User login
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
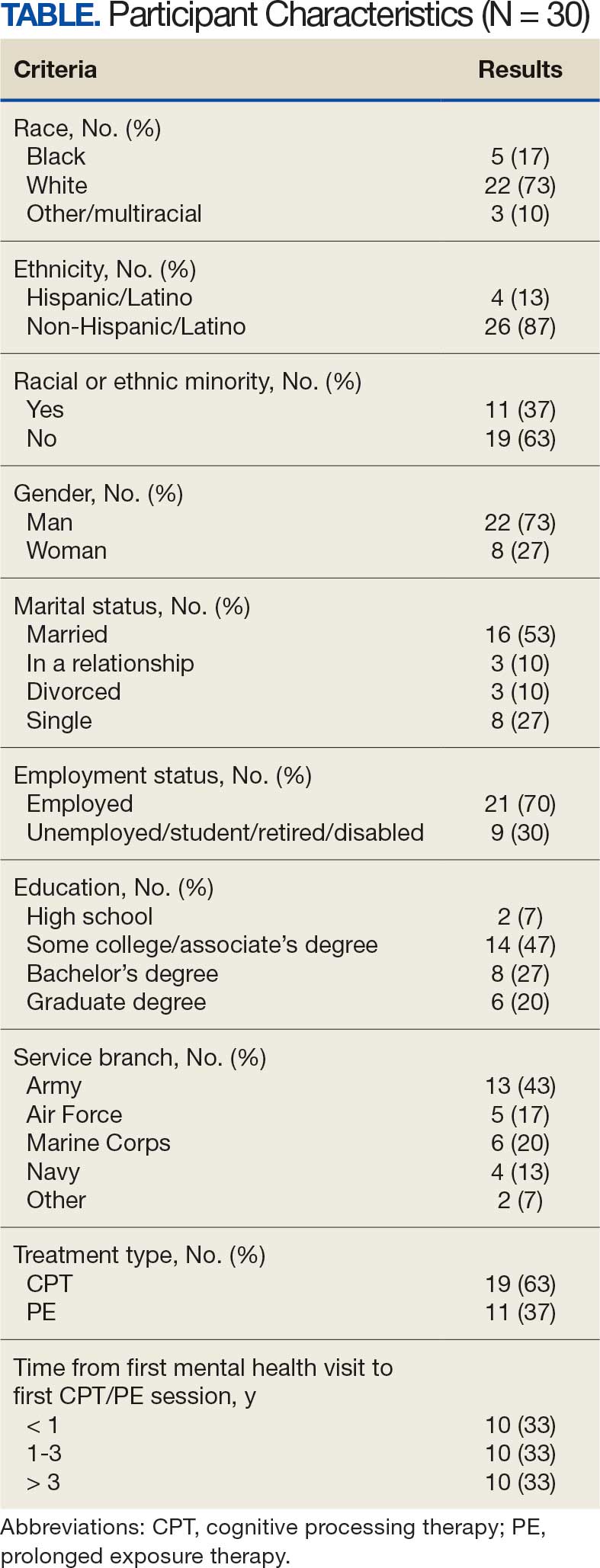
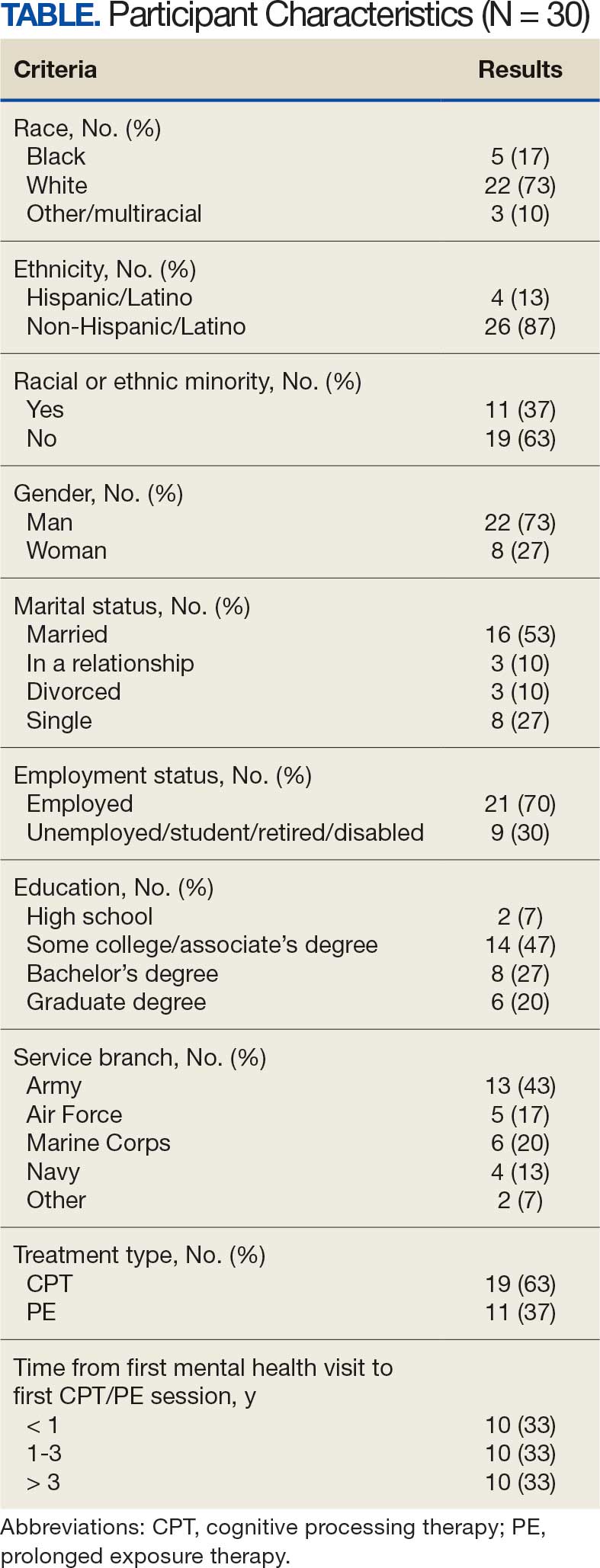
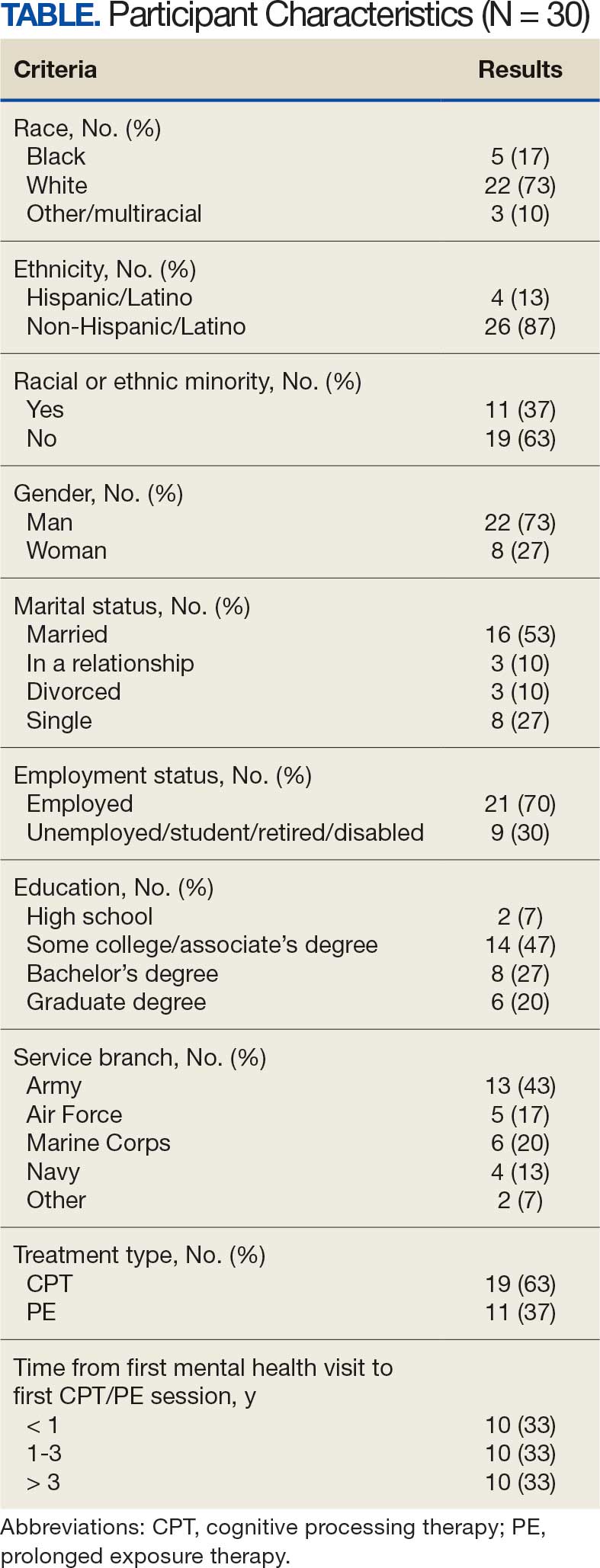
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Examining Moral Injury in Legal-Involved Veterans: Psychometric Properties of the Moral Injury Events Scale
Examining Moral Injury in Legal-Involved Veterans: Psychometric Properties of the Moral Injury Events Scale
Following exposure to potentially morally injurious events (PMIEs), some individuals may experience moral injury, which represents negative psychological, social, behavioral, and occasionally spiritual impacts.1 The consequences of PMIE exposure and moral injury are well documented. Individuals may begin to question the goodness and trustworthiness of oneself, others, or the world.1 Examples of other sequelae include guilt, demoralization, spiritual pain, loss of trust in the self or others, and difficulties with forgiveness.2-6 In addition, prior studies have found that moral injury is associated with an increased risk of suicidal thoughts and behaviors, posttraumatic stress disorder (PTSD) symptoms, spiritual distress, and interpersonal difficulties.7-11
Moral injury was first conceptualized in relation to combat trauma. However in recent years it has been examined in other groups such as health care practitioners, educators, refugees, and law enforcement personnel.12-17 Furthermore, there has been a recent call for the study of moral injury in other understudied groups. One such group is legal-involved individuals, defined as those who are currently involved or previously involved in the criminal justice system (ie, arrests, incarceration, parole, and probation).1,18-22
Many veterans are also involved with the legal system. Specifically, veterans currently comprise about 8% of the incarcerated US population, with an estimated > 180,000 veterans in prisons or jails and even more on parole or probation.23,24 Legal-involved veterans may be at heightened risk for homelessness, suicide, unemployment, and high prevalence rates of psychiatric diagnoses.25-28
Limited research has explored exposure to PMIEs as part of the legal process and the resulting expression of moral injury. The circumstances leading to incarceration, interactions with the US legal system, the environment of prison itself, and the subsequent challenges faced by legal-involved individuals after release all provide ample opportunity for PMIEs to occur.18 For example, engaging in a criminal act may represent a PMIE, particularly in violent offenses that involve harm to another individual. Moreover, the process of being convicted and charged with an offense may serve as a powerful reminder of the PMIE and tie this event to the individual’s identity and future. Furthermore, the physical and social environment of prison itself (eg, being surrounded by other offenders, witnessing the perpetration of violence, participating in violence for survival) presents a myriad of opportunities for PMIEs to occur.18
The consequences of PMIEs in the context of legal involvement may also have bearing on a touchstone of moral injury: changes in one’s schema of the self and world.4 At a societal level, legal-involved individuals are, by definition, deemed “guilty” and held culpable for their offense, which may reinforce a negative change in one’s view of self and the world.29 In line with identity theory, external negative appraisals about legal-involved individuals (eg, they are a danger to society, they cannot be trusted to do the right thing) may influence their self-perception.30 Furthermore, the affective characteristics often found in the context of moral injury (eg, guilt, shame, anger, contempt) may be exacerbated by legal involvement.29 Personal feelings of guilt and shame may be reinforced by receiving a verdict and sentence, as well as the negative perceptions of individuals around them (eg, disapproval from prior sources of social support). Additionally, feelings of betrayal and distrust towards the legal system may arise.
In sum, legal-involved veterans incur increased risk of moral injury due to the potential for exposure to PMIEs across multiple time points (eg, prior to military service, during military service, during arrest/sentencing, during imprisonment, and postincarceration). The stigma that accompanies legal involvement may limit access to treatment or a willingness to seek treatment for distress related to moral injury.29 Additionally, repeated exposure to PMIEs and resulting moral injury may compound over time, potentially exacerbating psychosocial functioning and increasing the risk for psychosocial stressors (eg, homelessness, unemployment) and mental health disorders (eg, depression, substance misuse).31
Although numerous measures of moral injury have been developed, most require that respondents consider a specific context (eg, military experiences).32 Therefore, study of legal-related moral injury requires adaptation of existing instruments to the legal context. The original and most commonly used scale of moral injury is the Moral Injury Events Scale (MIES).33 The MIES scales was originally developed to measure moral injury in military-related contexts but has since been adapted as a measure of exposure to context-specific PMIEs.34
Unfortunately, there are no validated measures for assessing legal-related moral injury. Such a gap in understanding is problematic, as it may impact measurement of the prevalence of PMIEs in both clinical and research settings for this at-risk population. The goal of this study was to conduct a psychometric evaluation of an adapted version of the MIES for legal-involved persons (MIES-LIP).
METHODS
A total of 177 veterans from the US Department of Veterans Affairs (VA) North Texas Health Care System were contacted for study enrollment between November 2020 and June 2021, yielding a final sample of 100 legal-involved veteran participants. Adults aged ≥ 18 years who were US military veterans and had ≥ 1 prior felony conviction resulting in incarceration were included. Participants were excluded if they had symptoms of psychosis that would preclude meaningful participation.
The study collected data on participants’ demographic and clinical characteristics using a semistructured survey instrument. Each participant completed an instructor-led questionnaire in a session that lasted about 1.5 hours. Participants who completed the visit in person received a $50 cash voucher for their time. Participants who were unable to meet with the study coordinator in person were able to complete the visit via telephone and received a $25 digital gift card. Of the total 100 participants, 79 participants completed the interview in person, and 21 completed by telephone. No significant differences were found in assessment measures between administration methods. Written informed consent was obtained during all in-person visits. For those completing via telephone, a waiver of written informed consent was obtained. This study was approved by the VA North Texas Health Care System’s Institutional Review Board.
Measures
The Moral Injury Events Scale (MIES) is a 9-item self-report measure that assesses exposure to PMIEs.33 Respondents rate their agreement with each item on a 6-point Likert scale (strongly disagree to strongly agree), with higher scores indicating greater moral injury. The MIES has a 2-factor structure: Factor 1 has 6 items on perceived transgressions and Factor 2 has 3 items on perceived betrayals.33
Creation of Legal-Involved Moral Injury Measure. To create the MIES-LIP, items and instructions from the MIES were modified to address moral injury in the context of legal involvement.33 Adaptations were finalized following consultation and approval by the authors of the original measure. Specifically, the instructions were changed to: “Please respond to these items based specifically in the context of your involvement with the legal system.” The instructions clarified that legal involvement could include experiences related to committing an offense, legal proceedings and sentencing, incarceration, or transitioning out of the legal system. This differs from the original measure, which focused on military experiences, with instructions stating: “Please respond to these items based specifically in the context of your military service (ie, events and experiences during enlistment, deployment, combat, etc).”
Other measures. The study collected data on demographic characteristics including sex, race and ethnicity, marital status, military service, combat experience, and legal involvement. PTSD symptom severity, based on the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), was assessed using the PTSD Checklist for DSM-5 (PCL-5).35,36 The PCL-5 is a 20-item self-report measure in which item scores are summed to create a total score. The PCL-5 has demonstrated strong psychometric properties, including good internal consistency, test-retest reliability convergent validity, and discriminant validity.37,38
Depressive symptom severity was measured using the Personal Health Questionnaire-9 (PHQ-9).39 The PHQ-9 is a 9-item self-report measure where item scores summed to create a total score. The PHQ-9 has demonstrated strong psychometric properties, including internal consistency and test-retest reliability.39
STATISTICAL METHODS
Descriptive statistics (mean and standard deviation for continuous variables; frequencies and percentages for categorical variables) were used to describe the study sample. Factor analysis was conducted to evaluate the psychometric properties of the MIES-LIP. Confirmatory factor analysis (CFA) was used to determine whether the MEIS-LIP had a similar factor structure to the MIES.40 Criteria for fit indices used for CFA include the Comparative Fit Index (CFI; values of > 0.95 suggest good fit), Tucker-Lewis index (TLI; values of > 0.95 suggest a good fit), root mean square error of approximation (RMSEA; values of ≥ 0.06 suggest good fit), and standardized root mean square residual (SRMR; values of ≥ 0.08 suggest good fit). With insufficient fit, subsequent exploratory factor analysis was conducted using maximum likelihood estimation with an Oblimin rotation. The Kaiser rule and a scree plot were considered when defining the factor structure. Reliability was evaluated using the McDonald omega coefficient test. Convergent validity was assessed through the association between adapted measures and other clinical measures (ie, PCL-5, PHQ-9). In addition, associations between the PCL-5 and PHQ-9 were examined as they related to the MIES and MIES-LIP.
RESULTS
Table 1 describes demographic characteristics of the study sample. Rates of potentially morally injurious experiences and the expression of moral injury in the legal context are presented in Table 2. Witnessing PMIEs while in the legal system was nearly ubiquitous, with > 90% of the sample endorsing this experience. More than half of the sample also endorsed engaging in morally injurious behavior by commission or omission, as well as experiencing betrayal while involved with the legal system.
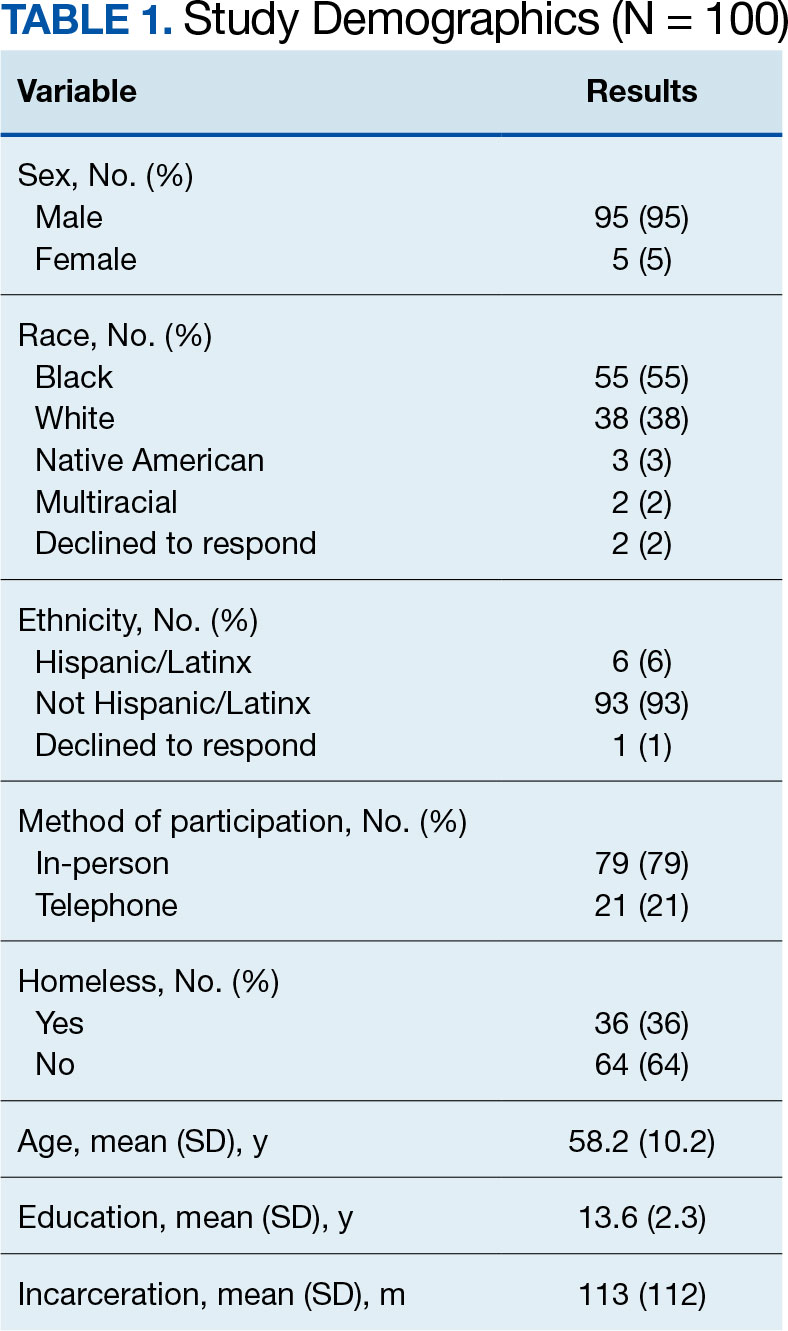
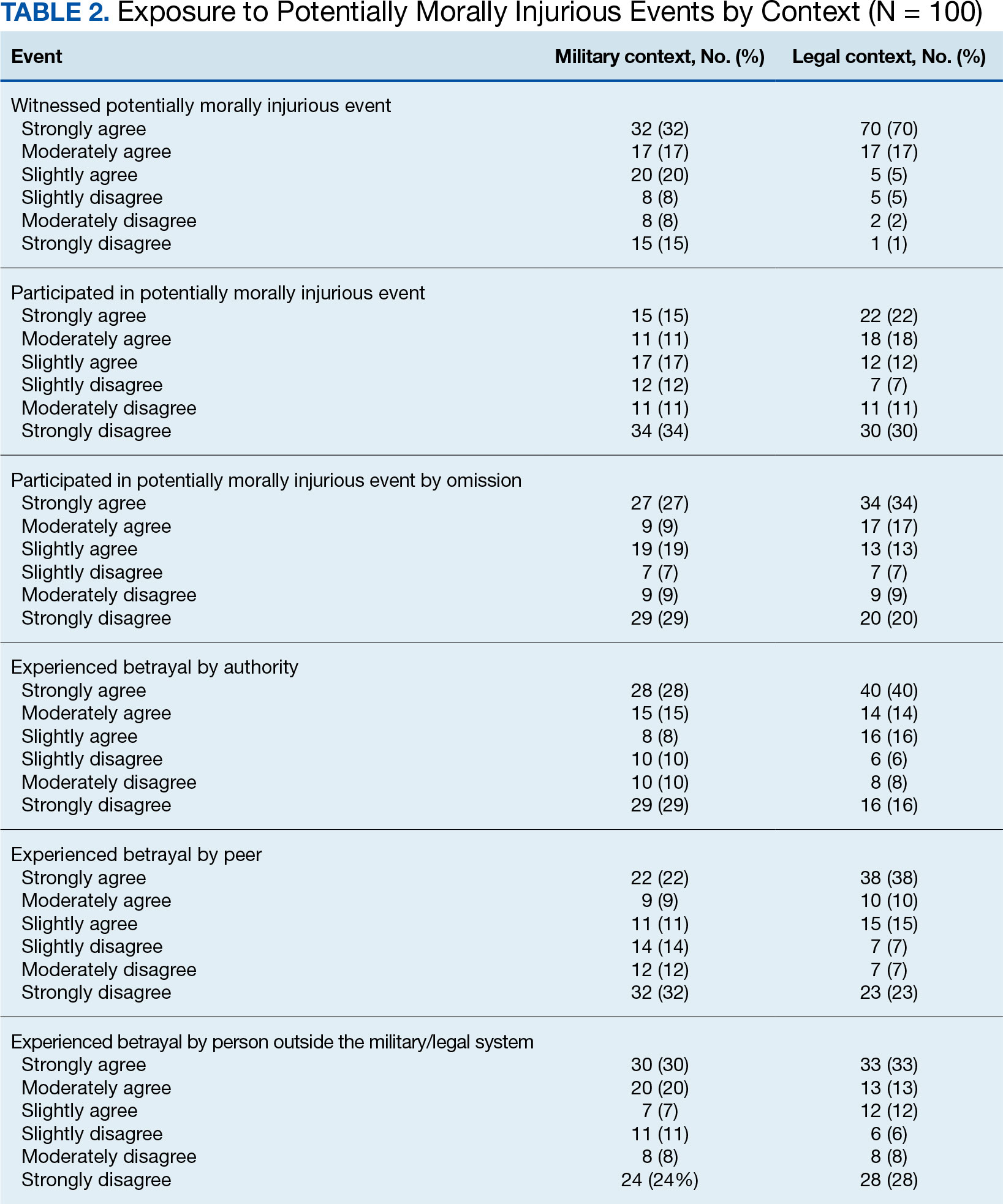
Factor Analysis
Confirmatory factor analysis (CFA) was utilized to test the factor structure of the adapted MIES-LIP in our sample compared to the published factor structures of the MIES.33 Results did not support the established factor structure. Analysis yielded unacceptable CFI (0.79), TLI (0.70), SRMR (0.14), and RMSEA (0.21). The unsatisfactory results of CFA warranted follow-up exploratory factor analysis (EFA) to examine the factor structure of the moral injury scales in this sample.
EFA of MIES-LIP
The factor structure of the MIES-LIP was examined using EFA. The factorability of the data was examined using the Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO value = 0.75) and Bartlett Test of Sphericity (X2 = 525.41; P < .001), both of which suggested that the data were appropriate for factor analysis. The number of factors to retain was selected based on the Kaiser criterion.41 After extraction, an Oblimin rotation was applied, given that we expected factors to be correlated. A 2-factor solution was found, explaining 65.76% of the common variance. All 9 items were retained as they had factor loadings > 0.30. Factor 1, comprised self-directed moral injury questions (3-6). Factor 2 comprised other directed moral injury questions (1, 2, 7-9) (Table 3). The factor correlation coefficient between Factor 1 and Factor 2 was 0.34, which supports utilizing an oblique rotation.
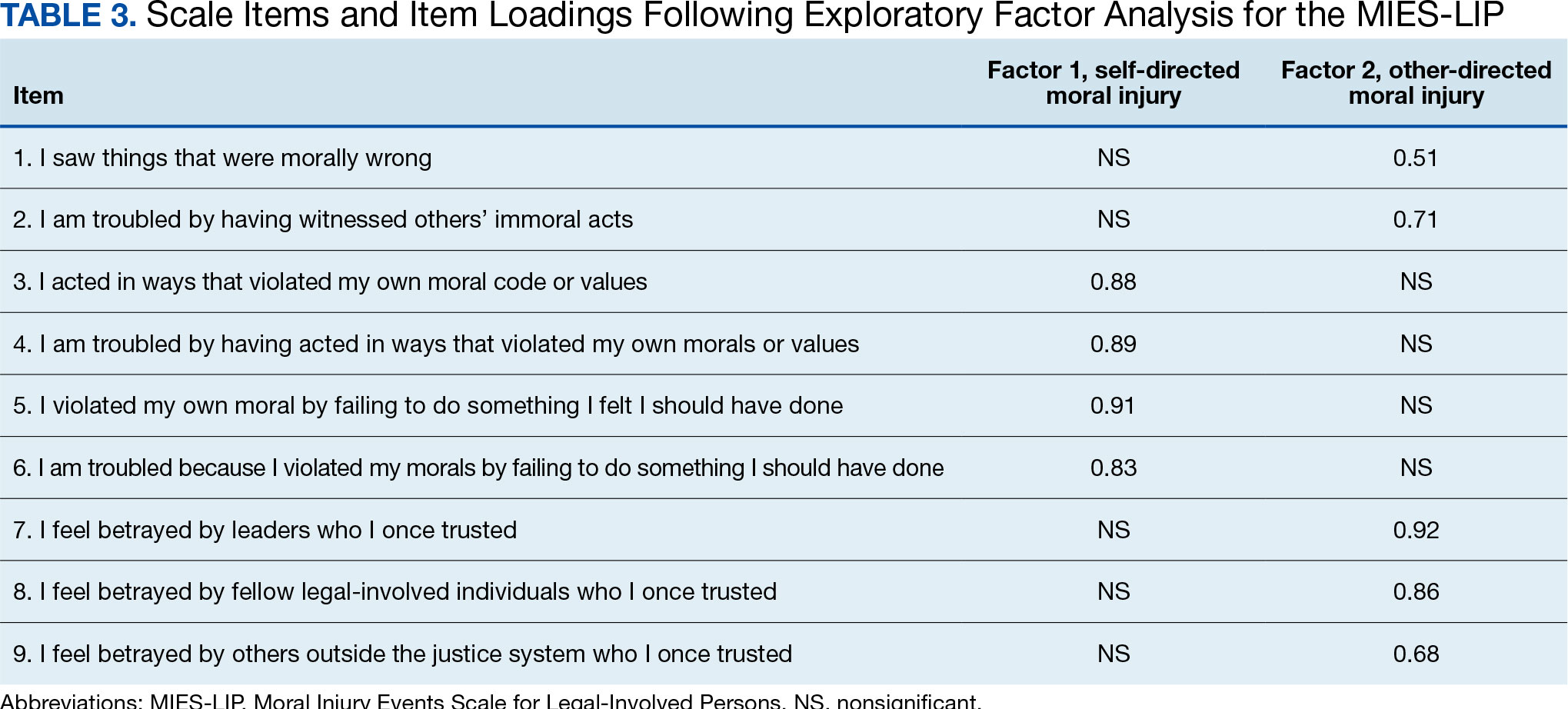
Reliability. We examined the reliability of the adapted MIES-LIP using measures of internal consistency, with both MIES-LIP factors demonstrating good reliability. The internal consistency of both factors of the MIES-LIP were found to be good (self-directed moral injury: Ω = 0.89; other-directed moral injury: Ω = 0.83).
Convergent Validity
Association between moral injury scales. A significant, moderate correlation was observed between all subscales of the MIES and MIES-LIP. Specifically, the self-directed moral injury factor of the MIES-LIP was associated with both the perceived transgressions (r = 0.41, P < .001) and the MIES perceived betrayals factors (r = 0.25, P < .05). Similarly, the other-directed moral injury factor of the MIES-LIP was associated with both the MIES perceived transgressions (r = 0.45, P < .001) and the MIES perceived betrayals factors (r = 0.45, P < .001).
Association with PTSD symptoms. All subscales of both the MIES and MIES-LIP were associated with PTSD symptom severity. The MIES perceived transgressions factor (r = 0.43, P < .001) and the perceived betrayals factor of the MIES (r = 0.39, P < .001) were moderately associated with the PCL-5. Mirroring this, the “self-directed moral injury” factor of the MIESLIP (r = 0.44, P < .001) and the “other-directed moral injury” factor of the MIES-LIP (r = 0.42, P < .001) were also positively associated with PCL-5.
Association with depression symptoms. All subscales of the MIES and MIES-LIP were also associated with depressive symptoms. The MIES perceived transgressions factor (r = 0.27, P < .01) and the MIES perceived betrayals factor (r = 0.23, P < .05) had a small association with the PHQ-9. In addition, the self-directed moral injury factor of the MIES-LIP (r = 0.40, P < .001) and the other-directed moral injury factor of the MIES-LIP (r = 0.31, P < .01) had small to moderate associations with the PCL-5.
DISCUSSION
Potentially morally injurious events appear to be a salient factor affecting legal-involved veterans. Among our sample, the vast majority of legal-involved veterans endorsed experiencing both legal- and military-related PMIEs. Witnessing or participating in a legal-related PMIE appears to be widespread among those who have experienced incarceration. The MIES-LIP yielded a 2-factor structure: self-directed moral injury and other-directed moral injury, in the evaluated population. The MIES-LIP showed similar psychometric performance to the MIES in our sample. Specifically, the MIES-LIP had good reliability and adequate convergent validity. While CFA did not confirm the anticipated factor structure of the MIES-LIP within our sample, EFA showed similarities in factor structure between the original and adapted measures. While further research and validation are needed, preliminary results show promise of the MIES-LIP in assessing legal-related moral injury.
Originally, the MIES was found to have a 2-factor structure, defined by perceived transgressions and perceived betrayals.33 However, additional research has identified a 3-factor structure, where the betrayal factor is maintained, and the transgressions factor is divided into transgressions by others and by self.8 The factor structure of the MIES-LIP was more closely related to the factor structure, with transgressions by others and betrayal mapped onto the same factor (ie, other-directed moral injury).8 While further research is needed, it is possible that the nature of morally injurious events experienced in legal contexts are experienced more in terms of self vs other, compared to morally injurious events experienced by veterans or active-duty service members.
Accurately identifying the types of moral injury experienced in a legal context may be important for determining the differences in drivers of legal-related moral injury compared to military-related moral injury. For example, self-directed moral injury in legal contexts may include a variety of actions the individual initiated that led to conviction and incarceration (eg, a criminal offense), as well as behaviors performed or witnessed while incarcerated (eg, engaging in violence). Inconsistent with military populations where other-directed moral injury clusters with self-directed moral injury, other-directed moral injury clustered with betrayal in legal contexts in our sample. This discrepancy may result from differences in identification with the military vs legal system. When veterans witness fellow service members engaging in PMIEs (eg, physical violence towards civilians in a military setting), this may be similar to self-directed moral injury due to the veteran’s identification with the same military system as the perpetrator.42 When legal-involved veterans witness other incarcerated individuals engaging in PMIEs (eg, physical violence toward other inmates), this may be experienced as similar to betrayal due to lack of personal identification with the criminal-legal system. Additional research is needed to better understand how self- and other-related moral injury are associated with betrayal in legal contexts.
Another potential driver of legal-related moral injury may be culpability. In order for moral injury to occur, an individual must perceive that something has taken place that deeply violated their sense of right and wrong.1 In terms of criminal offenses or even engaging in violent behavior while incarcerated, the potential for moral injury may differ based on whether an individual views themselves as culpable for the act(s).29 This may further distinguish between self-directed and other-directed moral injury in legal contexts. In situations where the individual views themselves as culpable, self-directed moral injury may be higher. In situations where the individual does not view themselves as culpable, other-directed moral injury may be higher based on the perception that the legal system is unfairly punishing them. Further research is needed to clarify how an individual’s view of their culpability relates to moral injury, as well as to elucidate which aspects of military service and legal involvement are most closely associated with moral injury among legal-involved veterans.
While this study treated legal-related and military-related moral injury as distinct, it is possible moral injury may have a cumulative effect over time with individuals experiencing morally injurious events across different contexts (eg, military, legal involvement). This, in turn, may compound risk for moral injury. These cumulative experiences may result in increased negative outcomes such as exacerbated psychiatric symptoms, substance misuse, and elevated suicide risk. Future studies should examine differences between groups who have experienced moral injury in differing contexts, as well as those with multiple sources of moral injury.
Limitations
The sample for this study included only veterans. The number of veterans incarcerated is large and the focus on veterans also allowed for a more robust comparison of moral injury related to the legal system and the more traditional military-related moral injury. However, the generalizability of the findings to nonveterans cannot be assured. The study used a relatively small sample (N = 100), which was overwhelmingly male. Although the PCL-5 was utilized to examine traumatic stress symptoms, this measure was not anchored to a specific criterion A trauma nor was it anchored specifically to a morally injurious experience. For all participants, their most recent military service preceded their most recent legal involvement which could affect the associations between variables. Furthermore, while all participants endorsed prior legal involvement, many participants reported no combat exposure.
CONCLUSIONS
This study resulted in several key findings. First, legal-involved veterans endorsed high rates of experiencing legal-related morally injurious experiences. Second, our adapted measure displayed adequate psychometric strength and suggests that legal-related moral injury is a salient and distinct phenomenon affecting legal-involved veterans. These items may not capture all the nuances of legal-related moral injury. Qualitative interviews with legal-involved persons may help identify relevant areas of legal-related moral injury not reflected in the current instrument. The MIES-LIP represents a practical measure that may help clinicians identify and address legal-related moral injury when working with legal-involved veterans. Given the high prevalence of PMIEs among legal-involved veterans, further examination of whether current interventions for moral injury and novel treatments being developed are effective for this population is needed.
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. J Clin Psychol. 2015;71(3):229-240. doi:10.1002/jclp.22134
- Jinkerson JD. Defining and assessing moral injury: a syndrome perspective. Traumatology. 2016;22(2):122-130. doi:10.1037/trm0000069
- Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
- Maguen S, Litz B. Moral injury in veterans of war. PTSD Res Q. 2012;23(1):1-6. www.vva1071.org/uploads/3/4/4/6/34460116/moral_injury_in_veterans_of_war.pdf
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17(1):8-13. doi:10.1177/1534765610395615
- Wisco BE, Marx BP, May CL, et al. Moral injury in U.S. combat veterans: results from the national health and resilience in veterans study. Depress Anxiety. 2017; 34(4):340-347. doi:10.1002/da.22614
- Bryan CJ, Bryan AO, Anestis MD, et al. Measuring moral injury: psychometric properties of the moral injury events scale in two military samples. Assessment. 2016;23(5):557- 570. doi:10.1177/1073191115590855
- Currier JM, Smith PN, Kuhlman S. Assessing the unique role of religious coping in suicidal behavior among U.S. Iraq and Afghanistan veterans. Psychol Relig Spiritual. 2017;9(1):118-123. doi:10.1037/rel0000055
- Kopacz MS, Connery AL, Bishop TM, et al. Moral injury: a new challenge for complementary and alternative medicine. Complement Ther Med. 2016;24:29-33. doi:10.1016/j.ctim.2015.11.003
- Vargas AF, Hanson T, Kraus D, Drescher K, Foy D. Moral injury themes in combat veterans’ narrative responses from the national vietnam veterans’ readjustment study. Traumatology. 2013;19(3):243-250. doi:10.1177/1534765613476099
- Borges LM, Barnes SM, Farnsworth JK, Bahraini NH, Brenner LA. A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S138-S140. doi:10.1037/tra0000698
- Borges LM, Holliday R, Barnes SM, et al. A longitudinal analysis of the role of potentially morally injurious events on COVID-19-related psychosocial functioning among healthcare providers. PLoS One. 2021;16(11):e0260033. doi:10.1371/journal.pone.0260033
- Currier JM, Holland JM, Rojas-Flores L, Herrera S, Foy D. Morally injurious experiences and meaning in Salvadorian teachers exposed to violence. Psychol Trauma. 2015;7(1):24-33. doi:10.1037/a0034092
- Nickerson A, Schnyder U, Bryant RA, Schick M, Mueller J, Morina N. Moral injury in traumatized refugees. Psychother Psychosom. 2015;84(2):122-123. doi:10.1159/000369353
- Papazoglou K, Chopko B. The role of moral suffering (moral distress and moral injury) in police compassion fatigue and PTSD: An unexplored topic. Front Psychol. 2017;8:1999. doi:10.3389/fpsyg.2017.01999
- Papazoglou K, Blumberg DM, Chiongbian VB, et al. The role of moral injury in PTSD among law enforcement officers: a brief report. Front Psychol. 2020;11:310. doi:10.3389/fpsyg.2020.00310
- Martin WB, Holliday R, LePage JP. Trauma and diversity: moral injury among justice involved veterans: an understudied clinical concern. Stresspoints. 2020;33(5).
- Currier JM, Drescher KD, Nieuwsma J. Future directions for addressing moral injury in clinical practice: concluding comments. In: Currier JM, Drescher KD, Nieuwsma J, eds. Addressing Moral Injury in Clinical Practice. American Psychological Association; 2021:261-271. doi:10.1037/0000204-015
- Alexander AR, Mendez L, Kerig PK. Moral injury as a transdiagnostic risk factor for mental health problems in detained youth. Crim Justice Behav. 2023;51(2):194-212. doi:10.1177/00938548231208203
- DeCaro JB, Straka K, Malek N, Zalta AK. Sentenced to shame: moral injury exposure in former lifers. Psychol Trauma. 2024; 15(5):722-730. doi:10.1037/tra0001400
- Orak U, Kelton K, Vaughn MG, Tsai J, Pietrzak RH. Homelessness and contact with the criminal legal system among U.S. combat veterans: an exploration of potential mediating factors. Crim Justice Behav. 2022;50(3):392-409. doi:10.1177/00938548221140352
- Bronson J, Carson EA, Noonan M. Veterans in Prison and Jail, 2011-12. US Department of Justice, Bureau of Justice Statistics; Published December 2015. Accessed March 4, 2025. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
- Maruschak LM, Bronson J, Alper M. Veterans in Prison: Survey of Prison Inmates, 2016. US Department of Justice, Bureau of Justice Statistics; March 2021. Accessed March 4, 2025. https://bjs.ojp.gov/redirect-legacy/content/pub/pdf/vpspi16st.pdf
- Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justiceinvolved veterans. Epidemiol Rev. 2015;37:163-176. doi:10.1093/epirev/mxu003
- Finlay AK, Owens MD, Taylor E, et al. A scoping review of military veterans involved in the criminal justice system and their health and healthcare. Health Justice. 2019;7(1):6. doi:10.1186/s40352-019-0086-9
- Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2020;30(1):41-49. doi:10.1080/10530789.2019.1711306
- Wortzel HS, Binswanger IA, Anderson CA, Adler LE. Suicide among incarcerated veterans. J Am Acad Psychiatry Law. 2009;37(1):82-91.
- Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. doi:10.1097/PRA.0000000000000520
- Asencio EK, Burke PJ. Does incarceration change the criminal identity? A synthesis of labeling and identity theory perspectives on identity change. Sociol Perspect. 2011;54(2):163-182. doi:10.1525/sop.2011.54.2.163
- Borges LM, Desai A, Barnes SM, Johnson JPS. The role of social determinants of health in moral injury: implications and future directions. Curr Treat Options Psychiatry. 2022;9(3):202-214. doi:10.1007/s40501-022-00272-4
- Houle SA, Ein N, Gervasio J, et al. Measuring moral distress and moral injury: a systematic review and content analysis of existing scales. Clin Psychol Rev. 2024;108:102377. doi:10.1016/j.cpr.2023.102377
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the moral injury events scale. Mil Med. 2013;178(6):646-652. doi:10.7205/MILMED-D-13-00017
- Zerach G, Ben-Yehuda A, Levi-Belz Y. Prospective associations between psychological factors, potentially morally injurious events, and psychiatric symptoms among Israeli combatants: the roles of ethical leadership and ethical preparation. Psychol Trauma. 2023;15(8):1367-1377. doi:10.1037/tra0001466
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Weathers FW, Litz BT, Keane TM, Palmeri PA, Marx BP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. Accessed March 4, 2025. www.ptsd.va.gov
- Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379-1391. doi:10.1037/pas0000254
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The osttraumatic stress disorder checklist for DSM-5 (PCL- 5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Kroenke K, Spi tzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Brown TA. Confirmatory Factor Analysis for Applied Research. 2nd ed. Guilford Press; 2015.
- Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141-151. doi:10.1177/001316446002000116
- Schorr Y, Stein NR, Maguen S, Barnes JB, Bosch J, Litz BT. Sources of moral injury among war veterans: a qualitative evaluation. J Clin Psychol. 2018;74(12):2203-2218. doi:10.1002/jclp.22660
Following exposure to potentially morally injurious events (PMIEs), some individuals may experience moral injury, which represents negative psychological, social, behavioral, and occasionally spiritual impacts.1 The consequences of PMIE exposure and moral injury are well documented. Individuals may begin to question the goodness and trustworthiness of oneself, others, or the world.1 Examples of other sequelae include guilt, demoralization, spiritual pain, loss of trust in the self or others, and difficulties with forgiveness.2-6 In addition, prior studies have found that moral injury is associated with an increased risk of suicidal thoughts and behaviors, posttraumatic stress disorder (PTSD) symptoms, spiritual distress, and interpersonal difficulties.7-11
Moral injury was first conceptualized in relation to combat trauma. However in recent years it has been examined in other groups such as health care practitioners, educators, refugees, and law enforcement personnel.12-17 Furthermore, there has been a recent call for the study of moral injury in other understudied groups. One such group is legal-involved individuals, defined as those who are currently involved or previously involved in the criminal justice system (ie, arrests, incarceration, parole, and probation).1,18-22
Many veterans are also involved with the legal system. Specifically, veterans currently comprise about 8% of the incarcerated US population, with an estimated > 180,000 veterans in prisons or jails and even more on parole or probation.23,24 Legal-involved veterans may be at heightened risk for homelessness, suicide, unemployment, and high prevalence rates of psychiatric diagnoses.25-28
Limited research has explored exposure to PMIEs as part of the legal process and the resulting expression of moral injury. The circumstances leading to incarceration, interactions with the US legal system, the environment of prison itself, and the subsequent challenges faced by legal-involved individuals after release all provide ample opportunity for PMIEs to occur.18 For example, engaging in a criminal act may represent a PMIE, particularly in violent offenses that involve harm to another individual. Moreover, the process of being convicted and charged with an offense may serve as a powerful reminder of the PMIE and tie this event to the individual’s identity and future. Furthermore, the physical and social environment of prison itself (eg, being surrounded by other offenders, witnessing the perpetration of violence, participating in violence for survival) presents a myriad of opportunities for PMIEs to occur.18
The consequences of PMIEs in the context of legal involvement may also have bearing on a touchstone of moral injury: changes in one’s schema of the self and world.4 At a societal level, legal-involved individuals are, by definition, deemed “guilty” and held culpable for their offense, which may reinforce a negative change in one’s view of self and the world.29 In line with identity theory, external negative appraisals about legal-involved individuals (eg, they are a danger to society, they cannot be trusted to do the right thing) may influence their self-perception.30 Furthermore, the affective characteristics often found in the context of moral injury (eg, guilt, shame, anger, contempt) may be exacerbated by legal involvement.29 Personal feelings of guilt and shame may be reinforced by receiving a verdict and sentence, as well as the negative perceptions of individuals around them (eg, disapproval from prior sources of social support). Additionally, feelings of betrayal and distrust towards the legal system may arise.
In sum, legal-involved veterans incur increased risk of moral injury due to the potential for exposure to PMIEs across multiple time points (eg, prior to military service, during military service, during arrest/sentencing, during imprisonment, and postincarceration). The stigma that accompanies legal involvement may limit access to treatment or a willingness to seek treatment for distress related to moral injury.29 Additionally, repeated exposure to PMIEs and resulting moral injury may compound over time, potentially exacerbating psychosocial functioning and increasing the risk for psychosocial stressors (eg, homelessness, unemployment) and mental health disorders (eg, depression, substance misuse).31
Although numerous measures of moral injury have been developed, most require that respondents consider a specific context (eg, military experiences).32 Therefore, study of legal-related moral injury requires adaptation of existing instruments to the legal context. The original and most commonly used scale of moral injury is the Moral Injury Events Scale (MIES).33 The MIES scales was originally developed to measure moral injury in military-related contexts but has since been adapted as a measure of exposure to context-specific PMIEs.34
Unfortunately, there are no validated measures for assessing legal-related moral injury. Such a gap in understanding is problematic, as it may impact measurement of the prevalence of PMIEs in both clinical and research settings for this at-risk population. The goal of this study was to conduct a psychometric evaluation of an adapted version of the MIES for legal-involved persons (MIES-LIP).
METHODS
A total of 177 veterans from the US Department of Veterans Affairs (VA) North Texas Health Care System were contacted for study enrollment between November 2020 and June 2021, yielding a final sample of 100 legal-involved veteran participants. Adults aged ≥ 18 years who were US military veterans and had ≥ 1 prior felony conviction resulting in incarceration were included. Participants were excluded if they had symptoms of psychosis that would preclude meaningful participation.
The study collected data on participants’ demographic and clinical characteristics using a semistructured survey instrument. Each participant completed an instructor-led questionnaire in a session that lasted about 1.5 hours. Participants who completed the visit in person received a $50 cash voucher for their time. Participants who were unable to meet with the study coordinator in person were able to complete the visit via telephone and received a $25 digital gift card. Of the total 100 participants, 79 participants completed the interview in person, and 21 completed by telephone. No significant differences were found in assessment measures between administration methods. Written informed consent was obtained during all in-person visits. For those completing via telephone, a waiver of written informed consent was obtained. This study was approved by the VA North Texas Health Care System’s Institutional Review Board.
Measures
The Moral Injury Events Scale (MIES) is a 9-item self-report measure that assesses exposure to PMIEs.33 Respondents rate their agreement with each item on a 6-point Likert scale (strongly disagree to strongly agree), with higher scores indicating greater moral injury. The MIES has a 2-factor structure: Factor 1 has 6 items on perceived transgressions and Factor 2 has 3 items on perceived betrayals.33
Creation of Legal-Involved Moral Injury Measure. To create the MIES-LIP, items and instructions from the MIES were modified to address moral injury in the context of legal involvement.33 Adaptations were finalized following consultation and approval by the authors of the original measure. Specifically, the instructions were changed to: “Please respond to these items based specifically in the context of your involvement with the legal system.” The instructions clarified that legal involvement could include experiences related to committing an offense, legal proceedings and sentencing, incarceration, or transitioning out of the legal system. This differs from the original measure, which focused on military experiences, with instructions stating: “Please respond to these items based specifically in the context of your military service (ie, events and experiences during enlistment, deployment, combat, etc).”
Other measures. The study collected data on demographic characteristics including sex, race and ethnicity, marital status, military service, combat experience, and legal involvement. PTSD symptom severity, based on the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), was assessed using the PTSD Checklist for DSM-5 (PCL-5).35,36 The PCL-5 is a 20-item self-report measure in which item scores are summed to create a total score. The PCL-5 has demonstrated strong psychometric properties, including good internal consistency, test-retest reliability convergent validity, and discriminant validity.37,38
Depressive symptom severity was measured using the Personal Health Questionnaire-9 (PHQ-9).39 The PHQ-9 is a 9-item self-report measure where item scores summed to create a total score. The PHQ-9 has demonstrated strong psychometric properties, including internal consistency and test-retest reliability.39
STATISTICAL METHODS
Descriptive statistics (mean and standard deviation for continuous variables; frequencies and percentages for categorical variables) were used to describe the study sample. Factor analysis was conducted to evaluate the psychometric properties of the MIES-LIP. Confirmatory factor analysis (CFA) was used to determine whether the MEIS-LIP had a similar factor structure to the MIES.40 Criteria for fit indices used for CFA include the Comparative Fit Index (CFI; values of > 0.95 suggest good fit), Tucker-Lewis index (TLI; values of > 0.95 suggest a good fit), root mean square error of approximation (RMSEA; values of ≥ 0.06 suggest good fit), and standardized root mean square residual (SRMR; values of ≥ 0.08 suggest good fit). With insufficient fit, subsequent exploratory factor analysis was conducted using maximum likelihood estimation with an Oblimin rotation. The Kaiser rule and a scree plot were considered when defining the factor structure. Reliability was evaluated using the McDonald omega coefficient test. Convergent validity was assessed through the association between adapted measures and other clinical measures (ie, PCL-5, PHQ-9). In addition, associations between the PCL-5 and PHQ-9 were examined as they related to the MIES and MIES-LIP.
RESULTS
Table 1 describes demographic characteristics of the study sample. Rates of potentially morally injurious experiences and the expression of moral injury in the legal context are presented in Table 2. Witnessing PMIEs while in the legal system was nearly ubiquitous, with > 90% of the sample endorsing this experience. More than half of the sample also endorsed engaging in morally injurious behavior by commission or omission, as well as experiencing betrayal while involved with the legal system.
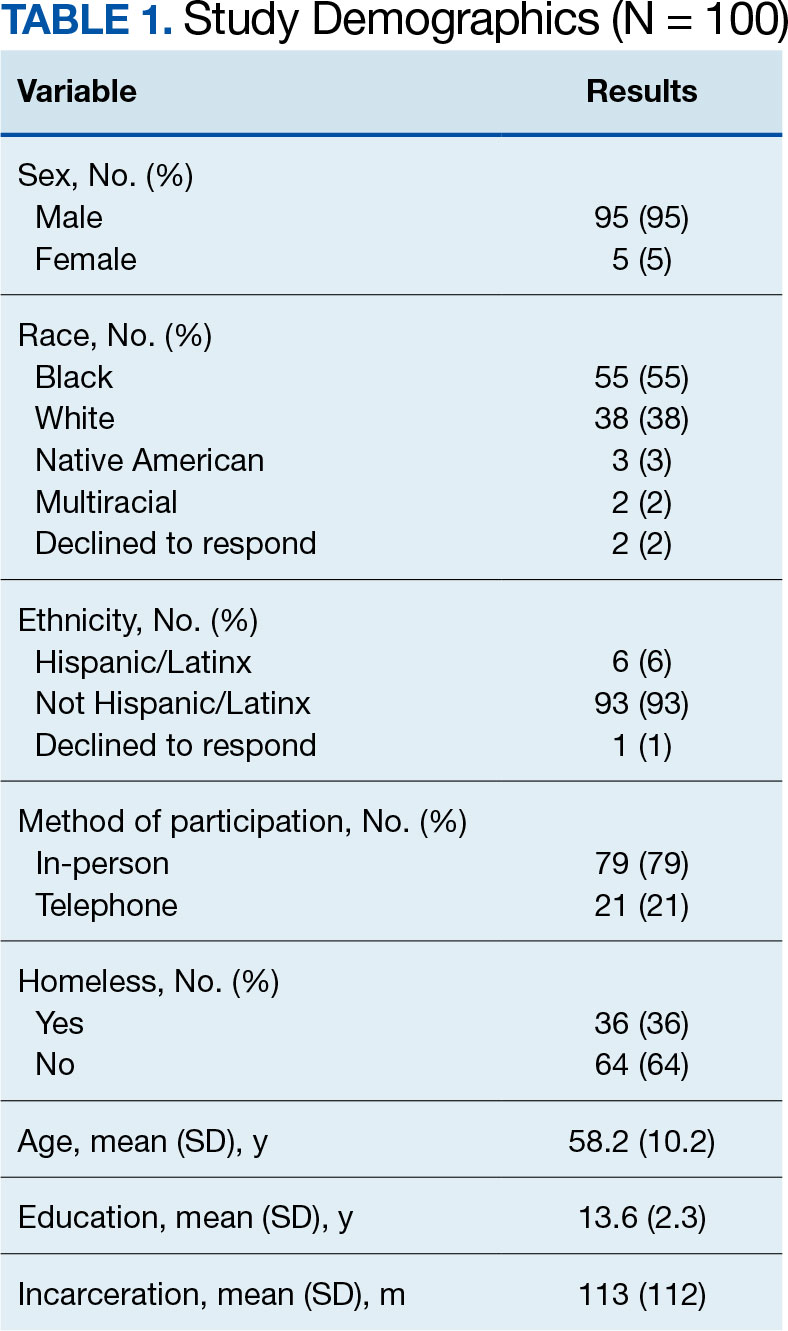
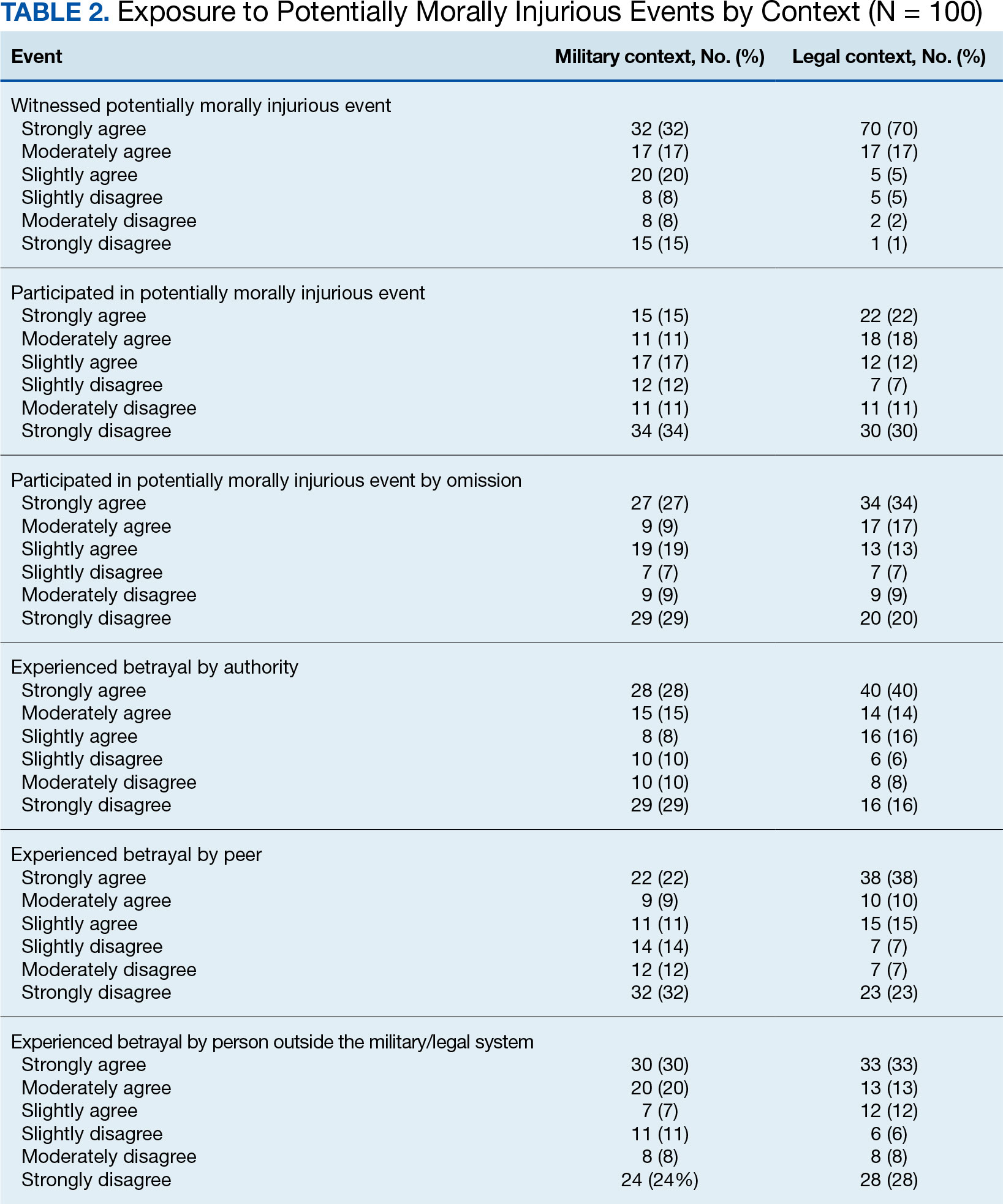
Factor Analysis
Confirmatory factor analysis (CFA) was utilized to test the factor structure of the adapted MIES-LIP in our sample compared to the published factor structures of the MIES.33 Results did not support the established factor structure. Analysis yielded unacceptable CFI (0.79), TLI (0.70), SRMR (0.14), and RMSEA (0.21). The unsatisfactory results of CFA warranted follow-up exploratory factor analysis (EFA) to examine the factor structure of the moral injury scales in this sample.
EFA of MIES-LIP
The factor structure of the MIES-LIP was examined using EFA. The factorability of the data was examined using the Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO value = 0.75) and Bartlett Test of Sphericity (X2 = 525.41; P < .001), both of which suggested that the data were appropriate for factor analysis. The number of factors to retain was selected based on the Kaiser criterion.41 After extraction, an Oblimin rotation was applied, given that we expected factors to be correlated. A 2-factor solution was found, explaining 65.76% of the common variance. All 9 items were retained as they had factor loadings > 0.30. Factor 1, comprised self-directed moral injury questions (3-6). Factor 2 comprised other directed moral injury questions (1, 2, 7-9) (Table 3). The factor correlation coefficient between Factor 1 and Factor 2 was 0.34, which supports utilizing an oblique rotation.
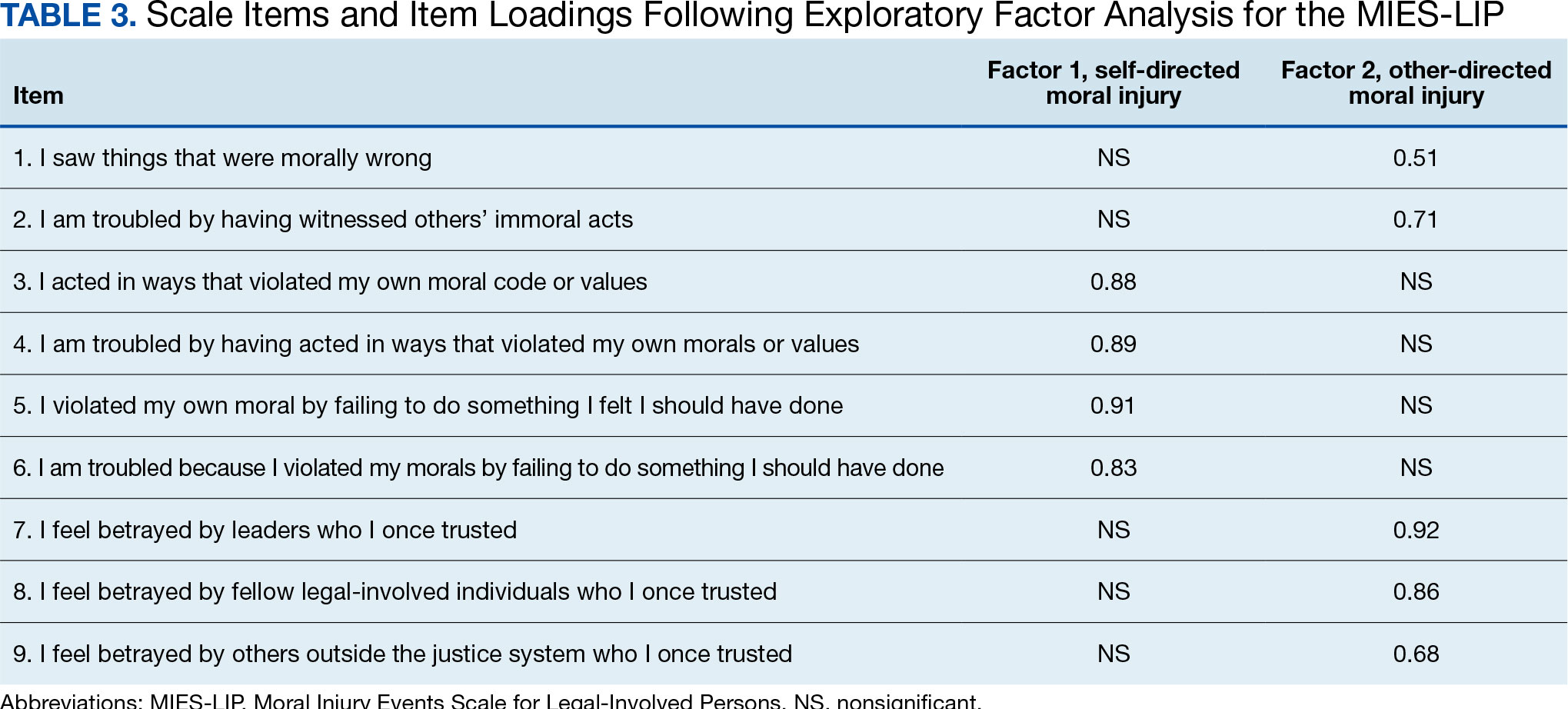
Reliability. We examined the reliability of the adapted MIES-LIP using measures of internal consistency, with both MIES-LIP factors demonstrating good reliability. The internal consistency of both factors of the MIES-LIP were found to be good (self-directed moral injury: Ω = 0.89; other-directed moral injury: Ω = 0.83).
Convergent Validity
Association between moral injury scales. A significant, moderate correlation was observed between all subscales of the MIES and MIES-LIP. Specifically, the self-directed moral injury factor of the MIES-LIP was associated with both the perceived transgressions (r = 0.41, P < .001) and the MIES perceived betrayals factors (r = 0.25, P < .05). Similarly, the other-directed moral injury factor of the MIES-LIP was associated with both the MIES perceived transgressions (r = 0.45, P < .001) and the MIES perceived betrayals factors (r = 0.45, P < .001).
Association with PTSD symptoms. All subscales of both the MIES and MIES-LIP were associated with PTSD symptom severity. The MIES perceived transgressions factor (r = 0.43, P < .001) and the perceived betrayals factor of the MIES (r = 0.39, P < .001) were moderately associated with the PCL-5. Mirroring this, the “self-directed moral injury” factor of the MIESLIP (r = 0.44, P < .001) and the “other-directed moral injury” factor of the MIES-LIP (r = 0.42, P < .001) were also positively associated with PCL-5.
Association with depression symptoms. All subscales of the MIES and MIES-LIP were also associated with depressive symptoms. The MIES perceived transgressions factor (r = 0.27, P < .01) and the MIES perceived betrayals factor (r = 0.23, P < .05) had a small association with the PHQ-9. In addition, the self-directed moral injury factor of the MIES-LIP (r = 0.40, P < .001) and the other-directed moral injury factor of the MIES-LIP (r = 0.31, P < .01) had small to moderate associations with the PCL-5.
DISCUSSION
Potentially morally injurious events appear to be a salient factor affecting legal-involved veterans. Among our sample, the vast majority of legal-involved veterans endorsed experiencing both legal- and military-related PMIEs. Witnessing or participating in a legal-related PMIE appears to be widespread among those who have experienced incarceration. The MIES-LIP yielded a 2-factor structure: self-directed moral injury and other-directed moral injury, in the evaluated population. The MIES-LIP showed similar psychometric performance to the MIES in our sample. Specifically, the MIES-LIP had good reliability and adequate convergent validity. While CFA did not confirm the anticipated factor structure of the MIES-LIP within our sample, EFA showed similarities in factor structure between the original and adapted measures. While further research and validation are needed, preliminary results show promise of the MIES-LIP in assessing legal-related moral injury.
Originally, the MIES was found to have a 2-factor structure, defined by perceived transgressions and perceived betrayals.33 However, additional research has identified a 3-factor structure, where the betrayal factor is maintained, and the transgressions factor is divided into transgressions by others and by self.8 The factor structure of the MIES-LIP was more closely related to the factor structure, with transgressions by others and betrayal mapped onto the same factor (ie, other-directed moral injury).8 While further research is needed, it is possible that the nature of morally injurious events experienced in legal contexts are experienced more in terms of self vs other, compared to morally injurious events experienced by veterans or active-duty service members.
Accurately identifying the types of moral injury experienced in a legal context may be important for determining the differences in drivers of legal-related moral injury compared to military-related moral injury. For example, self-directed moral injury in legal contexts may include a variety of actions the individual initiated that led to conviction and incarceration (eg, a criminal offense), as well as behaviors performed or witnessed while incarcerated (eg, engaging in violence). Inconsistent with military populations where other-directed moral injury clusters with self-directed moral injury, other-directed moral injury clustered with betrayal in legal contexts in our sample. This discrepancy may result from differences in identification with the military vs legal system. When veterans witness fellow service members engaging in PMIEs (eg, physical violence towards civilians in a military setting), this may be similar to self-directed moral injury due to the veteran’s identification with the same military system as the perpetrator.42 When legal-involved veterans witness other incarcerated individuals engaging in PMIEs (eg, physical violence toward other inmates), this may be experienced as similar to betrayal due to lack of personal identification with the criminal-legal system. Additional research is needed to better understand how self- and other-related moral injury are associated with betrayal in legal contexts.
Another potential driver of legal-related moral injury may be culpability. In order for moral injury to occur, an individual must perceive that something has taken place that deeply violated their sense of right and wrong.1 In terms of criminal offenses or even engaging in violent behavior while incarcerated, the potential for moral injury may differ based on whether an individual views themselves as culpable for the act(s).29 This may further distinguish between self-directed and other-directed moral injury in legal contexts. In situations where the individual views themselves as culpable, self-directed moral injury may be higher. In situations where the individual does not view themselves as culpable, other-directed moral injury may be higher based on the perception that the legal system is unfairly punishing them. Further research is needed to clarify how an individual’s view of their culpability relates to moral injury, as well as to elucidate which aspects of military service and legal involvement are most closely associated with moral injury among legal-involved veterans.
While this study treated legal-related and military-related moral injury as distinct, it is possible moral injury may have a cumulative effect over time with individuals experiencing morally injurious events across different contexts (eg, military, legal involvement). This, in turn, may compound risk for moral injury. These cumulative experiences may result in increased negative outcomes such as exacerbated psychiatric symptoms, substance misuse, and elevated suicide risk. Future studies should examine differences between groups who have experienced moral injury in differing contexts, as well as those with multiple sources of moral injury.
Limitations
The sample for this study included only veterans. The number of veterans incarcerated is large and the focus on veterans also allowed for a more robust comparison of moral injury related to the legal system and the more traditional military-related moral injury. However, the generalizability of the findings to nonveterans cannot be assured. The study used a relatively small sample (N = 100), which was overwhelmingly male. Although the PCL-5 was utilized to examine traumatic stress symptoms, this measure was not anchored to a specific criterion A trauma nor was it anchored specifically to a morally injurious experience. For all participants, their most recent military service preceded their most recent legal involvement which could affect the associations between variables. Furthermore, while all participants endorsed prior legal involvement, many participants reported no combat exposure.
CONCLUSIONS
This study resulted in several key findings. First, legal-involved veterans endorsed high rates of experiencing legal-related morally injurious experiences. Second, our adapted measure displayed adequate psychometric strength and suggests that legal-related moral injury is a salient and distinct phenomenon affecting legal-involved veterans. These items may not capture all the nuances of legal-related moral injury. Qualitative interviews with legal-involved persons may help identify relevant areas of legal-related moral injury not reflected in the current instrument. The MIES-LIP represents a practical measure that may help clinicians identify and address legal-related moral injury when working with legal-involved veterans. Given the high prevalence of PMIEs among legal-involved veterans, further examination of whether current interventions for moral injury and novel treatments being developed are effective for this population is needed.
Following exposure to potentially morally injurious events (PMIEs), some individuals may experience moral injury, which represents negative psychological, social, behavioral, and occasionally spiritual impacts.1 The consequences of PMIE exposure and moral injury are well documented. Individuals may begin to question the goodness and trustworthiness of oneself, others, or the world.1 Examples of other sequelae include guilt, demoralization, spiritual pain, loss of trust in the self or others, and difficulties with forgiveness.2-6 In addition, prior studies have found that moral injury is associated with an increased risk of suicidal thoughts and behaviors, posttraumatic stress disorder (PTSD) symptoms, spiritual distress, and interpersonal difficulties.7-11
Moral injury was first conceptualized in relation to combat trauma. However in recent years it has been examined in other groups such as health care practitioners, educators, refugees, and law enforcement personnel.12-17 Furthermore, there has been a recent call for the study of moral injury in other understudied groups. One such group is legal-involved individuals, defined as those who are currently involved or previously involved in the criminal justice system (ie, arrests, incarceration, parole, and probation).1,18-22
Many veterans are also involved with the legal system. Specifically, veterans currently comprise about 8% of the incarcerated US population, with an estimated > 180,000 veterans in prisons or jails and even more on parole or probation.23,24 Legal-involved veterans may be at heightened risk for homelessness, suicide, unemployment, and high prevalence rates of psychiatric diagnoses.25-28
Limited research has explored exposure to PMIEs as part of the legal process and the resulting expression of moral injury. The circumstances leading to incarceration, interactions with the US legal system, the environment of prison itself, and the subsequent challenges faced by legal-involved individuals after release all provide ample opportunity for PMIEs to occur.18 For example, engaging in a criminal act may represent a PMIE, particularly in violent offenses that involve harm to another individual. Moreover, the process of being convicted and charged with an offense may serve as a powerful reminder of the PMIE and tie this event to the individual’s identity and future. Furthermore, the physical and social environment of prison itself (eg, being surrounded by other offenders, witnessing the perpetration of violence, participating in violence for survival) presents a myriad of opportunities for PMIEs to occur.18
The consequences of PMIEs in the context of legal involvement may also have bearing on a touchstone of moral injury: changes in one’s schema of the self and world.4 At a societal level, legal-involved individuals are, by definition, deemed “guilty” and held culpable for their offense, which may reinforce a negative change in one’s view of self and the world.29 In line with identity theory, external negative appraisals about legal-involved individuals (eg, they are a danger to society, they cannot be trusted to do the right thing) may influence their self-perception.30 Furthermore, the affective characteristics often found in the context of moral injury (eg, guilt, shame, anger, contempt) may be exacerbated by legal involvement.29 Personal feelings of guilt and shame may be reinforced by receiving a verdict and sentence, as well as the negative perceptions of individuals around them (eg, disapproval from prior sources of social support). Additionally, feelings of betrayal and distrust towards the legal system may arise.
In sum, legal-involved veterans incur increased risk of moral injury due to the potential for exposure to PMIEs across multiple time points (eg, prior to military service, during military service, during arrest/sentencing, during imprisonment, and postincarceration). The stigma that accompanies legal involvement may limit access to treatment or a willingness to seek treatment for distress related to moral injury.29 Additionally, repeated exposure to PMIEs and resulting moral injury may compound over time, potentially exacerbating psychosocial functioning and increasing the risk for psychosocial stressors (eg, homelessness, unemployment) and mental health disorders (eg, depression, substance misuse).31
Although numerous measures of moral injury have been developed, most require that respondents consider a specific context (eg, military experiences).32 Therefore, study of legal-related moral injury requires adaptation of existing instruments to the legal context. The original and most commonly used scale of moral injury is the Moral Injury Events Scale (MIES).33 The MIES scales was originally developed to measure moral injury in military-related contexts but has since been adapted as a measure of exposure to context-specific PMIEs.34
Unfortunately, there are no validated measures for assessing legal-related moral injury. Such a gap in understanding is problematic, as it may impact measurement of the prevalence of PMIEs in both clinical and research settings for this at-risk population. The goal of this study was to conduct a psychometric evaluation of an adapted version of the MIES for legal-involved persons (MIES-LIP).
METHODS
A total of 177 veterans from the US Department of Veterans Affairs (VA) North Texas Health Care System were contacted for study enrollment between November 2020 and June 2021, yielding a final sample of 100 legal-involved veteran participants. Adults aged ≥ 18 years who were US military veterans and had ≥ 1 prior felony conviction resulting in incarceration were included. Participants were excluded if they had symptoms of psychosis that would preclude meaningful participation.
The study collected data on participants’ demographic and clinical characteristics using a semistructured survey instrument. Each participant completed an instructor-led questionnaire in a session that lasted about 1.5 hours. Participants who completed the visit in person received a $50 cash voucher for their time. Participants who were unable to meet with the study coordinator in person were able to complete the visit via telephone and received a $25 digital gift card. Of the total 100 participants, 79 participants completed the interview in person, and 21 completed by telephone. No significant differences were found in assessment measures between administration methods. Written informed consent was obtained during all in-person visits. For those completing via telephone, a waiver of written informed consent was obtained. This study was approved by the VA North Texas Health Care System’s Institutional Review Board.
Measures
The Moral Injury Events Scale (MIES) is a 9-item self-report measure that assesses exposure to PMIEs.33 Respondents rate their agreement with each item on a 6-point Likert scale (strongly disagree to strongly agree), with higher scores indicating greater moral injury. The MIES has a 2-factor structure: Factor 1 has 6 items on perceived transgressions and Factor 2 has 3 items on perceived betrayals.33
Creation of Legal-Involved Moral Injury Measure. To create the MIES-LIP, items and instructions from the MIES were modified to address moral injury in the context of legal involvement.33 Adaptations were finalized following consultation and approval by the authors of the original measure. Specifically, the instructions were changed to: “Please respond to these items based specifically in the context of your involvement with the legal system.” The instructions clarified that legal involvement could include experiences related to committing an offense, legal proceedings and sentencing, incarceration, or transitioning out of the legal system. This differs from the original measure, which focused on military experiences, with instructions stating: “Please respond to these items based specifically in the context of your military service (ie, events and experiences during enlistment, deployment, combat, etc).”
Other measures. The study collected data on demographic characteristics including sex, race and ethnicity, marital status, military service, combat experience, and legal involvement. PTSD symptom severity, based on the criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), was assessed using the PTSD Checklist for DSM-5 (PCL-5).35,36 The PCL-5 is a 20-item self-report measure in which item scores are summed to create a total score. The PCL-5 has demonstrated strong psychometric properties, including good internal consistency, test-retest reliability convergent validity, and discriminant validity.37,38
Depressive symptom severity was measured using the Personal Health Questionnaire-9 (PHQ-9).39 The PHQ-9 is a 9-item self-report measure where item scores summed to create a total score. The PHQ-9 has demonstrated strong psychometric properties, including internal consistency and test-retest reliability.39
STATISTICAL METHODS
Descriptive statistics (mean and standard deviation for continuous variables; frequencies and percentages for categorical variables) were used to describe the study sample. Factor analysis was conducted to evaluate the psychometric properties of the MIES-LIP. Confirmatory factor analysis (CFA) was used to determine whether the MEIS-LIP had a similar factor structure to the MIES.40 Criteria for fit indices used for CFA include the Comparative Fit Index (CFI; values of > 0.95 suggest good fit), Tucker-Lewis index (TLI; values of > 0.95 suggest a good fit), root mean square error of approximation (RMSEA; values of ≥ 0.06 suggest good fit), and standardized root mean square residual (SRMR; values of ≥ 0.08 suggest good fit). With insufficient fit, subsequent exploratory factor analysis was conducted using maximum likelihood estimation with an Oblimin rotation. The Kaiser rule and a scree plot were considered when defining the factor structure. Reliability was evaluated using the McDonald omega coefficient test. Convergent validity was assessed through the association between adapted measures and other clinical measures (ie, PCL-5, PHQ-9). In addition, associations between the PCL-5 and PHQ-9 were examined as they related to the MIES and MIES-LIP.
RESULTS
Table 1 describes demographic characteristics of the study sample. Rates of potentially morally injurious experiences and the expression of moral injury in the legal context are presented in Table 2. Witnessing PMIEs while in the legal system was nearly ubiquitous, with > 90% of the sample endorsing this experience. More than half of the sample also endorsed engaging in morally injurious behavior by commission or omission, as well as experiencing betrayal while involved with the legal system.
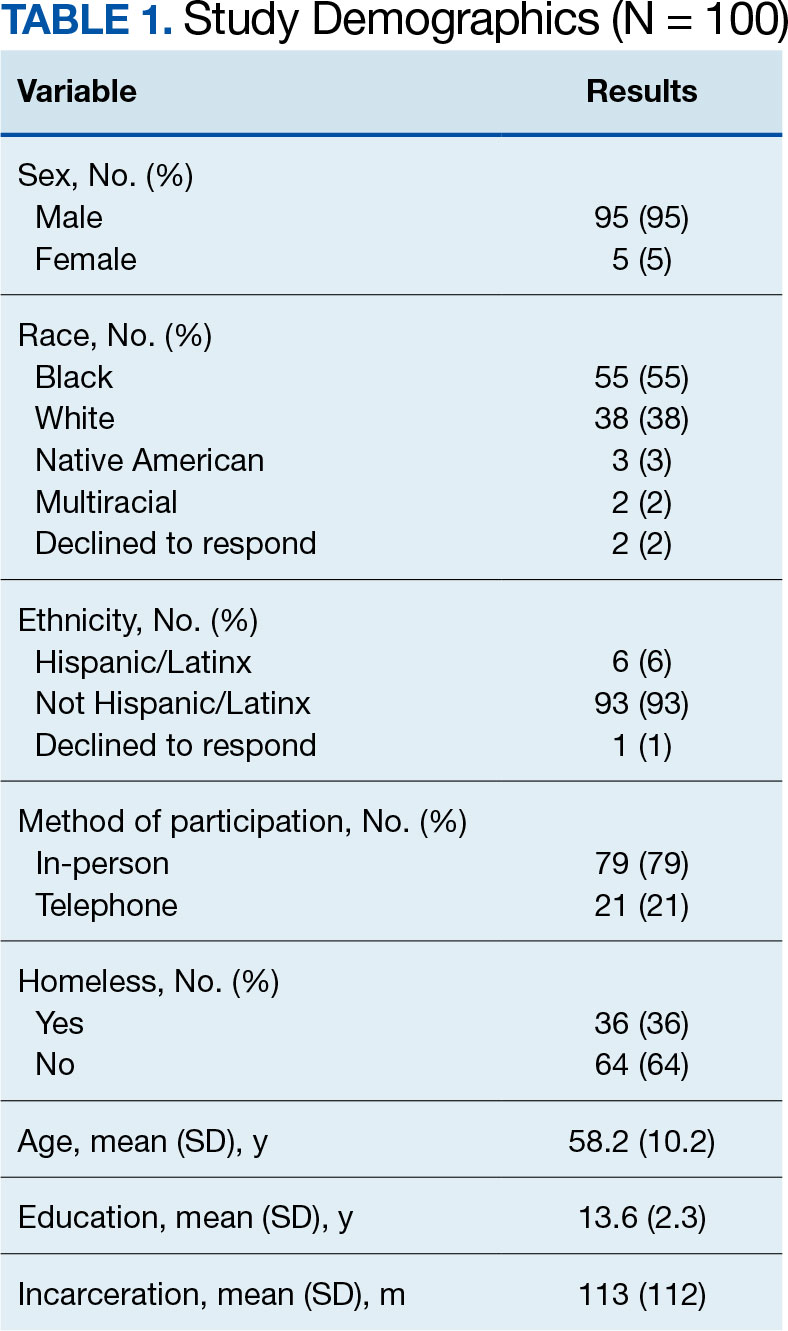
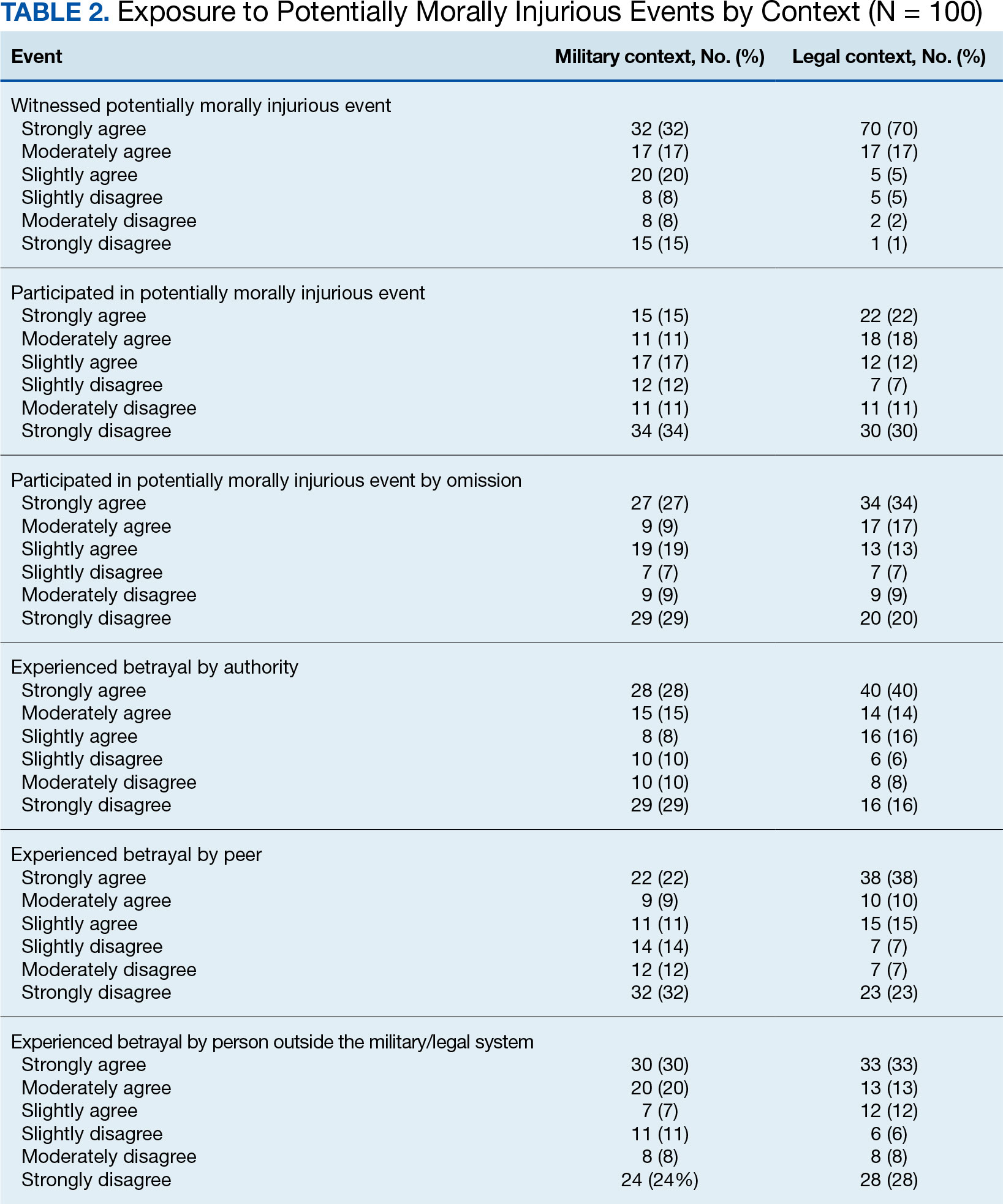
Factor Analysis
Confirmatory factor analysis (CFA) was utilized to test the factor structure of the adapted MIES-LIP in our sample compared to the published factor structures of the MIES.33 Results did not support the established factor structure. Analysis yielded unacceptable CFI (0.79), TLI (0.70), SRMR (0.14), and RMSEA (0.21). The unsatisfactory results of CFA warranted follow-up exploratory factor analysis (EFA) to examine the factor structure of the moral injury scales in this sample.
EFA of MIES-LIP
The factor structure of the MIES-LIP was examined using EFA. The factorability of the data was examined using the Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO value = 0.75) and Bartlett Test of Sphericity (X2 = 525.41; P < .001), both of which suggested that the data were appropriate for factor analysis. The number of factors to retain was selected based on the Kaiser criterion.41 After extraction, an Oblimin rotation was applied, given that we expected factors to be correlated. A 2-factor solution was found, explaining 65.76% of the common variance. All 9 items were retained as they had factor loadings > 0.30. Factor 1, comprised self-directed moral injury questions (3-6). Factor 2 comprised other directed moral injury questions (1, 2, 7-9) (Table 3). The factor correlation coefficient between Factor 1 and Factor 2 was 0.34, which supports utilizing an oblique rotation.
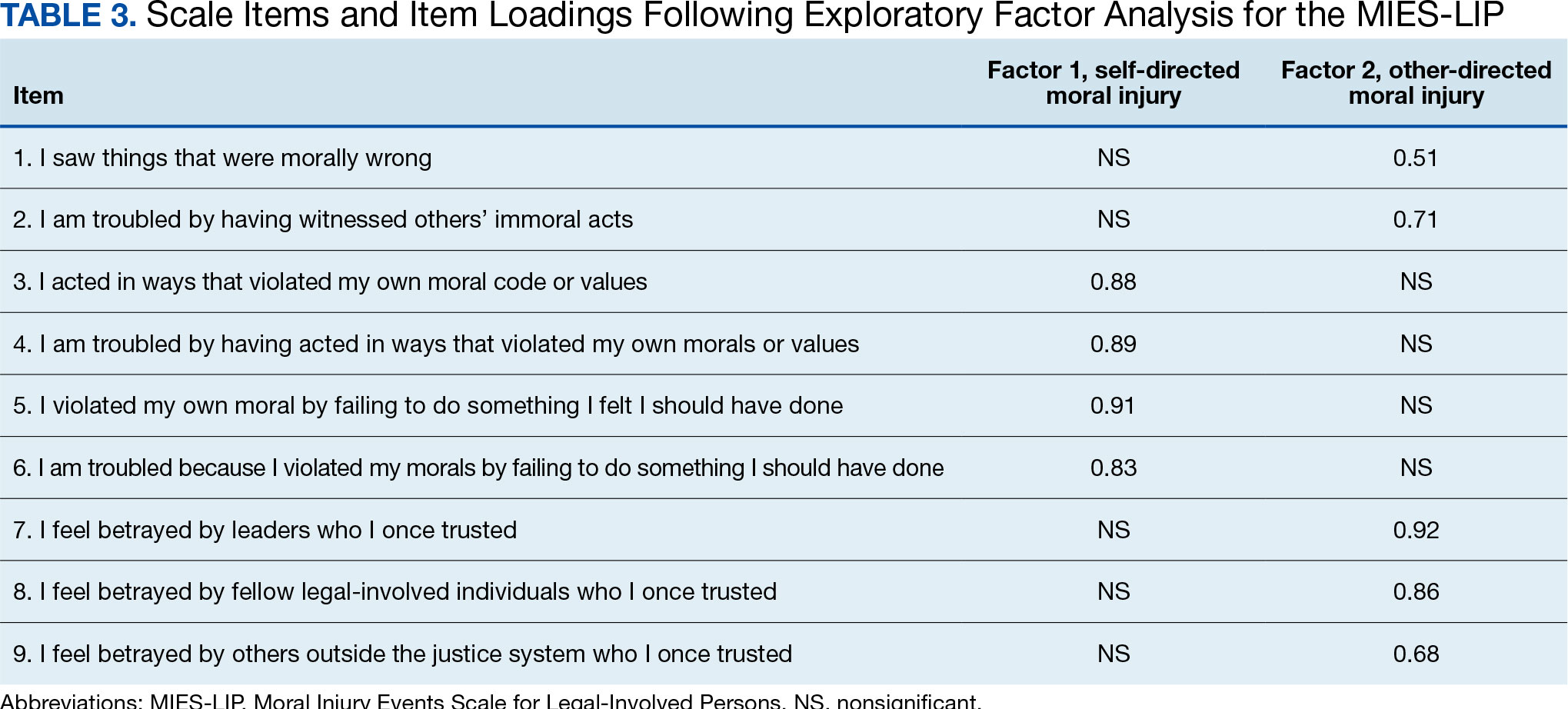
Reliability. We examined the reliability of the adapted MIES-LIP using measures of internal consistency, with both MIES-LIP factors demonstrating good reliability. The internal consistency of both factors of the MIES-LIP were found to be good (self-directed moral injury: Ω = 0.89; other-directed moral injury: Ω = 0.83).
Convergent Validity
Association between moral injury scales. A significant, moderate correlation was observed between all subscales of the MIES and MIES-LIP. Specifically, the self-directed moral injury factor of the MIES-LIP was associated with both the perceived transgressions (r = 0.41, P < .001) and the MIES perceived betrayals factors (r = 0.25, P < .05). Similarly, the other-directed moral injury factor of the MIES-LIP was associated with both the MIES perceived transgressions (r = 0.45, P < .001) and the MIES perceived betrayals factors (r = 0.45, P < .001).
Association with PTSD symptoms. All subscales of both the MIES and MIES-LIP were associated with PTSD symptom severity. The MIES perceived transgressions factor (r = 0.43, P < .001) and the perceived betrayals factor of the MIES (r = 0.39, P < .001) were moderately associated with the PCL-5. Mirroring this, the “self-directed moral injury” factor of the MIESLIP (r = 0.44, P < .001) and the “other-directed moral injury” factor of the MIES-LIP (r = 0.42, P < .001) were also positively associated with PCL-5.
Association with depression symptoms. All subscales of the MIES and MIES-LIP were also associated with depressive symptoms. The MIES perceived transgressions factor (r = 0.27, P < .01) and the MIES perceived betrayals factor (r = 0.23, P < .05) had a small association with the PHQ-9. In addition, the self-directed moral injury factor of the MIES-LIP (r = 0.40, P < .001) and the other-directed moral injury factor of the MIES-LIP (r = 0.31, P < .01) had small to moderate associations with the PCL-5.
DISCUSSION
Potentially morally injurious events appear to be a salient factor affecting legal-involved veterans. Among our sample, the vast majority of legal-involved veterans endorsed experiencing both legal- and military-related PMIEs. Witnessing or participating in a legal-related PMIE appears to be widespread among those who have experienced incarceration. The MIES-LIP yielded a 2-factor structure: self-directed moral injury and other-directed moral injury, in the evaluated population. The MIES-LIP showed similar psychometric performance to the MIES in our sample. Specifically, the MIES-LIP had good reliability and adequate convergent validity. While CFA did not confirm the anticipated factor structure of the MIES-LIP within our sample, EFA showed similarities in factor structure between the original and adapted measures. While further research and validation are needed, preliminary results show promise of the MIES-LIP in assessing legal-related moral injury.
Originally, the MIES was found to have a 2-factor structure, defined by perceived transgressions and perceived betrayals.33 However, additional research has identified a 3-factor structure, where the betrayal factor is maintained, and the transgressions factor is divided into transgressions by others and by self.8 The factor structure of the MIES-LIP was more closely related to the factor structure, with transgressions by others and betrayal mapped onto the same factor (ie, other-directed moral injury).8 While further research is needed, it is possible that the nature of morally injurious events experienced in legal contexts are experienced more in terms of self vs other, compared to morally injurious events experienced by veterans or active-duty service members.
Accurately identifying the types of moral injury experienced in a legal context may be important for determining the differences in drivers of legal-related moral injury compared to military-related moral injury. For example, self-directed moral injury in legal contexts may include a variety of actions the individual initiated that led to conviction and incarceration (eg, a criminal offense), as well as behaviors performed or witnessed while incarcerated (eg, engaging in violence). Inconsistent with military populations where other-directed moral injury clusters with self-directed moral injury, other-directed moral injury clustered with betrayal in legal contexts in our sample. This discrepancy may result from differences in identification with the military vs legal system. When veterans witness fellow service members engaging in PMIEs (eg, physical violence towards civilians in a military setting), this may be similar to self-directed moral injury due to the veteran’s identification with the same military system as the perpetrator.42 When legal-involved veterans witness other incarcerated individuals engaging in PMIEs (eg, physical violence toward other inmates), this may be experienced as similar to betrayal due to lack of personal identification with the criminal-legal system. Additional research is needed to better understand how self- and other-related moral injury are associated with betrayal in legal contexts.
Another potential driver of legal-related moral injury may be culpability. In order for moral injury to occur, an individual must perceive that something has taken place that deeply violated their sense of right and wrong.1 In terms of criminal offenses or even engaging in violent behavior while incarcerated, the potential for moral injury may differ based on whether an individual views themselves as culpable for the act(s).29 This may further distinguish between self-directed and other-directed moral injury in legal contexts. In situations where the individual views themselves as culpable, self-directed moral injury may be higher. In situations where the individual does not view themselves as culpable, other-directed moral injury may be higher based on the perception that the legal system is unfairly punishing them. Further research is needed to clarify how an individual’s view of their culpability relates to moral injury, as well as to elucidate which aspects of military service and legal involvement are most closely associated with moral injury among legal-involved veterans.
While this study treated legal-related and military-related moral injury as distinct, it is possible moral injury may have a cumulative effect over time with individuals experiencing morally injurious events across different contexts (eg, military, legal involvement). This, in turn, may compound risk for moral injury. These cumulative experiences may result in increased negative outcomes such as exacerbated psychiatric symptoms, substance misuse, and elevated suicide risk. Future studies should examine differences between groups who have experienced moral injury in differing contexts, as well as those with multiple sources of moral injury.
Limitations
The sample for this study included only veterans. The number of veterans incarcerated is large and the focus on veterans also allowed for a more robust comparison of moral injury related to the legal system and the more traditional military-related moral injury. However, the generalizability of the findings to nonveterans cannot be assured. The study used a relatively small sample (N = 100), which was overwhelmingly male. Although the PCL-5 was utilized to examine traumatic stress symptoms, this measure was not anchored to a specific criterion A trauma nor was it anchored specifically to a morally injurious experience. For all participants, their most recent military service preceded their most recent legal involvement which could affect the associations between variables. Furthermore, while all participants endorsed prior legal involvement, many participants reported no combat exposure.
CONCLUSIONS
This study resulted in several key findings. First, legal-involved veterans endorsed high rates of experiencing legal-related morally injurious experiences. Second, our adapted measure displayed adequate psychometric strength and suggests that legal-related moral injury is a salient and distinct phenomenon affecting legal-involved veterans. These items may not capture all the nuances of legal-related moral injury. Qualitative interviews with legal-involved persons may help identify relevant areas of legal-related moral injury not reflected in the current instrument. The MIES-LIP represents a practical measure that may help clinicians identify and address legal-related moral injury when working with legal-involved veterans. Given the high prevalence of PMIEs among legal-involved veterans, further examination of whether current interventions for moral injury and novel treatments being developed are effective for this population is needed.
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. J Clin Psychol. 2015;71(3):229-240. doi:10.1002/jclp.22134
- Jinkerson JD. Defining and assessing moral injury: a syndrome perspective. Traumatology. 2016;22(2):122-130. doi:10.1037/trm0000069
- Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
- Maguen S, Litz B. Moral injury in veterans of war. PTSD Res Q. 2012;23(1):1-6. www.vva1071.org/uploads/3/4/4/6/34460116/moral_injury_in_veterans_of_war.pdf
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17(1):8-13. doi:10.1177/1534765610395615
- Wisco BE, Marx BP, May CL, et al. Moral injury in U.S. combat veterans: results from the national health and resilience in veterans study. Depress Anxiety. 2017; 34(4):340-347. doi:10.1002/da.22614
- Bryan CJ, Bryan AO, Anestis MD, et al. Measuring moral injury: psychometric properties of the moral injury events scale in two military samples. Assessment. 2016;23(5):557- 570. doi:10.1177/1073191115590855
- Currier JM, Smith PN, Kuhlman S. Assessing the unique role of religious coping in suicidal behavior among U.S. Iraq and Afghanistan veterans. Psychol Relig Spiritual. 2017;9(1):118-123. doi:10.1037/rel0000055
- Kopacz MS, Connery AL, Bishop TM, et al. Moral injury: a new challenge for complementary and alternative medicine. Complement Ther Med. 2016;24:29-33. doi:10.1016/j.ctim.2015.11.003
- Vargas AF, Hanson T, Kraus D, Drescher K, Foy D. Moral injury themes in combat veterans’ narrative responses from the national vietnam veterans’ readjustment study. Traumatology. 2013;19(3):243-250. doi:10.1177/1534765613476099
- Borges LM, Barnes SM, Farnsworth JK, Bahraini NH, Brenner LA. A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S138-S140. doi:10.1037/tra0000698
- Borges LM, Holliday R, Barnes SM, et al. A longitudinal analysis of the role of potentially morally injurious events on COVID-19-related psychosocial functioning among healthcare providers. PLoS One. 2021;16(11):e0260033. doi:10.1371/journal.pone.0260033
- Currier JM, Holland JM, Rojas-Flores L, Herrera S, Foy D. Morally injurious experiences and meaning in Salvadorian teachers exposed to violence. Psychol Trauma. 2015;7(1):24-33. doi:10.1037/a0034092
- Nickerson A, Schnyder U, Bryant RA, Schick M, Mueller J, Morina N. Moral injury in traumatized refugees. Psychother Psychosom. 2015;84(2):122-123. doi:10.1159/000369353
- Papazoglou K, Chopko B. The role of moral suffering (moral distress and moral injury) in police compassion fatigue and PTSD: An unexplored topic. Front Psychol. 2017;8:1999. doi:10.3389/fpsyg.2017.01999
- Papazoglou K, Blumberg DM, Chiongbian VB, et al. The role of moral injury in PTSD among law enforcement officers: a brief report. Front Psychol. 2020;11:310. doi:10.3389/fpsyg.2020.00310
- Martin WB, Holliday R, LePage JP. Trauma and diversity: moral injury among justice involved veterans: an understudied clinical concern. Stresspoints. 2020;33(5).
- Currier JM, Drescher KD, Nieuwsma J. Future directions for addressing moral injury in clinical practice: concluding comments. In: Currier JM, Drescher KD, Nieuwsma J, eds. Addressing Moral Injury in Clinical Practice. American Psychological Association; 2021:261-271. doi:10.1037/0000204-015
- Alexander AR, Mendez L, Kerig PK. Moral injury as a transdiagnostic risk factor for mental health problems in detained youth. Crim Justice Behav. 2023;51(2):194-212. doi:10.1177/00938548231208203
- DeCaro JB, Straka K, Malek N, Zalta AK. Sentenced to shame: moral injury exposure in former lifers. Psychol Trauma. 2024; 15(5):722-730. doi:10.1037/tra0001400
- Orak U, Kelton K, Vaughn MG, Tsai J, Pietrzak RH. Homelessness and contact with the criminal legal system among U.S. combat veterans: an exploration of potential mediating factors. Crim Justice Behav. 2022;50(3):392-409. doi:10.1177/00938548221140352
- Bronson J, Carson EA, Noonan M. Veterans in Prison and Jail, 2011-12. US Department of Justice, Bureau of Justice Statistics; Published December 2015. Accessed March 4, 2025. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
- Maruschak LM, Bronson J, Alper M. Veterans in Prison: Survey of Prison Inmates, 2016. US Department of Justice, Bureau of Justice Statistics; March 2021. Accessed March 4, 2025. https://bjs.ojp.gov/redirect-legacy/content/pub/pdf/vpspi16st.pdf
- Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justiceinvolved veterans. Epidemiol Rev. 2015;37:163-176. doi:10.1093/epirev/mxu003
- Finlay AK, Owens MD, Taylor E, et al. A scoping review of military veterans involved in the criminal justice system and their health and healthcare. Health Justice. 2019;7(1):6. doi:10.1186/s40352-019-0086-9
- Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2020;30(1):41-49. doi:10.1080/10530789.2019.1711306
- Wortzel HS, Binswanger IA, Anderson CA, Adler LE. Suicide among incarcerated veterans. J Am Acad Psychiatry Law. 2009;37(1):82-91.
- Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. doi:10.1097/PRA.0000000000000520
- Asencio EK, Burke PJ. Does incarceration change the criminal identity? A synthesis of labeling and identity theory perspectives on identity change. Sociol Perspect. 2011;54(2):163-182. doi:10.1525/sop.2011.54.2.163
- Borges LM, Desai A, Barnes SM, Johnson JPS. The role of social determinants of health in moral injury: implications and future directions. Curr Treat Options Psychiatry. 2022;9(3):202-214. doi:10.1007/s40501-022-00272-4
- Houle SA, Ein N, Gervasio J, et al. Measuring moral distress and moral injury: a systematic review and content analysis of existing scales. Clin Psychol Rev. 2024;108:102377. doi:10.1016/j.cpr.2023.102377
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the moral injury events scale. Mil Med. 2013;178(6):646-652. doi:10.7205/MILMED-D-13-00017
- Zerach G, Ben-Yehuda A, Levi-Belz Y. Prospective associations between psychological factors, potentially morally injurious events, and psychiatric symptoms among Israeli combatants: the roles of ethical leadership and ethical preparation. Psychol Trauma. 2023;15(8):1367-1377. doi:10.1037/tra0001466
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Weathers FW, Litz BT, Keane TM, Palmeri PA, Marx BP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. Accessed March 4, 2025. www.ptsd.va.gov
- Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379-1391. doi:10.1037/pas0000254
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The osttraumatic stress disorder checklist for DSM-5 (PCL- 5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Kroenke K, Spi tzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Brown TA. Confirmatory Factor Analysis for Applied Research. 2nd ed. Guilford Press; 2015.
- Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141-151. doi:10.1177/001316446002000116
- Schorr Y, Stein NR, Maguen S, Barnes JB, Bosch J, Litz BT. Sources of moral injury among war veterans: a qualitative evaluation. J Clin Psychol. 2018;74(12):2203-2218. doi:10.1002/jclp.22660
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. J Clin Psychol. 2015;71(3):229-240. doi:10.1002/jclp.22134
- Jinkerson JD. Defining and assessing moral injury: a syndrome perspective. Traumatology. 2016;22(2):122-130. doi:10.1037/trm0000069
- Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
- Maguen S, Litz B. Moral injury in veterans of war. PTSD Res Q. 2012;23(1):1-6. www.vva1071.org/uploads/3/4/4/6/34460116/moral_injury_in_veterans_of_war.pdf
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17(1):8-13. doi:10.1177/1534765610395615
- Wisco BE, Marx BP, May CL, et al. Moral injury in U.S. combat veterans: results from the national health and resilience in veterans study. Depress Anxiety. 2017; 34(4):340-347. doi:10.1002/da.22614
- Bryan CJ, Bryan AO, Anestis MD, et al. Measuring moral injury: psychometric properties of the moral injury events scale in two military samples. Assessment. 2016;23(5):557- 570. doi:10.1177/1073191115590855
- Currier JM, Smith PN, Kuhlman S. Assessing the unique role of religious coping in suicidal behavior among U.S. Iraq and Afghanistan veterans. Psychol Relig Spiritual. 2017;9(1):118-123. doi:10.1037/rel0000055
- Kopacz MS, Connery AL, Bishop TM, et al. Moral injury: a new challenge for complementary and alternative medicine. Complement Ther Med. 2016;24:29-33. doi:10.1016/j.ctim.2015.11.003
- Vargas AF, Hanson T, Kraus D, Drescher K, Foy D. Moral injury themes in combat veterans’ narrative responses from the national vietnam veterans’ readjustment study. Traumatology. 2013;19(3):243-250. doi:10.1177/1534765613476099
- Borges LM, Barnes SM, Farnsworth JK, Bahraini NH, Brenner LA. A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S138-S140. doi:10.1037/tra0000698
- Borges LM, Holliday R, Barnes SM, et al. A longitudinal analysis of the role of potentially morally injurious events on COVID-19-related psychosocial functioning among healthcare providers. PLoS One. 2021;16(11):e0260033. doi:10.1371/journal.pone.0260033
- Currier JM, Holland JM, Rojas-Flores L, Herrera S, Foy D. Morally injurious experiences and meaning in Salvadorian teachers exposed to violence. Psychol Trauma. 2015;7(1):24-33. doi:10.1037/a0034092
- Nickerson A, Schnyder U, Bryant RA, Schick M, Mueller J, Morina N. Moral injury in traumatized refugees. Psychother Psychosom. 2015;84(2):122-123. doi:10.1159/000369353
- Papazoglou K, Chopko B. The role of moral suffering (moral distress and moral injury) in police compassion fatigue and PTSD: An unexplored topic. Front Psychol. 2017;8:1999. doi:10.3389/fpsyg.2017.01999
- Papazoglou K, Blumberg DM, Chiongbian VB, et al. The role of moral injury in PTSD among law enforcement officers: a brief report. Front Psychol. 2020;11:310. doi:10.3389/fpsyg.2020.00310
- Martin WB, Holliday R, LePage JP. Trauma and diversity: moral injury among justice involved veterans: an understudied clinical concern. Stresspoints. 2020;33(5).
- Currier JM, Drescher KD, Nieuwsma J. Future directions for addressing moral injury in clinical practice: concluding comments. In: Currier JM, Drescher KD, Nieuwsma J, eds. Addressing Moral Injury in Clinical Practice. American Psychological Association; 2021:261-271. doi:10.1037/0000204-015
- Alexander AR, Mendez L, Kerig PK. Moral injury as a transdiagnostic risk factor for mental health problems in detained youth. Crim Justice Behav. 2023;51(2):194-212. doi:10.1177/00938548231208203
- DeCaro JB, Straka K, Malek N, Zalta AK. Sentenced to shame: moral injury exposure in former lifers. Psychol Trauma. 2024; 15(5):722-730. doi:10.1037/tra0001400
- Orak U, Kelton K, Vaughn MG, Tsai J, Pietrzak RH. Homelessness and contact with the criminal legal system among U.S. combat veterans: an exploration of potential mediating factors. Crim Justice Behav. 2022;50(3):392-409. doi:10.1177/00938548221140352
- Bronson J, Carson EA, Noonan M. Veterans in Prison and Jail, 2011-12. US Department of Justice, Bureau of Justice Statistics; Published December 2015. Accessed March 4, 2025. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
- Maruschak LM, Bronson J, Alper M. Veterans in Prison: Survey of Prison Inmates, 2016. US Department of Justice, Bureau of Justice Statistics; March 2021. Accessed March 4, 2025. https://bjs.ojp.gov/redirect-legacy/content/pub/pdf/vpspi16st.pdf
- Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justiceinvolved veterans. Epidemiol Rev. 2015;37:163-176. doi:10.1093/epirev/mxu003
- Finlay AK, Owens MD, Taylor E, et al. A scoping review of military veterans involved in the criminal justice system and their health and healthcare. Health Justice. 2019;7(1):6. doi:10.1186/s40352-019-0086-9
- Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2020;30(1):41-49. doi:10.1080/10530789.2019.1711306
- Wortzel HS, Binswanger IA, Anderson CA, Adler LE. Suicide among incarcerated veterans. J Am Acad Psychiatry Law. 2009;37(1):82-91.
- Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. doi:10.1097/PRA.0000000000000520
- Asencio EK, Burke PJ. Does incarceration change the criminal identity? A synthesis of labeling and identity theory perspectives on identity change. Sociol Perspect. 2011;54(2):163-182. doi:10.1525/sop.2011.54.2.163
- Borges LM, Desai A, Barnes SM, Johnson JPS. The role of social determinants of health in moral injury: implications and future directions. Curr Treat Options Psychiatry. 2022;9(3):202-214. doi:10.1007/s40501-022-00272-4
- Houle SA, Ein N, Gervasio J, et al. Measuring moral distress and moral injury: a systematic review and content analysis of existing scales. Clin Psychol Rev. 2024;108:102377. doi:10.1016/j.cpr.2023.102377
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the moral injury events scale. Mil Med. 2013;178(6):646-652. doi:10.7205/MILMED-D-13-00017
- Zerach G, Ben-Yehuda A, Levi-Belz Y. Prospective associations between psychological factors, potentially morally injurious events, and psychiatric symptoms among Israeli combatants: the roles of ethical leadership and ethical preparation. Psychol Trauma. 2023;15(8):1367-1377. doi:10.1037/tra0001466
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American Psychiatric Association; 2013.
- Weathers FW, Litz BT, Keane TM, Palmeri PA, Marx BP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. Accessed March 4, 2025. www.ptsd.va.gov
- Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379-1391. doi:10.1037/pas0000254
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The osttraumatic stress disorder checklist for DSM-5 (PCL- 5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Kroenke K, Spi tzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Brown TA. Confirmatory Factor Analysis for Applied Research. 2nd ed. Guilford Press; 2015.
- Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141-151. doi:10.1177/001316446002000116
- Schorr Y, Stein NR, Maguen S, Barnes JB, Bosch J, Litz BT. Sources of moral injury among war veterans: a qualitative evaluation. J Clin Psychol. 2018;74(12):2203-2218. doi:10.1002/jclp.22660
Examining Moral Injury in Legal-Involved Veterans: Psychometric Properties of the Moral Injury Events Scale
Examining Moral Injury in Legal-Involved Veterans: Psychometric Properties of the Moral Injury Events Scale
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
Validation of the Timberlawn Couple and Family Evaluation Scales–Self-Report in Veterans with PTSD
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
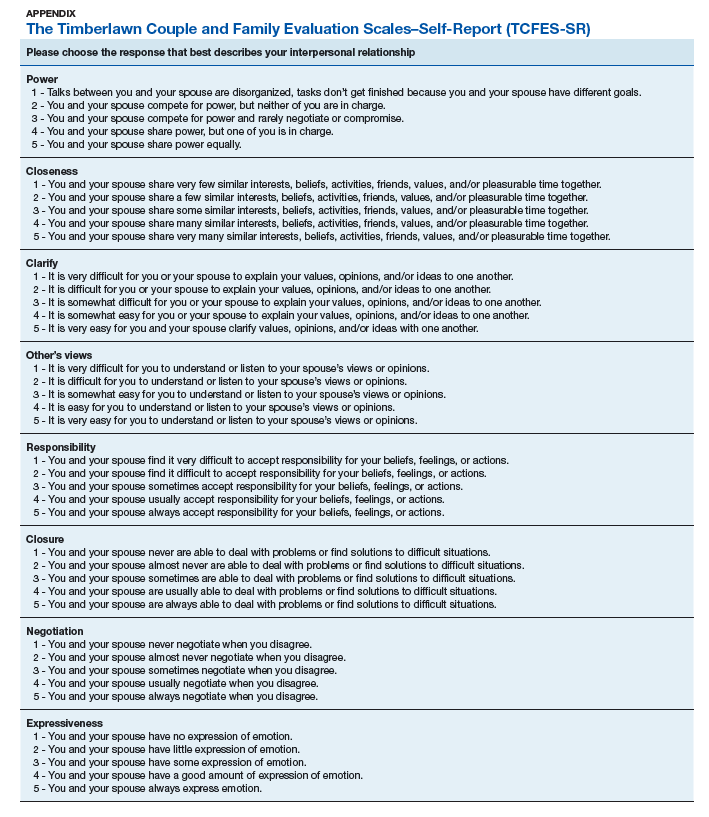
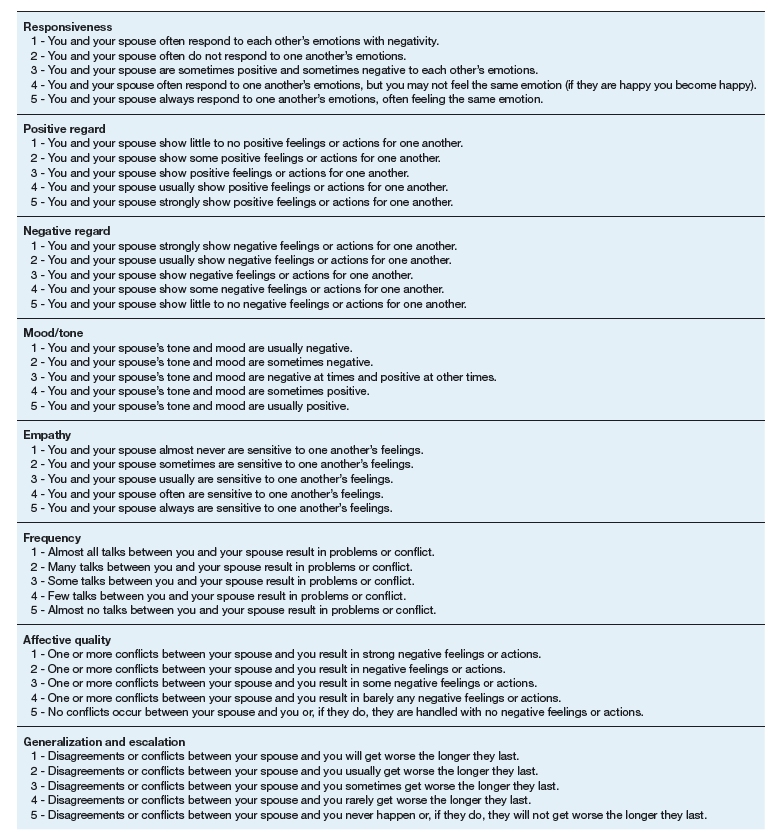
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
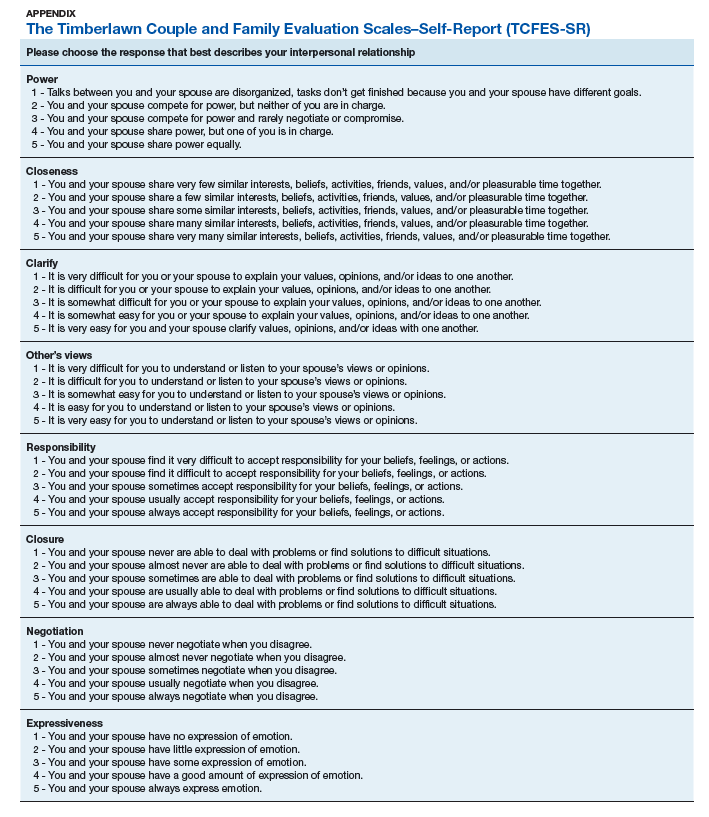
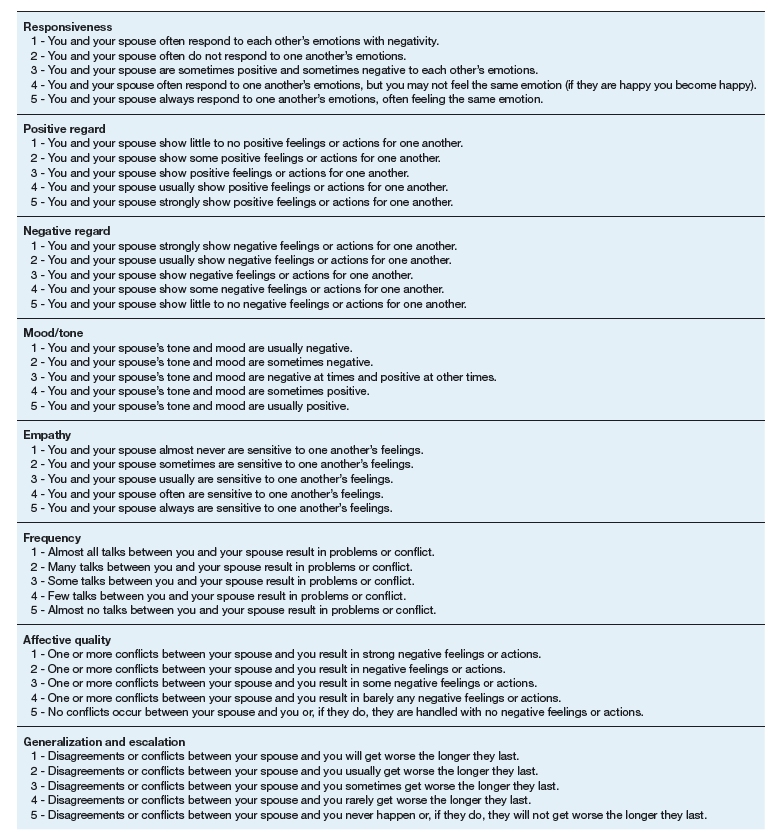
Although about 8.3% of the general adult civilian population will be diagnosed with posttraumatic stress disorder (PTSD) in their lifetime, rates of PTSD are even higher in the veteran population.1,2 PTSD is associated with a number of psychosocial consequences in veterans, including decreased intimate partner relationship functioning.3,4 For example, Cloitre and colleagues reported that PTSD is associated with difficulty with socializing, intimacy, responsibility, and control, all of which increase difficulties in intimate partner relationships.5 Similarly, researchers also have noted that traumatic experiences can affect an individual’s attachment style, resulting in progressive avoidance of interpersonal relationships, which can lead to marked difficulties in maintaining and beginning intimate partner relationships.6,7 Despite these known consequences of PTSD, as Dekel and Monson noted in a review,further research is still needed regarding the mechanisms by which trauma and PTSD result in decreased intimate partner relationship functioning among veterans.8 Nonetheless, as positive interpersonal relationships are associated with decreased PTSD symptom severity9,10 and increased engagement in PTSD treatment,11 determining methods of measuring intimate partner relationship functioning in veterans with PTSD is important to inform future research and aid the provision of care.
To date, limited research has examined the valid measurement of intimate partner relationship functioning among veterans with PTSD. Many existing measures that comprehensively assess intimate partner relationship functioning are time and resource intensive. One such measure, the Timberlawn Couple and Family Evaluation Scales (TCFES), comprehensively assesses multiple pertinent domains of intimate partner relationship functioning (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict).12 By assessing multiple domains, the TCFES offers a method of understanding the specific components of an individual’s intimate partner relationship in need of increased clinical attention.12 However, the TCFES is a time- and labor-intensive observational measure that requires a couple to interact while a blinded, independent rater observes and rates their interactions using an intricate coding process. This survey structure precludes the ability to quickly and comprehensively assess a veteran’s intimate partner functioning in settings such as mental health outpatient clinics where mental health providers engage in brief, time-limited psychotherapy. As such, brief measures of intimate partner relationship functioning are needed to best inform clinical care among veterans with PTSD.
The primary aim of the current study was to create a psychometrically valid, yet brief, self-report version of the TCFES to assess multiple domains of intimate partner relationship functioning. The psychometric properties of this measure were assessed among a sample of US veterans with PTSD who were in an intimate partner relationship. We specifically examined factor structure, reliability, and associations to established measures of specific domains of relational functioning.
Methods
Ninety-four veterans were recruited via posted advertisements, promotion in PTSD therapy groups/staff meetings, and word of mouth at the Dallas Veterans Affairs Medical Center (VAMC). Participants were eligible if they had a documented diagnosis of PTSD as confirmed in the veteran’s electronic medical record and an affirmative response to currently being involved in an intimate partner relationship (ie, legally married, common-law spouse, involved in a relationship/partnership). There were no exclusion criteria.
Interested veterans were invited to complete several study-related self-report measures concerning their intimate partner relationships that would take about an hour. They were informed that the surveys were voluntary and confidential, and that they would be compensated for their participation. All veterans who participated provided written consent and the study was approved by the Dallas VAMC institutional review board.
Of the 94 veterans recruited, 3 veterans’ data were removed from current analyses after informed consent but before completing the surveys when they indicated they were not currently in a relationship or were divorced. After consent, the 91 participants were administered several study-related self-report measures. The measures took between 30 and 55 minutes to complete. Participants were then compensated $25 for their participation.
Intimate Partner Relationship Functioning
The 16-item TCFES self-report version (TCFES-SR) was developed to assess multiple domains of interpersonal functioning (Appendix). The observational TCFES assesses 5 intimate partner relationship characteristic domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict) during a couple’s interaction by an independent trained rater.12 Each of the 16 TCFES-SR items were modeled after original constructs measured by the TCFES, including power, closeness, clarify, other’s views, responsibility, closure, negotiation, expressiveness, responsiveness, positive regard, negative regard, mood/tone, empathy, frequency, affective quality, and generalization and escalation. To maintain consistency with the TCFES, each item of the TCFES-SR was scored from 1 (severely dysfunctional) to 5 (highly functional). Additionally, all item wording for the TCFES-SR was based on wording in the TCFES manual after consultation with an expert who facilitated the development of the TCFES.12 On average, the TCFES-SR took 5 to 10 minutes to complete.
To measure concurrent validity of the modified TCFES-SR, several additional interpersonal measures were selected and administered based on prior research and established domains of the TCFES. The Positive and Negative Quality in Marriage Scale (PANQIMS) was administered to assess perceived attitudes toward a relationship.13,14 The PANQIMS generates 2 subscales: positive quality and negative quality in the relationship. Because the PANQIMS specifically assesses married relationships and our sample included married and nonmarried participants, wording was modified (eg, “spouse/partner”).
The relative power subscale of the Network Relationships Inventory–Relationship Qualities Version (NRI-RQV) measure was administered to assess the unequal/shared role romantic partners have in power equality (ie, relative power).15
The Revised Dyadic Adjustment Scale (RDAS) is a self-report measure that assesses multiple dimensions of marital adjustment and functioning.16 Six subscales of the RDAS were chosen based on items of the TCFES-SR: decision making, values, affection, conflict, activities, and discussion.
The Interpersonal Reactivity Index (IRI) empathetic concern subscale was administered to assess empathy across multiple contexts and situations17 and the Experiences in Close Relationships-Revised Questionnaire (ECR-R) was administered to assess relational functioning by determining attachment-related anxiety and avoidance.18
Sociodemographic Information
A sociodemographic questionnaire also was administered. The questionnaire assessed gender, age, education, service branch, length of interpersonal relationship, race, and ethnicity of the veteran as well as gender of the veteran’s partner.
Statistical Analysis
Factor structure of the TCFES-SR was determined by conducting an exploratory factor analysis. To allow for correlation between items, the Promax oblique rotation method was chosen.19 Number of factors was determined by agreement between number of eigenvalues ≥ 1, visual inspection of the scree plot, and a parallel analysis. Factor loadings of ≥ 0.3 were used to determine which items loaded on to which factors.
Convergent validity was assessed by conducting Pearson’s bivariate correlations between identified TCFES-SR factor(s) and other administered measures of interpersonal functioning (ie, PANQIMS positive and negative quality; NRI-RQV relative power subscale; RDAS decision making, values, affection, conflict, activities, and discussion subscales; IRI-empathetic concern subscale; and ECR-R attachment-related anxiety and avoidance subscales). Strength of relationship was determined based on the following guidelines: ± 0.3 to 0.49 = small, ± 0.5 to 0.69 = moderate, and ± 0.7 to 1.00 = large. Internal consistency was also determined for TCFES-SR factor(s) using Cronbach’s α. A standard level of significance (α=.05) was used for all statistical analyses.
Results
Eighty-six veterans provided complete data (Table 1). The Kaiser-Meyer-Olkin measure of sampling adequacy was indicative that sample size was adequate (.91), while Bartlett’s test of sphericity found the variables were suitable for structure detection, χ2 (120) = 800.00, P < .001. While 2 eigenvalues were ≥ 1, visual inspection of the scree plot and subsequent parallel analysis identified a unidimensional structure (ie, 1 factor) for the TCFES-SR. All items were found to load to this single factor, with all loadings being ≥ 0.5 (Table 2). Additionally, internal consistency was excellent for the scale (α = .93).
Pearson’s bivariate correlations were significant (P < .05) between TCFES-SR total score, and almost all administered interpersonal functioning measures (Table 3). Interestingly, no significant associations were found between any of the administered measures, including the TCFES-SR total score, and the IRI-empathetic concern subscale (P > .05).
Discussion
These findings provide initial support for the psychometric properties of the TCFES-SR, including excellent internal consistency and the adequate association of its total score to established measures of interpersonal functioning. Contrary to the TCFES, the TCFES-SR was shown to best fit a unidimensional factor rather than a multidimensional measure of relationship functioning. However, the TCFES-SR was also shown to have strong convergent validity with multiple domains of relationship functioning, indicating that the measure of overall intimate partner relationship functioning encompasses a number of relational domains (ie, structure, autonomy, problem solving, affect regulation, and disagreement/conflict). Critically, the TCFES-SR is brief and was administered easily in our sample, providing utility as clinical tool to be used in time-sensitive outpatient settings.
A unidimensional factor has particular strength in providing a global portrait of perceived intimate partner relationship functioning, and mental health providers can administer the TCFES-SR to assess for overall perceptions of intimate partner relationship functioning rather than administering a number of measures focusing on specific interpersonal domains (eg, decision making processes or positive/negative attitudes towards one’s relationship). This allows for the quick assessment (ie, 5-10 minutes) of overall intimate partner relationship functioning rather than administration of multiple self-report measures which can be time-intensive and expensive. However, the TCFES-SR also is limited by a lack of nuanced understanding of perceptions of functioning specific to particular domains. For example, the TCFES-SR score cannot describe intimate partner functioning in the domain of problem solving. Therefore, brief screening tools need to be developed that assess multiple intimate partner relationship domains.
Importantly, overall intimate partner relationship functioning as measured by the TCFES-SR may not incorporate perceptions of relationship empathy, as the total score did not correlate with a measure of empathetic concern (ie, the IRI-empathetic concern subscale). As empathy was based on one item in the TCFES-SR vs 7 in the IRI-empathetic concern subscale, it is unclear if the TCFES-SR only captures a portion of the construct of empathy (ie, sensitivity to partner) vs the comprehensive assessment of trait empathy that the IRI subscale measures. Additionally, the IRI-empathetic concern subscale did not significantly correlate with any of the other administered measures of relationship functioning. Given the role of empathy in positive, healthy intimate partner relationships, future research should explore the role of empathetic concern among veterans with PTSD as it relates to overall (eg, TCFES-SR) and specific aspects of intimate partner relationship functioning.20
While the clinical applicability of the TCFES-SR requires further examination, this measure has a number of potential uses. Information captured quickly by the TCFES-SR may help to inform appropriate referral for treatment. For instance, veterans reporting low total scores on the TCFES-SR may indicate a need for a referral for intervention focused on improving overall relationship functioning (eg, Integrative Behavioral Couple Therapy).21,22 Measurement-based care (ie, tracking and discussing changes in symptoms during treatment using validated self-report measures) is now required by the Joint Commission as a standard of care,and has been shown to improve outcomes in couples therapy.23,24 As a brief self-report measure, the TCFES-SR may be able to facilitate measurement-based care and assist providers in tracking changes in overall relationship functioning over the course of treatment. However, the purpose of the current study was to validate the TCFES-SR and not to examine the utility of the TCFES-SR in clinical care; additional research is needed to determine standardized cutoff scores to indicate a need for clinical intervention.
Limitations
Several limitations should be noted. The current study only assessed perceived intimate partner relationship functioning from the perspective of the veteran, thus limiting implications as it pertains to the spouse/partner of the veteran. PTSD diagnosis was based on chart review rather than a psychodiagnostic measure (eg, Clinician Administered PTSD Scale); therefore, whether this diagnosis was current or in remission was unclear. Although our sample was adequate to conduct an exploratory factor analysis,the overall sample size was modest, and results should be considered preliminary with need for further replication.25 The sample was also primarily male, white or black, and non-Hispanic; therefore, results may not generalize to a more sociodemographically diverse population. Finally, given the focus of the study to develop a self-report measure, we did not compare the TCFES-SR to the original TCFES. Thus, further research examining the relationship between the TCFES-SR and TCFES may be needed to better understand overlap and potential incongruence in these measures, and to ascertain any differences in their factor structures.
Conclusion
This study is novel in that it adapted a comprehensive observational measure of relationship functioning to a self-report measure piloted among a sample of veterans with PTSD in an intimate partner relationship, a clinical population that remains largely understudied. Although findings are preliminary, the TCFES-SR was found to be a reliable and valid measure of overall intimate partner relationship functioning. Given the rapid administration of this self-report measure, the TCFES-SR may hold clinical utility as a screen of intimate partner relationship deficits in need of clinical intervention. Replication in a larger, more diverse sample is needed to further examine the generalizability and confirm psychometric properties of the TCFES-SR. Additionally, further understanding of the clinical utility of the TCFES-SR in treatment settings remains critical to promote the development and maintenance of healthy intimate partner relationships among veterans with PTSD. Finally, development of effective self-report measures of intimate partner relationship functioning, such as the TCFES-SR, may help to facilitate needed research to understand the effect of PTSD on establishing and maintaining healthy intimate partner relationships among veterans.
Acknowledgments
The current study was funded by the Timberlawn Psychiatric Research Foundation. This material is the result of work supported in part by the US Department of Veterans Affairs; the Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC) for Suicide Prevention; Sierra Pacific MIRECC; and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
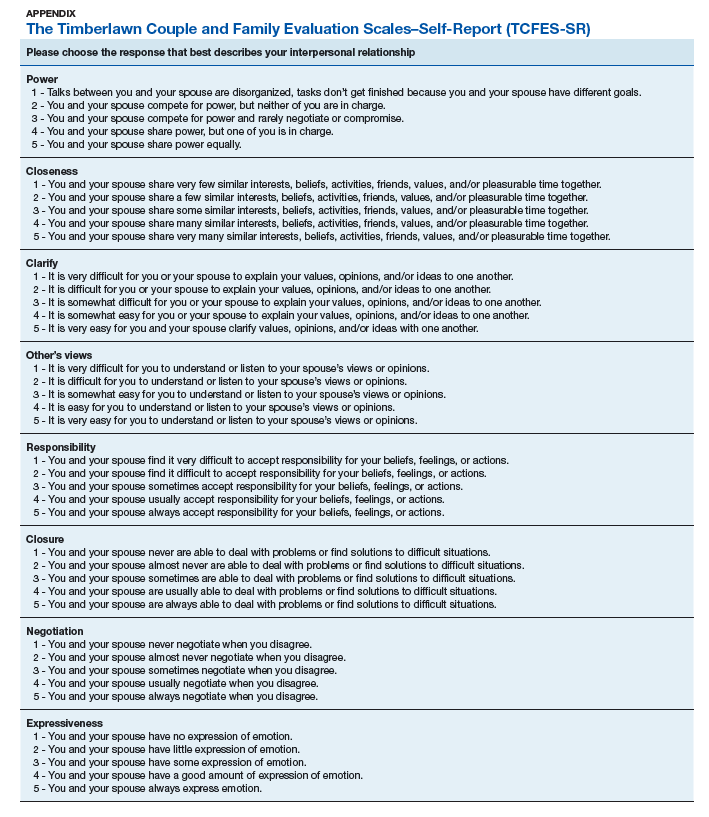
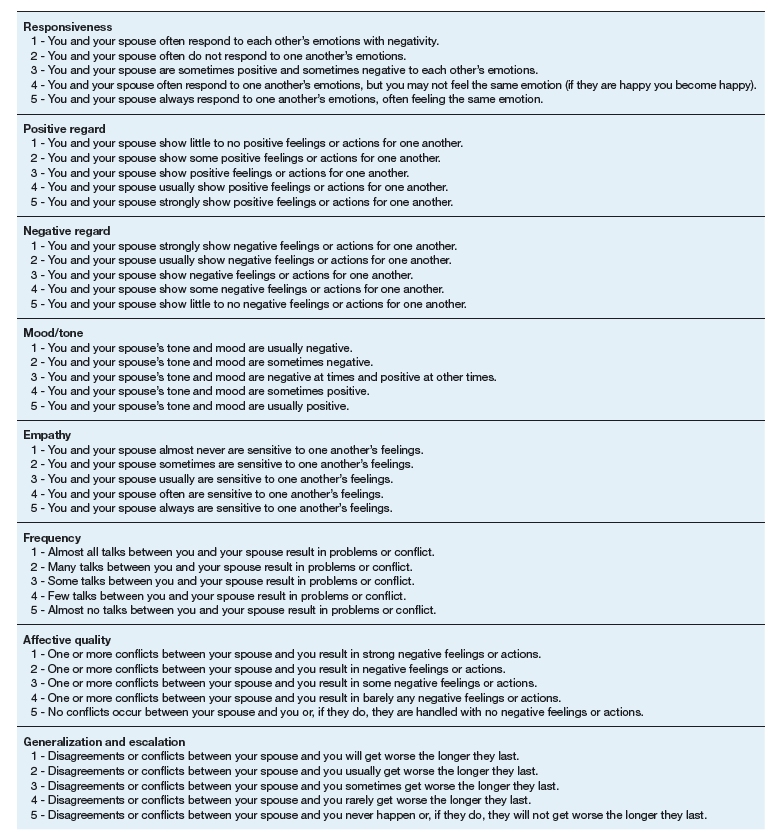
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.
1. Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537-547.
2. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953.
3. Galovski T, Lyons JA. Psychological sequelae of combat violence: a review of the impact of PTSD on the veteran’s family and possible interventions. Aggress Violent Behav. 2004;9(5):477-501.
4. Ray SL, Vanstone M. The impact of PTSD on veterans’ family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. 2009;46(6):838-847.
5. Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav Ther. 2005;36(2):119-124.
6. McFarlane AC, Bookless C. The effect of PTSD on interpersonal relationships: issues for emergency service works. Sex Relation Ther. 2001;16(3):261-267.
7. Itzhaky L, Stein JY, Levin Y, Solomon Z. Posttraumatic stress symptoms and marital adjustment among Israeli combat veterans: the role of loneliness and attachment. Psychol Trauma. 2017;9(6):655-662.
8. Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: current knowledge and future directions. Aggress Violent Behav. 2010;15(4):303-309.
9. Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J Fam Psychol. 2010;24(3):280-288.
10. Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress. 2008;21(4):394-401.
11. Meis LA, Noorbaloochi S, Hagel Campbell EM, et al. Sticking it out in trauma-focused treatment for PTSD: it takes a village. J Consult Clin Psychol. 2019;87(3):246-256.
12. Lewis JM, Gossett JT, Housson MM, Owen MT. Timberlawn Couple and Family Evaluation Scales. Dallas, TX: Timberlawn Psychiatric Research Foundation; 1999.
13. Fincham FD, Linfield KJ. A new look at marital quality: can spouses feel positive and negative about their marriage? J Fam Psychol. 1997;11(4):489-502.
14. Kaplan KJ. On the ambivalence-indifference problem in attitude theory and measurement: a suggested modification of the semantic differential technique. Psychol Bull. 1972;77(5):361-372.
15. Buhrmester D, Furman W. The Network of Relationship Inventory: Relationship Qualities Version [unpublished measure]. University of Texas at Dallas; 2008.
16. Busby DM, Christensen C, Crane DR, Larson JH. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J Marital Fam Ther. 1995;21(3):289-308.
17. Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog Sel Doc Psychol. 1980;10:85.
18. Fraley RC, Waller NG, Brennan KA. An item-response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78(2):350-365.
19. Tabachnick BG, Fidell L. Using Multivariate Statistics. 6th ed. Boston, MA: Pearson; 2013.
20. Sautter FJ, Armelie AP, Glynn SM, Wielt DB. The development of a couple-based treatment for PTSD in returning veterans. Prof Psychol Res Pr. 2011;42(1):63-69.
21. Jacobson NS, Christensen A, Prince SE, Cordova J, Eldridge K. Integrative behavioral couple therapy: an acceptance-based, promising new treatment of couple discord. J Consult Clin Psychol. 2000;9(2):351-355.
22. Makin-Byrd K, Gifford E, McCutcheon S, Glynn S. Family and couples treatment for newly returning veterans. Prof Psychol Res Pr. 2011;42(1):47-55.
23. Peterson K, Anderson J, Bourne D. Evidence Brief: Use of Patient Reported Outcome Measures for Measurement Based Care in Mental Health Shared Decision Making. Washington, DC: Department of Veterans Affairs; 2018. https://www.ncbi.nlm.nih.gov/books/NBK536143. Accessed September 13, 2019.
24. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179-188.
25. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1-9.