User login
The short cervix and preterm birth: 8 key questions and evidence-based answers
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
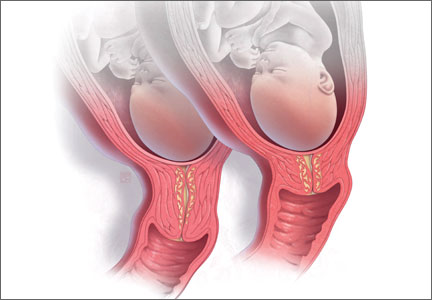
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
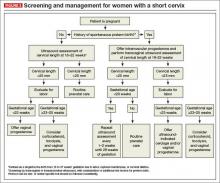
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, city and state. Stay in touch! Your feedback is important to us!
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, city and state. Stay in touch! Your feedback is important to us!
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.com Please include your name, city and state. Stay in touch! Your feedback is important to us!
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.