User login
Mitoxantrone lots recalled worldwide

Credit: Bill Branson
Hospira, Inc. has initiated a worldwide, user-level recall of 10 lots of Mitoxantrone (both human and veterinary) due to confirmed subpotency and elevated impurity levels.
Drugs in the affected lots may exhibit decreased effectiveness, require additional dosing, or prompt cumulative impurity toxicity requiring medical intervention.
However, Hospira has not received reports of any adverse events associated with subpotency and impurities for these lots to date.
The lots were distributed to hospitals and veterinary clinics worldwide from February 2013 through November 2014.
The following lots are affected by the recall. (To ensure this list displays properly, click the “Hide” icon on the right side of this page to hide the “In this Section” column.)
United States
Product NDC Number Lot Expiration Date
MitoXANTRONE Injection, USP, 61703-343-18 Z054636AA December 2014
(concentrate) 20 mg/10 mL, A014636AA April 2015
2 mg/mL in 10 mL, 10 mL Vial, A024636AB July 2015
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-65 A014643AA April 2015
(concentrate) 25 mg/12.5 mL,
2 mg/mL in 12.5 mL, 12.5 mL Vial,
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-66 A014645AA November 2015
(concentrate) 30 mg/15 mL,
2 mg/mL in 15 mL, 15 mL Vial,
Multi Dose Vial
Australia and New Zealand
Product Product Code Batch Number Expiration Date
DBL™ MitoXANTRONE M4636A A024636AA July 2015
Hydrochloride Injection
(concentrate) 20mg/10mL
Injection Vial
United Kingdom, Ireland, Cyprus, Saudi Arabia, Qatar, Oman and Bahrain
Product List Number Lot Expiration Date
MitoXANTRONE 2 mg/mL; M4636AGB1 A014636AB April 2015
Concentrate for Infusion A024636AD July 2015
Z054636AB Dec 2014
Canada
Product List Number DIN Lot Expiration Date
MitoXANTRONE for
Injection 20mg /10mL USP 4636A001 02244614 A024636AC July 2015
Anyone with an existing inventory of the recalled lots should stop use and distribution, and quarantine the product immediately. This recall is being carried out to the user level (both human and veterinary).
Hospira has notified its direct customers via a recall letter and is arranging for impacted product to be returned to Stericycle in the US. For additional assistance in the US, call Stericycle at 1-844-265-7407 between the hours of 8 am and 5 pm ET, Monday through Friday. Customers outside the US should work with their local Hospira offices to return the product per local recall notifications.
For medical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or medcom@hospira.com (Available 24 hours a day/7 days per week).
To report adverse events or for product complaints, contact Hospira Global Complaint Management at 1-800-441-4100 (M-F, 8 am to 5 pm CT).
Adverse events or quality problems associated with Mitoxantrone can also be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()

Credit: Bill Branson
Hospira, Inc. has initiated a worldwide, user-level recall of 10 lots of Mitoxantrone (both human and veterinary) due to confirmed subpotency and elevated impurity levels.
Drugs in the affected lots may exhibit decreased effectiveness, require additional dosing, or prompt cumulative impurity toxicity requiring medical intervention.
However, Hospira has not received reports of any adverse events associated with subpotency and impurities for these lots to date.
The lots were distributed to hospitals and veterinary clinics worldwide from February 2013 through November 2014.
The following lots are affected by the recall. (To ensure this list displays properly, click the “Hide” icon on the right side of this page to hide the “In this Section” column.)
United States
Product NDC Number Lot Expiration Date
MitoXANTRONE Injection, USP, 61703-343-18 Z054636AA December 2014
(concentrate) 20 mg/10 mL, A014636AA April 2015
2 mg/mL in 10 mL, 10 mL Vial, A024636AB July 2015
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-65 A014643AA April 2015
(concentrate) 25 mg/12.5 mL,
2 mg/mL in 12.5 mL, 12.5 mL Vial,
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-66 A014645AA November 2015
(concentrate) 30 mg/15 mL,
2 mg/mL in 15 mL, 15 mL Vial,
Multi Dose Vial
Australia and New Zealand
Product Product Code Batch Number Expiration Date
DBL™ MitoXANTRONE M4636A A024636AA July 2015
Hydrochloride Injection
(concentrate) 20mg/10mL
Injection Vial
United Kingdom, Ireland, Cyprus, Saudi Arabia, Qatar, Oman and Bahrain
Product List Number Lot Expiration Date
MitoXANTRONE 2 mg/mL; M4636AGB1 A014636AB April 2015
Concentrate for Infusion A024636AD July 2015
Z054636AB Dec 2014
Canada
Product List Number DIN Lot Expiration Date
MitoXANTRONE for
Injection 20mg /10mL USP 4636A001 02244614 A024636AC July 2015
Anyone with an existing inventory of the recalled lots should stop use and distribution, and quarantine the product immediately. This recall is being carried out to the user level (both human and veterinary).
Hospira has notified its direct customers via a recall letter and is arranging for impacted product to be returned to Stericycle in the US. For additional assistance in the US, call Stericycle at 1-844-265-7407 between the hours of 8 am and 5 pm ET, Monday through Friday. Customers outside the US should work with their local Hospira offices to return the product per local recall notifications.
For medical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or medcom@hospira.com (Available 24 hours a day/7 days per week).
To report adverse events or for product complaints, contact Hospira Global Complaint Management at 1-800-441-4100 (M-F, 8 am to 5 pm CT).
Adverse events or quality problems associated with Mitoxantrone can also be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()

Credit: Bill Branson
Hospira, Inc. has initiated a worldwide, user-level recall of 10 lots of Mitoxantrone (both human and veterinary) due to confirmed subpotency and elevated impurity levels.
Drugs in the affected lots may exhibit decreased effectiveness, require additional dosing, or prompt cumulative impurity toxicity requiring medical intervention.
However, Hospira has not received reports of any adverse events associated with subpotency and impurities for these lots to date.
The lots were distributed to hospitals and veterinary clinics worldwide from February 2013 through November 2014.
The following lots are affected by the recall. (To ensure this list displays properly, click the “Hide” icon on the right side of this page to hide the “In this Section” column.)
United States
Product NDC Number Lot Expiration Date
MitoXANTRONE Injection, USP, 61703-343-18 Z054636AA December 2014
(concentrate) 20 mg/10 mL, A014636AA April 2015
2 mg/mL in 10 mL, 10 mL Vial, A024636AB July 2015
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-65 A014643AA April 2015
(concentrate) 25 mg/12.5 mL,
2 mg/mL in 12.5 mL, 12.5 mL Vial,
Multi Dose Vial
MitoXANTRONE Injection, USP, 61703-343-66 A014645AA November 2015
(concentrate) 30 mg/15 mL,
2 mg/mL in 15 mL, 15 mL Vial,
Multi Dose Vial
Australia and New Zealand
Product Product Code Batch Number Expiration Date
DBL™ MitoXANTRONE M4636A A024636AA July 2015
Hydrochloride Injection
(concentrate) 20mg/10mL
Injection Vial
United Kingdom, Ireland, Cyprus, Saudi Arabia, Qatar, Oman and Bahrain
Product List Number Lot Expiration Date
MitoXANTRONE 2 mg/mL; M4636AGB1 A014636AB April 2015
Concentrate for Infusion A024636AD July 2015
Z054636AB Dec 2014
Canada
Product List Number DIN Lot Expiration Date
MitoXANTRONE for
Injection 20mg /10mL USP 4636A001 02244614 A024636AC July 2015
Anyone with an existing inventory of the recalled lots should stop use and distribution, and quarantine the product immediately. This recall is being carried out to the user level (both human and veterinary).
Hospira has notified its direct customers via a recall letter and is arranging for impacted product to be returned to Stericycle in the US. For additional assistance in the US, call Stericycle at 1-844-265-7407 between the hours of 8 am and 5 pm ET, Monday through Friday. Customers outside the US should work with their local Hospira offices to return the product per local recall notifications.
For medical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or medcom@hospira.com (Available 24 hours a day/7 days per week).
To report adverse events or for product complaints, contact Hospira Global Complaint Management at 1-800-441-4100 (M-F, 8 am to 5 pm CT).
Adverse events or quality problems associated with Mitoxantrone can also be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()
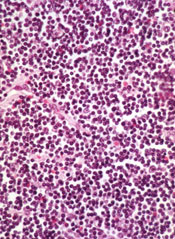
FDA approves new formulation of drug for ALL

The US Food and Drug Administration (FDA) has approved the intravenous administration of asparaginase Erwinia chrysanthemi (Erwinaze).
The product is indicated as a component of a multi-agent chemotherapy regimen to treat patients with acute lymphoblastic leukemia (ALL) who have developed hypersensitivity to E coli-derived asparaginase.
Previously, the only FDA-approved route of administration for asparaginase Erwinia chrysanthemi was through intramuscular injection.
The FDA’s decision to expand the drug’s use was based on a pharmacokinetic study (published in Blood in 2013) of intravenous asparaginase Erwinia chrysanthemi.
The trial included 30 patients with ALL or lymphoblastic lymphoma who developed hypersensitivity (grade ≥ 2) to E coli–derived asparaginase. The patients’ median age was 6.5 years (range, 1-17), 63% were male, and 83% were Caucasian.
Patients received intravenous asparaginase Erwinia chrysanthemi at 25,000 IU/m2/dose, on a Monday/Wednesday/Friday schedule for 2 consecutive weeks (6 doses=1 cycle) for each dose of pegaspargase remaining in their original treatment plan. All other chemotherapy was continued per the original treatment plan.
Before the first dose of intravenous asparaginase Erwinia chrysanthemi, nadir serum asparaginase activity (NSAA) levels were below the limit of quantification (defined as 0.0129 IU/mL) for 91% of patients.
The study’s primary endpoint was the proportion of patients who achieved NSAA ≥ 0.1 IU/mL, which has been associated with complete asparagine depletion, at 48 hours after dose 5 in cycle 1. Nineteen of the 23 evaluable patients (83%) achieved this endpoint.
A secondary objective of the study was to determine the proportion of patients who achieved NSAA ≥ 0.1 IU/mL at 72 hours after dose 6 in cycle 1. Nine patients (45%) achieved this endpoint.
In all 30 patients, the most common asparaginase-related toxicities reported during cycle 1 were hypersensitivity (23%), vomiting (20%), nausea (20%), and hyperglycemia (13%). Pancreatitis and thrombosis each occurred in 3% of patients. One patient experienced a transient ischemic attack.
The most common grade 3 or 4 adverse event was febrile neutropenia (7%). Four patients discontinued treatment before completing cycle 1—3 of them due to hypersensitivity and 1 due to pancreatitis. There were no deaths.
This study was funded by Jazz Pharmaceuticals, the company developing asparaginase Erwinia chrysanthemi. ![]()

The US Food and Drug Administration (FDA) has approved the intravenous administration of asparaginase Erwinia chrysanthemi (Erwinaze).
The product is indicated as a component of a multi-agent chemotherapy regimen to treat patients with acute lymphoblastic leukemia (ALL) who have developed hypersensitivity to E coli-derived asparaginase.
Previously, the only FDA-approved route of administration for asparaginase Erwinia chrysanthemi was through intramuscular injection.
The FDA’s decision to expand the drug’s use was based on a pharmacokinetic study (published in Blood in 2013) of intravenous asparaginase Erwinia chrysanthemi.
The trial included 30 patients with ALL or lymphoblastic lymphoma who developed hypersensitivity (grade ≥ 2) to E coli–derived asparaginase. The patients’ median age was 6.5 years (range, 1-17), 63% were male, and 83% were Caucasian.
Patients received intravenous asparaginase Erwinia chrysanthemi at 25,000 IU/m2/dose, on a Monday/Wednesday/Friday schedule for 2 consecutive weeks (6 doses=1 cycle) for each dose of pegaspargase remaining in their original treatment plan. All other chemotherapy was continued per the original treatment plan.
Before the first dose of intravenous asparaginase Erwinia chrysanthemi, nadir serum asparaginase activity (NSAA) levels were below the limit of quantification (defined as 0.0129 IU/mL) for 91% of patients.
The study’s primary endpoint was the proportion of patients who achieved NSAA ≥ 0.1 IU/mL, which has been associated with complete asparagine depletion, at 48 hours after dose 5 in cycle 1. Nineteen of the 23 evaluable patients (83%) achieved this endpoint.
A secondary objective of the study was to determine the proportion of patients who achieved NSAA ≥ 0.1 IU/mL at 72 hours after dose 6 in cycle 1. Nine patients (45%) achieved this endpoint.
In all 30 patients, the most common asparaginase-related toxicities reported during cycle 1 were hypersensitivity (23%), vomiting (20%), nausea (20%), and hyperglycemia (13%). Pancreatitis and thrombosis each occurred in 3% of patients. One patient experienced a transient ischemic attack.
The most common grade 3 or 4 adverse event was febrile neutropenia (7%). Four patients discontinued treatment before completing cycle 1—3 of them due to hypersensitivity and 1 due to pancreatitis. There were no deaths.
This study was funded by Jazz Pharmaceuticals, the company developing asparaginase Erwinia chrysanthemi. ![]()

The US Food and Drug Administration (FDA) has approved the intravenous administration of asparaginase Erwinia chrysanthemi (Erwinaze).
The product is indicated as a component of a multi-agent chemotherapy regimen to treat patients with acute lymphoblastic leukemia (ALL) who have developed hypersensitivity to E coli-derived asparaginase.
Previously, the only FDA-approved route of administration for asparaginase Erwinia chrysanthemi was through intramuscular injection.
The FDA’s decision to expand the drug’s use was based on a pharmacokinetic study (published in Blood in 2013) of intravenous asparaginase Erwinia chrysanthemi.
The trial included 30 patients with ALL or lymphoblastic lymphoma who developed hypersensitivity (grade ≥ 2) to E coli–derived asparaginase. The patients’ median age was 6.5 years (range, 1-17), 63% were male, and 83% were Caucasian.
Patients received intravenous asparaginase Erwinia chrysanthemi at 25,000 IU/m2/dose, on a Monday/Wednesday/Friday schedule for 2 consecutive weeks (6 doses=1 cycle) for each dose of pegaspargase remaining in their original treatment plan. All other chemotherapy was continued per the original treatment plan.
Before the first dose of intravenous asparaginase Erwinia chrysanthemi, nadir serum asparaginase activity (NSAA) levels were below the limit of quantification (defined as 0.0129 IU/mL) for 91% of patients.
The study’s primary endpoint was the proportion of patients who achieved NSAA ≥ 0.1 IU/mL, which has been associated with complete asparagine depletion, at 48 hours after dose 5 in cycle 1. Nineteen of the 23 evaluable patients (83%) achieved this endpoint.
A secondary objective of the study was to determine the proportion of patients who achieved NSAA ≥ 0.1 IU/mL at 72 hours after dose 6 in cycle 1. Nine patients (45%) achieved this endpoint.
In all 30 patients, the most common asparaginase-related toxicities reported during cycle 1 were hypersensitivity (23%), vomiting (20%), nausea (20%), and hyperglycemia (13%). Pancreatitis and thrombosis each occurred in 3% of patients. One patient experienced a transient ischemic attack.
The most common grade 3 or 4 adverse event was febrile neutropenia (7%). Four patients discontinued treatment before completing cycle 1—3 of them due to hypersensitivity and 1 due to pancreatitis. There were no deaths.
This study was funded by Jazz Pharmaceuticals, the company developing asparaginase Erwinia chrysanthemi. ![]()
CHMP supports expanding use of lenalidomide in MM

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending approval of continuous oral treatment with lenalidomide (Revlimid) in adults with previously untreated multiple myeloma (MM) who are ineligible for hematopoietic stem cell transplant (HSCT).
The European Commission, which generally follows the CHMP’s recommendations, is expected to make its final decision in about 2 months.
Lenalidomide is not currently approved to treat newly diagnosed MM in any country.
The drug is approved in the European Union (EU) for use in combination with dexamethasone to treat adults with MM who have received at least one prior therapy.
Lenalidomide is also approved in the EU to treat patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with 5q deletion when other therapeutic options are insufficient or inadequate.
The CHMP’s recommendation to extend the use of lenalidomide to HSCT-ineligible patients with newly diagnosed MM was based on the results of 2 studies: MM-015 and MM-020, also known as FIRST.
The FIRST trial
In the phase 3 FIRST trial, researchers enrolled 1623 patients who were newly diagnosed with MM and not eligible for HSCT.
Patients were randomized to receive lenalidomide and dexamethasone (Rd) in 28-day cycles until disease progression (n=535), 18 cycles of lenalidomide and dexamethasone (Rd18) for 72 weeks (n=541), or melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
Response rates were significantly better with continuous Rd (75%) and Rd18 (73%) than with MPT (62%, P<0.001 for both comparisons). Complete response rates were 15%, 14%, and 9%, respectively.
The median progression-free survival was 25.5 months with continuous Rd, 20.7 months with Rd18, and 21.2 months with MPT.
This resulted in a 28% reduction in the risk of progression or death for patients treated with continuous Rd compared with those treated with MPT (hazard ratio[HR]=0.72, P<0.001) and a 30% reduction compared with Rd18 (HR=0.70, P<0.001).
The pre-planned interim analysis of overall survival showed a 22% reduction in the risk of death for continuous Rd vs MPT (HR=0.78, P=0.02), but the difference did not cross the pre-specified superiority boundary (P<0.0096).
Adverse events reported in 20% or more of patients in the continuous Rd, Rd18, or MPT arms included diarrhea (45.5%, 38.5%, 16.5%), anemia (43.8%, 35.7%, 42.3%), neutropenia (35.0%, 33.0%, 60.6%), fatigue (32.5%, 32.8%, 28.5%), back pain (32.0%, 26.9%, 21.4%), insomnia (27.6%, 23.5%, 9.8%), asthenia (28.2%, 22.8%, 22.9%), rash (26.1%, 28.0%, 19.4%), decreased appetite (23.1%, 21.3%, 13.3%), cough (22.7%, 17.4%, 12.6%), pyrexia (21.4%, 18.9%, 14.0%), muscle spasms (20.5%, 18.9%, 11.3%) and abdominal pain (20.5%, 14.4%, 11.1%).
The incidence of invasive second primary malignancies was 3% in patients taking continuous Rd, 6% in patients taking Rd18, and 5% in those taking MPT. The overall incidence of solid tumors was identical in the continuous Rd and MPT arms (3%) and 5% in the Rd18 arm.
The MM-015 trial
In the phase 3 MM-015 study, researchers enrolled 459 patients who were 65 or older and newly diagnosed with MM. The team compared melphalan-prednisone-lenalidomide induction followed by lenalidomide maintenance (MPR-R) with melphalan-prednisone-lenalidomide (MPR) or melphalan-prednisone (MP) followed by placebo.
Patients who received MPR-R or MPR had significantly better response rates than patients who received MP, at 77%, 68%, and 50%, respectively (P<0.001 and P=0.002, respectively, for the comparison with MP).
And the median progression-free survival was significantly longer with MPR-R (31 months) than with MPR (14 months, HR=0.49, P<0.001) or MP (13 months, HR=0.40, P<0.001).
During induction, the most frequent adverse events were hematologic. Grade 4 neutropenia occurred in 35% of patients in the MPR-R arm, 32% in the MPR arm, and 8% in the MP arm. The 3-year rate of second primary malignancies was 7%, 7%, and 3%, respectively. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending approval of continuous oral treatment with lenalidomide (Revlimid) in adults with previously untreated multiple myeloma (MM) who are ineligible for hematopoietic stem cell transplant (HSCT).
The European Commission, which generally follows the CHMP’s recommendations, is expected to make its final decision in about 2 months.
Lenalidomide is not currently approved to treat newly diagnosed MM in any country.
The drug is approved in the European Union (EU) for use in combination with dexamethasone to treat adults with MM who have received at least one prior therapy.
Lenalidomide is also approved in the EU to treat patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with 5q deletion when other therapeutic options are insufficient or inadequate.
The CHMP’s recommendation to extend the use of lenalidomide to HSCT-ineligible patients with newly diagnosed MM was based on the results of 2 studies: MM-015 and MM-020, also known as FIRST.
The FIRST trial
In the phase 3 FIRST trial, researchers enrolled 1623 patients who were newly diagnosed with MM and not eligible for HSCT.
Patients were randomized to receive lenalidomide and dexamethasone (Rd) in 28-day cycles until disease progression (n=535), 18 cycles of lenalidomide and dexamethasone (Rd18) for 72 weeks (n=541), or melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
Response rates were significantly better with continuous Rd (75%) and Rd18 (73%) than with MPT (62%, P<0.001 for both comparisons). Complete response rates were 15%, 14%, and 9%, respectively.
The median progression-free survival was 25.5 months with continuous Rd, 20.7 months with Rd18, and 21.2 months with MPT.
This resulted in a 28% reduction in the risk of progression or death for patients treated with continuous Rd compared with those treated with MPT (hazard ratio[HR]=0.72, P<0.001) and a 30% reduction compared with Rd18 (HR=0.70, P<0.001).
The pre-planned interim analysis of overall survival showed a 22% reduction in the risk of death for continuous Rd vs MPT (HR=0.78, P=0.02), but the difference did not cross the pre-specified superiority boundary (P<0.0096).
Adverse events reported in 20% or more of patients in the continuous Rd, Rd18, or MPT arms included diarrhea (45.5%, 38.5%, 16.5%), anemia (43.8%, 35.7%, 42.3%), neutropenia (35.0%, 33.0%, 60.6%), fatigue (32.5%, 32.8%, 28.5%), back pain (32.0%, 26.9%, 21.4%), insomnia (27.6%, 23.5%, 9.8%), asthenia (28.2%, 22.8%, 22.9%), rash (26.1%, 28.0%, 19.4%), decreased appetite (23.1%, 21.3%, 13.3%), cough (22.7%, 17.4%, 12.6%), pyrexia (21.4%, 18.9%, 14.0%), muscle spasms (20.5%, 18.9%, 11.3%) and abdominal pain (20.5%, 14.4%, 11.1%).
The incidence of invasive second primary malignancies was 3% in patients taking continuous Rd, 6% in patients taking Rd18, and 5% in those taking MPT. The overall incidence of solid tumors was identical in the continuous Rd and MPT arms (3%) and 5% in the Rd18 arm.
The MM-015 trial
In the phase 3 MM-015 study, researchers enrolled 459 patients who were 65 or older and newly diagnosed with MM. The team compared melphalan-prednisone-lenalidomide induction followed by lenalidomide maintenance (MPR-R) with melphalan-prednisone-lenalidomide (MPR) or melphalan-prednisone (MP) followed by placebo.
Patients who received MPR-R or MPR had significantly better response rates than patients who received MP, at 77%, 68%, and 50%, respectively (P<0.001 and P=0.002, respectively, for the comparison with MP).
And the median progression-free survival was significantly longer with MPR-R (31 months) than with MPR (14 months, HR=0.49, P<0.001) or MP (13 months, HR=0.40, P<0.001).
During induction, the most frequent adverse events were hematologic. Grade 4 neutropenia occurred in 35% of patients in the MPR-R arm, 32% in the MPR arm, and 8% in the MP arm. The 3-year rate of second primary malignancies was 7%, 7%, and 3%, respectively. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) is recommending approval of continuous oral treatment with lenalidomide (Revlimid) in adults with previously untreated multiple myeloma (MM) who are ineligible for hematopoietic stem cell transplant (HSCT).
The European Commission, which generally follows the CHMP’s recommendations, is expected to make its final decision in about 2 months.
Lenalidomide is not currently approved to treat newly diagnosed MM in any country.
The drug is approved in the European Union (EU) for use in combination with dexamethasone to treat adults with MM who have received at least one prior therapy.
Lenalidomide is also approved in the EU to treat patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes associated with 5q deletion when other therapeutic options are insufficient or inadequate.
The CHMP’s recommendation to extend the use of lenalidomide to HSCT-ineligible patients with newly diagnosed MM was based on the results of 2 studies: MM-015 and MM-020, also known as FIRST.
The FIRST trial
In the phase 3 FIRST trial, researchers enrolled 1623 patients who were newly diagnosed with MM and not eligible for HSCT.
Patients were randomized to receive lenalidomide and dexamethasone (Rd) in 28-day cycles until disease progression (n=535), 18 cycles of lenalidomide and dexamethasone (Rd18) for 72 weeks (n=541), or melphalan, prednisone, and thalidomide (MPT) for 72 weeks (n=547).
Response rates were significantly better with continuous Rd (75%) and Rd18 (73%) than with MPT (62%, P<0.001 for both comparisons). Complete response rates were 15%, 14%, and 9%, respectively.
The median progression-free survival was 25.5 months with continuous Rd, 20.7 months with Rd18, and 21.2 months with MPT.
This resulted in a 28% reduction in the risk of progression or death for patients treated with continuous Rd compared with those treated with MPT (hazard ratio[HR]=0.72, P<0.001) and a 30% reduction compared with Rd18 (HR=0.70, P<0.001).
The pre-planned interim analysis of overall survival showed a 22% reduction in the risk of death for continuous Rd vs MPT (HR=0.78, P=0.02), but the difference did not cross the pre-specified superiority boundary (P<0.0096).
Adverse events reported in 20% or more of patients in the continuous Rd, Rd18, or MPT arms included diarrhea (45.5%, 38.5%, 16.5%), anemia (43.8%, 35.7%, 42.3%), neutropenia (35.0%, 33.0%, 60.6%), fatigue (32.5%, 32.8%, 28.5%), back pain (32.0%, 26.9%, 21.4%), insomnia (27.6%, 23.5%, 9.8%), asthenia (28.2%, 22.8%, 22.9%), rash (26.1%, 28.0%, 19.4%), decreased appetite (23.1%, 21.3%, 13.3%), cough (22.7%, 17.4%, 12.6%), pyrexia (21.4%, 18.9%, 14.0%), muscle spasms (20.5%, 18.9%, 11.3%) and abdominal pain (20.5%, 14.4%, 11.1%).
The incidence of invasive second primary malignancies was 3% in patients taking continuous Rd, 6% in patients taking Rd18, and 5% in those taking MPT. The overall incidence of solid tumors was identical in the continuous Rd and MPT arms (3%) and 5% in the Rd18 arm.
The MM-015 trial
In the phase 3 MM-015 study, researchers enrolled 459 patients who were 65 or older and newly diagnosed with MM. The team compared melphalan-prednisone-lenalidomide induction followed by lenalidomide maintenance (MPR-R) with melphalan-prednisone-lenalidomide (MPR) or melphalan-prednisone (MP) followed by placebo.
Patients who received MPR-R or MPR had significantly better response rates than patients who received MP, at 77%, 68%, and 50%, respectively (P<0.001 and P=0.002, respectively, for the comparison with MP).
And the median progression-free survival was significantly longer with MPR-R (31 months) than with MPR (14 months, HR=0.49, P<0.001) or MP (13 months, HR=0.40, P<0.001).
During induction, the most frequent adverse events were hematologic. Grade 4 neutropenia occurred in 35% of patients in the MPR-R arm, 32% in the MPR arm, and 8% in the MP arm. The 3-year rate of second primary malignancies was 7%, 7%, and 3%, respectively. ![]()
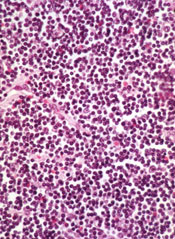
CHMP recommends bortezomib for MCL

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) who are unsuitable for hematopoietic stem cell transplant.
Bortezomib is already approved in the European Union to treat multiple myeloma, either as monotherapy or in combination with other treatment regimens.
The CHMP’s decision to expand the approved use of bortezomib is based on data from the phase 3 LYM-3002 study. Results from this trial were presented at the 2014 ASCO Annual Meeting (abstract 8500).
LYM-3002 included 487 patients newly diagnosed with MCL who were ineligible, or not considered, for transplant. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AE) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85%, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3%, respectively.
The CHMP’s positive opinion will be reviewed by the European Commission, which has the authority to grant a label extension for medicines in the European Economic Area. A final decision on the use of bortezomib in MCL is expected early next year. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) who are unsuitable for hematopoietic stem cell transplant.
Bortezomib is already approved in the European Union to treat multiple myeloma, either as monotherapy or in combination with other treatment regimens.
The CHMP’s decision to expand the approved use of bortezomib is based on data from the phase 3 LYM-3002 study. Results from this trial were presented at the 2014 ASCO Annual Meeting (abstract 8500).
LYM-3002 included 487 patients newly diagnosed with MCL who were ineligible, or not considered, for transplant. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AE) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85%, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3%, respectively.
The CHMP’s positive opinion will be reviewed by the European Commission, which has the authority to grant a label extension for medicines in the European Economic Area. A final decision on the use of bortezomib in MCL is expected early next year. ![]()

The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of bortezomib (Velcade) in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (VR-CAP) to treat adults with previously untreated mantle cell lymphoma (MCL) who are unsuitable for hematopoietic stem cell transplant.
Bortezomib is already approved in the European Union to treat multiple myeloma, either as monotherapy or in combination with other treatment regimens.
The CHMP’s decision to expand the approved use of bortezomib is based on data from the phase 3 LYM-3002 study. Results from this trial were presented at the 2014 ASCO Annual Meeting (abstract 8500).
LYM-3002 included 487 patients newly diagnosed with MCL who were ineligible, or not considered, for transplant. Patients were randomized to receive VR-CAP or R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
The VR-CAP regimen significantly improved progression-free survival (PFS), the primary endpoint, when compared to R-CHOP.
According to an independent review committee, there was a 59% improvement in PFS for the VR-CAP arm compared to the R-CHOP arm, with median PFS times of 24.7 months and 14.4 months, respectively (hazard ratio=0.63; P<0.001).
Study investigators reported a 96% increase in PFS with VR-CAP compared to R-CHOP, with median PFS times of 30.7 months and 16.1 months, respectively (hazard ratio=0.51, P<0.001).
VR-CAP was associated with additional, but manageable, toxicity when compared to R-CHOP. Serious adverse events (AE) were reported in 38% and 30% of patients, respectively. And grade 3 or higher AEs were reported in 93% and 85%, respectively.
Treatment discontinuation due to AEs occurred in 9% of patients in the VR-CAP arm and 7% in the R-CHOP arm. On-treatment, drug-related deaths occurred in 2% and 3%, respectively.
The CHMP’s positive opinion will be reviewed by the European Commission, which has the authority to grant a label extension for medicines in the European Economic Area. A final decision on the use of bortezomib in MCL is expected early next year. ![]()
NICE backs dabigatran for VTE

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has published a final guidance recommending the anticoagulant dabigatran (Pradaxa, Boehringer Ingelheim) as an option for treating and preventing recurrent deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
The guidance says dabigatran can provide a benefit for these patients, with cost- and clinical-effectiveness similar to rivaroxaban and added convenience compared to warfarin.
“For many people, using warfarin can be difficult because of the need for frequent tests to see if the blood is clotting properly, and having to adjust the dose of the
drug if it is not,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The appraisal committee felt that dabigatran represents a potential benefit for many people who have had a DVT or PE, particularly those who have risk factors for recurrence of a blood clot and who therefore need longer-term treatment. We are pleased, therefore, to be able to recommend dabigatran as a cost-effective option for treating DVT and PE and preventing further episodes in adults.”
NICE expects dabigatran to be available on the National Health Service within 3 months.
Cost considerations
Dabigatran costs £65.90 for a 60-capsule pack of the 150 mg or 110 mg doses (excluding tax) and £2.20 per day of treatment, although costs may vary in different settings.
The most plausible incremental cost-effectiveness ratio (ICER) for dabigatran compared with warfarin for acute treatment was uncertain.
However, both Boehringer Ingelheim’s and the evidence review group’s exploratory ICER remained in the range that could be considered a cost-effective use of National Health Service resources. That is, both were under £20,000 per quality-adjusted life-year gained (QALY).
Neither Boehringer Ingelheim nor the evidence review group found any significant difference in efficacy between dabigatran and rivaroxaban for acute treatment of venous thromboembolism (VTE) in their indirect comparisons, and the costs were also very similar between these two treatments.
For combined treatment and secondary prevention of VTE, the appraisal committee said the company’s base case ICER for dabigatran compared with warfarin was likely too low (£9973 per QALY gained).
But the evidence review group’s exploratory base case for dabigatran compared with warfarin may have overestimated the ICER (£35,786 per QALY gained). So the ICER probably lies somewhere between these estimates.
Clinical evidence
To assess the clinical effectiveness of dabigatran, the appraisal committee evaluated data from the RECOVER, RE-MEDY, and RESONATE trials.
In the first RE-COVER trial, dabigatran proved noninferior to warfarin for preventing VTE recurrence, and rates of major bleeding were similar between the treatment arms.
However, patients were more likely to discontinue dabigatran due to adverse events. Results from this trial were presented at ASH 2009 and published in NEJM.
The RE-COVER II trial also suggested that dabigatran was noninferior to warfarin for preventing VTE recurrence and related deaths, and dabigatran was associated with a lower rate of major bleeding.
Rates of death, adverse events, and acute coronary syndromes were similar between the treatment arms. Results from this trial were published in Circulation in 2013.
The RE-MEDY and RE-SONATE trials were designed to evaluate dabigatran as extended VTE prophylaxis. Results of both trials were reported in a single NEJM article published in 2013.
The RE-MEDY trial suggested that dabigatran was noninferior to warfarin as extended prophylaxis for recurrent VTE, and warfarin presented a significantly higher risk of bleeding.
Results of the RE-SONATE trial indicated that dabigatran was superior to placebo for preventing recurrent VTE, although the drug significantly increased the risk of major or clinically relevant bleeding. ![]()

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has published a final guidance recommending the anticoagulant dabigatran (Pradaxa, Boehringer Ingelheim) as an option for treating and preventing recurrent deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
The guidance says dabigatran can provide a benefit for these patients, with cost- and clinical-effectiveness similar to rivaroxaban and added convenience compared to warfarin.
“For many people, using warfarin can be difficult because of the need for frequent tests to see if the blood is clotting properly, and having to adjust the dose of the
drug if it is not,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The appraisal committee felt that dabigatran represents a potential benefit for many people who have had a DVT or PE, particularly those who have risk factors for recurrence of a blood clot and who therefore need longer-term treatment. We are pleased, therefore, to be able to recommend dabigatran as a cost-effective option for treating DVT and PE and preventing further episodes in adults.”
NICE expects dabigatran to be available on the National Health Service within 3 months.
Cost considerations
Dabigatran costs £65.90 for a 60-capsule pack of the 150 mg or 110 mg doses (excluding tax) and £2.20 per day of treatment, although costs may vary in different settings.
The most plausible incremental cost-effectiveness ratio (ICER) for dabigatran compared with warfarin for acute treatment was uncertain.
However, both Boehringer Ingelheim’s and the evidence review group’s exploratory ICER remained in the range that could be considered a cost-effective use of National Health Service resources. That is, both were under £20,000 per quality-adjusted life-year gained (QALY).
Neither Boehringer Ingelheim nor the evidence review group found any significant difference in efficacy between dabigatran and rivaroxaban for acute treatment of venous thromboembolism (VTE) in their indirect comparisons, and the costs were also very similar between these two treatments.
For combined treatment and secondary prevention of VTE, the appraisal committee said the company’s base case ICER for dabigatran compared with warfarin was likely too low (£9973 per QALY gained).
But the evidence review group’s exploratory base case for dabigatran compared with warfarin may have overestimated the ICER (£35,786 per QALY gained). So the ICER probably lies somewhere between these estimates.
Clinical evidence
To assess the clinical effectiveness of dabigatran, the appraisal committee evaluated data from the RECOVER, RE-MEDY, and RESONATE trials.
In the first RE-COVER trial, dabigatran proved noninferior to warfarin for preventing VTE recurrence, and rates of major bleeding were similar between the treatment arms.
However, patients were more likely to discontinue dabigatran due to adverse events. Results from this trial were presented at ASH 2009 and published in NEJM.
The RE-COVER II trial also suggested that dabigatran was noninferior to warfarin for preventing VTE recurrence and related deaths, and dabigatran was associated with a lower rate of major bleeding.
Rates of death, adverse events, and acute coronary syndromes were similar between the treatment arms. Results from this trial were published in Circulation in 2013.
The RE-MEDY and RE-SONATE trials were designed to evaluate dabigatran as extended VTE prophylaxis. Results of both trials were reported in a single NEJM article published in 2013.
The RE-MEDY trial suggested that dabigatran was noninferior to warfarin as extended prophylaxis for recurrent VTE, and warfarin presented a significantly higher risk of bleeding.
Results of the RE-SONATE trial indicated that dabigatran was superior to placebo for preventing recurrent VTE, although the drug significantly increased the risk of major or clinically relevant bleeding. ![]()

Credit: CDC
The UK’s National Institute for Health and Care Excellence (NICE) has published a final guidance recommending the anticoagulant dabigatran (Pradaxa, Boehringer Ingelheim) as an option for treating and preventing recurrent deep vein thrombosis (DVT) and pulmonary embolism (PE) in adults.
The guidance says dabigatran can provide a benefit for these patients, with cost- and clinical-effectiveness similar to rivaroxaban and added convenience compared to warfarin.
“For many people, using warfarin can be difficult because of the need for frequent tests to see if the blood is clotting properly, and having to adjust the dose of the
drug if it is not,” said Carole Longson, NICE Health Technology Evaluation Centre Director.
“The appraisal committee felt that dabigatran represents a potential benefit for many people who have had a DVT or PE, particularly those who have risk factors for recurrence of a blood clot and who therefore need longer-term treatment. We are pleased, therefore, to be able to recommend dabigatran as a cost-effective option for treating DVT and PE and preventing further episodes in adults.”
NICE expects dabigatran to be available on the National Health Service within 3 months.
Cost considerations
Dabigatran costs £65.90 for a 60-capsule pack of the 150 mg or 110 mg doses (excluding tax) and £2.20 per day of treatment, although costs may vary in different settings.
The most plausible incremental cost-effectiveness ratio (ICER) for dabigatran compared with warfarin for acute treatment was uncertain.
However, both Boehringer Ingelheim’s and the evidence review group’s exploratory ICER remained in the range that could be considered a cost-effective use of National Health Service resources. That is, both were under £20,000 per quality-adjusted life-year gained (QALY).
Neither Boehringer Ingelheim nor the evidence review group found any significant difference in efficacy between dabigatran and rivaroxaban for acute treatment of venous thromboembolism (VTE) in their indirect comparisons, and the costs were also very similar between these two treatments.
For combined treatment and secondary prevention of VTE, the appraisal committee said the company’s base case ICER for dabigatran compared with warfarin was likely too low (£9973 per QALY gained).
But the evidence review group’s exploratory base case for dabigatran compared with warfarin may have overestimated the ICER (£35,786 per QALY gained). So the ICER probably lies somewhere between these estimates.
Clinical evidence
To assess the clinical effectiveness of dabigatran, the appraisal committee evaluated data from the RECOVER, RE-MEDY, and RESONATE trials.
In the first RE-COVER trial, dabigatran proved noninferior to warfarin for preventing VTE recurrence, and rates of major bleeding were similar between the treatment arms.
However, patients were more likely to discontinue dabigatran due to adverse events. Results from this trial were presented at ASH 2009 and published in NEJM.
The RE-COVER II trial also suggested that dabigatran was noninferior to warfarin for preventing VTE recurrence and related deaths, and dabigatran was associated with a lower rate of major bleeding.
Rates of death, adverse events, and acute coronary syndromes were similar between the treatment arms. Results from this trial were published in Circulation in 2013.
The RE-MEDY and RE-SONATE trials were designed to evaluate dabigatran as extended VTE prophylaxis. Results of both trials were reported in a single NEJM article published in 2013.
The RE-MEDY trial suggested that dabigatran was noninferior to warfarin as extended prophylaxis for recurrent VTE, and warfarin presented a significantly higher risk of bleeding.
Results of the RE-SONATE trial indicated that dabigatran was superior to placebo for preventing recurrent VTE, although the drug significantly increased the risk of major or clinically relevant bleeding. ![]()
Encapsulating doxorubicin can reduce heart damage

Credit: USDA
VIENNA—Encapsulating the anthracycline doxorubicin in a liposome can reduce the risk of developing heart damage, according to a study presented at EuroEcho-Imaging 2014.
Researchers administered doxorubicin encased in a liposome to a small group of pigs and compared cardiac outcomes to those in pigs that received unmanipulated doxorubicin or epirubicin.
Pigs that received encapsulated doxorubicin still developed cardiotoxicity, but at lower rates than pigs that received traditional doxorubicin.
Pigs that received epirubicin were excluded due to low survival rates.
“[M]any chemotherapies—in particular, anthracyclines—cause cardiac side effects that can lead to cardiomyopathy and severe heart failure,” said study investigator Jutta Bergler-Klein, MD, of the Medical University of Vienna in Austria. “Cardiotoxicity can occur acutely or up to 30 years after chemotherapy and is the second most common cause of death in cancer patients, after secondary malignancy in childhood cancer survivors.”
“Liposomal encapsulation is a new technique which wraps the chemotherapy drug in a fatty cover called a liposome. More of the drug reaches the cancer cells because there is less degradation, and there are fewer side effects on healthy cells because the fat cover acts as a barrier.”
“The drug stays in the bloodstream longer, allowing higher cumulative doses to be given. We tested whether non-pegylated liposome encapsulation of the anthracycline doxorubicin (called Myocet) could decrease its cardiotoxicity compared to conventional doxorubicin or epirubicin, another anthracycline.”
The study included 24 pigs that were randomized to receive the human dose-equivalent of Myocet, conventional doxorubicin, or epirubicin in 3 cycles. The epirubicin group was excluded from the final analyses because of low survival levels.
The researchers assessed cardiac function by echocardiography and MRI at baseline and follow-up (after about 3 months). Laboratory follow-up included hematology, renal function, and measurement of the cardiac enzymes troponin and BNP.
“The dose, imaging methodology, and blood parameters simulate the monitoring that patients on this treatment would receive and produces valuable translational data,” Dr Bergler-Klein said.
The researchers found that the group receiving Myocet had better diastolic and systolic function in the left and right ventricles, compared to conventional doxorubicin. The Myocet group also had less fibrosis in the myocardium, as shown by MRI and histology staining.
“Our study shows that doxorubicin encapsulated in a liposome had fewer cardiac side effects than doxorubicin given in the conventional way,” Dr Bergler-Klein said.
“We did find cardiac toxicity in the Myocet group as well, despite the fact that the pigs were young, healthy, and received anthracyclines for only a short period. This emphasizes how important it is for all cancer patients taking anthracyclines to receive cardiac monitoring using echocardiography and biomarkers, and MRI where indicated.”
“Many patients who recover after chemotherapy have asymptomatic heart damage, which can become symptomatic as they get older. When heart problems are picked up early, patients can be given preventive treatment, including ACE inhibitors, angiotensin receptor blockers, or beta-blockers, to prevent the progression to overt heart failure.”
The researchers are now conducting gene-expression profiling on the histology samples, hoping to explain the better outcome and cardiac function after Myocet therapy. They have found differences in the expression of genes that control energy use and the metabolic state, with better regulation in the Myocet group. ![]()

Credit: USDA
VIENNA—Encapsulating the anthracycline doxorubicin in a liposome can reduce the risk of developing heart damage, according to a study presented at EuroEcho-Imaging 2014.
Researchers administered doxorubicin encased in a liposome to a small group of pigs and compared cardiac outcomes to those in pigs that received unmanipulated doxorubicin or epirubicin.
Pigs that received encapsulated doxorubicin still developed cardiotoxicity, but at lower rates than pigs that received traditional doxorubicin.
Pigs that received epirubicin were excluded due to low survival rates.
“[M]any chemotherapies—in particular, anthracyclines—cause cardiac side effects that can lead to cardiomyopathy and severe heart failure,” said study investigator Jutta Bergler-Klein, MD, of the Medical University of Vienna in Austria. “Cardiotoxicity can occur acutely or up to 30 years after chemotherapy and is the second most common cause of death in cancer patients, after secondary malignancy in childhood cancer survivors.”
“Liposomal encapsulation is a new technique which wraps the chemotherapy drug in a fatty cover called a liposome. More of the drug reaches the cancer cells because there is less degradation, and there are fewer side effects on healthy cells because the fat cover acts as a barrier.”
“The drug stays in the bloodstream longer, allowing higher cumulative doses to be given. We tested whether non-pegylated liposome encapsulation of the anthracycline doxorubicin (called Myocet) could decrease its cardiotoxicity compared to conventional doxorubicin or epirubicin, another anthracycline.”
The study included 24 pigs that were randomized to receive the human dose-equivalent of Myocet, conventional doxorubicin, or epirubicin in 3 cycles. The epirubicin group was excluded from the final analyses because of low survival levels.
The researchers assessed cardiac function by echocardiography and MRI at baseline and follow-up (after about 3 months). Laboratory follow-up included hematology, renal function, and measurement of the cardiac enzymes troponin and BNP.
“The dose, imaging methodology, and blood parameters simulate the monitoring that patients on this treatment would receive and produces valuable translational data,” Dr Bergler-Klein said.
The researchers found that the group receiving Myocet had better diastolic and systolic function in the left and right ventricles, compared to conventional doxorubicin. The Myocet group also had less fibrosis in the myocardium, as shown by MRI and histology staining.
“Our study shows that doxorubicin encapsulated in a liposome had fewer cardiac side effects than doxorubicin given in the conventional way,” Dr Bergler-Klein said.
“We did find cardiac toxicity in the Myocet group as well, despite the fact that the pigs were young, healthy, and received anthracyclines for only a short period. This emphasizes how important it is for all cancer patients taking anthracyclines to receive cardiac monitoring using echocardiography and biomarkers, and MRI where indicated.”
“Many patients who recover after chemotherapy have asymptomatic heart damage, which can become symptomatic as they get older. When heart problems are picked up early, patients can be given preventive treatment, including ACE inhibitors, angiotensin receptor blockers, or beta-blockers, to prevent the progression to overt heart failure.”
The researchers are now conducting gene-expression profiling on the histology samples, hoping to explain the better outcome and cardiac function after Myocet therapy. They have found differences in the expression of genes that control energy use and the metabolic state, with better regulation in the Myocet group. ![]()

Credit: USDA
VIENNA—Encapsulating the anthracycline doxorubicin in a liposome can reduce the risk of developing heart damage, according to a study presented at EuroEcho-Imaging 2014.
Researchers administered doxorubicin encased in a liposome to a small group of pigs and compared cardiac outcomes to those in pigs that received unmanipulated doxorubicin or epirubicin.
Pigs that received encapsulated doxorubicin still developed cardiotoxicity, but at lower rates than pigs that received traditional doxorubicin.
Pigs that received epirubicin were excluded due to low survival rates.
“[M]any chemotherapies—in particular, anthracyclines—cause cardiac side effects that can lead to cardiomyopathy and severe heart failure,” said study investigator Jutta Bergler-Klein, MD, of the Medical University of Vienna in Austria. “Cardiotoxicity can occur acutely or up to 30 years after chemotherapy and is the second most common cause of death in cancer patients, after secondary malignancy in childhood cancer survivors.”
“Liposomal encapsulation is a new technique which wraps the chemotherapy drug in a fatty cover called a liposome. More of the drug reaches the cancer cells because there is less degradation, and there are fewer side effects on healthy cells because the fat cover acts as a barrier.”
“The drug stays in the bloodstream longer, allowing higher cumulative doses to be given. We tested whether non-pegylated liposome encapsulation of the anthracycline doxorubicin (called Myocet) could decrease its cardiotoxicity compared to conventional doxorubicin or epirubicin, another anthracycline.”
The study included 24 pigs that were randomized to receive the human dose-equivalent of Myocet, conventional doxorubicin, or epirubicin in 3 cycles. The epirubicin group was excluded from the final analyses because of low survival levels.
The researchers assessed cardiac function by echocardiography and MRI at baseline and follow-up (after about 3 months). Laboratory follow-up included hematology, renal function, and measurement of the cardiac enzymes troponin and BNP.
“The dose, imaging methodology, and blood parameters simulate the monitoring that patients on this treatment would receive and produces valuable translational data,” Dr Bergler-Klein said.
The researchers found that the group receiving Myocet had better diastolic and systolic function in the left and right ventricles, compared to conventional doxorubicin. The Myocet group also had less fibrosis in the myocardium, as shown by MRI and histology staining.
“Our study shows that doxorubicin encapsulated in a liposome had fewer cardiac side effects than doxorubicin given in the conventional way,” Dr Bergler-Klein said.
“We did find cardiac toxicity in the Myocet group as well, despite the fact that the pigs were young, healthy, and received anthracyclines for only a short period. This emphasizes how important it is for all cancer patients taking anthracyclines to receive cardiac monitoring using echocardiography and biomarkers, and MRI where indicated.”
“Many patients who recover after chemotherapy have asymptomatic heart damage, which can become symptomatic as they get older. When heart problems are picked up early, patients can be given preventive treatment, including ACE inhibitors, angiotensin receptor blockers, or beta-blockers, to prevent the progression to overt heart failure.”
The researchers are now conducting gene-expression profiling on the histology samples, hoping to explain the better outcome and cardiac function after Myocet therapy. They have found differences in the expression of genes that control energy use and the metabolic state, with better regulation in the Myocet group. ![]()
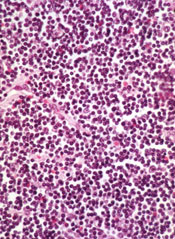
Health Canada approves ibrutinib for CLL
Health Canada recently approved the Bruton tyrosine kinase inhibitor ibrutinib (Imbruvica) for the treatment of chronic lymphocytic leukemia (CLL).
The drug can now be used to treat CLL patients, including those with 17p deletion, who have received at least one prior therapy. It can also be used as frontline treatment in CLL patients with 17p deletion.
Health Canada’s approval of ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib is being developed by Cilag GmbH International (a member of the Janssen Pharmaceutical Companies) and Pharmacyclics, Inc. Janssen will commercialize the drug in Canada, and Janssen affiliates will commercialize it around the world, except in the US, where Pharmacyclics and Janssen Biotech, Inc. co-market it. ![]()
Health Canada recently approved the Bruton tyrosine kinase inhibitor ibrutinib (Imbruvica) for the treatment of chronic lymphocytic leukemia (CLL).
The drug can now be used to treat CLL patients, including those with 17p deletion, who have received at least one prior therapy. It can also be used as frontline treatment in CLL patients with 17p deletion.
Health Canada’s approval of ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib is being developed by Cilag GmbH International (a member of the Janssen Pharmaceutical Companies) and Pharmacyclics, Inc. Janssen will commercialize the drug in Canada, and Janssen affiliates will commercialize it around the world, except in the US, where Pharmacyclics and Janssen Biotech, Inc. co-market it. ![]()
Health Canada recently approved the Bruton tyrosine kinase inhibitor ibrutinib (Imbruvica) for the treatment of chronic lymphocytic leukemia (CLL).
The drug can now be used to treat CLL patients, including those with 17p deletion, who have received at least one prior therapy. It can also be used as frontline treatment in CLL patients with 17p deletion.
Health Canada’s approval of ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib is being developed by Cilag GmbH International (a member of the Janssen Pharmaceutical Companies) and Pharmacyclics, Inc. Janssen will commercialize the drug in Canada, and Janssen affiliates will commercialize it around the world, except in the US, where Pharmacyclics and Janssen Biotech, Inc. co-market it. ![]()
NICE reconsiders obinutuzumab for CLL

Credit: Linda Bartlett
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance that recommends obinutuzumab, marketed by Roche as Gazyvaro, for certain patients with untreated chronic lymphocytic leukemia (CLL).
In an earlier preliminary guidance, NICE said it could not recommend the drug due to uncertainties in the company’s submission.
In response, Roche submitted revised cost-effectiveness analyses and a patient access scheme.
This prompted NICE to recommend obinutuzumab in combination with chlorambucil as an option for adults with untreated CLL who have comorbidities that make them ineligible for full-dose fludarabine-based therapy.
But NICE is only recommending this as an option if bendamustine-based therapy has been deemed unsuitable and if Roche provides obinutuzumab with the discount agreed in the patient access scheme.
“We are pleased that Roche responded to our consultation and provided further analyses to allow us to propose recommending obinutuzumab as a treatment option for untreated chronic lymphocytic leukemia,” said Carole Longson, director of the Centre for Health Technology Evaluation at NICE.
“Half of the people who need treatment for their condition are not able to use the standard first-line treatment of fludarabine combination therapy. NICE recommends alternative treatment with bendamustine, but there are some patients for whom this is also unsuitable. Obinutuzumab is a clinically effective treatment which is associated with fewer adverse events and provides another option to help prevent people’s disease from progressing.”
NICE recommends obinutuzumab on the basis that Roche provides the treatment to the National Health Service (NHS) at a reduced price. The company has agreed with the Department of Health that the size of the discount is to be confidential.
The list price of obinutuzumab is £3312 per 1000 mg vial (excluding value-added tax). According to Roche, a course of treatment costs £26,496 (£9936 for cycle 1 and £3312 for cycles 2 to 6, excluding tax).
Consultees, including the company, healthcare professionals, and members of the public, have until Tuesday, January 6, 2015, to comment on the preliminary recommendations via the NICE website.
NICE has not yet issued the final guidance to the NHS. Until then, NHS bodies should make decisions locally on the funding of specific treatments. ![]()

Credit: Linda Bartlett
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance that recommends obinutuzumab, marketed by Roche as Gazyvaro, for certain patients with untreated chronic lymphocytic leukemia (CLL).
In an earlier preliminary guidance, NICE said it could not recommend the drug due to uncertainties in the company’s submission.
In response, Roche submitted revised cost-effectiveness analyses and a patient access scheme.
This prompted NICE to recommend obinutuzumab in combination with chlorambucil as an option for adults with untreated CLL who have comorbidities that make them ineligible for full-dose fludarabine-based therapy.
But NICE is only recommending this as an option if bendamustine-based therapy has been deemed unsuitable and if Roche provides obinutuzumab with the discount agreed in the patient access scheme.
“We are pleased that Roche responded to our consultation and provided further analyses to allow us to propose recommending obinutuzumab as a treatment option for untreated chronic lymphocytic leukemia,” said Carole Longson, director of the Centre for Health Technology Evaluation at NICE.
“Half of the people who need treatment for their condition are not able to use the standard first-line treatment of fludarabine combination therapy. NICE recommends alternative treatment with bendamustine, but there are some patients for whom this is also unsuitable. Obinutuzumab is a clinically effective treatment which is associated with fewer adverse events and provides another option to help prevent people’s disease from progressing.”
NICE recommends obinutuzumab on the basis that Roche provides the treatment to the National Health Service (NHS) at a reduced price. The company has agreed with the Department of Health that the size of the discount is to be confidential.
The list price of obinutuzumab is £3312 per 1000 mg vial (excluding value-added tax). According to Roche, a course of treatment costs £26,496 (£9936 for cycle 1 and £3312 for cycles 2 to 6, excluding tax).
Consultees, including the company, healthcare professionals, and members of the public, have until Tuesday, January 6, 2015, to comment on the preliminary recommendations via the NICE website.
NICE has not yet issued the final guidance to the NHS. Until then, NHS bodies should make decisions locally on the funding of specific treatments. ![]()

Credit: Linda Bartlett
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance that recommends obinutuzumab, marketed by Roche as Gazyvaro, for certain patients with untreated chronic lymphocytic leukemia (CLL).
In an earlier preliminary guidance, NICE said it could not recommend the drug due to uncertainties in the company’s submission.
In response, Roche submitted revised cost-effectiveness analyses and a patient access scheme.
This prompted NICE to recommend obinutuzumab in combination with chlorambucil as an option for adults with untreated CLL who have comorbidities that make them ineligible for full-dose fludarabine-based therapy.
But NICE is only recommending this as an option if bendamustine-based therapy has been deemed unsuitable and if Roche provides obinutuzumab with the discount agreed in the patient access scheme.
“We are pleased that Roche responded to our consultation and provided further analyses to allow us to propose recommending obinutuzumab as a treatment option for untreated chronic lymphocytic leukemia,” said Carole Longson, director of the Centre for Health Technology Evaluation at NICE.
“Half of the people who need treatment for their condition are not able to use the standard first-line treatment of fludarabine combination therapy. NICE recommends alternative treatment with bendamustine, but there are some patients for whom this is also unsuitable. Obinutuzumab is a clinically effective treatment which is associated with fewer adverse events and provides another option to help prevent people’s disease from progressing.”
NICE recommends obinutuzumab on the basis that Roche provides the treatment to the National Health Service (NHS) at a reduced price. The company has agreed with the Department of Health that the size of the discount is to be confidential.
The list price of obinutuzumab is £3312 per 1000 mg vial (excluding value-added tax). According to Roche, a course of treatment costs £26,496 (£9936 for cycle 1 and £3312 for cycles 2 to 6, excluding tax).
Consultees, including the company, healthcare professionals, and members of the public, have until Tuesday, January 6, 2015, to comment on the preliminary recommendations via the NICE website.
NICE has not yet issued the final guidance to the NHS. Until then, NHS bodies should make decisions locally on the funding of specific treatments.
FDA approves first drug for polycythemia vera

Credit: AFIP
The US Food and Drug Administration (FDA) has expanded the approved use of ruxolitinib (Jakafi) to include treatment of patients with polycythemia vera (PV).
This is the first drug approved by the FDA for this condition.
Ruxolitinib can now be used to treat PV patients who have an inadequate response to hydroxyurea or cannot tolerate the drug.
The FDA said the approval of ruxolitinib for PV patients will help decrease splenomegaly and the need for phlebotomy.
“The approval of Jakafi for polycythemia vera underscores the importance of developing drugs matched to our increasing knowledge of the mechanisms of diseases,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“The trial used to evaluate Jakafi confirmed clinically meaningful reductions in spleen size and the need for phlebotomies to control the disease.”
Results from that study, the phase 3 RESPONSE trial, were presented at the 2014 ASCO Annual Meeting. RESPONSE was funded by Incyte Corporation, the company developing ruxolitinib.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy procedure, and exhibited an enlarged spleen.
They were randomized to receive ruxolitinib at a starting dose of 10 mg twice daily or best available therapy (BAT) as determined by the investigator on a participant-by-participant basis. The ruxolitinib dose was adjusted as needed throughout the study.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT. At week 32, 77% of patients on ruxolitinib and 20% on BAT achieved hematocrit control or spleen reduction.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles.
The FDA reviewed ruxolitinib’s use for PV under the agency’s priority review program because, at the time the application was submitted, the drug demonstrated the potential to be a significant improvement over available therapy. Ruxolitinib also received orphan product designation.
Ruxolitinib is currently approved in more than 60 countries for patients with myelofibrosis (MF). In 2011, the FDA approved the drug to treat patients with intermediate or high-risk MF, including primary MF, post-PV MF, and post-essential thrombocythemia MF.

Credit: AFIP
The US Food and Drug Administration (FDA) has expanded the approved use of ruxolitinib (Jakafi) to include treatment of patients with polycythemia vera (PV).
This is the first drug approved by the FDA for this condition.
Ruxolitinib can now be used to treat PV patients who have an inadequate response to hydroxyurea or cannot tolerate the drug.
The FDA said the approval of ruxolitinib for PV patients will help decrease splenomegaly and the need for phlebotomy.
“The approval of Jakafi for polycythemia vera underscores the importance of developing drugs matched to our increasing knowledge of the mechanisms of diseases,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“The trial used to evaluate Jakafi confirmed clinically meaningful reductions in spleen size and the need for phlebotomies to control the disease.”
Results from that study, the phase 3 RESPONSE trial, were presented at the 2014 ASCO Annual Meeting. RESPONSE was funded by Incyte Corporation, the company developing ruxolitinib.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy procedure, and exhibited an enlarged spleen.
They were randomized to receive ruxolitinib at a starting dose of 10 mg twice daily or best available therapy (BAT) as determined by the investigator on a participant-by-participant basis. The ruxolitinib dose was adjusted as needed throughout the study.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT. At week 32, 77% of patients on ruxolitinib and 20% on BAT achieved hematocrit control or spleen reduction.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles.
The FDA reviewed ruxolitinib’s use for PV under the agency’s priority review program because, at the time the application was submitted, the drug demonstrated the potential to be a significant improvement over available therapy. Ruxolitinib also received orphan product designation.
Ruxolitinib is currently approved in more than 60 countries for patients with myelofibrosis (MF). In 2011, the FDA approved the drug to treat patients with intermediate or high-risk MF, including primary MF, post-PV MF, and post-essential thrombocythemia MF.

Credit: AFIP
The US Food and Drug Administration (FDA) has expanded the approved use of ruxolitinib (Jakafi) to include treatment of patients with polycythemia vera (PV).
This is the first drug approved by the FDA for this condition.
Ruxolitinib can now be used to treat PV patients who have an inadequate response to hydroxyurea or cannot tolerate the drug.
The FDA said the approval of ruxolitinib for PV patients will help decrease splenomegaly and the need for phlebotomy.
“The approval of Jakafi for polycythemia vera underscores the importance of developing drugs matched to our increasing knowledge of the mechanisms of diseases,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“The trial used to evaluate Jakafi confirmed clinically meaningful reductions in spleen size and the need for phlebotomies to control the disease.”
Results from that study, the phase 3 RESPONSE trial, were presented at the 2014 ASCO Annual Meeting. RESPONSE was funded by Incyte Corporation, the company developing ruxolitinib.
The trial included 222 patients who had PV for at least 24 weeks. All patients had an inadequate response to or could not tolerate hydroxyurea, had undergone a phlebotomy procedure, and exhibited an enlarged spleen.
They were randomized to receive ruxolitinib at a starting dose of 10 mg twice daily or best available therapy (BAT) as determined by the investigator on a participant-by-participant basis. The ruxolitinib dose was adjusted as needed throughout the study.
The study was designed to measure the reduced need for phlebotomy beginning at week 8 and continuing through week 32, in addition to at least a 35% reduction in spleen volume at week 32.
Twenty-one percent of ruxolitinib-treated patients met this endpoint, compared to 1% of patients who received BAT. At week 32, 77% of patients on ruxolitinib and 20% on BAT achieved hematocrit control or spleen reduction.
Ruxolitinib was generally well-tolerated, but 3.6% of patients discontinued treatment due to adverse events, compared to 1.8% of patients on BAT.
The most common events associated with ruxolitinib were anemia and thrombocytopenia. The most common non-hematologic events were headache, diarrhea, fatigue, dizziness, constipation, and shingles.
The FDA reviewed ruxolitinib’s use for PV under the agency’s priority review program because, at the time the application was submitted, the drug demonstrated the potential to be a significant improvement over available therapy. Ruxolitinib also received orphan product designation.
Ruxolitinib is currently approved in more than 60 countries for patients with myelofibrosis (MF). In 2011, the FDA approved the drug to treat patients with intermediate or high-risk MF, including primary MF, post-PV MF, and post-essential thrombocythemia MF.
FDA approves first anti-CD19 drug

Credit: NIAID
The US Food and Drug Administration (FDA) has granted accelerated approval for blinatumomab (Blincyto) to treat adults with relapsed or refractory Philadelphia chromosome-negative precursor B-cell acute lymphoblastic leukemia (ALL).
Blinatumomab is a bispecific T-cell engager (BiTE®) antibody construct designed to direct the body’s T cells against target cells expressing CD19, a protein found on the surface of B cells.
Blinatumomab is the first anti-CD19 drug to receive FDA approval. It will be available as a 35 mcg single-use vial.
“Immunotherapies, especially Blincyto with its unique mechanism of action, are particularly promising for patients with leukemia,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“Recognizing the potential of this novel therapy, the FDA worked proactively with the sponsor under our breakthrough therapy designation program to facilitate the approval of this novel agent.”
Approval details
The FDA granted blinatumomab accelerated approval based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Before granting the drug full approval, the FDA is requiring that blinatumomab’s manufacturer, Amgen, conduct a study to verify that the drug improves survival in patients with relapsed or refractory Philadelphia-negative precursor B-cell ALL.
Blinatumomab was approved with a boxed warning detailing the risk of cytokine release syndrome and neurological toxicities. The FDA also approved the drug with a Risk Evaluation and Mitigation Strategy, which consists of a communication plan to inform healthcare providers about the serious risks and the potential for preparation and administration errors.
Blinatumomab was approved more than 5 months ahead of the date the FDA was scheduled to complete review of the drug’s application (May 19, 2015).
The agency had granted blinatumomab breakthrough therapy designation, priority review, and orphan product designation because Amgen demonstrated through preliminary clinical evidence that the drug may offer a substantial improvement over available therapies.
That evidence came in the form of a phase 2 study, the results of which were presented at the 19th Congress of the European Hematology Association (EHA) in June.
Trial results
Researchers evaluated blinatumomab monotherapy in 189 patients with relapsed or refractory B-cell ALL and a median age of 39 (range, 18-79). The patients received blinatumomab by continuous intravenous infusion—4 weeks on and 2 weeks off—for up to 5 cycles.
Thirty-three percent of patients achieved a complete remission, and 9% achieved a complete remission with partial hematologic recovery. Seventy-one percent of these patients were negative for minimal residual disease.
The median relapse-free survival was 5.9 months.
Major toxicities were related to cytokine release syndrome, but cytopenias and central nervous system events were also common. The most frequent adverse events were pyrexia (59%), headache (35%), and febrile neutropenia (29%).
The most frequent grade 3 or higher adverse events were febrile neutropenia (26%), anemia (15%), and neutropenia (15%). Two percent of patients had grade 3 or higher cytokine release syndrome.
The most common grade 3 or higher nervous system events were headache (4%), encephalopathy (3%), and ataxia (2%). Three patients (2%) had grade 5 events considered treatment-related—2 with sepsis and 1 with Candida infection. ![]()

Credit: NIAID
The US Food and Drug Administration (FDA) has granted accelerated approval for blinatumomab (Blincyto) to treat adults with relapsed or refractory Philadelphia chromosome-negative precursor B-cell acute lymphoblastic leukemia (ALL).
Blinatumomab is a bispecific T-cell engager (BiTE®) antibody construct designed to direct the body’s T cells against target cells expressing CD19, a protein found on the surface of B cells.
Blinatumomab is the first anti-CD19 drug to receive FDA approval. It will be available as a 35 mcg single-use vial.
“Immunotherapies, especially Blincyto with its unique mechanism of action, are particularly promising for patients with leukemia,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“Recognizing the potential of this novel therapy, the FDA worked proactively with the sponsor under our breakthrough therapy designation program to facilitate the approval of this novel agent.”
Approval details
The FDA granted blinatumomab accelerated approval based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Before granting the drug full approval, the FDA is requiring that blinatumomab’s manufacturer, Amgen, conduct a study to verify that the drug improves survival in patients with relapsed or refractory Philadelphia-negative precursor B-cell ALL.
Blinatumomab was approved with a boxed warning detailing the risk of cytokine release syndrome and neurological toxicities. The FDA also approved the drug with a Risk Evaluation and Mitigation Strategy, which consists of a communication plan to inform healthcare providers about the serious risks and the potential for preparation and administration errors.
Blinatumomab was approved more than 5 months ahead of the date the FDA was scheduled to complete review of the drug’s application (May 19, 2015).
The agency had granted blinatumomab breakthrough therapy designation, priority review, and orphan product designation because Amgen demonstrated through preliminary clinical evidence that the drug may offer a substantial improvement over available therapies.
That evidence came in the form of a phase 2 study, the results of which were presented at the 19th Congress of the European Hematology Association (EHA) in June.
Trial results
Researchers evaluated blinatumomab monotherapy in 189 patients with relapsed or refractory B-cell ALL and a median age of 39 (range, 18-79). The patients received blinatumomab by continuous intravenous infusion—4 weeks on and 2 weeks off—for up to 5 cycles.
Thirty-three percent of patients achieved a complete remission, and 9% achieved a complete remission with partial hematologic recovery. Seventy-one percent of these patients were negative for minimal residual disease.
The median relapse-free survival was 5.9 months.
Major toxicities were related to cytokine release syndrome, but cytopenias and central nervous system events were also common. The most frequent adverse events were pyrexia (59%), headache (35%), and febrile neutropenia (29%).
The most frequent grade 3 or higher adverse events were febrile neutropenia (26%), anemia (15%), and neutropenia (15%). Two percent of patients had grade 3 or higher cytokine release syndrome.
The most common grade 3 or higher nervous system events were headache (4%), encephalopathy (3%), and ataxia (2%). Three patients (2%) had grade 5 events considered treatment-related—2 with sepsis and 1 with Candida infection. ![]()

Credit: NIAID
The US Food and Drug Administration (FDA) has granted accelerated approval for blinatumomab (Blincyto) to treat adults with relapsed or refractory Philadelphia chromosome-negative precursor B-cell acute lymphoblastic leukemia (ALL).
Blinatumomab is a bispecific T-cell engager (BiTE®) antibody construct designed to direct the body’s T cells against target cells expressing CD19, a protein found on the surface of B cells.
Blinatumomab is the first anti-CD19 drug to receive FDA approval. It will be available as a 35 mcg single-use vial.
“Immunotherapies, especially Blincyto with its unique mechanism of action, are particularly promising for patients with leukemia,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“Recognizing the potential of this novel therapy, the FDA worked proactively with the sponsor under our breakthrough therapy designation program to facilitate the approval of this novel agent.”
Approval details
The FDA granted blinatumomab accelerated approval based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Before granting the drug full approval, the FDA is requiring that blinatumomab’s manufacturer, Amgen, conduct a study to verify that the drug improves survival in patients with relapsed or refractory Philadelphia-negative precursor B-cell ALL.
Blinatumomab was approved with a boxed warning detailing the risk of cytokine release syndrome and neurological toxicities. The FDA also approved the drug with a Risk Evaluation and Mitigation Strategy, which consists of a communication plan to inform healthcare providers about the serious risks and the potential for preparation and administration errors.
Blinatumomab was approved more than 5 months ahead of the date the FDA was scheduled to complete review of the drug’s application (May 19, 2015).
The agency had granted blinatumomab breakthrough therapy designation, priority review, and orphan product designation because Amgen demonstrated through preliminary clinical evidence that the drug may offer a substantial improvement over available therapies.
That evidence came in the form of a phase 2 study, the results of which were presented at the 19th Congress of the European Hematology Association (EHA) in June.
Trial results
Researchers evaluated blinatumomab monotherapy in 189 patients with relapsed or refractory B-cell ALL and a median age of 39 (range, 18-79). The patients received blinatumomab by continuous intravenous infusion—4 weeks on and 2 weeks off—for up to 5 cycles.
Thirty-three percent of patients achieved a complete remission, and 9% achieved a complete remission with partial hematologic recovery. Seventy-one percent of these patients were negative for minimal residual disease.
The median relapse-free survival was 5.9 months.
Major toxicities were related to cytokine release syndrome, but cytopenias and central nervous system events were also common. The most frequent adverse events were pyrexia (59%), headache (35%), and febrile neutropenia (29%).
The most frequent grade 3 or higher adverse events were febrile neutropenia (26%), anemia (15%), and neutropenia (15%). Two percent of patients had grade 3 or higher cytokine release syndrome.
The most common grade 3 or higher nervous system events were headache (4%), encephalopathy (3%), and ataxia (2%). Three patients (2%) had grade 5 events considered treatment-related—2 with sepsis and 1 with Candida infection. ![]()