User login
FIM at Discharge and Rehospitalization
Federally mandated pay‐for‐performance initiatives promote minimizing 30‐day hospital readmissions to improve healthcare quality and reduce costs. Although the reasons for readmissions are multifactorial, many patients are readmitted for a condition other than their initial hospital admitting diagnosis.[1] Impairments in functional status experienced during acute care hospitalization contribute to patients being discharged in a debilitated state and being vulnerable to postdischarge complications and potentially hospital readmission.[2] As such, decreased functional status may be an important and potentially modifiable risk factor for acute care hospital readmission.[3]
Previous studies have suggested that impaired functional status may be an important predictor of rehospitalization.[4, 5, 6, 7] However, inferences from existing studies are limited because they did not consider functional status as their primary focus, they only considered specific patient populations (eg, stroke) or readmissions occurring well beyond the 30‐day period defined by federal pay‐for‐performance standards.[4, 5, 6, 8, 9, 10] Our objective was to evaluate the association between functional status near the time of discharge from acute care hospital and 30‐day readmission for patients admitted to an acute inpatient rehabilitation facility. As a secondary objective, we sought to investigate the relationship between functional status and readmission by diagnostic category (medical, neurologic, or orthopedic).
METHODS
Study Population and Setting
We conducted a single‐center, retrospective study of patients admitted to an inpatient rehabilitation facility at a community hospital between July 1, 2006 and December 31, 2012. This facility provides intensive rehabilitation consisting of 3 hours of therapy per day, skilled nursing care on a 24‐hour basis, and medical care by a physiatrist. We excluded patients who died during inpatient rehabilitation (n=15, 0.2%) and patients not admitted directly from an acute care setting (n=178, 2.0%).
Data Source and Covariates
Data were derived from the Uniform Data System for Medical Rehabilitation (UDSMR), which is an administrative database providing the following data upon admission to an inpatient rehabilitation facility[11, 12, 13]: age, gender, race/ethnicity, marital status, the discharge setting, the admission Functional Independence Measure (FIM) score (details further below), and admission diagnostic category as defined by the primary discharge diagnosis from the acute care hospital and grouped by functional related groups (a case‐mix system for medical rehabilitation).[12, 14] The 3M ClinTrac management software (3M, St. Paul, MN), used for mandatory reporting to the State of Maryland, provided all‐payerrefined diagnosis related group (APRDRG) and severity of illness (SOI) combinations (a tool to group patients into clinically comparable disease and severity‐of‐illness categories expected to use similar resources and experience similar outcomes). The University HealthSystem Consortium (UHC) database provided national readmission rates for all APRDRG‐SOI combinations using a methodology that has been previously described.[15, 16] Expected readmission rates for APRDRG‐SOI combinations served as a patient risk stratification tool based on clinical logic that evaluates age, comorbidities, principal diagnosis during hospitalization, and procedures conducted during hospitalization.[17]
Primary Outcome: Acute Care Readmission
The primary outcome was all‐cause acute care readmission, defined as patient transfer to an acute care hospital during inpatient rehabilitation within 30 days from admission to inpatient rehabilitation. The care model for our inpatient rehabilitation unit is such that when patients become sick or develop a complication, they are admitted directly to a clinical unit (eg, intensive care unit) at the community hospital through a rapid‐response intervention, or the physiatrist arranges with an admitting inpatient attending to accept the patient directly to his or her service.
Primary Exposure: Functional Independence Measure
Functional status was measured using the FIM score.[18] The FIM score is an 18‐item measure of functional status, with each item scored on a scale from 1 to 7 (dependent to independent). Various aspects of motor function and cognitive function are assessed. The FIM has been validated and shown to be reliable and reproducible.[13, 19, 20] By definition for the FIM instrument, admission FIM scores are assessed by trained multidisciplinary personnel first over the 72 hours of the rehabilitation stay, and for this study served as a proxy for patient functional status upon discharge from the acute care setting in our analysis. This 72‐hour time window allows for full assessment by therapists and nurses; however, in clinical practice at the inpatient rehabilitation unit involved in this study, much of the FIM assessment occurs within the first 24 hours of the rehabilitation stay. For our analysis, we divided FIM scores into low, medium, and high functional groups. The thresholds for these groups were based on total FIM score tertiles from a prior study<60, 60 to 76, and >76.[16] As a secondary analysis we created 6 subscales of the overall FIM score based on previous research. These subscales included: transfers (transfer to chair/wheelchair, toilet, and tub/shower), locomotion (walking and stairs), self‐care (eating, grooming, bathing, dressing, and toileting), sphincter control (bladder and bowel management), communication (comprehension and expression), and social cognition (social interaction, problem solving, and memory).[21]
Statistical Analysis
To evaluate differences in patient characteristics by diagnostic category, analysis of variance and 2 tests were used for continuous and dichotomous variables, respectively. Logistic regression was used to evaluate the association between FIM score category and readmission status, adjusting for potentially confounding variables available from the UDSMR and UHC databases. We used interaction terms to test whether the association between the FIM score and readmissions varied significantly across diagnostic categories and by age. As a secondary analysis, we modeled FIM score as a continuous variable. We expressed the odds ratio in this analysis per 10‐point change in FIM, because this represents a clinically relevant change in function.[22] Logistic regression was also used to evaluate the association between FIM subscale scores (transfers, locomotion, self‐care, sphincter control, communication, and social cognition) and readmission status. Statistical significance was defined as a 2‐sided P<0.05. Data were analyzed with R (version 2.15.0;
RESULTS
Readmitted Patients and Diagnostic Categories
A total of 9405 consecutive eligible patients were admitted to the acute inpatient rehabilitation facility between July 1, 2006 and December 31, 2012. A total of 1182 (13%) patients were readmitted back to an acute care hospital from inpatient rehabilitation. Median (interquartile range) time to readmission from acute care hospital discharge was 6 days (310 days), and median length of stay for patients who were discharged to the community from inpatient rehabilitation was 8 days (612 days).
Table 1 shows characteristics of all inpatient rehabilitation patients by diagnostic category. For the neurologic category, the most common primary diagnoses were stroke and spinal cord injury; for the medical category, infection, renal failure, congestive heart failure, and chronic obstructive pulmonary disease; and for the orthopedic category, spinal arthrodesis, knee and hip replacements. Mean FIM scores were lowest and highest for patients admitted with a primarily neurologic and orthopedic diagnosis, respectively.
| Characteristic | All Patients, N=9405 | Diagnostic Category | |||
|---|---|---|---|---|---|
| Neurologic, n=3706 | Medical, n=2135 | Orthopedic, n=3564 | P Valueb | ||
| |||||
| Age, y | 67.8 (14.2) | 66.7 (15.3) | 67.0 (14.9) | 69.3 (12.4) | <0.001 |
| Male | 4,068 (43%) | 1,816 (49%) | 1,119 (52%) | 1,133 (32%) | <0.001 |
| Race | <0.001 | ||||
| Caucasian | 6,106 (65%) | 2344 (63%) | 1,320 (62%) | 2,442 (69%) | |
| African American | 2,501 (27%) | 984 (27%) | 658 (31%) | 859 (24%) | |
| Other | 798 (8%) | 378 (10%) | 157 (7%) | 263 (7%) | |
| Married | 4,330 (46%) | 1,683 (45%) | 931 (44%) | 1,716 (48%) | 0.002 |
| APRDRG‐SOI expected readmission rate | 18.0 (7.4) | 20.5 (6.8) | 21.3 (7.5) | 13.5 (5.6) | <0.001 |
| Total admission FIM score | 68.7 (17.2) | 60.4 (18.6) | 69.1 (15.5) | 77.2 (11.7) | <0.001 |
FIM Score Category and Risk of Readmission
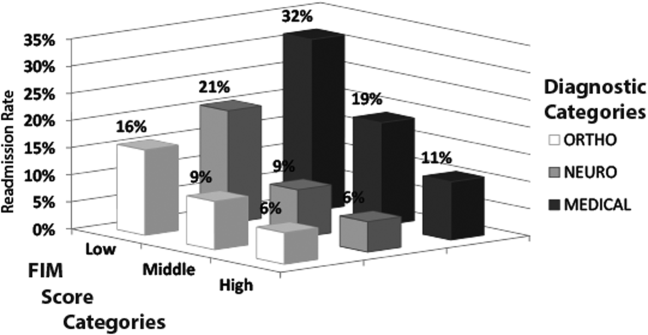
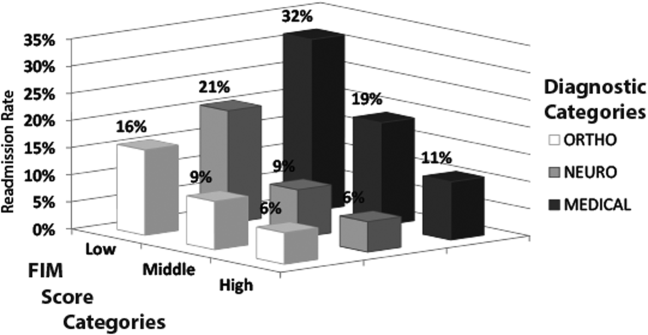
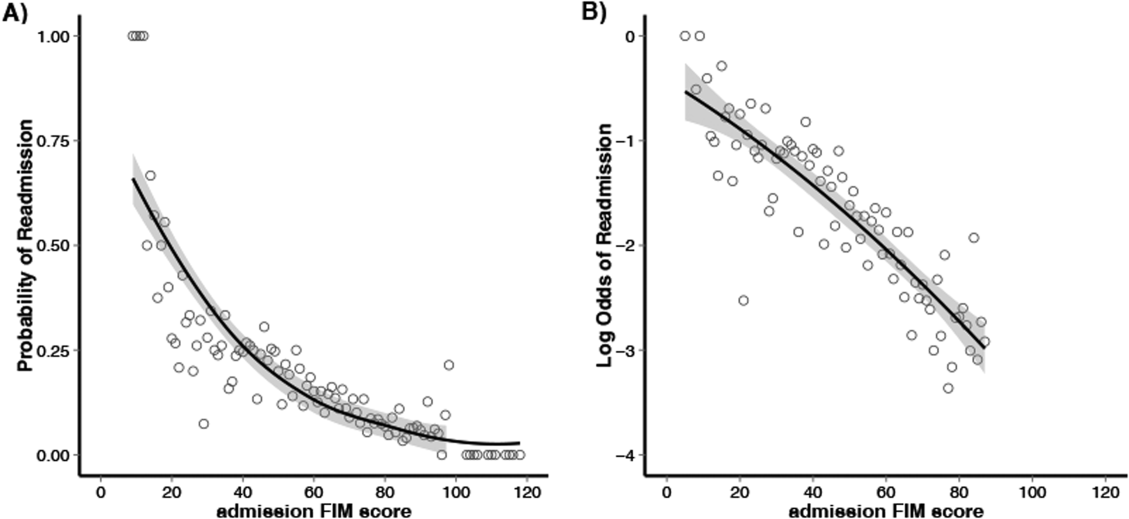
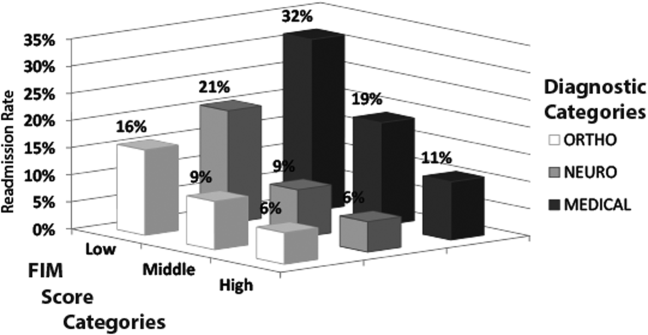
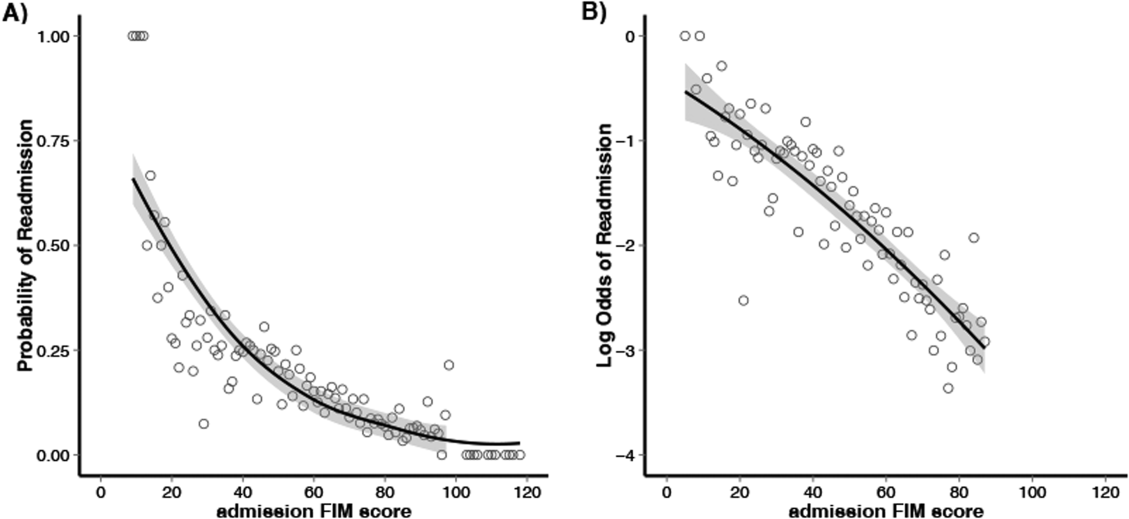
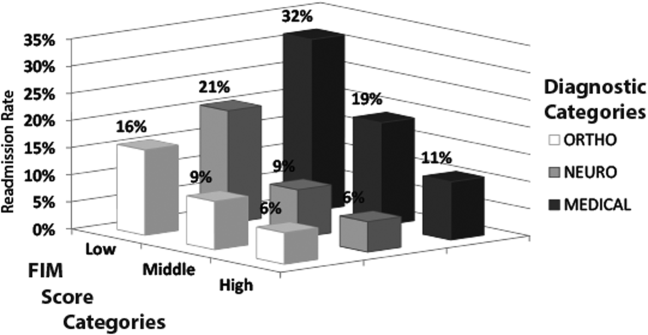
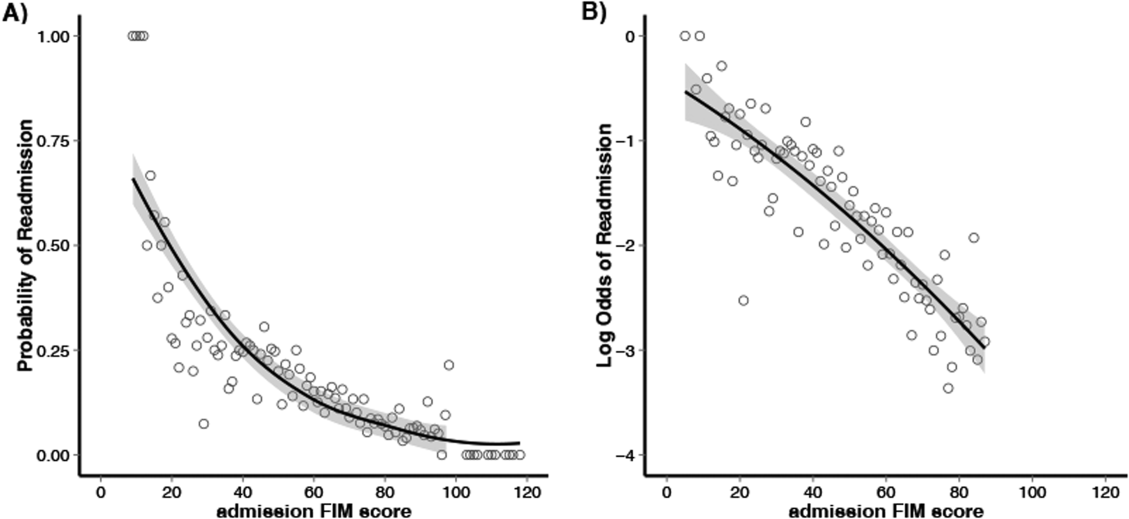
Figure 1 shows that patients in the low admission FIM score category had the highest unadjusted rate of readmission for each diagnostic category. In unadjusted analysis, Table 2 shows that younger age, male sex, APDRG‐SOI expected readmission rate, and orthopedic and medical diagnostic categories were associated with readmission. As a continuous variable, FIM scores were linearly associated with readmission (Figure 2), with an unadjusted odds ratio (OR) and 95% confidence interval (CI) of 1.4 (1.4‐1.4, P<0.001) for a 10‐point decrease in FIM. Compared to patients with high admission FIM scores, patients with low and middle FIM scores had higher unadjusted odds of readmission (OR: 4.0; 95% CI: 3.4‐4.7; P<0.001 and OR: 1.8; 95% CI: 1.5‐2.1; P<0.001, respectively). Mean FIM subscale scores for patients readmitted versus not readmitted were transfers (5.3 vs 7.0, P<0.001), locomotion (1.6 vs 2.3, P<0.001), self‐care (17.0 vs 20.8, P<0.001), communication (10.6 vs 11.5, P<0.001), and social cognition (15.1 vs 16.6, P<0.001).
| Bivariable Analysisb | Multivariable Analysisb | |||||
|---|---|---|---|---|---|---|
| Characteristic | All Patients, N=9405 | Readmitted, n=1,182 | OR (95% CI) | P Value | OR (95% CI) | P Value |
| ||||||
| Age, y | 68.0 (14.2) | 66.4 (14.5) | 0.9 (0.91.0) | <0.001 | 0.9 (0.91.0) | <0.001 |
| Male | 3,431 (42%) | 637 (54%) | 1.6 (1.41.8) | <0.001 | 1.3 (1.11.5) | < 0.001 |
| Race | ||||||
| Caucasian | 5,340 (65%) | 766 (65%) | 1.0 | 1.0 | ||
| African American | 2,177 (26%) | 324 (27%) | 1.0 (0.91.2) | 0.60 | 1.0 (0.81.1) | 0.75 |
| Other | 706 (9%) | 92 (8%) | 0.9 (0.71.1) | 0.41 | 0.8 (0.61.0) | 0.12 |
| Married | 3,775 (46%) | 555 (47%) | 1.0 (0.91.2) | 0.50 | 1.0 (0.91.2) | 0.67 |
| Admission diagnosis category | ||||||
| Neurologic | 3,205 (39%) | 501 (42%) | 1.0 | 1.0 | ||
| Medical | 1,726 (21%) | 409 (35%) | 1.5 (1.31.7) | <0.001 | 1.8 (1.62.1) | < 0.001 |
| Orthopedic | 3,292 (40%) | 272 (23%) | 0.5 (0.50.6) | <0.001 | 1.3 (1.11.6) | 0.005 |
| APDRG‐SOI expected readmission rate | 17.4 (7.1%) | 22.2 (8.0%) | 1.1 (1.11.1) | <0.001 | 1.1 (1.01.1) | < 0.001 |
| Total FIM score category | ||||||
| High FIM, >76 points | 3,517 (43%) | 257 (22%) | 1.0 | 1.0 | ||
| Middle FIM, 60points | 2,742 (33%) | 353 (30%) | 1.8 (1.52.1) | <0.001 | 1.5 (1.31.8) | < 0.001 |
| Low FIM, <60 points | 1,964 (24%) | 572 (48%) | 4.0 (3.44.7) | <0.001 | 3.0 (2.53.6) | < 0.001 |
Multivariable and Subset Analyses
Patients with a primary medical diagnosis had higher odds of readmission to the hospital, (OR: 1.8; 95% CI: 1.6‐2.1, P<0.001), relative to patients with a neurologic or orthopedic diagnosis (Table 2). Across all diagnoses, the adjusted odds ratios (95% CIs) for the low and middle versus high FIM score category were 3.0 (2.5‐3.6; P<0.001) and 1.5 (1.3‐1.8; P<0.001) respectively (Table 2). When modeled as a continuous variable, a 10‐point decrease in FIM score was associated with a significantly increased adjusted readmission rate (OR: 1.4; 95% CI: 1.3‐1.4; P<0.001). In adjusted analysis including all subscales of the FIM, only the physical subscales, transfers (P<0.001), locomotion (P=0.002), and self‐care (P<0.001), were significantly associated with readmission. For each diagnostic category, there were similar significant associations between admission FIM score group and readmission status (Table 3). The odds of readmission by FIM score did not differ significantly across the 3 major diagnostic categories (P=0.20 for interaction term), suggesting that the effect of functional status was similar across various types of patients. We also did not observe a statistical interaction between age and FIM score group in predicting readmission (P=0.58). Patients in the lowest FIM group with a medical diagnosis had the highest adjusted readmission rate of 28.7% (Table 3).
| Multivariable Analysisa | Adjusted Readmission Ratesb | |||
|---|---|---|---|---|
| No. | OR (95% CI) | P Value | % (95% CI) | |
| ||||
| Neurologic | ||||
| High FIM (>76 points) | 755 | 1.0 | 7.3 (4.710.0) | |
| Middle FIM (6076 points) | 1,283 | 1.4 (1.02.1) | 0.06 | 9.1 (7.011.1) |
| Low FIM (<60 points) | 1,668 | 3.3 (2.34.7) | <0.001 | 18.7 (16.820.6) |
| Medical | ||||
| High FIM (>76 points) | 807 | 1.0 | 11.2 (8.114.3) | |
| Middle FIM (6076 points) | 766 | 1.8 (1.32.4) | <0.001 | 17.7 (14.520.9) |
| Low FIM (<60 points) | 562 | 3.2 (2.44.3) | <0.001 | 28.7 (25.132.4) |
| Orthopedic | ||||
| High FIM (>76 points) | 2,212 | 1.0 | 6.1 (4.77.6) | |
| Middle FIM (6076 points) | 1,046 | 1.4 (1.11.9) | 0.02 | 8.3 (6.410.1) |
| Low FIM (<60 points) | 306 | 2.2 (1.53.3) | <0.001 | 13.5 (10.416.7) |
DISCUSSION
In this study of 9405 consecutive patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we investigated the association between functional status and readmission to an acute care hospital. We found that low functional status near the time of acute care hospital discharge was strongly associated with higher readmission rates. This relationship was consistently observed across major patient diagnostic categories, with low functioning medical patients having the highest rate of readmission (28.7%). Efforts to maintain or improve functional status during acute care hospitalization may be an important modifiable risk factor for acute care hospital readmission.
Previous studies have suggested that functional status may serve as an indicator of physiological reserve, and therefore vulnerability to medical complications and readmission.[6, 16, 23, 24, 25] Physiologic reserve refers to a person's ability to endure acute illness and is influenced by a number of factors, such as the adequacy of oxygen delivery to tissues, cardiovascular health, immune state, and nutritional status.[26] We found that motor subscales of the FIM score (transfers, locomotion, and self‐care), but not the other subscales, were independently associated with readmissions, which may suggest that lower motor scores are a stronger marker of physiologic reserve.[10, 16, 27] Although not our primary focus, we did note in our multivariable models that after adjusting for functional status, patients in a medical diagnostic category had higher readmission rates compared to patients with a primary neurologic or orthopedic diagnosis, but the impact of FIM score was consistent across all these diagnostic categories. We speculate that medical conditions that result in hospitalization, such as sepsis or acute kidney failure, may be more likely to result in multiorgan dysfunction that may impair physiological reserve and increase susceptibility to medical complications.[28, 29, 30, 31] In comparison, acute neurologic and orthopedic diagnoses, such as stroke or hip arthroplasty, directly impair gross motor function,[32, 33, 34, 35] with relative sparing of overall physiologic reserve.
The association between low functional status and readmissions is supported by previous studies across multiple hospital settings.[4, 5, 7, 8, 9, 27, 36] Despite this finding, routine inpatient medical practice may not fully address functional impairments. For instance, systematic measurement and documentation of functional status on admission and during hospitalization are not routine and may be a barrier to identifying medical patients at high risk for readmission.[37, 38, 39] Moreover, without recognition of functional impairment and its implications, current clinical practice may suboptimally prevent and treat physical impairments during inpatient care. However, such barriers can be surmounted. For example, in the medical intensive care unit setting, there is growing recognition that proactive and aggressive management of hospital‐acquired functional impairments through early rehabilitation is safe and feasible, improving patient outcomes while reducing hospital costs and readmissions.[3, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51] Moreover, 2 recent meta‐analyses have shown that physical therapy hospital‐based exercise programs can improve length of stay, overall hospital costs, and rates of discharge to home.[52, 53] Finally, a randomized trial has demonstrated that an individualized exercise regimen started in the acute hospital setting with long‐term telephone follow‐up can significantly reduce emergency hospital readmissions and improve quality of life in older adults.[54] Therefore, decreased functional status likely represents a modifiable risk factor for hospital readmission, and further research is necessary to more systematically identify low‐functioning patients and implement early mobility and activity programs to reduce hospital‐acquired functional impairment.[2, 49, 55]
Our analysis has potential limitations. First, this was an observational study and we are unable to demonstrate a direct cause‐and‐effect relationship between functional status and readmission. However, our results are consistent with prior literature in this field. Second, our cohort only included patients who were discharged from an acute hospital to a rehabilitation facility, which may limit its generalizability. However, we included a large patient sample size with a broad range of admission FIM scores, and our findings are consistent with other studies conducted in different clinical settings. Third, although 1 of our goals was to evaluate how readmission rates differed by diagnostic category, it is possible that individual diagnoses within each category may have different risks for readmission, and future larger studies could evaluate more detailed diagnostic grouping approaches. Fourth, we also recognize that although FIM score assessment has been validated, admission assessment occurs over a 72‐hour time period, during which patients' function could potentially change a clinically meaningful degree. Fifth, there may be residual confounding because of limitations in available data within our administrative dataset; however, we did account for severity of illness using a standardized measure, and prior research has demonstrated that the relationship between functional status and readmissions may be minimally confounded by demographic and clinical variables.[8, 16, 27, 56] Finally, we lacked readmission data following discharge from rehabilitation; it is possible that the association between FIM score at the time of rehabilitation initiation may have had limited predictive value among patients who successfully completed rehabilitation and were sent home.
CONCLUSION
In conclusion, in this study of patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we observed a strong association between decreased functional status and increased hospital readmission. In particular, medical patients with lower physical functioning exhibited an especially high rate of readmission. Incorporating functional status assessment into routine medical care may help identify patients at higher risk of readmission. Moreover, preventing and treating impaired functional status during inpatient admission, through early activity and mobility, should be evaluated as a way of improving patient outcomes and reducing hospital readmissions.
Disclosures: Erik Hoyer, MD, is supported by the Rehabilitation Medicine Scientist Training Program (RMSTP; 5K12HD001097). The authors report no conflicts of interest.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- . Post‐hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102.
- , , , et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341(5):373–377.
- , . Association of physical functioning with same‐hospital readmission after stroke. Am J Phys Med Rehabil. 2004;83(6):434–438.
- , , , . Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39(5):1449–1465.
- , , , , , . Risk factors for nonelective hospital readmissions. J Gen Intern Med. 1996;11(12):762–764.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , et al. Hospital readmission in persons with stroke following postacute inpatient rehabilitation. J Gerontol A Biol Sci Med Sci. 2012;67(8):875–881.
- , , , , , . Hospital readmission of persons with hip fracture following medical rehabilitation. Arch Gerontol Geriatr. 2003;36(1):15–22.
- , , , , , . Characteristics of persons rehospitalized after stroke rehabilitation. Arch Phys Med Rehabil. 2001;82(10):1367–1374.
- , , , et al. A classification system for inpatient rehabilitation patients: a review and proposed revisions to the functional independence measure‐function related groups. PB98–105992, September. Washington, DC: US Department of Commerce, National Technical Information Services; 1997.
- , , , , , . A case‐mix classification system for medical rehabilitation. Med Care. 1994;32(4):366–379.
- , , , . The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232.
- , , , , , . Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil. 1994;75(12):1277–1283.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA Intern Med. 2013;173(8):624–629.
- , , , , , . Functional status impairment is associated with unplanned readmissions. Arch Phys Med Rehabil. 2013;94(10):1951–1958.
- , , , et al. All patient refined diagnosis related groups (APR‐DRGs). Version 15.0. Report No.: 98‐054 Rev. 00. Wallingford, CT: 3M Health Information Systems; 1998.
- The inpatient rehabilitation facility–patient assessment instrument (IRF‐PAI) training manual. 2012. http://www.cms.gov/.
- , , , et al. Relationships between disability measures and nursing effort during medical rehabilitation for patients with traumatic brain and spinal cord injury. Arch Phys Med Rehabil. 1997;78(2):143–149.
- , , , . Interrater reliability of the 7‐level functional independence measure (FIM). Scand J Rehabil Med. 1994;26(3):115–119.
- , , , , , . Comparison of logistic regression and neural networks to predict rehospitalization in patients with stroke. J Clin Epidemiol. 2001;54(11):1159–1165.
- , , . Comparison of the responsiveness of the Barthel Index and the motor component of the Functional Independence Measure in stroke: the impact of using different methods for measuring responsiveness. J Clin Epidemiol. 2002;55(9):922–928.
- , . Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33(6):1560–1566.
- , , . Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298.
- , . Hospital readmission as an accountability measure. JAMA. 2011;305(5):504–505.
- . Susceptibility to critical illness: reserve, response and therapy. Intensive Care Med. 2000;26(suppl 1):S57–S63.
- , , , , . Predictors of discharge to acute care after inpatient rehabilitation in severely affected stroke patients. Am J Phys Med Rehabil. 2012;91(5):387–392.
- , , , et al. Clinical characteristics and outcomes of sepsis‐related vs non‐sepsis‐related ARDS. Chest. 2010;138(3):559–567.
- , . Long‐term outcomes from sepsis. Curr Infect Dis Rep. 2007;9(5):382–386.
- , . Heart failure performance measures and outcomes: real or illusory gains. JAMA. 2009;302(7):792–794.
- , , , , . Patients' self‐assessed functional status in heart failure by new york heart association class: a prognostic predictor of hospitalizations, quality of life and death. J Card Fail. 2010;16(2):150–156.
- , , , et al. Knee arthroplasty: disabilities in comparison to the general population and to hip arthroplasty using a French national longitudinal survey. PLoS One. 2008;3(7):e2561.
- , , , et al. Gait asymmetry in community‐ambulating stroke survivors. Arch Phys Med Rehabil. 2008;89(2):304–310.
- , , , . Recovery of upper extremity function in stroke patients: The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1994;75(4):394–398.
- , , , , , . The effect of admission physiological variables on 30 day outcome after stroke. J Clin Neurosci. 2005;12(8):905–910.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- . Can hospitalization‐associated disability be prevented? JAMA. 2011;306(16):1800–1801.
- , , . Hospitalization‐associated disability: “she was probably able to ambulate, but I'm not sure.” JAMA. 2011;306(16):1782–1793.
- , , , , , . Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193.
- . Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300(14):1685–1690.
- , , . Technology to enhance physical rehabilitation of critically ill patients. Crit Care Med. 2009;37(10 suppl):S436–S441.
- , , , et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542.
- , , , et al. ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med. 2013;41(3):717–724.
- , , , et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882.
- , , , et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243.
- , , , et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(1):139–145.
- , . Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 2010;17(4):271–281.
- , , , , . Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59(2):359–365.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304.
- , , , et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25(2):254–262.
- , , . Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;(1):CD005955.
- , , . Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil. 2011;92(9):1490–1500.
- , , , , , . Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24‐week exercise and telephone follow‐up program. J Am Geriatr Soc. 2009;57(3):395–402.
- , , , , , . Effects of an acute care for elders unit on costs and 30‐day readmissions. JAMA Intern Med. 2013:1–7.
- , , , , . Risks of acute hospital transfer and mortality during stroke rehabilitation. Arch Phys Med Rehabil. 2003;84(5):712–718.
Federally mandated pay‐for‐performance initiatives promote minimizing 30‐day hospital readmissions to improve healthcare quality and reduce costs. Although the reasons for readmissions are multifactorial, many patients are readmitted for a condition other than their initial hospital admitting diagnosis.[1] Impairments in functional status experienced during acute care hospitalization contribute to patients being discharged in a debilitated state and being vulnerable to postdischarge complications and potentially hospital readmission.[2] As such, decreased functional status may be an important and potentially modifiable risk factor for acute care hospital readmission.[3]
Previous studies have suggested that impaired functional status may be an important predictor of rehospitalization.[4, 5, 6, 7] However, inferences from existing studies are limited because they did not consider functional status as their primary focus, they only considered specific patient populations (eg, stroke) or readmissions occurring well beyond the 30‐day period defined by federal pay‐for‐performance standards.[4, 5, 6, 8, 9, 10] Our objective was to evaluate the association between functional status near the time of discharge from acute care hospital and 30‐day readmission for patients admitted to an acute inpatient rehabilitation facility. As a secondary objective, we sought to investigate the relationship between functional status and readmission by diagnostic category (medical, neurologic, or orthopedic).
METHODS
Study Population and Setting
We conducted a single‐center, retrospective study of patients admitted to an inpatient rehabilitation facility at a community hospital between July 1, 2006 and December 31, 2012. This facility provides intensive rehabilitation consisting of 3 hours of therapy per day, skilled nursing care on a 24‐hour basis, and medical care by a physiatrist. We excluded patients who died during inpatient rehabilitation (n=15, 0.2%) and patients not admitted directly from an acute care setting (n=178, 2.0%).
Data Source and Covariates
Data were derived from the Uniform Data System for Medical Rehabilitation (UDSMR), which is an administrative database providing the following data upon admission to an inpatient rehabilitation facility[11, 12, 13]: age, gender, race/ethnicity, marital status, the discharge setting, the admission Functional Independence Measure (FIM) score (details further below), and admission diagnostic category as defined by the primary discharge diagnosis from the acute care hospital and grouped by functional related groups (a case‐mix system for medical rehabilitation).[12, 14] The 3M ClinTrac management software (3M, St. Paul, MN), used for mandatory reporting to the State of Maryland, provided all‐payerrefined diagnosis related group (APRDRG) and severity of illness (SOI) combinations (a tool to group patients into clinically comparable disease and severity‐of‐illness categories expected to use similar resources and experience similar outcomes). The University HealthSystem Consortium (UHC) database provided national readmission rates for all APRDRG‐SOI combinations using a methodology that has been previously described.[15, 16] Expected readmission rates for APRDRG‐SOI combinations served as a patient risk stratification tool based on clinical logic that evaluates age, comorbidities, principal diagnosis during hospitalization, and procedures conducted during hospitalization.[17]
Primary Outcome: Acute Care Readmission
The primary outcome was all‐cause acute care readmission, defined as patient transfer to an acute care hospital during inpatient rehabilitation within 30 days from admission to inpatient rehabilitation. The care model for our inpatient rehabilitation unit is such that when patients become sick or develop a complication, they are admitted directly to a clinical unit (eg, intensive care unit) at the community hospital through a rapid‐response intervention, or the physiatrist arranges with an admitting inpatient attending to accept the patient directly to his or her service.
Primary Exposure: Functional Independence Measure
Functional status was measured using the FIM score.[18] The FIM score is an 18‐item measure of functional status, with each item scored on a scale from 1 to 7 (dependent to independent). Various aspects of motor function and cognitive function are assessed. The FIM has been validated and shown to be reliable and reproducible.[13, 19, 20] By definition for the FIM instrument, admission FIM scores are assessed by trained multidisciplinary personnel first over the 72 hours of the rehabilitation stay, and for this study served as a proxy for patient functional status upon discharge from the acute care setting in our analysis. This 72‐hour time window allows for full assessment by therapists and nurses; however, in clinical practice at the inpatient rehabilitation unit involved in this study, much of the FIM assessment occurs within the first 24 hours of the rehabilitation stay. For our analysis, we divided FIM scores into low, medium, and high functional groups. The thresholds for these groups were based on total FIM score tertiles from a prior study<60, 60 to 76, and >76.[16] As a secondary analysis we created 6 subscales of the overall FIM score based on previous research. These subscales included: transfers (transfer to chair/wheelchair, toilet, and tub/shower), locomotion (walking and stairs), self‐care (eating, grooming, bathing, dressing, and toileting), sphincter control (bladder and bowel management), communication (comprehension and expression), and social cognition (social interaction, problem solving, and memory).[21]
Statistical Analysis
To evaluate differences in patient characteristics by diagnostic category, analysis of variance and 2 tests were used for continuous and dichotomous variables, respectively. Logistic regression was used to evaluate the association between FIM score category and readmission status, adjusting for potentially confounding variables available from the UDSMR and UHC databases. We used interaction terms to test whether the association between the FIM score and readmissions varied significantly across diagnostic categories and by age. As a secondary analysis, we modeled FIM score as a continuous variable. We expressed the odds ratio in this analysis per 10‐point change in FIM, because this represents a clinically relevant change in function.[22] Logistic regression was also used to evaluate the association between FIM subscale scores (transfers, locomotion, self‐care, sphincter control, communication, and social cognition) and readmission status. Statistical significance was defined as a 2‐sided P<0.05. Data were analyzed with R (version 2.15.0;
RESULTS
Readmitted Patients and Diagnostic Categories
A total of 9405 consecutive eligible patients were admitted to the acute inpatient rehabilitation facility between July 1, 2006 and December 31, 2012. A total of 1182 (13%) patients were readmitted back to an acute care hospital from inpatient rehabilitation. Median (interquartile range) time to readmission from acute care hospital discharge was 6 days (310 days), and median length of stay for patients who were discharged to the community from inpatient rehabilitation was 8 days (612 days).
Table 1 shows characteristics of all inpatient rehabilitation patients by diagnostic category. For the neurologic category, the most common primary diagnoses were stroke and spinal cord injury; for the medical category, infection, renal failure, congestive heart failure, and chronic obstructive pulmonary disease; and for the orthopedic category, spinal arthrodesis, knee and hip replacements. Mean FIM scores were lowest and highest for patients admitted with a primarily neurologic and orthopedic diagnosis, respectively.
| Characteristic | All Patients, N=9405 | Diagnostic Category | |||
|---|---|---|---|---|---|
| Neurologic, n=3706 | Medical, n=2135 | Orthopedic, n=3564 | P Valueb | ||
| |||||
| Age, y | 67.8 (14.2) | 66.7 (15.3) | 67.0 (14.9) | 69.3 (12.4) | <0.001 |
| Male | 4,068 (43%) | 1,816 (49%) | 1,119 (52%) | 1,133 (32%) | <0.001 |
| Race | <0.001 | ||||
| Caucasian | 6,106 (65%) | 2344 (63%) | 1,320 (62%) | 2,442 (69%) | |
| African American | 2,501 (27%) | 984 (27%) | 658 (31%) | 859 (24%) | |
| Other | 798 (8%) | 378 (10%) | 157 (7%) | 263 (7%) | |
| Married | 4,330 (46%) | 1,683 (45%) | 931 (44%) | 1,716 (48%) | 0.002 |
| APRDRG‐SOI expected readmission rate | 18.0 (7.4) | 20.5 (6.8) | 21.3 (7.5) | 13.5 (5.6) | <0.001 |
| Total admission FIM score | 68.7 (17.2) | 60.4 (18.6) | 69.1 (15.5) | 77.2 (11.7) | <0.001 |
FIM Score Category and Risk of Readmission
Figure 1 shows that patients in the low admission FIM score category had the highest unadjusted rate of readmission for each diagnostic category. In unadjusted analysis, Table 2 shows that younger age, male sex, APDRG‐SOI expected readmission rate, and orthopedic and medical diagnostic categories were associated with readmission. As a continuous variable, FIM scores were linearly associated with readmission (Figure 2), with an unadjusted odds ratio (OR) and 95% confidence interval (CI) of 1.4 (1.4‐1.4, P<0.001) for a 10‐point decrease in FIM. Compared to patients with high admission FIM scores, patients with low and middle FIM scores had higher unadjusted odds of readmission (OR: 4.0; 95% CI: 3.4‐4.7; P<0.001 and OR: 1.8; 95% CI: 1.5‐2.1; P<0.001, respectively). Mean FIM subscale scores for patients readmitted versus not readmitted were transfers (5.3 vs 7.0, P<0.001), locomotion (1.6 vs 2.3, P<0.001), self‐care (17.0 vs 20.8, P<0.001), communication (10.6 vs 11.5, P<0.001), and social cognition (15.1 vs 16.6, P<0.001).
| Bivariable Analysisb | Multivariable Analysisb | |||||
|---|---|---|---|---|---|---|
| Characteristic | All Patients, N=9405 | Readmitted, n=1,182 | OR (95% CI) | P Value | OR (95% CI) | P Value |
| ||||||
| Age, y | 68.0 (14.2) | 66.4 (14.5) | 0.9 (0.91.0) | <0.001 | 0.9 (0.91.0) | <0.001 |
| Male | 3,431 (42%) | 637 (54%) | 1.6 (1.41.8) | <0.001 | 1.3 (1.11.5) | < 0.001 |
| Race | ||||||
| Caucasian | 5,340 (65%) | 766 (65%) | 1.0 | 1.0 | ||
| African American | 2,177 (26%) | 324 (27%) | 1.0 (0.91.2) | 0.60 | 1.0 (0.81.1) | 0.75 |
| Other | 706 (9%) | 92 (8%) | 0.9 (0.71.1) | 0.41 | 0.8 (0.61.0) | 0.12 |
| Married | 3,775 (46%) | 555 (47%) | 1.0 (0.91.2) | 0.50 | 1.0 (0.91.2) | 0.67 |
| Admission diagnosis category | ||||||
| Neurologic | 3,205 (39%) | 501 (42%) | 1.0 | 1.0 | ||
| Medical | 1,726 (21%) | 409 (35%) | 1.5 (1.31.7) | <0.001 | 1.8 (1.62.1) | < 0.001 |
| Orthopedic | 3,292 (40%) | 272 (23%) | 0.5 (0.50.6) | <0.001 | 1.3 (1.11.6) | 0.005 |
| APDRG‐SOI expected readmission rate | 17.4 (7.1%) | 22.2 (8.0%) | 1.1 (1.11.1) | <0.001 | 1.1 (1.01.1) | < 0.001 |
| Total FIM score category | ||||||
| High FIM, >76 points | 3,517 (43%) | 257 (22%) | 1.0 | 1.0 | ||
| Middle FIM, 60points | 2,742 (33%) | 353 (30%) | 1.8 (1.52.1) | <0.001 | 1.5 (1.31.8) | < 0.001 |
| Low FIM, <60 points | 1,964 (24%) | 572 (48%) | 4.0 (3.44.7) | <0.001 | 3.0 (2.53.6) | < 0.001 |
Multivariable and Subset Analyses
Patients with a primary medical diagnosis had higher odds of readmission to the hospital, (OR: 1.8; 95% CI: 1.6‐2.1, P<0.001), relative to patients with a neurologic or orthopedic diagnosis (Table 2). Across all diagnoses, the adjusted odds ratios (95% CIs) for the low and middle versus high FIM score category were 3.0 (2.5‐3.6; P<0.001) and 1.5 (1.3‐1.8; P<0.001) respectively (Table 2). When modeled as a continuous variable, a 10‐point decrease in FIM score was associated with a significantly increased adjusted readmission rate (OR: 1.4; 95% CI: 1.3‐1.4; P<0.001). In adjusted analysis including all subscales of the FIM, only the physical subscales, transfers (P<0.001), locomotion (P=0.002), and self‐care (P<0.001), were significantly associated with readmission. For each diagnostic category, there were similar significant associations between admission FIM score group and readmission status (Table 3). The odds of readmission by FIM score did not differ significantly across the 3 major diagnostic categories (P=0.20 for interaction term), suggesting that the effect of functional status was similar across various types of patients. We also did not observe a statistical interaction between age and FIM score group in predicting readmission (P=0.58). Patients in the lowest FIM group with a medical diagnosis had the highest adjusted readmission rate of 28.7% (Table 3).
| Multivariable Analysisa | Adjusted Readmission Ratesb | |||
|---|---|---|---|---|
| No. | OR (95% CI) | P Value | % (95% CI) | |
| ||||
| Neurologic | ||||
| High FIM (>76 points) | 755 | 1.0 | 7.3 (4.710.0) | |
| Middle FIM (6076 points) | 1,283 | 1.4 (1.02.1) | 0.06 | 9.1 (7.011.1) |
| Low FIM (<60 points) | 1,668 | 3.3 (2.34.7) | <0.001 | 18.7 (16.820.6) |
| Medical | ||||
| High FIM (>76 points) | 807 | 1.0 | 11.2 (8.114.3) | |
| Middle FIM (6076 points) | 766 | 1.8 (1.32.4) | <0.001 | 17.7 (14.520.9) |
| Low FIM (<60 points) | 562 | 3.2 (2.44.3) | <0.001 | 28.7 (25.132.4) |
| Orthopedic | ||||
| High FIM (>76 points) | 2,212 | 1.0 | 6.1 (4.77.6) | |
| Middle FIM (6076 points) | 1,046 | 1.4 (1.11.9) | 0.02 | 8.3 (6.410.1) |
| Low FIM (<60 points) | 306 | 2.2 (1.53.3) | <0.001 | 13.5 (10.416.7) |
DISCUSSION
In this study of 9405 consecutive patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we investigated the association between functional status and readmission to an acute care hospital. We found that low functional status near the time of acute care hospital discharge was strongly associated with higher readmission rates. This relationship was consistently observed across major patient diagnostic categories, with low functioning medical patients having the highest rate of readmission (28.7%). Efforts to maintain or improve functional status during acute care hospitalization may be an important modifiable risk factor for acute care hospital readmission.
Previous studies have suggested that functional status may serve as an indicator of physiological reserve, and therefore vulnerability to medical complications and readmission.[6, 16, 23, 24, 25] Physiologic reserve refers to a person's ability to endure acute illness and is influenced by a number of factors, such as the adequacy of oxygen delivery to tissues, cardiovascular health, immune state, and nutritional status.[26] We found that motor subscales of the FIM score (transfers, locomotion, and self‐care), but not the other subscales, were independently associated with readmissions, which may suggest that lower motor scores are a stronger marker of physiologic reserve.[10, 16, 27] Although not our primary focus, we did note in our multivariable models that after adjusting for functional status, patients in a medical diagnostic category had higher readmission rates compared to patients with a primary neurologic or orthopedic diagnosis, but the impact of FIM score was consistent across all these diagnostic categories. We speculate that medical conditions that result in hospitalization, such as sepsis or acute kidney failure, may be more likely to result in multiorgan dysfunction that may impair physiological reserve and increase susceptibility to medical complications.[28, 29, 30, 31] In comparison, acute neurologic and orthopedic diagnoses, such as stroke or hip arthroplasty, directly impair gross motor function,[32, 33, 34, 35] with relative sparing of overall physiologic reserve.
The association between low functional status and readmissions is supported by previous studies across multiple hospital settings.[4, 5, 7, 8, 9, 27, 36] Despite this finding, routine inpatient medical practice may not fully address functional impairments. For instance, systematic measurement and documentation of functional status on admission and during hospitalization are not routine and may be a barrier to identifying medical patients at high risk for readmission.[37, 38, 39] Moreover, without recognition of functional impairment and its implications, current clinical practice may suboptimally prevent and treat physical impairments during inpatient care. However, such barriers can be surmounted. For example, in the medical intensive care unit setting, there is growing recognition that proactive and aggressive management of hospital‐acquired functional impairments through early rehabilitation is safe and feasible, improving patient outcomes while reducing hospital costs and readmissions.[3, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51] Moreover, 2 recent meta‐analyses have shown that physical therapy hospital‐based exercise programs can improve length of stay, overall hospital costs, and rates of discharge to home.[52, 53] Finally, a randomized trial has demonstrated that an individualized exercise regimen started in the acute hospital setting with long‐term telephone follow‐up can significantly reduce emergency hospital readmissions and improve quality of life in older adults.[54] Therefore, decreased functional status likely represents a modifiable risk factor for hospital readmission, and further research is necessary to more systematically identify low‐functioning patients and implement early mobility and activity programs to reduce hospital‐acquired functional impairment.[2, 49, 55]
Our analysis has potential limitations. First, this was an observational study and we are unable to demonstrate a direct cause‐and‐effect relationship between functional status and readmission. However, our results are consistent with prior literature in this field. Second, our cohort only included patients who were discharged from an acute hospital to a rehabilitation facility, which may limit its generalizability. However, we included a large patient sample size with a broad range of admission FIM scores, and our findings are consistent with other studies conducted in different clinical settings. Third, although 1 of our goals was to evaluate how readmission rates differed by diagnostic category, it is possible that individual diagnoses within each category may have different risks for readmission, and future larger studies could evaluate more detailed diagnostic grouping approaches. Fourth, we also recognize that although FIM score assessment has been validated, admission assessment occurs over a 72‐hour time period, during which patients' function could potentially change a clinically meaningful degree. Fifth, there may be residual confounding because of limitations in available data within our administrative dataset; however, we did account for severity of illness using a standardized measure, and prior research has demonstrated that the relationship between functional status and readmissions may be minimally confounded by demographic and clinical variables.[8, 16, 27, 56] Finally, we lacked readmission data following discharge from rehabilitation; it is possible that the association between FIM score at the time of rehabilitation initiation may have had limited predictive value among patients who successfully completed rehabilitation and were sent home.
CONCLUSION
In conclusion, in this study of patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we observed a strong association between decreased functional status and increased hospital readmission. In particular, medical patients with lower physical functioning exhibited an especially high rate of readmission. Incorporating functional status assessment into routine medical care may help identify patients at higher risk of readmission. Moreover, preventing and treating impaired functional status during inpatient admission, through early activity and mobility, should be evaluated as a way of improving patient outcomes and reducing hospital readmissions.
Disclosures: Erik Hoyer, MD, is supported by the Rehabilitation Medicine Scientist Training Program (RMSTP; 5K12HD001097). The authors report no conflicts of interest.
Federally mandated pay‐for‐performance initiatives promote minimizing 30‐day hospital readmissions to improve healthcare quality and reduce costs. Although the reasons for readmissions are multifactorial, many patients are readmitted for a condition other than their initial hospital admitting diagnosis.[1] Impairments in functional status experienced during acute care hospitalization contribute to patients being discharged in a debilitated state and being vulnerable to postdischarge complications and potentially hospital readmission.[2] As such, decreased functional status may be an important and potentially modifiable risk factor for acute care hospital readmission.[3]
Previous studies have suggested that impaired functional status may be an important predictor of rehospitalization.[4, 5, 6, 7] However, inferences from existing studies are limited because they did not consider functional status as their primary focus, they only considered specific patient populations (eg, stroke) or readmissions occurring well beyond the 30‐day period defined by federal pay‐for‐performance standards.[4, 5, 6, 8, 9, 10] Our objective was to evaluate the association between functional status near the time of discharge from acute care hospital and 30‐day readmission for patients admitted to an acute inpatient rehabilitation facility. As a secondary objective, we sought to investigate the relationship between functional status and readmission by diagnostic category (medical, neurologic, or orthopedic).
METHODS
Study Population and Setting
We conducted a single‐center, retrospective study of patients admitted to an inpatient rehabilitation facility at a community hospital between July 1, 2006 and December 31, 2012. This facility provides intensive rehabilitation consisting of 3 hours of therapy per day, skilled nursing care on a 24‐hour basis, and medical care by a physiatrist. We excluded patients who died during inpatient rehabilitation (n=15, 0.2%) and patients not admitted directly from an acute care setting (n=178, 2.0%).
Data Source and Covariates
Data were derived from the Uniform Data System for Medical Rehabilitation (UDSMR), which is an administrative database providing the following data upon admission to an inpatient rehabilitation facility[11, 12, 13]: age, gender, race/ethnicity, marital status, the discharge setting, the admission Functional Independence Measure (FIM) score (details further below), and admission diagnostic category as defined by the primary discharge diagnosis from the acute care hospital and grouped by functional related groups (a case‐mix system for medical rehabilitation).[12, 14] The 3M ClinTrac management software (3M, St. Paul, MN), used for mandatory reporting to the State of Maryland, provided all‐payerrefined diagnosis related group (APRDRG) and severity of illness (SOI) combinations (a tool to group patients into clinically comparable disease and severity‐of‐illness categories expected to use similar resources and experience similar outcomes). The University HealthSystem Consortium (UHC) database provided national readmission rates for all APRDRG‐SOI combinations using a methodology that has been previously described.[15, 16] Expected readmission rates for APRDRG‐SOI combinations served as a patient risk stratification tool based on clinical logic that evaluates age, comorbidities, principal diagnosis during hospitalization, and procedures conducted during hospitalization.[17]
Primary Outcome: Acute Care Readmission
The primary outcome was all‐cause acute care readmission, defined as patient transfer to an acute care hospital during inpatient rehabilitation within 30 days from admission to inpatient rehabilitation. The care model for our inpatient rehabilitation unit is such that when patients become sick or develop a complication, they are admitted directly to a clinical unit (eg, intensive care unit) at the community hospital through a rapid‐response intervention, or the physiatrist arranges with an admitting inpatient attending to accept the patient directly to his or her service.
Primary Exposure: Functional Independence Measure
Functional status was measured using the FIM score.[18] The FIM score is an 18‐item measure of functional status, with each item scored on a scale from 1 to 7 (dependent to independent). Various aspects of motor function and cognitive function are assessed. The FIM has been validated and shown to be reliable and reproducible.[13, 19, 20] By definition for the FIM instrument, admission FIM scores are assessed by trained multidisciplinary personnel first over the 72 hours of the rehabilitation stay, and for this study served as a proxy for patient functional status upon discharge from the acute care setting in our analysis. This 72‐hour time window allows for full assessment by therapists and nurses; however, in clinical practice at the inpatient rehabilitation unit involved in this study, much of the FIM assessment occurs within the first 24 hours of the rehabilitation stay. For our analysis, we divided FIM scores into low, medium, and high functional groups. The thresholds for these groups were based on total FIM score tertiles from a prior study<60, 60 to 76, and >76.[16] As a secondary analysis we created 6 subscales of the overall FIM score based on previous research. These subscales included: transfers (transfer to chair/wheelchair, toilet, and tub/shower), locomotion (walking and stairs), self‐care (eating, grooming, bathing, dressing, and toileting), sphincter control (bladder and bowel management), communication (comprehension and expression), and social cognition (social interaction, problem solving, and memory).[21]
Statistical Analysis
To evaluate differences in patient characteristics by diagnostic category, analysis of variance and 2 tests were used for continuous and dichotomous variables, respectively. Logistic regression was used to evaluate the association between FIM score category and readmission status, adjusting for potentially confounding variables available from the UDSMR and UHC databases. We used interaction terms to test whether the association between the FIM score and readmissions varied significantly across diagnostic categories and by age. As a secondary analysis, we modeled FIM score as a continuous variable. We expressed the odds ratio in this analysis per 10‐point change in FIM, because this represents a clinically relevant change in function.[22] Logistic regression was also used to evaluate the association between FIM subscale scores (transfers, locomotion, self‐care, sphincter control, communication, and social cognition) and readmission status. Statistical significance was defined as a 2‐sided P<0.05. Data were analyzed with R (version 2.15.0;
RESULTS
Readmitted Patients and Diagnostic Categories
A total of 9405 consecutive eligible patients were admitted to the acute inpatient rehabilitation facility between July 1, 2006 and December 31, 2012. A total of 1182 (13%) patients were readmitted back to an acute care hospital from inpatient rehabilitation. Median (interquartile range) time to readmission from acute care hospital discharge was 6 days (310 days), and median length of stay for patients who were discharged to the community from inpatient rehabilitation was 8 days (612 days).
Table 1 shows characteristics of all inpatient rehabilitation patients by diagnostic category. For the neurologic category, the most common primary diagnoses were stroke and spinal cord injury; for the medical category, infection, renal failure, congestive heart failure, and chronic obstructive pulmonary disease; and for the orthopedic category, spinal arthrodesis, knee and hip replacements. Mean FIM scores were lowest and highest for patients admitted with a primarily neurologic and orthopedic diagnosis, respectively.
| Characteristic | All Patients, N=9405 | Diagnostic Category | |||
|---|---|---|---|---|---|
| Neurologic, n=3706 | Medical, n=2135 | Orthopedic, n=3564 | P Valueb | ||
| |||||
| Age, y | 67.8 (14.2) | 66.7 (15.3) | 67.0 (14.9) | 69.3 (12.4) | <0.001 |
| Male | 4,068 (43%) | 1,816 (49%) | 1,119 (52%) | 1,133 (32%) | <0.001 |
| Race | <0.001 | ||||
| Caucasian | 6,106 (65%) | 2344 (63%) | 1,320 (62%) | 2,442 (69%) | |
| African American | 2,501 (27%) | 984 (27%) | 658 (31%) | 859 (24%) | |
| Other | 798 (8%) | 378 (10%) | 157 (7%) | 263 (7%) | |
| Married | 4,330 (46%) | 1,683 (45%) | 931 (44%) | 1,716 (48%) | 0.002 |
| APRDRG‐SOI expected readmission rate | 18.0 (7.4) | 20.5 (6.8) | 21.3 (7.5) | 13.5 (5.6) | <0.001 |
| Total admission FIM score | 68.7 (17.2) | 60.4 (18.6) | 69.1 (15.5) | 77.2 (11.7) | <0.001 |
FIM Score Category and Risk of Readmission
Figure 1 shows that patients in the low admission FIM score category had the highest unadjusted rate of readmission for each diagnostic category. In unadjusted analysis, Table 2 shows that younger age, male sex, APDRG‐SOI expected readmission rate, and orthopedic and medical diagnostic categories were associated with readmission. As a continuous variable, FIM scores were linearly associated with readmission (Figure 2), with an unadjusted odds ratio (OR) and 95% confidence interval (CI) of 1.4 (1.4‐1.4, P<0.001) for a 10‐point decrease in FIM. Compared to patients with high admission FIM scores, patients with low and middle FIM scores had higher unadjusted odds of readmission (OR: 4.0; 95% CI: 3.4‐4.7; P<0.001 and OR: 1.8; 95% CI: 1.5‐2.1; P<0.001, respectively). Mean FIM subscale scores for patients readmitted versus not readmitted were transfers (5.3 vs 7.0, P<0.001), locomotion (1.6 vs 2.3, P<0.001), self‐care (17.0 vs 20.8, P<0.001), communication (10.6 vs 11.5, P<0.001), and social cognition (15.1 vs 16.6, P<0.001).
| Bivariable Analysisb | Multivariable Analysisb | |||||
|---|---|---|---|---|---|---|
| Characteristic | All Patients, N=9405 | Readmitted, n=1,182 | OR (95% CI) | P Value | OR (95% CI) | P Value |
| ||||||
| Age, y | 68.0 (14.2) | 66.4 (14.5) | 0.9 (0.91.0) | <0.001 | 0.9 (0.91.0) | <0.001 |
| Male | 3,431 (42%) | 637 (54%) | 1.6 (1.41.8) | <0.001 | 1.3 (1.11.5) | < 0.001 |
| Race | ||||||
| Caucasian | 5,340 (65%) | 766 (65%) | 1.0 | 1.0 | ||
| African American | 2,177 (26%) | 324 (27%) | 1.0 (0.91.2) | 0.60 | 1.0 (0.81.1) | 0.75 |
| Other | 706 (9%) | 92 (8%) | 0.9 (0.71.1) | 0.41 | 0.8 (0.61.0) | 0.12 |
| Married | 3,775 (46%) | 555 (47%) | 1.0 (0.91.2) | 0.50 | 1.0 (0.91.2) | 0.67 |
| Admission diagnosis category | ||||||
| Neurologic | 3,205 (39%) | 501 (42%) | 1.0 | 1.0 | ||
| Medical | 1,726 (21%) | 409 (35%) | 1.5 (1.31.7) | <0.001 | 1.8 (1.62.1) | < 0.001 |
| Orthopedic | 3,292 (40%) | 272 (23%) | 0.5 (0.50.6) | <0.001 | 1.3 (1.11.6) | 0.005 |
| APDRG‐SOI expected readmission rate | 17.4 (7.1%) | 22.2 (8.0%) | 1.1 (1.11.1) | <0.001 | 1.1 (1.01.1) | < 0.001 |
| Total FIM score category | ||||||
| High FIM, >76 points | 3,517 (43%) | 257 (22%) | 1.0 | 1.0 | ||
| Middle FIM, 60points | 2,742 (33%) | 353 (30%) | 1.8 (1.52.1) | <0.001 | 1.5 (1.31.8) | < 0.001 |
| Low FIM, <60 points | 1,964 (24%) | 572 (48%) | 4.0 (3.44.7) | <0.001 | 3.0 (2.53.6) | < 0.001 |
Multivariable and Subset Analyses
Patients with a primary medical diagnosis had higher odds of readmission to the hospital, (OR: 1.8; 95% CI: 1.6‐2.1, P<0.001), relative to patients with a neurologic or orthopedic diagnosis (Table 2). Across all diagnoses, the adjusted odds ratios (95% CIs) for the low and middle versus high FIM score category were 3.0 (2.5‐3.6; P<0.001) and 1.5 (1.3‐1.8; P<0.001) respectively (Table 2). When modeled as a continuous variable, a 10‐point decrease in FIM score was associated with a significantly increased adjusted readmission rate (OR: 1.4; 95% CI: 1.3‐1.4; P<0.001). In adjusted analysis including all subscales of the FIM, only the physical subscales, transfers (P<0.001), locomotion (P=0.002), and self‐care (P<0.001), were significantly associated with readmission. For each diagnostic category, there were similar significant associations between admission FIM score group and readmission status (Table 3). The odds of readmission by FIM score did not differ significantly across the 3 major diagnostic categories (P=0.20 for interaction term), suggesting that the effect of functional status was similar across various types of patients. We also did not observe a statistical interaction between age and FIM score group in predicting readmission (P=0.58). Patients in the lowest FIM group with a medical diagnosis had the highest adjusted readmission rate of 28.7% (Table 3).
| Multivariable Analysisa | Adjusted Readmission Ratesb | |||
|---|---|---|---|---|
| No. | OR (95% CI) | P Value | % (95% CI) | |
| ||||
| Neurologic | ||||
| High FIM (>76 points) | 755 | 1.0 | 7.3 (4.710.0) | |
| Middle FIM (6076 points) | 1,283 | 1.4 (1.02.1) | 0.06 | 9.1 (7.011.1) |
| Low FIM (<60 points) | 1,668 | 3.3 (2.34.7) | <0.001 | 18.7 (16.820.6) |
| Medical | ||||
| High FIM (>76 points) | 807 | 1.0 | 11.2 (8.114.3) | |
| Middle FIM (6076 points) | 766 | 1.8 (1.32.4) | <0.001 | 17.7 (14.520.9) |
| Low FIM (<60 points) | 562 | 3.2 (2.44.3) | <0.001 | 28.7 (25.132.4) |
| Orthopedic | ||||
| High FIM (>76 points) | 2,212 | 1.0 | 6.1 (4.77.6) | |
| Middle FIM (6076 points) | 1,046 | 1.4 (1.11.9) | 0.02 | 8.3 (6.410.1) |
| Low FIM (<60 points) | 306 | 2.2 (1.53.3) | <0.001 | 13.5 (10.416.7) |
DISCUSSION
In this study of 9405 consecutive patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we investigated the association between functional status and readmission to an acute care hospital. We found that low functional status near the time of acute care hospital discharge was strongly associated with higher readmission rates. This relationship was consistently observed across major patient diagnostic categories, with low functioning medical patients having the highest rate of readmission (28.7%). Efforts to maintain or improve functional status during acute care hospitalization may be an important modifiable risk factor for acute care hospital readmission.
Previous studies have suggested that functional status may serve as an indicator of physiological reserve, and therefore vulnerability to medical complications and readmission.[6, 16, 23, 24, 25] Physiologic reserve refers to a person's ability to endure acute illness and is influenced by a number of factors, such as the adequacy of oxygen delivery to tissues, cardiovascular health, immune state, and nutritional status.[26] We found that motor subscales of the FIM score (transfers, locomotion, and self‐care), but not the other subscales, were independently associated with readmissions, which may suggest that lower motor scores are a stronger marker of physiologic reserve.[10, 16, 27] Although not our primary focus, we did note in our multivariable models that after adjusting for functional status, patients in a medical diagnostic category had higher readmission rates compared to patients with a primary neurologic or orthopedic diagnosis, but the impact of FIM score was consistent across all these diagnostic categories. We speculate that medical conditions that result in hospitalization, such as sepsis or acute kidney failure, may be more likely to result in multiorgan dysfunction that may impair physiological reserve and increase susceptibility to medical complications.[28, 29, 30, 31] In comparison, acute neurologic and orthopedic diagnoses, such as stroke or hip arthroplasty, directly impair gross motor function,[32, 33, 34, 35] with relative sparing of overall physiologic reserve.
The association between low functional status and readmissions is supported by previous studies across multiple hospital settings.[4, 5, 7, 8, 9, 27, 36] Despite this finding, routine inpatient medical practice may not fully address functional impairments. For instance, systematic measurement and documentation of functional status on admission and during hospitalization are not routine and may be a barrier to identifying medical patients at high risk for readmission.[37, 38, 39] Moreover, without recognition of functional impairment and its implications, current clinical practice may suboptimally prevent and treat physical impairments during inpatient care. However, such barriers can be surmounted. For example, in the medical intensive care unit setting, there is growing recognition that proactive and aggressive management of hospital‐acquired functional impairments through early rehabilitation is safe and feasible, improving patient outcomes while reducing hospital costs and readmissions.[3, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51] Moreover, 2 recent meta‐analyses have shown that physical therapy hospital‐based exercise programs can improve length of stay, overall hospital costs, and rates of discharge to home.[52, 53] Finally, a randomized trial has demonstrated that an individualized exercise regimen started in the acute hospital setting with long‐term telephone follow‐up can significantly reduce emergency hospital readmissions and improve quality of life in older adults.[54] Therefore, decreased functional status likely represents a modifiable risk factor for hospital readmission, and further research is necessary to more systematically identify low‐functioning patients and implement early mobility and activity programs to reduce hospital‐acquired functional impairment.[2, 49, 55]
Our analysis has potential limitations. First, this was an observational study and we are unable to demonstrate a direct cause‐and‐effect relationship between functional status and readmission. However, our results are consistent with prior literature in this field. Second, our cohort only included patients who were discharged from an acute hospital to a rehabilitation facility, which may limit its generalizability. However, we included a large patient sample size with a broad range of admission FIM scores, and our findings are consistent with other studies conducted in different clinical settings. Third, although 1 of our goals was to evaluate how readmission rates differed by diagnostic category, it is possible that individual diagnoses within each category may have different risks for readmission, and future larger studies could evaluate more detailed diagnostic grouping approaches. Fourth, we also recognize that although FIM score assessment has been validated, admission assessment occurs over a 72‐hour time period, during which patients' function could potentially change a clinically meaningful degree. Fifth, there may be residual confounding because of limitations in available data within our administrative dataset; however, we did account for severity of illness using a standardized measure, and prior research has demonstrated that the relationship between functional status and readmissions may be minimally confounded by demographic and clinical variables.[8, 16, 27, 56] Finally, we lacked readmission data following discharge from rehabilitation; it is possible that the association between FIM score at the time of rehabilitation initiation may have had limited predictive value among patients who successfully completed rehabilitation and were sent home.
CONCLUSION
In conclusion, in this study of patients admitted from acute care hospitals to a single inpatient rehabilitation facility, we observed a strong association between decreased functional status and increased hospital readmission. In particular, medical patients with lower physical functioning exhibited an especially high rate of readmission. Incorporating functional status assessment into routine medical care may help identify patients at higher risk of readmission. Moreover, preventing and treating impaired functional status during inpatient admission, through early activity and mobility, should be evaluated as a way of improving patient outcomes and reducing hospital readmissions.
Disclosures: Erik Hoyer, MD, is supported by the Rehabilitation Medicine Scientist Training Program (RMSTP; 5K12HD001097). The authors report no conflicts of interest.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- . Post‐hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102.
- , , , et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341(5):373–377.
- , . Association of physical functioning with same‐hospital readmission after stroke. Am J Phys Med Rehabil. 2004;83(6):434–438.
- , , , . Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39(5):1449–1465.
- , , , , , . Risk factors for nonelective hospital readmissions. J Gen Intern Med. 1996;11(12):762–764.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , et al. Hospital readmission in persons with stroke following postacute inpatient rehabilitation. J Gerontol A Biol Sci Med Sci. 2012;67(8):875–881.
- , , , , , . Hospital readmission of persons with hip fracture following medical rehabilitation. Arch Gerontol Geriatr. 2003;36(1):15–22.
- , , , , , . Characteristics of persons rehospitalized after stroke rehabilitation. Arch Phys Med Rehabil. 2001;82(10):1367–1374.
- , , , et al. A classification system for inpatient rehabilitation patients: a review and proposed revisions to the functional independence measure‐function related groups. PB98–105992, September. Washington, DC: US Department of Commerce, National Technical Information Services; 1997.
- , , , , , . A case‐mix classification system for medical rehabilitation. Med Care. 1994;32(4):366–379.
- , , , . The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232.
- , , , , , . Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil. 1994;75(12):1277–1283.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA Intern Med. 2013;173(8):624–629.
- , , , , , . Functional status impairment is associated with unplanned readmissions. Arch Phys Med Rehabil. 2013;94(10):1951–1958.
- , , , et al. All patient refined diagnosis related groups (APR‐DRGs). Version 15.0. Report No.: 98‐054 Rev. 00. Wallingford, CT: 3M Health Information Systems; 1998.
- The inpatient rehabilitation facility–patient assessment instrument (IRF‐PAI) training manual. 2012. http://www.cms.gov/.
- , , , et al. Relationships between disability measures and nursing effort during medical rehabilitation for patients with traumatic brain and spinal cord injury. Arch Phys Med Rehabil. 1997;78(2):143–149.
- , , , . Interrater reliability of the 7‐level functional independence measure (FIM). Scand J Rehabil Med. 1994;26(3):115–119.
- , , , , , . Comparison of logistic regression and neural networks to predict rehospitalization in patients with stroke. J Clin Epidemiol. 2001;54(11):1159–1165.
- , , . Comparison of the responsiveness of the Barthel Index and the motor component of the Functional Independence Measure in stroke: the impact of using different methods for measuring responsiveness. J Clin Epidemiol. 2002;55(9):922–928.
- , . Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33(6):1560–1566.
- , , . Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298.
- , . Hospital readmission as an accountability measure. JAMA. 2011;305(5):504–505.
- . Susceptibility to critical illness: reserve, response and therapy. Intensive Care Med. 2000;26(suppl 1):S57–S63.
- , , , , . Predictors of discharge to acute care after inpatient rehabilitation in severely affected stroke patients. Am J Phys Med Rehabil. 2012;91(5):387–392.
- , , , et al. Clinical characteristics and outcomes of sepsis‐related vs non‐sepsis‐related ARDS. Chest. 2010;138(3):559–567.
- , . Long‐term outcomes from sepsis. Curr Infect Dis Rep. 2007;9(5):382–386.
- , . Heart failure performance measures and outcomes: real or illusory gains. JAMA. 2009;302(7):792–794.
- , , , , . Patients' self‐assessed functional status in heart failure by new york heart association class: a prognostic predictor of hospitalizations, quality of life and death. J Card Fail. 2010;16(2):150–156.
- , , , et al. Knee arthroplasty: disabilities in comparison to the general population and to hip arthroplasty using a French national longitudinal survey. PLoS One. 2008;3(7):e2561.
- , , , et al. Gait asymmetry in community‐ambulating stroke survivors. Arch Phys Med Rehabil. 2008;89(2):304–310.
- , , , . Recovery of upper extremity function in stroke patients: The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1994;75(4):394–398.
- , , , , , . The effect of admission physiological variables on 30 day outcome after stroke. J Clin Neurosci. 2005;12(8):905–910.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- . Can hospitalization‐associated disability be prevented? JAMA. 2011;306(16):1800–1801.
- , , . Hospitalization‐associated disability: “she was probably able to ambulate, but I'm not sure.” JAMA. 2011;306(16):1782–1793.
- , , , , , . Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193.
- . Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300(14):1685–1690.
- , , . Technology to enhance physical rehabilitation of critically ill patients. Crit Care Med. 2009;37(10 suppl):S436–S441.
- , , , et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542.
- , , , et al. ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med. 2013;41(3):717–724.
- , , , et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882.
- , , , et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243.
- , , , et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(1):139–145.
- , . Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 2010;17(4):271–281.
- , , , , . Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59(2):359–365.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304.
- , , , et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25(2):254–262.
- , , . Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;(1):CD005955.
- , , . Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil. 2011;92(9):1490–1500.
- , , , , , . Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24‐week exercise and telephone follow‐up program. J Am Geriatr Soc. 2009;57(3):395–402.
- , , , , , . Effects of an acute care for elders unit on costs and 30‐day readmissions. JAMA Intern Med. 2013:1–7.
- , , , , . Risks of acute hospital transfer and mortality during stroke rehabilitation. Arch Phys Med Rehabil. 2003;84(5):712–718.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- . Post‐hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102.
- , , , et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341(5):373–377.
- , . Association of physical functioning with same‐hospital readmission after stroke. Am J Phys Med Rehabil. 2004;83(6):434–438.
- , , , . Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39(5):1449–1465.
- , , , , , . Risk factors for nonelective hospital readmissions. J Gen Intern Med. 1996;11(12):762–764.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698.
- , , , et al. Hospital readmission in persons with stroke following postacute inpatient rehabilitation. J Gerontol A Biol Sci Med Sci. 2012;67(8):875–881.
- , , , , , . Hospital readmission of persons with hip fracture following medical rehabilitation. Arch Gerontol Geriatr. 2003;36(1):15–22.
- , , , , , . Characteristics of persons rehospitalized after stroke rehabilitation. Arch Phys Med Rehabil. 2001;82(10):1367–1374.
- , , , et al. A classification system for inpatient rehabilitation patients: a review and proposed revisions to the functional independence measure‐function related groups. PB98–105992, September. Washington, DC: US Department of Commerce, National Technical Information Services; 1997.
- , , , , , . A case‐mix classification system for medical rehabilitation. Med Care. 1994;32(4):366–379.
- , , , . The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232.
- , , , , , . Four methods for characterizing disability in the formation of function related groups. Arch Phys Med Rehabil. 1994;75(12):1277–1283.
- , , , et al. Association of self‐reported hospital discharge handoffs with 30‐day readmissions. JAMA Intern Med. 2013;173(8):624–629.
- , , , , , . Functional status impairment is associated with unplanned readmissions. Arch Phys Med Rehabil. 2013;94(10):1951–1958.
- , , , et al. All patient refined diagnosis related groups (APR‐DRGs). Version 15.0. Report No.: 98‐054 Rev. 00. Wallingford, CT: 3M Health Information Systems; 1998.
- The inpatient rehabilitation facility–patient assessment instrument (IRF‐PAI) training manual. 2012. http://www.cms.gov/.
- , , , et al. Relationships between disability measures and nursing effort during medical rehabilitation for patients with traumatic brain and spinal cord injury. Arch Phys Med Rehabil. 1997;78(2):143–149.
- , , , . Interrater reliability of the 7‐level functional independence measure (FIM). Scand J Rehabil Med. 1994;26(3):115–119.
- , , , , , . Comparison of logistic regression and neural networks to predict rehospitalization in patients with stroke. J Clin Epidemiol. 2001;54(11):1159–1165.
- , , . Comparison of the responsiveness of the Barthel Index and the motor component of the Functional Independence Measure in stroke: the impact of using different methods for measuring responsiveness. J Clin Epidemiol. 2002;55(9):922–928.
- , . Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33(6):1560–1566.
- , , . Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298.
- , . Hospital readmission as an accountability measure. JAMA. 2011;305(5):504–505.
- . Susceptibility to critical illness: reserve, response and therapy. Intensive Care Med. 2000;26(suppl 1):S57–S63.
- , , , , . Predictors of discharge to acute care after inpatient rehabilitation in severely affected stroke patients. Am J Phys Med Rehabil. 2012;91(5):387–392.
- , , , et al. Clinical characteristics and outcomes of sepsis‐related vs non‐sepsis‐related ARDS. Chest. 2010;138(3):559–567.
- , . Long‐term outcomes from sepsis. Curr Infect Dis Rep. 2007;9(5):382–386.
- , . Heart failure performance measures and outcomes: real or illusory gains. JAMA. 2009;302(7):792–794.
- , , , , . Patients' self‐assessed functional status in heart failure by new york heart association class: a prognostic predictor of hospitalizations, quality of life and death. J Card Fail. 2010;16(2):150–156.
- , , , et al. Knee arthroplasty: disabilities in comparison to the general population and to hip arthroplasty using a French national longitudinal survey. PLoS One. 2008;3(7):e2561.
- , , , et al. Gait asymmetry in community‐ambulating stroke survivors. Arch Phys Med Rehabil. 2008;89(2):304–310.
- , , , . Recovery of upper extremity function in stroke patients: The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1994;75(4):394–398.
- , , , , , . The effect of admission physiological variables on 30 day outcome after stroke. J Clin Neurosci. 2005;12(8):905–910.
- , , , et al. Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med. 2011;5(2):e104–e111.
- . Can hospitalization‐associated disability be prevented? JAMA. 2011;306(16):1800–1801.
- , , . Hospitalization‐associated disability: “she was probably able to ambulate, but I'm not sure.” JAMA. 2011;306(16):1782–1793.
- , , , , , . Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193.
- . Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300(14):1685–1690.
- , , . Technology to enhance physical rehabilitation of critically ill patients. Crit Care Med. 2009;37(10 suppl):S436–S441.
- , , , et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542.
- , , , et al. ICU early physical rehabilitation programs: financial modeling of cost savings. Crit Care Med. 2013;41(3):717–724.
- , , , et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882.
- , , , et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243.
- , , , et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(1):139–145.
- , . Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 2010;17(4):271–281.
- , , , , . Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59(2):359–365.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304.
- , , , et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25(2):254–262.
- , , . Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;(1):CD005955.
- , , . Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med Rehabil. 2011;92(9):1490–1500.
- , , , , , . Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24‐week exercise and telephone follow‐up program. J Am Geriatr Soc. 2009;57(3):395–402.
- , , , , , . Effects of an acute care for elders unit on costs and 30‐day readmissions. JAMA Intern Med. 2013:1–7.
- , , , , . Risks of acute hospital transfer and mortality during stroke rehabilitation. Arch Phys Med Rehabil. 2003;84(5):712–718.
© 2014 Society of Hospital Medicine
Predicting Safe Physician Workloads
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
Attending physician workload may be compromising patient safety and quality of care. Recent studies show hospitalists, intensivists, and surgeons report that excessive attending physician workload has a negative impact on patient care.[1, 2, 3] Because physician teams and hospitals differ in composition, function, and setting, it is difficult to directly compare one service to another within or between institutions. Identifying physician, team, and hospital characteristics associated with clinicians' impressions of unsafe workload provides physician leaders, hospital administrators, and policymakers with potential risk factors and specific targets for interventions.[4] In this study, we use a national survey of hospitalists to identify the physician, team, and hospital factors associated with physician report of an unsafe workload.
METHODS
We electronically surveyed 890 self‐identified hospitalists enrolled in
RESULTS
Of the 890 physicians contacted, 506 (57%) responded. Full characteristics of respondents are reported elsewhere.[1] Forty percent of physicians (n=202) indicated that their typical inpatient census exceeded safe levels at least monthly. A descriptive comparison of the lower and higher reporters of unsafe levels is provided (Table 1). Higher frequency of reporting an unsafe census was associated with higher percentages of clinical (P=0.004) and inpatient responsibilities (P<0.001) and more time seeing patients without midlevel or housestaff assistance (P=0.001) (Table 1). On the other hand, lower reported unsafe census was associated with more years in practice (P=0.02), greater percentage of personal time (P=0.02), and the presence of any system for census control (patient caps, fixed bed capacity, staffing augmentation plans) (P=0.007) (Table 1). Fixed census caps decreased the odds of reporting an unsafe census by 34% and was the only statistically significant workload control mechanism (odds ratio: 0.66; 95% confidence interval: 0.43‐0.99; P=0.04). There was no association between reported unsafe census and physician age (P=0.42), practice area (P=0.63), organization type (P=0.98), or compensation (salary [P=0.23], bonus [P=0.61], or total [P=0.54]).
| Characteristic | Report of Unsafe Workloada | Univariate Odds Ratio (95% CI) | Reported Effect on Unsafe Workload Frequency | |
|---|---|---|---|---|
| Lower | Higher | |||
| ||||
| Percentage of total work hours devoted to patient care, median [IQR] | 95 [80100] | 100 [90100] | 1.13b (1.041.23)c | Increased |
| Percentage of clinical care that is inpatient, median [IQR] | 75 [5085] | 80 [7090] | 1.21b (1.131.34)d | |
| Percentage of clinical work performed with no assistance from housestaff or midlevels, median [IQR] | 80 [25100] | 90 [50100] | 1.08b (1.031.14)c | |
| Years in practice, median [IQR] | 6 [311] | 5 [310] | 0.85e (0.750.98)f | Decreased |
| Percentage of workday allotted for personal time, median [IQR] | 5 [07] | 3 [05] | 0.50b (0.380.92)f | |
| Systems for increased patient volume, No. (%) | ||||
| Fixed census cap | 87 (30) | 45 (22) | 0.66 (0.430.99)f | |
| Fixed bed capacity | 36 (13) | 24 (12) | 0.94 (0.541.63) | |
| Staffing augmentation | 88 (31) | 58 (29) | 0.91 (0.611.35) | |
| Any system | 217 (76) | 130 (64) | 0.58 (0.390.86)g | |
| Primary practice area of hospital medicine, No. (%) | ||||
| Adult | 211 (73) | 173 (86) | 1 | Equivocal |
| Pediatric | 7 (2) | 1 (0.5) | 0.24 (0.032.10) | |
| Combined, adult and pediatric | 5 (2) | 3 (1) | 0.73 (0.173.10) | |
| Primary role, No. (%) | ||||
| Clinical | 242 (83) | 186 (92) | 1 | |
| Research | 5 (2) | 4 (2) | 1.04 (0.283.93) | |
| Administrative | 14 (5) | 6 (3) | 0.56 (0.211.48) | |
| Physician age, median [IQR], y | 36 [3242] | 37 [3342] | 0.96e (0.861.07) | |
| Compensation, median [IQR], thousands of dollars | ||||
| Salary only | 180 [130200] | 180 [150200] | 0.97h (0.981.05) | |
| Incentive pay only | 10 [025] | 10 [020] | 0.99h (0.941.04) | |
| Total | 190 [140220] | 196 [165220] | 0.99h (0.981.03) | |
| Practice area, No. (%) | ||||
| Urban | 128 (45) | 98 (49) | 1 | |
| Suburban | 126 (44) | 81 (41) | 0.84 (0.571.23) | |
| Rural | 33 (11) | 21 (10) | 0.83 (0.451.53) | |
| Practice location, No. (%) | ||||
| Academic | 82 (29) | 54 (27) | 1 | |
| Community | 153 (53) | 110 (55) | 1.09 (0.721.66) | |
| Veterans hospital | 7 (2) | 4 (2) | 0.87 (0.243.10) | |
| Group | 32 (11) | 25 (13) | 1.19 (0.632.21) | |
| Physician group size, median [IQR] | 12 [620] | 12 [822] | 0.99i (0.981.03) | |
| Localization of patients, No. (%) | ||||
| Multiple units | 179 (61) | 124 (61) | 1 | |
| Single or adjacent unit(s) | 87 (30) | 58 (29) | 0.96 (0.641.44) | |
| Multiple hospitals | 25 (9) | 20 (10) | 1.15 (0.612.17) | |
DISCUSSION
This is the first study to our knowledge to describe factors associated with provider reports of unsafe workload and identifies potential targets for intervention. By identifying modifiable factors affecting workload, such as different team structures with housestaff or midlevels, it may be possible to improve workload, efficiency, and perhaps safety.[5, 6] Less experience, decreased housestaff or midlevel assistance, higher percentages of inpatient and clinical responsibilities, and lack of systems for census control were strongly associated with reports of unsafe workload.
Having any system in place to address increased patient volumes reduced the odds of reporting an unsafe workload. However, only fixed patient census caps were statistically significant. A system that incorporates fixed service or admitting caps may provide greater control on workload but may also result in back‐ups and delays in the emergency room. Similarly, fixed caps may require overflow of patients to less experienced or willing services or increase the number of handoffs, which may adversely affect the quality of patient care. Use of separate admitting teams has the potential to increase efficiency, but is also subject to fluctuations in patient volume and increases the number of handoffs. Each institution should use a multidisciplinary systems approach to address patient throughput and enforce manageable workload such as through the creation of patient flow teams.[7]
Limitations of the study include the relatively small sample of hospitalists and self‐reporting of safety. Because of the diverse characteristics and structures of the individual programs, even if a predictor variable was not missing, if a particular value for that predictor occurred very infrequently, it generated very wide effect estimates. This limited our ability to effectively explore potential confounders and interactions. To our knowledge, this study is the first to explore potential predictors of unsafe attending physician workload. Large national surveys of physicians with greater statistical power can expand upon this initial work and further explore the association between, and interaction of, workload factors and varying perceptions of providers.[4] The most important limitation of this work is that we relied on self‐reporting to define a safe census. We do not have any measured clinical outcomes that can serve to validate the self‐reported impressions. We recognize, however, that adverse events in healthcare require multiple weaknesses to align, and typically, multiple barriers exist to prevent such events. This often makes it difficult to show direct causal links. Additionally, self‐reporting of safety may also be subject to recall bias, because adverse patient outcomes are often particularly memorable. However, high‐reliability organizations recognize the importance of front‐line provider input, such as on the sensitivity of operations (working conditions) and by deferring to expertise (insights and recommendations from providers most knowledgeable of conditions, regardless of seniority).[8]
We acknowledge that several workload factors, such as hospital setting, may not be readily modifiable. However, we also report factors that can be intervened upon, such as assistance[5, 6] or geographic localization of patients.[9, 10] An understanding of both modifiable and fixed factors in healthcare delivery is essential for improving patient care.
This study has significant research implications. It suggests that team structure and physician experience may be used to improve workload safety. Also, particularly if these self‐reported findings are verified using clinical outcomes, providing hospitalists with greater staffing assistance and systems responsive to census fluctuations may improve the safety, quality, and flow of patient care. Future research may identify the association of physician, team, and hospital factors with outcomes and objectively assess targeted interventions to improve both the efficiency and quality of care.
Acknowledgments
The authors thank the Johns Hopkins Clinical Research Network Hospitalists, General Internal Medicine Research in Progress Physicians, and Hospitalist Directors for the Maryland/District of Columbia region for sharing their models of care and comments on the survey content. They also thank Michael Paskavitz, BA (Editor‐in‐Chief) and Brian Driscoll, BA (Managing Editor) from Quantia Communications for all of their technical assistance in administering the survey.
Disclosures: Drs. Michtalik and Brotman had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Michtalik, Pronovost, Brotman. Analysis, interpretation of data: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Drafting of the manuscript: Michtalik, Brotman. Critical revision of the manuscript for important intellectual content: Michtalik, Pronovost, Marsteller, Spetz, Brotman. Dr. Brotman has received compensation from Quantia Communications, not exceeding $10,000 annually, for developing educational content. Dr. Michtalik was supported by NIH grant T32 HP10025‐17‐00 and NIH/Johns Hopkins Institute for Clinical and Translational Research KL2 Award 5KL2RR025006. The Johns Hopkins Hospitalist Scholars Fund provided funding for survey implementation and data acquisition by Quantia Communications. The funders had no role in the design, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The authors report no conflicts of interest.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , . Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- , , , et al. Does surgeon workload per day affect outcomes after pulmonary lobectomies? Ann Thorac Surg. 2012;94(3):966–972.
- , , , . Perceived effects of attending physician workload in academic medical intensive care units: a national survey of training program directors. Crit Care Med. 2012;40(2):400–405.
- , , , , . Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026–1028.
- , , , et al. A comparison of outcomes of general medical inpatient care provided by a hospitalist‐physician assistant model vs a traditional resident‐based model. J Hosp Med. 2011;6(3):122–130.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- , , , . Improving patient flow and reducing emergency department crowding: a guide for hospitals. AHRQ publication no. 11(12)−0094. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- , , , et al. Becoming a high reliability organization: operational advice for hospital leaders. AHRQ publication no. 08–0022. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
Review of VTE Prophylaxis Strategies
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), is estimated to affect 900,000 Americans each year and is a cause of significant morbidity and mortality with associated high healthcare costs.[1] Accordingly, the comparative effectiveness and safety of interventions for the prevention and treatment of VTE are among the national priorities for comparative effectiveness research.[2] Whereas we have evidence‐based guidelines for the prophylaxis of VTE in the general population, there are no guidelines informing the care of select patient populations. Select populations are those patients in whom there is decisional uncertainty about the optimal choice, timing, and dose of VTE prophylaxis. Not only do these patients have an increased risk of DVT and PE, but most are also at high risk of bleeding, the most important complication of VTE prophylaxis.[3, 4, 5, 6]
The objectives of this systematic review were to define the comparative effectiveness and safety of pharmacologic and mechanical strategies for VTE prevention in some of these select medical populations including obese patients, patients on concomitant antiplatelet therapy, patients with renal insufficiency, patients who are underweight, and patients with coagulopathy due to liver disease.
METHODS
The methods for this comparative effectiveness review (CER) follow the guidelines suggested in the Agency for Healthcare Research and Quality (AHRQ) Methods Guide for Effectiveness and Comparative Effectiveness Reviews.[7] The protocol was publically posted.[8]
Search Strategy
We searched MEDLINE, EMBASE, and SCOPUS through August 2011, CINAHL, International Pharmaceutical Abstracts,
Study Selection
We reviewed titles followed by abstracts to identify randomized controlled trials (RCTs) or observational studies with comparison groups reporting on the effectiveness or safety of VTE prevention in our populations. Two investigators independently reviewed abstracts, and we excluded the abstracts if both investigators agreed that the article met 1 or more of the exclusion criteria. We included only English‐language articles that evaluated the effectiveness of pharmacological or mechanical interventions that have been approved for clinical use in the United States. To be eligible, the studies must have addressed relevant key questions in the population of our interest. We resolved disagreements by consensus. We used DistillerSR (Evidence Partners Inc., Ottawa, Ontario, Canada), a Web‐based database management program to manage the review process. Two investigators assessed the risk of bias in each study independently, using the Downs and Black instrument for observational studies and trials.[10]
Data Synthesis
For each select population, we created detailed evidence tables containing the information abstracted from the eligible studies. After synthesizing the evidence, we graded the quantity, quality, and consistency of the best available evidence for each select population by adapting an evidence‐grading scheme recommended in the Methods Guide for Conducting Comparative Effectiveness Reviews.[7]
RESULTS
We identified 30,902 unique citations and included 9 studies (Figure 1). There were 5 RCTs with relevant subgroups and 4 observational studies (Table 1). Two studies reported on the risk of bleeding in patients given pharmacologic prophylaxis while they are concomitantly taking nonsteroidal anti‐inflammatory drugs (NSAIDS) or antiplatelet agents/aspirin, 1 RCT and 1 prospective observational study reported on obese patients, and 5 studies described outcomes of patients with renal insufficiency (see Supporting Information, Table 1, in the online version of this article). No study tested prophylaxis in underweight patients or those with liver disease.

| Study | Arm, n | Total VTE (DVT and PE) | Bleeding | Other Outcomes | |
|---|---|---|---|---|---|
| |||||
| Obese patients | |||||
| Kucher et al., 2005[11] | Arm 1 (dalteparin), 558 | 2.8% (95% CI: 1.34.3) | 0% | Mortality at 21 days: 4.6% | |
| Arm 2 (placebo), 560 | 4.3% (95% CI: 2.56.2) | 0.7% | Mortality at 21 days: 2.7% | ||
| Freeman et al., [12] | Arm 1 (fixed‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 19 % | |
| Arm 2 (lower‐dose enoxaparin), 9 | NR | NR | Peak anti‐factor Xa level 32 % | ||
| Arm 3 (higher‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 86 % | ||
| Patients on antiplatelet agents | |||||
| Eriksson et al., 2012[14] | Arm 1 (rivaroxaban), 563 | NR | 20 (3.6%), rate ratio for use vs nonuse: 1.32 (95% CI: 0.85‐2.05) | NR | |
| Arm 2 (enoxaparin/placebo), 526 | NR | 17 (3.2%), rate ratio for use vs nonuse: 1.40 (95% CI: 0.87‐2.25) | NR | ||
| Friedman et al., 2012[15] | Arm 2 (150 mg dabigatran, no ASA), 1149 | NR | 11 (1.0%)a | NR | |
| Arm 5 (150 mg dabigatran+ASA), 128 | NR | 2 (1.6%)a | NR | ||
| Arm 3 (enoxaparin, no ASA), 1167 | NR | 14 (1.2%)a | NR | ||
| Arm 6 (enoxaparin+ASA), 132 | NR | 4 (3.0%) | NR | ||
| 150 mg dabigatran compared with enoxaparinNo concomitant ASA therapy | NR | RR: 0.82 (95% CI: 0.37‐1.84) | NR | ||
| 150 mg dabigatran compared with enoxaparinWith concomitant ASA therapy | NR | RR: 0.55 (95% CI: 0.11‐2.78) | NR | ||
| Patients with renal insufficiency | |||||
| Bauersachs et al., 2011[16] | Arm 2 (GFR <30), 92 | Total DVT: 11.11%; Total PE: 0% | Major bleeding: 4/92 (4.35%), minor bleeding: 9/92 (9.78%) | Mortality: 5.81% | |
| Mah et al., 2007[17] | Arm 2 (tinzaparin), 27 | NR | Major bleeding: 2/27 (7.4%), minor bleeding: 3/27 (11.1%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.05 | |
| Arm 3 (enoxaparin), 28 | NR | Major bleeding: 1/28 (3.6%), minor bleeding: 3/28 (10.7%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.22 | ||
| Dahl et al., 2012[18] | Arm 1 (enoxaparin), 332 | Major VTE: 8 (9.0%) | Major bleeding: 6 (4.7%) | Infections and infestations: 25 (7.5%), Wound infection: 4 (1.2%) | |
| Arm 2 (dabigatran), 300 | Major VTE: 3 (4.3%) | Major bleeding: 0 (0%) | Infections and infestations: 21 (7.0%), Wound Infection: 3 (1.0%) | ||
| Shorr et al., 2012[19] | Arm 1 (enoxaparin, CrCL 60 mL/min), 353 | Total VTE: 17/275 (6.2%) | Major bleeding: 0/351 (0%) | NR | |
| Arm 2 (desirudin, CrCL 60 mL/min), 353 | Total VTE: 13/284 (4.3%) | Major bleeding: 2/349 (0.27%) | NR | ||
| Arm 3 (enoxaparin, CrCL 4559 mL/min), 369 | Total VTE: 18/282 (6.2%) | Major bleeding: 1/365 (0.27%) | NR | ||
| Arm 4 (desirudin, CrCL 4559 mL/min), 395 | Total VTE: 17/303 (5.6%) | Major bleeding: 1/393 (0.25%) | NR | ||
| Arm 5 (enoxaparin, CrCL <45 mL/min), 298 | Total VTE: 24/216 (11.1%) | Major bleeding: 1/294 (0.34%) | NR | ||
| Arm 6 (desirudin, CrCL <45 mL/min), 279 | Total VTE: 7/205 (3.4%) | Major bleeding: 5/275 (1.82%) | NR | ||
| Elsaid et al., 2012[20] | Arm 1 (enoxaparin, CrCL 60 mL/min), 17 | NR | Major bleeding: 2 (11.8%) | NR | |
| Arm 2 (enoxaparin, CrCL 3059 mL/min), 86 | NR | Major bleeding: 9 (10.5%) | NR | ||
| Arm 3 (enoxaparin, CrCL 30 mL/min), 53 | NR | Major bleeding: 10 (18.9%) | NR | ||
| Arm 4 (UFH, CrCL 60 mL/min), 19 | NR | Major bleeding: 2 (10.5%) | NR | ||
| Arm 5 (UFH, CrCL 3059 mL/min), 99 | NR | Major bleeding: 3 (3%) | NR | ||
| Arm 6 (UFH, CrCL 30 mL/min), 49 | NR | Major bleeding: 2 (4.1%) | NR | ||
Obese Patients
We found 1 subgroup analysis of an RCT (total 3706 patients, 2563 nonobese and 1118 obese patients) that reported on the comparative effectiveness and safety of fixed low‐dose dalteparin 5000 IU/day compared to placebo among 1118 hospitalized medically ill patients with body mass indices (BMI) greater than 30 kg/m2.11 Neither group received additional concurrent prophylactic therapies. The 3 most prevalent medical diagnoses prompting hospitalization were congestive heart failure, respiratory failure, and infectious diseases. Compression ultrasound was performed in all patients by day 21 of hospitalization. The primary end point was the composite of VTE, fatal PE, and sudden death, and secondary end points included DVT, bleeding, and thrombocytopenia by day 21 (Table 1). In obese patients, the primary end point occurred in 2.8% (95% confidence interval [CI]: 1.34.3) of the dalteparin group and in 4.3% (95% CI: 2.56.2) of the placebo group (relative risk [RR]: 0.64; 95% CI: 0.32‐1.28). In nonobese patients, the primary end point occurred in 2.8% (95% CI: 1.8‐3.8) and 5.2% (95% CI: 3.9‐6.6) of the dalteparin and placebo groups, respectively (RR: 0.53; 95% CI: 0.34‐0.82). When weight was modeled as a continuous variable, no statistically significant interaction between weight and dalteparin efficacy was observed (P=0.97). The authors calculated the RR in predefined BMI subgroups and found that dalteparin was effective in reducing VTE in patients with BMIs up to 40, with RRs of <1.0 for all (approximate range, 0.20.8). However, a fixed dose of dalteparin 5000 IU/day was not better than placebo for individuals with BMI >40 kg/m2. There was no significant difference in mortality or major hemorrhage by day 21 between treatment and placebo groups.
Freeman and colleagues prospectively assigned 31 medically ill patients with extreme obesity (BMI >40 kg/m2) to 1 of 3 dosing regimens of enoxaparin: a fixed dose of 40 mg daily enoxaparin (control group, n=11), enoxaparin at 0.4 mg/kg (n=9), or enoxaparin at 0.5 mg/kg (n=11).[12] The average BMI of the entire cohort was 62.1 kg/m2 (range, 40.582.4). All patients had anti‐factor Xa levels drawn on the day of enrollment and daily for 3 days (Table 2). The relationship between anti‐factor Xa levels and clinical efficacy of low‐molecular weight heparin (LMWH) in VTE prophylaxis is still unclear; however, an anti‐factor Xa level of 0.2 to 0.5 IU/mL, measured 4 hours after the fourth dose of LMWH, is the target level recommended for VTE prophylaxis.[13] Patients who received weight‐based enoxaparin at 0.5mg/kg achieved target anti‐factor Xa level 86% of the time compared to 32% of the time in those receiving 0.4 mg/kg and 19% of the time for those in the fixed‐dose group (P<0.001). No clinical outcomes were reported in this study.
| Intervention | Outcome | Risk of Bias | Evidence Statement and Magnitude of Effect |
|---|---|---|---|
| |||
| Patients on antiplatelet agents | |||
| Rivaroxaban vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic rivaroxaban or enoxaparin in patients concomitantly treated with antiplatelet agents; 3.6% vs 3.25% |
| Dabigatran vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic dabigatran or enoxaparin in patients concomitantly treated with aspirin; 1.6% vs 3.0% |
| Obese patients | |||
| Dalteparin vs placebo | VTE | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing total VTE in obese patients; 2.8% vs 4.3%, RR: 0.64, 95% CI: 0.32‐1.28 |
| Dalteparin vs placebo | Mortality | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing mortality in obese patients; 9.9% vs 8.6%, P=0.36 |
| Dalteparin vs placebo | Major bleeding | Moderate | Insufficient evidence for safety of dalteparin vs placebo in reducing major bleeding in obese patients; 0% vs 0.7%, P>0.99 |
| Enoxaparin 40 mg daily vs 0.4 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.4 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 32%, P=NR |
| Enoxaparin 40 mg daily vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 86%, P<0.001 |
| Enoxaparin 0.4 mg/kg vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 0.4 mg/kg versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 32% vs 86%, P=NR |
| Patients with renal insufficiency | |||
| Tinzaparin vs enoxaparin | VTE | High | Insufficient evidence about superiority of either drug for preventing VTE in patients with renal insufficiency, 0/27 vs 0/28* |
| Tinzaparin vs enoxaparin | Bleeding | High | Insufficient evidence about safety of either drug in patients with renal insufficiency; 5/27 vs 4/28, P=0.67 |
| Dabigatran vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of dabigatran in reducing VTE in severe renal compromise patients vs enoxaparin; 4.3% vs 9%, OR: 0.48, 95% CI: 0.13‐1.73, P=0.271 |
| Dabigatran vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of dabigatran vs enoxaparin in patients with renal impairment; 0 vs 4.7%, P=0.039 |
| Desirudin vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of desirudin vs enoxaparin in reducing VTE in patients with renal impairment; 4.9% vs 7.6%, P=0.019 |
| Desirudin vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of desirudin vs enoxaparin in patients with renal impairment; 0.8% vs 0.2%, P=0.109 |
| Enoxaparin vs UFH | Bleeding | High | Insufficient evidence for increased risk of bleeding with enoxaparin vs unfractionated heparin in patients with all levels of renal impairment, 13.5% vs 4.2%, RR: 3.2, 95% CI: 1.47.3; and for the subgroup of patients with creatinine clearance <30 mL/min; 18.9% vs 4.1%, RR: 4.68, 95% CI: 1.120.6 |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | VTE | Moderate | Insufficient evidence regarding differential benefit of unfractionated heparin by renal function; 2.6% of patients had a VTE event |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | Bleeding | Moderate | Insufficient evidence for differential harm from unfractionated heparin by renal function; 13 events in 92 patients |
Patients on Antiplatelet Drugs
We did not find studies that directly looked at the comparative effectiveness of VTE prophylaxis in patients who were on antiplatelet drugs including aspirin. However, there were 2 studies that looked at the risk of bleeding in patients who received VTE pharmacologic prophylaxis while concurrently taking antiplatelet agents including aspirin. Both studies used pooled data from large phase III trials.
The study by Eriksson et al. used data from the RECORD (Regulation of Coagulation in Orthopedic Surgery to Prevent Deep Venous Thrombosis and Pulmonary Embolism) trial where over 12,000 patients undergoing elective total knee or hip replacement were randomized to receive VTE prophylaxis with oral rivaroxaban or subcutaneous enoxaparin.[14] Nine percent of participants in each arm (563 in rivaroxaban and 526 in enoxaparin/placebo) were concomitantly using antiplatelet agents or aspirin at least once during the at risk period, defined as starting at day 1 of surgery up to 2 days after the last intake of the study drug. The only end point evaluated was bleeding, and the authors found no statistically significant bleeding difference among the 2 arms (Table 1). Any bleeding event in the rivaroxaban with antiplatelets or aspirin arm was found in 20 (3.6%) patients, whereas in those on enoxaparin/placebo with antiplatelets or aspirin arm it was 17 (3.2%). The relative rate of bleeding among users versus nonusers of antiplatelet drugs or aspirin was 1.32 (95% CI: 0.85‐2.05) in the rivaroxaban group and 1.40 (95% CI: 0.87‐2.25) in the enoxaparin arm (Table 1).
Friedman et al. used pooled data from the RE‐MODEL, RENOVATE, and REMOBILIZE trials, where patients who were undergoing hip or knee arthroplasty were randomized to 220 mg of dabigatran once daily, 150 mg of dabigatran once daily (we focused on this lower dosage as this is the only available dose used in the US), 40 mg of enoxaparin once daily, or 30 mg of enoxaparin twice a day.[15] Of the 8135 patients, 4.7% were on concomitant aspirin. The baseline characteristics of those on aspirin were similar to the other enrollees. The primary outcome was major bleeding events requiring transfusion, symptomatic internal bleeding, or bleeding requiring surgery. Among patients receiving 150 mg of dabigatran, bleeding events with and without concomitant aspirin occurred in 1.6% and 1.0%, respectively (odds ratio [OR]: 1.64; 95% CI: 0.36‐7.49; P=0.523). The percentages of participants with bleeding who received enoxaparin, with and without aspirin, were 3.0% and 1.2%, respectively (OR: 2.57; 95% CI: 0.83‐7.94; P=0.101). The RR of bleeding on dabigatran compared to enoxaparin with and without aspirin therapy was 0.55 (95% CI: 0.11‐2.78) and 0.82 (95% CI: 0.37‐1.84), respectively (Table 1).
Patients With Renal Insufficiency
We found 5 studies that evaluated the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE in patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, or patients receiving dialysis. Four studies were RCTs,[16, 17, 18, 19] and 1 used a cohort design assessing separate cohorts before and after a quality improvement intervention.[20] Bauersachs and colleagues conducted an RCT comparing unfractionated heparin at 5000 IU, 3 times daily to certoparin, which is not approved in the United States and is not further discussed here.[16] The rate of DVT among patients treated with unfractionated heparin in patients with a glomerular filtration rate >30 mL/min was marginally lower than those with severe renal dysfunction (10.3 vs 11.1%) (Table 1).
Patients with severe renal dysfunction who received 5000 IU of unfractionated heparin 3 times a day were at increased risk of all bleeds (RR: 3.4; 95% CI: 2.05.9), major bleeds (RR: 7.3; 95% CI: 3.316), and minor bleeds (RR: 2.6; 95% CI: 1.4‐4.9) compared to patients treated with unfractionated heparin without severe renal dysfunction.[16]
A randomized trial by Mah and colleagues compared drug accumulation and anti‐Xa activity in elderly patients with renal dysfunction (defined as a glomerular filtration rate of 20 to 50 mL/min) who received either tinzaparin at 4500 IU once daily or enoxaparin at 4000 IU once daily.[17] Enoxaparin accumulated to a greater extent from day 1 to day 8 than did tinzaparin; the ratio of maximum concentration on day 8 compared to day 1 was 1.22 for enoxaparin and 1.05 for tinzaparin (P=0.016). No VTE events were reported in patients who received tinzaparin or enoxaparin. There was no statistical difference in the incidence of bleeding events between patients receiving tinzaparin (5, including 2 major events) and enoxaparin (4, including 3 major events, P=0.67) (Table 1).
The trial by Dahl and colleagues randomly assigned patients who were over 75 years of age and/or who had moderate renal dysfunction (defined as creatinine clearance between 30 and 49 mL/min) to receive enoxaparin 40 mg daily or dabigatran 150 mg daily.[18] There was no significant difference in the rate of major VTE events between patients receiving dabigatran (4.3%) and enoxaparin (9%) (OR: 0.48; 95% CI: 0.13‐1.73; P=0.271) (Table 1). The rate of major bleeding was significantly higher among patients randomly assigned to receive enoxaparin (4.7%) versus dabigatran (0%) (P=0.039).[18]
Shorr and colleagues published a post hoc subgroup analysis of a multicenter trial in which orthopedic patients were randomly assigned to receive desirudin 15 mg twice daily or enoxaparin 40 mg once daily.[19] Evaluable patients (1565 of the 2079 patients randomized in the trial) receiving desirudin experienced a significantly lower rate of major VTE compared with patients receiving enoxaparin (4.9% vs 7.6%, P=0.019). This relationship was particularly pronounced for evaluable patients whose creatinine clearance was between 30 and 44 mL/min. In evaluable patients with this degree of renal dysfunction, 11% of patients taking enoxaparin compared to 3.4% of those taking desirudin had a major VTE (OR: 3.52; 95% CI: 1.48‐8.4; P=0.004). There was no significant difference in the rates of major bleeding among a subset of patients assessed for safety outcomes (2078 of the 2079 patients randomized in the trial) who received desirudin (0.8%) or enoxaparin (0.2%) (Table 1).
Elsaid and Collins assessed VTE and bleeding events associated with the use of unfractionated heparin 5000U either 2 or 3 times daily and enoxaparin 30 mg once or twice daily across patients stratified by renal function (creatinine clearance <30, 3059, and 60 mL/min). The investigators made assessments before and after a quality improvement intervention that was designed to eliminate the use of enoxaparin in patients whose creatinine clearance was <30 mL/min. No VTE events were reported. Patients receiving enoxaparin were significantly more likely to experience a major bleeding episode compared with patients receiving unfractionated heparin (overall rates for all levels of renal function: 13.5% vs 4. 2%; RR: 3.2; 95% CI: 1.47.3) (Table 2). This association was largely driven by the subgroup of patients with a creatinine clearance <30 mL/min. For this subgroup with severe renal insufficiency, patients receiving enoxaparin were significantly more likely to have a bleed compared with patients receiving unfractionated heparin (18.9% vs 4.1%; RR: 4.68; 95% CI: 1.120.6) (Tables 1 and 2). There was no difference in the bleeding rates for patients whose creatinine clearances were >60 mL/min.[20]
Strength of Evidence
Obese Patients
Overall, we found that the strength of evidence was insufficient regarding the composite end point of DVT, PE, and sudden death, and the outcomes of mortality and bleeding (Table 2). This was based on a paucity of available data, and a moderate risk of bias in the reviewed studies. Additionally, 92% of the enrolled patients in the studies were white, limiting the generalizability of the results to other ethnic groups.
Patients on Antiplatelets
The strength of evidence was insufficient in the studies reviewed here to conclude that there is no difference in rates of bleeding in patients who are concomitantly taking antiplatelet drugs while getting VTE prophylaxis with rivaroxaban, dabigatran, or enoxaparin. We based this rating because of the imprecision of results and unknown consistencies across multiple studies.
Patients With Renal Insufficiency
One RCT had a high risk of bias for our key question because data from only 1 study arm were useful for our review.[16] The other RCTs were judged to have a moderate risk of bias. The analyses led by Dahl and Shorr[18, 19] were based on post hoc (ie, not prespecified) analysis of data from RCTs. Additionally, outcomes in the Shorr et al. trial were reported for evaluable subpopulations of the cohort that was initially randomized in the clinical trial.
We rated the strength of evidence as insufficient to know the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE during hospitalization of patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, and patients receiving dialysis. We based this rating on the risk of bias associated with published studies and a lack of consistent evidence regarding associations that were reported. Similarly, we rated the strength of evidence as insufficient that 5000 U of unfractionated heparin 3 times daily increases the risk of major and minor bleeding events in patients with severely compromised renal function compared to this dose in patients without severely compromised renal function. We based this rating on a high risk of bias of included studies and inconsistent evidence. Likewise, we rated the strength of evidence as insufficient that enoxaparin significantly increases the risk of major bleeding compared with unfractionated heparin in patients with severe renal insufficiency. We based this rating on a high risk of bias and inconsistent published evidence.
We similarly found insufficient evidence to guide treatment decisions for patients with renal insufficiency. Our findings are consistent with other recent reviews. The American College of Chest Physicians (ACCP) practice guidelines[21] make dosing recommendations for the therapeutic use of enoxaparin. However, their assessment is that the data are insufficient to make direct recommendations about prophylaxis. Their assessment of the indirect evidence regarding bioaccumulation and increased anti‐factor Xa levels are consistent with ours. The ACCP guidelines also suggest that decreased clearance of enoxaparin has been associated with increased risk of bleeding events for patients with severe renal insufficiency. However, the cited study[20] compares patients with and without severe renal dysfunction who received the same therapy. Therefore, it is not possible to determine the additional risk conveyed by enoxaparin therapy, that is, above the baseline increased risk of bleeding among patients with renal insufficiency, particularly those receiving an alternate pharmacologic VTE prevention strategy, such as unfractionated heparin.
DISCUSSION
We found that the evidence was very limited about prevention of VTE in these select and yet prevalent patient populations. Despite the fact that there is an increasing number of obese patients and patients who are on antiplatelet therapies, most clinical practice guidelines do not address the care of these populations, which may be entirely appropriate given the state of the evidence.
The ACCP practice guidelines[21] suggest using a higher dose of enoxaparin for the prevention of VTE in obese patients. The subgroup analysis by Kucher et al.[11] showed effect attenuation of dalteparin when given at a fixed dose of 5000 IU/mL to patients with a BMI of >40 kg/m2. The Freeman study[12] showed that extremely obese patients (average BMI >62.1 kg/m2) who are given a fixed dose of enoxaparin achieved target anti‐factor Xa levels significantly less often than those who received a higher dose of enoxaparin. The 2 separate findings, although not conclusive, lend some credence to the current ACCP guidelines.[21]
The studies we reviewed on VTE prophylaxis in patients who are concomitantly on antiplatelets including aspirin reported no major increased risk of bleeding; however, in the Friedman et al. study,[15] 3.0% of patients who were put on enoxaparin while still on aspirin had a bleeding event compared to 1.2% of those on enoxaparin alone. This difference is not statistically significant but is a trend possibly worth noting, especially when one looks at the lower RR of bleeding at 0.55 compared to 0.82 when dabigatran is compared with enoxaparin with and without concomitant aspirin therapy, respectively (Table 1). The highest dose of aspirin used in either of the studies was 160 mg/day, and neither study addressed other potent antiplatelets such as clopidogrel or ticlopidine separately, which limits the generalizability of the finding to all antiplatelets. Current ACCP guidelines do not recommend aspirin as a sole option for the prevention of VTE in orthopedic surgery patients.[22] Concerns remain among clinicians that antiplatelets, including aspirin, on their own are unlikely to be fully effective to thwart venous thrombotic processes for most patients, and yet the risk of bleeding is not fully known when these agents are combined with other anticoagulants for VTE prophylaxis.
Our review has several limitations, including the possibility that we may have missed some observational studies, as the identification of relevant observational studies in electronic searches is more challenging than that of RCTs. The few studies made it impossible to quantitatively pool results. These results, however, have important implications, namely that additional research on the comparative effectiveness and safety of pharmacologic and mechanical strategies to prevent VTE is needed for the optimal care of these patient subgroups. This might be achieved with trials dedicated to enrolling these patients or prespecified subgroup analyses within larger trials. Observational data may be appropriate as long as attention is paid to confounding.
APPENDIX
MEDLINE Search Strategy
((pulmonary embolism[mh] OR PE[tiab] OR Pulmonary embolism[tiab] OR thromboembolism[mh] OR thromboembolism[tiab] OR thromboembolisms[tiab] OR Thrombosis[mh] OR thrombosis[tiab] OR DVT[tiab] OR VTE[tiab] OR clot[tiab]) AND (Anticoagulants[mh] OR Anticoagulants[tiab] OR Anticoagulant[tiab] OR thrombin inhibitors[tiab] OR Aspirin[mh] or aspirin[tiab] OR aspirins[tiab] or clopidogrel[nm] OR clopidogrel[tiab] OR Plavix[tiab] or ticlopidine[mh] or ticlopidine[tiab]OR ticlid[tiab] OR prasugrel[nm]Or prasugrel[tiab]OR effient[tiab]OR ticagrelor[NM] OR ticagrelor[tiab]OR Brilinta[tiab] OR cilostazol[NM] OR cilostazol[tiab]OR pletal[tiab] OR warfarin[mh]OR warfarin[tiab]OR coumadin[tiab] OR coumadine[tiab] OR Dipyridamole[mh]OR dipyridamole[tiab]OR persantine[tiab] OR dicoumarol[MH] OR dicoumarol[tiab] OR dicumarol[tiab] OR Dextran sulfate[mh] OR dextran sulfate[tiab] ORthrombin inhibitors[tiab] OR thrombin inhibitor[tiab] OR heparin[mh] OR Heparin[tiab] OR Heparins[tiab] OR LMWH[tiab] OR LDUH[tiab] OR Enoxaparin[mh] OR Enoxaparin[tiab] OR Lovenox[tiab] OR Dalteparin[tiab] OR Fragmin[tiab] OR Tinzaparin[tiab] OR innohep[tiab] OR Nadroparin[tiab] OR Fondaparinux[nm] OR Fondaparinux[tiab] OR Arixtra[tiab] OR Idraparinux[nm] OR Idraparinux[tiab] OR Rivaroxaban[nm] OR Rivaroxaban[tiab] OR novastan[tiab] OR Desirudin[nm] OR Desirudin[tiab] OR Iprivask[tiab]OR direct thrombin inhibitor[tiab] OR Argatroban[nm] OR Argatroban[tiab] OR Acova[tiab] OR Bivalirudin[nm] OR Bivalirudin[tiab] OR Angiomax[tiab] OR Lepirudin[nm] OR Lepirudin[tiab] OR Refludan[tiab] OR Dabigatran[nm] OR Dabigatran[tiab] OR Pradaxa[tiab] OR factor xa[mh] OR factor Xa[tiab] OR vena cava filters[mh] OR filters[tiab] OR filter[tiab] OR compression stockings[mh] OR intermittent pneumatic compression devices[mh] OR compression [tiab] OR Venous foot pump[tiab])) AND(prevent*[tiab] OR prophyla*[tiab] OR prevention and control[subheading]) NOT (animals[mh] NOT humans[mh]) NOT (editorial[pt] OR comment[pt]) NOT ((infant[mh] OR infant[tiab] OR child[mh] OR child[tiab] OR children[tiab] OR adolescent[mh] OR adolescent[tiab] OR teen‐age[tiab] OR pediatric[tiab] OR perinatal[tiab]) NOT (adult[tiab] OR adults[tiab] OR adult[mh])) NOT (mechanical valve[tiab] OR heart valve[tiab] OR atrial fibrillation[mh] OR atrial fibrillation[tiab] OR thrombophilia[mh] OR thrombophilia[tiab] OR pregnancy[mh])
- , , . Estimated annual number of incident and recurrent, non‐fatal and fatal venous thromboembolism (VTE) events in the US. Blood. 2005;106:910.
- Institute of Medicine. Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academies Press; 2009.
- Lovenox (enoxaparin sodium injection for subcutaneous and intravenous use: prescribing information). Bridgewater, NJ: SanofiAventis; 2011. Available at: http://products.sanofi.us/lovenox/lovenox.html. Accessed October 17, 2012.
- Innohep (tinzaparin sodium injection). Ballerup, Denmark: LEO Pharmaceutical Products; 2008. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/020484s011lbl.pdf. Accessed October 17, 2012.
- Leizorovicz A. Tinzaparin compared to unfractionated heparin for initial treatment of deep vein thrombosis in very elderly patients with renal insufficiency‐ the IRIS trial. [50th ASH Annual Meeting and Exposition abstract 434]. Blood. 2008;11:112.
- Fragmin (dalteparin sodium injection). New York, NY: Pfizer Inc.; 2007. Available at: http://www.pfizer.com/files/products/uspi_fragmin.pdf. Accessed October 17, 2012.
- Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; August 2011. AHRQ publication No. 10 (11)‐EHC063‐EF. Available at: http://www.effectivehealthcare.ahrq.gov. Accessed October 17, 2012.
- Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/928/VTE‐Special‐Populations_Protocol_20120112.pdf. Accessed April 17, 2012.
- , , , et al. Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Evidence Report/Technology Assessment (AHRQ). Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/1501/venous‐thromboembolism‐special‐populations‐report‐130529.pdf. 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Efficacy and safety of fixed low‐dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med. 2005;165(3):341–345.
- , , , . Prospective comparison of three enoxaparin dosing regimens to achieve target anti‐factor Xa levels in hospitalized, medically ill patients with extreme obesity. Am J Hematol. 2012;87(7):740–743.
- , , . Effect of prophylactic dalteparin on anti‐factor xa levels in morbidly obese patients after bariatric surgery. Obes Surg. 2010;20(4):487–491.
- , , , , . Concomitant use of medication with antiplatelet effects in patients receiving either rivaroxaban or enoxaparin after total hip or knee arthroplasty. Thromb Res. 2012;130(2):147–151.
- , , , , , . Dabigatran etexilate and concomitant use of non‐steroidal anti‐inflammatory drugs or acetylsalicylic acid in patients undergoing total hip and total knee arthroplasty: No increased risk of bleeding. Thromb Haemost. 2012;108(1):183–190.
- , , , et al. CERTIFY: prophylaxis of venous thromboembolism in patients with severe renal insufficiency. Thromb Haemost. 2011;105(6):981–988.
- , , , et al. Tinzaparin and enoxaparin given at prophylactic dose for eight days in medical elderly patients with impaired renal function: a comparative pharmacokinetic study. Thromb Haemost. 2007;97(4):581–586.
- , , , , , . Thromboprophylaxis in patients older than 75 years or with moderate renal impairment undergoing knee or hip replacement surgery [published correction appears in Int Orthop. 2012;36(5):1113]. Int Orthop. 2012;36(4):741–748.
- , , , . Impact of stage 3B chronic kidney disease on thrombosis and bleeding outcomes after orthopedic surgery in patients treated with desirudin or enoxaparin: insights from a randomized trial. J Thromb Haemost. 2012;10(8):1515–1520.
- , . Initiative to improve thromboprophylactic enoxaparin exposure in hospitalized patients with renal impairment. Am J Health Syst Pharm. 2012;69(5):390–396.
- , , , , ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence‐based clinical practice guidelines. Chest. 2012;141(2 suppl):7S–47S.
- , . Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence. Ann Pharmacother. 2013;47(1):63–74.
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), is estimated to affect 900,000 Americans each year and is a cause of significant morbidity and mortality with associated high healthcare costs.[1] Accordingly, the comparative effectiveness and safety of interventions for the prevention and treatment of VTE are among the national priorities for comparative effectiveness research.[2] Whereas we have evidence‐based guidelines for the prophylaxis of VTE in the general population, there are no guidelines informing the care of select patient populations. Select populations are those patients in whom there is decisional uncertainty about the optimal choice, timing, and dose of VTE prophylaxis. Not only do these patients have an increased risk of DVT and PE, but most are also at high risk of bleeding, the most important complication of VTE prophylaxis.[3, 4, 5, 6]
The objectives of this systematic review were to define the comparative effectiveness and safety of pharmacologic and mechanical strategies for VTE prevention in some of these select medical populations including obese patients, patients on concomitant antiplatelet therapy, patients with renal insufficiency, patients who are underweight, and patients with coagulopathy due to liver disease.
METHODS
The methods for this comparative effectiveness review (CER) follow the guidelines suggested in the Agency for Healthcare Research and Quality (AHRQ) Methods Guide for Effectiveness and Comparative Effectiveness Reviews.[7] The protocol was publically posted.[8]
Search Strategy
We searched MEDLINE, EMBASE, and SCOPUS through August 2011, CINAHL, International Pharmaceutical Abstracts,
Study Selection
We reviewed titles followed by abstracts to identify randomized controlled trials (RCTs) or observational studies with comparison groups reporting on the effectiveness or safety of VTE prevention in our populations. Two investigators independently reviewed abstracts, and we excluded the abstracts if both investigators agreed that the article met 1 or more of the exclusion criteria. We included only English‐language articles that evaluated the effectiveness of pharmacological or mechanical interventions that have been approved for clinical use in the United States. To be eligible, the studies must have addressed relevant key questions in the population of our interest. We resolved disagreements by consensus. We used DistillerSR (Evidence Partners Inc., Ottawa, Ontario, Canada), a Web‐based database management program to manage the review process. Two investigators assessed the risk of bias in each study independently, using the Downs and Black instrument for observational studies and trials.[10]
Data Synthesis
For each select population, we created detailed evidence tables containing the information abstracted from the eligible studies. After synthesizing the evidence, we graded the quantity, quality, and consistency of the best available evidence for each select population by adapting an evidence‐grading scheme recommended in the Methods Guide for Conducting Comparative Effectiveness Reviews.[7]
RESULTS
We identified 30,902 unique citations and included 9 studies (Figure 1). There were 5 RCTs with relevant subgroups and 4 observational studies (Table 1). Two studies reported on the risk of bleeding in patients given pharmacologic prophylaxis while they are concomitantly taking nonsteroidal anti‐inflammatory drugs (NSAIDS) or antiplatelet agents/aspirin, 1 RCT and 1 prospective observational study reported on obese patients, and 5 studies described outcomes of patients with renal insufficiency (see Supporting Information, Table 1, in the online version of this article). No study tested prophylaxis in underweight patients or those with liver disease.

| Study | Arm, n | Total VTE (DVT and PE) | Bleeding | Other Outcomes | |
|---|---|---|---|---|---|
| |||||
| Obese patients | |||||
| Kucher et al., 2005[11] | Arm 1 (dalteparin), 558 | 2.8% (95% CI: 1.34.3) | 0% | Mortality at 21 days: 4.6% | |
| Arm 2 (placebo), 560 | 4.3% (95% CI: 2.56.2) | 0.7% | Mortality at 21 days: 2.7% | ||
| Freeman et al., [12] | Arm 1 (fixed‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 19 % | |
| Arm 2 (lower‐dose enoxaparin), 9 | NR | NR | Peak anti‐factor Xa level 32 % | ||
| Arm 3 (higher‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 86 % | ||
| Patients on antiplatelet agents | |||||
| Eriksson et al., 2012[14] | Arm 1 (rivaroxaban), 563 | NR | 20 (3.6%), rate ratio for use vs nonuse: 1.32 (95% CI: 0.85‐2.05) | NR | |
| Arm 2 (enoxaparin/placebo), 526 | NR | 17 (3.2%), rate ratio for use vs nonuse: 1.40 (95% CI: 0.87‐2.25) | NR | ||
| Friedman et al., 2012[15] | Arm 2 (150 mg dabigatran, no ASA), 1149 | NR | 11 (1.0%)a | NR | |
| Arm 5 (150 mg dabigatran+ASA), 128 | NR | 2 (1.6%)a | NR | ||
| Arm 3 (enoxaparin, no ASA), 1167 | NR | 14 (1.2%)a | NR | ||
| Arm 6 (enoxaparin+ASA), 132 | NR | 4 (3.0%) | NR | ||
| 150 mg dabigatran compared with enoxaparinNo concomitant ASA therapy | NR | RR: 0.82 (95% CI: 0.37‐1.84) | NR | ||
| 150 mg dabigatran compared with enoxaparinWith concomitant ASA therapy | NR | RR: 0.55 (95% CI: 0.11‐2.78) | NR | ||
| Patients with renal insufficiency | |||||
| Bauersachs et al., 2011[16] | Arm 2 (GFR <30), 92 | Total DVT: 11.11%; Total PE: 0% | Major bleeding: 4/92 (4.35%), minor bleeding: 9/92 (9.78%) | Mortality: 5.81% | |
| Mah et al., 2007[17] | Arm 2 (tinzaparin), 27 | NR | Major bleeding: 2/27 (7.4%), minor bleeding: 3/27 (11.1%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.05 | |
| Arm 3 (enoxaparin), 28 | NR | Major bleeding: 1/28 (3.6%), minor bleeding: 3/28 (10.7%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.22 | ||
| Dahl et al., 2012[18] | Arm 1 (enoxaparin), 332 | Major VTE: 8 (9.0%) | Major bleeding: 6 (4.7%) | Infections and infestations: 25 (7.5%), Wound infection: 4 (1.2%) | |
| Arm 2 (dabigatran), 300 | Major VTE: 3 (4.3%) | Major bleeding: 0 (0%) | Infections and infestations: 21 (7.0%), Wound Infection: 3 (1.0%) | ||
| Shorr et al., 2012[19] | Arm 1 (enoxaparin, CrCL 60 mL/min), 353 | Total VTE: 17/275 (6.2%) | Major bleeding: 0/351 (0%) | NR | |
| Arm 2 (desirudin, CrCL 60 mL/min), 353 | Total VTE: 13/284 (4.3%) | Major bleeding: 2/349 (0.27%) | NR | ||
| Arm 3 (enoxaparin, CrCL 4559 mL/min), 369 | Total VTE: 18/282 (6.2%) | Major bleeding: 1/365 (0.27%) | NR | ||
| Arm 4 (desirudin, CrCL 4559 mL/min), 395 | Total VTE: 17/303 (5.6%) | Major bleeding: 1/393 (0.25%) | NR | ||
| Arm 5 (enoxaparin, CrCL <45 mL/min), 298 | Total VTE: 24/216 (11.1%) | Major bleeding: 1/294 (0.34%) | NR | ||
| Arm 6 (desirudin, CrCL <45 mL/min), 279 | Total VTE: 7/205 (3.4%) | Major bleeding: 5/275 (1.82%) | NR | ||
| Elsaid et al., 2012[20] | Arm 1 (enoxaparin, CrCL 60 mL/min), 17 | NR | Major bleeding: 2 (11.8%) | NR | |
| Arm 2 (enoxaparin, CrCL 3059 mL/min), 86 | NR | Major bleeding: 9 (10.5%) | NR | ||
| Arm 3 (enoxaparin, CrCL 30 mL/min), 53 | NR | Major bleeding: 10 (18.9%) | NR | ||
| Arm 4 (UFH, CrCL 60 mL/min), 19 | NR | Major bleeding: 2 (10.5%) | NR | ||
| Arm 5 (UFH, CrCL 3059 mL/min), 99 | NR | Major bleeding: 3 (3%) | NR | ||
| Arm 6 (UFH, CrCL 30 mL/min), 49 | NR | Major bleeding: 2 (4.1%) | NR | ||
Obese Patients
We found 1 subgroup analysis of an RCT (total 3706 patients, 2563 nonobese and 1118 obese patients) that reported on the comparative effectiveness and safety of fixed low‐dose dalteparin 5000 IU/day compared to placebo among 1118 hospitalized medically ill patients with body mass indices (BMI) greater than 30 kg/m2.11 Neither group received additional concurrent prophylactic therapies. The 3 most prevalent medical diagnoses prompting hospitalization were congestive heart failure, respiratory failure, and infectious diseases. Compression ultrasound was performed in all patients by day 21 of hospitalization. The primary end point was the composite of VTE, fatal PE, and sudden death, and secondary end points included DVT, bleeding, and thrombocytopenia by day 21 (Table 1). In obese patients, the primary end point occurred in 2.8% (95% confidence interval [CI]: 1.34.3) of the dalteparin group and in 4.3% (95% CI: 2.56.2) of the placebo group (relative risk [RR]: 0.64; 95% CI: 0.32‐1.28). In nonobese patients, the primary end point occurred in 2.8% (95% CI: 1.8‐3.8) and 5.2% (95% CI: 3.9‐6.6) of the dalteparin and placebo groups, respectively (RR: 0.53; 95% CI: 0.34‐0.82). When weight was modeled as a continuous variable, no statistically significant interaction between weight and dalteparin efficacy was observed (P=0.97). The authors calculated the RR in predefined BMI subgroups and found that dalteparin was effective in reducing VTE in patients with BMIs up to 40, with RRs of <1.0 for all (approximate range, 0.20.8). However, a fixed dose of dalteparin 5000 IU/day was not better than placebo for individuals with BMI >40 kg/m2. There was no significant difference in mortality or major hemorrhage by day 21 between treatment and placebo groups.
Freeman and colleagues prospectively assigned 31 medically ill patients with extreme obesity (BMI >40 kg/m2) to 1 of 3 dosing regimens of enoxaparin: a fixed dose of 40 mg daily enoxaparin (control group, n=11), enoxaparin at 0.4 mg/kg (n=9), or enoxaparin at 0.5 mg/kg (n=11).[12] The average BMI of the entire cohort was 62.1 kg/m2 (range, 40.582.4). All patients had anti‐factor Xa levels drawn on the day of enrollment and daily for 3 days (Table 2). The relationship between anti‐factor Xa levels and clinical efficacy of low‐molecular weight heparin (LMWH) in VTE prophylaxis is still unclear; however, an anti‐factor Xa level of 0.2 to 0.5 IU/mL, measured 4 hours after the fourth dose of LMWH, is the target level recommended for VTE prophylaxis.[13] Patients who received weight‐based enoxaparin at 0.5mg/kg achieved target anti‐factor Xa level 86% of the time compared to 32% of the time in those receiving 0.4 mg/kg and 19% of the time for those in the fixed‐dose group (P<0.001). No clinical outcomes were reported in this study.
| Intervention | Outcome | Risk of Bias | Evidence Statement and Magnitude of Effect |
|---|---|---|---|
| |||
| Patients on antiplatelet agents | |||
| Rivaroxaban vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic rivaroxaban or enoxaparin in patients concomitantly treated with antiplatelet agents; 3.6% vs 3.25% |
| Dabigatran vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic dabigatran or enoxaparin in patients concomitantly treated with aspirin; 1.6% vs 3.0% |
| Obese patients | |||
| Dalteparin vs placebo | VTE | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing total VTE in obese patients; 2.8% vs 4.3%, RR: 0.64, 95% CI: 0.32‐1.28 |
| Dalteparin vs placebo | Mortality | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing mortality in obese patients; 9.9% vs 8.6%, P=0.36 |
| Dalteparin vs placebo | Major bleeding | Moderate | Insufficient evidence for safety of dalteparin vs placebo in reducing major bleeding in obese patients; 0% vs 0.7%, P>0.99 |
| Enoxaparin 40 mg daily vs 0.4 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.4 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 32%, P=NR |
| Enoxaparin 40 mg daily vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 86%, P<0.001 |
| Enoxaparin 0.4 mg/kg vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 0.4 mg/kg versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 32% vs 86%, P=NR |
| Patients with renal insufficiency | |||
| Tinzaparin vs enoxaparin | VTE | High | Insufficient evidence about superiority of either drug for preventing VTE in patients with renal insufficiency, 0/27 vs 0/28* |
| Tinzaparin vs enoxaparin | Bleeding | High | Insufficient evidence about safety of either drug in patients with renal insufficiency; 5/27 vs 4/28, P=0.67 |
| Dabigatran vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of dabigatran in reducing VTE in severe renal compromise patients vs enoxaparin; 4.3% vs 9%, OR: 0.48, 95% CI: 0.13‐1.73, P=0.271 |
| Dabigatran vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of dabigatran vs enoxaparin in patients with renal impairment; 0 vs 4.7%, P=0.039 |
| Desirudin vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of desirudin vs enoxaparin in reducing VTE in patients with renal impairment; 4.9% vs 7.6%, P=0.019 |
| Desirudin vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of desirudin vs enoxaparin in patients with renal impairment; 0.8% vs 0.2%, P=0.109 |
| Enoxaparin vs UFH | Bleeding | High | Insufficient evidence for increased risk of bleeding with enoxaparin vs unfractionated heparin in patients with all levels of renal impairment, 13.5% vs 4.2%, RR: 3.2, 95% CI: 1.47.3; and for the subgroup of patients with creatinine clearance <30 mL/min; 18.9% vs 4.1%, RR: 4.68, 95% CI: 1.120.6 |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | VTE | Moderate | Insufficient evidence regarding differential benefit of unfractionated heparin by renal function; 2.6% of patients had a VTE event |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | Bleeding | Moderate | Insufficient evidence for differential harm from unfractionated heparin by renal function; 13 events in 92 patients |
Patients on Antiplatelet Drugs
We did not find studies that directly looked at the comparative effectiveness of VTE prophylaxis in patients who were on antiplatelet drugs including aspirin. However, there were 2 studies that looked at the risk of bleeding in patients who received VTE pharmacologic prophylaxis while concurrently taking antiplatelet agents including aspirin. Both studies used pooled data from large phase III trials.
The study by Eriksson et al. used data from the RECORD (Regulation of Coagulation in Orthopedic Surgery to Prevent Deep Venous Thrombosis and Pulmonary Embolism) trial where over 12,000 patients undergoing elective total knee or hip replacement were randomized to receive VTE prophylaxis with oral rivaroxaban or subcutaneous enoxaparin.[14] Nine percent of participants in each arm (563 in rivaroxaban and 526 in enoxaparin/placebo) were concomitantly using antiplatelet agents or aspirin at least once during the at risk period, defined as starting at day 1 of surgery up to 2 days after the last intake of the study drug. The only end point evaluated was bleeding, and the authors found no statistically significant bleeding difference among the 2 arms (Table 1). Any bleeding event in the rivaroxaban with antiplatelets or aspirin arm was found in 20 (3.6%) patients, whereas in those on enoxaparin/placebo with antiplatelets or aspirin arm it was 17 (3.2%). The relative rate of bleeding among users versus nonusers of antiplatelet drugs or aspirin was 1.32 (95% CI: 0.85‐2.05) in the rivaroxaban group and 1.40 (95% CI: 0.87‐2.25) in the enoxaparin arm (Table 1).
Friedman et al. used pooled data from the RE‐MODEL, RENOVATE, and REMOBILIZE trials, where patients who were undergoing hip or knee arthroplasty were randomized to 220 mg of dabigatran once daily, 150 mg of dabigatran once daily (we focused on this lower dosage as this is the only available dose used in the US), 40 mg of enoxaparin once daily, or 30 mg of enoxaparin twice a day.[15] Of the 8135 patients, 4.7% were on concomitant aspirin. The baseline characteristics of those on aspirin were similar to the other enrollees. The primary outcome was major bleeding events requiring transfusion, symptomatic internal bleeding, or bleeding requiring surgery. Among patients receiving 150 mg of dabigatran, bleeding events with and without concomitant aspirin occurred in 1.6% and 1.0%, respectively (odds ratio [OR]: 1.64; 95% CI: 0.36‐7.49; P=0.523). The percentages of participants with bleeding who received enoxaparin, with and without aspirin, were 3.0% and 1.2%, respectively (OR: 2.57; 95% CI: 0.83‐7.94; P=0.101). The RR of bleeding on dabigatran compared to enoxaparin with and without aspirin therapy was 0.55 (95% CI: 0.11‐2.78) and 0.82 (95% CI: 0.37‐1.84), respectively (Table 1).
Patients With Renal Insufficiency
We found 5 studies that evaluated the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE in patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, or patients receiving dialysis. Four studies were RCTs,[16, 17, 18, 19] and 1 used a cohort design assessing separate cohorts before and after a quality improvement intervention.[20] Bauersachs and colleagues conducted an RCT comparing unfractionated heparin at 5000 IU, 3 times daily to certoparin, which is not approved in the United States and is not further discussed here.[16] The rate of DVT among patients treated with unfractionated heparin in patients with a glomerular filtration rate >30 mL/min was marginally lower than those with severe renal dysfunction (10.3 vs 11.1%) (Table 1).
Patients with severe renal dysfunction who received 5000 IU of unfractionated heparin 3 times a day were at increased risk of all bleeds (RR: 3.4; 95% CI: 2.05.9), major bleeds (RR: 7.3; 95% CI: 3.316), and minor bleeds (RR: 2.6; 95% CI: 1.4‐4.9) compared to patients treated with unfractionated heparin without severe renal dysfunction.[16]
A randomized trial by Mah and colleagues compared drug accumulation and anti‐Xa activity in elderly patients with renal dysfunction (defined as a glomerular filtration rate of 20 to 50 mL/min) who received either tinzaparin at 4500 IU once daily or enoxaparin at 4000 IU once daily.[17] Enoxaparin accumulated to a greater extent from day 1 to day 8 than did tinzaparin; the ratio of maximum concentration on day 8 compared to day 1 was 1.22 for enoxaparin and 1.05 for tinzaparin (P=0.016). No VTE events were reported in patients who received tinzaparin or enoxaparin. There was no statistical difference in the incidence of bleeding events between patients receiving tinzaparin (5, including 2 major events) and enoxaparin (4, including 3 major events, P=0.67) (Table 1).
The trial by Dahl and colleagues randomly assigned patients who were over 75 years of age and/or who had moderate renal dysfunction (defined as creatinine clearance between 30 and 49 mL/min) to receive enoxaparin 40 mg daily or dabigatran 150 mg daily.[18] There was no significant difference in the rate of major VTE events between patients receiving dabigatran (4.3%) and enoxaparin (9%) (OR: 0.48; 95% CI: 0.13‐1.73; P=0.271) (Table 1). The rate of major bleeding was significantly higher among patients randomly assigned to receive enoxaparin (4.7%) versus dabigatran (0%) (P=0.039).[18]
Shorr and colleagues published a post hoc subgroup analysis of a multicenter trial in which orthopedic patients were randomly assigned to receive desirudin 15 mg twice daily or enoxaparin 40 mg once daily.[19] Evaluable patients (1565 of the 2079 patients randomized in the trial) receiving desirudin experienced a significantly lower rate of major VTE compared with patients receiving enoxaparin (4.9% vs 7.6%, P=0.019). This relationship was particularly pronounced for evaluable patients whose creatinine clearance was between 30 and 44 mL/min. In evaluable patients with this degree of renal dysfunction, 11% of patients taking enoxaparin compared to 3.4% of those taking desirudin had a major VTE (OR: 3.52; 95% CI: 1.48‐8.4; P=0.004). There was no significant difference in the rates of major bleeding among a subset of patients assessed for safety outcomes (2078 of the 2079 patients randomized in the trial) who received desirudin (0.8%) or enoxaparin (0.2%) (Table 1).
Elsaid and Collins assessed VTE and bleeding events associated with the use of unfractionated heparin 5000U either 2 or 3 times daily and enoxaparin 30 mg once or twice daily across patients stratified by renal function (creatinine clearance <30, 3059, and 60 mL/min). The investigators made assessments before and after a quality improvement intervention that was designed to eliminate the use of enoxaparin in patients whose creatinine clearance was <30 mL/min. No VTE events were reported. Patients receiving enoxaparin were significantly more likely to experience a major bleeding episode compared with patients receiving unfractionated heparin (overall rates for all levels of renal function: 13.5% vs 4. 2%; RR: 3.2; 95% CI: 1.47.3) (Table 2). This association was largely driven by the subgroup of patients with a creatinine clearance <30 mL/min. For this subgroup with severe renal insufficiency, patients receiving enoxaparin were significantly more likely to have a bleed compared with patients receiving unfractionated heparin (18.9% vs 4.1%; RR: 4.68; 95% CI: 1.120.6) (Tables 1 and 2). There was no difference in the bleeding rates for patients whose creatinine clearances were >60 mL/min.[20]
Strength of Evidence
Obese Patients
Overall, we found that the strength of evidence was insufficient regarding the composite end point of DVT, PE, and sudden death, and the outcomes of mortality and bleeding (Table 2). This was based on a paucity of available data, and a moderate risk of bias in the reviewed studies. Additionally, 92% of the enrolled patients in the studies were white, limiting the generalizability of the results to other ethnic groups.
Patients on Antiplatelets
The strength of evidence was insufficient in the studies reviewed here to conclude that there is no difference in rates of bleeding in patients who are concomitantly taking antiplatelet drugs while getting VTE prophylaxis with rivaroxaban, dabigatran, or enoxaparin. We based this rating because of the imprecision of results and unknown consistencies across multiple studies.
Patients With Renal Insufficiency
One RCT had a high risk of bias for our key question because data from only 1 study arm were useful for our review.[16] The other RCTs were judged to have a moderate risk of bias. The analyses led by Dahl and Shorr[18, 19] were based on post hoc (ie, not prespecified) analysis of data from RCTs. Additionally, outcomes in the Shorr et al. trial were reported for evaluable subpopulations of the cohort that was initially randomized in the clinical trial.
We rated the strength of evidence as insufficient to know the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE during hospitalization of patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, and patients receiving dialysis. We based this rating on the risk of bias associated with published studies and a lack of consistent evidence regarding associations that were reported. Similarly, we rated the strength of evidence as insufficient that 5000 U of unfractionated heparin 3 times daily increases the risk of major and minor bleeding events in patients with severely compromised renal function compared to this dose in patients without severely compromised renal function. We based this rating on a high risk of bias of included studies and inconsistent evidence. Likewise, we rated the strength of evidence as insufficient that enoxaparin significantly increases the risk of major bleeding compared with unfractionated heparin in patients with severe renal insufficiency. We based this rating on a high risk of bias and inconsistent published evidence.
We similarly found insufficient evidence to guide treatment decisions for patients with renal insufficiency. Our findings are consistent with other recent reviews. The American College of Chest Physicians (ACCP) practice guidelines[21] make dosing recommendations for the therapeutic use of enoxaparin. However, their assessment is that the data are insufficient to make direct recommendations about prophylaxis. Their assessment of the indirect evidence regarding bioaccumulation and increased anti‐factor Xa levels are consistent with ours. The ACCP guidelines also suggest that decreased clearance of enoxaparin has been associated with increased risk of bleeding events for patients with severe renal insufficiency. However, the cited study[20] compares patients with and without severe renal dysfunction who received the same therapy. Therefore, it is not possible to determine the additional risk conveyed by enoxaparin therapy, that is, above the baseline increased risk of bleeding among patients with renal insufficiency, particularly those receiving an alternate pharmacologic VTE prevention strategy, such as unfractionated heparin.
DISCUSSION
We found that the evidence was very limited about prevention of VTE in these select and yet prevalent patient populations. Despite the fact that there is an increasing number of obese patients and patients who are on antiplatelet therapies, most clinical practice guidelines do not address the care of these populations, which may be entirely appropriate given the state of the evidence.
The ACCP practice guidelines[21] suggest using a higher dose of enoxaparin for the prevention of VTE in obese patients. The subgroup analysis by Kucher et al.[11] showed effect attenuation of dalteparin when given at a fixed dose of 5000 IU/mL to patients with a BMI of >40 kg/m2. The Freeman study[12] showed that extremely obese patients (average BMI >62.1 kg/m2) who are given a fixed dose of enoxaparin achieved target anti‐factor Xa levels significantly less often than those who received a higher dose of enoxaparin. The 2 separate findings, although not conclusive, lend some credence to the current ACCP guidelines.[21]
The studies we reviewed on VTE prophylaxis in patients who are concomitantly on antiplatelets including aspirin reported no major increased risk of bleeding; however, in the Friedman et al. study,[15] 3.0% of patients who were put on enoxaparin while still on aspirin had a bleeding event compared to 1.2% of those on enoxaparin alone. This difference is not statistically significant but is a trend possibly worth noting, especially when one looks at the lower RR of bleeding at 0.55 compared to 0.82 when dabigatran is compared with enoxaparin with and without concomitant aspirin therapy, respectively (Table 1). The highest dose of aspirin used in either of the studies was 160 mg/day, and neither study addressed other potent antiplatelets such as clopidogrel or ticlopidine separately, which limits the generalizability of the finding to all antiplatelets. Current ACCP guidelines do not recommend aspirin as a sole option for the prevention of VTE in orthopedic surgery patients.[22] Concerns remain among clinicians that antiplatelets, including aspirin, on their own are unlikely to be fully effective to thwart venous thrombotic processes for most patients, and yet the risk of bleeding is not fully known when these agents are combined with other anticoagulants for VTE prophylaxis.
Our review has several limitations, including the possibility that we may have missed some observational studies, as the identification of relevant observational studies in electronic searches is more challenging than that of RCTs. The few studies made it impossible to quantitatively pool results. These results, however, have important implications, namely that additional research on the comparative effectiveness and safety of pharmacologic and mechanical strategies to prevent VTE is needed for the optimal care of these patient subgroups. This might be achieved with trials dedicated to enrolling these patients or prespecified subgroup analyses within larger trials. Observational data may be appropriate as long as attention is paid to confounding.
APPENDIX
MEDLINE Search Strategy
((pulmonary embolism[mh] OR PE[tiab] OR Pulmonary embolism[tiab] OR thromboembolism[mh] OR thromboembolism[tiab] OR thromboembolisms[tiab] OR Thrombosis[mh] OR thrombosis[tiab] OR DVT[tiab] OR VTE[tiab] OR clot[tiab]) AND (Anticoagulants[mh] OR Anticoagulants[tiab] OR Anticoagulant[tiab] OR thrombin inhibitors[tiab] OR Aspirin[mh] or aspirin[tiab] OR aspirins[tiab] or clopidogrel[nm] OR clopidogrel[tiab] OR Plavix[tiab] or ticlopidine[mh] or ticlopidine[tiab]OR ticlid[tiab] OR prasugrel[nm]Or prasugrel[tiab]OR effient[tiab]OR ticagrelor[NM] OR ticagrelor[tiab]OR Brilinta[tiab] OR cilostazol[NM] OR cilostazol[tiab]OR pletal[tiab] OR warfarin[mh]OR warfarin[tiab]OR coumadin[tiab] OR coumadine[tiab] OR Dipyridamole[mh]OR dipyridamole[tiab]OR persantine[tiab] OR dicoumarol[MH] OR dicoumarol[tiab] OR dicumarol[tiab] OR Dextran sulfate[mh] OR dextran sulfate[tiab] ORthrombin inhibitors[tiab] OR thrombin inhibitor[tiab] OR heparin[mh] OR Heparin[tiab] OR Heparins[tiab] OR LMWH[tiab] OR LDUH[tiab] OR Enoxaparin[mh] OR Enoxaparin[tiab] OR Lovenox[tiab] OR Dalteparin[tiab] OR Fragmin[tiab] OR Tinzaparin[tiab] OR innohep[tiab] OR Nadroparin[tiab] OR Fondaparinux[nm] OR Fondaparinux[tiab] OR Arixtra[tiab] OR Idraparinux[nm] OR Idraparinux[tiab] OR Rivaroxaban[nm] OR Rivaroxaban[tiab] OR novastan[tiab] OR Desirudin[nm] OR Desirudin[tiab] OR Iprivask[tiab]OR direct thrombin inhibitor[tiab] OR Argatroban[nm] OR Argatroban[tiab] OR Acova[tiab] OR Bivalirudin[nm] OR Bivalirudin[tiab] OR Angiomax[tiab] OR Lepirudin[nm] OR Lepirudin[tiab] OR Refludan[tiab] OR Dabigatran[nm] OR Dabigatran[tiab] OR Pradaxa[tiab] OR factor xa[mh] OR factor Xa[tiab] OR vena cava filters[mh] OR filters[tiab] OR filter[tiab] OR compression stockings[mh] OR intermittent pneumatic compression devices[mh] OR compression [tiab] OR Venous foot pump[tiab])) AND(prevent*[tiab] OR prophyla*[tiab] OR prevention and control[subheading]) NOT (animals[mh] NOT humans[mh]) NOT (editorial[pt] OR comment[pt]) NOT ((infant[mh] OR infant[tiab] OR child[mh] OR child[tiab] OR children[tiab] OR adolescent[mh] OR adolescent[tiab] OR teen‐age[tiab] OR pediatric[tiab] OR perinatal[tiab]) NOT (adult[tiab] OR adults[tiab] OR adult[mh])) NOT (mechanical valve[tiab] OR heart valve[tiab] OR atrial fibrillation[mh] OR atrial fibrillation[tiab] OR thrombophilia[mh] OR thrombophilia[tiab] OR pregnancy[mh])
Venous thromboembolism (VTE), including deep venous thrombosis (DVT) and pulmonary embolism (PE), is estimated to affect 900,000 Americans each year and is a cause of significant morbidity and mortality with associated high healthcare costs.[1] Accordingly, the comparative effectiveness and safety of interventions for the prevention and treatment of VTE are among the national priorities for comparative effectiveness research.[2] Whereas we have evidence‐based guidelines for the prophylaxis of VTE in the general population, there are no guidelines informing the care of select patient populations. Select populations are those patients in whom there is decisional uncertainty about the optimal choice, timing, and dose of VTE prophylaxis. Not only do these patients have an increased risk of DVT and PE, but most are also at high risk of bleeding, the most important complication of VTE prophylaxis.[3, 4, 5, 6]
The objectives of this systematic review were to define the comparative effectiveness and safety of pharmacologic and mechanical strategies for VTE prevention in some of these select medical populations including obese patients, patients on concomitant antiplatelet therapy, patients with renal insufficiency, patients who are underweight, and patients with coagulopathy due to liver disease.
METHODS
The methods for this comparative effectiveness review (CER) follow the guidelines suggested in the Agency for Healthcare Research and Quality (AHRQ) Methods Guide for Effectiveness and Comparative Effectiveness Reviews.[7] The protocol was publically posted.[8]
Search Strategy
We searched MEDLINE, EMBASE, and SCOPUS through August 2011, CINAHL, International Pharmaceutical Abstracts,
Study Selection
We reviewed titles followed by abstracts to identify randomized controlled trials (RCTs) or observational studies with comparison groups reporting on the effectiveness or safety of VTE prevention in our populations. Two investigators independently reviewed abstracts, and we excluded the abstracts if both investigators agreed that the article met 1 or more of the exclusion criteria. We included only English‐language articles that evaluated the effectiveness of pharmacological or mechanical interventions that have been approved for clinical use in the United States. To be eligible, the studies must have addressed relevant key questions in the population of our interest. We resolved disagreements by consensus. We used DistillerSR (Evidence Partners Inc., Ottawa, Ontario, Canada), a Web‐based database management program to manage the review process. Two investigators assessed the risk of bias in each study independently, using the Downs and Black instrument for observational studies and trials.[10]
Data Synthesis
For each select population, we created detailed evidence tables containing the information abstracted from the eligible studies. After synthesizing the evidence, we graded the quantity, quality, and consistency of the best available evidence for each select population by adapting an evidence‐grading scheme recommended in the Methods Guide for Conducting Comparative Effectiveness Reviews.[7]
RESULTS
We identified 30,902 unique citations and included 9 studies (Figure 1). There were 5 RCTs with relevant subgroups and 4 observational studies (Table 1). Two studies reported on the risk of bleeding in patients given pharmacologic prophylaxis while they are concomitantly taking nonsteroidal anti‐inflammatory drugs (NSAIDS) or antiplatelet agents/aspirin, 1 RCT and 1 prospective observational study reported on obese patients, and 5 studies described outcomes of patients with renal insufficiency (see Supporting Information, Table 1, in the online version of this article). No study tested prophylaxis in underweight patients or those with liver disease.

| Study | Arm, n | Total VTE (DVT and PE) | Bleeding | Other Outcomes | |
|---|---|---|---|---|---|
| |||||
| Obese patients | |||||
| Kucher et al., 2005[11] | Arm 1 (dalteparin), 558 | 2.8% (95% CI: 1.34.3) | 0% | Mortality at 21 days: 4.6% | |
| Arm 2 (placebo), 560 | 4.3% (95% CI: 2.56.2) | 0.7% | Mortality at 21 days: 2.7% | ||
| Freeman et al., [12] | Arm 1 (fixed‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 19 % | |
| Arm 2 (lower‐dose enoxaparin), 9 | NR | NR | Peak anti‐factor Xa level 32 % | ||
| Arm 3 (higher‐dose enoxaparin), 11 | NR | NR | Peak anti‐factor Xa level 86 % | ||
| Patients on antiplatelet agents | |||||
| Eriksson et al., 2012[14] | Arm 1 (rivaroxaban), 563 | NR | 20 (3.6%), rate ratio for use vs nonuse: 1.32 (95% CI: 0.85‐2.05) | NR | |
| Arm 2 (enoxaparin/placebo), 526 | NR | 17 (3.2%), rate ratio for use vs nonuse: 1.40 (95% CI: 0.87‐2.25) | NR | ||
| Friedman et al., 2012[15] | Arm 2 (150 mg dabigatran, no ASA), 1149 | NR | 11 (1.0%)a | NR | |
| Arm 5 (150 mg dabigatran+ASA), 128 | NR | 2 (1.6%)a | NR | ||
| Arm 3 (enoxaparin, no ASA), 1167 | NR | 14 (1.2%)a | NR | ||
| Arm 6 (enoxaparin+ASA), 132 | NR | 4 (3.0%) | NR | ||
| 150 mg dabigatran compared with enoxaparinNo concomitant ASA therapy | NR | RR: 0.82 (95% CI: 0.37‐1.84) | NR | ||
| 150 mg dabigatran compared with enoxaparinWith concomitant ASA therapy | NR | RR: 0.55 (95% CI: 0.11‐2.78) | NR | ||
| Patients with renal insufficiency | |||||
| Bauersachs et al., 2011[16] | Arm 2 (GFR <30), 92 | Total DVT: 11.11%; Total PE: 0% | Major bleeding: 4/92 (4.35%), minor bleeding: 9/92 (9.78%) | Mortality: 5.81% | |
| Mah et al., 2007[17] | Arm 2 (tinzaparin), 27 | NR | Major bleeding: 2/27 (7.4%), minor bleeding: 3/27 (11.1%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.05 | |
| Arm 3 (enoxaparin), 28 | NR | Major bleeding: 1/28 (3.6%), minor bleeding: 3/28 (10.7%) | Factor Xa level: AF: CmaxD8/Cmax D1=1.22 | ||
| Dahl et al., 2012[18] | Arm 1 (enoxaparin), 332 | Major VTE: 8 (9.0%) | Major bleeding: 6 (4.7%) | Infections and infestations: 25 (7.5%), Wound infection: 4 (1.2%) | |
| Arm 2 (dabigatran), 300 | Major VTE: 3 (4.3%) | Major bleeding: 0 (0%) | Infections and infestations: 21 (7.0%), Wound Infection: 3 (1.0%) | ||
| Shorr et al., 2012[19] | Arm 1 (enoxaparin, CrCL 60 mL/min), 353 | Total VTE: 17/275 (6.2%) | Major bleeding: 0/351 (0%) | NR | |
| Arm 2 (desirudin, CrCL 60 mL/min), 353 | Total VTE: 13/284 (4.3%) | Major bleeding: 2/349 (0.27%) | NR | ||
| Arm 3 (enoxaparin, CrCL 4559 mL/min), 369 | Total VTE: 18/282 (6.2%) | Major bleeding: 1/365 (0.27%) | NR | ||
| Arm 4 (desirudin, CrCL 4559 mL/min), 395 | Total VTE: 17/303 (5.6%) | Major bleeding: 1/393 (0.25%) | NR | ||
| Arm 5 (enoxaparin, CrCL <45 mL/min), 298 | Total VTE: 24/216 (11.1%) | Major bleeding: 1/294 (0.34%) | NR | ||
| Arm 6 (desirudin, CrCL <45 mL/min), 279 | Total VTE: 7/205 (3.4%) | Major bleeding: 5/275 (1.82%) | NR | ||
| Elsaid et al., 2012[20] | Arm 1 (enoxaparin, CrCL 60 mL/min), 17 | NR | Major bleeding: 2 (11.8%) | NR | |
| Arm 2 (enoxaparin, CrCL 3059 mL/min), 86 | NR | Major bleeding: 9 (10.5%) | NR | ||
| Arm 3 (enoxaparin, CrCL 30 mL/min), 53 | NR | Major bleeding: 10 (18.9%) | NR | ||
| Arm 4 (UFH, CrCL 60 mL/min), 19 | NR | Major bleeding: 2 (10.5%) | NR | ||
| Arm 5 (UFH, CrCL 3059 mL/min), 99 | NR | Major bleeding: 3 (3%) | NR | ||
| Arm 6 (UFH, CrCL 30 mL/min), 49 | NR | Major bleeding: 2 (4.1%) | NR | ||
Obese Patients
We found 1 subgroup analysis of an RCT (total 3706 patients, 2563 nonobese and 1118 obese patients) that reported on the comparative effectiveness and safety of fixed low‐dose dalteparin 5000 IU/day compared to placebo among 1118 hospitalized medically ill patients with body mass indices (BMI) greater than 30 kg/m2.11 Neither group received additional concurrent prophylactic therapies. The 3 most prevalent medical diagnoses prompting hospitalization were congestive heart failure, respiratory failure, and infectious diseases. Compression ultrasound was performed in all patients by day 21 of hospitalization. The primary end point was the composite of VTE, fatal PE, and sudden death, and secondary end points included DVT, bleeding, and thrombocytopenia by day 21 (Table 1). In obese patients, the primary end point occurred in 2.8% (95% confidence interval [CI]: 1.34.3) of the dalteparin group and in 4.3% (95% CI: 2.56.2) of the placebo group (relative risk [RR]: 0.64; 95% CI: 0.32‐1.28). In nonobese patients, the primary end point occurred in 2.8% (95% CI: 1.8‐3.8) and 5.2% (95% CI: 3.9‐6.6) of the dalteparin and placebo groups, respectively (RR: 0.53; 95% CI: 0.34‐0.82). When weight was modeled as a continuous variable, no statistically significant interaction between weight and dalteparin efficacy was observed (P=0.97). The authors calculated the RR in predefined BMI subgroups and found that dalteparin was effective in reducing VTE in patients with BMIs up to 40, with RRs of <1.0 for all (approximate range, 0.20.8). However, a fixed dose of dalteparin 5000 IU/day was not better than placebo for individuals with BMI >40 kg/m2. There was no significant difference in mortality or major hemorrhage by day 21 between treatment and placebo groups.
Freeman and colleagues prospectively assigned 31 medically ill patients with extreme obesity (BMI >40 kg/m2) to 1 of 3 dosing regimens of enoxaparin: a fixed dose of 40 mg daily enoxaparin (control group, n=11), enoxaparin at 0.4 mg/kg (n=9), or enoxaparin at 0.5 mg/kg (n=11).[12] The average BMI of the entire cohort was 62.1 kg/m2 (range, 40.582.4). All patients had anti‐factor Xa levels drawn on the day of enrollment and daily for 3 days (Table 2). The relationship between anti‐factor Xa levels and clinical efficacy of low‐molecular weight heparin (LMWH) in VTE prophylaxis is still unclear; however, an anti‐factor Xa level of 0.2 to 0.5 IU/mL, measured 4 hours after the fourth dose of LMWH, is the target level recommended for VTE prophylaxis.[13] Patients who received weight‐based enoxaparin at 0.5mg/kg achieved target anti‐factor Xa level 86% of the time compared to 32% of the time in those receiving 0.4 mg/kg and 19% of the time for those in the fixed‐dose group (P<0.001). No clinical outcomes were reported in this study.
| Intervention | Outcome | Risk of Bias | Evidence Statement and Magnitude of Effect |
|---|---|---|---|
| |||
| Patients on antiplatelet agents | |||
| Rivaroxaban vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic rivaroxaban or enoxaparin in patients concomitantly treated with antiplatelet agents; 3.6% vs 3.25% |
| Dabigatran vs enoxaparin | Major bleeding | Low | Insufficient to support no difference in rates of major bleeding with prophylactic dabigatran or enoxaparin in patients concomitantly treated with aspirin; 1.6% vs 3.0% |
| Obese patients | |||
| Dalteparin vs placebo | VTE | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing total VTE in obese patients; 2.8% vs 4.3%, RR: 0.64, 95% CI: 0.32‐1.28 |
| Dalteparin vs placebo | Mortality | Moderate | Insufficient evidence for effectiveness of dalteparin vs placebo in reducing mortality in obese patients; 9.9% vs 8.6%, P=0.36 |
| Dalteparin vs placebo | Major bleeding | Moderate | Insufficient evidence for safety of dalteparin vs placebo in reducing major bleeding in obese patients; 0% vs 0.7%, P>0.99 |
| Enoxaparin 40 mg daily vs 0.4 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.4 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 32%, P=NR |
| Enoxaparin 40 mg daily vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 40 mg daily versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 19% vs 86%, P<0.001 |
| Enoxaparin 0.4 mg/kg vs 0.5 mg/kg | Percentage of patients achieving target anti‐factor Xa level | Moderate | Insufficient evidence for effectiveness of enoxaparin 0.4 mg/kg versus 0.5 mg/kg in achieving peak anti‐factor Xa level in obese patients; 32% vs 86%, P=NR |
| Patients with renal insufficiency | |||
| Tinzaparin vs enoxaparin | VTE | High | Insufficient evidence about superiority of either drug for preventing VTE in patients with renal insufficiency, 0/27 vs 0/28* |
| Tinzaparin vs enoxaparin | Bleeding | High | Insufficient evidence about safety of either drug in patients with renal insufficiency; 5/27 vs 4/28, P=0.67 |
| Dabigatran vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of dabigatran in reducing VTE in severe renal compromise patients vs enoxaparin; 4.3% vs 9%, OR: 0.48, 95% CI: 0.13‐1.73, P=0.271 |
| Dabigatran vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of dabigatran vs enoxaparin in patients with renal impairment; 0 vs 4.7%, P=0.039 |
| Desirudin vs enoxaparin | VTE | Moderate | Insufficient evidence for effectiveness of desirudin vs enoxaparin in reducing VTE in patients with renal impairment; 4.9% vs 7.6%, P=0.019 |
| Desirudin vs enoxaparin | Bleeding | Moderate | Insufficient evidence for safety of desirudin vs enoxaparin in patients with renal impairment; 0.8% vs 0.2%, P=0.109 |
| Enoxaparin vs UFH | Bleeding | High | Insufficient evidence for increased risk of bleeding with enoxaparin vs unfractionated heparin in patients with all levels of renal impairment, 13.5% vs 4.2%, RR: 3.2, 95% CI: 1.47.3; and for the subgroup of patients with creatinine clearance <30 mL/min; 18.9% vs 4.1%, RR: 4.68, 95% CI: 1.120.6 |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | VTE | Moderate | Insufficient evidence regarding differential benefit of unfractionated heparin by renal function; 2.6% of patients had a VTE event |
| UFH in severe renal compromise vs all other renal status (undifferentiated) | Bleeding | Moderate | Insufficient evidence for differential harm from unfractionated heparin by renal function; 13 events in 92 patients |
Patients on Antiplatelet Drugs
We did not find studies that directly looked at the comparative effectiveness of VTE prophylaxis in patients who were on antiplatelet drugs including aspirin. However, there were 2 studies that looked at the risk of bleeding in patients who received VTE pharmacologic prophylaxis while concurrently taking antiplatelet agents including aspirin. Both studies used pooled data from large phase III trials.
The study by Eriksson et al. used data from the RECORD (Regulation of Coagulation in Orthopedic Surgery to Prevent Deep Venous Thrombosis and Pulmonary Embolism) trial where over 12,000 patients undergoing elective total knee or hip replacement were randomized to receive VTE prophylaxis with oral rivaroxaban or subcutaneous enoxaparin.[14] Nine percent of participants in each arm (563 in rivaroxaban and 526 in enoxaparin/placebo) were concomitantly using antiplatelet agents or aspirin at least once during the at risk period, defined as starting at day 1 of surgery up to 2 days after the last intake of the study drug. The only end point evaluated was bleeding, and the authors found no statistically significant bleeding difference among the 2 arms (Table 1). Any bleeding event in the rivaroxaban with antiplatelets or aspirin arm was found in 20 (3.6%) patients, whereas in those on enoxaparin/placebo with antiplatelets or aspirin arm it was 17 (3.2%). The relative rate of bleeding among users versus nonusers of antiplatelet drugs or aspirin was 1.32 (95% CI: 0.85‐2.05) in the rivaroxaban group and 1.40 (95% CI: 0.87‐2.25) in the enoxaparin arm (Table 1).
Friedman et al. used pooled data from the RE‐MODEL, RENOVATE, and REMOBILIZE trials, where patients who were undergoing hip or knee arthroplasty were randomized to 220 mg of dabigatran once daily, 150 mg of dabigatran once daily (we focused on this lower dosage as this is the only available dose used in the US), 40 mg of enoxaparin once daily, or 30 mg of enoxaparin twice a day.[15] Of the 8135 patients, 4.7% were on concomitant aspirin. The baseline characteristics of those on aspirin were similar to the other enrollees. The primary outcome was major bleeding events requiring transfusion, symptomatic internal bleeding, or bleeding requiring surgery. Among patients receiving 150 mg of dabigatran, bleeding events with and without concomitant aspirin occurred in 1.6% and 1.0%, respectively (odds ratio [OR]: 1.64; 95% CI: 0.36‐7.49; P=0.523). The percentages of participants with bleeding who received enoxaparin, with and without aspirin, were 3.0% and 1.2%, respectively (OR: 2.57; 95% CI: 0.83‐7.94; P=0.101). The RR of bleeding on dabigatran compared to enoxaparin with and without aspirin therapy was 0.55 (95% CI: 0.11‐2.78) and 0.82 (95% CI: 0.37‐1.84), respectively (Table 1).
Patients With Renal Insufficiency
We found 5 studies that evaluated the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE in patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, or patients receiving dialysis. Four studies were RCTs,[16, 17, 18, 19] and 1 used a cohort design assessing separate cohorts before and after a quality improvement intervention.[20] Bauersachs and colleagues conducted an RCT comparing unfractionated heparin at 5000 IU, 3 times daily to certoparin, which is not approved in the United States and is not further discussed here.[16] The rate of DVT among patients treated with unfractionated heparin in patients with a glomerular filtration rate >30 mL/min was marginally lower than those with severe renal dysfunction (10.3 vs 11.1%) (Table 1).
Patients with severe renal dysfunction who received 5000 IU of unfractionated heparin 3 times a day were at increased risk of all bleeds (RR: 3.4; 95% CI: 2.05.9), major bleeds (RR: 7.3; 95% CI: 3.316), and minor bleeds (RR: 2.6; 95% CI: 1.4‐4.9) compared to patients treated with unfractionated heparin without severe renal dysfunction.[16]
A randomized trial by Mah and colleagues compared drug accumulation and anti‐Xa activity in elderly patients with renal dysfunction (defined as a glomerular filtration rate of 20 to 50 mL/min) who received either tinzaparin at 4500 IU once daily or enoxaparin at 4000 IU once daily.[17] Enoxaparin accumulated to a greater extent from day 1 to day 8 than did tinzaparin; the ratio of maximum concentration on day 8 compared to day 1 was 1.22 for enoxaparin and 1.05 for tinzaparin (P=0.016). No VTE events were reported in patients who received tinzaparin or enoxaparin. There was no statistical difference in the incidence of bleeding events between patients receiving tinzaparin (5, including 2 major events) and enoxaparin (4, including 3 major events, P=0.67) (Table 1).
The trial by Dahl and colleagues randomly assigned patients who were over 75 years of age and/or who had moderate renal dysfunction (defined as creatinine clearance between 30 and 49 mL/min) to receive enoxaparin 40 mg daily or dabigatran 150 mg daily.[18] There was no significant difference in the rate of major VTE events between patients receiving dabigatran (4.3%) and enoxaparin (9%) (OR: 0.48; 95% CI: 0.13‐1.73; P=0.271) (Table 1). The rate of major bleeding was significantly higher among patients randomly assigned to receive enoxaparin (4.7%) versus dabigatran (0%) (P=0.039).[18]
Shorr and colleagues published a post hoc subgroup analysis of a multicenter trial in which orthopedic patients were randomly assigned to receive desirudin 15 mg twice daily or enoxaparin 40 mg once daily.[19] Evaluable patients (1565 of the 2079 patients randomized in the trial) receiving desirudin experienced a significantly lower rate of major VTE compared with patients receiving enoxaparin (4.9% vs 7.6%, P=0.019). This relationship was particularly pronounced for evaluable patients whose creatinine clearance was between 30 and 44 mL/min. In evaluable patients with this degree of renal dysfunction, 11% of patients taking enoxaparin compared to 3.4% of those taking desirudin had a major VTE (OR: 3.52; 95% CI: 1.48‐8.4; P=0.004). There was no significant difference in the rates of major bleeding among a subset of patients assessed for safety outcomes (2078 of the 2079 patients randomized in the trial) who received desirudin (0.8%) or enoxaparin (0.2%) (Table 1).
Elsaid and Collins assessed VTE and bleeding events associated with the use of unfractionated heparin 5000U either 2 or 3 times daily and enoxaparin 30 mg once or twice daily across patients stratified by renal function (creatinine clearance <30, 3059, and 60 mL/min). The investigators made assessments before and after a quality improvement intervention that was designed to eliminate the use of enoxaparin in patients whose creatinine clearance was <30 mL/min. No VTE events were reported. Patients receiving enoxaparin were significantly more likely to experience a major bleeding episode compared with patients receiving unfractionated heparin (overall rates for all levels of renal function: 13.5% vs 4. 2%; RR: 3.2; 95% CI: 1.47.3) (Table 2). This association was largely driven by the subgroup of patients with a creatinine clearance <30 mL/min. For this subgroup with severe renal insufficiency, patients receiving enoxaparin were significantly more likely to have a bleed compared with patients receiving unfractionated heparin (18.9% vs 4.1%; RR: 4.68; 95% CI: 1.120.6) (Tables 1 and 2). There was no difference in the bleeding rates for patients whose creatinine clearances were >60 mL/min.[20]
Strength of Evidence
Obese Patients
Overall, we found that the strength of evidence was insufficient regarding the composite end point of DVT, PE, and sudden death, and the outcomes of mortality and bleeding (Table 2). This was based on a paucity of available data, and a moderate risk of bias in the reviewed studies. Additionally, 92% of the enrolled patients in the studies were white, limiting the generalizability of the results to other ethnic groups.
Patients on Antiplatelets
The strength of evidence was insufficient in the studies reviewed here to conclude that there is no difference in rates of bleeding in patients who are concomitantly taking antiplatelet drugs while getting VTE prophylaxis with rivaroxaban, dabigatran, or enoxaparin. We based this rating because of the imprecision of results and unknown consistencies across multiple studies.
Patients With Renal Insufficiency
One RCT had a high risk of bias for our key question because data from only 1 study arm were useful for our review.[16] The other RCTs were judged to have a moderate risk of bias. The analyses led by Dahl and Shorr[18, 19] were based on post hoc (ie, not prespecified) analysis of data from RCTs. Additionally, outcomes in the Shorr et al. trial were reported for evaluable subpopulations of the cohort that was initially randomized in the clinical trial.
We rated the strength of evidence as insufficient to know the comparative effectiveness and safety of pharmacologic prophylaxis for prevention of VTE during hospitalization of patients with acute kidney injury, moderate renal insufficiency, severe renal insufficiency not undergoing dialysis, and patients receiving dialysis. We based this rating on the risk of bias associated with published studies and a lack of consistent evidence regarding associations that were reported. Similarly, we rated the strength of evidence as insufficient that 5000 U of unfractionated heparin 3 times daily increases the risk of major and minor bleeding events in patients with severely compromised renal function compared to this dose in patients without severely compromised renal function. We based this rating on a high risk of bias of included studies and inconsistent evidence. Likewise, we rated the strength of evidence as insufficient that enoxaparin significantly increases the risk of major bleeding compared with unfractionated heparin in patients with severe renal insufficiency. We based this rating on a high risk of bias and inconsistent published evidence.
We similarly found insufficient evidence to guide treatment decisions for patients with renal insufficiency. Our findings are consistent with other recent reviews. The American College of Chest Physicians (ACCP) practice guidelines[21] make dosing recommendations for the therapeutic use of enoxaparin. However, their assessment is that the data are insufficient to make direct recommendations about prophylaxis. Their assessment of the indirect evidence regarding bioaccumulation and increased anti‐factor Xa levels are consistent with ours. The ACCP guidelines also suggest that decreased clearance of enoxaparin has been associated with increased risk of bleeding events for patients with severe renal insufficiency. However, the cited study[20] compares patients with and without severe renal dysfunction who received the same therapy. Therefore, it is not possible to determine the additional risk conveyed by enoxaparin therapy, that is, above the baseline increased risk of bleeding among patients with renal insufficiency, particularly those receiving an alternate pharmacologic VTE prevention strategy, such as unfractionated heparin.
DISCUSSION
We found that the evidence was very limited about prevention of VTE in these select and yet prevalent patient populations. Despite the fact that there is an increasing number of obese patients and patients who are on antiplatelet therapies, most clinical practice guidelines do not address the care of these populations, which may be entirely appropriate given the state of the evidence.
The ACCP practice guidelines[21] suggest using a higher dose of enoxaparin for the prevention of VTE in obese patients. The subgroup analysis by Kucher et al.[11] showed effect attenuation of dalteparin when given at a fixed dose of 5000 IU/mL to patients with a BMI of >40 kg/m2. The Freeman study[12] showed that extremely obese patients (average BMI >62.1 kg/m2) who are given a fixed dose of enoxaparin achieved target anti‐factor Xa levels significantly less often than those who received a higher dose of enoxaparin. The 2 separate findings, although not conclusive, lend some credence to the current ACCP guidelines.[21]
The studies we reviewed on VTE prophylaxis in patients who are concomitantly on antiplatelets including aspirin reported no major increased risk of bleeding; however, in the Friedman et al. study,[15] 3.0% of patients who were put on enoxaparin while still on aspirin had a bleeding event compared to 1.2% of those on enoxaparin alone. This difference is not statistically significant but is a trend possibly worth noting, especially when one looks at the lower RR of bleeding at 0.55 compared to 0.82 when dabigatran is compared with enoxaparin with and without concomitant aspirin therapy, respectively (Table 1). The highest dose of aspirin used in either of the studies was 160 mg/day, and neither study addressed other potent antiplatelets such as clopidogrel or ticlopidine separately, which limits the generalizability of the finding to all antiplatelets. Current ACCP guidelines do not recommend aspirin as a sole option for the prevention of VTE in orthopedic surgery patients.[22] Concerns remain among clinicians that antiplatelets, including aspirin, on their own are unlikely to be fully effective to thwart venous thrombotic processes for most patients, and yet the risk of bleeding is not fully known when these agents are combined with other anticoagulants for VTE prophylaxis.
Our review has several limitations, including the possibility that we may have missed some observational studies, as the identification of relevant observational studies in electronic searches is more challenging than that of RCTs. The few studies made it impossible to quantitatively pool results. These results, however, have important implications, namely that additional research on the comparative effectiveness and safety of pharmacologic and mechanical strategies to prevent VTE is needed for the optimal care of these patient subgroups. This might be achieved with trials dedicated to enrolling these patients or prespecified subgroup analyses within larger trials. Observational data may be appropriate as long as attention is paid to confounding.
APPENDIX
MEDLINE Search Strategy
((pulmonary embolism[mh] OR PE[tiab] OR Pulmonary embolism[tiab] OR thromboembolism[mh] OR thromboembolism[tiab] OR thromboembolisms[tiab] OR Thrombosis[mh] OR thrombosis[tiab] OR DVT[tiab] OR VTE[tiab] OR clot[tiab]) AND (Anticoagulants[mh] OR Anticoagulants[tiab] OR Anticoagulant[tiab] OR thrombin inhibitors[tiab] OR Aspirin[mh] or aspirin[tiab] OR aspirins[tiab] or clopidogrel[nm] OR clopidogrel[tiab] OR Plavix[tiab] or ticlopidine[mh] or ticlopidine[tiab]OR ticlid[tiab] OR prasugrel[nm]Or prasugrel[tiab]OR effient[tiab]OR ticagrelor[NM] OR ticagrelor[tiab]OR Brilinta[tiab] OR cilostazol[NM] OR cilostazol[tiab]OR pletal[tiab] OR warfarin[mh]OR warfarin[tiab]OR coumadin[tiab] OR coumadine[tiab] OR Dipyridamole[mh]OR dipyridamole[tiab]OR persantine[tiab] OR dicoumarol[MH] OR dicoumarol[tiab] OR dicumarol[tiab] OR Dextran sulfate[mh] OR dextran sulfate[tiab] ORthrombin inhibitors[tiab] OR thrombin inhibitor[tiab] OR heparin[mh] OR Heparin[tiab] OR Heparins[tiab] OR LMWH[tiab] OR LDUH[tiab] OR Enoxaparin[mh] OR Enoxaparin[tiab] OR Lovenox[tiab] OR Dalteparin[tiab] OR Fragmin[tiab] OR Tinzaparin[tiab] OR innohep[tiab] OR Nadroparin[tiab] OR Fondaparinux[nm] OR Fondaparinux[tiab] OR Arixtra[tiab] OR Idraparinux[nm] OR Idraparinux[tiab] OR Rivaroxaban[nm] OR Rivaroxaban[tiab] OR novastan[tiab] OR Desirudin[nm] OR Desirudin[tiab] OR Iprivask[tiab]OR direct thrombin inhibitor[tiab] OR Argatroban[nm] OR Argatroban[tiab] OR Acova[tiab] OR Bivalirudin[nm] OR Bivalirudin[tiab] OR Angiomax[tiab] OR Lepirudin[nm] OR Lepirudin[tiab] OR Refludan[tiab] OR Dabigatran[nm] OR Dabigatran[tiab] OR Pradaxa[tiab] OR factor xa[mh] OR factor Xa[tiab] OR vena cava filters[mh] OR filters[tiab] OR filter[tiab] OR compression stockings[mh] OR intermittent pneumatic compression devices[mh] OR compression [tiab] OR Venous foot pump[tiab])) AND(prevent*[tiab] OR prophyla*[tiab] OR prevention and control[subheading]) NOT (animals[mh] NOT humans[mh]) NOT (editorial[pt] OR comment[pt]) NOT ((infant[mh] OR infant[tiab] OR child[mh] OR child[tiab] OR children[tiab] OR adolescent[mh] OR adolescent[tiab] OR teen‐age[tiab] OR pediatric[tiab] OR perinatal[tiab]) NOT (adult[tiab] OR adults[tiab] OR adult[mh])) NOT (mechanical valve[tiab] OR heart valve[tiab] OR atrial fibrillation[mh] OR atrial fibrillation[tiab] OR thrombophilia[mh] OR thrombophilia[tiab] OR pregnancy[mh])
- , , . Estimated annual number of incident and recurrent, non‐fatal and fatal venous thromboembolism (VTE) events in the US. Blood. 2005;106:910.
- Institute of Medicine. Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academies Press; 2009.
- Lovenox (enoxaparin sodium injection for subcutaneous and intravenous use: prescribing information). Bridgewater, NJ: SanofiAventis; 2011. Available at: http://products.sanofi.us/lovenox/lovenox.html. Accessed October 17, 2012.
- Innohep (tinzaparin sodium injection). Ballerup, Denmark: LEO Pharmaceutical Products; 2008. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/020484s011lbl.pdf. Accessed October 17, 2012.
- Leizorovicz A. Tinzaparin compared to unfractionated heparin for initial treatment of deep vein thrombosis in very elderly patients with renal insufficiency‐ the IRIS trial. [50th ASH Annual Meeting and Exposition abstract 434]. Blood. 2008;11:112.
- Fragmin (dalteparin sodium injection). New York, NY: Pfizer Inc.; 2007. Available at: http://www.pfizer.com/files/products/uspi_fragmin.pdf. Accessed October 17, 2012.
- Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; August 2011. AHRQ publication No. 10 (11)‐EHC063‐EF. Available at: http://www.effectivehealthcare.ahrq.gov. Accessed October 17, 2012.
- Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/928/VTE‐Special‐Populations_Protocol_20120112.pdf. Accessed April 17, 2012.
- , , , et al. Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Evidence Report/Technology Assessment (AHRQ). Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/1501/venous‐thromboembolism‐special‐populations‐report‐130529.pdf. 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Efficacy and safety of fixed low‐dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med. 2005;165(3):341–345.
- , , , . Prospective comparison of three enoxaparin dosing regimens to achieve target anti‐factor Xa levels in hospitalized, medically ill patients with extreme obesity. Am J Hematol. 2012;87(7):740–743.
- , , . Effect of prophylactic dalteparin on anti‐factor xa levels in morbidly obese patients after bariatric surgery. Obes Surg. 2010;20(4):487–491.
- , , , , . Concomitant use of medication with antiplatelet effects in patients receiving either rivaroxaban or enoxaparin after total hip or knee arthroplasty. Thromb Res. 2012;130(2):147–151.
- , , , , , . Dabigatran etexilate and concomitant use of non‐steroidal anti‐inflammatory drugs or acetylsalicylic acid in patients undergoing total hip and total knee arthroplasty: No increased risk of bleeding. Thromb Haemost. 2012;108(1):183–190.
- , , , et al. CERTIFY: prophylaxis of venous thromboembolism in patients with severe renal insufficiency. Thromb Haemost. 2011;105(6):981–988.
- , , , et al. Tinzaparin and enoxaparin given at prophylactic dose for eight days in medical elderly patients with impaired renal function: a comparative pharmacokinetic study. Thromb Haemost. 2007;97(4):581–586.
- , , , , , . Thromboprophylaxis in patients older than 75 years or with moderate renal impairment undergoing knee or hip replacement surgery [published correction appears in Int Orthop. 2012;36(5):1113]. Int Orthop. 2012;36(4):741–748.
- , , , . Impact of stage 3B chronic kidney disease on thrombosis and bleeding outcomes after orthopedic surgery in patients treated with desirudin or enoxaparin: insights from a randomized trial. J Thromb Haemost. 2012;10(8):1515–1520.
- , . Initiative to improve thromboprophylactic enoxaparin exposure in hospitalized patients with renal impairment. Am J Health Syst Pharm. 2012;69(5):390–396.
- , , , , ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence‐based clinical practice guidelines. Chest. 2012;141(2 suppl):7S–47S.
- , . Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence. Ann Pharmacother. 2013;47(1):63–74.
- , , . Estimated annual number of incident and recurrent, non‐fatal and fatal venous thromboembolism (VTE) events in the US. Blood. 2005;106:910.
- Institute of Medicine. Institute of Medicine. Initial National Priorities for Comparative Effectiveness Research. Washington, DC: National Academies Press; 2009.
- Lovenox (enoxaparin sodium injection for subcutaneous and intravenous use: prescribing information). Bridgewater, NJ: SanofiAventis; 2011. Available at: http://products.sanofi.us/lovenox/lovenox.html. Accessed October 17, 2012.
- Innohep (tinzaparin sodium injection). Ballerup, Denmark: LEO Pharmaceutical Products; 2008. Available at: http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/020484s011lbl.pdf. Accessed October 17, 2012.
- Leizorovicz A. Tinzaparin compared to unfractionated heparin for initial treatment of deep vein thrombosis in very elderly patients with renal insufficiency‐ the IRIS trial. [50th ASH Annual Meeting and Exposition abstract 434]. Blood. 2008;11:112.
- Fragmin (dalteparin sodium injection). New York, NY: Pfizer Inc.; 2007. Available at: http://www.pfizer.com/files/products/uspi_fragmin.pdf. Accessed October 17, 2012.
- Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; August 2011. AHRQ publication No. 10 (11)‐EHC063‐EF. Available at: http://www.effectivehealthcare.ahrq.gov. Accessed October 17, 2012.
- Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/928/VTE‐Special‐Populations_Protocol_20120112.pdf. Accessed April 17, 2012.
- , , , et al. Comparative effectiveness of pharmacologic and mechanical prophylaxis of venous thromboembolism among special populations. Evidence Report/Technology Assessment (AHRQ). Available at: http://effectivehealthcare.ahrq.gov/ehc/products/341/1501/venous‐thromboembolism‐special‐populations‐report‐130529.pdf. 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Efficacy and safety of fixed low‐dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med. 2005;165(3):341–345.
- , , , . Prospective comparison of three enoxaparin dosing regimens to achieve target anti‐factor Xa levels in hospitalized, medically ill patients with extreme obesity. Am J Hematol. 2012;87(7):740–743.
- , , . Effect of prophylactic dalteparin on anti‐factor xa levels in morbidly obese patients after bariatric surgery. Obes Surg. 2010;20(4):487–491.
- , , , , . Concomitant use of medication with antiplatelet effects in patients receiving either rivaroxaban or enoxaparin after total hip or knee arthroplasty. Thromb Res. 2012;130(2):147–151.
- , , , , , . Dabigatran etexilate and concomitant use of non‐steroidal anti‐inflammatory drugs or acetylsalicylic acid in patients undergoing total hip and total knee arthroplasty: No increased risk of bleeding. Thromb Haemost. 2012;108(1):183–190.
- , , , et al. CERTIFY: prophylaxis of venous thromboembolism in patients with severe renal insufficiency. Thromb Haemost. 2011;105(6):981–988.
- , , , et al. Tinzaparin and enoxaparin given at prophylactic dose for eight days in medical elderly patients with impaired renal function: a comparative pharmacokinetic study. Thromb Haemost. 2007;97(4):581–586.
- , , , , , . Thromboprophylaxis in patients older than 75 years or with moderate renal impairment undergoing knee or hip replacement surgery [published correction appears in Int Orthop. 2012;36(5):1113]. Int Orthop. 2012;36(4):741–748.
- , , , . Impact of stage 3B chronic kidney disease on thrombosis and bleeding outcomes after orthopedic surgery in patients treated with desirudin or enoxaparin: insights from a randomized trial. J Thromb Haemost. 2012;10(8):1515–1520.
- , . Initiative to improve thromboprophylactic enoxaparin exposure in hospitalized patients with renal impairment. Am J Health Syst Pharm. 2012;69(5):390–396.
- , , , , ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence‐based clinical practice guidelines. Chest. 2012;141(2 suppl):7S–47S.
- , . Aspirin for the prophylaxis of venous thromboembolic events in orthopedic surgery patients: a comparison of the AAOS and ACCP guidelines with review of the evidence. Ann Pharmacother. 2013;47(1):63–74.
Retrievable Vena Cava Filters
Vena cava filters were introduced in the 1960s as a mechanical means to prevent pulmonary embolism (PE).1 Since that time, the number of filters placed has grown steadily, to over 49,000 annually in the United States alone.2 However, patients with vena cava filters can develop complications from the filter itself, which can lead to significant morbidity and, rarely, mortality. In particular, the interruption of venous flow caused by the filter can precipitate lower extremity deep vein thrombosis (DVT),3 as well as vena caval thrombosis involving the filter itself. This has led some experts to recommend indefinite anticoagulation in patients with vena caval filters,4, 5 potentially exposing many patients to the risks of anticoagulation. Given these long‐term safety concerns, there has been recent enthusiasm for the development of optional filters. Optional vena cava filters can be classified into 2 types: temporary and retrievable. Temporary filters, which are not currently available in the United States, are held in place by a tether or catheter5 and cannot be used as permanent devices. Retrievable filters, on the other hand, maintain their position by hooks, radial pressure, or barbs and can either be removed within a prescribed time period after placement or remain in place permanently. In this way, optional filters offer the possibility of avoiding long‐term filter complications in patients with temporary contraindications to anticoagulation. Not surprisingly, the use of retrievable filters has increased dramatically, with many filters being placed for prophylactic indications in patients without known venous thromboembolism (VTE).6 In this work we review the different types of retrievable vena cava filters, current indications for placement, complications, and areas for future research.
Filter Design and Efficacy
Currently, there are 5 U.S. Food and Drug Administration (FDA)‐approved filters in the United States that can be used as retrievable filters: ALN (ALN Implants Chirurgicaux, Ghisonaccia, France); Celect (Cook Medical Incorporated, Bloomington, IN); Gunther‐Tulip (Cook Medical Incorporated, Bloomington, IN); G2 (Bard Peripheral Vascular, Tempe, AZ); and OptEase (Cordis Corporation, Miami Lakes, FL) (Table 1). Three more devices are in U.S. clinical trials: SafeFlo (Rafael Medical Technologies, Hasselt, Belgium); Crux (Crux Biomedical, Portola Valley, CA); and Option (Rex Medical, Conshohocken, PA). Filters are constructed from magnetic resonance imaging (MRI)‐compatible, nonferromagnetic alloys and are produced in either a hexagonal or conical shape. There are potential advantages and disadvantages to both designs. A hexagonal design is thought to be better for trapping small thrombi, but conical filters may have a decreased propensity toward thrombosis.7 When a hexagonal filter becomes partially occluded in vitro, flow disturbances can lead to turbulence, stasis, and progressive clot formation.7 Some clinical studies have demonstrated an increased incidence of thrombosis with hexagonal filters,8 but further investigation is needed to determine if a true correlation exists. Comparisons of the 2 types of filter design are limited but have shown no difference in their efficacy in the prevention of PE.9 Therefore, filter choice is usually dependent upon the physician performing the procedure, although other factors, such as caval size, clot extent, available venous access, and route of retrieval also may affect this decision. Furthermore, retrospective reviews have shown no difference in efficacy between retrievable and permanent filters.10
| Filter | Image | Insertion Site | Retrieval Site | Maximum Successful Documented Dwell Time |
|---|---|---|---|---|
| Gunther‐Tulip (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 204 days42 | |
| Optease (photo courtesy of Cordis Corporation, Miami Lakes, FL) | Femoral or jugular | Femoral | 48 days43 | |
| ALN (photo courtesy of ALN Implants Chirurgicaux, Ghisonaccia, France) | Femoral, jugular, or brachial | Jugular | 352 days44 | |
| Celect (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 357 days45 | |
| G2 (photo courtesy of Bard Peripheral Vascular, Tempe, AZ) | Femoral or jugular | Jugular | 300 days46 |
Insertion of filters is typically performed under fluoroscopy in the operating room or interventional radiology suite. Placement can also occur at the bedside using intravascular ultrasound. This option is particularly useful for critically ill patients who are not stable enough to leave the intensive care unit (ICU) for insertion. The safety of this approach has been documented for both retrievable and permanent filters.11, 12 Duplex ultrasonography has been used to allow bedside placement of permanent filters, but published experience with this modality in placement of retrievable filters is lacking.13, 14
There are no set time limits for retrieving filters, although the retrieval success rate decreases as the time postplacement increases. Rather, the decision to remove them is based on the clinical situation. Table 1 shows data on some of the longest documented successful dwell times for the various retrievable filters. Prior to filter retrieval, a venogram is performed to ensure that there is no clot in the inferior vena cava (IVC) or common iliac veins (Figure 1). Removal of a retrievable filter involves snaring one end of the filter with a hook and then slipping a sheath over the filter, which retracts the filter from the vessel wall as it is being pulled into the sheath (Figure 2). Retrieval rates from various studies are listed in Table 2. Common reasons for nonretrieval include loss to follow up,15 ongoing contraindications to anticoagulation,11, 1618 presence of large thrombi in the filter,16, 1820 poor patient prognosis,16, 18 unrelated death,1618 and filter tilting or embedment.19, 21
| Study | Total Number of Patients | Study Type | Filter Type | Follow‐Up Duration (months) | PE [number (%)] | IVC Thrombosis [number (%)] | DVT [number (%)] | Retrieval Attempted/ Successful Retrieval [number (%)] | Mean Duration Between Filter Placement and Retrieval (days) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Millward et al., 200116 | 90 | RO/PO | G | 3.4 | 0 | 1/39 (2.6) | 1/39 (2.6) | 53 (59)/52 (98) | 9 |
| de Gregorio et al., 200319 | 87 | RO | G | N/R | 0 | 0 | 0 | 69 (79)/68 (99) | 13 |
| Wicky et al., 200317 | 71 | RO | G | 30 | 0 | 0 | 0 | 47 (66)/33 (70) | 8.2 |
| Rosenthal et al., 200411 | 94 | PO | O | N/R | 0 | 0 | 1 (1.1) | 34 (36)/31 (91) | 19 |
| Grande et al., 200515 | 106 | RO | R | N/R | 3 (2.8) | 0 | 0 | 15 (14)/14 (93) | 150 |
| Oliva et al., 200547 | 27 | PO | O | N/R | 0 | 0 | 1/27 (3.7) | 21 (78)/21 (100) | 11.1 |
| Hoppe et al., 200618 | 41 | PO | G | 3 | 1 (2.4) | 1 (2.4) | 1 (2.4) | 23 (57)/23 (100) | 11.1 |
| Kalva et al., 200648 | 96 | RO | R | 5.3 | 1 (1.0) | 0 | 10/53 (18) | 11 (12)/9 (82) | 117 |
| Meier et al., 200635 | 37 | PO | O | 5 | 0 | 1/5 (20) | 1/5 (20) | 32 (86)/32 (100) | 16 |
| Ray et al., 200649 | 197 | RO | G, R | N/R | 1 (0.5)‐G | 2 (1.0)‐G | 0 | 94 (48)/80 (85) | 11 (G)/28 (R) |
| Rosenthal et al., 200650 | 127 | RO | G, R, O | N/R | 0 | 0 | 0 | 70 (52)/66 (94) | 71 |
| Looby et al., 200721 | 147 | RO | G | N/R | 1 (0.7) | 0 | 0 | 45 (31)/36 (80) | 33.6 |
| Yamagami et al., 200751 | 86 | RO | G | N/R | 0 | N/R | N/R | 80 (93)/77 (96) | 13.4 |
| Kim et al, 200852 | 427 | RO | G, P, R, G2 | 10.4 | 20 (4.7) | 2 (0.5) | 54 (12.6) | 60 (15.5)/46 (69.7) | 20.4 |
Indications for Filter Placement
Patients with Known VTE
Suggested indications for the use of vena cava filters in patients with proven VTE are listed in Table 3. For patients at risk for either recurrent or severe bleeding (eg, multiple falls, recurrent gastrointestinal or intracranial hemorrhage) or most patients who have failed treatment with therapeutic anticoagulation, a permanent filter is usually the preferred mechanical option. However, for certain conditions (such as Trousseau's syndrome, heparin‐induced thrombocytopenia, antiphospholipid syndrome, or anatomic abnormalities such as thoracic outlet syndrome‐Paget‐von Schroetter syndrome, or May‐Thurner syndrome‐iliac vein compression syndrome), vena cava filters have been shown either to be ineffective or to worsen thrombosis. In these cases, alternative therapies must be used, based on the underlying disorder and the clinical situation.
| Anticipated Transient Need for Anticoagulation | Anticipated Long‐Term Need for Anticoagulation* | |
|---|---|---|
| ||
| Transient bleeding risk in a patient at high risk for recurrent thromboembolism | Retrievable filter appropriate | Retrievable filter appropriate |
| Permanent, or likely recurrent, bleeding risk | Retrievable filter with extended dwell time | Permanent filter appropriate |
| No unusual bleeding risk | No filter indicated | No filter indicated |
A retrievable filter should only be considered in patients who have a transient contraindication to anticoagulation (Table 5). Such contraindications include isolated but treatable episodes of hemorrhage, urgent surgeries, or procedures associated with a high risk of bleeding, and trauma. The risk of recurrent VTE in the absence of anticoagulation has been estimated at 40% in the first month after VTE and then 10% during the second and third months.22 Therefore, it is reasonable to place a retrievable filter in perioperative patients who cannot be treated with therapeutic anticoagulation during the first 30 days after an acute VTE. If more than 30 days have passed since the thrombotic event, a filter is probably not necessary for patients who will have temporary interruptions in anticoagulation therapy. Instead, bridging anticoagulation (eg, unfractionated heparin [UFH] or low molecular weight heparin [LMWH]) can be given while warfarin is being held prior to surgery. Then, the patient can be transitioned back to warfarin therapy with prophylactic and then therapeutic LMWH or UFH in the postoperative period.
|
| Recurrent VTE |
| Idiopathic VTE |
| Near‐fatal thrombosis |
| Thrombosis at an unusual site (eg, mesenteric vein) |
| VTE in high‐risk thrombophilic disorders: |
| Antiphospholipid antibody syndrome |
| Protein C or S deficiency |
| Antithrombin III deficiency |
| Heterozygous mutations for both the Factor V Leiden and the Prothrombin gene mutation (compound heterozygosity) |
| Homozygous Factor V Leiden mutation |
| Cancer‐associated VTE |
| Major trauma |
| Peripartum |
| Isolated and treatable causes of hemorrhage (eg, peptic ulcer) |
| Bleeding complications after procedures or surgeries53 |
| Liver or kidney biopsy |
| Urgent surgery associated with a high bleeding risk54 |
| Cardiac (coronary artery bypass or valve replacement) |
| Vascular (aortic aneurysm repair, peripheral artery bypass) |
| Neurosurgical (intracranial or spinal) |
| Urologic (prostate and bladder) |
| Major cancer surgery |
Controversy remains regarding the use of retrievable filters in patients with calf vein DVT. It also exists for patients with massive or submassive PE who are receiving anticoagulation therapy but are at high risk for poor outcomes should another PEeven if smalloccur while they are on anticoagulation therapy. Vena cava filters are generally not recommended for patients with distal VTE unless they have a persistent contraindication to anticoagulation therapy and have shown clot propagation on serial duplex studies. At least 1 institution, however, has noted an increased use of filter placement in this population since the advent of retrievable filters.23 Randomized controlled trials and practice guidelines are still lacking in this area. Therefore, there is currently insufficient evidence to recommend retrievable filters for distal VTE.
There is also insufficient evidence to recommend filters for patients with massive or submassive PE who can tolerate anticoagulation therapy. Only 1 registry study has compared patients with massive PE (defined by a systolic blood pressure <90 mmHg at presentation) who were treated with vena cava filters to those who were not.24 Though there was a reduction in recurrent PE and mortality at 90 days in patients who received filters, this result requires further confirmation due to the small number of patients who received filters (11 patients) and a possible selection bias (patients who received filters were, on average, 16 years younger than those who did not). More evidence will be needed to weigh not only the cost but the risks of filter insertion (such as insertion site hematoma, increased incidence of DVT, or contrast nephropathy) against any benefit. Until then, routine filter use in patients with massive or submassive PE cannot be routinely recommended, but may be considered in those with massive PE and impending hemodynamic collapse.
Prophylaxis in High‐Risk Patients
Controversy also exists in the use of retrievable filters in patients without VTE who are at high risk for thromboembolic events. Currently, there are no randomized controlled trials that have established the efficacy of retrievable filters as prophylaxis in these patients. However, there are a number of prospective and retrospective studies that examine this topic, particularly in trauma patients.
Trauma
The Eastern Association for the Surgery of Trauma currently recommends that prophylactic filters be considered in trauma patients who are at increased risk for bleeding and prolonged immobilization (level III).25 These patients include those with severe closed head injury, incomplete spinal cord injury with paraplegia or quadriplegia, multiple long bone fractures, and complex pelvic fractures with multiple long bone fractures. The largest study to date on retrievable filters in trauma patients was done by the American Association for the Surgery of Trauma.26 The incidence of new PE after filter placement was 0.5%, which compares favorably with permanent filter recipients (PE 0.7%) and historical controls (2.1%).27 OptEase filters were more commonly associated with caval thrombosis. The majority of filters (78%) were not retrieved, primarily because patients were lost to follow up. Failure to retrieve filters has become a major issue as these devices grow in popularity.28, 29 In this situation, the benefit of using retrievable filters could be mitigated by the same long‐term complications associated with permanent filters. Therefore, well‐coordinated patient follow‐up is essential to ensure optimal use of retrievable filters. Furthermore, randomized studies of retrievable filters are urgently needed to confirm that vena cava filters are associated with net benefit compared with conventional approaches to VTE prophylaxis (enoxaparin, sequential compression devices) in trauma patients.
Other High‐Risk Situations
The use of permanent filters has been studied in neurosurgical, bariatric, orthopedic, and pregnant patients. However, there are very few studies that look at the use of retrievable filters specifically in these populations. One such study was done in obese (body mass index [BMI] > 55 kg/m2) patients undergoing gastric bypass surgery.30 Filter retrieval rates were high (87%), and there were no DVTs or PEs prior to or after removal. The authors attributed their high removal rates to a dedicated follow‐up program and close collaboration with the interventional radiologists. More research needs to be done comparing outcomes with filters to conventional pharmacologic VTE prophylaxis before these devices can be recommended in these patients.
Filter Complications
During Filter Placement
Complications related to both retrievable and nonretrievable filter placement are rare but have been documented in several studies. Failure of the filter to deploy properly has been reported.21 The same study also noted pneumothorax as a complication in some patients whose filters were inserted via the jugular vein.21 Therefore, location of access and retrieval should be an important consideration for patients with significant underlying pulmonary disease. Insertion site thrombosis and arteriovenous fistula formation have been reported primarily with permanent filters31, 32; that risk could be extrapolated to retrievable filters given that the method of placement is the same. Iodine contrast‐induced nephropathy is of concern for high‐risk patients, although the procedure can be performed using gadolinium‐based contrast, carbon dioxide contrast, or without contrast (under ultrasound guidance).
During Filter Retrieval
Filter tilting and clot trapping under the filter that occurs during the filter removal process are infrequent causes of non‐retrieval. Tilting of the filter sometimes can pose problems, but if this occurs, the filter can be repositioned so that the degree of tilt no longer precludes removal. Severe cases of tilting that lead to nonretrieval are very rare. When thrombus is trapped in the filter (Figure 3), retrieval often depends on the amount of thrombus. A visual scale to assist in judgment of thrombus volume has been developed to assist in retrieval decision‐making.33 In some cases, catheter‐directed thrombolysis has been used to facilitate thrombus dissolution.34
VTE After Placement
Table 2 lists the incidence of VTE after retrievable filter placement. The overall incidence of PE is low, but that of DVT varies widely. These data raise the possibility that some filters may not be removed due to the occurrence of a new DVT, thereby becoming permanent filters with the associated risks of recurrent DVT, caval thrombosis, and PE. Only a few studies have investigated the differences in the rate of PE between permanent and retrievable filters and have shown no differences.29 The long‐term complication rates of retrievable filters and how they may differ from permanent filters warrants further investigation.
Some studies have also noted the development of PE after filter retrieval.35, 36 It is possible that a subclinical DVT was present at the time of removal or that the filter was retrieved before the risk of thrombosis had resolved. Therefore, consideration should be given to the use of duplex ultrasound evaluation for DVT prior to filter removal to ensure that patients with active thrombosis receive therapeutic anticoagulation for an appropriate duration.
Because of the concern for DVT and PE associated with retrievable filters, anticoagulation should ideally occur before and after retrieval, once the bleeding risk has become acceptable. Consensus guidelines support this practice,5, 37 though one systematic review has found insufficient evidence regarding the use of anticoagulation in patients with vena cava filters.4 Retrospective reviews have shown that filters can be both placed and removed without bleeding complications, even in patients who are therapeutically anticoagulated with warfarin and/or LMWH.38, 39 Further investigation would be useful to confirm whether this is an effective approach to VTE prevention at the time of retrieval.
Other Adverse Events
Other complications that have been associated with retrievable filters include migration, fracture, infection, and perforation. It may be difficult to estimate the true incidence of these complications, as most of the literature on this topic comes from case reports. Vena cava perforation with hooks may be not uncommon but in most cases is not clinically significant.40 Filter fracture is more common but rarely reported. Filter migration toward the heart is a very rare but potentially life‐threatening complication. The Recovery filter was taken off the market due in part to concerns about migration.26 As the use of retrievable filters increases, complications related to filters will need to be monitored.
Ongoing and Future Research
Other types of removable filters are currently in development. Convertible filters that can be converted into a stent once they are no longer needed are under investigation. Other devices, such as absorbable or drug‐eluting filters, are also being studied.5 In addition, there is ongoing research to better characterize the safety and efficacy of available filters. The Prevention du Risque d'Embolie Pulmonaire par Interruption Cave (PREPIC) 2 will assess their use in the first prospective, randomized, controlled trial of retrievable filters in patients with acute VTE receiving anticoagulation (
Conclusions
There is growing concern over the increased use of vena caval filters for the prevention of PE.41 Retrievable filters offer the possibility of protection without the risk of long‐term complications attributable to permanent filters. The advent of these devices has lead to an increase in overall filter use but also could result in filter placement without adequate consideration of the potential complications or consequences of nonretrieval. More evidence is needed in order to establish best practice guidelines for retrievable filter use. Until these data are available, these devices should be used only in patients with acute VTE who are at risk for recurrent thromboembolism and have a transient risk for bleeding.
- ,,, et al.A vena caval filter for the prevention of pulmonary embolus.Surg Forum.1967;18.
- ,,.Twenty‐one‐year trends in the use of inferior vena cava filters.Arch Intern Med.2004;164:1541–1545.
- ,,, et al.A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep‐vein thrombosis. Prevention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group.N Engl J Med.1998;338:409–415.
- ,.The need for anticoagulation following inferior vena cava filter placement: systematic review.Cardiovasc Intervent Radiol.2008;31:316–324.
- ,,, et al.Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference.J Vasc Interv Radiol.2006;17:449–459.
- ,,, et al.Changing patterns in the use of inferior vena cava filters: review of a single center experience.J Am Coll Surg.2007;205:564–569.
- ,,.Hemodynamic effects of clot entrapment in the TrapEase inferior vena cava filter.J Vasc Interv Radiol.2004;15:485–490.
- ,,, et al.Vena cava filters and inferior vena cava thrombosis.J Vasc Surg.2007;45:789–794.
- ,,, et al.Clinical comparison of two optional vena cava filters.J Vasc Interv Radiol.2007;18:505–511.
- ,,, et al.Use of retrievable compared to permanent inferior vena cava filters: a single‐institution experience.Cardiovasc Intervent Radiol.2008;31:308–315.
- ,,, et al.Role of prophylactic temporary inferior vena cava filters placed at the ICU bedside under intravascular ultrasound guidance in patients with multiple trauma.J Vasc Surg.2004;40:958–964.
- ,,.Bedside vena cava filter placement with intravascular ultrasound: a simple, accurate, single venous access method.J Vasc Surg.2007;46:1284–1286.
- ,,.The bedside insertion of inferior vena cava filters using ultrasound guidance.Perspect Vasc Surg Endovasc Ther.2007;19:78–84.
- ,,, et al.Comparison of bedside transabdominal duplex ultrasound versus contrast venography for inferior vena cava filter placement: what is the best imaging modality?Ann Vasc Surg.2005;19:229–234.
- ,,, et al.Experience with the recovery filter as a retrievable inferior vena cava filter.J Vasc Interv Radiol.2005;16:1189–1193.
- ,,, et al.Gunther Tulip retrievable vena cava filter: results from the Registry of the Canadian Interventional Radiology Association.J Vasc Interv Radiol.2001;12:1053–1058.
- ,,, et al.Clinical experience with retrievable Gunther Tulip vena cava filters.J Endovasc Ther.2003;10:994–1000.
- ,,, et al.Gunther Tulip filter retrievability multicenter study including CT follow‐up: final report.J Vasc Interv Radiol.2006;17:1017–1023.
- ,,, et al.The Gunther Tulip retrievable filter: prolonged temporary filtration by repositioning within the inferior vena cava.J Vasc Interv Radiol.2003;14:1259–1265.
- ,,, et al.Retrievable inferior vena cava filters: early clinical experience.J Cardiovasc Surg (Torino).2005;46:163–169.
- ,,, et al.Gunther Tulip retrievable inferior vena caval filters: indications, efficacy, retrieval, and complications.Cardiovasc Intervent Radiol.2007;30:59–65.
- ,.Management of anticoagulation before and after elective surgery.N Engl J Med.1997;336:1506–1511.
- ,,, et al.Changes in inferior vena cava filter placement over the past decade at a large community‐based academic health center.J Vasc Surg.2008;47:157–165.
- ,,, et al.Massive pulmonary embolism.Circulation.2006;113:577–582.
- ,,, et al.Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group.J Trauma.2002;53:142–164.
- ,,, et al.Practice patterns and outcomes of retrievable vena cava filters in trauma patients: an AAST multicenter study.J Trauma.2007;62:17–24; discussion 24‐25.
- ,.Inferior vena cava interruption. In: Crowther M, et al., eds.Evidence‐Based Hematology.West Sussex, UK:Wiley‐Blackwell Publishing;2008:99–109.
- ,,, et al.Are temporary inferior vena cava filters really temporary?Am J Surg.2005;190:858–863.
- ,,, et al.Retrievable vena cava filters for preventing pulmonary embolism in trauma patients: a cautionary tale.J Trauma.2006;60:35–40.
- ,,, et al.Safety, feasibility, and outcome of retrievable vena cava filters in high‐risk surgical patients.J Vasc Surg.2007;45:784–788; discussion 788.
- ,,, et al.Femoral arteriovenous fistula after placement of a Kimray‐Greenfield filter.AJR Am J Roentgenol.1988;151:681–682.
- ,,, et al.Prophylactic Greenfield filters: acute complications and long‐term follow‐up.J Trauma.1996;41:231–236; discussion 236‐237.
- ,,.Estimation of trapped thrombus volumes in retrievable inferior vena cava filters: a visual scale.J Vasc Interv Radiol.2007;18:273–276.
- ,,, et al.Endovascular recanalization of the thrombosed filter‐bearing inferior vena cava.J Vasc Interv Radiol.2003;14:893–903.
- ,,, et al.Early experience with the retrievable OptEase vena cava filter in high‐risk trauma patients.Eur J Vasc Endovasc Surg.2006;32:589–595.
- ,,, et al.Current trends in vena caval filtration with the introduction of a retrievable filter at a level I trauma center.J Trauma.2004;57:32–36.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Safety of inferior vena cava filter retrieval in anticoagulated patients.Chest.2007;132:31–36.
- ,,, et al.Should anticoagulant therapy be stopped or reversed before venous intervention?Can Assoc Radiol J.1999;50:306–309.
- ,,.Retrievable vena cava filters: clinical experience.Curr Opin Pulm Med.2006;12:304–309.
- .Use of emboli‐blocking filters increases, but rigorous data are lacking.JAMA.2006;295:989–990.
- ,,, et al.Extended interval for retrieval of vena cava filters is safe and may maximize protection against pulmonary embolism.Am J Surg.2006;192:789–794.
- ,,, et al.Long‐term retrievability of IVC filters: should we abandon permanent devices?Cardiovasc Intervent Radiol.2007;30:820–827.
- ,,, et al.A prospective long‐term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism.Chest.2007;131:223–229.
- ,,, et al.The Cook Celect filter: the UK and global experience so far. In:European Congress of Radiology.2008;European Society of Radiology:Vienna, Austria.
- ,,, et al.Multicenter retrievability trial of the recovery G2 filter.J Vasc Interv Radiol.2008;19:S28.
- ,,, et al.The Jonas study: evaluation of the retrievability of the Cordis OptEase inferior vena cava filter.J Vasc Interv Radiol.2005;16:1439–1445.
- ,,, et al.“Recovery” vena cava filter: experience in 96 patients.Cardiovasc Intervent Radiol.2006;29:559–564.
- ,,, et al.Outcomes with retrievable inferior vena cava filters: a multicenter study.J Vasc Interv Radiol.2006;17:1595–1604.
- ,,, et al.Retrievable inferior vena cava filters: initial clinical results.Ann Vasc Surg.2006;20:157–165.
- ,,, et al.Evaluation of retrievability of the Günther Tulip vena cava filter.Cardiovasc Intervent Radiol.2007;30:226–231.
- ,,, et al.A comparison of clinical outcomes with retrievable and permanent inferior vena cava filters.J Vasc Interv Radiol.2008;19:393–399.
- .The management of anticoagulation before and after procedures.Med Clin North Am.2001;85:1109–1116.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines, 8th ed.Chest.2008;133:299S–339S.
Vena cava filters were introduced in the 1960s as a mechanical means to prevent pulmonary embolism (PE).1 Since that time, the number of filters placed has grown steadily, to over 49,000 annually in the United States alone.2 However, patients with vena cava filters can develop complications from the filter itself, which can lead to significant morbidity and, rarely, mortality. In particular, the interruption of venous flow caused by the filter can precipitate lower extremity deep vein thrombosis (DVT),3 as well as vena caval thrombosis involving the filter itself. This has led some experts to recommend indefinite anticoagulation in patients with vena caval filters,4, 5 potentially exposing many patients to the risks of anticoagulation. Given these long‐term safety concerns, there has been recent enthusiasm for the development of optional filters. Optional vena cava filters can be classified into 2 types: temporary and retrievable. Temporary filters, which are not currently available in the United States, are held in place by a tether or catheter5 and cannot be used as permanent devices. Retrievable filters, on the other hand, maintain their position by hooks, radial pressure, or barbs and can either be removed within a prescribed time period after placement or remain in place permanently. In this way, optional filters offer the possibility of avoiding long‐term filter complications in patients with temporary contraindications to anticoagulation. Not surprisingly, the use of retrievable filters has increased dramatically, with many filters being placed for prophylactic indications in patients without known venous thromboembolism (VTE).6 In this work we review the different types of retrievable vena cava filters, current indications for placement, complications, and areas for future research.
Filter Design and Efficacy
Currently, there are 5 U.S. Food and Drug Administration (FDA)‐approved filters in the United States that can be used as retrievable filters: ALN (ALN Implants Chirurgicaux, Ghisonaccia, France); Celect (Cook Medical Incorporated, Bloomington, IN); Gunther‐Tulip (Cook Medical Incorporated, Bloomington, IN); G2 (Bard Peripheral Vascular, Tempe, AZ); and OptEase (Cordis Corporation, Miami Lakes, FL) (Table 1). Three more devices are in U.S. clinical trials: SafeFlo (Rafael Medical Technologies, Hasselt, Belgium); Crux (Crux Biomedical, Portola Valley, CA); and Option (Rex Medical, Conshohocken, PA). Filters are constructed from magnetic resonance imaging (MRI)‐compatible, nonferromagnetic alloys and are produced in either a hexagonal or conical shape. There are potential advantages and disadvantages to both designs. A hexagonal design is thought to be better for trapping small thrombi, but conical filters may have a decreased propensity toward thrombosis.7 When a hexagonal filter becomes partially occluded in vitro, flow disturbances can lead to turbulence, stasis, and progressive clot formation.7 Some clinical studies have demonstrated an increased incidence of thrombosis with hexagonal filters,8 but further investigation is needed to determine if a true correlation exists. Comparisons of the 2 types of filter design are limited but have shown no difference in their efficacy in the prevention of PE.9 Therefore, filter choice is usually dependent upon the physician performing the procedure, although other factors, such as caval size, clot extent, available venous access, and route of retrieval also may affect this decision. Furthermore, retrospective reviews have shown no difference in efficacy between retrievable and permanent filters.10
| Filter | Image | Insertion Site | Retrieval Site | Maximum Successful Documented Dwell Time |
|---|---|---|---|---|
| Gunther‐Tulip (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 204 days42 | |
| Optease (photo courtesy of Cordis Corporation, Miami Lakes, FL) | Femoral or jugular | Femoral | 48 days43 | |
| ALN (photo courtesy of ALN Implants Chirurgicaux, Ghisonaccia, France) | Femoral, jugular, or brachial | Jugular | 352 days44 | |
| Celect (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 357 days45 | |
| G2 (photo courtesy of Bard Peripheral Vascular, Tempe, AZ) | Femoral or jugular | Jugular | 300 days46 |
Insertion of filters is typically performed under fluoroscopy in the operating room or interventional radiology suite. Placement can also occur at the bedside using intravascular ultrasound. This option is particularly useful for critically ill patients who are not stable enough to leave the intensive care unit (ICU) for insertion. The safety of this approach has been documented for both retrievable and permanent filters.11, 12 Duplex ultrasonography has been used to allow bedside placement of permanent filters, but published experience with this modality in placement of retrievable filters is lacking.13, 14
There are no set time limits for retrieving filters, although the retrieval success rate decreases as the time postplacement increases. Rather, the decision to remove them is based on the clinical situation. Table 1 shows data on some of the longest documented successful dwell times for the various retrievable filters. Prior to filter retrieval, a venogram is performed to ensure that there is no clot in the inferior vena cava (IVC) or common iliac veins (Figure 1). Removal of a retrievable filter involves snaring one end of the filter with a hook and then slipping a sheath over the filter, which retracts the filter from the vessel wall as it is being pulled into the sheath (Figure 2). Retrieval rates from various studies are listed in Table 2. Common reasons for nonretrieval include loss to follow up,15 ongoing contraindications to anticoagulation,11, 1618 presence of large thrombi in the filter,16, 1820 poor patient prognosis,16, 18 unrelated death,1618 and filter tilting or embedment.19, 21
| Study | Total Number of Patients | Study Type | Filter Type | Follow‐Up Duration (months) | PE [number (%)] | IVC Thrombosis [number (%)] | DVT [number (%)] | Retrieval Attempted/ Successful Retrieval [number (%)] | Mean Duration Between Filter Placement and Retrieval (days) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Millward et al., 200116 | 90 | RO/PO | G | 3.4 | 0 | 1/39 (2.6) | 1/39 (2.6) | 53 (59)/52 (98) | 9 |
| de Gregorio et al., 200319 | 87 | RO | G | N/R | 0 | 0 | 0 | 69 (79)/68 (99) | 13 |
| Wicky et al., 200317 | 71 | RO | G | 30 | 0 | 0 | 0 | 47 (66)/33 (70) | 8.2 |
| Rosenthal et al., 200411 | 94 | PO | O | N/R | 0 | 0 | 1 (1.1) | 34 (36)/31 (91) | 19 |
| Grande et al., 200515 | 106 | RO | R | N/R | 3 (2.8) | 0 | 0 | 15 (14)/14 (93) | 150 |
| Oliva et al., 200547 | 27 | PO | O | N/R | 0 | 0 | 1/27 (3.7) | 21 (78)/21 (100) | 11.1 |
| Hoppe et al., 200618 | 41 | PO | G | 3 | 1 (2.4) | 1 (2.4) | 1 (2.4) | 23 (57)/23 (100) | 11.1 |
| Kalva et al., 200648 | 96 | RO | R | 5.3 | 1 (1.0) | 0 | 10/53 (18) | 11 (12)/9 (82) | 117 |
| Meier et al., 200635 | 37 | PO | O | 5 | 0 | 1/5 (20) | 1/5 (20) | 32 (86)/32 (100) | 16 |
| Ray et al., 200649 | 197 | RO | G, R | N/R | 1 (0.5)‐G | 2 (1.0)‐G | 0 | 94 (48)/80 (85) | 11 (G)/28 (R) |
| Rosenthal et al., 200650 | 127 | RO | G, R, O | N/R | 0 | 0 | 0 | 70 (52)/66 (94) | 71 |
| Looby et al., 200721 | 147 | RO | G | N/R | 1 (0.7) | 0 | 0 | 45 (31)/36 (80) | 33.6 |
| Yamagami et al., 200751 | 86 | RO | G | N/R | 0 | N/R | N/R | 80 (93)/77 (96) | 13.4 |
| Kim et al, 200852 | 427 | RO | G, P, R, G2 | 10.4 | 20 (4.7) | 2 (0.5) | 54 (12.6) | 60 (15.5)/46 (69.7) | 20.4 |
Indications for Filter Placement
Patients with Known VTE
Suggested indications for the use of vena cava filters in patients with proven VTE are listed in Table 3. For patients at risk for either recurrent or severe bleeding (eg, multiple falls, recurrent gastrointestinal or intracranial hemorrhage) or most patients who have failed treatment with therapeutic anticoagulation, a permanent filter is usually the preferred mechanical option. However, for certain conditions (such as Trousseau's syndrome, heparin‐induced thrombocytopenia, antiphospholipid syndrome, or anatomic abnormalities such as thoracic outlet syndrome‐Paget‐von Schroetter syndrome, or May‐Thurner syndrome‐iliac vein compression syndrome), vena cava filters have been shown either to be ineffective or to worsen thrombosis. In these cases, alternative therapies must be used, based on the underlying disorder and the clinical situation.
| Anticipated Transient Need for Anticoagulation | Anticipated Long‐Term Need for Anticoagulation* | |
|---|---|---|
| ||
| Transient bleeding risk in a patient at high risk for recurrent thromboembolism | Retrievable filter appropriate | Retrievable filter appropriate |
| Permanent, or likely recurrent, bleeding risk | Retrievable filter with extended dwell time | Permanent filter appropriate |
| No unusual bleeding risk | No filter indicated | No filter indicated |
A retrievable filter should only be considered in patients who have a transient contraindication to anticoagulation (Table 5). Such contraindications include isolated but treatable episodes of hemorrhage, urgent surgeries, or procedures associated with a high risk of bleeding, and trauma. The risk of recurrent VTE in the absence of anticoagulation has been estimated at 40% in the first month after VTE and then 10% during the second and third months.22 Therefore, it is reasonable to place a retrievable filter in perioperative patients who cannot be treated with therapeutic anticoagulation during the first 30 days after an acute VTE. If more than 30 days have passed since the thrombotic event, a filter is probably not necessary for patients who will have temporary interruptions in anticoagulation therapy. Instead, bridging anticoagulation (eg, unfractionated heparin [UFH] or low molecular weight heparin [LMWH]) can be given while warfarin is being held prior to surgery. Then, the patient can be transitioned back to warfarin therapy with prophylactic and then therapeutic LMWH or UFH in the postoperative period.
|
| Recurrent VTE |
| Idiopathic VTE |
| Near‐fatal thrombosis |
| Thrombosis at an unusual site (eg, mesenteric vein) |
| VTE in high‐risk thrombophilic disorders: |
| Antiphospholipid antibody syndrome |
| Protein C or S deficiency |
| Antithrombin III deficiency |
| Heterozygous mutations for both the Factor V Leiden and the Prothrombin gene mutation (compound heterozygosity) |
| Homozygous Factor V Leiden mutation |
| Cancer‐associated VTE |
| Major trauma |
| Peripartum |
| Isolated and treatable causes of hemorrhage (eg, peptic ulcer) |
| Bleeding complications after procedures or surgeries53 |
| Liver or kidney biopsy |
| Urgent surgery associated with a high bleeding risk54 |
| Cardiac (coronary artery bypass or valve replacement) |
| Vascular (aortic aneurysm repair, peripheral artery bypass) |
| Neurosurgical (intracranial or spinal) |
| Urologic (prostate and bladder) |
| Major cancer surgery |
Controversy remains regarding the use of retrievable filters in patients with calf vein DVT. It also exists for patients with massive or submassive PE who are receiving anticoagulation therapy but are at high risk for poor outcomes should another PEeven if smalloccur while they are on anticoagulation therapy. Vena cava filters are generally not recommended for patients with distal VTE unless they have a persistent contraindication to anticoagulation therapy and have shown clot propagation on serial duplex studies. At least 1 institution, however, has noted an increased use of filter placement in this population since the advent of retrievable filters.23 Randomized controlled trials and practice guidelines are still lacking in this area. Therefore, there is currently insufficient evidence to recommend retrievable filters for distal VTE.
There is also insufficient evidence to recommend filters for patients with massive or submassive PE who can tolerate anticoagulation therapy. Only 1 registry study has compared patients with massive PE (defined by a systolic blood pressure <90 mmHg at presentation) who were treated with vena cava filters to those who were not.24 Though there was a reduction in recurrent PE and mortality at 90 days in patients who received filters, this result requires further confirmation due to the small number of patients who received filters (11 patients) and a possible selection bias (patients who received filters were, on average, 16 years younger than those who did not). More evidence will be needed to weigh not only the cost but the risks of filter insertion (such as insertion site hematoma, increased incidence of DVT, or contrast nephropathy) against any benefit. Until then, routine filter use in patients with massive or submassive PE cannot be routinely recommended, but may be considered in those with massive PE and impending hemodynamic collapse.
Prophylaxis in High‐Risk Patients
Controversy also exists in the use of retrievable filters in patients without VTE who are at high risk for thromboembolic events. Currently, there are no randomized controlled trials that have established the efficacy of retrievable filters as prophylaxis in these patients. However, there are a number of prospective and retrospective studies that examine this topic, particularly in trauma patients.
Trauma
The Eastern Association for the Surgery of Trauma currently recommends that prophylactic filters be considered in trauma patients who are at increased risk for bleeding and prolonged immobilization (level III).25 These patients include those with severe closed head injury, incomplete spinal cord injury with paraplegia or quadriplegia, multiple long bone fractures, and complex pelvic fractures with multiple long bone fractures. The largest study to date on retrievable filters in trauma patients was done by the American Association for the Surgery of Trauma.26 The incidence of new PE after filter placement was 0.5%, which compares favorably with permanent filter recipients (PE 0.7%) and historical controls (2.1%).27 OptEase filters were more commonly associated with caval thrombosis. The majority of filters (78%) were not retrieved, primarily because patients were lost to follow up. Failure to retrieve filters has become a major issue as these devices grow in popularity.28, 29 In this situation, the benefit of using retrievable filters could be mitigated by the same long‐term complications associated with permanent filters. Therefore, well‐coordinated patient follow‐up is essential to ensure optimal use of retrievable filters. Furthermore, randomized studies of retrievable filters are urgently needed to confirm that vena cava filters are associated with net benefit compared with conventional approaches to VTE prophylaxis (enoxaparin, sequential compression devices) in trauma patients.
Other High‐Risk Situations
The use of permanent filters has been studied in neurosurgical, bariatric, orthopedic, and pregnant patients. However, there are very few studies that look at the use of retrievable filters specifically in these populations. One such study was done in obese (body mass index [BMI] > 55 kg/m2) patients undergoing gastric bypass surgery.30 Filter retrieval rates were high (87%), and there were no DVTs or PEs prior to or after removal. The authors attributed their high removal rates to a dedicated follow‐up program and close collaboration with the interventional radiologists. More research needs to be done comparing outcomes with filters to conventional pharmacologic VTE prophylaxis before these devices can be recommended in these patients.
Filter Complications
During Filter Placement
Complications related to both retrievable and nonretrievable filter placement are rare but have been documented in several studies. Failure of the filter to deploy properly has been reported.21 The same study also noted pneumothorax as a complication in some patients whose filters were inserted via the jugular vein.21 Therefore, location of access and retrieval should be an important consideration for patients with significant underlying pulmonary disease. Insertion site thrombosis and arteriovenous fistula formation have been reported primarily with permanent filters31, 32; that risk could be extrapolated to retrievable filters given that the method of placement is the same. Iodine contrast‐induced nephropathy is of concern for high‐risk patients, although the procedure can be performed using gadolinium‐based contrast, carbon dioxide contrast, or without contrast (under ultrasound guidance).
During Filter Retrieval
Filter tilting and clot trapping under the filter that occurs during the filter removal process are infrequent causes of non‐retrieval. Tilting of the filter sometimes can pose problems, but if this occurs, the filter can be repositioned so that the degree of tilt no longer precludes removal. Severe cases of tilting that lead to nonretrieval are very rare. When thrombus is trapped in the filter (Figure 3), retrieval often depends on the amount of thrombus. A visual scale to assist in judgment of thrombus volume has been developed to assist in retrieval decision‐making.33 In some cases, catheter‐directed thrombolysis has been used to facilitate thrombus dissolution.34
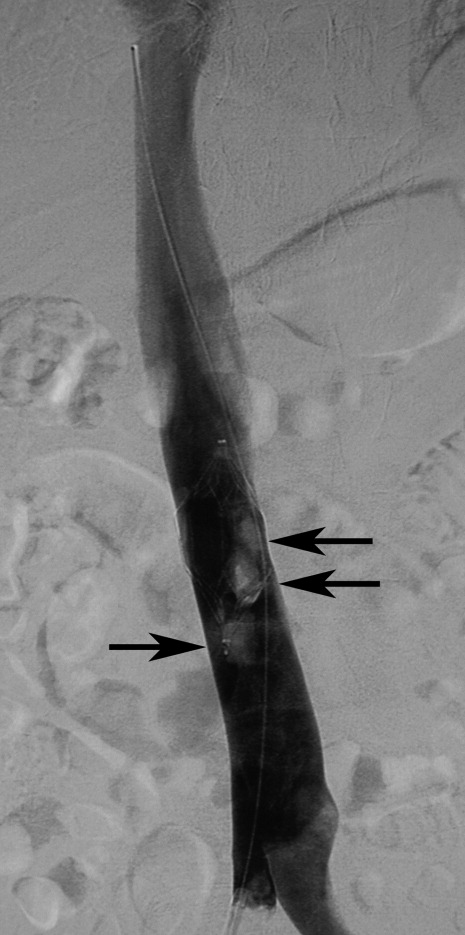
VTE After Placement
Table 2 lists the incidence of VTE after retrievable filter placement. The overall incidence of PE is low, but that of DVT varies widely. These data raise the possibility that some filters may not be removed due to the occurrence of a new DVT, thereby becoming permanent filters with the associated risks of recurrent DVT, caval thrombosis, and PE. Only a few studies have investigated the differences in the rate of PE between permanent and retrievable filters and have shown no differences.29 The long‐term complication rates of retrievable filters and how they may differ from permanent filters warrants further investigation.
Some studies have also noted the development of PE after filter retrieval.35, 36 It is possible that a subclinical DVT was present at the time of removal or that the filter was retrieved before the risk of thrombosis had resolved. Therefore, consideration should be given to the use of duplex ultrasound evaluation for DVT prior to filter removal to ensure that patients with active thrombosis receive therapeutic anticoagulation for an appropriate duration.
Because of the concern for DVT and PE associated with retrievable filters, anticoagulation should ideally occur before and after retrieval, once the bleeding risk has become acceptable. Consensus guidelines support this practice,5, 37 though one systematic review has found insufficient evidence regarding the use of anticoagulation in patients with vena cava filters.4 Retrospective reviews have shown that filters can be both placed and removed without bleeding complications, even in patients who are therapeutically anticoagulated with warfarin and/or LMWH.38, 39 Further investigation would be useful to confirm whether this is an effective approach to VTE prevention at the time of retrieval.
Other Adverse Events
Other complications that have been associated with retrievable filters include migration, fracture, infection, and perforation. It may be difficult to estimate the true incidence of these complications, as most of the literature on this topic comes from case reports. Vena cava perforation with hooks may be not uncommon but in most cases is not clinically significant.40 Filter fracture is more common but rarely reported. Filter migration toward the heart is a very rare but potentially life‐threatening complication. The Recovery filter was taken off the market due in part to concerns about migration.26 As the use of retrievable filters increases, complications related to filters will need to be monitored.
Ongoing and Future Research
Other types of removable filters are currently in development. Convertible filters that can be converted into a stent once they are no longer needed are under investigation. Other devices, such as absorbable or drug‐eluting filters, are also being studied.5 In addition, there is ongoing research to better characterize the safety and efficacy of available filters. The Prevention du Risque d'Embolie Pulmonaire par Interruption Cave (PREPIC) 2 will assess their use in the first prospective, randomized, controlled trial of retrievable filters in patients with acute VTE receiving anticoagulation (
Conclusions
There is growing concern over the increased use of vena caval filters for the prevention of PE.41 Retrievable filters offer the possibility of protection without the risk of long‐term complications attributable to permanent filters. The advent of these devices has lead to an increase in overall filter use but also could result in filter placement without adequate consideration of the potential complications or consequences of nonretrieval. More evidence is needed in order to establish best practice guidelines for retrievable filter use. Until these data are available, these devices should be used only in patients with acute VTE who are at risk for recurrent thromboembolism and have a transient risk for bleeding.
Vena cava filters were introduced in the 1960s as a mechanical means to prevent pulmonary embolism (PE).1 Since that time, the number of filters placed has grown steadily, to over 49,000 annually in the United States alone.2 However, patients with vena cava filters can develop complications from the filter itself, which can lead to significant morbidity and, rarely, mortality. In particular, the interruption of venous flow caused by the filter can precipitate lower extremity deep vein thrombosis (DVT),3 as well as vena caval thrombosis involving the filter itself. This has led some experts to recommend indefinite anticoagulation in patients with vena caval filters,4, 5 potentially exposing many patients to the risks of anticoagulation. Given these long‐term safety concerns, there has been recent enthusiasm for the development of optional filters. Optional vena cava filters can be classified into 2 types: temporary and retrievable. Temporary filters, which are not currently available in the United States, are held in place by a tether or catheter5 and cannot be used as permanent devices. Retrievable filters, on the other hand, maintain their position by hooks, radial pressure, or barbs and can either be removed within a prescribed time period after placement or remain in place permanently. In this way, optional filters offer the possibility of avoiding long‐term filter complications in patients with temporary contraindications to anticoagulation. Not surprisingly, the use of retrievable filters has increased dramatically, with many filters being placed for prophylactic indications in patients without known venous thromboembolism (VTE).6 In this work we review the different types of retrievable vena cava filters, current indications for placement, complications, and areas for future research.
Filter Design and Efficacy
Currently, there are 5 U.S. Food and Drug Administration (FDA)‐approved filters in the United States that can be used as retrievable filters: ALN (ALN Implants Chirurgicaux, Ghisonaccia, France); Celect (Cook Medical Incorporated, Bloomington, IN); Gunther‐Tulip (Cook Medical Incorporated, Bloomington, IN); G2 (Bard Peripheral Vascular, Tempe, AZ); and OptEase (Cordis Corporation, Miami Lakes, FL) (Table 1). Three more devices are in U.S. clinical trials: SafeFlo (Rafael Medical Technologies, Hasselt, Belgium); Crux (Crux Biomedical, Portola Valley, CA); and Option (Rex Medical, Conshohocken, PA). Filters are constructed from magnetic resonance imaging (MRI)‐compatible, nonferromagnetic alloys and are produced in either a hexagonal or conical shape. There are potential advantages and disadvantages to both designs. A hexagonal design is thought to be better for trapping small thrombi, but conical filters may have a decreased propensity toward thrombosis.7 When a hexagonal filter becomes partially occluded in vitro, flow disturbances can lead to turbulence, stasis, and progressive clot formation.7 Some clinical studies have demonstrated an increased incidence of thrombosis with hexagonal filters,8 but further investigation is needed to determine if a true correlation exists. Comparisons of the 2 types of filter design are limited but have shown no difference in their efficacy in the prevention of PE.9 Therefore, filter choice is usually dependent upon the physician performing the procedure, although other factors, such as caval size, clot extent, available venous access, and route of retrieval also may affect this decision. Furthermore, retrospective reviews have shown no difference in efficacy between retrievable and permanent filters.10
| Filter | Image | Insertion Site | Retrieval Site | Maximum Successful Documented Dwell Time |
|---|---|---|---|---|
| Gunther‐Tulip (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 204 days42 | |
| Optease (photo courtesy of Cordis Corporation, Miami Lakes, FL) | Femoral or jugular | Femoral | 48 days43 | |
| ALN (photo courtesy of ALN Implants Chirurgicaux, Ghisonaccia, France) | Femoral, jugular, or brachial | Jugular | 352 days44 | |
| Celect (photo courtesy of Cook Medical Incorporated, Bloomington, IN) | Femoral or jugular | Jugular | 357 days45 | |
| G2 (photo courtesy of Bard Peripheral Vascular, Tempe, AZ) | Femoral or jugular | Jugular | 300 days46 |
Insertion of filters is typically performed under fluoroscopy in the operating room or interventional radiology suite. Placement can also occur at the bedside using intravascular ultrasound. This option is particularly useful for critically ill patients who are not stable enough to leave the intensive care unit (ICU) for insertion. The safety of this approach has been documented for both retrievable and permanent filters.11, 12 Duplex ultrasonography has been used to allow bedside placement of permanent filters, but published experience with this modality in placement of retrievable filters is lacking.13, 14
There are no set time limits for retrieving filters, although the retrieval success rate decreases as the time postplacement increases. Rather, the decision to remove them is based on the clinical situation. Table 1 shows data on some of the longest documented successful dwell times for the various retrievable filters. Prior to filter retrieval, a venogram is performed to ensure that there is no clot in the inferior vena cava (IVC) or common iliac veins (Figure 1). Removal of a retrievable filter involves snaring one end of the filter with a hook and then slipping a sheath over the filter, which retracts the filter from the vessel wall as it is being pulled into the sheath (Figure 2). Retrieval rates from various studies are listed in Table 2. Common reasons for nonretrieval include loss to follow up,15 ongoing contraindications to anticoagulation,11, 1618 presence of large thrombi in the filter,16, 1820 poor patient prognosis,16, 18 unrelated death,1618 and filter tilting or embedment.19, 21
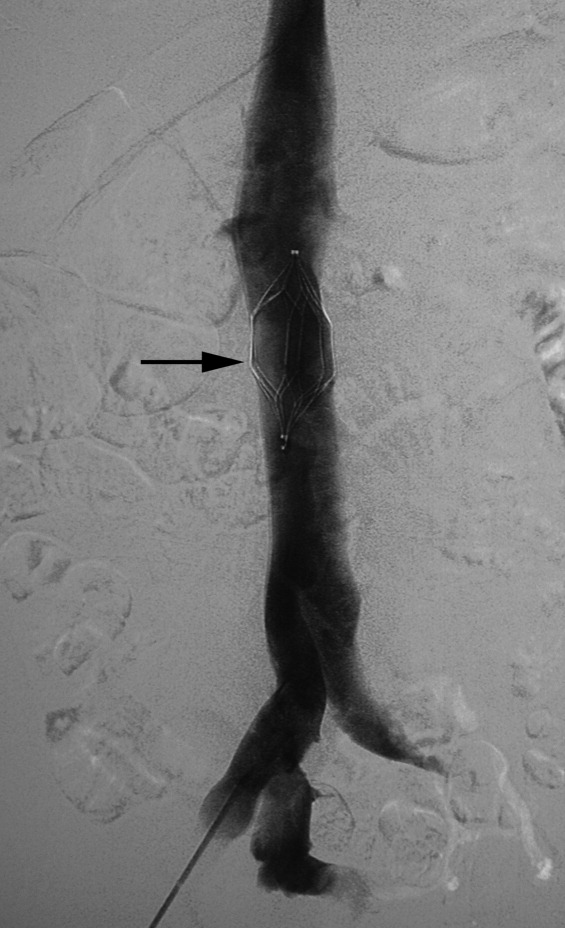
| Study | Total Number of Patients | Study Type | Filter Type | Follow‐Up Duration (months) | PE [number (%)] | IVC Thrombosis [number (%)] | DVT [number (%)] | Retrieval Attempted/ Successful Retrieval [number (%)] | Mean Duration Between Filter Placement and Retrieval (days) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Millward et al., 200116 | 90 | RO/PO | G | 3.4 | 0 | 1/39 (2.6) | 1/39 (2.6) | 53 (59)/52 (98) | 9 |
| de Gregorio et al., 200319 | 87 | RO | G | N/R | 0 | 0 | 0 | 69 (79)/68 (99) | 13 |
| Wicky et al., 200317 | 71 | RO | G | 30 | 0 | 0 | 0 | 47 (66)/33 (70) | 8.2 |
| Rosenthal et al., 200411 | 94 | PO | O | N/R | 0 | 0 | 1 (1.1) | 34 (36)/31 (91) | 19 |
| Grande et al., 200515 | 106 | RO | R | N/R | 3 (2.8) | 0 | 0 | 15 (14)/14 (93) | 150 |
| Oliva et al., 200547 | 27 | PO | O | N/R | 0 | 0 | 1/27 (3.7) | 21 (78)/21 (100) | 11.1 |
| Hoppe et al., 200618 | 41 | PO | G | 3 | 1 (2.4) | 1 (2.4) | 1 (2.4) | 23 (57)/23 (100) | 11.1 |
| Kalva et al., 200648 | 96 | RO | R | 5.3 | 1 (1.0) | 0 | 10/53 (18) | 11 (12)/9 (82) | 117 |
| Meier et al., 200635 | 37 | PO | O | 5 | 0 | 1/5 (20) | 1/5 (20) | 32 (86)/32 (100) | 16 |
| Ray et al., 200649 | 197 | RO | G, R | N/R | 1 (0.5)‐G | 2 (1.0)‐G | 0 | 94 (48)/80 (85) | 11 (G)/28 (R) |
| Rosenthal et al., 200650 | 127 | RO | G, R, O | N/R | 0 | 0 | 0 | 70 (52)/66 (94) | 71 |
| Looby et al., 200721 | 147 | RO | G | N/R | 1 (0.7) | 0 | 0 | 45 (31)/36 (80) | 33.6 |
| Yamagami et al., 200751 | 86 | RO | G | N/R | 0 | N/R | N/R | 80 (93)/77 (96) | 13.4 |
| Kim et al, 200852 | 427 | RO | G, P, R, G2 | 10.4 | 20 (4.7) | 2 (0.5) | 54 (12.6) | 60 (15.5)/46 (69.7) | 20.4 |
Indications for Filter Placement
Patients with Known VTE
Suggested indications for the use of vena cava filters in patients with proven VTE are listed in Table 3. For patients at risk for either recurrent or severe bleeding (eg, multiple falls, recurrent gastrointestinal or intracranial hemorrhage) or most patients who have failed treatment with therapeutic anticoagulation, a permanent filter is usually the preferred mechanical option. However, for certain conditions (such as Trousseau's syndrome, heparin‐induced thrombocytopenia, antiphospholipid syndrome, or anatomic abnormalities such as thoracic outlet syndrome‐Paget‐von Schroetter syndrome, or May‐Thurner syndrome‐iliac vein compression syndrome), vena cava filters have been shown either to be ineffective or to worsen thrombosis. In these cases, alternative therapies must be used, based on the underlying disorder and the clinical situation.
| Anticipated Transient Need for Anticoagulation | Anticipated Long‐Term Need for Anticoagulation* | |
|---|---|---|
| ||
| Transient bleeding risk in a patient at high risk for recurrent thromboembolism | Retrievable filter appropriate | Retrievable filter appropriate |
| Permanent, or likely recurrent, bleeding risk | Retrievable filter with extended dwell time | Permanent filter appropriate |
| No unusual bleeding risk | No filter indicated | No filter indicated |
A retrievable filter should only be considered in patients who have a transient contraindication to anticoagulation (Table 5). Such contraindications include isolated but treatable episodes of hemorrhage, urgent surgeries, or procedures associated with a high risk of bleeding, and trauma. The risk of recurrent VTE in the absence of anticoagulation has been estimated at 40% in the first month after VTE and then 10% during the second and third months.22 Therefore, it is reasonable to place a retrievable filter in perioperative patients who cannot be treated with therapeutic anticoagulation during the first 30 days after an acute VTE. If more than 30 days have passed since the thrombotic event, a filter is probably not necessary for patients who will have temporary interruptions in anticoagulation therapy. Instead, bridging anticoagulation (eg, unfractionated heparin [UFH] or low molecular weight heparin [LMWH]) can be given while warfarin is being held prior to surgery. Then, the patient can be transitioned back to warfarin therapy with prophylactic and then therapeutic LMWH or UFH in the postoperative period.
|
| Recurrent VTE |
| Idiopathic VTE |
| Near‐fatal thrombosis |
| Thrombosis at an unusual site (eg, mesenteric vein) |
| VTE in high‐risk thrombophilic disorders: |
| Antiphospholipid antibody syndrome |
| Protein C or S deficiency |
| Antithrombin III deficiency |
| Heterozygous mutations for both the Factor V Leiden and the Prothrombin gene mutation (compound heterozygosity) |
| Homozygous Factor V Leiden mutation |
| Cancer‐associated VTE |
| Major trauma |
| Peripartum |
| Isolated and treatable causes of hemorrhage (eg, peptic ulcer) |
| Bleeding complications after procedures or surgeries53 |
| Liver or kidney biopsy |
| Urgent surgery associated with a high bleeding risk54 |
| Cardiac (coronary artery bypass or valve replacement) |
| Vascular (aortic aneurysm repair, peripheral artery bypass) |
| Neurosurgical (intracranial or spinal) |
| Urologic (prostate and bladder) |
| Major cancer surgery |
Controversy remains regarding the use of retrievable filters in patients with calf vein DVT. It also exists for patients with massive or submassive PE who are receiving anticoagulation therapy but are at high risk for poor outcomes should another PEeven if smalloccur while they are on anticoagulation therapy. Vena cava filters are generally not recommended for patients with distal VTE unless they have a persistent contraindication to anticoagulation therapy and have shown clot propagation on serial duplex studies. At least 1 institution, however, has noted an increased use of filter placement in this population since the advent of retrievable filters.23 Randomized controlled trials and practice guidelines are still lacking in this area. Therefore, there is currently insufficient evidence to recommend retrievable filters for distal VTE.
There is also insufficient evidence to recommend filters for patients with massive or submassive PE who can tolerate anticoagulation therapy. Only 1 registry study has compared patients with massive PE (defined by a systolic blood pressure <90 mmHg at presentation) who were treated with vena cava filters to those who were not.24 Though there was a reduction in recurrent PE and mortality at 90 days in patients who received filters, this result requires further confirmation due to the small number of patients who received filters (11 patients) and a possible selection bias (patients who received filters were, on average, 16 years younger than those who did not). More evidence will be needed to weigh not only the cost but the risks of filter insertion (such as insertion site hematoma, increased incidence of DVT, or contrast nephropathy) against any benefit. Until then, routine filter use in patients with massive or submassive PE cannot be routinely recommended, but may be considered in those with massive PE and impending hemodynamic collapse.
Prophylaxis in High‐Risk Patients
Controversy also exists in the use of retrievable filters in patients without VTE who are at high risk for thromboembolic events. Currently, there are no randomized controlled trials that have established the efficacy of retrievable filters as prophylaxis in these patients. However, there are a number of prospective and retrospective studies that examine this topic, particularly in trauma patients.
Trauma
The Eastern Association for the Surgery of Trauma currently recommends that prophylactic filters be considered in trauma patients who are at increased risk for bleeding and prolonged immobilization (level III).25 These patients include those with severe closed head injury, incomplete spinal cord injury with paraplegia or quadriplegia, multiple long bone fractures, and complex pelvic fractures with multiple long bone fractures. The largest study to date on retrievable filters in trauma patients was done by the American Association for the Surgery of Trauma.26 The incidence of new PE after filter placement was 0.5%, which compares favorably with permanent filter recipients (PE 0.7%) and historical controls (2.1%).27 OptEase filters were more commonly associated with caval thrombosis. The majority of filters (78%) were not retrieved, primarily because patients were lost to follow up. Failure to retrieve filters has become a major issue as these devices grow in popularity.28, 29 In this situation, the benefit of using retrievable filters could be mitigated by the same long‐term complications associated with permanent filters. Therefore, well‐coordinated patient follow‐up is essential to ensure optimal use of retrievable filters. Furthermore, randomized studies of retrievable filters are urgently needed to confirm that vena cava filters are associated with net benefit compared with conventional approaches to VTE prophylaxis (enoxaparin, sequential compression devices) in trauma patients.
Other High‐Risk Situations
The use of permanent filters has been studied in neurosurgical, bariatric, orthopedic, and pregnant patients. However, there are very few studies that look at the use of retrievable filters specifically in these populations. One such study was done in obese (body mass index [BMI] > 55 kg/m2) patients undergoing gastric bypass surgery.30 Filter retrieval rates were high (87%), and there were no DVTs or PEs prior to or after removal. The authors attributed their high removal rates to a dedicated follow‐up program and close collaboration with the interventional radiologists. More research needs to be done comparing outcomes with filters to conventional pharmacologic VTE prophylaxis before these devices can be recommended in these patients.
Filter Complications
During Filter Placement
Complications related to both retrievable and nonretrievable filter placement are rare but have been documented in several studies. Failure of the filter to deploy properly has been reported.21 The same study also noted pneumothorax as a complication in some patients whose filters were inserted via the jugular vein.21 Therefore, location of access and retrieval should be an important consideration for patients with significant underlying pulmonary disease. Insertion site thrombosis and arteriovenous fistula formation have been reported primarily with permanent filters31, 32; that risk could be extrapolated to retrievable filters given that the method of placement is the same. Iodine contrast‐induced nephropathy is of concern for high‐risk patients, although the procedure can be performed using gadolinium‐based contrast, carbon dioxide contrast, or without contrast (under ultrasound guidance).
During Filter Retrieval
Filter tilting and clot trapping under the filter that occurs during the filter removal process are infrequent causes of non‐retrieval. Tilting of the filter sometimes can pose problems, but if this occurs, the filter can be repositioned so that the degree of tilt no longer precludes removal. Severe cases of tilting that lead to nonretrieval are very rare. When thrombus is trapped in the filter (Figure 3), retrieval often depends on the amount of thrombus. A visual scale to assist in judgment of thrombus volume has been developed to assist in retrieval decision‐making.33 In some cases, catheter‐directed thrombolysis has been used to facilitate thrombus dissolution.34
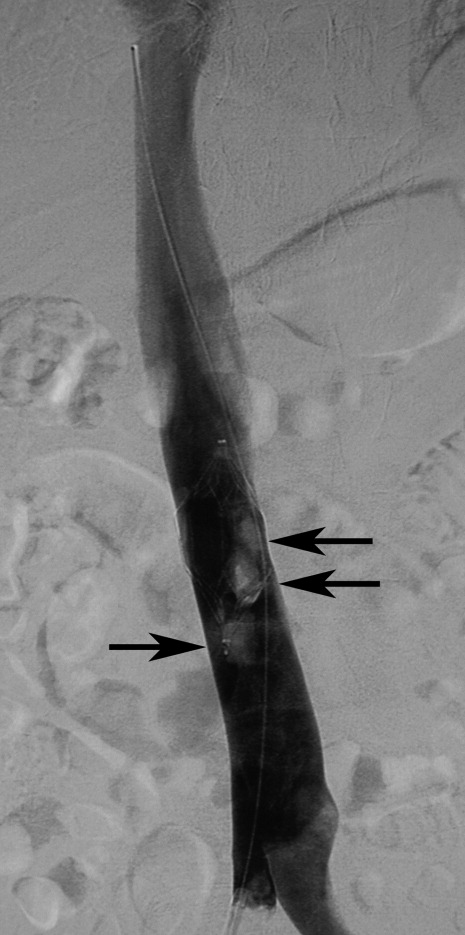
VTE After Placement
Table 2 lists the incidence of VTE after retrievable filter placement. The overall incidence of PE is low, but that of DVT varies widely. These data raise the possibility that some filters may not be removed due to the occurrence of a new DVT, thereby becoming permanent filters with the associated risks of recurrent DVT, caval thrombosis, and PE. Only a few studies have investigated the differences in the rate of PE between permanent and retrievable filters and have shown no differences.29 The long‐term complication rates of retrievable filters and how they may differ from permanent filters warrants further investigation.
Some studies have also noted the development of PE after filter retrieval.35, 36 It is possible that a subclinical DVT was present at the time of removal or that the filter was retrieved before the risk of thrombosis had resolved. Therefore, consideration should be given to the use of duplex ultrasound evaluation for DVT prior to filter removal to ensure that patients with active thrombosis receive therapeutic anticoagulation for an appropriate duration.
Because of the concern for DVT and PE associated with retrievable filters, anticoagulation should ideally occur before and after retrieval, once the bleeding risk has become acceptable. Consensus guidelines support this practice,5, 37 though one systematic review has found insufficient evidence regarding the use of anticoagulation in patients with vena cava filters.4 Retrospective reviews have shown that filters can be both placed and removed without bleeding complications, even in patients who are therapeutically anticoagulated with warfarin and/or LMWH.38, 39 Further investigation would be useful to confirm whether this is an effective approach to VTE prevention at the time of retrieval.
Other Adverse Events
Other complications that have been associated with retrievable filters include migration, fracture, infection, and perforation. It may be difficult to estimate the true incidence of these complications, as most of the literature on this topic comes from case reports. Vena cava perforation with hooks may be not uncommon but in most cases is not clinically significant.40 Filter fracture is more common but rarely reported. Filter migration toward the heart is a very rare but potentially life‐threatening complication. The Recovery filter was taken off the market due in part to concerns about migration.26 As the use of retrievable filters increases, complications related to filters will need to be monitored.
Ongoing and Future Research
Other types of removable filters are currently in development. Convertible filters that can be converted into a stent once they are no longer needed are under investigation. Other devices, such as absorbable or drug‐eluting filters, are also being studied.5 In addition, there is ongoing research to better characterize the safety and efficacy of available filters. The Prevention du Risque d'Embolie Pulmonaire par Interruption Cave (PREPIC) 2 will assess their use in the first prospective, randomized, controlled trial of retrievable filters in patients with acute VTE receiving anticoagulation (
Conclusions
There is growing concern over the increased use of vena caval filters for the prevention of PE.41 Retrievable filters offer the possibility of protection without the risk of long‐term complications attributable to permanent filters. The advent of these devices has lead to an increase in overall filter use but also could result in filter placement without adequate consideration of the potential complications or consequences of nonretrieval. More evidence is needed in order to establish best practice guidelines for retrievable filter use. Until these data are available, these devices should be used only in patients with acute VTE who are at risk for recurrent thromboembolism and have a transient risk for bleeding.
- ,,, et al.A vena caval filter for the prevention of pulmonary embolus.Surg Forum.1967;18.
- ,,.Twenty‐one‐year trends in the use of inferior vena cava filters.Arch Intern Med.2004;164:1541–1545.
- ,,, et al.A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep‐vein thrombosis. Prevention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group.N Engl J Med.1998;338:409–415.
- ,.The need for anticoagulation following inferior vena cava filter placement: systematic review.Cardiovasc Intervent Radiol.2008;31:316–324.
- ,,, et al.Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference.J Vasc Interv Radiol.2006;17:449–459.
- ,,, et al.Changing patterns in the use of inferior vena cava filters: review of a single center experience.J Am Coll Surg.2007;205:564–569.
- ,,.Hemodynamic effects of clot entrapment in the TrapEase inferior vena cava filter.J Vasc Interv Radiol.2004;15:485–490.
- ,,, et al.Vena cava filters and inferior vena cava thrombosis.J Vasc Surg.2007;45:789–794.
- ,,, et al.Clinical comparison of two optional vena cava filters.J Vasc Interv Radiol.2007;18:505–511.
- ,,, et al.Use of retrievable compared to permanent inferior vena cava filters: a single‐institution experience.Cardiovasc Intervent Radiol.2008;31:308–315.
- ,,, et al.Role of prophylactic temporary inferior vena cava filters placed at the ICU bedside under intravascular ultrasound guidance in patients with multiple trauma.J Vasc Surg.2004;40:958–964.
- ,,.Bedside vena cava filter placement with intravascular ultrasound: a simple, accurate, single venous access method.J Vasc Surg.2007;46:1284–1286.
- ,,.The bedside insertion of inferior vena cava filters using ultrasound guidance.Perspect Vasc Surg Endovasc Ther.2007;19:78–84.
- ,,, et al.Comparison of bedside transabdominal duplex ultrasound versus contrast venography for inferior vena cava filter placement: what is the best imaging modality?Ann Vasc Surg.2005;19:229–234.
- ,,, et al.Experience with the recovery filter as a retrievable inferior vena cava filter.J Vasc Interv Radiol.2005;16:1189–1193.
- ,,, et al.Gunther Tulip retrievable vena cava filter: results from the Registry of the Canadian Interventional Radiology Association.J Vasc Interv Radiol.2001;12:1053–1058.
- ,,, et al.Clinical experience with retrievable Gunther Tulip vena cava filters.J Endovasc Ther.2003;10:994–1000.
- ,,, et al.Gunther Tulip filter retrievability multicenter study including CT follow‐up: final report.J Vasc Interv Radiol.2006;17:1017–1023.
- ,,, et al.The Gunther Tulip retrievable filter: prolonged temporary filtration by repositioning within the inferior vena cava.J Vasc Interv Radiol.2003;14:1259–1265.
- ,,, et al.Retrievable inferior vena cava filters: early clinical experience.J Cardiovasc Surg (Torino).2005;46:163–169.
- ,,, et al.Gunther Tulip retrievable inferior vena caval filters: indications, efficacy, retrieval, and complications.Cardiovasc Intervent Radiol.2007;30:59–65.
- ,.Management of anticoagulation before and after elective surgery.N Engl J Med.1997;336:1506–1511.
- ,,, et al.Changes in inferior vena cava filter placement over the past decade at a large community‐based academic health center.J Vasc Surg.2008;47:157–165.
- ,,, et al.Massive pulmonary embolism.Circulation.2006;113:577–582.
- ,,, et al.Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group.J Trauma.2002;53:142–164.
- ,,, et al.Practice patterns and outcomes of retrievable vena cava filters in trauma patients: an AAST multicenter study.J Trauma.2007;62:17–24; discussion 24‐25.
- ,.Inferior vena cava interruption. In: Crowther M, et al., eds.Evidence‐Based Hematology.West Sussex, UK:Wiley‐Blackwell Publishing;2008:99–109.
- ,,, et al.Are temporary inferior vena cava filters really temporary?Am J Surg.2005;190:858–863.
- ,,, et al.Retrievable vena cava filters for preventing pulmonary embolism in trauma patients: a cautionary tale.J Trauma.2006;60:35–40.
- ,,, et al.Safety, feasibility, and outcome of retrievable vena cava filters in high‐risk surgical patients.J Vasc Surg.2007;45:784–788; discussion 788.
- ,,, et al.Femoral arteriovenous fistula after placement of a Kimray‐Greenfield filter.AJR Am J Roentgenol.1988;151:681–682.
- ,,, et al.Prophylactic Greenfield filters: acute complications and long‐term follow‐up.J Trauma.1996;41:231–236; discussion 236‐237.
- ,,.Estimation of trapped thrombus volumes in retrievable inferior vena cava filters: a visual scale.J Vasc Interv Radiol.2007;18:273–276.
- ,,, et al.Endovascular recanalization of the thrombosed filter‐bearing inferior vena cava.J Vasc Interv Radiol.2003;14:893–903.
- ,,, et al.Early experience with the retrievable OptEase vena cava filter in high‐risk trauma patients.Eur J Vasc Endovasc Surg.2006;32:589–595.
- ,,, et al.Current trends in vena caval filtration with the introduction of a retrievable filter at a level I trauma center.J Trauma.2004;57:32–36.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Safety of inferior vena cava filter retrieval in anticoagulated patients.Chest.2007;132:31–36.
- ,,, et al.Should anticoagulant therapy be stopped or reversed before venous intervention?Can Assoc Radiol J.1999;50:306–309.
- ,,.Retrievable vena cava filters: clinical experience.Curr Opin Pulm Med.2006;12:304–309.
- .Use of emboli‐blocking filters increases, but rigorous data are lacking.JAMA.2006;295:989–990.
- ,,, et al.Extended interval for retrieval of vena cava filters is safe and may maximize protection against pulmonary embolism.Am J Surg.2006;192:789–794.
- ,,, et al.Long‐term retrievability of IVC filters: should we abandon permanent devices?Cardiovasc Intervent Radiol.2007;30:820–827.
- ,,, et al.A prospective long‐term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism.Chest.2007;131:223–229.
- ,,, et al.The Cook Celect filter: the UK and global experience so far. In:European Congress of Radiology.2008;European Society of Radiology:Vienna, Austria.
- ,,, et al.Multicenter retrievability trial of the recovery G2 filter.J Vasc Interv Radiol.2008;19:S28.
- ,,, et al.The Jonas study: evaluation of the retrievability of the Cordis OptEase inferior vena cava filter.J Vasc Interv Radiol.2005;16:1439–1445.
- ,,, et al.“Recovery” vena cava filter: experience in 96 patients.Cardiovasc Intervent Radiol.2006;29:559–564.
- ,,, et al.Outcomes with retrievable inferior vena cava filters: a multicenter study.J Vasc Interv Radiol.2006;17:1595–1604.
- ,,, et al.Retrievable inferior vena cava filters: initial clinical results.Ann Vasc Surg.2006;20:157–165.
- ,,, et al.Evaluation of retrievability of the Günther Tulip vena cava filter.Cardiovasc Intervent Radiol.2007;30:226–231.
- ,,, et al.A comparison of clinical outcomes with retrievable and permanent inferior vena cava filters.J Vasc Interv Radiol.2008;19:393–399.
- .The management of anticoagulation before and after procedures.Med Clin North Am.2001;85:1109–1116.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines, 8th ed.Chest.2008;133:299S–339S.
- ,,, et al.A vena caval filter for the prevention of pulmonary embolus.Surg Forum.1967;18.
- ,,.Twenty‐one‐year trends in the use of inferior vena cava filters.Arch Intern Med.2004;164:1541–1545.
- ,,, et al.A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep‐vein thrombosis. Prevention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group.N Engl J Med.1998;338:409–415.
- ,.The need for anticoagulation following inferior vena cava filter placement: systematic review.Cardiovasc Intervent Radiol.2008;31:316–324.
- ,,, et al.Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference.J Vasc Interv Radiol.2006;17:449–459.
- ,,, et al.Changing patterns in the use of inferior vena cava filters: review of a single center experience.J Am Coll Surg.2007;205:564–569.
- ,,.Hemodynamic effects of clot entrapment in the TrapEase inferior vena cava filter.J Vasc Interv Radiol.2004;15:485–490.
- ,,, et al.Vena cava filters and inferior vena cava thrombosis.J Vasc Surg.2007;45:789–794.
- ,,, et al.Clinical comparison of two optional vena cava filters.J Vasc Interv Radiol.2007;18:505–511.
- ,,, et al.Use of retrievable compared to permanent inferior vena cava filters: a single‐institution experience.Cardiovasc Intervent Radiol.2008;31:308–315.
- ,,, et al.Role of prophylactic temporary inferior vena cava filters placed at the ICU bedside under intravascular ultrasound guidance in patients with multiple trauma.J Vasc Surg.2004;40:958–964.
- ,,.Bedside vena cava filter placement with intravascular ultrasound: a simple, accurate, single venous access method.J Vasc Surg.2007;46:1284–1286.
- ,,.The bedside insertion of inferior vena cava filters using ultrasound guidance.Perspect Vasc Surg Endovasc Ther.2007;19:78–84.
- ,,, et al.Comparison of bedside transabdominal duplex ultrasound versus contrast venography for inferior vena cava filter placement: what is the best imaging modality?Ann Vasc Surg.2005;19:229–234.
- ,,, et al.Experience with the recovery filter as a retrievable inferior vena cava filter.J Vasc Interv Radiol.2005;16:1189–1193.
- ,,, et al.Gunther Tulip retrievable vena cava filter: results from the Registry of the Canadian Interventional Radiology Association.J Vasc Interv Radiol.2001;12:1053–1058.
- ,,, et al.Clinical experience with retrievable Gunther Tulip vena cava filters.J Endovasc Ther.2003;10:994–1000.
- ,,, et al.Gunther Tulip filter retrievability multicenter study including CT follow‐up: final report.J Vasc Interv Radiol.2006;17:1017–1023.
- ,,, et al.The Gunther Tulip retrievable filter: prolonged temporary filtration by repositioning within the inferior vena cava.J Vasc Interv Radiol.2003;14:1259–1265.
- ,,, et al.Retrievable inferior vena cava filters: early clinical experience.J Cardiovasc Surg (Torino).2005;46:163–169.
- ,,, et al.Gunther Tulip retrievable inferior vena caval filters: indications, efficacy, retrieval, and complications.Cardiovasc Intervent Radiol.2007;30:59–65.
- ,.Management of anticoagulation before and after elective surgery.N Engl J Med.1997;336:1506–1511.
- ,,, et al.Changes in inferior vena cava filter placement over the past decade at a large community‐based academic health center.J Vasc Surg.2008;47:157–165.
- ,,, et al.Massive pulmonary embolism.Circulation.2006;113:577–582.
- ,,, et al.Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group.J Trauma.2002;53:142–164.
- ,,, et al.Practice patterns and outcomes of retrievable vena cava filters in trauma patients: an AAST multicenter study.J Trauma.2007;62:17–24; discussion 24‐25.
- ,.Inferior vena cava interruption. In: Crowther M, et al., eds.Evidence‐Based Hematology.West Sussex, UK:Wiley‐Blackwell Publishing;2008:99–109.
- ,,, et al.Are temporary inferior vena cava filters really temporary?Am J Surg.2005;190:858–863.
- ,,, et al.Retrievable vena cava filters for preventing pulmonary embolism in trauma patients: a cautionary tale.J Trauma.2006;60:35–40.
- ,,, et al.Safety, feasibility, and outcome of retrievable vena cava filters in high‐risk surgical patients.J Vasc Surg.2007;45:784–788; discussion 788.
- ,,, et al.Femoral arteriovenous fistula after placement of a Kimray‐Greenfield filter.AJR Am J Roentgenol.1988;151:681–682.
- ,,, et al.Prophylactic Greenfield filters: acute complications and long‐term follow‐up.J Trauma.1996;41:231–236; discussion 236‐237.
- ,,.Estimation of trapped thrombus volumes in retrievable inferior vena cava filters: a visual scale.J Vasc Interv Radiol.2007;18:273–276.
- ,,, et al.Endovascular recanalization of the thrombosed filter‐bearing inferior vena cava.J Vasc Interv Radiol.2003;14:893–903.
- ,,, et al.Early experience with the retrievable OptEase vena cava filter in high‐risk trauma patients.Eur J Vasc Endovasc Surg.2006;32:589–595.
- ,,, et al.Current trends in vena caval filtration with the introduction of a retrievable filter at a level I trauma center.J Trauma.2004;57:32–36.
- ,,, et al.Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126:401S–428S.
- ,,, et al.Safety of inferior vena cava filter retrieval in anticoagulated patients.Chest.2007;132:31–36.
- ,,, et al.Should anticoagulant therapy be stopped or reversed before venous intervention?Can Assoc Radiol J.1999;50:306–309.
- ,,.Retrievable vena cava filters: clinical experience.Curr Opin Pulm Med.2006;12:304–309.
- .Use of emboli‐blocking filters increases, but rigorous data are lacking.JAMA.2006;295:989–990.
- ,,, et al.Extended interval for retrieval of vena cava filters is safe and may maximize protection against pulmonary embolism.Am J Surg.2006;192:789–794.
- ,,, et al.Long‐term retrievability of IVC filters: should we abandon permanent devices?Cardiovasc Intervent Radiol.2007;30:820–827.
- ,,, et al.A prospective long‐term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism.Chest.2007;131:223–229.
- ,,, et al.The Cook Celect filter: the UK and global experience so far. In:European Congress of Radiology.2008;European Society of Radiology:Vienna, Austria.
- ,,, et al.Multicenter retrievability trial of the recovery G2 filter.J Vasc Interv Radiol.2008;19:S28.
- ,,, et al.The Jonas study: evaluation of the retrievability of the Cordis OptEase inferior vena cava filter.J Vasc Interv Radiol.2005;16:1439–1445.
- ,,, et al.“Recovery” vena cava filter: experience in 96 patients.Cardiovasc Intervent Radiol.2006;29:559–564.
- ,,, et al.Outcomes with retrievable inferior vena cava filters: a multicenter study.J Vasc Interv Radiol.2006;17:1595–1604.
- ,,, et al.Retrievable inferior vena cava filters: initial clinical results.Ann Vasc Surg.2006;20:157–165.
- ,,, et al.Evaluation of retrievability of the Günther Tulip vena cava filter.Cardiovasc Intervent Radiol.2007;30:226–231.
- ,,, et al.A comparison of clinical outcomes with retrievable and permanent inferior vena cava filters.J Vasc Interv Radiol.2008;19:393–399.
- .The management of anticoagulation before and after procedures.Med Clin North Am.2001;85:1109–1116.
- ,,, et al.The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines, 8th ed.Chest.2008;133:299S–339S.
In reply: VTE prevention in major orthopedic surgery
Editor's Note: This letter concerns an article in a Cleveland Clinic Journal of Medicine supplement (Preventing Venous Thromboembolism Throughout the Continuum of Care) distributed to only a portion of the Journal's regular readership, owing to the terms of the grant supporting the supplement.
In Reply: We appreciate the comments by Drs. Fishmann and Boyd, but we strongly disagree with their suggestion that aspirin monotherapy is an appropriate option for the prevention of venous thromboembolism (VTE) following major orthopedic surgery.
As discussed in our original article,1 multiple large-scale clinical trials in patients undergoing elective hip arthroplasty, knee arthroplasty, or hip fracture surgery have demonstrated the thromboprophylactic efficacy of warfarin, unfractionated heparin, low-molecular-weight heparin (LMWH), fondaparinux, and oral direct thrombin inhibitors. The relative risk reduction with these agents has been greater than 50% in most studies. In contrast, in a large meta-analysis of VTE prophylaxis following total hip replacement, which included data from 56 randomized trials published between 1966 and 1993, aspirin was not beneficial in preventing DVT.14
The largest prospective randomized trial comparing aspirin with placebo for VTE prevention was conducted between 1992 and 1998 among 17,444 patients in five countries.5 It involved 13,356 patients requiring hip fracture surgery and 4,088 patients requiring elective hip arthroplasty. Patients were randomized to receive aspirin 160 mg/day or placebo for 35 days. However, additional forms of VTE prophylaxis were allowed if deemed necessary by the clinician. In fact, 26% of patients received LMWH in addition to aspirin, and dual therapy was probably more common in those patients at highest thromboembolic risk. As such, the 36% relative risk reduction in VTE ascribed to aspirin should be viewed with caution. Further, this is a smaller risk reduction than that observed in trials of other anticoagulant agents.
A large, well-designed, randomized clinical trial comparing aspirin to LMWH or fondaparinux remains to be conducted.
Dr. Fishmann cites a small study of patients undergoing knee arthroplasty who received spinal anesthesia and intermittent calf compression devices.7 In this underpowered study, 275 patients were randomized to receive aspirin 325 mg twice daily or enoxaparin 30 mg twice daily for 3 weeks. The overall DVT rates were 14.1% in the enoxaparin group vs 17.8% in the aspirin group (P = .27).7 Patients who received aspirin had significantly more postoperative drainage than those randomized to enoxaparin. In addition, the protocol for scheduling enoxaparin 48 hours postoperatively is not consistent with recommendations of the American College of Chest Physicians (ACCP) and may have reduced the efficacy of enoxaparin.
The other evidence in support of aspirin cited by Dr. Fishmann includes an editorial,9 an uncontrolled retrospective analysis,8 a single-center retrospective review,10 and a review article.6 Although there is evidence that the use of aspirin is probably associated with a modest reduction in postoperative VTE risk, it has been unequivocally surpassed in efficacy by other anticoagulants.
Both the latest (2004) ACCP guidelines on VTE2 and the 2006 International Consensus Statement on VTE prevention and treatment15 advise against aspirin monotherapy as VTE prophylaxis in any patient groups. It is likely that the upcoming 2008 ACCP guidelines will also advocate against using aspirin as well.
Lastly, the most recent guideline from the American Academy of Orthopaedic Surgeons advocating aspirin as monotherapy11 is based on the assumption that the major important clinical end point in the orthopedic surgery patient is clinical pulmonary embolism, an end point that was not included as a lone primary end point in any of the modern randomized controlled studies in major orthopedic surgery. This represents a flawed logic for the development of evidence-based guideline recommendations, and this recommendation has not been advocated by well-respected bodies such as the ACCP and the international groups that developed the International Consensus Statement. Furthermore, if this practice is going to be advocated by the American Academy of Orthopaedic Surgeons, then large rigorously designed randomized trials must be conducted to compare aspirin to currently available anticoagulants, and the type of joint surgery should be clearly defined.
- Deitelzweig SB, McKean SC, Amin AN, Brotman DJ, Jaffer AK, Spyropoulos AC. Prevention of venous thromboembolism in the orthopedic surgery patient. Cleve Clin J Med 2008; 75(suppl 3):S27–S36.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 suppl):338S–400S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 suppl):132S–175S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty. J Am Acad Orthop Surg 1996; 4:54–62.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Berend KR, Lombardi AV. Multimodal venous thromboembolic disease prevention for patients undergoing primary or revision total joint arthroplasty: the role of aspirin. Am J Orthop 2006; 35:24–29.
- Westrich GH, Bottner F, Windsor RE, Laskin RS, Haas SB, Sculco TP. VenaFlow plus Lovenox vs VenaFlow plus aspirin for thromboembolic disease prophylaxis in total knee arthroplasty. J Arthroplasty 2006; 21(6 suppl 2):139–143.
- Lotke PA, Lonner JH. The benefit of aspirin chemoprophylaxis for thromboembolism after total knee arthroplasty. Clin Orthop Relat Res 2006; 452:175–180.
- Callaghan JJ, Dorr LD, Engh GA, et al. Prophylaxis for thromboembolic disease: recommendations from the American College of Chest Physicians—are they appropriate for orthopaedic surgery? J Arthroplasty 2005; 20:273–274.
- Dorr LD, Gendelman V, Maheshwari AV, Boutary M, Wan Z, Long WT. Multimodal thromboprophylaxis for total hip and knee arthroplasty based on risk assessment. J Bone Joint Surg Am 2007; 89:2648–2657.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_summary.pdf. Accessed April 16, 2008.
- Parvizi J, Ghanem E, Joshi A, Sharkey PF, Hozack WJ, Rothman RH. Does “excessive” anticoagulation predispose to periprosthetic infection? J Arthroplasty 2007; 22(6 suppl 2):24–28.
- Bern M, Deshmukh RV, Nelson R, et al. Low-dose warfarin coupled with lower leg compression is effective prophylaxis against thromboembolic disease after hip arthroplasty. J Arthroplasty 2007; 22:644–650.
- Imperiale TF, Speroff T. A meta-analysis of methods to prevent venous thromboembolism following total hip replacement. JAMA 1994; 271:1780–1785.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
Editor's Note: This letter concerns an article in a Cleveland Clinic Journal of Medicine supplement (Preventing Venous Thromboembolism Throughout the Continuum of Care) distributed to only a portion of the Journal's regular readership, owing to the terms of the grant supporting the supplement.
In Reply: We appreciate the comments by Drs. Fishmann and Boyd, but we strongly disagree with their suggestion that aspirin monotherapy is an appropriate option for the prevention of venous thromboembolism (VTE) following major orthopedic surgery.
As discussed in our original article,1 multiple large-scale clinical trials in patients undergoing elective hip arthroplasty, knee arthroplasty, or hip fracture surgery have demonstrated the thromboprophylactic efficacy of warfarin, unfractionated heparin, low-molecular-weight heparin (LMWH), fondaparinux, and oral direct thrombin inhibitors. The relative risk reduction with these agents has been greater than 50% in most studies. In contrast, in a large meta-analysis of VTE prophylaxis following total hip replacement, which included data from 56 randomized trials published between 1966 and 1993, aspirin was not beneficial in preventing DVT.14
The largest prospective randomized trial comparing aspirin with placebo for VTE prevention was conducted between 1992 and 1998 among 17,444 patients in five countries.5 It involved 13,356 patients requiring hip fracture surgery and 4,088 patients requiring elective hip arthroplasty. Patients were randomized to receive aspirin 160 mg/day or placebo for 35 days. However, additional forms of VTE prophylaxis were allowed if deemed necessary by the clinician. In fact, 26% of patients received LMWH in addition to aspirin, and dual therapy was probably more common in those patients at highest thromboembolic risk. As such, the 36% relative risk reduction in VTE ascribed to aspirin should be viewed with caution. Further, this is a smaller risk reduction than that observed in trials of other anticoagulant agents.
A large, well-designed, randomized clinical trial comparing aspirin to LMWH or fondaparinux remains to be conducted.
Dr. Fishmann cites a small study of patients undergoing knee arthroplasty who received spinal anesthesia and intermittent calf compression devices.7 In this underpowered study, 275 patients were randomized to receive aspirin 325 mg twice daily or enoxaparin 30 mg twice daily for 3 weeks. The overall DVT rates were 14.1% in the enoxaparin group vs 17.8% in the aspirin group (P = .27).7 Patients who received aspirin had significantly more postoperative drainage than those randomized to enoxaparin. In addition, the protocol for scheduling enoxaparin 48 hours postoperatively is not consistent with recommendations of the American College of Chest Physicians (ACCP) and may have reduced the efficacy of enoxaparin.
The other evidence in support of aspirin cited by Dr. Fishmann includes an editorial,9 an uncontrolled retrospective analysis,8 a single-center retrospective review,10 and a review article.6 Although there is evidence that the use of aspirin is probably associated with a modest reduction in postoperative VTE risk, it has been unequivocally surpassed in efficacy by other anticoagulants.
Both the latest (2004) ACCP guidelines on VTE2 and the 2006 International Consensus Statement on VTE prevention and treatment15 advise against aspirin monotherapy as VTE prophylaxis in any patient groups. It is likely that the upcoming 2008 ACCP guidelines will also advocate against using aspirin as well.
Lastly, the most recent guideline from the American Academy of Orthopaedic Surgeons advocating aspirin as monotherapy11 is based on the assumption that the major important clinical end point in the orthopedic surgery patient is clinical pulmonary embolism, an end point that was not included as a lone primary end point in any of the modern randomized controlled studies in major orthopedic surgery. This represents a flawed logic for the development of evidence-based guideline recommendations, and this recommendation has not been advocated by well-respected bodies such as the ACCP and the international groups that developed the International Consensus Statement. Furthermore, if this practice is going to be advocated by the American Academy of Orthopaedic Surgeons, then large rigorously designed randomized trials must be conducted to compare aspirin to currently available anticoagulants, and the type of joint surgery should be clearly defined.
Editor's Note: This letter concerns an article in a Cleveland Clinic Journal of Medicine supplement (Preventing Venous Thromboembolism Throughout the Continuum of Care) distributed to only a portion of the Journal's regular readership, owing to the terms of the grant supporting the supplement.
In Reply: We appreciate the comments by Drs. Fishmann and Boyd, but we strongly disagree with their suggestion that aspirin monotherapy is an appropriate option for the prevention of venous thromboembolism (VTE) following major orthopedic surgery.
As discussed in our original article,1 multiple large-scale clinical trials in patients undergoing elective hip arthroplasty, knee arthroplasty, or hip fracture surgery have demonstrated the thromboprophylactic efficacy of warfarin, unfractionated heparin, low-molecular-weight heparin (LMWH), fondaparinux, and oral direct thrombin inhibitors. The relative risk reduction with these agents has been greater than 50% in most studies. In contrast, in a large meta-analysis of VTE prophylaxis following total hip replacement, which included data from 56 randomized trials published between 1966 and 1993, aspirin was not beneficial in preventing DVT.14
The largest prospective randomized trial comparing aspirin with placebo for VTE prevention was conducted between 1992 and 1998 among 17,444 patients in five countries.5 It involved 13,356 patients requiring hip fracture surgery and 4,088 patients requiring elective hip arthroplasty. Patients were randomized to receive aspirin 160 mg/day or placebo for 35 days. However, additional forms of VTE prophylaxis were allowed if deemed necessary by the clinician. In fact, 26% of patients received LMWH in addition to aspirin, and dual therapy was probably more common in those patients at highest thromboembolic risk. As such, the 36% relative risk reduction in VTE ascribed to aspirin should be viewed with caution. Further, this is a smaller risk reduction than that observed in trials of other anticoagulant agents.
A large, well-designed, randomized clinical trial comparing aspirin to LMWH or fondaparinux remains to be conducted.
Dr. Fishmann cites a small study of patients undergoing knee arthroplasty who received spinal anesthesia and intermittent calf compression devices.7 In this underpowered study, 275 patients were randomized to receive aspirin 325 mg twice daily or enoxaparin 30 mg twice daily for 3 weeks. The overall DVT rates were 14.1% in the enoxaparin group vs 17.8% in the aspirin group (P = .27).7 Patients who received aspirin had significantly more postoperative drainage than those randomized to enoxaparin. In addition, the protocol for scheduling enoxaparin 48 hours postoperatively is not consistent with recommendations of the American College of Chest Physicians (ACCP) and may have reduced the efficacy of enoxaparin.
The other evidence in support of aspirin cited by Dr. Fishmann includes an editorial,9 an uncontrolled retrospective analysis,8 a single-center retrospective review,10 and a review article.6 Although there is evidence that the use of aspirin is probably associated with a modest reduction in postoperative VTE risk, it has been unequivocally surpassed in efficacy by other anticoagulants.
Both the latest (2004) ACCP guidelines on VTE2 and the 2006 International Consensus Statement on VTE prevention and treatment15 advise against aspirin monotherapy as VTE prophylaxis in any patient groups. It is likely that the upcoming 2008 ACCP guidelines will also advocate against using aspirin as well.
Lastly, the most recent guideline from the American Academy of Orthopaedic Surgeons advocating aspirin as monotherapy11 is based on the assumption that the major important clinical end point in the orthopedic surgery patient is clinical pulmonary embolism, an end point that was not included as a lone primary end point in any of the modern randomized controlled studies in major orthopedic surgery. This represents a flawed logic for the development of evidence-based guideline recommendations, and this recommendation has not been advocated by well-respected bodies such as the ACCP and the international groups that developed the International Consensus Statement. Furthermore, if this practice is going to be advocated by the American Academy of Orthopaedic Surgeons, then large rigorously designed randomized trials must be conducted to compare aspirin to currently available anticoagulants, and the type of joint surgery should be clearly defined.
- Deitelzweig SB, McKean SC, Amin AN, Brotman DJ, Jaffer AK, Spyropoulos AC. Prevention of venous thromboembolism in the orthopedic surgery patient. Cleve Clin J Med 2008; 75(suppl 3):S27–S36.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 suppl):338S–400S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 suppl):132S–175S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty. J Am Acad Orthop Surg 1996; 4:54–62.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Berend KR, Lombardi AV. Multimodal venous thromboembolic disease prevention for patients undergoing primary or revision total joint arthroplasty: the role of aspirin. Am J Orthop 2006; 35:24–29.
- Westrich GH, Bottner F, Windsor RE, Laskin RS, Haas SB, Sculco TP. VenaFlow plus Lovenox vs VenaFlow plus aspirin for thromboembolic disease prophylaxis in total knee arthroplasty. J Arthroplasty 2006; 21(6 suppl 2):139–143.
- Lotke PA, Lonner JH. The benefit of aspirin chemoprophylaxis for thromboembolism after total knee arthroplasty. Clin Orthop Relat Res 2006; 452:175–180.
- Callaghan JJ, Dorr LD, Engh GA, et al. Prophylaxis for thromboembolic disease: recommendations from the American College of Chest Physicians—are they appropriate for orthopaedic surgery? J Arthroplasty 2005; 20:273–274.
- Dorr LD, Gendelman V, Maheshwari AV, Boutary M, Wan Z, Long WT. Multimodal thromboprophylaxis for total hip and knee arthroplasty based on risk assessment. J Bone Joint Surg Am 2007; 89:2648–2657.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_summary.pdf. Accessed April 16, 2008.
- Parvizi J, Ghanem E, Joshi A, Sharkey PF, Hozack WJ, Rothman RH. Does “excessive” anticoagulation predispose to periprosthetic infection? J Arthroplasty 2007; 22(6 suppl 2):24–28.
- Bern M, Deshmukh RV, Nelson R, et al. Low-dose warfarin coupled with lower leg compression is effective prophylaxis against thromboembolic disease after hip arthroplasty. J Arthroplasty 2007; 22:644–650.
- Imperiale TF, Speroff T. A meta-analysis of methods to prevent venous thromboembolism following total hip replacement. JAMA 1994; 271:1780–1785.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
- Deitelzweig SB, McKean SC, Amin AN, Brotman DJ, Jaffer AK, Spyropoulos AC. Prevention of venous thromboembolism in the orthopedic surgery patient. Cleve Clin J Med 2008; 75(suppl 3):S27–S36.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 suppl):338S–400S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 suppl):132S–175S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty. J Am Acad Orthop Surg 1996; 4:54–62.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Berend KR, Lombardi AV. Multimodal venous thromboembolic disease prevention for patients undergoing primary or revision total joint arthroplasty: the role of aspirin. Am J Orthop 2006; 35:24–29.
- Westrich GH, Bottner F, Windsor RE, Laskin RS, Haas SB, Sculco TP. VenaFlow plus Lovenox vs VenaFlow plus aspirin for thromboembolic disease prophylaxis in total knee arthroplasty. J Arthroplasty 2006; 21(6 suppl 2):139–143.
- Lotke PA, Lonner JH. The benefit of aspirin chemoprophylaxis for thromboembolism after total knee arthroplasty. Clin Orthop Relat Res 2006; 452:175–180.
- Callaghan JJ, Dorr LD, Engh GA, et al. Prophylaxis for thromboembolic disease: recommendations from the American College of Chest Physicians—are they appropriate for orthopaedic surgery? J Arthroplasty 2005; 20:273–274.
- Dorr LD, Gendelman V, Maheshwari AV, Boutary M, Wan Z, Long WT. Multimodal thromboprophylaxis for total hip and knee arthroplasty based on risk assessment. J Bone Joint Surg Am 2007; 89:2648–2657.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_summary.pdf. Accessed April 16, 2008.
- Parvizi J, Ghanem E, Joshi A, Sharkey PF, Hozack WJ, Rothman RH. Does “excessive” anticoagulation predispose to periprosthetic infection? J Arthroplasty 2007; 22(6 suppl 2):24–28.
- Bern M, Deshmukh RV, Nelson R, et al. Low-dose warfarin coupled with lower leg compression is effective prophylaxis against thromboembolic disease after hip arthroplasty. J Arthroplasty 2007; 22:644–650.
- Imperiale TF, Speroff T. A meta-analysis of methods to prevent venous thromboembolism following total hip replacement. JAMA 1994; 271:1780–1785.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
Prevention of venous thromboembolism in the hospitalized medical patient
The need for prophylaxis of venous thromboembolism (VTE) in hospitalized acutely ill medical patients is well established. Without prophylaxis, hospitalized medical patients develop VTE at a rate of 5% to 15%.1–3 Moreover, pulmonary embolism (PE) occurs more frequently in hospitalized medical patients than in nonmedical patients, and is a leading cause of sudden death in hospitalized medical patients.4,5 Without appropriate prophylaxis, 1 in 20 hospitalized medical patients may suffer a fatal PE.4
PROPHYLAXIS IN MEDICAL PATIENTS: UNDERUSED AND OFTEN INAPPROPRIATE
Despite these risks and the clear indications for VTE prophylaxis in hospitalized medical patients, prophylaxis of VTE is omitted more often in these patients than in hospitalized surgical patients.5 Even when prophylaxis is given, it is often used inappropriately in the medical population. So concludes a recent analysis of data from 196,104 patients with acute medical conditions who were discharged from 227 US hospitals from January 2002 to September 2005.6 Criteria for inclusion in the analysis were patient age of 40 years or older, a hospital stay of 6 days or greater, and an absence of contraindications to anticoagulation. Appropriate prophylaxis was defined in accordance with the Sixth American College of Chest Physicians (ACCP) Consensus Conference on Antithrombotic Therapy.7
The analysis revealed an overall VTE prophylaxis rate of 61.8%, but the rate of appropriate prophylaxis was only 33.9%, meaning that two-thirds of discharged patients did not receive prophylaxis in accordance with ACCP guidelines. When temporal trends were analyzed according to groups based on patients’ diagnosis at admission (acute myocardial infarction, severe lung disease, ischemic stroke, cancer, heart failure, or trauma), the rate of appropriate prophylaxis remained essentially flat from the beginning to the end of the study period for virtually all diagnosis groups.6
Similar findings have emerged from the International Medical Prevention Registry on Venous Thromboembolism (IMPROVE), an ongoing international registry of acutely ill medical patients.8 Data from the first 15,156 patients, enrolled from July 2002 through September 2006, reveal that 50% of patients received pharmacologic and/or mechanical VTE prophylaxis in the hospital, and only 60% of patients who met established criteria for VTE prophylaxis actually received it.
Analysis of the US portion of the IMPROVE data shows that 54% of the US patient sample received some form of VTE prophylaxis; 22% of US patients received intermittent pneumatic compression, 21% received unfractionated heparin (UFH), 14% received low-molecular-weight heparin (LMWH), and 3% wore compression stockings.8 Thus, despite a paucity of data supporting a benefit of intermittent pneumatic compression in this population,9 it was the most frequently used form of prophylaxis in US patients.
CLINICAL TRIALS OF PHARMACOLOGIC PROPHYLAXIS IN MEDICAL PATIENTS
The Prophylaxis in Medical Patients with Enoxaparin (MEDENOX) trial1 randomized 1,102 hospitalized patients to one of two doses of the LMWH enoxaparin (20 mg or 40 mg once daily subcutaneously) or placebo for 6 to 14 days. Compared with placebo, the 40-mg dose of enoxaparin was associated with a 63% reduction in risk of VTE over 3 months of follow-up (P < .001) (Figure 1).
The Prospective Evaluation of Dalteparin Efficacy for Prevention of VTE in Immobilized Patients Trial (PREVENT)2 was a multicenter, randomized, double-blind study comparing the LMWH dalteparin (5,000 IU daily given subcutaneously for 14 days) with placebo in 3,706 acutely ill medical patients. Over 90 days of follow-up, the risk of VTE was reduced by 44% in patients assigned to dalteparin compared with those assigned to placebo (P = .0015) (Figure 1).
The Arixtra for Thromboembolism Prevention in a Medical Indications Study (ARTEMIS)3 randomized 849 medical patients 60 years or older to 6 to 14 days of therapy with the selective factor Xa inhibitor fondaparinux (2.5 mg once daily subcutaneously) or placebo. Compared with the placebo group, fondaparinux recipients had a 47% lower risk of developing VTE by day 15 (P = .029) (Figure 1).
Fewer events and fatal PEs, but no effect on all-cause mortality
A recent meta-analysis by Dentali et al10 further demonstrates the efficacy of anticoagulant therapy for preventing symptomatic VTE in hospitalized medical patients. This analysis included several other trials in addition to the three reviewed above,1–3 for a total of nine randomized studies (seven of which were dou-ble-blind) comprising 19,958 patients. Across the nine studies, anticoagulant prophylaxis was clearly superior to placebo in preventing fatal PE (relative risk, 0.38 [95% CI, 0.21 to 0.69]). There was a strong trend toward a reduction in symptomatic deep vein thrombosis (DVT) with prophylaxis but no effect on all-cause mortality. The meta-analysis also provided reassurance that prophylaxis does not increase the rate of major bleeding.
HOW DO THE PROPHYLAXIS OPTIONS STACK UP?
What the ACCP recommends
Current ACCP guidelines recommend the use of either LMWH or low-dose UFH (5,000 U subcutaneously two or three times daily) as a Grade 1A recommendation for VTE prophylaxis in patients with medical conditions and risk factors for VTE.9 This represents the guidelines’ highest level of recommendation, ie, one that is based on randomized controlled trials (RCTs) without important limitations. In contrast, the 2006 International Consensus Statement, developed as a collaborative effort among expert bodies on VTE, specified a more narrow dosing recommendation for UFH in this patient population (5,000 U three times daily, not twice daily) as well as specifying 40 mg once daily as the recommended dose of enoxaparin and 5,000 IU once daily as the recommended dose of dalteparin.11
For medical patients with risk factors for VTE who have a contraindication to anticoagulant prophylaxis, the ACCP guidelines recommend the use of graduated compression stockings or intermittent pneumatic compression devices as a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”9).
Current ACCP guidelines do not address the use of fondaparinux in their recommendations for VTE prophylaxis in medical patients.
Getting a handle on bleeding risk
Patient characteristics that exclude pharmacologic thromboprophylaxis due to bleeding risk are generally limited to active bleeding or coagulopathy, as demonstrated by a platelet count less than 50,000 cells/µL or an international normalized ratio greater than 1.5. Additionally, bleeding risk should be carefully assessed if an invasive procedure is planned during a patient’s hospital stay.
It is worth noting that the anticoagulant doses used for VTE prophylaxis are a fraction of those used for treatment of VTE. Thus, if a patient would be treated with full-dose anticoagulation if VTE developed, then that patient should be eligible for VTE prophylaxis.
Because the use of mechanical forms of prophylaxis in medical patients is not truly evidence-based, mechanical prophylaxis should be reserved for medical patients who have a contraindication to anticoagulants, or for use in combination with anticoagulants in patients at very high risk of VTE.
UFH vs LMWH
Two meta-analyses have compared UFH with LMWH for VTE prevention in medical patients.12,13 In a recent analysis that included 10 trials directly comparing the two therapies, 14 trials comparing UFH with control, and 11 trials comparing LMWH with control, Wein et al found a lower risk of DVT with LMWH than with UFH (relative risk, 0.68 [95% CI, 0.52 to 0.88]) but no difference between the therapies in mortality or bleeding risk.12 In an earlier and smaller analysis, Mismetti et al found no significant differences between UFH and LMWH in preventing DVT or death but did find a significant reduction in major bleeding episodes with LMWH versus three-times-daily UFH (52% relative reduction; P = .049).13
Randomized trials also reveal that enoxaparin 40 mg once daily is as efficacious as UFH 5,000 U three times daily for VTE prevention in medical patients.14,15 The above analysis by Wein et al12 and an additional meta-analysis by King and colleagues16 found that three-times-daily dosing of UFH is more efficacious than twice-daily dosing of UFH, but at the expense of more bleeding, including major bleeding.
Economic considerations
Because of differences in drug acquisition costs between UFH and the LMWH agents, several economic evaluations have compared the use of these therapies for prophylaxis in medical patients at risk of VTE.
In an analysis of hospital costs for medical patients receiving VTE prophylaxis from more than 330 US hospitals for the period 2001–2004, Burleigh et al found that mean total hospital costs were higher for patients who received UFH than for those who received LMWH ($7,615 vs $6,866) even though mean drug costs were higher for LMWH ($791 vs $569 for UFH).17 A reduction in hospital length of stay appeared to contribute to the overall savings with LMWH; other contributors may have included costs associated with heparin-induced thrombocytopenia (HIT) in UFH recipients or the extra nursing time required for administering UFH in two or three daily doses.
Leykum et al used a decision analysis model to estimate the economic effect of substituting enoxaparin for UFH in hospitalized medical patients for whom VTE prophylaxis is indicated.18 Cost data were based on Medicare reimbursement rates as well as drug and laboratory costs for a multi-institutional health system. The model assumed HIT incidence rates of 2.7% with UFH and 0.3% with enoxaparin. It also assumed the cost of a daily dose to be $4 for UFH versus $84 for enoxaparin. From the payer perspective, the model showed that substituting enoxaparin for UFH would reduce the overall cost of care by $28.61 per day on a per-patient basis, despite enoxaparin’s higher acquisition cost, and would save $4,550 per quality-adjusted life-year by reducing the incidence of HIT.
Another cost analysis confirms the association between HIT and increased hospital costs. Creekmore et al retrospectively analyzed data from 10,121 adult medical patients who received VTE prophylaxis at the University of Utah Hospital in Salt Lake City from August 2000 to November 2004.19 They found that an admission during which HIT developed incurred a mean cost of $56,364, compared with $15,231 for an admission without HIT. Because LMWH was associated with a lower incidence of HIT compared with UFH (0.084% vs 0.51%, respectively), LMWH reduced the incremental cost of VTE prophylaxis by $13.88 per patient compared with UFH.
THE EXCLAIM TRIAL: IS THERE A ROLE FOR EXTENDED PROPHYLAXIS?
Although the previously discussed studies have clearly demonstrated the benefit of in-hospital VTE prophylaxis for acutely ill medical patients, none has rigorously examined extended-duration out-of-hospital prophylaxis in these patients. This represents an important gap in the literature, since a substantial proportion of VTE develops in the outpatient setting within 3 months of a hospitalization, and most outpatient VTE episodes occur within 1 month of a preceding hospitalization.20
To begin to fill this gap, the Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial was conducted to compare extended-duration LMWH prophylaxis with a standard LMWH prophylaxis regimen in acutely ill medical patients using a prospective, multicenter, randomized, double-blind, placebo-controlled design.21
Patients and study design
Patients were eligible for enrollment if they were aged 40 years or older and had recent immobilization (≤ 3 days), a predefined acute medical illness, and either level 1 mobility (total bed rest or sedentary state) or level 2 mobility (level 1 with bathroom privileges). The predefined acute medical illnesses consisted of New York Heart Association class III/IV heart failure, acute respiratory insufficiency, or other acute medical conditions, including post-acute ischemic stroke, acute infection without septic shock, and active cancer.
All patients received open-label enoxaparin 40 mg subcutaneously once daily for 10 ± 4 days, after which they were randomized to either enoxaparin 40 mg subcutaneously once daily or placebo for an additional 28 ± 4 days.
The primary efficacy end point was the incidence of VTE events, defined as asymptomatic DVT documented by mandatory ultrasonography at the end of the double-blind treatment period (28 ± 4 days) or as symptomatic DVT, symptomatic PE, or fatal PE at any time during the double-blind period. Symptomatic DVT was confirmed by objective tests; PE was confirmed by ventilation-perfusion scan, computed tomography, angiography, or autopsy.
Secondary efficacy end points were mortality at the end of the double-blind period, at 3 months, and at 6 months, as well as the incidence of VTE at 3 months.
The primary safety outcome measure was the incidence of major hemorrhage during the double-blind period; secondary safety measures were rates of major and minor hemorrhage, minor hemorrhage, HIT, and serious adverse events.
Population amended at planned interim analysis
After approximately half of the patients were enrolled, a planned and blinded interim analysis for futility concluded that the study was unlikely to show a statistically significant advantage of enoxaparin over placebo. The trial’s steering committee followed the suggestion of its data safety monitoring board to redefine the inclusion criteria to refocus enrollment on patients with a high risk of VTE. A blinded analysis was performed to identify this subgroup.
The resulting amended inclusion criteria were the same as above except that level 2 mobility had to be accompanied by at least one of three additional high-risk criteria: (1) age greater than 75 years, (2) history of prior VTE, or (3) diagnosis of cancer.
The trial’s main exclusion criteria were evidence of active bleeding, a contraindication to anticoagulation, receipt of prophylactic LMWH or UFH more than 72 hours prior to enrollment, treatment with an oral anticoagulant within 72 hours of enrollment, major surgery within the prior 3 months, cerebral stroke with bleeding, and persistent renal failure (creatinine clearance < 30 mL/min).
Results
The amended study population included 5,105 patients, 5,049 of whom received open-label enoxaparin. Of this group, 2,013 were randomized to active extended prophylaxis with enoxparain and 2,027 to placebo. Baseline characteristics, including level of mobility, were similar between the two groups.
The efficacy of extended prophylaxis with enoxaparin was enduring, as the cumulative incidence of VTE events at day 90 was significantly lower in enoxaparin recipients than in placebo recipients (3.0% vs 5.2%; relative reduction of 42%; P = .0115).
There was no difference in all-cause mortality at 6 months between the enoxaparin and placebo groups (10.1% vs 8.9%, respectively; P = .179).
Safety. Major hemorrhage was significantly more frequent in the enoxaparin arm, occurring in 0.60% of enoxaparin recipients compared with 0.15% of placebo recipients (P = .019). Minor bleeding was also more common with enoxaparin (5.20% vs 3.70%; P = .024).
Conclusions
The EXCLAIM trial found that an extended-duration (38-day) enoxaparin regimen significantly reduced the overall incidence of VTE relative to a 10-day enoxaparin regimen in acutely ill medical patients with reduced mobility. At the same time, the extended regimen was associated with a significant increase in the rate of major bleeding, although the incidence of major bleeding was low. The investigators concluded that the net clinical effect of extended-duration prophylaxis with enoxaparin is favorable, as only 46 patients would need to be treated to prevent one VTE event, whereas 224 patients would need to be treated to result in one major bleeding event.21
For this reason, it is reasonable to consider extended prophylaxis for hospitalized medical patients after identifying these patients’ risk factors. In keeping with the trial’s amended inclusion criteria, patients older than age 75 and those with cancer or prior VTE should receive special consideration for extended prophylaxis.
RECOMMENDED APPROACH TO VTE PREVENTION IN HOSPITALIZED MEDICAL PATIENTS
- All hospitalized medical patients should be screened at the time of admission, and patients at risk for VTE should receive prophylaxis.
- All patients with reduced mobility and one or more other risk factors for VTE are candidates for prophylaxis.
- Patients should be reassessed daily for the development of VTE risk factors during their hospitalization if risk factors are absent on admission.
- If screening or reassessment reveals any VTE risk factors, pharmacologic prophylaxis is the mainstay of therapy. If exclusion criteria for pharmacologic prophylaxis are present, mechanical prophylaxis with graduated compression stockings and intermittent compression devices should be used. For very high-risk medical patients without a contraindication to anticoagulants, combination prophylaxis with both an anticoagulant and mechanical devices is preferred.
- In this patient population, LMWH agents are preferred as pharmacologic prophylaxis over UFH and over fondaparinux (which is not currently approved by the US Food and Drug Administration for this population).
- If UFH is to be used in this patient population, 5,000 U three times daily is the preferred dosage.
- Extended pharmacologic prophylaxis should be considered in patients older than age 75 and in patients with a cancer diagnosis or a prior VTE episode.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: Dr. Spyropoulos, are there any guidelines, other than those from the ACCP, that speak to VTE prophylaxis in hospitalized medical patients? If so, what are their take-home messages and how do they differ from the ACCP guidelines?
Dr. Spyropoulos: I was part of the group that developed the International Consensus Statement (ICS) published in International Angiology in 2006,11 which is more recent than the latest ACCP guidelines, which were published in 2004. The ICS drew on much of the same data that the ACCP did, but we did an updated review of clinical trials.
For VTE prophylaxis in hospitalized medical patients, the ICS recommendations are more specific with regard to the type, dose, and dosing frequency of anticoagulant agents. First, they specify doses for both LMWH agents in this patient setting: 40 mg once daily for enoxaparin, and 5,000 IU once daily for dalteparin.
The ICS document also states that if UFH is the choice for prophylaxis, a regimen of 5,000 U three times daily should be considered. In the past year alone, two analyses suggest that three-times-daily dosing of UFH in medical patients provides superior efficacy to twice-daily dosing, although perhaps at the expense of more bleeding episodes.12,16 It is important to remember that no large placebo-controlled trial supports the efficacy of a UFH regimen of 5,000 U twice daily in this population.
Finally, the ICS document states that fondaparinux 2.5 mg once daily is a viable option for prophylaxis in medical patients, based on the ARTEMIS trial,3 even though this represents an off-label use.
Dr. Jaffer: Real-world use of VTE prophylaxis is far from optimal, especially in medical patients, and this is partly a result of system-of-care issues. I’d like to conclude by asking each of my colleagues to offer your perspectives on how your own institutions have improved their systems of care to promote better use of VTE prophylaxis and what lessons might be shared with others. Dr. McKean, you work at Brigham and Women’s Hospital, which recently reported impressive results with an electronic alert system designed to increase clinicians’ consideration of VTE risk assessment and use of prophylaxis.24 Please tell us about that study and the alert system.
Dr. McKean: Despite many educational initiatives at Brigham and Women’s Hospital, there were still some patients at high risk for VTE who were not receiving appropriate prophylaxis. What Dr. Samuel Goldhaber and his colleagues wanted to determine was whether changing the system of care could result in a reduced incidence of VTE.24 They devised a computer software program linked to the patient database that used eight common risk factors to determine each hospitalized patient’s risk profile for VTE. Each risk factor was weighted according to a point scale, with major risk factors (cancer, prior VTE, or hypercoagulability) assigned 3 points, the intermediate risk factor of surgery assigned 2 points, and minor risk factors (advanced age, obesity, immobility, or use of hormone replacement therapy or oral contraceptives) assigned 1 point. For patients with a total risk score of 4 or greater, the computer screen generates a color-coded VTE risk alert that requires the physician to acknowledge the alert and choose one of three options: order prophylaxis as appropriate, review a 60-page document on the computer to learn more about prophylaxis, or do nothing.
The study found that hospitalized patients who were randomized to treatment under the computer alert system were significantly more likely to receive VTE prophylaxis and significantly less likely to develop VTE than were patients randomized to a control group. The alert system reduced the risk of DVT or PE at 90 days by 41% in patients considered to be at high risk. It was particularly interesting that the incidence of VTE was lower in the intervention group even when physicians chose not to use prophylaxis, which suggests that simply having this alert system in place improved outcomes, perhaps by raising awareness of the risk of VTE.24
Additional studies are needed to better understand physicians’ behavior and determine why they seem to have a disproportionate fear of the risk of bleeding relative to the risk of clotting, including fatal PE, because that is really the heart of the matter. When patients are not given prophylaxis, often it is because of fear of bleeding. It is not clear, however, why some of these patients did not receive mechanical devices as an alternative form of prophylaxis, but this seems to be the case worldwide, as shown recently by the multinational ENDORSE study.22 Meanwhile, as we await studies to better understand physician perceptions and behaviors regarding prophylaxis, we need to work hard to change the system of care.
Dr. Deitelzweig: Over the past couple of years, the Ochsner Clinic has grown from a one-hospital teaching organization to a seven-hospital system with a mix of closed and open medical staff. The challenge is how to take a process that worked well in the one center, where appropriate prophylaxis was used about 90% of the time, and transfer it to the other centers in the larger system. We have endorsed several types of performance tools, such as the change-acceleration processes used by General Electric. The aim is to share a vision of heightening awareness. To do that, we have worked to mobilize the key stakeholders, at least half of them, to build algorithms that they all will endorse. It is easier said than done, however, and we have found it essential to involve both physicians and non-physician colleagues from pharmacy and nursing who have political and organizational clout.
Dr. Brotman: At Johns Hopkins, I took a bit more draconian approach to this issue because I thought that hospitalists often knew that they should be using VTE prophylaxis but sometimes weren’t, and I am not convinced that clinicians always look at prompts. So we came up with a system that incorporates both billing and documentation simultaneously. We put a hard stop on users’ documentation so that they could not sign off on a note or bill for their care until they checked off the kind of VTE prophylaxis they were using. Since hospitalists ultimately care about billing for their work, this system has at least ensured that everybody has considered and documented VTE prophylaxis on a daily basis. There are other hard stops that can be implemented in computer order-entry systems as well, and we are considering ways to roll them out on a broader scale.
However, all of these systems can have problems because patient situations change from day to day. For instance, VTE prophylaxis is not necessarily indicated in a 38-year-old ambulatory patient who comes in with a sickle cell crisis, but you will need to reconsider if the patient ends up in acute chest syndrome in the intensive care unit. I do not yet have a good way to ensure that this is being done on a daily basis with all patients.
Dr. Amin: At the University of California, Irvine, we implemented an electronic alert system, but we locked users in so that they could not complete their admission orders until they answered questions about VTE prevention. This practice increased our VTE prophylaxis rates tremendously. Because we are a level I trauma center, we allow users to bypass the screens one time, but the next time they log in, even to get a simple lab result, they have to answer the questions about VTE prevention.
With any system you develop, you also have to continue with the education process, because clinicians sometimes get into bad habits or simply forget things.
Dr. Spyropolous: At Lovelace Medical Center, we didn’t have the sophistication of an electronic order-entry system, but we had an experienced clinical pharmacist (the director of inpatient pharmacy) who helped to develop and champion VTE prevention guidelines that have then been used throughout the system in close conjunction with our hospitalists’ rounds. This system has been used successfully for the past 7 years.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thrombo-embolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med 1999; 341:793–800.
- Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 2004; 110:874–879.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 2006; 332:325–329.
- Baglin TP, White K, Charles A. Fatal pulmonary embolism in hos-pitalised medical patients. J Clin Pathol 1997; 50:609–610.
- Piazza G, Seddighzadeh A, Goldhaber SZ. Double trouble for 2,609 hospitalized medical patients who developed deep vein thrombosis: prophylaxis omitted more often and pulmonary embolism more frequent. Chest 2007; 132:554–561.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thrombo-embolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med 2007; 167:1476–1486.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost 2000; 83:14–19.
- Lechler E, Schramm W, Flosbach CW. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular-weight heparin (enoxaparin). The Prime Study Group. Haemostasis 1996; 26(Suppl 2):49–56.
- Kleber FX, Witt C, Vogel G, et al; the PRINCE Study Group. Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease. Am Heart J 2003; 145:614–621.
- King CS, Holley AB, Jackson JL, Shorr AF, Moores LK. Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a meta-analysis. Chest 2007; 131:507–516.
- Burleigh E, Wang C, Foster D, et al. Thromboprophylaxis in medically ill patients at risk for venous thromboembolism. Am J Health Syst Pharm 2006; 63(20 Suppl 6):S23–S29.
- Leykum L, Pugh J, Diuguid D, Papadopoulos K. Cost utility of substituting enoxaparin for unfractionated heparin for prophylaxis of venous thrombosis in the hospitalized medical patient. J Hosp Med 2006; 1:168–176.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med 2007; 167:1471–1475.
- Hull RD, Schellong SM Tapson VF, et al. Extended-duration venous thromboembolism (VTE) prophylaxis in acutely ill medical patients with recent reduced mobility: the EXCLAIM study. Presentation at: International Society on Thrombosis and Haemo-stasis XXIst Congress; July 6–12, 2007; Geneva, Switzerland.
- Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008; 371:387–394.
- Kahn SR, Panju A, Geerts W, et al; CURVE study investigators. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 2007; 119:145–155.
- Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent thromboembolism among hospitalized patients. N Engl J Med 2005; 352:969–977.
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med 1991; 151:933–938.
- Howell MD, Geraci JM, Knowlton AA. Congestive heart failure and outpatient risk of venous thromboembolism: a retrospective, case-control study. J Clin Epidemiol 2001; 54:810–816.
- Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet 2006; 367:1075–1079.
- Alikhan R, Cohen AT, Combe S, et al. Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Firbinolysis 2003; 14:341–346.
- Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003; 107(23 Suppl 1):I9–I16.
- Greinacher A, Warkentin TE. Recognition, treatment, and prevention of heparin-induced thrombocytopenia: review and update. Thromb Res 2006; 118:165–176.
- Martel N, Lee J, Wells PS. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 2005; 106:2710–2715.
- Sanderink GJ, Guimart CG, Ozoux ML, Jariwala NU, Shukla UA, Boutouyrie BX. Pharmacokinetics and pharmacodynamics of the prophylactic dose of enoxaparin once daily over 4 days in patients with renal impairment. Thromb Res 2002; 105:225–231.
- Douketis J, Cook D, Zytaruk N, et al. Dalteparin thromboprophylaxis in critically ill patients with severe renal insufficiency: the DIRECT study [abstract]. J Thromb Haemost 2007; 5(Suppl 2): P-S-680.
- Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 2002; 12:19–24.
The need for prophylaxis of venous thromboembolism (VTE) in hospitalized acutely ill medical patients is well established. Without prophylaxis, hospitalized medical patients develop VTE at a rate of 5% to 15%.1–3 Moreover, pulmonary embolism (PE) occurs more frequently in hospitalized medical patients than in nonmedical patients, and is a leading cause of sudden death in hospitalized medical patients.4,5 Without appropriate prophylaxis, 1 in 20 hospitalized medical patients may suffer a fatal PE.4
PROPHYLAXIS IN MEDICAL PATIENTS: UNDERUSED AND OFTEN INAPPROPRIATE
Despite these risks and the clear indications for VTE prophylaxis in hospitalized medical patients, prophylaxis of VTE is omitted more often in these patients than in hospitalized surgical patients.5 Even when prophylaxis is given, it is often used inappropriately in the medical population. So concludes a recent analysis of data from 196,104 patients with acute medical conditions who were discharged from 227 US hospitals from January 2002 to September 2005.6 Criteria for inclusion in the analysis were patient age of 40 years or older, a hospital stay of 6 days or greater, and an absence of contraindications to anticoagulation. Appropriate prophylaxis was defined in accordance with the Sixth American College of Chest Physicians (ACCP) Consensus Conference on Antithrombotic Therapy.7
The analysis revealed an overall VTE prophylaxis rate of 61.8%, but the rate of appropriate prophylaxis was only 33.9%, meaning that two-thirds of discharged patients did not receive prophylaxis in accordance with ACCP guidelines. When temporal trends were analyzed according to groups based on patients’ diagnosis at admission (acute myocardial infarction, severe lung disease, ischemic stroke, cancer, heart failure, or trauma), the rate of appropriate prophylaxis remained essentially flat from the beginning to the end of the study period for virtually all diagnosis groups.6
Similar findings have emerged from the International Medical Prevention Registry on Venous Thromboembolism (IMPROVE), an ongoing international registry of acutely ill medical patients.8 Data from the first 15,156 patients, enrolled from July 2002 through September 2006, reveal that 50% of patients received pharmacologic and/or mechanical VTE prophylaxis in the hospital, and only 60% of patients who met established criteria for VTE prophylaxis actually received it.
Analysis of the US portion of the IMPROVE data shows that 54% of the US patient sample received some form of VTE prophylaxis; 22% of US patients received intermittent pneumatic compression, 21% received unfractionated heparin (UFH), 14% received low-molecular-weight heparin (LMWH), and 3% wore compression stockings.8 Thus, despite a paucity of data supporting a benefit of intermittent pneumatic compression in this population,9 it was the most frequently used form of prophylaxis in US patients.
CLINICAL TRIALS OF PHARMACOLOGIC PROPHYLAXIS IN MEDICAL PATIENTS
The Prophylaxis in Medical Patients with Enoxaparin (MEDENOX) trial1 randomized 1,102 hospitalized patients to one of two doses of the LMWH enoxaparin (20 mg or 40 mg once daily subcutaneously) or placebo for 6 to 14 days. Compared with placebo, the 40-mg dose of enoxaparin was associated with a 63% reduction in risk of VTE over 3 months of follow-up (P < .001) (Figure 1).
The Prospective Evaluation of Dalteparin Efficacy for Prevention of VTE in Immobilized Patients Trial (PREVENT)2 was a multicenter, randomized, double-blind study comparing the LMWH dalteparin (5,000 IU daily given subcutaneously for 14 days) with placebo in 3,706 acutely ill medical patients. Over 90 days of follow-up, the risk of VTE was reduced by 44% in patients assigned to dalteparin compared with those assigned to placebo (P = .0015) (Figure 1).
The Arixtra for Thromboembolism Prevention in a Medical Indications Study (ARTEMIS)3 randomized 849 medical patients 60 years or older to 6 to 14 days of therapy with the selective factor Xa inhibitor fondaparinux (2.5 mg once daily subcutaneously) or placebo. Compared with the placebo group, fondaparinux recipients had a 47% lower risk of developing VTE by day 15 (P = .029) (Figure 1).
Fewer events and fatal PEs, but no effect on all-cause mortality
A recent meta-analysis by Dentali et al10 further demonstrates the efficacy of anticoagulant therapy for preventing symptomatic VTE in hospitalized medical patients. This analysis included several other trials in addition to the three reviewed above,1–3 for a total of nine randomized studies (seven of which were dou-ble-blind) comprising 19,958 patients. Across the nine studies, anticoagulant prophylaxis was clearly superior to placebo in preventing fatal PE (relative risk, 0.38 [95% CI, 0.21 to 0.69]). There was a strong trend toward a reduction in symptomatic deep vein thrombosis (DVT) with prophylaxis but no effect on all-cause mortality. The meta-analysis also provided reassurance that prophylaxis does not increase the rate of major bleeding.
HOW DO THE PROPHYLAXIS OPTIONS STACK UP?
What the ACCP recommends
Current ACCP guidelines recommend the use of either LMWH or low-dose UFH (5,000 U subcutaneously two or three times daily) as a Grade 1A recommendation for VTE prophylaxis in patients with medical conditions and risk factors for VTE.9 This represents the guidelines’ highest level of recommendation, ie, one that is based on randomized controlled trials (RCTs) without important limitations. In contrast, the 2006 International Consensus Statement, developed as a collaborative effort among expert bodies on VTE, specified a more narrow dosing recommendation for UFH in this patient population (5,000 U three times daily, not twice daily) as well as specifying 40 mg once daily as the recommended dose of enoxaparin and 5,000 IU once daily as the recommended dose of dalteparin.11
For medical patients with risk factors for VTE who have a contraindication to anticoagulant prophylaxis, the ACCP guidelines recommend the use of graduated compression stockings or intermittent pneumatic compression devices as a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”9).
Current ACCP guidelines do not address the use of fondaparinux in their recommendations for VTE prophylaxis in medical patients.
Getting a handle on bleeding risk
Patient characteristics that exclude pharmacologic thromboprophylaxis due to bleeding risk are generally limited to active bleeding or coagulopathy, as demonstrated by a platelet count less than 50,000 cells/µL or an international normalized ratio greater than 1.5. Additionally, bleeding risk should be carefully assessed if an invasive procedure is planned during a patient’s hospital stay.
It is worth noting that the anticoagulant doses used for VTE prophylaxis are a fraction of those used for treatment of VTE. Thus, if a patient would be treated with full-dose anticoagulation if VTE developed, then that patient should be eligible for VTE prophylaxis.
Because the use of mechanical forms of prophylaxis in medical patients is not truly evidence-based, mechanical prophylaxis should be reserved for medical patients who have a contraindication to anticoagulants, or for use in combination with anticoagulants in patients at very high risk of VTE.
UFH vs LMWH
Two meta-analyses have compared UFH with LMWH for VTE prevention in medical patients.12,13 In a recent analysis that included 10 trials directly comparing the two therapies, 14 trials comparing UFH with control, and 11 trials comparing LMWH with control, Wein et al found a lower risk of DVT with LMWH than with UFH (relative risk, 0.68 [95% CI, 0.52 to 0.88]) but no difference between the therapies in mortality or bleeding risk.12 In an earlier and smaller analysis, Mismetti et al found no significant differences between UFH and LMWH in preventing DVT or death but did find a significant reduction in major bleeding episodes with LMWH versus three-times-daily UFH (52% relative reduction; P = .049).13
Randomized trials also reveal that enoxaparin 40 mg once daily is as efficacious as UFH 5,000 U three times daily for VTE prevention in medical patients.14,15 The above analysis by Wein et al12 and an additional meta-analysis by King and colleagues16 found that three-times-daily dosing of UFH is more efficacious than twice-daily dosing of UFH, but at the expense of more bleeding, including major bleeding.
Economic considerations
Because of differences in drug acquisition costs between UFH and the LMWH agents, several economic evaluations have compared the use of these therapies for prophylaxis in medical patients at risk of VTE.
In an analysis of hospital costs for medical patients receiving VTE prophylaxis from more than 330 US hospitals for the period 2001–2004, Burleigh et al found that mean total hospital costs were higher for patients who received UFH than for those who received LMWH ($7,615 vs $6,866) even though mean drug costs were higher for LMWH ($791 vs $569 for UFH).17 A reduction in hospital length of stay appeared to contribute to the overall savings with LMWH; other contributors may have included costs associated with heparin-induced thrombocytopenia (HIT) in UFH recipients or the extra nursing time required for administering UFH in two or three daily doses.
Leykum et al used a decision analysis model to estimate the economic effect of substituting enoxaparin for UFH in hospitalized medical patients for whom VTE prophylaxis is indicated.18 Cost data were based on Medicare reimbursement rates as well as drug and laboratory costs for a multi-institutional health system. The model assumed HIT incidence rates of 2.7% with UFH and 0.3% with enoxaparin. It also assumed the cost of a daily dose to be $4 for UFH versus $84 for enoxaparin. From the payer perspective, the model showed that substituting enoxaparin for UFH would reduce the overall cost of care by $28.61 per day on a per-patient basis, despite enoxaparin’s higher acquisition cost, and would save $4,550 per quality-adjusted life-year by reducing the incidence of HIT.
Another cost analysis confirms the association between HIT and increased hospital costs. Creekmore et al retrospectively analyzed data from 10,121 adult medical patients who received VTE prophylaxis at the University of Utah Hospital in Salt Lake City from August 2000 to November 2004.19 They found that an admission during which HIT developed incurred a mean cost of $56,364, compared with $15,231 for an admission without HIT. Because LMWH was associated with a lower incidence of HIT compared with UFH (0.084% vs 0.51%, respectively), LMWH reduced the incremental cost of VTE prophylaxis by $13.88 per patient compared with UFH.
THE EXCLAIM TRIAL: IS THERE A ROLE FOR EXTENDED PROPHYLAXIS?
Although the previously discussed studies have clearly demonstrated the benefit of in-hospital VTE prophylaxis for acutely ill medical patients, none has rigorously examined extended-duration out-of-hospital prophylaxis in these patients. This represents an important gap in the literature, since a substantial proportion of VTE develops in the outpatient setting within 3 months of a hospitalization, and most outpatient VTE episodes occur within 1 month of a preceding hospitalization.20
To begin to fill this gap, the Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial was conducted to compare extended-duration LMWH prophylaxis with a standard LMWH prophylaxis regimen in acutely ill medical patients using a prospective, multicenter, randomized, double-blind, placebo-controlled design.21
Patients and study design
Patients were eligible for enrollment if they were aged 40 years or older and had recent immobilization (≤ 3 days), a predefined acute medical illness, and either level 1 mobility (total bed rest or sedentary state) or level 2 mobility (level 1 with bathroom privileges). The predefined acute medical illnesses consisted of New York Heart Association class III/IV heart failure, acute respiratory insufficiency, or other acute medical conditions, including post-acute ischemic stroke, acute infection without septic shock, and active cancer.
All patients received open-label enoxaparin 40 mg subcutaneously once daily for 10 ± 4 days, after which they were randomized to either enoxaparin 40 mg subcutaneously once daily or placebo for an additional 28 ± 4 days.
The primary efficacy end point was the incidence of VTE events, defined as asymptomatic DVT documented by mandatory ultrasonography at the end of the double-blind treatment period (28 ± 4 days) or as symptomatic DVT, symptomatic PE, or fatal PE at any time during the double-blind period. Symptomatic DVT was confirmed by objective tests; PE was confirmed by ventilation-perfusion scan, computed tomography, angiography, or autopsy.
Secondary efficacy end points were mortality at the end of the double-blind period, at 3 months, and at 6 months, as well as the incidence of VTE at 3 months.
The primary safety outcome measure was the incidence of major hemorrhage during the double-blind period; secondary safety measures were rates of major and minor hemorrhage, minor hemorrhage, HIT, and serious adverse events.
Population amended at planned interim analysis
After approximately half of the patients were enrolled, a planned and blinded interim analysis for futility concluded that the study was unlikely to show a statistically significant advantage of enoxaparin over placebo. The trial’s steering committee followed the suggestion of its data safety monitoring board to redefine the inclusion criteria to refocus enrollment on patients with a high risk of VTE. A blinded analysis was performed to identify this subgroup.
The resulting amended inclusion criteria were the same as above except that level 2 mobility had to be accompanied by at least one of three additional high-risk criteria: (1) age greater than 75 years, (2) history of prior VTE, or (3) diagnosis of cancer.
The trial’s main exclusion criteria were evidence of active bleeding, a contraindication to anticoagulation, receipt of prophylactic LMWH or UFH more than 72 hours prior to enrollment, treatment with an oral anticoagulant within 72 hours of enrollment, major surgery within the prior 3 months, cerebral stroke with bleeding, and persistent renal failure (creatinine clearance < 30 mL/min).
Results
The amended study population included 5,105 patients, 5,049 of whom received open-label enoxaparin. Of this group, 2,013 were randomized to active extended prophylaxis with enoxparain and 2,027 to placebo. Baseline characteristics, including level of mobility, were similar between the two groups.
The efficacy of extended prophylaxis with enoxaparin was enduring, as the cumulative incidence of VTE events at day 90 was significantly lower in enoxaparin recipients than in placebo recipients (3.0% vs 5.2%; relative reduction of 42%; P = .0115).
There was no difference in all-cause mortality at 6 months between the enoxaparin and placebo groups (10.1% vs 8.9%, respectively; P = .179).
Safety. Major hemorrhage was significantly more frequent in the enoxaparin arm, occurring in 0.60% of enoxaparin recipients compared with 0.15% of placebo recipients (P = .019). Minor bleeding was also more common with enoxaparin (5.20% vs 3.70%; P = .024).
Conclusions
The EXCLAIM trial found that an extended-duration (38-day) enoxaparin regimen significantly reduced the overall incidence of VTE relative to a 10-day enoxaparin regimen in acutely ill medical patients with reduced mobility. At the same time, the extended regimen was associated with a significant increase in the rate of major bleeding, although the incidence of major bleeding was low. The investigators concluded that the net clinical effect of extended-duration prophylaxis with enoxaparin is favorable, as only 46 patients would need to be treated to prevent one VTE event, whereas 224 patients would need to be treated to result in one major bleeding event.21
For this reason, it is reasonable to consider extended prophylaxis for hospitalized medical patients after identifying these patients’ risk factors. In keeping with the trial’s amended inclusion criteria, patients older than age 75 and those with cancer or prior VTE should receive special consideration for extended prophylaxis.
RECOMMENDED APPROACH TO VTE PREVENTION IN HOSPITALIZED MEDICAL PATIENTS
- All hospitalized medical patients should be screened at the time of admission, and patients at risk for VTE should receive prophylaxis.
- All patients with reduced mobility and one or more other risk factors for VTE are candidates for prophylaxis.
- Patients should be reassessed daily for the development of VTE risk factors during their hospitalization if risk factors are absent on admission.
- If screening or reassessment reveals any VTE risk factors, pharmacologic prophylaxis is the mainstay of therapy. If exclusion criteria for pharmacologic prophylaxis are present, mechanical prophylaxis with graduated compression stockings and intermittent compression devices should be used. For very high-risk medical patients without a contraindication to anticoagulants, combination prophylaxis with both an anticoagulant and mechanical devices is preferred.
- In this patient population, LMWH agents are preferred as pharmacologic prophylaxis over UFH and over fondaparinux (which is not currently approved by the US Food and Drug Administration for this population).
- If UFH is to be used in this patient population, 5,000 U three times daily is the preferred dosage.
- Extended pharmacologic prophylaxis should be considered in patients older than age 75 and in patients with a cancer diagnosis or a prior VTE episode.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: Dr. Spyropoulos, are there any guidelines, other than those from the ACCP, that speak to VTE prophylaxis in hospitalized medical patients? If so, what are their take-home messages and how do they differ from the ACCP guidelines?
Dr. Spyropoulos: I was part of the group that developed the International Consensus Statement (ICS) published in International Angiology in 2006,11 which is more recent than the latest ACCP guidelines, which were published in 2004. The ICS drew on much of the same data that the ACCP did, but we did an updated review of clinical trials.
For VTE prophylaxis in hospitalized medical patients, the ICS recommendations are more specific with regard to the type, dose, and dosing frequency of anticoagulant agents. First, they specify doses for both LMWH agents in this patient setting: 40 mg once daily for enoxaparin, and 5,000 IU once daily for dalteparin.
The ICS document also states that if UFH is the choice for prophylaxis, a regimen of 5,000 U three times daily should be considered. In the past year alone, two analyses suggest that three-times-daily dosing of UFH in medical patients provides superior efficacy to twice-daily dosing, although perhaps at the expense of more bleeding episodes.12,16 It is important to remember that no large placebo-controlled trial supports the efficacy of a UFH regimen of 5,000 U twice daily in this population.
Finally, the ICS document states that fondaparinux 2.5 mg once daily is a viable option for prophylaxis in medical patients, based on the ARTEMIS trial,3 even though this represents an off-label use.
Dr. Jaffer: Real-world use of VTE prophylaxis is far from optimal, especially in medical patients, and this is partly a result of system-of-care issues. I’d like to conclude by asking each of my colleagues to offer your perspectives on how your own institutions have improved their systems of care to promote better use of VTE prophylaxis and what lessons might be shared with others. Dr. McKean, you work at Brigham and Women’s Hospital, which recently reported impressive results with an electronic alert system designed to increase clinicians’ consideration of VTE risk assessment and use of prophylaxis.24 Please tell us about that study and the alert system.
Dr. McKean: Despite many educational initiatives at Brigham and Women’s Hospital, there were still some patients at high risk for VTE who were not receiving appropriate prophylaxis. What Dr. Samuel Goldhaber and his colleagues wanted to determine was whether changing the system of care could result in a reduced incidence of VTE.24 They devised a computer software program linked to the patient database that used eight common risk factors to determine each hospitalized patient’s risk profile for VTE. Each risk factor was weighted according to a point scale, with major risk factors (cancer, prior VTE, or hypercoagulability) assigned 3 points, the intermediate risk factor of surgery assigned 2 points, and minor risk factors (advanced age, obesity, immobility, or use of hormone replacement therapy or oral contraceptives) assigned 1 point. For patients with a total risk score of 4 or greater, the computer screen generates a color-coded VTE risk alert that requires the physician to acknowledge the alert and choose one of three options: order prophylaxis as appropriate, review a 60-page document on the computer to learn more about prophylaxis, or do nothing.
The study found that hospitalized patients who were randomized to treatment under the computer alert system were significantly more likely to receive VTE prophylaxis and significantly less likely to develop VTE than were patients randomized to a control group. The alert system reduced the risk of DVT or PE at 90 days by 41% in patients considered to be at high risk. It was particularly interesting that the incidence of VTE was lower in the intervention group even when physicians chose not to use prophylaxis, which suggests that simply having this alert system in place improved outcomes, perhaps by raising awareness of the risk of VTE.24
Additional studies are needed to better understand physicians’ behavior and determine why they seem to have a disproportionate fear of the risk of bleeding relative to the risk of clotting, including fatal PE, because that is really the heart of the matter. When patients are not given prophylaxis, often it is because of fear of bleeding. It is not clear, however, why some of these patients did not receive mechanical devices as an alternative form of prophylaxis, but this seems to be the case worldwide, as shown recently by the multinational ENDORSE study.22 Meanwhile, as we await studies to better understand physician perceptions and behaviors regarding prophylaxis, we need to work hard to change the system of care.
Dr. Deitelzweig: Over the past couple of years, the Ochsner Clinic has grown from a one-hospital teaching organization to a seven-hospital system with a mix of closed and open medical staff. The challenge is how to take a process that worked well in the one center, where appropriate prophylaxis was used about 90% of the time, and transfer it to the other centers in the larger system. We have endorsed several types of performance tools, such as the change-acceleration processes used by General Electric. The aim is to share a vision of heightening awareness. To do that, we have worked to mobilize the key stakeholders, at least half of them, to build algorithms that they all will endorse. It is easier said than done, however, and we have found it essential to involve both physicians and non-physician colleagues from pharmacy and nursing who have political and organizational clout.
Dr. Brotman: At Johns Hopkins, I took a bit more draconian approach to this issue because I thought that hospitalists often knew that they should be using VTE prophylaxis but sometimes weren’t, and I am not convinced that clinicians always look at prompts. So we came up with a system that incorporates both billing and documentation simultaneously. We put a hard stop on users’ documentation so that they could not sign off on a note or bill for their care until they checked off the kind of VTE prophylaxis they were using. Since hospitalists ultimately care about billing for their work, this system has at least ensured that everybody has considered and documented VTE prophylaxis on a daily basis. There are other hard stops that can be implemented in computer order-entry systems as well, and we are considering ways to roll them out on a broader scale.
However, all of these systems can have problems because patient situations change from day to day. For instance, VTE prophylaxis is not necessarily indicated in a 38-year-old ambulatory patient who comes in with a sickle cell crisis, but you will need to reconsider if the patient ends up in acute chest syndrome in the intensive care unit. I do not yet have a good way to ensure that this is being done on a daily basis with all patients.
Dr. Amin: At the University of California, Irvine, we implemented an electronic alert system, but we locked users in so that they could not complete their admission orders until they answered questions about VTE prevention. This practice increased our VTE prophylaxis rates tremendously. Because we are a level I trauma center, we allow users to bypass the screens one time, but the next time they log in, even to get a simple lab result, they have to answer the questions about VTE prevention.
With any system you develop, you also have to continue with the education process, because clinicians sometimes get into bad habits or simply forget things.
Dr. Spyropolous: At Lovelace Medical Center, we didn’t have the sophistication of an electronic order-entry system, but we had an experienced clinical pharmacist (the director of inpatient pharmacy) who helped to develop and champion VTE prevention guidelines that have then been used throughout the system in close conjunction with our hospitalists’ rounds. This system has been used successfully for the past 7 years.
The need for prophylaxis of venous thromboembolism (VTE) in hospitalized acutely ill medical patients is well established. Without prophylaxis, hospitalized medical patients develop VTE at a rate of 5% to 15%.1–3 Moreover, pulmonary embolism (PE) occurs more frequently in hospitalized medical patients than in nonmedical patients, and is a leading cause of sudden death in hospitalized medical patients.4,5 Without appropriate prophylaxis, 1 in 20 hospitalized medical patients may suffer a fatal PE.4
PROPHYLAXIS IN MEDICAL PATIENTS: UNDERUSED AND OFTEN INAPPROPRIATE
Despite these risks and the clear indications for VTE prophylaxis in hospitalized medical patients, prophylaxis of VTE is omitted more often in these patients than in hospitalized surgical patients.5 Even when prophylaxis is given, it is often used inappropriately in the medical population. So concludes a recent analysis of data from 196,104 patients with acute medical conditions who were discharged from 227 US hospitals from January 2002 to September 2005.6 Criteria for inclusion in the analysis were patient age of 40 years or older, a hospital stay of 6 days or greater, and an absence of contraindications to anticoagulation. Appropriate prophylaxis was defined in accordance with the Sixth American College of Chest Physicians (ACCP) Consensus Conference on Antithrombotic Therapy.7
The analysis revealed an overall VTE prophylaxis rate of 61.8%, but the rate of appropriate prophylaxis was only 33.9%, meaning that two-thirds of discharged patients did not receive prophylaxis in accordance with ACCP guidelines. When temporal trends were analyzed according to groups based on patients’ diagnosis at admission (acute myocardial infarction, severe lung disease, ischemic stroke, cancer, heart failure, or trauma), the rate of appropriate prophylaxis remained essentially flat from the beginning to the end of the study period for virtually all diagnosis groups.6
Similar findings have emerged from the International Medical Prevention Registry on Venous Thromboembolism (IMPROVE), an ongoing international registry of acutely ill medical patients.8 Data from the first 15,156 patients, enrolled from July 2002 through September 2006, reveal that 50% of patients received pharmacologic and/or mechanical VTE prophylaxis in the hospital, and only 60% of patients who met established criteria for VTE prophylaxis actually received it.
Analysis of the US portion of the IMPROVE data shows that 54% of the US patient sample received some form of VTE prophylaxis; 22% of US patients received intermittent pneumatic compression, 21% received unfractionated heparin (UFH), 14% received low-molecular-weight heparin (LMWH), and 3% wore compression stockings.8 Thus, despite a paucity of data supporting a benefit of intermittent pneumatic compression in this population,9 it was the most frequently used form of prophylaxis in US patients.
CLINICAL TRIALS OF PHARMACOLOGIC PROPHYLAXIS IN MEDICAL PATIENTS
The Prophylaxis in Medical Patients with Enoxaparin (MEDENOX) trial1 randomized 1,102 hospitalized patients to one of two doses of the LMWH enoxaparin (20 mg or 40 mg once daily subcutaneously) or placebo for 6 to 14 days. Compared with placebo, the 40-mg dose of enoxaparin was associated with a 63% reduction in risk of VTE over 3 months of follow-up (P < .001) (Figure 1).
The Prospective Evaluation of Dalteparin Efficacy for Prevention of VTE in Immobilized Patients Trial (PREVENT)2 was a multicenter, randomized, double-blind study comparing the LMWH dalteparin (5,000 IU daily given subcutaneously for 14 days) with placebo in 3,706 acutely ill medical patients. Over 90 days of follow-up, the risk of VTE was reduced by 44% in patients assigned to dalteparin compared with those assigned to placebo (P = .0015) (Figure 1).
The Arixtra for Thromboembolism Prevention in a Medical Indications Study (ARTEMIS)3 randomized 849 medical patients 60 years or older to 6 to 14 days of therapy with the selective factor Xa inhibitor fondaparinux (2.5 mg once daily subcutaneously) or placebo. Compared with the placebo group, fondaparinux recipients had a 47% lower risk of developing VTE by day 15 (P = .029) (Figure 1).
Fewer events and fatal PEs, but no effect on all-cause mortality
A recent meta-analysis by Dentali et al10 further demonstrates the efficacy of anticoagulant therapy for preventing symptomatic VTE in hospitalized medical patients. This analysis included several other trials in addition to the three reviewed above,1–3 for a total of nine randomized studies (seven of which were dou-ble-blind) comprising 19,958 patients. Across the nine studies, anticoagulant prophylaxis was clearly superior to placebo in preventing fatal PE (relative risk, 0.38 [95% CI, 0.21 to 0.69]). There was a strong trend toward a reduction in symptomatic deep vein thrombosis (DVT) with prophylaxis but no effect on all-cause mortality. The meta-analysis also provided reassurance that prophylaxis does not increase the rate of major bleeding.
HOW DO THE PROPHYLAXIS OPTIONS STACK UP?
What the ACCP recommends
Current ACCP guidelines recommend the use of either LMWH or low-dose UFH (5,000 U subcutaneously two or three times daily) as a Grade 1A recommendation for VTE prophylaxis in patients with medical conditions and risk factors for VTE.9 This represents the guidelines’ highest level of recommendation, ie, one that is based on randomized controlled trials (RCTs) without important limitations. In contrast, the 2006 International Consensus Statement, developed as a collaborative effort among expert bodies on VTE, specified a more narrow dosing recommendation for UFH in this patient population (5,000 U three times daily, not twice daily) as well as specifying 40 mg once daily as the recommended dose of enoxaparin and 5,000 IU once daily as the recommended dose of dalteparin.11
For medical patients with risk factors for VTE who have a contraindication to anticoagulant prophylaxis, the ACCP guidelines recommend the use of graduated compression stockings or intermittent pneumatic compression devices as a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”9).
Current ACCP guidelines do not address the use of fondaparinux in their recommendations for VTE prophylaxis in medical patients.
Getting a handle on bleeding risk
Patient characteristics that exclude pharmacologic thromboprophylaxis due to bleeding risk are generally limited to active bleeding or coagulopathy, as demonstrated by a platelet count less than 50,000 cells/µL or an international normalized ratio greater than 1.5. Additionally, bleeding risk should be carefully assessed if an invasive procedure is planned during a patient’s hospital stay.
It is worth noting that the anticoagulant doses used for VTE prophylaxis are a fraction of those used for treatment of VTE. Thus, if a patient would be treated with full-dose anticoagulation if VTE developed, then that patient should be eligible for VTE prophylaxis.
Because the use of mechanical forms of prophylaxis in medical patients is not truly evidence-based, mechanical prophylaxis should be reserved for medical patients who have a contraindication to anticoagulants, or for use in combination with anticoagulants in patients at very high risk of VTE.
UFH vs LMWH
Two meta-analyses have compared UFH with LMWH for VTE prevention in medical patients.12,13 In a recent analysis that included 10 trials directly comparing the two therapies, 14 trials comparing UFH with control, and 11 trials comparing LMWH with control, Wein et al found a lower risk of DVT with LMWH than with UFH (relative risk, 0.68 [95% CI, 0.52 to 0.88]) but no difference between the therapies in mortality or bleeding risk.12 In an earlier and smaller analysis, Mismetti et al found no significant differences between UFH and LMWH in preventing DVT or death but did find a significant reduction in major bleeding episodes with LMWH versus three-times-daily UFH (52% relative reduction; P = .049).13
Randomized trials also reveal that enoxaparin 40 mg once daily is as efficacious as UFH 5,000 U three times daily for VTE prevention in medical patients.14,15 The above analysis by Wein et al12 and an additional meta-analysis by King and colleagues16 found that three-times-daily dosing of UFH is more efficacious than twice-daily dosing of UFH, but at the expense of more bleeding, including major bleeding.
Economic considerations
Because of differences in drug acquisition costs between UFH and the LMWH agents, several economic evaluations have compared the use of these therapies for prophylaxis in medical patients at risk of VTE.
In an analysis of hospital costs for medical patients receiving VTE prophylaxis from more than 330 US hospitals for the period 2001–2004, Burleigh et al found that mean total hospital costs were higher for patients who received UFH than for those who received LMWH ($7,615 vs $6,866) even though mean drug costs were higher for LMWH ($791 vs $569 for UFH).17 A reduction in hospital length of stay appeared to contribute to the overall savings with LMWH; other contributors may have included costs associated with heparin-induced thrombocytopenia (HIT) in UFH recipients or the extra nursing time required for administering UFH in two or three daily doses.
Leykum et al used a decision analysis model to estimate the economic effect of substituting enoxaparin for UFH in hospitalized medical patients for whom VTE prophylaxis is indicated.18 Cost data were based on Medicare reimbursement rates as well as drug and laboratory costs for a multi-institutional health system. The model assumed HIT incidence rates of 2.7% with UFH and 0.3% with enoxaparin. It also assumed the cost of a daily dose to be $4 for UFH versus $84 for enoxaparin. From the payer perspective, the model showed that substituting enoxaparin for UFH would reduce the overall cost of care by $28.61 per day on a per-patient basis, despite enoxaparin’s higher acquisition cost, and would save $4,550 per quality-adjusted life-year by reducing the incidence of HIT.
Another cost analysis confirms the association between HIT and increased hospital costs. Creekmore et al retrospectively analyzed data from 10,121 adult medical patients who received VTE prophylaxis at the University of Utah Hospital in Salt Lake City from August 2000 to November 2004.19 They found that an admission during which HIT developed incurred a mean cost of $56,364, compared with $15,231 for an admission without HIT. Because LMWH was associated with a lower incidence of HIT compared with UFH (0.084% vs 0.51%, respectively), LMWH reduced the incremental cost of VTE prophylaxis by $13.88 per patient compared with UFH.
THE EXCLAIM TRIAL: IS THERE A ROLE FOR EXTENDED PROPHYLAXIS?
Although the previously discussed studies have clearly demonstrated the benefit of in-hospital VTE prophylaxis for acutely ill medical patients, none has rigorously examined extended-duration out-of-hospital prophylaxis in these patients. This represents an important gap in the literature, since a substantial proportion of VTE develops in the outpatient setting within 3 months of a hospitalization, and most outpatient VTE episodes occur within 1 month of a preceding hospitalization.20
To begin to fill this gap, the Extended Clinical Prophylaxis in Acutely Ill Medical Patients (EXCLAIM) trial was conducted to compare extended-duration LMWH prophylaxis with a standard LMWH prophylaxis regimen in acutely ill medical patients using a prospective, multicenter, randomized, double-blind, placebo-controlled design.21
Patients and study design
Patients were eligible for enrollment if they were aged 40 years or older and had recent immobilization (≤ 3 days), a predefined acute medical illness, and either level 1 mobility (total bed rest or sedentary state) or level 2 mobility (level 1 with bathroom privileges). The predefined acute medical illnesses consisted of New York Heart Association class III/IV heart failure, acute respiratory insufficiency, or other acute medical conditions, including post-acute ischemic stroke, acute infection without septic shock, and active cancer.
All patients received open-label enoxaparin 40 mg subcutaneously once daily for 10 ± 4 days, after which they were randomized to either enoxaparin 40 mg subcutaneously once daily or placebo for an additional 28 ± 4 days.
The primary efficacy end point was the incidence of VTE events, defined as asymptomatic DVT documented by mandatory ultrasonography at the end of the double-blind treatment period (28 ± 4 days) or as symptomatic DVT, symptomatic PE, or fatal PE at any time during the double-blind period. Symptomatic DVT was confirmed by objective tests; PE was confirmed by ventilation-perfusion scan, computed tomography, angiography, or autopsy.
Secondary efficacy end points were mortality at the end of the double-blind period, at 3 months, and at 6 months, as well as the incidence of VTE at 3 months.
The primary safety outcome measure was the incidence of major hemorrhage during the double-blind period; secondary safety measures were rates of major and minor hemorrhage, minor hemorrhage, HIT, and serious adverse events.
Population amended at planned interim analysis
After approximately half of the patients were enrolled, a planned and blinded interim analysis for futility concluded that the study was unlikely to show a statistically significant advantage of enoxaparin over placebo. The trial’s steering committee followed the suggestion of its data safety monitoring board to redefine the inclusion criteria to refocus enrollment on patients with a high risk of VTE. A blinded analysis was performed to identify this subgroup.
The resulting amended inclusion criteria were the same as above except that level 2 mobility had to be accompanied by at least one of three additional high-risk criteria: (1) age greater than 75 years, (2) history of prior VTE, or (3) diagnosis of cancer.
The trial’s main exclusion criteria were evidence of active bleeding, a contraindication to anticoagulation, receipt of prophylactic LMWH or UFH more than 72 hours prior to enrollment, treatment with an oral anticoagulant within 72 hours of enrollment, major surgery within the prior 3 months, cerebral stroke with bleeding, and persistent renal failure (creatinine clearance < 30 mL/min).
Results
The amended study population included 5,105 patients, 5,049 of whom received open-label enoxaparin. Of this group, 2,013 were randomized to active extended prophylaxis with enoxparain and 2,027 to placebo. Baseline characteristics, including level of mobility, were similar between the two groups.
The efficacy of extended prophylaxis with enoxaparin was enduring, as the cumulative incidence of VTE events at day 90 was significantly lower in enoxaparin recipients than in placebo recipients (3.0% vs 5.2%; relative reduction of 42%; P = .0115).
There was no difference in all-cause mortality at 6 months between the enoxaparin and placebo groups (10.1% vs 8.9%, respectively; P = .179).
Safety. Major hemorrhage was significantly more frequent in the enoxaparin arm, occurring in 0.60% of enoxaparin recipients compared with 0.15% of placebo recipients (P = .019). Minor bleeding was also more common with enoxaparin (5.20% vs 3.70%; P = .024).
Conclusions
The EXCLAIM trial found that an extended-duration (38-day) enoxaparin regimen significantly reduced the overall incidence of VTE relative to a 10-day enoxaparin regimen in acutely ill medical patients with reduced mobility. At the same time, the extended regimen was associated with a significant increase in the rate of major bleeding, although the incidence of major bleeding was low. The investigators concluded that the net clinical effect of extended-duration prophylaxis with enoxaparin is favorable, as only 46 patients would need to be treated to prevent one VTE event, whereas 224 patients would need to be treated to result in one major bleeding event.21
For this reason, it is reasonable to consider extended prophylaxis for hospitalized medical patients after identifying these patients’ risk factors. In keeping with the trial’s amended inclusion criteria, patients older than age 75 and those with cancer or prior VTE should receive special consideration for extended prophylaxis.
RECOMMENDED APPROACH TO VTE PREVENTION IN HOSPITALIZED MEDICAL PATIENTS
- All hospitalized medical patients should be screened at the time of admission, and patients at risk for VTE should receive prophylaxis.
- All patients with reduced mobility and one or more other risk factors for VTE are candidates for prophylaxis.
- Patients should be reassessed daily for the development of VTE risk factors during their hospitalization if risk factors are absent on admission.
- If screening or reassessment reveals any VTE risk factors, pharmacologic prophylaxis is the mainstay of therapy. If exclusion criteria for pharmacologic prophylaxis are present, mechanical prophylaxis with graduated compression stockings and intermittent compression devices should be used. For very high-risk medical patients without a contraindication to anticoagulants, combination prophylaxis with both an anticoagulant and mechanical devices is preferred.
- In this patient population, LMWH agents are preferred as pharmacologic prophylaxis over UFH and over fondaparinux (which is not currently approved by the US Food and Drug Administration for this population).
- If UFH is to be used in this patient population, 5,000 U three times daily is the preferred dosage.
- Extended pharmacologic prophylaxis should be considered in patients older than age 75 and in patients with a cancer diagnosis or a prior VTE episode.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: Dr. Spyropoulos, are there any guidelines, other than those from the ACCP, that speak to VTE prophylaxis in hospitalized medical patients? If so, what are their take-home messages and how do they differ from the ACCP guidelines?
Dr. Spyropoulos: I was part of the group that developed the International Consensus Statement (ICS) published in International Angiology in 2006,11 which is more recent than the latest ACCP guidelines, which were published in 2004. The ICS drew on much of the same data that the ACCP did, but we did an updated review of clinical trials.
For VTE prophylaxis in hospitalized medical patients, the ICS recommendations are more specific with regard to the type, dose, and dosing frequency of anticoagulant agents. First, they specify doses for both LMWH agents in this patient setting: 40 mg once daily for enoxaparin, and 5,000 IU once daily for dalteparin.
The ICS document also states that if UFH is the choice for prophylaxis, a regimen of 5,000 U three times daily should be considered. In the past year alone, two analyses suggest that three-times-daily dosing of UFH in medical patients provides superior efficacy to twice-daily dosing, although perhaps at the expense of more bleeding episodes.12,16 It is important to remember that no large placebo-controlled trial supports the efficacy of a UFH regimen of 5,000 U twice daily in this population.
Finally, the ICS document states that fondaparinux 2.5 mg once daily is a viable option for prophylaxis in medical patients, based on the ARTEMIS trial,3 even though this represents an off-label use.
Dr. Jaffer: Real-world use of VTE prophylaxis is far from optimal, especially in medical patients, and this is partly a result of system-of-care issues. I’d like to conclude by asking each of my colleagues to offer your perspectives on how your own institutions have improved their systems of care to promote better use of VTE prophylaxis and what lessons might be shared with others. Dr. McKean, you work at Brigham and Women’s Hospital, which recently reported impressive results with an electronic alert system designed to increase clinicians’ consideration of VTE risk assessment and use of prophylaxis.24 Please tell us about that study and the alert system.
Dr. McKean: Despite many educational initiatives at Brigham and Women’s Hospital, there were still some patients at high risk for VTE who were not receiving appropriate prophylaxis. What Dr. Samuel Goldhaber and his colleagues wanted to determine was whether changing the system of care could result in a reduced incidence of VTE.24 They devised a computer software program linked to the patient database that used eight common risk factors to determine each hospitalized patient’s risk profile for VTE. Each risk factor was weighted according to a point scale, with major risk factors (cancer, prior VTE, or hypercoagulability) assigned 3 points, the intermediate risk factor of surgery assigned 2 points, and minor risk factors (advanced age, obesity, immobility, or use of hormone replacement therapy or oral contraceptives) assigned 1 point. For patients with a total risk score of 4 or greater, the computer screen generates a color-coded VTE risk alert that requires the physician to acknowledge the alert and choose one of three options: order prophylaxis as appropriate, review a 60-page document on the computer to learn more about prophylaxis, or do nothing.
The study found that hospitalized patients who were randomized to treatment under the computer alert system were significantly more likely to receive VTE prophylaxis and significantly less likely to develop VTE than were patients randomized to a control group. The alert system reduced the risk of DVT or PE at 90 days by 41% in patients considered to be at high risk. It was particularly interesting that the incidence of VTE was lower in the intervention group even when physicians chose not to use prophylaxis, which suggests that simply having this alert system in place improved outcomes, perhaps by raising awareness of the risk of VTE.24
Additional studies are needed to better understand physicians’ behavior and determine why they seem to have a disproportionate fear of the risk of bleeding relative to the risk of clotting, including fatal PE, because that is really the heart of the matter. When patients are not given prophylaxis, often it is because of fear of bleeding. It is not clear, however, why some of these patients did not receive mechanical devices as an alternative form of prophylaxis, but this seems to be the case worldwide, as shown recently by the multinational ENDORSE study.22 Meanwhile, as we await studies to better understand physician perceptions and behaviors regarding prophylaxis, we need to work hard to change the system of care.
Dr. Deitelzweig: Over the past couple of years, the Ochsner Clinic has grown from a one-hospital teaching organization to a seven-hospital system with a mix of closed and open medical staff. The challenge is how to take a process that worked well in the one center, where appropriate prophylaxis was used about 90% of the time, and transfer it to the other centers in the larger system. We have endorsed several types of performance tools, such as the change-acceleration processes used by General Electric. The aim is to share a vision of heightening awareness. To do that, we have worked to mobilize the key stakeholders, at least half of them, to build algorithms that they all will endorse. It is easier said than done, however, and we have found it essential to involve both physicians and non-physician colleagues from pharmacy and nursing who have political and organizational clout.
Dr. Brotman: At Johns Hopkins, I took a bit more draconian approach to this issue because I thought that hospitalists often knew that they should be using VTE prophylaxis but sometimes weren’t, and I am not convinced that clinicians always look at prompts. So we came up with a system that incorporates both billing and documentation simultaneously. We put a hard stop on users’ documentation so that they could not sign off on a note or bill for their care until they checked off the kind of VTE prophylaxis they were using. Since hospitalists ultimately care about billing for their work, this system has at least ensured that everybody has considered and documented VTE prophylaxis on a daily basis. There are other hard stops that can be implemented in computer order-entry systems as well, and we are considering ways to roll them out on a broader scale.
However, all of these systems can have problems because patient situations change from day to day. For instance, VTE prophylaxis is not necessarily indicated in a 38-year-old ambulatory patient who comes in with a sickle cell crisis, but you will need to reconsider if the patient ends up in acute chest syndrome in the intensive care unit. I do not yet have a good way to ensure that this is being done on a daily basis with all patients.
Dr. Amin: At the University of California, Irvine, we implemented an electronic alert system, but we locked users in so that they could not complete their admission orders until they answered questions about VTE prevention. This practice increased our VTE prophylaxis rates tremendously. Because we are a level I trauma center, we allow users to bypass the screens one time, but the next time they log in, even to get a simple lab result, they have to answer the questions about VTE prevention.
With any system you develop, you also have to continue with the education process, because clinicians sometimes get into bad habits or simply forget things.
Dr. Spyropolous: At Lovelace Medical Center, we didn’t have the sophistication of an electronic order-entry system, but we had an experienced clinical pharmacist (the director of inpatient pharmacy) who helped to develop and champion VTE prevention guidelines that have then been used throughout the system in close conjunction with our hospitalists’ rounds. This system has been used successfully for the past 7 years.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thrombo-embolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med 1999; 341:793–800.
- Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 2004; 110:874–879.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 2006; 332:325–329.
- Baglin TP, White K, Charles A. Fatal pulmonary embolism in hos-pitalised medical patients. J Clin Pathol 1997; 50:609–610.
- Piazza G, Seddighzadeh A, Goldhaber SZ. Double trouble for 2,609 hospitalized medical patients who developed deep vein thrombosis: prophylaxis omitted more often and pulmonary embolism more frequent. Chest 2007; 132:554–561.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thrombo-embolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med 2007; 167:1476–1486.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost 2000; 83:14–19.
- Lechler E, Schramm W, Flosbach CW. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular-weight heparin (enoxaparin). The Prime Study Group. Haemostasis 1996; 26(Suppl 2):49–56.
- Kleber FX, Witt C, Vogel G, et al; the PRINCE Study Group. Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease. Am Heart J 2003; 145:614–621.
- King CS, Holley AB, Jackson JL, Shorr AF, Moores LK. Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a meta-analysis. Chest 2007; 131:507–516.
- Burleigh E, Wang C, Foster D, et al. Thromboprophylaxis in medically ill patients at risk for venous thromboembolism. Am J Health Syst Pharm 2006; 63(20 Suppl 6):S23–S29.
- Leykum L, Pugh J, Diuguid D, Papadopoulos K. Cost utility of substituting enoxaparin for unfractionated heparin for prophylaxis of venous thrombosis in the hospitalized medical patient. J Hosp Med 2006; 1:168–176.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med 2007; 167:1471–1475.
- Hull RD, Schellong SM Tapson VF, et al. Extended-duration venous thromboembolism (VTE) prophylaxis in acutely ill medical patients with recent reduced mobility: the EXCLAIM study. Presentation at: International Society on Thrombosis and Haemo-stasis XXIst Congress; July 6–12, 2007; Geneva, Switzerland.
- Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008; 371:387–394.
- Kahn SR, Panju A, Geerts W, et al; CURVE study investigators. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 2007; 119:145–155.
- Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent thromboembolism among hospitalized patients. N Engl J Med 2005; 352:969–977.
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med 1991; 151:933–938.
- Howell MD, Geraci JM, Knowlton AA. Congestive heart failure and outpatient risk of venous thromboembolism: a retrospective, case-control study. J Clin Epidemiol 2001; 54:810–816.
- Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet 2006; 367:1075–1079.
- Alikhan R, Cohen AT, Combe S, et al. Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Firbinolysis 2003; 14:341–346.
- Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003; 107(23 Suppl 1):I9–I16.
- Greinacher A, Warkentin TE. Recognition, treatment, and prevention of heparin-induced thrombocytopenia: review and update. Thromb Res 2006; 118:165–176.
- Martel N, Lee J, Wells PS. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 2005; 106:2710–2715.
- Sanderink GJ, Guimart CG, Ozoux ML, Jariwala NU, Shukla UA, Boutouyrie BX. Pharmacokinetics and pharmacodynamics of the prophylactic dose of enoxaparin once daily over 4 days in patients with renal impairment. Thromb Res 2002; 105:225–231.
- Douketis J, Cook D, Zytaruk N, et al. Dalteparin thromboprophylaxis in critically ill patients with severe renal insufficiency: the DIRECT study [abstract]. J Thromb Haemost 2007; 5(Suppl 2): P-S-680.
- Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 2002; 12:19–24.
- Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thrombo-embolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med 1999; 341:793–800.
- Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 2004; 110:874–879.
- Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 2006; 332:325–329.
- Baglin TP, White K, Charles A. Fatal pulmonary embolism in hos-pitalised medical patients. J Clin Pathol 1997; 50:609–610.
- Piazza G, Seddighzadeh A, Goldhaber SZ. Double trouble for 2,609 hospitalized medical patients who developed deep vein thrombosis: prophylaxis omitted more often and pulmonary embolism more frequent. Chest 2007; 132:554–561.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thrombo-embolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cardiovascular Disease Educational and Research Trust; Cyprus Cardiovascular Disease Educational and Research Trust; European Venous Forum; International Surgical Thrombosis Forum; International Union of Angiology; Union Internationale de Phlébologie. Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence). Int Angiol 2006; 25:101–161.
- Wein L, Wein S, Haas SJ, Shaw J, Krum H. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med 2007; 167:1476–1486.
- Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost 2000; 83:14–19.
- Lechler E, Schramm W, Flosbach CW. The venous thrombotic risk in non-surgical patients: epidemiological data and efficacy/safety profile of a low-molecular-weight heparin (enoxaparin). The Prime Study Group. Haemostasis 1996; 26(Suppl 2):49–56.
- Kleber FX, Witt C, Vogel G, et al; the PRINCE Study Group. Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease. Am Heart J 2003; 145:614–621.
- King CS, Holley AB, Jackson JL, Shorr AF, Moores LK. Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a meta-analysis. Chest 2007; 131:507–516.
- Burleigh E, Wang C, Foster D, et al. Thromboprophylaxis in medically ill patients at risk for venous thromboembolism. Am J Health Syst Pharm 2006; 63(20 Suppl 6):S23–S29.
- Leykum L, Pugh J, Diuguid D, Papadopoulos K. Cost utility of substituting enoxaparin for unfractionated heparin for prophylaxis of venous thrombosis in the hospitalized medical patient. J Hosp Med 2006; 1:168–176.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med 2007; 167:1471–1475.
- Hull RD, Schellong SM Tapson VF, et al. Extended-duration venous thromboembolism (VTE) prophylaxis in acutely ill medical patients with recent reduced mobility: the EXCLAIM study. Presentation at: International Society on Thrombosis and Haemo-stasis XXIst Congress; July 6–12, 2007; Geneva, Switzerland.
- Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008; 371:387–394.
- Kahn SR, Panju A, Geerts W, et al; CURVE study investigators. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res 2007; 119:145–155.
- Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent thromboembolism among hospitalized patients. N Engl J Med 2005; 352:969–977.
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med 1991; 151:933–938.
- Howell MD, Geraci JM, Knowlton AA. Congestive heart failure and outpatient risk of venous thromboembolism: a retrospective, case-control study. J Clin Epidemiol 2001; 54:810–816.
- Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet 2006; 367:1075–1079.
- Alikhan R, Cohen AT, Combe S, et al. Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Firbinolysis 2003; 14:341–346.
- Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003; 107(23 Suppl 1):I9–I16.
- Greinacher A, Warkentin TE. Recognition, treatment, and prevention of heparin-induced thrombocytopenia: review and update. Thromb Res 2006; 118:165–176.
- Martel N, Lee J, Wells PS. Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 2005; 106:2710–2715.
- Sanderink GJ, Guimart CG, Ozoux ML, Jariwala NU, Shukla UA, Boutouyrie BX. Pharmacokinetics and pharmacodynamics of the prophylactic dose of enoxaparin once daily over 4 days in patients with renal impairment. Thromb Res 2002; 105:225–231.
- Douketis J, Cook D, Zytaruk N, et al. Dalteparin thromboprophylaxis in critically ill patients with severe renal insufficiency: the DIRECT study [abstract]. J Thromb Haemost 2007; 5(Suppl 2): P-S-680.
- Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg 2002; 12:19–24.
Prevention of venous thromboembolism in the cancer surgery patient
Venous thromboembolism (VTE) is a major complication of cancer, occurring in 4% to 20% of patients,1 and is one of the leading causes of death in cancer patients, although these figures are believed to be underestimates, given the low autopsy rates among cancer patients.2 In hospitalized cancer patients specifically, VTE is the second leading cause of death.3,4 The risk of VTE in cancer patients undergoing surgery is three to five times greater than that in surgical patients without cancer.4 Moreover, cancer patients with symptomatic deep vein thrombosis (DVT) exhibit a high risk of recurrent VTE that may persist for many years after the index event.5
VTE PREVENTION POSES PARTICULAR CHALLENGES IN CANCER PATIENTS
Until recently, data on VTE prevention specific to cancer patients have been sparse. Cancer patients have represented only a small subset (< 20%) of participants in most of the largest clinical trials of VTE prophylaxis. Until the past 2 or 3 years, clinicians largely have had to extrapolate their approach to VTE prophylaxis in cancer patients from data in patients without cancer, bearing in mind that cancer patients are among the populations at highest risk of developing VTE.
High rates of VTE, even with prophylaxis
Further insights have come from the @RISTOS project, a Web-based prospective registry of patients undergoing general, urologic, or gynecologic surgery for cancer at multiple centers in Italy.8 Of the 2,372 patients tracked in this study, 82% received in-hospital VTE prophylaxis and 31% received prophylaxis following discharge. Despite this relatively high frequency of prophylaxis, however, the incidence of clinically overt VTE was 2.1% and the incidence of fatal VTE was 0.8%. Notably, most VTE events occurred after hospital discharge, and VTE was the most common cause of 30-day postoperative death in this registry.
RISK FACTORS: CANCER TYPE AND TREATMENT LOOM LARGE
Both the type and stage of a patient’s cancer are important in assessing the risk of VTE. For men, cancers of the prostate, colon, brain, and lung have been associated with an increased risk of VTE. Among women, cancers of the breast, ovary, and lung have been especially implicated as risk factors for VTE.9,10
The type of cancer therapy also influences VTE risk:
- Surgery. Among patients who undergo cancer-related surgery, the rate of proximal DVT is 10% to 20%, the rate of clinically evident PE is 4% to 10%, and the incidence of fatal PE is 0.2% to 5%.8,11
- Systemic treatments, including chemotherapy and hormone therapy, are also associated with an increased risk of VTE.12–15
- Central venous catheters. Approximately 4% of cancer patients who have central venous catheters placed develop clinically relevant VTE.16,17
In addition to the above risks related to cancer treatments, the following have been identified as risk factors for VTE in surgical oncology patients:
- Age greater than 40 years (risk also increases steeply after age 60 and again after age 75)
- Cancer procoagulants
- Thrombophilia
- Length and complications of cancer surgery (ie, often involving tissue trauma and immobilization)
- Debilitation and slow recovery.
Another risk factor worth noting is perioperative transfusion, as illustrated in a recent study of 14,104 adults undergoing colorectal cancer resection.18 The overall incidence of VTE in these patients was 1.0%, and the risk of death was nearly four times as great in patients who developed VTE as in those who did not. Notably, the need for transfusion was a marker of increased risk of VTE, particularly in women: women who received perioperative transfusions had almost double the risk of developing VTE compared with women who did not receive transfusions (P = .004).
CLINICAL TRIALS OF PROPHYLAXIS IN CANCER SURGERY PATIENTS
LMWH vs UFH for in-hospital prophylaxis
Two large randomized, double-blind trials have compared low-molecular-weight heparin (LMWH) with low-dose unfractionated heparin (UFH) for VTE prophylaxis in surgical patients with cancer—the Enoxaparin and Cancer (ENOXACAN) study19 and the Canadian Colorectal Surgery DVT Prophylaxis Trial.20 Patients in these studies underwent surgery for abdominal or pelvic cancer (mostly colorectal cancer). Both studies compared 40 mg of the LMWH enoxaparin given once daily with 5,000 U of UFH given three times daily for 7 to 10 days postoperatively. Outcome measures were the presence of DVT determined by venography on day 7 to 10 and the incidence of symptomatic VTE. Rates of VTE were statistically equivalent between the two treatment arms in both ENOXACAN (14.7% with LMWH vs 18.2% with UFH) and the Canadian Colorectal Surgery study (9.4% with both therapies), as were rates of major bleeding (4.1% with LMWH vs 2.9% with UFH in ENOXACAN; 2.7% with LMWH vs 1.5% with UFH in the Canadian study).
These findings are consistent with a 2001 meta-analysis by Mismetti et al of all available randomized trials comparing LMWH with placebo or with UFH for VTE prophylaxis in general surgery.21 This analysis found no differences in rates of asymptomatic DVT, clinical PE, clinical thromboembolism, death, major hemorrhage, total hemorrhage, wound hematoma, or need for transfusion between LMWH and UFH in patients undergoing either cancer-related surgery or surgery not related to cancer.
Fondaparinux for in-hospital prophylaxis
Subgroup analysis of the large randomized trial known as PEGASUS22 sheds some light on the efficacy of the factor Xa inhibitor fondaparinux relative to LMWH for thromboprophylaxis in cancer surgery patients. PEGASUS compared fondaparinux 2.5 mg once daily with the LMWH dalteparin 5,000 IU once daily for 5 to 9 days in patients undergoing high-risk abdominal surgery. Among the study’s 1,408 patients undergoing surgery for cancer, rates of VTE were 4.7% in the fondaparinux group compared with 7.7% in the LMWH group, a relative risk reduction of 38.6% with fondaparinux (95% CI, 6.7% to 59.6%). In contrast, in the rest of the PEGASUS population (patients undergoing abdominal surgery for reasons other than cancer), LMWH was nonsignificantly more efficacious at preventing VTE than was fondaparinux. Rates of major bleeding in this cancer subgroup were comparable between the two treatments.
Extended prophylaxis
Two additional randomized trials have evaluated extended prophylaxis with LMWH in surgical cancer patients—ENOXACAN II23 and the Fragmin After Major Abdominal Surgery (FAME) study.24
In ENOXACAN II, patients undergoing surgery for abdominal or pelvic cancer first received 6 to 10 days of prophylaxis with enoxaparin 40 mg once daily and then were randomized in a double-blind fashion to an additional 21 days of enoxaparin or placebo.23 Among 332 patients in the intent-to-treat analysis, the rate of VTE at the end of the double-blind phase was reduced from 12.0% with placebo to 4.8% with extended-duration enoxaparin (P = .02), an effect that was maintained at 3-month follow-up (P = .01). There was no significant difference between the two groups in rates of major bleeding events or any bleeding events.
In FAME, patients received 5,000 IU of dalteparin once daily for 1 week following major abdominal surgery and then were randomized in open-label fashion to either placebo or extended prophylaxis with dalteparin for 3 more weeks; a subanalysis examined outcomes in the 198 FAME participants whose abdominal surgery was for cancer.24 Among these 198 cancer surgery patients, the rate of venography-documented VTE at 4 weeks was reduced from 19.6% with placebo to 8.8% with extended-duration dalteparin, a relative reduction of 55% (P = .03). The rate of proximal DVT was reduced from 10.4% to 2.2% with extended prophylaxis, a relative reduction of 79% (P = .02).
The number needed to treat with extended LMWH prophylaxis to prevent one VTE event was 14 in ENOXACAN II23 and 9 in the FAME subanalysis of cancer surgery patients.24
New systematic review of relevant trials
Leonardi et al recently published a systematic review of 26 randomized controlled trials of DVT prophylaxis in 7,639 cancer surgery patients.25 They found the overall incidence of DVT to be 12.7% in those who received pharmacologic prophylaxis compared with 35.2% in controls. They also found high-dose LMWH therapy (> 3,400 U daily) to be associated with a significantly lower incidence of DVT than low-dose LMWH therapy (≤ 3,400 U daily) (7.9% vs 14.5%, respectively; P < .01). No differences were demonstrated between LMWH and UFH in preventing DVT, DVT location, or bleeding. Bleeding complications requiring discontinuation of pharmacologic prophylaxis occurred in 3% of patients overall.
Implications of HIT
The sequelae of heparin-induced thrombocytopenia (HIT) can have major consequences for cancer surgery patients. The incidence of HIT is markedly lower with LMWH than with UFH, as demonstrated in a nested case-control study by Creekmore et al.26 These researchers also found that the average cost of an admission during which HIT developed was nearly four times as great as the average cost of an admission during which UFH or LMWH was given without development of HIT ($56,364 vs $15,231; P < .001).
EVIDENCE IN SPECIFIC ONCOLOGIC POPULATIONS
Most of the patients in the trials reviewed above underwent abdominal surgery for malignancy. Although studies of VTE prophylaxis in patients undergoing nonabdominal cancer surgery are relatively few, some data are available for a few other specific oncologic populations, as reviewed below.
Surgery for gynecologic cancer
There is a paucity of randomized controlled trials or prospective observational studies on VTE and its prevention in the gynecologic cancer surgery population. Based on small historical studies, the postoperative risk of VTE in this population varies from 12% to 35%.27,28 Twice-daily administration of UFH 5,000 U appears to be ineffective as VTE prophylaxis in this population, but increasing the frequency to three times daily reduces VTE risk by 50% to 60% compared with placebo. Once-daily LMWH is comparable to three-times-daily UFH in efficacy and safety in this population.
A systematic Cochrane review of eight randomized controlled trials in patients undergoing major gynecologic surgery revealed that heparin prophylaxis (either UFH or LMWH) reduces the risk of DVT by 70% compared with no prophylaxis, with an identical risk reduction specifically among women with malignancy (odds ratio, 0.30; 95% CI, 0.10 to 0.89).29 This review found no evidence that anticoagulation reduces the risk of PE following major gynecologic surgery. LMWH and UFH were similar in efficacy for preventing DVT and had a comparable risk of bleeding complications.
Surgery for urologic cancer
The risk of VTE and the benefits of thromboprophylaxis also are poorly studied in patients undergoing surgery for urologic cancer.
The risk of VTE varies with the type of urologic surgery and the method used to diagnose VTE. For instance, patients undergoing radical retropubic prostatectomy have been reported to develop DVT at rates of 1% to 3%, PE at rates of 1% to 3%, and fatal PE at a rate of 0.6%, whereas the incidences of these events are somewhat higher in patients undergoing cystectomy: 8% for DVT, 2% to 4% for PE, and 2% for fatal PE. Radiologic diagnosis of thromboembolism in pelvic surgery patients has yielded higher incidences, with DVT rates of 21% to 51% and PE rates of 11% to 22%.30
Small studies suggest that prophylaxis with either low-dose UFH or LMWH is both effective in reducing VTE risk and safe in urologic cancer surgery patients, although pharmacologic prophylaxis poses a possible increased risk of pelvic hematoma and lymphocele formation in this population.30
Neurosurgery
Most neurosurgical procedures are performed for malignancies. The risk of venography-confirmed VTE in patients undergoing neurosurgery is approximately 30% to 40%.31,32 Likewise, the risks of intracranial or intraspinal hemorrhage in these patients are high. For this reason, mechanical methods of VTE prophylaxis are preferred in these patients. The use of anticoagulant prophylaxis remains controversial in this setting, although more recent data suggest that it might be safer than previously recognized.
GUIDELINES FOR VTE PROPHYLAXIS IN THE CANCER SURGERY PATIENT
American College of Chest Physicians
National Comprehensive Cancer Network
The National Comprehensive Cancer Network (NCCN) recently published clinical practice guidelines on venous thromboembolic disease in cancer patients.35 The defined at-risk population for these guidelines is the adult cancer inpatient with a diagnosis of (or clinical suspicion for) cancer. The guidelines recommend prophylactic anticoagulation (category 1 recommendation) with or without a sequential compression device as initial prophylaxis, unless the patient has a relative contraindication to anticoagulation, in which case mechanical prophylaxis (sequential compression device or graduated compression stockings) is recommended. (A category 1 recommendation indicates “uniform NCCN consensus, based on high-level evidence.”)
The NCCN guidelines include a specific recommended risk-factor assessment, which includes noting the patient’s age (VTE risk increases beginning at age 40 and then steeply again at age 75), any prior VTE, the presence of familial thrombophilia or active cancer, the use of medications associated with increased VTE risk (chemotherapy, exogenous estrogen compounds, and thalidomide or lenalidomide), and a number of other risk factors for VTE as outlined in the prior two articles in this supplement. The NCCN guidelines explicitly call for assessment of modifiable risk factors for VTE (ie, smoking or other tobacco use, obesity, and a low level of activity or lack of exercise) and call for active patient education on these factors.
American Society of Clinical Oncology
Our recommended algorithm
LINGERING CHALLENGE OF UNDERUTILIZATION
Despite this consensus on ways to reduce thromboembolic risk in this population and the clear evidence of the benefit of VTE prophylaxis in patients with cancer, data from several registries confirm a persistently low utilization of prophylaxis in patients with cancer.36–38 The global Fundamental Research in Oncology and Thrombosis (FRONTLINE) study surveyed 3,891 clinicians who treat cancer patients regarding their practices with respect to VTE in those patients.36 The survey found that only 52% of respondents routinely used thromboprophylaxis for their surgical patients with cancer. More striking, however, was the finding that most respondents routinely considered thrombo-prophylaxis in only 5% of their medical oncology patients. These data are echoed by findings of other retrospective medical record reviews in patients undergoing major abdominal or abdominothoracic surgery (in many cases for cancer), with VTE prophylaxis rates ranging from 38% to 75%.37,38
SUMMARY
Patients undergoing surgery for cancer have an increased risk of VTE and fatal PE, even when thromboprophylaxis is used. Nevertheless, prophylaxis with either LMWH or UFH does reduce venographic VTE event rates in these patients. If UFH is chosen for prophylaxis, a three-times-daily regimen should be used in this population. In specific surgical cancer populations, especially those undergoing abdominal surgery, out-of-hospital prophylaxis with once-daily LMWH is warranted. Current registries reveal that compliance with established guidelines for VTE prophylaxis in this population is low.


Dr. Jaffer: Dr. Amin, based on your study on thrombo-prophylaxis rates in US medical centers, will you comment on rates of prophylaxis for cancer surgery patients?
Dr. Amin: The overall study included approximately 200,000 medical patients and about 80,000 surgical patients enrolled over more than a 3-year period between 2002 and 2005.39,40 Our goal was to assess rates of prophylaxis and, when it was provided, whether it was appropriate (in terms of type, dosage, and duration) based on the ACCP guidelines. A subanalysis assessed medical cancer patients and surgical cancer patients separately. Medical cancer patients received thromboprophylaxis 56% of the time but received appropriate prophylaxis only 28% of the time. Among surgical cancer patients, appropriate prophylaxis was given only about 24% of the time for those undergoing gynecologic surgery and about 12% of the time for those undergoing neurosurgery. These percentages are consistent with data from other national registries, such as the IMPROVE registry, which documented prophylaxis rates on the order of 45% in medical patients with cancer.41 We also analyzed the data according to individual practitioners and found that medical oncologists use prophylaxis about 25% of the time, which is relatively consistent with other providers, such as internists and surgeons.
So there is a huge opportunity to improve rates of prophylaxis for this group of patients that national guidelines say are at high risk. Why is prophylaxis so underutilized in the cancer population? One factor may be a misperception about the risk of bleeding with anticoagulants. Yet several studies have shown that the rate of bleeding from prophylaxis is extremely low, whether LMWH or UFH is used, so more awareness of actual bleeding risk is needed. Another factor is the obvious focus among internists and oncologists on treating the patient, with perhaps a reduced consideration of prophylaxis and prevention. A third factor may be a concern about thrombocytopenia. However, in our study of prophylaxis rates in US medical centers, we excluded patients who had thrombocytopenia, yet rates of prophylaxis were still low. Nothing in the literature indicates that anticoagulants cannot be used in patients with platelet counts of 50,000 to 150,000 cells/µL or higher, so this suggests that we need to do more education.
Dr. Jaffer: Dr. Brotman, can you tell us more about how clinicians in practice should use prophylaxis in their neurosurgery patients, such as those undergoing craniotomy or spine surgery for cancer? What is the safest and most efficacious way to prevent DVT in these patients?
Dr. Brotman: First, it’s important to recognize that some sort of prophylaxis needs to be used. Neurosurgery patients are at an extremely high risk for thromboembolic events, and such events are often fatal in these patients. Having said that, the jury is still out on whether the prophylaxis in these patients should be compression devices or anticoagulation. This gives physicians some latitude in their decisions. They can decide not to use pharmacologic prophylaxis so long as they use pneumatic compression devices consistently, perhaps even starting during the operation and certainly throughout hospitalization when the patient is immobilized.
Certainly, the concerns about using full-dose anticoagulation in the immediate postoperative setting in neurosurgery patients are valid. Yet these patients are at very high risk for thromboembolic events, and if we take too cautious an approach to prophylaxis in the immediate perioperative setting, more patients are going to have thromboembolic events, at which point management decisions become much more difficult. The risk of intracranial bleeding with anticoagulation to treat a patient who develops a DVT at postoperative day 10 will certainly be higher than it would have been with lower-dose perioperative prophylactic anticoagulation. Plus, if you put in a filter at that point, the outcomes tend to be poor. Therefore, I believe there is some degree of risk that we should be willing to take with regard to perioperative bleeding, even in neurosurgery patients.
Dr. McKean: I’d like to make a point about combination prophylaxis. At many institutions, compression stockings and sequential compression devices are used preoperatively and intraoperatively, and then pharmacologic prophylaxis—for example, twice-daily UFH—is used postoperatively. There is concern that these patients are hypercoagulable, and most clinicians believe that mechanical prophylaxis alone, even with sequential compression devices plus compression stockings, is not aggressive enough in these high-risk patients.
Dr. Jaffer: Dr. Spyropoulos, what is the optimal duration of pharmacologic prophylaxis for cancer surgery patients?
Dr. Spyropoulos: First let’s consider in-hospital prophylaxis. The supportive data for in-hospital prophylaxis are strong, and the duration of therapy used in the major in-hospital prophylaxis trials was 7 to 10 days. With regard to extended prophylaxis, we have at least two moderately sized randomized controlled trials, ENOXACAN II23 and the substudy of FAME,24 that demonstrated that extending prophylaxis with LMWH at doses of 3,400 U once daily (5,000 IU of dalteparin; 40 mg of enoxaparin) reduces VTE risk at postoperative day 30. Also, recent data from the @RISTOS registry show that in cancer surgery patients, especially those having abdominal or pelvic procedures, the leading cause of 30-day mortality was VTE.8 This registry also shows that despite prophylaxis, the rate of symptomatic VTE can be as high as 2%, with the rate of fatal VTE approaching 1%. Thus, in cancer patients undergoing abdominal or pelvic surgery, physicians should strongly consider prophylaxis of up to 30 days’ duration.
Dr. Jaffer: One striking finding from the @RISTOS registry was that 40% of VTE events in these cancer surgery patients occurred after postoperative day 21. This really underscores the need to consider prophylaxis for at least 4 weeks in these patients in real-world practice.
Dr. Brotman: The other striking finding from that registry was that the in-hospital prophylaxis rate was quite high, about 80%, and the rate of extended prophylaxis approached 35%. These are rates that are rarely achieved in clinical practice. Yet despite these high levels of prophylaxis, patients in this registry still had a high incidence of morbidity and mortality from VTE. This suggests that we need to improve our out-of-hospital VTE prevention paradigms.
Dr. Jaffer: Dr. Deitelzweig, oncologists and internists are often unsure about whether their ambulatory cancer patients who are receiving chemotherapy should be on any form of prophylaxis. What is your opinion?
Dr. Deitelzweig: That question comes up regularly because these patients are encountered across many medical specialties. At this point, all of the large organizations, including ASCO and NCCN, are advocating that prophylaxis is not indicated for such patients.
- Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007; 25:5490–5505.
- Khorana AA, Francis CW, Culakova E, et al. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost 2007; 5:632–634.
- Ambrus JL, Ambrus CM, Mink IB, Pickren JW. Causes of death in cancer patients. J Med 1975; 6:61–64.
- Donati MB. Cancer and thrombosis. Haemostasis 1994; 24:128–131.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 1996; 125:1–7.
- Haas S, Wolf H, Kakkar AK, Fareed J, Encke A. Prevention of fatal pulmonary embolism and mortality in surgical patients: a randomized double-blind comparison of LMWH with unfractionated heparin. Thromb Haemost 2005; 94:814–819.
- Kakkar AK, Haas S, Wolf H, Encke A. Evaluation of perioperative fatal pulmonary embolism and death in cancer surgical patients: the MC-4 cancer substudy. Thromb Haemost 2005; 94:867–871.
- Agnelli G, Bolis G, Capussotti L, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 2006; 243:89–95.
- Levitan N, Dowlati A, Remick SC, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy: risk analysis using Medicare claims data. Medicine (Baltimore) 1999; 78:285–291.
- Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med 1996; 334:677–681.
- Bergqvist D. Risk of venous thromboembolism in patients undergoing cancer surgery and options for thromboprophylaxis. J Surg Oncol 2007; 95:167–174.
- Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 2000; 160:809–815.
- Sallah S, Wan JY, Nguyen NP. Venous thrombosis in patients with solid tumors: determination of frequency and characteristics. Thromb Haemost 2002; 87:575–579.
- Kröger K, Weiland D, Ose C, et al. Risk factors for venous thromboembolic events in cancer patients. Ann Oncol 2006; 17:297–303.
- Blom JW, Vanderschoot JP, Oostindiër MJ, et al. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: results of a record linkage study. J Thromb Haemost 2006; 4:529–535.
- Couban S, Simpson DR, Barnett MJ, et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 2002; 100:1525–1531.
- Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002; 20:3276–3281.
- Nilsson KR, Berenholtz SM, Garrett-Mayer E, et al. Association between venous thromboembolism and perioperative allogeneic transfusion. Arch Surg 2007; 142:126–133.
- Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. ENOXACAN Study Group. Br J Surg 1997; 84:1099–1103.
- McLeod RS, Geerts WH, Sniderman KW, et al. Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian Colorectal DVT Prophylaxis Trial: a randomized, double-blind trial. Ann Surg 2001; 233:438–444.
- Mismetti P, Laporte S, Darmon JY, Buchmüller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg 2001; 88:913–930.
- Agnelli G, Bergqvist D, Cohen AT, et al, on behalf of the PEGASUS investigators. Randomized clinical trial of postoperative fondaparinux versus perioperative dalteparin for prevention of venous thromboembolism in high-risk abdominal surgery. Br J Surg 2005; 92:1212–1220.
- Bergqvist D, Agnelli G, Cohen AT, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 2002; 346:975–980.
- Rasmussen MS, Wille-Jorgensen P, Jorgensen LN, et al. Prolonged thromboprophylaxis with low molecular weight heparin (dalteparin) following major abdominal surgery for malignancy [abstract 186]. Blood 2003; 102:56a.
- Leonardi MJ, McGory ML, Ko CY. A systematic review of deep venous thrombosis prophylaxis in cancer patients: implications for improving quality. Ann Surg Oncol 2007; 14:929–936.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Walsh JJ, Bonnar J, Wright FW. A study of pulmonary embolism and deep leg vein thrombosis after major gynaecological surgery using labeled fibrinogen-phlebography and lung scanning. J Obstet Gynaecol Br Commonw 1974; 81:311–316.
- Clarke-Pearson DL, Synan IS, Coleman RE, et al. The natural history of postoperative venous thromboemboli in gynecologic oncology: a prospective study of 382 patients. Am J Obstet Gynecol 1984; 148:1051–1054.
- Oates-Whitehead RM, D’Angelo A, Mol B. Anticoagulant and aspirin prophylaxis for preventing thromboembolism after major gynaecological surgery. Cochrane Database Syst Rev 2003; (4):CD003679.
- Kibel AS, Loughlin KR. Pathogenesis and prophylaxis of postoperative thromboembolic disease in urological pelvic surgery. J Urol 1995; 153:1763–1774.
- Agnelli G, Piovella F, Buoncristiani P, et al. Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 1998; 339:80–85.
- Semrad TJ, O’Donnell R, Wun T, et al. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 2007; 106:601–608.
- Iorio A, Agnelli G. Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Intern Med 2000; 160:2327–2332.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Venous thromboembolic disease. V.1.2007. http://www.nccn.org/professionals/physician_gls/PDF/vte.pdf. Accessed December 5, 2007.
- Kakkar AK, Levine M, Pinedo HM, Wolff R, Wong J. Venous thrombosis in cancer patients: insights from the FRONTLINE survey. Oncologist 2003; 8:381–388.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- Bratzler DW, Raskob GE, Murray CK, Bumpus LJ, Piatt DS. Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting. Arch Intern Med 1998; 158:1909–1912.
- Amin A, Stemkowski S, Lin J, et al. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis in US hospitals: adherence to the 6th American College of Chest Physicians’ recommendations for at-risk medical and surgical patients. Abstract presented at: 41st Midyear Clinical Meeting of the American Society of Health-System Pharmacists; December 3–7, 2006; Anaheim, CA.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Clarke-Pearson DL, Synan IS, Dodge R, et al. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol 1993; 168:1146–1154.
- Einstein MH, Pritts EA, Hartenbach EM. Venous thromboembolism prevention in gynecologic cancer surgery: a systematic review. Gynecol Oncol 2007; 105:813–819.
- Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol 1984; 63:92–98.
- Ruff RL, Posner JB. Incidence and treatment of peripheral venous thrombosis in patients with glioma. Ann Neurol 1983; 13:334–336.
- Levin JM, Schiff D, Loeffler JS, Fine HA, Black PM, Wen PY. Complications of therapy for venous thromboembolic disease in patients with brain tumors. Neurology 1993; 43:1111–1114.
Venous thromboembolism (VTE) is a major complication of cancer, occurring in 4% to 20% of patients,1 and is one of the leading causes of death in cancer patients, although these figures are believed to be underestimates, given the low autopsy rates among cancer patients.2 In hospitalized cancer patients specifically, VTE is the second leading cause of death.3,4 The risk of VTE in cancer patients undergoing surgery is three to five times greater than that in surgical patients without cancer.4 Moreover, cancer patients with symptomatic deep vein thrombosis (DVT) exhibit a high risk of recurrent VTE that may persist for many years after the index event.5
VTE PREVENTION POSES PARTICULAR CHALLENGES IN CANCER PATIENTS
Until recently, data on VTE prevention specific to cancer patients have been sparse. Cancer patients have represented only a small subset (< 20%) of participants in most of the largest clinical trials of VTE prophylaxis. Until the past 2 or 3 years, clinicians largely have had to extrapolate their approach to VTE prophylaxis in cancer patients from data in patients without cancer, bearing in mind that cancer patients are among the populations at highest risk of developing VTE.
High rates of VTE, even with prophylaxis
Further insights have come from the @RISTOS project, a Web-based prospective registry of patients undergoing general, urologic, or gynecologic surgery for cancer at multiple centers in Italy.8 Of the 2,372 patients tracked in this study, 82% received in-hospital VTE prophylaxis and 31% received prophylaxis following discharge. Despite this relatively high frequency of prophylaxis, however, the incidence of clinically overt VTE was 2.1% and the incidence of fatal VTE was 0.8%. Notably, most VTE events occurred after hospital discharge, and VTE was the most common cause of 30-day postoperative death in this registry.
RISK FACTORS: CANCER TYPE AND TREATMENT LOOM LARGE
Both the type and stage of a patient’s cancer are important in assessing the risk of VTE. For men, cancers of the prostate, colon, brain, and lung have been associated with an increased risk of VTE. Among women, cancers of the breast, ovary, and lung have been especially implicated as risk factors for VTE.9,10
The type of cancer therapy also influences VTE risk:
- Surgery. Among patients who undergo cancer-related surgery, the rate of proximal DVT is 10% to 20%, the rate of clinically evident PE is 4% to 10%, and the incidence of fatal PE is 0.2% to 5%.8,11
- Systemic treatments, including chemotherapy and hormone therapy, are also associated with an increased risk of VTE.12–15
- Central venous catheters. Approximately 4% of cancer patients who have central venous catheters placed develop clinically relevant VTE.16,17
In addition to the above risks related to cancer treatments, the following have been identified as risk factors for VTE in surgical oncology patients:
- Age greater than 40 years (risk also increases steeply after age 60 and again after age 75)
- Cancer procoagulants
- Thrombophilia
- Length and complications of cancer surgery (ie, often involving tissue trauma and immobilization)
- Debilitation and slow recovery.
Another risk factor worth noting is perioperative transfusion, as illustrated in a recent study of 14,104 adults undergoing colorectal cancer resection.18 The overall incidence of VTE in these patients was 1.0%, and the risk of death was nearly four times as great in patients who developed VTE as in those who did not. Notably, the need for transfusion was a marker of increased risk of VTE, particularly in women: women who received perioperative transfusions had almost double the risk of developing VTE compared with women who did not receive transfusions (P = .004).
CLINICAL TRIALS OF PROPHYLAXIS IN CANCER SURGERY PATIENTS
LMWH vs UFH for in-hospital prophylaxis
Two large randomized, double-blind trials have compared low-molecular-weight heparin (LMWH) with low-dose unfractionated heparin (UFH) for VTE prophylaxis in surgical patients with cancer—the Enoxaparin and Cancer (ENOXACAN) study19 and the Canadian Colorectal Surgery DVT Prophylaxis Trial.20 Patients in these studies underwent surgery for abdominal or pelvic cancer (mostly colorectal cancer). Both studies compared 40 mg of the LMWH enoxaparin given once daily with 5,000 U of UFH given three times daily for 7 to 10 days postoperatively. Outcome measures were the presence of DVT determined by venography on day 7 to 10 and the incidence of symptomatic VTE. Rates of VTE were statistically equivalent between the two treatment arms in both ENOXACAN (14.7% with LMWH vs 18.2% with UFH) and the Canadian Colorectal Surgery study (9.4% with both therapies), as were rates of major bleeding (4.1% with LMWH vs 2.9% with UFH in ENOXACAN; 2.7% with LMWH vs 1.5% with UFH in the Canadian study).
These findings are consistent with a 2001 meta-analysis by Mismetti et al of all available randomized trials comparing LMWH with placebo or with UFH for VTE prophylaxis in general surgery.21 This analysis found no differences in rates of asymptomatic DVT, clinical PE, clinical thromboembolism, death, major hemorrhage, total hemorrhage, wound hematoma, or need for transfusion between LMWH and UFH in patients undergoing either cancer-related surgery or surgery not related to cancer.
Fondaparinux for in-hospital prophylaxis
Subgroup analysis of the large randomized trial known as PEGASUS22 sheds some light on the efficacy of the factor Xa inhibitor fondaparinux relative to LMWH for thromboprophylaxis in cancer surgery patients. PEGASUS compared fondaparinux 2.5 mg once daily with the LMWH dalteparin 5,000 IU once daily for 5 to 9 days in patients undergoing high-risk abdominal surgery. Among the study’s 1,408 patients undergoing surgery for cancer, rates of VTE were 4.7% in the fondaparinux group compared with 7.7% in the LMWH group, a relative risk reduction of 38.6% with fondaparinux (95% CI, 6.7% to 59.6%). In contrast, in the rest of the PEGASUS population (patients undergoing abdominal surgery for reasons other than cancer), LMWH was nonsignificantly more efficacious at preventing VTE than was fondaparinux. Rates of major bleeding in this cancer subgroup were comparable between the two treatments.
Extended prophylaxis
Two additional randomized trials have evaluated extended prophylaxis with LMWH in surgical cancer patients—ENOXACAN II23 and the Fragmin After Major Abdominal Surgery (FAME) study.24
In ENOXACAN II, patients undergoing surgery for abdominal or pelvic cancer first received 6 to 10 days of prophylaxis with enoxaparin 40 mg once daily and then were randomized in a double-blind fashion to an additional 21 days of enoxaparin or placebo.23 Among 332 patients in the intent-to-treat analysis, the rate of VTE at the end of the double-blind phase was reduced from 12.0% with placebo to 4.8% with extended-duration enoxaparin (P = .02), an effect that was maintained at 3-month follow-up (P = .01). There was no significant difference between the two groups in rates of major bleeding events or any bleeding events.
In FAME, patients received 5,000 IU of dalteparin once daily for 1 week following major abdominal surgery and then were randomized in open-label fashion to either placebo or extended prophylaxis with dalteparin for 3 more weeks; a subanalysis examined outcomes in the 198 FAME participants whose abdominal surgery was for cancer.24 Among these 198 cancer surgery patients, the rate of venography-documented VTE at 4 weeks was reduced from 19.6% with placebo to 8.8% with extended-duration dalteparin, a relative reduction of 55% (P = .03). The rate of proximal DVT was reduced from 10.4% to 2.2% with extended prophylaxis, a relative reduction of 79% (P = .02).
The number needed to treat with extended LMWH prophylaxis to prevent one VTE event was 14 in ENOXACAN II23 and 9 in the FAME subanalysis of cancer surgery patients.24
New systematic review of relevant trials
Leonardi et al recently published a systematic review of 26 randomized controlled trials of DVT prophylaxis in 7,639 cancer surgery patients.25 They found the overall incidence of DVT to be 12.7% in those who received pharmacologic prophylaxis compared with 35.2% in controls. They also found high-dose LMWH therapy (> 3,400 U daily) to be associated with a significantly lower incidence of DVT than low-dose LMWH therapy (≤ 3,400 U daily) (7.9% vs 14.5%, respectively; P < .01). No differences were demonstrated between LMWH and UFH in preventing DVT, DVT location, or bleeding. Bleeding complications requiring discontinuation of pharmacologic prophylaxis occurred in 3% of patients overall.
Implications of HIT
The sequelae of heparin-induced thrombocytopenia (HIT) can have major consequences for cancer surgery patients. The incidence of HIT is markedly lower with LMWH than with UFH, as demonstrated in a nested case-control study by Creekmore et al.26 These researchers also found that the average cost of an admission during which HIT developed was nearly four times as great as the average cost of an admission during which UFH or LMWH was given without development of HIT ($56,364 vs $15,231; P < .001).
EVIDENCE IN SPECIFIC ONCOLOGIC POPULATIONS
Most of the patients in the trials reviewed above underwent abdominal surgery for malignancy. Although studies of VTE prophylaxis in patients undergoing nonabdominal cancer surgery are relatively few, some data are available for a few other specific oncologic populations, as reviewed below.
Surgery for gynecologic cancer
There is a paucity of randomized controlled trials or prospective observational studies on VTE and its prevention in the gynecologic cancer surgery population. Based on small historical studies, the postoperative risk of VTE in this population varies from 12% to 35%.27,28 Twice-daily administration of UFH 5,000 U appears to be ineffective as VTE prophylaxis in this population, but increasing the frequency to three times daily reduces VTE risk by 50% to 60% compared with placebo. Once-daily LMWH is comparable to three-times-daily UFH in efficacy and safety in this population.
A systematic Cochrane review of eight randomized controlled trials in patients undergoing major gynecologic surgery revealed that heparin prophylaxis (either UFH or LMWH) reduces the risk of DVT by 70% compared with no prophylaxis, with an identical risk reduction specifically among women with malignancy (odds ratio, 0.30; 95% CI, 0.10 to 0.89).29 This review found no evidence that anticoagulation reduces the risk of PE following major gynecologic surgery. LMWH and UFH were similar in efficacy for preventing DVT and had a comparable risk of bleeding complications.
Surgery for urologic cancer
The risk of VTE and the benefits of thromboprophylaxis also are poorly studied in patients undergoing surgery for urologic cancer.
The risk of VTE varies with the type of urologic surgery and the method used to diagnose VTE. For instance, patients undergoing radical retropubic prostatectomy have been reported to develop DVT at rates of 1% to 3%, PE at rates of 1% to 3%, and fatal PE at a rate of 0.6%, whereas the incidences of these events are somewhat higher in patients undergoing cystectomy: 8% for DVT, 2% to 4% for PE, and 2% for fatal PE. Radiologic diagnosis of thromboembolism in pelvic surgery patients has yielded higher incidences, with DVT rates of 21% to 51% and PE rates of 11% to 22%.30
Small studies suggest that prophylaxis with either low-dose UFH or LMWH is both effective in reducing VTE risk and safe in urologic cancer surgery patients, although pharmacologic prophylaxis poses a possible increased risk of pelvic hematoma and lymphocele formation in this population.30
Neurosurgery
Most neurosurgical procedures are performed for malignancies. The risk of venography-confirmed VTE in patients undergoing neurosurgery is approximately 30% to 40%.31,32 Likewise, the risks of intracranial or intraspinal hemorrhage in these patients are high. For this reason, mechanical methods of VTE prophylaxis are preferred in these patients. The use of anticoagulant prophylaxis remains controversial in this setting, although more recent data suggest that it might be safer than previously recognized.
GUIDELINES FOR VTE PROPHYLAXIS IN THE CANCER SURGERY PATIENT
American College of Chest Physicians
National Comprehensive Cancer Network
The National Comprehensive Cancer Network (NCCN) recently published clinical practice guidelines on venous thromboembolic disease in cancer patients.35 The defined at-risk population for these guidelines is the adult cancer inpatient with a diagnosis of (or clinical suspicion for) cancer. The guidelines recommend prophylactic anticoagulation (category 1 recommendation) with or without a sequential compression device as initial prophylaxis, unless the patient has a relative contraindication to anticoagulation, in which case mechanical prophylaxis (sequential compression device or graduated compression stockings) is recommended. (A category 1 recommendation indicates “uniform NCCN consensus, based on high-level evidence.”)
The NCCN guidelines include a specific recommended risk-factor assessment, which includes noting the patient’s age (VTE risk increases beginning at age 40 and then steeply again at age 75), any prior VTE, the presence of familial thrombophilia or active cancer, the use of medications associated with increased VTE risk (chemotherapy, exogenous estrogen compounds, and thalidomide or lenalidomide), and a number of other risk factors for VTE as outlined in the prior two articles in this supplement. The NCCN guidelines explicitly call for assessment of modifiable risk factors for VTE (ie, smoking or other tobacco use, obesity, and a low level of activity or lack of exercise) and call for active patient education on these factors.
American Society of Clinical Oncology
Our recommended algorithm
LINGERING CHALLENGE OF UNDERUTILIZATION
Despite this consensus on ways to reduce thromboembolic risk in this population and the clear evidence of the benefit of VTE prophylaxis in patients with cancer, data from several registries confirm a persistently low utilization of prophylaxis in patients with cancer.36–38 The global Fundamental Research in Oncology and Thrombosis (FRONTLINE) study surveyed 3,891 clinicians who treat cancer patients regarding their practices with respect to VTE in those patients.36 The survey found that only 52% of respondents routinely used thromboprophylaxis for their surgical patients with cancer. More striking, however, was the finding that most respondents routinely considered thrombo-prophylaxis in only 5% of their medical oncology patients. These data are echoed by findings of other retrospective medical record reviews in patients undergoing major abdominal or abdominothoracic surgery (in many cases for cancer), with VTE prophylaxis rates ranging from 38% to 75%.37,38
SUMMARY
Patients undergoing surgery for cancer have an increased risk of VTE and fatal PE, even when thromboprophylaxis is used. Nevertheless, prophylaxis with either LMWH or UFH does reduce venographic VTE event rates in these patients. If UFH is chosen for prophylaxis, a three-times-daily regimen should be used in this population. In specific surgical cancer populations, especially those undergoing abdominal surgery, out-of-hospital prophylaxis with once-daily LMWH is warranted. Current registries reveal that compliance with established guidelines for VTE prophylaxis in this population is low.


Dr. Jaffer: Dr. Amin, based on your study on thrombo-prophylaxis rates in US medical centers, will you comment on rates of prophylaxis for cancer surgery patients?
Dr. Amin: The overall study included approximately 200,000 medical patients and about 80,000 surgical patients enrolled over more than a 3-year period between 2002 and 2005.39,40 Our goal was to assess rates of prophylaxis and, when it was provided, whether it was appropriate (in terms of type, dosage, and duration) based on the ACCP guidelines. A subanalysis assessed medical cancer patients and surgical cancer patients separately. Medical cancer patients received thromboprophylaxis 56% of the time but received appropriate prophylaxis only 28% of the time. Among surgical cancer patients, appropriate prophylaxis was given only about 24% of the time for those undergoing gynecologic surgery and about 12% of the time for those undergoing neurosurgery. These percentages are consistent with data from other national registries, such as the IMPROVE registry, which documented prophylaxis rates on the order of 45% in medical patients with cancer.41 We also analyzed the data according to individual practitioners and found that medical oncologists use prophylaxis about 25% of the time, which is relatively consistent with other providers, such as internists and surgeons.
So there is a huge opportunity to improve rates of prophylaxis for this group of patients that national guidelines say are at high risk. Why is prophylaxis so underutilized in the cancer population? One factor may be a misperception about the risk of bleeding with anticoagulants. Yet several studies have shown that the rate of bleeding from prophylaxis is extremely low, whether LMWH or UFH is used, so more awareness of actual bleeding risk is needed. Another factor is the obvious focus among internists and oncologists on treating the patient, with perhaps a reduced consideration of prophylaxis and prevention. A third factor may be a concern about thrombocytopenia. However, in our study of prophylaxis rates in US medical centers, we excluded patients who had thrombocytopenia, yet rates of prophylaxis were still low. Nothing in the literature indicates that anticoagulants cannot be used in patients with platelet counts of 50,000 to 150,000 cells/µL or higher, so this suggests that we need to do more education.
Dr. Jaffer: Dr. Brotman, can you tell us more about how clinicians in practice should use prophylaxis in their neurosurgery patients, such as those undergoing craniotomy or spine surgery for cancer? What is the safest and most efficacious way to prevent DVT in these patients?
Dr. Brotman: First, it’s important to recognize that some sort of prophylaxis needs to be used. Neurosurgery patients are at an extremely high risk for thromboembolic events, and such events are often fatal in these patients. Having said that, the jury is still out on whether the prophylaxis in these patients should be compression devices or anticoagulation. This gives physicians some latitude in their decisions. They can decide not to use pharmacologic prophylaxis so long as they use pneumatic compression devices consistently, perhaps even starting during the operation and certainly throughout hospitalization when the patient is immobilized.
Certainly, the concerns about using full-dose anticoagulation in the immediate postoperative setting in neurosurgery patients are valid. Yet these patients are at very high risk for thromboembolic events, and if we take too cautious an approach to prophylaxis in the immediate perioperative setting, more patients are going to have thromboembolic events, at which point management decisions become much more difficult. The risk of intracranial bleeding with anticoagulation to treat a patient who develops a DVT at postoperative day 10 will certainly be higher than it would have been with lower-dose perioperative prophylactic anticoagulation. Plus, if you put in a filter at that point, the outcomes tend to be poor. Therefore, I believe there is some degree of risk that we should be willing to take with regard to perioperative bleeding, even in neurosurgery patients.
Dr. McKean: I’d like to make a point about combination prophylaxis. At many institutions, compression stockings and sequential compression devices are used preoperatively and intraoperatively, and then pharmacologic prophylaxis—for example, twice-daily UFH—is used postoperatively. There is concern that these patients are hypercoagulable, and most clinicians believe that mechanical prophylaxis alone, even with sequential compression devices plus compression stockings, is not aggressive enough in these high-risk patients.
Dr. Jaffer: Dr. Spyropoulos, what is the optimal duration of pharmacologic prophylaxis for cancer surgery patients?
Dr. Spyropoulos: First let’s consider in-hospital prophylaxis. The supportive data for in-hospital prophylaxis are strong, and the duration of therapy used in the major in-hospital prophylaxis trials was 7 to 10 days. With regard to extended prophylaxis, we have at least two moderately sized randomized controlled trials, ENOXACAN II23 and the substudy of FAME,24 that demonstrated that extending prophylaxis with LMWH at doses of 3,400 U once daily (5,000 IU of dalteparin; 40 mg of enoxaparin) reduces VTE risk at postoperative day 30. Also, recent data from the @RISTOS registry show that in cancer surgery patients, especially those having abdominal or pelvic procedures, the leading cause of 30-day mortality was VTE.8 This registry also shows that despite prophylaxis, the rate of symptomatic VTE can be as high as 2%, with the rate of fatal VTE approaching 1%. Thus, in cancer patients undergoing abdominal or pelvic surgery, physicians should strongly consider prophylaxis of up to 30 days’ duration.
Dr. Jaffer: One striking finding from the @RISTOS registry was that 40% of VTE events in these cancer surgery patients occurred after postoperative day 21. This really underscores the need to consider prophylaxis for at least 4 weeks in these patients in real-world practice.
Dr. Brotman: The other striking finding from that registry was that the in-hospital prophylaxis rate was quite high, about 80%, and the rate of extended prophylaxis approached 35%. These are rates that are rarely achieved in clinical practice. Yet despite these high levels of prophylaxis, patients in this registry still had a high incidence of morbidity and mortality from VTE. This suggests that we need to improve our out-of-hospital VTE prevention paradigms.
Dr. Jaffer: Dr. Deitelzweig, oncologists and internists are often unsure about whether their ambulatory cancer patients who are receiving chemotherapy should be on any form of prophylaxis. What is your opinion?
Dr. Deitelzweig: That question comes up regularly because these patients are encountered across many medical specialties. At this point, all of the large organizations, including ASCO and NCCN, are advocating that prophylaxis is not indicated for such patients.
Venous thromboembolism (VTE) is a major complication of cancer, occurring in 4% to 20% of patients,1 and is one of the leading causes of death in cancer patients, although these figures are believed to be underestimates, given the low autopsy rates among cancer patients.2 In hospitalized cancer patients specifically, VTE is the second leading cause of death.3,4 The risk of VTE in cancer patients undergoing surgery is three to five times greater than that in surgical patients without cancer.4 Moreover, cancer patients with symptomatic deep vein thrombosis (DVT) exhibit a high risk of recurrent VTE that may persist for many years after the index event.5
VTE PREVENTION POSES PARTICULAR CHALLENGES IN CANCER PATIENTS
Until recently, data on VTE prevention specific to cancer patients have been sparse. Cancer patients have represented only a small subset (< 20%) of participants in most of the largest clinical trials of VTE prophylaxis. Until the past 2 or 3 years, clinicians largely have had to extrapolate their approach to VTE prophylaxis in cancer patients from data in patients without cancer, bearing in mind that cancer patients are among the populations at highest risk of developing VTE.
High rates of VTE, even with prophylaxis
Further insights have come from the @RISTOS project, a Web-based prospective registry of patients undergoing general, urologic, or gynecologic surgery for cancer at multiple centers in Italy.8 Of the 2,372 patients tracked in this study, 82% received in-hospital VTE prophylaxis and 31% received prophylaxis following discharge. Despite this relatively high frequency of prophylaxis, however, the incidence of clinically overt VTE was 2.1% and the incidence of fatal VTE was 0.8%. Notably, most VTE events occurred after hospital discharge, and VTE was the most common cause of 30-day postoperative death in this registry.
RISK FACTORS: CANCER TYPE AND TREATMENT LOOM LARGE
Both the type and stage of a patient’s cancer are important in assessing the risk of VTE. For men, cancers of the prostate, colon, brain, and lung have been associated with an increased risk of VTE. Among women, cancers of the breast, ovary, and lung have been especially implicated as risk factors for VTE.9,10
The type of cancer therapy also influences VTE risk:
- Surgery. Among patients who undergo cancer-related surgery, the rate of proximal DVT is 10% to 20%, the rate of clinically evident PE is 4% to 10%, and the incidence of fatal PE is 0.2% to 5%.8,11
- Systemic treatments, including chemotherapy and hormone therapy, are also associated with an increased risk of VTE.12–15
- Central venous catheters. Approximately 4% of cancer patients who have central venous catheters placed develop clinically relevant VTE.16,17
In addition to the above risks related to cancer treatments, the following have been identified as risk factors for VTE in surgical oncology patients:
- Age greater than 40 years (risk also increases steeply after age 60 and again after age 75)
- Cancer procoagulants
- Thrombophilia
- Length and complications of cancer surgery (ie, often involving tissue trauma and immobilization)
- Debilitation and slow recovery.
Another risk factor worth noting is perioperative transfusion, as illustrated in a recent study of 14,104 adults undergoing colorectal cancer resection.18 The overall incidence of VTE in these patients was 1.0%, and the risk of death was nearly four times as great in patients who developed VTE as in those who did not. Notably, the need for transfusion was a marker of increased risk of VTE, particularly in women: women who received perioperative transfusions had almost double the risk of developing VTE compared with women who did not receive transfusions (P = .004).
CLINICAL TRIALS OF PROPHYLAXIS IN CANCER SURGERY PATIENTS
LMWH vs UFH for in-hospital prophylaxis
Two large randomized, double-blind trials have compared low-molecular-weight heparin (LMWH) with low-dose unfractionated heparin (UFH) for VTE prophylaxis in surgical patients with cancer—the Enoxaparin and Cancer (ENOXACAN) study19 and the Canadian Colorectal Surgery DVT Prophylaxis Trial.20 Patients in these studies underwent surgery for abdominal or pelvic cancer (mostly colorectal cancer). Both studies compared 40 mg of the LMWH enoxaparin given once daily with 5,000 U of UFH given three times daily for 7 to 10 days postoperatively. Outcome measures were the presence of DVT determined by venography on day 7 to 10 and the incidence of symptomatic VTE. Rates of VTE were statistically equivalent between the two treatment arms in both ENOXACAN (14.7% with LMWH vs 18.2% with UFH) and the Canadian Colorectal Surgery study (9.4% with both therapies), as were rates of major bleeding (4.1% with LMWH vs 2.9% with UFH in ENOXACAN; 2.7% with LMWH vs 1.5% with UFH in the Canadian study).
These findings are consistent with a 2001 meta-analysis by Mismetti et al of all available randomized trials comparing LMWH with placebo or with UFH for VTE prophylaxis in general surgery.21 This analysis found no differences in rates of asymptomatic DVT, clinical PE, clinical thromboembolism, death, major hemorrhage, total hemorrhage, wound hematoma, or need for transfusion between LMWH and UFH in patients undergoing either cancer-related surgery or surgery not related to cancer.
Fondaparinux for in-hospital prophylaxis
Subgroup analysis of the large randomized trial known as PEGASUS22 sheds some light on the efficacy of the factor Xa inhibitor fondaparinux relative to LMWH for thromboprophylaxis in cancer surgery patients. PEGASUS compared fondaparinux 2.5 mg once daily with the LMWH dalteparin 5,000 IU once daily for 5 to 9 days in patients undergoing high-risk abdominal surgery. Among the study’s 1,408 patients undergoing surgery for cancer, rates of VTE were 4.7% in the fondaparinux group compared with 7.7% in the LMWH group, a relative risk reduction of 38.6% with fondaparinux (95% CI, 6.7% to 59.6%). In contrast, in the rest of the PEGASUS population (patients undergoing abdominal surgery for reasons other than cancer), LMWH was nonsignificantly more efficacious at preventing VTE than was fondaparinux. Rates of major bleeding in this cancer subgroup were comparable between the two treatments.
Extended prophylaxis
Two additional randomized trials have evaluated extended prophylaxis with LMWH in surgical cancer patients—ENOXACAN II23 and the Fragmin After Major Abdominal Surgery (FAME) study.24
In ENOXACAN II, patients undergoing surgery for abdominal or pelvic cancer first received 6 to 10 days of prophylaxis with enoxaparin 40 mg once daily and then were randomized in a double-blind fashion to an additional 21 days of enoxaparin or placebo.23 Among 332 patients in the intent-to-treat analysis, the rate of VTE at the end of the double-blind phase was reduced from 12.0% with placebo to 4.8% with extended-duration enoxaparin (P = .02), an effect that was maintained at 3-month follow-up (P = .01). There was no significant difference between the two groups in rates of major bleeding events or any bleeding events.
In FAME, patients received 5,000 IU of dalteparin once daily for 1 week following major abdominal surgery and then were randomized in open-label fashion to either placebo or extended prophylaxis with dalteparin for 3 more weeks; a subanalysis examined outcomes in the 198 FAME participants whose abdominal surgery was for cancer.24 Among these 198 cancer surgery patients, the rate of venography-documented VTE at 4 weeks was reduced from 19.6% with placebo to 8.8% with extended-duration dalteparin, a relative reduction of 55% (P = .03). The rate of proximal DVT was reduced from 10.4% to 2.2% with extended prophylaxis, a relative reduction of 79% (P = .02).
The number needed to treat with extended LMWH prophylaxis to prevent one VTE event was 14 in ENOXACAN II23 and 9 in the FAME subanalysis of cancer surgery patients.24
New systematic review of relevant trials
Leonardi et al recently published a systematic review of 26 randomized controlled trials of DVT prophylaxis in 7,639 cancer surgery patients.25 They found the overall incidence of DVT to be 12.7% in those who received pharmacologic prophylaxis compared with 35.2% in controls. They also found high-dose LMWH therapy (> 3,400 U daily) to be associated with a significantly lower incidence of DVT than low-dose LMWH therapy (≤ 3,400 U daily) (7.9% vs 14.5%, respectively; P < .01). No differences were demonstrated between LMWH and UFH in preventing DVT, DVT location, or bleeding. Bleeding complications requiring discontinuation of pharmacologic prophylaxis occurred in 3% of patients overall.
Implications of HIT
The sequelae of heparin-induced thrombocytopenia (HIT) can have major consequences for cancer surgery patients. The incidence of HIT is markedly lower with LMWH than with UFH, as demonstrated in a nested case-control study by Creekmore et al.26 These researchers also found that the average cost of an admission during which HIT developed was nearly four times as great as the average cost of an admission during which UFH or LMWH was given without development of HIT ($56,364 vs $15,231; P < .001).
EVIDENCE IN SPECIFIC ONCOLOGIC POPULATIONS
Most of the patients in the trials reviewed above underwent abdominal surgery for malignancy. Although studies of VTE prophylaxis in patients undergoing nonabdominal cancer surgery are relatively few, some data are available for a few other specific oncologic populations, as reviewed below.
Surgery for gynecologic cancer
There is a paucity of randomized controlled trials or prospective observational studies on VTE and its prevention in the gynecologic cancer surgery population. Based on small historical studies, the postoperative risk of VTE in this population varies from 12% to 35%.27,28 Twice-daily administration of UFH 5,000 U appears to be ineffective as VTE prophylaxis in this population, but increasing the frequency to three times daily reduces VTE risk by 50% to 60% compared with placebo. Once-daily LMWH is comparable to three-times-daily UFH in efficacy and safety in this population.
A systematic Cochrane review of eight randomized controlled trials in patients undergoing major gynecologic surgery revealed that heparin prophylaxis (either UFH or LMWH) reduces the risk of DVT by 70% compared with no prophylaxis, with an identical risk reduction specifically among women with malignancy (odds ratio, 0.30; 95% CI, 0.10 to 0.89).29 This review found no evidence that anticoagulation reduces the risk of PE following major gynecologic surgery. LMWH and UFH were similar in efficacy for preventing DVT and had a comparable risk of bleeding complications.
Surgery for urologic cancer
The risk of VTE and the benefits of thromboprophylaxis also are poorly studied in patients undergoing surgery for urologic cancer.
The risk of VTE varies with the type of urologic surgery and the method used to diagnose VTE. For instance, patients undergoing radical retropubic prostatectomy have been reported to develop DVT at rates of 1% to 3%, PE at rates of 1% to 3%, and fatal PE at a rate of 0.6%, whereas the incidences of these events are somewhat higher in patients undergoing cystectomy: 8% for DVT, 2% to 4% for PE, and 2% for fatal PE. Radiologic diagnosis of thromboembolism in pelvic surgery patients has yielded higher incidences, with DVT rates of 21% to 51% and PE rates of 11% to 22%.30
Small studies suggest that prophylaxis with either low-dose UFH or LMWH is both effective in reducing VTE risk and safe in urologic cancer surgery patients, although pharmacologic prophylaxis poses a possible increased risk of pelvic hematoma and lymphocele formation in this population.30
Neurosurgery
Most neurosurgical procedures are performed for malignancies. The risk of venography-confirmed VTE in patients undergoing neurosurgery is approximately 30% to 40%.31,32 Likewise, the risks of intracranial or intraspinal hemorrhage in these patients are high. For this reason, mechanical methods of VTE prophylaxis are preferred in these patients. The use of anticoagulant prophylaxis remains controversial in this setting, although more recent data suggest that it might be safer than previously recognized.
GUIDELINES FOR VTE PROPHYLAXIS IN THE CANCER SURGERY PATIENT
American College of Chest Physicians
National Comprehensive Cancer Network
The National Comprehensive Cancer Network (NCCN) recently published clinical practice guidelines on venous thromboembolic disease in cancer patients.35 The defined at-risk population for these guidelines is the adult cancer inpatient with a diagnosis of (or clinical suspicion for) cancer. The guidelines recommend prophylactic anticoagulation (category 1 recommendation) with or without a sequential compression device as initial prophylaxis, unless the patient has a relative contraindication to anticoagulation, in which case mechanical prophylaxis (sequential compression device or graduated compression stockings) is recommended. (A category 1 recommendation indicates “uniform NCCN consensus, based on high-level evidence.”)
The NCCN guidelines include a specific recommended risk-factor assessment, which includes noting the patient’s age (VTE risk increases beginning at age 40 and then steeply again at age 75), any prior VTE, the presence of familial thrombophilia or active cancer, the use of medications associated with increased VTE risk (chemotherapy, exogenous estrogen compounds, and thalidomide or lenalidomide), and a number of other risk factors for VTE as outlined in the prior two articles in this supplement. The NCCN guidelines explicitly call for assessment of modifiable risk factors for VTE (ie, smoking or other tobacco use, obesity, and a low level of activity or lack of exercise) and call for active patient education on these factors.
American Society of Clinical Oncology
Our recommended algorithm
LINGERING CHALLENGE OF UNDERUTILIZATION
Despite this consensus on ways to reduce thromboembolic risk in this population and the clear evidence of the benefit of VTE prophylaxis in patients with cancer, data from several registries confirm a persistently low utilization of prophylaxis in patients with cancer.36–38 The global Fundamental Research in Oncology and Thrombosis (FRONTLINE) study surveyed 3,891 clinicians who treat cancer patients regarding their practices with respect to VTE in those patients.36 The survey found that only 52% of respondents routinely used thromboprophylaxis for their surgical patients with cancer. More striking, however, was the finding that most respondents routinely considered thrombo-prophylaxis in only 5% of their medical oncology patients. These data are echoed by findings of other retrospective medical record reviews in patients undergoing major abdominal or abdominothoracic surgery (in many cases for cancer), with VTE prophylaxis rates ranging from 38% to 75%.37,38
SUMMARY
Patients undergoing surgery for cancer have an increased risk of VTE and fatal PE, even when thromboprophylaxis is used. Nevertheless, prophylaxis with either LMWH or UFH does reduce venographic VTE event rates in these patients. If UFH is chosen for prophylaxis, a three-times-daily regimen should be used in this population. In specific surgical cancer populations, especially those undergoing abdominal surgery, out-of-hospital prophylaxis with once-daily LMWH is warranted. Current registries reveal that compliance with established guidelines for VTE prophylaxis in this population is low.


Dr. Jaffer: Dr. Amin, based on your study on thrombo-prophylaxis rates in US medical centers, will you comment on rates of prophylaxis for cancer surgery patients?
Dr. Amin: The overall study included approximately 200,000 medical patients and about 80,000 surgical patients enrolled over more than a 3-year period between 2002 and 2005.39,40 Our goal was to assess rates of prophylaxis and, when it was provided, whether it was appropriate (in terms of type, dosage, and duration) based on the ACCP guidelines. A subanalysis assessed medical cancer patients and surgical cancer patients separately. Medical cancer patients received thromboprophylaxis 56% of the time but received appropriate prophylaxis only 28% of the time. Among surgical cancer patients, appropriate prophylaxis was given only about 24% of the time for those undergoing gynecologic surgery and about 12% of the time for those undergoing neurosurgery. These percentages are consistent with data from other national registries, such as the IMPROVE registry, which documented prophylaxis rates on the order of 45% in medical patients with cancer.41 We also analyzed the data according to individual practitioners and found that medical oncologists use prophylaxis about 25% of the time, which is relatively consistent with other providers, such as internists and surgeons.
So there is a huge opportunity to improve rates of prophylaxis for this group of patients that national guidelines say are at high risk. Why is prophylaxis so underutilized in the cancer population? One factor may be a misperception about the risk of bleeding with anticoagulants. Yet several studies have shown that the rate of bleeding from prophylaxis is extremely low, whether LMWH or UFH is used, so more awareness of actual bleeding risk is needed. Another factor is the obvious focus among internists and oncologists on treating the patient, with perhaps a reduced consideration of prophylaxis and prevention. A third factor may be a concern about thrombocytopenia. However, in our study of prophylaxis rates in US medical centers, we excluded patients who had thrombocytopenia, yet rates of prophylaxis were still low. Nothing in the literature indicates that anticoagulants cannot be used in patients with platelet counts of 50,000 to 150,000 cells/µL or higher, so this suggests that we need to do more education.
Dr. Jaffer: Dr. Brotman, can you tell us more about how clinicians in practice should use prophylaxis in their neurosurgery patients, such as those undergoing craniotomy or spine surgery for cancer? What is the safest and most efficacious way to prevent DVT in these patients?
Dr. Brotman: First, it’s important to recognize that some sort of prophylaxis needs to be used. Neurosurgery patients are at an extremely high risk for thromboembolic events, and such events are often fatal in these patients. Having said that, the jury is still out on whether the prophylaxis in these patients should be compression devices or anticoagulation. This gives physicians some latitude in their decisions. They can decide not to use pharmacologic prophylaxis so long as they use pneumatic compression devices consistently, perhaps even starting during the operation and certainly throughout hospitalization when the patient is immobilized.
Certainly, the concerns about using full-dose anticoagulation in the immediate postoperative setting in neurosurgery patients are valid. Yet these patients are at very high risk for thromboembolic events, and if we take too cautious an approach to prophylaxis in the immediate perioperative setting, more patients are going to have thromboembolic events, at which point management decisions become much more difficult. The risk of intracranial bleeding with anticoagulation to treat a patient who develops a DVT at postoperative day 10 will certainly be higher than it would have been with lower-dose perioperative prophylactic anticoagulation. Plus, if you put in a filter at that point, the outcomes tend to be poor. Therefore, I believe there is some degree of risk that we should be willing to take with regard to perioperative bleeding, even in neurosurgery patients.
Dr. McKean: I’d like to make a point about combination prophylaxis. At many institutions, compression stockings and sequential compression devices are used preoperatively and intraoperatively, and then pharmacologic prophylaxis—for example, twice-daily UFH—is used postoperatively. There is concern that these patients are hypercoagulable, and most clinicians believe that mechanical prophylaxis alone, even with sequential compression devices plus compression stockings, is not aggressive enough in these high-risk patients.
Dr. Jaffer: Dr. Spyropoulos, what is the optimal duration of pharmacologic prophylaxis for cancer surgery patients?
Dr. Spyropoulos: First let’s consider in-hospital prophylaxis. The supportive data for in-hospital prophylaxis are strong, and the duration of therapy used in the major in-hospital prophylaxis trials was 7 to 10 days. With regard to extended prophylaxis, we have at least two moderately sized randomized controlled trials, ENOXACAN II23 and the substudy of FAME,24 that demonstrated that extending prophylaxis with LMWH at doses of 3,400 U once daily (5,000 IU of dalteparin; 40 mg of enoxaparin) reduces VTE risk at postoperative day 30. Also, recent data from the @RISTOS registry show that in cancer surgery patients, especially those having abdominal or pelvic procedures, the leading cause of 30-day mortality was VTE.8 This registry also shows that despite prophylaxis, the rate of symptomatic VTE can be as high as 2%, with the rate of fatal VTE approaching 1%. Thus, in cancer patients undergoing abdominal or pelvic surgery, physicians should strongly consider prophylaxis of up to 30 days’ duration.
Dr. Jaffer: One striking finding from the @RISTOS registry was that 40% of VTE events in these cancer surgery patients occurred after postoperative day 21. This really underscores the need to consider prophylaxis for at least 4 weeks in these patients in real-world practice.
Dr. Brotman: The other striking finding from that registry was that the in-hospital prophylaxis rate was quite high, about 80%, and the rate of extended prophylaxis approached 35%. These are rates that are rarely achieved in clinical practice. Yet despite these high levels of prophylaxis, patients in this registry still had a high incidence of morbidity and mortality from VTE. This suggests that we need to improve our out-of-hospital VTE prevention paradigms.
Dr. Jaffer: Dr. Deitelzweig, oncologists and internists are often unsure about whether their ambulatory cancer patients who are receiving chemotherapy should be on any form of prophylaxis. What is your opinion?
Dr. Deitelzweig: That question comes up regularly because these patients are encountered across many medical specialties. At this point, all of the large organizations, including ASCO and NCCN, are advocating that prophylaxis is not indicated for such patients.
- Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007; 25:5490–5505.
- Khorana AA, Francis CW, Culakova E, et al. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost 2007; 5:632–634.
- Ambrus JL, Ambrus CM, Mink IB, Pickren JW. Causes of death in cancer patients. J Med 1975; 6:61–64.
- Donati MB. Cancer and thrombosis. Haemostasis 1994; 24:128–131.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 1996; 125:1–7.
- Haas S, Wolf H, Kakkar AK, Fareed J, Encke A. Prevention of fatal pulmonary embolism and mortality in surgical patients: a randomized double-blind comparison of LMWH with unfractionated heparin. Thromb Haemost 2005; 94:814–819.
- Kakkar AK, Haas S, Wolf H, Encke A. Evaluation of perioperative fatal pulmonary embolism and death in cancer surgical patients: the MC-4 cancer substudy. Thromb Haemost 2005; 94:867–871.
- Agnelli G, Bolis G, Capussotti L, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 2006; 243:89–95.
- Levitan N, Dowlati A, Remick SC, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy: risk analysis using Medicare claims data. Medicine (Baltimore) 1999; 78:285–291.
- Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med 1996; 334:677–681.
- Bergqvist D. Risk of venous thromboembolism in patients undergoing cancer surgery and options for thromboprophylaxis. J Surg Oncol 2007; 95:167–174.
- Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 2000; 160:809–815.
- Sallah S, Wan JY, Nguyen NP. Venous thrombosis in patients with solid tumors: determination of frequency and characteristics. Thromb Haemost 2002; 87:575–579.
- Kröger K, Weiland D, Ose C, et al. Risk factors for venous thromboembolic events in cancer patients. Ann Oncol 2006; 17:297–303.
- Blom JW, Vanderschoot JP, Oostindiër MJ, et al. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: results of a record linkage study. J Thromb Haemost 2006; 4:529–535.
- Couban S, Simpson DR, Barnett MJ, et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 2002; 100:1525–1531.
- Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002; 20:3276–3281.
- Nilsson KR, Berenholtz SM, Garrett-Mayer E, et al. Association between venous thromboembolism and perioperative allogeneic transfusion. Arch Surg 2007; 142:126–133.
- Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. ENOXACAN Study Group. Br J Surg 1997; 84:1099–1103.
- McLeod RS, Geerts WH, Sniderman KW, et al. Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian Colorectal DVT Prophylaxis Trial: a randomized, double-blind trial. Ann Surg 2001; 233:438–444.
- Mismetti P, Laporte S, Darmon JY, Buchmüller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg 2001; 88:913–930.
- Agnelli G, Bergqvist D, Cohen AT, et al, on behalf of the PEGASUS investigators. Randomized clinical trial of postoperative fondaparinux versus perioperative dalteparin for prevention of venous thromboembolism in high-risk abdominal surgery. Br J Surg 2005; 92:1212–1220.
- Bergqvist D, Agnelli G, Cohen AT, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 2002; 346:975–980.
- Rasmussen MS, Wille-Jorgensen P, Jorgensen LN, et al. Prolonged thromboprophylaxis with low molecular weight heparin (dalteparin) following major abdominal surgery for malignancy [abstract 186]. Blood 2003; 102:56a.
- Leonardi MJ, McGory ML, Ko CY. A systematic review of deep venous thrombosis prophylaxis in cancer patients: implications for improving quality. Ann Surg Oncol 2007; 14:929–936.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Walsh JJ, Bonnar J, Wright FW. A study of pulmonary embolism and deep leg vein thrombosis after major gynaecological surgery using labeled fibrinogen-phlebography and lung scanning. J Obstet Gynaecol Br Commonw 1974; 81:311–316.
- Clarke-Pearson DL, Synan IS, Coleman RE, et al. The natural history of postoperative venous thromboemboli in gynecologic oncology: a prospective study of 382 patients. Am J Obstet Gynecol 1984; 148:1051–1054.
- Oates-Whitehead RM, D’Angelo A, Mol B. Anticoagulant and aspirin prophylaxis for preventing thromboembolism after major gynaecological surgery. Cochrane Database Syst Rev 2003; (4):CD003679.
- Kibel AS, Loughlin KR. Pathogenesis and prophylaxis of postoperative thromboembolic disease in urological pelvic surgery. J Urol 1995; 153:1763–1774.
- Agnelli G, Piovella F, Buoncristiani P, et al. Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 1998; 339:80–85.
- Semrad TJ, O’Donnell R, Wun T, et al. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 2007; 106:601–608.
- Iorio A, Agnelli G. Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Intern Med 2000; 160:2327–2332.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Venous thromboembolic disease. V.1.2007. http://www.nccn.org/professionals/physician_gls/PDF/vte.pdf. Accessed December 5, 2007.
- Kakkar AK, Levine M, Pinedo HM, Wolff R, Wong J. Venous thrombosis in cancer patients: insights from the FRONTLINE survey. Oncologist 2003; 8:381–388.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- Bratzler DW, Raskob GE, Murray CK, Bumpus LJ, Piatt DS. Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting. Arch Intern Med 1998; 158:1909–1912.
- Amin A, Stemkowski S, Lin J, et al. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis in US hospitals: adherence to the 6th American College of Chest Physicians’ recommendations for at-risk medical and surgical patients. Abstract presented at: 41st Midyear Clinical Meeting of the American Society of Health-System Pharmacists; December 3–7, 2006; Anaheim, CA.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Clarke-Pearson DL, Synan IS, Dodge R, et al. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol 1993; 168:1146–1154.
- Einstein MH, Pritts EA, Hartenbach EM. Venous thromboembolism prevention in gynecologic cancer surgery: a systematic review. Gynecol Oncol 2007; 105:813–819.
- Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol 1984; 63:92–98.
- Ruff RL, Posner JB. Incidence and treatment of peripheral venous thrombosis in patients with glioma. Ann Neurol 1983; 13:334–336.
- Levin JM, Schiff D, Loeffler JS, Fine HA, Black PM, Wen PY. Complications of therapy for venous thromboembolic disease in patients with brain tumors. Neurology 1993; 43:1111–1114.
- Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007; 25:5490–5505.
- Khorana AA, Francis CW, Culakova E, et al. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost 2007; 5:632–634.
- Ambrus JL, Ambrus CM, Mink IB, Pickren JW. Causes of death in cancer patients. J Med 1975; 6:61–64.
- Donati MB. Cancer and thrombosis. Haemostasis 1994; 24:128–131.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 1996; 125:1–7.
- Haas S, Wolf H, Kakkar AK, Fareed J, Encke A. Prevention of fatal pulmonary embolism and mortality in surgical patients: a randomized double-blind comparison of LMWH with unfractionated heparin. Thromb Haemost 2005; 94:814–819.
- Kakkar AK, Haas S, Wolf H, Encke A. Evaluation of perioperative fatal pulmonary embolism and death in cancer surgical patients: the MC-4 cancer substudy. Thromb Haemost 2005; 94:867–871.
- Agnelli G, Bolis G, Capussotti L, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 2006; 243:89–95.
- Levitan N, Dowlati A, Remick SC, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy: risk analysis using Medicare claims data. Medicine (Baltimore) 1999; 78:285–291.
- Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med 1996; 334:677–681.
- Bergqvist D. Risk of venous thromboembolism in patients undergoing cancer surgery and options for thromboprophylaxis. J Surg Oncol 2007; 95:167–174.
- Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 2000; 160:809–815.
- Sallah S, Wan JY, Nguyen NP. Venous thrombosis in patients with solid tumors: determination of frequency and characteristics. Thromb Haemost 2002; 87:575–579.
- Kröger K, Weiland D, Ose C, et al. Risk factors for venous thromboembolic events in cancer patients. Ann Oncol 2006; 17:297–303.
- Blom JW, Vanderschoot JP, Oostindiër MJ, et al. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: results of a record linkage study. J Thromb Haemost 2006; 4:529–535.
- Couban S, Simpson DR, Barnett MJ, et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 2002; 100:1525–1531.
- Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002; 20:3276–3281.
- Nilsson KR, Berenholtz SM, Garrett-Mayer E, et al. Association between venous thromboembolism and perioperative allogeneic transfusion. Arch Surg 2007; 142:126–133.
- Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. ENOXACAN Study Group. Br J Surg 1997; 84:1099–1103.
- McLeod RS, Geerts WH, Sniderman KW, et al. Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian Colorectal DVT Prophylaxis Trial: a randomized, double-blind trial. Ann Surg 2001; 233:438–444.
- Mismetti P, Laporte S, Darmon JY, Buchmüller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg 2001; 88:913–930.
- Agnelli G, Bergqvist D, Cohen AT, et al, on behalf of the PEGASUS investigators. Randomized clinical trial of postoperative fondaparinux versus perioperative dalteparin for prevention of venous thromboembolism in high-risk abdominal surgery. Br J Surg 2005; 92:1212–1220.
- Bergqvist D, Agnelli G, Cohen AT, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 2002; 346:975–980.
- Rasmussen MS, Wille-Jorgensen P, Jorgensen LN, et al. Prolonged thromboprophylaxis with low molecular weight heparin (dalteparin) following major abdominal surgery for malignancy [abstract 186]. Blood 2003; 102:56a.
- Leonardi MJ, McGory ML, Ko CY. A systematic review of deep venous thrombosis prophylaxis in cancer patients: implications for improving quality. Ann Surg Oncol 2007; 14:929–936.
- Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy 2006; 26:1438–1445.
- Walsh JJ, Bonnar J, Wright FW. A study of pulmonary embolism and deep leg vein thrombosis after major gynaecological surgery using labeled fibrinogen-phlebography and lung scanning. J Obstet Gynaecol Br Commonw 1974; 81:311–316.
- Clarke-Pearson DL, Synan IS, Coleman RE, et al. The natural history of postoperative venous thromboemboli in gynecologic oncology: a prospective study of 382 patients. Am J Obstet Gynecol 1984; 148:1051–1054.
- Oates-Whitehead RM, D’Angelo A, Mol B. Anticoagulant and aspirin prophylaxis for preventing thromboembolism after major gynaecological surgery. Cochrane Database Syst Rev 2003; (4):CD003679.
- Kibel AS, Loughlin KR. Pathogenesis and prophylaxis of postoperative thromboembolic disease in urological pelvic surgery. J Urol 1995; 153:1763–1774.
- Agnelli G, Piovella F, Buoncristiani P, et al. Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 1998; 339:80–85.
- Semrad TJ, O’Donnell R, Wun T, et al. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 2007; 106:601–608.
- Iorio A, Agnelli G. Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Intern Med 2000; 160:2327–2332.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Venous thromboembolic disease. V.1.2007. http://www.nccn.org/professionals/physician_gls/PDF/vte.pdf. Accessed December 5, 2007.
- Kakkar AK, Levine M, Pinedo HM, Wolff R, Wong J. Venous thrombosis in cancer patients: insights from the FRONTLINE survey. Oncologist 2003; 8:381–388.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 American College of Chest Physicians consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- Bratzler DW, Raskob GE, Murray CK, Bumpus LJ, Piatt DS. Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting. Arch Intern Med 1998; 158:1909–1912.
- Amin A, Stemkowski S, Lin J, et al. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 2007; 5:1610–1616.
- Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis in US hospitals: adherence to the 6th American College of Chest Physicians’ recommendations for at-risk medical and surgical patients. Abstract presented at: 41st Midyear Clinical Meeting of the American Society of Health-System Pharmacists; December 3–7, 2006; Anaheim, CA.
- Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest 2007; 132:936–945.
- Clarke-Pearson DL, Synan IS, Dodge R, et al. A randomized trial of low-dose heparin and intermittent pneumatic calf compression for the prevention of deep venous thrombosis after gynecologic oncology surgery. Am J Obstet Gynecol 1993; 168:1146–1154.
- Einstein MH, Pritts EA, Hartenbach EM. Venous thromboembolism prevention in gynecologic cancer surgery: a systematic review. Gynecol Oncol 2007; 105:813–819.
- Clarke-Pearson DL, Synan IS, Hinshaw WM, Coleman RE, Creasman WT. Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol 1984; 63:92–98.
- Ruff RL, Posner JB. Incidence and treatment of peripheral venous thrombosis in patients with glioma. Ann Neurol 1983; 13:334–336.
- Levin JM, Schiff D, Loeffler JS, Fine HA, Black PM, Wen PY. Complications of therapy for venous thromboembolic disease in patients with brain tumors. Neurology 1993; 43:1111–1114.
Prevention of venous thromboembolism in the orthopedic surgery patient
Nearly half of orthopedic surgery patients do not receive appropriate prophylaxis for venous thromboembolism (VTE), as defined by American College of Chest Physicians (ACCP) consensus guidelines, according to a recent analysis of a nationwide database of hospital admissions.1 Even in teaching hospitals, compliance with consensus guidelines for thromboprophylaxis is suboptimal. In a study of adherence to the ACCP guidelines for VTE prevention among 1,907 surgical patients at 10 teaching hospitals, only 45.2% of hip fracture patients received optimal VTE prophylaxis.2 Rates of optimal prophylaxis were higher among patients undergoing hip arthroplasty and knee arthroplasty—84.3% and 75.9%, respectively—but were still in need of improvement.2
GROWING INTEREST IN POSTOPERATIVE VTE PROPHYLAXIS AS A QUALITY INDICATOR
As noted in the introductory article in this supplement, the Joint Commission on Accreditation of Healthcare Organizations has taken notice of these shortcomings and has proposed national consensus standards for VTE prevention and treatment.3 Among its proposed standards are two related to risk assessment and prophylaxis: whether risk assessment/prophylaxis is ordered within 24 hours of hospital admission and within 24 hours of transfer to the intensive care unit.
Other quality-monitoring initiatives are focused specifically on VTE in the surgical population. The Surgical Care Improvement Project (SCIP) has approved two quality measures with respect to VTE prevention: (1) the proportion of surgical patients for whom recommended VTE prophylaxis is ordered, and (2) the proportion of patients who receive appropriate VTE prophylaxis (based on ACCP guideline recommendations) within 24 hours before or after surgery.4
In the future, two other VTE-related quality measures from SCIP may be implemented by the Centers for Medicare and Medicaid Services: (1) how often intra- or postoperative pulmonary embolism (PE) is diagnosed during the index hospitalization and within 30 days of surgery, and (2) how often intra- or postoperative deep vein thrombosis (DVT) is diagnosed during the index hospitalization and within 30 days of surgery.5
VTE RISK IN ORTHOPEDIC SURGERY
Surgical patients can be stratified into four VTE risk levels—low, moderate, high, and highest—based on age, surgery type, surgery duration, duration of immobilization, and other risk factors.6 For patients undergoing orthopedic surgery, these levels may be defined according to the following patient and surgical characteristics:
- Low risk—surgery duration of less than 30 minutes, age less than 40 years, repair of small fractures
- Moderate risk—age of 40 to 60 years, arthroscopy or repair of lower leg fractures, postoperative plaster cast
- High risk—age greater than 60 years, or age 40 to 60 years with additional VTE risk factors, or immobilization for greater than 4 days
- Highest risk—hip or knee arthroplasty, hip fracture repair, repair of open lower leg fractures, major trauma or spinal cord injury, or multiple risk factors for VTE (age > 40 years, prior VTE, cancer, or hypercoagulable state).
For patients in the low-risk category, no specific prophylaxis is indicated beyond early and aggressive ambulation.6 For those in all other risk categories, prophylaxis with pharmacologic anticoagulant agents and/or mechanical devices is indicated, as reviewed below.
All major orthopedic procedures confer highest risk level
Notably, the “highest risk” category includes any patient undergoing hip or knee arthroplasty or hip fracture repair. Among orthopedic surgery patients in this highest-risk category, rates of VTE events in the absence of prophylaxis are as follows:6
- Calf DVT, 40% to 80%
- Proximal DVT, 10% to 20%
- Clinical PE, 4% to 10%
- Fatal PE, 0.2% to 5%.
Hip replacement poses greater risk than knee replacement
Within this overall highest-risk category, thromboembolic risk in the absence of prophylaxis differs among procedures. Although patients undergoing hip replacement and those undergoing knee replacement have similar rates of DVT of any type,6,7 hip replacement is associated with higher rates of the more clinically important events, specifically proximal DVT and PE. In the absence of prophylaxis, proximal DVT occurs in 23% to 36% of hip replacement patients as opposed to 9% to 20% of knee replacement patients; similarly, PE occurs in 0.7% to 30% of hip replacement patients as compared with 1.8% to 7.0% of knee replacement patients.6,7
What about bleeding risk?
For many orthopedic surgeons, the risk of bleeding as a result of anticoagulant prophylaxis of VTE looms larger than the risk of VTE itself. This is likely because bleeding, when it does occur, is likely to occur more acutely than VTE does and may directly compromise the result of the operation. For this reason, orthopedic surgeons may be more likely to actually witness bleeding events than VTE events (especially fatal PEs) while their patients are still under their care, leading to a misperception of the relative risks of anticoagulation-related bleeding and thromboembolism.
In reality, rates of major bleeding with pharmacologic prophylaxis of VTE are a tiny fraction of the above-listed rates of VTE events in the absence of prophylaxis in patients undergoing major orthopedic surgery. Reported 30-day rates of major bleeding in patients receiving VTE prophylaxis with heparins range from 0.2% to 1.7%; these rates barely differ from the rates among placebo recipients in the same VTE prophylaxis trials, which range from 0.2% to 1.5%.8,9 Additionally, within the continuum of risk of major bleeding from various medical interventions, VTE prophylaxis with heparins is one of the lowest-risk interventions, posing far less risk than, for example, the use of warfarin in ischemic stroke patients or in patients older than 75 years.
PHARMACOLOGIC OPTIONS FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
As reviewed in the introductory article of this supplement, the arsenal of anticoagulants for use in VTE prophylaxis includes low-dose unfractionated heparin (UFH), low-molecular-weight heparin (LMWH) agents such as dalteparin and enoxaparin, and the factor Xa inhibitor fondaparinux. A few additional comments about these and other anticoagulant options is warranted in the specific context of orthopedic surgery.
Fondaparinux. Because most of its formal US indications are for use as VTE prophylaxis in major orthopedic surgery—including hip replacement, knee replacement, and hip fracture repair—fondaparinux has been studied more widely in orthopedic surgery patients than in the other populations reviewed earlier in this supplement. Nevertheless, its use even in these settings has remained somewhat limited. This may be because of concerns over possible increased bleeding risk relative to some other anticoagulants. Because of bleeding risk, fondaparinux is contraindicated in patients who weigh less than 50 kg, and its package insert recommends caution when it is used in the elderly due to an increased risk of bleeding in patients aged 65 or older. Additionally, the Pentasaccharide in Major Knee Surgery (PENTAMAKS) study found fondaparinux to be associated with a significantly higher incidence of major bleeding compared with enoxaparin (2.1% vs 0.2%; P = .006) in major knee surgery, although it was superior to enoxaparin in preventing VTE.10 Other possible reasons for slow adoption of fondaparinux include its long half-life, which results in a sustained antithrombotic effect, its lack of easy reversibility, and a contraindication in patients with renal insufficiency.11
Limited role for UFH. Low-dose UFH has a more limited role in orthopedic surgery than in other settings requiring VTE prophylaxis, as current ACCP guidelines for VTE prevention recognize it only as a possible option in hip fracture surgery and state that it is not to be considered as sole prophylaxis in patients undergoing hip or knee replacement.6
Warfarin. Although not indicated for use in other VTE prophylaxis settings, the vitamin K antagonist warfarin is recommended as an option for all three major orthopedic surgery indications—knee replacement, hip replacement, and hip fracture repair.6
The key to effective prophylaxis with warfarin is achieving the appropriate intensity of anticoagulation. In two separate analyses, Hylek et al demonstrated a balance between safety and efficacy with warfarin therapy targeted to an international normalized ratio (INR) of 2.0 to 3.0.12,13 An INR greater than 4.0 greatly increased the risk of intracranial hemorrhage, whereas thrombosis was not effectively prevented with an INR less than 2.0.12,13 This latter point should be stressed to orthopedic surgeons, who sometimes aim for INR values below 2.0.
Although anticoagulation clinics are superior to usual care at maintaining the INR within the window of 2.0 to 3.0, only about one-third of patients nationally who take warfarin receive care in such clinics.14 Even with optimal care in anticoagulation clinics, some patients will still receive subtherapeutic or supertherapeutic levels of warfarin, which is one of this agent’s limitations.
Aspirin not recommended as sole agent. Although aspirin is still used as thromboprophylaxis in orthopedic surgery patients, current ACCP guidelines recommend against its use as the sole means of VTE prophylaxis in any patient group.6 The limitations of the evidence for aspirin in this setting are illustrated by the Pulmonary Embolism Prevention study, a multicenter randomized trial in patients undergoing hip fracture (n = 13,356) or hip/knee replacement (n = 4,088).15 Patients received aspirin 160 mg/day or placebo for 5 weeks, starting preoperatively, and were evaluated for outcomes at day 35. Among the hip fracture patients, the rate of symptomatic DVT was lower in the aspirin group than in the placebo group (1.0% vs 1.5%; P = .03), as was the rate of PE (0.7% vs 1.2%, respectively; P = .002), but there was no significant difference in outcomes between the groups among the patients undergoing hip or knee replacement. Notably, 40% of patients in the study also received UFH or LMWH. Further confounding the results, some patients received nonpharmacologic VTE prophylaxis modalities, and others received nonsteroidal anti-inflammatory drugs other than aspirin.
Heparin-induced thrombocytopenia. As noted earlier in this supplement, the incidence of heparin-induced thrombocytopenia (HIT) is markedly higher in patients who receive UFH than in those who receive LMWH. This difference in frequency, which constitutes about a sixfold to eightfold differential, is due to the relationship between standard heparin and platelet factor IV, which can induce formation of IgG antibodies.16 A 50% or greater reduction in platelet count in heparin recipients should prompt consideration of HIT.
Oral direct thrombin inhibitors. Although the oral direct thrombin inhibitor ximelagatran was rejected for approval by the US Food and Drug Administration (FDA) and recently withdrawn from the market worldwide as a result of hepatic risks, other oral direct thrombin inhibitors are in phase 3 studies for use in orthopedic surgery and may be commercially available options for postoperative VTE prophylaxis before long.
GUIDELINES FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
The ACCP guidelines referred to throughout this article are widely recognized as a practice standard for VTE prevention and treatment, and have been regularly updated throughout recent decades. The most recent version, issued in 2004, is formally known as the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.6 Key orthopedic surgery-related recommendations and notable changes from the previous version of the guidelines, issued in 2001, are outlined below, along with pertinent supportive or illustrative studies.
Hip replacement surgery
In a change from the previous guidelines, the Seventh ACCP Conference recommends extended prophylaxis, for up to 28 to 35 days after surgery, for patients undergoing hip replacement or hip fracture surgery. For hip replacement surgery, this is a Grade 1A recommendation for prophylaxis with either LMWH or warfarin and a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”) for prophylaxis with fondaparinux.6
Knee replacement surgery
The same three anticoagulant options that received Grade 1A recommendations for patients undergoing total hip replacement—LMWH, fondaparinux, and adjusted-dose warfarin—are also given Grade 1A recommendations as routine thromboprophylaxis in patients undergoing elective knee replacement (see Table 1 for dosing). In addition, optimal use of intermittent pneumatic compression devices is recommended as an alternative option to anticoagulant prophylaxis in these patients (Grade 1B, indicating a “strong recommendation” based on RCTs with important limitations). Use of UFH as the sole agent for prophylaxis is recommended against.6
For both hip and knee replacement surgery, the Seventh ACCP Conference does not endorse superiority of any one of its three recommended prophylaxis options—LMWH, fondaparinux, and adjusted-dose warfarin—over the other two. However, at least four large randomized trials have directly compared LMWH and adjusted-dose warfarin in the setting of arthroplasty—two in total hip replacement surgery19,20 and two in total knee replacement surgery.21,22 Each of these four studies found LMWH to be significantly more effective than warfarin in preventing VTE. In three of the four trials, there was no significant difference between the therapies in rates of major bleeding.19,21,22 In the remaining trial, which was conducted in hip replacement surgery patients and compared postoperative warfarin with dalteparin initiated either immediately before or early after surgery, patients who received preoperative dalteparin initiation (but not those who received postoperative dalteparin initiation) had an increased rate of major bleeding compared with warfarin recipients (P = .01).20
Hip fracture surgery
The supportive evidence for anticoagulant prophylaxis in hip fracture surgery is less robust than that in hip and knee replacement surgery. As a result, only fondaparinux has a Grade 1A recommendation as routine prophylaxis in patients undergoing hip fracture surgery. Options with less definitive recommendations are LMWH (Grade 1C+), low-dose UFH (Grade 1B), and adjusted-dose warfarin (Grade 2B, indicating a “weak recommendation” based on RCTs with important limitations) (see Table 1 for dosing of all agents).6
These differing recommendations are supported by the double-blind Pentasaccharide in Hip Fracture Surgery Study (PENTHIFRA) of 1,711 consecutive patients undergoing surgery for hip fracture repair.23 Patients were randomized to at least 5 days of fondaparinux 2.5 mg once daily, initiated postoperatively, or enoxaparin 40 mg once daily, initiated preoperatively. The incidence of DVT or PE by postoperative day 11 was 8.3% in the fondaparinux arm versus 19.1% in the enoxaparin arm, a statistically significant difference (P < .001) in favor of fondaparinux. There were no differences between the groups in rates of death or clinically relevant bleeding.
As noted above, the newly added recommendation in the Seventh ACCP Conference for extended prophylaxis, for up to 28 to 35 days after surgery, applies to patients undergoing hip fracture surgery as well as those undergoing hip replacement surgery. In the setting of hip fracture repair, extended prophylaxis is a Grade 1A recommendation with the use of fondaparinux and a Grade 1C+ recommendation with the use of either LMWH or adjusted-dose warfarin.6
Lower extremity fractures and trauma
Although lower extremity fractures are very common, the risk of DVT has been poorly studied in this setting. For patients with isolated lower extremity fractures, the Seventh ACCP Conference recommends that clinicians not use thromboprophylaxis routinely (Grade 2A, indicating an “intermediate-strength recommendation” based on RCTs without important limitations).6
Trauma patients, in contrast, are well recognized as being at very high risk for DVT and PE. The Seventh ACCP Conference gives a Grade 1A recommendation to thromboprophylaxis for all trauma patients who have at least one risk factor for VTE. LMWH is recommended (Grade 1A) as the agent of choice for this purpose, provided there are no contraindications to its use, and should be administered as soon as safely possible. Mechanical modalities are reserved for trauma patients with active bleeding or high risk for hemorrhage (Grade 1B). The guidelines recommend against use of inferior vena cava (IVC) filters as primary thromboprophylaxis in trauma patients (Grade 1C, indicating an “intermediate-strength recommendation” based on observational studies).6
Use of ultrasonography
Duplex ultrasonographic screening is recommended in orthopedic trauma patients who are at high risk for VTE and have received suboptimal or no prophylaxis (Grade 1C). In contrast, the Seventh ACCP Conference recommends against routine use of duplex ultrasonography to screen for VTE at hospital discharge in asymptomatic patients following major orthopedic surgery (Grade 1A).6
Knee arthroscopy
Arthroscopic knee procedures are increasing in frequency and raise the specter of a potential role for thromboprophylaxis. However, the clinical diagnosis of DVT is unreliable, and even diagnosis by ultrasonography is unreliable following knee arthroscopy, as interpreting scans of veins below the knee is challenging in this setting.24
The Seventh ACCP Conference recommends that clinicians not use routine thromboprophylaxis, other than early mobilization, for patients who undergo knee arthroscopy (Grade 2B). However, for arthroscopy patients who have inherent risk factors for VTE or who undergo a prolonged or complicated arthroscopy procedure, thromboprophylaxis with LMWH is suggested (Grade 2B).6
RECOMMENDED APPROACH TO VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
Drawing on the ACCP guidelines and the evidence reviewed above, we have outlined our evidence-based recommendations for pharmacologic VTE prophylaxis in patients undergoing orthopedic surgery, as presented in Table 1. All patients undergoing major orthopedic surgical procedures (ie, procedures other than arthroscopy) should routinely receive anticoagulant prophylaxis unless they have contraindications to anticoagulation. Recommended agents and their duration of use vary according to the type of surgery, as detailed in Table 1.
Extended-duration prophylaxis is recommended for patients undergoing total hip replacement and hip fracture surgery. Aspirin is not recommended as the sole agent for prophylaxis in any orthopedic surgery setting.
Importance of a postoperative prophylaxis protocol
In addition to these broad pharmacologic recommendations, it is important that a postoperative VTE prophylaxis protocol be in place at all hospitals.
At the Ochsner Medical Center in New Orleans, where one of us (S.B.D.) practices, postoperative orders include antithrombotic therapy for surgical patients, starting with placement of thigh-high antiembolism stockings on both legs on the day of surgery for patients undergoing hip replacement and on postoperative day 1 in those undergoing knee replacement. Plantar pneumatic compression devices are applied to both legs in the recovery room and kept on except when the patient is walking. The hospitalist team dictates further anticoagulation orders. If extended prophylaxis is prescribed, the discharge planner sets up drug delivery and reimbursement, provides a LMWH discharge kit, and teaches the patient to self-inject. If there is concern about increasing swelling at the surgical site while anticoagulant therapy continues, the protocol calls for prompt notification of the responsible physician. To minimize the risk that spinal or epidural hematomas will develop, all agents that increase bleeding propensity should be recognized and ordered accordingly.
SUMMARY
VTE in patients undergoing major orthopedic surgery is a serious health problem that is highly preventable, yet VTE prophylaxis remains underused in this patient population. Despite the availability of practice guidelines for VTE prevention in the orthopedic surgery setting, recommendations are not widely implemented in clinical practice. Recommended prophylactic options differ somewhat among various orthopedic procedures, and the supportive evidence differs for various anticoagulant options.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: The ACCP recommends against the routine use of aspirin as primary prophylaxis against VTE in major orthopedic surgery, yet orthopedic surgeons across the country still continue to use aspirin in this setting. What are your thoughts on this, Dr. McKean?
Dr. McKean: We agree with the ACCP’s recommendation against aspirin as primary VTE prophylaxis in orthopedic patients. The percentage of US knee arthroplasty patients who develop VTE after receiving no prophylaxis at all is roughly 64%; this percentage declines only slightly (to 56%) for knee arthroplasty patients who receive prophylaxis with aspirin.25 Since we clearly want to reduce VTE risk as much as possible, I would not use aspirin alone. I would use it only if the patient were already on aspirin, but then I would add either LMWH or fondaparinux.
Dr. Jaffer: Warfarin is another agent that is widely used for prophylaxis in major orthopedic surgery. In fact, the large registries of VTE prevention in major orthopedic surgery suggest that the use of warfarin may be slightly higher than the use of LMWH. If clinicians choose to use warfarin in their practice, what are your recommendations, Dr. Deitelzweig?
Dr. Deitelzweig: As primary prophylaxis for orthopedic surgery patients, warfarin must be dosed to achieve an INR of 2.0 to 3.0; the need for a value in this range is unequivocal. This is a challenging target to attain in the hospital setting.
Dr. Brotman: A study I was involved with a few years ago suggested that warfarin may be inadequate for VTE prevention in the first few days after orthopedic surgery.26 Orthopedic surgeons at the Cleveland Clinic, where I was practicing at the time, routinely used systematic ultrasonography to assess for thrombosis on postoperative day 2 or 3 following hip or knee arthroplasty, so we conducted a secondary analysis of a case-control study in these ultrasonographically screened arthroplasty patients to assess rates of early VTE and look for any associations with the type of prophylaxis used. We found that there was about a tenfold increase in the risk of VTE, both distal and proximal, on postoperative day 2 or 3 among patients who received warfarin compared with those who received LMWH. We concluded that warfarin’s delayed antithrombotic effects may not provide sufficient VTE prophylaxis in the immediate postoperative setting.26
Dr. Deitelzweig: That’s a good point. Although it’s important to achieve a therapeutic level of warfarin, we now have evidence that it takes some time to achieve that level, and in the interim, bad things can happen to patients.
Dr. Jaffer: Orthopedic surgery encompasses several types of procedures. Dr. Amin, which specific orthopedic surgery patients stand to benefit from extended prophylaxis, and how long should extended prophylaxis last?
Dr. Amin: Major orthopedic surgery comprises hip fracture repair, total hip replacement, and total knee replacement. For hip fracture, there are strong data to support the use of extended prophylaxis with fondaparinux 2.5 mg/day, which showed about an 88% relative reduction in the risk of symptomatic VTE compared with standard-duration fondaparinux (6 to 8 days) followed by matching placebo for the extended phase.27 The total duration of fondaparinux therapy in the extended-duration arm was 4 to 5 weeks.
Likewise, data support extended prophylaxis in hip arthroplasty patients, for whom the recommended duration is also 4 to 5 weeks. The systematic review by Hull et al17 demonstrated a 0.41 relative risk of DVT with extended-duration LMWH prophylaxis versus placebo in hip replacement patients (Figure 1), which was a highly statistically significant result.
In contrast, we do not yet have good data to support extended prophylaxis for patients undergoing total knee replacement, which is a bit surprising. In this setting, prophylaxis is recommended for 7 to 14 days but not beyond that.
Dr. Jaffer: Arthroscopy is probably the most common orthopedic procedure performed in the United States today. Dr. Brotman, what is the role of prophylaxis in patients undergoing arthroscopy?
Dr. Brotman: Minor surgery such as arthroscopy can typically be performed safely without routine prophylaxis, other than having the patient ambulate as soon as possible after the procedure. There may be exceptions to this rule, however. I believe that there is potentially a role for pharmacologic prophylaxis in arthroscopy patients who have major risk factors for VTE, such as a personal history of VTE, or who are not expected to become mobile again in a normal rapid fashion after the operation, but prophylaxis has not been studied systematically in such patients.
Dr. Jaffer: Dr. Spyropoulos, there are several new anticoagulants in the pipeline, specifically agents such as the oral direct factor Xa inhibitors and the direct thrombin inhibitors. What do recent clinical trials suggest with regard to the efficacy of these two drug classes for thromboprophylaxis in major orthopedic surgery?
Dr. Spyropoulos: The agents with the most available data are the oral direct factor Xa inhibitors apixaban and rivaroxaban and the oral direct thrombin inhibitor dabigatran. For prophylaxis in orthopedic surgery populations, phase 2 studies have been completed for apixaban and phase 3 trials have been completed for rivaroxaban and dabigatran.
It appears that the factor Xa inhibitors, apixaban and rivaroxaban, are efficacious in comparison with both adjusted-dose warfarin and LMWH, which is the gold standard for this group of patients.28,29 So these indeed appear to be promising agents. Rivaroxaban has been submitted to European regulatory agencies for approval for the prevention of VTE in patients undergoing major orthopedic surgery, and its developer plans to submit it to the FDA in 2008 for a similar indication in the United States.
The data are more equivocal with dabigatran. There have been several positive phase 3 studies in orthopedic surgery comparing two dabigatran dosing schemes, 150 and 220 mg once daily, with the European regimen of enoxaparin (40 mg once daily),30 but a recent study that compared these doses with the North American enoxaparin regimen (30 mg twice daily) failed to meet the criteria for noninferiority.31 Further clinical trial development is necessary for dabigatran, although in January 2008 the European Medicines Agency recommended its marketing approval for thromboprophylaxis in patients undergoing orthopedic procedures.32
I believe that in the next 3 to 5 years our armamentarium will see the addition of at least one, if not more, of these new agents that offer the promise of oral anticoagulation with highly predictable pharmacokinetics and pharmacodynamics and no need for monitoring.
- Yu HT, Dylan ML, Lin J, Dubois RW. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm 2007; 64:69–76.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 ACCP consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- National Consensus Standards for Prevention and Care of Venous Thromboembolism (VTE). The Joint Commission Web site. http://www.jointcommission.org/PerformanceMeasurement/Perform anceMeasurement/VTE.htm. Accessed January 8, 2008.
- Surgical Care Improvement Project. MedQIC Web site. http://www.medqic.org/scip. Accessed January 8, 2008.
- SCIP process and outcome measures, October 2005. MedQIC Web site. http://www.medqic.org. Accessed January 1, 2007.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty.J Am Acad Orthop Surg 1996; 4:54–62.
- Planes A, Vochelle N, Mazas F, et al. Prevention of postoperative venous thrombosis: a randomized trial comparing unfractionated heparin with low molecular weight heparin in patients undergoing total hip replacement. Thromb Haemost 1988; 60:407–410.
- Colwell CW Jr, Spiro TE, Trowbridge AA, et al. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep venous thrombosis after elective knee arthroplasty. Clin Orthop Relat Res 1995; 321:19–27.
- Bauer KA, Eriksson BI, Lassen MR, Turpie AG. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med 2001; 345:1305–1310.
- Turpie AGG. Pentasaccharide Org31540/SR90107A clinical trials update: lessons for practice. Am Heart J 2001; 142(Suppl):S9–S15.
- Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 1994; 120:897–902.
- Hylek EM, Skates SJ, Sheehan MA, Singer DE. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. N Engl J Med 1996; 335:540–546.
- Samsa GP, Matchar DB, Goldstein LB, et al. Quality of anticoagulation management among patients with atrial fibrillation: review of medical records from 2 communities. Arch Intern Med 2000; 160:967–973.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Warkentin TE. Heparin-induced thrombocytopenia: pathogenesis and management. Br J Haemotol 2003; 121:535–555.
- Hull RD, Pineo GF, Stein PD, et al. Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 2001; 135:858–869.
- Haentjens P, De Groote K, Annemans L. Prolonged enoxaparin therapy to prevent venous thromboembolism after primary hip or knee replacement: a cost-utility analysis. Arch Orthop Trauma Surg 2004; 124:507–517.
- Colwell CW Jr, Collis DK, Paulson R, et al. Comparison of enoxaparin and warfarin for the prevention of venous thromboembolic disease after total hip arthroplasty: evaluation during hospitalization and three months after discharge. J Bone Joint Surg Am 1999; 81:932–940.
- Hull RD, Pineo GF, Francis C, et al. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs warfarin in hip arthroplasty patients: a double-blind, randomized comparison. Arch Intern Med 2000; 160:2199–2207.
- Leclerc JR, Geerts WH, Desjardins L, et al. Prevention of venous thromboembolism after knee arthroplasty: a randomized, double-blind trial comparing enoxaparin with warfarin. Ann Intern Med 1996; 124:619–626.
- Fitzgerald RH Jr, Spiro TE, Trowbridge AA, et al. Prevention of venous thromboembolic disease following primary total knee arthroplasty: a randomized, multicenter, open-label, parallel-group comparison of enoxaparin and warfarin. J Bone Joint Surg Am 2001; 83-A:900–906.
- Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med 2001; 345:1298–1304.
- Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med 1998; 158:47–50.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Brotman DJ, Jaffer AK, Hurbanek JG, Morra N. Warfarin prophylaxis and venous thromboembolism in the first 5 days following hip and knee arthroplasty. Thromb Haemost 2004; 92:1012–1017.
- Eriksson BI, Lassen MR; Pentasaccharide in Hip-Fracture Surgery Plus Investigators. Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med 2003; 163:1337–1342.
- The Botticelli Investigators. Late-breaking clinical trial: a dose-finding study of the oral direct factor Xa inhibitor apixaban in the treatment of patients with acute symptomatic deep vein thrombosis [abstract]. Presented at the 21st Congress of the International Society on Thrombosis and Haemostasis; July 2007; Geneva, Switzerland.
- Fisher WD, Eriksson BI, Bauer KA, et al. Rivaroxaban for thromboprophylaxis after orthopaedic surgery: pooled analysis of two studies. Thromb Haemost 2007; 97:931–937.
- Haas S. New oral Xa and IIa inhibitors: updates on clinical trial results. J Thromb Thrombolysis 2008; 25:52–60.
- Friedman RJ, Caprini JA, Comp PC, et al. Dabigatran etexilate vs enoxaparin in preventing venous thromboembolism following total knee arthroplasty. Presented at: 2007 Congress of the International Society on Thrombosis and Haemostasis; July 7–13, 2007; Geneva, Switzerland.
- Committee for Medicinal Products for Human Use summary of positive opinion for Pradaxa [news release]. London, UK: European Medicines Agency. January 24, 2008. http://www.emea.europa.eu/pdfs/human/ opinion/Pradaxa_3503008en.pdf. Accessed February 21, 2008.
- Goldhaber SZ, Grodstein F, Stampfer MJ. A prospective study of risk factors for pulmonary embolism in women. JAMA 1997; 277:642–645.
- Turpie AGG, Bauer KA, Eriksson BI, Lassen MR, for the Steering Committees of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery. Arch Intern Med 2002; 162:1833–1840.
- Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med 2007; 120:871–879.
- Goldhaber SZ. Diagnosis of acute pulmonary embolism: always be vigilant. Am J Med 2007; 120:827–828.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_ summary.pdf. Accessed December 10, 2007.
Nearly half of orthopedic surgery patients do not receive appropriate prophylaxis for venous thromboembolism (VTE), as defined by American College of Chest Physicians (ACCP) consensus guidelines, according to a recent analysis of a nationwide database of hospital admissions.1 Even in teaching hospitals, compliance with consensus guidelines for thromboprophylaxis is suboptimal. In a study of adherence to the ACCP guidelines for VTE prevention among 1,907 surgical patients at 10 teaching hospitals, only 45.2% of hip fracture patients received optimal VTE prophylaxis.2 Rates of optimal prophylaxis were higher among patients undergoing hip arthroplasty and knee arthroplasty—84.3% and 75.9%, respectively—but were still in need of improvement.2
GROWING INTEREST IN POSTOPERATIVE VTE PROPHYLAXIS AS A QUALITY INDICATOR
As noted in the introductory article in this supplement, the Joint Commission on Accreditation of Healthcare Organizations has taken notice of these shortcomings and has proposed national consensus standards for VTE prevention and treatment.3 Among its proposed standards are two related to risk assessment and prophylaxis: whether risk assessment/prophylaxis is ordered within 24 hours of hospital admission and within 24 hours of transfer to the intensive care unit.
Other quality-monitoring initiatives are focused specifically on VTE in the surgical population. The Surgical Care Improvement Project (SCIP) has approved two quality measures with respect to VTE prevention: (1) the proportion of surgical patients for whom recommended VTE prophylaxis is ordered, and (2) the proportion of patients who receive appropriate VTE prophylaxis (based on ACCP guideline recommendations) within 24 hours before or after surgery.4
In the future, two other VTE-related quality measures from SCIP may be implemented by the Centers for Medicare and Medicaid Services: (1) how often intra- or postoperative pulmonary embolism (PE) is diagnosed during the index hospitalization and within 30 days of surgery, and (2) how often intra- or postoperative deep vein thrombosis (DVT) is diagnosed during the index hospitalization and within 30 days of surgery.5
VTE RISK IN ORTHOPEDIC SURGERY
Surgical patients can be stratified into four VTE risk levels—low, moderate, high, and highest—based on age, surgery type, surgery duration, duration of immobilization, and other risk factors.6 For patients undergoing orthopedic surgery, these levels may be defined according to the following patient and surgical characteristics:
- Low risk—surgery duration of less than 30 minutes, age less than 40 years, repair of small fractures
- Moderate risk—age of 40 to 60 years, arthroscopy or repair of lower leg fractures, postoperative plaster cast
- High risk—age greater than 60 years, or age 40 to 60 years with additional VTE risk factors, or immobilization for greater than 4 days
- Highest risk—hip or knee arthroplasty, hip fracture repair, repair of open lower leg fractures, major trauma or spinal cord injury, or multiple risk factors for VTE (age > 40 years, prior VTE, cancer, or hypercoagulable state).
For patients in the low-risk category, no specific prophylaxis is indicated beyond early and aggressive ambulation.6 For those in all other risk categories, prophylaxis with pharmacologic anticoagulant agents and/or mechanical devices is indicated, as reviewed below.
All major orthopedic procedures confer highest risk level
Notably, the “highest risk” category includes any patient undergoing hip or knee arthroplasty or hip fracture repair. Among orthopedic surgery patients in this highest-risk category, rates of VTE events in the absence of prophylaxis are as follows:6
- Calf DVT, 40% to 80%
- Proximal DVT, 10% to 20%
- Clinical PE, 4% to 10%
- Fatal PE, 0.2% to 5%.
Hip replacement poses greater risk than knee replacement
Within this overall highest-risk category, thromboembolic risk in the absence of prophylaxis differs among procedures. Although patients undergoing hip replacement and those undergoing knee replacement have similar rates of DVT of any type,6,7 hip replacement is associated with higher rates of the more clinically important events, specifically proximal DVT and PE. In the absence of prophylaxis, proximal DVT occurs in 23% to 36% of hip replacement patients as opposed to 9% to 20% of knee replacement patients; similarly, PE occurs in 0.7% to 30% of hip replacement patients as compared with 1.8% to 7.0% of knee replacement patients.6,7
What about bleeding risk?
For many orthopedic surgeons, the risk of bleeding as a result of anticoagulant prophylaxis of VTE looms larger than the risk of VTE itself. This is likely because bleeding, when it does occur, is likely to occur more acutely than VTE does and may directly compromise the result of the operation. For this reason, orthopedic surgeons may be more likely to actually witness bleeding events than VTE events (especially fatal PEs) while their patients are still under their care, leading to a misperception of the relative risks of anticoagulation-related bleeding and thromboembolism.
In reality, rates of major bleeding with pharmacologic prophylaxis of VTE are a tiny fraction of the above-listed rates of VTE events in the absence of prophylaxis in patients undergoing major orthopedic surgery. Reported 30-day rates of major bleeding in patients receiving VTE prophylaxis with heparins range from 0.2% to 1.7%; these rates barely differ from the rates among placebo recipients in the same VTE prophylaxis trials, which range from 0.2% to 1.5%.8,9 Additionally, within the continuum of risk of major bleeding from various medical interventions, VTE prophylaxis with heparins is one of the lowest-risk interventions, posing far less risk than, for example, the use of warfarin in ischemic stroke patients or in patients older than 75 years.
PHARMACOLOGIC OPTIONS FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
As reviewed in the introductory article of this supplement, the arsenal of anticoagulants for use in VTE prophylaxis includes low-dose unfractionated heparin (UFH), low-molecular-weight heparin (LMWH) agents such as dalteparin and enoxaparin, and the factor Xa inhibitor fondaparinux. A few additional comments about these and other anticoagulant options is warranted in the specific context of orthopedic surgery.
Fondaparinux. Because most of its formal US indications are for use as VTE prophylaxis in major orthopedic surgery—including hip replacement, knee replacement, and hip fracture repair—fondaparinux has been studied more widely in orthopedic surgery patients than in the other populations reviewed earlier in this supplement. Nevertheless, its use even in these settings has remained somewhat limited. This may be because of concerns over possible increased bleeding risk relative to some other anticoagulants. Because of bleeding risk, fondaparinux is contraindicated in patients who weigh less than 50 kg, and its package insert recommends caution when it is used in the elderly due to an increased risk of bleeding in patients aged 65 or older. Additionally, the Pentasaccharide in Major Knee Surgery (PENTAMAKS) study found fondaparinux to be associated with a significantly higher incidence of major bleeding compared with enoxaparin (2.1% vs 0.2%; P = .006) in major knee surgery, although it was superior to enoxaparin in preventing VTE.10 Other possible reasons for slow adoption of fondaparinux include its long half-life, which results in a sustained antithrombotic effect, its lack of easy reversibility, and a contraindication in patients with renal insufficiency.11
Limited role for UFH. Low-dose UFH has a more limited role in orthopedic surgery than in other settings requiring VTE prophylaxis, as current ACCP guidelines for VTE prevention recognize it only as a possible option in hip fracture surgery and state that it is not to be considered as sole prophylaxis in patients undergoing hip or knee replacement.6
Warfarin. Although not indicated for use in other VTE prophylaxis settings, the vitamin K antagonist warfarin is recommended as an option for all three major orthopedic surgery indications—knee replacement, hip replacement, and hip fracture repair.6
The key to effective prophylaxis with warfarin is achieving the appropriate intensity of anticoagulation. In two separate analyses, Hylek et al demonstrated a balance between safety and efficacy with warfarin therapy targeted to an international normalized ratio (INR) of 2.0 to 3.0.12,13 An INR greater than 4.0 greatly increased the risk of intracranial hemorrhage, whereas thrombosis was not effectively prevented with an INR less than 2.0.12,13 This latter point should be stressed to orthopedic surgeons, who sometimes aim for INR values below 2.0.
Although anticoagulation clinics are superior to usual care at maintaining the INR within the window of 2.0 to 3.0, only about one-third of patients nationally who take warfarin receive care in such clinics.14 Even with optimal care in anticoagulation clinics, some patients will still receive subtherapeutic or supertherapeutic levels of warfarin, which is one of this agent’s limitations.
Aspirin not recommended as sole agent. Although aspirin is still used as thromboprophylaxis in orthopedic surgery patients, current ACCP guidelines recommend against its use as the sole means of VTE prophylaxis in any patient group.6 The limitations of the evidence for aspirin in this setting are illustrated by the Pulmonary Embolism Prevention study, a multicenter randomized trial in patients undergoing hip fracture (n = 13,356) or hip/knee replacement (n = 4,088).15 Patients received aspirin 160 mg/day or placebo for 5 weeks, starting preoperatively, and were evaluated for outcomes at day 35. Among the hip fracture patients, the rate of symptomatic DVT was lower in the aspirin group than in the placebo group (1.0% vs 1.5%; P = .03), as was the rate of PE (0.7% vs 1.2%, respectively; P = .002), but there was no significant difference in outcomes between the groups among the patients undergoing hip or knee replacement. Notably, 40% of patients in the study also received UFH or LMWH. Further confounding the results, some patients received nonpharmacologic VTE prophylaxis modalities, and others received nonsteroidal anti-inflammatory drugs other than aspirin.
Heparin-induced thrombocytopenia. As noted earlier in this supplement, the incidence of heparin-induced thrombocytopenia (HIT) is markedly higher in patients who receive UFH than in those who receive LMWH. This difference in frequency, which constitutes about a sixfold to eightfold differential, is due to the relationship between standard heparin and platelet factor IV, which can induce formation of IgG antibodies.16 A 50% or greater reduction in platelet count in heparin recipients should prompt consideration of HIT.
Oral direct thrombin inhibitors. Although the oral direct thrombin inhibitor ximelagatran was rejected for approval by the US Food and Drug Administration (FDA) and recently withdrawn from the market worldwide as a result of hepatic risks, other oral direct thrombin inhibitors are in phase 3 studies for use in orthopedic surgery and may be commercially available options for postoperative VTE prophylaxis before long.
GUIDELINES FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
The ACCP guidelines referred to throughout this article are widely recognized as a practice standard for VTE prevention and treatment, and have been regularly updated throughout recent decades. The most recent version, issued in 2004, is formally known as the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.6 Key orthopedic surgery-related recommendations and notable changes from the previous version of the guidelines, issued in 2001, are outlined below, along with pertinent supportive or illustrative studies.
Hip replacement surgery
In a change from the previous guidelines, the Seventh ACCP Conference recommends extended prophylaxis, for up to 28 to 35 days after surgery, for patients undergoing hip replacement or hip fracture surgery. For hip replacement surgery, this is a Grade 1A recommendation for prophylaxis with either LMWH or warfarin and a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”) for prophylaxis with fondaparinux.6
Knee replacement surgery
The same three anticoagulant options that received Grade 1A recommendations for patients undergoing total hip replacement—LMWH, fondaparinux, and adjusted-dose warfarin—are also given Grade 1A recommendations as routine thromboprophylaxis in patients undergoing elective knee replacement (see Table 1 for dosing). In addition, optimal use of intermittent pneumatic compression devices is recommended as an alternative option to anticoagulant prophylaxis in these patients (Grade 1B, indicating a “strong recommendation” based on RCTs with important limitations). Use of UFH as the sole agent for prophylaxis is recommended against.6
For both hip and knee replacement surgery, the Seventh ACCP Conference does not endorse superiority of any one of its three recommended prophylaxis options—LMWH, fondaparinux, and adjusted-dose warfarin—over the other two. However, at least four large randomized trials have directly compared LMWH and adjusted-dose warfarin in the setting of arthroplasty—two in total hip replacement surgery19,20 and two in total knee replacement surgery.21,22 Each of these four studies found LMWH to be significantly more effective than warfarin in preventing VTE. In three of the four trials, there was no significant difference between the therapies in rates of major bleeding.19,21,22 In the remaining trial, which was conducted in hip replacement surgery patients and compared postoperative warfarin with dalteparin initiated either immediately before or early after surgery, patients who received preoperative dalteparin initiation (but not those who received postoperative dalteparin initiation) had an increased rate of major bleeding compared with warfarin recipients (P = .01).20
Hip fracture surgery
The supportive evidence for anticoagulant prophylaxis in hip fracture surgery is less robust than that in hip and knee replacement surgery. As a result, only fondaparinux has a Grade 1A recommendation as routine prophylaxis in patients undergoing hip fracture surgery. Options with less definitive recommendations are LMWH (Grade 1C+), low-dose UFH (Grade 1B), and adjusted-dose warfarin (Grade 2B, indicating a “weak recommendation” based on RCTs with important limitations) (see Table 1 for dosing of all agents).6
These differing recommendations are supported by the double-blind Pentasaccharide in Hip Fracture Surgery Study (PENTHIFRA) of 1,711 consecutive patients undergoing surgery for hip fracture repair.23 Patients were randomized to at least 5 days of fondaparinux 2.5 mg once daily, initiated postoperatively, or enoxaparin 40 mg once daily, initiated preoperatively. The incidence of DVT or PE by postoperative day 11 was 8.3% in the fondaparinux arm versus 19.1% in the enoxaparin arm, a statistically significant difference (P < .001) in favor of fondaparinux. There were no differences between the groups in rates of death or clinically relevant bleeding.
As noted above, the newly added recommendation in the Seventh ACCP Conference for extended prophylaxis, for up to 28 to 35 days after surgery, applies to patients undergoing hip fracture surgery as well as those undergoing hip replacement surgery. In the setting of hip fracture repair, extended prophylaxis is a Grade 1A recommendation with the use of fondaparinux and a Grade 1C+ recommendation with the use of either LMWH or adjusted-dose warfarin.6
Lower extremity fractures and trauma
Although lower extremity fractures are very common, the risk of DVT has been poorly studied in this setting. For patients with isolated lower extremity fractures, the Seventh ACCP Conference recommends that clinicians not use thromboprophylaxis routinely (Grade 2A, indicating an “intermediate-strength recommendation” based on RCTs without important limitations).6
Trauma patients, in contrast, are well recognized as being at very high risk for DVT and PE. The Seventh ACCP Conference gives a Grade 1A recommendation to thromboprophylaxis for all trauma patients who have at least one risk factor for VTE. LMWH is recommended (Grade 1A) as the agent of choice for this purpose, provided there are no contraindications to its use, and should be administered as soon as safely possible. Mechanical modalities are reserved for trauma patients with active bleeding or high risk for hemorrhage (Grade 1B). The guidelines recommend against use of inferior vena cava (IVC) filters as primary thromboprophylaxis in trauma patients (Grade 1C, indicating an “intermediate-strength recommendation” based on observational studies).6
Use of ultrasonography
Duplex ultrasonographic screening is recommended in orthopedic trauma patients who are at high risk for VTE and have received suboptimal or no prophylaxis (Grade 1C). In contrast, the Seventh ACCP Conference recommends against routine use of duplex ultrasonography to screen for VTE at hospital discharge in asymptomatic patients following major orthopedic surgery (Grade 1A).6
Knee arthroscopy
Arthroscopic knee procedures are increasing in frequency and raise the specter of a potential role for thromboprophylaxis. However, the clinical diagnosis of DVT is unreliable, and even diagnosis by ultrasonography is unreliable following knee arthroscopy, as interpreting scans of veins below the knee is challenging in this setting.24
The Seventh ACCP Conference recommends that clinicians not use routine thromboprophylaxis, other than early mobilization, for patients who undergo knee arthroscopy (Grade 2B). However, for arthroscopy patients who have inherent risk factors for VTE or who undergo a prolonged or complicated arthroscopy procedure, thromboprophylaxis with LMWH is suggested (Grade 2B).6
RECOMMENDED APPROACH TO VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
Drawing on the ACCP guidelines and the evidence reviewed above, we have outlined our evidence-based recommendations for pharmacologic VTE prophylaxis in patients undergoing orthopedic surgery, as presented in Table 1. All patients undergoing major orthopedic surgical procedures (ie, procedures other than arthroscopy) should routinely receive anticoagulant prophylaxis unless they have contraindications to anticoagulation. Recommended agents and their duration of use vary according to the type of surgery, as detailed in Table 1.
Extended-duration prophylaxis is recommended for patients undergoing total hip replacement and hip fracture surgery. Aspirin is not recommended as the sole agent for prophylaxis in any orthopedic surgery setting.
Importance of a postoperative prophylaxis protocol
In addition to these broad pharmacologic recommendations, it is important that a postoperative VTE prophylaxis protocol be in place at all hospitals.
At the Ochsner Medical Center in New Orleans, where one of us (S.B.D.) practices, postoperative orders include antithrombotic therapy for surgical patients, starting with placement of thigh-high antiembolism stockings on both legs on the day of surgery for patients undergoing hip replacement and on postoperative day 1 in those undergoing knee replacement. Plantar pneumatic compression devices are applied to both legs in the recovery room and kept on except when the patient is walking. The hospitalist team dictates further anticoagulation orders. If extended prophylaxis is prescribed, the discharge planner sets up drug delivery and reimbursement, provides a LMWH discharge kit, and teaches the patient to self-inject. If there is concern about increasing swelling at the surgical site while anticoagulant therapy continues, the protocol calls for prompt notification of the responsible physician. To minimize the risk that spinal or epidural hematomas will develop, all agents that increase bleeding propensity should be recognized and ordered accordingly.
SUMMARY
VTE in patients undergoing major orthopedic surgery is a serious health problem that is highly preventable, yet VTE prophylaxis remains underused in this patient population. Despite the availability of practice guidelines for VTE prevention in the orthopedic surgery setting, recommendations are not widely implemented in clinical practice. Recommended prophylactic options differ somewhat among various orthopedic procedures, and the supportive evidence differs for various anticoagulant options.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: The ACCP recommends against the routine use of aspirin as primary prophylaxis against VTE in major orthopedic surgery, yet orthopedic surgeons across the country still continue to use aspirin in this setting. What are your thoughts on this, Dr. McKean?
Dr. McKean: We agree with the ACCP’s recommendation against aspirin as primary VTE prophylaxis in orthopedic patients. The percentage of US knee arthroplasty patients who develop VTE after receiving no prophylaxis at all is roughly 64%; this percentage declines only slightly (to 56%) for knee arthroplasty patients who receive prophylaxis with aspirin.25 Since we clearly want to reduce VTE risk as much as possible, I would not use aspirin alone. I would use it only if the patient were already on aspirin, but then I would add either LMWH or fondaparinux.
Dr. Jaffer: Warfarin is another agent that is widely used for prophylaxis in major orthopedic surgery. In fact, the large registries of VTE prevention in major orthopedic surgery suggest that the use of warfarin may be slightly higher than the use of LMWH. If clinicians choose to use warfarin in their practice, what are your recommendations, Dr. Deitelzweig?
Dr. Deitelzweig: As primary prophylaxis for orthopedic surgery patients, warfarin must be dosed to achieve an INR of 2.0 to 3.0; the need for a value in this range is unequivocal. This is a challenging target to attain in the hospital setting.
Dr. Brotman: A study I was involved with a few years ago suggested that warfarin may be inadequate for VTE prevention in the first few days after orthopedic surgery.26 Orthopedic surgeons at the Cleveland Clinic, where I was practicing at the time, routinely used systematic ultrasonography to assess for thrombosis on postoperative day 2 or 3 following hip or knee arthroplasty, so we conducted a secondary analysis of a case-control study in these ultrasonographically screened arthroplasty patients to assess rates of early VTE and look for any associations with the type of prophylaxis used. We found that there was about a tenfold increase in the risk of VTE, both distal and proximal, on postoperative day 2 or 3 among patients who received warfarin compared with those who received LMWH. We concluded that warfarin’s delayed antithrombotic effects may not provide sufficient VTE prophylaxis in the immediate postoperative setting.26
Dr. Deitelzweig: That’s a good point. Although it’s important to achieve a therapeutic level of warfarin, we now have evidence that it takes some time to achieve that level, and in the interim, bad things can happen to patients.
Dr. Jaffer: Orthopedic surgery encompasses several types of procedures. Dr. Amin, which specific orthopedic surgery patients stand to benefit from extended prophylaxis, and how long should extended prophylaxis last?
Dr. Amin: Major orthopedic surgery comprises hip fracture repair, total hip replacement, and total knee replacement. For hip fracture, there are strong data to support the use of extended prophylaxis with fondaparinux 2.5 mg/day, which showed about an 88% relative reduction in the risk of symptomatic VTE compared with standard-duration fondaparinux (6 to 8 days) followed by matching placebo for the extended phase.27 The total duration of fondaparinux therapy in the extended-duration arm was 4 to 5 weeks.
Likewise, data support extended prophylaxis in hip arthroplasty patients, for whom the recommended duration is also 4 to 5 weeks. The systematic review by Hull et al17 demonstrated a 0.41 relative risk of DVT with extended-duration LMWH prophylaxis versus placebo in hip replacement patients (Figure 1), which was a highly statistically significant result.
In contrast, we do not yet have good data to support extended prophylaxis for patients undergoing total knee replacement, which is a bit surprising. In this setting, prophylaxis is recommended for 7 to 14 days but not beyond that.
Dr. Jaffer: Arthroscopy is probably the most common orthopedic procedure performed in the United States today. Dr. Brotman, what is the role of prophylaxis in patients undergoing arthroscopy?
Dr. Brotman: Minor surgery such as arthroscopy can typically be performed safely without routine prophylaxis, other than having the patient ambulate as soon as possible after the procedure. There may be exceptions to this rule, however. I believe that there is potentially a role for pharmacologic prophylaxis in arthroscopy patients who have major risk factors for VTE, such as a personal history of VTE, or who are not expected to become mobile again in a normal rapid fashion after the operation, but prophylaxis has not been studied systematically in such patients.
Dr. Jaffer: Dr. Spyropoulos, there are several new anticoagulants in the pipeline, specifically agents such as the oral direct factor Xa inhibitors and the direct thrombin inhibitors. What do recent clinical trials suggest with regard to the efficacy of these two drug classes for thromboprophylaxis in major orthopedic surgery?
Dr. Spyropoulos: The agents with the most available data are the oral direct factor Xa inhibitors apixaban and rivaroxaban and the oral direct thrombin inhibitor dabigatran. For prophylaxis in orthopedic surgery populations, phase 2 studies have been completed for apixaban and phase 3 trials have been completed for rivaroxaban and dabigatran.
It appears that the factor Xa inhibitors, apixaban and rivaroxaban, are efficacious in comparison with both adjusted-dose warfarin and LMWH, which is the gold standard for this group of patients.28,29 So these indeed appear to be promising agents. Rivaroxaban has been submitted to European regulatory agencies for approval for the prevention of VTE in patients undergoing major orthopedic surgery, and its developer plans to submit it to the FDA in 2008 for a similar indication in the United States.
The data are more equivocal with dabigatran. There have been several positive phase 3 studies in orthopedic surgery comparing two dabigatran dosing schemes, 150 and 220 mg once daily, with the European regimen of enoxaparin (40 mg once daily),30 but a recent study that compared these doses with the North American enoxaparin regimen (30 mg twice daily) failed to meet the criteria for noninferiority.31 Further clinical trial development is necessary for dabigatran, although in January 2008 the European Medicines Agency recommended its marketing approval for thromboprophylaxis in patients undergoing orthopedic procedures.32
I believe that in the next 3 to 5 years our armamentarium will see the addition of at least one, if not more, of these new agents that offer the promise of oral anticoagulation with highly predictable pharmacokinetics and pharmacodynamics and no need for monitoring.
Nearly half of orthopedic surgery patients do not receive appropriate prophylaxis for venous thromboembolism (VTE), as defined by American College of Chest Physicians (ACCP) consensus guidelines, according to a recent analysis of a nationwide database of hospital admissions.1 Even in teaching hospitals, compliance with consensus guidelines for thromboprophylaxis is suboptimal. In a study of adherence to the ACCP guidelines for VTE prevention among 1,907 surgical patients at 10 teaching hospitals, only 45.2% of hip fracture patients received optimal VTE prophylaxis.2 Rates of optimal prophylaxis were higher among patients undergoing hip arthroplasty and knee arthroplasty—84.3% and 75.9%, respectively—but were still in need of improvement.2
GROWING INTEREST IN POSTOPERATIVE VTE PROPHYLAXIS AS A QUALITY INDICATOR
As noted in the introductory article in this supplement, the Joint Commission on Accreditation of Healthcare Organizations has taken notice of these shortcomings and has proposed national consensus standards for VTE prevention and treatment.3 Among its proposed standards are two related to risk assessment and prophylaxis: whether risk assessment/prophylaxis is ordered within 24 hours of hospital admission and within 24 hours of transfer to the intensive care unit.
Other quality-monitoring initiatives are focused specifically on VTE in the surgical population. The Surgical Care Improvement Project (SCIP) has approved two quality measures with respect to VTE prevention: (1) the proportion of surgical patients for whom recommended VTE prophylaxis is ordered, and (2) the proportion of patients who receive appropriate VTE prophylaxis (based on ACCP guideline recommendations) within 24 hours before or after surgery.4
In the future, two other VTE-related quality measures from SCIP may be implemented by the Centers for Medicare and Medicaid Services: (1) how often intra- or postoperative pulmonary embolism (PE) is diagnosed during the index hospitalization and within 30 days of surgery, and (2) how often intra- or postoperative deep vein thrombosis (DVT) is diagnosed during the index hospitalization and within 30 days of surgery.5
VTE RISK IN ORTHOPEDIC SURGERY
Surgical patients can be stratified into four VTE risk levels—low, moderate, high, and highest—based on age, surgery type, surgery duration, duration of immobilization, and other risk factors.6 For patients undergoing orthopedic surgery, these levels may be defined according to the following patient and surgical characteristics:
- Low risk—surgery duration of less than 30 minutes, age less than 40 years, repair of small fractures
- Moderate risk—age of 40 to 60 years, arthroscopy or repair of lower leg fractures, postoperative plaster cast
- High risk—age greater than 60 years, or age 40 to 60 years with additional VTE risk factors, or immobilization for greater than 4 days
- Highest risk—hip or knee arthroplasty, hip fracture repair, repair of open lower leg fractures, major trauma or spinal cord injury, or multiple risk factors for VTE (age > 40 years, prior VTE, cancer, or hypercoagulable state).
For patients in the low-risk category, no specific prophylaxis is indicated beyond early and aggressive ambulation.6 For those in all other risk categories, prophylaxis with pharmacologic anticoagulant agents and/or mechanical devices is indicated, as reviewed below.
All major orthopedic procedures confer highest risk level
Notably, the “highest risk” category includes any patient undergoing hip or knee arthroplasty or hip fracture repair. Among orthopedic surgery patients in this highest-risk category, rates of VTE events in the absence of prophylaxis are as follows:6
- Calf DVT, 40% to 80%
- Proximal DVT, 10% to 20%
- Clinical PE, 4% to 10%
- Fatal PE, 0.2% to 5%.
Hip replacement poses greater risk than knee replacement
Within this overall highest-risk category, thromboembolic risk in the absence of prophylaxis differs among procedures. Although patients undergoing hip replacement and those undergoing knee replacement have similar rates of DVT of any type,6,7 hip replacement is associated with higher rates of the more clinically important events, specifically proximal DVT and PE. In the absence of prophylaxis, proximal DVT occurs in 23% to 36% of hip replacement patients as opposed to 9% to 20% of knee replacement patients; similarly, PE occurs in 0.7% to 30% of hip replacement patients as compared with 1.8% to 7.0% of knee replacement patients.6,7
What about bleeding risk?
For many orthopedic surgeons, the risk of bleeding as a result of anticoagulant prophylaxis of VTE looms larger than the risk of VTE itself. This is likely because bleeding, when it does occur, is likely to occur more acutely than VTE does and may directly compromise the result of the operation. For this reason, orthopedic surgeons may be more likely to actually witness bleeding events than VTE events (especially fatal PEs) while their patients are still under their care, leading to a misperception of the relative risks of anticoagulation-related bleeding and thromboembolism.
In reality, rates of major bleeding with pharmacologic prophylaxis of VTE are a tiny fraction of the above-listed rates of VTE events in the absence of prophylaxis in patients undergoing major orthopedic surgery. Reported 30-day rates of major bleeding in patients receiving VTE prophylaxis with heparins range from 0.2% to 1.7%; these rates barely differ from the rates among placebo recipients in the same VTE prophylaxis trials, which range from 0.2% to 1.5%.8,9 Additionally, within the continuum of risk of major bleeding from various medical interventions, VTE prophylaxis with heparins is one of the lowest-risk interventions, posing far less risk than, for example, the use of warfarin in ischemic stroke patients or in patients older than 75 years.
PHARMACOLOGIC OPTIONS FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
As reviewed in the introductory article of this supplement, the arsenal of anticoagulants for use in VTE prophylaxis includes low-dose unfractionated heparin (UFH), low-molecular-weight heparin (LMWH) agents such as dalteparin and enoxaparin, and the factor Xa inhibitor fondaparinux. A few additional comments about these and other anticoagulant options is warranted in the specific context of orthopedic surgery.
Fondaparinux. Because most of its formal US indications are for use as VTE prophylaxis in major orthopedic surgery—including hip replacement, knee replacement, and hip fracture repair—fondaparinux has been studied more widely in orthopedic surgery patients than in the other populations reviewed earlier in this supplement. Nevertheless, its use even in these settings has remained somewhat limited. This may be because of concerns over possible increased bleeding risk relative to some other anticoagulants. Because of bleeding risk, fondaparinux is contraindicated in patients who weigh less than 50 kg, and its package insert recommends caution when it is used in the elderly due to an increased risk of bleeding in patients aged 65 or older. Additionally, the Pentasaccharide in Major Knee Surgery (PENTAMAKS) study found fondaparinux to be associated with a significantly higher incidence of major bleeding compared with enoxaparin (2.1% vs 0.2%; P = .006) in major knee surgery, although it was superior to enoxaparin in preventing VTE.10 Other possible reasons for slow adoption of fondaparinux include its long half-life, which results in a sustained antithrombotic effect, its lack of easy reversibility, and a contraindication in patients with renal insufficiency.11
Limited role for UFH. Low-dose UFH has a more limited role in orthopedic surgery than in other settings requiring VTE prophylaxis, as current ACCP guidelines for VTE prevention recognize it only as a possible option in hip fracture surgery and state that it is not to be considered as sole prophylaxis in patients undergoing hip or knee replacement.6
Warfarin. Although not indicated for use in other VTE prophylaxis settings, the vitamin K antagonist warfarin is recommended as an option for all three major orthopedic surgery indications—knee replacement, hip replacement, and hip fracture repair.6
The key to effective prophylaxis with warfarin is achieving the appropriate intensity of anticoagulation. In two separate analyses, Hylek et al demonstrated a balance between safety and efficacy with warfarin therapy targeted to an international normalized ratio (INR) of 2.0 to 3.0.12,13 An INR greater than 4.0 greatly increased the risk of intracranial hemorrhage, whereas thrombosis was not effectively prevented with an INR less than 2.0.12,13 This latter point should be stressed to orthopedic surgeons, who sometimes aim for INR values below 2.0.
Although anticoagulation clinics are superior to usual care at maintaining the INR within the window of 2.0 to 3.0, only about one-third of patients nationally who take warfarin receive care in such clinics.14 Even with optimal care in anticoagulation clinics, some patients will still receive subtherapeutic or supertherapeutic levels of warfarin, which is one of this agent’s limitations.
Aspirin not recommended as sole agent. Although aspirin is still used as thromboprophylaxis in orthopedic surgery patients, current ACCP guidelines recommend against its use as the sole means of VTE prophylaxis in any patient group.6 The limitations of the evidence for aspirin in this setting are illustrated by the Pulmonary Embolism Prevention study, a multicenter randomized trial in patients undergoing hip fracture (n = 13,356) or hip/knee replacement (n = 4,088).15 Patients received aspirin 160 mg/day or placebo for 5 weeks, starting preoperatively, and were evaluated for outcomes at day 35. Among the hip fracture patients, the rate of symptomatic DVT was lower in the aspirin group than in the placebo group (1.0% vs 1.5%; P = .03), as was the rate of PE (0.7% vs 1.2%, respectively; P = .002), but there was no significant difference in outcomes between the groups among the patients undergoing hip or knee replacement. Notably, 40% of patients in the study also received UFH or LMWH. Further confounding the results, some patients received nonpharmacologic VTE prophylaxis modalities, and others received nonsteroidal anti-inflammatory drugs other than aspirin.
Heparin-induced thrombocytopenia. As noted earlier in this supplement, the incidence of heparin-induced thrombocytopenia (HIT) is markedly higher in patients who receive UFH than in those who receive LMWH. This difference in frequency, which constitutes about a sixfold to eightfold differential, is due to the relationship between standard heparin and platelet factor IV, which can induce formation of IgG antibodies.16 A 50% or greater reduction in platelet count in heparin recipients should prompt consideration of HIT.
Oral direct thrombin inhibitors. Although the oral direct thrombin inhibitor ximelagatran was rejected for approval by the US Food and Drug Administration (FDA) and recently withdrawn from the market worldwide as a result of hepatic risks, other oral direct thrombin inhibitors are in phase 3 studies for use in orthopedic surgery and may be commercially available options for postoperative VTE prophylaxis before long.
GUIDELINES FOR VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
The ACCP guidelines referred to throughout this article are widely recognized as a practice standard for VTE prevention and treatment, and have been regularly updated throughout recent decades. The most recent version, issued in 2004, is formally known as the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.6 Key orthopedic surgery-related recommendations and notable changes from the previous version of the guidelines, issued in 2001, are outlined below, along with pertinent supportive or illustrative studies.
Hip replacement surgery
In a change from the previous guidelines, the Seventh ACCP Conference recommends extended prophylaxis, for up to 28 to 35 days after surgery, for patients undergoing hip replacement or hip fracture surgery. For hip replacement surgery, this is a Grade 1A recommendation for prophylaxis with either LMWH or warfarin and a Grade 1C+ recommendation (“no RCTs but strong RCT results can be unequivocally extrapolated, or overwhelming evidence from observational studies”) for prophylaxis with fondaparinux.6
Knee replacement surgery
The same three anticoagulant options that received Grade 1A recommendations for patients undergoing total hip replacement—LMWH, fondaparinux, and adjusted-dose warfarin—are also given Grade 1A recommendations as routine thromboprophylaxis in patients undergoing elective knee replacement (see Table 1 for dosing). In addition, optimal use of intermittent pneumatic compression devices is recommended as an alternative option to anticoagulant prophylaxis in these patients (Grade 1B, indicating a “strong recommendation” based on RCTs with important limitations). Use of UFH as the sole agent for prophylaxis is recommended against.6
For both hip and knee replacement surgery, the Seventh ACCP Conference does not endorse superiority of any one of its three recommended prophylaxis options—LMWH, fondaparinux, and adjusted-dose warfarin—over the other two. However, at least four large randomized trials have directly compared LMWH and adjusted-dose warfarin in the setting of arthroplasty—two in total hip replacement surgery19,20 and two in total knee replacement surgery.21,22 Each of these four studies found LMWH to be significantly more effective than warfarin in preventing VTE. In three of the four trials, there was no significant difference between the therapies in rates of major bleeding.19,21,22 In the remaining trial, which was conducted in hip replacement surgery patients and compared postoperative warfarin with dalteparin initiated either immediately before or early after surgery, patients who received preoperative dalteparin initiation (but not those who received postoperative dalteparin initiation) had an increased rate of major bleeding compared with warfarin recipients (P = .01).20
Hip fracture surgery
The supportive evidence for anticoagulant prophylaxis in hip fracture surgery is less robust than that in hip and knee replacement surgery. As a result, only fondaparinux has a Grade 1A recommendation as routine prophylaxis in patients undergoing hip fracture surgery. Options with less definitive recommendations are LMWH (Grade 1C+), low-dose UFH (Grade 1B), and adjusted-dose warfarin (Grade 2B, indicating a “weak recommendation” based on RCTs with important limitations) (see Table 1 for dosing of all agents).6
These differing recommendations are supported by the double-blind Pentasaccharide in Hip Fracture Surgery Study (PENTHIFRA) of 1,711 consecutive patients undergoing surgery for hip fracture repair.23 Patients were randomized to at least 5 days of fondaparinux 2.5 mg once daily, initiated postoperatively, or enoxaparin 40 mg once daily, initiated preoperatively. The incidence of DVT or PE by postoperative day 11 was 8.3% in the fondaparinux arm versus 19.1% in the enoxaparin arm, a statistically significant difference (P < .001) in favor of fondaparinux. There were no differences between the groups in rates of death or clinically relevant bleeding.
As noted above, the newly added recommendation in the Seventh ACCP Conference for extended prophylaxis, for up to 28 to 35 days after surgery, applies to patients undergoing hip fracture surgery as well as those undergoing hip replacement surgery. In the setting of hip fracture repair, extended prophylaxis is a Grade 1A recommendation with the use of fondaparinux and a Grade 1C+ recommendation with the use of either LMWH or adjusted-dose warfarin.6
Lower extremity fractures and trauma
Although lower extremity fractures are very common, the risk of DVT has been poorly studied in this setting. For patients with isolated lower extremity fractures, the Seventh ACCP Conference recommends that clinicians not use thromboprophylaxis routinely (Grade 2A, indicating an “intermediate-strength recommendation” based on RCTs without important limitations).6
Trauma patients, in contrast, are well recognized as being at very high risk for DVT and PE. The Seventh ACCP Conference gives a Grade 1A recommendation to thromboprophylaxis for all trauma patients who have at least one risk factor for VTE. LMWH is recommended (Grade 1A) as the agent of choice for this purpose, provided there are no contraindications to its use, and should be administered as soon as safely possible. Mechanical modalities are reserved for trauma patients with active bleeding or high risk for hemorrhage (Grade 1B). The guidelines recommend against use of inferior vena cava (IVC) filters as primary thromboprophylaxis in trauma patients (Grade 1C, indicating an “intermediate-strength recommendation” based on observational studies).6
Use of ultrasonography
Duplex ultrasonographic screening is recommended in orthopedic trauma patients who are at high risk for VTE and have received suboptimal or no prophylaxis (Grade 1C). In contrast, the Seventh ACCP Conference recommends against routine use of duplex ultrasonography to screen for VTE at hospital discharge in asymptomatic patients following major orthopedic surgery (Grade 1A).6
Knee arthroscopy
Arthroscopic knee procedures are increasing in frequency and raise the specter of a potential role for thromboprophylaxis. However, the clinical diagnosis of DVT is unreliable, and even diagnosis by ultrasonography is unreliable following knee arthroscopy, as interpreting scans of veins below the knee is challenging in this setting.24
The Seventh ACCP Conference recommends that clinicians not use routine thromboprophylaxis, other than early mobilization, for patients who undergo knee arthroscopy (Grade 2B). However, for arthroscopy patients who have inherent risk factors for VTE or who undergo a prolonged or complicated arthroscopy procedure, thromboprophylaxis with LMWH is suggested (Grade 2B).6
RECOMMENDED APPROACH TO VTE PROPHYLAXIS IN ORTHOPEDIC SURGERY
Drawing on the ACCP guidelines and the evidence reviewed above, we have outlined our evidence-based recommendations for pharmacologic VTE prophylaxis in patients undergoing orthopedic surgery, as presented in Table 1. All patients undergoing major orthopedic surgical procedures (ie, procedures other than arthroscopy) should routinely receive anticoagulant prophylaxis unless they have contraindications to anticoagulation. Recommended agents and their duration of use vary according to the type of surgery, as detailed in Table 1.
Extended-duration prophylaxis is recommended for patients undergoing total hip replacement and hip fracture surgery. Aspirin is not recommended as the sole agent for prophylaxis in any orthopedic surgery setting.
Importance of a postoperative prophylaxis protocol
In addition to these broad pharmacologic recommendations, it is important that a postoperative VTE prophylaxis protocol be in place at all hospitals.
At the Ochsner Medical Center in New Orleans, where one of us (S.B.D.) practices, postoperative orders include antithrombotic therapy for surgical patients, starting with placement of thigh-high antiembolism stockings on both legs on the day of surgery for patients undergoing hip replacement and on postoperative day 1 in those undergoing knee replacement. Plantar pneumatic compression devices are applied to both legs in the recovery room and kept on except when the patient is walking. The hospitalist team dictates further anticoagulation orders. If extended prophylaxis is prescribed, the discharge planner sets up drug delivery and reimbursement, provides a LMWH discharge kit, and teaches the patient to self-inject. If there is concern about increasing swelling at the surgical site while anticoagulant therapy continues, the protocol calls for prompt notification of the responsible physician. To minimize the risk that spinal or epidural hematomas will develop, all agents that increase bleeding propensity should be recognized and ordered accordingly.
SUMMARY
VTE in patients undergoing major orthopedic surgery is a serious health problem that is highly preventable, yet VTE prophylaxis remains underused in this patient population. Despite the availability of practice guidelines for VTE prevention in the orthopedic surgery setting, recommendations are not widely implemented in clinical practice. Recommended prophylactic options differ somewhat among various orthopedic procedures, and the supportive evidence differs for various anticoagulant options.
DISCUSSION: ADDITIONAL PERSPECTIVES FROM THE AUTHORS
Dr. Jaffer: The ACCP recommends against the routine use of aspirin as primary prophylaxis against VTE in major orthopedic surgery, yet orthopedic surgeons across the country still continue to use aspirin in this setting. What are your thoughts on this, Dr. McKean?
Dr. McKean: We agree with the ACCP’s recommendation against aspirin as primary VTE prophylaxis in orthopedic patients. The percentage of US knee arthroplasty patients who develop VTE after receiving no prophylaxis at all is roughly 64%; this percentage declines only slightly (to 56%) for knee arthroplasty patients who receive prophylaxis with aspirin.25 Since we clearly want to reduce VTE risk as much as possible, I would not use aspirin alone. I would use it only if the patient were already on aspirin, but then I would add either LMWH or fondaparinux.
Dr. Jaffer: Warfarin is another agent that is widely used for prophylaxis in major orthopedic surgery. In fact, the large registries of VTE prevention in major orthopedic surgery suggest that the use of warfarin may be slightly higher than the use of LMWH. If clinicians choose to use warfarin in their practice, what are your recommendations, Dr. Deitelzweig?
Dr. Deitelzweig: As primary prophylaxis for orthopedic surgery patients, warfarin must be dosed to achieve an INR of 2.0 to 3.0; the need for a value in this range is unequivocal. This is a challenging target to attain in the hospital setting.
Dr. Brotman: A study I was involved with a few years ago suggested that warfarin may be inadequate for VTE prevention in the first few days after orthopedic surgery.26 Orthopedic surgeons at the Cleveland Clinic, where I was practicing at the time, routinely used systematic ultrasonography to assess for thrombosis on postoperative day 2 or 3 following hip or knee arthroplasty, so we conducted a secondary analysis of a case-control study in these ultrasonographically screened arthroplasty patients to assess rates of early VTE and look for any associations with the type of prophylaxis used. We found that there was about a tenfold increase in the risk of VTE, both distal and proximal, on postoperative day 2 or 3 among patients who received warfarin compared with those who received LMWH. We concluded that warfarin’s delayed antithrombotic effects may not provide sufficient VTE prophylaxis in the immediate postoperative setting.26
Dr. Deitelzweig: That’s a good point. Although it’s important to achieve a therapeutic level of warfarin, we now have evidence that it takes some time to achieve that level, and in the interim, bad things can happen to patients.
Dr. Jaffer: Orthopedic surgery encompasses several types of procedures. Dr. Amin, which specific orthopedic surgery patients stand to benefit from extended prophylaxis, and how long should extended prophylaxis last?
Dr. Amin: Major orthopedic surgery comprises hip fracture repair, total hip replacement, and total knee replacement. For hip fracture, there are strong data to support the use of extended prophylaxis with fondaparinux 2.5 mg/day, which showed about an 88% relative reduction in the risk of symptomatic VTE compared with standard-duration fondaparinux (6 to 8 days) followed by matching placebo for the extended phase.27 The total duration of fondaparinux therapy in the extended-duration arm was 4 to 5 weeks.
Likewise, data support extended prophylaxis in hip arthroplasty patients, for whom the recommended duration is also 4 to 5 weeks. The systematic review by Hull et al17 demonstrated a 0.41 relative risk of DVT with extended-duration LMWH prophylaxis versus placebo in hip replacement patients (Figure 1), which was a highly statistically significant result.
In contrast, we do not yet have good data to support extended prophylaxis for patients undergoing total knee replacement, which is a bit surprising. In this setting, prophylaxis is recommended for 7 to 14 days but not beyond that.
Dr. Jaffer: Arthroscopy is probably the most common orthopedic procedure performed in the United States today. Dr. Brotman, what is the role of prophylaxis in patients undergoing arthroscopy?
Dr. Brotman: Minor surgery such as arthroscopy can typically be performed safely without routine prophylaxis, other than having the patient ambulate as soon as possible after the procedure. There may be exceptions to this rule, however. I believe that there is potentially a role for pharmacologic prophylaxis in arthroscopy patients who have major risk factors for VTE, such as a personal history of VTE, or who are not expected to become mobile again in a normal rapid fashion after the operation, but prophylaxis has not been studied systematically in such patients.
Dr. Jaffer: Dr. Spyropoulos, there are several new anticoagulants in the pipeline, specifically agents such as the oral direct factor Xa inhibitors and the direct thrombin inhibitors. What do recent clinical trials suggest with regard to the efficacy of these two drug classes for thromboprophylaxis in major orthopedic surgery?
Dr. Spyropoulos: The agents with the most available data are the oral direct factor Xa inhibitors apixaban and rivaroxaban and the oral direct thrombin inhibitor dabigatran. For prophylaxis in orthopedic surgery populations, phase 2 studies have been completed for apixaban and phase 3 trials have been completed for rivaroxaban and dabigatran.
It appears that the factor Xa inhibitors, apixaban and rivaroxaban, are efficacious in comparison with both adjusted-dose warfarin and LMWH, which is the gold standard for this group of patients.28,29 So these indeed appear to be promising agents. Rivaroxaban has been submitted to European regulatory agencies for approval for the prevention of VTE in patients undergoing major orthopedic surgery, and its developer plans to submit it to the FDA in 2008 for a similar indication in the United States.
The data are more equivocal with dabigatran. There have been several positive phase 3 studies in orthopedic surgery comparing two dabigatran dosing schemes, 150 and 220 mg once daily, with the European regimen of enoxaparin (40 mg once daily),30 but a recent study that compared these doses with the North American enoxaparin regimen (30 mg twice daily) failed to meet the criteria for noninferiority.31 Further clinical trial development is necessary for dabigatran, although in January 2008 the European Medicines Agency recommended its marketing approval for thromboprophylaxis in patients undergoing orthopedic procedures.32
I believe that in the next 3 to 5 years our armamentarium will see the addition of at least one, if not more, of these new agents that offer the promise of oral anticoagulation with highly predictable pharmacokinetics and pharmacodynamics and no need for monitoring.
- Yu HT, Dylan ML, Lin J, Dubois RW. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm 2007; 64:69–76.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 ACCP consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- National Consensus Standards for Prevention and Care of Venous Thromboembolism (VTE). The Joint Commission Web site. http://www.jointcommission.org/PerformanceMeasurement/Perform anceMeasurement/VTE.htm. Accessed January 8, 2008.
- Surgical Care Improvement Project. MedQIC Web site. http://www.medqic.org/scip. Accessed January 8, 2008.
- SCIP process and outcome measures, October 2005. MedQIC Web site. http://www.medqic.org. Accessed January 1, 2007.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty.J Am Acad Orthop Surg 1996; 4:54–62.
- Planes A, Vochelle N, Mazas F, et al. Prevention of postoperative venous thrombosis: a randomized trial comparing unfractionated heparin with low molecular weight heparin in patients undergoing total hip replacement. Thromb Haemost 1988; 60:407–410.
- Colwell CW Jr, Spiro TE, Trowbridge AA, et al. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep venous thrombosis after elective knee arthroplasty. Clin Orthop Relat Res 1995; 321:19–27.
- Bauer KA, Eriksson BI, Lassen MR, Turpie AG. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med 2001; 345:1305–1310.
- Turpie AGG. Pentasaccharide Org31540/SR90107A clinical trials update: lessons for practice. Am Heart J 2001; 142(Suppl):S9–S15.
- Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 1994; 120:897–902.
- Hylek EM, Skates SJ, Sheehan MA, Singer DE. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. N Engl J Med 1996; 335:540–546.
- Samsa GP, Matchar DB, Goldstein LB, et al. Quality of anticoagulation management among patients with atrial fibrillation: review of medical records from 2 communities. Arch Intern Med 2000; 160:967–973.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Warkentin TE. Heparin-induced thrombocytopenia: pathogenesis and management. Br J Haemotol 2003; 121:535–555.
- Hull RD, Pineo GF, Stein PD, et al. Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 2001; 135:858–869.
- Haentjens P, De Groote K, Annemans L. Prolonged enoxaparin therapy to prevent venous thromboembolism after primary hip or knee replacement: a cost-utility analysis. Arch Orthop Trauma Surg 2004; 124:507–517.
- Colwell CW Jr, Collis DK, Paulson R, et al. Comparison of enoxaparin and warfarin for the prevention of venous thromboembolic disease after total hip arthroplasty: evaluation during hospitalization and three months after discharge. J Bone Joint Surg Am 1999; 81:932–940.
- Hull RD, Pineo GF, Francis C, et al. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs warfarin in hip arthroplasty patients: a double-blind, randomized comparison. Arch Intern Med 2000; 160:2199–2207.
- Leclerc JR, Geerts WH, Desjardins L, et al. Prevention of venous thromboembolism after knee arthroplasty: a randomized, double-blind trial comparing enoxaparin with warfarin. Ann Intern Med 1996; 124:619–626.
- Fitzgerald RH Jr, Spiro TE, Trowbridge AA, et al. Prevention of venous thromboembolic disease following primary total knee arthroplasty: a randomized, multicenter, open-label, parallel-group comparison of enoxaparin and warfarin. J Bone Joint Surg Am 2001; 83-A:900–906.
- Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med 2001; 345:1298–1304.
- Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med 1998; 158:47–50.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Brotman DJ, Jaffer AK, Hurbanek JG, Morra N. Warfarin prophylaxis and venous thromboembolism in the first 5 days following hip and knee arthroplasty. Thromb Haemost 2004; 92:1012–1017.
- Eriksson BI, Lassen MR; Pentasaccharide in Hip-Fracture Surgery Plus Investigators. Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med 2003; 163:1337–1342.
- The Botticelli Investigators. Late-breaking clinical trial: a dose-finding study of the oral direct factor Xa inhibitor apixaban in the treatment of patients with acute symptomatic deep vein thrombosis [abstract]. Presented at the 21st Congress of the International Society on Thrombosis and Haemostasis; July 2007; Geneva, Switzerland.
- Fisher WD, Eriksson BI, Bauer KA, et al. Rivaroxaban for thromboprophylaxis after orthopaedic surgery: pooled analysis of two studies. Thromb Haemost 2007; 97:931–937.
- Haas S. New oral Xa and IIa inhibitors: updates on clinical trial results. J Thromb Thrombolysis 2008; 25:52–60.
- Friedman RJ, Caprini JA, Comp PC, et al. Dabigatran etexilate vs enoxaparin in preventing venous thromboembolism following total knee arthroplasty. Presented at: 2007 Congress of the International Society on Thrombosis and Haemostasis; July 7–13, 2007; Geneva, Switzerland.
- Committee for Medicinal Products for Human Use summary of positive opinion for Pradaxa [news release]. London, UK: European Medicines Agency. January 24, 2008. http://www.emea.europa.eu/pdfs/human/ opinion/Pradaxa_3503008en.pdf. Accessed February 21, 2008.
- Goldhaber SZ, Grodstein F, Stampfer MJ. A prospective study of risk factors for pulmonary embolism in women. JAMA 1997; 277:642–645.
- Turpie AGG, Bauer KA, Eriksson BI, Lassen MR, for the Steering Committees of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery. Arch Intern Med 2002; 162:1833–1840.
- Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med 2007; 120:871–879.
- Goldhaber SZ. Diagnosis of acute pulmonary embolism: always be vigilant. Am J Med 2007; 120:827–828.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_ summary.pdf. Accessed December 10, 2007.
- Yu HT, Dylan ML, Lin J, Dubois RW. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm 2007; 64:69–76.
- Stratton MA, Anderson FA, Bussey HI, et al. Prevention of venous thromboembolism: adherence to the 1995 ACCP consensus guidelines for surgical patients. Arch Intern Med 2000; 160:334–340.
- National Consensus Standards for Prevention and Care of Venous Thromboembolism (VTE). The Joint Commission Web site. http://www.jointcommission.org/PerformanceMeasurement/Perform anceMeasurement/VTE.htm. Accessed January 8, 2008.
- Surgical Care Improvement Project. MedQIC Web site. http://www.medqic.org/scip. Accessed January 8, 2008.
- SCIP process and outcome measures, October 2005. MedQIC Web site. http://www.medqic.org. Accessed January 1, 2007.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(3 Suppl):338S–400S.
- Zimlich RH, Fulbright BM, Friedman RJ. Current status of anticoagulation therapy after total hip and total knee arthroplasty.J Am Acad Orthop Surg 1996; 4:54–62.
- Planes A, Vochelle N, Mazas F, et al. Prevention of postoperative venous thrombosis: a randomized trial comparing unfractionated heparin with low molecular weight heparin in patients undergoing total hip replacement. Thromb Haemost 1988; 60:407–410.
- Colwell CW Jr, Spiro TE, Trowbridge AA, et al. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep venous thrombosis after elective knee arthroplasty. Clin Orthop Relat Res 1995; 321:19–27.
- Bauer KA, Eriksson BI, Lassen MR, Turpie AG. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med 2001; 345:1305–1310.
- Turpie AGG. Pentasaccharide Org31540/SR90107A clinical trials update: lessons for practice. Am Heart J 2001; 142(Suppl):S9–S15.
- Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 1994; 120:897–902.
- Hylek EM, Skates SJ, Sheehan MA, Singer DE. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. N Engl J Med 1996; 335:540–546.
- Samsa GP, Matchar DB, Goldstein LB, et al. Quality of anticoagulation management among patients with atrial fibrillation: review of medical records from 2 communities. Arch Intern Med 2000; 160:967–973.
- PEP Trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355:1295–1302.
- Warkentin TE. Heparin-induced thrombocytopenia: pathogenesis and management. Br J Haemotol 2003; 121:535–555.
- Hull RD, Pineo GF, Stein PD, et al. Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 2001; 135:858–869.
- Haentjens P, De Groote K, Annemans L. Prolonged enoxaparin therapy to prevent venous thromboembolism after primary hip or knee replacement: a cost-utility analysis. Arch Orthop Trauma Surg 2004; 124:507–517.
- Colwell CW Jr, Collis DK, Paulson R, et al. Comparison of enoxaparin and warfarin for the prevention of venous thromboembolic disease after total hip arthroplasty: evaluation during hospitalization and three months after discharge. J Bone Joint Surg Am 1999; 81:932–940.
- Hull RD, Pineo GF, Francis C, et al. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs warfarin in hip arthroplasty patients: a double-blind, randomized comparison. Arch Intern Med 2000; 160:2199–2207.
- Leclerc JR, Geerts WH, Desjardins L, et al. Prevention of venous thromboembolism after knee arthroplasty: a randomized, double-blind trial comparing enoxaparin with warfarin. Ann Intern Med 1996; 124:619–626.
- Fitzgerald RH Jr, Spiro TE, Trowbridge AA, et al. Prevention of venous thromboembolic disease following primary total knee arthroplasty: a randomized, multicenter, open-label, parallel-group comparison of enoxaparin and warfarin. J Bone Joint Surg Am 2001; 83-A:900–906.
- Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med 2001; 345:1298–1304.
- Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med 1998; 158:47–50.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001; 119(1 Suppl):132S–175S.
- Brotman DJ, Jaffer AK, Hurbanek JG, Morra N. Warfarin prophylaxis and venous thromboembolism in the first 5 days following hip and knee arthroplasty. Thromb Haemost 2004; 92:1012–1017.
- Eriksson BI, Lassen MR; Pentasaccharide in Hip-Fracture Surgery Plus Investigators. Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery: a multicenter, randomized, placebo-controlled, double-blind study. Arch Intern Med 2003; 163:1337–1342.
- The Botticelli Investigators. Late-breaking clinical trial: a dose-finding study of the oral direct factor Xa inhibitor apixaban in the treatment of patients with acute symptomatic deep vein thrombosis [abstract]. Presented at the 21st Congress of the International Society on Thrombosis and Haemostasis; July 2007; Geneva, Switzerland.
- Fisher WD, Eriksson BI, Bauer KA, et al. Rivaroxaban for thromboprophylaxis after orthopaedic surgery: pooled analysis of two studies. Thromb Haemost 2007; 97:931–937.
- Haas S. New oral Xa and IIa inhibitors: updates on clinical trial results. J Thromb Thrombolysis 2008; 25:52–60.
- Friedman RJ, Caprini JA, Comp PC, et al. Dabigatran etexilate vs enoxaparin in preventing venous thromboembolism following total knee arthroplasty. Presented at: 2007 Congress of the International Society on Thrombosis and Haemostasis; July 7–13, 2007; Geneva, Switzerland.
- Committee for Medicinal Products for Human Use summary of positive opinion for Pradaxa [news release]. London, UK: European Medicines Agency. January 24, 2008. http://www.emea.europa.eu/pdfs/human/ opinion/Pradaxa_3503008en.pdf. Accessed February 21, 2008.
- Goldhaber SZ, Grodstein F, Stampfer MJ. A prospective study of risk factors for pulmonary embolism in women. JAMA 1997; 277:642–645.
- Turpie AGG, Bauer KA, Eriksson BI, Lassen MR, for the Steering Committees of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery. Arch Intern Med 2002; 162:1833–1840.
- Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med 2007; 120:871–879.
- Goldhaber SZ. Diagnosis of acute pulmonary embolism: always be vigilant. Am J Med 2007; 120:827–828.
- American Academy of Orthopaedic Surgeons Clinical Guideline on Prevention of Symptomatic Pulmonary Embolism in Patients Undergoing Total Hip or Knee Arthroplasty: Summary of Recommendations. http://www.aaos.org/Research/guidelines/PE_ summary.pdf. Accessed December 10, 2007.
Hospital‐Acquired Gastrointestinal Bleeding
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
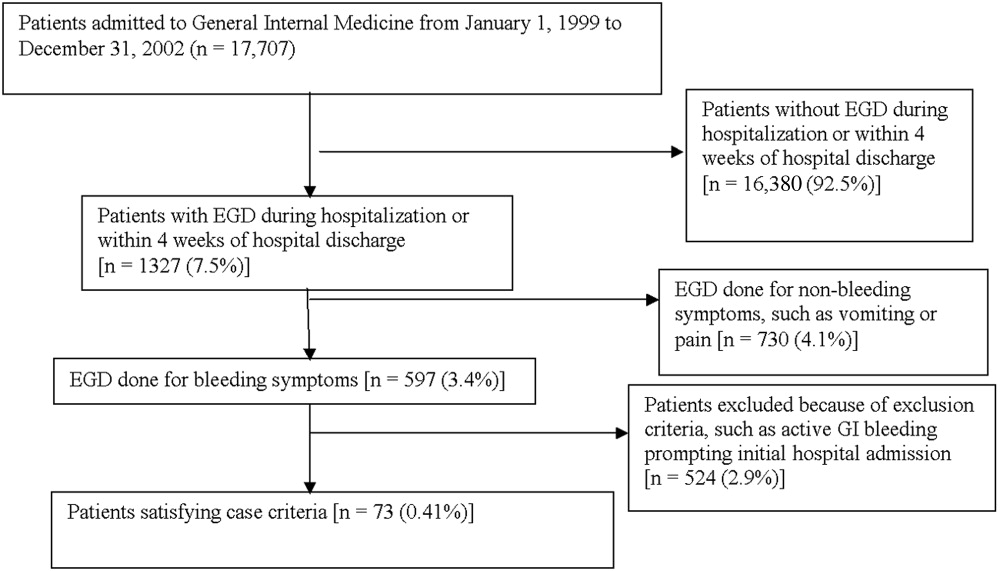
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
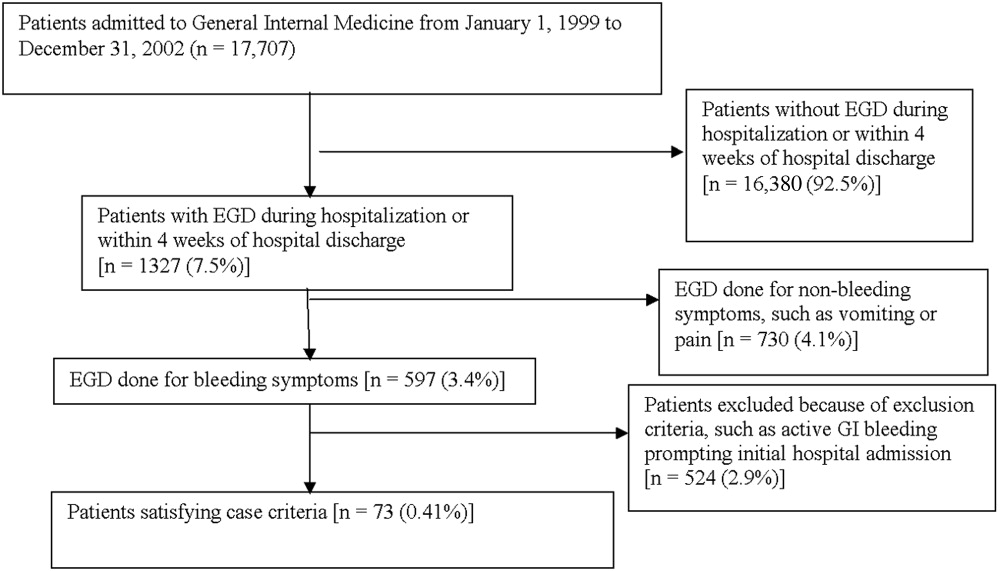
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
Gastrointestinal bleeding occurring in hospitalized patients admitted for nongastrointestinal disorders has been extensively studied in intensive care unit patients. However, a systematic study in noncritically ill medical patients has not yet been done. In critically ill patients the incidence of hospital‐acquired gastrointestinal bleeding (GIB) varies from 0.17% to 5%, depending on its definition.16 These bleeding events significantly increase the morbidity and duration of hospitalization.1, 5, 79
Risk factors for bleeding in the intensive care unit include mechanical ventilation, coagulopathy, burns, chronic renal failure, and neurological insults.15 Several studies have found that stress ulcer prophylaxis with histamine‐2 (H2) receptor antagonists, sucralfate, or proton pump inhibitors (PPIs) decreases bleeding in this group of patients, with a relative risk reduction of 29%61%.10, 11 However, use of these drugs outside this high‐risk group has been questioned because of the low overall risk of bleeding.1, 11, 12 Despite their being an unproven benefit in the noncritically ill population, prophylactic H2 antagonists or PPIs are prescribed in an indiscriminant fashion to up to 30%50% of patients admitted to the hospital,13, 14 suggesting that physician preference dictates this practice. To shed light on this issue in noncritically ill patients, we conducted a retrospective casecontrol study in order to identify risk factors that predict hospital‐acquired gastrointestinal bleeding in this group of patients and to assess whether treatment with prophylactic acid suppression was associated with fewer bleeding events. We also sought to characterize the endoscopic lesions in these patients.
MATERIALS AND METHODS
Study Patients
The institutional review board of the Cleveland Clinic Foundation (Cleveland, OH) approved this study. All patients admitted to the General Internal Medicine service between January 1, 1999, and December 31, 2002, were eligible for inclusion. Two types of cases were included: 1) patients admitted for nongastrointestinal illnesses who developed bleeding at least 24 hours after admission and required esophagogastroduodenoscopy (EGD) during hospitalization (designated in‐hospital bleeding), and 2) patients admitted with gastrointestinal bleeding (requiring EGD) who had been hospitalized on the General Medical service during the preceding 4 weeks for a nongastrointestinal illness (designated out‐of‐hospital bleeding). This second group was included to identify risk factors for delayed bleeding that might not be obvious during hospitalization.
Medical records of all General Medicine patients who underwent EGD were reviewed in a standardized fashion (Fig. 1). We excluded patients with documented gastrointestinal complaints (including bleeding) at the time of the index admission or within 24 hours of admission, bleeding in the intensive care unit (ICU) or in another hospital prior to transfer to the General Medicine service, or a history of gastrointestinal bleeding during the month prior to admission. ICU stay prior to General Medicine admission, if not associated with GI bleeding, was not an exclusion criterion for our study.
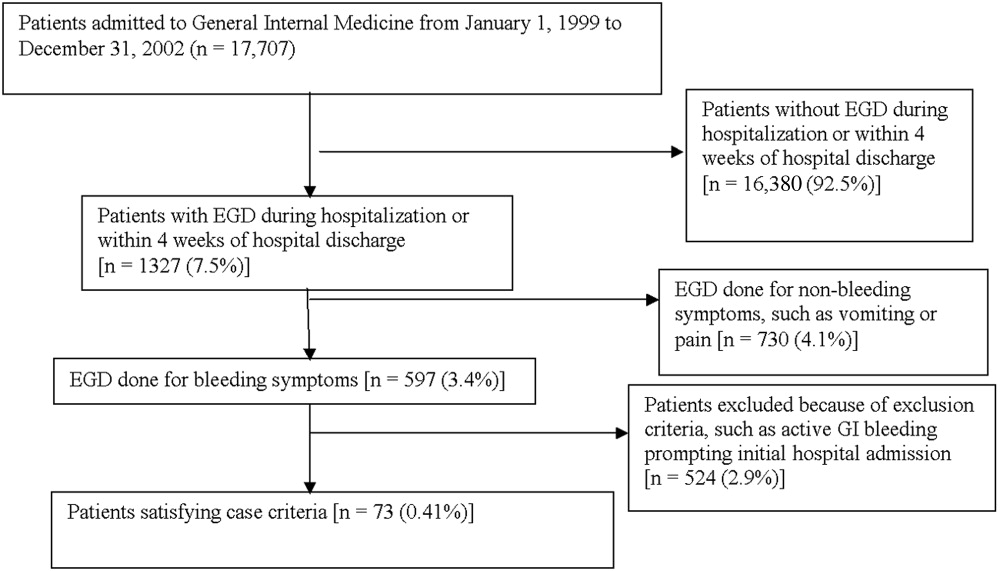
Controls, also without any acute gastrointestinal symptoms at admission, were randomly matched to cases in a 1:1 ratio by date of admission. We used this liberal matching strategy because any factors matched for would no longer be eligible to be risk factors for bleeding. If more than one control was admitted on the same day as a case, then a random number was used to select the control.
Definition of Prophylactic Acid Suppression
We defined prophylactic acid suppression as in‐hospital de novo treatment with histamine‐2 receptor antagonists and/or proton pump inhibitors received prior to the onset of any symptoms that would suggest GI bleeding (for cases) or any time during hospitalization (for controls). Patients taking these drugs prior to admission were deemed ineligible for in‐hospital prophylactic acid blockade and were excluded from the related analyses.
Data Collection
We extracted demographic information, medical history, medication usage, and laboratory data by chart review. For those patients readmitted for gastrointestinal bleeding following discharge, data from the initial (nongastrointestinal illnessassociated) hospitalization were recorded. Bleeding symptoms triggering endoscopy were grouped into four categories: 1) melena or hematochezia; 2) hematemesis (frank blood in vomitus or coffee‐grounds emesis); 3) melena or hematochezia plus hematemesis (both 1 and 2); 4) stool positivity for occult blood or unexplained drop in hemoglobin in the absence of overt bleeding. Endoscopic findings were categorized by the nature of the visualized lesions, and if multiple lesions were noted, the endoscopist's impression of the most likely bleeding site was used to define the source of bleeding. We recorded colonoscopy findings for patients undergoing this evaluation.
Statistical Analysis
We analyzed data utilizing JMP 5.1 (SAS Institute, Cary, NC). Random controls were chosen using computer‐generated random numbers. The proportions of patients with various categorical characteristics were compared using the chi‐square test or Fisher's exact test as appropriate. We used the Student t test or Wilcoxon's test to compare continuous variables. Odds ratios and adjusted odds ratios were calculated by logistic regression. Two‐tailed P values less than .05 were considered statistically significant.
RESULTS: Identification of Cases and Controls
Of 17,707 patients admitted to the General Medicine service, 1327 (7.5%) underwent EGD during hospitalization or within 1 month of discharge. Only 73 (0.41%) of the total number of patients met the case definition (Fig. 1). Of these cases, 62 (84.9%) had developed gastrointestinal bleeding during the index hospitalization, whereas 11 (15.1%) were readmitted for bleeding within 4 weeks of hospital discharge. The remaining 1254 patients who underwent EGD were excluded based on exclusion criteria, including an absence of documented bleeding prompting the EGD.
Clinical Risk Factors for Bleeding
In univariate analysis, as shown in Table 1, predictors of GIB included: 1) age (P = .02); 2) admission diagnosis (P = .01); 3) preexisting coronary artery disease (P = .004); 4) treatment with blood‐thinning medications, including warfarin (P = .0004), intravenous heparin (P = .0003), and clopidogrel (P = .02); and 5) treatment with PPIs (P = .02). After adjusting for the use of full‐dose anticoagulation and/or clopidogrel, the only of these risk factors that remained significantly associated with GIB was treatment with PPIs prior to hospitalization (adjusted OR = 2.1; 95% CI 1.17.0; P = .04), suggesting that PPI treatment in the outpatient setting may be a marker for GI vulnerability.
| Characteristic | Cases n = 73 | Controls n = 73 | Unadjusted | Adjusted for treatment with full‐dose anticoagulants or clopidogrel | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value (2‐tailed) | Odds ratio (95% CI) | P value (2‐tailed) | |||
| ||||||
| Demographics | ||||||
| Women | 36 (49.3%) | 29 (39.7%) | 1.5 (0.82.9) | .24 | 1.6 (0.83.3) | .19 |
| Age (years), mean (SD) | 71.6 (13.7) | 65.7 (17.2) | 1.5 (1.12.1)c | .02 | 1.3 (0.91.8) | .19 |
| Caucasian | 42 (58.3%) | 32 (44.4%) | 1.7 (0.93.4) | .09 | 1.3 (0.62.6) | .50 |
| Nursing home residents | 5 (6.9%) | 5 (6.9%) | 1.0 (0.33.7) | >.99 | 0.5 (0.12.2) | .35 |
| Admission diagnosisa | .01d | .30d | ||||
| Cardiovascular (non‐thrombotic) | 15 (20.5%) | 6 (8.2%) | 2.9 (1.18.5) | .04 | 2.1 (0.76.5) | .19 |
| Arterial or venous thrombosis | 13 (17.8%) | 2 (2.7%) | 7.9 (2.050.4) | .009 | 3.3 (0.822.1) | .15 |
| Infection | 21 (28.8%) | 24 (32.9%) | 0.8 (0.41.7) | .59 | 1.1 (0.52.3) | .86 |
| Pulmonary (noninfectious) | 4 (5.5%) | 10 (13.7%) | 0.4 (0.11.2) | .10 | 0.5 (0.11.7) | .31 |
| Altered level of consciousness | 7 (9.6%) | 10 (13.7%) | 0.7 (0.21.8) | .44 | 0.7 (0.22.2) | .59 |
| Other | 13 (17.8%) | 21 (28.8%) | 0.5 (0.21.2) | .12 | 0.6 (0.31.5) | .29 |
| Baseline medical conditions | ||||||
| Diabetes mellitus | 28 (38.4%) | 25 (34.3%) | 1.2 (0.62.4) | .61 | 1.3 (0.62.7) | .48 |
| Hypertension | 50 (68.5%) | 48 (65.8%) | 1.1 (0.62.3) | .72 | 1.2 (0.52.5) | .71 |
| Coronary artery disease | 36 (49.3%) | 19 (26.0%) | 2.8 (1.45.6) | .004 | 2.0 (1.04.3) | .06 |
| Atrial fibrillation | 18 (24.7%) | 10 (13.7%) | 2.1 (0.95.0) | .09 | 1.4 (0.53.6) | .49 |
| Congestive heart failure | 25 (34.3%) | 16 (21.9%) | 1.9 (0.93.9) | .10 | 1.5 (0.73.3) | .35 |
| Renal insufficiency (creatinine > 2) | 18 (24.7%) | 11 (15.1%) | 1.8 (0.84.4) | .14 | 1.9 (0.84.7) | .33 |
| Chronic obstructive pulmonary disease | 21 (28.8%) | 20 (27.4%) | 1.1 (0.52.2) | .85 | 1.5 (0.73.4) | .29 |
| Stroke | 13 (17.8%) | 16 (21.9%) | 0.8 (0.31.7) | .53 | 0.7 (0.31.6) | .39 |
| Active malignancy | 6 (8.2%) | 8 (11.0%) | 0.7 (0.32.2) | .57 | 1.0 (0.33.5) | .80 |
| Gastroesophageal reflux (GERD) | 10 (13.7%) | 10 (13.7%) | 1.0 (0.42.6) | >.99 | 1.0 (0.32.7) | .92 |
| Liver disease | 7 (9.6%) | 6 (8.2%) | 1.2 (0.43.9) | .77 | 1.4 (0.44.9) | .59 |
| Peptic ulcer disease | 13 (17.8%) | 5 (6.9%) | 2.9 (1.09.6) | .04 | 2.7 (0.99.4) | .09 |
| Colonic disease (diverticulosis, polyp, or AVM) | 7 (9.6%) | 4 (5.5%) | 1.8 (0.57.3) | .34 | 1.2 (0.35.2) | .79 |
| Prior gastrointestinal hemorrhage | 15 (20.1%) | 7 (9.6%) | 2.4 (1.06.8) | .06 | 2.0 (0.75.8) | .20 |
| Tobacco abuse (current smoking) | 9 (12.3%) | 18 (24.7%) | 0.4 (0.21.0) | .05 | 0.6 (0.21.5) | .26 |
| Heavy drinking (>8 drinks/day) | 2 (2.7%) | 2 (2.7%) | 1.0 (0.18.5) | >.99 | 1.3 (0.111.7) | .83 |
| Medication exposure prior to bleeding (excluding acid blockade)b | ||||||
| Aspirin (with or without NSAID) | 34 (46.6%) | 32 (43.8%) | 1.1 (0.62.1) | .74 | 0.7 (0.31.5) | .42 |
| Nonselective NSAID (without aspirin) | 3 (4.1%) | 5 (6.9%) | 0.6 (0.12.5) | .72 | 0.6 (0.12.6) | .44 |
| COX‐2 inhibitors | 3 (4.1%) | 7 (9.6%) | 0.4 (0.11.5) | .18 | 0.3 (0.11.4) | .15 |
| Glucocorticoids | 17 (23.3%) | 20 (27.4%) | 0.8 (0.41.7) | .57 | 0.9 (0.42.1) | .89 |
| Warfarin | 24 (32.9%) | 7 (9.6%) | 4.6 (1.912.4) | .004 | N/A | N/A |
| Unfractionated heparin, UFH (full‐dose intravenous | 23 (31.5%) | 6 (20.7%) | 5.1 (2.114.8) | .0003 | N/A | N/A |
| Full‐dose low‐molecular‐weight heparin (LMWH) | 2 (2.7%) | 0 (0%) | infinity | .50 | N/A | N/A |
| Clopidogrel | 9 (12.3%) | 2 (2.7%) | 5.0 (1.233.5) | .02 | N/A | N/A |
| Prophylactic LMWH or UFH (among 103 patients not on full‐dose anticoagulants) | 19 (47.5%) | 32 (50.8%) | 0.9 (0.41.9) | .74 | N/A | N/A |
| Any treatment with warfarin, full‐dose UFH, full‐ dose LMWH, and/or clopidogrel | 41 (56.2%) | 14 (19.2%) | 5.4 (2.611.7) | <.0001 | N/A | N/A |
| Gastric acid suppression (prior to any gastrointestinal hemorrhage) | ||||||
| H2‐receptor antagonists (H2RA) (total) | 11 (15.1%) | 19 (26.0%) | 0.5 (0.21.1) | .10 | 0.6 (0.31.5) | .31 |
| Taken prior to admission | 6 (8.2%) | 9 (12.3%) | 0.6 (0.21.9) | .41 | 0.6 (0.22.1) | .47 |
| Started de novo at admission | 5 (6.9%) | 10 (13.7%) | 0.5 (0.11.4) | .17 | 0.7 (0.22.2) | .53 |
| Proton‐pump inhibitor (PPI) (total) | 28 (38.6%) | 16 (21.9%) | 2.2 (1.14.7) | .03 | 2.1 (1.04.6) | .07 |
| Taken prior to admission | 20 (27.4%) | 9 (12.3%) | 2.2 (1.14.7) | .02 | 2.7 (1.17.0) | .04 |
| Started de novo at admission | 8 (11.0%) | 7 (9.6%) | 1.2 (0.43.5) | .79 | 1.0 (0.33.2) | .99 |
| Any treatment with PPI or H2RA prior to hemorrhage (total) | 39 (53.4%) | 33 (45.2%) | 1.4 (0.72.7) | .32 | 1.5 (0.73.0) | .28 |
| Taken prior to admission | 26 (35.6%) | 18 (24.7%) | 1.7 (0.83.5) | .15 | 1.7 (0.83.7) | .18 |
| Started de novo at admission (among the 102 patients not taking prior to admission) | 13 (27.7%) | 15 (27.3%) | 1.0 (0.42.4) | .97 | 1.1 (0.42.9) | .80 |
Among patients on warfarin, the peak international normalized ratio (median [IQR]) was 3.0 (1.25.0) for cases and 1.9 (1.64.8) for controls (P = .52). For those on heparin (23 cases and 6 controls), the median peak activated partial thromboplastin time (aPTT) was 67 (5082) and 128 (67180) seconds for cases and controls, respectively (P = .03), a surprising finding that was likely a result of type III error and small sample size.
Outcomes
We found no evidence of major complications from bleeding, as shown in Table 2. As expected, cases were more likely to receive blood transfusions than were controls, but clinically serious outcomes were uncommon in both groups.
| Characteristic | Cases n = 73 | Controls n = 73 | P value |
|---|---|---|---|
| |||
| Pulmonary complicationsa | 4 ( 5.5%) | 2 (2.7%) | .68 |
| Cardiac complicationsb | 4 ( 5.5%) | 3 (4.1%) | >.99 |
| Acute renal failure requiring dialysis | 0 ( 0.0%) | 1 (1.4%) | >.99 |
| Stroke or transient cerebral ischemia | 1 ( 1.4%) | 1 (1.4%) | >.99 |
| Transfer to intensive care unit | 9 (12.3%) | 4 (5.5%) | .14 |
| Blood transfusion required | 46 (63.0%) | 3 (4.1%) | <.0001 |
| All‐cause mortality | 3 ( 4.1%) | 2 (2.7%) | >.99 |
Gastrointestinal Symptoms and Endoscopic Findings
Bleeding symptoms prompting EGD and associated endoscopic findings are shown in Table 3. Findings on colonoscopy (performed in 34 patients) are included. Overall, 54 (74%) patients had a detected abnormality on EGD and/or colonoscopy that was believed to be a likely source of bleeding by the endoscopist, and 19 (26%) had no apparent culprit lesions. Melena and stool positivity for occult blood were the most common manifestations of gastrointestinal bleeding (77%) and also accounted for all the normal endoscopic evaluations. Of the 21 ulcers, 18 (85.7%) had a clean base, 1 (4.8%) had a red spot, and 2 (9.5%) had an adherent clot. None had a bleeding vessel. Endoscopic treatment was performed in one patient and angiography in one patient. A possible gastric stromal tumor (not the source of bleeding) was seen in one patient, but no mucosal malignant lesions were identified. Of the 73 cases, 41 (56.2% of cases and 0.2% of the total cohort of 17,707 patients) had culprit lesions that might have been preventable with gastric acid suppression (including peptic ulcers, esophagitis, and duodenitis).
| Most likely primary source of bleeding based on EGD with or without colonoscopya | Hematemesis only n = 10 (13.7% of cases) | Melena or hematochezia n = 33 (45.2% of cases) | Hematemesis plus either melena or hematochezia n = 4 (5.5% of cases) | Occult blood (+) and/or drop in hemoglobin (without overt bleeding) n = 26 (35.6% of cases) |
|---|---|---|---|---|
| ||||
| Normal (no lesions identified n = 19 (26.0% of cases) | 0 | 12 | 0 | 7 |
| Peptic ulcer n = 21 (28.8% of cases) | 4 | 10 | 0 | 7 |
| Esophagitis n = 8 (11.0% of cases) | 2 | 2 | 2 | 2 |
| Gastritis or duodenitis n = 12 (16.4% of cases) | 1 | 6 | 1 | 4 |
| Lower GI source only n = 1 (1.4% of cases) | 0 | 0 | 0 | 1 |
| Miscellaneous upper GI sourceb n = 12 (16.4% of cases) | 3 | 3 | 1 | 5 |
Prophylactic Gastric Acid Suppression
One hundred and two patients were not taking any acid‐suppressive prophylaxis on admission to the hospital. Of these patients, on admission 28 (27.5%) were prescribed either histamine‐2 receptor antagonists or proton pump inhibitors. We identified no clinical features associated with the prescriptions for these medications (Table 4), suggesting that physician preference, rather than perceived risk factors for bleeding, determined which patients received prophylactic acid blockade. There was no association between this prophylaxis and GI bleeding, but because of the small size of our sample, the confidence interval was wide (OR = 1.0; 95% CI 0.42.4; P = .97). In the analysis of the subgroup of patients receiving anticoagulation or clopidogrel, prophylaxis showed a nonsignificant trend toward benefit (OR = 0.71; 95% CI 0.23.9; P = .67). There was no significant interaction between the presence of anticoagulation or clopidogrel and prophylaxis (P = .61). Similarly, when we excluded those without prior GI bleeding from analysis, there was still no apparent protective effect of acid‐suppressive prophylaxis (OR = 1.0; 95% CI 0.42.5; P = .97). Finally, there was no significant association between the use of prophylaxis and lesions (theoretically) preventable by acid blockade (OR = 0.9; 95% CI 0.32.3; P = .84).
| Characteristic | Prophylaxis | |||
|---|---|---|---|---|
| Initiated n = 28 (27.5%) | Withheld n = 74 (72.5%) | Odds ratio (95% CI) | P value | |
| ||||
| Cases | ||||
| All lesions | 13 (46.4%) | 34 (46.0%) | 1.0 (0.42.4) | .97 |
| Lesions preventable with acid blockadeb | 8 (28.6%) | 20 (27.0%) | 1.1 (0.42.8) | .88 |
| Demographics | ||||
| Age, in years (SD) | 70.3 (18.6) | 66.9 (15.7) | 1.2 (0.81.9) | .40 |
| Female | 10 (35.7%) | 36 (48.7%) | 0.6 (0.21.4) | .24 |
| Medical history | ||||
| Prior gastrointestinal bleeding | 4 (14.3%) | 7 ( 9.5%) | 1.6 (0.45.8) | .49 |
| History of GERD | 1 ( 3.6%) | 4 ( 5.4%) | 0.6 (0.04.6) | >.99 |
| History of peptic ulcer disease | 3 (10.7%) | 5 ( 6.8%) | 1.7 (0.37.3) | .68 |
| Hospitalization variables | ||||
| Transferred from ICU | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Cardiovascular admission diagnosis | 7 (25.0%) | 21 (28.4%) | 0.8 (0.32.2) | .73 |
| Medication exposure | ||||
| Aspirin (with or without NSAID) | 13 (46.4%) | 30 (40.5%) | 1.3 (0.53.1) | .59 |
| NSAID alone (nonselective) | 2 ( 7.1%) | 4 ( 5.4%) | 1.3 (0.27.3) | .67 |
| Glucocorticoids | 6 (21.4%) | 19 (25.7%) | 0.8 (0.32.2) | .65 |
| Warfarin, clopidogrel, or IV heparin | 9 (32.1%) | 28 (37.8%) | 0.8 (0.31.9) | .59 |
DISCUSSION
Our data suggest that the incidence of hospital‐acquired gastrointestinal bleeding in noncritically ill medical patients is low (approximately 0.4%) and that treatment with anticoagulants or clopidogrel predisposes to this complication. Anticoagulation is a well‐known risk factor for gastrointestinal bleeding, with an estimated odds ratio of 2416; our study confirmed this risk.
Although some studies have questioned the utility of prophylactic acid blockade in the intensive care unit,15 the weight of current evidence supports prophylaxis in selected critically ill patients. In a randomized double‐blind study of 1200 mechanically ventilated patients, the relative risk of gastrointestinal bleeding in patients treated with ranitidine was 0.44 (95% CI 0.210.92 P = .02).11 Many experts discourage indiscriminant use of prophylaxes, even by patients in intensive care units, recommending that it be used only in patients with established risk factors for bleeding.1, 12
Despite the absence of evidence of any benefit of the use of prophylactic acid blockade outside the intensive care unit, this practice is common. In our study, 27.5% of patients who were not on outpatient acid suppression medications (PPIs or H2 antagonists) were started on them on admission to the hospital, presumably as prophylaxes, as we excluded patients admitted for acute gastrointestinal complaints. Other studies have reported prophylaxis rates of 30%50%.13, 14 Many patients started on this prophylaxis during hospitalization go on to take these drugs following discharge, creating an unnecessary economic burden.13, 14 In our study, GI prophylaxis did not appear to prevent hospital‐acquired gastrointestinal bleeding. However, the odds ratio associating the use of prophylactic acid suppression with gastrointestinal bleeding (1.0) was associated with a wide 95% confidence interval (0.42.4), so we cannot exclude the possibility that these medications might provide a relative risk reduction that we were unable to detect. Finally, although gastrointestinal bleeding in the intensive care unit is associated with significant morbidity and mortality,8, 9 we found no evidence to suggest that gastrointestinal bleeding in our patients was associated with poor outcomes.
In interpreting the data from this study, it is important to note that the definition of hospital‐acquired gastrointestinal bleeding in the literature has been inconsistent. Some studies have required that bleeding be hemodynamically significant1, 2, 5, 11a stringent criterion that may be present in only 10%15% of patients with bleeding16whereas other studies defined gastrointestinal bleeding on the basis of occult‐blood‐positive nasogastric aspirates or positive endoscopic findings.7, 15 Because the definition used in the present study required a hard clinical event (EGD), it excluded bleeding events that were considered clinically insignificant by treating physicians. We justified this definition on our belief that any bleeding that warrants invasive evaluation is clinically relevant because it is expensive and puts the patient at some physical risk. Even though some of our patients were diagnosed with GIB without obvious melena or hematemesis (ie, based on stool positivity for occult blood), many of these patients had significant drops in hemoglobin during hospitalization, which, accompanied by occult blood positivity, justified inpatient EGD. We do not believe our definition of GI bleeding was too restrictive, at least for our institution, as physicians at the Cleveland Clinic generally pursue inpatient EGD with clinically apparent gastrointestinal bleeding; we maintain that bleeding that is minor enough not to change management is of limited clinical relevance. Nevertheless, the threshold for EGD at a given institution could affect the rate of EGD for soft indications and the overall prevalence of nosocomial GI bleeding based on our definition.
It also is worth noting that our definition of nosocomial bleeding encompassed some patients with recent hospitalization on the medical service who bled following discharge (15% of cases in this study). This inclusion criterion was chosen because of our concern that the stress of hospitalization might lead to complications even after discharge. We chose an arbitrary postdischarge cutoff of 4 weeks. When we excluded these patients from analysis, the results were similar (data not shown). Although it is possible that we missed some patient who presented to other institutions with GI bleeding following discharge from the Cleveland Clinic, we suspect that the number of such patients was very small based on current referral patterns.
We do not have complete information to determine exactly why patients were on acid‐suppressive therapy prior to admission, but the available data suggest that many had gastroesophageal reflux disease (GERD), PUD, or prior GI bleeding. For this reason, we focused the investigation of the potential efficacy of prophylactic initiation of acid blockade among patients who at presentation were not taking these medications, as prior GERD (or undocumented GIB) leading to chronic use of acid blockade may predispose to subsequent GIB. Although we analyzed only those patients who had newly started taking acid‐suppressive medications, we acknowledge that a few of them may have been started on these medications for other reasons, like chest pain or GERD. However, the evidence suggests that an overwhelming number are started on these medications for the sole purpose of GI prophylaxis.13, 14
Our study was limited by its retrospective casecontrol design. However, because of the low prevalence of hospital‐acquired gastrointestinal bleeding outside the critical care unit, a prospective study would have to enroll thousands of patients in order to generate statistically meaningful results.
In summary, hospital‐acquired gastrointestinal bleeding outside the intensive care unit is uncommon, with an incidence of about 0.4% according to our definition of bleeding. We found no evidence that these bleeding episodes are associated with increased mortality or with occult malignancy. Furthermore, we found no evidence that prophylactic gastric acid suppression prevents these events, and only 41 patients (0.2% of the total cohort) had lesions that might be preventable with gastric acid blockade. We discourage the indiscriminant use of prophylactic acid suppressants in general medical patients.
Acknowledgements
The authors thank Donna M. Richey and Betty Lou Harrison for clerical support.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
- ,,, et al.Risk factors for gastrointestinal bleeding in critically ill patients. Canadian Critical Care Trials Group.N Engl J Med.1994;330:377–381.
- ,,, et al.Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.Crit Care Med.1999;27:2812–2817.
- ,,,,.Prospective evaluation of the risk of upper gastrointestinal bleeding after admission to a medical intensive care unit.Am J Med.1984;76:623–630.
- ,,, et al.Risk factors for hospitalized gastrointestinal bleeding among older persons. Cardiovascular Health Study Investigators.J Am Geriatr Soc.2001;49:126–133.
- ,.Gastrointestinal bleeding in the hospitalized patient: a case–control study to assess risk factors, causes, and outcome.Am J Med.1998;104:349–354.
- ,,.Characterization of gastrointestinal bleeding in severely ill hospitalized patients.Crit Care Med.2000;28:46–50.
- ,,,,.Clinically significant gastrointestinal bleeding in critically ill patients in an era of prophylaxis.Am J Gastroenterol.2000;95:2801–2806.
- ,,, et al.The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients.Crit Care.2001;5:368–375.
- ,,,.Risks for developing critical illness with GI hemorrhage.Chest.2000;118:473–478.
- .Stress ulcer prophylaxis: gastrointestinal bleeding and nosocomial pneumonia. Best evidence synthesis.Scand J GastroenterolSuppl.1995;210:48–52.
- ,,, et al.A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. Canadian Critical Care Trials Group.N Engl J Med.1998;338:791–797.
- ,.Stress ulcer: is routine prophylaxis necessary?Am J Gastroenterol.1995;90:708–712.
- ,,, et al.Hospital use of acid‐suppressive medications and its fall‐out on prescribing in general practice: a 1‐month survey.Aliment Pharmacol Ther.2003;17:1503–1506.
- ,,.Overuse of acid‐suppressive therapy in hospitalized patients.Am J Gastroenterol.2000;95:3118–122.
- ,,, et al.Prophylaxis for stress‐related gastric hemorrhage in the medical intensive care unit. A randomized, controlled, single‐blind study.Ann Intern Med.1994;121:568–575.
- .Low incidence of hemodynamic instability in patients with gastrointestinal hemorrhage.South Med J.1996;89:386–390.
Copyright © 2006 Society of Hospital Medicine