almost $2 million, with the power of compounded interest working for you. And the earlier you start, the better.
It is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house or for college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your funds grow tax free until you withdraw them, presumably in a lower tax bracket.
At any age, it’s hard to motivate yourself to save, because it generally requires spending less money now. The way I do it is to pay myself first; that is, each month I make my regular savings contribution before considering any new purchases.
In the end, the strategy is very straightforward: Fill your retirement plan to its legal limit and let it grow, tax deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
Wasteful health care spending could reach $935 billion
Wasteful spending in health care could reach almost $1 trillion, according to new research published in JAMA.
Review “of the current literature of the cost of waste in the U.S. health care system and evidence about projected savings from interventions that reduce waste suggest that the estimated total costs of waste and potential savings from interventions that address waste are as high as $760 billion to $935 billion and $191 billion to $282 billion, respectively,” William Shrank, MD, chief medical and corporate affairs officer at Humana, and colleagues wrote in an article published Oct. 7, 2019, in JAMA.
“These estimates represent approximately 25% of total health care expenditures in the Unites States, which have been projected to be $3.82 trillion for 2019,” the authors noted, adding that it is a little lower than other estimates that have waste as high as 34% of spending.
Authors looked at waste across six domains, including failure of care delivery, failure of care coordination, overtreatment or low-value care, pricing failure, fraud and abuse, and administrative complexity.
adding that there are no studies that identified savings from interventions to alleviate administrative complexity.
“Some of that complexity results from fragmentation in the health care system,” they stated. “Recent proposals by CMS [the Centers for Medicare & Medicaid Services] and the Office of the National Coordinator of [sic] Health Information Technology to foster data interoperability and government initiatives such as Blue Button 2.0 will hopefully alleviate some burden as information flows more freely and billing and authorization processes become more automated.”
They also point to greater use of value-based payments as a possible avenue toward greater cost savings in this category.
The second largest contributor is pricing failure, which is estimated to be in the range from $230.7 billion to $240.5 billion, with interventions generating savings ranging from $81.4 billion to $91.2 billion.
And as the health care system evolves to a value-based paradigm, it is expected to have the least impact in this category “since pharmaceutical pricing represents a major component of this waste domain and would not be affected by new approaches to care delivery and reimbursement,” Dr. Shrank and colleagues wrote.
That being said, the authors stated that policy interventions “are needed to drive meaningful reductions in waste in this domain. Additionally, in the dynamic health care marketplace, where profit-motivated firms will respond to any new policy with strategies to protect their margins, no single policy is likely to suffice; a coordinated policy effort is likely needed to create long-standing change that will meaningfully reduce waste resulting from pricing failure.”
The three domains of failure of care delivery, failure of care coordination, and overtreatment or low-value care combined to account for $200 billion in waste, and the authors stated that there is “compelling empirical evidence in all three categories that interventions can produce meaningful savings and may reduce waste by as much as half.”
SOURCE: Shrank W et al. JAMA. 2019 Oct 7. doi: 10.1001/jama.2019.13978.
The biggest challenge in removing waste from the health care system is one of politics. People and organizations make huge profits from the current system and have a vested interest in maintaining the status quo and aren’t afraid to lobby both sides of the aisle to keep things as close to how they are.
Physicians hold power in this by championing more shared-risk payment structures that encourage everyone to be more conscious of waste. They also need to ensure their voices are heard politically to oppose greed and deception in pricing policies whenever they arise.
Donald M. Berwick, MD, president emeritus and senior fellow, the Institute for Health Care Improvement, Boston, and former CMS administrator, made his comments in an editorial published online in JAMA (2019 Oct 7. doi: 10.1001/jama.2019.14610 ).
The biggest challenge in removing waste from the health care system is one of politics. People and organizations make huge profits from the current system and have a vested interest in maintaining the status quo and aren’t afraid to lobby both sides of the aisle to keep things as close to how they are.
Physicians hold power in this by championing more shared-risk payment structures that encourage everyone to be more conscious of waste. They also need to ensure their voices are heard politically to oppose greed and deception in pricing policies whenever they arise.
Donald M. Berwick, MD, president emeritus and senior fellow, the Institute for Health Care Improvement, Boston, and former CMS administrator, made his comments in an editorial published online in JAMA (2019 Oct 7. doi: 10.1001/jama.2019.14610 ).
The biggest challenge in removing waste from the health care system is one of politics. People and organizations make huge profits from the current system and have a vested interest in maintaining the status quo and aren’t afraid to lobby both sides of the aisle to keep things as close to how they are.
Physicians hold power in this by championing more shared-risk payment structures that encourage everyone to be more conscious of waste. They also need to ensure their voices are heard politically to oppose greed and deception in pricing policies whenever they arise.
Donald M. Berwick, MD, president emeritus and senior fellow, the Institute for Health Care Improvement, Boston, and former CMS administrator, made his comments in an editorial published online in JAMA (2019 Oct 7. doi: 10.1001/jama.2019.14610 ).
Wasteful spending in health care could reach almost $1 trillion, according to new research published in JAMA.
Review “of the current literature of the cost of waste in the U.S. health care system and evidence about projected savings from interventions that reduce waste suggest that the estimated total costs of waste and potential savings from interventions that address waste are as high as $760 billion to $935 billion and $191 billion to $282 billion, respectively,” William Shrank, MD, chief medical and corporate affairs officer at Humana, and colleagues wrote in an article published Oct. 7, 2019, in JAMA.
“These estimates represent approximately 25% of total health care expenditures in the Unites States, which have been projected to be $3.82 trillion for 2019,” the authors noted, adding that it is a little lower than other estimates that have waste as high as 34% of spending.
Authors looked at waste across six domains, including failure of care delivery, failure of care coordination, overtreatment or low-value care, pricing failure, fraud and abuse, and administrative complexity.
adding that there are no studies that identified savings from interventions to alleviate administrative complexity.
“Some of that complexity results from fragmentation in the health care system,” they stated. “Recent proposals by CMS [the Centers for Medicare & Medicaid Services] and the Office of the National Coordinator of [sic] Health Information Technology to foster data interoperability and government initiatives such as Blue Button 2.0 will hopefully alleviate some burden as information flows more freely and billing and authorization processes become more automated.”
They also point to greater use of value-based payments as a possible avenue toward greater cost savings in this category.
The second largest contributor is pricing failure, which is estimated to be in the range from $230.7 billion to $240.5 billion, with interventions generating savings ranging from $81.4 billion to $91.2 billion.
And as the health care system evolves to a value-based paradigm, it is expected to have the least impact in this category “since pharmaceutical pricing represents a major component of this waste domain and would not be affected by new approaches to care delivery and reimbursement,” Dr. Shrank and colleagues wrote.
That being said, the authors stated that policy interventions “are needed to drive meaningful reductions in waste in this domain. Additionally, in the dynamic health care marketplace, where profit-motivated firms will respond to any new policy with strategies to protect their margins, no single policy is likely to suffice; a coordinated policy effort is likely needed to create long-standing change that will meaningfully reduce waste resulting from pricing failure.”
The three domains of failure of care delivery, failure of care coordination, and overtreatment or low-value care combined to account for $200 billion in waste, and the authors stated that there is “compelling empirical evidence in all three categories that interventions can produce meaningful savings and may reduce waste by as much as half.”
SOURCE: Shrank W et al. JAMA. 2019 Oct 7. doi: 10.1001/jama.2019.13978.
Wasteful spending in health care could reach almost $1 trillion, according to new research published in JAMA.
Review “of the current literature of the cost of waste in the U.S. health care system and evidence about projected savings from interventions that reduce waste suggest that the estimated total costs of waste and potential savings from interventions that address waste are as high as $760 billion to $935 billion and $191 billion to $282 billion, respectively,” William Shrank, MD, chief medical and corporate affairs officer at Humana, and colleagues wrote in an article published Oct. 7, 2019, in JAMA.
“These estimates represent approximately 25% of total health care expenditures in the Unites States, which have been projected to be $3.82 trillion for 2019,” the authors noted, adding that it is a little lower than other estimates that have waste as high as 34% of spending.
Authors looked at waste across six domains, including failure of care delivery, failure of care coordination, overtreatment or low-value care, pricing failure, fraud and abuse, and administrative complexity.
adding that there are no studies that identified savings from interventions to alleviate administrative complexity.
“Some of that complexity results from fragmentation in the health care system,” they stated. “Recent proposals by CMS [the Centers for Medicare & Medicaid Services] and the Office of the National Coordinator of [sic] Health Information Technology to foster data interoperability and government initiatives such as Blue Button 2.0 will hopefully alleviate some burden as information flows more freely and billing and authorization processes become more automated.”
They also point to greater use of value-based payments as a possible avenue toward greater cost savings in this category.
The second largest contributor is pricing failure, which is estimated to be in the range from $230.7 billion to $240.5 billion, with interventions generating savings ranging from $81.4 billion to $91.2 billion.
And as the health care system evolves to a value-based paradigm, it is expected to have the least impact in this category “since pharmaceutical pricing represents a major component of this waste domain and would not be affected by new approaches to care delivery and reimbursement,” Dr. Shrank and colleagues wrote.
That being said, the authors stated that policy interventions “are needed to drive meaningful reductions in waste in this domain. Additionally, in the dynamic health care marketplace, where profit-motivated firms will respond to any new policy with strategies to protect their margins, no single policy is likely to suffice; a coordinated policy effort is likely needed to create long-standing change that will meaningfully reduce waste resulting from pricing failure.”
The three domains of failure of care delivery, failure of care coordination, and overtreatment or low-value care combined to account for $200 billion in waste, and the authors stated that there is “compelling empirical evidence in all three categories that interventions can produce meaningful savings and may reduce waste by as much as half.”
SOURCE: Shrank W et al. JAMA. 2019 Oct 7. doi: 10.1001/jama.2019.13978.
FROM JAMA
HHS floats Stark/anti-kickback revisions to support value-based care
The long-awaited reforms would create permanent exemptions and safe harbors to protect doctors participating in legitimate value-based arrangements. If finalized, the proposals also would offer flexibility for innovation and improved care coordination, while easing the compliance burden for health care professionals and maintaining safeguards against actual fraud and abuse, according to the U.S. Department of Health & Human Services.
The proposals acknowledge that the Stark Law has been an unintentional roadblock to value-based programs in part because it circumscribed parties’ exchanges of rewards for good behavior, said Donna K. Thiel, a Washington-based health law attorney.
“This should be helpful to doctors in that it removes some of the risk in such arrangements under the existing law,” she said in an interview. “If finalized, the new regulations will alleviate some roadblocks created by the Stark Law with respect to hospital-physician and other arrangements designed to enhance care coordination, improve quality, and reduce waste. Likewise, the changes to the [Anti-Kickback Statute] and Beneficiary Inducement laws loosen the reins on compensation arrangements that might be technical violations of those laws where the arrangement fosters [value-based payments] or efficiency, transparency, or innovation in the provision of health care.”
“These proposed rules would be a historic reform of how healthcare is regulated in America,” HHS Deputy Secretary Eric Hargan said in a statement. “They are part of a much broader effort to update, reform, and cut back our regulations to allow innovation toward a more affordable, higher quality, value-based health care system, while maintaining the important protections patients need.”
The two proposed measures – one rule by the Centers for Medicare and Medicaid Services and the other rule by the Office of Inspector General – include safe harbors for certain remuneration exchanged among participants in a value-based arrangement that fosters better coordinated and managed patient care. This includes care arrangements that improve quality, health outcomes, and efficiency, value-based arrangements with substantial downside financial risk, and value-based arrangements with full financial risk.
In addition, the proposals would protect certain tools and supports shared or delivered under patient engagement and support arrangements to improve quality, health outcomes, and efficiency. For example, a specialty physician practice could share data analytics services with a primary care physician practice in an effort to coordinate care and better manage shared patients, according to the HHS.
If finalized, the changes would modify existing safe harbor for personal services and management contracts to add flexibility with respect to outcomes-based payments and part-time arrangements, according to a fact sheet by the OIG. The rule would also modify existing safe harbors for local transportation to expand and modify mileage limits for rural areas and for transportation for discharged patients.
The proposals include guidance on several requirements that must be met for physicians and health care providers to comply with the Stark Law. For example, compensation provided to a doctor by another health care provider generally must be at fair-market value. As part of the proposals, the HHS offers guidance on how to determine if compensation meets this requirement and provides clarity on a range of other technical compliance requirements.
If the rules are approved, more physicians may be encouraged to become part of value-based arrangements, according to Anjali N.C. Downs, a health law attorney based in Washington.
“As stakeholders have long known, physicians are key components to achieving value-based health care delivery and payment systems,” Ms. Downs said in an interview. “The proposed rules remove regulatory barriers that chill physician’s willingness and ability to participate in or even consider participating in integrated care delivery models, alternative payment models, and incentive based arrangements based on outcomes and reductions in cost.”
However, Ms. Thiel noted the proposed rules do not scale back the affected laws as comprehensively as some stakeholders hoped.
“Some would like to see the Stark law repealed completely, opining that the Stark Law has become too complex, creating obstacles in the transition from the fee-for-service model,” Ms. Thiel said. “Because Stark is a strict liability law, meaning no proof of specific intent to violate is required, providers and doctors can violate Stark even when there is no corrupt intent involved. This new regulation purports to fix some of those issues, but others will remain. Some in the industry believe full repeal is necessary to allow the health industry to move forward with pay-for-performance initiatives.”
The agency is also proposing a safe harbor for donations of cybersecurity technology and services between aligned providers in both the fee-for-service and the value-based settings. For example, a local hospital looking to improve its cybersecurity and that of nearby providers could donate cybersecurity software to each physician that refers patients to its hospital, according to the HHS. In addition, the proposals would add protections for certain cybersecurity technology included as part of an electronic health records (EHR) arrangement.
Physician organizations expressed cautious optimism about the proposed changes.
“While the [American Medical Association] is assessing the full scope of today’s proposals, we are pleased to see that the administration has acknowledged a need for policy revisions in response to potential barriers that impede the delivery of patient-centric care,” AMA President Patrice A. Harris, MD, said in a statement. “Currently, the Stark Law and Anti-Kickback Statute can have a negative impact on the ability of physicians to assist with coordination because they inhibit collaborative partnerships, care continuity, and the engagement of patients in their care. These obstacles can hinder the health care system’s movement to value-based care.”
The proposed rules have been submitted to the Federal Registry and are not yet published. The HHS will accept mail and electronic comments about the proposals up to 75 days after publication in the registry.
The long-awaited reforms would create permanent exemptions and safe harbors to protect doctors participating in legitimate value-based arrangements. If finalized, the proposals also would offer flexibility for innovation and improved care coordination, while easing the compliance burden for health care professionals and maintaining safeguards against actual fraud and abuse, according to the U.S. Department of Health & Human Services.
The proposals acknowledge that the Stark Law has been an unintentional roadblock to value-based programs in part because it circumscribed parties’ exchanges of rewards for good behavior, said Donna K. Thiel, a Washington-based health law attorney.
“This should be helpful to doctors in that it removes some of the risk in such arrangements under the existing law,” she said in an interview. “If finalized, the new regulations will alleviate some roadblocks created by the Stark Law with respect to hospital-physician and other arrangements designed to enhance care coordination, improve quality, and reduce waste. Likewise, the changes to the [Anti-Kickback Statute] and Beneficiary Inducement laws loosen the reins on compensation arrangements that might be technical violations of those laws where the arrangement fosters [value-based payments] or efficiency, transparency, or innovation in the provision of health care.”
“These proposed rules would be a historic reform of how healthcare is regulated in America,” HHS Deputy Secretary Eric Hargan said in a statement. “They are part of a much broader effort to update, reform, and cut back our regulations to allow innovation toward a more affordable, higher quality, value-based health care system, while maintaining the important protections patients need.”
The two proposed measures – one rule by the Centers for Medicare and Medicaid Services and the other rule by the Office of Inspector General – include safe harbors for certain remuneration exchanged among participants in a value-based arrangement that fosters better coordinated and managed patient care. This includes care arrangements that improve quality, health outcomes, and efficiency, value-based arrangements with substantial downside financial risk, and value-based arrangements with full financial risk.
In addition, the proposals would protect certain tools and supports shared or delivered under patient engagement and support arrangements to improve quality, health outcomes, and efficiency. For example, a specialty physician practice could share data analytics services with a primary care physician practice in an effort to coordinate care and better manage shared patients, according to the HHS.
If finalized, the changes would modify existing safe harbor for personal services and management contracts to add flexibility with respect to outcomes-based payments and part-time arrangements, according to a fact sheet by the OIG. The rule would also modify existing safe harbors for local transportation to expand and modify mileage limits for rural areas and for transportation for discharged patients.
The proposals include guidance on several requirements that must be met for physicians and health care providers to comply with the Stark Law. For example, compensation provided to a doctor by another health care provider generally must be at fair-market value. As part of the proposals, the HHS offers guidance on how to determine if compensation meets this requirement and provides clarity on a range of other technical compliance requirements.
If the rules are approved, more physicians may be encouraged to become part of value-based arrangements, according to Anjali N.C. Downs, a health law attorney based in Washington.
“As stakeholders have long known, physicians are key components to achieving value-based health care delivery and payment systems,” Ms. Downs said in an interview. “The proposed rules remove regulatory barriers that chill physician’s willingness and ability to participate in or even consider participating in integrated care delivery models, alternative payment models, and incentive based arrangements based on outcomes and reductions in cost.”
However, Ms. Thiel noted the proposed rules do not scale back the affected laws as comprehensively as some stakeholders hoped.
“Some would like to see the Stark law repealed completely, opining that the Stark Law has become too complex, creating obstacles in the transition from the fee-for-service model,” Ms. Thiel said. “Because Stark is a strict liability law, meaning no proof of specific intent to violate is required, providers and doctors can violate Stark even when there is no corrupt intent involved. This new regulation purports to fix some of those issues, but others will remain. Some in the industry believe full repeal is necessary to allow the health industry to move forward with pay-for-performance initiatives.”
The agency is also proposing a safe harbor for donations of cybersecurity technology and services between aligned providers in both the fee-for-service and the value-based settings. For example, a local hospital looking to improve its cybersecurity and that of nearby providers could donate cybersecurity software to each physician that refers patients to its hospital, according to the HHS. In addition, the proposals would add protections for certain cybersecurity technology included as part of an electronic health records (EHR) arrangement.
Physician organizations expressed cautious optimism about the proposed changes.
“While the [American Medical Association] is assessing the full scope of today’s proposals, we are pleased to see that the administration has acknowledged a need for policy revisions in response to potential barriers that impede the delivery of patient-centric care,” AMA President Patrice A. Harris, MD, said in a statement. “Currently, the Stark Law and Anti-Kickback Statute can have a negative impact on the ability of physicians to assist with coordination because they inhibit collaborative partnerships, care continuity, and the engagement of patients in their care. These obstacles can hinder the health care system’s movement to value-based care.”
The proposed rules have been submitted to the Federal Registry and are not yet published. The HHS will accept mail and electronic comments about the proposals up to 75 days after publication in the registry.
The long-awaited reforms would create permanent exemptions and safe harbors to protect doctors participating in legitimate value-based arrangements. If finalized, the proposals also would offer flexibility for innovation and improved care coordination, while easing the compliance burden for health care professionals and maintaining safeguards against actual fraud and abuse, according to the U.S. Department of Health & Human Services.
The proposals acknowledge that the Stark Law has been an unintentional roadblock to value-based programs in part because it circumscribed parties’ exchanges of rewards for good behavior, said Donna K. Thiel, a Washington-based health law attorney.
“This should be helpful to doctors in that it removes some of the risk in such arrangements under the existing law,” she said in an interview. “If finalized, the new regulations will alleviate some roadblocks created by the Stark Law with respect to hospital-physician and other arrangements designed to enhance care coordination, improve quality, and reduce waste. Likewise, the changes to the [Anti-Kickback Statute] and Beneficiary Inducement laws loosen the reins on compensation arrangements that might be technical violations of those laws where the arrangement fosters [value-based payments] or efficiency, transparency, or innovation in the provision of health care.”
“These proposed rules would be a historic reform of how healthcare is regulated in America,” HHS Deputy Secretary Eric Hargan said in a statement. “They are part of a much broader effort to update, reform, and cut back our regulations to allow innovation toward a more affordable, higher quality, value-based health care system, while maintaining the important protections patients need.”
The two proposed measures – one rule by the Centers for Medicare and Medicaid Services and the other rule by the Office of Inspector General – include safe harbors for certain remuneration exchanged among participants in a value-based arrangement that fosters better coordinated and managed patient care. This includes care arrangements that improve quality, health outcomes, and efficiency, value-based arrangements with substantial downside financial risk, and value-based arrangements with full financial risk.
In addition, the proposals would protect certain tools and supports shared or delivered under patient engagement and support arrangements to improve quality, health outcomes, and efficiency. For example, a specialty physician practice could share data analytics services with a primary care physician practice in an effort to coordinate care and better manage shared patients, according to the HHS.
If finalized, the changes would modify existing safe harbor for personal services and management contracts to add flexibility with respect to outcomes-based payments and part-time arrangements, according to a fact sheet by the OIG. The rule would also modify existing safe harbors for local transportation to expand and modify mileage limits for rural areas and for transportation for discharged patients.
The proposals include guidance on several requirements that must be met for physicians and health care providers to comply with the Stark Law. For example, compensation provided to a doctor by another health care provider generally must be at fair-market value. As part of the proposals, the HHS offers guidance on how to determine if compensation meets this requirement and provides clarity on a range of other technical compliance requirements.
If the rules are approved, more physicians may be encouraged to become part of value-based arrangements, according to Anjali N.C. Downs, a health law attorney based in Washington.
“As stakeholders have long known, physicians are key components to achieving value-based health care delivery and payment systems,” Ms. Downs said in an interview. “The proposed rules remove regulatory barriers that chill physician’s willingness and ability to participate in or even consider participating in integrated care delivery models, alternative payment models, and incentive based arrangements based on outcomes and reductions in cost.”
However, Ms. Thiel noted the proposed rules do not scale back the affected laws as comprehensively as some stakeholders hoped.
“Some would like to see the Stark law repealed completely, opining that the Stark Law has become too complex, creating obstacles in the transition from the fee-for-service model,” Ms. Thiel said. “Because Stark is a strict liability law, meaning no proof of specific intent to violate is required, providers and doctors can violate Stark even when there is no corrupt intent involved. This new regulation purports to fix some of those issues, but others will remain. Some in the industry believe full repeal is necessary to allow the health industry to move forward with pay-for-performance initiatives.”
The agency is also proposing a safe harbor for donations of cybersecurity technology and services between aligned providers in both the fee-for-service and the value-based settings. For example, a local hospital looking to improve its cybersecurity and that of nearby providers could donate cybersecurity software to each physician that refers patients to its hospital, according to the HHS. In addition, the proposals would add protections for certain cybersecurity technology included as part of an electronic health records (EHR) arrangement.
Physician organizations expressed cautious optimism about the proposed changes.
“While the [American Medical Association] is assessing the full scope of today’s proposals, we are pleased to see that the administration has acknowledged a need for policy revisions in response to potential barriers that impede the delivery of patient-centric care,” AMA President Patrice A. Harris, MD, said in a statement. “Currently, the Stark Law and Anti-Kickback Statute can have a negative impact on the ability of physicians to assist with coordination because they inhibit collaborative partnerships, care continuity, and the engagement of patients in their care. These obstacles can hinder the health care system’s movement to value-based care.”
The proposed rules have been submitted to the Federal Registry and are not yet published. The HHS will accept mail and electronic comments about the proposals up to 75 days after publication in the registry.
BP screening nearly universal among Medicare enrollees
and just under 90% saw a physician during the year, according to new data released by the Centers for Medicare & Medicaid Services.

The latest edition of Medicare Beneficiaries at a Glance takes a look at some of the services provided in 2017, and BP checks were high on the list, with 96% of enrollees getting screened. BP was also prominent on another list featured in the Medicare snapshot for 2017, as hypertension was the most common chronic condition among beneficiaries with a prevalence of 58%, the CMS said.
A second glance at the report shows that 41% of enrollees had high cholesterol that year, making it the next-most common chronic condition, with arthritis third at 33%, the CMS said. Diabetes was fourth and heart disease was fifth, but rounding gives them the same prevalence of 27%.
and just under 90% saw a physician during the year, according to new data released by the Centers for Medicare & Medicaid Services.

The latest edition of Medicare Beneficiaries at a Glance takes a look at some of the services provided in 2017, and BP checks were high on the list, with 96% of enrollees getting screened. BP was also prominent on another list featured in the Medicare snapshot for 2017, as hypertension was the most common chronic condition among beneficiaries with a prevalence of 58%, the CMS said.
A second glance at the report shows that 41% of enrollees had high cholesterol that year, making it the next-most common chronic condition, with arthritis third at 33%, the CMS said. Diabetes was fourth and heart disease was fifth, but rounding gives them the same prevalence of 27%.
and just under 90% saw a physician during the year, according to new data released by the Centers for Medicare & Medicaid Services.

The latest edition of Medicare Beneficiaries at a Glance takes a look at some of the services provided in 2017, and BP checks were high on the list, with 96% of enrollees getting screened. BP was also prominent on another list featured in the Medicare snapshot for 2017, as hypertension was the most common chronic condition among beneficiaries with a prevalence of 58%, the CMS said.
A second glance at the report shows that 41% of enrollees had high cholesterol that year, making it the next-most common chronic condition, with arthritis third at 33%, the CMS said. Diabetes was fourth and heart disease was fifth, but rounding gives them the same prevalence of 27%.
They enrolled in medical school to practice rural medicine. What happened?
SALINA, KAN. – The University of Kansas School of Medicine–Salina opened in 2011 – a one-building campus in the heart of wheat country dedicated to producing the rural doctors that the country needs.
Now, 8 years later, the school’s first graduates are settling into their chosen practices – and locales. And those choices are cause for both hope and despair.
Of the eight graduates, just three chose to go where the shortages are most evident. Two went to small cities with populations of fewer than 50,000. And three chose the big cities of Topeka (estimated 2018 population: 125,904) and Wichita (389,255) instead.
But the mission is critical: About two-thirds of the primary care health professional shortage areas designated by the federal Health Resources and Services Administration in June were in rural or partially rural areas. And it’s only getting worse.
As more baby boomer doctors in rural areas reach retirement age, not nearly enough physicians are willing to take their place. By 2030, the New England Journal of Medicine predicts, nearly a quarter fewer rural physicians will be practicing medicine than today. Over half of rural doctors were at least 50 years old in 2017.
So Salina’s creation of a few rural physicians a year is a start, and, surprisingly, one of the country’s most promising.
Only 40 out of the nation’s more than 180 medical schools offer a rural track. The Association of American Medical Colleges ranked KU School of Medicine, which includes Salina, Wichita and Kansas City campuses, in the 96th percentile last year for producing doctors working in rural settings 10-15 years after graduation.
“The addition of one physician is huge,” said William Cathcart-Rake, MD, the founding dean of the Salina campus. “One physician choosing to come may be the difference of communities surviving or dissolving.”
The draw of rural life
By placing the new campus in Salina (population: 46,716), surrounded by small towns for at least 50 miles in every direction, the university hoped to attract and foster students who had – and would deepen – a bond to rural communities.
And, for some, it worked out pretty much as planned.
One of the school’s first graduates, Sara Ritterling Patry, MD, lives in Hutchinson (population: 40,623). Less than an hour from Wichita, it isn’t the most rural community, but it’s small enough that she still runs into her patients at Dillons, the local grocery store.
“Just being in a smaller community like this feels like to me that I can actually get to know my patients and spend a little extra time with them,” she said.
After all, part of the allure of a rural practice is providing care womb to tomb. The doctor learns how to deliver the town’s babies, while serving as the county coroner and the public health expert all at once, said Robert Moser, MD, the head of the University of Kansas School of Medicine–Salina and former head of the state health department.
He would know – he worked for 22 years in Tribune, Kan. (population: 742).
For another of the original Salina eight, Tyson Wisinger, MD, that calling brought him back to his hometown of Phillipsburg (population: 2,486) after his residency. His kids will go to his old high school, where his graduating class was all of 13 people, and he’ll take care of their baseball teammates. Plus, they’ll grow up living minutes away from generations of extended family.
“I can’t have imagined a situation that could have been more rewarding,” Dr. Wisinger said.
The rural challenge
But the road to rural family medicine also includes a thing called “windshield time” – the amount of time needed to travel between clinics or head to the closest Walmart.
Then there’s figuring out just how far their patients will need to drive to get to the nearest hospital – which for Daniel Linville, MD, and Jill Corpstein Linville, MD, is a solid 4 hours for more advanced care from their new practice in Lakin, Kan. (population: 2,195).
Their outpost in southwestern Kansas can feel a little bit like a fishbowl. “We do life with some of our patients,” Dr. Corpstein Linville said.
Already, the Linvilles have delivered babies and handled a variety of ailments there.
The pair met and married during their 4 years in Salina – they jokingly call it a “full-service med school.” They completed a family medicine residency in Muncie, Ind. Then they were recruited by a rural practice that helped them avoid what Dr. Moser calls the most dreaded words in rural medicine: “solo practice.”
New doctors don’t want to practice alone, especially as they develop their sea legs, because of the strains of constantly being on call and having singular responsibility for a town. Telemedicine, where doctors can easily consult with other physicians around the country via Web video or phone, is helping, as are physician assistants.
Diverging from the path
Claire Hinrichsen Groskurth, MD, another member of the first graduating class, always intended to return to a small town similar to where she grew up.
“The first thing that threw me off was I fell in love with surgery and ob.gyn.,” she said. “Then the second thing that threw me off was marrying another doctor,” whose life goals headed in a different direction.
She’d been a member of the Scholars in Rural Health program at Kansas University that seeks out rural college students who are interested in medicine. She also had committed to the Kansas Medical Student Loan program, which promises to forgive physicians’ tuition and gives a monthly stipend if they agree to work in counties that need physicians, or in other critical capacities.
But when she realized she might specialize, she decided to take out federal loans for her final years. She had to pay back the first year of the special loan with 15% interest.
Plus, her now-husband, who went to Kansas University’s Wichita campus, needed to be in a large enough city to accommodate further training to become a surgeon. So Dr. Hinrichsen Groskurth delivers babies as she thought she would – but in Wichita.
The spousal coin can flip both ways: Dr. Ritterling Patry needed to find a place that worked for her husband’s farming of corn, sorghum, soybeans and wheat. So the smaller city of Hutchinson it was.
Flaws in the pipeline
Most medical school students come from urban areas and are destined to stay there, said Alan Morgan, the head of the National Rural Health Association. Producing doctors for the vast swaths of rural America needs to be more of a priority at every step in the education pipeline, experts said.
Many academic centers sell students on the party line that they’ll be overworked, underappreciated and underpaid, according to Mark Deutchman, MD, director of the University of Colorado School of Medicine’s rural program. “They take people who are interested in primary care or rural and beat it out of them throughout their training,” he said.
And that kind of rhetoric often influences the opinion of their medical school peers, which those in rural health might resent.
“Small does not mean stupid,” Dr. Moser said.
Medical students everywhere should be exposed to rural options, according to Randall Longenecker, MD, who runs Ohio University Heritage College of Osteopathic Medicine’s rural programs in Athens.
“If a medical student never ever goes to a rural place, they never find out,” he said. “That’s why students need to meet rural doctors who love what they do.”
The federal government recently allocated $20 million in grants to help create 27 rural residency programs – institutions where newly minted doctors go for practical training before they can be fully licensed. That’s a big jump from the 92 programs now active.
For Dr. Corpstein Linville, the pipeline also needs to start at more schools like Salina that are promoting rural medicine from day one.
“So when you hear rural medicine, you know that it’s a thing and don’t kind of cringe,” she said. “You don’t think it’s someone taking care of a cow.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
SALINA, KAN. – The University of Kansas School of Medicine–Salina opened in 2011 – a one-building campus in the heart of wheat country dedicated to producing the rural doctors that the country needs.
Now, 8 years later, the school’s first graduates are settling into their chosen practices – and locales. And those choices are cause for both hope and despair.
Of the eight graduates, just three chose to go where the shortages are most evident. Two went to small cities with populations of fewer than 50,000. And three chose the big cities of Topeka (estimated 2018 population: 125,904) and Wichita (389,255) instead.
But the mission is critical: About two-thirds of the primary care health professional shortage areas designated by the federal Health Resources and Services Administration in June were in rural or partially rural areas. And it’s only getting worse.
As more baby boomer doctors in rural areas reach retirement age, not nearly enough physicians are willing to take their place. By 2030, the New England Journal of Medicine predicts, nearly a quarter fewer rural physicians will be practicing medicine than today. Over half of rural doctors were at least 50 years old in 2017.
So Salina’s creation of a few rural physicians a year is a start, and, surprisingly, one of the country’s most promising.
Only 40 out of the nation’s more than 180 medical schools offer a rural track. The Association of American Medical Colleges ranked KU School of Medicine, which includes Salina, Wichita and Kansas City campuses, in the 96th percentile last year for producing doctors working in rural settings 10-15 years after graduation.
“The addition of one physician is huge,” said William Cathcart-Rake, MD, the founding dean of the Salina campus. “One physician choosing to come may be the difference of communities surviving or dissolving.”
The draw of rural life
By placing the new campus in Salina (population: 46,716), surrounded by small towns for at least 50 miles in every direction, the university hoped to attract and foster students who had – and would deepen – a bond to rural communities.
And, for some, it worked out pretty much as planned.
One of the school’s first graduates, Sara Ritterling Patry, MD, lives in Hutchinson (population: 40,623). Less than an hour from Wichita, it isn’t the most rural community, but it’s small enough that she still runs into her patients at Dillons, the local grocery store.
“Just being in a smaller community like this feels like to me that I can actually get to know my patients and spend a little extra time with them,” she said.
After all, part of the allure of a rural practice is providing care womb to tomb. The doctor learns how to deliver the town’s babies, while serving as the county coroner and the public health expert all at once, said Robert Moser, MD, the head of the University of Kansas School of Medicine–Salina and former head of the state health department.
He would know – he worked for 22 years in Tribune, Kan. (population: 742).
For another of the original Salina eight, Tyson Wisinger, MD, that calling brought him back to his hometown of Phillipsburg (population: 2,486) after his residency. His kids will go to his old high school, where his graduating class was all of 13 people, and he’ll take care of their baseball teammates. Plus, they’ll grow up living minutes away from generations of extended family.
“I can’t have imagined a situation that could have been more rewarding,” Dr. Wisinger said.
The rural challenge
But the road to rural family medicine also includes a thing called “windshield time” – the amount of time needed to travel between clinics or head to the closest Walmart.
Then there’s figuring out just how far their patients will need to drive to get to the nearest hospital – which for Daniel Linville, MD, and Jill Corpstein Linville, MD, is a solid 4 hours for more advanced care from their new practice in Lakin, Kan. (population: 2,195).
Their outpost in southwestern Kansas can feel a little bit like a fishbowl. “We do life with some of our patients,” Dr. Corpstein Linville said.
Already, the Linvilles have delivered babies and handled a variety of ailments there.
The pair met and married during their 4 years in Salina – they jokingly call it a “full-service med school.” They completed a family medicine residency in Muncie, Ind. Then they were recruited by a rural practice that helped them avoid what Dr. Moser calls the most dreaded words in rural medicine: “solo practice.”
New doctors don’t want to practice alone, especially as they develop their sea legs, because of the strains of constantly being on call and having singular responsibility for a town. Telemedicine, where doctors can easily consult with other physicians around the country via Web video or phone, is helping, as are physician assistants.
Diverging from the path
Claire Hinrichsen Groskurth, MD, another member of the first graduating class, always intended to return to a small town similar to where she grew up.
“The first thing that threw me off was I fell in love with surgery and ob.gyn.,” she said. “Then the second thing that threw me off was marrying another doctor,” whose life goals headed in a different direction.
She’d been a member of the Scholars in Rural Health program at Kansas University that seeks out rural college students who are interested in medicine. She also had committed to the Kansas Medical Student Loan program, which promises to forgive physicians’ tuition and gives a monthly stipend if they agree to work in counties that need physicians, or in other critical capacities.
But when she realized she might specialize, she decided to take out federal loans for her final years. She had to pay back the first year of the special loan with 15% interest.
Plus, her now-husband, who went to Kansas University’s Wichita campus, needed to be in a large enough city to accommodate further training to become a surgeon. So Dr. Hinrichsen Groskurth delivers babies as she thought she would – but in Wichita.
The spousal coin can flip both ways: Dr. Ritterling Patry needed to find a place that worked for her husband’s farming of corn, sorghum, soybeans and wheat. So the smaller city of Hutchinson it was.
Flaws in the pipeline
Most medical school students come from urban areas and are destined to stay there, said Alan Morgan, the head of the National Rural Health Association. Producing doctors for the vast swaths of rural America needs to be more of a priority at every step in the education pipeline, experts said.
Many academic centers sell students on the party line that they’ll be overworked, underappreciated and underpaid, according to Mark Deutchman, MD, director of the University of Colorado School of Medicine’s rural program. “They take people who are interested in primary care or rural and beat it out of them throughout their training,” he said.
And that kind of rhetoric often influences the opinion of their medical school peers, which those in rural health might resent.
“Small does not mean stupid,” Dr. Moser said.
Medical students everywhere should be exposed to rural options, according to Randall Longenecker, MD, who runs Ohio University Heritage College of Osteopathic Medicine’s rural programs in Athens.
“If a medical student never ever goes to a rural place, they never find out,” he said. “That’s why students need to meet rural doctors who love what they do.”
The federal government recently allocated $20 million in grants to help create 27 rural residency programs – institutions where newly minted doctors go for practical training before they can be fully licensed. That’s a big jump from the 92 programs now active.
For Dr. Corpstein Linville, the pipeline also needs to start at more schools like Salina that are promoting rural medicine from day one.
“So when you hear rural medicine, you know that it’s a thing and don’t kind of cringe,” she said. “You don’t think it’s someone taking care of a cow.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
SALINA, KAN. – The University of Kansas School of Medicine–Salina opened in 2011 – a one-building campus in the heart of wheat country dedicated to producing the rural doctors that the country needs.
Now, 8 years later, the school’s first graduates are settling into their chosen practices – and locales. And those choices are cause for both hope and despair.
Of the eight graduates, just three chose to go where the shortages are most evident. Two went to small cities with populations of fewer than 50,000. And three chose the big cities of Topeka (estimated 2018 population: 125,904) and Wichita (389,255) instead.
But the mission is critical: About two-thirds of the primary care health professional shortage areas designated by the federal Health Resources and Services Administration in June were in rural or partially rural areas. And it’s only getting worse.
As more baby boomer doctors in rural areas reach retirement age, not nearly enough physicians are willing to take their place. By 2030, the New England Journal of Medicine predicts, nearly a quarter fewer rural physicians will be practicing medicine than today. Over half of rural doctors were at least 50 years old in 2017.
So Salina’s creation of a few rural physicians a year is a start, and, surprisingly, one of the country’s most promising.
Only 40 out of the nation’s more than 180 medical schools offer a rural track. The Association of American Medical Colleges ranked KU School of Medicine, which includes Salina, Wichita and Kansas City campuses, in the 96th percentile last year for producing doctors working in rural settings 10-15 years after graduation.
“The addition of one physician is huge,” said William Cathcart-Rake, MD, the founding dean of the Salina campus. “One physician choosing to come may be the difference of communities surviving or dissolving.”
The draw of rural life
By placing the new campus in Salina (population: 46,716), surrounded by small towns for at least 50 miles in every direction, the university hoped to attract and foster students who had – and would deepen – a bond to rural communities.
And, for some, it worked out pretty much as planned.
One of the school’s first graduates, Sara Ritterling Patry, MD, lives in Hutchinson (population: 40,623). Less than an hour from Wichita, it isn’t the most rural community, but it’s small enough that she still runs into her patients at Dillons, the local grocery store.
“Just being in a smaller community like this feels like to me that I can actually get to know my patients and spend a little extra time with them,” she said.
After all, part of the allure of a rural practice is providing care womb to tomb. The doctor learns how to deliver the town’s babies, while serving as the county coroner and the public health expert all at once, said Robert Moser, MD, the head of the University of Kansas School of Medicine–Salina and former head of the state health department.
He would know – he worked for 22 years in Tribune, Kan. (population: 742).
For another of the original Salina eight, Tyson Wisinger, MD, that calling brought him back to his hometown of Phillipsburg (population: 2,486) after his residency. His kids will go to his old high school, where his graduating class was all of 13 people, and he’ll take care of their baseball teammates. Plus, they’ll grow up living minutes away from generations of extended family.
“I can’t have imagined a situation that could have been more rewarding,” Dr. Wisinger said.
The rural challenge
But the road to rural family medicine also includes a thing called “windshield time” – the amount of time needed to travel between clinics or head to the closest Walmart.
Then there’s figuring out just how far their patients will need to drive to get to the nearest hospital – which for Daniel Linville, MD, and Jill Corpstein Linville, MD, is a solid 4 hours for more advanced care from their new practice in Lakin, Kan. (population: 2,195).
Their outpost in southwestern Kansas can feel a little bit like a fishbowl. “We do life with some of our patients,” Dr. Corpstein Linville said.
Already, the Linvilles have delivered babies and handled a variety of ailments there.
The pair met and married during their 4 years in Salina – they jokingly call it a “full-service med school.” They completed a family medicine residency in Muncie, Ind. Then they were recruited by a rural practice that helped them avoid what Dr. Moser calls the most dreaded words in rural medicine: “solo practice.”
New doctors don’t want to practice alone, especially as they develop their sea legs, because of the strains of constantly being on call and having singular responsibility for a town. Telemedicine, where doctors can easily consult with other physicians around the country via Web video or phone, is helping, as are physician assistants.
Diverging from the path
Claire Hinrichsen Groskurth, MD, another member of the first graduating class, always intended to return to a small town similar to where she grew up.
“The first thing that threw me off was I fell in love with surgery and ob.gyn.,” she said. “Then the second thing that threw me off was marrying another doctor,” whose life goals headed in a different direction.
She’d been a member of the Scholars in Rural Health program at Kansas University that seeks out rural college students who are interested in medicine. She also had committed to the Kansas Medical Student Loan program, which promises to forgive physicians’ tuition and gives a monthly stipend if they agree to work in counties that need physicians, or in other critical capacities.
But when she realized she might specialize, she decided to take out federal loans for her final years. She had to pay back the first year of the special loan with 15% interest.
Plus, her now-husband, who went to Kansas University’s Wichita campus, needed to be in a large enough city to accommodate further training to become a surgeon. So Dr. Hinrichsen Groskurth delivers babies as she thought she would – but in Wichita.
The spousal coin can flip both ways: Dr. Ritterling Patry needed to find a place that worked for her husband’s farming of corn, sorghum, soybeans and wheat. So the smaller city of Hutchinson it was.
Flaws in the pipeline
Most medical school students come from urban areas and are destined to stay there, said Alan Morgan, the head of the National Rural Health Association. Producing doctors for the vast swaths of rural America needs to be more of a priority at every step in the education pipeline, experts said.
Many academic centers sell students on the party line that they’ll be overworked, underappreciated and underpaid, according to Mark Deutchman, MD, director of the University of Colorado School of Medicine’s rural program. “They take people who are interested in primary care or rural and beat it out of them throughout their training,” he said.
And that kind of rhetoric often influences the opinion of their medical school peers, which those in rural health might resent.
“Small does not mean stupid,” Dr. Moser said.
Medical students everywhere should be exposed to rural options, according to Randall Longenecker, MD, who runs Ohio University Heritage College of Osteopathic Medicine’s rural programs in Athens.
“If a medical student never ever goes to a rural place, they never find out,” he said. “That’s why students need to meet rural doctors who love what they do.”
The federal government recently allocated $20 million in grants to help create 27 rural residency programs – institutions where newly minted doctors go for practical training before they can be fully licensed. That’s a big jump from the 92 programs now active.
For Dr. Corpstein Linville, the pipeline also needs to start at more schools like Salina that are promoting rural medicine from day one.
“So when you hear rural medicine, you know that it’s a thing and don’t kind of cringe,” she said. “You don’t think it’s someone taking care of a cow.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.