User login
FRAX Prediction With and Without Bone Mineral Density Testing
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
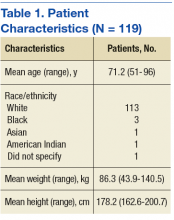
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
In the U.S. about 2 million men have osteoporosis.1 About 1 in 5 men will experience an osteoporotic-related fracture in his lifetime.2 In addition, men with hip fracture have a higher mortality rate compared with that of women with hip fracture.3 The National Osteoporosis Foundation guidelines and the Endocrine Society guidelines recommend that all men aged ≥ 70 years have bone mineral density (BMD) testing. Depending on risk factors, osteoporosis screening may be appropriate for men aged ≥ 50 years. A BMD with a T-score of -2.5 or lower is classified as osteoporosis.2
In addition to osteoporosis, osteopenia also negatively impacts men. Osteopenia is defined as a BMD with a T-score of -1 to -2.5.2 According to the National Health and Nutrition Examination Survey (NHANES), about 30% of men aged ≥ 50 years have osteopenia.4 FRAX is a fracture risk assessment tool that is used to predict the 10-year risk of fracture in untreated patients with osteopenia. The FRAX tool has been validated with the use of BMD testing only at the femoral neck; it has not been validated in other parts of the body. Treatment is indicated if the 10-year fracture risk is > 20% for major osteoporotic fractures and > 3% for hip fractures, based on the FRAX calculation.2
The following risk factors are used in the FRAX calculation: age; sex; weight (kilograms); height (centimeters); previous fracture (yes or no); parental history of hip fracture (yes or no); current smoker (yes or no); oral glucocorticoid exposure currently or for > 3 months in the past (yes or no); rheumatoid arthritis (yes or no); secondary osteoporosis or a disorder strongly associated with osteoporosis, including type 1 diabetes mellitus, osteogenesis imperfecta in adults, untreated long-standing hyperthyroidism, hypogonadism, premature menopause, chronic malnutrition, malabsorption, or chronic liver disease (yes or no); 3 or more units of alcohol daily (yes or no); and BMD.5
A dual-energy X-ray absorptiometry (DXA) examination is needed to determine BMD. However, a DXA examination is not always feasible for patients who have limited access, transportation challenges, require the use of assistive devices, and may be unaware of the importance of BMD testing.
The FRAX calculation can be obtained with or without BMD. Gadam and colleagues compared FRAX calculations with and without BMD to predict the 10-year risk of fracture.6 Their study found that 84% of patients had an identical fracture risk prediction whether or not BMD was included. The only risk factor evaluated that was significantly different between those with different treatment predictions and those with identical treatment predictions was age. However, the majority of patients included were female (96%).
No studies existed that compared fracture prediction risk with and without BMD in a male-only population. The purpose of this study was to determine whether FRAX without BMD was as effective as FRAX with BMD to predict the risk of osteoporotic fractures and provide an identical treatment recommendation in male veteran patients at the Lexington VAMC in Kentucky.
Methods
A retrospective chart review was conducted at the Lexington VAMC. Approval was obtained from the Lexington VAMC Institutional Review Board and Research and Development Committee. Patients were identified using the computerized patient record system (CPRS). Included patients were male, ≥ 50 years, had a documented DXA in CPRS from January 2006 to September 2015, and had a previous fracture determined by ICD-9 codes. Patients were excluded if they were diagnosed with osteoporosis or were ever treated for osteoporosis before a DXA scan.
Data collection included patient’s age, gender, race, glucocorticoid use for at least 3 months within 1 year prior to DXA, body weight within 3 months prior to DXA, height within 1 year prior to DXA, family history of fracture, previous fall or fracture, diagnosis of rheumatoid arthritis, smoking status at the time of DXA, alcohol intake of at least 3 drinks per day at the time of DXA, and vitamin D level within 1 year prior to DXA. In order to find a clinically significant difference (P < .05) with a power of 80%, a sample size of 64 patients was needed.
Each patient’s FRAX predictions were calculated with and without BMD. Patients were then separated into 2 groups: those who had an identical treatment recommendation when calculating FRAX with and without BMD, and those who had a different treatment recommendation when calculating FRAX with and without BMD. Binary variables for each group were compared using the Fisher exact test, and numeric variables were compared using a simple Student’s t test.
Results
After screening 1,510 patients, only 119 patients met the criteria and were included in the study (Figure). All patients included were male. Mean age was 71.2 years and 113 (95.0%) were white (Table 1).
Of the 119 patients included in the study, 98 patients (82.4%) had the same treatment recommendation when the FRAX score was calculated with and without BMD. The remaining 21 patients (17.6%) had different treatment recommendations when FRAX scores were calculated with BMD compared with FRAX scores calculated without BMD. Treatment was recommended based on risk prediction for 43 of the 98 patients who had identical treatment recommendations. Of the 21 patients who had different treatment recommendations, treatment was recommended based on risk prediction for 14 patients when FRAX scores were calculated with BMD. Treatment was recommended for the other 7 patients when FRAX scores were calculated without BMD.
Of the numeric variables evaluated, mean age, femoral neck BMD, and T-score were all significantly different between the 2 groups (Table 2). Patients with an identical treatment recommendation were a mean age of 67.9 years (SD: 10.2 y), and patients with different treatment recommendations were a mean age of 62.2 years (SD: 8.9 y) (P = .011). Patients with an identical treatment recommendation had a mean BMD of 0.9 (SD: 0.2), and patients with different treatment recommendations had a mean BMD of 0.8 (SD: 0.1) (P = .021). Patients with an identical treatment recommendation had a mean T-score of -1.7 (SD: 1.2), and patients with different treatment recommendations had a mean T-score of -2.3 (SD: 1.1) (P = .031). Mean weight, height, and vitamin D level were not statistically significantly different between the 2 groups.
Of the binary variables evaluated, only glucocorticoid use was significantly different between the 2 groups. Of the patients with an identical treatment recommendation, 4 (4.1%) received a glucocorticoid.
Discussion
The purpose of this retrospective study was to determine whether using FRAX without BMD was as effective as using FRAX with BMD in predicting the risk of osteoporotic fractures and in providing identical treatment recommendations in male veteran patients. The results of this study revealed that FRAX calculations without BMD provided identical treatment recommendations as FRAX calculations with BMD for 82.4% of male veteran patients. These findings were similar to the findings of another study by Gadam and colleagues, in which 84% of patients had identical treatment recommendations when calculating FRAX scores with and without BMD.6 In contrast, a prospective cohort study by Ettinger and colleagues found that the addition of BMD to the FRAX calculation enhanced the performance of the FRAX tool by correctly identifying more patients who experienced a fracture within the following 10 years.8
Several of the risk factors evaluated in the present study were indicative of an identical treatment recommendation. Age was one of the risk factors that differed significantly between the 2 groups. The mean age of patients with an identical treatment recommendation was 67.9 years, and the mean age of patients with different treatment recommendations was 62.2 years (P = .011). These findings opposed the findings in the Gadam and colleagues’ study.6 The results of that study revealed that younger age rather than older age was more indicative of an identical treatment recommendation. The study by Gadam and colleagues included both male and female patients; however, the majority of patients included in the Gadam study were female (96%).6 Because the present study included only male patients, a comparison of the results was difficult because of the different patient populations.
A higher T-score (P = .031) and a higher BMD (P = .021) were the other 2 risk factors associated with an identical treatment recommendation with and without BMD. The Gadam and colleagues study did not find these to be significant risk factors for identifying an identical treatment recommendation.6
The FRAX calculation without BMD identified all the patients meeting treatment criteria based on the FRAX calculation with BMD except for 14 of the 119 patients (11.8%). Therefore, > 88% of patients who met treatment criteria based on FRAX calculated with BMD also met treatment criteria based on FRAX without BMD.
The FRAX calculation has several advantages, including risk stratification in men and identifying those with other conditions that may predispose them to a fracture.7 Therefore, before obtaining a DXA scan, it would be reasonable to calculate a FRAX score without BMD to identify patients who are at high risk for fracture but who may not receive treatment because they are not considered to need a DXA scan or a DXA scan is not feasible.
Limitations
Currently, FRAX is validated only using femoral neck BMD. This study was a retrospective chart review only; no information was obtained from communicating with the patient, including the patient’s past medical history and family history. Also, this study had a small sample size: Of the 1,510 patients screened, only 119 met inclusion criteria. None of the 119 patients evaluated had a family history of fracture documented in their CPRS. Therefore, several of the patient’s 10-year fracture risk scores may be underestimated if one or both of their parents experienced a fracture. Last, the majority of patients included in this study were white, so the results of this study cannot necessarily be generalized to other races.
Conclusion
The majority of male patients had an identical treatment recommendation when a FRAX score was calculated with and without BMD. Older age, higher BMD, and higher T-score were all indicative of an identical treatment recommendation. Larger studies are necessary in order to validate the FRAX tool without the use of femoral neck BMD. However, the FRAX tool alone can be beneficial to identify male patients who should have a DXA scan performed to obtain a BMD. If a male patient’s FRAX score suggests risk for osteoporotic fracture, then a DXA scan should be completed to obtain a BMD if feasible.
Additionally, when obtaining a BMD is not feasible to predict fracture risk, the FRAX tool alone may be useful a majority of the time to accurately determine treatment recommendations in male patients aged > 65 years. The results of this study lead the authors to believe that FRAX without BMD in male patients aged > 65 years will appropriately identify more patients for treatment. ˜
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Lexington VA Medical Center.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.
1. Sweet MG, Sweet JM, Jeremiah MP, Galazka SS. Diagnosis and treatment of osteoporosis. Am Fam Physician. 2009;79(3):193-200.
2. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381.
3. Khan AA, Hodsman AB, Papaioannou A, Kendler D, Brown JP, Olszynski WP. Management of osteoporosis in men: an update and case example. CMAJ. 2007;176(3):345-348.
4. Looker AC, Melton LJ III, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005-2006 compared with NHANES III. J Bone Miner Res. 2010;25(1):64-71.
5. Kanas JA; World Health Organization Scientific Group. Assessment of osteoporosis at the primary health care level. https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Published 2007. Accessed March 29, 2017.
6. Gadam RK, Schlauch K, Izuora KE. FRAX prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract. 2013;19(5):780-784.
7. Siris E, Delmas PD. Assessment of 10-year absolute fracture risk: a new paradigm with worldwide application. Osteoporosis Int. 2008;19(4):383-384.
8. Ettinger B, Liu H, Blackwell T, et al. Validation of FRC, a fracture risk assessment tool, in a cohort of older men: the osteoporotic fractures in men (MrOS) study. J Clin Densitom. 2012;15(3):334-342.