User login
For MD-IQ use only
Death of a sales pitch
The EHR and our troubled health care system, Part 1
In 2000, the Institute of Medicine published “To Err Is Human,” a landmark study that warned that as many as 98,000 people die annually as a result of medical errors. One conclusion of the report stated, “When patients see multiple providers in different settings, none of whom has access to complete information, it becomes easier for things to go wrong.” Government and public reaction to the study resulted in the rushed integration of electronic health records into the U.S. medical system. EHR vendors promised solutions that included a dramatic reduction of preventable errors, a simplified system of physician communication, and the consolidation of a patient’s salient medical information into a single, transferable file. Now, almost 20 years later, these promises remain mostly unfilled. How did we get here?
Systems of medical records have been in place since 1600 B.C. For thousands of years, they consisted mainly of the patient’s diagnosis and the physician’s treatment. In 1968, the New England Journal of Medicine published the special article “Medical Records That Guide and Teach” by Lawrence L. Weed, MD. In the report, Dr. Weed advocated for the organization of medical records by problems rather than by a single diagnosis. This was the birth of our modern system. Medical records would now include lists of symptoms, findings, and problems that would organize the physician’s planning and allow third parties to confirm the initial diagnosis. Nearly concurrent with this publication, the next major innovation was developing in a very unusual location.
In 1999, Fortune magazine labeled Jack Welch “Manager of the Century” for his innovative work as CEO of General Electric. His techniques involved cutting waste and streamlining his workforce. While these methods were somewhat controversial, GE’s market value increased dramatically under his watch. The publishers at Fortune became interested in finding similar innovators in other fields. In this pursuit, they sent journalist Philip Longman to find the “Jack Welch” of health care.
Mr. Longman had recently lost his wife to breast cancer and was becoming obsessed with medical errors and health care quality integration. He set out to discover the best health care system in the United States. After months of research, Mr. Longman reached a startling conclusion. By nearly every metric, the Veterans Affairs system produced the highest quality of care. The key factor in upholding that quality appeared to be the EHR system VistA (Veterans Information Systems and Technology Architecture).
The development of VistA was a grassroots effort begun in the 1970s. Using Tandy computers and Wang processors, the VA “hardhats” sought to develop an electronic system for medical records and communication. This effort was initially opposed and driven underground by the central bureaucracy. Laptops were confiscated, people were fired. Still, development continued, and in 1978, the Decentralized Hospital Computer Program was launched at 20 VA sites. The national rollout occurred in 1994 under the name VistA.
VistA was developed by doctors, for doctors, and routinely enjoys the highest satisfaction rates among all available EHRs. VistA also is an open source model; its code is readily available on the VA website. After seeing the evidence of VistA’s efficacy, Representative Pete Stark (D-CA) introduced HR 6898 on Sept. 15, 2008. The bill would establish a large federal open source health IT system that private hospitals could leverage. The bill also mandated that only open source solutions would receive federal funding. As opposed to proprietary systems, open source models allow for rapid innovation, easy personal configuration, and incorporation of open source apps from unlimited numbers of contributors.
HR 6898 never passed, despite initial bipartisan support. By relying on lobbyists, marketing, and money, the proprietary EHR vendors killed the Stark bill. After a 4-month scramble, the Health Information Technology for Economic and Clinical Health Act (HITECH) passed, with EHR vendor support. HITECH established a certification system for EHRs. While the Stark bill envisioned a single, open source network, there were soon hundreds of certified EHR systems in the United States.
Before the HITECH Act, many EHRs existed, but several barriers blocked full implementation. Early systems were essentially electronic filing cabinets. Their developers had not anticipated the lack of standardization among physicians and hospital systems. The need for custom EHR bases frustrated the vendors. The question of marketing was omnipresent. Who was the actual customer? An economic model developed in which clinicians would bear the time and even financial costs as the benefits would be passed on to insurers, hospitals, and, presumably, the patients.
EHRs needed to become practical, affordable, and interoperable, but who was demanding this? Where was the financial motivation? In the beginning, vendors of EHRs had to convince doctors, the public, and the government of their worth. Now, essentially mandated by the HITECH Act, they only had to sell themselves to hospital administrators, who often had a different motive. Profits.
Many of today’s EHRs are simply modified billing platforms, and doctors are paying the price. The Meaningful Use standards were meant to provide financial incentives for EHR adoption. Stage 2 required EHRs to be able to transport clinical information from one system to another. Looking at our actual practices can provide a master class in the gap between “be able to” and “actually doing.” Again, who does the EHR vendor see as the customer? Certainly not the physician. My patients can list every type of inferior vena cava filter (or at least those with pending legal action), but most of them have never heard of an EHR. Just like “service lines,” EHRs can make it very difficult for patients to seek care outside of their primary system. Who would see this barrier in communication as a perk and not a deficiency? Hospital administrators. The free transfer of medical records is bad for business. Therefore, hospitals don’t prioritize it in their EHRs. The EHR vendors also benefit since an easy transfer of records would simplify a hospital’s transition from one EHR to another. So, as with most deficiencies in the EHR, physicians are left to find ways around these problems. Sometimes, we need to go to comical lengths.
Two months ago, a patient pointed to a large machine behind our check-in desk. “What is that,” he asked incredulously; it was a fax machine. While my competence with this apparatus is marginal (my office staff has taken to yelling “doctor faxing!” to alert one another that I am about to inadvertently copy or scan my documents into oblivion), faxes remain a mainstay of medical care. Abandoned by modern business practices as a relic of the 1980s, why are we constantly faxing medical information? Because we are not the customer.
Disruption is now a favorable term in business. Doctors are busy people. BUSY people. Most of us walk a tightrope, a razor-thin timeline. Will we see the next patient in time, the next surgery? Will we get the medical records done today? Will we get the dictations done before being suspended? Will we make the committee meeting, the conference call, the next clinic across town? Will we have dinner with our spouse or see our kids today? Will we make it to the parent-teacher conference inexplicably scheduled for 10:45 a.m. on a Tuesday??!! When deciding between work commitments and family, we side with work overwhelmingly (and depressingly). Explaining this to a layperson is an impossible feat. I have stopped trying, stopped making excuses. Only we know how catastrophic “disruption” can be. Disruption in a 40-patient clinic. Disruption in the trauma bay. I have seen physicians reduced to tears by this disruption. Some activities need disruption. Typing with your back to the patient. Onerous documentation to facilitate billing. Faxing medical records. Will these be disrupted? Who is the customer?
In 1999, the Institute of Medicine started this process, telling us, “To err is human.” I now respond with another Alexander Pope quote, “The same ambition can destroy or save.” The money and influence of EHR vendors destroyed the chance to nationalize the most successful EHR our country has ever seen. What happens now? EHRs are incontrovertibly associated with burnout. Burnout is incontrovertibly associated with outcomes ranging from early retirement to suicide. EHRs cause physician harm. Major vendors can follow the Big Tobacco play book and deny the obvious, but the burden of proof is shifting to them. With their billions of dollars in profits, what have they done to study this problem? To help?
Who is their customer?
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
References
Institute of Medicine (US) Committee on Quality of Health Care in America. 2000. To Err Is Human: Building a Safer Health System. Washington: The National Academies Press.
Weed LL. Medical records that guide and teach. N Engl J Med. 1968 Mar 14;278(11):593-600.
Longman P. “Best Care Anywhere: Why VA Health Care Is Better Than Yours.” (Oakland: Berrett-Koehler Publishers).
The EHR and our troubled health care system, Part 1
The EHR and our troubled health care system, Part 1
In 2000, the Institute of Medicine published “To Err Is Human,” a landmark study that warned that as many as 98,000 people die annually as a result of medical errors. One conclusion of the report stated, “When patients see multiple providers in different settings, none of whom has access to complete information, it becomes easier for things to go wrong.” Government and public reaction to the study resulted in the rushed integration of electronic health records into the U.S. medical system. EHR vendors promised solutions that included a dramatic reduction of preventable errors, a simplified system of physician communication, and the consolidation of a patient’s salient medical information into a single, transferable file. Now, almost 20 years later, these promises remain mostly unfilled. How did we get here?
Systems of medical records have been in place since 1600 B.C. For thousands of years, they consisted mainly of the patient’s diagnosis and the physician’s treatment. In 1968, the New England Journal of Medicine published the special article “Medical Records That Guide and Teach” by Lawrence L. Weed, MD. In the report, Dr. Weed advocated for the organization of medical records by problems rather than by a single diagnosis. This was the birth of our modern system. Medical records would now include lists of symptoms, findings, and problems that would organize the physician’s planning and allow third parties to confirm the initial diagnosis. Nearly concurrent with this publication, the next major innovation was developing in a very unusual location.
In 1999, Fortune magazine labeled Jack Welch “Manager of the Century” for his innovative work as CEO of General Electric. His techniques involved cutting waste and streamlining his workforce. While these methods were somewhat controversial, GE’s market value increased dramatically under his watch. The publishers at Fortune became interested in finding similar innovators in other fields. In this pursuit, they sent journalist Philip Longman to find the “Jack Welch” of health care.
Mr. Longman had recently lost his wife to breast cancer and was becoming obsessed with medical errors and health care quality integration. He set out to discover the best health care system in the United States. After months of research, Mr. Longman reached a startling conclusion. By nearly every metric, the Veterans Affairs system produced the highest quality of care. The key factor in upholding that quality appeared to be the EHR system VistA (Veterans Information Systems and Technology Architecture).
The development of VistA was a grassroots effort begun in the 1970s. Using Tandy computers and Wang processors, the VA “hardhats” sought to develop an electronic system for medical records and communication. This effort was initially opposed and driven underground by the central bureaucracy. Laptops were confiscated, people were fired. Still, development continued, and in 1978, the Decentralized Hospital Computer Program was launched at 20 VA sites. The national rollout occurred in 1994 under the name VistA.
VistA was developed by doctors, for doctors, and routinely enjoys the highest satisfaction rates among all available EHRs. VistA also is an open source model; its code is readily available on the VA website. After seeing the evidence of VistA’s efficacy, Representative Pete Stark (D-CA) introduced HR 6898 on Sept. 15, 2008. The bill would establish a large federal open source health IT system that private hospitals could leverage. The bill also mandated that only open source solutions would receive federal funding. As opposed to proprietary systems, open source models allow for rapid innovation, easy personal configuration, and incorporation of open source apps from unlimited numbers of contributors.
HR 6898 never passed, despite initial bipartisan support. By relying on lobbyists, marketing, and money, the proprietary EHR vendors killed the Stark bill. After a 4-month scramble, the Health Information Technology for Economic and Clinical Health Act (HITECH) passed, with EHR vendor support. HITECH established a certification system for EHRs. While the Stark bill envisioned a single, open source network, there were soon hundreds of certified EHR systems in the United States.
Before the HITECH Act, many EHRs existed, but several barriers blocked full implementation. Early systems were essentially electronic filing cabinets. Their developers had not anticipated the lack of standardization among physicians and hospital systems. The need for custom EHR bases frustrated the vendors. The question of marketing was omnipresent. Who was the actual customer? An economic model developed in which clinicians would bear the time and even financial costs as the benefits would be passed on to insurers, hospitals, and, presumably, the patients.
EHRs needed to become practical, affordable, and interoperable, but who was demanding this? Where was the financial motivation? In the beginning, vendors of EHRs had to convince doctors, the public, and the government of their worth. Now, essentially mandated by the HITECH Act, they only had to sell themselves to hospital administrators, who often had a different motive. Profits.
Many of today’s EHRs are simply modified billing platforms, and doctors are paying the price. The Meaningful Use standards were meant to provide financial incentives for EHR adoption. Stage 2 required EHRs to be able to transport clinical information from one system to another. Looking at our actual practices can provide a master class in the gap between “be able to” and “actually doing.” Again, who does the EHR vendor see as the customer? Certainly not the physician. My patients can list every type of inferior vena cava filter (or at least those with pending legal action), but most of them have never heard of an EHR. Just like “service lines,” EHRs can make it very difficult for patients to seek care outside of their primary system. Who would see this barrier in communication as a perk and not a deficiency? Hospital administrators. The free transfer of medical records is bad for business. Therefore, hospitals don’t prioritize it in their EHRs. The EHR vendors also benefit since an easy transfer of records would simplify a hospital’s transition from one EHR to another. So, as with most deficiencies in the EHR, physicians are left to find ways around these problems. Sometimes, we need to go to comical lengths.
Two months ago, a patient pointed to a large machine behind our check-in desk. “What is that,” he asked incredulously; it was a fax machine. While my competence with this apparatus is marginal (my office staff has taken to yelling “doctor faxing!” to alert one another that I am about to inadvertently copy or scan my documents into oblivion), faxes remain a mainstay of medical care. Abandoned by modern business practices as a relic of the 1980s, why are we constantly faxing medical information? Because we are not the customer.
Disruption is now a favorable term in business. Doctors are busy people. BUSY people. Most of us walk a tightrope, a razor-thin timeline. Will we see the next patient in time, the next surgery? Will we get the medical records done today? Will we get the dictations done before being suspended? Will we make the committee meeting, the conference call, the next clinic across town? Will we have dinner with our spouse or see our kids today? Will we make it to the parent-teacher conference inexplicably scheduled for 10:45 a.m. on a Tuesday??!! When deciding between work commitments and family, we side with work overwhelmingly (and depressingly). Explaining this to a layperson is an impossible feat. I have stopped trying, stopped making excuses. Only we know how catastrophic “disruption” can be. Disruption in a 40-patient clinic. Disruption in the trauma bay. I have seen physicians reduced to tears by this disruption. Some activities need disruption. Typing with your back to the patient. Onerous documentation to facilitate billing. Faxing medical records. Will these be disrupted? Who is the customer?
In 1999, the Institute of Medicine started this process, telling us, “To err is human.” I now respond with another Alexander Pope quote, “The same ambition can destroy or save.” The money and influence of EHR vendors destroyed the chance to nationalize the most successful EHR our country has ever seen. What happens now? EHRs are incontrovertibly associated with burnout. Burnout is incontrovertibly associated with outcomes ranging from early retirement to suicide. EHRs cause physician harm. Major vendors can follow the Big Tobacco play book and deny the obvious, but the burden of proof is shifting to them. With their billions of dollars in profits, what have they done to study this problem? To help?
Who is their customer?
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
References
Institute of Medicine (US) Committee on Quality of Health Care in America. 2000. To Err Is Human: Building a Safer Health System. Washington: The National Academies Press.
Weed LL. Medical records that guide and teach. N Engl J Med. 1968 Mar 14;278(11):593-600.
Longman P. “Best Care Anywhere: Why VA Health Care Is Better Than Yours.” (Oakland: Berrett-Koehler Publishers).
In 2000, the Institute of Medicine published “To Err Is Human,” a landmark study that warned that as many as 98,000 people die annually as a result of medical errors. One conclusion of the report stated, “When patients see multiple providers in different settings, none of whom has access to complete information, it becomes easier for things to go wrong.” Government and public reaction to the study resulted in the rushed integration of electronic health records into the U.S. medical system. EHR vendors promised solutions that included a dramatic reduction of preventable errors, a simplified system of physician communication, and the consolidation of a patient’s salient medical information into a single, transferable file. Now, almost 20 years later, these promises remain mostly unfilled. How did we get here?
Systems of medical records have been in place since 1600 B.C. For thousands of years, they consisted mainly of the patient’s diagnosis and the physician’s treatment. In 1968, the New England Journal of Medicine published the special article “Medical Records That Guide and Teach” by Lawrence L. Weed, MD. In the report, Dr. Weed advocated for the organization of medical records by problems rather than by a single diagnosis. This was the birth of our modern system. Medical records would now include lists of symptoms, findings, and problems that would organize the physician’s planning and allow third parties to confirm the initial diagnosis. Nearly concurrent with this publication, the next major innovation was developing in a very unusual location.
In 1999, Fortune magazine labeled Jack Welch “Manager of the Century” for his innovative work as CEO of General Electric. His techniques involved cutting waste and streamlining his workforce. While these methods were somewhat controversial, GE’s market value increased dramatically under his watch. The publishers at Fortune became interested in finding similar innovators in other fields. In this pursuit, they sent journalist Philip Longman to find the “Jack Welch” of health care.
Mr. Longman had recently lost his wife to breast cancer and was becoming obsessed with medical errors and health care quality integration. He set out to discover the best health care system in the United States. After months of research, Mr. Longman reached a startling conclusion. By nearly every metric, the Veterans Affairs system produced the highest quality of care. The key factor in upholding that quality appeared to be the EHR system VistA (Veterans Information Systems and Technology Architecture).
The development of VistA was a grassroots effort begun in the 1970s. Using Tandy computers and Wang processors, the VA “hardhats” sought to develop an electronic system for medical records and communication. This effort was initially opposed and driven underground by the central bureaucracy. Laptops were confiscated, people were fired. Still, development continued, and in 1978, the Decentralized Hospital Computer Program was launched at 20 VA sites. The national rollout occurred in 1994 under the name VistA.
VistA was developed by doctors, for doctors, and routinely enjoys the highest satisfaction rates among all available EHRs. VistA also is an open source model; its code is readily available on the VA website. After seeing the evidence of VistA’s efficacy, Representative Pete Stark (D-CA) introduced HR 6898 on Sept. 15, 2008. The bill would establish a large federal open source health IT system that private hospitals could leverage. The bill also mandated that only open source solutions would receive federal funding. As opposed to proprietary systems, open source models allow for rapid innovation, easy personal configuration, and incorporation of open source apps from unlimited numbers of contributors.
HR 6898 never passed, despite initial bipartisan support. By relying on lobbyists, marketing, and money, the proprietary EHR vendors killed the Stark bill. After a 4-month scramble, the Health Information Technology for Economic and Clinical Health Act (HITECH) passed, with EHR vendor support. HITECH established a certification system for EHRs. While the Stark bill envisioned a single, open source network, there were soon hundreds of certified EHR systems in the United States.
Before the HITECH Act, many EHRs existed, but several barriers blocked full implementation. Early systems were essentially electronic filing cabinets. Their developers had not anticipated the lack of standardization among physicians and hospital systems. The need for custom EHR bases frustrated the vendors. The question of marketing was omnipresent. Who was the actual customer? An economic model developed in which clinicians would bear the time and even financial costs as the benefits would be passed on to insurers, hospitals, and, presumably, the patients.
EHRs needed to become practical, affordable, and interoperable, but who was demanding this? Where was the financial motivation? In the beginning, vendors of EHRs had to convince doctors, the public, and the government of their worth. Now, essentially mandated by the HITECH Act, they only had to sell themselves to hospital administrators, who often had a different motive. Profits.
Many of today’s EHRs are simply modified billing platforms, and doctors are paying the price. The Meaningful Use standards were meant to provide financial incentives for EHR adoption. Stage 2 required EHRs to be able to transport clinical information from one system to another. Looking at our actual practices can provide a master class in the gap between “be able to” and “actually doing.” Again, who does the EHR vendor see as the customer? Certainly not the physician. My patients can list every type of inferior vena cava filter (or at least those with pending legal action), but most of them have never heard of an EHR. Just like “service lines,” EHRs can make it very difficult for patients to seek care outside of their primary system. Who would see this barrier in communication as a perk and not a deficiency? Hospital administrators. The free transfer of medical records is bad for business. Therefore, hospitals don’t prioritize it in their EHRs. The EHR vendors also benefit since an easy transfer of records would simplify a hospital’s transition from one EHR to another. So, as with most deficiencies in the EHR, physicians are left to find ways around these problems. Sometimes, we need to go to comical lengths.
Two months ago, a patient pointed to a large machine behind our check-in desk. “What is that,” he asked incredulously; it was a fax machine. While my competence with this apparatus is marginal (my office staff has taken to yelling “doctor faxing!” to alert one another that I am about to inadvertently copy or scan my documents into oblivion), faxes remain a mainstay of medical care. Abandoned by modern business practices as a relic of the 1980s, why are we constantly faxing medical information? Because we are not the customer.
Disruption is now a favorable term in business. Doctors are busy people. BUSY people. Most of us walk a tightrope, a razor-thin timeline. Will we see the next patient in time, the next surgery? Will we get the medical records done today? Will we get the dictations done before being suspended? Will we make the committee meeting, the conference call, the next clinic across town? Will we have dinner with our spouse or see our kids today? Will we make it to the parent-teacher conference inexplicably scheduled for 10:45 a.m. on a Tuesday??!! When deciding between work commitments and family, we side with work overwhelmingly (and depressingly). Explaining this to a layperson is an impossible feat. I have stopped trying, stopped making excuses. Only we know how catastrophic “disruption” can be. Disruption in a 40-patient clinic. Disruption in the trauma bay. I have seen physicians reduced to tears by this disruption. Some activities need disruption. Typing with your back to the patient. Onerous documentation to facilitate billing. Faxing medical records. Will these be disrupted? Who is the customer?
In 1999, the Institute of Medicine started this process, telling us, “To err is human.” I now respond with another Alexander Pope quote, “The same ambition can destroy or save.” The money and influence of EHR vendors destroyed the chance to nationalize the most successful EHR our country has ever seen. What happens now? EHRs are incontrovertibly associated with burnout. Burnout is incontrovertibly associated with outcomes ranging from early retirement to suicide. EHRs cause physician harm. Major vendors can follow the Big Tobacco play book and deny the obvious, but the burden of proof is shifting to them. With their billions of dollars in profits, what have they done to study this problem? To help?
Who is their customer?
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, division of vascular and endovascular surgery, Louisiana State University Health Sciences Center, New Orleans.
References
Institute of Medicine (US) Committee on Quality of Health Care in America. 2000. To Err Is Human: Building a Safer Health System. Washington: The National Academies Press.
Weed LL. Medical records that guide and teach. N Engl J Med. 1968 Mar 14;278(11):593-600.
Longman P. “Best Care Anywhere: Why VA Health Care Is Better Than Yours.” (Oakland: Berrett-Koehler Publishers).
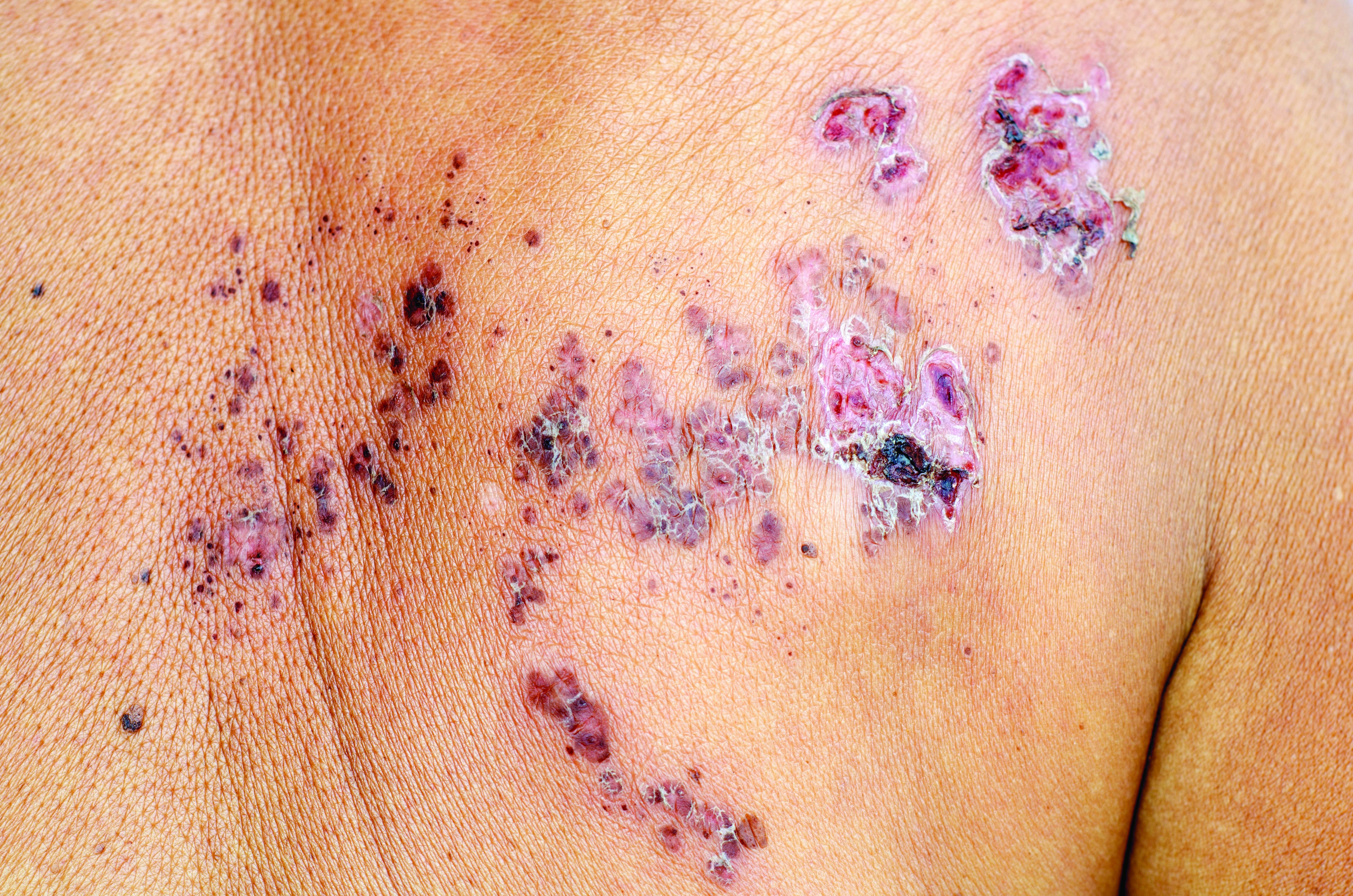
Thiopurines linked to zoster in IBD patients
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: For patients with inflammatory bowel disease, thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid monotherapy.
Major finding: The adjusted hazard ratio was 1.47 (95% confidence interval, 1.31-1.65; P less than .001).
Study details: Two large retrospective cohort studies of veterans with and without inflammatory bowel disease.
Disclosures: Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
Source: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
NIH Program Enhances Diversity Among Researchers
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
The NIH has chosen 13 researchers for the inaugural class of the Distinguished Scholars Program (DSP), launched earlier this year to build diversity within the NIH Intramural Research Program. “Nurturing diversity in the NIH Intramural Research Program is paramount to upholding our mission,” said NIH Director Francis Collins, MD, PhD. Research has shown that a “diversity of perspectives” is vital to the improved quality and number of discoveries, he adds.
The DSP aims to facilitate hiring and career progression of tenure-track investigators who have demonstrated commitment to promoting diversity and inclusion in the biomedical research workforce, according to the NIH. The DSP is unique in its focus on early-stage investigators, says Hannah A. Valantine, MD, NIH Chief Officer for Scientific Workforce Diversity. She says that is the “major point where we lose underrepresented groups from scientific careers.”
Dr. Collins says the DSP can serve as a model for universities to prevent the attrition of underrepresented groups, including women, blacks, Hispanics or Latinos, American Indians and Alaska Natives, Native Hawaiians and other Pacific Islanders, individuals with disabilities, and individuals from disadvantaged backgrounds.
The pilot program will fund 3 cohorts of up to 15 scholars each. Nominees are chosen for their scientific excellence and commitment to diversity and inclusion, shown through participation in activities, such as mentoring programs.
Scholars will receive 4 years of research support of up to $2.35 million from the DSP; their nominating institute or center will continue to fund their research throughout their tenure track. Each scholar also will be mentored by a highly experienced NIH senior investigator and receive professional leadership training, workshops on management skills, and networking opportunities with NIH leadership.
Source:
NIH selects first scholars in pioneering program to enhance diversity within inhouse research program [news release]. Bethesda, MD: National Institutes of Health; October 23, 2018. https://www.nih.gov/news-events/news-releases/nih-selects-first-scholars-pioneering-program-enhance-diversity-within-house-research-program . Accessed October 31, 2018.
Palliative care update highlights role of nonspecialists
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
Jack Rozel: Gun violence
Dr. Rozel makes his home and practices in Pittsburgh, the site of the tragic mass shooting at the Tree of Life temple.
Dr. Rozel makes his home and practices in Pittsburgh, the site of the tragic mass shooting at the Tree of Life temple.
Dr. Rozel makes his home and practices in Pittsburgh, the site of the tragic mass shooting at the Tree of Life temple.
NSAID risk score validated for CV events
Also today, the ACIP resuscitates pertussis working group, it’s important to talk to adolescents about sexual assault, and costs increase for gun injuries in children.
Amazon Alexa
Apple Podcasts
Spotify
Also today, the ACIP resuscitates pertussis working group, it’s important to talk to adolescents about sexual assault, and costs increase for gun injuries in children.
Amazon Alexa
Apple Podcasts
Spotify
Also today, the ACIP resuscitates pertussis working group, it’s important to talk to adolescents about sexual assault, and costs increase for gun injuries in children.
Amazon Alexa
Apple Podcasts
Spotify
Part B scheme raises concerns
Also today, statins cut all-cause mortality in spinal cord injury, ACR readies first-ever guidelines on managing reproductive health, and primary care holds the key to curbing early-onset colorectal cancer.
Amazon Alexa
Apple Podcasts
Spotify
Also today, statins cut all-cause mortality in spinal cord injury, ACR readies first-ever guidelines on managing reproductive health, and primary care holds the key to curbing early-onset colorectal cancer.
Amazon Alexa
Apple Podcasts
Spotify
Also today, statins cut all-cause mortality in spinal cord injury, ACR readies first-ever guidelines on managing reproductive health, and primary care holds the key to curbing early-onset colorectal cancer.
Amazon Alexa
Apple Podcasts
Spotify
VA Honors Elizabeth Dole—and Caregivers—in New Center of Excellence
The Elizabeth Dole Center of Excellence for Veteran and Caregiver Research, the first of its kind, recognizes Senator Dole for her national leadership and advocacy on behalf of the nation’s 5.5 million military and veteran caregivers.
Managed by the Office of Health Services, the center will “serve as the model for excellence” for peer-reviewed research on innovation, training, evaluation, implementation, and dissemination of best practices in supporting caregivers of veterans.
The team of VA investigators will be led by Dr. Luci Leykum of the South Texas Veterans Health Care System. Collaborating sites and leaders include Dr. Stuti Dang of the Miami VA Health Care System, Dr. Mary Jo Pugh of the VA Salt Lake City Health Care System, and Dr. Ranak Trivedi of the VA Palo Alto Health Care System.
The Elizabeth Dole Center of Excellence for Veteran and Caregiver Research, the first of its kind, recognizes Senator Dole for her national leadership and advocacy on behalf of the nation’s 5.5 million military and veteran caregivers.
Managed by the Office of Health Services, the center will “serve as the model for excellence” for peer-reviewed research on innovation, training, evaluation, implementation, and dissemination of best practices in supporting caregivers of veterans.
The team of VA investigators will be led by Dr. Luci Leykum of the South Texas Veterans Health Care System. Collaborating sites and leaders include Dr. Stuti Dang of the Miami VA Health Care System, Dr. Mary Jo Pugh of the VA Salt Lake City Health Care System, and Dr. Ranak Trivedi of the VA Palo Alto Health Care System.
The Elizabeth Dole Center of Excellence for Veteran and Caregiver Research, the first of its kind, recognizes Senator Dole for her national leadership and advocacy on behalf of the nation’s 5.5 million military and veteran caregivers.
Managed by the Office of Health Services, the center will “serve as the model for excellence” for peer-reviewed research on innovation, training, evaluation, implementation, and dissemination of best practices in supporting caregivers of veterans.
The team of VA investigators will be led by Dr. Luci Leykum of the South Texas Veterans Health Care System. Collaborating sites and leaders include Dr. Stuti Dang of the Miami VA Health Care System, Dr. Mary Jo Pugh of the VA Salt Lake City Health Care System, and Dr. Ranak Trivedi of the VA Palo Alto Health Care System.
Most Americans incorrectly identify homicide as more common than suicide
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Only 13.5% of U.S. adults – and 20% of health care professionals – could identify the most frequent cause of violent death in their state.
Major finding:
Study details: A study of 3,811 responses to the National Firearms Survey.
Disclosures: The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
Source: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
AKI linked to later dementia
ACIP votes unanimously in favor of immunization schedule updated and redesign, could daptomycin/fosfomycin be a new standard for MRSA bacteremia? Plus, expert analysis on Justice Kavanaugh’s lasting healthcare impact.
Amazon Alexa
Apple Podcasts
Spotify
ACIP votes unanimously in favor of immunization schedule updated and redesign, could daptomycin/fosfomycin be a new standard for MRSA bacteremia? Plus, expert analysis on Justice Kavanaugh’s lasting healthcare impact.
Amazon Alexa
Apple Podcasts
Spotify
ACIP votes unanimously in favor of immunization schedule updated and redesign, could daptomycin/fosfomycin be a new standard for MRSA bacteremia? Plus, expert analysis on Justice Kavanaugh’s lasting healthcare impact.
Amazon Alexa
Apple Podcasts
Spotify