User login
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
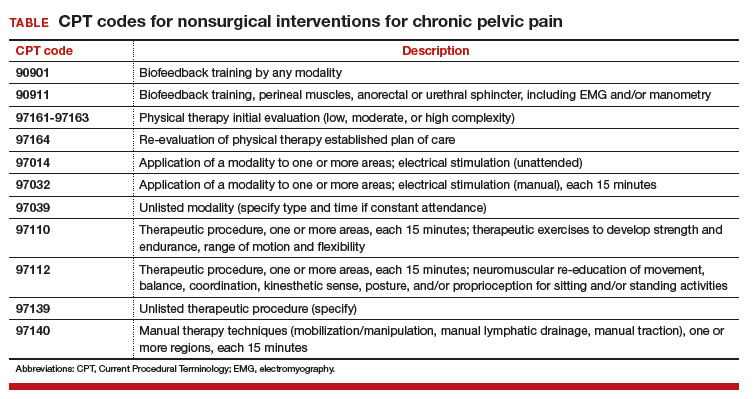
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
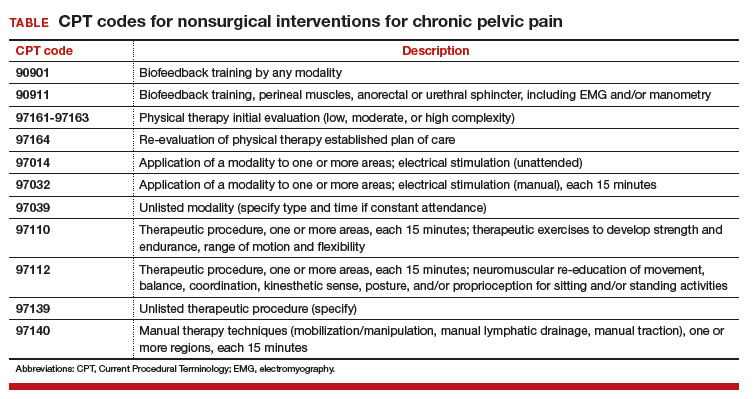
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
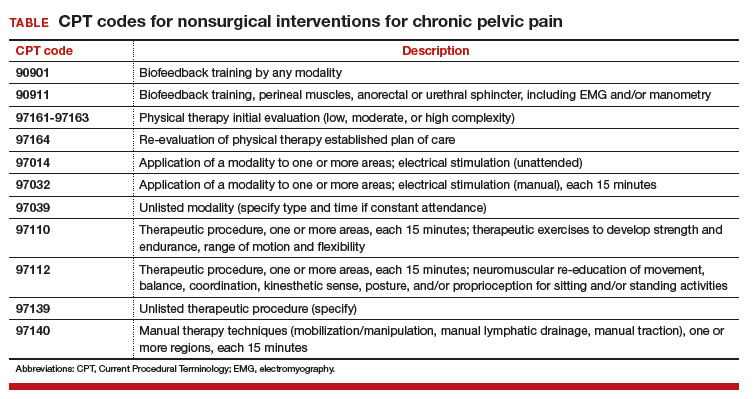
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.

