User login
Loss of Independence after Surgery and Subsequent Outcomes in Older Patients
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
Clinical Question: What is the incidence of loss of independence (LOI) for older adults after surgery, and is there an association between LOI and readmission or death?
Background: LOI is being increasingly recognized as an important measure of patient-centered care and a potential opportunity for intervention to prevent disablement. This study is the first to examine links between LOI and rates of readmission or death following surgery.
Study Design: Retrospective cohort.
Setting: 26 U.S. hospitals participating in a national quality improvement project.
Synopsis: The authors examined data from 5,077 patients age 65 or older undergoing an inpatient surgical procedure. They examined ability to perform activities of daily living (ADLs), mobility, and living situation before and after surgery, and they defined LOI as a change in one or more of these factors at the time of discharge.
They found that LOI increased with age, with 49.9% of patients ages 65–74, 67.3% of patients ages 75–84, and 83.9% of patients age 85 or older experiencing LOI. The study also showed an association between LOI and negative outcomes, including readmission (odds ratio, 1.7) and death after discharge (odds ratio, 6.7).
Although this study was retrospective, the findings indicate that LOI is strongly correlated with negative short-term outcomes, especially in older populations. LOI related to surgery is a measure that deserves closer attention and greater future study as a potential target for clinical initiatives and intervention.
Bottom Line: LOI (functional ability, mobility, and living situation) after surgery increases with age and is associated with negative short-term outcomes including readmission and death.
Citation: Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016;151(9):e161689.
Short Take
Transition to New Electronic Health Records Systems Does Not Increase Adverse Outcomes
An observational study comparing 17 hospitals implementing new electronic health records systems with 399 control hospitals showed no difference in the rate of adverse safety events or readmissions following implementation.
Citation: Barnett ML, Mehrotra A, Jena AB. Adverse inpatient outcomes during the transition to a new electronic health record system: observational study. BMJ. 2016;354:i3835.
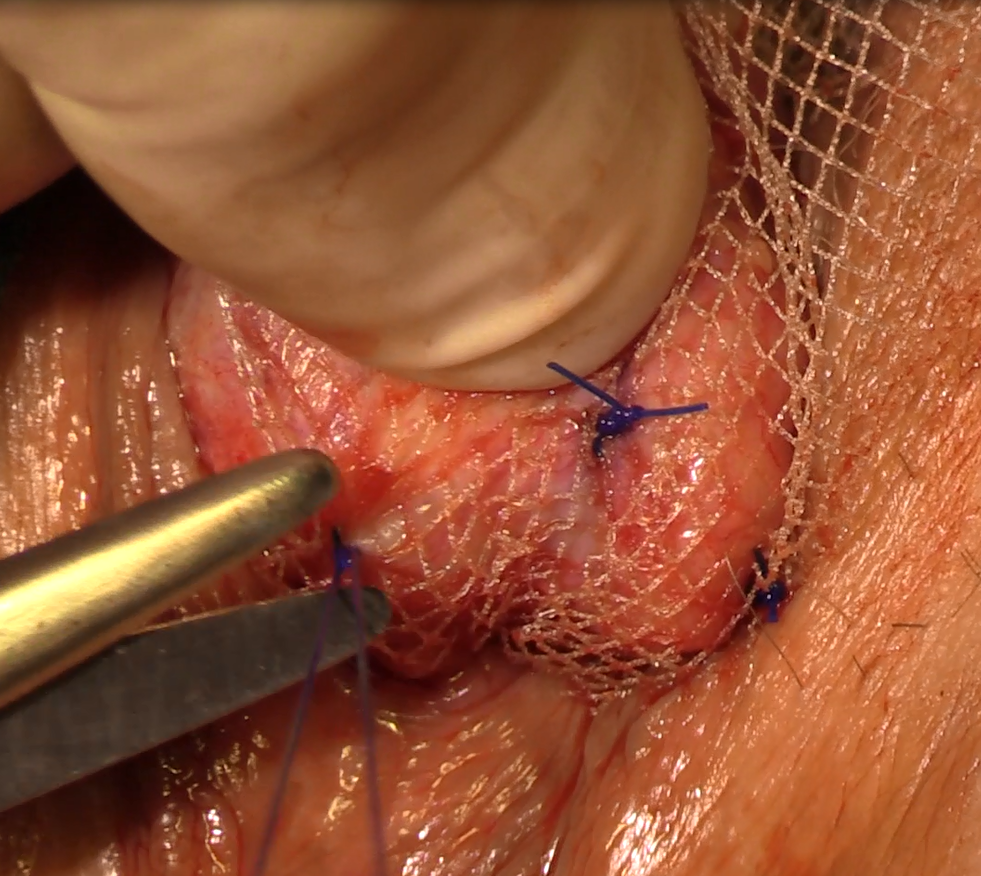
Natural orifice sacral colpopexy
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Alternative options for visualizing ureteral patency during intraoperative cystoscopy
- Use of suprapubic Carter-Thomason needle to assist in cystoscopic excision of an intravesical foreign object
- Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
This video brought to you by 
Letters to the Editor: Risk-reducing surgery for BRCA mutation carriers
“SHOULD RISK-REDUCING GYNECOLOGIC SURGERY FOR BRCA MUTATION CARRIERS INCLUDE HYSTERECTOMY?”
ANDREW M. KAUNITZ, MD (WEB EXCLUSIVE, AUGUST 28, 2016)
Hysterectomy warranted?
I am wondering if Dr. Kaunitz really is recommending performing 270 hysterectomies to prevent one endometrial cancer? Is this justified given the risks from the hysterectomy itself, the economics of the disease, or any significant reductions in endometrial cancer mortality?
David O. Holtz, MD
Paoli, Pennsylvania
Dr. Kaunitz responds
I appreciate Dr. Holtz’s interest in my commentary on the role of hysterectomy as part of risk-reducing surgery in BRCA mutation carriers. Women who are mutation carriers are at increased risk for serous or serous-like endometrial cancers. Further, hysterectomy offers specific advantages for young mutation carriers for whom menopausal hormone therapy is often indicated after risk-reducing salpingo-oophorectomy. Accordingly, I would indeed encourage such women to consider hysterectomy as part of risk-reducing gynecologic surgery if such surgery can be accomplished via minimally invasive techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
“SHOULD RISK-REDUCING GYNECOLOGIC SURGERY FOR BRCA MUTATION CARRIERS INCLUDE HYSTERECTOMY?”
ANDREW M. KAUNITZ, MD (WEB EXCLUSIVE, AUGUST 28, 2016)
Hysterectomy warranted?
I am wondering if Dr. Kaunitz really is recommending performing 270 hysterectomies to prevent one endometrial cancer? Is this justified given the risks from the hysterectomy itself, the economics of the disease, or any significant reductions in endometrial cancer mortality?
David O. Holtz, MD
Paoli, Pennsylvania
Dr. Kaunitz responds
I appreciate Dr. Holtz’s interest in my commentary on the role of hysterectomy as part of risk-reducing surgery in BRCA mutation carriers. Women who are mutation carriers are at increased risk for serous or serous-like endometrial cancers. Further, hysterectomy offers specific advantages for young mutation carriers for whom menopausal hormone therapy is often indicated after risk-reducing salpingo-oophorectomy. Accordingly, I would indeed encourage such women to consider hysterectomy as part of risk-reducing gynecologic surgery if such surgery can be accomplished via minimally invasive techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
“SHOULD RISK-REDUCING GYNECOLOGIC SURGERY FOR BRCA MUTATION CARRIERS INCLUDE HYSTERECTOMY?”
ANDREW M. KAUNITZ, MD (WEB EXCLUSIVE, AUGUST 28, 2016)
Hysterectomy warranted?
I am wondering if Dr. Kaunitz really is recommending performing 270 hysterectomies to prevent one endometrial cancer? Is this justified given the risks from the hysterectomy itself, the economics of the disease, or any significant reductions in endometrial cancer mortality?
David O. Holtz, MD
Paoli, Pennsylvania
Dr. Kaunitz responds
I appreciate Dr. Holtz’s interest in my commentary on the role of hysterectomy as part of risk-reducing surgery in BRCA mutation carriers. Women who are mutation carriers are at increased risk for serous or serous-like endometrial cancers. Further, hysterectomy offers specific advantages for young mutation carriers for whom menopausal hormone therapy is often indicated after risk-reducing salpingo-oophorectomy. Accordingly, I would indeed encourage such women to consider hysterectomy as part of risk-reducing gynecologic surgery if such surgery can be accomplished via minimally invasive techniques.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Newborns with CHD have reduced cerebral oxygen delivery
Using a newer form of MRI to investigate oxygen levels in newborns with congenital heart disease, researchers in Canada reported that these patients may have impaired brain growth and development in the first weeks of life because of significantly lower cerebral oxygen delivery levels.
These findings suggest that oxygen delivery may impact brain growth, particularly in newborns with single-ventricle physiology, reported Jessie Mei Lim, BSc, of the University of Toronto, and her colleagues from McGill University, Montreal, and the Hospital for Sick Children, Toronto. The findings were published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1095-103). Ms. Lim and her colleagues used cine phase-contrast (PC) MRI to measure cerebral blood flow in newborns with congenital heard disease (CHD). Previous studies used optical measures of tissue oxygenation and MRI arterial spin labeling to suggests that newborns with severe CHD have impaired CBF and cerebral oxygen delivery (CDO2) and CBF.
This single-center study involved 63 newborns from June 2013 to April 2015 at the Hospital for Sick Children. These subjects received an MRI of the head before surgery at an average of age 7.5 days. The scans were done without sedation or contrast while the infants were asleep. The study compared 31 age-matched controls with 32 subjects with various forms of CHD – 12 were managed surgically along a single-ventricle pathway (SVP), 4 had coarctation of the aorta, 13 had transposition of the great arteries (TGA), and 3 had other forms of CHD.
The researchers validated their method by reporting similarities between flows in the basilar and vertebral arteries in 14 controls, “suggesting good consistency and accuracy of our method for measuring CBF,” Ms. Lim and her coauthors noted. A comparison of CBF measured with an unpaired Student t test revealed no significant differences between the CHD group and controls. The average net CBF in CHD patients was 103.5 mL/min vs. 119.7 mL/min in controls.
However, when evaluating CDO2 using a Student t test, the researchers found significantly lower levels in the CHD group – an average of 1,1881 mLO2/min. vs. 2,712 mL O2/min in controls (P less than .0001). And when the researchers indexed CDO2 to brain volume yielding indexed oxygen delivery, the difference between the two groups was still significant: an average of 523.1 mL O2/min-1 .100 g-1 in the CHD group and 685.6 mL O2/min-1.100 g-1 in controls (P = .0006).
Among the CHD group, those with SVP and TGA had significantly lower CDO2 than that of controls. Brain volumes were also lower in those with CHD (mean of 338.5 mL vs. 377.7 mL in controls, P = .002).
The MRI findings were telling in the study population, Ms. Lim and her coauthors said. Five subjects in the CHD group had a combination of diffuse excessive high-signal intensity (DEHSI) and white-matter injury (WMI), 10 had an isolated finding of DEHSI, two had WMI alone and five others had other minor brain abnormalities. But the control group had no abnormal findings on conventional brain MRI.
The researchers acknowledged that, while the impact of reduced cerebral oxygen delivery is unknown, “theoretical reasons for thinking it might adversely impact ongoing brain growth and development during this period of rapid brain growth are considered.”
Cardiovascular surgeons should consider these findings when deciding on when to operate on newborns with CHD, the researchers said. “Further support for the concept that such a mechanism could lead to irreversible deficits in brain growth and development might result in attempts to expedite surgical repair of congenital cardiac lesions, which have conventionally not been addressed in the neonatal period,” they wrote.
Ms. Lim and her coauthors had no financial relationships to disclose.
Congenital heart disease (CHD) is heterogeneous and different types of lesions may cause different hemodynamics, Caitlin K. Rollins, MD, of Boston Children’s Hospital and Harvard Medical School said in her invited commentary (J Thorac Cardiovasc Surg. 2016;152-960-1).
Ms. Lim and her colleagues in this study confirmed that premise with their finding that newborns with CHD and controls had similar cerebral blood flow, but that those with CHD had reduced oxygen delivery. “These differences were most apparent in the neonates with single-ventricle physiology and transposition of the great arteries,” Dr. Rollins said. The study authors’ finding of an association between reduced oxygen delivery and impaired brain development, along with this group’s previous reports (Circulation 2015;131:1313-23) suggesting preserved cerebral blood flow in the late prenatal period, differ from other studies using traditional methods to show reduced cerebral blood flow in obstructive left-sided lesions, Dr. Rollins said. “Although technical differences may in part account for the discrepancy, the contrasting results also reflect that the relative contributions of abnormal cerebral blood flow and oxygenation differ among forms of CHD,” Dr. Rollins said.
Congenital heart disease (CHD) is heterogeneous and different types of lesions may cause different hemodynamics, Caitlin K. Rollins, MD, of Boston Children’s Hospital and Harvard Medical School said in her invited commentary (J Thorac Cardiovasc Surg. 2016;152-960-1).
Ms. Lim and her colleagues in this study confirmed that premise with their finding that newborns with CHD and controls had similar cerebral blood flow, but that those with CHD had reduced oxygen delivery. “These differences were most apparent in the neonates with single-ventricle physiology and transposition of the great arteries,” Dr. Rollins said. The study authors’ finding of an association between reduced oxygen delivery and impaired brain development, along with this group’s previous reports (Circulation 2015;131:1313-23) suggesting preserved cerebral blood flow in the late prenatal period, differ from other studies using traditional methods to show reduced cerebral blood flow in obstructive left-sided lesions, Dr. Rollins said. “Although technical differences may in part account for the discrepancy, the contrasting results also reflect that the relative contributions of abnormal cerebral blood flow and oxygenation differ among forms of CHD,” Dr. Rollins said.
Congenital heart disease (CHD) is heterogeneous and different types of lesions may cause different hemodynamics, Caitlin K. Rollins, MD, of Boston Children’s Hospital and Harvard Medical School said in her invited commentary (J Thorac Cardiovasc Surg. 2016;152-960-1).
Ms. Lim and her colleagues in this study confirmed that premise with their finding that newborns with CHD and controls had similar cerebral blood flow, but that those with CHD had reduced oxygen delivery. “These differences were most apparent in the neonates with single-ventricle physiology and transposition of the great arteries,” Dr. Rollins said. The study authors’ finding of an association between reduced oxygen delivery and impaired brain development, along with this group’s previous reports (Circulation 2015;131:1313-23) suggesting preserved cerebral blood flow in the late prenatal period, differ from other studies using traditional methods to show reduced cerebral blood flow in obstructive left-sided lesions, Dr. Rollins said. “Although technical differences may in part account for the discrepancy, the contrasting results also reflect that the relative contributions of abnormal cerebral blood flow and oxygenation differ among forms of CHD,” Dr. Rollins said.
Using a newer form of MRI to investigate oxygen levels in newborns with congenital heart disease, researchers in Canada reported that these patients may have impaired brain growth and development in the first weeks of life because of significantly lower cerebral oxygen delivery levels.
These findings suggest that oxygen delivery may impact brain growth, particularly in newborns with single-ventricle physiology, reported Jessie Mei Lim, BSc, of the University of Toronto, and her colleagues from McGill University, Montreal, and the Hospital for Sick Children, Toronto. The findings were published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1095-103). Ms. Lim and her colleagues used cine phase-contrast (PC) MRI to measure cerebral blood flow in newborns with congenital heard disease (CHD). Previous studies used optical measures of tissue oxygenation and MRI arterial spin labeling to suggests that newborns with severe CHD have impaired CBF and cerebral oxygen delivery (CDO2) and CBF.
This single-center study involved 63 newborns from June 2013 to April 2015 at the Hospital for Sick Children. These subjects received an MRI of the head before surgery at an average of age 7.5 days. The scans were done without sedation or contrast while the infants were asleep. The study compared 31 age-matched controls with 32 subjects with various forms of CHD – 12 were managed surgically along a single-ventricle pathway (SVP), 4 had coarctation of the aorta, 13 had transposition of the great arteries (TGA), and 3 had other forms of CHD.
The researchers validated their method by reporting similarities between flows in the basilar and vertebral arteries in 14 controls, “suggesting good consistency and accuracy of our method for measuring CBF,” Ms. Lim and her coauthors noted. A comparison of CBF measured with an unpaired Student t test revealed no significant differences between the CHD group and controls. The average net CBF in CHD patients was 103.5 mL/min vs. 119.7 mL/min in controls.
However, when evaluating CDO2 using a Student t test, the researchers found significantly lower levels in the CHD group – an average of 1,1881 mLO2/min. vs. 2,712 mL O2/min in controls (P less than .0001). And when the researchers indexed CDO2 to brain volume yielding indexed oxygen delivery, the difference between the two groups was still significant: an average of 523.1 mL O2/min-1 .100 g-1 in the CHD group and 685.6 mL O2/min-1.100 g-1 in controls (P = .0006).
Among the CHD group, those with SVP and TGA had significantly lower CDO2 than that of controls. Brain volumes were also lower in those with CHD (mean of 338.5 mL vs. 377.7 mL in controls, P = .002).
The MRI findings were telling in the study population, Ms. Lim and her coauthors said. Five subjects in the CHD group had a combination of diffuse excessive high-signal intensity (DEHSI) and white-matter injury (WMI), 10 had an isolated finding of DEHSI, two had WMI alone and five others had other minor brain abnormalities. But the control group had no abnormal findings on conventional brain MRI.
The researchers acknowledged that, while the impact of reduced cerebral oxygen delivery is unknown, “theoretical reasons for thinking it might adversely impact ongoing brain growth and development during this period of rapid brain growth are considered.”
Cardiovascular surgeons should consider these findings when deciding on when to operate on newborns with CHD, the researchers said. “Further support for the concept that such a mechanism could lead to irreversible deficits in brain growth and development might result in attempts to expedite surgical repair of congenital cardiac lesions, which have conventionally not been addressed in the neonatal period,” they wrote.
Ms. Lim and her coauthors had no financial relationships to disclose.
Using a newer form of MRI to investigate oxygen levels in newborns with congenital heart disease, researchers in Canada reported that these patients may have impaired brain growth and development in the first weeks of life because of significantly lower cerebral oxygen delivery levels.
These findings suggest that oxygen delivery may impact brain growth, particularly in newborns with single-ventricle physiology, reported Jessie Mei Lim, BSc, of the University of Toronto, and her colleagues from McGill University, Montreal, and the Hospital for Sick Children, Toronto. The findings were published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1095-103). Ms. Lim and her colleagues used cine phase-contrast (PC) MRI to measure cerebral blood flow in newborns with congenital heard disease (CHD). Previous studies used optical measures of tissue oxygenation and MRI arterial spin labeling to suggests that newborns with severe CHD have impaired CBF and cerebral oxygen delivery (CDO2) and CBF.
This single-center study involved 63 newborns from June 2013 to April 2015 at the Hospital for Sick Children. These subjects received an MRI of the head before surgery at an average of age 7.5 days. The scans were done without sedation or contrast while the infants were asleep. The study compared 31 age-matched controls with 32 subjects with various forms of CHD – 12 were managed surgically along a single-ventricle pathway (SVP), 4 had coarctation of the aorta, 13 had transposition of the great arteries (TGA), and 3 had other forms of CHD.
The researchers validated their method by reporting similarities between flows in the basilar and vertebral arteries in 14 controls, “suggesting good consistency and accuracy of our method for measuring CBF,” Ms. Lim and her coauthors noted. A comparison of CBF measured with an unpaired Student t test revealed no significant differences between the CHD group and controls. The average net CBF in CHD patients was 103.5 mL/min vs. 119.7 mL/min in controls.
However, when evaluating CDO2 using a Student t test, the researchers found significantly lower levels in the CHD group – an average of 1,1881 mLO2/min. vs. 2,712 mL O2/min in controls (P less than .0001). And when the researchers indexed CDO2 to brain volume yielding indexed oxygen delivery, the difference between the two groups was still significant: an average of 523.1 mL O2/min-1 .100 g-1 in the CHD group and 685.6 mL O2/min-1.100 g-1 in controls (P = .0006).
Among the CHD group, those with SVP and TGA had significantly lower CDO2 than that of controls. Brain volumes were also lower in those with CHD (mean of 338.5 mL vs. 377.7 mL in controls, P = .002).
The MRI findings were telling in the study population, Ms. Lim and her coauthors said. Five subjects in the CHD group had a combination of diffuse excessive high-signal intensity (DEHSI) and white-matter injury (WMI), 10 had an isolated finding of DEHSI, two had WMI alone and five others had other minor brain abnormalities. But the control group had no abnormal findings on conventional brain MRI.
The researchers acknowledged that, while the impact of reduced cerebral oxygen delivery is unknown, “theoretical reasons for thinking it might adversely impact ongoing brain growth and development during this period of rapid brain growth are considered.”
Cardiovascular surgeons should consider these findings when deciding on when to operate on newborns with CHD, the researchers said. “Further support for the concept that such a mechanism could lead to irreversible deficits in brain growth and development might result in attempts to expedite surgical repair of congenital cardiac lesions, which have conventionally not been addressed in the neonatal period,” they wrote.
Ms. Lim and her coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Cerebral blood flow is maintained but cerebral oxygen delivery is decreased in preoperative newborns with cyanotic congenital heart disease (CHD).
Major finding: Average cerebral oxygen delivery measured 1,1881 mLO2/min in the CHD group when measured with Student t testing vs. 2,712 mLO2/min in controls (P less than .0001).
Data source: Single-center study of 32 neonates with various forms of CHD 31 age-matched controls.
Disclosures: Ms. Lim and coauthors have no financial relationships to disclose.
VIDEO: The surgical treatment of pelvic congestion
BY CHARLES E. MILLER, MD
Chronic pelvic pain is described as the presence of lower abdominal or pelvic pain for longer than 6 months. It is believed to affect approximately one in six women and 12%-15% of women of reproductive age. The diagnosis and treatment of chronic pelvic pain adds as much as a $2 billion burden to our health system annually.
It was first described clinically in the literature in 1857, while the existence of pelvic varicosities wasn’t documented for nearly another 100 years. Pelvic congestion syndrome (PCS) accounts for 30%-70% of cases presenting with chronic pelvic pain. PCS can be due to pelvic venous insufficiency, characterized by reflux into pelvic veins leading to pelvic varicosities or alternative venous pathways secondary to varicose veins of the leg.
Other etiologies of PCS include nutcracker syndrome (left renal vein compressed between the aorta and the superior mesenteric artery), May-Thurner syndrome (compression of the left common iliac vein by the right common iliac artery) or, less likely, tumor thrombosis of the inferior vena cava, portal vein thrombosis, renal cell carcinoma, left renal thrombosis, or left kidney arterial-venous fistula.
While there appears to be significant literature indicating a long-term success rate of greater than 80% in patients treated by percutaneous endovascular procedures (embolization, stenting), there is far less information on the postsurgical success of blocking the varicose gonadal vein. Nevertheless, our long-term results with gonadal vein clipping is virtually the same as that of our radiological colleagues.
It is a pleasure to welcome Courtney Steller, DO, to this edition of the Master Class in Gynecologic Surgery to discuss the diagnosis and treatment of PCS, with an emphasis on surgical correction.
Dr. Steller is a recent graduate of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. She is currently in private practice and is an associate at the Family Health Centers of San Diego, Calif.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at obnews@frontlinemedcom.com.
Pelvic congestion syndrome: A treatable cause of pain
BY COURTNEY STELLER, DO
Pelvic congestion syndrome is a poorly understood and underdiagnosed disease. Yet, over the last decade, the syndrome has become less controversial as the etiology has become better understood and as the diagnostic approach has become more specific. Through these advances, treatments have also become increasingly more successful.
This is an important shift, because the chronic pelvic pain experienced by patients with pelvic congestion significantly impacts their quality of life and well-being. As the pain persists, it can become exceedingly difficult to manage. Many patients we have ultimately treated for pelvic congestion syndrome have had years of various work-ups, significant diagnostic investigations, and trials of different treatments without having any cause of their pain identified or achieving any lasting symptom relief.
The pelvic pain in patients with pelvic congestion syndrome (PCS) can be noncyclical or cyclical. It is present most of the time but tends to get worse at the end of the day and after long periods of standing and/or sitting. The pain also may worsen with intercourse, largely afterward. The syndrome tends to occur in premenopausal and multiparous women, but it’s important to appreciate that this is not always the case; we have diagnosed and treated PCS in several young, nulliparous patients as well.
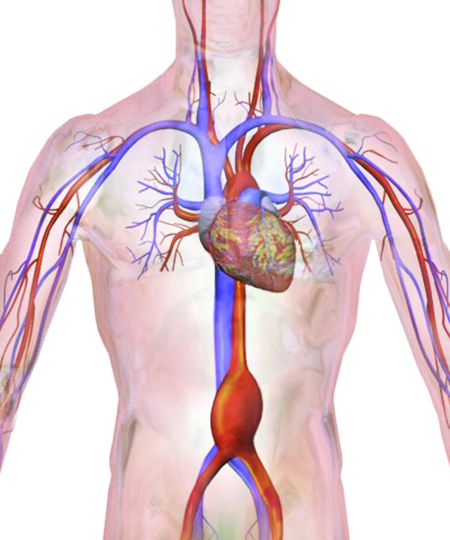
Features and diagnosis
PCS is a disorder of pelvic venous circulation that predominantly affects the ovarian veins. It is sometimes referred to as pelvic vein incompetence or pelvic vascular dysfunction. Just as veins in the legs can enlarge and become varicose, the ovarian veins – and sometimes the internal iliac veins – can become incompetent and unable to effectively return blood back to the heart.
Pregnancy may predispose patients to developing the abnormally dilated and refluxing veins that characterize PCS, as the increase in pelvic vein capacity and uterine compression can lead to significant stasis of blood in the pelvis and subsequent damage to the veins and the venous valves. There also is believed to be an estrogen component to the development of PCS, because estrogen is known to act as a vasodilator. Moreover, a congenital absence and incompetence of venous valves in some cases has been reported.
In a recent study looking at pelvic vein incompetence and symptoms of chronic pelvic pain, these women were reported to have a distinctive symptom profile, with the “most notable” features being the presence of dull pelvic pain that radiates to the upper thighs and is aggravated by prolonged standing and walking – symptoms that are similar to the leg symptoms experienced by patients with severe varicose veins (Eur J Obstet Gynecol Reprod Biol. 2016 Jan;196:21-5).
Other investigators have similarly described the pelvic pain related to PCS as a dull ache or heaviness sensation that is most severe at the end of the day and that is lessened with supine positioning (though not necessarily immediately) and often exacerbated with sexual intercourse, especially post coitus. These descriptions are in line with my experience with PCS. There is usually exquisite tenderness on pelvic exam, especially localized to the adnexa. Patients will often have varicose veins on their upper legs or labia.
Interestingly, it has been repeatedly shown that many women have dilated and incompetent pelvic veins without also having such pathognomonic pain. We therefore cannot treat women based solely on the finding of abnormal veins.
On the other hand we must determine which patients with chronic pelvic pain have PCS. The differential diagnosis for PCS includes endometriosis, adenomyosis chronic pelvic inflammatory disease, adhesive disease, adnexal masses, adnexal torsion, and several nongynecologic diseases including interstitial cystitis and irritable bowel syndrome.
Venography has become the gold standard for diagnosing pelvic congestion. The procedure involves catheterization of the ovarian veins through a femoral or jugular approach. In our experience, the common femoral vein is the more frequently used access point. Using a contrast injection, the interventional radiologist can assess the degree of venous dilation and reflux in the pelvis.

There currently is no consensus on a cutoff for vein diameter or on any validated measures for congestion. According to one report on PCS authored by interventional radiologists, the diagnosis of PCS is confirmed with the venographic findings of ovarian vein diameter greater than 6 mm, retrograde ovarian or pelvic venous flow, presence of several tortuous collateral pelvic venous pathways, and delayed or stagnant clearance on contrast (Semin Intervent Radiol. 2008 Dec;25[4]:361-8).
The criteria vary, however. A recent literature review on pelvic congestion syndrome by Chiara Borghi, MD, and Lucio Dell’Atti, MD, states that incompetent pelvic veins are defined as more than 5-10 mm in diameter (Arch Gynecol Obstet. 2016 Feb;293[2]:291-301).
To more accurately diagnose PCS, our patients undergo tilt-table venography. The patient is placed into a reverse-Trendelenburg upright or semi-upright position to potentially exacerbate any venous reflux or dilation.
Other methods of identifying and diagnosing pelvic congestion have included transabdominal and transvaginal ultrasound, CT, and MRI. While CT and MRI both offer an overview of the pelvic vasculature and are helpful for ruling out other causes of chronic pelvic pain, they have low specificity for pelvic varices, according to the Italian review.
Sonography performed in the supine position, on the other hand, appears to be increasingly viewed as an acceptable screening tool for determining which patients may ultimately benefit from venography. It is also important in evaluation to rule out other pathologies not yet excluded. However, it should not be used for diagnosis of PCS.
Treating PCS
There are two main approaches to treating PCS: venous ligation (a gynecologic surgical approach) and percutaneous transcatheter embolization (performed by interventional radiologists).
The literature and evidence base is still in its infancy, but is growing. In our experience, both approaches lead to good resolution of symptoms over time in the majority of patients, and appear superior to the medical therapies that have been proposed for treating PCS, such as progestins and gonadotropin-releasing hormone agonists. Success rates with medical therapy are more variable and appear to be more short lived.
A review published this year on the effectiveness of embolization of pelvic veins for reducing chronic pelvic pain showed that 75% of women undergoing embolization had symptomatic relief that generally increased over time and was sustained. The authors concluded that embolization appears to be effective for the majority of women, and is safe, although they also noted that the quality of the evidence is low (J Vasc Interv Radiol. 2016 Oct;27[10]:1478-86.e8). Their review was based almost entirely on prospective case series.
Dr. Borghi and Dr. Dell’Atti offered a similar assessment of embolization for PCS, stating in their review article that clinical success has been reported in 70%-85% of patients. They also report nearly equivalent success rates of up to 75% with treatment via surgical ligation of ovarian and/or pelvic vasculature. These findings are from mostly observational data and case series.
Decisions about which approach to take should be individualized. If there are no differences with respect to insurance coverage for the patient, then embolization may be the preferred approach because it is the most minimally invasive technique and can potentially be performed at the time of diagnostic venography, negating the need for a second procedure. A skilled interventional radiologist familiar with the disease and the treatment is necessary. Various embolic agents are utilized, including coils, glues, foams, and other agents that cause sclerosis of the abnormal veins.
In other cases, venous ligation is preferred, especially when an additional gynecologic surgery, such as a cystectomy or myomectomy, is required.
Surgical ligation of ovarian veins was initially performed via laparotomy using a traditional retroperitoneal approach. The surgical goal is to isolate the ovarian vein significantly above the pelvic brim and before the vein becomes substantially dilated. Laparotomy therefore requires a vertical mid-line incision to provide adequate access to the appropriate portion of the ovarian vessels, leading to potentially high morbidity and poor cosmesis.
More recently, gynecologic surgeons skilled in laparoscopy have successfully managed PCS transperitoneally. A few small series of bilateral laparoscopic transperitoneal ligation of ovarian veins have been reported, including one by Tigellio Gargiulo, MD, who clipped both veins in their upper third, near their distal ends at the inferior vena cava (right) and the renal vein (left) (J Am Assoc Gynecol Laparosc. 2003 Nov;10[4]:501-4).
We prefer a robot-assisted laparoscopic approach for most of our patients. Not only does the improved dexterity help while working with sensitive vasculature, but more importantly we are able to use Firefly fluorescence.
The procedure generally is as follows. The uterine adnexa on the affected side is grasped and placed on tension so that the infundibulopelvic (IP) ligament can be visualized as it courses up and above the pelvic brim. The peritoneum immediately over the IP ligament is gently grasped and tented upward, and a small incision is made into the peritoneum, providing access into the retroperitoneum. The ureter should be visualized medial to this dissection.
The peritoneal tissue is then gently dissected off the ovarian vessels. Once the vessels are freed from the peritoneal tissue, the dilated ovarian vein is often clearly visualized. It is important to note that if no venous dilation is seen during laparoscopy, the procedure should not be aborted. Due to the Trendelenburg position that is utilized in gynecologic – and especially laparoscopic – surgery, the venous system sometimes appears falsely “normal” at this time.
Once the ovarian vessels have been isolated, the arteries must be separated from the veins. The adventitial tissue is dissected until the vessels are separated. Great care should be taken to ensure that all movements run parallel to the vessels and not perpendicular, therefore decreasing the risk of bleeding.
This process can be challenging. The surgeon is working with delicate vasculature. Often there are several branches from the vein that have formed due to the abnormal venous system. The best way to approach it is to identify planes and separate those planes in order to isolate individual vessels. If difficulties are still encountered, the surgeon should restart the dissection higher.
Once the dilated ovarian vein is isolated, one to two clips are placed.
Usually the artery is clearly distinct from the vein as it is smaller, more elastic, and can be seen pulsing. However, occasionally it is difficult to distinguish. In these cases, assistance with the da Vinci surgical system is useful: Indocyanine green (ICG) dye can be injected intravenously and visualized with a near-infrared light on the da Vinci platform. The dye is then seen glowing green as it first courses through the artery and then the vein.
For patients who have been found on venography to have bilateral disease, we perform the ligation procedure bilaterally. Once ligation is complete, the more competent collateral veins in the pelvis will assume more of the venous circulation.
In our experience, patients have ultimately noted substantial pain relief after these procedures, both with the endoscopic embolization and the surgical ligation. Patients are counseled that it can take several months to notice a relief in the pain.
In rare cases, pelvic congestion is related to extrinsic compression. For instance, the left renal vein can become compressed between the aorta and the superior mesenteric artery (the nutcracker syndrome), or the left common iliac vein can be compressed between the overlying right internal iliac artery and the underlying vertebral body (May-Thurner syndrome). Both of these conditions can lead to secondary PCS.
Such complex conditions are usually treated by vascular surgeons. May-Thurner syndrome is treated via stenting, while nutcracker syndrome can be treated with stenting or transposition of the renal vein to the distal vena cava.
Dr. Steller is an associate at the Family Health Centers of San Diego. She reported having no relevant financial disclosures.
BY CHARLES E. MILLER, MD
Chronic pelvic pain is described as the presence of lower abdominal or pelvic pain for longer than 6 months. It is believed to affect approximately one in six women and 12%-15% of women of reproductive age. The diagnosis and treatment of chronic pelvic pain adds as much as a $2 billion burden to our health system annually.
It was first described clinically in the literature in 1857, while the existence of pelvic varicosities wasn’t documented for nearly another 100 years. Pelvic congestion syndrome (PCS) accounts for 30%-70% of cases presenting with chronic pelvic pain. PCS can be due to pelvic venous insufficiency, characterized by reflux into pelvic veins leading to pelvic varicosities or alternative venous pathways secondary to varicose veins of the leg.
Other etiologies of PCS include nutcracker syndrome (left renal vein compressed between the aorta and the superior mesenteric artery), May-Thurner syndrome (compression of the left common iliac vein by the right common iliac artery) or, less likely, tumor thrombosis of the inferior vena cava, portal vein thrombosis, renal cell carcinoma, left renal thrombosis, or left kidney arterial-venous fistula.
While there appears to be significant literature indicating a long-term success rate of greater than 80% in patients treated by percutaneous endovascular procedures (embolization, stenting), there is far less information on the postsurgical success of blocking the varicose gonadal vein. Nevertheless, our long-term results with gonadal vein clipping is virtually the same as that of our radiological colleagues.
It is a pleasure to welcome Courtney Steller, DO, to this edition of the Master Class in Gynecologic Surgery to discuss the diagnosis and treatment of PCS, with an emphasis on surgical correction.
Dr. Steller is a recent graduate of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. She is currently in private practice and is an associate at the Family Health Centers of San Diego, Calif.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at obnews@frontlinemedcom.com.
Pelvic congestion syndrome: A treatable cause of pain
BY COURTNEY STELLER, DO
Pelvic congestion syndrome is a poorly understood and underdiagnosed disease. Yet, over the last decade, the syndrome has become less controversial as the etiology has become better understood and as the diagnostic approach has become more specific. Through these advances, treatments have also become increasingly more successful.
This is an important shift, because the chronic pelvic pain experienced by patients with pelvic congestion significantly impacts their quality of life and well-being. As the pain persists, it can become exceedingly difficult to manage. Many patients we have ultimately treated for pelvic congestion syndrome have had years of various work-ups, significant diagnostic investigations, and trials of different treatments without having any cause of their pain identified or achieving any lasting symptom relief.
The pelvic pain in patients with pelvic congestion syndrome (PCS) can be noncyclical or cyclical. It is present most of the time but tends to get worse at the end of the day and after long periods of standing and/or sitting. The pain also may worsen with intercourse, largely afterward. The syndrome tends to occur in premenopausal and multiparous women, but it’s important to appreciate that this is not always the case; we have diagnosed and treated PCS in several young, nulliparous patients as well.
Features and diagnosis
PCS is a disorder of pelvic venous circulation that predominantly affects the ovarian veins. It is sometimes referred to as pelvic vein incompetence or pelvic vascular dysfunction. Just as veins in the legs can enlarge and become varicose, the ovarian veins – and sometimes the internal iliac veins – can become incompetent and unable to effectively return blood back to the heart.
Pregnancy may predispose patients to developing the abnormally dilated and refluxing veins that characterize PCS, as the increase in pelvic vein capacity and uterine compression can lead to significant stasis of blood in the pelvis and subsequent damage to the veins and the venous valves. There also is believed to be an estrogen component to the development of PCS, because estrogen is known to act as a vasodilator. Moreover, a congenital absence and incompetence of venous valves in some cases has been reported.
In a recent study looking at pelvic vein incompetence and symptoms of chronic pelvic pain, these women were reported to have a distinctive symptom profile, with the “most notable” features being the presence of dull pelvic pain that radiates to the upper thighs and is aggravated by prolonged standing and walking – symptoms that are similar to the leg symptoms experienced by patients with severe varicose veins (Eur J Obstet Gynecol Reprod Biol. 2016 Jan;196:21-5).
Other investigators have similarly described the pelvic pain related to PCS as a dull ache or heaviness sensation that is most severe at the end of the day and that is lessened with supine positioning (though not necessarily immediately) and often exacerbated with sexual intercourse, especially post coitus. These descriptions are in line with my experience with PCS. There is usually exquisite tenderness on pelvic exam, especially localized to the adnexa. Patients will often have varicose veins on their upper legs or labia.
Interestingly, it has been repeatedly shown that many women have dilated and incompetent pelvic veins without also having such pathognomonic pain. We therefore cannot treat women based solely on the finding of abnormal veins.
On the other hand we must determine which patients with chronic pelvic pain have PCS. The differential diagnosis for PCS includes endometriosis, adenomyosis chronic pelvic inflammatory disease, adhesive disease, adnexal masses, adnexal torsion, and several nongynecologic diseases including interstitial cystitis and irritable bowel syndrome.
Venography has become the gold standard for diagnosing pelvic congestion. The procedure involves catheterization of the ovarian veins through a femoral or jugular approach. In our experience, the common femoral vein is the more frequently used access point. Using a contrast injection, the interventional radiologist can assess the degree of venous dilation and reflux in the pelvis.

There currently is no consensus on a cutoff for vein diameter or on any validated measures for congestion. According to one report on PCS authored by interventional radiologists, the diagnosis of PCS is confirmed with the venographic findings of ovarian vein diameter greater than 6 mm, retrograde ovarian or pelvic venous flow, presence of several tortuous collateral pelvic venous pathways, and delayed or stagnant clearance on contrast (Semin Intervent Radiol. 2008 Dec;25[4]:361-8).
The criteria vary, however. A recent literature review on pelvic congestion syndrome by Chiara Borghi, MD, and Lucio Dell’Atti, MD, states that incompetent pelvic veins are defined as more than 5-10 mm in diameter (Arch Gynecol Obstet. 2016 Feb;293[2]:291-301).
To more accurately diagnose PCS, our patients undergo tilt-table venography. The patient is placed into a reverse-Trendelenburg upright or semi-upright position to potentially exacerbate any venous reflux or dilation.
Other methods of identifying and diagnosing pelvic congestion have included transabdominal and transvaginal ultrasound, CT, and MRI. While CT and MRI both offer an overview of the pelvic vasculature and are helpful for ruling out other causes of chronic pelvic pain, they have low specificity for pelvic varices, according to the Italian review.
Sonography performed in the supine position, on the other hand, appears to be increasingly viewed as an acceptable screening tool for determining which patients may ultimately benefit from venography. It is also important in evaluation to rule out other pathologies not yet excluded. However, it should not be used for diagnosis of PCS.
Treating PCS
There are two main approaches to treating PCS: venous ligation (a gynecologic surgical approach) and percutaneous transcatheter embolization (performed by interventional radiologists).
The literature and evidence base is still in its infancy, but is growing. In our experience, both approaches lead to good resolution of symptoms over time in the majority of patients, and appear superior to the medical therapies that have been proposed for treating PCS, such as progestins and gonadotropin-releasing hormone agonists. Success rates with medical therapy are more variable and appear to be more short lived.
A review published this year on the effectiveness of embolization of pelvic veins for reducing chronic pelvic pain showed that 75% of women undergoing embolization had symptomatic relief that generally increased over time and was sustained. The authors concluded that embolization appears to be effective for the majority of women, and is safe, although they also noted that the quality of the evidence is low (J Vasc Interv Radiol. 2016 Oct;27[10]:1478-86.e8). Their review was based almost entirely on prospective case series.
Dr. Borghi and Dr. Dell’Atti offered a similar assessment of embolization for PCS, stating in their review article that clinical success has been reported in 70%-85% of patients. They also report nearly equivalent success rates of up to 75% with treatment via surgical ligation of ovarian and/or pelvic vasculature. These findings are from mostly observational data and case series.
Decisions about which approach to take should be individualized. If there are no differences with respect to insurance coverage for the patient, then embolization may be the preferred approach because it is the most minimally invasive technique and can potentially be performed at the time of diagnostic venography, negating the need for a second procedure. A skilled interventional radiologist familiar with the disease and the treatment is necessary. Various embolic agents are utilized, including coils, glues, foams, and other agents that cause sclerosis of the abnormal veins.
In other cases, venous ligation is preferred, especially when an additional gynecologic surgery, such as a cystectomy or myomectomy, is required.
Surgical ligation of ovarian veins was initially performed via laparotomy using a traditional retroperitoneal approach. The surgical goal is to isolate the ovarian vein significantly above the pelvic brim and before the vein becomes substantially dilated. Laparotomy therefore requires a vertical mid-line incision to provide adequate access to the appropriate portion of the ovarian vessels, leading to potentially high morbidity and poor cosmesis.
More recently, gynecologic surgeons skilled in laparoscopy have successfully managed PCS transperitoneally. A few small series of bilateral laparoscopic transperitoneal ligation of ovarian veins have been reported, including one by Tigellio Gargiulo, MD, who clipped both veins in their upper third, near their distal ends at the inferior vena cava (right) and the renal vein (left) (J Am Assoc Gynecol Laparosc. 2003 Nov;10[4]:501-4).
We prefer a robot-assisted laparoscopic approach for most of our patients. Not only does the improved dexterity help while working with sensitive vasculature, but more importantly we are able to use Firefly fluorescence.
The procedure generally is as follows. The uterine adnexa on the affected side is grasped and placed on tension so that the infundibulopelvic (IP) ligament can be visualized as it courses up and above the pelvic brim. The peritoneum immediately over the IP ligament is gently grasped and tented upward, and a small incision is made into the peritoneum, providing access into the retroperitoneum. The ureter should be visualized medial to this dissection.
The peritoneal tissue is then gently dissected off the ovarian vessels. Once the vessels are freed from the peritoneal tissue, the dilated ovarian vein is often clearly visualized. It is important to note that if no venous dilation is seen during laparoscopy, the procedure should not be aborted. Due to the Trendelenburg position that is utilized in gynecologic – and especially laparoscopic – surgery, the venous system sometimes appears falsely “normal” at this time.
Once the ovarian vessels have been isolated, the arteries must be separated from the veins. The adventitial tissue is dissected until the vessels are separated. Great care should be taken to ensure that all movements run parallel to the vessels and not perpendicular, therefore decreasing the risk of bleeding.
This process can be challenging. The surgeon is working with delicate vasculature. Often there are several branches from the vein that have formed due to the abnormal venous system. The best way to approach it is to identify planes and separate those planes in order to isolate individual vessels. If difficulties are still encountered, the surgeon should restart the dissection higher.
Once the dilated ovarian vein is isolated, one to two clips are placed.
Usually the artery is clearly distinct from the vein as it is smaller, more elastic, and can be seen pulsing. However, occasionally it is difficult to distinguish. In these cases, assistance with the da Vinci surgical system is useful: Indocyanine green (ICG) dye can be injected intravenously and visualized with a near-infrared light on the da Vinci platform. The dye is then seen glowing green as it first courses through the artery and then the vein.
For patients who have been found on venography to have bilateral disease, we perform the ligation procedure bilaterally. Once ligation is complete, the more competent collateral veins in the pelvis will assume more of the venous circulation.
In our experience, patients have ultimately noted substantial pain relief after these procedures, both with the endoscopic embolization and the surgical ligation. Patients are counseled that it can take several months to notice a relief in the pain.
In rare cases, pelvic congestion is related to extrinsic compression. For instance, the left renal vein can become compressed between the aorta and the superior mesenteric artery (the nutcracker syndrome), or the left common iliac vein can be compressed between the overlying right internal iliac artery and the underlying vertebral body (May-Thurner syndrome). Both of these conditions can lead to secondary PCS.
Such complex conditions are usually treated by vascular surgeons. May-Thurner syndrome is treated via stenting, while nutcracker syndrome can be treated with stenting or transposition of the renal vein to the distal vena cava.
Dr. Steller is an associate at the Family Health Centers of San Diego. She reported having no relevant financial disclosures.
BY CHARLES E. MILLER, MD
Chronic pelvic pain is described as the presence of lower abdominal or pelvic pain for longer than 6 months. It is believed to affect approximately one in six women and 12%-15% of women of reproductive age. The diagnosis and treatment of chronic pelvic pain adds as much as a $2 billion burden to our health system annually.
It was first described clinically in the literature in 1857, while the existence of pelvic varicosities wasn’t documented for nearly another 100 years. Pelvic congestion syndrome (PCS) accounts for 30%-70% of cases presenting with chronic pelvic pain. PCS can be due to pelvic venous insufficiency, characterized by reflux into pelvic veins leading to pelvic varicosities or alternative venous pathways secondary to varicose veins of the leg.
Other etiologies of PCS include nutcracker syndrome (left renal vein compressed between the aorta and the superior mesenteric artery), May-Thurner syndrome (compression of the left common iliac vein by the right common iliac artery) or, less likely, tumor thrombosis of the inferior vena cava, portal vein thrombosis, renal cell carcinoma, left renal thrombosis, or left kidney arterial-venous fistula.
While there appears to be significant literature indicating a long-term success rate of greater than 80% in patients treated by percutaneous endovascular procedures (embolization, stenting), there is far less information on the postsurgical success of blocking the varicose gonadal vein. Nevertheless, our long-term results with gonadal vein clipping is virtually the same as that of our radiological colleagues.
It is a pleasure to welcome Courtney Steller, DO, to this edition of the Master Class in Gynecologic Surgery to discuss the diagnosis and treatment of PCS, with an emphasis on surgical correction.
Dr. Steller is a recent graduate of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill. She is currently in private practice and is an associate at the Family Health Centers of San Diego, Calif.
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, and past president of the AAGL and the International Society for Gynecologic Endoscopy. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville and Schaumburg, Ill.; director of minimally invasive gynecologic surgery and the director of the AAGL/SRS Fellowship in Minimally Invasive Gynecologic Surgery at Advocate Lutheran General Hospital, Park Ridge, Ill.; and the medical editor of this column, Master Class. He reported having no financial disclosures relevant to this column. Email him at obnews@frontlinemedcom.com.
Pelvic congestion syndrome: A treatable cause of pain
BY COURTNEY STELLER, DO
Pelvic congestion syndrome is a poorly understood and underdiagnosed disease. Yet, over the last decade, the syndrome has become less controversial as the etiology has become better understood and as the diagnostic approach has become more specific. Through these advances, treatments have also become increasingly more successful.
This is an important shift, because the chronic pelvic pain experienced by patients with pelvic congestion significantly impacts their quality of life and well-being. As the pain persists, it can become exceedingly difficult to manage. Many patients we have ultimately treated for pelvic congestion syndrome have had years of various work-ups, significant diagnostic investigations, and trials of different treatments without having any cause of their pain identified or achieving any lasting symptom relief.
The pelvic pain in patients with pelvic congestion syndrome (PCS) can be noncyclical or cyclical. It is present most of the time but tends to get worse at the end of the day and after long periods of standing and/or sitting. The pain also may worsen with intercourse, largely afterward. The syndrome tends to occur in premenopausal and multiparous women, but it’s important to appreciate that this is not always the case; we have diagnosed and treated PCS in several young, nulliparous patients as well.
Features and diagnosis
PCS is a disorder of pelvic venous circulation that predominantly affects the ovarian veins. It is sometimes referred to as pelvic vein incompetence or pelvic vascular dysfunction. Just as veins in the legs can enlarge and become varicose, the ovarian veins – and sometimes the internal iliac veins – can become incompetent and unable to effectively return blood back to the heart.
Pregnancy may predispose patients to developing the abnormally dilated and refluxing veins that characterize PCS, as the increase in pelvic vein capacity and uterine compression can lead to significant stasis of blood in the pelvis and subsequent damage to the veins and the venous valves. There also is believed to be an estrogen component to the development of PCS, because estrogen is known to act as a vasodilator. Moreover, a congenital absence and incompetence of venous valves in some cases has been reported.
In a recent study looking at pelvic vein incompetence and symptoms of chronic pelvic pain, these women were reported to have a distinctive symptom profile, with the “most notable” features being the presence of dull pelvic pain that radiates to the upper thighs and is aggravated by prolonged standing and walking – symptoms that are similar to the leg symptoms experienced by patients with severe varicose veins (Eur J Obstet Gynecol Reprod Biol. 2016 Jan;196:21-5).
Other investigators have similarly described the pelvic pain related to PCS as a dull ache or heaviness sensation that is most severe at the end of the day and that is lessened with supine positioning (though not necessarily immediately) and often exacerbated with sexual intercourse, especially post coitus. These descriptions are in line with my experience with PCS. There is usually exquisite tenderness on pelvic exam, especially localized to the adnexa. Patients will often have varicose veins on their upper legs or labia.
Interestingly, it has been repeatedly shown that many women have dilated and incompetent pelvic veins without also having such pathognomonic pain. We therefore cannot treat women based solely on the finding of abnormal veins.
On the other hand we must determine which patients with chronic pelvic pain have PCS. The differential diagnosis for PCS includes endometriosis, adenomyosis chronic pelvic inflammatory disease, adhesive disease, adnexal masses, adnexal torsion, and several nongynecologic diseases including interstitial cystitis and irritable bowel syndrome.
Venography has become the gold standard for diagnosing pelvic congestion. The procedure involves catheterization of the ovarian veins through a femoral or jugular approach. In our experience, the common femoral vein is the more frequently used access point. Using a contrast injection, the interventional radiologist can assess the degree of venous dilation and reflux in the pelvis.

There currently is no consensus on a cutoff for vein diameter or on any validated measures for congestion. According to one report on PCS authored by interventional radiologists, the diagnosis of PCS is confirmed with the venographic findings of ovarian vein diameter greater than 6 mm, retrograde ovarian or pelvic venous flow, presence of several tortuous collateral pelvic venous pathways, and delayed or stagnant clearance on contrast (Semin Intervent Radiol. 2008 Dec;25[4]:361-8).
The criteria vary, however. A recent literature review on pelvic congestion syndrome by Chiara Borghi, MD, and Lucio Dell’Atti, MD, states that incompetent pelvic veins are defined as more than 5-10 mm in diameter (Arch Gynecol Obstet. 2016 Feb;293[2]:291-301).
To more accurately diagnose PCS, our patients undergo tilt-table venography. The patient is placed into a reverse-Trendelenburg upright or semi-upright position to potentially exacerbate any venous reflux or dilation.
Other methods of identifying and diagnosing pelvic congestion have included transabdominal and transvaginal ultrasound, CT, and MRI. While CT and MRI both offer an overview of the pelvic vasculature and are helpful for ruling out other causes of chronic pelvic pain, they have low specificity for pelvic varices, according to the Italian review.
Sonography performed in the supine position, on the other hand, appears to be increasingly viewed as an acceptable screening tool for determining which patients may ultimately benefit from venography. It is also important in evaluation to rule out other pathologies not yet excluded. However, it should not be used for diagnosis of PCS.
Treating PCS
There are two main approaches to treating PCS: venous ligation (a gynecologic surgical approach) and percutaneous transcatheter embolization (performed by interventional radiologists).
The literature and evidence base is still in its infancy, but is growing. In our experience, both approaches lead to good resolution of symptoms over time in the majority of patients, and appear superior to the medical therapies that have been proposed for treating PCS, such as progestins and gonadotropin-releasing hormone agonists. Success rates with medical therapy are more variable and appear to be more short lived.
A review published this year on the effectiveness of embolization of pelvic veins for reducing chronic pelvic pain showed that 75% of women undergoing embolization had symptomatic relief that generally increased over time and was sustained. The authors concluded that embolization appears to be effective for the majority of women, and is safe, although they also noted that the quality of the evidence is low (J Vasc Interv Radiol. 2016 Oct;27[10]:1478-86.e8). Their review was based almost entirely on prospective case series.
Dr. Borghi and Dr. Dell’Atti offered a similar assessment of embolization for PCS, stating in their review article that clinical success has been reported in 70%-85% of patients. They also report nearly equivalent success rates of up to 75% with treatment via surgical ligation of ovarian and/or pelvic vasculature. These findings are from mostly observational data and case series.
Decisions about which approach to take should be individualized. If there are no differences with respect to insurance coverage for the patient, then embolization may be the preferred approach because it is the most minimally invasive technique and can potentially be performed at the time of diagnostic venography, negating the need for a second procedure. A skilled interventional radiologist familiar with the disease and the treatment is necessary. Various embolic agents are utilized, including coils, glues, foams, and other agents that cause sclerosis of the abnormal veins.
In other cases, venous ligation is preferred, especially when an additional gynecologic surgery, such as a cystectomy or myomectomy, is required.
Surgical ligation of ovarian veins was initially performed via laparotomy using a traditional retroperitoneal approach. The surgical goal is to isolate the ovarian vein significantly above the pelvic brim and before the vein becomes substantially dilated. Laparotomy therefore requires a vertical mid-line incision to provide adequate access to the appropriate portion of the ovarian vessels, leading to potentially high morbidity and poor cosmesis.
More recently, gynecologic surgeons skilled in laparoscopy have successfully managed PCS transperitoneally. A few small series of bilateral laparoscopic transperitoneal ligation of ovarian veins have been reported, including one by Tigellio Gargiulo, MD, who clipped both veins in their upper third, near their distal ends at the inferior vena cava (right) and the renal vein (left) (J Am Assoc Gynecol Laparosc. 2003 Nov;10[4]:501-4).
We prefer a robot-assisted laparoscopic approach for most of our patients. Not only does the improved dexterity help while working with sensitive vasculature, but more importantly we are able to use Firefly fluorescence.
The procedure generally is as follows. The uterine adnexa on the affected side is grasped and placed on tension so that the infundibulopelvic (IP) ligament can be visualized as it courses up and above the pelvic brim. The peritoneum immediately over the IP ligament is gently grasped and tented upward, and a small incision is made into the peritoneum, providing access into the retroperitoneum. The ureter should be visualized medial to this dissection.
The peritoneal tissue is then gently dissected off the ovarian vessels. Once the vessels are freed from the peritoneal tissue, the dilated ovarian vein is often clearly visualized. It is important to note that if no venous dilation is seen during laparoscopy, the procedure should not be aborted. Due to the Trendelenburg position that is utilized in gynecologic – and especially laparoscopic – surgery, the venous system sometimes appears falsely “normal” at this time.
Once the ovarian vessels have been isolated, the arteries must be separated from the veins. The adventitial tissue is dissected until the vessels are separated. Great care should be taken to ensure that all movements run parallel to the vessels and not perpendicular, therefore decreasing the risk of bleeding.
This process can be challenging. The surgeon is working with delicate vasculature. Often there are several branches from the vein that have formed due to the abnormal venous system. The best way to approach it is to identify planes and separate those planes in order to isolate individual vessels. If difficulties are still encountered, the surgeon should restart the dissection higher.
Once the dilated ovarian vein is isolated, one to two clips are placed.
Usually the artery is clearly distinct from the vein as it is smaller, more elastic, and can be seen pulsing. However, occasionally it is difficult to distinguish. In these cases, assistance with the da Vinci surgical system is useful: Indocyanine green (ICG) dye can be injected intravenously and visualized with a near-infrared light on the da Vinci platform. The dye is then seen glowing green as it first courses through the artery and then the vein.
For patients who have been found on venography to have bilateral disease, we perform the ligation procedure bilaterally. Once ligation is complete, the more competent collateral veins in the pelvis will assume more of the venous circulation.
In our experience, patients have ultimately noted substantial pain relief after these procedures, both with the endoscopic embolization and the surgical ligation. Patients are counseled that it can take several months to notice a relief in the pain.
In rare cases, pelvic congestion is related to extrinsic compression. For instance, the left renal vein can become compressed between the aorta and the superior mesenteric artery (the nutcracker syndrome), or the left common iliac vein can be compressed between the overlying right internal iliac artery and the underlying vertebral body (May-Thurner syndrome). Both of these conditions can lead to secondary PCS.
Such complex conditions are usually treated by vascular surgeons. May-Thurner syndrome is treated via stenting, while nutcracker syndrome can be treated with stenting or transposition of the renal vein to the distal vena cava.
Dr. Steller is an associate at the Family Health Centers of San Diego. She reported having no relevant financial disclosures.
AAA screening showed no mortality reduction in new trial
In contrast to previous studies, screening for abdominal aortic aneurysms in older men does not appear to have a significant effect on overall mortality, according to a prospective, randomized study.
Mortality from ruptured AAA remains high in older men, which has prompted four previous large randomized trials to explore whether screening men aged 65 years and older might reduce mortality.
Writing in the October 31 online edition of JAMA Internal Medicine, the authors reported the long-term outcomes of an Australian population-based trial of screening for abdominal aortic aneurysms in 49,801 men aged 64-83 years, of whom 19 249 were invited to screening and 12,203 of those underwent screening (isrctn.org Identifier: ISRCTN16171472).
After a mean 12.8 years of follow-up, there was a non-significant 9% lower mortality in the invited screening group compared to the control group and a non-significant 8% lower mortality among men aged 65-74 years.
Overall, there were 90 deaths from ruptured AAA in the screening group and 98 in the control group (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6633).
The prevalence of abdominal aortic aneurysms with a diameter at or above 30 mm was 6.6% in men aged 65-74, and 0.4% for those with a diameter of 55 mm or above.
While the rate of ruptured abdominal aortic aneurysms was significantly lower in the invited group compared to the control group (72 vs. 99, P = .04), the 30-day mortality after surgery for rupture was higher in the invited group compared to the control group (61.5% vs. 43.2%).
Screening had no meaningful impact on the risk of all-cause, cardiovascular, and other mortality, but men who had smoked had a higher risk of rupture and of death from a rupture than those who had never smoked, regardless of screening status.
The rate of total elective operations was significantly higher in the invited group compared to controls (536 vs. 414, P < .001), mainly in the first year after screening.
The authors calculated that to prevent one death from a ruptured abdominal aortic aneurysm in five years, 4784 men aged 64-83 years or 3290 men aged 65-74 years would need to be invited for screening.
While the strength of the study was that it was truly population-based – using the electoral roll – the authors said the lack of a benefit from screening was likely due to the relatively low rate of rupture and death from AAA, as well as a high rate of elective surgery for this condition, in the control group.
The non-significant 8% reduction in mortality observed in the study was significantly less than the 42% and 66% reductions seen in previous trials with a similar length of follow-up.
The authors suggested this may also have been related to a lower fraction of invited men participating in screening, but pointed out that the incidence of AAA in men is declining.
“The reason for the decrease in incidence and prevalence is multifactorial but is probably driven by differences in rates of smoking and cessation because the relative risk for AAA events is 3- to 6-fold higher in smokers compared with non-smokers,” they wrote.
The authors said selective screening of smokers or ex-smokers may be more effective, but pointed out that this approach would miss around one-quarter of aneurysms. However they suggested more targeted screening may yet achieve a benefit.
“The small overall benefit of population-wide screening does not mean that finding AAAs in suitable older men is not worthwhile because deaths from AAAs in men who actually attended for screening were halved by early detection and successful treatment.”
The study was supported by the National Health and Medical Research Council Project. The authors reported that they had no conflicts of interest.
These new data will not change the finding of robust reduction in AAA-related mortality from screening seen in all previous meta-analyses. However, the most recently updated meta-analyses now reveal the small reduction in all-cause mortality with screening to be statistically significant.
So although the findings of the Western Australian trial remain negative and raise some concerns about screening, their aggregation with other studies does not change the overall conclusions that screening substantially reduced AAA-related mortality and also resulted in a statistically significant reduction in all-cause mortality. Restricting screening to men who have smoked (the strongest risk factor for AAA) further lowers cost and increases efficiency.
Frank A. Lederle, MD, is from the Center for Chronic Disease Outcomes Research at the Veterans Affairs Medical Center. These comments are taken from an accompanying editorial (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6663). No conflicts of interest were declared.
These new data will not change the finding of robust reduction in AAA-related mortality from screening seen in all previous meta-analyses. However, the most recently updated meta-analyses now reveal the small reduction in all-cause mortality with screening to be statistically significant.
So although the findings of the Western Australian trial remain negative and raise some concerns about screening, their aggregation with other studies does not change the overall conclusions that screening substantially reduced AAA-related mortality and also resulted in a statistically significant reduction in all-cause mortality. Restricting screening to men who have smoked (the strongest risk factor for AAA) further lowers cost and increases efficiency.
Frank A. Lederle, MD, is from the Center for Chronic Disease Outcomes Research at the Veterans Affairs Medical Center. These comments are taken from an accompanying editorial (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6663). No conflicts of interest were declared.
These new data will not change the finding of robust reduction in AAA-related mortality from screening seen in all previous meta-analyses. However, the most recently updated meta-analyses now reveal the small reduction in all-cause mortality with screening to be statistically significant.
So although the findings of the Western Australian trial remain negative and raise some concerns about screening, their aggregation with other studies does not change the overall conclusions that screening substantially reduced AAA-related mortality and also resulted in a statistically significant reduction in all-cause mortality. Restricting screening to men who have smoked (the strongest risk factor for AAA) further lowers cost and increases efficiency.
Frank A. Lederle, MD, is from the Center for Chronic Disease Outcomes Research at the Veterans Affairs Medical Center. These comments are taken from an accompanying editorial (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6663). No conflicts of interest were declared.
In contrast to previous studies, screening for abdominal aortic aneurysms in older men does not appear to have a significant effect on overall mortality, according to a prospective, randomized study.
Mortality from ruptured AAA remains high in older men, which has prompted four previous large randomized trials to explore whether screening men aged 65 years and older might reduce mortality.
Writing in the October 31 online edition of JAMA Internal Medicine, the authors reported the long-term outcomes of an Australian population-based trial of screening for abdominal aortic aneurysms in 49,801 men aged 64-83 years, of whom 19 249 were invited to screening and 12,203 of those underwent screening (isrctn.org Identifier: ISRCTN16171472).
After a mean 12.8 years of follow-up, there was a non-significant 9% lower mortality in the invited screening group compared to the control group and a non-significant 8% lower mortality among men aged 65-74 years.
Overall, there were 90 deaths from ruptured AAA in the screening group and 98 in the control group (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6633).
The prevalence of abdominal aortic aneurysms with a diameter at or above 30 mm was 6.6% in men aged 65-74, and 0.4% for those with a diameter of 55 mm or above.
While the rate of ruptured abdominal aortic aneurysms was significantly lower in the invited group compared to the control group (72 vs. 99, P = .04), the 30-day mortality after surgery for rupture was higher in the invited group compared to the control group (61.5% vs. 43.2%).
Screening had no meaningful impact on the risk of all-cause, cardiovascular, and other mortality, but men who had smoked had a higher risk of rupture and of death from a rupture than those who had never smoked, regardless of screening status.
The rate of total elective operations was significantly higher in the invited group compared to controls (536 vs. 414, P < .001), mainly in the first year after screening.
The authors calculated that to prevent one death from a ruptured abdominal aortic aneurysm in five years, 4784 men aged 64-83 years or 3290 men aged 65-74 years would need to be invited for screening.
While the strength of the study was that it was truly population-based – using the electoral roll – the authors said the lack of a benefit from screening was likely due to the relatively low rate of rupture and death from AAA, as well as a high rate of elective surgery for this condition, in the control group.
The non-significant 8% reduction in mortality observed in the study was significantly less than the 42% and 66% reductions seen in previous trials with a similar length of follow-up.
The authors suggested this may also have been related to a lower fraction of invited men participating in screening, but pointed out that the incidence of AAA in men is declining.
“The reason for the decrease in incidence and prevalence is multifactorial but is probably driven by differences in rates of smoking and cessation because the relative risk for AAA events is 3- to 6-fold higher in smokers compared with non-smokers,” they wrote.
The authors said selective screening of smokers or ex-smokers may be more effective, but pointed out that this approach would miss around one-quarter of aneurysms. However they suggested more targeted screening may yet achieve a benefit.
“The small overall benefit of population-wide screening does not mean that finding AAAs in suitable older men is not worthwhile because deaths from AAAs in men who actually attended for screening were halved by early detection and successful treatment.”
The study was supported by the National Health and Medical Research Council Project. The authors reported that they had no conflicts of interest.
In contrast to previous studies, screening for abdominal aortic aneurysms in older men does not appear to have a significant effect on overall mortality, according to a prospective, randomized study.
Mortality from ruptured AAA remains high in older men, which has prompted four previous large randomized trials to explore whether screening men aged 65 years and older might reduce mortality.
Writing in the October 31 online edition of JAMA Internal Medicine, the authors reported the long-term outcomes of an Australian population-based trial of screening for abdominal aortic aneurysms in 49,801 men aged 64-83 years, of whom 19 249 were invited to screening and 12,203 of those underwent screening (isrctn.org Identifier: ISRCTN16171472).
After a mean 12.8 years of follow-up, there was a non-significant 9% lower mortality in the invited screening group compared to the control group and a non-significant 8% lower mortality among men aged 65-74 years.
Overall, there were 90 deaths from ruptured AAA in the screening group and 98 in the control group (JAMA Internal Medicine 2016, October 31. DOI:10.1001/jamainternmed.2016.6633).
The prevalence of abdominal aortic aneurysms with a diameter at or above 30 mm was 6.6% in men aged 65-74, and 0.4% for those with a diameter of 55 mm or above.
While the rate of ruptured abdominal aortic aneurysms was significantly lower in the invited group compared to the control group (72 vs. 99, P = .04), the 30-day mortality after surgery for rupture was higher in the invited group compared to the control group (61.5% vs. 43.2%).
Screening had no meaningful impact on the risk of all-cause, cardiovascular, and other mortality, but men who had smoked had a higher risk of rupture and of death from a rupture than those who had never smoked, regardless of screening status.
The rate of total elective operations was significantly higher in the invited group compared to controls (536 vs. 414, P < .001), mainly in the first year after screening.
The authors calculated that to prevent one death from a ruptured abdominal aortic aneurysm in five years, 4784 men aged 64-83 years or 3290 men aged 65-74 years would need to be invited for screening.
While the strength of the study was that it was truly population-based – using the electoral roll – the authors said the lack of a benefit from screening was likely due to the relatively low rate of rupture and death from AAA, as well as a high rate of elective surgery for this condition, in the control group.
The non-significant 8% reduction in mortality observed in the study was significantly less than the 42% and 66% reductions seen in previous trials with a similar length of follow-up.
The authors suggested this may also have been related to a lower fraction of invited men participating in screening, but pointed out that the incidence of AAA in men is declining.
“The reason for the decrease in incidence and prevalence is multifactorial but is probably driven by differences in rates of smoking and cessation because the relative risk for AAA events is 3- to 6-fold higher in smokers compared with non-smokers,” they wrote.
The authors said selective screening of smokers or ex-smokers may be more effective, but pointed out that this approach would miss around one-quarter of aneurysms. However they suggested more targeted screening may yet achieve a benefit.
“The small overall benefit of population-wide screening does not mean that finding AAAs in suitable older men is not worthwhile because deaths from AAAs in men who actually attended for screening were halved by early detection and successful treatment.”
The study was supported by the National Health and Medical Research Council Project. The authors reported that they had no conflicts of interest.
Key clinical point:
Major finding: Men invited to undergo screening for abdominal aortic aneurysms had a non-significant 9% lower mortality compared to a control group.
Data source: Prospective, population-based randomized controlled trial in 49,801 men aged 64-83 years.
Disclosures: The study was supported by the National Health and Medical Research Council Project. The authors reported that they had no conflicts of interest.
Fostering surgical innovation: The path forward
Click here to download the PDF.
Key learning objectives
The faculty for this roundtable aim to:
- Explain the process for bringing an innovation to market, including the roles of surgeon inventor, engineer, manufacturer, and industry
- Discuss best practices, based on lessons learned, when pursuing an innovative idea for patient care
- Articulate ways to improve upon the entire development process for new techniques, devices, etc, being brought to the FDA for possible approval and to market for patient use.
Click here to download the PDF.
Key learning objectives
The faculty for this roundtable aim to:
- Explain the process for bringing an innovation to market, including the roles of surgeon inventor, engineer, manufacturer, and industry
- Discuss best practices, based on lessons learned, when pursuing an innovative idea for patient care
- Articulate ways to improve upon the entire development process for new techniques, devices, etc, being brought to the FDA for possible approval and to market for patient use.
Click here to download the PDF.
Key learning objectives
The faculty for this roundtable aim to:
- Explain the process for bringing an innovation to market, including the roles of surgeon inventor, engineer, manufacturer, and industry
- Discuss best practices, based on lessons learned, when pursuing an innovative idea for patient care
- Articulate ways to improve upon the entire development process for new techniques, devices, etc, being brought to the FDA for possible approval and to market for patient use.
Product Update: Kyleena; LapCap2
NEW LNG IUS: GOOD FOR 5 YEARS
FOR MORE INFORMATION, VISIT:
https://hcp.kyleena-us.com/
EASIER LAPAROSCOPIC ACCESS
To use LapCap2, says Life Care, center it over the umbilicus, attach a hose to the suction port, and apply negative pressure. The abdomen immediately rises for Veress needle insertion. Inert gas is then delivered to replace the negative pressure, and the procedure can continue.
FOR MORE INFORMATION, VISIT:
http://www.lcmd.com/products/lapcap2
NEW LNG IUS: GOOD FOR 5 YEARS
FOR MORE INFORMATION, VISIT:
https://hcp.kyleena-us.com/
EASIER LAPAROSCOPIC ACCESS
To use LapCap2, says Life Care, center it over the umbilicus, attach a hose to the suction port, and apply negative pressure. The abdomen immediately rises for Veress needle insertion. Inert gas is then delivered to replace the negative pressure, and the procedure can continue.
FOR MORE INFORMATION, VISIT:
http://www.lcmd.com/products/lapcap2
NEW LNG IUS: GOOD FOR 5 YEARS
FOR MORE INFORMATION, VISIT:
https://hcp.kyleena-us.com/
EASIER LAPAROSCOPIC ACCESS
To use LapCap2, says Life Care, center it over the umbilicus, attach a hose to the suction port, and apply negative pressure. The abdomen immediately rises for Veress needle insertion. Inert gas is then delivered to replace the negative pressure, and the procedure can continue.
FOR MORE INFORMATION, VISIT:
http://www.lcmd.com/products/lapcap2
Pediatric OSA improved with oral montelukast
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
The majority of children with obstructive sleep apnea (OSA) who took oral montelukast showed reductions in their apnea-hypopnea index (AHI) scores, in a randomized, double-blind placebo-controlled study.
Typically, OSA in children is treated by adenotonsillectomy, according to Leila Kheirandish-Gozal, MD, director of clinical sleep research at the University of Chicago, and her colleagues. Prior to this study, only one randomized controlled trial had showed that children with mild OSA “responded favorably” to the leukotriene modifier montelukast (Pediatrics. 2012 Aug 31. doi: 10.1542/peds.2012-0310).
Twenty (71%) of the children who received montelukast had fewer AHI events per hour of total sleep time at the end of the study. The average number of such events for these patients was 4.2 plus or minus 2.8 after taking the drug, compared with 9.2 plus or minus 4.1 at the beginning of the study (P less than .0001). Only two (6.9%) of the patients who took the placebo had lower AHI scores at the end of the study, with the average AHI score for the placebo group having been 8.7 plus or minus 4.9 events per hour of total sleep time. At baseline, the average score for patients in the placebo group was 8.2 plus or minus 5.0 AHI events per hour of total sleep time at baseline.
Another improvement seen by patients who received the drug was a decrease in the number of 3% reductions in arterial oxygen saturation per hour of sleep. At the beginning of the study, these patients had 7.2 plus or minus 3.1 of these events; by the end of the study, the number of these events was down to 2.8 plus or minus 1.8 (P less than .001). No significant decrease in the number of these events was seen among patients in the placebo group.
In this study, “montelukast emerges as favorably reducing the severity of OSA short term in children 2-10 years of age. These findings add to the existing evidence supporting a therapeutic role for anti-inflammatory approaches in the management of this highly prevalent condition in children, and clearly justify future studies targeting the long-term benefits of these approaches in children with OSA,” the researchers wrote.
All patients participated in overnight sleep studies following a referral to one of two sleep clinics by their primary care pediatrician or pediatric otolaryngologist, at the beginning of the study. Children who had been diagnosed with symptomatic snoring and had an AHI score of greater than 2 events per hour of total sleep time, and for whom adenotonsillectomy was contemplated, were included in the study.
Central, obstructive, mixed apneic events were counted and hypopneas were assessed. OSA was defined “as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths,” the investigators said. Hypopneas were defined “as a decrease in oronasal flow greater than 50% on either the thermistor or nasal pressure transducer signal. with a corresponding decrease in arterial oxygen saturation greater than 3% or arousal,” Dr. Kheirandish-Gozal and her coauthors said.
Patients were excluded from the study for a variety of reasons, including having severe OSA requiring early surgical intervention.
Adverse events included headache in two children, one from the experimental group and one from the placebo group, and nausea in two subjects from the placebo group and in one from the montelukast group.
Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
Key clinical point:
Major finding: 71% of patients who took montelukast had a significant reduction in AHI events per hour of total sleep time (P less than .0001).
Data source: A prospective, randomized, double-blind placebo-controlled study of 57 children with obstructive sleep apnea.
Disclosures: Merck provided tablets used in this study. Dr. Kheirandish-Gozal reported grants from Merck and the National Institutes of Health during the conduct of the study. David Gozal, MD, is supported by the Herbert T. Abelson Chair in Pediatrics at the University of Chicago.
Age of blood did not affect mortality in transfused patients
In-hospital mortality did not vary for patients who received transfusions of blood that had been stored for 2 weeks and for patients who got blood that had been stored for 4 weeks, based on results from 20,858 hospitalized patients in the randomized, controlled INFORM (Informing Fresh versus Old Red Cell Management) trial conducted at six hospitals in four countries.
While previous trials have concluded that the storage time of blood did not affect patient mortality, those studies largely included high-risk patients and were not statistically powered to detect small mortality differences, Nancy M. Heddle, professor of medicine and director of the McMaster (University) transfusion research program, Hamilton, Ont., and colleagues reported in an article published online in the New England Journal of Medicine (doi: 10.1056/NEJMoa1609014). Standard practice is to transfuse with the oldest available blood, which can be stored up to 42 days.
Their study included general hospitalized patients who required a red cell transfusion. From April 2012 through October 2015, patients were randomly assigned in a 1:2 ratio patients to receive blood that had been stored for the shortest duration (mean duration 13 days, 6,936 patients) or the longest duration (mean duration 23.6 days, 13,922 patients).
Only patients with type A or O blood were included in the study’s primary analysis, because of the difficulty of achieving a difference of at least 10 days in the mean duration of blood storage with other blood types.
There were 634 deaths (9.1% mortality) among patients in the short-term blood storage group and 1,213 deaths (8.7% mortality) in the long-term blood storage group. The difference was not statistically significant. Similar results were seen when the analysis was expanded to include all 24,736 patients with any blood type; the mortality rates were 9.1% and 8.8%, respectively.
An additional analysis found similar results in three prespecified high-risk subgroups – patients undergoing cardiovascular surgery, those admitted to intensive care, and those with cancer.
INFORM, Current Controlled Trials number ISRCTN08118744, was funded by the Canadian Institutes of Health Research, Canadian Blood Services, and Health Canada. Ms. Heddle had no relevant financial disclosures.
mdales@frontlinemedcom.com
On Twitter @maryjodales
The results of the INFORM trial should end the debate regarding whether short-term or long-term storage of blood is advantageous. However, questions remain about whether red cells transfused during the last allowed week of storage (35-42 days) pose more risk. Observational studies continue to raise concerns about the use of the oldest blood.
The INFORM trial, with its large numbers of patients, should permit researchers to analyze enough data to address this remaining issue. The transfusion medicine community needs to know whether the storage period should be reduced to less than 35 and whether new preservative solutions should be sought.
Aaron A.R. Tobian, MD, PhD, and Paul M. Ness, MD, are with the division of transfusion medicine, department of pathology, Johns Hopkins University, Baltimore. They had no relevant financial conflicts of interest and made their remarks in an editorial (10.1056/NEJMe1612444) that accompanied the published study.
The results of the INFORM trial should end the debate regarding whether short-term or long-term storage of blood is advantageous. However, questions remain about whether red cells transfused during the last allowed week of storage (35-42 days) pose more risk. Observational studies continue to raise concerns about the use of the oldest blood.
The INFORM trial, with its large numbers of patients, should permit researchers to analyze enough data to address this remaining issue. The transfusion medicine community needs to know whether the storage period should be reduced to less than 35 and whether new preservative solutions should be sought.
Aaron A.R. Tobian, MD, PhD, and Paul M. Ness, MD, are with the division of transfusion medicine, department of pathology, Johns Hopkins University, Baltimore. They had no relevant financial conflicts of interest and made their remarks in an editorial (10.1056/NEJMe1612444) that accompanied the published study.
The results of the INFORM trial should end the debate regarding whether short-term or long-term storage of blood is advantageous. However, questions remain about whether red cells transfused during the last allowed week of storage (35-42 days) pose more risk. Observational studies continue to raise concerns about the use of the oldest blood.
The INFORM trial, with its large numbers of patients, should permit researchers to analyze enough data to address this remaining issue. The transfusion medicine community needs to know whether the storage period should be reduced to less than 35 and whether new preservative solutions should be sought.
Aaron A.R. Tobian, MD, PhD, and Paul M. Ness, MD, are with the division of transfusion medicine, department of pathology, Johns Hopkins University, Baltimore. They had no relevant financial conflicts of interest and made their remarks in an editorial (10.1056/NEJMe1612444) that accompanied the published study.
In-hospital mortality did not vary for patients who received transfusions of blood that had been stored for 2 weeks and for patients who got blood that had been stored for 4 weeks, based on results from 20,858 hospitalized patients in the randomized, controlled INFORM (Informing Fresh versus Old Red Cell Management) trial conducted at six hospitals in four countries.
While previous trials have concluded that the storage time of blood did not affect patient mortality, those studies largely included high-risk patients and were not statistically powered to detect small mortality differences, Nancy M. Heddle, professor of medicine and director of the McMaster (University) transfusion research program, Hamilton, Ont., and colleagues reported in an article published online in the New England Journal of Medicine (doi: 10.1056/NEJMoa1609014). Standard practice is to transfuse with the oldest available blood, which can be stored up to 42 days.
Their study included general hospitalized patients who required a red cell transfusion. From April 2012 through October 2015, patients were randomly assigned in a 1:2 ratio patients to receive blood that had been stored for the shortest duration (mean duration 13 days, 6,936 patients) or the longest duration (mean duration 23.6 days, 13,922 patients).
Only patients with type A or O blood were included in the study’s primary analysis, because of the difficulty of achieving a difference of at least 10 days in the mean duration of blood storage with other blood types.
There were 634 deaths (9.1% mortality) among patients in the short-term blood storage group and 1,213 deaths (8.7% mortality) in the long-term blood storage group. The difference was not statistically significant. Similar results were seen when the analysis was expanded to include all 24,736 patients with any blood type; the mortality rates were 9.1% and 8.8%, respectively.
An additional analysis found similar results in three prespecified high-risk subgroups – patients undergoing cardiovascular surgery, those admitted to intensive care, and those with cancer.
INFORM, Current Controlled Trials number ISRCTN08118744, was funded by the Canadian Institutes of Health Research, Canadian Blood Services, and Health Canada. Ms. Heddle had no relevant financial disclosures.
mdales@frontlinemedcom.com
On Twitter @maryjodales
In-hospital mortality did not vary for patients who received transfusions of blood that had been stored for 2 weeks and for patients who got blood that had been stored for 4 weeks, based on results from 20,858 hospitalized patients in the randomized, controlled INFORM (Informing Fresh versus Old Red Cell Management) trial conducted at six hospitals in four countries.
While previous trials have concluded that the storage time of blood did not affect patient mortality, those studies largely included high-risk patients and were not statistically powered to detect small mortality differences, Nancy M. Heddle, professor of medicine and director of the McMaster (University) transfusion research program, Hamilton, Ont., and colleagues reported in an article published online in the New England Journal of Medicine (doi: 10.1056/NEJMoa1609014). Standard practice is to transfuse with the oldest available blood, which can be stored up to 42 days.
Their study included general hospitalized patients who required a red cell transfusion. From April 2012 through October 2015, patients were randomly assigned in a 1:2 ratio patients to receive blood that had been stored for the shortest duration (mean duration 13 days, 6,936 patients) or the longest duration (mean duration 23.6 days, 13,922 patients).
Only patients with type A or O blood were included in the study’s primary analysis, because of the difficulty of achieving a difference of at least 10 days in the mean duration of blood storage with other blood types.
There were 634 deaths (9.1% mortality) among patients in the short-term blood storage group and 1,213 deaths (8.7% mortality) in the long-term blood storage group. The difference was not statistically significant. Similar results were seen when the analysis was expanded to include all 24,736 patients with any blood type; the mortality rates were 9.1% and 8.8%, respectively.
An additional analysis found similar results in three prespecified high-risk subgroups – patients undergoing cardiovascular surgery, those admitted to intensive care, and those with cancer.
INFORM, Current Controlled Trials number ISRCTN08118744, was funded by the Canadian Institutes of Health Research, Canadian Blood Services, and Health Canada. Ms. Heddle had no relevant financial disclosures.
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: There were 634 deaths (9.1% mortality) among patients in the short-term blood storage group and 1,213 deaths (8.7% mortality) in the long-term blood storage group.
Data source: The randomized, controlled INFORM (Informing Fresh versus Old Red Cell Management) trial.
Disclosures: INFORM, Current Controlled Trials number ISRCTN08118744, was funded by the Canadian Institutes of Health Research, Canadian Blood Services, and Health Canada. Ms. Heddle had no relevant financial disclosures.