User login
Bendamustine plus rituximab may have edge for treating indolent NHL, MCL
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
mdales@frontlinemedcom.com
On Twitter @maryjodales
AT ASCO 2017
Key clinical point:
Major finding: For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively.
Data source: In BRIGHT, 224 treatment-naive patients with indolent non-Hodgkin lymphoma or mantle cell lymphoma were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients).
Disclosures: Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
Severe health conditions decline in childhood cancer survivors
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have steadily declined, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study, funded by the National Institutes of Health.
For all childhood cancer survivors, the 15-year cumulative incidence of severe health conditions decreased from 12.7% in those diagnosed in the 1970s, to 10.1% in the 1980s, and to 8.8% among those diagnosed in the 1990s (per 10 years: hazard ratio, 0.84 [95% confidence interval, 0.80-0.89]), Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, reported at a press conference at the annual meeting of the American Society of Clinical Oncology.
The association with diagnosis decade was attenuated (HR, 0.92 [95% CI, 0.85-1.00]) when detailed treatment data were included in the model, indicating that treatment reductions mediated risk.
Changes in childhood cancer treatment protocols to reduce the intensity of therapy – along with improved screening and early detection – have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity, Dr. Gibson said.
As the data address children diagnosed over 15 years ago, it is likely that improvements since then in determining patient risk and targeting therapy might result in further incremental improvements, he said in an interview.
By cancer type, severe health problems by 15 years after diagnosis decreased from 13% to 5% among survivors of Wilms’ tumor, from 18% to 11% among survivors of Hodgkin lymphoma, from 15% to 9% among survivors of astrocytoma, from 10% to 6% among survivors of non-Hodgkin lymphoma, and from 9% to 7% among survivors of acute lymphoblastic leukemia. The conclusions are based on the incidence of severe, disabling/life-threatening, or fatal chronic health conditions (Common Terminology Criteria for Adverse Events, grades 3-5) among 5-year survivors diagnosed prior to age 21 years from 1970 through 1999.
Adjusted for sex and attained age, significant reduction in risk over time was found among survivors of Wilms tumor (HR, 0.57 [95% CI, 0.46-0.70]), Hodgkin lymphoma (HR, 0.75 [95% CI, 0.65-0.85]), astrocytoma (HR, 0.77 [95% CI, 0.64-0.92]), non-Hodgkin lymphoma (HR, 0.79 [95% CI, 0.63-0.99]), and acute lymphoblastic leukemia (HR, 0.86 [95% CI, 0.76-0.98]).
The decreases in serious health conditions were largely driven by a reduced incidence of endocrine conditions (1970s: 4.0% vs. 1990s: 1.6%; HR, 0.66 [95% CI, 0.59-0.73]) and subsequent malignant neoplasms (1970s: 2.4% vs. 1990s: 1.6%; HR, 0.85 [95% CI, 0.76-0.96]).
Gastrointestinal (HR, 0.80 [95% CI, 0.66-0.97]) and neurological conditions (HR, 0.77 [95% CI, 0.65-0.91]) also were reduced, but cardiac and pulmonary conditions were not. Changes in childhood cancer treatment protocols have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity in this population, Dr. Gibson concluded.
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have steadily declined, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study, funded by the National Institutes of Health.
For all childhood cancer survivors, the 15-year cumulative incidence of severe health conditions decreased from 12.7% in those diagnosed in the 1970s, to 10.1% in the 1980s, and to 8.8% among those diagnosed in the 1990s (per 10 years: hazard ratio, 0.84 [95% confidence interval, 0.80-0.89]), Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, reported at a press conference at the annual meeting of the American Society of Clinical Oncology.
The association with diagnosis decade was attenuated (HR, 0.92 [95% CI, 0.85-1.00]) when detailed treatment data were included in the model, indicating that treatment reductions mediated risk.
Changes in childhood cancer treatment protocols to reduce the intensity of therapy – along with improved screening and early detection – have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity, Dr. Gibson said.
As the data address children diagnosed over 15 years ago, it is likely that improvements since then in determining patient risk and targeting therapy might result in further incremental improvements, he said in an interview.
By cancer type, severe health problems by 15 years after diagnosis decreased from 13% to 5% among survivors of Wilms’ tumor, from 18% to 11% among survivors of Hodgkin lymphoma, from 15% to 9% among survivors of astrocytoma, from 10% to 6% among survivors of non-Hodgkin lymphoma, and from 9% to 7% among survivors of acute lymphoblastic leukemia. The conclusions are based on the incidence of severe, disabling/life-threatening, or fatal chronic health conditions (Common Terminology Criteria for Adverse Events, grades 3-5) among 5-year survivors diagnosed prior to age 21 years from 1970 through 1999.
Adjusted for sex and attained age, significant reduction in risk over time was found among survivors of Wilms tumor (HR, 0.57 [95% CI, 0.46-0.70]), Hodgkin lymphoma (HR, 0.75 [95% CI, 0.65-0.85]), astrocytoma (HR, 0.77 [95% CI, 0.64-0.92]), non-Hodgkin lymphoma (HR, 0.79 [95% CI, 0.63-0.99]), and acute lymphoblastic leukemia (HR, 0.86 [95% CI, 0.76-0.98]).
The decreases in serious health conditions were largely driven by a reduced incidence of endocrine conditions (1970s: 4.0% vs. 1990s: 1.6%; HR, 0.66 [95% CI, 0.59-0.73]) and subsequent malignant neoplasms (1970s: 2.4% vs. 1990s: 1.6%; HR, 0.85 [95% CI, 0.76-0.96]).
Gastrointestinal (HR, 0.80 [95% CI, 0.66-0.97]) and neurological conditions (HR, 0.77 [95% CI, 0.65-0.91]) also were reduced, but cardiac and pulmonary conditions were not. Changes in childhood cancer treatment protocols have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity in this population, Dr. Gibson concluded.
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have steadily declined, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study, funded by the National Institutes of Health.
For all childhood cancer survivors, the 15-year cumulative incidence of severe health conditions decreased from 12.7% in those diagnosed in the 1970s, to 10.1% in the 1980s, and to 8.8% among those diagnosed in the 1990s (per 10 years: hazard ratio, 0.84 [95% confidence interval, 0.80-0.89]), Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, reported at a press conference at the annual meeting of the American Society of Clinical Oncology.
The association with diagnosis decade was attenuated (HR, 0.92 [95% CI, 0.85-1.00]) when detailed treatment data were included in the model, indicating that treatment reductions mediated risk.
Changes in childhood cancer treatment protocols to reduce the intensity of therapy – along with improved screening and early detection – have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity, Dr. Gibson said.
As the data address children diagnosed over 15 years ago, it is likely that improvements since then in determining patient risk and targeting therapy might result in further incremental improvements, he said in an interview.
By cancer type, severe health problems by 15 years after diagnosis decreased from 13% to 5% among survivors of Wilms’ tumor, from 18% to 11% among survivors of Hodgkin lymphoma, from 15% to 9% among survivors of astrocytoma, from 10% to 6% among survivors of non-Hodgkin lymphoma, and from 9% to 7% among survivors of acute lymphoblastic leukemia. The conclusions are based on the incidence of severe, disabling/life-threatening, or fatal chronic health conditions (Common Terminology Criteria for Adverse Events, grades 3-5) among 5-year survivors diagnosed prior to age 21 years from 1970 through 1999.
Adjusted for sex and attained age, significant reduction in risk over time was found among survivors of Wilms tumor (HR, 0.57 [95% CI, 0.46-0.70]), Hodgkin lymphoma (HR, 0.75 [95% CI, 0.65-0.85]), astrocytoma (HR, 0.77 [95% CI, 0.64-0.92]), non-Hodgkin lymphoma (HR, 0.79 [95% CI, 0.63-0.99]), and acute lymphoblastic leukemia (HR, 0.86 [95% CI, 0.76-0.98]).
The decreases in serious health conditions were largely driven by a reduced incidence of endocrine conditions (1970s: 4.0% vs. 1990s: 1.6%; HR, 0.66 [95% CI, 0.59-0.73]) and subsequent malignant neoplasms (1970s: 2.4% vs. 1990s: 1.6%; HR, 0.85 [95% CI, 0.76-0.96]).
Gastrointestinal (HR, 0.80 [95% CI, 0.66-0.97]) and neurological conditions (HR, 0.77 [95% CI, 0.65-0.91]) also were reduced, but cardiac and pulmonary conditions were not. Changes in childhood cancer treatment protocols have not only extended lifespan for many survivors, but also have reduced the incidence of serious chronic morbidity in this population, Dr. Gibson concluded.
mdales@frontlinemedcom.com
On Twitter @maryjodales
AT ASCO 2017
Key clinical point:
Major finding: For all childhood cancer survivors, the 15-year cumulative incidence of severe health conditions decreased from 12.7% in those diagnosed in the 1970s, to 10.1% in the 1980s, and to 8.8% among those diagnosed in the 1990s (per 10 years: HR, 0.84 [95% CI, 0.80-0.89]).
Data source: An analysis of 23,600 participants in the Childhood Cancer Survivor Study.
Disclosures: The study was funded by the National Institutes of Health.
VIDEO: Childhood cancer survivors living longer with fewer severe health problems
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have been steadily declining, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study (CCSS), funded by the National Institutes of Health.
Watch our video interview with lead author Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, who reported the data at a press conference at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have been steadily declining, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study (CCSS), funded by the National Institutes of Health.
Watch our video interview with lead author Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, who reported the data at a press conference at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
CHICAGO – Severe health problems occurring 5 or more years after diagnosis of a childhood cancer have been steadily declining, based on an analysis of 23,600 participants in the Childhood Cancer Survivor Study (CCSS), funded by the National Institutes of Health.
Watch our video interview with lead author Todd M. Gibson, PhD, of St. Jude Children’s Research Hospital, Memphis, who reported the data at a press conference at the annual meeting of the American Society of Clinical Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mdales@frontlinemedcom.com
On Twitter @maryjodales
AT ASCO 2017
Early allo SCT advised for high-risk mantle cell lymphoma
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
mdales@frontlinemedcom.com
On Twitter @maryjodales
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
mdales@frontlinemedcom.com
On Twitter @maryjodales
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM ASCO 2017 ANNUAL MEETING
Key clinical point:
Major finding: Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (HR, 0.1; 95% CI, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Data source: A retrospective study of all 29 patients who were treated with an allo stem cell transplant for mantle cell lymphoma at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016.
Disclosures: Dr. Kobrinski had no relationships to disclose.
Citation: Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558.
ALC/AMC prognostic in mantle cell lymphoma
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
mdales@frontlinemedcom.com
On Twitter @maryjodales
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
mdales@frontlinemedcom.com
On Twitter @maryjodales
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
mdales@frontlinemedcom.com
On Twitter @maryjodales
IN CONJUNCTION WITH ASCO 2017
Key clinical point:
Major finding: The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Data source: A retrospective review study of 96 patients.
Disclosures: Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Citation: Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
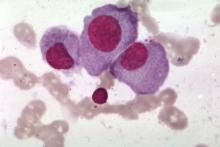
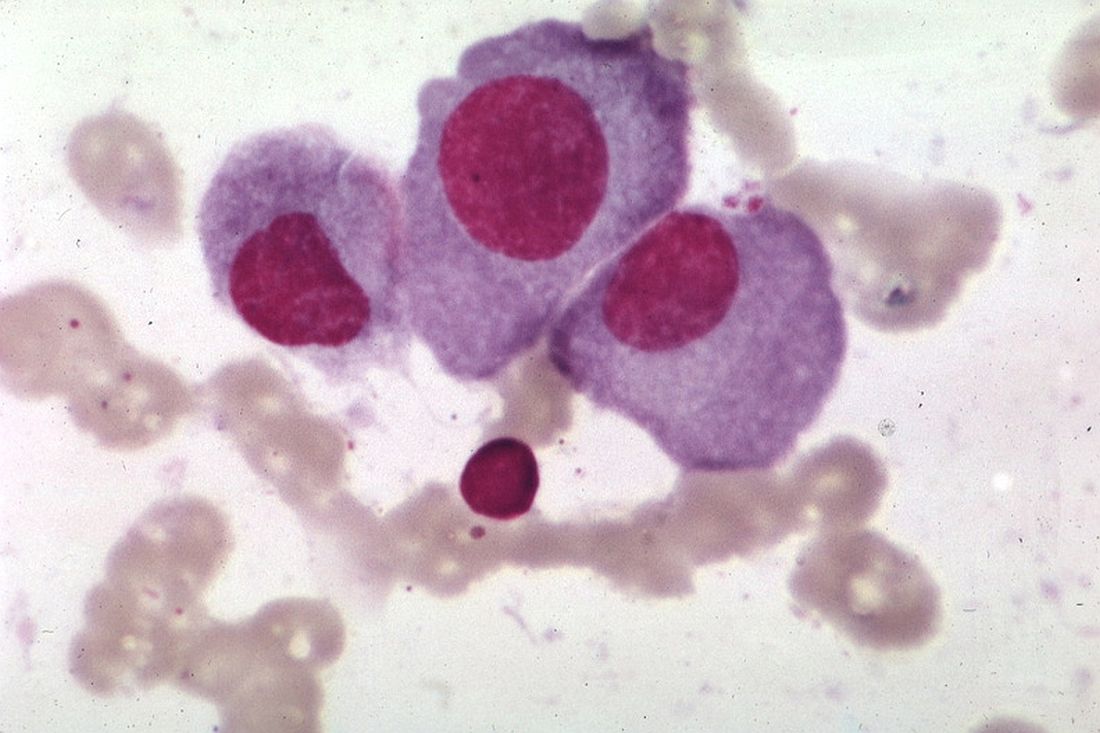
Smoldering myeloma progressed more rapidly in patients with elevated BMIs
An elevated body mass index appears to be a risk factor for progression of smoldering multiple myeloma, according to Wilson I. Gonsalves, MD, and his colleagues at Mayo Clinic, Rochester, Minn.
The findings, based on median follow up data of 106 months from 306 patients diagnosed with smoldering multiple myeloma from 2000-2010 at the Mayo Clinic, need to be confirmed in larger studies. Nevertheless, the results imply that patient weight is a potentially modifiable risk factor for progression from smoldering disease to multiple myeloma, Dr. Gonsalves and his colleagues wrote.
At initial evaluation, 28% of patients had myeloma defining events, such as a serum free light chain ratio greater than 100 or over 60% clonal bone marrow plasma cells. Myeloma defining events were present in 17% of patients with normal BMIs and 33% of patients with elevated BMIs, a statistically significant difference (P = .011).
When the analysis was limited to the 187 patients without myeloma-defining events at initial evaluation, the 2-year rate of progression to symptomatic multiple myeloma was 15% in those with a normal BMI and 33% in those with an elevated BMI (P = .013).
In a multivariable model, only elevated BMI (P = .004) and increasing clonal bone marrow plasma cells (P = .001) were statistically significant in predicting 2-year progression to multiple myeloma.
At last follow-up, 66% of patients had progressed to symptomatic multiple myeloma.
Dr. Gonsalves had no relationships to disclose.
The impact of body mass index on the risk of early progression of smoldering multiple myeloma to symptomatic myeloma. 2017 ASCO annual meeting. Abstract No: 8032.
mdales@frontlinemedcom.com
On Twitter @maryjodales
An elevated body mass index appears to be a risk factor for progression of smoldering multiple myeloma, according to Wilson I. Gonsalves, MD, and his colleagues at Mayo Clinic, Rochester, Minn.
The findings, based on median follow up data of 106 months from 306 patients diagnosed with smoldering multiple myeloma from 2000-2010 at the Mayo Clinic, need to be confirmed in larger studies. Nevertheless, the results imply that patient weight is a potentially modifiable risk factor for progression from smoldering disease to multiple myeloma, Dr. Gonsalves and his colleagues wrote.
At initial evaluation, 28% of patients had myeloma defining events, such as a serum free light chain ratio greater than 100 or over 60% clonal bone marrow plasma cells. Myeloma defining events were present in 17% of patients with normal BMIs and 33% of patients with elevated BMIs, a statistically significant difference (P = .011).
When the analysis was limited to the 187 patients without myeloma-defining events at initial evaluation, the 2-year rate of progression to symptomatic multiple myeloma was 15% in those with a normal BMI and 33% in those with an elevated BMI (P = .013).
In a multivariable model, only elevated BMI (P = .004) and increasing clonal bone marrow plasma cells (P = .001) were statistically significant in predicting 2-year progression to multiple myeloma.
At last follow-up, 66% of patients had progressed to symptomatic multiple myeloma.
Dr. Gonsalves had no relationships to disclose.
The impact of body mass index on the risk of early progression of smoldering multiple myeloma to symptomatic myeloma. 2017 ASCO annual meeting. Abstract No: 8032.
mdales@frontlinemedcom.com
On Twitter @maryjodales
An elevated body mass index appears to be a risk factor for progression of smoldering multiple myeloma, according to Wilson I. Gonsalves, MD, and his colleagues at Mayo Clinic, Rochester, Minn.
The findings, based on median follow up data of 106 months from 306 patients diagnosed with smoldering multiple myeloma from 2000-2010 at the Mayo Clinic, need to be confirmed in larger studies. Nevertheless, the results imply that patient weight is a potentially modifiable risk factor for progression from smoldering disease to multiple myeloma, Dr. Gonsalves and his colleagues wrote.
At initial evaluation, 28% of patients had myeloma defining events, such as a serum free light chain ratio greater than 100 or over 60% clonal bone marrow plasma cells. Myeloma defining events were present in 17% of patients with normal BMIs and 33% of patients with elevated BMIs, a statistically significant difference (P = .011).
When the analysis was limited to the 187 patients without myeloma-defining events at initial evaluation, the 2-year rate of progression to symptomatic multiple myeloma was 15% in those with a normal BMI and 33% in those with an elevated BMI (P = .013).
In a multivariable model, only elevated BMI (P = .004) and increasing clonal bone marrow plasma cells (P = .001) were statistically significant in predicting 2-year progression to multiple myeloma.
At last follow-up, 66% of patients had progressed to symptomatic multiple myeloma.
Dr. Gonsalves had no relationships to disclose.
The impact of body mass index on the risk of early progression of smoldering multiple myeloma to symptomatic myeloma. 2017 ASCO annual meeting. Abstract No: 8032.
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM ASCO 2017
Key clinical point:
Major finding: The 2-year rate of progression from smoldering disease to symptomatic multiple myeloma was 16% in patients with a normal BMI and 42% in patients with an elevated BMI (P less than 0.0001).
Data source: Median follow up data of 106 months from 306 patients diagnosed with smoldering multiple myeloma during 2000-2010 at the Mayo Clinic.
Disclosures: Dr. Gonsalves had no relationships to disclose.
Citation: The impact of body mass index on the risk of early progression of smoldering multiple myeloma to symptomatic myeloma. 2017 ASCO annual meeting. Abstract No: 8032.
Myeloma patients who get solid tumor cancers do as well as other cancer patients
With improved treatment, patients with multiple myeloma are surviving long enough to develop other cancers, Jorge J. Castillo, MD, and Adam J. Olszewski, MD, reported in a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The good news is that myeloma patients, when diagnosed with a subsequent solid tumor, are just as likely to respond to treatment and do just as well as patients without myeloma, according to Dr. Castillo of Dana-Farber Cancer Institute, Boston, and Dr. Olszewski of Alpert Medical School of Brown University, Providence, R.I.
They based their conclusion on Surveillance, Epidemiology, and End Results (SEER) data for patients diagnosed with six common cancers from 2004-2013.
“Among them, we identified [nearly 1,300] myeloma survivors, and we matched each to 50 randomly sampled controls with the same cancer by age, sex, race, and year of diagnosis. We then compared [cancer specific survival], cumulative incidence function (CIF) for death from the non-myeloma index cancer, and whether patients had surgery for non-metastastic, stage-matched tumors only,” the researchers wrote in their abstract.
They did analyses for breast, lung, prostate, colorectal, melanoma, and bladder cancers. The median time from diagnosis of myeloma to diagnosis of the second ranged from 35 months (bladder [133 myeloma patients] and lung [286 myeloma patients] cancers) to 50 months (melanoma [140 myeloma patients]). The median time after myeloma diagnosis was 40 months for those patients who developed breast, prostate, or colorectal cancers.
In the comparisons, myeloma survivors were significantly older (P less than .001) than patients initially diagnosed with the same respective cancers. In the case-control analysis, breast (P = .002) and lung cancers (P = .003) were more often diagnosed at an early stage among myeloma survivors.
The hazard ratio (HR) for cancer-specific survival for 189 myeloma patients diagnosed with breast cancer as compared to other breast cancer patients, for example, was 0.99, 95% confidence interval (CI) 0.61-1.61. The HR for the cumulative incidence function of cancer death was 0.82, 95% CI 0.50-1.35.
Myeloma patients were no less likely than were case-control subjects to have surgery for their cancers, with the exception of the 330 myeloma patients who developed prostate cancer (odds ratio, 0.59, 95% CI, 0.44-0.81).
Cancer-specific survival significantly differed (P less than .05) only for lung cancer, and was better among the 286 myeloma patients with lung cancer even when stratified by stage (HR 0.64, 95% CI 0.54-0.75). For cumulative incidence function of cancer death for lung cancer, the hazard ratio was 0.52 (95% CI 0.44-0.61). Better outcomes in lung cancer are not fully explained by earlier detection, suggesting a biological difference, the researchers reported.
Cumulative incidence function of cancer death was significantly lower for myeloma patients with lung and colorectal cancers.
Dr. Castillo disclosed honoraria from Celgene and Janssen; a consulting or advisory role with Biogen, Otsuka, and Pharmacyclics; and institutional research funding from Abbvie, Gilead Sciences, Millennium, and Pharmacyclics. Dr. Olszewski disclosed institutional research funding from Genentech, Incyte, and TG Therapeutics.
Citation: Outcomes of secondary cancers among myeloma survivors. 2017 ASCO annual meeting. Abstract No. 8043.
mdales@frontlinemedcom.com
On Twitter @maryjodales
With improved treatment, patients with multiple myeloma are surviving long enough to develop other cancers, Jorge J. Castillo, MD, and Adam J. Olszewski, MD, reported in a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The good news is that myeloma patients, when diagnosed with a subsequent solid tumor, are just as likely to respond to treatment and do just as well as patients without myeloma, according to Dr. Castillo of Dana-Farber Cancer Institute, Boston, and Dr. Olszewski of Alpert Medical School of Brown University, Providence, R.I.
They based their conclusion on Surveillance, Epidemiology, and End Results (SEER) data for patients diagnosed with six common cancers from 2004-2013.
“Among them, we identified [nearly 1,300] myeloma survivors, and we matched each to 50 randomly sampled controls with the same cancer by age, sex, race, and year of diagnosis. We then compared [cancer specific survival], cumulative incidence function (CIF) for death from the non-myeloma index cancer, and whether patients had surgery for non-metastastic, stage-matched tumors only,” the researchers wrote in their abstract.
They did analyses for breast, lung, prostate, colorectal, melanoma, and bladder cancers. The median time from diagnosis of myeloma to diagnosis of the second ranged from 35 months (bladder [133 myeloma patients] and lung [286 myeloma patients] cancers) to 50 months (melanoma [140 myeloma patients]). The median time after myeloma diagnosis was 40 months for those patients who developed breast, prostate, or colorectal cancers.
In the comparisons, myeloma survivors were significantly older (P less than .001) than patients initially diagnosed with the same respective cancers. In the case-control analysis, breast (P = .002) and lung cancers (P = .003) were more often diagnosed at an early stage among myeloma survivors.
The hazard ratio (HR) for cancer-specific survival for 189 myeloma patients diagnosed with breast cancer as compared to other breast cancer patients, for example, was 0.99, 95% confidence interval (CI) 0.61-1.61. The HR for the cumulative incidence function of cancer death was 0.82, 95% CI 0.50-1.35.
Myeloma patients were no less likely than were case-control subjects to have surgery for their cancers, with the exception of the 330 myeloma patients who developed prostate cancer (odds ratio, 0.59, 95% CI, 0.44-0.81).
Cancer-specific survival significantly differed (P less than .05) only for lung cancer, and was better among the 286 myeloma patients with lung cancer even when stratified by stage (HR 0.64, 95% CI 0.54-0.75). For cumulative incidence function of cancer death for lung cancer, the hazard ratio was 0.52 (95% CI 0.44-0.61). Better outcomes in lung cancer are not fully explained by earlier detection, suggesting a biological difference, the researchers reported.
Cumulative incidence function of cancer death was significantly lower for myeloma patients with lung and colorectal cancers.
Dr. Castillo disclosed honoraria from Celgene and Janssen; a consulting or advisory role with Biogen, Otsuka, and Pharmacyclics; and institutional research funding from Abbvie, Gilead Sciences, Millennium, and Pharmacyclics. Dr. Olszewski disclosed institutional research funding from Genentech, Incyte, and TG Therapeutics.
Citation: Outcomes of secondary cancers among myeloma survivors. 2017 ASCO annual meeting. Abstract No. 8043.
mdales@frontlinemedcom.com
On Twitter @maryjodales
With improved treatment, patients with multiple myeloma are surviving long enough to develop other cancers, Jorge J. Castillo, MD, and Adam J. Olszewski, MD, reported in a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The good news is that myeloma patients, when diagnosed with a subsequent solid tumor, are just as likely to respond to treatment and do just as well as patients without myeloma, according to Dr. Castillo of Dana-Farber Cancer Institute, Boston, and Dr. Olszewski of Alpert Medical School of Brown University, Providence, R.I.
They based their conclusion on Surveillance, Epidemiology, and End Results (SEER) data for patients diagnosed with six common cancers from 2004-2013.
“Among them, we identified [nearly 1,300] myeloma survivors, and we matched each to 50 randomly sampled controls with the same cancer by age, sex, race, and year of diagnosis. We then compared [cancer specific survival], cumulative incidence function (CIF) for death from the non-myeloma index cancer, and whether patients had surgery for non-metastastic, stage-matched tumors only,” the researchers wrote in their abstract.
They did analyses for breast, lung, prostate, colorectal, melanoma, and bladder cancers. The median time from diagnosis of myeloma to diagnosis of the second ranged from 35 months (bladder [133 myeloma patients] and lung [286 myeloma patients] cancers) to 50 months (melanoma [140 myeloma patients]). The median time after myeloma diagnosis was 40 months for those patients who developed breast, prostate, or colorectal cancers.
In the comparisons, myeloma survivors were significantly older (P less than .001) than patients initially diagnosed with the same respective cancers. In the case-control analysis, breast (P = .002) and lung cancers (P = .003) were more often diagnosed at an early stage among myeloma survivors.
The hazard ratio (HR) for cancer-specific survival for 189 myeloma patients diagnosed with breast cancer as compared to other breast cancer patients, for example, was 0.99, 95% confidence interval (CI) 0.61-1.61. The HR for the cumulative incidence function of cancer death was 0.82, 95% CI 0.50-1.35.
Myeloma patients were no less likely than were case-control subjects to have surgery for their cancers, with the exception of the 330 myeloma patients who developed prostate cancer (odds ratio, 0.59, 95% CI, 0.44-0.81).
Cancer-specific survival significantly differed (P less than .05) only for lung cancer, and was better among the 286 myeloma patients with lung cancer even when stratified by stage (HR 0.64, 95% CI 0.54-0.75). For cumulative incidence function of cancer death for lung cancer, the hazard ratio was 0.52 (95% CI 0.44-0.61). Better outcomes in lung cancer are not fully explained by earlier detection, suggesting a biological difference, the researchers reported.
Cumulative incidence function of cancer death was significantly lower for myeloma patients with lung and colorectal cancers.
Dr. Castillo disclosed honoraria from Celgene and Janssen; a consulting or advisory role with Biogen, Otsuka, and Pharmacyclics; and institutional research funding from Abbvie, Gilead Sciences, Millennium, and Pharmacyclics. Dr. Olszewski disclosed institutional research funding from Genentech, Incyte, and TG Therapeutics.
Citation: Outcomes of secondary cancers among myeloma survivors. 2017 ASCO annual meeting. Abstract No. 8043.
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: Cancer-specific survival significantly differed (P less than .05) only for lung cancer, and was better among the 286 myeloma patients with lung cancer even when stratified by stage (HR, 0.64, 95% CI 0.54-0.75).
Data source: Surveillance, Epidemiology, and End Results (SEER) data for patients diagnosed with six common cancers from 2004-2013.
Disclosures: Dr. Castillo disclosed honoraria from Celgene and Janssen; a consulting or advisory role with Biogen, Otsuka, and Pharmacyclics; and institutional research funding from Abbvie, Gilead Sciences, Millennium, and Pharmacyclics. Dr. Olszewski disclosed institutional research funding from Genentech, Incyte, and TG Therapeutics.
Citation: Outcomes of secondary cancers among myeloma survivors. 2017 ASCO annual meeting. Abstract No. 8043.
Lenalidomide maintenance boosted depth of response in myeloma patients
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: 48% of patients who had minimal residual disease before maintenance therapy and had a second evaluation for MRD after at least 1 year of lenalidomide therapy became MRD negative.
Data source: A 3-year study of 316 patients who were evaluable before maintenance therapy in the EMN02/HO95 trial.
Disclosures: Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
Daratumumab, elotuzumab eyed for initial treatment of myeloma
The emerging role for immunotherapies as an essential component of multiple myeloma therapy is examined in a review article in Leukemia by Cyrille Touzeau, MD, and his colleagues.
The reviewers detail research examining a string of monoclonal antibodies that fell short in earlier evaluations. They focus on the two approved agents that target CD38 (daratumumab) and SLAMF7 (elotuzumab) and have succeeded in combination therapies for patients with relapsed myeloma. These two antibodies, and other immunotherapy possibilities in the pipeline, are expected to have a strong impact on treatment modalities and outcomes in patients with multiple myeloma, including transplant eligible and elderly patients, Dr. Touzeau, of the service d’hématologie clinique, Nantes, France, and his fellow researchers wrote.
In two phase III randomized studies, ELO 1 (NCT01891643) and ELOQUENT 1 (NCT01335399), previously untreated myeloma patients are receiving lenalidomide/dexamethasone with or without elotuzumab.
In another ongoing trial, elotuzumab is being evaluated in combination with the anti-KIR antibody lirilumab and the anti-CD137 antibody urelumab (NCT02252263). Elotuzumab also is being studied in combination with lenalidomide as maintenance after high-dose therapy (NCT02420860).
Additionally, elotuzumab in combination with pomalidomide-dexamethasone is being examined for relapsed myeloma in an ongoing phase II randomized trial (NCT02654132). SLAMF7 is also being evaluated as a target for immunoconjugate therapy, with an ongoing trial of an auristatin E conjugate (ABBV-838) in patients with relapsed or refractory disease (NCT02462525), the reviewers note.
Daratumumab is being examined in combination with VTD [bortezomib (Velcade)/thalidomide/dexamethasone] as induction therapy and for its role as maintenance after high-dose therapy, among previously untreated transplant-eligible myeloma patients in the phase III randomized Cassiopeia study (NCT02541383).
In patients not eligible for transplant, the phase III randomized trial, MAIA, is evaluating the addition of daratumumab to lenalidomide-dexamethasone (NCT02252172). In high-risk smoldering myeloma, daratumumab is being evaluated in the phase III randomized CENTAURUS trial (NCT02316106). PAVO is a phase 1b study of the subcutaneous administration of daratumumab (NCT02519452). Preliminary results determined that the fixed subcutaneous dose of 1800 mg was consistent with the 16 mg/kg IV dose in terms of pharmacokinetics.
Dr. Touzeau declared no conflicts of interest. His coauthors participate in advisory boards and receive honoraria from several drug makers including the makers of immunotherapies.
mdales@frontlinemedcom.com
On Twitter @maryjodales
The emerging role for immunotherapies as an essential component of multiple myeloma therapy is examined in a review article in Leukemia by Cyrille Touzeau, MD, and his colleagues.
The reviewers detail research examining a string of monoclonal antibodies that fell short in earlier evaluations. They focus on the two approved agents that target CD38 (daratumumab) and SLAMF7 (elotuzumab) and have succeeded in combination therapies for patients with relapsed myeloma. These two antibodies, and other immunotherapy possibilities in the pipeline, are expected to have a strong impact on treatment modalities and outcomes in patients with multiple myeloma, including transplant eligible and elderly patients, Dr. Touzeau, of the service d’hématologie clinique, Nantes, France, and his fellow researchers wrote.
In two phase III randomized studies, ELO 1 (NCT01891643) and ELOQUENT 1 (NCT01335399), previously untreated myeloma patients are receiving lenalidomide/dexamethasone with or without elotuzumab.
In another ongoing trial, elotuzumab is being evaluated in combination with the anti-KIR antibody lirilumab and the anti-CD137 antibody urelumab (NCT02252263). Elotuzumab also is being studied in combination with lenalidomide as maintenance after high-dose therapy (NCT02420860).
Additionally, elotuzumab in combination with pomalidomide-dexamethasone is being examined for relapsed myeloma in an ongoing phase II randomized trial (NCT02654132). SLAMF7 is also being evaluated as a target for immunoconjugate therapy, with an ongoing trial of an auristatin E conjugate (ABBV-838) in patients with relapsed or refractory disease (NCT02462525), the reviewers note.
Daratumumab is being examined in combination with VTD [bortezomib (Velcade)/thalidomide/dexamethasone] as induction therapy and for its role as maintenance after high-dose therapy, among previously untreated transplant-eligible myeloma patients in the phase III randomized Cassiopeia study (NCT02541383).
In patients not eligible for transplant, the phase III randomized trial, MAIA, is evaluating the addition of daratumumab to lenalidomide-dexamethasone (NCT02252172). In high-risk smoldering myeloma, daratumumab is being evaluated in the phase III randomized CENTAURUS trial (NCT02316106). PAVO is a phase 1b study of the subcutaneous administration of daratumumab (NCT02519452). Preliminary results determined that the fixed subcutaneous dose of 1800 mg was consistent with the 16 mg/kg IV dose in terms of pharmacokinetics.
Dr. Touzeau declared no conflicts of interest. His coauthors participate in advisory boards and receive honoraria from several drug makers including the makers of immunotherapies.
mdales@frontlinemedcom.com
On Twitter @maryjodales
The emerging role for immunotherapies as an essential component of multiple myeloma therapy is examined in a review article in Leukemia by Cyrille Touzeau, MD, and his colleagues.
The reviewers detail research examining a string of monoclonal antibodies that fell short in earlier evaluations. They focus on the two approved agents that target CD38 (daratumumab) and SLAMF7 (elotuzumab) and have succeeded in combination therapies for patients with relapsed myeloma. These two antibodies, and other immunotherapy possibilities in the pipeline, are expected to have a strong impact on treatment modalities and outcomes in patients with multiple myeloma, including transplant eligible and elderly patients, Dr. Touzeau, of the service d’hématologie clinique, Nantes, France, and his fellow researchers wrote.
In two phase III randomized studies, ELO 1 (NCT01891643) and ELOQUENT 1 (NCT01335399), previously untreated myeloma patients are receiving lenalidomide/dexamethasone with or without elotuzumab.
In another ongoing trial, elotuzumab is being evaluated in combination with the anti-KIR antibody lirilumab and the anti-CD137 antibody urelumab (NCT02252263). Elotuzumab also is being studied in combination with lenalidomide as maintenance after high-dose therapy (NCT02420860).
Additionally, elotuzumab in combination with pomalidomide-dexamethasone is being examined for relapsed myeloma in an ongoing phase II randomized trial (NCT02654132). SLAMF7 is also being evaluated as a target for immunoconjugate therapy, with an ongoing trial of an auristatin E conjugate (ABBV-838) in patients with relapsed or refractory disease (NCT02462525), the reviewers note.
Daratumumab is being examined in combination with VTD [bortezomib (Velcade)/thalidomide/dexamethasone] as induction therapy and for its role as maintenance after high-dose therapy, among previously untreated transplant-eligible myeloma patients in the phase III randomized Cassiopeia study (NCT02541383).
In patients not eligible for transplant, the phase III randomized trial, MAIA, is evaluating the addition of daratumumab to lenalidomide-dexamethasone (NCT02252172). In high-risk smoldering myeloma, daratumumab is being evaluated in the phase III randomized CENTAURUS trial (NCT02316106). PAVO is a phase 1b study of the subcutaneous administration of daratumumab (NCT02519452). Preliminary results determined that the fixed subcutaneous dose of 1800 mg was consistent with the 16 mg/kg IV dose in terms of pharmacokinetics.
Dr. Touzeau declared no conflicts of interest. His coauthors participate in advisory boards and receive honoraria from several drug makers including the makers of immunotherapies.
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM LEUKEMIA
Guideline endorses doublet therapy after pancreatic cancer surgery in chemo-naive patients
A recommendation on postop adjuvant chemotherapy has been updated in the Potentially Curable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline, according to an article published online on April 11 in the Journal of Clinical Oncology.
In the absence of medical or surgical contraindications, all patients who have resected pancreatic cancer and did not receive preoperative therapy should be offered 6 months of adjuvant chemotherapy, according to the new recommendation. “The doublet regimen of gemcitabine and capecitabine is preferred in the absence of concerns for toxicity or tolerance; alternatively, monotherapy with gemcitabine or fluorouracil plus folinic acid can be offered. Adjuvant treatment should be initiated within 8 weeks of surgical resection, assuming complete recovery,” Alok A. Khorana, MD, of the Cleveland Clinic, and members of the guideline committee wrote.
The recommendation was based on results of the ESPAC-4 study, a multicenter, international, open-label randomized controlled phase III trial (Lancet. 2017;389:1011-24). ESPAC-4 compared adjuvant combination chemotherapy of gemcitabine and capecitabine with gemcitabine monotherapy in 730 evaluable patients with resected pancreatic ductal adenocarcinoma.
Median overall survival was 28 months (95% confidence interval, 23.5-31.5 months) in the doublet arm and 25.5 months (95% CI, 22.7 to 27.9 months) for gemcitabine alone (hazard ratio, 0.82; 95% CI, 0.68-0.98; P = .032). Grade 3 and 4 adverse events were similar in both arms, although higher rates of hand-foot syndrome and diarrhea occurred in patients randomly assigned to the doublet arm.
The remaining recommendations from the original 2016 ASCO guideline are unchanged.
The revised guideline is available at this link.
mdales@frontlinemedcom.com
On Twitter @maryjodales
A recommendation on postop adjuvant chemotherapy has been updated in the Potentially Curable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline, according to an article published online on April 11 in the Journal of Clinical Oncology.
In the absence of medical or surgical contraindications, all patients who have resected pancreatic cancer and did not receive preoperative therapy should be offered 6 months of adjuvant chemotherapy, according to the new recommendation. “The doublet regimen of gemcitabine and capecitabine is preferred in the absence of concerns for toxicity or tolerance; alternatively, monotherapy with gemcitabine or fluorouracil plus folinic acid can be offered. Adjuvant treatment should be initiated within 8 weeks of surgical resection, assuming complete recovery,” Alok A. Khorana, MD, of the Cleveland Clinic, and members of the guideline committee wrote.
The recommendation was based on results of the ESPAC-4 study, a multicenter, international, open-label randomized controlled phase III trial (Lancet. 2017;389:1011-24). ESPAC-4 compared adjuvant combination chemotherapy of gemcitabine and capecitabine with gemcitabine monotherapy in 730 evaluable patients with resected pancreatic ductal adenocarcinoma.
Median overall survival was 28 months (95% confidence interval, 23.5-31.5 months) in the doublet arm and 25.5 months (95% CI, 22.7 to 27.9 months) for gemcitabine alone (hazard ratio, 0.82; 95% CI, 0.68-0.98; P = .032). Grade 3 and 4 adverse events were similar in both arms, although higher rates of hand-foot syndrome and diarrhea occurred in patients randomly assigned to the doublet arm.
The remaining recommendations from the original 2016 ASCO guideline are unchanged.
The revised guideline is available at this link.
mdales@frontlinemedcom.com
On Twitter @maryjodales
A recommendation on postop adjuvant chemotherapy has been updated in the Potentially Curable Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline, according to an article published online on April 11 in the Journal of Clinical Oncology.
In the absence of medical or surgical contraindications, all patients who have resected pancreatic cancer and did not receive preoperative therapy should be offered 6 months of adjuvant chemotherapy, according to the new recommendation. “The doublet regimen of gemcitabine and capecitabine is preferred in the absence of concerns for toxicity or tolerance; alternatively, monotherapy with gemcitabine or fluorouracil plus folinic acid can be offered. Adjuvant treatment should be initiated within 8 weeks of surgical resection, assuming complete recovery,” Alok A. Khorana, MD, of the Cleveland Clinic, and members of the guideline committee wrote.
The recommendation was based on results of the ESPAC-4 study, a multicenter, international, open-label randomized controlled phase III trial (Lancet. 2017;389:1011-24). ESPAC-4 compared adjuvant combination chemotherapy of gemcitabine and capecitabine with gemcitabine monotherapy in 730 evaluable patients with resected pancreatic ductal adenocarcinoma.
Median overall survival was 28 months (95% confidence interval, 23.5-31.5 months) in the doublet arm and 25.5 months (95% CI, 22.7 to 27.9 months) for gemcitabine alone (hazard ratio, 0.82; 95% CI, 0.68-0.98; P = .032). Grade 3 and 4 adverse events were similar in both arms, although higher rates of hand-foot syndrome and diarrhea occurred in patients randomly assigned to the doublet arm.
The remaining recommendations from the original 2016 ASCO guideline are unchanged.
The revised guideline is available at this link.
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM THE JOURNAL OF CLINICAL ONCOLOGY