User login
COVID-19: Addressing the mental health needs of clinicians
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
New tetracycline antibiotic effective in acute bacterial skin and skin-structure infections
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Progress report: Elimination of neonatal tetanus
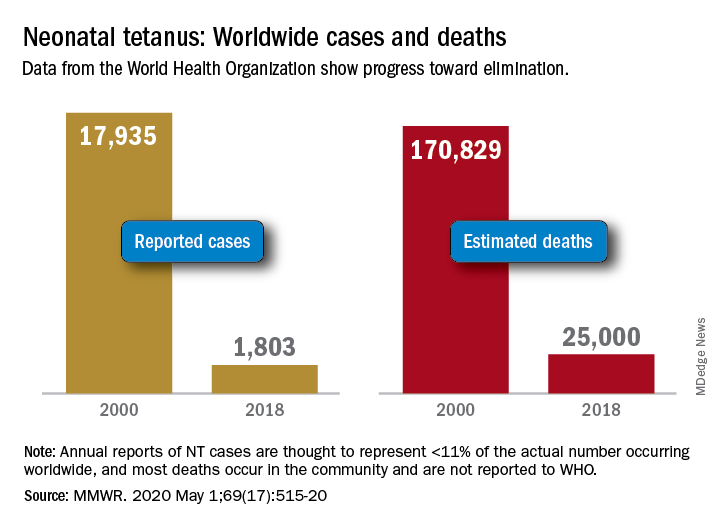
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
FROM MMWR
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
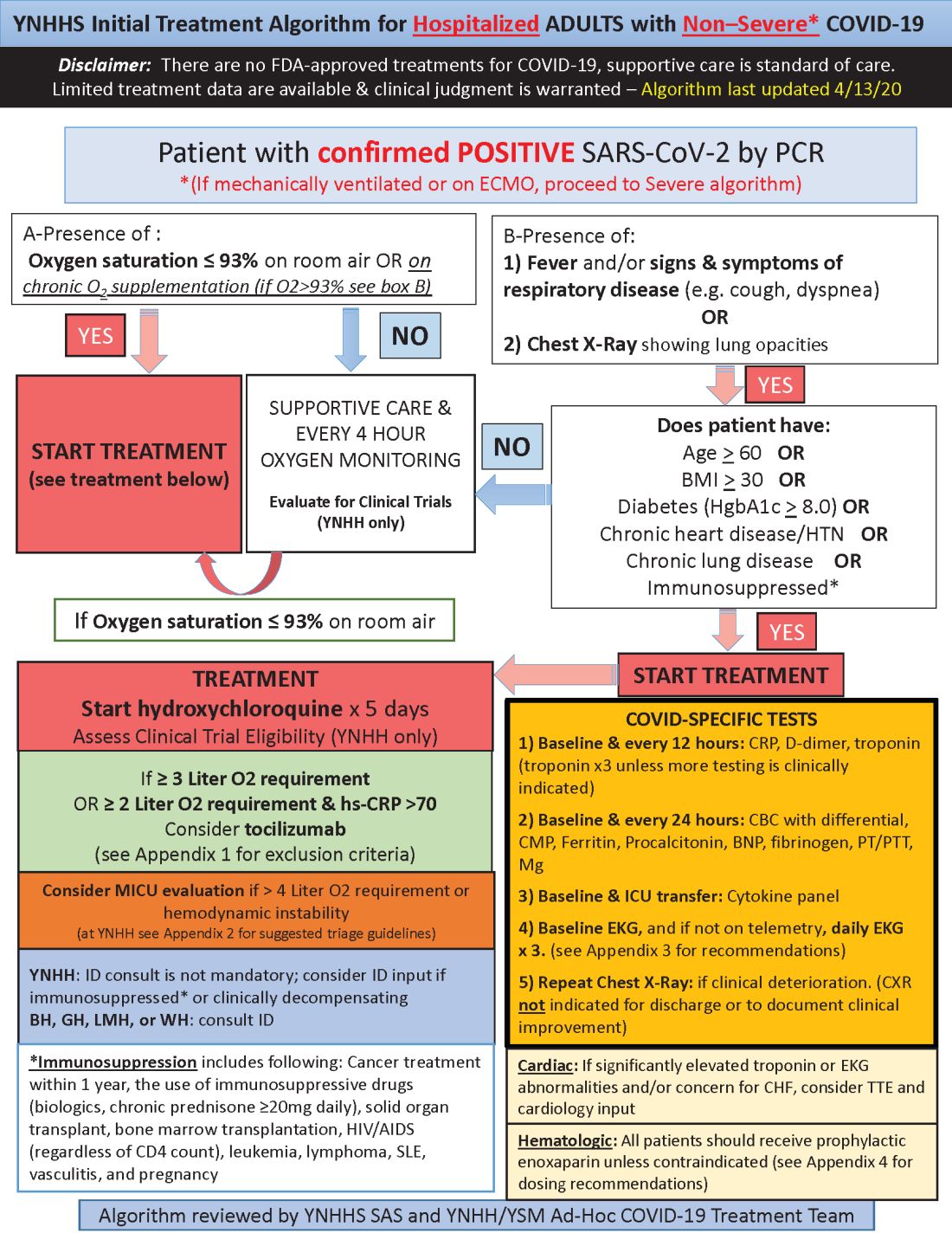
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
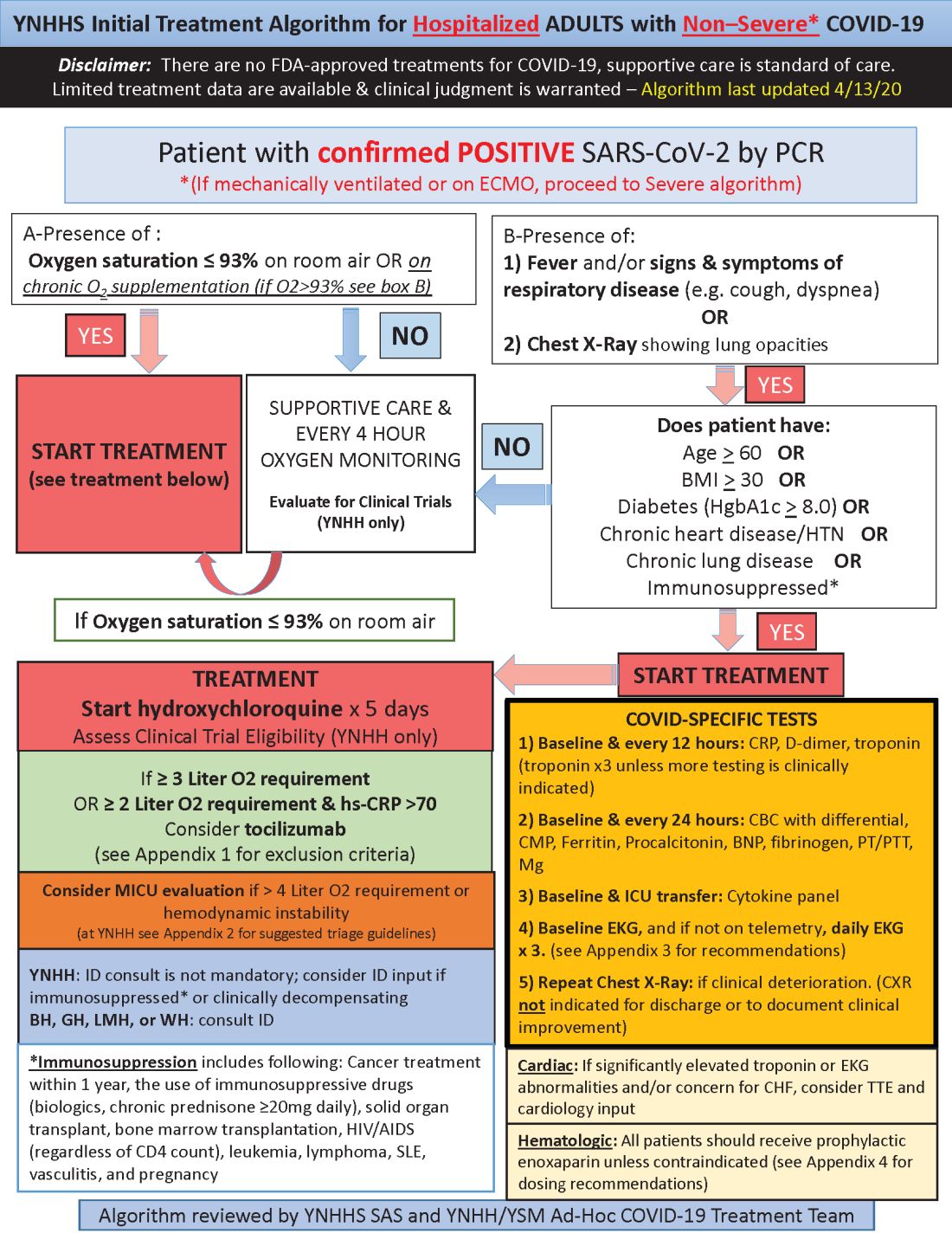
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
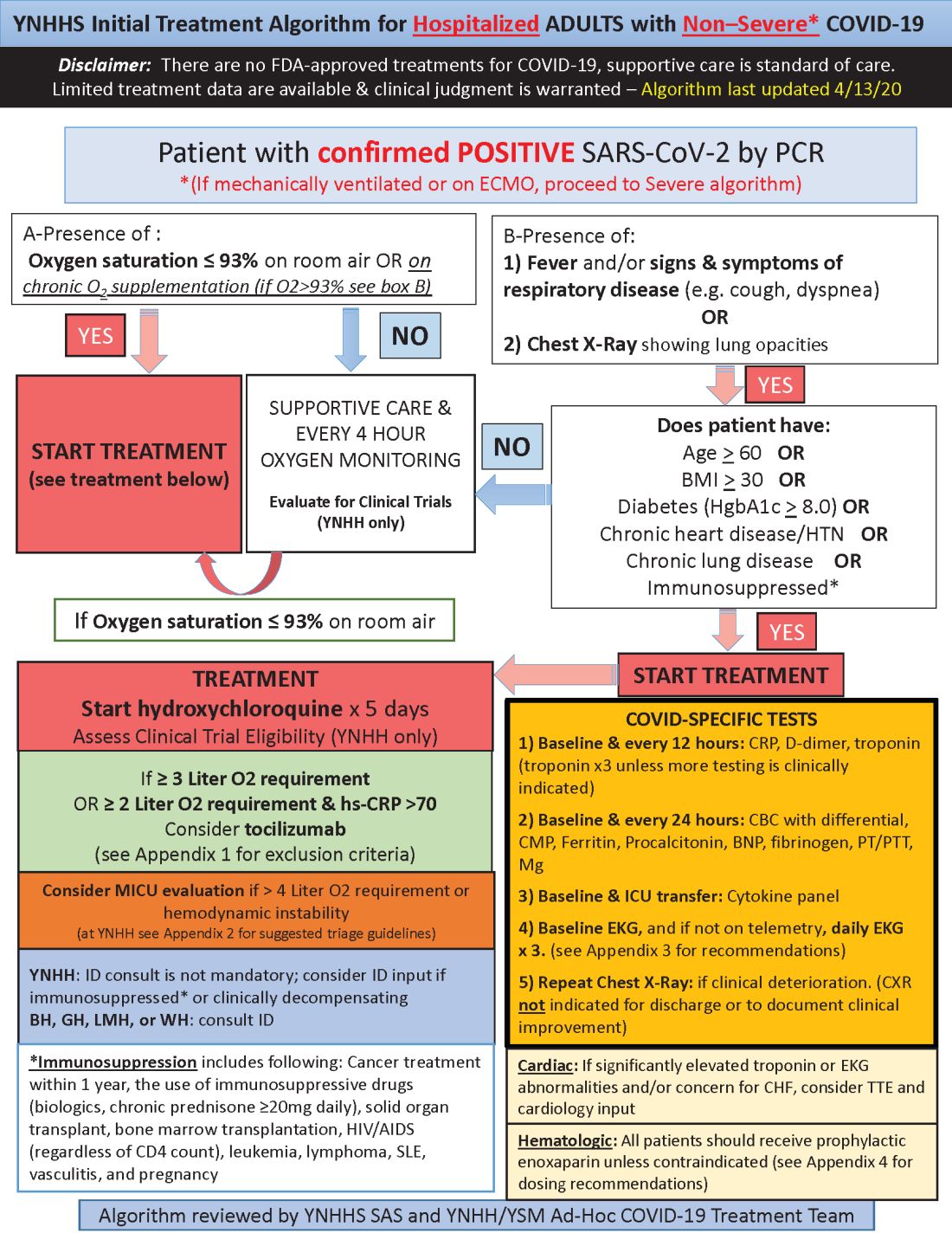
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
POPCoRN network mobilizes pediatric capacity during pandemic
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Med-Peds hospitalists were an organizing force
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
AAP releases updated guidance on male teen sexual, reproductive health
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
FROM PEDIATRICS
IDSA guidelines cover N95 use and reuse
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
FROM INFECTIOUS DISEASE SOCIETY OF AMERICA
New tetracycline antibiotic effective in community-acquired bacterial pneumonia
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Remdesivir now ‘standard of care’ for COVID-19, Fauci says
, according to a preliminary data analysis from a U.S.-led randomized, controlled trial.
On the basis of as yet unpublished data, remdesivir “will be the standard of care” for patients with COVID-19, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), said during a press conference at the White House April 29.
The randomized, placebo-controlled international trial was sponsored by NIAID, which is part of the National Institutes of Health, and enrolled 1,063 patients. It began on Feb. 21.
The interim results, discussed in the press conference and in a NIAID press release, show that time to recovery (i.e., being well enough for hospital discharge or to return to normal activity level) was 31% faster for patients who received remdesivir than for those who received placebo (P < .001).
The median time to recovery was 11 days for patients treated with remdesivir, compared with 15 days for those who received placebo. Results also suggested a survival benefit, with a mortality rate of 8.0% for the group receiving remdesivir and 11.6% for the patients who received placebo (P = .059).
The study, known as the Adaptive COVID-19 Treatment Trial (ACTT), is the first clinical trial launched in the United States to evaluate an experimental treatment for COVID-19. It is being conducted at 68 sites – 47 in the United States and 21 in countries in Europe and Asia.
The data are being released after an interim review by the independent data safety monitoring board found significant benefit with the drug, Dr. Fauci said.
“The reason we are making the announcement now is something that people don’t fully appreciate: Whenever you have clear-cut evidence that a drug works, you have an ethical obligation to let the people in the placebo group know so they could have access,” he explained.
“When I was looking at the data with our team the other night, it was reminiscent of 34 years ago in 1986 when we were struggling for drugs for HIV,” said Dr. Fauci, who was a key figure in HIV/AIDS research. “We did the first randomized, placebo-controlled trial with AZT. It turned out to have an effect that was modest but that was not the endgame because, building on that, every year after, we did better and better.”
Similarly, new trials of drugs for COVID-19 will build on remdesivir, with other agents being added to block other pathways or viral enzymes, Dr. Fauci said.
The study will be submitted to a journal for peer review, he noted, but the New York Times is reporting that the Food and Drug Administration will approve remdesivir for emergency use soon.
In contrast to the positive results Dr. Fauci described from the NIAID-sponsored trial, a randomized, placebo-controlled clinical trial of remdesivir among hospitalized patients with severe COVID-19 in China was inconclusive.
The study, published online in The Lancet, showed some nonsignificant trends toward benefit but did not meet its primary endpoint.
The study was stopped early after 237 of the intended 453 patients were enrolled, owing to a lack of additional patients who met the eligibility criteria. The trial was thus underpowered.
Results showed that treatment with remdesivir did not significantly speed recovery or reduce deaths from COVID-19, but with regard to prespecified secondary outcomes, time to clinical improvement and duration of invasive mechanical ventilation were shorter among a subgroup of patients who began undergoing treatment with remdesivir within 10 days of showing symptoms, in comparison with patients who received standard care.
“To me, the studies reported here in The Lancet appear to be less promising than some statements released today from the NIH, so the situation is a bit puzzling to me,” said Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, who was not involved in the study. “I would need to look more closely at the data which NIH is looking at to understand the differences.”
Trial details
The published trial was conducted at 10 hospitals in Hubei, China. Enrollment criteria included being admitted to hospital with laboratory-confirmed SARS-CoV-2 infection within 12 days of symptom onset, having oxygen saturation of 94% or less, and having radiologically confirmed pneumonia.
Patients were randomly assigned in a 2:1 ratio to receive intravenous remdesivir (200 mg on day 1 followed by 100 mg on days 2–10 in single daily infusions) or placebo infusions for 10 days. Patients were permitted concomitant use of lopinavir-ritonavir, interferons, and corticosteroids.
The primary endpoint was time to clinical improvement to day 28, defined as the time (in days) from randomization to the point of a decline of two levels on a six-point ordinal scale of clinical status (on that scale, 1 indicated that the patient was discharged, and 6 indicated death) or to the patient’s being discharged alive from hospital, whichever came first.
The trial was stopped early because stringent public health measures used in Wuhan led to marked reductions in new patient presentations and because lack of available hospital beds resulted in most patients being enrolled later in the course of disease.
Between Feb. 6, 2020, and March 12, 2020, 237 patients were enrolled and were randomly assigned to receive either remdesivir (n = 158) or placebo (n = 79).
Results showed that use of remdesivir was not associated with a difference in time to clinical improvement (hazard ratio [HR], 1.23; 95% confidence interval [CI], 0.87-1.75).
Although not statistically significant, time to clinical improvement was numerically faster for patients who received remdesivir than for those who received placebo among patients with symptom duration of 10 days or less (median, 18 days vs. 23 days; HR, 1.52; 95% CI, 0.95-2.43).
The mortality rates were similar for the two groups (14% of patients who received remdesivir died vs. 13% of those who received placebo). There was no signal that viral load decreased differentially over time between the two groups.
Adverse events were reported in 66% of remdesivir recipients, vs. 64% of those who received placebo. Remdesivir was stopped early because of adverse events in 12% of patients; it was stopped early for 5% of those who received placebo.
The authors, led by Yeming Wang, MD, China-Japan Friendship Hospital, Beijing, noted that compared with a previous study of compassionate use of remdesivir, the population in the current study was less ill and was treated somewhat earlier in the disease course (median, 10 days vs. 12 days).
Because the study was terminated early, the researchers said they could not adequately assess whether earlier treatment with remdesivir might have provided clinical benefit.
“However, among patients who were treated within 10 days of symptom onset, remdesivir was not a significant factor but was associated with a numerical reduction of 5 days in median time to clinical improvement,” they stated.
They added that remdesivir was adequately tolerated and that no new safety concerns were identified.
In an accompanying comment in The Lancet, John David Norrie, MD, Edinburgh Clinical Trials Unit, United Kingdom, pointed out that this study “has not shown a statistically significant finding that confirms a remdesivir treatment benefit of at least the minimally clinically important difference, nor has it ruled such a benefit out.”
Dr. Norrie was cautious about the fact that the subgroup analysis suggested possible benefit for those treated within 10 days.
Although he said it seems biologically plausible that treating patients earlier could be more effective, he added that “as well as being vigilant against overinterpretation, we need to ensure that hypotheses generated in efficacy-based trials, even in subgroups, are confirmed or refuted in subsequent adequately powered trials or meta-analyses.”
Noting that several other trials of remdesivir are underway, he concluded: “With each individual study at heightened risk of being incomplete, pooling data across possibly several underpowered but high-quality studies looks like our best way to obtain robust insights into what works, safely, and on whom.”
A version of this article originally appeared on Medscape.com.
, according to a preliminary data analysis from a U.S.-led randomized, controlled trial.
On the basis of as yet unpublished data, remdesivir “will be the standard of care” for patients with COVID-19, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), said during a press conference at the White House April 29.
The randomized, placebo-controlled international trial was sponsored by NIAID, which is part of the National Institutes of Health, and enrolled 1,063 patients. It began on Feb. 21.
The interim results, discussed in the press conference and in a NIAID press release, show that time to recovery (i.e., being well enough for hospital discharge or to return to normal activity level) was 31% faster for patients who received remdesivir than for those who received placebo (P < .001).
The median time to recovery was 11 days for patients treated with remdesivir, compared with 15 days for those who received placebo. Results also suggested a survival benefit, with a mortality rate of 8.0% for the group receiving remdesivir and 11.6% for the patients who received placebo (P = .059).
The study, known as the Adaptive COVID-19 Treatment Trial (ACTT), is the first clinical trial launched in the United States to evaluate an experimental treatment for COVID-19. It is being conducted at 68 sites – 47 in the United States and 21 in countries in Europe and Asia.
The data are being released after an interim review by the independent data safety monitoring board found significant benefit with the drug, Dr. Fauci said.
“The reason we are making the announcement now is something that people don’t fully appreciate: Whenever you have clear-cut evidence that a drug works, you have an ethical obligation to let the people in the placebo group know so they could have access,” he explained.
“When I was looking at the data with our team the other night, it was reminiscent of 34 years ago in 1986 when we were struggling for drugs for HIV,” said Dr. Fauci, who was a key figure in HIV/AIDS research. “We did the first randomized, placebo-controlled trial with AZT. It turned out to have an effect that was modest but that was not the endgame because, building on that, every year after, we did better and better.”
Similarly, new trials of drugs for COVID-19 will build on remdesivir, with other agents being added to block other pathways or viral enzymes, Dr. Fauci said.
The study will be submitted to a journal for peer review, he noted, but the New York Times is reporting that the Food and Drug Administration will approve remdesivir for emergency use soon.
In contrast to the positive results Dr. Fauci described from the NIAID-sponsored trial, a randomized, placebo-controlled clinical trial of remdesivir among hospitalized patients with severe COVID-19 in China was inconclusive.
The study, published online in The Lancet, showed some nonsignificant trends toward benefit but did not meet its primary endpoint.
The study was stopped early after 237 of the intended 453 patients were enrolled, owing to a lack of additional patients who met the eligibility criteria. The trial was thus underpowered.
Results showed that treatment with remdesivir did not significantly speed recovery or reduce deaths from COVID-19, but with regard to prespecified secondary outcomes, time to clinical improvement and duration of invasive mechanical ventilation were shorter among a subgroup of patients who began undergoing treatment with remdesivir within 10 days of showing symptoms, in comparison with patients who received standard care.
“To me, the studies reported here in The Lancet appear to be less promising than some statements released today from the NIH, so the situation is a bit puzzling to me,” said Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, who was not involved in the study. “I would need to look more closely at the data which NIH is looking at to understand the differences.”
Trial details
The published trial was conducted at 10 hospitals in Hubei, China. Enrollment criteria included being admitted to hospital with laboratory-confirmed SARS-CoV-2 infection within 12 days of symptom onset, having oxygen saturation of 94% or less, and having radiologically confirmed pneumonia.
Patients were randomly assigned in a 2:1 ratio to receive intravenous remdesivir (200 mg on day 1 followed by 100 mg on days 2–10 in single daily infusions) or placebo infusions for 10 days. Patients were permitted concomitant use of lopinavir-ritonavir, interferons, and corticosteroids.
The primary endpoint was time to clinical improvement to day 28, defined as the time (in days) from randomization to the point of a decline of two levels on a six-point ordinal scale of clinical status (on that scale, 1 indicated that the patient was discharged, and 6 indicated death) or to the patient’s being discharged alive from hospital, whichever came first.
The trial was stopped early because stringent public health measures used in Wuhan led to marked reductions in new patient presentations and because lack of available hospital beds resulted in most patients being enrolled later in the course of disease.
Between Feb. 6, 2020, and March 12, 2020, 237 patients were enrolled and were randomly assigned to receive either remdesivir (n = 158) or placebo (n = 79).
Results showed that use of remdesivir was not associated with a difference in time to clinical improvement (hazard ratio [HR], 1.23; 95% confidence interval [CI], 0.87-1.75).
Although not statistically significant, time to clinical improvement was numerically faster for patients who received remdesivir than for those who received placebo among patients with symptom duration of 10 days or less (median, 18 days vs. 23 days; HR, 1.52; 95% CI, 0.95-2.43).
The mortality rates were similar for the two groups (14% of patients who received remdesivir died vs. 13% of those who received placebo). There was no signal that viral load decreased differentially over time between the two groups.
Adverse events were reported in 66% of remdesivir recipients, vs. 64% of those who received placebo. Remdesivir was stopped early because of adverse events in 12% of patients; it was stopped early for 5% of those who received placebo.
The authors, led by Yeming Wang, MD, China-Japan Friendship Hospital, Beijing, noted that compared with a previous study of compassionate use of remdesivir, the population in the current study was less ill and was treated somewhat earlier in the disease course (median, 10 days vs. 12 days).
Because the study was terminated early, the researchers said they could not adequately assess whether earlier treatment with remdesivir might have provided clinical benefit.
“However, among patients who were treated within 10 days of symptom onset, remdesivir was not a significant factor but was associated with a numerical reduction of 5 days in median time to clinical improvement,” they stated.
They added that remdesivir was adequately tolerated and that no new safety concerns were identified.
In an accompanying comment in The Lancet, John David Norrie, MD, Edinburgh Clinical Trials Unit, United Kingdom, pointed out that this study “has not shown a statistically significant finding that confirms a remdesivir treatment benefit of at least the minimally clinically important difference, nor has it ruled such a benefit out.”
Dr. Norrie was cautious about the fact that the subgroup analysis suggested possible benefit for those treated within 10 days.
Although he said it seems biologically plausible that treating patients earlier could be more effective, he added that “as well as being vigilant against overinterpretation, we need to ensure that hypotheses generated in efficacy-based trials, even in subgroups, are confirmed or refuted in subsequent adequately powered trials or meta-analyses.”
Noting that several other trials of remdesivir are underway, he concluded: “With each individual study at heightened risk of being incomplete, pooling data across possibly several underpowered but high-quality studies looks like our best way to obtain robust insights into what works, safely, and on whom.”
A version of this article originally appeared on Medscape.com.
, according to a preliminary data analysis from a U.S.-led randomized, controlled trial.
On the basis of as yet unpublished data, remdesivir “will be the standard of care” for patients with COVID-19, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases (NIAID), said during a press conference at the White House April 29.
The randomized, placebo-controlled international trial was sponsored by NIAID, which is part of the National Institutes of Health, and enrolled 1,063 patients. It began on Feb. 21.
The interim results, discussed in the press conference and in a NIAID press release, show that time to recovery (i.e., being well enough for hospital discharge or to return to normal activity level) was 31% faster for patients who received remdesivir than for those who received placebo (P < .001).
The median time to recovery was 11 days for patients treated with remdesivir, compared with 15 days for those who received placebo. Results also suggested a survival benefit, with a mortality rate of 8.0% for the group receiving remdesivir and 11.6% for the patients who received placebo (P = .059).
The study, known as the Adaptive COVID-19 Treatment Trial (ACTT), is the first clinical trial launched in the United States to evaluate an experimental treatment for COVID-19. It is being conducted at 68 sites – 47 in the United States and 21 in countries in Europe and Asia.
The data are being released after an interim review by the independent data safety monitoring board found significant benefit with the drug, Dr. Fauci said.
“The reason we are making the announcement now is something that people don’t fully appreciate: Whenever you have clear-cut evidence that a drug works, you have an ethical obligation to let the people in the placebo group know so they could have access,” he explained.
“When I was looking at the data with our team the other night, it was reminiscent of 34 years ago in 1986 when we were struggling for drugs for HIV,” said Dr. Fauci, who was a key figure in HIV/AIDS research. “We did the first randomized, placebo-controlled trial with AZT. It turned out to have an effect that was modest but that was not the endgame because, building on that, every year after, we did better and better.”
Similarly, new trials of drugs for COVID-19 will build on remdesivir, with other agents being added to block other pathways or viral enzymes, Dr. Fauci said.
The study will be submitted to a journal for peer review, he noted, but the New York Times is reporting that the Food and Drug Administration will approve remdesivir for emergency use soon.
In contrast to the positive results Dr. Fauci described from the NIAID-sponsored trial, a randomized, placebo-controlled clinical trial of remdesivir among hospitalized patients with severe COVID-19 in China was inconclusive.
The study, published online in The Lancet, showed some nonsignificant trends toward benefit but did not meet its primary endpoint.
The study was stopped early after 237 of the intended 453 patients were enrolled, owing to a lack of additional patients who met the eligibility criteria. The trial was thus underpowered.
Results showed that treatment with remdesivir did not significantly speed recovery or reduce deaths from COVID-19, but with regard to prespecified secondary outcomes, time to clinical improvement and duration of invasive mechanical ventilation were shorter among a subgroup of patients who began undergoing treatment with remdesivir within 10 days of showing symptoms, in comparison with patients who received standard care.
“To me, the studies reported here in The Lancet appear to be less promising than some statements released today from the NIH, so the situation is a bit puzzling to me,” said Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, who was not involved in the study. “I would need to look more closely at the data which NIH is looking at to understand the differences.”
Trial details
The published trial was conducted at 10 hospitals in Hubei, China. Enrollment criteria included being admitted to hospital with laboratory-confirmed SARS-CoV-2 infection within 12 days of symptom onset, having oxygen saturation of 94% or less, and having radiologically confirmed pneumonia.
Patients were randomly assigned in a 2:1 ratio to receive intravenous remdesivir (200 mg on day 1 followed by 100 mg on days 2–10 in single daily infusions) or placebo infusions for 10 days. Patients were permitted concomitant use of lopinavir-ritonavir, interferons, and corticosteroids.
The primary endpoint was time to clinical improvement to day 28, defined as the time (in days) from randomization to the point of a decline of two levels on a six-point ordinal scale of clinical status (on that scale, 1 indicated that the patient was discharged, and 6 indicated death) or to the patient’s being discharged alive from hospital, whichever came first.
The trial was stopped early because stringent public health measures used in Wuhan led to marked reductions in new patient presentations and because lack of available hospital beds resulted in most patients being enrolled later in the course of disease.
Between Feb. 6, 2020, and March 12, 2020, 237 patients were enrolled and were randomly assigned to receive either remdesivir (n = 158) or placebo (n = 79).
Results showed that use of remdesivir was not associated with a difference in time to clinical improvement (hazard ratio [HR], 1.23; 95% confidence interval [CI], 0.87-1.75).
Although not statistically significant, time to clinical improvement was numerically faster for patients who received remdesivir than for those who received placebo among patients with symptom duration of 10 days or less (median, 18 days vs. 23 days; HR, 1.52; 95% CI, 0.95-2.43).
The mortality rates were similar for the two groups (14% of patients who received remdesivir died vs. 13% of those who received placebo). There was no signal that viral load decreased differentially over time between the two groups.
Adverse events were reported in 66% of remdesivir recipients, vs. 64% of those who received placebo. Remdesivir was stopped early because of adverse events in 12% of patients; it was stopped early for 5% of those who received placebo.
The authors, led by Yeming Wang, MD, China-Japan Friendship Hospital, Beijing, noted that compared with a previous study of compassionate use of remdesivir, the population in the current study was less ill and was treated somewhat earlier in the disease course (median, 10 days vs. 12 days).
Because the study was terminated early, the researchers said they could not adequately assess whether earlier treatment with remdesivir might have provided clinical benefit.
“However, among patients who were treated within 10 days of symptom onset, remdesivir was not a significant factor but was associated with a numerical reduction of 5 days in median time to clinical improvement,” they stated.
They added that remdesivir was adequately tolerated and that no new safety concerns were identified.
In an accompanying comment in The Lancet, John David Norrie, MD, Edinburgh Clinical Trials Unit, United Kingdom, pointed out that this study “has not shown a statistically significant finding that confirms a remdesivir treatment benefit of at least the minimally clinically important difference, nor has it ruled such a benefit out.”
Dr. Norrie was cautious about the fact that the subgroup analysis suggested possible benefit for those treated within 10 days.
Although he said it seems biologically plausible that treating patients earlier could be more effective, he added that “as well as being vigilant against overinterpretation, we need to ensure that hypotheses generated in efficacy-based trials, even in subgroups, are confirmed or refuted in subsequent adequately powered trials or meta-analyses.”
Noting that several other trials of remdesivir are underway, he concluded: “With each individual study at heightened risk of being incomplete, pooling data across possibly several underpowered but high-quality studies looks like our best way to obtain robust insights into what works, safely, and on whom.”
A version of this article originally appeared on Medscape.com.
Standing orders for vaccines may improve pediatric vaccination rates
The biggest barrier to using standing orders for childhood immunizations is concern that patients will receive the wrong vaccine, according to a survey of pediatricians published in Pediatrics.
The other top reasons pediatricians give for not using standing orders for vaccines are concerns that parents may want to talk to the doctor about the vaccine before their child gets it, and a belief that the doctor should be the one who personally recommends a vaccine for their patient.
But with severe drops in vaccination rates resulting from the COVID-19 pandemic, standing orders may be a valuable tool for ensuring children get their vaccines on time, suggested lead author, Jessica Cataldi, MD, of the University of Colorado and Children’s Hospital Colorado in Aurora.
“As we work to bring more families back to their pediatrician’s office for well-child checks, standing orders are one process that can streamline the visit by saving providers time and increasing vaccine delivery,” she said in an interview. “We will also need use standing orders to support different ways to get children their immunizations during times of social distancing. This could take the form of drive-through immunization clinics or telehealth well-child checks that are paired with a quick immunization-only visit.”
The American Academy of Pediatrics issued guidance April 14 that emphasizes the need to prioritize immunization of children through 2-years-old.
Paul A. Offit, MD, director of the Vaccine Education Center and an attending physician in the division of infectious diseases at Children’s Hospital of Philadelphia, agreed that it’s essential children do not fall behind on the recommended schedule during the pandemic.
“It’s important not to have greater collateral damage from this COVID-19 pandemic by putting children at increased risk from other infections that are circulating, like measles and pertussis,” he said, noting that nearly 1,300 measles cases and more than 15,000 pertussis cases occurred in the United States in 2019.
It’s important “not to delay those primary vaccines because it’s hard to catch up,” he said in an interview
Although “standing orders” may go by other names in non–inpatient settings, the researchers defined them in their survey as “a written or verbal policy that persons other than a medical provider, such as a nurse or medical assistant, may consent and vaccinate a person without speaking with the physician or advanced care provider first.” Further, the “vaccine may be given before or after a physician encounter or in the absence of a physician encounter altogether.”
Research strongly suggests that standing orders for childhood vaccines are cost-effective and increase immunization rates, the authors noted. The Centers for Disease Control and Prevention, its Advisory Committee on Immunization Practices, the American Academy of Pediatrics, and the federal National Vaccine Advisory Committee all recommend using standing orders to improve vaccination access and rates.
The authors sought to understand how many pediatricians use standing orders and what reasons stop them from doing so. During June-September 2017, they sent out 471 online and mail surveys to a nationally representative sample of AAP members who spent at least half their time in primary care.
The 372 pediatricians who completed the survey made up a response rate of 79%, with no differences in response based on age, sex, years in practice, practice setting, region or rural/urban location.
More than half the respondents (59%) used standing orders for childhood immunizations. Just over a third of respondents (36%) said they use standing orders for all routinely recommended vaccines, and 23% use them for some vaccines.
Among those who did not use standing orders, 68% cited the concern that patients would get the incorrect vaccine by mistake as a barrier to using them. That came as a surprise to Dr Offit, who would expect standing orders to reduce the likelihood of error.
“The standing order should make things a little more foolproof so that you’re less likely to make a mistake,” Dr Offit said.
No studies have shown that vaccine errors occur more often in clinics that use standing orders for immunizations, but the question merits continued monitoring, Dr Cataldi said.
“It is important for any clinic that is new to the use of standing orders to provide adequate education to providers and other staff about when and how to use standing orders, and to always leave room for staff to bring vaccination questions to the provider,” Dr Cataldi told this newspaper
Nearly as many physicians (62%) believed that families would want to speak to the doctor about a vaccine before getting it, and 57% of respondents who didn’t use standing orders believed they should be the one who recommends a vaccine to their patient’s parents.
All three of these reasons also ranked highest as barriers in responses from all respondents, including those who use standing orders. But those who didn’t use them were significantly more likely to cite these reasons (P less than .0001).
Since the survey occurred in 2017, however, it’s possible the pandemic and the rapid increase in telehealth as a result may influence perceptions moving forward.
“With provider concerns that standing orders remove physicians from the vaccination conversation, it may be that those conversations become less crucial as some families may start to value and accept immunizations more as a result of this pandemic,” Dr Cataldi said. “Or for families with vaccine questions, telehealth might support those conversations with a provider well.”
After adjusting for potential confounders, the only practice or physician factor significantly associated with not using standing orders for vaccines was physicians’ having a higher “physician responsibility score.” Doctors with these higher scores also were marginally more likely to make independent decisions about vaccines than counterparts working at practices where system-level decisions occur.
“Perhaps physicians who feel more personal responsibility about their role in vaccination are more likely to choose practice settings where they have more independent decision-making ability,” the authors wrote. “Alternatively, knowing the level of decision-making about vaccines in the practice may influence the amount of personal responsibility that pediatricians feel about their role in vaccine delivery.”
Again, attitudes may have shifted since the coronavirus pandemic began. The biggest risk to children in terms of immunizations is not getting them, Dr Offit said.
“The parents are scared, and the doctors are scared,” he said. “They feel that going to a doctor’s office is going to a concentrated area where they’re more likely to pick up this virus.”
He’s expressed uncertainty about whether standing orders could play a role in alleviating that anxiety. But Dr Cataldi suggests it’s possible.
“I think standing orders will be important to increasing vaccination rates during a pandemic as they can be used to support delivery of vaccines through public health departments and through vaccine-only nurse visits,” she said.
The research was funded by the Centers for Disease Control and Prevention. The authors had no relevant financial disclosures.
SOURCE: Cataldi J et al. Pediatrics. 2020 Apr;e20191855.
The biggest barrier to using standing orders for childhood immunizations is concern that patients will receive the wrong vaccine, according to a survey of pediatricians published in Pediatrics.
The other top reasons pediatricians give for not using standing orders for vaccines are concerns that parents may want to talk to the doctor about the vaccine before their child gets it, and a belief that the doctor should be the one who personally recommends a vaccine for their patient.
But with severe drops in vaccination rates resulting from the COVID-19 pandemic, standing orders may be a valuable tool for ensuring children get their vaccines on time, suggested lead author, Jessica Cataldi, MD, of the University of Colorado and Children’s Hospital Colorado in Aurora.
“As we work to bring more families back to their pediatrician’s office for well-child checks, standing orders are one process that can streamline the visit by saving providers time and increasing vaccine delivery,” she said in an interview. “We will also need use standing orders to support different ways to get children their immunizations during times of social distancing. This could take the form of drive-through immunization clinics or telehealth well-child checks that are paired with a quick immunization-only visit.”
The American Academy of Pediatrics issued guidance April 14 that emphasizes the need to prioritize immunization of children through 2-years-old.
Paul A. Offit, MD, director of the Vaccine Education Center and an attending physician in the division of infectious diseases at Children’s Hospital of Philadelphia, agreed that it’s essential children do not fall behind on the recommended schedule during the pandemic.
“It’s important not to have greater collateral damage from this COVID-19 pandemic by putting children at increased risk from other infections that are circulating, like measles and pertussis,” he said, noting that nearly 1,300 measles cases and more than 15,000 pertussis cases occurred in the United States in 2019.
It’s important “not to delay those primary vaccines because it’s hard to catch up,” he said in an interview
Although “standing orders” may go by other names in non–inpatient settings, the researchers defined them in their survey as “a written or verbal policy that persons other than a medical provider, such as a nurse or medical assistant, may consent and vaccinate a person without speaking with the physician or advanced care provider first.” Further, the “vaccine may be given before or after a physician encounter or in the absence of a physician encounter altogether.”
Research strongly suggests that standing orders for childhood vaccines are cost-effective and increase immunization rates, the authors noted. The Centers for Disease Control and Prevention, its Advisory Committee on Immunization Practices, the American Academy of Pediatrics, and the federal National Vaccine Advisory Committee all recommend using standing orders to improve vaccination access and rates.
The authors sought to understand how many pediatricians use standing orders and what reasons stop them from doing so. During June-September 2017, they sent out 471 online and mail surveys to a nationally representative sample of AAP members who spent at least half their time in primary care.
The 372 pediatricians who completed the survey made up a response rate of 79%, with no differences in response based on age, sex, years in practice, practice setting, region or rural/urban location.
More than half the respondents (59%) used standing orders for childhood immunizations. Just over a third of respondents (36%) said they use standing orders for all routinely recommended vaccines, and 23% use them for some vaccines.
Among those who did not use standing orders, 68% cited the concern that patients would get the incorrect vaccine by mistake as a barrier to using them. That came as a surprise to Dr Offit, who would expect standing orders to reduce the likelihood of error.
“The standing order should make things a little more foolproof so that you’re less likely to make a mistake,” Dr Offit said.
No studies have shown that vaccine errors occur more often in clinics that use standing orders for immunizations, but the question merits continued monitoring, Dr Cataldi said.
“It is important for any clinic that is new to the use of standing orders to provide adequate education to providers and other staff about when and how to use standing orders, and to always leave room for staff to bring vaccination questions to the provider,” Dr Cataldi told this newspaper
Nearly as many physicians (62%) believed that families would want to speak to the doctor about a vaccine before getting it, and 57% of respondents who didn’t use standing orders believed they should be the one who recommends a vaccine to their patient’s parents.
All three of these reasons also ranked highest as barriers in responses from all respondents, including those who use standing orders. But those who didn’t use them were significantly more likely to cite these reasons (P less than .0001).
Since the survey occurred in 2017, however, it’s possible the pandemic and the rapid increase in telehealth as a result may influence perceptions moving forward.
“With provider concerns that standing orders remove physicians from the vaccination conversation, it may be that those conversations become less crucial as some families may start to value and accept immunizations more as a result of this pandemic,” Dr Cataldi said. “Or for families with vaccine questions, telehealth might support those conversations with a provider well.”
After adjusting for potential confounders, the only practice or physician factor significantly associated with not using standing orders for vaccines was physicians’ having a higher “physician responsibility score.” Doctors with these higher scores also were marginally more likely to make independent decisions about vaccines than counterparts working at practices where system-level decisions occur.
“Perhaps physicians who feel more personal responsibility about their role in vaccination are more likely to choose practice settings where they have more independent decision-making ability,” the authors wrote. “Alternatively, knowing the level of decision-making about vaccines in the practice may influence the amount of personal responsibility that pediatricians feel about their role in vaccine delivery.”
Again, attitudes may have shifted since the coronavirus pandemic began. The biggest risk to children in terms of immunizations is not getting them, Dr Offit said.
“The parents are scared, and the doctors are scared,” he said. “They feel that going to a doctor’s office is going to a concentrated area where they’re more likely to pick up this virus.”
He’s expressed uncertainty about whether standing orders could play a role in alleviating that anxiety. But Dr Cataldi suggests it’s possible.
“I think standing orders will be important to increasing vaccination rates during a pandemic as they can be used to support delivery of vaccines through public health departments and through vaccine-only nurse visits,” she said.
The research was funded by the Centers for Disease Control and Prevention. The authors had no relevant financial disclosures.
SOURCE: Cataldi J et al. Pediatrics. 2020 Apr;e20191855.
The biggest barrier to using standing orders for childhood immunizations is concern that patients will receive the wrong vaccine, according to a survey of pediatricians published in Pediatrics.
The other top reasons pediatricians give for not using standing orders for vaccines are concerns that parents may want to talk to the doctor about the vaccine before their child gets it, and a belief that the doctor should be the one who personally recommends a vaccine for their patient.
But with severe drops in vaccination rates resulting from the COVID-19 pandemic, standing orders may be a valuable tool for ensuring children get their vaccines on time, suggested lead author, Jessica Cataldi, MD, of the University of Colorado and Children’s Hospital Colorado in Aurora.
“As we work to bring more families back to their pediatrician’s office for well-child checks, standing orders are one process that can streamline the visit by saving providers time and increasing vaccine delivery,” she said in an interview. “We will also need use standing orders to support different ways to get children their immunizations during times of social distancing. This could take the form of drive-through immunization clinics or telehealth well-child checks that are paired with a quick immunization-only visit.”
The American Academy of Pediatrics issued guidance April 14 that emphasizes the need to prioritize immunization of children through 2-years-old.
Paul A. Offit, MD, director of the Vaccine Education Center and an attending physician in the division of infectious diseases at Children’s Hospital of Philadelphia, agreed that it’s essential children do not fall behind on the recommended schedule during the pandemic.
“It’s important not to have greater collateral damage from this COVID-19 pandemic by putting children at increased risk from other infections that are circulating, like measles and pertussis,” he said, noting that nearly 1,300 measles cases and more than 15,000 pertussis cases occurred in the United States in 2019.
It’s important “not to delay those primary vaccines because it’s hard to catch up,” he said in an interview
Although “standing orders” may go by other names in non–inpatient settings, the researchers defined them in their survey as “a written or verbal policy that persons other than a medical provider, such as a nurse or medical assistant, may consent and vaccinate a person without speaking with the physician or advanced care provider first.” Further, the “vaccine may be given before or after a physician encounter or in the absence of a physician encounter altogether.”
Research strongly suggests that standing orders for childhood vaccines are cost-effective and increase immunization rates, the authors noted. The Centers for Disease Control and Prevention, its Advisory Committee on Immunization Practices, the American Academy of Pediatrics, and the federal National Vaccine Advisory Committee all recommend using standing orders to improve vaccination access and rates.
The authors sought to understand how many pediatricians use standing orders and what reasons stop them from doing so. During June-September 2017, they sent out 471 online and mail surveys to a nationally representative sample of AAP members who spent at least half their time in primary care.
The 372 pediatricians who completed the survey made up a response rate of 79%, with no differences in response based on age, sex, years in practice, practice setting, region or rural/urban location.
More than half the respondents (59%) used standing orders for childhood immunizations. Just over a third of respondents (36%) said they use standing orders for all routinely recommended vaccines, and 23% use them for some vaccines.
Among those who did not use standing orders, 68% cited the concern that patients would get the incorrect vaccine by mistake as a barrier to using them. That came as a surprise to Dr Offit, who would expect standing orders to reduce the likelihood of error.
“The standing order should make things a little more foolproof so that you’re less likely to make a mistake,” Dr Offit said.
No studies have shown that vaccine errors occur more often in clinics that use standing orders for immunizations, but the question merits continued monitoring, Dr Cataldi said.
“It is important for any clinic that is new to the use of standing orders to provide adequate education to providers and other staff about when and how to use standing orders, and to always leave room for staff to bring vaccination questions to the provider,” Dr Cataldi told this newspaper
Nearly as many physicians (62%) believed that families would want to speak to the doctor about a vaccine before getting it, and 57% of respondents who didn’t use standing orders believed they should be the one who recommends a vaccine to their patient’s parents.
All three of these reasons also ranked highest as barriers in responses from all respondents, including those who use standing orders. But those who didn’t use them were significantly more likely to cite these reasons (P less than .0001).
Since the survey occurred in 2017, however, it’s possible the pandemic and the rapid increase in telehealth as a result may influence perceptions moving forward.
“With provider concerns that standing orders remove physicians from the vaccination conversation, it may be that those conversations become less crucial as some families may start to value and accept immunizations more as a result of this pandemic,” Dr Cataldi said. “Or for families with vaccine questions, telehealth might support those conversations with a provider well.”
After adjusting for potential confounders, the only practice or physician factor significantly associated with not using standing orders for vaccines was physicians’ having a higher “physician responsibility score.” Doctors with these higher scores also were marginally more likely to make independent decisions about vaccines than counterparts working at practices where system-level decisions occur.
“Perhaps physicians who feel more personal responsibility about their role in vaccination are more likely to choose practice settings where they have more independent decision-making ability,” the authors wrote. “Alternatively, knowing the level of decision-making about vaccines in the practice may influence the amount of personal responsibility that pediatricians feel about their role in vaccine delivery.”
Again, attitudes may have shifted since the coronavirus pandemic began. The biggest risk to children in terms of immunizations is not getting them, Dr Offit said.
“The parents are scared, and the doctors are scared,” he said. “They feel that going to a doctor’s office is going to a concentrated area where they’re more likely to pick up this virus.”
He’s expressed uncertainty about whether standing orders could play a role in alleviating that anxiety. But Dr Cataldi suggests it’s possible.
“I think standing orders will be important to increasing vaccination rates during a pandemic as they can be used to support delivery of vaccines through public health departments and through vaccine-only nurse visits,” she said.
The research was funded by the Centers for Disease Control and Prevention. The authors had no relevant financial disclosures.
SOURCE: Cataldi J et al. Pediatrics. 2020 Apr;e20191855.
FROM PEDIATRICS