User login
Efficacy of Skin Preparation in Eradicating Organisms Before Total Knee Arthroplasty
Knee arthroplasty continues to be one of the most common and successful methods for treating severe arthritis and other painful arthropathies. Increasing steadily from 1998 to 2008, and with more than 676,000 procedures performed in 2008, knee arthroplasty remains the most common surgical joint replacement procedure.1
Although perioperative and long-term complications are uncommon, infection remains one of the most serious complications of total knee arthroplasty (TKA). Some studies have found a post-TKA infection rate of less than 1%.2 The solution of 2% chlorhexidine gluconate and 70% isopropyl alcohol (Chloraprep; Medi-Flex, Overland Park, Kansas) is commonly used for antiseptic skin preparation before surgery. Studies have shown significant decreases in post-TKA infection rates with preoperative use.3,4 Another study evaluated the efficacy of 3 different skin solutions and found Chloraprep to be the most efficient in eradicating bacteria from the foot and ankle before surgery. The investigators noted that, even with preoperative use of Chloraprep, 23% of patients had residual bacteria on the surface of the skin between the toes.5 Like the foot, the popliteal fossa is an intertriginous area that may harbor normal flora, including gram-positive cocci, in large numbers, mainly because of the contact between 2 skin surfaces. Although postoperative infection rates decrease with use of Chloraprep, its presurgical efficacy in killing bacteria on another intertriginous area, the popliteal fossa, is largely unknown. Also unknown are susceptible organism species and organism population numbers.
Concerned that our skin preparation might be ineffective, we conducted a study to evaluate the efficacy of Chloraprep skin preparation in eradicating organisms before TKA, to isolate the type and number of organisms, and to evaluate several other contributing factors that could lead to infection.
Materials and Methods
This prospective study included 99 patients who were undergoing primary TKA at John Peter Smith Hospital between July 1, 2011 and August 31, 2012. An attempt was made to enroll consecutive TKA patients, and all patients agreed to participate, but a few were not enrolled because the study team had not asked for their consent before they were taken to the operating room. Patients did not receive monetary compensation for participation. Exclusion criteria were pregnancy, imprisonment, and age under 18 years. The study was approved by the institutional review boards at John Peter Smith Hospital and the University of North Texas Health Science Center.
Each lower extremity was prepared with Chloraprep according to the manufacturer’s instructions. Preparation was done by well-trained operating room staff members who were supervised by the surgeon (Dr. Sanchez or Dr. Wagner) but were not involved in the study. With use of the Chloraprep applicator, the solution was applied in a back-and-forth manner to the entire operative leg for at least 30 seconds, and then discarded. This scrub procedure was repeated with a second applicator before standard drapes were placed. The leg was left to air-dry for at least 30 seconds, and the drapes were placed before postsolution swabbing and before the iodine-impregnated adhesive drape was placed around the knee. During drying, the solution was not blotted, wiped away, or touched with instrumentation. Patients were swabbed with an epidermal sterile swab in the popliteal fossa of the knee undergoing surgery, both before solution application (presolution swab) and after (postsolution swab). Only the operating surgeon participated in swabbing the patients. Aerobic and anaerobic swabs were vigorously rubbed over a 2- to 3-in wide area across the entire posterior flexion crease surface.
The collected pre- and postsolution swabs were sent to John Peter Smith Laboratory for identification of organisms. Anaerobic swabs were cultured in thioglycolate broth and on 4 plates: MacConkey agar, Columbia colistin–nalidixic acid agar, chocolate agar, and sheep blood agar. Aerobic swabs were cultured in thioglycolate broth with hemin and vitamin K and on 4 plates: anaerobic blood agar, bile esculin agar, kanamycin and vancomycin agar, and Columbia colistin–nalidixic acid agar. Anaerobic plates were incubated in an anoxic environment. The plates were then read daily, and final reports were issued after 48 hours (for aerobic bacterial isolates) and 72 hours (for anaerobic bacterial isolates), as was the standard at the time.
Additional patient data were collected for possible correlations: American Society of Anesthesiologists (ASA) classification (physical status),6 body mass index (BMI), age, sex, arthroplasty type (unilateral, bilateral), and diabetic status. In addition, patients were asked if they had used Hibiclens antiseptic/antimicrobial skin cleanser daily during the week before surgery—as they had been instructed to do—and the number of times they had used the cleanser.
Study data were analyzed and were used to stratify patients into several groups. Each group had multiple factors evaluated.
Descriptive statistics were used to characterize the patient demographic information. Chi-square analyses were performed to evaluate the difference between presence of organisms before and after solution application, and the data were also layered with reported Hibiclens cleanser use. In addition, binary logistic regression was used to determine if demographic variables could predict presence of organism isolates before and after solution application. Data analyses were conducted using IBM SPSS Statistics Version 20.
Results
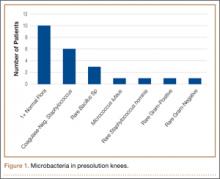
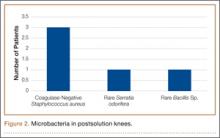
No patient had a postoperative infection. Culture isolates grew in 20 (20%) of the 99 patients before solution application and in 5 (5%) of the 99 after application. Of the 20 patients with presolution culture isolates, 16 (80%) had 1 bacterial isolate, and 4 (20%) had 2 or more species. Presolution isolates included normal flora (10, 50%), coagulase-negative Staphylococcus aureus (6, 30%), rare Bacillus (3, 15%), Micrococcus luteus (1, 5%), rare gram-negative (1, 5%), rare gram-positive (1, 5%), and Staphylococcus hominis (1, 5%) (Figure 1). Postsolution isolates included coagulase-negative S aureus (3, 60%), rare Bacillus (1, 20%), and rare Serratia odorifera (1, 20%) (Figure 2). Two postsolution isolates did not have an associated presolution isolate. Presolution organism isolation was an important predictor of postsolution organism isolation (P < .046).
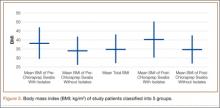
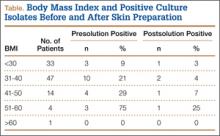
BMI was recorded for all patients. Mean BMI was 35 (range, 20-63). Distribution was as follows: BMI under 20 (3 patients), under 30 (30 patients), under 40 (47 patients), under 50 (14 patients), under 60 (4 patients), and over 60 (1 patient). Mean presolution BMI was significantly (P < .03) higher for patients with bacterial isolates than for patients without isolates (38 and 34, respectively). Mean postsolution BMI was 40 for patients with bacterial isolates and 35 for patients without isolates (Figure 3). Of the 33 patients with BMI under 30, 3 (9%) had presolution isolates and 1 (3%) had postsolution isolates. Of the 66 patients with BMI over 30, 17 (26%) had presolution isolates and 4 (6%) had postsolution isolates (Table).
Of the 99 patients, 30 (30%) had diabetes. Of these 30 patients, 9 (30%) had presolution isolates (45% of all presolution isolates) and 3 (10%) had postsolution isolates (60% of all postsolution isolates.) Although neither pre- nor postsolution results were statistically significant (P = .172) for increasing organism isolation in patients with diabetes, the odds ratio for these patients was 3.6 when the focus was on the likelihood of postsolution organism isolation.
Mean age was 57 years (range, 29-87 years). Results were not statistically significant for age being a likely factor for organism isolate prediction.
There were 81 women and 18 men in the study. Of the 81 women, 16 (20%) had positive presolution cultures and 5 (6%) had positive postsolution cultures. Of the 18 men, 4 (22%) had positive presolution cultures and none had a positive postsolution culture.
Race was recorded. Forty-nine patients were white, 27 black, 18 Hispanic, and 5 unknown. Presolution, 12 whites (24%), 5 blacks (19%), and 3 Hispanics (17%) had positive cultures. Postsolution, 1 white (2%), 1 black (4%), 3 Hispanics (17%), and 1 patient of unknown race (20%) had positive cultures.
ASA classifications were recorded and analyzed. Of the 99 patients, 38 were classified ASA-2, 60 were ASA-3, and 1 was ASA-4. Presolution, 9 (24%) of the 38 ASA-2 patients and 11 (18%) of the 60 ASA-3 patients had positive cultures; postsolution, 2 (5%) of the 38 ASA-2 patients and 3 (5%) of the 60 ASA-3 patients had positive cultures. The 1 ASA-4 patient had neither presolution nor postsolution positive cultures.
Types of TKA (bilateral, unilateral) were recorded. Of the 99 patients, 89 had unilateral TKAs and 10 had bilateral TKAs. Presolution, 19 (21%) of the 89 unilaterals and 1 (10%) of the 10 bilaterals had positive cultures. Postsolution, 5 (6%) of the 89 unilaterals and none of the 10 bilaterals had positive cultures.
Patients were also verbally asked how many cleanser baths they had taken before surgery. Of the 99 patients, 88 reported having taken 1 or more cleanser baths, and 1 reported no baths; 10 patients’ responses were not available. The 88 patients who had taken at least 1 cleanser bath were divided into 3 groups: 1 bath (35 patients), 2 baths (49 patients), and 3 or more baths (4 patients). Presolution, positive cultures were found for 18 (20%) of the 88 patients; for 7 (20%) of the 35 patients with 1 bath; for 10 (20%) of the 49 patients with 2 baths; and for 1 (25%) of the 4 patients with 3 or more baths. Postsolution, positive cultures were found for 5 (6%) of the 88 patients; for 2 (6%) of the 35 patients with 1 bath; for 3 (6%) of the 49 patients with 2 baths; and for 0 (0%) of the 4 patients with 3 or more baths. The 1 patient with no baths did not have a positive culture. Of the 10 patients whose responses were unavailable, 2 patients had positive presolution cultures and no patients had a positive postsolution culture.
Discussion
The efficacy of using Chloraprep before TKA has not been well assessed in orthopedic practice. However, compared with other preoperative solutions, chlorhexidine has been shown to be significantly better in preventing post-TKA infections.4 Other studies have found it far more effective than other commonly used surgical preparations in eliminating microorganisms in hip arthroplasty and foot surgery.5,7 Our study, focused on the efficacy of Chloraprep in killing bacteria, found the solution effective in removing 85% (17/20) of cultured presolution organisms.
Of the bacterial isolates cultured, normal flora were effectively removed from all associated postsolution cultures. Although most of the bacterial isolates were eliminated after solution application, both coagulase-negative S aureus and rare Bacillus species were found both pre- and postsolution, suggesting either inadequate skin preparation or resistant bacteria.
With respect to the secondary variables, our study data showed that BMI was an important predictor for bacterial isolates, significantly so presolution (P < .03). Mean BMI for the overall study was 35, firmly in the obese category. Only when BMI increased to 38 did it become significant as a predictor for postsolution organisms. Mean postsolution BMI was even higher, 40, which is in the morbidly obese category. Interestingly, the percentage of nonobese patients (BMI, <30) with positive presolution cultures was only 9%, versus the 20% with positive presolution cultures overall. In addition, 1 nonobese patient had positive postsolution cultures.
Other studies have linked higher BMI to higher rates of surgical site infection and other complications, but it is unknown if the infections are due to higher bacterial counts in the patients with high BMI or to other factors, such as reduced wound healing or decreased immune response. More research is needed to determine if the number of organisms in patients with high BMI correlates to a higher risk for surgical site infection.8 As expected, along with BMI (>38), presolution organism isolation was an important predictor for postsolution organism isolation. Patients with presolution organism isolation were 24 times more likely to have postsolution isolates.
Even though diabetic status was not significant for predicting bacterial isolation, patients with diabetes were 3.6 times more likely than patients without diabetes to have a positive culture. Other studies have shown that, compared with patients without diabetes, patients with diabetes had a higher chance of postoperative infection.9,10
In this study, 18 of 20 patients with presolution organism isolates reported they had been compliant in taking the recommended preoperative cleanser baths. This finding may indicate that preoperative cleanser baths are ineffective. However, only 20% of our patients had positive presolution cultures, whereas Ostrander and colleagues5 reported 30% positive pre-preparation cultures from the anterior knee. A recent Cochrane Database System Review did not provide clear evidence of benefit for preoperative showering or bathing with chlorhexidine over other wash products.11 Although their benefit may be questionable, we will continue to recommend preoperative cleanser baths.
One limitation of this study is sample size. Although size was sufficient for determining the efficacy of Chloraprep in the intertriginous area of the back of the knee, the lack of statistical significance (eg, effect of diabetes) may not be accurate. In addition, because the nurse who prepared patients’ skin was aware of the study and was supervised in every case, it is possible that the preparation was done more carefully than usual, resulting in more negative cultures than average. Also, compliance in taking preoperative cleanser baths was subjectively determined. Patients may have reported more baths than were actually taken. Still another study limitation is that 2 postsolution isolates did not have an associated presolution isolate. Although we think this may have resulted from laboratory contamination, it is possible the presolution swabs did not accurately determine true bacterial counts in these cases.
Conclusion
A study that showed significant residual bacteria between patients’ toes after chlorhexidine skin preparation5 left us concerned that Chloraprep skin preparation for TKA might not be adequate. The present study showed that this solution was effective in eliminating bacteria from the intertriginous area of the back of the knee in 95% of patients. Skin preparation appears to be less effective in patients with higher BMI.
1. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201-207.
2. Poultsides LA, Ma Y, Della Valle AG, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty—incidence and risk factors. J Arthroplasty. 2013;28(3):385-389.
3. Johnson AJ, Kapadia BH, Daley JA, Molina CB, Mont MA. Chlorhexidine reduces infections in knee arthroplasty. J Knee Surg. 2013;26(3):213-218.
4. Zywiel MG, Daley JA, Delanois RE, Naziri Q, Johnson AJ, Mont MA. Advance pre-operative chlorhexidine reduces the incidence of surgical site infections in knee arthroplasty. Int Orthop. 2011;35(7):1001-1006.
5. Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg Am. 2005;87(5):980-985.
6. Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217-222.
7. Johnson AJ, Daley JA, Zywiel MG, Delanois RE, Mont MA. Preoperative chlorhexidine preparation and the incidence of surgical site infections after hip arthroplasty. J Arthroplasty. 2010;25(6 suppl):98-102.
8. Samson AJ, Mercer GE, Campbell DG. Total knee replacement in the morbidly obese: a literature review. ANZ J Surg. 2010;80(9):595-599.
9. Iorio R, Williams KM, Marcantonio AJ, Specht LM, Tilzey JF, Healy WL. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty. 2012;27(5):726-729.
10. Viens NA, Hug KT, Marchant MH, Cook C, Vail TP, Bolognesi MP. Role of diabetes type in perioperative outcomes after hip and knee arthroplasty in the United States. J Surg Orthop Adv. 2012;21(4):253-260.
11. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.
Knee arthroplasty continues to be one of the most common and successful methods for treating severe arthritis and other painful arthropathies. Increasing steadily from 1998 to 2008, and with more than 676,000 procedures performed in 2008, knee arthroplasty remains the most common surgical joint replacement procedure.1
Although perioperative and long-term complications are uncommon, infection remains one of the most serious complications of total knee arthroplasty (TKA). Some studies have found a post-TKA infection rate of less than 1%.2 The solution of 2% chlorhexidine gluconate and 70% isopropyl alcohol (Chloraprep; Medi-Flex, Overland Park, Kansas) is commonly used for antiseptic skin preparation before surgery. Studies have shown significant decreases in post-TKA infection rates with preoperative use.3,4 Another study evaluated the efficacy of 3 different skin solutions and found Chloraprep to be the most efficient in eradicating bacteria from the foot and ankle before surgery. The investigators noted that, even with preoperative use of Chloraprep, 23% of patients had residual bacteria on the surface of the skin between the toes.5 Like the foot, the popliteal fossa is an intertriginous area that may harbor normal flora, including gram-positive cocci, in large numbers, mainly because of the contact between 2 skin surfaces. Although postoperative infection rates decrease with use of Chloraprep, its presurgical efficacy in killing bacteria on another intertriginous area, the popliteal fossa, is largely unknown. Also unknown are susceptible organism species and organism population numbers.
Concerned that our skin preparation might be ineffective, we conducted a study to evaluate the efficacy of Chloraprep skin preparation in eradicating organisms before TKA, to isolate the type and number of organisms, and to evaluate several other contributing factors that could lead to infection.
Materials and Methods
This prospective study included 99 patients who were undergoing primary TKA at John Peter Smith Hospital between July 1, 2011 and August 31, 2012. An attempt was made to enroll consecutive TKA patients, and all patients agreed to participate, but a few were not enrolled because the study team had not asked for their consent before they were taken to the operating room. Patients did not receive monetary compensation for participation. Exclusion criteria were pregnancy, imprisonment, and age under 18 years. The study was approved by the institutional review boards at John Peter Smith Hospital and the University of North Texas Health Science Center.
Each lower extremity was prepared with Chloraprep according to the manufacturer’s instructions. Preparation was done by well-trained operating room staff members who were supervised by the surgeon (Dr. Sanchez or Dr. Wagner) but were not involved in the study. With use of the Chloraprep applicator, the solution was applied in a back-and-forth manner to the entire operative leg for at least 30 seconds, and then discarded. This scrub procedure was repeated with a second applicator before standard drapes were placed. The leg was left to air-dry for at least 30 seconds, and the drapes were placed before postsolution swabbing and before the iodine-impregnated adhesive drape was placed around the knee. During drying, the solution was not blotted, wiped away, or touched with instrumentation. Patients were swabbed with an epidermal sterile swab in the popliteal fossa of the knee undergoing surgery, both before solution application (presolution swab) and after (postsolution swab). Only the operating surgeon participated in swabbing the patients. Aerobic and anaerobic swabs were vigorously rubbed over a 2- to 3-in wide area across the entire posterior flexion crease surface.
The collected pre- and postsolution swabs were sent to John Peter Smith Laboratory for identification of organisms. Anaerobic swabs were cultured in thioglycolate broth and on 4 plates: MacConkey agar, Columbia colistin–nalidixic acid agar, chocolate agar, and sheep blood agar. Aerobic swabs were cultured in thioglycolate broth with hemin and vitamin K and on 4 plates: anaerobic blood agar, bile esculin agar, kanamycin and vancomycin agar, and Columbia colistin–nalidixic acid agar. Anaerobic plates were incubated in an anoxic environment. The plates were then read daily, and final reports were issued after 48 hours (for aerobic bacterial isolates) and 72 hours (for anaerobic bacterial isolates), as was the standard at the time.
Additional patient data were collected for possible correlations: American Society of Anesthesiologists (ASA) classification (physical status),6 body mass index (BMI), age, sex, arthroplasty type (unilateral, bilateral), and diabetic status. In addition, patients were asked if they had used Hibiclens antiseptic/antimicrobial skin cleanser daily during the week before surgery—as they had been instructed to do—and the number of times they had used the cleanser.
Study data were analyzed and were used to stratify patients into several groups. Each group had multiple factors evaluated.
Descriptive statistics were used to characterize the patient demographic information. Chi-square analyses were performed to evaluate the difference between presence of organisms before and after solution application, and the data were also layered with reported Hibiclens cleanser use. In addition, binary logistic regression was used to determine if demographic variables could predict presence of organism isolates before and after solution application. Data analyses were conducted using IBM SPSS Statistics Version 20.
Results
No patient had a postoperative infection. Culture isolates grew in 20 (20%) of the 99 patients before solution application and in 5 (5%) of the 99 after application. Of the 20 patients with presolution culture isolates, 16 (80%) had 1 bacterial isolate, and 4 (20%) had 2 or more species. Presolution isolates included normal flora (10, 50%), coagulase-negative Staphylococcus aureus (6, 30%), rare Bacillus (3, 15%), Micrococcus luteus (1, 5%), rare gram-negative (1, 5%), rare gram-positive (1, 5%), and Staphylococcus hominis (1, 5%) (Figure 1). Postsolution isolates included coagulase-negative S aureus (3, 60%), rare Bacillus (1, 20%), and rare Serratia odorifera (1, 20%) (Figure 2). Two postsolution isolates did not have an associated presolution isolate. Presolution organism isolation was an important predictor of postsolution organism isolation (P < .046).
BMI was recorded for all patients. Mean BMI was 35 (range, 20-63). Distribution was as follows: BMI under 20 (3 patients), under 30 (30 patients), under 40 (47 patients), under 50 (14 patients), under 60 (4 patients), and over 60 (1 patient). Mean presolution BMI was significantly (P < .03) higher for patients with bacterial isolates than for patients without isolates (38 and 34, respectively). Mean postsolution BMI was 40 for patients with bacterial isolates and 35 for patients without isolates (Figure 3). Of the 33 patients with BMI under 30, 3 (9%) had presolution isolates and 1 (3%) had postsolution isolates. Of the 66 patients with BMI over 30, 17 (26%) had presolution isolates and 4 (6%) had postsolution isolates (Table).
Of the 99 patients, 30 (30%) had diabetes. Of these 30 patients, 9 (30%) had presolution isolates (45% of all presolution isolates) and 3 (10%) had postsolution isolates (60% of all postsolution isolates.) Although neither pre- nor postsolution results were statistically significant (P = .172) for increasing organism isolation in patients with diabetes, the odds ratio for these patients was 3.6 when the focus was on the likelihood of postsolution organism isolation.
Mean age was 57 years (range, 29-87 years). Results were not statistically significant for age being a likely factor for organism isolate prediction.
There were 81 women and 18 men in the study. Of the 81 women, 16 (20%) had positive presolution cultures and 5 (6%) had positive postsolution cultures. Of the 18 men, 4 (22%) had positive presolution cultures and none had a positive postsolution culture.
Race was recorded. Forty-nine patients were white, 27 black, 18 Hispanic, and 5 unknown. Presolution, 12 whites (24%), 5 blacks (19%), and 3 Hispanics (17%) had positive cultures. Postsolution, 1 white (2%), 1 black (4%), 3 Hispanics (17%), and 1 patient of unknown race (20%) had positive cultures.
ASA classifications were recorded and analyzed. Of the 99 patients, 38 were classified ASA-2, 60 were ASA-3, and 1 was ASA-4. Presolution, 9 (24%) of the 38 ASA-2 patients and 11 (18%) of the 60 ASA-3 patients had positive cultures; postsolution, 2 (5%) of the 38 ASA-2 patients and 3 (5%) of the 60 ASA-3 patients had positive cultures. The 1 ASA-4 patient had neither presolution nor postsolution positive cultures.
Types of TKA (bilateral, unilateral) were recorded. Of the 99 patients, 89 had unilateral TKAs and 10 had bilateral TKAs. Presolution, 19 (21%) of the 89 unilaterals and 1 (10%) of the 10 bilaterals had positive cultures. Postsolution, 5 (6%) of the 89 unilaterals and none of the 10 bilaterals had positive cultures.
Patients were also verbally asked how many cleanser baths they had taken before surgery. Of the 99 patients, 88 reported having taken 1 or more cleanser baths, and 1 reported no baths; 10 patients’ responses were not available. The 88 patients who had taken at least 1 cleanser bath were divided into 3 groups: 1 bath (35 patients), 2 baths (49 patients), and 3 or more baths (4 patients). Presolution, positive cultures were found for 18 (20%) of the 88 patients; for 7 (20%) of the 35 patients with 1 bath; for 10 (20%) of the 49 patients with 2 baths; and for 1 (25%) of the 4 patients with 3 or more baths. Postsolution, positive cultures were found for 5 (6%) of the 88 patients; for 2 (6%) of the 35 patients with 1 bath; for 3 (6%) of the 49 patients with 2 baths; and for 0 (0%) of the 4 patients with 3 or more baths. The 1 patient with no baths did not have a positive culture. Of the 10 patients whose responses were unavailable, 2 patients had positive presolution cultures and no patients had a positive postsolution culture.
Discussion
The efficacy of using Chloraprep before TKA has not been well assessed in orthopedic practice. However, compared with other preoperative solutions, chlorhexidine has been shown to be significantly better in preventing post-TKA infections.4 Other studies have found it far more effective than other commonly used surgical preparations in eliminating microorganisms in hip arthroplasty and foot surgery.5,7 Our study, focused on the efficacy of Chloraprep in killing bacteria, found the solution effective in removing 85% (17/20) of cultured presolution organisms.
Of the bacterial isolates cultured, normal flora were effectively removed from all associated postsolution cultures. Although most of the bacterial isolates were eliminated after solution application, both coagulase-negative S aureus and rare Bacillus species were found both pre- and postsolution, suggesting either inadequate skin preparation or resistant bacteria.
With respect to the secondary variables, our study data showed that BMI was an important predictor for bacterial isolates, significantly so presolution (P < .03). Mean BMI for the overall study was 35, firmly in the obese category. Only when BMI increased to 38 did it become significant as a predictor for postsolution organisms. Mean postsolution BMI was even higher, 40, which is in the morbidly obese category. Interestingly, the percentage of nonobese patients (BMI, <30) with positive presolution cultures was only 9%, versus the 20% with positive presolution cultures overall. In addition, 1 nonobese patient had positive postsolution cultures.
Other studies have linked higher BMI to higher rates of surgical site infection and other complications, but it is unknown if the infections are due to higher bacterial counts in the patients with high BMI or to other factors, such as reduced wound healing or decreased immune response. More research is needed to determine if the number of organisms in patients with high BMI correlates to a higher risk for surgical site infection.8 As expected, along with BMI (>38), presolution organism isolation was an important predictor for postsolution organism isolation. Patients with presolution organism isolation were 24 times more likely to have postsolution isolates.
Even though diabetic status was not significant for predicting bacterial isolation, patients with diabetes were 3.6 times more likely than patients without diabetes to have a positive culture. Other studies have shown that, compared with patients without diabetes, patients with diabetes had a higher chance of postoperative infection.9,10
In this study, 18 of 20 patients with presolution organism isolates reported they had been compliant in taking the recommended preoperative cleanser baths. This finding may indicate that preoperative cleanser baths are ineffective. However, only 20% of our patients had positive presolution cultures, whereas Ostrander and colleagues5 reported 30% positive pre-preparation cultures from the anterior knee. A recent Cochrane Database System Review did not provide clear evidence of benefit for preoperative showering or bathing with chlorhexidine over other wash products.11 Although their benefit may be questionable, we will continue to recommend preoperative cleanser baths.
One limitation of this study is sample size. Although size was sufficient for determining the efficacy of Chloraprep in the intertriginous area of the back of the knee, the lack of statistical significance (eg, effect of diabetes) may not be accurate. In addition, because the nurse who prepared patients’ skin was aware of the study and was supervised in every case, it is possible that the preparation was done more carefully than usual, resulting in more negative cultures than average. Also, compliance in taking preoperative cleanser baths was subjectively determined. Patients may have reported more baths than were actually taken. Still another study limitation is that 2 postsolution isolates did not have an associated presolution isolate. Although we think this may have resulted from laboratory contamination, it is possible the presolution swabs did not accurately determine true bacterial counts in these cases.
Conclusion
A study that showed significant residual bacteria between patients’ toes after chlorhexidine skin preparation5 left us concerned that Chloraprep skin preparation for TKA might not be adequate. The present study showed that this solution was effective in eliminating bacteria from the intertriginous area of the back of the knee in 95% of patients. Skin preparation appears to be less effective in patients with higher BMI.
Knee arthroplasty continues to be one of the most common and successful methods for treating severe arthritis and other painful arthropathies. Increasing steadily from 1998 to 2008, and with more than 676,000 procedures performed in 2008, knee arthroplasty remains the most common surgical joint replacement procedure.1
Although perioperative and long-term complications are uncommon, infection remains one of the most serious complications of total knee arthroplasty (TKA). Some studies have found a post-TKA infection rate of less than 1%.2 The solution of 2% chlorhexidine gluconate and 70% isopropyl alcohol (Chloraprep; Medi-Flex, Overland Park, Kansas) is commonly used for antiseptic skin preparation before surgery. Studies have shown significant decreases in post-TKA infection rates with preoperative use.3,4 Another study evaluated the efficacy of 3 different skin solutions and found Chloraprep to be the most efficient in eradicating bacteria from the foot and ankle before surgery. The investigators noted that, even with preoperative use of Chloraprep, 23% of patients had residual bacteria on the surface of the skin between the toes.5 Like the foot, the popliteal fossa is an intertriginous area that may harbor normal flora, including gram-positive cocci, in large numbers, mainly because of the contact between 2 skin surfaces. Although postoperative infection rates decrease with use of Chloraprep, its presurgical efficacy in killing bacteria on another intertriginous area, the popliteal fossa, is largely unknown. Also unknown are susceptible organism species and organism population numbers.
Concerned that our skin preparation might be ineffective, we conducted a study to evaluate the efficacy of Chloraprep skin preparation in eradicating organisms before TKA, to isolate the type and number of organisms, and to evaluate several other contributing factors that could lead to infection.
Materials and Methods
This prospective study included 99 patients who were undergoing primary TKA at John Peter Smith Hospital between July 1, 2011 and August 31, 2012. An attempt was made to enroll consecutive TKA patients, and all patients agreed to participate, but a few were not enrolled because the study team had not asked for their consent before they were taken to the operating room. Patients did not receive monetary compensation for participation. Exclusion criteria were pregnancy, imprisonment, and age under 18 years. The study was approved by the institutional review boards at John Peter Smith Hospital and the University of North Texas Health Science Center.
Each lower extremity was prepared with Chloraprep according to the manufacturer’s instructions. Preparation was done by well-trained operating room staff members who were supervised by the surgeon (Dr. Sanchez or Dr. Wagner) but were not involved in the study. With use of the Chloraprep applicator, the solution was applied in a back-and-forth manner to the entire operative leg for at least 30 seconds, and then discarded. This scrub procedure was repeated with a second applicator before standard drapes were placed. The leg was left to air-dry for at least 30 seconds, and the drapes were placed before postsolution swabbing and before the iodine-impregnated adhesive drape was placed around the knee. During drying, the solution was not blotted, wiped away, or touched with instrumentation. Patients were swabbed with an epidermal sterile swab in the popliteal fossa of the knee undergoing surgery, both before solution application (presolution swab) and after (postsolution swab). Only the operating surgeon participated in swabbing the patients. Aerobic and anaerobic swabs were vigorously rubbed over a 2- to 3-in wide area across the entire posterior flexion crease surface.
The collected pre- and postsolution swabs were sent to John Peter Smith Laboratory for identification of organisms. Anaerobic swabs were cultured in thioglycolate broth and on 4 plates: MacConkey agar, Columbia colistin–nalidixic acid agar, chocolate agar, and sheep blood agar. Aerobic swabs were cultured in thioglycolate broth with hemin and vitamin K and on 4 plates: anaerobic blood agar, bile esculin agar, kanamycin and vancomycin agar, and Columbia colistin–nalidixic acid agar. Anaerobic plates were incubated in an anoxic environment. The plates were then read daily, and final reports were issued after 48 hours (for aerobic bacterial isolates) and 72 hours (for anaerobic bacterial isolates), as was the standard at the time.
Additional patient data were collected for possible correlations: American Society of Anesthesiologists (ASA) classification (physical status),6 body mass index (BMI), age, sex, arthroplasty type (unilateral, bilateral), and diabetic status. In addition, patients were asked if they had used Hibiclens antiseptic/antimicrobial skin cleanser daily during the week before surgery—as they had been instructed to do—and the number of times they had used the cleanser.
Study data were analyzed and were used to stratify patients into several groups. Each group had multiple factors evaluated.
Descriptive statistics were used to characterize the patient demographic information. Chi-square analyses were performed to evaluate the difference between presence of organisms before and after solution application, and the data were also layered with reported Hibiclens cleanser use. In addition, binary logistic regression was used to determine if demographic variables could predict presence of organism isolates before and after solution application. Data analyses were conducted using IBM SPSS Statistics Version 20.
Results
No patient had a postoperative infection. Culture isolates grew in 20 (20%) of the 99 patients before solution application and in 5 (5%) of the 99 after application. Of the 20 patients with presolution culture isolates, 16 (80%) had 1 bacterial isolate, and 4 (20%) had 2 or more species. Presolution isolates included normal flora (10, 50%), coagulase-negative Staphylococcus aureus (6, 30%), rare Bacillus (3, 15%), Micrococcus luteus (1, 5%), rare gram-negative (1, 5%), rare gram-positive (1, 5%), and Staphylococcus hominis (1, 5%) (Figure 1). Postsolution isolates included coagulase-negative S aureus (3, 60%), rare Bacillus (1, 20%), and rare Serratia odorifera (1, 20%) (Figure 2). Two postsolution isolates did not have an associated presolution isolate. Presolution organism isolation was an important predictor of postsolution organism isolation (P < .046).
BMI was recorded for all patients. Mean BMI was 35 (range, 20-63). Distribution was as follows: BMI under 20 (3 patients), under 30 (30 patients), under 40 (47 patients), under 50 (14 patients), under 60 (4 patients), and over 60 (1 patient). Mean presolution BMI was significantly (P < .03) higher for patients with bacterial isolates than for patients without isolates (38 and 34, respectively). Mean postsolution BMI was 40 for patients with bacterial isolates and 35 for patients without isolates (Figure 3). Of the 33 patients with BMI under 30, 3 (9%) had presolution isolates and 1 (3%) had postsolution isolates. Of the 66 patients with BMI over 30, 17 (26%) had presolution isolates and 4 (6%) had postsolution isolates (Table).
Of the 99 patients, 30 (30%) had diabetes. Of these 30 patients, 9 (30%) had presolution isolates (45% of all presolution isolates) and 3 (10%) had postsolution isolates (60% of all postsolution isolates.) Although neither pre- nor postsolution results were statistically significant (P = .172) for increasing organism isolation in patients with diabetes, the odds ratio for these patients was 3.6 when the focus was on the likelihood of postsolution organism isolation.
Mean age was 57 years (range, 29-87 years). Results were not statistically significant for age being a likely factor for organism isolate prediction.
There were 81 women and 18 men in the study. Of the 81 women, 16 (20%) had positive presolution cultures and 5 (6%) had positive postsolution cultures. Of the 18 men, 4 (22%) had positive presolution cultures and none had a positive postsolution culture.
Race was recorded. Forty-nine patients were white, 27 black, 18 Hispanic, and 5 unknown. Presolution, 12 whites (24%), 5 blacks (19%), and 3 Hispanics (17%) had positive cultures. Postsolution, 1 white (2%), 1 black (4%), 3 Hispanics (17%), and 1 patient of unknown race (20%) had positive cultures.
ASA classifications were recorded and analyzed. Of the 99 patients, 38 were classified ASA-2, 60 were ASA-3, and 1 was ASA-4. Presolution, 9 (24%) of the 38 ASA-2 patients and 11 (18%) of the 60 ASA-3 patients had positive cultures; postsolution, 2 (5%) of the 38 ASA-2 patients and 3 (5%) of the 60 ASA-3 patients had positive cultures. The 1 ASA-4 patient had neither presolution nor postsolution positive cultures.
Types of TKA (bilateral, unilateral) were recorded. Of the 99 patients, 89 had unilateral TKAs and 10 had bilateral TKAs. Presolution, 19 (21%) of the 89 unilaterals and 1 (10%) of the 10 bilaterals had positive cultures. Postsolution, 5 (6%) of the 89 unilaterals and none of the 10 bilaterals had positive cultures.
Patients were also verbally asked how many cleanser baths they had taken before surgery. Of the 99 patients, 88 reported having taken 1 or more cleanser baths, and 1 reported no baths; 10 patients’ responses were not available. The 88 patients who had taken at least 1 cleanser bath were divided into 3 groups: 1 bath (35 patients), 2 baths (49 patients), and 3 or more baths (4 patients). Presolution, positive cultures were found for 18 (20%) of the 88 patients; for 7 (20%) of the 35 patients with 1 bath; for 10 (20%) of the 49 patients with 2 baths; and for 1 (25%) of the 4 patients with 3 or more baths. Postsolution, positive cultures were found for 5 (6%) of the 88 patients; for 2 (6%) of the 35 patients with 1 bath; for 3 (6%) of the 49 patients with 2 baths; and for 0 (0%) of the 4 patients with 3 or more baths. The 1 patient with no baths did not have a positive culture. Of the 10 patients whose responses were unavailable, 2 patients had positive presolution cultures and no patients had a positive postsolution culture.
Discussion
The efficacy of using Chloraprep before TKA has not been well assessed in orthopedic practice. However, compared with other preoperative solutions, chlorhexidine has been shown to be significantly better in preventing post-TKA infections.4 Other studies have found it far more effective than other commonly used surgical preparations in eliminating microorganisms in hip arthroplasty and foot surgery.5,7 Our study, focused on the efficacy of Chloraprep in killing bacteria, found the solution effective in removing 85% (17/20) of cultured presolution organisms.
Of the bacterial isolates cultured, normal flora were effectively removed from all associated postsolution cultures. Although most of the bacterial isolates were eliminated after solution application, both coagulase-negative S aureus and rare Bacillus species were found both pre- and postsolution, suggesting either inadequate skin preparation or resistant bacteria.
With respect to the secondary variables, our study data showed that BMI was an important predictor for bacterial isolates, significantly so presolution (P < .03). Mean BMI for the overall study was 35, firmly in the obese category. Only when BMI increased to 38 did it become significant as a predictor for postsolution organisms. Mean postsolution BMI was even higher, 40, which is in the morbidly obese category. Interestingly, the percentage of nonobese patients (BMI, <30) with positive presolution cultures was only 9%, versus the 20% with positive presolution cultures overall. In addition, 1 nonobese patient had positive postsolution cultures.
Other studies have linked higher BMI to higher rates of surgical site infection and other complications, but it is unknown if the infections are due to higher bacterial counts in the patients with high BMI or to other factors, such as reduced wound healing or decreased immune response. More research is needed to determine if the number of organisms in patients with high BMI correlates to a higher risk for surgical site infection.8 As expected, along with BMI (>38), presolution organism isolation was an important predictor for postsolution organism isolation. Patients with presolution organism isolation were 24 times more likely to have postsolution isolates.
Even though diabetic status was not significant for predicting bacterial isolation, patients with diabetes were 3.6 times more likely than patients without diabetes to have a positive culture. Other studies have shown that, compared with patients without diabetes, patients with diabetes had a higher chance of postoperative infection.9,10
In this study, 18 of 20 patients with presolution organism isolates reported they had been compliant in taking the recommended preoperative cleanser baths. This finding may indicate that preoperative cleanser baths are ineffective. However, only 20% of our patients had positive presolution cultures, whereas Ostrander and colleagues5 reported 30% positive pre-preparation cultures from the anterior knee. A recent Cochrane Database System Review did not provide clear evidence of benefit for preoperative showering or bathing with chlorhexidine over other wash products.11 Although their benefit may be questionable, we will continue to recommend preoperative cleanser baths.
One limitation of this study is sample size. Although size was sufficient for determining the efficacy of Chloraprep in the intertriginous area of the back of the knee, the lack of statistical significance (eg, effect of diabetes) may not be accurate. In addition, because the nurse who prepared patients’ skin was aware of the study and was supervised in every case, it is possible that the preparation was done more carefully than usual, resulting in more negative cultures than average. Also, compliance in taking preoperative cleanser baths was subjectively determined. Patients may have reported more baths than were actually taken. Still another study limitation is that 2 postsolution isolates did not have an associated presolution isolate. Although we think this may have resulted from laboratory contamination, it is possible the presolution swabs did not accurately determine true bacterial counts in these cases.
Conclusion
A study that showed significant residual bacteria between patients’ toes after chlorhexidine skin preparation5 left us concerned that Chloraprep skin preparation for TKA might not be adequate. The present study showed that this solution was effective in eliminating bacteria from the intertriginous area of the back of the knee in 95% of patients. Skin preparation appears to be less effective in patients with higher BMI.
1. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201-207.
2. Poultsides LA, Ma Y, Della Valle AG, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty—incidence and risk factors. J Arthroplasty. 2013;28(3):385-389.
3. Johnson AJ, Kapadia BH, Daley JA, Molina CB, Mont MA. Chlorhexidine reduces infections in knee arthroplasty. J Knee Surg. 2013;26(3):213-218.
4. Zywiel MG, Daley JA, Delanois RE, Naziri Q, Johnson AJ, Mont MA. Advance pre-operative chlorhexidine reduces the incidence of surgical site infections in knee arthroplasty. Int Orthop. 2011;35(7):1001-1006.
5. Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg Am. 2005;87(5):980-985.
6. Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217-222.
7. Johnson AJ, Daley JA, Zywiel MG, Delanois RE, Mont MA. Preoperative chlorhexidine preparation and the incidence of surgical site infections after hip arthroplasty. J Arthroplasty. 2010;25(6 suppl):98-102.
8. Samson AJ, Mercer GE, Campbell DG. Total knee replacement in the morbidly obese: a literature review. ANZ J Surg. 2010;80(9):595-599.
9. Iorio R, Williams KM, Marcantonio AJ, Specht LM, Tilzey JF, Healy WL. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty. 2012;27(5):726-729.
10. Viens NA, Hug KT, Marchant MH, Cook C, Vail TP, Bolognesi MP. Role of diabetes type in perioperative outcomes after hip and knee arthroplasty in the United States. J Surg Orthop Adv. 2012;21(4):253-260.
11. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.
1. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201-207.
2. Poultsides LA, Ma Y, Della Valle AG, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty—incidence and risk factors. J Arthroplasty. 2013;28(3):385-389.
3. Johnson AJ, Kapadia BH, Daley JA, Molina CB, Mont MA. Chlorhexidine reduces infections in knee arthroplasty. J Knee Surg. 2013;26(3):213-218.
4. Zywiel MG, Daley JA, Delanois RE, Naziri Q, Johnson AJ, Mont MA. Advance pre-operative chlorhexidine reduces the incidence of surgical site infections in knee arthroplasty. Int Orthop. 2011;35(7):1001-1006.
5. Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg Am. 2005;87(5):980-985.
6. Wolters U, Wolf T, Stützer H, Schröder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217-222.
7. Johnson AJ, Daley JA, Zywiel MG, Delanois RE, Mont MA. Preoperative chlorhexidine preparation and the incidence of surgical site infections after hip arthroplasty. J Arthroplasty. 2010;25(6 suppl):98-102.
8. Samson AJ, Mercer GE, Campbell DG. Total knee replacement in the morbidly obese: a literature review. ANZ J Surg. 2010;80(9):595-599.
9. Iorio R, Williams KM, Marcantonio AJ, Specht LM, Tilzey JF, Healy WL. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty. 2012;27(5):726-729.
10. Viens NA, Hug KT, Marchant MH, Cook C, Vail TP, Bolognesi MP. Role of diabetes type in perioperative outcomes after hip and knee arthroplasty in the United States. J Surg Orthop Adv. 2012;21(4):253-260.
11. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.