User login
Unstable Dorsal Proximal Interphalangeal Joint Fracture-Dislocations Treated With Extension-Block Pinning
The proximal interphalangeal (PIP) joint plays a crucial role in hand function, accounting for an estimated 85% of the motion required to grasp an object.1 The anatomy and biomechanics of the PIP joint, however, make it particularly prone to injury.2,3 Dorsal PIP fracture-dislocations represent a subset of PIP injuries that often require surgical intervention.2 The stability of these fracture-dislocations largely depends on the extent of articular involvement of the base of the middle phalanx. Fractures that involve less than 30% of the joint surface typically remain stable after reduction.2,4,5 In cases in which involvement ranges from 30% to 50%, PIP joint stability is more tenuous, and more joint flexion is required to maintain concentric reduction. Fractures that involve more than 50% of the articular surface are unstable and require operative intervention.2,5,6 Fractures that require more than 30° of flexion for reduction maintenance are generally considered unstable and may benefit from surgical intervention.2
The goals of treatment for this injury are to restore a stable, concentrically reduced joint and initiate early joint mobilization to prevent stiffness, pain, recurrent instability, and posttraumatic arthritis.3,7 Numerous surgical interventions for unstable PIP fracture-dislocations have been proposed, including open reduction and internal fixation (ORIF),8-10 extension-block pinning (EBP),11-13 dynamic external fixation,14-17 volar plate arthroplasty,18,19 and hemi-hamate resurfacing arthroplasty.20,21 Many of these techniques can be technically demanding and may require prolonged immobilization. EBP can be performed easily and efficiently and allows for early joint motion.
Extension-block pinning—placing a Kirschner wire (K-wire) into the head of the proximal phalanx at an angle that blocks PIP extension and prevents joint subluxation—was first described by Sugawa and colleagues12 in 1979. In a study by Inoue and Tamura,11 patients treated with EBP had a mean PIP range of motion (ROM) of 94° at a mean follow-up of 14 months. In a series of 3 case reports, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM in patients treated with EBP.
We conducted a study to expand on previous research on pain, function, and satisfaction outcomes in addition to ROM. We hypothesized that percutaneous EBP is an effective treatment for unstable dorsal PIP fracture-dislocations and has efficacy similar to that of more complex and technically demanding methods of treatment.
Materials and Methods
We retrospectively reviewed patient charts to identify candidates for this study. Inclusion criteria were unstable dorsal PIP fracture-dislocations treated with EBP and minimum 4-month follow-up. (Fracture-dislocations were deemed unstable if they involved at least 30% of the articular surface or required more than 30° of flexion for reduction maintenance.) Exclusion criteria were open injury, neurovascular or tendon injury, or any prior injury to the PIP joint.
Twelve patients (5 females, 7 males) treated over a 4-year period (2002–2006) met the inclusion criteria. Mean age was 30 years (range, 15-64 years). Each surgery was performed by Dr. Hagberg or Dr. Balk. Half the cases involved the dominant hand. Two small fingers, 4 ring fingers, 2 long fingers, and 4 index fingers were injured. The injuries were sustained in an all-terrain vehicle accident (n = 1), in falls (n = 2), while swimming (n = 1), or while playing softball (n = 3), football (n = 4), or soccer (n = 1). Mean time from injury to surgery was 7.5 days (range, 4-27 days). Extent of articular surface involvement of the base of the fractured middle phalanx was calculated using preoperatively obtained lateral radiographs.
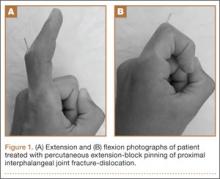
Surgical intervention was performed in a reproducible fashion. All patients were treated with closed reduction of the PIP joint under fluoroscopic guidance. Before pinning, joint stability was assessed fluoroscopically both at rest and through an arc of motion. A single smooth 0.045-in K-wire was then inserted percutaneously into the distal and dorsal aspects of the proximal phalanx in retrograde fashion (Figure 1). During wire insertion, the distal interphalangeal joint was flexed to relax the intrinsic mechanism, and the central slip tendon was pierced just proximal to its insertion. We have not noted significant adhesion formation about the central slip with this technique, likely because of limited tendon excursion in this location. Stable joint reduction was confirmed with fluoroscopy. No attempt was made to reduce the intra-articular fracture at the base of the middle phalanx.
A therapy program was initiated 2 to 9 days after surgery. At the first postoperative visit, patients were allowed to perform active ROM (AROM) with the pin in place (Figure 1). K-wires were removed a mean of 25 days (range, 17-31 days) after surgery. A static dorsal block splint was then applied, and patients were encouraged to remove it several times per day for AROM between 20° and full flexion until 6 weeks after surgery. At that time, formal occupational therapy was commenced for another 6 weeks. If there was residual flexion contracture of the PIP joint, dynamic extension splinting was initiated after fracture consolidation.
Mean follow-up was 35.5 months (range, 4-94 months). Postoperative anteroposterior and lateral radiographs were used to evaluate maintenance of joint congruity, fracture union, remodeling, and evidence of degenerative changes. At final follow-up, grip strength of injured and contralateral hands was measured with a dynamometer (Jamar; Patterson Medical, Warrenville, Illinois). AROM and passive ROM (PROM) of the PIP joint was documented at follow-up visits. In addition, patients rated their pain on a 0-to-10 visual analog scale (VAS), with 0 representing no pain and 10 representing excruciating pain. Patients also completed a questionnaire assessing satisfaction with surgical outcome. Physical function and disability were assessed with the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire. Any complications, including the need for further surgeries, were documented. Pearson correlation coefficients and Student t tests (with significance set at P < .05) were used to compare outcomes.
Results
Radiographic reduction of joint dislocation was achieved and maintained in 11 of the 12 patients at a mean follow-up of 35.5 months (range, 4-94 months). Extent of joint surface involvement, based on preoperative lateral radiographs, averaged 43% (range, 25%-75%). Although no direct articular reduction was performed, remodeling of the joint surface was consistently noted at follow-up (Figure 2). Mild radiographic degenerative changes were noted at final follow-up in 4 patients, and moderate changes were noted in 1 patient. Radiographic union was achieved in all cases, and no pin-tract infections were noted.
Mean AROM of the PIP joint at final follow-up was 84° (range, 50°-110°), with patients lacking a mean of 7° of full extension and achieving mean flexion of 91°. Mean PROM was 93° (range, 75°-110°). There was no correlation between extent of articular surface involvement and ROM. Furthermore, no correlation was found between time from injury to surgery and ROM. Patients regained full grip strength in the operative hand. At final follow-up, mean grip strength was 79.4 pounds in the operative hand and 79.6 pounds in the contralateral hand, demonstrating equal grip strengths bilaterally.
Patients overall had very low levels of pain; mean VAS score was 0.64 (range, 0-3). Mean QuickDASH score was 5.7 (range, 0-30), suggesting minimal functional impairment. One patient developed a malunion of the middle phalanx fracture resulting in a rotational deformity and required corrective osteotomy. This patient’s VAS score (3) and QuickDASH score (30) were significantly higher than those of the other patients in the study. No other complications were noted by final follow-up.
A higher level of patient satisfaction was found to be directly related to length of follow-up (P < .05). Satisfaction was inversely related to higher VAS score (P < .05) and higher QuickDASH score (P < .001). Pain at work correlated with lower satisfaction level (P < .05). There was no correlation between patient satisfaction and AROM or PROM.
Discussion
The results of this study demonstrate the efficacy of EBP in the treatment of dorsal PIP joint fracture-dislocations. EBP maintained joint dislocation reduction and allowed for early mobilization, which resulted in good ROM, minimal pain, and good functional outcomes. Of note, postoperative patient satisfaction correlated with pain but not with ROM. It is possible that EBP yielded sufficient functional ROM in all patients such that improvement beyond this threshold did not lead to further improvement in satisfaction. Hume and colleagues23 found that mean PIP joint flexion of 60° is needed for activities of daily living. As mean PIP active flexion was 91° (range, 70°-105°) in the present study, it is possible that satisfaction did not correlate with ROM, as all 12 patients achieved active flexion of more than 60°. Despite the lack of correlation between ROM and satisfaction, early PIP joint mobilization is likely a key contributor to positive outcomes because of its significant role in cartilage healing.24
Postoperative ROM in the present study is consistent with that in other reports of patients with PIP joint fracture-dislocations treated with EBP.11,12,22 In a study by Inoue and Tamura,11 14 such patients had mean PIP ROM of 94° at a mean follow-up of 14 months. Viegas22 followed a series of 3 patients for a mean of 7 weeks. At final follow-up, their mean PIP arc of motion was 71°; they lacked 12° of full extension and achieved 83° of flexion. The larger PIP arc of motion (84°) found in the present study may be due to our significantly longer follow-up (35 months). Unlike us, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM. Our finding a lack of correlation may be a result of the significant amount of joint remodeling noted on follow-up radiographs.
Studies of transarticular pinning of PIP joints after dorsal PIP fracture-dislocations have reported outcomes similar to ours.25,26 Newington and colleagues25 evaluated 10 cases of transarticular pinning of the PIP joint and found mean arc of motion of 85° and equal grip strengths between injured and contralateral hands. In a series of 19 patients with PIP fracture-dislocations, Aladin and Davis26 noted similar outcomes of transarticular K-wire fixation and ORIF. In both of their treatment groups, however, there was evidence of PIP joint incongruity and subluxation. Of note, PIP arc motion was lower in their study than in ours.
Recent studies have evaluated unstable PIP fracture-dislocations treated with both EBP and percutaneous reduction and pinning with a second K-wire.13,27 At a mean follow-up of 18 months, Vitale and colleagues13 noted maintenance of concentric fracture reduction, good PIP ROM (mean range, 4°-93°), and low VAS and DASH scores (1.4 and 8, respectively). Waris and Alanen27 noted mean PIP AROM of 83° and low VAS and DASH scores (1 and 4, respectively). The EBP technique used in the present study did not involve percutaneous fracture reduction but achieved equally good ROM and VAS and QuickDASH scores.
Clinical outcomes of EBP of PIP joint fracture-dislocations are also comparable to outcomes of more complex treatment methods.8-10,15-19,21,26,28-33 Dynamic distraction external fixation has led to equally good ROM (mean AROM, 80°-85°15,16) and VAS scores, but with a higher incidence of pin-site infection.14-17 ORIF of the intra-articular middle phalanx fracture has the advantage of obtaining a direct anatomical reduction, but clinical outcomes are similar to those in the present study (mean AROM, 70°; 78% pain-free9), and flexion contractures have been noted.8-10 Furthermore, reduction of the fractured PIP joint articular surface has not been shown to be necessary for good outcomes.16,34 This may be explained in part by PIP joint remodeling, which has been routinely observed on long-term follow-up by the senior authors of the present study. Hemi-hamate autografting and volar plate arthroplasty are other options that have had promising results in the treatment of acute and chronic unstable PIP fracture-dislocations.18-21 However, the postoperative ROM (mean AROM, 61°-85°18,21), VAS scores, and patient satisfaction (91% very satisfied21) of these operations are similar to those of EBP in the present study and may not justify the longer operative times and technical challenges associated with these techniques.
We believe that our study group’s 1 complication, a malunion that was treated with corrective osteotomy, resulted from lack of appreciation of the degree of injury. The teenaged female patient’s index finger PIP joint had a rotational malalignment that was not appreciated before or during surgery. After pinning and after ROM was restored, the index finger was observed crossing over the middle finger with digital flexion. The patient returned to the operating room for corrective osteotomy.
We recommend that surgeons assess alignment carefully, before and during surgery, when considering this technique. Although complications are rare, the technique is not for patients with rotational malalignment; ORIF may be more suitable in these cases. In addition, though EBP may be appropriate for pilon-type injuries, as it allows for early AROM, our procedure of choice for pilon fracture is dynamic external fixation, which in addition to allowing for AROM provides ligamentotaxis. In the event that a large volar articular fragment extends into the middle phalanx diaphysis, we typically proceed with ORIF through a volar shotgun approach. At our institution, injuries lasting more than 3 months are often treated with volar plate arthroplasty or hemi-hamate resurfacing. Finally, we believe that caution should be exercised when using this technique in patients with more than 50% articular involvement. In the present study, though we used this treatment in cases of up to 75% surface involvement, alternative techniques, such as hemi-hamate resurfacing arthroplasty, may provide a better volar bony buttress and limit the risk for recurrent instability. Despite its relative contraindications, our technique has been appropriate for more than 90% of the acute PIP fracture-dislocations we have seen.
This study expands on prior research by demonstrating good function, satisfaction, and pain outcomes of percutaneous EBP in the treatment of unstable dorsal PIP fracture-dislocations. In addition, this study demonstrated that the efficacy of EBP is similar to that of more complex and technically demanding methods of treatment. Our technique has the advantage of simplicity. It obviates the soft-tissue damage required for ORIF and more complex fixation techniques. Furthermore, use of this simple technique may save time and costs and lead to more reproducible outcomes.
One limitation of this study is its small sample size. It is possible that outcomes may have been different with a larger sample. Furthermore, we did not make a direct comparison with other treatment methods. To better determine the optimal treatment method for this fracture type, future studies should prospectively evaluate outcomes for multiple treatment modalities in a randomized fashion.
1. Leibovic SJ, Bowers WH. Anatomy of the proximal interphalangeal joint. Hand Clin. 1994;10(2):169-178.
2. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368-380.
3. Ng CY, Oliver CW. Fractures of the proximal interphalangeal joints of the fingers. J Bone Joint Surg Br. 2009;91(6):705-712.
4. Isani A. Small joint injuries requiring surgical treatment. Orthop Clin North Am. 1986;17(3):407-419.
5. McElfresh EC, Dobyns JH, O’Brien ET. Management of fracture-dislocation of the proximal interphalangeal joints by extension-block splinting. J Bone Joint Surg Am. 1972;54(8):1705-1711.
6. Hastings H 2nd, Carroll C 4th. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4(3):503-527.
7. O’Rourke SK, Gaur S, Barton NJ. Long-term outcome of articular fractures of the phalanges: an eleven year follow up. J Hand Surg Br. 1989;14(2):183-193.
8. Grant I, Berger AC, Tham SK. Internal fixation of unstable fracture dislocations of the proximal interphalangeal joint. J Hand Surg Br. 2005;30(5):492-498.
9. Hamilton SC, Stern PJ, Fassler PR, Kiefhaber TR. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31(8):1349-1354.
10. Lee JY, Teoh LC. Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: indications, approaches and results. J Hand Surg Br. 2006;31(2):138-146.
11. Inoue G, Tamura Y. Treatment of fracture-dislocation of the proximal interphalangeal joint using extension-block Kirschner wire. Ann Chir Main Memb Super. 1991;10(6):564-568.
12. Sugawa I, Otani K, Kobayashi A. Treatment of fracture dislocation PIP-joint by Kirschner wire extension block method. Cent Jpn J Orthop Traumat. 1979;22:1409-1412.
13. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011;36(9):1453-1459.
14. Badia A, Riano F, Ravikoff J, Khouri R, Gonzalez-Hernandez E, Orbay JL. Dynamic intradigital external fixation for proximal interphalangeal joint fracture dislocations. J Hand Surg Am. 2005;30(1):154-160.
15. Ellis SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: a pins and rubber band system. J Hand Surg Am. 2007;32(8):1242-1250.
16. Morgan JP, Gordon DA, Klug MS, Perry PE, Barre PS. Dynamic digital traction for unstable comminuted intra-articular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1995;20(4):565-573.
17. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19-25.
18. Dionysian E, Eaton RG. The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg Am. 2000;25(3):429-437.
19. Durham-Smith G, McCarten GM. Volar plate arthroplasty for closed proximal interphalangeal joint injuries. J Hand Surg Br. 1992;17(4):422-428.
20. Calfee RP, Kiefhaber TR, Sommerkamp TG, Stern PJ. Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2009;34(7):1232-1241.
21. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856-865.
22. Viegas SF. Extension block pinning for proximal interphalangeal joint fracture dislocations: preliminary report of a new technique. J Hand Surg Am. 1992;17(5):896-901.
23. Hume MC, Gellman H, McKellop H, Brumfield RH Jr. Functional range of motion of the joints of the hand. J Hand Surg Am. 1990;15(2):240-243.
24. Salter RB. The physiologic basis of continuous passive motion for articular cartilage healing and regeneration. Hand Clin. 1994;10(2):211-220.
25. Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537-540.
26. Aladin A, Davis TR. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30(2):120-128.
27. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010;35(12):2046-2052.
28. Bain GI, Mehta JA, Heptinstall RJ, Bria M. Dynamic external fixation for injuries of the proximal interphalangeal joint. J Bone Joint Surg Br. 1998;80(6):1014-1019.
29. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5(3):260-268.
30. Green A, Smith J, Redding M, Akelman E. Acute open reduction and rigid internal fixation of proximal interphalangeal joint fracture dislocation. J Hand Surg Am. 1992;17(3):512-517.
31. Inanami H, Ninomiya S, Okutsu I, Tarui T. Dynamic external finger fixator for fracture dislocation of the proximal interphalangeal joint. J Hand Surg Am. 1993;18(1):160-164.
32. Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19(1):98-107.
33. Weiss AP. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop. 1996;(327):21-28.
34. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop. 1987;(214):101-112.
The proximal interphalangeal (PIP) joint plays a crucial role in hand function, accounting for an estimated 85% of the motion required to grasp an object.1 The anatomy and biomechanics of the PIP joint, however, make it particularly prone to injury.2,3 Dorsal PIP fracture-dislocations represent a subset of PIP injuries that often require surgical intervention.2 The stability of these fracture-dislocations largely depends on the extent of articular involvement of the base of the middle phalanx. Fractures that involve less than 30% of the joint surface typically remain stable after reduction.2,4,5 In cases in which involvement ranges from 30% to 50%, PIP joint stability is more tenuous, and more joint flexion is required to maintain concentric reduction. Fractures that involve more than 50% of the articular surface are unstable and require operative intervention.2,5,6 Fractures that require more than 30° of flexion for reduction maintenance are generally considered unstable and may benefit from surgical intervention.2
The goals of treatment for this injury are to restore a stable, concentrically reduced joint and initiate early joint mobilization to prevent stiffness, pain, recurrent instability, and posttraumatic arthritis.3,7 Numerous surgical interventions for unstable PIP fracture-dislocations have been proposed, including open reduction and internal fixation (ORIF),8-10 extension-block pinning (EBP),11-13 dynamic external fixation,14-17 volar plate arthroplasty,18,19 and hemi-hamate resurfacing arthroplasty.20,21 Many of these techniques can be technically demanding and may require prolonged immobilization. EBP can be performed easily and efficiently and allows for early joint motion.
Extension-block pinning—placing a Kirschner wire (K-wire) into the head of the proximal phalanx at an angle that blocks PIP extension and prevents joint subluxation—was first described by Sugawa and colleagues12 in 1979. In a study by Inoue and Tamura,11 patients treated with EBP had a mean PIP range of motion (ROM) of 94° at a mean follow-up of 14 months. In a series of 3 case reports, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM in patients treated with EBP.
We conducted a study to expand on previous research on pain, function, and satisfaction outcomes in addition to ROM. We hypothesized that percutaneous EBP is an effective treatment for unstable dorsal PIP fracture-dislocations and has efficacy similar to that of more complex and technically demanding methods of treatment.
Materials and Methods
We retrospectively reviewed patient charts to identify candidates for this study. Inclusion criteria were unstable dorsal PIP fracture-dislocations treated with EBP and minimum 4-month follow-up. (Fracture-dislocations were deemed unstable if they involved at least 30% of the articular surface or required more than 30° of flexion for reduction maintenance.) Exclusion criteria were open injury, neurovascular or tendon injury, or any prior injury to the PIP joint.
Twelve patients (5 females, 7 males) treated over a 4-year period (2002–2006) met the inclusion criteria. Mean age was 30 years (range, 15-64 years). Each surgery was performed by Dr. Hagberg or Dr. Balk. Half the cases involved the dominant hand. Two small fingers, 4 ring fingers, 2 long fingers, and 4 index fingers were injured. The injuries were sustained in an all-terrain vehicle accident (n = 1), in falls (n = 2), while swimming (n = 1), or while playing softball (n = 3), football (n = 4), or soccer (n = 1). Mean time from injury to surgery was 7.5 days (range, 4-27 days). Extent of articular surface involvement of the base of the fractured middle phalanx was calculated using preoperatively obtained lateral radiographs.
Surgical intervention was performed in a reproducible fashion. All patients were treated with closed reduction of the PIP joint under fluoroscopic guidance. Before pinning, joint stability was assessed fluoroscopically both at rest and through an arc of motion. A single smooth 0.045-in K-wire was then inserted percutaneously into the distal and dorsal aspects of the proximal phalanx in retrograde fashion (Figure 1). During wire insertion, the distal interphalangeal joint was flexed to relax the intrinsic mechanism, and the central slip tendon was pierced just proximal to its insertion. We have not noted significant adhesion formation about the central slip with this technique, likely because of limited tendon excursion in this location. Stable joint reduction was confirmed with fluoroscopy. No attempt was made to reduce the intra-articular fracture at the base of the middle phalanx.
A therapy program was initiated 2 to 9 days after surgery. At the first postoperative visit, patients were allowed to perform active ROM (AROM) with the pin in place (Figure 1). K-wires were removed a mean of 25 days (range, 17-31 days) after surgery. A static dorsal block splint was then applied, and patients were encouraged to remove it several times per day for AROM between 20° and full flexion until 6 weeks after surgery. At that time, formal occupational therapy was commenced for another 6 weeks. If there was residual flexion contracture of the PIP joint, dynamic extension splinting was initiated after fracture consolidation.
Mean follow-up was 35.5 months (range, 4-94 months). Postoperative anteroposterior and lateral radiographs were used to evaluate maintenance of joint congruity, fracture union, remodeling, and evidence of degenerative changes. At final follow-up, grip strength of injured and contralateral hands was measured with a dynamometer (Jamar; Patterson Medical, Warrenville, Illinois). AROM and passive ROM (PROM) of the PIP joint was documented at follow-up visits. In addition, patients rated their pain on a 0-to-10 visual analog scale (VAS), with 0 representing no pain and 10 representing excruciating pain. Patients also completed a questionnaire assessing satisfaction with surgical outcome. Physical function and disability were assessed with the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire. Any complications, including the need for further surgeries, were documented. Pearson correlation coefficients and Student t tests (with significance set at P < .05) were used to compare outcomes.
Results
Radiographic reduction of joint dislocation was achieved and maintained in 11 of the 12 patients at a mean follow-up of 35.5 months (range, 4-94 months). Extent of joint surface involvement, based on preoperative lateral radiographs, averaged 43% (range, 25%-75%). Although no direct articular reduction was performed, remodeling of the joint surface was consistently noted at follow-up (Figure 2). Mild radiographic degenerative changes were noted at final follow-up in 4 patients, and moderate changes were noted in 1 patient. Radiographic union was achieved in all cases, and no pin-tract infections were noted.
Mean AROM of the PIP joint at final follow-up was 84° (range, 50°-110°), with patients lacking a mean of 7° of full extension and achieving mean flexion of 91°. Mean PROM was 93° (range, 75°-110°). There was no correlation between extent of articular surface involvement and ROM. Furthermore, no correlation was found between time from injury to surgery and ROM. Patients regained full grip strength in the operative hand. At final follow-up, mean grip strength was 79.4 pounds in the operative hand and 79.6 pounds in the contralateral hand, demonstrating equal grip strengths bilaterally.
Patients overall had very low levels of pain; mean VAS score was 0.64 (range, 0-3). Mean QuickDASH score was 5.7 (range, 0-30), suggesting minimal functional impairment. One patient developed a malunion of the middle phalanx fracture resulting in a rotational deformity and required corrective osteotomy. This patient’s VAS score (3) and QuickDASH score (30) were significantly higher than those of the other patients in the study. No other complications were noted by final follow-up.
A higher level of patient satisfaction was found to be directly related to length of follow-up (P < .05). Satisfaction was inversely related to higher VAS score (P < .05) and higher QuickDASH score (P < .001). Pain at work correlated with lower satisfaction level (P < .05). There was no correlation between patient satisfaction and AROM or PROM.
Discussion
The results of this study demonstrate the efficacy of EBP in the treatment of dorsal PIP joint fracture-dislocations. EBP maintained joint dislocation reduction and allowed for early mobilization, which resulted in good ROM, minimal pain, and good functional outcomes. Of note, postoperative patient satisfaction correlated with pain but not with ROM. It is possible that EBP yielded sufficient functional ROM in all patients such that improvement beyond this threshold did not lead to further improvement in satisfaction. Hume and colleagues23 found that mean PIP joint flexion of 60° is needed for activities of daily living. As mean PIP active flexion was 91° (range, 70°-105°) in the present study, it is possible that satisfaction did not correlate with ROM, as all 12 patients achieved active flexion of more than 60°. Despite the lack of correlation between ROM and satisfaction, early PIP joint mobilization is likely a key contributor to positive outcomes because of its significant role in cartilage healing.24
Postoperative ROM in the present study is consistent with that in other reports of patients with PIP joint fracture-dislocations treated with EBP.11,12,22 In a study by Inoue and Tamura,11 14 such patients had mean PIP ROM of 94° at a mean follow-up of 14 months. Viegas22 followed a series of 3 patients for a mean of 7 weeks. At final follow-up, their mean PIP arc of motion was 71°; they lacked 12° of full extension and achieved 83° of flexion. The larger PIP arc of motion (84°) found in the present study may be due to our significantly longer follow-up (35 months). Unlike us, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM. Our finding a lack of correlation may be a result of the significant amount of joint remodeling noted on follow-up radiographs.
Studies of transarticular pinning of PIP joints after dorsal PIP fracture-dislocations have reported outcomes similar to ours.25,26 Newington and colleagues25 evaluated 10 cases of transarticular pinning of the PIP joint and found mean arc of motion of 85° and equal grip strengths between injured and contralateral hands. In a series of 19 patients with PIP fracture-dislocations, Aladin and Davis26 noted similar outcomes of transarticular K-wire fixation and ORIF. In both of their treatment groups, however, there was evidence of PIP joint incongruity and subluxation. Of note, PIP arc motion was lower in their study than in ours.
Recent studies have evaluated unstable PIP fracture-dislocations treated with both EBP and percutaneous reduction and pinning with a second K-wire.13,27 At a mean follow-up of 18 months, Vitale and colleagues13 noted maintenance of concentric fracture reduction, good PIP ROM (mean range, 4°-93°), and low VAS and DASH scores (1.4 and 8, respectively). Waris and Alanen27 noted mean PIP AROM of 83° and low VAS and DASH scores (1 and 4, respectively). The EBP technique used in the present study did not involve percutaneous fracture reduction but achieved equally good ROM and VAS and QuickDASH scores.
Clinical outcomes of EBP of PIP joint fracture-dislocations are also comparable to outcomes of more complex treatment methods.8-10,15-19,21,26,28-33 Dynamic distraction external fixation has led to equally good ROM (mean AROM, 80°-85°15,16) and VAS scores, but with a higher incidence of pin-site infection.14-17 ORIF of the intra-articular middle phalanx fracture has the advantage of obtaining a direct anatomical reduction, but clinical outcomes are similar to those in the present study (mean AROM, 70°; 78% pain-free9), and flexion contractures have been noted.8-10 Furthermore, reduction of the fractured PIP joint articular surface has not been shown to be necessary for good outcomes.16,34 This may be explained in part by PIP joint remodeling, which has been routinely observed on long-term follow-up by the senior authors of the present study. Hemi-hamate autografting and volar plate arthroplasty are other options that have had promising results in the treatment of acute and chronic unstable PIP fracture-dislocations.18-21 However, the postoperative ROM (mean AROM, 61°-85°18,21), VAS scores, and patient satisfaction (91% very satisfied21) of these operations are similar to those of EBP in the present study and may not justify the longer operative times and technical challenges associated with these techniques.
We believe that our study group’s 1 complication, a malunion that was treated with corrective osteotomy, resulted from lack of appreciation of the degree of injury. The teenaged female patient’s index finger PIP joint had a rotational malalignment that was not appreciated before or during surgery. After pinning and after ROM was restored, the index finger was observed crossing over the middle finger with digital flexion. The patient returned to the operating room for corrective osteotomy.
We recommend that surgeons assess alignment carefully, before and during surgery, when considering this technique. Although complications are rare, the technique is not for patients with rotational malalignment; ORIF may be more suitable in these cases. In addition, though EBP may be appropriate for pilon-type injuries, as it allows for early AROM, our procedure of choice for pilon fracture is dynamic external fixation, which in addition to allowing for AROM provides ligamentotaxis. In the event that a large volar articular fragment extends into the middle phalanx diaphysis, we typically proceed with ORIF through a volar shotgun approach. At our institution, injuries lasting more than 3 months are often treated with volar plate arthroplasty or hemi-hamate resurfacing. Finally, we believe that caution should be exercised when using this technique in patients with more than 50% articular involvement. In the present study, though we used this treatment in cases of up to 75% surface involvement, alternative techniques, such as hemi-hamate resurfacing arthroplasty, may provide a better volar bony buttress and limit the risk for recurrent instability. Despite its relative contraindications, our technique has been appropriate for more than 90% of the acute PIP fracture-dislocations we have seen.
This study expands on prior research by demonstrating good function, satisfaction, and pain outcomes of percutaneous EBP in the treatment of unstable dorsal PIP fracture-dislocations. In addition, this study demonstrated that the efficacy of EBP is similar to that of more complex and technically demanding methods of treatment. Our technique has the advantage of simplicity. It obviates the soft-tissue damage required for ORIF and more complex fixation techniques. Furthermore, use of this simple technique may save time and costs and lead to more reproducible outcomes.
One limitation of this study is its small sample size. It is possible that outcomes may have been different with a larger sample. Furthermore, we did not make a direct comparison with other treatment methods. To better determine the optimal treatment method for this fracture type, future studies should prospectively evaluate outcomes for multiple treatment modalities in a randomized fashion.
The proximal interphalangeal (PIP) joint plays a crucial role in hand function, accounting for an estimated 85% of the motion required to grasp an object.1 The anatomy and biomechanics of the PIP joint, however, make it particularly prone to injury.2,3 Dorsal PIP fracture-dislocations represent a subset of PIP injuries that often require surgical intervention.2 The stability of these fracture-dislocations largely depends on the extent of articular involvement of the base of the middle phalanx. Fractures that involve less than 30% of the joint surface typically remain stable after reduction.2,4,5 In cases in which involvement ranges from 30% to 50%, PIP joint stability is more tenuous, and more joint flexion is required to maintain concentric reduction. Fractures that involve more than 50% of the articular surface are unstable and require operative intervention.2,5,6 Fractures that require more than 30° of flexion for reduction maintenance are generally considered unstable and may benefit from surgical intervention.2
The goals of treatment for this injury are to restore a stable, concentrically reduced joint and initiate early joint mobilization to prevent stiffness, pain, recurrent instability, and posttraumatic arthritis.3,7 Numerous surgical interventions for unstable PIP fracture-dislocations have been proposed, including open reduction and internal fixation (ORIF),8-10 extension-block pinning (EBP),11-13 dynamic external fixation,14-17 volar plate arthroplasty,18,19 and hemi-hamate resurfacing arthroplasty.20,21 Many of these techniques can be technically demanding and may require prolonged immobilization. EBP can be performed easily and efficiently and allows for early joint motion.
Extension-block pinning—placing a Kirschner wire (K-wire) into the head of the proximal phalanx at an angle that blocks PIP extension and prevents joint subluxation—was first described by Sugawa and colleagues12 in 1979. In a study by Inoue and Tamura,11 patients treated with EBP had a mean PIP range of motion (ROM) of 94° at a mean follow-up of 14 months. In a series of 3 case reports, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM in patients treated with EBP.
We conducted a study to expand on previous research on pain, function, and satisfaction outcomes in addition to ROM. We hypothesized that percutaneous EBP is an effective treatment for unstable dorsal PIP fracture-dislocations and has efficacy similar to that of more complex and technically demanding methods of treatment.
Materials and Methods
We retrospectively reviewed patient charts to identify candidates for this study. Inclusion criteria were unstable dorsal PIP fracture-dislocations treated with EBP and minimum 4-month follow-up. (Fracture-dislocations were deemed unstable if they involved at least 30% of the articular surface or required more than 30° of flexion for reduction maintenance.) Exclusion criteria were open injury, neurovascular or tendon injury, or any prior injury to the PIP joint.
Twelve patients (5 females, 7 males) treated over a 4-year period (2002–2006) met the inclusion criteria. Mean age was 30 years (range, 15-64 years). Each surgery was performed by Dr. Hagberg or Dr. Balk. Half the cases involved the dominant hand. Two small fingers, 4 ring fingers, 2 long fingers, and 4 index fingers were injured. The injuries were sustained in an all-terrain vehicle accident (n = 1), in falls (n = 2), while swimming (n = 1), or while playing softball (n = 3), football (n = 4), or soccer (n = 1). Mean time from injury to surgery was 7.5 days (range, 4-27 days). Extent of articular surface involvement of the base of the fractured middle phalanx was calculated using preoperatively obtained lateral radiographs.
Surgical intervention was performed in a reproducible fashion. All patients were treated with closed reduction of the PIP joint under fluoroscopic guidance. Before pinning, joint stability was assessed fluoroscopically both at rest and through an arc of motion. A single smooth 0.045-in K-wire was then inserted percutaneously into the distal and dorsal aspects of the proximal phalanx in retrograde fashion (Figure 1). During wire insertion, the distal interphalangeal joint was flexed to relax the intrinsic mechanism, and the central slip tendon was pierced just proximal to its insertion. We have not noted significant adhesion formation about the central slip with this technique, likely because of limited tendon excursion in this location. Stable joint reduction was confirmed with fluoroscopy. No attempt was made to reduce the intra-articular fracture at the base of the middle phalanx.
A therapy program was initiated 2 to 9 days after surgery. At the first postoperative visit, patients were allowed to perform active ROM (AROM) with the pin in place (Figure 1). K-wires were removed a mean of 25 days (range, 17-31 days) after surgery. A static dorsal block splint was then applied, and patients were encouraged to remove it several times per day for AROM between 20° and full flexion until 6 weeks after surgery. At that time, formal occupational therapy was commenced for another 6 weeks. If there was residual flexion contracture of the PIP joint, dynamic extension splinting was initiated after fracture consolidation.
Mean follow-up was 35.5 months (range, 4-94 months). Postoperative anteroposterior and lateral radiographs were used to evaluate maintenance of joint congruity, fracture union, remodeling, and evidence of degenerative changes. At final follow-up, grip strength of injured and contralateral hands was measured with a dynamometer (Jamar; Patterson Medical, Warrenville, Illinois). AROM and passive ROM (PROM) of the PIP joint was documented at follow-up visits. In addition, patients rated their pain on a 0-to-10 visual analog scale (VAS), with 0 representing no pain and 10 representing excruciating pain. Patients also completed a questionnaire assessing satisfaction with surgical outcome. Physical function and disability were assessed with the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire. Any complications, including the need for further surgeries, were documented. Pearson correlation coefficients and Student t tests (with significance set at P < .05) were used to compare outcomes.
Results
Radiographic reduction of joint dislocation was achieved and maintained in 11 of the 12 patients at a mean follow-up of 35.5 months (range, 4-94 months). Extent of joint surface involvement, based on preoperative lateral radiographs, averaged 43% (range, 25%-75%). Although no direct articular reduction was performed, remodeling of the joint surface was consistently noted at follow-up (Figure 2). Mild radiographic degenerative changes were noted at final follow-up in 4 patients, and moderate changes were noted in 1 patient. Radiographic union was achieved in all cases, and no pin-tract infections were noted.
Mean AROM of the PIP joint at final follow-up was 84° (range, 50°-110°), with patients lacking a mean of 7° of full extension and achieving mean flexion of 91°. Mean PROM was 93° (range, 75°-110°). There was no correlation between extent of articular surface involvement and ROM. Furthermore, no correlation was found between time from injury to surgery and ROM. Patients regained full grip strength in the operative hand. At final follow-up, mean grip strength was 79.4 pounds in the operative hand and 79.6 pounds in the contralateral hand, demonstrating equal grip strengths bilaterally.
Patients overall had very low levels of pain; mean VAS score was 0.64 (range, 0-3). Mean QuickDASH score was 5.7 (range, 0-30), suggesting minimal functional impairment. One patient developed a malunion of the middle phalanx fracture resulting in a rotational deformity and required corrective osteotomy. This patient’s VAS score (3) and QuickDASH score (30) were significantly higher than those of the other patients in the study. No other complications were noted by final follow-up.
A higher level of patient satisfaction was found to be directly related to length of follow-up (P < .05). Satisfaction was inversely related to higher VAS score (P < .05) and higher QuickDASH score (P < .001). Pain at work correlated with lower satisfaction level (P < .05). There was no correlation between patient satisfaction and AROM or PROM.
Discussion
The results of this study demonstrate the efficacy of EBP in the treatment of dorsal PIP joint fracture-dislocations. EBP maintained joint dislocation reduction and allowed for early mobilization, which resulted in good ROM, minimal pain, and good functional outcomes. Of note, postoperative patient satisfaction correlated with pain but not with ROM. It is possible that EBP yielded sufficient functional ROM in all patients such that improvement beyond this threshold did not lead to further improvement in satisfaction. Hume and colleagues23 found that mean PIP joint flexion of 60° is needed for activities of daily living. As mean PIP active flexion was 91° (range, 70°-105°) in the present study, it is possible that satisfaction did not correlate with ROM, as all 12 patients achieved active flexion of more than 60°. Despite the lack of correlation between ROM and satisfaction, early PIP joint mobilization is likely a key contributor to positive outcomes because of its significant role in cartilage healing.24
Postoperative ROM in the present study is consistent with that in other reports of patients with PIP joint fracture-dislocations treated with EBP.11,12,22 In a study by Inoue and Tamura,11 14 such patients had mean PIP ROM of 94° at a mean follow-up of 14 months. Viegas22 followed a series of 3 patients for a mean of 7 weeks. At final follow-up, their mean PIP arc of motion was 71°; they lacked 12° of full extension and achieved 83° of flexion. The larger PIP arc of motion (84°) found in the present study may be due to our significantly longer follow-up (35 months). Unlike us, Viegas22 noted an inverse relationship between extent of articular surface involvement and postoperative ROM. Our finding a lack of correlation may be a result of the significant amount of joint remodeling noted on follow-up radiographs.
Studies of transarticular pinning of PIP joints after dorsal PIP fracture-dislocations have reported outcomes similar to ours.25,26 Newington and colleagues25 evaluated 10 cases of transarticular pinning of the PIP joint and found mean arc of motion of 85° and equal grip strengths between injured and contralateral hands. In a series of 19 patients with PIP fracture-dislocations, Aladin and Davis26 noted similar outcomes of transarticular K-wire fixation and ORIF. In both of their treatment groups, however, there was evidence of PIP joint incongruity and subluxation. Of note, PIP arc motion was lower in their study than in ours.
Recent studies have evaluated unstable PIP fracture-dislocations treated with both EBP and percutaneous reduction and pinning with a second K-wire.13,27 At a mean follow-up of 18 months, Vitale and colleagues13 noted maintenance of concentric fracture reduction, good PIP ROM (mean range, 4°-93°), and low VAS and DASH scores (1.4 and 8, respectively). Waris and Alanen27 noted mean PIP AROM of 83° and low VAS and DASH scores (1 and 4, respectively). The EBP technique used in the present study did not involve percutaneous fracture reduction but achieved equally good ROM and VAS and QuickDASH scores.
Clinical outcomes of EBP of PIP joint fracture-dislocations are also comparable to outcomes of more complex treatment methods.8-10,15-19,21,26,28-33 Dynamic distraction external fixation has led to equally good ROM (mean AROM, 80°-85°15,16) and VAS scores, but with a higher incidence of pin-site infection.14-17 ORIF of the intra-articular middle phalanx fracture has the advantage of obtaining a direct anatomical reduction, but clinical outcomes are similar to those in the present study (mean AROM, 70°; 78% pain-free9), and flexion contractures have been noted.8-10 Furthermore, reduction of the fractured PIP joint articular surface has not been shown to be necessary for good outcomes.16,34 This may be explained in part by PIP joint remodeling, which has been routinely observed on long-term follow-up by the senior authors of the present study. Hemi-hamate autografting and volar plate arthroplasty are other options that have had promising results in the treatment of acute and chronic unstable PIP fracture-dislocations.18-21 However, the postoperative ROM (mean AROM, 61°-85°18,21), VAS scores, and patient satisfaction (91% very satisfied21) of these operations are similar to those of EBP in the present study and may not justify the longer operative times and technical challenges associated with these techniques.
We believe that our study group’s 1 complication, a malunion that was treated with corrective osteotomy, resulted from lack of appreciation of the degree of injury. The teenaged female patient’s index finger PIP joint had a rotational malalignment that was not appreciated before or during surgery. After pinning and after ROM was restored, the index finger was observed crossing over the middle finger with digital flexion. The patient returned to the operating room for corrective osteotomy.
We recommend that surgeons assess alignment carefully, before and during surgery, when considering this technique. Although complications are rare, the technique is not for patients with rotational malalignment; ORIF may be more suitable in these cases. In addition, though EBP may be appropriate for pilon-type injuries, as it allows for early AROM, our procedure of choice for pilon fracture is dynamic external fixation, which in addition to allowing for AROM provides ligamentotaxis. In the event that a large volar articular fragment extends into the middle phalanx diaphysis, we typically proceed with ORIF through a volar shotgun approach. At our institution, injuries lasting more than 3 months are often treated with volar plate arthroplasty or hemi-hamate resurfacing. Finally, we believe that caution should be exercised when using this technique in patients with more than 50% articular involvement. In the present study, though we used this treatment in cases of up to 75% surface involvement, alternative techniques, such as hemi-hamate resurfacing arthroplasty, may provide a better volar bony buttress and limit the risk for recurrent instability. Despite its relative contraindications, our technique has been appropriate for more than 90% of the acute PIP fracture-dislocations we have seen.
This study expands on prior research by demonstrating good function, satisfaction, and pain outcomes of percutaneous EBP in the treatment of unstable dorsal PIP fracture-dislocations. In addition, this study demonstrated that the efficacy of EBP is similar to that of more complex and technically demanding methods of treatment. Our technique has the advantage of simplicity. It obviates the soft-tissue damage required for ORIF and more complex fixation techniques. Furthermore, use of this simple technique may save time and costs and lead to more reproducible outcomes.
One limitation of this study is its small sample size. It is possible that outcomes may have been different with a larger sample. Furthermore, we did not make a direct comparison with other treatment methods. To better determine the optimal treatment method for this fracture type, future studies should prospectively evaluate outcomes for multiple treatment modalities in a randomized fashion.
1. Leibovic SJ, Bowers WH. Anatomy of the proximal interphalangeal joint. Hand Clin. 1994;10(2):169-178.
2. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368-380.
3. Ng CY, Oliver CW. Fractures of the proximal interphalangeal joints of the fingers. J Bone Joint Surg Br. 2009;91(6):705-712.
4. Isani A. Small joint injuries requiring surgical treatment. Orthop Clin North Am. 1986;17(3):407-419.
5. McElfresh EC, Dobyns JH, O’Brien ET. Management of fracture-dislocation of the proximal interphalangeal joints by extension-block splinting. J Bone Joint Surg Am. 1972;54(8):1705-1711.
6. Hastings H 2nd, Carroll C 4th. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4(3):503-527.
7. O’Rourke SK, Gaur S, Barton NJ. Long-term outcome of articular fractures of the phalanges: an eleven year follow up. J Hand Surg Br. 1989;14(2):183-193.
8. Grant I, Berger AC, Tham SK. Internal fixation of unstable fracture dislocations of the proximal interphalangeal joint. J Hand Surg Br. 2005;30(5):492-498.
9. Hamilton SC, Stern PJ, Fassler PR, Kiefhaber TR. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31(8):1349-1354.
10. Lee JY, Teoh LC. Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: indications, approaches and results. J Hand Surg Br. 2006;31(2):138-146.
11. Inoue G, Tamura Y. Treatment of fracture-dislocation of the proximal interphalangeal joint using extension-block Kirschner wire. Ann Chir Main Memb Super. 1991;10(6):564-568.
12. Sugawa I, Otani K, Kobayashi A. Treatment of fracture dislocation PIP-joint by Kirschner wire extension block method. Cent Jpn J Orthop Traumat. 1979;22:1409-1412.
13. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011;36(9):1453-1459.
14. Badia A, Riano F, Ravikoff J, Khouri R, Gonzalez-Hernandez E, Orbay JL. Dynamic intradigital external fixation for proximal interphalangeal joint fracture dislocations. J Hand Surg Am. 2005;30(1):154-160.
15. Ellis SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: a pins and rubber band system. J Hand Surg Am. 2007;32(8):1242-1250.
16. Morgan JP, Gordon DA, Klug MS, Perry PE, Barre PS. Dynamic digital traction for unstable comminuted intra-articular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1995;20(4):565-573.
17. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19-25.
18. Dionysian E, Eaton RG. The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg Am. 2000;25(3):429-437.
19. Durham-Smith G, McCarten GM. Volar plate arthroplasty for closed proximal interphalangeal joint injuries. J Hand Surg Br. 1992;17(4):422-428.
20. Calfee RP, Kiefhaber TR, Sommerkamp TG, Stern PJ. Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2009;34(7):1232-1241.
21. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856-865.
22. Viegas SF. Extension block pinning for proximal interphalangeal joint fracture dislocations: preliminary report of a new technique. J Hand Surg Am. 1992;17(5):896-901.
23. Hume MC, Gellman H, McKellop H, Brumfield RH Jr. Functional range of motion of the joints of the hand. J Hand Surg Am. 1990;15(2):240-243.
24. Salter RB. The physiologic basis of continuous passive motion for articular cartilage healing and regeneration. Hand Clin. 1994;10(2):211-220.
25. Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537-540.
26. Aladin A, Davis TR. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30(2):120-128.
27. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010;35(12):2046-2052.
28. Bain GI, Mehta JA, Heptinstall RJ, Bria M. Dynamic external fixation for injuries of the proximal interphalangeal joint. J Bone Joint Surg Br. 1998;80(6):1014-1019.
29. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5(3):260-268.
30. Green A, Smith J, Redding M, Akelman E. Acute open reduction and rigid internal fixation of proximal interphalangeal joint fracture dislocation. J Hand Surg Am. 1992;17(3):512-517.
31. Inanami H, Ninomiya S, Okutsu I, Tarui T. Dynamic external finger fixator for fracture dislocation of the proximal interphalangeal joint. J Hand Surg Am. 1993;18(1):160-164.
32. Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19(1):98-107.
33. Weiss AP. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop. 1996;(327):21-28.
34. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop. 1987;(214):101-112.
1. Leibovic SJ, Bowers WH. Anatomy of the proximal interphalangeal joint. Hand Clin. 1994;10(2):169-178.
2. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368-380.
3. Ng CY, Oliver CW. Fractures of the proximal interphalangeal joints of the fingers. J Bone Joint Surg Br. 2009;91(6):705-712.
4. Isani A. Small joint injuries requiring surgical treatment. Orthop Clin North Am. 1986;17(3):407-419.
5. McElfresh EC, Dobyns JH, O’Brien ET. Management of fracture-dislocation of the proximal interphalangeal joints by extension-block splinting. J Bone Joint Surg Am. 1972;54(8):1705-1711.
6. Hastings H 2nd, Carroll C 4th. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4(3):503-527.
7. O’Rourke SK, Gaur S, Barton NJ. Long-term outcome of articular fractures of the phalanges: an eleven year follow up. J Hand Surg Br. 1989;14(2):183-193.
8. Grant I, Berger AC, Tham SK. Internal fixation of unstable fracture dislocations of the proximal interphalangeal joint. J Hand Surg Br. 2005;30(5):492-498.
9. Hamilton SC, Stern PJ, Fassler PR, Kiefhaber TR. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31(8):1349-1354.
10. Lee JY, Teoh LC. Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: indications, approaches and results. J Hand Surg Br. 2006;31(2):138-146.
11. Inoue G, Tamura Y. Treatment of fracture-dislocation of the proximal interphalangeal joint using extension-block Kirschner wire. Ann Chir Main Memb Super. 1991;10(6):564-568.
12. Sugawa I, Otani K, Kobayashi A. Treatment of fracture dislocation PIP-joint by Kirschner wire extension block method. Cent Jpn J Orthop Traumat. 1979;22:1409-1412.
13. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011;36(9):1453-1459.
14. Badia A, Riano F, Ravikoff J, Khouri R, Gonzalez-Hernandez E, Orbay JL. Dynamic intradigital external fixation for proximal interphalangeal joint fracture dislocations. J Hand Surg Am. 2005;30(1):154-160.
15. Ellis SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: a pins and rubber band system. J Hand Surg Am. 2007;32(8):1242-1250.
16. Morgan JP, Gordon DA, Klug MS, Perry PE, Barre PS. Dynamic digital traction for unstable comminuted intra-articular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1995;20(4):565-573.
17. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19-25.
18. Dionysian E, Eaton RG. The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg Am. 2000;25(3):429-437.
19. Durham-Smith G, McCarten GM. Volar plate arthroplasty for closed proximal interphalangeal joint injuries. J Hand Surg Br. 1992;17(4):422-428.
20. Calfee RP, Kiefhaber TR, Sommerkamp TG, Stern PJ. Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2009;34(7):1232-1241.
21. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856-865.
22. Viegas SF. Extension block pinning for proximal interphalangeal joint fracture dislocations: preliminary report of a new technique. J Hand Surg Am. 1992;17(5):896-901.
23. Hume MC, Gellman H, McKellop H, Brumfield RH Jr. Functional range of motion of the joints of the hand. J Hand Surg Am. 1990;15(2):240-243.
24. Salter RB. The physiologic basis of continuous passive motion for articular cartilage healing and regeneration. Hand Clin. 1994;10(2):211-220.
25. Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537-540.
26. Aladin A, Davis TR. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30(2):120-128.
27. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010;35(12):2046-2052.
28. Bain GI, Mehta JA, Heptinstall RJ, Bria M. Dynamic external fixation for injuries of the proximal interphalangeal joint. J Bone Joint Surg Br. 1998;80(6):1014-1019.
29. Eaton RG, Malerich MM. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5(3):260-268.
30. Green A, Smith J, Redding M, Akelman E. Acute open reduction and rigid internal fixation of proximal interphalangeal joint fracture dislocation. J Hand Surg Am. 1992;17(3):512-517.
31. Inanami H, Ninomiya S, Okutsu I, Tarui T. Dynamic external finger fixator for fracture dislocation of the proximal interphalangeal joint. J Hand Surg Am. 1993;18(1):160-164.
32. Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19(1):98-107.
33. Weiss AP. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop. 1996;(327):21-28.
34. Agee JM. Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop. 1987;(214):101-112.