User login
Chronic conditions contribute to increasing health care expenditures, and a small number of patients with chronic medical conditions consume a disproportionately larger amount of health care resources.1,2 Naessens and colleagues showed that 2.6% of adult patients accounted for 20.7% of all primary care clinic visits during a calendar year.2 These high-risk patients may be using much of the health care resources but have unmet needs even with the increased amount of health care services they receive.
The impact of interprofessional forms of chronic disease management on patient outcomes is unclear.3-5 Definitions for high-risk patients and interprofessional care are broad, making comparison of studies difficult. In a team setting, it is difficult to discern the exact contributions of a single member of the team. Katon and colleagues concluded in a randomized, controlled trial that a nurse care manager collaborative treatment program added additional depression-free days and quality-adjusted life-years in adults with depression and poorly controlled diabetes mellitus (DM), coronary artery disease, or both.3 The intervention also resulted in improvements in a composite outcome of hemoglobin A1c (A1c), low-densitylipoprotein cholesterol, systolic blood pressure (BP) levels, and depression symptoms at 12 months, but these improvements were not sustained at 24 months.3,4
A study looked at interprofessional team care provided by primary care internal medicine residents, nurse practitioner students, and pharmacy students, compared with usual care by only internal medicine residents. The study showed improvements in patient assessments and a trend toward the decreased use of urgent care in patients with type 2 DM over 18 months but no significant improvements in A1c or BP values.5 The impact of pharmacists participating in team-based care and patient-centered medical home models has also been shown to be positive regarding metabolic parameters.6,7Patient aligned care teams (PACT), the VA patient-centered medical home model initiative, seek to optimize patient care through provision of interprofessional, team-based care. At the Boise VAMC in Idaho, PACT training occurs at a primary care academic training clinic that includes 40 primary care providers, supervisors, and trainees in internal medicine, nurse practitioner programs, pharmacy, and behavioral health.
The Boise VAMC is also 1 of 5 VA Centers of Excellence in Primary Care Education (CoEPCE), institutions that prepare health care trainees from many disciplines to participate in interprofessional PACTs, provide patient-centered, team-based care, and learn and understand the roles of other team members.8 This VAMC CoEPCE, implemented in 2010, is an academic partnership with area professional schools of medicine, nursing, and pharmacy.
Team-Based Care
At the Boise VAMC CoEPCE, primary care trainees are taught a team-based approach to providing more effective care for high-risk patients through a complex curriculum that includes interprofessional case conferences called PACT interprofessional care updates (ICU). During these case conferences, high-risk patients on a primary care trainee’s panel are presented to an interprofessional group of health care professionals (HCPs) for recommendations to improve care. Trainees from the various disciplines participate in these PACT ICU presentations during time spent rotating through the institution’s academic clinic.
The CoEPCE activities include PACT ICU, interprofessional didactic sessions, and provision of primary care to patients in an interprofessional clinic. Physician trainees participate in one-half day per week of ambulatory didactics and conferences during a 2-week clinic block, which occurs every 2 months. Other health care disciplines participate in PACT ICU during longitudinal experiences (ranging from 4 to 12 months) in the primary care training clinic throughout the academic year.
The PACT ICU case conferences occur weekly at the academic clinic with 2 patient cases presented and discussed at each meeting. Prior to each conference, a primary care trainee, generally an internal medicine resident, is given a list of the top 5 high-risk patients from their panel, determined by a care assessment needs score that is based on high health care use and risk of hospitalization or death within 90 days. To determine care assessment needs scores, patient electronic health records (EHRs) are scanned weekly to review more than 150 data elements, including vital signs; recent clinic, urgent care, and emergency department (ED) visits; medications; laboratory values; and the number and types of illnesses. Statistical analyses are run on the EHR data to provide up-to-date estimates of likelihood of hospital admission or death.
Trainees may also select any patient on their panel whose health care they feel would benefit from a case conference discussion. The trainee presents all medical and social problems related to the selected patient to a team of HCPs, including other trainees and their supervisors, from multiple different disciplines, such as medicine, nursing, pharmacy, behavioral health, and social work. The interprofessional team then provides recommendations.
A care plan is developed by the group to implement as appropriate. The care plan may consist of various recommendations from the different disciplines, such as consults to a pharmacist for medication review or medication management, referrals to social work to coordinate care with home health services, or asking the nurse care manager to follow up with a patient by phone on a more regular basis. Trainees are encouraged to use alternate forms of care, including team-based care from other health care disciplines as well as other methods of communication, such as secure electronic messaging to increase access.
Interprofessional patient case conferences could offer another tool for HCPs to improve the care of high-risk patients through team-based efforts if the effect on patient outcomes or health care use is beneficial. The objective of this study was to evaluate the relationship of interprofessional case conferences and A1c levels in high-risk patients with DM and BP measurements in patients with hypertension whose case was discussed at PACT ICU case conferences at the Boise VAMC. The authors hypothesized that the PACT ICU presentation intervention would lead to improved metabolic parameters as care plans were implemented. This evaluation is a subset of a larger study assessing the impact of PACT ICU presentation on various patient, trainee, and team level outcomes.
Methods
This study was a retrospective, observational analysis of patients seen at the Boise VAMC academic clinic whose cases were discussed at PACT ICU case conferences from January 2013 to April 2014. For the analysis of A1c values, patients must have been discussed at a PACT ICU presentation during the study time period and had a diagnosis of DM in the EHR. Those included must have A1c results in the EHR before and after the patient case presentation. The most recent A1c measured prior to presentation was chosen as the prepresentation value. The next measured value 2 to 6 months after the case presentation date was chosen as the postpresentation value. This was chosen as the postpresentation value because it may be more indicative of the impact of the PACT ICU care plan. An A1c measured at least 2 months following the case conference intervention was chosen to allow all possible measurements to be included in the analysis, according to usual care for measuring A1c at the clinic. The primary outcome was the mean change in A1c values pre- and post-PACT ICU presentation.
Blood pressure analyses were included if patients had a diagnosis of hypertension in the EHR as well as recorded BP values measured during the 6 months prior to PACT ICU presentation and 1 to 6 months after presentation. Blood pressure values were limited to 1 to 6 months after presentation to be more suggestive of the case conference care plan impact. Blood pressure measured during hospitalizations, urgent care, or ED visits were excluded from the analysis. The primary outcome in the BP analysis was the mean change in systolic and diastolic BP pre- and post-PACT ICU presentation. The mean of all in-clinic BP measurements was calculated as the prepresentation value and compared with the mean of all postpresentation BP measurements in the designated time period.
Assessment of DM or hypertension control was not a factor for inclusion in the study. The types of interventions and recommendations resulting from the case conferences were not evaluated.
Results
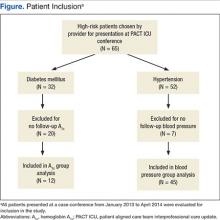
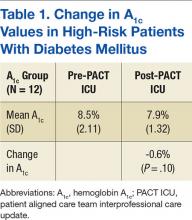
During the study period, 65 patients were discussed at a PACT ICU case conferences (Figure). The average age was 67 years, and 89% of patients were male. Of these patients, 32 had a DM diagnosis. A total of 12 patients had A1c values within the parameters specified for this study and were included in the final analysis for the A1c group.
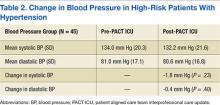
Of all patients discussed at a PACT ICU case conference, 52 had a diagnosis of hypertension (Table 2).
Discussion
High-risk patients with DM enrolled in this primary care academic clinic and discussed at interprofessional case conferences did not have a statistically significant change in A1c values following the case conferences. There was also no statistically significant change in systolic and diastolic BP measurements following PACT ICU case conferences in high-risk patients with hypertension. The relationship between PACT ICU presentations and patient outcomes may not be direct, but the potential to decrease A1c values by 0.6% may be of clinical benefit to patients enrolled at the Boise VAMC academic clinic.
The results of this study are comparable with other studies where the impact of interprofessional forms of care on patient outcomes such as A1c and BP is not as apparent.3-5 The patients included in this study were high-risk compared with other patients, and patient outcome goals for DM and hypertension management according to clinical practice guidelines may be less stringent for these patients.9-11
Interprofessional case conferences are being used at the Boise VAMC academic clinic to teach primary care trainees how to improve care for patients by working on teams, with a goal of promoting alternate forms of health care. Referrals of patients to pharmacy services for chronic disease management may result from these case conferences, and patients could benefit from pharmacy review and management of medications for the treatment of DM and hypertension. There may be other advantages to patients and to the health system in the form of more appropriate health care use, increased contact with providers, and use of other health care resources to decrease costs and medication burden, although these are speculative at this time.
Limitations
This study had several limitations. The patients included in this study were high-risk patients seen by primary care trainees at the Boise VAMC academic clinic, and a small number of patients were included in the final analysis, limiting the generalizability of the results to other patient populations. Finding a difference in A1c and BP values before and after PACT ICU case conferences was also limited by the small number of patients who met inclusion criteria. Many patients included in the study also had reasonably controlled A1c and BP levels prior to PACT ICU case conferences; therefore, a difference would be more difficult to determine.
The PACT ICU case conferences occur at one point in time, but the impact of the intervention and recommendations may take longer to appreciate. A longer study duration may be needed to determine differences in A1c and BP values over time. Regression to the mean is also a possibility given the type of data collected. As each primary care trainee selects the patient to be discussed at a PACT ICU case conference, bias could also be present, because the provider may focus on patients with recent clinic visits or on patients who are the most difficult for the provider to manage or contact.
The Boise VAMC PACTs include many different health care disciplines; therefore, the institution may foster interprofessional, team-based care more easily compared with that of other health care systems. Trainees in the CoEPCE also are aware of other team members’ roles, and clinical pharmacists are currently part of PACTs at the institution. The idea of interprofessional case conferences may be simple, but the process at this institution requires time and effort from a nurse care manager who coordinates patient selection and information distribution and an attending physician supervisor who facilitates each case conference. The Boise VAMC also supports pharmacy chronic disease management services, and several of these patients with uncontrolled DM or resistant hypertension may have been seen by the pharmacy-managed insulin titration or hypertension clinics. Finally, there is also limited documentation of whether DM or hypertension management was discussed at the case conferences.
Despite the medical complexities seen in these patients, discussions during PACT ICU presentations may involve many social and behavioral interventions, and DM and hypertension issues may not be significant enough for review at a case conference. However, the intervention of PACT ICU case conferences encompassed a variety of care plans, and this study evaluated the impact of the entire discussion and recommendations and not any individual component. Other recommendations were not evaluated due to the wide variety of interventions that were potentially discussed, and a process for tracking these was not in place.
The results of this study did not show that the care plans that develop at PACT ICU case conferences impacted high-risk patients with DM or hypertension, likely due to small sample sizes (2 patient cases were discussed per week). The impact could be better determined through a larger sample size, longer duration, or assessment of patients whose disease was not controlled. The impact may also be more significant for individuals who benefit from the increased review and assessment of their chronic medical conditions and increased access to care.
Seeing a possible trend toward benefit in A1c values in this short time frame helps support continuing and expanding case conferences at the Boise VAMC. The goals of these interprofessional case conferences include developing a proactive approach to identify high-risk patients to improve the care of these patients and increase use of more appropriate health care resources. Other outcomes currently being studied include the impact of PACT ICU presentations on health care use, the impact on alternate health care consult patterns, and trainee participant opinions. Future directions for the interprofessional case conferences include expansion to other nonacademic primary care teams. The benefit of PACT ICU case conferences also extends to the primary care trainees as they continue to learn how to best work with other HCPs as part of a team and how to use the resources available through these other health care disciplines.
Conclusions
Presentation at an interprofessional case conference was not associated with a statistically significant change in mean A1c or BP values in a small group of high-risk patients at the Boise VAMC PACT academic clinic. Although there was a trend toward a decrease in A1c values, it is difficult to determine whether there is a relation to the interprofessional case conferences. Interprofessional case conferences are still occurring at the Boise VAMC with efforts in place to incorporate concurrent PACT ICU outcomes data collection and further the educational goals of primary care trainees.
Acknowledgments
The authors would like to express their appreciation to Rick Tivis, MPH, and Tim Gordon, MA, MPH, MS, for their assistance in the analysis and collection of data for this study.
1. Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood). 2010;29(4):718-724.
2. Naessens JM, Baird MA, Van Houten HK, Vanness DJ, Campbell CR. Predicting persistently high primary care use. Ann Fam Med. 2005;3(4):324-330.
3. Katon W, Russo J, Lin EH, et al. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Arch Gen Psychiatry. 2012;69(5):506-514.
4. Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
5. Janson SL, Cooke M, McGrath K, Kroon LA, Robinson S, Baron RB. Improving chronic care of type 2 diabetes using teams of interprofessional learners. Acad Med. 2009;84 (11):1540-1548.
6. Lamb KD, Baker JW, McFarland MS. Implementation of a pharmacotherapy clinic into the patient centered medical home model by a second year pharmacy resident. Am J Health Syst Pharm. 2015;72(17)(suppl 2):S83-S89.
7. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923-933.
8. Gilman SC, Chokshi DA, Bowen JL, Rugen KW, Cox M. Connecting the dots: interprofessional health education and delivery system redesign at the Veterans Health Administration. Acad Med. 2014;89(8):1113-1116.
9. Department of Veteran Affairs, Department of Defense. VA/DoD clinical practice guideline for the management of diabetes mellitus (DM). Department of Veteran Affairs Website. http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Published August 2010. Accessed January 19, 2016.
10. American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care. 2014;37(suppl 1):S14-S80.
11. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
Chronic conditions contribute to increasing health care expenditures, and a small number of patients with chronic medical conditions consume a disproportionately larger amount of health care resources.1,2 Naessens and colleagues showed that 2.6% of adult patients accounted for 20.7% of all primary care clinic visits during a calendar year.2 These high-risk patients may be using much of the health care resources but have unmet needs even with the increased amount of health care services they receive.
The impact of interprofessional forms of chronic disease management on patient outcomes is unclear.3-5 Definitions for high-risk patients and interprofessional care are broad, making comparison of studies difficult. In a team setting, it is difficult to discern the exact contributions of a single member of the team. Katon and colleagues concluded in a randomized, controlled trial that a nurse care manager collaborative treatment program added additional depression-free days and quality-adjusted life-years in adults with depression and poorly controlled diabetes mellitus (DM), coronary artery disease, or both.3 The intervention also resulted in improvements in a composite outcome of hemoglobin A1c (A1c), low-densitylipoprotein cholesterol, systolic blood pressure (BP) levels, and depression symptoms at 12 months, but these improvements were not sustained at 24 months.3,4
A study looked at interprofessional team care provided by primary care internal medicine residents, nurse practitioner students, and pharmacy students, compared with usual care by only internal medicine residents. The study showed improvements in patient assessments and a trend toward the decreased use of urgent care in patients with type 2 DM over 18 months but no significant improvements in A1c or BP values.5 The impact of pharmacists participating in team-based care and patient-centered medical home models has also been shown to be positive regarding metabolic parameters.6,7Patient aligned care teams (PACT), the VA patient-centered medical home model initiative, seek to optimize patient care through provision of interprofessional, team-based care. At the Boise VAMC in Idaho, PACT training occurs at a primary care academic training clinic that includes 40 primary care providers, supervisors, and trainees in internal medicine, nurse practitioner programs, pharmacy, and behavioral health.
The Boise VAMC is also 1 of 5 VA Centers of Excellence in Primary Care Education (CoEPCE), institutions that prepare health care trainees from many disciplines to participate in interprofessional PACTs, provide patient-centered, team-based care, and learn and understand the roles of other team members.8 This VAMC CoEPCE, implemented in 2010, is an academic partnership with area professional schools of medicine, nursing, and pharmacy.
Team-Based Care
At the Boise VAMC CoEPCE, primary care trainees are taught a team-based approach to providing more effective care for high-risk patients through a complex curriculum that includes interprofessional case conferences called PACT interprofessional care updates (ICU). During these case conferences, high-risk patients on a primary care trainee’s panel are presented to an interprofessional group of health care professionals (HCPs) for recommendations to improve care. Trainees from the various disciplines participate in these PACT ICU presentations during time spent rotating through the institution’s academic clinic.
The CoEPCE activities include PACT ICU, interprofessional didactic sessions, and provision of primary care to patients in an interprofessional clinic. Physician trainees participate in one-half day per week of ambulatory didactics and conferences during a 2-week clinic block, which occurs every 2 months. Other health care disciplines participate in PACT ICU during longitudinal experiences (ranging from 4 to 12 months) in the primary care training clinic throughout the academic year.
The PACT ICU case conferences occur weekly at the academic clinic with 2 patient cases presented and discussed at each meeting. Prior to each conference, a primary care trainee, generally an internal medicine resident, is given a list of the top 5 high-risk patients from their panel, determined by a care assessment needs score that is based on high health care use and risk of hospitalization or death within 90 days. To determine care assessment needs scores, patient electronic health records (EHRs) are scanned weekly to review more than 150 data elements, including vital signs; recent clinic, urgent care, and emergency department (ED) visits; medications; laboratory values; and the number and types of illnesses. Statistical analyses are run on the EHR data to provide up-to-date estimates of likelihood of hospital admission or death.
Trainees may also select any patient on their panel whose health care they feel would benefit from a case conference discussion. The trainee presents all medical and social problems related to the selected patient to a team of HCPs, including other trainees and their supervisors, from multiple different disciplines, such as medicine, nursing, pharmacy, behavioral health, and social work. The interprofessional team then provides recommendations.
A care plan is developed by the group to implement as appropriate. The care plan may consist of various recommendations from the different disciplines, such as consults to a pharmacist for medication review or medication management, referrals to social work to coordinate care with home health services, or asking the nurse care manager to follow up with a patient by phone on a more regular basis. Trainees are encouraged to use alternate forms of care, including team-based care from other health care disciplines as well as other methods of communication, such as secure electronic messaging to increase access.
Interprofessional patient case conferences could offer another tool for HCPs to improve the care of high-risk patients through team-based efforts if the effect on patient outcomes or health care use is beneficial. The objective of this study was to evaluate the relationship of interprofessional case conferences and A1c levels in high-risk patients with DM and BP measurements in patients with hypertension whose case was discussed at PACT ICU case conferences at the Boise VAMC. The authors hypothesized that the PACT ICU presentation intervention would lead to improved metabolic parameters as care plans were implemented. This evaluation is a subset of a larger study assessing the impact of PACT ICU presentation on various patient, trainee, and team level outcomes.
Methods
This study was a retrospective, observational analysis of patients seen at the Boise VAMC academic clinic whose cases were discussed at PACT ICU case conferences from January 2013 to April 2014. For the analysis of A1c values, patients must have been discussed at a PACT ICU presentation during the study time period and had a diagnosis of DM in the EHR. Those included must have A1c results in the EHR before and after the patient case presentation. The most recent A1c measured prior to presentation was chosen as the prepresentation value. The next measured value 2 to 6 months after the case presentation date was chosen as the postpresentation value. This was chosen as the postpresentation value because it may be more indicative of the impact of the PACT ICU care plan. An A1c measured at least 2 months following the case conference intervention was chosen to allow all possible measurements to be included in the analysis, according to usual care for measuring A1c at the clinic. The primary outcome was the mean change in A1c values pre- and post-PACT ICU presentation.
Blood pressure analyses were included if patients had a diagnosis of hypertension in the EHR as well as recorded BP values measured during the 6 months prior to PACT ICU presentation and 1 to 6 months after presentation. Blood pressure values were limited to 1 to 6 months after presentation to be more suggestive of the case conference care plan impact. Blood pressure measured during hospitalizations, urgent care, or ED visits were excluded from the analysis. The primary outcome in the BP analysis was the mean change in systolic and diastolic BP pre- and post-PACT ICU presentation. The mean of all in-clinic BP measurements was calculated as the prepresentation value and compared with the mean of all postpresentation BP measurements in the designated time period.
Assessment of DM or hypertension control was not a factor for inclusion in the study. The types of interventions and recommendations resulting from the case conferences were not evaluated.
Results
During the study period, 65 patients were discussed at a PACT ICU case conferences (Figure). The average age was 67 years, and 89% of patients were male. Of these patients, 32 had a DM diagnosis. A total of 12 patients had A1c values within the parameters specified for this study and were included in the final analysis for the A1c group.
Of all patients discussed at a PACT ICU case conference, 52 had a diagnosis of hypertension (Table 2).
Discussion
High-risk patients with DM enrolled in this primary care academic clinic and discussed at interprofessional case conferences did not have a statistically significant change in A1c values following the case conferences. There was also no statistically significant change in systolic and diastolic BP measurements following PACT ICU case conferences in high-risk patients with hypertension. The relationship between PACT ICU presentations and patient outcomes may not be direct, but the potential to decrease A1c values by 0.6% may be of clinical benefit to patients enrolled at the Boise VAMC academic clinic.
The results of this study are comparable with other studies where the impact of interprofessional forms of care on patient outcomes such as A1c and BP is not as apparent.3-5 The patients included in this study were high-risk compared with other patients, and patient outcome goals for DM and hypertension management according to clinical practice guidelines may be less stringent for these patients.9-11
Interprofessional case conferences are being used at the Boise VAMC academic clinic to teach primary care trainees how to improve care for patients by working on teams, with a goal of promoting alternate forms of health care. Referrals of patients to pharmacy services for chronic disease management may result from these case conferences, and patients could benefit from pharmacy review and management of medications for the treatment of DM and hypertension. There may be other advantages to patients and to the health system in the form of more appropriate health care use, increased contact with providers, and use of other health care resources to decrease costs and medication burden, although these are speculative at this time.
Limitations
This study had several limitations. The patients included in this study were high-risk patients seen by primary care trainees at the Boise VAMC academic clinic, and a small number of patients were included in the final analysis, limiting the generalizability of the results to other patient populations. Finding a difference in A1c and BP values before and after PACT ICU case conferences was also limited by the small number of patients who met inclusion criteria. Many patients included in the study also had reasonably controlled A1c and BP levels prior to PACT ICU case conferences; therefore, a difference would be more difficult to determine.
The PACT ICU case conferences occur at one point in time, but the impact of the intervention and recommendations may take longer to appreciate. A longer study duration may be needed to determine differences in A1c and BP values over time. Regression to the mean is also a possibility given the type of data collected. As each primary care trainee selects the patient to be discussed at a PACT ICU case conference, bias could also be present, because the provider may focus on patients with recent clinic visits or on patients who are the most difficult for the provider to manage or contact.
The Boise VAMC PACTs include many different health care disciplines; therefore, the institution may foster interprofessional, team-based care more easily compared with that of other health care systems. Trainees in the CoEPCE also are aware of other team members’ roles, and clinical pharmacists are currently part of PACTs at the institution. The idea of interprofessional case conferences may be simple, but the process at this institution requires time and effort from a nurse care manager who coordinates patient selection and information distribution and an attending physician supervisor who facilitates each case conference. The Boise VAMC also supports pharmacy chronic disease management services, and several of these patients with uncontrolled DM or resistant hypertension may have been seen by the pharmacy-managed insulin titration or hypertension clinics. Finally, there is also limited documentation of whether DM or hypertension management was discussed at the case conferences.
Despite the medical complexities seen in these patients, discussions during PACT ICU presentations may involve many social and behavioral interventions, and DM and hypertension issues may not be significant enough for review at a case conference. However, the intervention of PACT ICU case conferences encompassed a variety of care plans, and this study evaluated the impact of the entire discussion and recommendations and not any individual component. Other recommendations were not evaluated due to the wide variety of interventions that were potentially discussed, and a process for tracking these was not in place.
The results of this study did not show that the care plans that develop at PACT ICU case conferences impacted high-risk patients with DM or hypertension, likely due to small sample sizes (2 patient cases were discussed per week). The impact could be better determined through a larger sample size, longer duration, or assessment of patients whose disease was not controlled. The impact may also be more significant for individuals who benefit from the increased review and assessment of their chronic medical conditions and increased access to care.
Seeing a possible trend toward benefit in A1c values in this short time frame helps support continuing and expanding case conferences at the Boise VAMC. The goals of these interprofessional case conferences include developing a proactive approach to identify high-risk patients to improve the care of these patients and increase use of more appropriate health care resources. Other outcomes currently being studied include the impact of PACT ICU presentations on health care use, the impact on alternate health care consult patterns, and trainee participant opinions. Future directions for the interprofessional case conferences include expansion to other nonacademic primary care teams. The benefit of PACT ICU case conferences also extends to the primary care trainees as they continue to learn how to best work with other HCPs as part of a team and how to use the resources available through these other health care disciplines.
Conclusions
Presentation at an interprofessional case conference was not associated with a statistically significant change in mean A1c or BP values in a small group of high-risk patients at the Boise VAMC PACT academic clinic. Although there was a trend toward a decrease in A1c values, it is difficult to determine whether there is a relation to the interprofessional case conferences. Interprofessional case conferences are still occurring at the Boise VAMC with efforts in place to incorporate concurrent PACT ICU outcomes data collection and further the educational goals of primary care trainees.
Acknowledgments
The authors would like to express their appreciation to Rick Tivis, MPH, and Tim Gordon, MA, MPH, MS, for their assistance in the analysis and collection of data for this study.
Chronic conditions contribute to increasing health care expenditures, and a small number of patients with chronic medical conditions consume a disproportionately larger amount of health care resources.1,2 Naessens and colleagues showed that 2.6% of adult patients accounted for 20.7% of all primary care clinic visits during a calendar year.2 These high-risk patients may be using much of the health care resources but have unmet needs even with the increased amount of health care services they receive.
The impact of interprofessional forms of chronic disease management on patient outcomes is unclear.3-5 Definitions for high-risk patients and interprofessional care are broad, making comparison of studies difficult. In a team setting, it is difficult to discern the exact contributions of a single member of the team. Katon and colleagues concluded in a randomized, controlled trial that a nurse care manager collaborative treatment program added additional depression-free days and quality-adjusted life-years in adults with depression and poorly controlled diabetes mellitus (DM), coronary artery disease, or both.3 The intervention also resulted in improvements in a composite outcome of hemoglobin A1c (A1c), low-densitylipoprotein cholesterol, systolic blood pressure (BP) levels, and depression symptoms at 12 months, but these improvements were not sustained at 24 months.3,4
A study looked at interprofessional team care provided by primary care internal medicine residents, nurse practitioner students, and pharmacy students, compared with usual care by only internal medicine residents. The study showed improvements in patient assessments and a trend toward the decreased use of urgent care in patients with type 2 DM over 18 months but no significant improvements in A1c or BP values.5 The impact of pharmacists participating in team-based care and patient-centered medical home models has also been shown to be positive regarding metabolic parameters.6,7Patient aligned care teams (PACT), the VA patient-centered medical home model initiative, seek to optimize patient care through provision of interprofessional, team-based care. At the Boise VAMC in Idaho, PACT training occurs at a primary care academic training clinic that includes 40 primary care providers, supervisors, and trainees in internal medicine, nurse practitioner programs, pharmacy, and behavioral health.
The Boise VAMC is also 1 of 5 VA Centers of Excellence in Primary Care Education (CoEPCE), institutions that prepare health care trainees from many disciplines to participate in interprofessional PACTs, provide patient-centered, team-based care, and learn and understand the roles of other team members.8 This VAMC CoEPCE, implemented in 2010, is an academic partnership with area professional schools of medicine, nursing, and pharmacy.
Team-Based Care
At the Boise VAMC CoEPCE, primary care trainees are taught a team-based approach to providing more effective care for high-risk patients through a complex curriculum that includes interprofessional case conferences called PACT interprofessional care updates (ICU). During these case conferences, high-risk patients on a primary care trainee’s panel are presented to an interprofessional group of health care professionals (HCPs) for recommendations to improve care. Trainees from the various disciplines participate in these PACT ICU presentations during time spent rotating through the institution’s academic clinic.
The CoEPCE activities include PACT ICU, interprofessional didactic sessions, and provision of primary care to patients in an interprofessional clinic. Physician trainees participate in one-half day per week of ambulatory didactics and conferences during a 2-week clinic block, which occurs every 2 months. Other health care disciplines participate in PACT ICU during longitudinal experiences (ranging from 4 to 12 months) in the primary care training clinic throughout the academic year.
The PACT ICU case conferences occur weekly at the academic clinic with 2 patient cases presented and discussed at each meeting. Prior to each conference, a primary care trainee, generally an internal medicine resident, is given a list of the top 5 high-risk patients from their panel, determined by a care assessment needs score that is based on high health care use and risk of hospitalization or death within 90 days. To determine care assessment needs scores, patient electronic health records (EHRs) are scanned weekly to review more than 150 data elements, including vital signs; recent clinic, urgent care, and emergency department (ED) visits; medications; laboratory values; and the number and types of illnesses. Statistical analyses are run on the EHR data to provide up-to-date estimates of likelihood of hospital admission or death.
Trainees may also select any patient on their panel whose health care they feel would benefit from a case conference discussion. The trainee presents all medical and social problems related to the selected patient to a team of HCPs, including other trainees and their supervisors, from multiple different disciplines, such as medicine, nursing, pharmacy, behavioral health, and social work. The interprofessional team then provides recommendations.
A care plan is developed by the group to implement as appropriate. The care plan may consist of various recommendations from the different disciplines, such as consults to a pharmacist for medication review or medication management, referrals to social work to coordinate care with home health services, or asking the nurse care manager to follow up with a patient by phone on a more regular basis. Trainees are encouraged to use alternate forms of care, including team-based care from other health care disciplines as well as other methods of communication, such as secure electronic messaging to increase access.
Interprofessional patient case conferences could offer another tool for HCPs to improve the care of high-risk patients through team-based efforts if the effect on patient outcomes or health care use is beneficial. The objective of this study was to evaluate the relationship of interprofessional case conferences and A1c levels in high-risk patients with DM and BP measurements in patients with hypertension whose case was discussed at PACT ICU case conferences at the Boise VAMC. The authors hypothesized that the PACT ICU presentation intervention would lead to improved metabolic parameters as care plans were implemented. This evaluation is a subset of a larger study assessing the impact of PACT ICU presentation on various patient, trainee, and team level outcomes.
Methods
This study was a retrospective, observational analysis of patients seen at the Boise VAMC academic clinic whose cases were discussed at PACT ICU case conferences from January 2013 to April 2014. For the analysis of A1c values, patients must have been discussed at a PACT ICU presentation during the study time period and had a diagnosis of DM in the EHR. Those included must have A1c results in the EHR before and after the patient case presentation. The most recent A1c measured prior to presentation was chosen as the prepresentation value. The next measured value 2 to 6 months after the case presentation date was chosen as the postpresentation value. This was chosen as the postpresentation value because it may be more indicative of the impact of the PACT ICU care plan. An A1c measured at least 2 months following the case conference intervention was chosen to allow all possible measurements to be included in the analysis, according to usual care for measuring A1c at the clinic. The primary outcome was the mean change in A1c values pre- and post-PACT ICU presentation.
Blood pressure analyses were included if patients had a diagnosis of hypertension in the EHR as well as recorded BP values measured during the 6 months prior to PACT ICU presentation and 1 to 6 months after presentation. Blood pressure values were limited to 1 to 6 months after presentation to be more suggestive of the case conference care plan impact. Blood pressure measured during hospitalizations, urgent care, or ED visits were excluded from the analysis. The primary outcome in the BP analysis was the mean change in systolic and diastolic BP pre- and post-PACT ICU presentation. The mean of all in-clinic BP measurements was calculated as the prepresentation value and compared with the mean of all postpresentation BP measurements in the designated time period.
Assessment of DM or hypertension control was not a factor for inclusion in the study. The types of interventions and recommendations resulting from the case conferences were not evaluated.
Results
During the study period, 65 patients were discussed at a PACT ICU case conferences (Figure). The average age was 67 years, and 89% of patients were male. Of these patients, 32 had a DM diagnosis. A total of 12 patients had A1c values within the parameters specified for this study and were included in the final analysis for the A1c group.
Of all patients discussed at a PACT ICU case conference, 52 had a diagnosis of hypertension (Table 2).
Discussion
High-risk patients with DM enrolled in this primary care academic clinic and discussed at interprofessional case conferences did not have a statistically significant change in A1c values following the case conferences. There was also no statistically significant change in systolic and diastolic BP measurements following PACT ICU case conferences in high-risk patients with hypertension. The relationship between PACT ICU presentations and patient outcomes may not be direct, but the potential to decrease A1c values by 0.6% may be of clinical benefit to patients enrolled at the Boise VAMC academic clinic.
The results of this study are comparable with other studies where the impact of interprofessional forms of care on patient outcomes such as A1c and BP is not as apparent.3-5 The patients included in this study were high-risk compared with other patients, and patient outcome goals for DM and hypertension management according to clinical practice guidelines may be less stringent for these patients.9-11
Interprofessional case conferences are being used at the Boise VAMC academic clinic to teach primary care trainees how to improve care for patients by working on teams, with a goal of promoting alternate forms of health care. Referrals of patients to pharmacy services for chronic disease management may result from these case conferences, and patients could benefit from pharmacy review and management of medications for the treatment of DM and hypertension. There may be other advantages to patients and to the health system in the form of more appropriate health care use, increased contact with providers, and use of other health care resources to decrease costs and medication burden, although these are speculative at this time.
Limitations
This study had several limitations. The patients included in this study were high-risk patients seen by primary care trainees at the Boise VAMC academic clinic, and a small number of patients were included in the final analysis, limiting the generalizability of the results to other patient populations. Finding a difference in A1c and BP values before and after PACT ICU case conferences was also limited by the small number of patients who met inclusion criteria. Many patients included in the study also had reasonably controlled A1c and BP levels prior to PACT ICU case conferences; therefore, a difference would be more difficult to determine.
The PACT ICU case conferences occur at one point in time, but the impact of the intervention and recommendations may take longer to appreciate. A longer study duration may be needed to determine differences in A1c and BP values over time. Regression to the mean is also a possibility given the type of data collected. As each primary care trainee selects the patient to be discussed at a PACT ICU case conference, bias could also be present, because the provider may focus on patients with recent clinic visits or on patients who are the most difficult for the provider to manage or contact.
The Boise VAMC PACTs include many different health care disciplines; therefore, the institution may foster interprofessional, team-based care more easily compared with that of other health care systems. Trainees in the CoEPCE also are aware of other team members’ roles, and clinical pharmacists are currently part of PACTs at the institution. The idea of interprofessional case conferences may be simple, but the process at this institution requires time and effort from a nurse care manager who coordinates patient selection and information distribution and an attending physician supervisor who facilitates each case conference. The Boise VAMC also supports pharmacy chronic disease management services, and several of these patients with uncontrolled DM or resistant hypertension may have been seen by the pharmacy-managed insulin titration or hypertension clinics. Finally, there is also limited documentation of whether DM or hypertension management was discussed at the case conferences.
Despite the medical complexities seen in these patients, discussions during PACT ICU presentations may involve many social and behavioral interventions, and DM and hypertension issues may not be significant enough for review at a case conference. However, the intervention of PACT ICU case conferences encompassed a variety of care plans, and this study evaluated the impact of the entire discussion and recommendations and not any individual component. Other recommendations were not evaluated due to the wide variety of interventions that were potentially discussed, and a process for tracking these was not in place.
The results of this study did not show that the care plans that develop at PACT ICU case conferences impacted high-risk patients with DM or hypertension, likely due to small sample sizes (2 patient cases were discussed per week). The impact could be better determined through a larger sample size, longer duration, or assessment of patients whose disease was not controlled. The impact may also be more significant for individuals who benefit from the increased review and assessment of their chronic medical conditions and increased access to care.
Seeing a possible trend toward benefit in A1c values in this short time frame helps support continuing and expanding case conferences at the Boise VAMC. The goals of these interprofessional case conferences include developing a proactive approach to identify high-risk patients to improve the care of these patients and increase use of more appropriate health care resources. Other outcomes currently being studied include the impact of PACT ICU presentations on health care use, the impact on alternate health care consult patterns, and trainee participant opinions. Future directions for the interprofessional case conferences include expansion to other nonacademic primary care teams. The benefit of PACT ICU case conferences also extends to the primary care trainees as they continue to learn how to best work with other HCPs as part of a team and how to use the resources available through these other health care disciplines.
Conclusions
Presentation at an interprofessional case conference was not associated with a statistically significant change in mean A1c or BP values in a small group of high-risk patients at the Boise VAMC PACT academic clinic. Although there was a trend toward a decrease in A1c values, it is difficult to determine whether there is a relation to the interprofessional case conferences. Interprofessional case conferences are still occurring at the Boise VAMC with efforts in place to incorporate concurrent PACT ICU outcomes data collection and further the educational goals of primary care trainees.
Acknowledgments
The authors would like to express their appreciation to Rick Tivis, MPH, and Tim Gordon, MA, MPH, MS, for their assistance in the analysis and collection of data for this study.
1. Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood). 2010;29(4):718-724.
2. Naessens JM, Baird MA, Van Houten HK, Vanness DJ, Campbell CR. Predicting persistently high primary care use. Ann Fam Med. 2005;3(4):324-330.
3. Katon W, Russo J, Lin EH, et al. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Arch Gen Psychiatry. 2012;69(5):506-514.
4. Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
5. Janson SL, Cooke M, McGrath K, Kroon LA, Robinson S, Baron RB. Improving chronic care of type 2 diabetes using teams of interprofessional learners. Acad Med. 2009;84 (11):1540-1548.
6. Lamb KD, Baker JW, McFarland MS. Implementation of a pharmacotherapy clinic into the patient centered medical home model by a second year pharmacy resident. Am J Health Syst Pharm. 2015;72(17)(suppl 2):S83-S89.
7. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923-933.
8. Gilman SC, Chokshi DA, Bowen JL, Rugen KW, Cox M. Connecting the dots: interprofessional health education and delivery system redesign at the Veterans Health Administration. Acad Med. 2014;89(8):1113-1116.
9. Department of Veteran Affairs, Department of Defense. VA/DoD clinical practice guideline for the management of diabetes mellitus (DM). Department of Veteran Affairs Website. http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Published August 2010. Accessed January 19, 2016.
10. American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care. 2014;37(suppl 1):S14-S80.
11. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
1. Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood). 2010;29(4):718-724.
2. Naessens JM, Baird MA, Van Houten HK, Vanness DJ, Campbell CR. Predicting persistently high primary care use. Ann Fam Med. 2005;3(4):324-330.
3. Katon W, Russo J, Lin EH, et al. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Arch Gen Psychiatry. 2012;69(5):506-514.
4. Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611-2620.
5. Janson SL, Cooke M, McGrath K, Kroon LA, Robinson S, Baron RB. Improving chronic care of type 2 diabetes using teams of interprofessional learners. Acad Med. 2009;84 (11):1540-1548.
6. Lamb KD, Baker JW, McFarland MS. Implementation of a pharmacotherapy clinic into the patient centered medical home model by a second year pharmacy resident. Am J Health Syst Pharm. 2015;72(17)(suppl 2):S83-S89.
7. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923-933.
8. Gilman SC, Chokshi DA, Bowen JL, Rugen KW, Cox M. Connecting the dots: interprofessional health education and delivery system redesign at the Veterans Health Administration. Acad Med. 2014;89(8):1113-1116.
9. Department of Veteran Affairs, Department of Defense. VA/DoD clinical practice guideline for the management of diabetes mellitus (DM). Department of Veteran Affairs Website. http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Published August 2010. Accessed January 19, 2016.
10. American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care. 2014;37(suppl 1):S14-S80.
11. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.