User login
High-Risk Musculoskeletal Injuries
Case
A 2-year-old girl was carried into the ED after falling off her bed earlier in the evening. The parents did not see the child fall, but heard her crying in her room. On physical examination, the patient was in a lot of pain, would not move her left arm, and had a left elbow effusion. The radial pulse was strong, and she was able to move all of her fingers but would not move her elbow. A lateral X-ray taken of the left elbow is shown below (Figure 1).
Supracondylar Fractures
Supracondylar fractures are the most common pediatric elbow injury and disposition can range from outpatient follow-up to urgent surgical intervention. The average age of presentation is between 3 to 10 years, and the injury typically results from a fall on an outstretched hand (FOOSH) with hyperextension of the elbow. Supracondylar fractures may also occur after a direct blow to the elbow or hyperflexion.1
The supracondylar area in children, the distal portion of the humerus, is thin and weak. The force transmitted to this region by a direct blow or FOOSH injury can fracture the humerus. The brachial artery runs along the anterior humerus and can easily sustain injury. Median, ulnar, or radial nerve injuries are also common and can result in permanent disability.2 Immediate neurovascular examination is mandatory, and diminished or absent pulses, poor perfusion, and pallor are signs of ischemia. Examination should include assessment of the radial pulse and the sensory and motor function of the median, radial, and ulnar nerves. To test the median nerve (via the anterior interosseous branch), ask the patient make an “OK” sign with his or her fingers; to test the radial nerve, instruct the child to make a “thumb’s up” sign; and to test the ulnar nerve, have the child hold his or her fingers spread-out against resistance. In addition, sensation of the palmer and dorsal surfaces and in between the fingers should be confirmed.
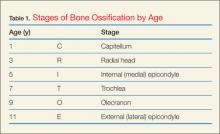
Plain radiographs, including anteroposterior (AP), oblique, and true lateral views, should be obtained. Interpretation of pediatric elbow films can be difficult, and the stages of ossification must be considered. The helpful acronym for remembering the order of bone ossification is CRITOE (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, and external [lateral] epicondyle) (Table 1).
If the anterior humeral line—a line drawn through the anterior cortex of the humerus—fails to intersect the capitellum in its middle third, fracture of the distal humerus is present (Figure 2). The radial head should be aligned with the capitellum. Close inspection for a posterior fat pad, or “sail sign” is imperative as it indicates hemorrhage, joint effusion, or occult fracture. The presence of an anterior fat pad can be a normal variant; however, if the pad is wide and creates a “sail sign” then fracture must be assumed.1
Fracture Types
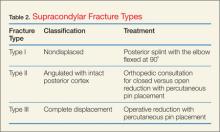
Type III supracondylar fractures are completely displaced with a fracture through the anterior and posterior cortex. Since a high-risk of injury to the upper extremity vessels and nerves is associated with these very unstable fractures, routine neurovascular checks (while awaiting operative repair) are required. Supracondylar fractures are often associated with forearm or distal radius fractures; therefore, forearm radiographs should also be obtained.3
Diskitis
Tumors
Spondylolysis
Pediatric Cervical Spine Clearance
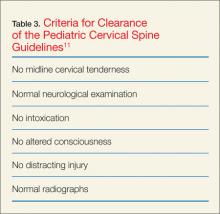
Thankfully, cervical spine injuries are rare, occurring in approximately 1% of children after blunt trauma.9 Left unrecognized, however, these injuries may result in permanent neurological disability. Children younger than 8 years of age are more likely to injure the upper cervical spine (C1 to C3) than older children and adults. This is because children have relatively larger heads than bodies and weaker cervical muscles and ligaments, making the upper cervical spine more mobile. The Emergency X-Radiography Utilization Study (NEXUS) criteria have been validated in adults; however, criteria for clearing the pediatric cervical spine are poorly studied. Because of limited data, there are few evidence-based guidelines for the clearance of the pediatric cervical spine. A study in 2001 found that the NEXUS guidelines where helpful in reducing imaging in 20% of children, but due to the low numbers of infants in this study, caution is advised when applying the NEXUS criteria to children under 2 years of age.9
Nonaccidental Trauma: Abuse
Orthopedic injury due to nonaccidental trauma (NAT) can be difficult to distinguish from normal childhood injuries. Identification of high-risk presentations is key in diagnosing these injuries and hopefully preventing further abuse. Femur fractures in children younger than age 1 year have a high likelihood of being nonaccidental, with between 60% to 80% of femoral shaft fractures resulting from abuse. No particular pattern of fracture is pathognomonic for NAT. The American Academy of Orthopaedic Surgeons recommends that children younger than age 36 months with a diaphyseal femur fracture be evaluated for child abuse.12
Spiral fractures and transverse fractures of long bones also raise suspicion for NAT. Injury to the metaphysis of long bones, especially in nonambulatory children, is considered highly suggestive of child abuse. The classic metaphyseal lesion, called a “corner” or “bucket-handle” fracture, occurs when the extremity (usually the forearm) is pulled or twisted forcibly, or the child is shaken. X-ray will demonstrate a disruption of the metaphysis with lucency. As the developing ribs are flexible and difficult to break with minor injuries, a child with a rib fracture and no history of severe trauma, such as a motor vehicle crash or fall from a significant height, has a high likelihood of being a victim of child abuse. Skull fractures caused from accidental injury and abuse may have similar presentations. The history and mechanism are important to correlate with physical examination findings for potential inconsistencies.13
Case Conclusion
The child in this case sustained a type II supracondylar fracture. Orthopedic surgery was consulted, and the patient was taken to the operating room for closed reduction and percutaneous pinning. She was placed in a cast, and pins were removed at follow-up 4 weeks later. No residual pain or deficits remained, and she regained full function of her arm.
Dr Hewett is a pediatric emergency medicine fellow, College of Medicine, Medical University of South Carolina, Charleston.
Dr Titus is vice chair, pediatric fellowships, and fellowship director, pediatric emergency medicine; and an associate professor of pediatrics, Medical University of South Carolina, Charleston.
- Bachman D, Santora S. Orthopedic trauma. In: Fleisher GR, Ludwig S, et al, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:1538.
- Carson S, Woolridge DP, Colletti J, Kilgore K. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53(1):41.
- Slack SE, Clancy MJ. Clearing the cervical spine of paediatric trauma patients. Emer Med J. 2004;21(2):189-193
- Brown M. Hussain K, McHugh K, Novelli V, Jones D. Discitis in young children. J Bone Joint Surg. 2001;83(1):106-111.
- Cushing AH. Diskitis in children. Clin Infect Dis. 1993;17(1):1-6.
- Selbst SM, Lavelle JM, Soyupak SK, Markowitz RI. Back pain in children who present to the emergency department. Clin Pediatr (Phila). 1999;38(7):401-406.
- Widhe B, Widhe T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint Surg Am. 2000;82(5):667-674.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20.
- Hendey GW, Wolfson AB, Mower WR, Hoffman JR; National Emergency X-Radiography Utilization Study Group. Spinal cord injury without radiographic abnormality: results of the National Emergency X-Radiography Utilization Study in blunt cervical trauma. J Trauma. 2002;53(1):1-4
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
- Offiah A, van Rijn RR, Perez-Rossello JM, Kleinman PK. Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol. 2009;39(5):461-470.
- Bonfield, CM, Naran S et al. Pediatric skull fractures: the need for surgical intervention, characteristics, complications, and outcomes. J Neurosurg Pediatr. 2014;14(2):205-211.
Case
A 2-year-old girl was carried into the ED after falling off her bed earlier in the evening. The parents did not see the child fall, but heard her crying in her room. On physical examination, the patient was in a lot of pain, would not move her left arm, and had a left elbow effusion. The radial pulse was strong, and she was able to move all of her fingers but would not move her elbow. A lateral X-ray taken of the left elbow is shown below (Figure 1).
Supracondylar Fractures
Supracondylar fractures are the most common pediatric elbow injury and disposition can range from outpatient follow-up to urgent surgical intervention. The average age of presentation is between 3 to 10 years, and the injury typically results from a fall on an outstretched hand (FOOSH) with hyperextension of the elbow. Supracondylar fractures may also occur after a direct blow to the elbow or hyperflexion.1
The supracondylar area in children, the distal portion of the humerus, is thin and weak. The force transmitted to this region by a direct blow or FOOSH injury can fracture the humerus. The brachial artery runs along the anterior humerus and can easily sustain injury. Median, ulnar, or radial nerve injuries are also common and can result in permanent disability.2 Immediate neurovascular examination is mandatory, and diminished or absent pulses, poor perfusion, and pallor are signs of ischemia. Examination should include assessment of the radial pulse and the sensory and motor function of the median, radial, and ulnar nerves. To test the median nerve (via the anterior interosseous branch), ask the patient make an “OK” sign with his or her fingers; to test the radial nerve, instruct the child to make a “thumb’s up” sign; and to test the ulnar nerve, have the child hold his or her fingers spread-out against resistance. In addition, sensation of the palmer and dorsal surfaces and in between the fingers should be confirmed.
Plain radiographs, including anteroposterior (AP), oblique, and true lateral views, should be obtained. Interpretation of pediatric elbow films can be difficult, and the stages of ossification must be considered. The helpful acronym for remembering the order of bone ossification is CRITOE (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, and external [lateral] epicondyle) (Table 1).
If the anterior humeral line—a line drawn through the anterior cortex of the humerus—fails to intersect the capitellum in its middle third, fracture of the distal humerus is present (Figure 2). The radial head should be aligned with the capitellum. Close inspection for a posterior fat pad, or “sail sign” is imperative as it indicates hemorrhage, joint effusion, or occult fracture. The presence of an anterior fat pad can be a normal variant; however, if the pad is wide and creates a “sail sign” then fracture must be assumed.1
Fracture Types
Type III supracondylar fractures are completely displaced with a fracture through the anterior and posterior cortex. Since a high-risk of injury to the upper extremity vessels and nerves is associated with these very unstable fractures, routine neurovascular checks (while awaiting operative repair) are required. Supracondylar fractures are often associated with forearm or distal radius fractures; therefore, forearm radiographs should also be obtained.3
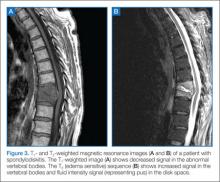
Diskitis
Tumors
Spondylolysis
Pediatric Cervical Spine Clearance
Thankfully, cervical spine injuries are rare, occurring in approximately 1% of children after blunt trauma.9 Left unrecognized, however, these injuries may result in permanent neurological disability. Children younger than 8 years of age are more likely to injure the upper cervical spine (C1 to C3) than older children and adults. This is because children have relatively larger heads than bodies and weaker cervical muscles and ligaments, making the upper cervical spine more mobile. The Emergency X-Radiography Utilization Study (NEXUS) criteria have been validated in adults; however, criteria for clearing the pediatric cervical spine are poorly studied. Because of limited data, there are few evidence-based guidelines for the clearance of the pediatric cervical spine. A study in 2001 found that the NEXUS guidelines where helpful in reducing imaging in 20% of children, but due to the low numbers of infants in this study, caution is advised when applying the NEXUS criteria to children under 2 years of age.9
Nonaccidental Trauma: Abuse
Orthopedic injury due to nonaccidental trauma (NAT) can be difficult to distinguish from normal childhood injuries. Identification of high-risk presentations is key in diagnosing these injuries and hopefully preventing further abuse. Femur fractures in children younger than age 1 year have a high likelihood of being nonaccidental, with between 60% to 80% of femoral shaft fractures resulting from abuse. No particular pattern of fracture is pathognomonic for NAT. The American Academy of Orthopaedic Surgeons recommends that children younger than age 36 months with a diaphyseal femur fracture be evaluated for child abuse.12
Spiral fractures and transverse fractures of long bones also raise suspicion for NAT. Injury to the metaphysis of long bones, especially in nonambulatory children, is considered highly suggestive of child abuse. The classic metaphyseal lesion, called a “corner” or “bucket-handle” fracture, occurs when the extremity (usually the forearm) is pulled or twisted forcibly, or the child is shaken. X-ray will demonstrate a disruption of the metaphysis with lucency. As the developing ribs are flexible and difficult to break with minor injuries, a child with a rib fracture and no history of severe trauma, such as a motor vehicle crash or fall from a significant height, has a high likelihood of being a victim of child abuse. Skull fractures caused from accidental injury and abuse may have similar presentations. The history and mechanism are important to correlate with physical examination findings for potential inconsistencies.13
Case Conclusion
The child in this case sustained a type II supracondylar fracture. Orthopedic surgery was consulted, and the patient was taken to the operating room for closed reduction and percutaneous pinning. She was placed in a cast, and pins were removed at follow-up 4 weeks later. No residual pain or deficits remained, and she regained full function of her arm.
Dr Hewett is a pediatric emergency medicine fellow, College of Medicine, Medical University of South Carolina, Charleston.
Dr Titus is vice chair, pediatric fellowships, and fellowship director, pediatric emergency medicine; and an associate professor of pediatrics, Medical University of South Carolina, Charleston.
Case
A 2-year-old girl was carried into the ED after falling off her bed earlier in the evening. The parents did not see the child fall, but heard her crying in her room. On physical examination, the patient was in a lot of pain, would not move her left arm, and had a left elbow effusion. The radial pulse was strong, and she was able to move all of her fingers but would not move her elbow. A lateral X-ray taken of the left elbow is shown below (Figure 1).
Supracondylar Fractures
Supracondylar fractures are the most common pediatric elbow injury and disposition can range from outpatient follow-up to urgent surgical intervention. The average age of presentation is between 3 to 10 years, and the injury typically results from a fall on an outstretched hand (FOOSH) with hyperextension of the elbow. Supracondylar fractures may also occur after a direct blow to the elbow or hyperflexion.1
The supracondylar area in children, the distal portion of the humerus, is thin and weak. The force transmitted to this region by a direct blow or FOOSH injury can fracture the humerus. The brachial artery runs along the anterior humerus and can easily sustain injury. Median, ulnar, or radial nerve injuries are also common and can result in permanent disability.2 Immediate neurovascular examination is mandatory, and diminished or absent pulses, poor perfusion, and pallor are signs of ischemia. Examination should include assessment of the radial pulse and the sensory and motor function of the median, radial, and ulnar nerves. To test the median nerve (via the anterior interosseous branch), ask the patient make an “OK” sign with his or her fingers; to test the radial nerve, instruct the child to make a “thumb’s up” sign; and to test the ulnar nerve, have the child hold his or her fingers spread-out against resistance. In addition, sensation of the palmer and dorsal surfaces and in between the fingers should be confirmed.
Plain radiographs, including anteroposterior (AP), oblique, and true lateral views, should be obtained. Interpretation of pediatric elbow films can be difficult, and the stages of ossification must be considered. The helpful acronym for remembering the order of bone ossification is CRITOE (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, and external [lateral] epicondyle) (Table 1).
If the anterior humeral line—a line drawn through the anterior cortex of the humerus—fails to intersect the capitellum in its middle third, fracture of the distal humerus is present (Figure 2). The radial head should be aligned with the capitellum. Close inspection for a posterior fat pad, or “sail sign” is imperative as it indicates hemorrhage, joint effusion, or occult fracture. The presence of an anterior fat pad can be a normal variant; however, if the pad is wide and creates a “sail sign” then fracture must be assumed.1
Fracture Types
Type III supracondylar fractures are completely displaced with a fracture through the anterior and posterior cortex. Since a high-risk of injury to the upper extremity vessels and nerves is associated with these very unstable fractures, routine neurovascular checks (while awaiting operative repair) are required. Supracondylar fractures are often associated with forearm or distal radius fractures; therefore, forearm radiographs should also be obtained.3
Diskitis
Tumors
Spondylolysis
Pediatric Cervical Spine Clearance
Thankfully, cervical spine injuries are rare, occurring in approximately 1% of children after blunt trauma.9 Left unrecognized, however, these injuries may result in permanent neurological disability. Children younger than 8 years of age are more likely to injure the upper cervical spine (C1 to C3) than older children and adults. This is because children have relatively larger heads than bodies and weaker cervical muscles and ligaments, making the upper cervical spine more mobile. The Emergency X-Radiography Utilization Study (NEXUS) criteria have been validated in adults; however, criteria for clearing the pediatric cervical spine are poorly studied. Because of limited data, there are few evidence-based guidelines for the clearance of the pediatric cervical spine. A study in 2001 found that the NEXUS guidelines where helpful in reducing imaging in 20% of children, but due to the low numbers of infants in this study, caution is advised when applying the NEXUS criteria to children under 2 years of age.9
Nonaccidental Trauma: Abuse
Orthopedic injury due to nonaccidental trauma (NAT) can be difficult to distinguish from normal childhood injuries. Identification of high-risk presentations is key in diagnosing these injuries and hopefully preventing further abuse. Femur fractures in children younger than age 1 year have a high likelihood of being nonaccidental, with between 60% to 80% of femoral shaft fractures resulting from abuse. No particular pattern of fracture is pathognomonic for NAT. The American Academy of Orthopaedic Surgeons recommends that children younger than age 36 months with a diaphyseal femur fracture be evaluated for child abuse.12
Spiral fractures and transverse fractures of long bones also raise suspicion for NAT. Injury to the metaphysis of long bones, especially in nonambulatory children, is considered highly suggestive of child abuse. The classic metaphyseal lesion, called a “corner” or “bucket-handle” fracture, occurs when the extremity (usually the forearm) is pulled or twisted forcibly, or the child is shaken. X-ray will demonstrate a disruption of the metaphysis with lucency. As the developing ribs are flexible and difficult to break with minor injuries, a child with a rib fracture and no history of severe trauma, such as a motor vehicle crash or fall from a significant height, has a high likelihood of being a victim of child abuse. Skull fractures caused from accidental injury and abuse may have similar presentations. The history and mechanism are important to correlate with physical examination findings for potential inconsistencies.13
Case Conclusion
The child in this case sustained a type II supracondylar fracture. Orthopedic surgery was consulted, and the patient was taken to the operating room for closed reduction and percutaneous pinning. She was placed in a cast, and pins were removed at follow-up 4 weeks later. No residual pain or deficits remained, and she regained full function of her arm.
Dr Hewett is a pediatric emergency medicine fellow, College of Medicine, Medical University of South Carolina, Charleston.
Dr Titus is vice chair, pediatric fellowships, and fellowship director, pediatric emergency medicine; and an associate professor of pediatrics, Medical University of South Carolina, Charleston.
- Bachman D, Santora S. Orthopedic trauma. In: Fleisher GR, Ludwig S, et al, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:1538.
- Carson S, Woolridge DP, Colletti J, Kilgore K. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53(1):41.
- Slack SE, Clancy MJ. Clearing the cervical spine of paediatric trauma patients. Emer Med J. 2004;21(2):189-193
- Brown M. Hussain K, McHugh K, Novelli V, Jones D. Discitis in young children. J Bone Joint Surg. 2001;83(1):106-111.
- Cushing AH. Diskitis in children. Clin Infect Dis. 1993;17(1):1-6.
- Selbst SM, Lavelle JM, Soyupak SK, Markowitz RI. Back pain in children who present to the emergency department. Clin Pediatr (Phila). 1999;38(7):401-406.
- Widhe B, Widhe T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint Surg Am. 2000;82(5):667-674.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20.
- Hendey GW, Wolfson AB, Mower WR, Hoffman JR; National Emergency X-Radiography Utilization Study Group. Spinal cord injury without radiographic abnormality: results of the National Emergency X-Radiography Utilization Study in blunt cervical trauma. J Trauma. 2002;53(1):1-4
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
- Offiah A, van Rijn RR, Perez-Rossello JM, Kleinman PK. Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol. 2009;39(5):461-470.
- Bonfield, CM, Naran S et al. Pediatric skull fractures: the need for surgical intervention, characteristics, complications, and outcomes. J Neurosurg Pediatr. 2014;14(2):205-211.
- Bachman D, Santora S. Orthopedic trauma. In: Fleisher GR, Ludwig S, et al, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:1538.
- Carson S, Woolridge DP, Colletti J, Kilgore K. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53(1):41.
- Slack SE, Clancy MJ. Clearing the cervical spine of paediatric trauma patients. Emer Med J. 2004;21(2):189-193
- Brown M. Hussain K, McHugh K, Novelli V, Jones D. Discitis in young children. J Bone Joint Surg. 2001;83(1):106-111.
- Cushing AH. Diskitis in children. Clin Infect Dis. 1993;17(1):1-6.
- Selbst SM, Lavelle JM, Soyupak SK, Markowitz RI. Back pain in children who present to the emergency department. Clin Pediatr (Phila). 1999;38(7):401-406.
- Widhe B, Widhe T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint Surg Am. 2000;82(5):667-674.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR; NEXUS Group. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108(2):E20.
- Hendey GW, Wolfson AB, Mower WR, Hoffman JR; National Emergency X-Radiography Utilization Study Group. Spinal cord injury without radiographic abnormality: results of the National Emergency X-Radiography Utilization Study in blunt cervical trauma. J Trauma. 2002;53(1):1-4
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
- Offiah A, van Rijn RR, Perez-Rossello JM, Kleinman PK. Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol. 2009;39(5):461-470.
- Bonfield, CM, Naran S et al. Pediatric skull fractures: the need for surgical intervention, characteristics, complications, and outcomes. J Neurosurg Pediatr. 2014;14(2):205-211.