User login
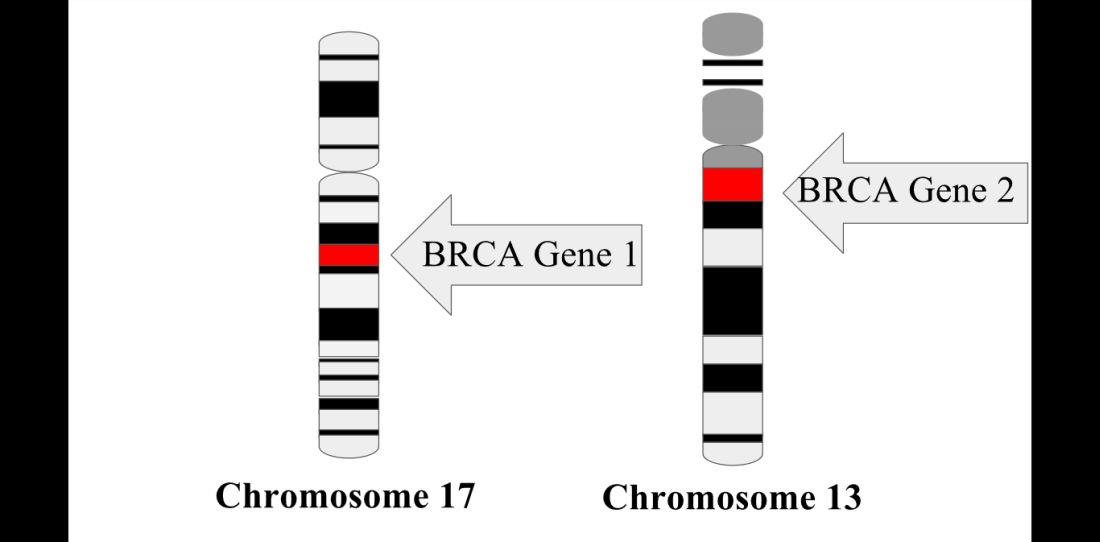
For women with young-onset breast cancer, presence of a BRCA mutation did not significantly impact survival, according to results of the Prospective Outcomes in Sporadic versus Hereditary breast cancer (POSH) study.
BRCA-positive and BRCA-negative women had similar overall survival at 2 years, 5 years, and 10 years after diagnosis, according to lead author Ellen R. Copson, MD, a senior lecturer in medical oncology in the cancer sciences division, University of Southampton (England) and her study coauthors.
Currently, young women with breast cancer and a BRCA mutation frequently are offered bilateral mastectomy, the authors noted.
The prospective cohort study by Dr. Copson and her colleagues included 2,733 women with breast cancer who were aged 40 years or younger at first diagnosis. Of those patients, 338 (12%) had either a BRCA1 or BRCA2 mutation, according to investigators.
At 2 years after diagnosis, overall survival was 97.0% and 96.6% for BRCA-positive and BRCA-negative patients, respectively, the report said. Similarly, overall survival was 83.8% and 85.0% for the two groups at 5 years after diagnosis, and 73.4% vs. 70.1% at 10 years.
Multivariable analysis accounting for known prognostic factors including ethnicity and body mass index showed there was no significant difference between groups (hazard ratio, 0.96; 95% confidence interval, 0.76-1.22; P = .76), the authors wrote.
Triple-negative breast cancer patients with a BRCA mutation might have a survival advantage in the first few years following diagnosis,compared with non-BRCA carriers, the POSH study also found. Researchers reported a significant difference at 2 years (95% for BRCA-positive vs. 91% for BRCA-negative patients; P = .047), but there was no significant difference between arms at 5 or 10 years.
POSH is believed to be the largest prospective cohort study to compare breast cancer outcomes for patients with BRCA mutations to those with sporadic breast cancer. Previous studies, primarily retrospective, have suggested “better, worse, or similar outcomes” for BRCA-positive versus BRCA-negative patients, the authors wrote. Dr. Copson reported receiving honoraria from Roche, while her coauthors reported honoraria from GSK, Pfizer, AstraZeneca, and Pierre Fabre. Funding for the study was provided by the Wessex Cancer Trust, Cancer Research UK, and Breast Cancer Now.
SOURCE: Copson et al. Lancet Oncol. 2018 Jan 11 doi: 10.1016/S1470-2045(17)30891-4.
The POSH prospective cohort study, which showed no significant difference in survival for BRCA-positive versus BRCA-negative young onset breast cancer patients, has contributed to the understanding of this patient population, providing “comprehensive data about patient, tumor, and treatment characteristics, along with extensive follow-up data,” wrote Peter A. Fasching, MD, in accompanying editorial.
“Understanding prognosis in young patients is important because patients with BRCA mutations are at increased risk of developing specific conditions, such as secondary cancers,” Dr. Fasching said. “These risks determine treatment, and knowing that BRCA1 or BRCA2 mutations do not result in a different prognosis might change the therapeutic approach for these risks.”
Moreover, in retrospective analyses, bilateral mastectomy conferred an overall survival benefit for BRCA mutation carriers: “This important topic needs more prospective research, as preventive surgical measures might have an effect on what might be a very long life after a diagnosis of breast cancer at a young age,” said Dr. Fasching. “The data from POSH deliver a rationale for prospective studies to address these questions.”
Dr. Peter A. Fasching is with Friedrich-Alexander University Erlangen-Nuremberg, Germany. These comments are based on his editorial appearing in Lancet Oncology (2018 Jan 11. doi: 10.1016/S1470-2045(18)30008-1). Dr. Fasching declared grants from Novartis, along with personal fees from Novartis, Pfizer, Roche, Teva, and Amgen.
The POSH prospective cohort study, which showed no significant difference in survival for BRCA-positive versus BRCA-negative young onset breast cancer patients, has contributed to the understanding of this patient population, providing “comprehensive data about patient, tumor, and treatment characteristics, along with extensive follow-up data,” wrote Peter A. Fasching, MD, in accompanying editorial.
“Understanding prognosis in young patients is important because patients with BRCA mutations are at increased risk of developing specific conditions, such as secondary cancers,” Dr. Fasching said. “These risks determine treatment, and knowing that BRCA1 or BRCA2 mutations do not result in a different prognosis might change the therapeutic approach for these risks.”
Moreover, in retrospective analyses, bilateral mastectomy conferred an overall survival benefit for BRCA mutation carriers: “This important topic needs more prospective research, as preventive surgical measures might have an effect on what might be a very long life after a diagnosis of breast cancer at a young age,” said Dr. Fasching. “The data from POSH deliver a rationale for prospective studies to address these questions.”
Dr. Peter A. Fasching is with Friedrich-Alexander University Erlangen-Nuremberg, Germany. These comments are based on his editorial appearing in Lancet Oncology (2018 Jan 11. doi: 10.1016/S1470-2045(18)30008-1). Dr. Fasching declared grants from Novartis, along with personal fees from Novartis, Pfizer, Roche, Teva, and Amgen.
The POSH prospective cohort study, which showed no significant difference in survival for BRCA-positive versus BRCA-negative young onset breast cancer patients, has contributed to the understanding of this patient population, providing “comprehensive data about patient, tumor, and treatment characteristics, along with extensive follow-up data,” wrote Peter A. Fasching, MD, in accompanying editorial.
“Understanding prognosis in young patients is important because patients with BRCA mutations are at increased risk of developing specific conditions, such as secondary cancers,” Dr. Fasching said. “These risks determine treatment, and knowing that BRCA1 or BRCA2 mutations do not result in a different prognosis might change the therapeutic approach for these risks.”
Moreover, in retrospective analyses, bilateral mastectomy conferred an overall survival benefit for BRCA mutation carriers: “This important topic needs more prospective research, as preventive surgical measures might have an effect on what might be a very long life after a diagnosis of breast cancer at a young age,” said Dr. Fasching. “The data from POSH deliver a rationale for prospective studies to address these questions.”
Dr. Peter A. Fasching is with Friedrich-Alexander University Erlangen-Nuremberg, Germany. These comments are based on his editorial appearing in Lancet Oncology (2018 Jan 11. doi: 10.1016/S1470-2045(18)30008-1). Dr. Fasching declared grants from Novartis, along with personal fees from Novartis, Pfizer, Roche, Teva, and Amgen.
For women with young-onset breast cancer, presence of a BRCA mutation did not significantly impact survival, according to results of the Prospective Outcomes in Sporadic versus Hereditary breast cancer (POSH) study.
BRCA-positive and BRCA-negative women had similar overall survival at 2 years, 5 years, and 10 years after diagnosis, according to lead author Ellen R. Copson, MD, a senior lecturer in medical oncology in the cancer sciences division, University of Southampton (England) and her study coauthors.
Currently, young women with breast cancer and a BRCA mutation frequently are offered bilateral mastectomy, the authors noted.
The prospective cohort study by Dr. Copson and her colleagues included 2,733 women with breast cancer who were aged 40 years or younger at first diagnosis. Of those patients, 338 (12%) had either a BRCA1 or BRCA2 mutation, according to investigators.
At 2 years after diagnosis, overall survival was 97.0% and 96.6% for BRCA-positive and BRCA-negative patients, respectively, the report said. Similarly, overall survival was 83.8% and 85.0% for the two groups at 5 years after diagnosis, and 73.4% vs. 70.1% at 10 years.
Multivariable analysis accounting for known prognostic factors including ethnicity and body mass index showed there was no significant difference between groups (hazard ratio, 0.96; 95% confidence interval, 0.76-1.22; P = .76), the authors wrote.
Triple-negative breast cancer patients with a BRCA mutation might have a survival advantage in the first few years following diagnosis,compared with non-BRCA carriers, the POSH study also found. Researchers reported a significant difference at 2 years (95% for BRCA-positive vs. 91% for BRCA-negative patients; P = .047), but there was no significant difference between arms at 5 or 10 years.
POSH is believed to be the largest prospective cohort study to compare breast cancer outcomes for patients with BRCA mutations to those with sporadic breast cancer. Previous studies, primarily retrospective, have suggested “better, worse, or similar outcomes” for BRCA-positive versus BRCA-negative patients, the authors wrote. Dr. Copson reported receiving honoraria from Roche, while her coauthors reported honoraria from GSK, Pfizer, AstraZeneca, and Pierre Fabre. Funding for the study was provided by the Wessex Cancer Trust, Cancer Research UK, and Breast Cancer Now.
SOURCE: Copson et al. Lancet Oncol. 2018 Jan 11 doi: 10.1016/S1470-2045(17)30891-4.
For women with young-onset breast cancer, presence of a BRCA mutation did not significantly impact survival, according to results of the Prospective Outcomes in Sporadic versus Hereditary breast cancer (POSH) study.
BRCA-positive and BRCA-negative women had similar overall survival at 2 years, 5 years, and 10 years after diagnosis, according to lead author Ellen R. Copson, MD, a senior lecturer in medical oncology in the cancer sciences division, University of Southampton (England) and her study coauthors.
Currently, young women with breast cancer and a BRCA mutation frequently are offered bilateral mastectomy, the authors noted.
The prospective cohort study by Dr. Copson and her colleagues included 2,733 women with breast cancer who were aged 40 years or younger at first diagnosis. Of those patients, 338 (12%) had either a BRCA1 or BRCA2 mutation, according to investigators.
At 2 years after diagnosis, overall survival was 97.0% and 96.6% for BRCA-positive and BRCA-negative patients, respectively, the report said. Similarly, overall survival was 83.8% and 85.0% for the two groups at 5 years after diagnosis, and 73.4% vs. 70.1% at 10 years.
Multivariable analysis accounting for known prognostic factors including ethnicity and body mass index showed there was no significant difference between groups (hazard ratio, 0.96; 95% confidence interval, 0.76-1.22; P = .76), the authors wrote.
Triple-negative breast cancer patients with a BRCA mutation might have a survival advantage in the first few years following diagnosis,compared with non-BRCA carriers, the POSH study also found. Researchers reported a significant difference at 2 years (95% for BRCA-positive vs. 91% for BRCA-negative patients; P = .047), but there was no significant difference between arms at 5 or 10 years.
POSH is believed to be the largest prospective cohort study to compare breast cancer outcomes for patients with BRCA mutations to those with sporadic breast cancer. Previous studies, primarily retrospective, have suggested “better, worse, or similar outcomes” for BRCA-positive versus BRCA-negative patients, the authors wrote. Dr. Copson reported receiving honoraria from Roche, while her coauthors reported honoraria from GSK, Pfizer, AstraZeneca, and Pierre Fabre. Funding for the study was provided by the Wessex Cancer Trust, Cancer Research UK, and Breast Cancer Now.
SOURCE: Copson et al. Lancet Oncol. 2018 Jan 11 doi: 10.1016/S1470-2045(17)30891-4.
FROM LANCET ONCOLOGY
Key clinical point: Presence of BRCA1 or BRCA2 germline mutations did not significantly affect overall survival in women with young onset breast cancer.
Major finding: At 2 years, overall survival was 97.0% for BRCA mutation carriers and 96.6% for non-carriers, with similar results reported at 5 and 10 years.
Data source: A prospective cohort study including 2,733 women with breast cancer who were aged 40 years or younger at first diagnosis.
Disclosures: Funding for the study was provided by the Wessex Cancer Trust, Cancer Research UK, and Breast Cancer Now. Study authors declared honoraria from Roche, GSK, Pfizer, AstraZeneca, and Pierre Fabre.
Source: Copson ER et al. Lancet Oncol. 2018 Jan 11. doi: 10.1016/S1470-2045(17)30891-4.