User login
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
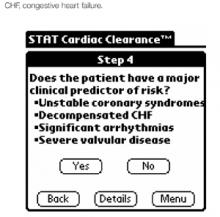
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
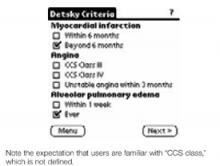
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
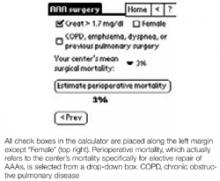
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
Stating that a patient is “cleared for surgery” is no longer considered adequate; rather, the patient should be assessed for surgical risk, a major component of which is cardiovascular risk. The risk level helps the surgical team determine which preoperative, intraoperative, and postoperative assessments and therapies are indicated.1
Clinical decision tools to assist physicians perform preoperative cardiovascular assessment have been developed and validated, and some have been adapted to handheld computers (Table 1).1-8 Yet few prospective or randomized studies have been conducted to establish the value of various preoperative assessment strategies on outcome.1 In this report, we review the studies underlying these rules and the corresponding software programs for handheld computers (also known as personal digital assistants, or PDAs). Our goal is to find readily applicable software that assists physicians in performing rapid preoperative cardiovascular assessment of patients in the office or hospital.
Cardiovascular Decision Tools
Some cardiovascular decision tools, such as those developed by the American College of Physicians (ACP) and American College of Cardiology/American Heart Association (ACC/AHA), are algorithmic approaches that make direct recommendations about whether to pursue cardiac testing. These tools are designed to be widely applicable to potential candidates for noncardiac surgery.
Other decision tools provide a risk score or index, which the user must interpret and translate into perioperative recommendations. The physician must also assure that the index is appropriate to the patient being evaluated by considering the original study’s patient selection criteria, the setting in which the rule was validated (eg, referral center), and which outcomes the rule predicts. Table 2provides more detailed information about each rule, as well as an assessment of each rule’s methodologic rigor (adapted from methodologic standards for clinical prediction rules developed by Wasson et al10).
Limitations
Even when applied correctly, these indices have substantial limits. The positive predictive values (percentage of patients predicted to have complications who actually suffer a complication) are generally low and, especially in the case of higher-risk surgery, a low risk score does not eliminate the risk of complications.2
It is therefore important to consider the overall risk of adverse outcomes for patients undergoing a particular kind of surgery (the “pretest probability”): the same patient planning cataract surgery and vascular surgery has 2 distinctly different risks, despite having the same score on the biomedical components of the index. Also, these decision support tools were developed using information from patients enrolled during past decades, and their results may not be directly applicable to current surgical risks.4 Finally, these indices cannot be used on all patients. For example, a patient with a rare or unusual problem such as left atrial myxoma may be at a higher risk than would otherwise be indicated by one of the decision support tools.3
TABLE 1
Program information
| Algorithm | Program | Version | Size | Cost | Source |
|---|---|---|---|---|---|
| ACC/AHA1 2002 | STAT Cardiac Clearance | 1.1 | 97 KB | Free | http://www.statcoder.com |
| Detsky3 | MedRules | 2.5 | 324 KB | Free | http://pbrain.hypermart.net/ |
| Detsky6 | InfoRetriever | 4.2 (beta) | 2.1 MB | Beta is free;cost of final version unknown | http://www.infopoems.com |
TABLE 2
Selected characteristics of studies of perioperative risk assessment
| Decision rule | Study population characteristics | Derivation and validation set sample size; years of enrollment | Prospective data collection and reviewer blinding | Major outcomes measured and number of outcomes | Pretest probabilities† | |
|---|---|---|---|---|---|---|
| ACC/AHA1 | All noncardiac surgery, major & minor | N/A / N/A Evidencebased guideline | N/A | N/A | N/A | |
| ACP2 | All noncardiac surgery, major & minor | N/A / N/A Evidence based consensus guideline | N/A | N/A | N/A | |
| Detsky3,6 | All noncardiac surgery, major & minor, at a large teaching hospital. Patients were 40 years and older, referred by the surgical services for consultation because of a question of cardiac risk or chronic disease.a | Not specified/ 455; Enrollment years not specified | Blinded,* prospective collection of validation data | Cardiac death, nonfatal myocardial infarction, ventricular tachycardia or fibrillation requiring counter shock, and nonfatal alveolar pulmonary edema;30 outcomes occurred3 | Major surgery‡
| |
| Minor surgery 1.6%/2.1% (eg, TURP, cataracts) | ||||||
| Mangano/Goldman4,9 | Consecutive unselected patients at a large teaching hospital. Patients were 40 years and older; patients with angina or those undergoing minor surgery were excludedb | 1001/None; 1975–1976 | Derivation set data not uniformly prospective; blinding not mentioned | Myocardial infarction,pulmonary edema, ventricular tachycardia; 58 outcomes occurred | 5.8% | |
| Lee5 | All patients at a large teaching hospital, 50 years and older, with an anticipated surgical length of stay ≥ 2 daysc | 2893/1422; 1989–1994 | Blinded, prospective collection of derivation and validation set data | Myocardial infarction,pulmonary edema, ventricular fibrillation or cardiac arrest, complete heart block; 36 outcomes occurred | 2.5% | |
| Steyerberg7 | Consecutive patients for primary elective abdominal aortic aneurysm surgery at a university hospital in the Netherlandsd | 238/None; 1977–1988 | Unclear whether data collection was prospective and whether reviewer was blinded | Surgical mortality; 18 deaths | 7.6% | |
| L’Italien8 | Consecutive vascular surgery patients at 5 teaching hospitals referred to their respective institutions’ nuclear cardiology laboratory for preoperative ipyridamole-thallium testing.e | 567/514; 1988–1991 | Derivation data collection was retrospective; validation data collection was prospective. Unclear whether reviewer was blinded | Cardiac death, fatal/nonfatal myocardial infarction, not pulmonary edema or congestive heart failure; 39 outcomes occurred | Surgical type | Training/Validation sets |
| Aortic | 6% / 6% | |||||
| Infrainguinal | 13% / 10% | |||||
| Carotid | 6% / 6% | |||||
| Total | 8% / 8% | |||||
| All studies described the mathematical model used in constructing the decision rule. None of the studies reported measuring the clinical effect of applying the decision rule. It is evident most rules are based on studies with methodologic concerns and relatively small numbers of target outcomes. The small numbers of outcome events in any 1 subgroup, group, or study means that a difference of 1 or 2 more or fewer outcomes could substantially change the reported results, especially the pretest probability. | ||||||
| *Blinding of postoperative evaluators to preoperative information and classification. | ||||||
| †Overall rate in study of target outcomes when more specific data are not available. | ||||||
| ‡First percentage: Rate of cardiac death, myocardial infarction, pulmonary edema; second percentage additionally includes worsened coronary insufficiency and congestive heart failure without pulmonary edema. | ||||||
| a. "Not a sample of consecutive patients undergoing surgery, and, therefore, our pretest probabilities will be higher than those that would be found in [a consecutive series]." | ||||||
| b. Because 1977 data excluded minor surgery, unclear how 1995 revision was constructed to include patients undergoing minor procedures. Subject to ascertainment bias because all patients were not studied postoperatively for silent myocardial infarction and other complications. | ||||||
| c. Validation set performed poorly for abdominal aortic aneurysm surgery; authors speculated low number of patients (~100) in derivation set responsible. | ||||||
| d. Patient sample from Netherlands. 238 patients represents "core" because authors used "unique" methods ("We used a new statistical method to quantify the combined effect...") that may be subject to question to "expand" their sample size beyond the actual number of patients studied. | ||||||
| e. Applicable to vascular surgery candidates who require preoperative nuclear stress tests. | ||||||
| N/A, not applicable, none or not specified, not available; TURP, transurethral prostatectomy. | ||||||
Assessing risk factors
Regardless of the risk assessment strategy, physicians should avoid overly aggressive preoperative investigation. The ACC/AHA state in their guideline on perioperative risk assessment that “intervention is rarely necessary simply to lower the risk of surgery unless such intervention is indicated irrespective of the preoperative context.”1
Coronary arteriography has a 0.3% mortality risk. Coronary artery bypass grafting (CABG) is associated with an overall operative mortality risk of 3%.11 In patients undergoing noncardiac surgery who have significant coronary artery disease without antecedent CABG, overall cardiac mortality is 2.4%, compared with 0.5% for those with antecedent CABG.12 Therefore, performing otherwise unnecessary bypass grafting simply to lower the risk of a subsequent surgical procedure incurs an antecedent mortality of greater than 3% from the CABG, whereas proceeding directly to the indicated procedure, on average, produces a 2.4% cardiac mortality.
However, patients who are otherwise candidates for CABG may be first identified when being evaluated for another surgical procedure. In such cases, when the intended surgery can be safely delayed, performing the CABG first is then most logical because the combined mortality of the procedures will be lowest when the CABG is performed first.
All of these tools focus exclusively on cardiovascular risk stratification or preoperative cardiac management (except the decision tool of Steyerburg et al 7; see below). Interestingly, few or none incorporate such risk factors as smoking, hypertension, or serum albumin, which are not independent predictors of major perioperative cardiac events. Two risk factors common to all algorithms are heart failure and prior myocardial infarction (MI). Seven of the 8 algorithms incorporate renal insufficiency, signs or symptoms of current coronary ischemia, and age. In branching algorithms, factors that may be included in an algorithm may not always be considered for a particular patient.
Electronic Decision Tools
STAT Cardiac Clearance
STAT Cardiac Clearance (STAT CC) version 1.1 (March 2002) is single-function software that exclusively performs cardiac preoperative assessment. After starting the program, the user chooses between the ACC/AHA 2002 algorithm and the ACP 1997 algorithm. Both of these algorithms provide management recommendations based on patient characteristics and surgical type. Both algorithms present users a series of yes/no questions (Figure 1), check boxes, and multiple choice questions, all completed by a tap with the stylus on the handheld computer’s touch-sensitive screen.
For the ACP algorithm, users eventually arrive at a management recommendation, such as “Sequence coronary revascularization and noncardiac management according to relative urgency of each and patient preference” or “Proceed directly to surgery.” Similarly, following the ACC/AHA algorithm, users receive recommendations such as “Operating room. Postoperative risk stratification and risk factor management.” The only problem in following either protocol’s implementation for the handheld is STAT CC-ACP algorithm’s use of “creatinine >260 mmol/L” (this value should be 260 μmol/L) and failure to note that this value is equivalent to 3 mg/dL. Both algorithms include patients with known coronary heart disease and patients undergoing major noncardiac and minor surgical procedures. The full text of the executive summary of the ACC/AHA article is available on STAT CC’s pull-down menu.
An addendum in the print version of the ACP protocol recommends “the perioperative use of atenolol in patients with coronary artery disease or risk factors for coronary artery disease… unless the patient has significant contraindications” based on information that became available after the guidelines were approved.2 This recommendation is not mentioned in the electronic implementation.
FIGURE 1
Stat Cardiac Clearance’s implementation of ACC/AHA guidelines
MedRules
MedRules (version 2.5, 2002) is a compilation of about 40 clinical prediction rules. Among these are 3 preoperative risk indices. Other than providing the literature citation for each rule, no assistance is provided in applying the rules. For example, users are not provided information to determine to which specific patient populations each rule applies.
MedRules’ Detsky calculator is a series of 3 screens of check boxes, all straightforward except the undefined “CCS Class” (Figure 2). Users can easily navigate among these screens to change entries if desired. The final result is a point total, risk class, and prediction of risk of major cardiac complications, eg, “15/100 points = class III: 20% risk of major cardiac complications.” Similarly, MedRules’ Goldman calculator is 3 screens of check boxes, also easily navigable in both directions.
In MedRules’ incarnation, an obvious major difference between the Detsky and Goldman implementations is Goldman’s categorization of surgical type into low-risk (minor) and high-risk (major) surgery. With other factors equal, risk of major cardiac complications may range from 3% (minor surgery) to 30% (high-risk procedure). An example result from MedRules’ Goldman index is “14/53 points = class III: 12% risk of major cardiac complications.” The original reference 4 and the software yield the same point totals and risk class.
However, at break points in the classification system, marked changes in risk occur with a 1-point differential in score. For example, for major noncardiac surgery, no difference in risk is reported between 6 and 12 points (4%) and no difference between 13 and 25 points (12%), but risk triples from 4% to 12% by adding 1 point from 12 to 13 points.
MedRules’ third algorithm, Lee’s Simple Cardiac Risk Score,5 fits on 2 screens. The maximum Lee score is 6 points. However, 1 point yields a risk of about 1%, whereas “class IV” is 3 or more points, for which the risk according to Lee et al5 is 9.1% in the derivation set and 11.0% in the validation set. For 3 or more points, MedRules’ calculator indicates “at high risk, >10% risk of major cardiac complications.” At 2 points, the risk is estimated at 7%, regardless of which factors are selected. With either 0 or 1 point, the Lee calculator returns a “<1% risk of major cardiac complications,” even if that risk is abdominal aortic aneurysm repair or a positive exercise stress test.
Obviously, with a 6-point scale and essentially 3 risk categories (in MedRules’ implementation, <1%, 7%, >10%), the Lee algorithm is extremely insensitive to small changes in risk.
FIGURE 2
MedRules’ Detsky calculator
InfoRetriever
The 3 preoperative risk assessment tools on InfoRetriever (version 4.2 for Palm OS, 2002) comprise a tiny piece of this large (by palmtop standards) 2088K (2.1MB) collection of 90 clinical decision rules and other clinical tools. InfoRetriever’s opening screen offers a choice among “Clinical decision rules,” “Diagnostic tests,” and “History and physical.” After choosing “Clinical decision rules,” the user taps to invoke a drop-down menu, and then selects “CV–pre-op eval.” At this point, choices for 3 decision rules appear: “AAA surgery” (Steyerberg), “Non-vascular surgery” (Detsky), and “Vascular surgery” (L’Italien).
The major difference between InfoRetriever’s and MedRules’ Detsky calculators is that InfoRetriever divides surgery into major or minor procedures. The 2 algorithms also differ in asking whether unstable angina has been present in the past 3 months (MedRules) or past 6 months (InfoRetriever). Interestingly, Detsky’s 2 publications about his 1 study also differ in this regard.3,6 InfoRetriever defines angina class, eg, “class III: symptoms w/ level walking of 1 to 2 blocks or climbing ≥1 flight stairs,” whereas MedRules does not. Both of Detsky’s publications allow users to choose any desired pretest probability (overall operation-specific surgical risk) and, from a nomogram that includes the Detsky score, find the corresponding posttest probability (patient’s specific calculated risk).
Neither InfoRetriever’s nor MedRules’ Detsky calculators allow user input of pretest probability. InfoRetriever uses 2 stated, predetermined pretest probabilities (eg, 5% and 10%) and generates 2 corresponding, patient-specific posttest probabilities. MedRules uses a single, unstated pretest probability. Therefore, although both programs accurately calculate Detsky point totals, we conclude that neither completely reproduces the originally published material.
Comparing results between InfoRetriever’s and MedRules’ Detsky calculators, entering the same data for a patient whose MedRules’ Detsky result is 25/100 points, or a 20% risk of major cardiac complications, into InfoRetriever’s Detsky calculator results in “Moderate risk (II): Peri-operative risk of MI, CHF, or death is 15.9% given a pretest risk of 5%; 28.5% given a pretest risk of 10%.” Entering a higher-risk patient, MedRules’ Detsky calculates 40/100 points, and a “100% risk of major cardiac complications,” whereas InfoRetriever’s Detsky calculation produces “44% given a pretest risk of 5%, 62.3% given a pretest risk of 10%.” In contrast to MedRules, for this (and its other indices), InfoRetriever’s information screens discuss the patient population, provide a “quality score” (but no explanation of it) for the index’s referenced study, and specify the number of patients in the study. However, we believe this information is inadequate to guide clinicians in using the indices.
InfoRetriever’s vascular surgery risk index includes risk stratification based on whether a dipyridamole-thallium stress test was performed and, if so, whether a fixed defect, reversible defect, ≥1 mm ST segment depression, or any combination of these findings, was identified.8 The calculator requires the “complication rate at your institution (%),” without providing additional assistance. From the article by L’Italien et al,8 the reader can infer that the “average risk of a major perioperative cardiac event among vascular surgery candidates” would be acceptable as the input for the complication rate. However, the pretest probability for the specific type of vascular surgery (eg, carotid, infrainguinal) would be preferable (Table 2). Study end points were cardiac death, fatal and nonfatal MI, but not pulmonary edema caused by cardiac ischemia.
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.
1. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force onPractice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002;39:542-53.
2. Guidelines for assessing and managing the perioperative risk from coronary artery disease associated with major noncardiac surgery-American College of Physicians. Ann Intern Med 1997;127:309-12.Also available at: http://www.acponline.org/journals/annals/15aug97/ppcad1.htm.
3. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 1986;146:2131-4.
4. Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333:1750-6.
5. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9.
6. Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986;1:211-9.
7. Steyerberg EW, Kievit J, de Mol Van Otterloo JC, van Bockel JH, Eijkemans MJ, Habbema JD. Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Arch Intern Med 1995;155:1998-2004.
8. L’Italien GJ, Paul SD, Hendel RC, et al. Development and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candidates. J Am Coll Cardiol 1996;27:779-86.
9. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
10. Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985;313:793-9.
11. Romero L, de Virgilio C. Preoperative cardiac risk assessment: an updated approach. Arch Surg 2001;136:1370-6.
12. Hollenberg SM. Preoperative cardiac risk assessment. Chest 1999;115(suppl):51S-57S.
13. Paul SD, Eagle KA. A stepwise strategy for coronary risk assessment for noncardiac surgery. Med Clin North Am 1995;79:1241-62.