User login
Patients with mood disorders may have altered microbiome
Discuss dietary interventions, such as probiotics, as ‘supplemental therapeutic options’
CRYSTAL CITY, VA. – Individuals with mood disorders might have an altered microbiome, but more information is needed to understand how the microorganisms that make up the microbiome affect patients’ health, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“An increased understanding of the neurobiology of the microbiome is required so that the benefit that these microorganisms serve to human health can be fully harnessed,” said Emily G. Severance, PhD, assistant professor of pediatrics at John Hopkins University, Baltimore.
Diseases that involve the microbiome include those with a single identifiable infectious agent that produces persistent inflammation, central nervous system diseases with mucosal surface involvement, and diseases with “variable response to antibiotic and anti-inflammatory agents.”
“It’s becoming clear that [the microbiome is] integral for the modulation of the central nervous system,” which occurs through neurotransmitter production, Dr. Severance said at the meeting presented by Global Academy for Medical Education.
“We have an extensive enteric nervous system that has the very same receptors that the brain does,” she said. “If you have those receptors activated in the gut or [are] having the neurotransmitters produced in the gut, and if there’s a way for those neurotransmitters to reach the brain, that’s a very powerful mechanism to illustrate the gut-brain axis.”
In addition to neuropsychiatric diseases, the microbiome also can be involved in inflammatory gastrointestinal, systemic rheumatoid and autoimmune, chronic inflammatory lung, and periodontal diseases, as well as immune-mediated skin disorders. Mood disorders in particular have evidence for dysbiosis in low-level inflammation and leaky gut pathology, which is present in patients with depression, Dr. Severance said. “All these data suggest that We can do that because gut bacteria are easily accessed and can be altered through probiotics, prebiotics, diet, and fecal transplant, and in patients, Lactobacillus and Bifidobacterium combinations may improve mood, reduce anxiety, and enhance cognitive function.”
In addition, epidemiological studies show that antibiotic exposure can be a risk factor for developing mood disorders. One recent study found that anti-infective agents, particularly antibiotics, increased the risk of schizophrenia (hazard rate ratio, 2.05; 95% confidence interval, 1.77-2.38) and affective disorders (HRR, 2.59; 95% CI, 2.31-2.89), which the researchers attributed to brain inflammation, the microbiome, and environmental factors (Acta Psychiatr Scand. 2016 Nov 21. doi: 10.1111/acps.12671). In mice, other researchers found that those that received a fecal transplant with a “depression microbiota” showed symptoms of major depressive disorder, compared with mice that received a “healthy microbiota.” Those results suggest that change in microbiota can induce mood disorders (Mol Psychiatry. 2016 Apr 12. doi: 10.1038/mp.2016.44).
The evidence for probiotics is mixed, primarily because the study population in trials are so heterogeneous, but there is evidence for its efficacy in patients with mood disorders, Dr. Severance said. Probiotics have been shown to prevent rehospitalization for patients in mania. For example, one study showed reduced rehospitalization in patients with mania (8 of 33 patients) who received probiotics, compared with placebo (24 of 33 patients). Also, probiotic use was associated with fewer days of rehospitalization (Bipolar Disord. 2018 Apr 25. doi: 10. 1111/bdi.12652).
Meanwhile, a pilot study analyzing patients with irritable bowel syndrome and mild to moderate anxiety and/or depression found use of B. longum in this population reduced depression scores, but not anxiety or irritable bowel syndrome symptoms, compared with placebo (Gastroenterology. 2017 May 5. doi: 10.1053/j.gastro.2017.05.003).
Probiotic efficacy can be variable for patients with mood disorders, but the intervention is a “relatively low-risk, potentially high reward” option for these patients, Dr. Severance said. “Clinicians should inquire about patient GI conditions and overall GI health. Dietary interventions and the use of probiotics and their limitations should be discussed as supplemental therapeutic options.”
Dr. Severance reported no relevant financial disclosures.
Global Academy and this news organization are owned by the same parent company.
Discuss dietary interventions, such as probiotics, as ‘supplemental therapeutic options’
Discuss dietary interventions, such as probiotics, as ‘supplemental therapeutic options’
CRYSTAL CITY, VA. – Individuals with mood disorders might have an altered microbiome, but more information is needed to understand how the microorganisms that make up the microbiome affect patients’ health, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“An increased understanding of the neurobiology of the microbiome is required so that the benefit that these microorganisms serve to human health can be fully harnessed,” said Emily G. Severance, PhD, assistant professor of pediatrics at John Hopkins University, Baltimore.
Diseases that involve the microbiome include those with a single identifiable infectious agent that produces persistent inflammation, central nervous system diseases with mucosal surface involvement, and diseases with “variable response to antibiotic and anti-inflammatory agents.”
“It’s becoming clear that [the microbiome is] integral for the modulation of the central nervous system,” which occurs through neurotransmitter production, Dr. Severance said at the meeting presented by Global Academy for Medical Education.
“We have an extensive enteric nervous system that has the very same receptors that the brain does,” she said. “If you have those receptors activated in the gut or [are] having the neurotransmitters produced in the gut, and if there’s a way for those neurotransmitters to reach the brain, that’s a very powerful mechanism to illustrate the gut-brain axis.”
In addition to neuropsychiatric diseases, the microbiome also can be involved in inflammatory gastrointestinal, systemic rheumatoid and autoimmune, chronic inflammatory lung, and periodontal diseases, as well as immune-mediated skin disorders. Mood disorders in particular have evidence for dysbiosis in low-level inflammation and leaky gut pathology, which is present in patients with depression, Dr. Severance said. “All these data suggest that We can do that because gut bacteria are easily accessed and can be altered through probiotics, prebiotics, diet, and fecal transplant, and in patients, Lactobacillus and Bifidobacterium combinations may improve mood, reduce anxiety, and enhance cognitive function.”
In addition, epidemiological studies show that antibiotic exposure can be a risk factor for developing mood disorders. One recent study found that anti-infective agents, particularly antibiotics, increased the risk of schizophrenia (hazard rate ratio, 2.05; 95% confidence interval, 1.77-2.38) and affective disorders (HRR, 2.59; 95% CI, 2.31-2.89), which the researchers attributed to brain inflammation, the microbiome, and environmental factors (Acta Psychiatr Scand. 2016 Nov 21. doi: 10.1111/acps.12671). In mice, other researchers found that those that received a fecal transplant with a “depression microbiota” showed symptoms of major depressive disorder, compared with mice that received a “healthy microbiota.” Those results suggest that change in microbiota can induce mood disorders (Mol Psychiatry. 2016 Apr 12. doi: 10.1038/mp.2016.44).
The evidence for probiotics is mixed, primarily because the study population in trials are so heterogeneous, but there is evidence for its efficacy in patients with mood disorders, Dr. Severance said. Probiotics have been shown to prevent rehospitalization for patients in mania. For example, one study showed reduced rehospitalization in patients with mania (8 of 33 patients) who received probiotics, compared with placebo (24 of 33 patients). Also, probiotic use was associated with fewer days of rehospitalization (Bipolar Disord. 2018 Apr 25. doi: 10. 1111/bdi.12652).
Meanwhile, a pilot study analyzing patients with irritable bowel syndrome and mild to moderate anxiety and/or depression found use of B. longum in this population reduced depression scores, but not anxiety or irritable bowel syndrome symptoms, compared with placebo (Gastroenterology. 2017 May 5. doi: 10.1053/j.gastro.2017.05.003).
Probiotic efficacy can be variable for patients with mood disorders, but the intervention is a “relatively low-risk, potentially high reward” option for these patients, Dr. Severance said. “Clinicians should inquire about patient GI conditions and overall GI health. Dietary interventions and the use of probiotics and their limitations should be discussed as supplemental therapeutic options.”
Dr. Severance reported no relevant financial disclosures.
Global Academy and this news organization are owned by the same parent company.
CRYSTAL CITY, VA. – Individuals with mood disorders might have an altered microbiome, but more information is needed to understand how the microorganisms that make up the microbiome affect patients’ health, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“An increased understanding of the neurobiology of the microbiome is required so that the benefit that these microorganisms serve to human health can be fully harnessed,” said Emily G. Severance, PhD, assistant professor of pediatrics at John Hopkins University, Baltimore.
Diseases that involve the microbiome include those with a single identifiable infectious agent that produces persistent inflammation, central nervous system diseases with mucosal surface involvement, and diseases with “variable response to antibiotic and anti-inflammatory agents.”
“It’s becoming clear that [the microbiome is] integral for the modulation of the central nervous system,” which occurs through neurotransmitter production, Dr. Severance said at the meeting presented by Global Academy for Medical Education.
“We have an extensive enteric nervous system that has the very same receptors that the brain does,” she said. “If you have those receptors activated in the gut or [are] having the neurotransmitters produced in the gut, and if there’s a way for those neurotransmitters to reach the brain, that’s a very powerful mechanism to illustrate the gut-brain axis.”
In addition to neuropsychiatric diseases, the microbiome also can be involved in inflammatory gastrointestinal, systemic rheumatoid and autoimmune, chronic inflammatory lung, and periodontal diseases, as well as immune-mediated skin disorders. Mood disorders in particular have evidence for dysbiosis in low-level inflammation and leaky gut pathology, which is present in patients with depression, Dr. Severance said. “All these data suggest that We can do that because gut bacteria are easily accessed and can be altered through probiotics, prebiotics, diet, and fecal transplant, and in patients, Lactobacillus and Bifidobacterium combinations may improve mood, reduce anxiety, and enhance cognitive function.”
In addition, epidemiological studies show that antibiotic exposure can be a risk factor for developing mood disorders. One recent study found that anti-infective agents, particularly antibiotics, increased the risk of schizophrenia (hazard rate ratio, 2.05; 95% confidence interval, 1.77-2.38) and affective disorders (HRR, 2.59; 95% CI, 2.31-2.89), which the researchers attributed to brain inflammation, the microbiome, and environmental factors (Acta Psychiatr Scand. 2016 Nov 21. doi: 10.1111/acps.12671). In mice, other researchers found that those that received a fecal transplant with a “depression microbiota” showed symptoms of major depressive disorder, compared with mice that received a “healthy microbiota.” Those results suggest that change in microbiota can induce mood disorders (Mol Psychiatry. 2016 Apr 12. doi: 10.1038/mp.2016.44).
The evidence for probiotics is mixed, primarily because the study population in trials are so heterogeneous, but there is evidence for its efficacy in patients with mood disorders, Dr. Severance said. Probiotics have been shown to prevent rehospitalization for patients in mania. For example, one study showed reduced rehospitalization in patients with mania (8 of 33 patients) who received probiotics, compared with placebo (24 of 33 patients). Also, probiotic use was associated with fewer days of rehospitalization (Bipolar Disord. 2018 Apr 25. doi: 10. 1111/bdi.12652).
Meanwhile, a pilot study analyzing patients with irritable bowel syndrome and mild to moderate anxiety and/or depression found use of B. longum in this population reduced depression scores, but not anxiety or irritable bowel syndrome symptoms, compared with placebo (Gastroenterology. 2017 May 5. doi: 10.1053/j.gastro.2017.05.003).
Probiotic efficacy can be variable for patients with mood disorders, but the intervention is a “relatively low-risk, potentially high reward” option for these patients, Dr. Severance said. “Clinicians should inquire about patient GI conditions and overall GI health. Dietary interventions and the use of probiotics and their limitations should be discussed as supplemental therapeutic options.”
Dr. Severance reported no relevant financial disclosures.
Global Academy and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM FOCUS ON NEUROPSYCHIATRY 2019
Suicide rates rise in U.S. adolescents and young adults
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Suicides in teens and young adults reached 6,241 in 2017, the highest since 2000, according to data from a review of the Centers for Disease Control and Prevention Underlying Cause of Death database.
The suicide rate overall was 12 per 100,000 in 2017 for 15-19 year olds.
Although suicide rates have increased across all age groups in the United States since 2000, “adolescents are of particular concern, with increases in social media use, anxiety, depression, and self-inflicted injuries,” wrote Oren Miron of Harvard Medical School, Boston, and colleagues.
In a research letter published in JAMA, the researchers analyzed trends in teen and young adult suicides from 2000 to 2017. The combined suicide rate for males and females aged 15-19 years in 2000 was 8 per 100,000 with no significant changes until 2007, followed by an annual percentage change (APC) of 3% from 2007 to 2014 and 10% from 2014 to 2017.
When the data were broken out by gender, Of note, these young men showed a decreasing trend in APC of –2% from 2000 to 2007 before increasing.
Among females aged 15-19 years, no increase was noted until 2010, then researchers identified an APC of 8% from 2010 to 2017.
For ages 20-24 years, the combined suicide rate for males and females was 13 per 100,000 in 2000, which rose to 17 per 100,000 in 2017. The APC in the older group was 1% from 2000 to 2013 and 6% from 2013 to 2017. Increasing trends were observed for both males and females over the study period.
The study was limited by the potential inaccuracy in cause of death listed on death certificates, such as mistaking a suicide for an accidental overdose, and the increased suicide rate could reflect more accurate reporting, the researchers noted.
Nonetheless, the results support the need for more studies of contributing factors to teen and young adult suicides to help develop prevention strategies and analysis of factors that may have contributed to declines in suicide rates in the past, they said.
Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
SOURCE: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
FROM JAMA
Key clinical point: Suicide rates in U.S. adolescents and young adults have increased since 2000.
Major finding: The combined suicide rate for males and females aged 15-19 years underwent an annual percentage change of 3% from 2007 to 2014 and 10% from 2014 to 2017.
Study details: The data come from the CDC Underlying Cause of Death database.
Disclosures: Coauthor Dr. Yu was supported by the Harvard Data Science Fellowship. The researchers had no relevant financial disclosures.
Source: Miron O et al. JAMA. 2019 Jun 28;321:2362-4.
Ask patients about worst example of suicidal ideation
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
EXPERT ANALYSIS FROM FOCUS ON NEUROPSYCHIATRY 2019
LTC-associated suicide among older adults more common than previously thought
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
Filling the gap in knowledge about the consequences of transitioning into long-term care is sorely needed, wrote Yoram Barak, MD, MHA, and Chris Gale, MB,ChB, MPH, given that fewer than 20 studies on the subject have been published in the past 30 years. A 2015 systematic review of nursing home suicides included only eight studies and 101 suicide deaths.
Despite the limits of an epidemiologic study on long-term care in elderly adults, such as the significant differences between elderly populations in America and other countries, this study by Mezuk et al. provides useful information on a longer period of time than would be possible with case-control studies and at a more granular level than data that would be available from national case registers, Dr. Barak and Dr. Gale wrote.
Dr. Barak and Dr. Gale are with the department of psychological medicine at the University of Otago in Dunedin, New Zealand. They made these comments in an editorial published in JAMA Network Open (2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5634). They did not report any conflicts of interest.
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
The rate of suicide associated with residential long-term care (LTC) in adults aged 55 years and older may be significantly higher than the injury location coding of the National Violent Death Reporting System (NVDRS) suggests, according to new research.
The Centers for Disease Control and Prevention reports that there are about 16,000 nursing homes and 31,000 assisted living facilities in the United States and they currently house about 25% of all Medicare beneficiaries. “As such, residential LTC may be a potential location for identifying individuals at high risk of self-harm and for implementing interventions to reduce suicide risk, wrote Briana Mezuk, PhD, and associates from the University of Michigan, Ann Arbor. The study was published in JAMA Network Open.
Dr. Mezuk and colleagues conducted a cross-sectional, epidemiologic study using a natural language–processing algorithm to analyze restricted-access data from the NVDRS between 2003 and 2015. A total of 47,759 suicides and undetermined deaths in adults aged 55 years and older from 27 states were included in the analysis (median age, 64 years; 77.6% male; 90.0% non-Hispanic white).
The algorithm identified 1,037 (2.2% of the total) suicide deaths associated with LTC, with 428 occurring in adults living in LTC, 449 occurring during the transition into or out of LTC, and 160 otherwise associated with LTC. Decedents in this group had a median age of 79 years, were 73.8% male, and were 94.3% non-Hispanic white. The number of suicide deaths varied widely from year to year, but no trend was found in the change over the study period.
Deaths while living in LTC were more likely among women, which the investigators noted is to be expected because LTC residents are disproportionately women. Death while transitioning into or out of LTC was more likely among adults who previously had expressed suicide ideation and had a physical health problem cited as a contributing circumstance. Death otherwise associated with LTC was more likely in adults who were married or in a relationship, had a depressed mood, and had a recent crisis cited as a contributing factor.
“Living in LTC or transitioning to LTC is also correlated with a host of characteristics that are established risk factors for suicide,” the investigators noted.
In further analysis, the investigators compared the number of suicide deaths the algorithm identified as occurring within an LTC facility (n = 428) with the injury location code SRF (supervised residential facility; n = 263) and the death location code LTC/nursing home (n = 567) within the NVDRS. Of the 263 SRF injuries, 106 were identified as occurring within a LTC facility by the algorithm. The agreement between the algorithm and the SRF coding was poor (kappa statistic, 0.30; 95% confidence interval, 0.26-0.35).
“Leaders in the field have continued to call for a shift away from a medicalized paradigm of residential LTC toward institutional practices that instead focus on fostering meaningful interactions between residents, promote engagement in care, and enhance quality of life. In addition, existing, scalable programs that support older adults living in the community offer the potential to promote quality of life for older adults who may be considering transitioning into or out of residential LTC,” the investigators concluded. “These findings emphasize the importance of such efforts for the mental health of older adults.”
The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
SOURCE: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
FROM JAMA NETWORK OPEN
Key clinical point: Suicide associated with long-term care may be more common than previous data have indicated.
Major finding: About 2.2% of the suicide deaths reported to the National Violent Death Reporting System occurred or were associated with long-term care.
Study details: An analysis of 47,759 suicides and undetermined deaths in adults aged at least 55 years with data included in the National Violent Death Reporting System.Disclosures: The study was supported by a grant from the National Institute of Mental Health. The investigators reported no conflicts of interest.
Source: Mezuk B et al. JAMA Netw Open. 2019 Jun 14. doi: 10.1001/jamanetworkopen.2019.5627.
FDA overlooked red flags in esketamine testing
For some patients, it also has dwelled in the shadows of conventional medicine as a depression treatment – prescribed by their doctors, but not approved for that purpose by the federal agency responsible for determining which treatments are “safe and effective.”
That effectively changed in March, when the Food and Drug Administration approved a ketamine cousin called esketamine, taken as a nasal spray, for patients with intractable depression. With that, the esketamine nasal spray, under the brand name Spravato, was introduced as a miracle drug – announced in press releases, celebrated on the evening news, and embraced by major health care providers like the Department of Veterans Affairs.
The problem, critics say, is that the drug’s manufacturer, Janssen, provided the FDA with at best modest evidence it worked and then only in limited trials. It presented no information about the safety of Spravato for long-term use beyond 60 weeks. And three patients who received the drug died by suicide during clinical trials, compared with none in the control group, which raised red flags Janssen and the FDA dismissed.
The FDA, under political pressure to rapidly green-light drugs that treat life-threatening conditions, approved it anyway. And, though Spravato’s appearance on the market was greeted with public applause, some deep misgivings were expressed at its day-long review meeting and in the agency’s own briefing materials, according to public recordings, documents, and interviews with participants, KHN found.
Jess Fiedorowicz, MD, director of the Mood Disorders Center at the University of Iowa, Iowa City, and a member of the FDA advisory committee that reviewed the drug, described its benefit as “almost certainly exaggerated” after hearing the evidence.
Dr. Fiedorowicz said he expected at least a split decision by the committee. “And then it went strongly in favor, which surprised me,” he said in an interview.
Esketamine’s trajectory to approval shows – step by step – how drugmakers can take advantage of shortcuts in the FDA process with the agency’s blessing and maneuver through safety and efficacy reviews to bring a lucrative drug to market.
Step 1: In late 2013, Janssen got the FDA to designate esketamine a “breakthrough therapy” because it showed the potential to reverse depression rapidly — a holy grail for suicidal patients, such as those in an emergency room. That potential was based on a 2-day study during which 30 patients were given esketamine intravenously.
“Breakthrough therapy” status puts drugs on a fast track to approval, with more frequent input from the FDA.
Step 2: But discussions between regulators and drug manufacturers can affect the amount and quality of evidence required by the agency. In the case of Spravato, they involved questions like “How many drugs must fail before a patient’s depression is considered intractable or ‘treatment resistant’?” and “How many successful clinical trials are necessary for FDA approval?”
Step 3: Any prior agreements can leave the FDA’s expert advisory committees hamstrung in reaching a verdict. Dr. Fiedorowicz abstained on Spravato because, though he considered Janssen’s study design flawed, the FDA had approved it.
The expert panel cleared the drug according to the evidence that the agency and Janssen had determined was sufficient. Matthew Rudorfer, MD, an associate director at the National Institute of Mental Health, concluded that the “benefits outweighed the risks.” Explaining his “yes” vote, he said, “I think we’re all agreeing on the very important, and sometimes life-or-death, risk of inadequately treated depression that factored into my equation.”
But others who also voted “yes” were more explicit in their qualms. “I don’t think that we really understand what happens when you take this week after week for weeks and months and years,” said Steven Meisel, PharmD, system director of medication safety for Fairview Health Services based in Minneapolis.
A Nasal Spray Offers A Path To A Patent
Spravato is available only under supervision at a certified facility where patients must be monitored for at least two hours after taking the drug to watch for side effects like dizziness, detachment from reality, and increased blood pressure, as well as to reduce the risk of abuse. Patients must take it with an oral antidepressant.
Despite those requirements, Janssen, part of Johnson & Johnson, defended its new offering. “Until the recent FDA approval of Spravato, health care providers haven’t had any new medication options,” Kristina Chang, a Janssen spokeswoman, wrote in an emailed statement.
Esketamine is the first new type of drug approved to treat severe depression in about three decades.
Although ketamine has been used off-label for years to treat depression and posttraumatic stress disorder, drugmakers saw little profit in doing the studies to prove to the FDA that it worked for that purpose. But a nasal spray of esketamine, which is derived from ketamine and is (in some studies) more potent, could be patented as a new drug.
Although Spravato costs more than $4,700 for the first month of treatment (not including the cost of monitoring or the oral antidepressant), insurers are more likely to reimburse for Spravato than for ketamine, since the latter is not approved for depression.
Shortly before the committee began voting, a study participant identifying herself only as “Patient 20015525” said, “I am offering real-world proof of efficacy, and that is I am both alive and here today.”
The drug did not work “for the majority of people who took it,” Dr. Meisel, the medication safety expert, said in an interview. “But for a subset of those for whom it did work, it was dramatic.”
Concerns About Testing Precedents
Those considerations apparently helped outweigh several scientific red flags that committee members called out during the hearing.
Although the drug had gotten breakthrough status because of its potential for results within 24 hours, the trials were not persuasive enough for the FDA to label it “rapid acting.”
The FDA typically requires that applicants provide at least two clinical trials demonstrating the drug’s efficacy, “each convincing on its own.” Janssen provided just one successful short-term, double-blind trial of esketamine. Two other trials it ran to test efficacy fell short.
To reach the two-trial threshold, the FDA broke its precedent for psychiatric drugs and allowed the company to count a trial conducted to study a different topic: relapse and remission trends. But, by definition, every patient in the trial had already taken and seen improvement from esketamine.
What’s more, that single positive efficacy trial showed just a 4-point improvement in depression symptoms, compared with the placebo treatment, on a 60-point scale some clinicians use to measure depression severity. Some committee members noted the trial wasn’t really blind since participants could recognize they were getting the drug from side effects like a temporary out-of-body sensation.
Finally, the FDA lowered the bar for “treatment-resistant depression.” Initially, for inclusion, trial participants would have had to have failed two classes of oral antidepressants.
Less than 2 years later, the FDA loosened that definition, saying a patient needed only to have taken two different pills, no matter the class.
Forty-nine of the 227 people who participated in Janssen’s only successful efficacy trial had failed just one class of oral antidepressants. “They weeded out the true treatment-resistant patients,” said Erick Turner, MD, a former FDA reviewer who serves on the committee but did not attend the meeting.
Six participants died during the studies, three by suicide. Janssen and the FDA dismissed the deaths as unrelated to the drug, noting the low number and lack of a pattern among hundreds of participants. They also pointed out that suicidal behavior is associated with severe depression – even though those who had suicidal ideation with some intent to act in the previous 6 months, or a history of suicidal behavior in the previous year, were excluded from the studies.
In a recent commentary in the American Journal of Psychiatry, Alan Schatzberg, MD, a Stanford (Calif.) University researcher who has studied ketamine, suggested there might be a link caused by “a protracted withdrawal reaction, as has been reported with opioids,” since ketamine appears to interact with the brain’s opioid receptors (Am J Psych. 2019. doi: 10.1176/appi.ajp.2019.19040423).
Kim Witczak, the committee’s consumer representative, found Janssen’s conclusion about the suicides unsatisfying. “I just feel like it was kind of a quick brush-over,” Ms. Witczak said in an interview. She voted against the drug.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For some patients, it also has dwelled in the shadows of conventional medicine as a depression treatment – prescribed by their doctors, but not approved for that purpose by the federal agency responsible for determining which treatments are “safe and effective.”
That effectively changed in March, when the Food and Drug Administration approved a ketamine cousin called esketamine, taken as a nasal spray, for patients with intractable depression. With that, the esketamine nasal spray, under the brand name Spravato, was introduced as a miracle drug – announced in press releases, celebrated on the evening news, and embraced by major health care providers like the Department of Veterans Affairs.
The problem, critics say, is that the drug’s manufacturer, Janssen, provided the FDA with at best modest evidence it worked and then only in limited trials. It presented no information about the safety of Spravato for long-term use beyond 60 weeks. And three patients who received the drug died by suicide during clinical trials, compared with none in the control group, which raised red flags Janssen and the FDA dismissed.
The FDA, under political pressure to rapidly green-light drugs that treat life-threatening conditions, approved it anyway. And, though Spravato’s appearance on the market was greeted with public applause, some deep misgivings were expressed at its day-long review meeting and in the agency’s own briefing materials, according to public recordings, documents, and interviews with participants, KHN found.
Jess Fiedorowicz, MD, director of the Mood Disorders Center at the University of Iowa, Iowa City, and a member of the FDA advisory committee that reviewed the drug, described its benefit as “almost certainly exaggerated” after hearing the evidence.
Dr. Fiedorowicz said he expected at least a split decision by the committee. “And then it went strongly in favor, which surprised me,” he said in an interview.
Esketamine’s trajectory to approval shows – step by step – how drugmakers can take advantage of shortcuts in the FDA process with the agency’s blessing and maneuver through safety and efficacy reviews to bring a lucrative drug to market.
Step 1: In late 2013, Janssen got the FDA to designate esketamine a “breakthrough therapy” because it showed the potential to reverse depression rapidly — a holy grail for suicidal patients, such as those in an emergency room. That potential was based on a 2-day study during which 30 patients were given esketamine intravenously.
“Breakthrough therapy” status puts drugs on a fast track to approval, with more frequent input from the FDA.
Step 2: But discussions between regulators and drug manufacturers can affect the amount and quality of evidence required by the agency. In the case of Spravato, they involved questions like “How many drugs must fail before a patient’s depression is considered intractable or ‘treatment resistant’?” and “How many successful clinical trials are necessary for FDA approval?”
Step 3: Any prior agreements can leave the FDA’s expert advisory committees hamstrung in reaching a verdict. Dr. Fiedorowicz abstained on Spravato because, though he considered Janssen’s study design flawed, the FDA had approved it.
The expert panel cleared the drug according to the evidence that the agency and Janssen had determined was sufficient. Matthew Rudorfer, MD, an associate director at the National Institute of Mental Health, concluded that the “benefits outweighed the risks.” Explaining his “yes” vote, he said, “I think we’re all agreeing on the very important, and sometimes life-or-death, risk of inadequately treated depression that factored into my equation.”
But others who also voted “yes” were more explicit in their qualms. “I don’t think that we really understand what happens when you take this week after week for weeks and months and years,” said Steven Meisel, PharmD, system director of medication safety for Fairview Health Services based in Minneapolis.
A Nasal Spray Offers A Path To A Patent
Spravato is available only under supervision at a certified facility where patients must be monitored for at least two hours after taking the drug to watch for side effects like dizziness, detachment from reality, and increased blood pressure, as well as to reduce the risk of abuse. Patients must take it with an oral antidepressant.
Despite those requirements, Janssen, part of Johnson & Johnson, defended its new offering. “Until the recent FDA approval of Spravato, health care providers haven’t had any new medication options,” Kristina Chang, a Janssen spokeswoman, wrote in an emailed statement.
Esketamine is the first new type of drug approved to treat severe depression in about three decades.
Although ketamine has been used off-label for years to treat depression and posttraumatic stress disorder, drugmakers saw little profit in doing the studies to prove to the FDA that it worked for that purpose. But a nasal spray of esketamine, which is derived from ketamine and is (in some studies) more potent, could be patented as a new drug.
Although Spravato costs more than $4,700 for the first month of treatment (not including the cost of monitoring or the oral antidepressant), insurers are more likely to reimburse for Spravato than for ketamine, since the latter is not approved for depression.
Shortly before the committee began voting, a study participant identifying herself only as “Patient 20015525” said, “I am offering real-world proof of efficacy, and that is I am both alive and here today.”
The drug did not work “for the majority of people who took it,” Dr. Meisel, the medication safety expert, said in an interview. “But for a subset of those for whom it did work, it was dramatic.”
Concerns About Testing Precedents
Those considerations apparently helped outweigh several scientific red flags that committee members called out during the hearing.
Although the drug had gotten breakthrough status because of its potential for results within 24 hours, the trials were not persuasive enough for the FDA to label it “rapid acting.”
The FDA typically requires that applicants provide at least two clinical trials demonstrating the drug’s efficacy, “each convincing on its own.” Janssen provided just one successful short-term, double-blind trial of esketamine. Two other trials it ran to test efficacy fell short.
To reach the two-trial threshold, the FDA broke its precedent for psychiatric drugs and allowed the company to count a trial conducted to study a different topic: relapse and remission trends. But, by definition, every patient in the trial had already taken and seen improvement from esketamine.
What’s more, that single positive efficacy trial showed just a 4-point improvement in depression symptoms, compared with the placebo treatment, on a 60-point scale some clinicians use to measure depression severity. Some committee members noted the trial wasn’t really blind since participants could recognize they were getting the drug from side effects like a temporary out-of-body sensation.
Finally, the FDA lowered the bar for “treatment-resistant depression.” Initially, for inclusion, trial participants would have had to have failed two classes of oral antidepressants.
Less than 2 years later, the FDA loosened that definition, saying a patient needed only to have taken two different pills, no matter the class.
Forty-nine of the 227 people who participated in Janssen’s only successful efficacy trial had failed just one class of oral antidepressants. “They weeded out the true treatment-resistant patients,” said Erick Turner, MD, a former FDA reviewer who serves on the committee but did not attend the meeting.
Six participants died during the studies, three by suicide. Janssen and the FDA dismissed the deaths as unrelated to the drug, noting the low number and lack of a pattern among hundreds of participants. They also pointed out that suicidal behavior is associated with severe depression – even though those who had suicidal ideation with some intent to act in the previous 6 months, or a history of suicidal behavior in the previous year, were excluded from the studies.
In a recent commentary in the American Journal of Psychiatry, Alan Schatzberg, MD, a Stanford (Calif.) University researcher who has studied ketamine, suggested there might be a link caused by “a protracted withdrawal reaction, as has been reported with opioids,” since ketamine appears to interact with the brain’s opioid receptors (Am J Psych. 2019. doi: 10.1176/appi.ajp.2019.19040423).
Kim Witczak, the committee’s consumer representative, found Janssen’s conclusion about the suicides unsatisfying. “I just feel like it was kind of a quick brush-over,” Ms. Witczak said in an interview. She voted against the drug.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For some patients, it also has dwelled in the shadows of conventional medicine as a depression treatment – prescribed by their doctors, but not approved for that purpose by the federal agency responsible for determining which treatments are “safe and effective.”
That effectively changed in March, when the Food and Drug Administration approved a ketamine cousin called esketamine, taken as a nasal spray, for patients with intractable depression. With that, the esketamine nasal spray, under the brand name Spravato, was introduced as a miracle drug – announced in press releases, celebrated on the evening news, and embraced by major health care providers like the Department of Veterans Affairs.
The problem, critics say, is that the drug’s manufacturer, Janssen, provided the FDA with at best modest evidence it worked and then only in limited trials. It presented no information about the safety of Spravato for long-term use beyond 60 weeks. And three patients who received the drug died by suicide during clinical trials, compared with none in the control group, which raised red flags Janssen and the FDA dismissed.
The FDA, under political pressure to rapidly green-light drugs that treat life-threatening conditions, approved it anyway. And, though Spravato’s appearance on the market was greeted with public applause, some deep misgivings were expressed at its day-long review meeting and in the agency’s own briefing materials, according to public recordings, documents, and interviews with participants, KHN found.
Jess Fiedorowicz, MD, director of the Mood Disorders Center at the University of Iowa, Iowa City, and a member of the FDA advisory committee that reviewed the drug, described its benefit as “almost certainly exaggerated” after hearing the evidence.
Dr. Fiedorowicz said he expected at least a split decision by the committee. “And then it went strongly in favor, which surprised me,” he said in an interview.
Esketamine’s trajectory to approval shows – step by step – how drugmakers can take advantage of shortcuts in the FDA process with the agency’s blessing and maneuver through safety and efficacy reviews to bring a lucrative drug to market.
Step 1: In late 2013, Janssen got the FDA to designate esketamine a “breakthrough therapy” because it showed the potential to reverse depression rapidly — a holy grail for suicidal patients, such as those in an emergency room. That potential was based on a 2-day study during which 30 patients were given esketamine intravenously.
“Breakthrough therapy” status puts drugs on a fast track to approval, with more frequent input from the FDA.
Step 2: But discussions between regulators and drug manufacturers can affect the amount and quality of evidence required by the agency. In the case of Spravato, they involved questions like “How many drugs must fail before a patient’s depression is considered intractable or ‘treatment resistant’?” and “How many successful clinical trials are necessary for FDA approval?”
Step 3: Any prior agreements can leave the FDA’s expert advisory committees hamstrung in reaching a verdict. Dr. Fiedorowicz abstained on Spravato because, though he considered Janssen’s study design flawed, the FDA had approved it.
The expert panel cleared the drug according to the evidence that the agency and Janssen had determined was sufficient. Matthew Rudorfer, MD, an associate director at the National Institute of Mental Health, concluded that the “benefits outweighed the risks.” Explaining his “yes” vote, he said, “I think we’re all agreeing on the very important, and sometimes life-or-death, risk of inadequately treated depression that factored into my equation.”
But others who also voted “yes” were more explicit in their qualms. “I don’t think that we really understand what happens when you take this week after week for weeks and months and years,” said Steven Meisel, PharmD, system director of medication safety for Fairview Health Services based in Minneapolis.
A Nasal Spray Offers A Path To A Patent
Spravato is available only under supervision at a certified facility where patients must be monitored for at least two hours after taking the drug to watch for side effects like dizziness, detachment from reality, and increased blood pressure, as well as to reduce the risk of abuse. Patients must take it with an oral antidepressant.
Despite those requirements, Janssen, part of Johnson & Johnson, defended its new offering. “Until the recent FDA approval of Spravato, health care providers haven’t had any new medication options,” Kristina Chang, a Janssen spokeswoman, wrote in an emailed statement.
Esketamine is the first new type of drug approved to treat severe depression in about three decades.
Although ketamine has been used off-label for years to treat depression and posttraumatic stress disorder, drugmakers saw little profit in doing the studies to prove to the FDA that it worked for that purpose. But a nasal spray of esketamine, which is derived from ketamine and is (in some studies) more potent, could be patented as a new drug.
Although Spravato costs more than $4,700 for the first month of treatment (not including the cost of monitoring or the oral antidepressant), insurers are more likely to reimburse for Spravato than for ketamine, since the latter is not approved for depression.
Shortly before the committee began voting, a study participant identifying herself only as “Patient 20015525” said, “I am offering real-world proof of efficacy, and that is I am both alive and here today.”
The drug did not work “for the majority of people who took it,” Dr. Meisel, the medication safety expert, said in an interview. “But for a subset of those for whom it did work, it was dramatic.”
Concerns About Testing Precedents
Those considerations apparently helped outweigh several scientific red flags that committee members called out during the hearing.
Although the drug had gotten breakthrough status because of its potential for results within 24 hours, the trials were not persuasive enough for the FDA to label it “rapid acting.”
The FDA typically requires that applicants provide at least two clinical trials demonstrating the drug’s efficacy, “each convincing on its own.” Janssen provided just one successful short-term, double-blind trial of esketamine. Two other trials it ran to test efficacy fell short.
To reach the two-trial threshold, the FDA broke its precedent for psychiatric drugs and allowed the company to count a trial conducted to study a different topic: relapse and remission trends. But, by definition, every patient in the trial had already taken and seen improvement from esketamine.
What’s more, that single positive efficacy trial showed just a 4-point improvement in depression symptoms, compared with the placebo treatment, on a 60-point scale some clinicians use to measure depression severity. Some committee members noted the trial wasn’t really blind since participants could recognize they were getting the drug from side effects like a temporary out-of-body sensation.
Finally, the FDA lowered the bar for “treatment-resistant depression.” Initially, for inclusion, trial participants would have had to have failed two classes of oral antidepressants.
Less than 2 years later, the FDA loosened that definition, saying a patient needed only to have taken two different pills, no matter the class.
Forty-nine of the 227 people who participated in Janssen’s only successful efficacy trial had failed just one class of oral antidepressants. “They weeded out the true treatment-resistant patients,” said Erick Turner, MD, a former FDA reviewer who serves on the committee but did not attend the meeting.
Six participants died during the studies, three by suicide. Janssen and the FDA dismissed the deaths as unrelated to the drug, noting the low number and lack of a pattern among hundreds of participants. They also pointed out that suicidal behavior is associated with severe depression – even though those who had suicidal ideation with some intent to act in the previous 6 months, or a history of suicidal behavior in the previous year, were excluded from the studies.
In a recent commentary in the American Journal of Psychiatry, Alan Schatzberg, MD, a Stanford (Calif.) University researcher who has studied ketamine, suggested there might be a link caused by “a protracted withdrawal reaction, as has been reported with opioids,” since ketamine appears to interact with the brain’s opioid receptors (Am J Psych. 2019. doi: 10.1176/appi.ajp.2019.19040423).
Kim Witczak, the committee’s consumer representative, found Janssen’s conclusion about the suicides unsatisfying. “I just feel like it was kind of a quick brush-over,” Ms. Witczak said in an interview. She voted against the drug.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Intranasal esketamine plus antidepressant deflects relapse
Esketamine nasal spray used with an oral antidepressant was significantly more effective at delaying a relapse of depression compared with placebo, based on data from 297 adults in remission.
Patients with treatment-resistant depression are more likely to relapse, wrote Ella J. Daly, MD, of Janssen Research and Development, Titusville, N.J., and colleagues.
In the SUSTAIN-1 study, published in JAMA Psychiatry, the researchers randomized 297 adults in the maintenance phase of depression treatment to esketamine hydrochloride or placebo. The average age of the patients was 46 years, and 66% were female.
among the 176 patients who achieved stable remission. In addition, relapse occurred in 25.8% in the esketamine and antidepressant group and 57.6 in the antidepressant and placebo among the patients who achieved stable response.
The median duration esketamine use during the maintenance phase was 17.7 weeks among patients who achieved stable remission and 19.4 among those who achieved stable response.
The study was designed to include a 4-week screening and prospective observation phase, a 4-week open-label induction phase, a 12-week optimization phase, a maintenance phase, and a 2-week posttreatment follow-up phase.
The most common adverse events reported by esketamine patients were transient dysgeusia, vertigo, dissociation, somnolence, and dizziness. Most of these effects were moderate; no cases of respiratory depression, interstitial cystitis, or death were reported.
The results were limited by several factors, including the transient effects of esketamine that made blinding difficult, the researchers noted. However, the findings support the safety of the spray and “significant, clinically meaningful superiority” of the spray, compared with placebo, for relapse prevention in patients with treatment-resistant depression, they concluded.
Janssen Research and Development funded the study. Dr. Daly and several coauthors are employees of the company.
SOURCE: Daly E et al. JAMA Psychiatry. 2019 Jun 5. doi: 10.1001/jamapsychiatry.2019.1189.
Esketamine nasal spray used with an oral antidepressant was significantly more effective at delaying a relapse of depression compared with placebo, based on data from 297 adults in remission.
Patients with treatment-resistant depression are more likely to relapse, wrote Ella J. Daly, MD, of Janssen Research and Development, Titusville, N.J., and colleagues.
In the SUSTAIN-1 study, published in JAMA Psychiatry, the researchers randomized 297 adults in the maintenance phase of depression treatment to esketamine hydrochloride or placebo. The average age of the patients was 46 years, and 66% were female.
among the 176 patients who achieved stable remission. In addition, relapse occurred in 25.8% in the esketamine and antidepressant group and 57.6 in the antidepressant and placebo among the patients who achieved stable response.
The median duration esketamine use during the maintenance phase was 17.7 weeks among patients who achieved stable remission and 19.4 among those who achieved stable response.
The study was designed to include a 4-week screening and prospective observation phase, a 4-week open-label induction phase, a 12-week optimization phase, a maintenance phase, and a 2-week posttreatment follow-up phase.
The most common adverse events reported by esketamine patients were transient dysgeusia, vertigo, dissociation, somnolence, and dizziness. Most of these effects were moderate; no cases of respiratory depression, interstitial cystitis, or death were reported.
The results were limited by several factors, including the transient effects of esketamine that made blinding difficult, the researchers noted. However, the findings support the safety of the spray and “significant, clinically meaningful superiority” of the spray, compared with placebo, for relapse prevention in patients with treatment-resistant depression, they concluded.
Janssen Research and Development funded the study. Dr. Daly and several coauthors are employees of the company.
SOURCE: Daly E et al. JAMA Psychiatry. 2019 Jun 5. doi: 10.1001/jamapsychiatry.2019.1189.
Esketamine nasal spray used with an oral antidepressant was significantly more effective at delaying a relapse of depression compared with placebo, based on data from 297 adults in remission.
Patients with treatment-resistant depression are more likely to relapse, wrote Ella J. Daly, MD, of Janssen Research and Development, Titusville, N.J., and colleagues.
In the SUSTAIN-1 study, published in JAMA Psychiatry, the researchers randomized 297 adults in the maintenance phase of depression treatment to esketamine hydrochloride or placebo. The average age of the patients was 46 years, and 66% were female.
among the 176 patients who achieved stable remission. In addition, relapse occurred in 25.8% in the esketamine and antidepressant group and 57.6 in the antidepressant and placebo among the patients who achieved stable response.
The median duration esketamine use during the maintenance phase was 17.7 weeks among patients who achieved stable remission and 19.4 among those who achieved stable response.
The study was designed to include a 4-week screening and prospective observation phase, a 4-week open-label induction phase, a 12-week optimization phase, a maintenance phase, and a 2-week posttreatment follow-up phase.
The most common adverse events reported by esketamine patients were transient dysgeusia, vertigo, dissociation, somnolence, and dizziness. Most of these effects were moderate; no cases of respiratory depression, interstitial cystitis, or death were reported.
The results were limited by several factors, including the transient effects of esketamine that made blinding difficult, the researchers noted. However, the findings support the safety of the spray and “significant, clinically meaningful superiority” of the spray, compared with placebo, for relapse prevention in patients with treatment-resistant depression, they concluded.
Janssen Research and Development funded the study. Dr. Daly and several coauthors are employees of the company.
SOURCE: Daly E et al. JAMA Psychiatry. 2019 Jun 5. doi: 10.1001/jamapsychiatry.2019.1189.
FROM JAMA PSYCHIATRY
Medical community confronts physician depression, suicide
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
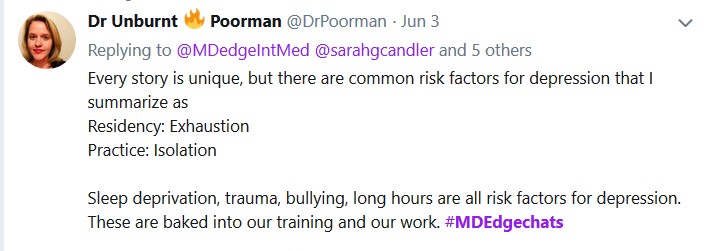
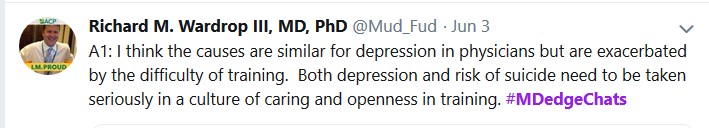
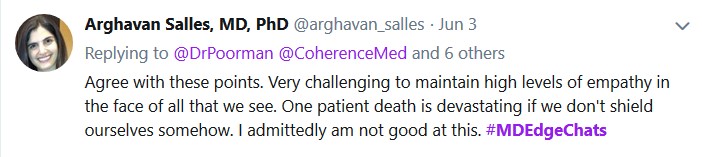
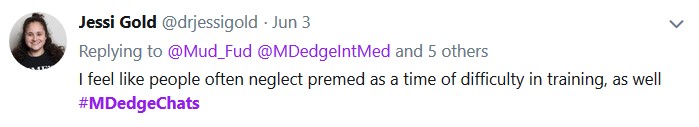
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.
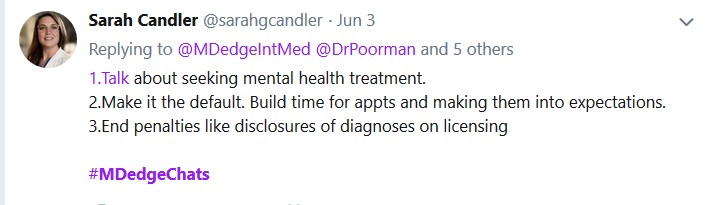
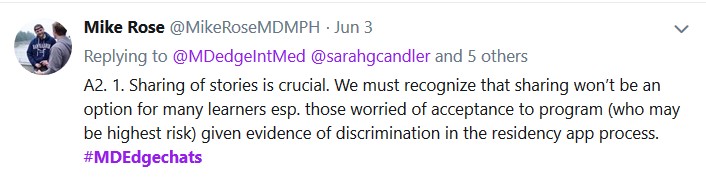
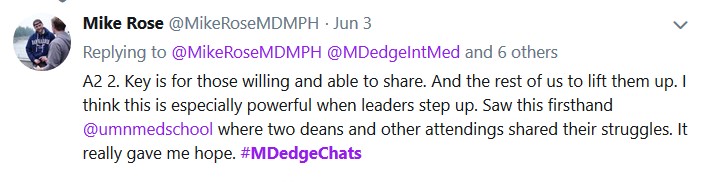

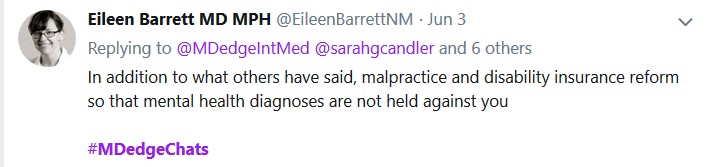
Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


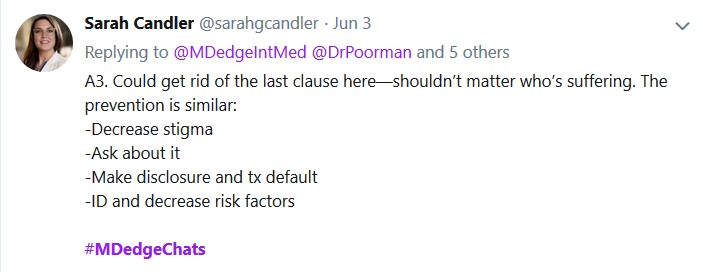
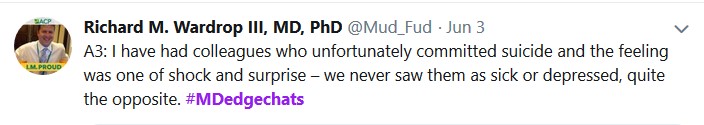
Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.
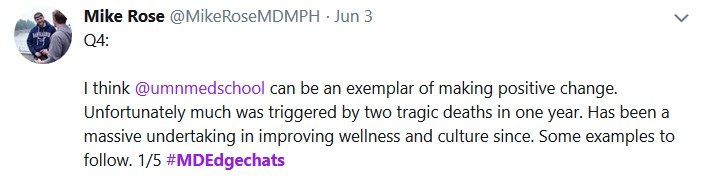
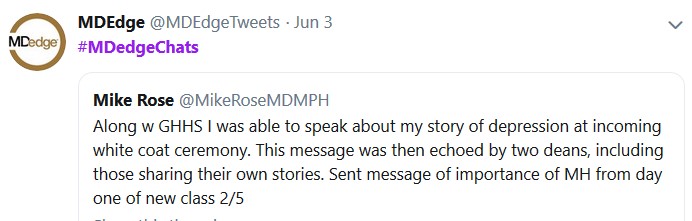
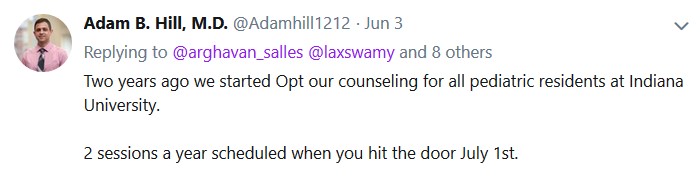
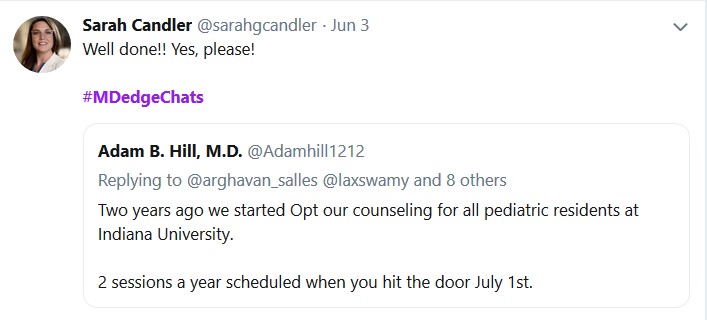


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
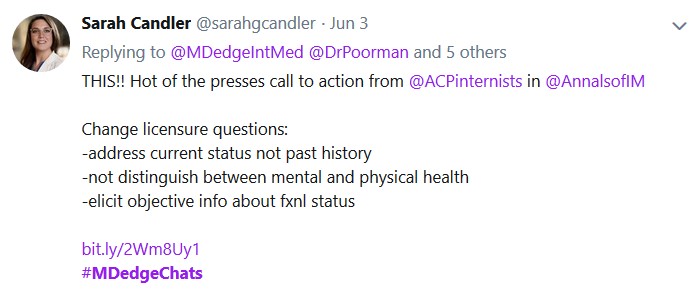
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
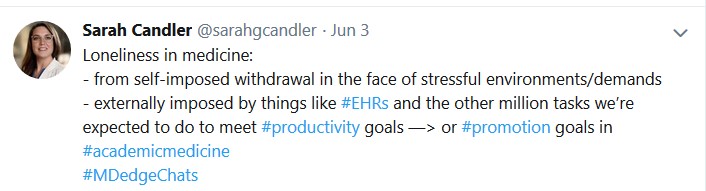
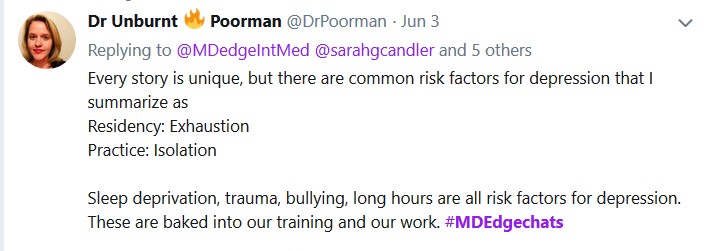
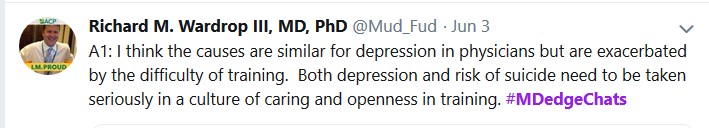
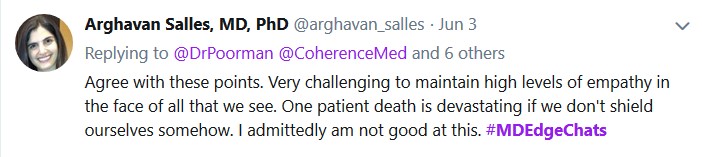
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.
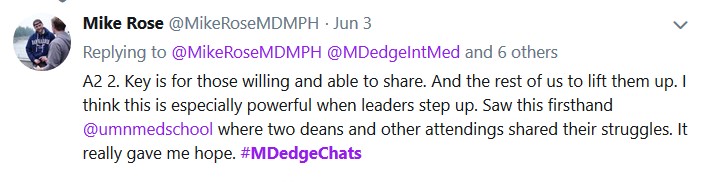

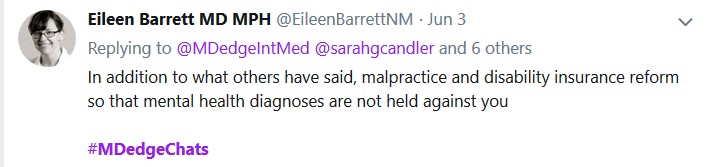
Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


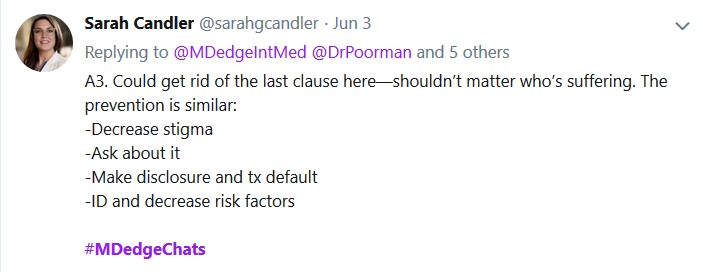
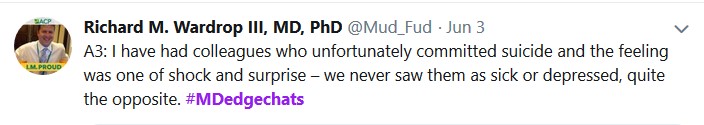
Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.
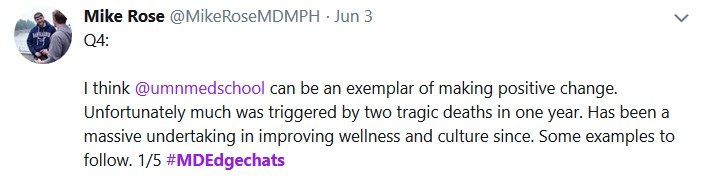
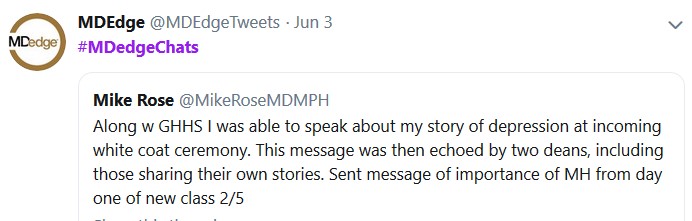
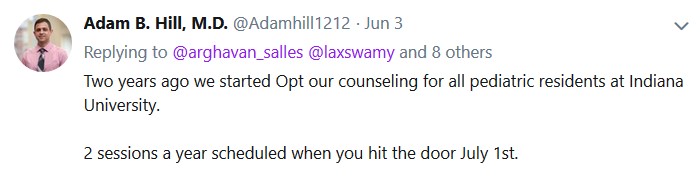


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
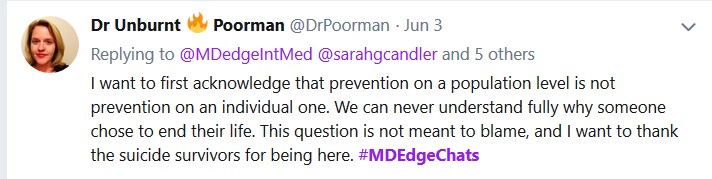
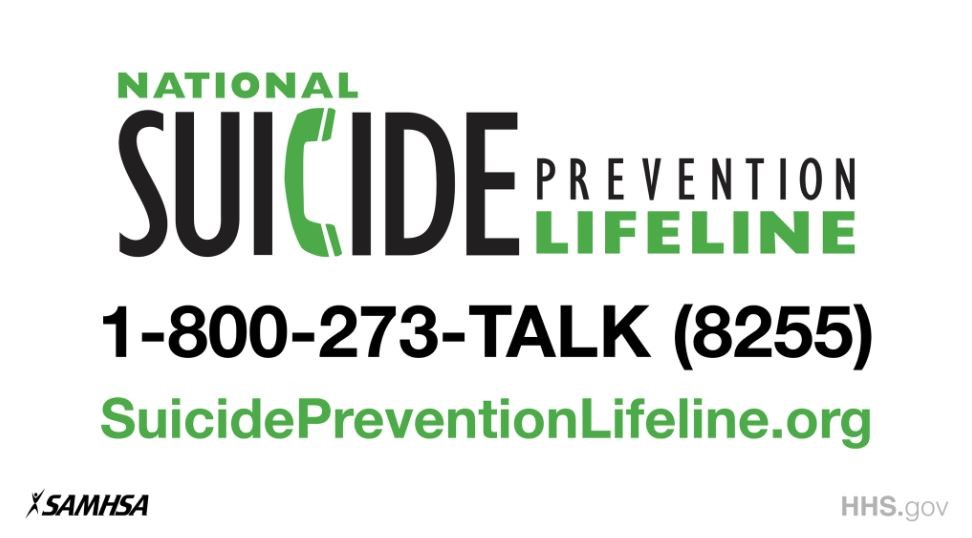
Many physicians work long hours and may ignore the fatigue and emotional toll that comes with those pressures. The stress cannot only lead to crippling depression but also to declined mental health and even thoughts of suicide.
Each year, an estimated 400 physicians take their own lives, mostly because of depression and stress, according to the West Journal of Emergency Medicine.
MDedge Internal Medicine recently hosted a Twitter conversation (#MDedgeChats) on how the health care community can address this emerging crisis and help their colleagues understand that they are not alone. Two primary care physicians — Sarah Candler, MD, and Elisabeth Poorman, MD — led the conversation, with guests Michael Rose, MD, Arghavan Salles, MD, Richard M. Wardrop III, MD, Jessica Gold, MD, and Janae Sharp.
Throughout the conversation, physicians encouraged other medical professionals to seek help if it is needed. “If you don’t feel comfortable sharing with your team, feel free to share with folks you met here,” Dr. Candler wrote. “Please seek professional solace with a therapist! That’s what this is about – the support to do what you need for yourself. Good doctors take care of themselves, too.”
These issues are not just important in the medical community “because everyone will get sick, and we are failing each other. We are failing our patients and our communities when we won’t fight for change. The center will not hold here,” said Dr. Elizabeth Poorman.
The following is an edited version of the discussion.
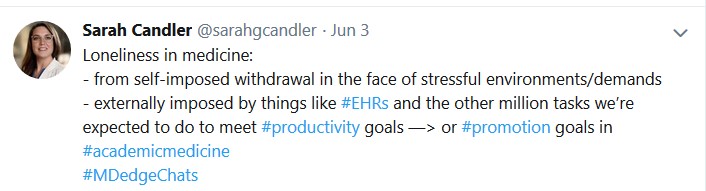
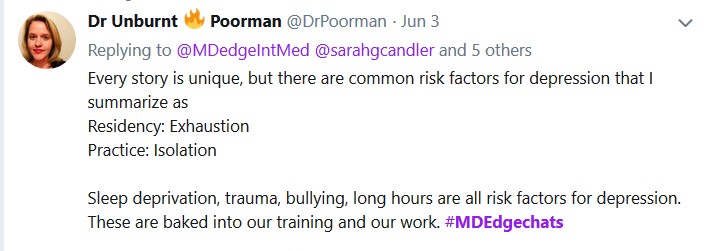
Question 2: "How can we end stigma against seeking mental health treatment among physicians?" is on the next page.
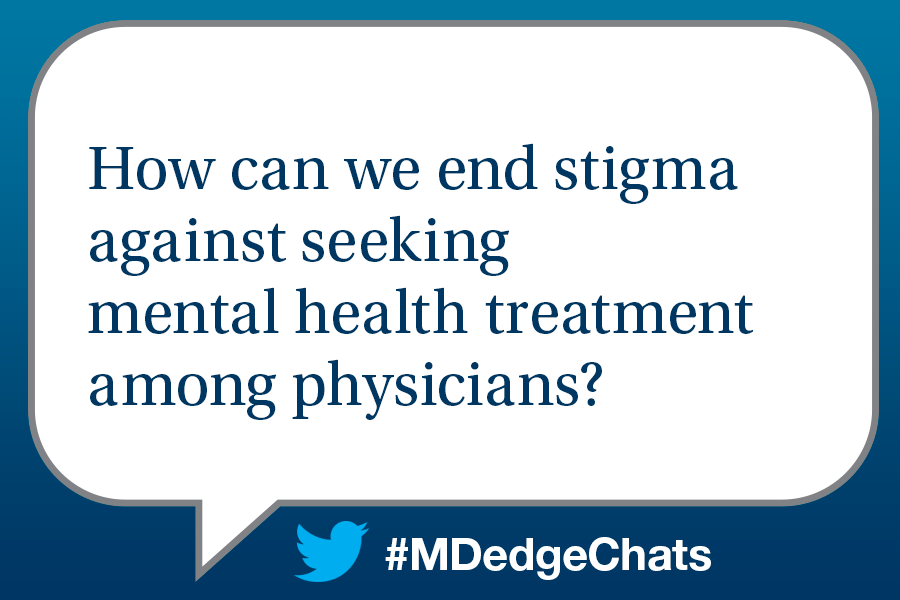
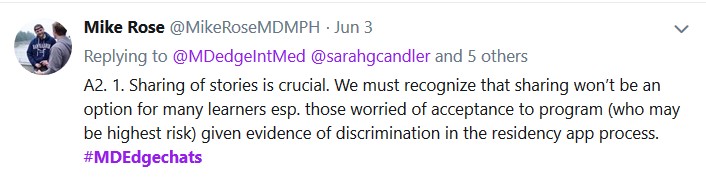
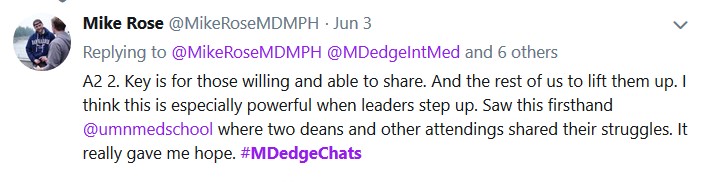

Question 3: "How can we prevent depression and suicide among medical students and physicians" is on the next page.


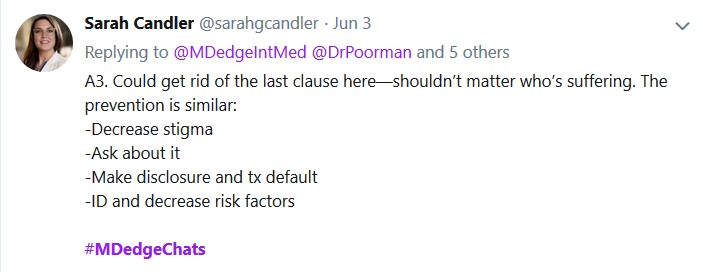
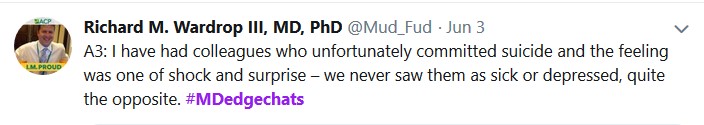
Question 4: "Which institutions or programs are exemplars in providing resources to improve mental health?" is on the next page.


Question 5: "What organizational and political changes are likely to reduce physician suicides?" is on the next page.
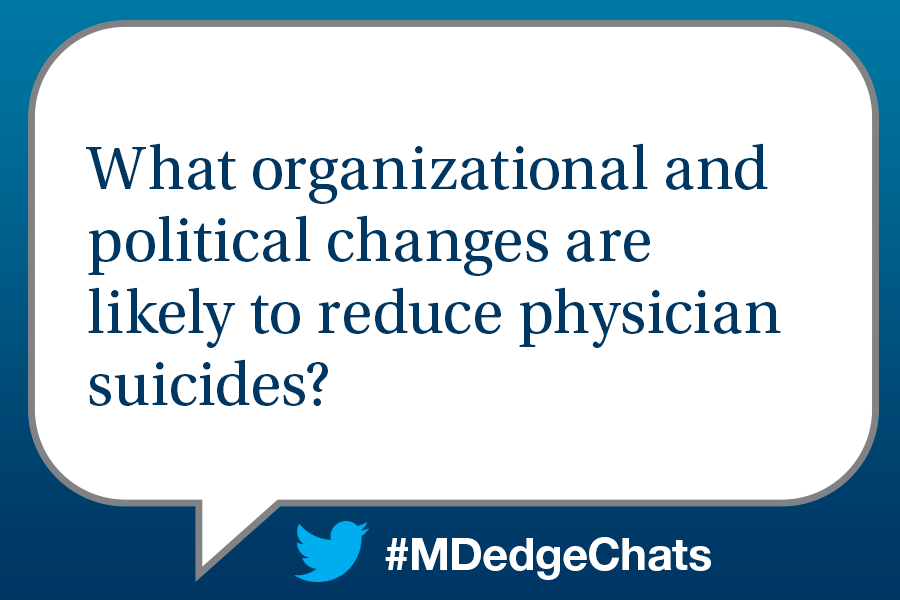
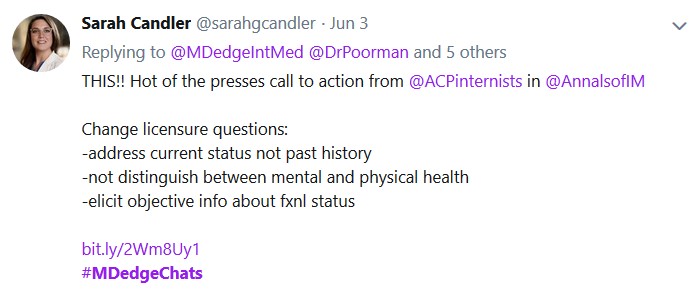
Gun ownership practices linked to soldier suicide risk
U.S. soldiers who own firearms, store a loaded gun at home, or carry a gun publicly when not on duty are at significantly greater risk of suicide death, a case-control study of 135 U.S. Army soldiers who died by suicide shows.
“Our findings concurred with earlier studies by showing that factors beyond ownership of a firearm were associated with an increased risk of suicide,” wrote Catherine L. Dempsey, PhD, MPH, and her coauthors.
Since 2004, the rate of suicide deaths among Army soldiers has exceeded the rate of combat deaths each year, which prompted Dr. Dempsey, of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences, Bethesda, Md., and her coauthors to investigate whether increased access to firearms might be associated with an increased risk of suicide. The study was published by JAMA Network Open.
In the study, the researchers interviewed the next of kin or supervisors of 135 Army soldiers who had taken their own lives while on active duty between 2011 and 2013, 55% of whom used firearms to do so. They compared those findings with those 137 controls matched for suicide propensity based on sociodemographic and Army history risk factors, and 118 soldiers who had experienced suicidal ideation in the past year.
This analysis showed that soldiers who had stored a loaded gun with ammunition at home, or who had carried a personal gun in public had nearly fourfold higher odds of suicide (odds ratio, 3.9; P = .002), compared with propensity-matched controls.
Similarly, those who owned one or more handguns, stored a gun loaded with ammunition at home, and carried a personal gun in public had a greater than threefold odds of suicide.
, four times more likely to store that gun loaded with ammunition at home, and three times more likely to carry a gun in public, compared with controls.
There was the suggestion that the use of safety locks at home was protective, but this did not reach statistical significance.
However, the study did not find significant differences in firearm accessibility characteristics between the soldiers who died by suicide, and the controls with suicidal ideation.
“Some current theories of suicide (eg., the interpersonal theory of suicide) suggest that fatal suicidal behavior results require not only the presence of suicidal desire but also a developed capability or capacity for suicidal behavior,” the authors wrote. “According to the interpersonal theory of suicide, this capability for lethal self-injury is acquired through repeated exposure to painful and fear-inducing experiences, thus habituating an individual to the pain and fear required to enact a fatal suicide attempt.”
Dr. Dempsey and her coauthors argued that their study supported a continued focus on “means restriction” counseling; limiting or removing access to lethal methods for suicide; and “motivational interviewing.”
They cited the fairly small sample size and relatively small response rates to surveys as limitations. However, they wrote, the response rates “were high for multi-informant interviews conducted within a military population.”
The study was supported by the U.S. Department of the Army, U.S. Department of Defense, U.S. Department of Health & Human Services, National Institutes of Health, and National Institute of Mental Health. One author declared grants from the Military Suicide Research Consortium outside the submitted work, and one author declared support, consultancies, and advisory board positions with the pharmaceutical industry, and co-ownership of a mental health market research firm. No other conflicts of interest were declared.
SOURCE: Dempsey CL et al. JAMA Netw Open. 2019 Jun 7. doi: 10.1001/jamanetworkopen.2019.5383.
These findings add to the growing body of evidence that firearm-related behaviors, beyond just gun ownership, may influence suicide risk, and support the most evidence-based and conceptually sound recommendation for suicide prevention, which is to remove the firearm from the home.
There are some limitations to this study. For example, the validity of the “psychological autopsy” approach used in the study has not been determined, and there is also a question mark over the accuracy of family members’ reports about gun ownership and storage practices. Despite this, the study provides support for recommendations for a change in firearm behaviors to reduce the risk of suicide.
Joseph A. Simonetti, MD, MPH, is affiliated with the Rocky Mountain Mental Illness, Research, Education and Clinical Center for Suicide Prevention at the Rocky Mountain Regional VA Medical Center, Aurora, Colo. Ali Rowhani-Rahbar, MD, MPH, PhD, is affiliated with the Harborview Injury Prevention and Research Center at the University of Washington, Seattle. Those comments are adapted from an accompanying editorial (JAMA Netw Open. 2019. Jun 7. doi: 10.1001/jamanetworkopen.2019.5400). No conflicts of interest were declared.
These findings add to the growing body of evidence that firearm-related behaviors, beyond just gun ownership, may influence suicide risk, and support the most evidence-based and conceptually sound recommendation for suicide prevention, which is to remove the firearm from the home.
There are some limitations to this study. For example, the validity of the “psychological autopsy” approach used in the study has not been determined, and there is also a question mark over the accuracy of family members’ reports about gun ownership and storage practices. Despite this, the study provides support for recommendations for a change in firearm behaviors to reduce the risk of suicide.
Joseph A. Simonetti, MD, MPH, is affiliated with the Rocky Mountain Mental Illness, Research, Education and Clinical Center for Suicide Prevention at the Rocky Mountain Regional VA Medical Center, Aurora, Colo. Ali Rowhani-Rahbar, MD, MPH, PhD, is affiliated with the Harborview Injury Prevention and Research Center at the University of Washington, Seattle. Those comments are adapted from an accompanying editorial (JAMA Netw Open. 2019. Jun 7. doi: 10.1001/jamanetworkopen.2019.5400). No conflicts of interest were declared.
These findings add to the growing body of evidence that firearm-related behaviors, beyond just gun ownership, may influence suicide risk, and support the most evidence-based and conceptually sound recommendation for suicide prevention, which is to remove the firearm from the home.
There are some limitations to this study. For example, the validity of the “psychological autopsy” approach used in the study has not been determined, and there is also a question mark over the accuracy of family members’ reports about gun ownership and storage practices. Despite this, the study provides support for recommendations for a change in firearm behaviors to reduce the risk of suicide.
Joseph A. Simonetti, MD, MPH, is affiliated with the Rocky Mountain Mental Illness, Research, Education and Clinical Center for Suicide Prevention at the Rocky Mountain Regional VA Medical Center, Aurora, Colo. Ali Rowhani-Rahbar, MD, MPH, PhD, is affiliated with the Harborview Injury Prevention and Research Center at the University of Washington, Seattle. Those comments are adapted from an accompanying editorial (JAMA Netw Open. 2019. Jun 7. doi: 10.1001/jamanetworkopen.2019.5400). No conflicts of interest were declared.
U.S. soldiers who own firearms, store a loaded gun at home, or carry a gun publicly when not on duty are at significantly greater risk of suicide death, a case-control study of 135 U.S. Army soldiers who died by suicide shows.
“Our findings concurred with earlier studies by showing that factors beyond ownership of a firearm were associated with an increased risk of suicide,” wrote Catherine L. Dempsey, PhD, MPH, and her coauthors.
Since 2004, the rate of suicide deaths among Army soldiers has exceeded the rate of combat deaths each year, which prompted Dr. Dempsey, of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences, Bethesda, Md., and her coauthors to investigate whether increased access to firearms might be associated with an increased risk of suicide. The study was published by JAMA Network Open.
In the study, the researchers interviewed the next of kin or supervisors of 135 Army soldiers who had taken their own lives while on active duty between 2011 and 2013, 55% of whom used firearms to do so. They compared those findings with those 137 controls matched for suicide propensity based on sociodemographic and Army history risk factors, and 118 soldiers who had experienced suicidal ideation in the past year.
This analysis showed that soldiers who had stored a loaded gun with ammunition at home, or who had carried a personal gun in public had nearly fourfold higher odds of suicide (odds ratio, 3.9; P = .002), compared with propensity-matched controls.
Similarly, those who owned one or more handguns, stored a gun loaded with ammunition at home, and carried a personal gun in public had a greater than threefold odds of suicide.
, four times more likely to store that gun loaded with ammunition at home, and three times more likely to carry a gun in public, compared with controls.
There was the suggestion that the use of safety locks at home was protective, but this did not reach statistical significance.
However, the study did not find significant differences in firearm accessibility characteristics between the soldiers who died by suicide, and the controls with suicidal ideation.
“Some current theories of suicide (eg., the interpersonal theory of suicide) suggest that fatal suicidal behavior results require not only the presence of suicidal desire but also a developed capability or capacity for suicidal behavior,” the authors wrote. “According to the interpersonal theory of suicide, this capability for lethal self-injury is acquired through repeated exposure to painful and fear-inducing experiences, thus habituating an individual to the pain and fear required to enact a fatal suicide attempt.”
Dr. Dempsey and her coauthors argued that their study supported a continued focus on “means restriction” counseling; limiting or removing access to lethal methods for suicide; and “motivational interviewing.”
They cited the fairly small sample size and relatively small response rates to surveys as limitations. However, they wrote, the response rates “were high for multi-informant interviews conducted within a military population.”
The study was supported by the U.S. Department of the Army, U.S. Department of Defense, U.S. Department of Health & Human Services, National Institutes of Health, and National Institute of Mental Health. One author declared grants from the Military Suicide Research Consortium outside the submitted work, and one author declared support, consultancies, and advisory board positions with the pharmaceutical industry, and co-ownership of a mental health market research firm. No other conflicts of interest were declared.
SOURCE: Dempsey CL et al. JAMA Netw Open. 2019 Jun 7. doi: 10.1001/jamanetworkopen.2019.5383.
U.S. soldiers who own firearms, store a loaded gun at home, or carry a gun publicly when not on duty are at significantly greater risk of suicide death, a case-control study of 135 U.S. Army soldiers who died by suicide shows.
“Our findings concurred with earlier studies by showing that factors beyond ownership of a firearm were associated with an increased risk of suicide,” wrote Catherine L. Dempsey, PhD, MPH, and her coauthors.
Since 2004, the rate of suicide deaths among Army soldiers has exceeded the rate of combat deaths each year, which prompted Dr. Dempsey, of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences, Bethesda, Md., and her coauthors to investigate whether increased access to firearms might be associated with an increased risk of suicide. The study was published by JAMA Network Open.
In the study, the researchers interviewed the next of kin or supervisors of 135 Army soldiers who had taken their own lives while on active duty between 2011 and 2013, 55% of whom used firearms to do so. They compared those findings with those 137 controls matched for suicide propensity based on sociodemographic and Army history risk factors, and 118 soldiers who had experienced suicidal ideation in the past year.
This analysis showed that soldiers who had stored a loaded gun with ammunition at home, or who had carried a personal gun in public had nearly fourfold higher odds of suicide (odds ratio, 3.9; P = .002), compared with propensity-matched controls.
Similarly, those who owned one or more handguns, stored a gun loaded with ammunition at home, and carried a personal gun in public had a greater than threefold odds of suicide.
, four times more likely to store that gun loaded with ammunition at home, and three times more likely to carry a gun in public, compared with controls.
There was the suggestion that the use of safety locks at home was protective, but this did not reach statistical significance.
However, the study did not find significant differences in firearm accessibility characteristics between the soldiers who died by suicide, and the controls with suicidal ideation.
“Some current theories of suicide (eg., the interpersonal theory of suicide) suggest that fatal suicidal behavior results require not only the presence of suicidal desire but also a developed capability or capacity for suicidal behavior,” the authors wrote. “According to the interpersonal theory of suicide, this capability for lethal self-injury is acquired through repeated exposure to painful and fear-inducing experiences, thus habituating an individual to the pain and fear required to enact a fatal suicide attempt.”
Dr. Dempsey and her coauthors argued that their study supported a continued focus on “means restriction” counseling; limiting or removing access to lethal methods for suicide; and “motivational interviewing.”
They cited the fairly small sample size and relatively small response rates to surveys as limitations. However, they wrote, the response rates “were high for multi-informant interviews conducted within a military population.”
The study was supported by the U.S. Department of the Army, U.S. Department of Defense, U.S. Department of Health & Human Services, National Institutes of Health, and National Institute of Mental Health. One author declared grants from the Military Suicide Research Consortium outside the submitted work, and one author declared support, consultancies, and advisory board positions with the pharmaceutical industry, and co-ownership of a mental health market research firm. No other conflicts of interest were declared.
SOURCE: Dempsey CL et al. JAMA Netw Open. 2019 Jun 7. doi: 10.1001/jamanetworkopen.2019.5383.
FROM JAMA NETWORK OPEN
Review clarifies depression, anxiety risk among hidradenitis suppurativa patients
and meta-analysis of more than 40,000 adults.
Previous studies of psychiatric comorbidities in HS patients have suggested an increased rate of depression, anxiety, and suicide risk, but have varied in methodology. “Therefore, the exact magnitude of the prevalence and odds of depression and anxiety in patients with HS is unclear,” wrote Myrela O. Machado, MD, of the division of dermatology, Women’s College Hospital, Toronto, and colleagues.
In a review of PubMed/MEDLINE, Embase, and PsycINFO electronic databases through July 2018, the researchers identified 10 studies comprising 40,307 adults with HS. The overall prevalence of depression was 16.9%, and in the studies that included a comparison group, the odds ratio for depression was 1.84 for HS patients, compared with controls who did not have HS. The overall prevalence of anxiety was 4.9%, but data were insufficient to determine an odds ratio for anxiety. The study was published in JAMA Dermatology.
All 10 studies assessed depression; 4 assessed anxiety. In subgroup analyses, the prevalence of depression was 11.9% in studies with a diagnosis based on clinical criteria and 26.8% in studies that used a screening instrument. The prevalence was 25.9% for outpatients with HS.
“Although our findings indicate that depression and anxiety may be common among people with HS, whether there is a causal relationship in those associations remains to be proved,” the researchers wrote.
However, they noted, “the consequences of depression and anxiety on HS-related outcomes have recently received more attention.”
The study findings were limited by several factors including the lack of data from structured diagnostic interviews, variation in methodological quality, and variation in comparison groups across studies, as well as a high level of heterogeneity across studies, the researchers noted. However, the results support the need to recognize and treat psychiatric conditions in HS patients, and to develop new management strategies, they said.
Dr. Machado had no financial conflicts to disclose. Several coauthors disclosed relationships with Galderma, LEO Pharma, Janssen, Novartis, AbbVie, Celgene, Naos, Lilly, Sanofi, Valeant, and La Roche-Posay.
SOURCE: Machado M et al. JAMA Dermatol. 2019 June 5. doi: 10.1001/jamadermatol.2019.0759.
and meta-analysis of more than 40,000 adults.
Previous studies of psychiatric comorbidities in HS patients have suggested an increased rate of depression, anxiety, and suicide risk, but have varied in methodology. “Therefore, the exact magnitude of the prevalence and odds of depression and anxiety in patients with HS is unclear,” wrote Myrela O. Machado, MD, of the division of dermatology, Women’s College Hospital, Toronto, and colleagues.
In a review of PubMed/MEDLINE, Embase, and PsycINFO electronic databases through July 2018, the researchers identified 10 studies comprising 40,307 adults with HS. The overall prevalence of depression was 16.9%, and in the studies that included a comparison group, the odds ratio for depression was 1.84 for HS patients, compared with controls who did not have HS. The overall prevalence of anxiety was 4.9%, but data were insufficient to determine an odds ratio for anxiety. The study was published in JAMA Dermatology.
All 10 studies assessed depression; 4 assessed anxiety. In subgroup analyses, the prevalence of depression was 11.9% in studies with a diagnosis based on clinical criteria and 26.8% in studies that used a screening instrument. The prevalence was 25.9% for outpatients with HS.
“Although our findings indicate that depression and anxiety may be common among people with HS, whether there is a causal relationship in those associations remains to be proved,” the researchers wrote.
However, they noted, “the consequences of depression and anxiety on HS-related outcomes have recently received more attention.”
The study findings were limited by several factors including the lack of data from structured diagnostic interviews, variation in methodological quality, and variation in comparison groups across studies, as well as a high level of heterogeneity across studies, the researchers noted. However, the results support the need to recognize and treat psychiatric conditions in HS patients, and to develop new management strategies, they said.
Dr. Machado had no financial conflicts to disclose. Several coauthors disclosed relationships with Galderma, LEO Pharma, Janssen, Novartis, AbbVie, Celgene, Naos, Lilly, Sanofi, Valeant, and La Roche-Posay.
SOURCE: Machado M et al. JAMA Dermatol. 2019 June 5. doi: 10.1001/jamadermatol.2019.0759.
and meta-analysis of more than 40,000 adults.
Previous studies of psychiatric comorbidities in HS patients have suggested an increased rate of depression, anxiety, and suicide risk, but have varied in methodology. “Therefore, the exact magnitude of the prevalence and odds of depression and anxiety in patients with HS is unclear,” wrote Myrela O. Machado, MD, of the division of dermatology, Women’s College Hospital, Toronto, and colleagues.
In a review of PubMed/MEDLINE, Embase, and PsycINFO electronic databases through July 2018, the researchers identified 10 studies comprising 40,307 adults with HS. The overall prevalence of depression was 16.9%, and in the studies that included a comparison group, the odds ratio for depression was 1.84 for HS patients, compared with controls who did not have HS. The overall prevalence of anxiety was 4.9%, but data were insufficient to determine an odds ratio for anxiety. The study was published in JAMA Dermatology.
All 10 studies assessed depression; 4 assessed anxiety. In subgroup analyses, the prevalence of depression was 11.9% in studies with a diagnosis based on clinical criteria and 26.8% in studies that used a screening instrument. The prevalence was 25.9% for outpatients with HS.
“Although our findings indicate that depression and anxiety may be common among people with HS, whether there is a causal relationship in those associations remains to be proved,” the researchers wrote.
However, they noted, “the consequences of depression and anxiety on HS-related outcomes have recently received more attention.”
The study findings were limited by several factors including the lack of data from structured diagnostic interviews, variation in methodological quality, and variation in comparison groups across studies, as well as a high level of heterogeneity across studies, the researchers noted. However, the results support the need to recognize and treat psychiatric conditions in HS patients, and to develop new management strategies, they said.
Dr. Machado had no financial conflicts to disclose. Several coauthors disclosed relationships with Galderma, LEO Pharma, Janssen, Novartis, AbbVie, Celgene, Naos, Lilly, Sanofi, Valeant, and La Roche-Posay.
SOURCE: Machado M et al. JAMA Dermatol. 2019 June 5. doi: 10.1001/jamadermatol.2019.0759.
FROM JAMA DERMATOLOGY
Increasingly violent storms may strain mental health
SAN FRANCISCO – Longer and more powerful storms caused by climate change will put increasing pressure on mental health care. The unusually powerful 2017 hurricane season, highlighted by damage done to Puerto Rico by Hurricane Maria and to Houston by Hurricane Harvey, may serve as a harbinger of more intense storm seasons to come, according to James M. Shultz, PhD, director of the Center for Disaster and Extreme Event Preparedness at the University of Miami.
Overall, 2017 was something of a “perfect storm” season. “We’ve had predictions about what climate change would do to extreme storms. It was quite exceptional in bringing together all of the elements we have seen predicted by climate scientists,” Dr. Shultz said during a press conference at the annual meeting of the American Psychiatric Association. Study coauthor Zelde Espinel, MD, MPH, also of the center at the university, presented the poster at the meeting.
Aside from greater intensity, climate change is causing a slowing of storms once they make landfall, which increases rainfall and the risks of floods. Nowhere was that more apparent than in Houston in the aftermath of Hurricane Harvey, where tens of thousands of spontaneous rescue efforts arose to rescue people trapped in their homes.
These storms put tremendous pressure on health care systems, as in Puerto Rico when Hurricane Maria knocked out electrical grids, some of which stayed down for 6 months or more. This kind of upheaval interrupts health care infrastructure, including psychiatric services, leaving vulnerable individuals at even greater risk.
Then there are the direct and indirect effects of storms on mental health. When air conditioning and fans are inoperative because of power outages, people get exposed to extreme and relentless heat. They may experience food and water shortages. In worst cases, they may be forced out of their homes on a temporary or even permanent basis. Dr. Shultz recounted research looking at victims of Hurricane Maria.
Researchers used standardized measures to assess both survivors who remained in Puerto Rico, and others who were forced to relocate, mostly to Florida. Sixty-six percent of those interviewed had clinically significant elevated symptoms of PTSD, major depression, or generalized anxiety. A study looking at people displaced from Puerto Rico and those who stayed also found high rates of posttraumatic stress disorder and depression in both samples, and rates were actually higher in those who were displaced to Florida, Dr. Shultz said (Disaster Med Public Health Prep. 2019 Feb;13[13]:24-7).
These effects will only worsen as climate change brings more and more powerful storms, and psychiatrists must be ready to help. The year 2017 “is just a snapshot. It may in fact be just a garden variety year when we look back later in this century.
Many countries most affected by climate change are poor in resources and may have few psychiatrists available in the first place. After a storm, infrastructure and the number of trained mental health professionals may further decline. That calls for outside assistance: “We’ve been talking about the possibility of bringing interpersonal psychotherapy (to affected areas) and to have lay personnel supervised by psychiatrists be able to deliver these sorts of interventions,” he said.
Dr. Shultz has no relevant financial disclosures.
SAN FRANCISCO – Longer and more powerful storms caused by climate change will put increasing pressure on mental health care. The unusually powerful 2017 hurricane season, highlighted by damage done to Puerto Rico by Hurricane Maria and to Houston by Hurricane Harvey, may serve as a harbinger of more intense storm seasons to come, according to James M. Shultz, PhD, director of the Center for Disaster and Extreme Event Preparedness at the University of Miami.
Overall, 2017 was something of a “perfect storm” season. “We’ve had predictions about what climate change would do to extreme storms. It was quite exceptional in bringing together all of the elements we have seen predicted by climate scientists,” Dr. Shultz said during a press conference at the annual meeting of the American Psychiatric Association. Study coauthor Zelde Espinel, MD, MPH, also of the center at the university, presented the poster at the meeting.
Aside from greater intensity, climate change is causing a slowing of storms once they make landfall, which increases rainfall and the risks of floods. Nowhere was that more apparent than in Houston in the aftermath of Hurricane Harvey, where tens of thousands of spontaneous rescue efforts arose to rescue people trapped in their homes.
These storms put tremendous pressure on health care systems, as in Puerto Rico when Hurricane Maria knocked out electrical grids, some of which stayed down for 6 months or more. This kind of upheaval interrupts health care infrastructure, including psychiatric services, leaving vulnerable individuals at even greater risk.
Then there are the direct and indirect effects of storms on mental health. When air conditioning and fans are inoperative because of power outages, people get exposed to extreme and relentless heat. They may experience food and water shortages. In worst cases, they may be forced out of their homes on a temporary or even permanent basis. Dr. Shultz recounted research looking at victims of Hurricane Maria.
Researchers used standardized measures to assess both survivors who remained in Puerto Rico, and others who were forced to relocate, mostly to Florida. Sixty-six percent of those interviewed had clinically significant elevated symptoms of PTSD, major depression, or generalized anxiety. A study looking at people displaced from Puerto Rico and those who stayed also found high rates of posttraumatic stress disorder and depression in both samples, and rates were actually higher in those who were displaced to Florida, Dr. Shultz said (Disaster Med Public Health Prep. 2019 Feb;13[13]:24-7).
These effects will only worsen as climate change brings more and more powerful storms, and psychiatrists must be ready to help. The year 2017 “is just a snapshot. It may in fact be just a garden variety year when we look back later in this century.
Many countries most affected by climate change are poor in resources and may have few psychiatrists available in the first place. After a storm, infrastructure and the number of trained mental health professionals may further decline. That calls for outside assistance: “We’ve been talking about the possibility of bringing interpersonal psychotherapy (to affected areas) and to have lay personnel supervised by psychiatrists be able to deliver these sorts of interventions,” he said.
Dr. Shultz has no relevant financial disclosures.
SAN FRANCISCO – Longer and more powerful storms caused by climate change will put increasing pressure on mental health care. The unusually powerful 2017 hurricane season, highlighted by damage done to Puerto Rico by Hurricane Maria and to Houston by Hurricane Harvey, may serve as a harbinger of more intense storm seasons to come, according to James M. Shultz, PhD, director of the Center for Disaster and Extreme Event Preparedness at the University of Miami.
Overall, 2017 was something of a “perfect storm” season. “We’ve had predictions about what climate change would do to extreme storms. It was quite exceptional in bringing together all of the elements we have seen predicted by climate scientists,” Dr. Shultz said during a press conference at the annual meeting of the American Psychiatric Association. Study coauthor Zelde Espinel, MD, MPH, also of the center at the university, presented the poster at the meeting.
Aside from greater intensity, climate change is causing a slowing of storms once they make landfall, which increases rainfall and the risks of floods. Nowhere was that more apparent than in Houston in the aftermath of Hurricane Harvey, where tens of thousands of spontaneous rescue efforts arose to rescue people trapped in their homes.
These storms put tremendous pressure on health care systems, as in Puerto Rico when Hurricane Maria knocked out electrical grids, some of which stayed down for 6 months or more. This kind of upheaval interrupts health care infrastructure, including psychiatric services, leaving vulnerable individuals at even greater risk.
Then there are the direct and indirect effects of storms on mental health. When air conditioning and fans are inoperative because of power outages, people get exposed to extreme and relentless heat. They may experience food and water shortages. In worst cases, they may be forced out of their homes on a temporary or even permanent basis. Dr. Shultz recounted research looking at victims of Hurricane Maria.
Researchers used standardized measures to assess both survivors who remained in Puerto Rico, and others who were forced to relocate, mostly to Florida. Sixty-six percent of those interviewed had clinically significant elevated symptoms of PTSD, major depression, or generalized anxiety. A study looking at people displaced from Puerto Rico and those who stayed also found high rates of posttraumatic stress disorder and depression in both samples, and rates were actually higher in those who were displaced to Florida, Dr. Shultz said (Disaster Med Public Health Prep. 2019 Feb;13[13]:24-7).
These effects will only worsen as climate change brings more and more powerful storms, and psychiatrists must be ready to help. The year 2017 “is just a snapshot. It may in fact be just a garden variety year when we look back later in this century.
Many countries most affected by climate change are poor in resources and may have few psychiatrists available in the first place. After a storm, infrastructure and the number of trained mental health professionals may further decline. That calls for outside assistance: “We’ve been talking about the possibility of bringing interpersonal psychotherapy (to affected areas) and to have lay personnel supervised by psychiatrists be able to deliver these sorts of interventions,” he said.
Dr. Shultz has no relevant financial disclosures.
REPORTING FROM APA 2019