User login
Smartphone Policy for Attending Rounds
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
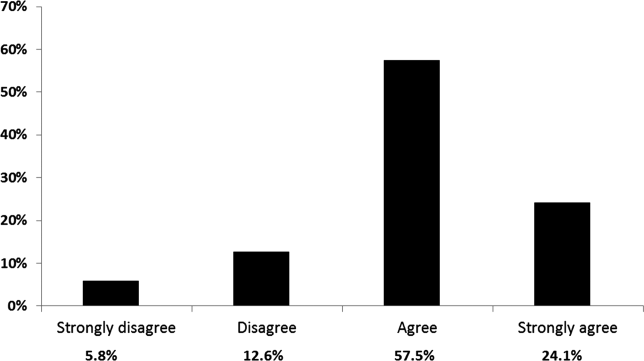
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
Despite the many benefits of smartphones for physicians, there are also potential downsides to utilizing these devices in the patient care setting. Prior research at our hospital found that smartphone use during inpatient attending rounds can distract faculty and residents, and nearly 80% of attendings favored the institution of codes of conduct governing appropriate use of smartphones during rounds.[1] Based on these findings, a policy regulating faculty and resident smartphone use was instituted in February 2012 in the Departments of Medicine and Pediatrics at our hospital.[1]
Although our faculty's enthusiasm for the smartphone policy was clear, residents' attitudes toward this new regulation were unknown. Born in the 1980s, today's residents are members of the millennial generation, who seamlessly integrate technology into their lives.[2, 3, 4, 5] Millennials generally do not perceive their multitasking with technology to be rude or distracting.[2] Having grown up with the Internet, they employ digital tools as an inherent sixth sense,[3] and view their use of technology as the defining characteristic of their generation.[5]
Housestaff feedback was instrumental in shaping the specifics of the smartphone policy.[1] However, given the primacy of technology in the life of the millennial, it is plausible that residents would resent restrictions on their smartphone use. Such resentment could limit a policy's effectiveness, as well as negatively impact resident morale. With increasing discussion about the need to manage personal electronic device use in the patient care setting,[2, 6, 7, 8] we sought to assess residents' attitudes toward our hospital's smartphone policy.
METHODS
A brief survey instrument was designed to increase housestaff awareness of and evaluate their attitudes toward the smartphone policy. In November 2012, the anonymous survey was administered via SurveyMonkey (
The survey provided a summary of the policy: The smartphone code of conduct policy was instituted to minimize distraction during attending rounds. The policy applies to all team members, including faculty, and essentially states that at the start of attending rounds, all phones must be silenced or turned off. These devices are to be used during rounds only for patient care or for urgent personal/family concerns. Any use must be made explicit to the person leading rounds. Residents also received a copy of the complete policy as an attachment to the request email. A copy of this policy is available as an appendix to Katz‐Sidlow et al.[1]
The survey requested information regarding departmental affiliation, and asked whether the resident had prior awareness of the smartphone policy. Residents' attitudes were evaluated by asking for their level of agreement with the following statement: It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds. This statement was graded on a 4‐point frequency scale (strongly disagree, disagree, agree, or strongly agree). Residents' attitudes were further explored in a follow‐up question: Which statement most closely expresses your feelings? Three options were offered: (1) There should be no guidelines as to how team members should use smartphones during inpatient attending rounds. Every person should decide for him/herself how and when to use the phone during rounds. (2) I agree that a smartphone code of conduct for attending rounds is a good idea, but I suggest modifying the current policy (please use the text box below to explain). (3) I agree with the current smartphone code of conduct policy for attending rounds. A text box was provided for comments.
RESULTS
The overall response rate was 65% (93/142), representing 58% (57/98) of all Department of Medicine residents and 82% (36/44) of all Department of Pediatrics residents. Seventy‐one percent of respondents (57% Department of Medicine; 92% Department of Pediatrics) indicated a prior knowledge of the smartphone policy.
Overall, 82% of respondents agreed or strongly agreed with the statement, It is a good idea to have clear guidelines and expectations about how team members should use smartphones during attending rounds (Figure 1). Residents' responses to the follow‐up question revealed that nearly 60% agreed with the stipulations of the current policy; another 18% believed that a policy is needed, but felt that the current code should be modified. Only one resident provided a modification suggestion, which was to expand the policy to include resident work rounds.

Responses to these 2 questions differed slightly for trainees with an awareness of the preexisting policy as compared to those without prior awareness; however, these differences were not statistically significant.
CONCLUSIONS
Despite concerns that residents would resent policies regulating their use of technology, we found that the majority of residents indicated a desire for, and acceptance of, clear guidelines regarding smartphone use during inpatient rounds. Our findings are in line with prior research suggesting that millennials appreciate a structured work environment and explicit guidance regarding workplace expectations.[2, 3, 4] To minimize distraction and support residents' professionalism, we recommend that training programs develop and implement clear expectations regarding smartphone use in the active patient care setting.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.
- , , , . Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–599.
- , . The challenges and opportunities of teaching “generation y.” J Grad Med Educ. 2011;3:458–461.
- , . Millennials and the world of work: an organization and management perspective. J Bus Psychol. 2010;25:211–223.
- , , . Is your residency program ready for generation y? J Surg Educ. 2010;67:108–111.
- Pew Research Center. Millennials: a portrait of generation next. Pew Research Center Web site. February 2010. Available at: http://www.pewsocialtrends.org/files/2010/10/millennials‐confident‐connected‐open‐to‐change.pdf. Accessed May 9, 2013.
- . Spotlight case. Order interrupted by text: multitasking mishap. Agency for Healthcare Research and Quality Web site. December 2011. Available at: http://webmm.ahrq.gov/case.aspx?caseID=257. Accessed May 9, 2013.
- . Training health care professionals to deal with an explosion of electronic distraction. Neurocrit Care. 2013;18:115–117.
- ECRI Institute. Top 10 health technology hazards for 2013. ECRI Institute Web site. Available at: https://www.ecri.org/Documents/Secure/Health_Devices_Top_10_Hazards_2013.pdf. Accessed May 9, 2013.
Smartphone Use During Attending Rounds
Healthcare market research has predicted that over 80% of physicians will use smartphones by 2012.1 These handheld devices allow users immediate access to various forms of electronic media such as Internet, instant messaging, and e‐mail. Smartphones provide numerous benefits to physicians, including rapid access to medical references, research applications, and patient information.2 These devices have been used for teleconsultation3 and patient education,4 and applications have been developed for numerous clinical specialties.48
Housestaff perceive that communication improves when they use smartphones rather than traditional pagers on the inpatient service,9 and patients may have a positive view of physicians' use of handheld computers.10 Medical schools and residency programs are increasingly requiring smartphone ownership for their trainees, with the expectation that smartphone use will enhance the educational experience, ensure the highest level of patient care, improve user efficiency, and help control the costs associated with purchasing updated textbooks.7, 1113 In the future, hospitals may rely on smartphone technologies to help reduce the enormous economic burden created by inefficient communication.14
Despite their numerous benefits for physicians and patients, little is known about the potential for smartphones to distract users in clinical care settings. Studies from the psychology and traffic safety fields have documented untoward consequences when individuals use electronic devices to multitask.1519 Given these concerns, we investigated the prevalence and patterns of smartphone use during inpatient attending rounds, and whether these devices can distract team members in this period of important information transfer.
METHODS
At our institution, attending rounds are faculty‐led inpatient teaching rounds that focus on clinical care and patient management; these sessions may be conducted either in the classroom or at the bedside, depending on patient and learner needs, and faculty preference. Inpatient teams are comprised of 1 attending, housestaff, and third and fourth year medical students. Each team conducts attending rounds independently; these rounds range in length from 1 hour (Pediatrics) to 2 hours (Medicine).
A survey instrument was designed to evaluate smartphone usage patterns during hospital inpatient attending rounds, and perceived distraction from smartphones in this setting. A preliminary version of the survey was pilot tested by a group of housestaff for face validity, redundancy, and ease of use, and it was subsequently revised. For the purposes of this study, a smartphone was defined broadly as any mobile, personal communication device (cellphone, iPhone, Android, Blackberry, iPad, etc). Residents were asked about their own smartphone use, as well as their observations of supervising attendings and other learners' devices use during rounds (see Supporting Appendix 1 in the online version of this article).
In February 2011, the anonymous online survey was administered using Survey Monkey (
Respondents were not required to answer each question in order to complete the survey. With the exception of free‐text comments, all responses were either yes/no or were graded on a 5‐point frequency scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). This scale was chosen because it allowed for adequate dispersion of responses, and for the identification of meaningful smartphone usage among respondents (score 3) and data dichotomization. The z test was used to compare the proportions between independent groups.
All free‐text comments were imported into a Microsoft Word table. Comments were separated into 2 groups: housestaff and attending. Each comment was hand‐coded by 2 authors (R.J.K.‐S. and R.S.) to reach consensus for 1 of the following 4 categories: the comment was a positive statement; a negative statement; a positive/negative statement; or a neutral one, ie, neither positive nor negative. The terms positive and negative here refer to whether the statement explicitly highlighted benefits of smartphone use or a negative aspect of smartphone use, respectively. A comment was coded as positive/negative if it highlighted both benefits and drawbacks in the same comment. In addition, each comment that mentioned texting or call functions was secondarily coded as personal, patient, both, or unknown depending on the purpose of the texting or calls described in each comment. Comments were also reviewed for possible subthemes.
RESULTS
The overall response rate was 73% (156/214), with 81% (116/143) of housestaff and 56% (40/71) of faculty participating. The mean tenure of faculty respondents was 13 years. Eighty‐nine percent (103/116) of residents and 98% (39/40) of faculty owned devices, with 57% of housestaff and 28% of attendings reporting regular personal use of smartphones during attending rounds (Table 1).
| Smartphone User | Self‐Report % (n/N) | Resident Observations of Other Team Members % (n/N) | Faculty Observations of Trainees % (n/N) |
|---|---|---|---|
| |||
| Resident | 57% (59/103) | 91% (103/113)* | 73% (29/40) |
| Faculty | 28% (11/39) | 43% (49/113)* | n/a |
Respondents reported that they used their smartphones during attending rounds for the following reasons: 1) patient care (85% residents, 48% faculty); 2) reading/responding to personal texts/e‐mails (37% residents, 12% faculty); and 3) other non‐patient care uses, such as Web surfing (15% residents, 0% faculty) (Tables 2 and 3). Nineteen percent of residents reported that they missed important clinical information due to distraction from smartphone use, as did 12% of attendings (Table 4). Respondents reported observing other team members using smartphones and missing important clinical data at higher rates than they reported for themselves (see Tables 1, 4, and 5). A majority of both residents (56%) and faculty (73%) agreed (score >3) that smartphones can be a serious distraction during attending rounds, and 77% of attendings affirmed that teaching hospitals should establish smartphone use codes of conduct in order to minimize unnecessary distraction during attending rounds.
| Reason | Based on Housestaff Self‐Report (n = 85)* | Based on Trainee Observations of One Another (n = 112) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 85% | 86% | NS |
| Reading or responding to personal texts or e‐mail | 37% | 55% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 15% | 37% | <0.01 |
| Reason | Based on Faculty Self‐Report (n = 25)* | Based on Housestaff Observations of Faculty (n = 91) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 48% | 48% | NS |
| Reading or responding to personal texts or e‐mail | 12% | 47% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 0% | 20% | <0.05 |
| Smartphone User | Self‐Report % (n/N) |
|---|---|
| |
| Housestaff | 19% (18/85)* |
| Faculty | 12% (3/25)* |
| Smartphone User | Based on Housestaff Observation % (n/N) | Based on Faculty Observation % (n/N) |
|---|---|---|
| ||
| Trainee | 34% (38/112)* | 43% (17/40) |
| Faculty | 20% (18/91)* | n/a |
Despite not requiring responses in order to complete the questionnaires, we found that, in general, few eligible faculty or residents skipped questions on the survey. Nevertheless, there was a substantial drop in responses (91/116) for the last 2 questions on the housestaff survey. These questions asked for resident observations of attending smartphone usage patterns during rounds, and whether they had seen attendings miss clinical information because of distractions from smartphone use.
There were 25 free‐text comments from residents and 11 from attendings. The resultant comments highlight differences in residents' and attendings' perspectives toward smartphone use during attending rounds. Housestaff comments included 7 positive comments, 7 positive/negative comments, 1 negative comment, and 10 neutral comments. A subtheme that emerged in 2 of the housestaff comments was the importance of personal autonomy in being able to use one's smartphone. Attending comments included 2 positive comments, 0 positive/negative comments, 4 negative comments, and 5 neutral comments. Faculty comments revealed that attendings use their smartphones' e‐mail/texting and call capabilities during rounds both for patient care issues (3 comments) and/or urgent family concerns (2 comments). In 2 other attending comments, the reason for calls/texts during rounds was not specified.
Housestaff comments included: I do not know why it is that attendings never use it these phones are so easy to use and [enhance] patient care in a number of ways, Depending on how they are used, if strictly for pt care then they can be a great mobile tool, Of course they can be a distraction, but they are also a very good tool. You take the good with the bad, If you are bored you will find other things to occupy your mind. If you can look up some info at the time of rounding you are actively participating. Please, do not make it worse than it is already, and It is a personal choice. Faculty negative comments highlighted the potential for distraction from the e‐mail beeps, the fact that some of the housestaff will be tuned into their SmartPhones, that residents frequently check their phones during roundsa distraction and frankly rude when the attending or fellow are giving a brief lecture, and that sometimes more focus is on the SmartPhone than rounds.
DISCUSSION
Physicians and their patients benefit from the wide‐ranging capabilities of personal, mobile communication devices in the healthcare environment. Smartphones house the latest medical references, provide access to patients' medical records and imaging studies, can photograph or video physical findings, and educate and monitor patients.28 Smartphones can facilitate information transfer in the medical setting and may improve housestaff efficiency and communication.9
Despite their significant benefits, smartphones introduce another source of interruption, multitasking, and distraction into the hospital environment. There is increasing awareness that breaks‐in‐task in the clinical setting may have negative consequences.2024 While some types of interruptions are beneficial and can facilitate patient care (eg, an alarm ringing to indicate abnormal vitals signs on a patient),2024 other forms of interruptions, even those that are self‐initiated,22 can be distracting and detrimental. Along these lines, recommendations for safe handoffs and information transfer have specifically included advice to minimize potential distractions.25
In addition, studies from the psychology and education literature have previously documented negative consequences on learning when individuals use electronic devices to multitask.1517 Students who used a laptop in class were likely to multitask, become distracted, and distract others; the more a student used the laptop in class, the lower the student's class performance.15 Multitasking with a cellphone during driving can be especially hazardous.18, 19 According to National Highway Traffic Safety Administration data, 20% of injury crashes in 2009 involved reports of distracted driving, and cellphones were implicated in 18% of distracted driving deaths that year.18
Little is known about any negative effects of using personal electronic devices in the context of patient care. A 2011 study of Internal Medicine residents who used smartphones for team communication documented both positive and negative consequences of smartphone use in the hospital setting. Negative consequences included frequent interruptions, a weakening of interprofessional behaviors as housestaff relied on texting over direct communication with nurses, and unprofessional housestaff behaviors.26 The Agency for Healthcare Quality and Research published a case report in which a resident's smartphone use during clinical care resulted in patient harm.27 To our knowledge, this is the first study to detail housestaff and faculty smartphone usage patterns and potential for user distractibility during inpatient attending rounds.
Our data show that device use during attending rounds is prevalent among residents and faculty alike, with the majority of use related to patient care. However, attendings were half as likely as residents to report using devices regularly during rounds. This finding may reflect attendings' inability to multitask while leading the rounds, or a deliberate role‐modeling of desired conduct during rounds. Generational differences may also play a role, with residents more likely than their older attendings to multitask and self‐interrupt. Along these lines, traffic safety research has found that younger drivers are more likely to text during driving; approximately 30% of drivers under 30 years old reported texting while driving in the previous 30 days, compared to 9% of respondents over 30 years old.19 Increased smartphone use by housestaff during rounds may also reflect attitudinal differences between the 2 groups. As seen in the free‐text comments, housestaff tended to emphasize the benefits of smartphone use, and with 1 exception, all negative housestaff comments were balanced by a positive statement. Faculty more commonly underscored the negative aspects of smartphone use during rounds, including the devices' adverse effects on housestaff professional behavior in this setting.
Faculty and housestaff consistently reported observing others using smartphones at higher rates than they reported for themselves. This discrepancy may reflect underrecognition of self‐use, or a discomfort in reporting self‐use during attending rounds. In addition, residents' observations of other trainees' usage of smartphones (91%) was higher than faculty observation of the same group (73%). Trainees' smartphone use may be less obvious to attendings who are involved in facilitating rounds. Alternatively, trainees may use their smartphones in subtle ways to prevent attending awareness.
There are several limitations to our study. Our research focused specifically on attending rounds. Smartphone usage patterns by faculty and housestaff at other times in the work day, such as during resident handoffs, at a patient's bedside, or during academic conferences, may differ. Nevertheless, we specifically chose to study smartphone use during attending rounds, as these sessions are discrete time frames during which important teaching occurs and clinical management decisions are made. With recent Accreditation Council for Graduate Medical Education (ACGME) work hour restrictions, these faculty‐led rounds may become increasingly important in ensuring the safe transition of patient care. Secondly, despite asking respondents how often they use their smartphones for personal texts or e‐mails, it was clear from the free‐text comments that respondents use their smartphone e‐mail/texting capabilities and take urgent calls during rounds for both patient care and/or family issues. It is not possible from the data to sort out the subset of respondents who use texting or e‐mailing exclusively for patient care during rounds. Third, we did not survey medical students on the teams, so it is possible that their device use on rounds differs from that of housestaff and faculty. Fourth, since the survey could be completed without answering every question, response rates for some items varied slightly; there was a substantial reduction in the number of eligible residents who answered the final 2 questions on the survey about their observations of attendings' smartphone usage patterns and distraction during rounds. While the flexibility in survey completion was intended to enhance overall study participation, it is unknown how nonresponders might have affected the study results; as such, those specific results should be interpreted with some caution. Finally, our findings were based on respondents' retrospective recall, and therefore may not accurately reflect true usage patterns. Timemotion studies with real‐time observation of smartphone use would provide more accurate data.
A majority of residents and attendings in our study agreed that smartphones can pose a serious distraction during attending rounds, and attendings strongly favored the institution of formal codes of conduct for smartphone use during inpatient attending rounds. The development of such policies are important for patient safety; at the same time, they are in line with medical institutions' increasing awareness about the need for guidelines regarding other aspects of digital professionalism.28 In February 2012, our hospital instituted a policy regarding appropriate device use during inpatient attending rounds (see Supporting Appendix 3 in the online version of this article). Because our research found differences in housestaff and faculty attitudes toward smartphone use during rounds, we developed our policy after discussion with, and feedback from, all members of the inpatient team, including faculty, residents, and medical students. Incorporating the various perspectives of all stakeholders can be helpful to institutions in developing guidelines that maximize the benefits of smartphone use in the learning environment, while reducing the potential for distraction and adverse outcomes.
Acknowledgements
Disclosure: Nothing to report.
- . 72 percent of US physicians use smartphones. MobiHealthNews. Available at: http://mobihealthnews.com/7505/72‐percent‐of‐us‐physicians‐use‐smartphones/. Accessed April 16, 2012.
- . Smartphones in clinical practice, medical education, and research. Arch Intern Med. 2011;171(14):1294–1296.
- ,. Telemedicine using smartphones for oral and maxillofacial surgery consultation, communication, and treatment planning.J Oral Maxillofac Surg.2009;67:2505–2509.
- . Mobile phones to improve the practice of neurology. Neurol Clin. 2010;28(2):395–410.
- , , . Infectious diseases resources for the iPhone. Clin Infect Dis. 2010;50(9):1268–1274.
- , , , . Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117:1274–1274.e3.
- , , . The uses of the iPhone for surgeons. Surgeon. 2011;9(1):44–48.
- . Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res. 2011;469(7):2042–2048.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Patient attitudes toward physician use of tablet computers in the exam room. Fam Med. 2010;42(9):643–647.
- . iPads to be distributed to incoming class by Stanford Medical School. Available at: http://med.stanford.edu/ism/2010/august/ipad.html. Accessed April 16, 2012.
- University of Virginia School of Medicine. Third year medical student mobile device requirement. Available at: http://www.medicine.virginia.edu/education/medical‐students/ome/edtech/pda_recom‐page/. Accessed April 16, 2012.
- . Tablet computers in the hospital. ACP Hospitalist 2011. Available at: http://www.acphospitalist.org/archives/2011/08/tablet. htm. Accessed April 16, 2012.
- , , . Quantifying the economic impact of communication inefficiencies in US hospitals. Available at: http://www.rhsmith.umd.edu/chids/pdfs_docs/ResearchBriefings/CHIDS‐ResearchBriefing‐Vol3Issue1b.pdf. Accessed April 16, 2012.
- . In‐class laptop use and its effects on student learning. Computers 50(3):906–914.
- , , . Distractions, distractions: does instant messaging affect college students' performance on a concurrent reading comprehension task? CyberPsychology 12(1):51–53.
- , , , . Can students really multitask? An experimental study of instant messaging while reading. Computers 54(4):927–931.
- US Department of Transportation. Statistics and facts about distracted driving. Available at: http://www.distraction.gov/stats‐and‐facts/index.html. Accessed November 17, 2011.
- Driving distracted. Consumer Reports. April 2011:22–25. See also: http://www.distraction.gov/files/for‐media/2011/2011–03‐04‐cr‐dot‐distracted‐driving‐initiative.pdf. Accessed November 25, 2011.
- , , , . Emergency department workplace interruptions: are emergency physicians “interrupt‐driven” and “multitasking”? Acad Emerg Med. 2000;7(11):1239–1243.
- , . Interruptions and multitasking in nursing care. Jt Comm J Qual Paient Saf. 2010;36(3):126–132.
- , . Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care. 2010;19(4):304–312.
- , , . How hospitalists spend their time: insights on efficiency and safety. J Hosp Med. 2006;1(2):88–93.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , , , . Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- Agency for Healthcare Research and Quality. Spotlight case. Order interrupted by text: multitasking mishap. Commentary by Halamka J. December 2011. Available at: http://www.webmm.ahrq.gov/case.aspx?caseID=257. Accessed April 16, 2012.
- , , , . Social media policies at US medical schools. Med Educ Online. 2010;15:5324. DOI: 10.3402/meo.v15i0.5324.
Healthcare market research has predicted that over 80% of physicians will use smartphones by 2012.1 These handheld devices allow users immediate access to various forms of electronic media such as Internet, instant messaging, and e‐mail. Smartphones provide numerous benefits to physicians, including rapid access to medical references, research applications, and patient information.2 These devices have been used for teleconsultation3 and patient education,4 and applications have been developed for numerous clinical specialties.48
Housestaff perceive that communication improves when they use smartphones rather than traditional pagers on the inpatient service,9 and patients may have a positive view of physicians' use of handheld computers.10 Medical schools and residency programs are increasingly requiring smartphone ownership for their trainees, with the expectation that smartphone use will enhance the educational experience, ensure the highest level of patient care, improve user efficiency, and help control the costs associated with purchasing updated textbooks.7, 1113 In the future, hospitals may rely on smartphone technologies to help reduce the enormous economic burden created by inefficient communication.14
Despite their numerous benefits for physicians and patients, little is known about the potential for smartphones to distract users in clinical care settings. Studies from the psychology and traffic safety fields have documented untoward consequences when individuals use electronic devices to multitask.1519 Given these concerns, we investigated the prevalence and patterns of smartphone use during inpatient attending rounds, and whether these devices can distract team members in this period of important information transfer.
METHODS
At our institution, attending rounds are faculty‐led inpatient teaching rounds that focus on clinical care and patient management; these sessions may be conducted either in the classroom or at the bedside, depending on patient and learner needs, and faculty preference. Inpatient teams are comprised of 1 attending, housestaff, and third and fourth year medical students. Each team conducts attending rounds independently; these rounds range in length from 1 hour (Pediatrics) to 2 hours (Medicine).
A survey instrument was designed to evaluate smartphone usage patterns during hospital inpatient attending rounds, and perceived distraction from smartphones in this setting. A preliminary version of the survey was pilot tested by a group of housestaff for face validity, redundancy, and ease of use, and it was subsequently revised. For the purposes of this study, a smartphone was defined broadly as any mobile, personal communication device (cellphone, iPhone, Android, Blackberry, iPad, etc). Residents were asked about their own smartphone use, as well as their observations of supervising attendings and other learners' devices use during rounds (see Supporting Appendix 1 in the online version of this article).
In February 2011, the anonymous online survey was administered using Survey Monkey (
Respondents were not required to answer each question in order to complete the survey. With the exception of free‐text comments, all responses were either yes/no or were graded on a 5‐point frequency scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). This scale was chosen because it allowed for adequate dispersion of responses, and for the identification of meaningful smartphone usage among respondents (score 3) and data dichotomization. The z test was used to compare the proportions between independent groups.
All free‐text comments were imported into a Microsoft Word table. Comments were separated into 2 groups: housestaff and attending. Each comment was hand‐coded by 2 authors (R.J.K.‐S. and R.S.) to reach consensus for 1 of the following 4 categories: the comment was a positive statement; a negative statement; a positive/negative statement; or a neutral one, ie, neither positive nor negative. The terms positive and negative here refer to whether the statement explicitly highlighted benefits of smartphone use or a negative aspect of smartphone use, respectively. A comment was coded as positive/negative if it highlighted both benefits and drawbacks in the same comment. In addition, each comment that mentioned texting or call functions was secondarily coded as personal, patient, both, or unknown depending on the purpose of the texting or calls described in each comment. Comments were also reviewed for possible subthemes.
RESULTS
The overall response rate was 73% (156/214), with 81% (116/143) of housestaff and 56% (40/71) of faculty participating. The mean tenure of faculty respondents was 13 years. Eighty‐nine percent (103/116) of residents and 98% (39/40) of faculty owned devices, with 57% of housestaff and 28% of attendings reporting regular personal use of smartphones during attending rounds (Table 1).
| Smartphone User | Self‐Report % (n/N) | Resident Observations of Other Team Members % (n/N) | Faculty Observations of Trainees % (n/N) |
|---|---|---|---|
| |||
| Resident | 57% (59/103) | 91% (103/113)* | 73% (29/40) |
| Faculty | 28% (11/39) | 43% (49/113)* | n/a |
Respondents reported that they used their smartphones during attending rounds for the following reasons: 1) patient care (85% residents, 48% faculty); 2) reading/responding to personal texts/e‐mails (37% residents, 12% faculty); and 3) other non‐patient care uses, such as Web surfing (15% residents, 0% faculty) (Tables 2 and 3). Nineteen percent of residents reported that they missed important clinical information due to distraction from smartphone use, as did 12% of attendings (Table 4). Respondents reported observing other team members using smartphones and missing important clinical data at higher rates than they reported for themselves (see Tables 1, 4, and 5). A majority of both residents (56%) and faculty (73%) agreed (score >3) that smartphones can be a serious distraction during attending rounds, and 77% of attendings affirmed that teaching hospitals should establish smartphone use codes of conduct in order to minimize unnecessary distraction during attending rounds.
| Reason | Based on Housestaff Self‐Report (n = 85)* | Based on Trainee Observations of One Another (n = 112) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 85% | 86% | NS |
| Reading or responding to personal texts or e‐mail | 37% | 55% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 15% | 37% | <0.01 |
| Reason | Based on Faculty Self‐Report (n = 25)* | Based on Housestaff Observations of Faculty (n = 91) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 48% | 48% | NS |
| Reading or responding to personal texts or e‐mail | 12% | 47% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 0% | 20% | <0.05 |
| Smartphone User | Self‐Report % (n/N) |
|---|---|
| |
| Housestaff | 19% (18/85)* |
| Faculty | 12% (3/25)* |
| Smartphone User | Based on Housestaff Observation % (n/N) | Based on Faculty Observation % (n/N) |
|---|---|---|
| ||
| Trainee | 34% (38/112)* | 43% (17/40) |
| Faculty | 20% (18/91)* | n/a |
Despite not requiring responses in order to complete the questionnaires, we found that, in general, few eligible faculty or residents skipped questions on the survey. Nevertheless, there was a substantial drop in responses (91/116) for the last 2 questions on the housestaff survey. These questions asked for resident observations of attending smartphone usage patterns during rounds, and whether they had seen attendings miss clinical information because of distractions from smartphone use.
There were 25 free‐text comments from residents and 11 from attendings. The resultant comments highlight differences in residents' and attendings' perspectives toward smartphone use during attending rounds. Housestaff comments included 7 positive comments, 7 positive/negative comments, 1 negative comment, and 10 neutral comments. A subtheme that emerged in 2 of the housestaff comments was the importance of personal autonomy in being able to use one's smartphone. Attending comments included 2 positive comments, 0 positive/negative comments, 4 negative comments, and 5 neutral comments. Faculty comments revealed that attendings use their smartphones' e‐mail/texting and call capabilities during rounds both for patient care issues (3 comments) and/or urgent family concerns (2 comments). In 2 other attending comments, the reason for calls/texts during rounds was not specified.
Housestaff comments included: I do not know why it is that attendings never use it these phones are so easy to use and [enhance] patient care in a number of ways, Depending on how they are used, if strictly for pt care then they can be a great mobile tool, Of course they can be a distraction, but they are also a very good tool. You take the good with the bad, If you are bored you will find other things to occupy your mind. If you can look up some info at the time of rounding you are actively participating. Please, do not make it worse than it is already, and It is a personal choice. Faculty negative comments highlighted the potential for distraction from the e‐mail beeps, the fact that some of the housestaff will be tuned into their SmartPhones, that residents frequently check their phones during roundsa distraction and frankly rude when the attending or fellow are giving a brief lecture, and that sometimes more focus is on the SmartPhone than rounds.
DISCUSSION
Physicians and their patients benefit from the wide‐ranging capabilities of personal, mobile communication devices in the healthcare environment. Smartphones house the latest medical references, provide access to patients' medical records and imaging studies, can photograph or video physical findings, and educate and monitor patients.28 Smartphones can facilitate information transfer in the medical setting and may improve housestaff efficiency and communication.9
Despite their significant benefits, smartphones introduce another source of interruption, multitasking, and distraction into the hospital environment. There is increasing awareness that breaks‐in‐task in the clinical setting may have negative consequences.2024 While some types of interruptions are beneficial and can facilitate patient care (eg, an alarm ringing to indicate abnormal vitals signs on a patient),2024 other forms of interruptions, even those that are self‐initiated,22 can be distracting and detrimental. Along these lines, recommendations for safe handoffs and information transfer have specifically included advice to minimize potential distractions.25
In addition, studies from the psychology and education literature have previously documented negative consequences on learning when individuals use electronic devices to multitask.1517 Students who used a laptop in class were likely to multitask, become distracted, and distract others; the more a student used the laptop in class, the lower the student's class performance.15 Multitasking with a cellphone during driving can be especially hazardous.18, 19 According to National Highway Traffic Safety Administration data, 20% of injury crashes in 2009 involved reports of distracted driving, and cellphones were implicated in 18% of distracted driving deaths that year.18
Little is known about any negative effects of using personal electronic devices in the context of patient care. A 2011 study of Internal Medicine residents who used smartphones for team communication documented both positive and negative consequences of smartphone use in the hospital setting. Negative consequences included frequent interruptions, a weakening of interprofessional behaviors as housestaff relied on texting over direct communication with nurses, and unprofessional housestaff behaviors.26 The Agency for Healthcare Quality and Research published a case report in which a resident's smartphone use during clinical care resulted in patient harm.27 To our knowledge, this is the first study to detail housestaff and faculty smartphone usage patterns and potential for user distractibility during inpatient attending rounds.
Our data show that device use during attending rounds is prevalent among residents and faculty alike, with the majority of use related to patient care. However, attendings were half as likely as residents to report using devices regularly during rounds. This finding may reflect attendings' inability to multitask while leading the rounds, or a deliberate role‐modeling of desired conduct during rounds. Generational differences may also play a role, with residents more likely than their older attendings to multitask and self‐interrupt. Along these lines, traffic safety research has found that younger drivers are more likely to text during driving; approximately 30% of drivers under 30 years old reported texting while driving in the previous 30 days, compared to 9% of respondents over 30 years old.19 Increased smartphone use by housestaff during rounds may also reflect attitudinal differences between the 2 groups. As seen in the free‐text comments, housestaff tended to emphasize the benefits of smartphone use, and with 1 exception, all negative housestaff comments were balanced by a positive statement. Faculty more commonly underscored the negative aspects of smartphone use during rounds, including the devices' adverse effects on housestaff professional behavior in this setting.
Faculty and housestaff consistently reported observing others using smartphones at higher rates than they reported for themselves. This discrepancy may reflect underrecognition of self‐use, or a discomfort in reporting self‐use during attending rounds. In addition, residents' observations of other trainees' usage of smartphones (91%) was higher than faculty observation of the same group (73%). Trainees' smartphone use may be less obvious to attendings who are involved in facilitating rounds. Alternatively, trainees may use their smartphones in subtle ways to prevent attending awareness.
There are several limitations to our study. Our research focused specifically on attending rounds. Smartphone usage patterns by faculty and housestaff at other times in the work day, such as during resident handoffs, at a patient's bedside, or during academic conferences, may differ. Nevertheless, we specifically chose to study smartphone use during attending rounds, as these sessions are discrete time frames during which important teaching occurs and clinical management decisions are made. With recent Accreditation Council for Graduate Medical Education (ACGME) work hour restrictions, these faculty‐led rounds may become increasingly important in ensuring the safe transition of patient care. Secondly, despite asking respondents how often they use their smartphones for personal texts or e‐mails, it was clear from the free‐text comments that respondents use their smartphone e‐mail/texting capabilities and take urgent calls during rounds for both patient care and/or family issues. It is not possible from the data to sort out the subset of respondents who use texting or e‐mailing exclusively for patient care during rounds. Third, we did not survey medical students on the teams, so it is possible that their device use on rounds differs from that of housestaff and faculty. Fourth, since the survey could be completed without answering every question, response rates for some items varied slightly; there was a substantial reduction in the number of eligible residents who answered the final 2 questions on the survey about their observations of attendings' smartphone usage patterns and distraction during rounds. While the flexibility in survey completion was intended to enhance overall study participation, it is unknown how nonresponders might have affected the study results; as such, those specific results should be interpreted with some caution. Finally, our findings were based on respondents' retrospective recall, and therefore may not accurately reflect true usage patterns. Timemotion studies with real‐time observation of smartphone use would provide more accurate data.
A majority of residents and attendings in our study agreed that smartphones can pose a serious distraction during attending rounds, and attendings strongly favored the institution of formal codes of conduct for smartphone use during inpatient attending rounds. The development of such policies are important for patient safety; at the same time, they are in line with medical institutions' increasing awareness about the need for guidelines regarding other aspects of digital professionalism.28 In February 2012, our hospital instituted a policy regarding appropriate device use during inpatient attending rounds (see Supporting Appendix 3 in the online version of this article). Because our research found differences in housestaff and faculty attitudes toward smartphone use during rounds, we developed our policy after discussion with, and feedback from, all members of the inpatient team, including faculty, residents, and medical students. Incorporating the various perspectives of all stakeholders can be helpful to institutions in developing guidelines that maximize the benefits of smartphone use in the learning environment, while reducing the potential for distraction and adverse outcomes.
Acknowledgements
Disclosure: Nothing to report.
Healthcare market research has predicted that over 80% of physicians will use smartphones by 2012.1 These handheld devices allow users immediate access to various forms of electronic media such as Internet, instant messaging, and e‐mail. Smartphones provide numerous benefits to physicians, including rapid access to medical references, research applications, and patient information.2 These devices have been used for teleconsultation3 and patient education,4 and applications have been developed for numerous clinical specialties.48
Housestaff perceive that communication improves when they use smartphones rather than traditional pagers on the inpatient service,9 and patients may have a positive view of physicians' use of handheld computers.10 Medical schools and residency programs are increasingly requiring smartphone ownership for their trainees, with the expectation that smartphone use will enhance the educational experience, ensure the highest level of patient care, improve user efficiency, and help control the costs associated with purchasing updated textbooks.7, 1113 In the future, hospitals may rely on smartphone technologies to help reduce the enormous economic burden created by inefficient communication.14
Despite their numerous benefits for physicians and patients, little is known about the potential for smartphones to distract users in clinical care settings. Studies from the psychology and traffic safety fields have documented untoward consequences when individuals use electronic devices to multitask.1519 Given these concerns, we investigated the prevalence and patterns of smartphone use during inpatient attending rounds, and whether these devices can distract team members in this period of important information transfer.
METHODS
At our institution, attending rounds are faculty‐led inpatient teaching rounds that focus on clinical care and patient management; these sessions may be conducted either in the classroom or at the bedside, depending on patient and learner needs, and faculty preference. Inpatient teams are comprised of 1 attending, housestaff, and third and fourth year medical students. Each team conducts attending rounds independently; these rounds range in length from 1 hour (Pediatrics) to 2 hours (Medicine).
A survey instrument was designed to evaluate smartphone usage patterns during hospital inpatient attending rounds, and perceived distraction from smartphones in this setting. A preliminary version of the survey was pilot tested by a group of housestaff for face validity, redundancy, and ease of use, and it was subsequently revised. For the purposes of this study, a smartphone was defined broadly as any mobile, personal communication device (cellphone, iPhone, Android, Blackberry, iPad, etc). Residents were asked about their own smartphone use, as well as their observations of supervising attendings and other learners' devices use during rounds (see Supporting Appendix 1 in the online version of this article).
In February 2011, the anonymous online survey was administered using Survey Monkey (
Respondents were not required to answer each question in order to complete the survey. With the exception of free‐text comments, all responses were either yes/no or were graded on a 5‐point frequency scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = always). This scale was chosen because it allowed for adequate dispersion of responses, and for the identification of meaningful smartphone usage among respondents (score 3) and data dichotomization. The z test was used to compare the proportions between independent groups.
All free‐text comments were imported into a Microsoft Word table. Comments were separated into 2 groups: housestaff and attending. Each comment was hand‐coded by 2 authors (R.J.K.‐S. and R.S.) to reach consensus for 1 of the following 4 categories: the comment was a positive statement; a negative statement; a positive/negative statement; or a neutral one, ie, neither positive nor negative. The terms positive and negative here refer to whether the statement explicitly highlighted benefits of smartphone use or a negative aspect of smartphone use, respectively. A comment was coded as positive/negative if it highlighted both benefits and drawbacks in the same comment. In addition, each comment that mentioned texting or call functions was secondarily coded as personal, patient, both, or unknown depending on the purpose of the texting or calls described in each comment. Comments were also reviewed for possible subthemes.
RESULTS
The overall response rate was 73% (156/214), with 81% (116/143) of housestaff and 56% (40/71) of faculty participating. The mean tenure of faculty respondents was 13 years. Eighty‐nine percent (103/116) of residents and 98% (39/40) of faculty owned devices, with 57% of housestaff and 28% of attendings reporting regular personal use of smartphones during attending rounds (Table 1).
| Smartphone User | Self‐Report % (n/N) | Resident Observations of Other Team Members % (n/N) | Faculty Observations of Trainees % (n/N) |
|---|---|---|---|
| |||
| Resident | 57% (59/103) | 91% (103/113)* | 73% (29/40) |
| Faculty | 28% (11/39) | 43% (49/113)* | n/a |
Respondents reported that they used their smartphones during attending rounds for the following reasons: 1) patient care (85% residents, 48% faculty); 2) reading/responding to personal texts/e‐mails (37% residents, 12% faculty); and 3) other non‐patient care uses, such as Web surfing (15% residents, 0% faculty) (Tables 2 and 3). Nineteen percent of residents reported that they missed important clinical information due to distraction from smartphone use, as did 12% of attendings (Table 4). Respondents reported observing other team members using smartphones and missing important clinical data at higher rates than they reported for themselves (see Tables 1, 4, and 5). A majority of both residents (56%) and faculty (73%) agreed (score >3) that smartphones can be a serious distraction during attending rounds, and 77% of attendings affirmed that teaching hospitals should establish smartphone use codes of conduct in order to minimize unnecessary distraction during attending rounds.
| Reason | Based on Housestaff Self‐Report (n = 85)* | Based on Trainee Observations of One Another (n = 112) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 85% | 86% | NS |
| Reading or responding to personal texts or e‐mail | 37% | 55% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 15% | 37% | <0.01 |
| Reason | Based on Faculty Self‐Report (n = 25)* | Based on Housestaff Observations of Faculty (n = 91) | P Value |
|---|---|---|---|
| |||
| Patient care‐related use (ePocrates, MedCalc, Medline, Google Scholar) | 48% | 48% | NS |
| Reading or responding to personal texts or e‐mail | 12% | 47% | <0.01 |
| Other non‐patient care‐related use, Web surfing | 0% | 20% | <0.05 |
| Smartphone User | Self‐Report % (n/N) |
|---|---|
| |
| Housestaff | 19% (18/85)* |
| Faculty | 12% (3/25)* |
| Smartphone User | Based on Housestaff Observation % (n/N) | Based on Faculty Observation % (n/N) |
|---|---|---|
| ||
| Trainee | 34% (38/112)* | 43% (17/40) |
| Faculty | 20% (18/91)* | n/a |
Despite not requiring responses in order to complete the questionnaires, we found that, in general, few eligible faculty or residents skipped questions on the survey. Nevertheless, there was a substantial drop in responses (91/116) for the last 2 questions on the housestaff survey. These questions asked for resident observations of attending smartphone usage patterns during rounds, and whether they had seen attendings miss clinical information because of distractions from smartphone use.
There were 25 free‐text comments from residents and 11 from attendings. The resultant comments highlight differences in residents' and attendings' perspectives toward smartphone use during attending rounds. Housestaff comments included 7 positive comments, 7 positive/negative comments, 1 negative comment, and 10 neutral comments. A subtheme that emerged in 2 of the housestaff comments was the importance of personal autonomy in being able to use one's smartphone. Attending comments included 2 positive comments, 0 positive/negative comments, 4 negative comments, and 5 neutral comments. Faculty comments revealed that attendings use their smartphones' e‐mail/texting and call capabilities during rounds both for patient care issues (3 comments) and/or urgent family concerns (2 comments). In 2 other attending comments, the reason for calls/texts during rounds was not specified.
Housestaff comments included: I do not know why it is that attendings never use it these phones are so easy to use and [enhance] patient care in a number of ways, Depending on how they are used, if strictly for pt care then they can be a great mobile tool, Of course they can be a distraction, but they are also a very good tool. You take the good with the bad, If you are bored you will find other things to occupy your mind. If you can look up some info at the time of rounding you are actively participating. Please, do not make it worse than it is already, and It is a personal choice. Faculty negative comments highlighted the potential for distraction from the e‐mail beeps, the fact that some of the housestaff will be tuned into their SmartPhones, that residents frequently check their phones during roundsa distraction and frankly rude when the attending or fellow are giving a brief lecture, and that sometimes more focus is on the SmartPhone than rounds.
DISCUSSION
Physicians and their patients benefit from the wide‐ranging capabilities of personal, mobile communication devices in the healthcare environment. Smartphones house the latest medical references, provide access to patients' medical records and imaging studies, can photograph or video physical findings, and educate and monitor patients.28 Smartphones can facilitate information transfer in the medical setting and may improve housestaff efficiency and communication.9
Despite their significant benefits, smartphones introduce another source of interruption, multitasking, and distraction into the hospital environment. There is increasing awareness that breaks‐in‐task in the clinical setting may have negative consequences.2024 While some types of interruptions are beneficial and can facilitate patient care (eg, an alarm ringing to indicate abnormal vitals signs on a patient),2024 other forms of interruptions, even those that are self‐initiated,22 can be distracting and detrimental. Along these lines, recommendations for safe handoffs and information transfer have specifically included advice to minimize potential distractions.25
In addition, studies from the psychology and education literature have previously documented negative consequences on learning when individuals use electronic devices to multitask.1517 Students who used a laptop in class were likely to multitask, become distracted, and distract others; the more a student used the laptop in class, the lower the student's class performance.15 Multitasking with a cellphone during driving can be especially hazardous.18, 19 According to National Highway Traffic Safety Administration data, 20% of injury crashes in 2009 involved reports of distracted driving, and cellphones were implicated in 18% of distracted driving deaths that year.18
Little is known about any negative effects of using personal electronic devices in the context of patient care. A 2011 study of Internal Medicine residents who used smartphones for team communication documented both positive and negative consequences of smartphone use in the hospital setting. Negative consequences included frequent interruptions, a weakening of interprofessional behaviors as housestaff relied on texting over direct communication with nurses, and unprofessional housestaff behaviors.26 The Agency for Healthcare Quality and Research published a case report in which a resident's smartphone use during clinical care resulted in patient harm.27 To our knowledge, this is the first study to detail housestaff and faculty smartphone usage patterns and potential for user distractibility during inpatient attending rounds.
Our data show that device use during attending rounds is prevalent among residents and faculty alike, with the majority of use related to patient care. However, attendings were half as likely as residents to report using devices regularly during rounds. This finding may reflect attendings' inability to multitask while leading the rounds, or a deliberate role‐modeling of desired conduct during rounds. Generational differences may also play a role, with residents more likely than their older attendings to multitask and self‐interrupt. Along these lines, traffic safety research has found that younger drivers are more likely to text during driving; approximately 30% of drivers under 30 years old reported texting while driving in the previous 30 days, compared to 9% of respondents over 30 years old.19 Increased smartphone use by housestaff during rounds may also reflect attitudinal differences between the 2 groups. As seen in the free‐text comments, housestaff tended to emphasize the benefits of smartphone use, and with 1 exception, all negative housestaff comments were balanced by a positive statement. Faculty more commonly underscored the negative aspects of smartphone use during rounds, including the devices' adverse effects on housestaff professional behavior in this setting.
Faculty and housestaff consistently reported observing others using smartphones at higher rates than they reported for themselves. This discrepancy may reflect underrecognition of self‐use, or a discomfort in reporting self‐use during attending rounds. In addition, residents' observations of other trainees' usage of smartphones (91%) was higher than faculty observation of the same group (73%). Trainees' smartphone use may be less obvious to attendings who are involved in facilitating rounds. Alternatively, trainees may use their smartphones in subtle ways to prevent attending awareness.
There are several limitations to our study. Our research focused specifically on attending rounds. Smartphone usage patterns by faculty and housestaff at other times in the work day, such as during resident handoffs, at a patient's bedside, or during academic conferences, may differ. Nevertheless, we specifically chose to study smartphone use during attending rounds, as these sessions are discrete time frames during which important teaching occurs and clinical management decisions are made. With recent Accreditation Council for Graduate Medical Education (ACGME) work hour restrictions, these faculty‐led rounds may become increasingly important in ensuring the safe transition of patient care. Secondly, despite asking respondents how often they use their smartphones for personal texts or e‐mails, it was clear from the free‐text comments that respondents use their smartphone e‐mail/texting capabilities and take urgent calls during rounds for both patient care and/or family issues. It is not possible from the data to sort out the subset of respondents who use texting or e‐mailing exclusively for patient care during rounds. Third, we did not survey medical students on the teams, so it is possible that their device use on rounds differs from that of housestaff and faculty. Fourth, since the survey could be completed without answering every question, response rates for some items varied slightly; there was a substantial reduction in the number of eligible residents who answered the final 2 questions on the survey about their observations of attendings' smartphone usage patterns and distraction during rounds. While the flexibility in survey completion was intended to enhance overall study participation, it is unknown how nonresponders might have affected the study results; as such, those specific results should be interpreted with some caution. Finally, our findings were based on respondents' retrospective recall, and therefore may not accurately reflect true usage patterns. Timemotion studies with real‐time observation of smartphone use would provide more accurate data.
A majority of residents and attendings in our study agreed that smartphones can pose a serious distraction during attending rounds, and attendings strongly favored the institution of formal codes of conduct for smartphone use during inpatient attending rounds. The development of such policies are important for patient safety; at the same time, they are in line with medical institutions' increasing awareness about the need for guidelines regarding other aspects of digital professionalism.28 In February 2012, our hospital instituted a policy regarding appropriate device use during inpatient attending rounds (see Supporting Appendix 3 in the online version of this article). Because our research found differences in housestaff and faculty attitudes toward smartphone use during rounds, we developed our policy after discussion with, and feedback from, all members of the inpatient team, including faculty, residents, and medical students. Incorporating the various perspectives of all stakeholders can be helpful to institutions in developing guidelines that maximize the benefits of smartphone use in the learning environment, while reducing the potential for distraction and adverse outcomes.
Acknowledgements
Disclosure: Nothing to report.
- . 72 percent of US physicians use smartphones. MobiHealthNews. Available at: http://mobihealthnews.com/7505/72‐percent‐of‐us‐physicians‐use‐smartphones/. Accessed April 16, 2012.
- . Smartphones in clinical practice, medical education, and research. Arch Intern Med. 2011;171(14):1294–1296.
- ,. Telemedicine using smartphones for oral and maxillofacial surgery consultation, communication, and treatment planning.J Oral Maxillofac Surg.2009;67:2505–2509.
- . Mobile phones to improve the practice of neurology. Neurol Clin. 2010;28(2):395–410.
- , , . Infectious diseases resources for the iPhone. Clin Infect Dis. 2010;50(9):1268–1274.
- , , , . Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117:1274–1274.e3.
- , , . The uses of the iPhone for surgeons. Surgeon. 2011;9(1):44–48.
- . Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res. 2011;469(7):2042–2048.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Patient attitudes toward physician use of tablet computers in the exam room. Fam Med. 2010;42(9):643–647.
- . iPads to be distributed to incoming class by Stanford Medical School. Available at: http://med.stanford.edu/ism/2010/august/ipad.html. Accessed April 16, 2012.
- University of Virginia School of Medicine. Third year medical student mobile device requirement. Available at: http://www.medicine.virginia.edu/education/medical‐students/ome/edtech/pda_recom‐page/. Accessed April 16, 2012.
- . Tablet computers in the hospital. ACP Hospitalist 2011. Available at: http://www.acphospitalist.org/archives/2011/08/tablet. htm. Accessed April 16, 2012.
- , , . Quantifying the economic impact of communication inefficiencies in US hospitals. Available at: http://www.rhsmith.umd.edu/chids/pdfs_docs/ResearchBriefings/CHIDS‐ResearchBriefing‐Vol3Issue1b.pdf. Accessed April 16, 2012.
- . In‐class laptop use and its effects on student learning. Computers 50(3):906–914.
- , , . Distractions, distractions: does instant messaging affect college students' performance on a concurrent reading comprehension task? CyberPsychology 12(1):51–53.
- , , , . Can students really multitask? An experimental study of instant messaging while reading. Computers 54(4):927–931.
- US Department of Transportation. Statistics and facts about distracted driving. Available at: http://www.distraction.gov/stats‐and‐facts/index.html. Accessed November 17, 2011.
- Driving distracted. Consumer Reports. April 2011:22–25. See also: http://www.distraction.gov/files/for‐media/2011/2011–03‐04‐cr‐dot‐distracted‐driving‐initiative.pdf. Accessed November 25, 2011.
- , , , . Emergency department workplace interruptions: are emergency physicians “interrupt‐driven” and “multitasking”? Acad Emerg Med. 2000;7(11):1239–1243.
- , . Interruptions and multitasking in nursing care. Jt Comm J Qual Paient Saf. 2010;36(3):126–132.
- , . Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care. 2010;19(4):304–312.
- , , . How hospitalists spend their time: insights on efficiency and safety. J Hosp Med. 2006;1(2):88–93.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , , , . Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- Agency for Healthcare Research and Quality. Spotlight case. Order interrupted by text: multitasking mishap. Commentary by Halamka J. December 2011. Available at: http://www.webmm.ahrq.gov/case.aspx?caseID=257. Accessed April 16, 2012.
- , , , . Social media policies at US medical schools. Med Educ Online. 2010;15:5324. DOI: 10.3402/meo.v15i0.5324.
- . 72 percent of US physicians use smartphones. MobiHealthNews. Available at: http://mobihealthnews.com/7505/72‐percent‐of‐us‐physicians‐use‐smartphones/. Accessed April 16, 2012.
- . Smartphones in clinical practice, medical education, and research. Arch Intern Med. 2011;171(14):1294–1296.
- ,. Telemedicine using smartphones for oral and maxillofacial surgery consultation, communication, and treatment planning.J Oral Maxillofac Surg.2009;67:2505–2509.
- . Mobile phones to improve the practice of neurology. Neurol Clin. 2010;28(2):395–410.
- , , . Infectious diseases resources for the iPhone. Clin Infect Dis. 2010;50(9):1268–1274.
- , , , . Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117:1274–1274.e3.
- , , . The uses of the iPhone for surgeons. Surgeon. 2011;9(1):44–48.
- . Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res. 2011;469(7):2042–2048.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Patient attitudes toward physician use of tablet computers in the exam room. Fam Med. 2010;42(9):643–647.
- . iPads to be distributed to incoming class by Stanford Medical School. Available at: http://med.stanford.edu/ism/2010/august/ipad.html. Accessed April 16, 2012.
- University of Virginia School of Medicine. Third year medical student mobile device requirement. Available at: http://www.medicine.virginia.edu/education/medical‐students/ome/edtech/pda_recom‐page/. Accessed April 16, 2012.
- . Tablet computers in the hospital. ACP Hospitalist 2011. Available at: http://www.acphospitalist.org/archives/2011/08/tablet. htm. Accessed April 16, 2012.
- , , . Quantifying the economic impact of communication inefficiencies in US hospitals. Available at: http://www.rhsmith.umd.edu/chids/pdfs_docs/ResearchBriefings/CHIDS‐ResearchBriefing‐Vol3Issue1b.pdf. Accessed April 16, 2012.
- . In‐class laptop use and its effects on student learning. Computers 50(3):906–914.
- , , . Distractions, distractions: does instant messaging affect college students' performance on a concurrent reading comprehension task? CyberPsychology 12(1):51–53.
- , , , . Can students really multitask? An experimental study of instant messaging while reading. Computers 54(4):927–931.
- US Department of Transportation. Statistics and facts about distracted driving. Available at: http://www.distraction.gov/stats‐and‐facts/index.html. Accessed November 17, 2011.
- Driving distracted. Consumer Reports. April 2011:22–25. See also: http://www.distraction.gov/files/for‐media/2011/2011–03‐04‐cr‐dot‐distracted‐driving‐initiative.pdf. Accessed November 25, 2011.
- , , , . Emergency department workplace interruptions: are emergency physicians “interrupt‐driven” and “multitasking”? Acad Emerg Med. 2000;7(11):1239–1243.
- , . Interruptions and multitasking in nursing care. Jt Comm J Qual Paient Saf. 2010;36(3):126–132.
- , . Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care. 2010;19(4):304–312.
- , , . How hospitalists spend their time: insights on efficiency and safety. J Hosp Med. 2006;1(2):88–93.
- , , , , . Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med. 2010;170(8):683–690.
- , , , . Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- Agency for Healthcare Research and Quality. Spotlight case. Order interrupted by text: multitasking mishap. Commentary by Halamka J. December 2011. Available at: http://www.webmm.ahrq.gov/case.aspx?caseID=257. Accessed April 16, 2012.
- , , , . Social media policies at US medical schools. Med Educ Online. 2010;15:5324. DOI: 10.3402/meo.v15i0.5324.
Copyright © 2012 Society of Hospital Medicine