User login
Richard Quinn is an award-winning journalist with 15 years’ experience. He has worked at the Asbury Park Press in New Jersey and The Virginian-Pilot in Norfolk, Va., and currently is managing editor for a leading commercial real estate publication. His freelance work has appeared in The Jewish State, The Hospitalist, The Rheumatologist, ACEP Now, and ENT Today. He lives in New Jersey with his wife and three cats.
ONLINE EXCLUSIVE: Listen to former Obama healthcare advisor Bob Kocher, MD
Click here to listen to Dr. Kocher
Click here to listen to Dr. Kocher
Click here to listen to Dr. Kocher
HM11 PREVIEW: Teacher As Student
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The position of visiting professor is a bit amorphous at the SHM annual meeting. The honoree presides over the best of the Research, Innovations, and Clinical Vignettes (RIV) presentations and leads rounds of the RIV poster sessions. They can serve as an informal mentor to early-career physicians and be a sounding board for seasoned practitioners.
This year, the visiting professor will be as much a student as a teacher.
“I always think when I go to educate others … the best way of doing that is to have a bidirectional kind of interchange,” says Malcolm Cox, MD, chief academic affiliations officer for the U.S. Department of Veterans Affairs in Washington, D.C., and an adjunct professor of medicine at the University of Pennsylvania in Philadelphia. “I inevitably learn more from my ‘students’ than I think I ever provide to my students, in any teaching opportunity. That’s just a philosophy I’ve had for 40 years.”
Dr. Cox, a kidney specialist and career academician, was invited to be the visiting professor by SHM President Jeff Wiese, MD, FACP, SFHM. Dr. Cox views his role as that of an “interrogative fly on the wall,” and he hopes to stimulate discussions about HM’s role in the broader medical landscape.
“How hospitalists can work with their other colleagues to enhance continuity,” he says, “and, in particular, within that more narrow frame, an even more narrow frame is how they would relate to and work with primary-care folks in the aftercare environment to enhance continuity of care.” HM11
Richard Quinn is a freelance writer based in New Jersey.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The position of visiting professor is a bit amorphous at the SHM annual meeting. The honoree presides over the best of the Research, Innovations, and Clinical Vignettes (RIV) presentations and leads rounds of the RIV poster sessions. They can serve as an informal mentor to early-career physicians and be a sounding board for seasoned practitioners.
This year, the visiting professor will be as much a student as a teacher.
“I always think when I go to educate others … the best way of doing that is to have a bidirectional kind of interchange,” says Malcolm Cox, MD, chief academic affiliations officer for the U.S. Department of Veterans Affairs in Washington, D.C., and an adjunct professor of medicine at the University of Pennsylvania in Philadelphia. “I inevitably learn more from my ‘students’ than I think I ever provide to my students, in any teaching opportunity. That’s just a philosophy I’ve had for 40 years.”
Dr. Cox, a kidney specialist and career academician, was invited to be the visiting professor by SHM President Jeff Wiese, MD, FACP, SFHM. Dr. Cox views his role as that of an “interrogative fly on the wall,” and he hopes to stimulate discussions about HM’s role in the broader medical landscape.
“How hospitalists can work with their other colleagues to enhance continuity,” he says, “and, in particular, within that more narrow frame, an even more narrow frame is how they would relate to and work with primary-care folks in the aftercare environment to enhance continuity of care.” HM11
Richard Quinn is a freelance writer based in New Jersey.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The position of visiting professor is a bit amorphous at the SHM annual meeting. The honoree presides over the best of the Research, Innovations, and Clinical Vignettes (RIV) presentations and leads rounds of the RIV poster sessions. They can serve as an informal mentor to early-career physicians and be a sounding board for seasoned practitioners.
This year, the visiting professor will be as much a student as a teacher.
“I always think when I go to educate others … the best way of doing that is to have a bidirectional kind of interchange,” says Malcolm Cox, MD, chief academic affiliations officer for the U.S. Department of Veterans Affairs in Washington, D.C., and an adjunct professor of medicine at the University of Pennsylvania in Philadelphia. “I inevitably learn more from my ‘students’ than I think I ever provide to my students, in any teaching opportunity. That’s just a philosophy I’ve had for 40 years.”
Dr. Cox, a kidney specialist and career academician, was invited to be the visiting professor by SHM President Jeff Wiese, MD, FACP, SFHM. Dr. Cox views his role as that of an “interrogative fly on the wall,” and he hopes to stimulate discussions about HM’s role in the broader medical landscape.
“How hospitalists can work with their other colleagues to enhance continuity,” he says, “and, in particular, within that more narrow frame, an even more narrow frame is how they would relate to and work with primary-care folks in the aftercare environment to enhance continuity of care.” HM11
Richard Quinn is a freelance writer based in New Jersey.
HM11 PREVIEW: Different Strokes
Ron Greeno, MD, SFHM, chief medical officer for Brentwood, Tenn.-based Cogent Healthcare, will arrive at HM11 and embark on a whirlwind of meet-and-greets, dinners, drinks, and introductions. At the same time, first-year attendee Amaka Nweke, assistant site director for Hospitalists Management Group at Kenosha Medical Center in Wisconsin, will focus on sessions that will help her learn the management skills she can use to further her career.
To be sure, Dr. Greeno will attend a few classes to brush up on specific topics. And Dr. Nweke will ask for business cards as she builds a professional network. But each has to pick a strategy to navigate the four-day annual meeting in Grapevine, Texas.
“You can’t do everything,” says Daniel Dressler, MD, MSc, SFHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta, SHM board member, and HM11’s course director. “You have to plan and ask, ‘What do I want to get out of this meeting this year?’ ”
The Hospitalist talked to more than a half-dozen providers in various HM roles to determine just what they expect out of their annual meeting. The physicians fall into broad categories that capture most of the roughly 2,500 attendees at the annual meeting: first-timer, veteran, academic, rural hospitalist, up-and-comer, socialite. And while each says plenary sessions and keynote addresses are must-sees, the tack they take for the rest of the week is custom-made.
The First-Timer
Dr. Nweke, who finished her residency in 2009, wasn’t sure how to map out her meeting schedule until she decided to attend two medical conferences this year. She plans to get her clinical refreshers at the annual meeting of the American College of Physicians (ACP), and use SHM’s affair to teach her the managerial and administrative skills she needs to eventually become an HM group leader. Her particular focuses include process improvement and length-of-stay (LOS) reduction methods.
“Originally, when I wasn’t sure what I wanted to get out of SHM, it was very daunting,” she says. “For meetings like this, you have to figure out what you want out of the course. Once you figure that out, it makes it easy to register for a course. If you don’t know and you’re just going, it’s definitely extremely daunting.”
The Veteran
Jeffrey Dichter, MD, FACP, SFHM, medical director for the cardiovascular ICU at Regions Hospital in St. Paul, Minn., only missed two of the first 14 annual meetings. He picks a topic area each year that he wants to focus on, then tailors his schedule to that idea. This year, it’s quality improvement. An academician at heart, he also attends the abstract poster sessions to get “a real flavor for the researchers and what people are thinking about for HM.”
“You’re not going to get to everything every year,” he says knowingly. “You just try to mix and match. Early on, you could see everything. Since it’s grown, you realize you can’t see everything. You learn to adapt.”
The Academic
Danielle Scheurer, MD, MSc, SFHM, medical director of quality and safety at the Medical University of South Carolina in Charleston, uses the meeting as a sounding board to solve problems. Community HM groups don’t have the sort of turnover issues that academic medical centers do, so meeting with like-minded colleagues provides the chance to find the “little pearls from any medical center that you can take back.”
“Since I do a lot of quality improvement, I just like the opportunity to see how other people are doing things that we are struggling with,” says Dr. Scheurer, SHM’s physician advisor. “It amazes me the ubiquity of how we all struggle around the same types of things.”
The Rural Hospitalist
Martin Johns, MD, a hospitalist at Gifford Medical Center in Randolph, Vt., (pop. 4,853) could use an entire focused track on rural medicine. In particular, rural hospitalists often perform multiple roles—administrative or clinical—and best-practice recommendations would be valuable. Networking has its place at the meeting, but given that many rural physicians have long tenures, the real goal is bring useful information back to the group. “What is good about the SHM [meeting] is you are exposed to know what’s happening regionally,” Dr. Johns says. “You get a flavor for the national tenor. That’s important, because in a small place, you only have a certain allotment for CME funds.”
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The Up-and-Comer
Christina Payne, MD, an academic hospitalist at Emory University Hospital in Atlanta who finished her residency in June, sees herself as a potential future leader in the field. She presented a poster at last year’s meeting and works on a SHM committee for early-career hospitalists.
A quality-minded academician, Dr. Payne plans to take advantage of meeting the leading minds in HM and use them as mentors to help her help the field.
“It’s learning to walk the walk and talk the talk,” she says. “I’m still new at that, but I’m ready to put myself out there. … My excitement for hospital medicine puts me in an ideal spot. In 20 years, hopefully, we’ll be the ones for other people to come to for mentorship.”
The Socialite
Dr. Dressler refers to Dr. Greeno, a cofounder of Cogent, as the “ultimate socialite.” Dr. Greeno is often a panelist at the annual meeting and spends much of his time catching up with colleagues around the country he does not often see in person. He makes sure to catch three or four handpicked sessions but typically looks most forward to being approached by younger physicians as he sees the young field of HM take hold with a new generation.
“The entire time I’m there, I’m talking to someone, whether it’s planned or I run into someone,” he says. “It’s the one time I usually end up having dinner and end up having drinks with folks and talking with people well into the night. It really does give you a chance to recharge your battery and get excited about what we’re doing again.” HM11
Richard Quinn is a freelance writer based in New Jersey.
Ron Greeno, MD, SFHM, chief medical officer for Brentwood, Tenn.-based Cogent Healthcare, will arrive at HM11 and embark on a whirlwind of meet-and-greets, dinners, drinks, and introductions. At the same time, first-year attendee Amaka Nweke, assistant site director for Hospitalists Management Group at Kenosha Medical Center in Wisconsin, will focus on sessions that will help her learn the management skills she can use to further her career.
To be sure, Dr. Greeno will attend a few classes to brush up on specific topics. And Dr. Nweke will ask for business cards as she builds a professional network. But each has to pick a strategy to navigate the four-day annual meeting in Grapevine, Texas.
“You can’t do everything,” says Daniel Dressler, MD, MSc, SFHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta, SHM board member, and HM11’s course director. “You have to plan and ask, ‘What do I want to get out of this meeting this year?’ ”
The Hospitalist talked to more than a half-dozen providers in various HM roles to determine just what they expect out of their annual meeting. The physicians fall into broad categories that capture most of the roughly 2,500 attendees at the annual meeting: first-timer, veteran, academic, rural hospitalist, up-and-comer, socialite. And while each says plenary sessions and keynote addresses are must-sees, the tack they take for the rest of the week is custom-made.
The First-Timer
Dr. Nweke, who finished her residency in 2009, wasn’t sure how to map out her meeting schedule until she decided to attend two medical conferences this year. She plans to get her clinical refreshers at the annual meeting of the American College of Physicians (ACP), and use SHM’s affair to teach her the managerial and administrative skills she needs to eventually become an HM group leader. Her particular focuses include process improvement and length-of-stay (LOS) reduction methods.
“Originally, when I wasn’t sure what I wanted to get out of SHM, it was very daunting,” she says. “For meetings like this, you have to figure out what you want out of the course. Once you figure that out, it makes it easy to register for a course. If you don’t know and you’re just going, it’s definitely extremely daunting.”
The Veteran
Jeffrey Dichter, MD, FACP, SFHM, medical director for the cardiovascular ICU at Regions Hospital in St. Paul, Minn., only missed two of the first 14 annual meetings. He picks a topic area each year that he wants to focus on, then tailors his schedule to that idea. This year, it’s quality improvement. An academician at heart, he also attends the abstract poster sessions to get “a real flavor for the researchers and what people are thinking about for HM.”
“You’re not going to get to everything every year,” he says knowingly. “You just try to mix and match. Early on, you could see everything. Since it’s grown, you realize you can’t see everything. You learn to adapt.”
The Academic
Danielle Scheurer, MD, MSc, SFHM, medical director of quality and safety at the Medical University of South Carolina in Charleston, uses the meeting as a sounding board to solve problems. Community HM groups don’t have the sort of turnover issues that academic medical centers do, so meeting with like-minded colleagues provides the chance to find the “little pearls from any medical center that you can take back.”
“Since I do a lot of quality improvement, I just like the opportunity to see how other people are doing things that we are struggling with,” says Dr. Scheurer, SHM’s physician advisor. “It amazes me the ubiquity of how we all struggle around the same types of things.”
The Rural Hospitalist
Martin Johns, MD, a hospitalist at Gifford Medical Center in Randolph, Vt., (pop. 4,853) could use an entire focused track on rural medicine. In particular, rural hospitalists often perform multiple roles—administrative or clinical—and best-practice recommendations would be valuable. Networking has its place at the meeting, but given that many rural physicians have long tenures, the real goal is bring useful information back to the group. “What is good about the SHM [meeting] is you are exposed to know what’s happening regionally,” Dr. Johns says. “You get a flavor for the national tenor. That’s important, because in a small place, you only have a certain allotment for CME funds.”
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The Up-and-Comer
Christina Payne, MD, an academic hospitalist at Emory University Hospital in Atlanta who finished her residency in June, sees herself as a potential future leader in the field. She presented a poster at last year’s meeting and works on a SHM committee for early-career hospitalists.
A quality-minded academician, Dr. Payne plans to take advantage of meeting the leading minds in HM and use them as mentors to help her help the field.
“It’s learning to walk the walk and talk the talk,” she says. “I’m still new at that, but I’m ready to put myself out there. … My excitement for hospital medicine puts me in an ideal spot. In 20 years, hopefully, we’ll be the ones for other people to come to for mentorship.”
The Socialite
Dr. Dressler refers to Dr. Greeno, a cofounder of Cogent, as the “ultimate socialite.” Dr. Greeno is often a panelist at the annual meeting and spends much of his time catching up with colleagues around the country he does not often see in person. He makes sure to catch three or four handpicked sessions but typically looks most forward to being approached by younger physicians as he sees the young field of HM take hold with a new generation.
“The entire time I’m there, I’m talking to someone, whether it’s planned or I run into someone,” he says. “It’s the one time I usually end up having dinner and end up having drinks with folks and talking with people well into the night. It really does give you a chance to recharge your battery and get excited about what we’re doing again.” HM11
Richard Quinn is a freelance writer based in New Jersey.
Ron Greeno, MD, SFHM, chief medical officer for Brentwood, Tenn.-based Cogent Healthcare, will arrive at HM11 and embark on a whirlwind of meet-and-greets, dinners, drinks, and introductions. At the same time, first-year attendee Amaka Nweke, assistant site director for Hospitalists Management Group at Kenosha Medical Center in Wisconsin, will focus on sessions that will help her learn the management skills she can use to further her career.
To be sure, Dr. Greeno will attend a few classes to brush up on specific topics. And Dr. Nweke will ask for business cards as she builds a professional network. But each has to pick a strategy to navigate the four-day annual meeting in Grapevine, Texas.
“You can’t do everything,” says Daniel Dressler, MD, MSc, SFHM, associate professor and director of internal-medicine teaching services at Emory University Hospital in Atlanta, SHM board member, and HM11’s course director. “You have to plan and ask, ‘What do I want to get out of this meeting this year?’ ”
The Hospitalist talked to more than a half-dozen providers in various HM roles to determine just what they expect out of their annual meeting. The physicians fall into broad categories that capture most of the roughly 2,500 attendees at the annual meeting: first-timer, veteran, academic, rural hospitalist, up-and-comer, socialite. And while each says plenary sessions and keynote addresses are must-sees, the tack they take for the rest of the week is custom-made.
The First-Timer
Dr. Nweke, who finished her residency in 2009, wasn’t sure how to map out her meeting schedule until she decided to attend two medical conferences this year. She plans to get her clinical refreshers at the annual meeting of the American College of Physicians (ACP), and use SHM’s affair to teach her the managerial and administrative skills she needs to eventually become an HM group leader. Her particular focuses include process improvement and length-of-stay (LOS) reduction methods.
“Originally, when I wasn’t sure what I wanted to get out of SHM, it was very daunting,” she says. “For meetings like this, you have to figure out what you want out of the course. Once you figure that out, it makes it easy to register for a course. If you don’t know and you’re just going, it’s definitely extremely daunting.”
The Veteran
Jeffrey Dichter, MD, FACP, SFHM, medical director for the cardiovascular ICU at Regions Hospital in St. Paul, Minn., only missed two of the first 14 annual meetings. He picks a topic area each year that he wants to focus on, then tailors his schedule to that idea. This year, it’s quality improvement. An academician at heart, he also attends the abstract poster sessions to get “a real flavor for the researchers and what people are thinking about for HM.”
“You’re not going to get to everything every year,” he says knowingly. “You just try to mix and match. Early on, you could see everything. Since it’s grown, you realize you can’t see everything. You learn to adapt.”
The Academic
Danielle Scheurer, MD, MSc, SFHM, medical director of quality and safety at the Medical University of South Carolina in Charleston, uses the meeting as a sounding board to solve problems. Community HM groups don’t have the sort of turnover issues that academic medical centers do, so meeting with like-minded colleagues provides the chance to find the “little pearls from any medical center that you can take back.”
“Since I do a lot of quality improvement, I just like the opportunity to see how other people are doing things that we are struggling with,” says Dr. Scheurer, SHM’s physician advisor. “It amazes me the ubiquity of how we all struggle around the same types of things.”
The Rural Hospitalist
Martin Johns, MD, a hospitalist at Gifford Medical Center in Randolph, Vt., (pop. 4,853) could use an entire focused track on rural medicine. In particular, rural hospitalists often perform multiple roles—administrative or clinical—and best-practice recommendations would be valuable. Networking has its place at the meeting, but given that many rural physicians have long tenures, the real goal is bring useful information back to the group. “What is good about the SHM [meeting] is you are exposed to know what’s happening regionally,” Dr. Johns says. “You get a flavor for the national tenor. That’s important, because in a small place, you only have a certain allotment for CME funds.”
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
The Up-and-Comer
Christina Payne, MD, an academic hospitalist at Emory University Hospital in Atlanta who finished her residency in June, sees herself as a potential future leader in the field. She presented a poster at last year’s meeting and works on a SHM committee for early-career hospitalists.
A quality-minded academician, Dr. Payne plans to take advantage of meeting the leading minds in HM and use them as mentors to help her help the field.
“It’s learning to walk the walk and talk the talk,” she says. “I’m still new at that, but I’m ready to put myself out there. … My excitement for hospital medicine puts me in an ideal spot. In 20 years, hopefully, we’ll be the ones for other people to come to for mentorship.”
The Socialite
Dr. Dressler refers to Dr. Greeno, a cofounder of Cogent, as the “ultimate socialite.” Dr. Greeno is often a panelist at the annual meeting and spends much of his time catching up with colleagues around the country he does not often see in person. He makes sure to catch three or four handpicked sessions but typically looks most forward to being approached by younger physicians as he sees the young field of HM take hold with a new generation.
“The entire time I’m there, I’m talking to someone, whether it’s planned or I run into someone,” he says. “It’s the one time I usually end up having dinner and end up having drinks with folks and talking with people well into the night. It really does give you a chance to recharge your battery and get excited about what we’re doing again.” HM11
Richard Quinn is a freelance writer based in New Jersey.
HM11 PREVIEW: Lots to See, Lots to Do in ‘Big D’
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
A billion-dollar football stadium that offers on-field tours. A real-life cattle ride. A chance to honor the country’s last assassinated president. And don’t overlook the museums, art galleries, and restaurants.
Hospitalists from across the country will have the opportunity to experience all of it during HM11 at the Gaylord Texan Hotel & Convention Center in Grapevine, Texas, situated between Dallas and Fort Worth.
“I think it’s a nice blend of both sides,” says Ben Lee, MD, a hospitalist at Children’s Medical Center of Dallas and assistant professor of pediatrics at University of Texas Southwestern. “You can get the modern amenities, but you also have a capturing of, ‘Hey, this is stuff that’s occurred in the past that’s still available.’ ”
For the sports-minded, Dallas is a veritable Mecca. Cowboys Stadium, which hosted Super Bowl XV in February, offers VIP and self-guided tours. For more information, call 800-745-3000. The Texas Rangers baseball team will be playing at home in Arlington the week of HM11, while NBA fans might be able to catch a Dallas Mavericks playoff game. The same could be true of the NHL’s Dallas Stars.
The art-minded and culturists should not fret, though. Dallas offers both the eponymous Dallas Museum of Art and the outdoor Nasher Sculpture Center. Meanwhile, Fort Worth offers the Modern Art Museum of Forth Worth and a half-dozen other arts institutions in its downtown cultural district.
History buffs can try the Fort Worth Stockyards National Historic District, a nod to Texas’ frontier history that includes twice-daily cattle drives, or the Sixth Floor Museum at Dealey Plaza to learn about the assassination of President Kennedy.
When you’re hungry, steak and Tex-Mex are the specialties. If you aren’t able to leave the Gaylord, try the Old Hickory Steakhouse (just make sure to reserve a table early). Away from the hotel, look for local Tex-Mex chains like Uncle Julio’s or Gloria’s.
One last tip, if we may. “I would definitely rent a car,” Dr. Lee says. “Texas is wide open.” HM11
Richard Quinn is a freelance writer based in New Jersey.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
A billion-dollar football stadium that offers on-field tours. A real-life cattle ride. A chance to honor the country’s last assassinated president. And don’t overlook the museums, art galleries, and restaurants.
Hospitalists from across the country will have the opportunity to experience all of it during HM11 at the Gaylord Texan Hotel & Convention Center in Grapevine, Texas, situated between Dallas and Fort Worth.
“I think it’s a nice blend of both sides,” says Ben Lee, MD, a hospitalist at Children’s Medical Center of Dallas and assistant professor of pediatrics at University of Texas Southwestern. “You can get the modern amenities, but you also have a capturing of, ‘Hey, this is stuff that’s occurred in the past that’s still available.’ ”
For the sports-minded, Dallas is a veritable Mecca. Cowboys Stadium, which hosted Super Bowl XV in February, offers VIP and self-guided tours. For more information, call 800-745-3000. The Texas Rangers baseball team will be playing at home in Arlington the week of HM11, while NBA fans might be able to catch a Dallas Mavericks playoff game. The same could be true of the NHL’s Dallas Stars.
The art-minded and culturists should not fret, though. Dallas offers both the eponymous Dallas Museum of Art and the outdoor Nasher Sculpture Center. Meanwhile, Fort Worth offers the Modern Art Museum of Forth Worth and a half-dozen other arts institutions in its downtown cultural district.
History buffs can try the Fort Worth Stockyards National Historic District, a nod to Texas’ frontier history that includes twice-daily cattle drives, or the Sixth Floor Museum at Dealey Plaza to learn about the assassination of President Kennedy.
When you’re hungry, steak and Tex-Mex are the specialties. If you aren’t able to leave the Gaylord, try the Old Hickory Steakhouse (just make sure to reserve a table early). Away from the hotel, look for local Tex-Mex chains like Uncle Julio’s or Gloria’s.
One last tip, if we may. “I would definitely rent a car,” Dr. Lee says. “Texas is wide open.” HM11
Richard Quinn is a freelance writer based in New Jersey.
More HM11 Preview
Former Obama advisor will speak to hospitalists about health reform
HM11’s visiting professor to serve as mentor, stimulate discussion
Hospitalists come from all walks; HM11 has a place for all of them
HM11 attendees can earn as many as 18.75 CME credits
Industry pioneer recounts HM’s meteoric rise, sees bright future for hospitalists
Lots to See, Lots to Do in ‘Big D’
From sports to culture to Tex-Mex, Dallas metroplex has something for every visitor
You may also
HM11 PREVIEW SUPPLEMENT
in pdf format.
A billion-dollar football stadium that offers on-field tours. A real-life cattle ride. A chance to honor the country’s last assassinated president. And don’t overlook the museums, art galleries, and restaurants.
Hospitalists from across the country will have the opportunity to experience all of it during HM11 at the Gaylord Texan Hotel & Convention Center in Grapevine, Texas, situated between Dallas and Fort Worth.
“I think it’s a nice blend of both sides,” says Ben Lee, MD, a hospitalist at Children’s Medical Center of Dallas and assistant professor of pediatrics at University of Texas Southwestern. “You can get the modern amenities, but you also have a capturing of, ‘Hey, this is stuff that’s occurred in the past that’s still available.’ ”
For the sports-minded, Dallas is a veritable Mecca. Cowboys Stadium, which hosted Super Bowl XV in February, offers VIP and self-guided tours. For more information, call 800-745-3000. The Texas Rangers baseball team will be playing at home in Arlington the week of HM11, while NBA fans might be able to catch a Dallas Mavericks playoff game. The same could be true of the NHL’s Dallas Stars.
The art-minded and culturists should not fret, though. Dallas offers both the eponymous Dallas Museum of Art and the outdoor Nasher Sculpture Center. Meanwhile, Fort Worth offers the Modern Art Museum of Forth Worth and a half-dozen other arts institutions in its downtown cultural district.
History buffs can try the Fort Worth Stockyards National Historic District, a nod to Texas’ frontier history that includes twice-daily cattle drives, or the Sixth Floor Museum at Dealey Plaza to learn about the assassination of President Kennedy.
When you’re hungry, steak and Tex-Mex are the specialties. If you aren’t able to leave the Gaylord, try the Old Hickory Steakhouse (just make sure to reserve a table early). Away from the hotel, look for local Tex-Mex chains like Uncle Julio’s or Gloria’s.
One last tip, if we may. “I would definitely rent a car,” Dr. Lee says. “Texas is wide open.” HM11
Richard Quinn is a freelance writer based in New Jersey.
SHM Honors Four Hospitalists
SHM will induct its second class of Masters in Hospital Medicine (MHM) at HM11 in May, and while each of the four honorees says the title is a personal honor, they all emphasize that it is a professional point of pride to see just how far HM has come in the past 15 years.
"For the specialty, it brings identity and awareness of all that we do," Erin Stucky, MD, MHM, a pediatric hospitalist at Rady Children's Hospital in San Diego, wrote in an email. "We are QI in mortal form, acting and pressing on to deliver excellence in healthcare within our systems. Each of us, members of the society, those with FHM, SFHM, and MHM—we each deliver on this promise every day."
The other MHMs, each of whom spoke to The Hospitalist via email, are:
Ron Greeno, MD, MHM, chief medical officer for Cogent Healthcare and a member of SHM's Public Policy Committee. "I've had the privilege of working in hospital medicine for 18 years and, along with my colleagues at Cogent, have helped shape the field," Dr. Greeno says. "To be one of a handful of hospitalists to be named a Master in Hospital Medicine is truly exciting, but equally exciting is to see the growing leadership capabilities of a number of our younger colleagues who will become the future leaders of our specialty."
Russell L. Holman, MD, MHM, Cogent's COO and past president of SHM. "Our specialty is constantly evolving; there is no paved road before us," Dr. Holman says. "We are cutting the path, and are part of an historical transformation of the way care is provided in this country. Twenty years from now we will reflect on an enduring legacy of dramatically improving the quality, safety, and sustainability of care for hospitalized patients. The privilege of being part of this movement is rewarding and inspirational for me."
Mary Jo Gorman, MD, MBA, MHM, former SHM president and CEO of St. Louis-based Advanced ICU Care. "It is a terrific honor to be recognized by SHM in this way," Dr. Gorman says. "The group that is included has accomplished many things and it's gratifying to be recognized with them. It’s hard to believe that SHM has come so far that we have fellows and masters in the society! Those early days seem a long way away!"
SHM has now recognized seven MHMs. Last year's class consisted of Winthrop F. Whitcomb, MD, MHM, Robert Wachter, MD, MHM, and John Nelson, MD, MHM. Each is recognized for what SHM says is the "utmost demonstration of dedication to the field of hospital medicine through significant contributions to the development and maturation of the profession."
SHM will induct its second class of Masters in Hospital Medicine (MHM) at HM11 in May, and while each of the four honorees says the title is a personal honor, they all emphasize that it is a professional point of pride to see just how far HM has come in the past 15 years.
"For the specialty, it brings identity and awareness of all that we do," Erin Stucky, MD, MHM, a pediatric hospitalist at Rady Children's Hospital in San Diego, wrote in an email. "We are QI in mortal form, acting and pressing on to deliver excellence in healthcare within our systems. Each of us, members of the society, those with FHM, SFHM, and MHM—we each deliver on this promise every day."
The other MHMs, each of whom spoke to The Hospitalist via email, are:
Ron Greeno, MD, MHM, chief medical officer for Cogent Healthcare and a member of SHM's Public Policy Committee. "I've had the privilege of working in hospital medicine for 18 years and, along with my colleagues at Cogent, have helped shape the field," Dr. Greeno says. "To be one of a handful of hospitalists to be named a Master in Hospital Medicine is truly exciting, but equally exciting is to see the growing leadership capabilities of a number of our younger colleagues who will become the future leaders of our specialty."
Russell L. Holman, MD, MHM, Cogent's COO and past president of SHM. "Our specialty is constantly evolving; there is no paved road before us," Dr. Holman says. "We are cutting the path, and are part of an historical transformation of the way care is provided in this country. Twenty years from now we will reflect on an enduring legacy of dramatically improving the quality, safety, and sustainability of care for hospitalized patients. The privilege of being part of this movement is rewarding and inspirational for me."
Mary Jo Gorman, MD, MBA, MHM, former SHM president and CEO of St. Louis-based Advanced ICU Care. "It is a terrific honor to be recognized by SHM in this way," Dr. Gorman says. "The group that is included has accomplished many things and it's gratifying to be recognized with them. It’s hard to believe that SHM has come so far that we have fellows and masters in the society! Those early days seem a long way away!"
SHM has now recognized seven MHMs. Last year's class consisted of Winthrop F. Whitcomb, MD, MHM, Robert Wachter, MD, MHM, and John Nelson, MD, MHM. Each is recognized for what SHM says is the "utmost demonstration of dedication to the field of hospital medicine through significant contributions to the development and maturation of the profession."
SHM will induct its second class of Masters in Hospital Medicine (MHM) at HM11 in May, and while each of the four honorees says the title is a personal honor, they all emphasize that it is a professional point of pride to see just how far HM has come in the past 15 years.
"For the specialty, it brings identity and awareness of all that we do," Erin Stucky, MD, MHM, a pediatric hospitalist at Rady Children's Hospital in San Diego, wrote in an email. "We are QI in mortal form, acting and pressing on to deliver excellence in healthcare within our systems. Each of us, members of the society, those with FHM, SFHM, and MHM—we each deliver on this promise every day."
The other MHMs, each of whom spoke to The Hospitalist via email, are:
Ron Greeno, MD, MHM, chief medical officer for Cogent Healthcare and a member of SHM's Public Policy Committee. "I've had the privilege of working in hospital medicine for 18 years and, along with my colleagues at Cogent, have helped shape the field," Dr. Greeno says. "To be one of a handful of hospitalists to be named a Master in Hospital Medicine is truly exciting, but equally exciting is to see the growing leadership capabilities of a number of our younger colleagues who will become the future leaders of our specialty."
Russell L. Holman, MD, MHM, Cogent's COO and past president of SHM. "Our specialty is constantly evolving; there is no paved road before us," Dr. Holman says. "We are cutting the path, and are part of an historical transformation of the way care is provided in this country. Twenty years from now we will reflect on an enduring legacy of dramatically improving the quality, safety, and sustainability of care for hospitalized patients. The privilege of being part of this movement is rewarding and inspirational for me."
Mary Jo Gorman, MD, MBA, MHM, former SHM president and CEO of St. Louis-based Advanced ICU Care. "It is a terrific honor to be recognized by SHM in this way," Dr. Gorman says. "The group that is included has accomplished many things and it's gratifying to be recognized with them. It’s hard to believe that SHM has come so far that we have fellows and masters in the society! Those early days seem a long way away!"
SHM has now recognized seven MHMs. Last year's class consisted of Winthrop F. Whitcomb, MD, MHM, Robert Wachter, MD, MHM, and John Nelson, MD, MHM. Each is recognized for what SHM says is the "utmost demonstration of dedication to the field of hospital medicine through significant contributions to the development and maturation of the profession."
Touchscreen Medicine
Mobile technology, such as tablet computers, Internet-enabled smartphones, and the applications both devices use, will change the face of HM and other physician specialties, one medical software executive says.
"Mobile technology will improve efficiency and reduce costs," Mark Cain, chief technology officer of MIM Software Inc., writes in an e-mail to The Hospitalist. "Compare the cost of an iPad to that of an exam room PC. If I was making the decision, I'd find a way to remove every exam room PC [with their keyboards, CPUs, mice, monitors, and network cables] and instead supply iPads to be carried by the staff. With a good Wi-Fi network and iPads, every room is digitally equipped as soon as the doctor walks in."
Cain has seen the paradigm shift of touchscreen technology firsthand: The FDA recently approved an application from Cleveland-based MIM to let doctors make medical diagnoses based on computed tomography (CT) and magnetic resonance imaging (MRI) via an application available for the iPhone and iPad. The application, the first with the FDA's imprimatur for diagnostic radiology, allows hospitalists and other physicians to access data via a secure network transfer.
The app for that is just the latest sign that the growing prevalence of touchscreen technology is changing the face of HM.
The evolution has its pitfalls, though. Patient privacy, wireless security, and the hesitancy of physicians to adopt change will likely slow the adoption of technology, but "the integration of interactive devices into a physician's daily workflow could become as commonplace in 10 years as the presence of hospitalists is today," Cain says.
Mobile technology, such as tablet computers, Internet-enabled smartphones, and the applications both devices use, will change the face of HM and other physician specialties, one medical software executive says.
"Mobile technology will improve efficiency and reduce costs," Mark Cain, chief technology officer of MIM Software Inc., writes in an e-mail to The Hospitalist. "Compare the cost of an iPad to that of an exam room PC. If I was making the decision, I'd find a way to remove every exam room PC [with their keyboards, CPUs, mice, monitors, and network cables] and instead supply iPads to be carried by the staff. With a good Wi-Fi network and iPads, every room is digitally equipped as soon as the doctor walks in."
Cain has seen the paradigm shift of touchscreen technology firsthand: The FDA recently approved an application from Cleveland-based MIM to let doctors make medical diagnoses based on computed tomography (CT) and magnetic resonance imaging (MRI) via an application available for the iPhone and iPad. The application, the first with the FDA's imprimatur for diagnostic radiology, allows hospitalists and other physicians to access data via a secure network transfer.
The app for that is just the latest sign that the growing prevalence of touchscreen technology is changing the face of HM.
The evolution has its pitfalls, though. Patient privacy, wireless security, and the hesitancy of physicians to adopt change will likely slow the adoption of technology, but "the integration of interactive devices into a physician's daily workflow could become as commonplace in 10 years as the presence of hospitalists is today," Cain says.
Mobile technology, such as tablet computers, Internet-enabled smartphones, and the applications both devices use, will change the face of HM and other physician specialties, one medical software executive says.
"Mobile technology will improve efficiency and reduce costs," Mark Cain, chief technology officer of MIM Software Inc., writes in an e-mail to The Hospitalist. "Compare the cost of an iPad to that of an exam room PC. If I was making the decision, I'd find a way to remove every exam room PC [with their keyboards, CPUs, mice, monitors, and network cables] and instead supply iPads to be carried by the staff. With a good Wi-Fi network and iPads, every room is digitally equipped as soon as the doctor walks in."
Cain has seen the paradigm shift of touchscreen technology firsthand: The FDA recently approved an application from Cleveland-based MIM to let doctors make medical diagnoses based on computed tomography (CT) and magnetic resonance imaging (MRI) via an application available for the iPhone and iPad. The application, the first with the FDA's imprimatur for diagnostic radiology, allows hospitalists and other physicians to access data via a secure network transfer.
The app for that is just the latest sign that the growing prevalence of touchscreen technology is changing the face of HM.
The evolution has its pitfalls, though. Patient privacy, wireless security, and the hesitancy of physicians to adopt change will likely slow the adoption of technology, but "the integration of interactive devices into a physician's daily workflow could become as commonplace in 10 years as the presence of hospitalists is today," Cain says.
HM Improves Quality in Singapore
The HM model has solidified its global status.
A group of family physicians in Singapore studied the implementation of a hospitalist program at Singapore General Hospital, according to a Journal of Hospital Medicine report. The researchers found that, compared with patients under the care of specialists, those cared for by hospitalists had shorter lengths of stay (adjusted LOS, geometric mean, GM 4.4 vs. 5.3 days; P<0.001) and reduced costs (adjusted cost, GM, $2,250.70 vs. $2,500; P=0.003). The researchers also found a similar inpatient mortality rate (4.2% vs. 5.3%, P=0.307) and 30-day all-cause unscheduled readmission rate (7.5% vs. 8.4%, P=0.231).
"These findings suggest that the hospitalist care model can be adapted for health systems outside North America and may produce similar beneficial effects in care efficiency and cost savings," the authors concluded.
The initiative in Singapore, a city-state in Southeast Asia with a population close to 5 million, is not the first adoption of the HM model outside the U.S. But the data showing reduced LOS and costs is further evidence of both the growth and the efficacy of the HM movement worldwide, says Kheng Hock Lee, MBBS, MMed, FCFP, one of the study authors.
"Our study showed very similar improvement in care outcomes with hospitalist programs in the United States, although we are thousands of miles apart and with a different culture and healthcare system," Kheng Hock wrote in an e-mail to The Hospitalist eWire. "I think the success of the hospitalist care model stems from the recognition that it fulfills an emergent need that has resulted from the increase in complexity of healthcare and the need for specialization in medicine.
"The need for a good generalist in the hospital setting who can coordinate care and treat patient holistically is intuitively recognized by policymakers, healthcare providers, and patients."
The HM model has solidified its global status.
A group of family physicians in Singapore studied the implementation of a hospitalist program at Singapore General Hospital, according to a Journal of Hospital Medicine report. The researchers found that, compared with patients under the care of specialists, those cared for by hospitalists had shorter lengths of stay (adjusted LOS, geometric mean, GM 4.4 vs. 5.3 days; P<0.001) and reduced costs (adjusted cost, GM, $2,250.70 vs. $2,500; P=0.003). The researchers also found a similar inpatient mortality rate (4.2% vs. 5.3%, P=0.307) and 30-day all-cause unscheduled readmission rate (7.5% vs. 8.4%, P=0.231).
"These findings suggest that the hospitalist care model can be adapted for health systems outside North America and may produce similar beneficial effects in care efficiency and cost savings," the authors concluded.
The initiative in Singapore, a city-state in Southeast Asia with a population close to 5 million, is not the first adoption of the HM model outside the U.S. But the data showing reduced LOS and costs is further evidence of both the growth and the efficacy of the HM movement worldwide, says Kheng Hock Lee, MBBS, MMed, FCFP, one of the study authors.
"Our study showed very similar improvement in care outcomes with hospitalist programs in the United States, although we are thousands of miles apart and with a different culture and healthcare system," Kheng Hock wrote in an e-mail to The Hospitalist eWire. "I think the success of the hospitalist care model stems from the recognition that it fulfills an emergent need that has resulted from the increase in complexity of healthcare and the need for specialization in medicine.
"The need for a good generalist in the hospital setting who can coordinate care and treat patient holistically is intuitively recognized by policymakers, healthcare providers, and patients."
The HM model has solidified its global status.
A group of family physicians in Singapore studied the implementation of a hospitalist program at Singapore General Hospital, according to a Journal of Hospital Medicine report. The researchers found that, compared with patients under the care of specialists, those cared for by hospitalists had shorter lengths of stay (adjusted LOS, geometric mean, GM 4.4 vs. 5.3 days; P<0.001) and reduced costs (adjusted cost, GM, $2,250.70 vs. $2,500; P=0.003). The researchers also found a similar inpatient mortality rate (4.2% vs. 5.3%, P=0.307) and 30-day all-cause unscheduled readmission rate (7.5% vs. 8.4%, P=0.231).
"These findings suggest that the hospitalist care model can be adapted for health systems outside North America and may produce similar beneficial effects in care efficiency and cost savings," the authors concluded.
The initiative in Singapore, a city-state in Southeast Asia with a population close to 5 million, is not the first adoption of the HM model outside the U.S. But the data showing reduced LOS and costs is further evidence of both the growth and the efficacy of the HM movement worldwide, says Kheng Hock Lee, MBBS, MMed, FCFP, one of the study authors.
"Our study showed very similar improvement in care outcomes with hospitalist programs in the United States, although we are thousands of miles apart and with a different culture and healthcare system," Kheng Hock wrote in an e-mail to The Hospitalist eWire. "I think the success of the hospitalist care model stems from the recognition that it fulfills an emergent need that has resulted from the increase in complexity of healthcare and the need for specialization in medicine.
"The need for a good generalist in the hospital setting who can coordinate care and treat patient holistically is intuitively recognized by policymakers, healthcare providers, and patients."
Pricey Problems
Hospitalists working to reduce readmissions and medication errors would do well to consider a new policy report that suggests the two systemic problems cost the healthcare system $46 billion a year.
The white paper sets out to identify specific actions—such as creating detailed discharge plans, having pharmacists make follow-up calls after discharge, and using bar-code technology to verify drug dosages—that public and private decision-makers can use to help tackle the issues. While the bureaucratic checklist devised by the New England Healthcare Institute (NEHI) and the National Priorities Partnership is a good broad brush, the report's value may lie in how it prods physicians to change the way care is delivered.
"It's a quick and easy guide, but what's beneath it is quite complex," says Karen Nelson, a former nurse and senior vice president for clinical affairs for the Massachusetts Hospital Association. "We've seen terrific pockets of expertise … but the real work has to come for all providers and programs to do this at the same time."
Nelson believes hospitalists are "clearly essential team leaders" in fighting both medication errors and readmissions. Medication reconciliation is a problem in each of those silos that HM groups battle daily. To wit, the Agency for Healthcare Research and Quality (AHRQ) has awarded SHM a $1.5 million grant for a three-year, multicenter medication reconciliation QI study. “As care-transition managers, hospitalists are well-positioned to analyze the pitfalls of care coordination and develop and implement quality-improvement solutions to improve patient safety," says Joseph Miller, SHM's senior vice president and chief solutions officer.
Nelson says NEHI's "compact action briefs" suggest that payment bundling is one answer to wasteful spending. However, while hospitalists agree the payment system needs work, they caution against the potential consequences of such a drastic shift.
"It really makes the case to move away from the fee-for-service model," Nelson says. "What we need to do is redesign the system to cover the patient regardless of encounter or what the driver is."
Hospitalists working to reduce readmissions and medication errors would do well to consider a new policy report that suggests the two systemic problems cost the healthcare system $46 billion a year.
The white paper sets out to identify specific actions—such as creating detailed discharge plans, having pharmacists make follow-up calls after discharge, and using bar-code technology to verify drug dosages—that public and private decision-makers can use to help tackle the issues. While the bureaucratic checklist devised by the New England Healthcare Institute (NEHI) and the National Priorities Partnership is a good broad brush, the report's value may lie in how it prods physicians to change the way care is delivered.
"It's a quick and easy guide, but what's beneath it is quite complex," says Karen Nelson, a former nurse and senior vice president for clinical affairs for the Massachusetts Hospital Association. "We've seen terrific pockets of expertise … but the real work has to come for all providers and programs to do this at the same time."
Nelson believes hospitalists are "clearly essential team leaders" in fighting both medication errors and readmissions. Medication reconciliation is a problem in each of those silos that HM groups battle daily. To wit, the Agency for Healthcare Research and Quality (AHRQ) has awarded SHM a $1.5 million grant for a three-year, multicenter medication reconciliation QI study. “As care-transition managers, hospitalists are well-positioned to analyze the pitfalls of care coordination and develop and implement quality-improvement solutions to improve patient safety," says Joseph Miller, SHM's senior vice president and chief solutions officer.
Nelson says NEHI's "compact action briefs" suggest that payment bundling is one answer to wasteful spending. However, while hospitalists agree the payment system needs work, they caution against the potential consequences of such a drastic shift.
"It really makes the case to move away from the fee-for-service model," Nelson says. "What we need to do is redesign the system to cover the patient regardless of encounter or what the driver is."
Hospitalists working to reduce readmissions and medication errors would do well to consider a new policy report that suggests the two systemic problems cost the healthcare system $46 billion a year.
The white paper sets out to identify specific actions—such as creating detailed discharge plans, having pharmacists make follow-up calls after discharge, and using bar-code technology to verify drug dosages—that public and private decision-makers can use to help tackle the issues. While the bureaucratic checklist devised by the New England Healthcare Institute (NEHI) and the National Priorities Partnership is a good broad brush, the report's value may lie in how it prods physicians to change the way care is delivered.
"It's a quick and easy guide, but what's beneath it is quite complex," says Karen Nelson, a former nurse and senior vice president for clinical affairs for the Massachusetts Hospital Association. "We've seen terrific pockets of expertise … but the real work has to come for all providers and programs to do this at the same time."
Nelson believes hospitalists are "clearly essential team leaders" in fighting both medication errors and readmissions. Medication reconciliation is a problem in each of those silos that HM groups battle daily. To wit, the Agency for Healthcare Research and Quality (AHRQ) has awarded SHM a $1.5 million grant for a three-year, multicenter medication reconciliation QI study. “As care-transition managers, hospitalists are well-positioned to analyze the pitfalls of care coordination and develop and implement quality-improvement solutions to improve patient safety," says Joseph Miller, SHM's senior vice president and chief solutions officer.
Nelson says NEHI's "compact action briefs" suggest that payment bundling is one answer to wasteful spending. However, while hospitalists agree the payment system needs work, they caution against the potential consequences of such a drastic shift.
"It really makes the case to move away from the fee-for-service model," Nelson says. "What we need to do is redesign the system to cover the patient regardless of encounter or what the driver is."
The Facebook of Medical Records
A California hospitalist has launched a website that he envisions as an electronic health records (EHR) portal for physicians and patients alike.
MDblackbox aims to blend the interactive familiarity of such social networks as Facebook with the institutional-grade security necessary to comply with the Health Insurance Portability and Accountability Act (HIPPA), according to its inventor, Sami Bogale, MD, a hospitalist at Mills-Peninsula Medical Center in Burlingame, Calif.
"The idea is for any doctor to sign up, nationwide, and [the site] will provide uninterrupted communication" both between doctors and between physicians and patients, says Dr. Bogale, CEO of MDblackbox Inc. "The idea from the patient side is that if a patient goes out of town or goes to a new physician, they have a real copy of their medical record right there."
Dr. Bogale says he's been working on the site for the better part of three years and has spent $250,000 or so on its development. (He jokes that he doesn’t want to know how much time he’s spent on it.) He decided to launch the site this month as he saw other entrepreneurs and physicians looking to take advantage of the momentum behind EHR, buzz attributable in large part to health reform. In fact, the Centers for Medicare & Medicaid Services announced in January that registration had begun for applications to garner a piece of the $20 billion the federal government has set aside for doctors and hospitals that adopt new technologies.
Dr. Bogale continues to look for venture capitalists to back his site, which includes records management, appointment scheduling and reminder, lab orders and voice recordings that can be attached to medical files. Most services are free.
"The idea is to have a nationwide system where every doctor could pretty much have their own personal page and interact with doctors and patients," Dr. Bogale says. "I could see it really growing."
A California hospitalist has launched a website that he envisions as an electronic health records (EHR) portal for physicians and patients alike.
MDblackbox aims to blend the interactive familiarity of such social networks as Facebook with the institutional-grade security necessary to comply with the Health Insurance Portability and Accountability Act (HIPPA), according to its inventor, Sami Bogale, MD, a hospitalist at Mills-Peninsula Medical Center in Burlingame, Calif.
"The idea is for any doctor to sign up, nationwide, and [the site] will provide uninterrupted communication" both between doctors and between physicians and patients, says Dr. Bogale, CEO of MDblackbox Inc. "The idea from the patient side is that if a patient goes out of town or goes to a new physician, they have a real copy of their medical record right there."
Dr. Bogale says he's been working on the site for the better part of three years and has spent $250,000 or so on its development. (He jokes that he doesn’t want to know how much time he’s spent on it.) He decided to launch the site this month as he saw other entrepreneurs and physicians looking to take advantage of the momentum behind EHR, buzz attributable in large part to health reform. In fact, the Centers for Medicare & Medicaid Services announced in January that registration had begun for applications to garner a piece of the $20 billion the federal government has set aside for doctors and hospitals that adopt new technologies.
Dr. Bogale continues to look for venture capitalists to back his site, which includes records management, appointment scheduling and reminder, lab orders and voice recordings that can be attached to medical files. Most services are free.
"The idea is to have a nationwide system where every doctor could pretty much have their own personal page and interact with doctors and patients," Dr. Bogale says. "I could see it really growing."
A California hospitalist has launched a website that he envisions as an electronic health records (EHR) portal for physicians and patients alike.
MDblackbox aims to blend the interactive familiarity of such social networks as Facebook with the institutional-grade security necessary to comply with the Health Insurance Portability and Accountability Act (HIPPA), according to its inventor, Sami Bogale, MD, a hospitalist at Mills-Peninsula Medical Center in Burlingame, Calif.
"The idea is for any doctor to sign up, nationwide, and [the site] will provide uninterrupted communication" both between doctors and between physicians and patients, says Dr. Bogale, CEO of MDblackbox Inc. "The idea from the patient side is that if a patient goes out of town or goes to a new physician, they have a real copy of their medical record right there."
Dr. Bogale says he's been working on the site for the better part of three years and has spent $250,000 or so on its development. (He jokes that he doesn’t want to know how much time he’s spent on it.) He decided to launch the site this month as he saw other entrepreneurs and physicians looking to take advantage of the momentum behind EHR, buzz attributable in large part to health reform. In fact, the Centers for Medicare & Medicaid Services announced in January that registration had begun for applications to garner a piece of the $20 billion the federal government has set aside for doctors and hospitals that adopt new technologies.
Dr. Bogale continues to look for venture capitalists to back his site, which includes records management, appointment scheduling and reminder, lab orders and voice recordings that can be attached to medical files. Most services are free.
"The idea is to have a nationwide system where every doctor could pretty much have their own personal page and interact with doctors and patients," Dr. Bogale says. "I could see it really growing."
The Future is Near
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
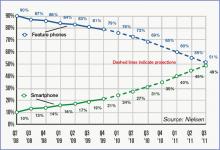
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.