User login
Increased Incidence of Patella Baja After Total Knee Arthroplasty Revision for Infection
Patellar height may be important in determining function after total knee arthroplasty (TKA). By altering patellofemoral joint mechanics, patella baja may cause several functional issues after TKA.1-8 Patella baja leads to decreased range of motion (ROM) affecting both extension and flexion.5,8,9 Deep flexion can be restricted in TKA patients with patella baja because of tracking limitations associated with an inferiorly displaced patella. As the knee is brought into flexion, the patella can impinge on the anterior aspect of the tibial polyethylene or the tibial tray—presenting a true block to flexion and potentially altering wear.1,10
Another functional issue with patella baja is loss of strength in the extensor mechanism. The patella serves as a fulcrum for the extensor muscles of the knee. When positioned properly and functioning properly, the patella increases the extensor forces generated. When the patella is positioned in baja, the knee generates decreased extensor mechanism force.6,7 This can result in a lag, with the patient being unable to fully extend the knee. Extension-dependent activities are impaired. Patients with weak extensor function can experience poor function with stair climbing, rising from a chair, and exiting an automobile. The improper function and scarring of the patella can result in increased anterior knee pain and worse functional outcome scores after TKAs.3,9
An abnormally positioned patella can either result from or lead to increased scarring in the knee.9,11 Patellar height is often measured with the Insall-Salvati ratio (ISR), which is the patella tendon length (measurement of the tendon from the tibial tubercle to the inferior pole of the patella) divided by the patellar length (longest measured dimension of the patella) (Figure 1).12 Patella baja is defined as an ISR of less than 0.8. Other indices that reference off the tibial plateau (Blackburne-Peel ratio, Canton-Deschamps ratio) reflect an elevation of the joint line, or pseudobaja, and are unreliable for analysis of patella baja after TKA.13
Postoperative patella baja has been reported in 10% to 34% of primary TKAs.4,7 Inferior positioning of the patella and scarring can cause intraoperative difficulty with exposure and may complicate outcomes.9,13 The exposure scar is often larger in TKA revisions for infection compared with primary TKAs.
We conducted a study to compare the incidence of patella baja in noninfected and infected TKA revisions. We hypothesized that, compared with noninfected knees, infected knees treated with nonarticulating spacers would have a higher incidence of patella baja both before and after surgery secondary to more inflammation, immobilization, and related scarring.
Materials and Methods
We conducted a retrospective case–cohort study of 148 consecutive TKA revisions. All TKA revisions were performed between 2003 and 2009 using a mobile-bearing revision system from a single manufacturer. All surgeries were done at a single institution by the 2 senior surgeons. The surgical approach was a standard medial parapatellar approach without patellar eversion. Our institutional review board approved the study and waived the requirement for informed consent, as this was a retrospective study of existing medical records that posed no more than minimal risk to patients.
To properly evaluate patellar height, orthopedic specialty–trained radiologic technicians obtained preoperative and postoperative weight-bearing radiographs using a standardized lateral radiograph in clinic. Two blinded investigators measured ISR radiographically both before surgery (preexplant for septic revisions) and at latest follow-up (postreplant for septic revisions). Patients with inadequate films and/or patellectomies were excluded, along with patients who had less than 6 months of postoperative follow-up.
Ninety-one patients (101 TKAs) met the study inclusion criteria. Two groups of cases were compared: aseptic revisions (n = 67) and septic revisions (n = 34). Reasons for aseptic revisions included implant loosening (24/67, 35.8%), instability (12/67, 17.9%), pain (12/67, 17.9%), lysis (5/67, 7.5%), stiffness (3/67, 4.5%), and malrotation (2/67, 3.0%). Infection was determined by Musculoskeletal Infection Society criteria, as documented by positive aspirations and/or intraoperative tissue cultures taken at prosthesis explantation, elevated white blood cell count in the aspirate, elevated percentage of polymorphonuclear (PMN) cells in the aspirate, gross purulence, presence of chronic draining sinus, or histologic analysis revealing acute inflammation with more than 5 PMN cells per high power field.14,15
All infected TKAs were treated with 2-stage revisions. The standard of care at our institution through this series was to use a nonarticulating spacer for the treatment of infection. Weight-bearing status varied by extent of bone damage. Six weeks of culture-specific intravenous antibiotics were administered with assistance from an infectious disease consultant. Reimplantation was performed when clinical and laboratory criteria for resolution of infection were met—specifically, when erythrocyte sedimentation rate was less than 30 mm/h, C-reactive protein level was less than 10 mg/L, and aspirates were culture-negative. Mean (range) follow-up was 33.9 (6.2-75.7) months for aseptic revisions and 32.3 (7.5-94.2) months for septic revisions. Radiographic follow-up was performed at each visit, with weight-bearing anteroposterior and posteroanterior views, along with a lateral knee radiograph. At final follow-up, ROM was recorded by the senior attending evaluating the patient.
Categorical variables were statistically analyzed with χ2 tests, and continuous variables were analyzed with Student t test, analysis of variance, and univariate analysis of covariance (ANCOVA). Statistical significance was set at P < .05. Intrarater reliability was measured with the intraclass correlation coefficient (ICC). All statistical analysis was performed with Predictive Analytics SoftWare Statistics Version 20.0 (SPSS, Chicago, Illinois).
Results
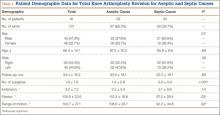
Ninety-one consecutive patients (43 men, 48 women) were included in this study. Mean (SD) age was 66.4 (10.1) years. Mean (SD) preoperative ISR in septic and aseptic cases was 0.94 (0.25) for men and 1.02 (0.23) for women (P = .10). Mean postoperative ISR in septic and aseptic cases was 0.84 (0.27) for men and 0.99 (0.23) for women (P = .004). There was a sex difference between septic and aseptic revisions. There were 22 men and 36 women in the aseptic group and 21 men and 12 women in the septic group (P = .01). Men were more likely than women to have septic revisions and patella baja. Table 1 compares the patient demographics of the 2 patient populations. Mean (SD) number of surgeries, including irrigation and débridement procedures before reimplantation, was larger for septic revisions, 2.9 (0.9), than for aseptic revisions, 1.4 (0.8) (P < .001).
Infection was the most common reason for revision and accounted for 33.7% (34/101) of all revisions. Noninfectious indications, in declining order of frequency, included loosening (23.8%, 24/101), instability (11.9%, 12/101), pain (11.9%, 12/101), osteolysis (5.0%, 5/101), polyethylene wear (5.0%, 5/101), failed unicompartmental knee (4.0%, 4/101), stiffness (3.0%, 3/101), and patellar problems (2.0%, 2/101) (Table 2). ISR decreased significantly only in infected revisions. It is important to note that there was not a high incidence of stiffness or patellofemoral failure in revision patients before surgery.
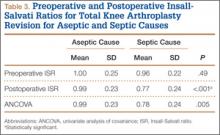
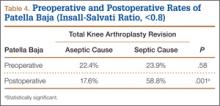
Mean (SD) ISR did not differ between groups before surgery, 1.00 (0.25) for aseptic and 0.96 (0.22) for septic (P = .49), but differed significantly after surgery, 0.99 (0.23) for aseptic and 0.77 (0.24) for septic (P < .001) (Figure 2). The univariate ANCOVA also demonstrated a postoperative difference between groups when taking the preoperative ratio into account: 0.99 (0.23) for aseptic and 0.78 (0.24) for septic (P = .005) (Table 3). Before surgery, 22.4% and 23.9% of the aseptic and septic groups, respectively, had patella baja (P = .58). After surgery, 17.6% and 58.8% of the aseptic and septic groups had patella baja (P = .001) (Table 4). The ICC for preoperative ISR was 0.94, and the ICC for postoperative ISR was 0.96, which indicates excellent agreement of measurements between the 2 blinded investigators.
ROM differed between septic and aseptic groups owing to the difference in postoperative flexion. Mean (SD) postoperative extension was 2.2° (5.4°) for the aseptic group and 5.1° (9.8°) for the septic group—not significantly different (P = .13). Mean (SD) postoperative flexion was 110.2° (18.8°) for the aseptic group and 97.2° (29.4°) for the septic group—significantly different (P = .02). The groups differed significantly (P = .02) in mean (SD) ROM: 108.0° (20.7°) for aseptic and 92.2° (34.6°) for septic (Table 1). ROM was also significantly associated with patella baja (P = .04), as patients with ISR of less than 0.8 had mean (SD) postoperative ROM of 95.1° (31.6°), and patients without patella baja had mean (SD) postoperative ROM of 106.8° (23.6°).
For the septic group, mean (SD) time between first and second stages was 13.0 (8.3) weeks (range, 1-44.3 weeks). Mean (SD) timing of spacer placement was not statistically significantly different (P = .90) between patients who had patella baja, 12.9 (8.8) weeks, and patients who did not have patella baja, 13.2 (7.8) weeks.
Discussion
This study demonstrated that TKAs done for septic reasons resulted in a higher incidence of patella baja and decreased ROM. Incidence of patella baja was higher both before and after revision in septic TKAs than in aseptic TKAs, proving the hypothesis under study. Prerevision incidence was not significantly different, but there was a trend that could not be ignored. This may suggest that there is already an ongoing process in the infected knee that contributes to patella baja; the precise etiology remains unclear and is likely multifactorial. For example, scar formation may be increased in patients with chronic infection, predisposing to patella baja. This assertion is indirectly supported by a recent study from our institution revealing longer average surgical time in septic versus aseptic knee revisions; the difference was thought to reflect increased scar-tissue formation.16 That study also found that patients who underwent septic revisions had significantly more surgical procedures than patients who underwent aseptic revisions. Repetitive surgeries—specifically, repetitive arthrotomies during irrigation and débridement before reimplantation—lead to increased scar formation, which may contribute to preoperative and postoperative patella baja. This may be reflected in the findings that ROM was decreased in patients in the septic group versus patients in the aseptic group and that ROM was decreased in patients with patella baja. In addition, our study found that male patients were more likely to undergo TKA revision for septic reasons and to develop postoperative patella baja. This finding contrasts with that of a study5 that compared preoperative and postoperative ISR in primary TKA and found that women were more likely than men to have patella baja. Although women are more likely to undergo TKA revision,17 men may be more susceptible to infection and subsequent patella baja.
The higher postoperative rate of patella baja in the septic group became statistically significant even when preoperative incidence was considered. This may have been caused by infection-related scarring and by prolonged immobilization of septic knees with use of nonarticulating antibiotic spacers. By keeping these knees immobile with a nonarticulating spacer for a prolonged period in the healing phase of the infection, scar tissue may mature and form over the time between stages. A comparable example may be high tibial osteotomies, in which a high incidence of patella baja has been partly attributed to prolonged casting.11 Future work comparing the results of articulating and nonarticulating spacers will help to determine if immobilization contributes to patella baja in infected TKAs.
There are several limitations to our study. Patient outcome questionnaires were not used, and they would have allowed for the assessment of physical outcomes and emotional satisfaction by comparing outcomes between patients with and without patella baja and comparing septic and aseptic TKAs. In addition, there was no standard method for quantifying difficulty of revision, which would have enabled us to compare difficulty of revision in patients with patella baja.
Conclusion
This study identified a high rate of patella baja and decreased ROM in TKA revisions, particularly infected revisions treated with a nonarticulating spacer. It is important to determine if there are functional consequences. Further investigation is needed regarding the cause, prevention, and management of this potentially debilitating outcome after revision TKA.
1. Aglietti P, Buzzi R, Gaudenzi A. Patello-femoral functional results and complications with the posterior stabilised total condylar knee prosthesis. J Arthroplasty. 1988;3(1):17-25.
2. Fern ED, Winson IG, Getty CJM. Anterior knee pain in rheumatoid patients after total knee replacement: possible selection criteria for patellar resurfacing. J Bone Joint Surg Br. 1992;74(5):745-748.
3. Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Surg Surg Am. 1986;68(7):1035-1040.
4. Floren M, Davis J, Peterson MG, Laskin RS. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patellar baja. J Arthroplasty. 2007;22(6 Suppl 2):51-57.
5. Meneghini RM, Ritter MA, Pierson JL, Meding JB, Berend ME, Faris PM. The effect of the Insall-Salvati ratio on outcome after total knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):116-120.
6. Singerman R, Davy DT, Goldberg VM. Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech. 1994;27(8):1059-1065.
7. Van Eijden TM, Kouwenhoven E, Weijs WA. Mechanics of the patellar articulation: effects of patellar ligament length studied with a mathematical model. Acta Orthop Scand. 1987;58(5):560-566.
8. Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81(5):790-795.
9. Chonko DJ, Lombardi AV Jr, Berend KR. Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int. 2004;12:231-238.
10. Cameron HU, Jung YB. Patella baja complicating total knee arthroplasty. A report of two cases. J Arthroplasty. 1988;3(2):177-180.
11. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71(2):245-248.
12. Insall JN, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104.
13. Grelsamer RP. Patella baja after total knee arthroplasty: is it really patella baja? J Arthroplasty. 2002;17(1):66-69.
14. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
15. Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;26(8):1136-1138.
16. Laudermilch DJ, Fedorka CJ, Heyl A, Rao N, McGough RL. Outcomes of revision total knee arthroplasty after methicillin-resistant Staphylococcus aureus infection. Clin Orthop. 2010;468(8):2067-2073.
17. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop. 2010;468(1):45-51.
Patellar height may be important in determining function after total knee arthroplasty (TKA). By altering patellofemoral joint mechanics, patella baja may cause several functional issues after TKA.1-8 Patella baja leads to decreased range of motion (ROM) affecting both extension and flexion.5,8,9 Deep flexion can be restricted in TKA patients with patella baja because of tracking limitations associated with an inferiorly displaced patella. As the knee is brought into flexion, the patella can impinge on the anterior aspect of the tibial polyethylene or the tibial tray—presenting a true block to flexion and potentially altering wear.1,10
Another functional issue with patella baja is loss of strength in the extensor mechanism. The patella serves as a fulcrum for the extensor muscles of the knee. When positioned properly and functioning properly, the patella increases the extensor forces generated. When the patella is positioned in baja, the knee generates decreased extensor mechanism force.6,7 This can result in a lag, with the patient being unable to fully extend the knee. Extension-dependent activities are impaired. Patients with weak extensor function can experience poor function with stair climbing, rising from a chair, and exiting an automobile. The improper function and scarring of the patella can result in increased anterior knee pain and worse functional outcome scores after TKAs.3,9
An abnormally positioned patella can either result from or lead to increased scarring in the knee.9,11 Patellar height is often measured with the Insall-Salvati ratio (ISR), which is the patella tendon length (measurement of the tendon from the tibial tubercle to the inferior pole of the patella) divided by the patellar length (longest measured dimension of the patella) (Figure 1).12 Patella baja is defined as an ISR of less than 0.8. Other indices that reference off the tibial plateau (Blackburne-Peel ratio, Canton-Deschamps ratio) reflect an elevation of the joint line, or pseudobaja, and are unreliable for analysis of patella baja after TKA.13
Postoperative patella baja has been reported in 10% to 34% of primary TKAs.4,7 Inferior positioning of the patella and scarring can cause intraoperative difficulty with exposure and may complicate outcomes.9,13 The exposure scar is often larger in TKA revisions for infection compared with primary TKAs.
We conducted a study to compare the incidence of patella baja in noninfected and infected TKA revisions. We hypothesized that, compared with noninfected knees, infected knees treated with nonarticulating spacers would have a higher incidence of patella baja both before and after surgery secondary to more inflammation, immobilization, and related scarring.
Materials and Methods
We conducted a retrospective case–cohort study of 148 consecutive TKA revisions. All TKA revisions were performed between 2003 and 2009 using a mobile-bearing revision system from a single manufacturer. All surgeries were done at a single institution by the 2 senior surgeons. The surgical approach was a standard medial parapatellar approach without patellar eversion. Our institutional review board approved the study and waived the requirement for informed consent, as this was a retrospective study of existing medical records that posed no more than minimal risk to patients.
To properly evaluate patellar height, orthopedic specialty–trained radiologic technicians obtained preoperative and postoperative weight-bearing radiographs using a standardized lateral radiograph in clinic. Two blinded investigators measured ISR radiographically both before surgery (preexplant for septic revisions) and at latest follow-up (postreplant for septic revisions). Patients with inadequate films and/or patellectomies were excluded, along with patients who had less than 6 months of postoperative follow-up.
Ninety-one patients (101 TKAs) met the study inclusion criteria. Two groups of cases were compared: aseptic revisions (n = 67) and septic revisions (n = 34). Reasons for aseptic revisions included implant loosening (24/67, 35.8%), instability (12/67, 17.9%), pain (12/67, 17.9%), lysis (5/67, 7.5%), stiffness (3/67, 4.5%), and malrotation (2/67, 3.0%). Infection was determined by Musculoskeletal Infection Society criteria, as documented by positive aspirations and/or intraoperative tissue cultures taken at prosthesis explantation, elevated white blood cell count in the aspirate, elevated percentage of polymorphonuclear (PMN) cells in the aspirate, gross purulence, presence of chronic draining sinus, or histologic analysis revealing acute inflammation with more than 5 PMN cells per high power field.14,15
All infected TKAs were treated with 2-stage revisions. The standard of care at our institution through this series was to use a nonarticulating spacer for the treatment of infection. Weight-bearing status varied by extent of bone damage. Six weeks of culture-specific intravenous antibiotics were administered with assistance from an infectious disease consultant. Reimplantation was performed when clinical and laboratory criteria for resolution of infection were met—specifically, when erythrocyte sedimentation rate was less than 30 mm/h, C-reactive protein level was less than 10 mg/L, and aspirates were culture-negative. Mean (range) follow-up was 33.9 (6.2-75.7) months for aseptic revisions and 32.3 (7.5-94.2) months for septic revisions. Radiographic follow-up was performed at each visit, with weight-bearing anteroposterior and posteroanterior views, along with a lateral knee radiograph. At final follow-up, ROM was recorded by the senior attending evaluating the patient.
Categorical variables were statistically analyzed with χ2 tests, and continuous variables were analyzed with Student t test, analysis of variance, and univariate analysis of covariance (ANCOVA). Statistical significance was set at P < .05. Intrarater reliability was measured with the intraclass correlation coefficient (ICC). All statistical analysis was performed with Predictive Analytics SoftWare Statistics Version 20.0 (SPSS, Chicago, Illinois).
Results
Ninety-one consecutive patients (43 men, 48 women) were included in this study. Mean (SD) age was 66.4 (10.1) years. Mean (SD) preoperative ISR in septic and aseptic cases was 0.94 (0.25) for men and 1.02 (0.23) for women (P = .10). Mean postoperative ISR in septic and aseptic cases was 0.84 (0.27) for men and 0.99 (0.23) for women (P = .004). There was a sex difference between septic and aseptic revisions. There were 22 men and 36 women in the aseptic group and 21 men and 12 women in the septic group (P = .01). Men were more likely than women to have septic revisions and patella baja. Table 1 compares the patient demographics of the 2 patient populations. Mean (SD) number of surgeries, including irrigation and débridement procedures before reimplantation, was larger for septic revisions, 2.9 (0.9), than for aseptic revisions, 1.4 (0.8) (P < .001).
Infection was the most common reason for revision and accounted for 33.7% (34/101) of all revisions. Noninfectious indications, in declining order of frequency, included loosening (23.8%, 24/101), instability (11.9%, 12/101), pain (11.9%, 12/101), osteolysis (5.0%, 5/101), polyethylene wear (5.0%, 5/101), failed unicompartmental knee (4.0%, 4/101), stiffness (3.0%, 3/101), and patellar problems (2.0%, 2/101) (Table 2). ISR decreased significantly only in infected revisions. It is important to note that there was not a high incidence of stiffness or patellofemoral failure in revision patients before surgery.
Mean (SD) ISR did not differ between groups before surgery, 1.00 (0.25) for aseptic and 0.96 (0.22) for septic (P = .49), but differed significantly after surgery, 0.99 (0.23) for aseptic and 0.77 (0.24) for septic (P < .001) (Figure 2). The univariate ANCOVA also demonstrated a postoperative difference between groups when taking the preoperative ratio into account: 0.99 (0.23) for aseptic and 0.78 (0.24) for septic (P = .005) (Table 3). Before surgery, 22.4% and 23.9% of the aseptic and septic groups, respectively, had patella baja (P = .58). After surgery, 17.6% and 58.8% of the aseptic and septic groups had patella baja (P = .001) (Table 4). The ICC for preoperative ISR was 0.94, and the ICC for postoperative ISR was 0.96, which indicates excellent agreement of measurements between the 2 blinded investigators.
ROM differed between septic and aseptic groups owing to the difference in postoperative flexion. Mean (SD) postoperative extension was 2.2° (5.4°) for the aseptic group and 5.1° (9.8°) for the septic group—not significantly different (P = .13). Mean (SD) postoperative flexion was 110.2° (18.8°) for the aseptic group and 97.2° (29.4°) for the septic group—significantly different (P = .02). The groups differed significantly (P = .02) in mean (SD) ROM: 108.0° (20.7°) for aseptic and 92.2° (34.6°) for septic (Table 1). ROM was also significantly associated with patella baja (P = .04), as patients with ISR of less than 0.8 had mean (SD) postoperative ROM of 95.1° (31.6°), and patients without patella baja had mean (SD) postoperative ROM of 106.8° (23.6°).
For the septic group, mean (SD) time between first and second stages was 13.0 (8.3) weeks (range, 1-44.3 weeks). Mean (SD) timing of spacer placement was not statistically significantly different (P = .90) between patients who had patella baja, 12.9 (8.8) weeks, and patients who did not have patella baja, 13.2 (7.8) weeks.
Discussion
This study demonstrated that TKAs done for septic reasons resulted in a higher incidence of patella baja and decreased ROM. Incidence of patella baja was higher both before and after revision in septic TKAs than in aseptic TKAs, proving the hypothesis under study. Prerevision incidence was not significantly different, but there was a trend that could not be ignored. This may suggest that there is already an ongoing process in the infected knee that contributes to patella baja; the precise etiology remains unclear and is likely multifactorial. For example, scar formation may be increased in patients with chronic infection, predisposing to patella baja. This assertion is indirectly supported by a recent study from our institution revealing longer average surgical time in septic versus aseptic knee revisions; the difference was thought to reflect increased scar-tissue formation.16 That study also found that patients who underwent septic revisions had significantly more surgical procedures than patients who underwent aseptic revisions. Repetitive surgeries—specifically, repetitive arthrotomies during irrigation and débridement before reimplantation—lead to increased scar formation, which may contribute to preoperative and postoperative patella baja. This may be reflected in the findings that ROM was decreased in patients in the septic group versus patients in the aseptic group and that ROM was decreased in patients with patella baja. In addition, our study found that male patients were more likely to undergo TKA revision for septic reasons and to develop postoperative patella baja. This finding contrasts with that of a study5 that compared preoperative and postoperative ISR in primary TKA and found that women were more likely than men to have patella baja. Although women are more likely to undergo TKA revision,17 men may be more susceptible to infection and subsequent patella baja.
The higher postoperative rate of patella baja in the septic group became statistically significant even when preoperative incidence was considered. This may have been caused by infection-related scarring and by prolonged immobilization of septic knees with use of nonarticulating antibiotic spacers. By keeping these knees immobile with a nonarticulating spacer for a prolonged period in the healing phase of the infection, scar tissue may mature and form over the time between stages. A comparable example may be high tibial osteotomies, in which a high incidence of patella baja has been partly attributed to prolonged casting.11 Future work comparing the results of articulating and nonarticulating spacers will help to determine if immobilization contributes to patella baja in infected TKAs.
There are several limitations to our study. Patient outcome questionnaires were not used, and they would have allowed for the assessment of physical outcomes and emotional satisfaction by comparing outcomes between patients with and without patella baja and comparing septic and aseptic TKAs. In addition, there was no standard method for quantifying difficulty of revision, which would have enabled us to compare difficulty of revision in patients with patella baja.
Conclusion
This study identified a high rate of patella baja and decreased ROM in TKA revisions, particularly infected revisions treated with a nonarticulating spacer. It is important to determine if there are functional consequences. Further investigation is needed regarding the cause, prevention, and management of this potentially debilitating outcome after revision TKA.
Patellar height may be important in determining function after total knee arthroplasty (TKA). By altering patellofemoral joint mechanics, patella baja may cause several functional issues after TKA.1-8 Patella baja leads to decreased range of motion (ROM) affecting both extension and flexion.5,8,9 Deep flexion can be restricted in TKA patients with patella baja because of tracking limitations associated with an inferiorly displaced patella. As the knee is brought into flexion, the patella can impinge on the anterior aspect of the tibial polyethylene or the tibial tray—presenting a true block to flexion and potentially altering wear.1,10
Another functional issue with patella baja is loss of strength in the extensor mechanism. The patella serves as a fulcrum for the extensor muscles of the knee. When positioned properly and functioning properly, the patella increases the extensor forces generated. When the patella is positioned in baja, the knee generates decreased extensor mechanism force.6,7 This can result in a lag, with the patient being unable to fully extend the knee. Extension-dependent activities are impaired. Patients with weak extensor function can experience poor function with stair climbing, rising from a chair, and exiting an automobile. The improper function and scarring of the patella can result in increased anterior knee pain and worse functional outcome scores after TKAs.3,9
An abnormally positioned patella can either result from or lead to increased scarring in the knee.9,11 Patellar height is often measured with the Insall-Salvati ratio (ISR), which is the patella tendon length (measurement of the tendon from the tibial tubercle to the inferior pole of the patella) divided by the patellar length (longest measured dimension of the patella) (Figure 1).12 Patella baja is defined as an ISR of less than 0.8. Other indices that reference off the tibial plateau (Blackburne-Peel ratio, Canton-Deschamps ratio) reflect an elevation of the joint line, or pseudobaja, and are unreliable for analysis of patella baja after TKA.13
Postoperative patella baja has been reported in 10% to 34% of primary TKAs.4,7 Inferior positioning of the patella and scarring can cause intraoperative difficulty with exposure and may complicate outcomes.9,13 The exposure scar is often larger in TKA revisions for infection compared with primary TKAs.
We conducted a study to compare the incidence of patella baja in noninfected and infected TKA revisions. We hypothesized that, compared with noninfected knees, infected knees treated with nonarticulating spacers would have a higher incidence of patella baja both before and after surgery secondary to more inflammation, immobilization, and related scarring.
Materials and Methods
We conducted a retrospective case–cohort study of 148 consecutive TKA revisions. All TKA revisions were performed between 2003 and 2009 using a mobile-bearing revision system from a single manufacturer. All surgeries were done at a single institution by the 2 senior surgeons. The surgical approach was a standard medial parapatellar approach without patellar eversion. Our institutional review board approved the study and waived the requirement for informed consent, as this was a retrospective study of existing medical records that posed no more than minimal risk to patients.
To properly evaluate patellar height, orthopedic specialty–trained radiologic technicians obtained preoperative and postoperative weight-bearing radiographs using a standardized lateral radiograph in clinic. Two blinded investigators measured ISR radiographically both before surgery (preexplant for septic revisions) and at latest follow-up (postreplant for septic revisions). Patients with inadequate films and/or patellectomies were excluded, along with patients who had less than 6 months of postoperative follow-up.
Ninety-one patients (101 TKAs) met the study inclusion criteria. Two groups of cases were compared: aseptic revisions (n = 67) and septic revisions (n = 34). Reasons for aseptic revisions included implant loosening (24/67, 35.8%), instability (12/67, 17.9%), pain (12/67, 17.9%), lysis (5/67, 7.5%), stiffness (3/67, 4.5%), and malrotation (2/67, 3.0%). Infection was determined by Musculoskeletal Infection Society criteria, as documented by positive aspirations and/or intraoperative tissue cultures taken at prosthesis explantation, elevated white blood cell count in the aspirate, elevated percentage of polymorphonuclear (PMN) cells in the aspirate, gross purulence, presence of chronic draining sinus, or histologic analysis revealing acute inflammation with more than 5 PMN cells per high power field.14,15
All infected TKAs were treated with 2-stage revisions. The standard of care at our institution through this series was to use a nonarticulating spacer for the treatment of infection. Weight-bearing status varied by extent of bone damage. Six weeks of culture-specific intravenous antibiotics were administered with assistance from an infectious disease consultant. Reimplantation was performed when clinical and laboratory criteria for resolution of infection were met—specifically, when erythrocyte sedimentation rate was less than 30 mm/h, C-reactive protein level was less than 10 mg/L, and aspirates were culture-negative. Mean (range) follow-up was 33.9 (6.2-75.7) months for aseptic revisions and 32.3 (7.5-94.2) months for septic revisions. Radiographic follow-up was performed at each visit, with weight-bearing anteroposterior and posteroanterior views, along with a lateral knee radiograph. At final follow-up, ROM was recorded by the senior attending evaluating the patient.
Categorical variables were statistically analyzed with χ2 tests, and continuous variables were analyzed with Student t test, analysis of variance, and univariate analysis of covariance (ANCOVA). Statistical significance was set at P < .05. Intrarater reliability was measured with the intraclass correlation coefficient (ICC). All statistical analysis was performed with Predictive Analytics SoftWare Statistics Version 20.0 (SPSS, Chicago, Illinois).
Results
Ninety-one consecutive patients (43 men, 48 women) were included in this study. Mean (SD) age was 66.4 (10.1) years. Mean (SD) preoperative ISR in septic and aseptic cases was 0.94 (0.25) for men and 1.02 (0.23) for women (P = .10). Mean postoperative ISR in septic and aseptic cases was 0.84 (0.27) for men and 0.99 (0.23) for women (P = .004). There was a sex difference between septic and aseptic revisions. There were 22 men and 36 women in the aseptic group and 21 men and 12 women in the septic group (P = .01). Men were more likely than women to have septic revisions and patella baja. Table 1 compares the patient demographics of the 2 patient populations. Mean (SD) number of surgeries, including irrigation and débridement procedures before reimplantation, was larger for septic revisions, 2.9 (0.9), than for aseptic revisions, 1.4 (0.8) (P < .001).
Infection was the most common reason for revision and accounted for 33.7% (34/101) of all revisions. Noninfectious indications, in declining order of frequency, included loosening (23.8%, 24/101), instability (11.9%, 12/101), pain (11.9%, 12/101), osteolysis (5.0%, 5/101), polyethylene wear (5.0%, 5/101), failed unicompartmental knee (4.0%, 4/101), stiffness (3.0%, 3/101), and patellar problems (2.0%, 2/101) (Table 2). ISR decreased significantly only in infected revisions. It is important to note that there was not a high incidence of stiffness or patellofemoral failure in revision patients before surgery.
Mean (SD) ISR did not differ between groups before surgery, 1.00 (0.25) for aseptic and 0.96 (0.22) for septic (P = .49), but differed significantly after surgery, 0.99 (0.23) for aseptic and 0.77 (0.24) for septic (P < .001) (Figure 2). The univariate ANCOVA also demonstrated a postoperative difference between groups when taking the preoperative ratio into account: 0.99 (0.23) for aseptic and 0.78 (0.24) for septic (P = .005) (Table 3). Before surgery, 22.4% and 23.9% of the aseptic and septic groups, respectively, had patella baja (P = .58). After surgery, 17.6% and 58.8% of the aseptic and septic groups had patella baja (P = .001) (Table 4). The ICC for preoperative ISR was 0.94, and the ICC for postoperative ISR was 0.96, which indicates excellent agreement of measurements between the 2 blinded investigators.
ROM differed between septic and aseptic groups owing to the difference in postoperative flexion. Mean (SD) postoperative extension was 2.2° (5.4°) for the aseptic group and 5.1° (9.8°) for the septic group—not significantly different (P = .13). Mean (SD) postoperative flexion was 110.2° (18.8°) for the aseptic group and 97.2° (29.4°) for the septic group—significantly different (P = .02). The groups differed significantly (P = .02) in mean (SD) ROM: 108.0° (20.7°) for aseptic and 92.2° (34.6°) for septic (Table 1). ROM was also significantly associated with patella baja (P = .04), as patients with ISR of less than 0.8 had mean (SD) postoperative ROM of 95.1° (31.6°), and patients without patella baja had mean (SD) postoperative ROM of 106.8° (23.6°).
For the septic group, mean (SD) time between first and second stages was 13.0 (8.3) weeks (range, 1-44.3 weeks). Mean (SD) timing of spacer placement was not statistically significantly different (P = .90) between patients who had patella baja, 12.9 (8.8) weeks, and patients who did not have patella baja, 13.2 (7.8) weeks.
Discussion
This study demonstrated that TKAs done for septic reasons resulted in a higher incidence of patella baja and decreased ROM. Incidence of patella baja was higher both before and after revision in septic TKAs than in aseptic TKAs, proving the hypothesis under study. Prerevision incidence was not significantly different, but there was a trend that could not be ignored. This may suggest that there is already an ongoing process in the infected knee that contributes to patella baja; the precise etiology remains unclear and is likely multifactorial. For example, scar formation may be increased in patients with chronic infection, predisposing to patella baja. This assertion is indirectly supported by a recent study from our institution revealing longer average surgical time in septic versus aseptic knee revisions; the difference was thought to reflect increased scar-tissue formation.16 That study also found that patients who underwent septic revisions had significantly more surgical procedures than patients who underwent aseptic revisions. Repetitive surgeries—specifically, repetitive arthrotomies during irrigation and débridement before reimplantation—lead to increased scar formation, which may contribute to preoperative and postoperative patella baja. This may be reflected in the findings that ROM was decreased in patients in the septic group versus patients in the aseptic group and that ROM was decreased in patients with patella baja. In addition, our study found that male patients were more likely to undergo TKA revision for septic reasons and to develop postoperative patella baja. This finding contrasts with that of a study5 that compared preoperative and postoperative ISR in primary TKA and found that women were more likely than men to have patella baja. Although women are more likely to undergo TKA revision,17 men may be more susceptible to infection and subsequent patella baja.
The higher postoperative rate of patella baja in the septic group became statistically significant even when preoperative incidence was considered. This may have been caused by infection-related scarring and by prolonged immobilization of septic knees with use of nonarticulating antibiotic spacers. By keeping these knees immobile with a nonarticulating spacer for a prolonged period in the healing phase of the infection, scar tissue may mature and form over the time between stages. A comparable example may be high tibial osteotomies, in which a high incidence of patella baja has been partly attributed to prolonged casting.11 Future work comparing the results of articulating and nonarticulating spacers will help to determine if immobilization contributes to patella baja in infected TKAs.
There are several limitations to our study. Patient outcome questionnaires were not used, and they would have allowed for the assessment of physical outcomes and emotional satisfaction by comparing outcomes between patients with and without patella baja and comparing septic and aseptic TKAs. In addition, there was no standard method for quantifying difficulty of revision, which would have enabled us to compare difficulty of revision in patients with patella baja.
Conclusion
This study identified a high rate of patella baja and decreased ROM in TKA revisions, particularly infected revisions treated with a nonarticulating spacer. It is important to determine if there are functional consequences. Further investigation is needed regarding the cause, prevention, and management of this potentially debilitating outcome after revision TKA.
1. Aglietti P, Buzzi R, Gaudenzi A. Patello-femoral functional results and complications with the posterior stabilised total condylar knee prosthesis. J Arthroplasty. 1988;3(1):17-25.
2. Fern ED, Winson IG, Getty CJM. Anterior knee pain in rheumatoid patients after total knee replacement: possible selection criteria for patellar resurfacing. J Bone Joint Surg Br. 1992;74(5):745-748.
3. Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Surg Surg Am. 1986;68(7):1035-1040.
4. Floren M, Davis J, Peterson MG, Laskin RS. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patellar baja. J Arthroplasty. 2007;22(6 Suppl 2):51-57.
5. Meneghini RM, Ritter MA, Pierson JL, Meding JB, Berend ME, Faris PM. The effect of the Insall-Salvati ratio on outcome after total knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):116-120.
6. Singerman R, Davy DT, Goldberg VM. Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech. 1994;27(8):1059-1065.
7. Van Eijden TM, Kouwenhoven E, Weijs WA. Mechanics of the patellar articulation: effects of patellar ligament length studied with a mathematical model. Acta Orthop Scand. 1987;58(5):560-566.
8. Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81(5):790-795.
9. Chonko DJ, Lombardi AV Jr, Berend KR. Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int. 2004;12:231-238.
10. Cameron HU, Jung YB. Patella baja complicating total knee arthroplasty. A report of two cases. J Arthroplasty. 1988;3(2):177-180.
11. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71(2):245-248.
12. Insall JN, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104.
13. Grelsamer RP. Patella baja after total knee arthroplasty: is it really patella baja? J Arthroplasty. 2002;17(1):66-69.
14. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
15. Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;26(8):1136-1138.
16. Laudermilch DJ, Fedorka CJ, Heyl A, Rao N, McGough RL. Outcomes of revision total knee arthroplasty after methicillin-resistant Staphylococcus aureus infection. Clin Orthop. 2010;468(8):2067-2073.
17. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop. 2010;468(1):45-51.
1. Aglietti P, Buzzi R, Gaudenzi A. Patello-femoral functional results and complications with the posterior stabilised total condylar knee prosthesis. J Arthroplasty. 1988;3(1):17-25.
2. Fern ED, Winson IG, Getty CJM. Anterior knee pain in rheumatoid patients after total knee replacement: possible selection criteria for patellar resurfacing. J Bone Joint Surg Br. 1992;74(5):745-748.
3. Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Surg Surg Am. 1986;68(7):1035-1040.
4. Floren M, Davis J, Peterson MG, Laskin RS. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patellar baja. J Arthroplasty. 2007;22(6 Suppl 2):51-57.
5. Meneghini RM, Ritter MA, Pierson JL, Meding JB, Berend ME, Faris PM. The effect of the Insall-Salvati ratio on outcome after total knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):116-120.
6. Singerman R, Davy DT, Goldberg VM. Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech. 1994;27(8):1059-1065.
7. Van Eijden TM, Kouwenhoven E, Weijs WA. Mechanics of the patellar articulation: effects of patellar ligament length studied with a mathematical model. Acta Orthop Scand. 1987;58(5):560-566.
8. Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81(5):790-795.
9. Chonko DJ, Lombardi AV Jr, Berend KR. Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int. 2004;12:231-238.
10. Cameron HU, Jung YB. Patella baja complicating total knee arthroplasty. A report of two cases. J Arthroplasty. 1988;3(2):177-180.
11. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71(2):245-248.
12. Insall JN, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104.
13. Grelsamer RP. Patella baja after total knee arthroplasty: is it really patella baja? J Arthroplasty. 2002;17(1):66-69.
14. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
15. Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;26(8):1136-1138.
16. Laudermilch DJ, Fedorka CJ, Heyl A, Rao N, McGough RL. Outcomes of revision total knee arthroplasty after methicillin-resistant Staphylococcus aureus infection. Clin Orthop. 2010;468(8):2067-2073.
17. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop. 2010;468(1):45-51.