User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Nivolumab linked to CNS disorder in case report
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
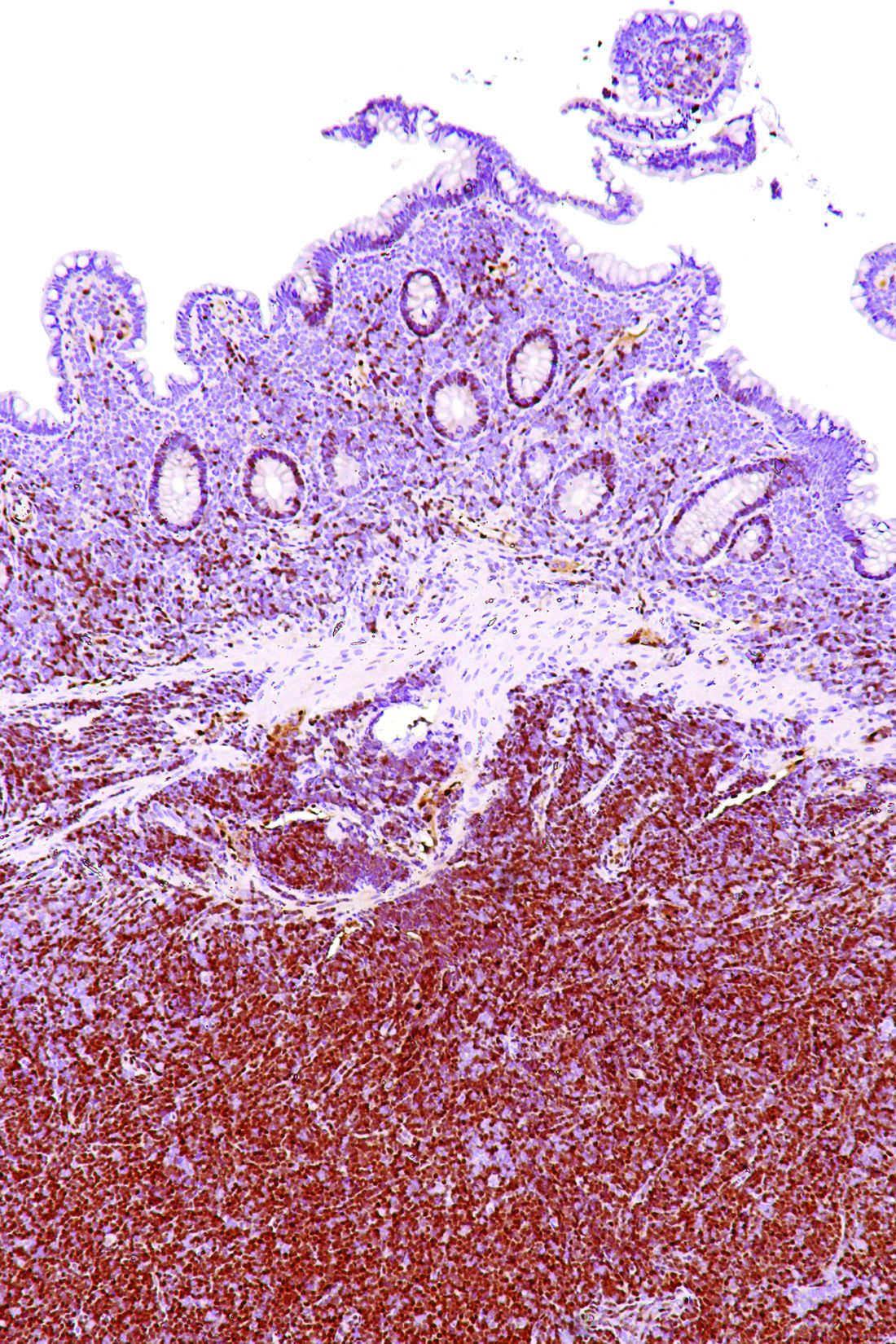
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
Autoimmune encephalitis may be a potentially severe complication of immune checkpoint inhibitor therapy, a case report suggests.
The recently published report describes a 53-year-old man with B-cell non-Hodgkin lymphoma who presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with the immune checkpoint inhibitor nivolumab.
Neuropathologic examination of a biopsied brain lesion found on cranial MRI showed a T cell–dominated inflammatory process thought to be autoimmune in origin, according to Herwig Strik, MD, of the department of neurology at Philipps University of Marburg (Germany), and his colleagues (Eur J Cancer. 2017 Oct 16. doi: 10.1016/j.ejca.2017.09.026).
After the patient stopped taking nivolumab and the inflammatory process was treated, his “clinical neurological and radiological status remained stable but disabling with fluctuating dysarthria and ataxia,” Dr. Strik and his colleagues wrote.
“Since these novel anticancer agents are increasingly used, this severe complication should be recognized soon and treatment should be terminated to avoid chronification,” they said in the report.
Nivolumab and other checkpoint inhibitors are known to have autoimmune side effects in some cases that can affect the pulmonary, gastrointestinal, and endocrine systems, the authors said.
Several previous case reports have detailed encephalitis occurring in cancer patients receiving nivolumab, the combination of nivolumab plus the immune checkpoint inhibitor ipilimumab, or ipilimumab alone. The authors said they believe that this case report is the first to describe multifocal CNS inflammation following nivolumab treatment for systemic lymphoma.
The patient was diagnosed with B-cell non-Hodgkin lymphoma in 2005, according to the case report. He was first treated in 2009 with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), followed by stem cell apheresis, radioimmunotherapy, and rituximab; he then received R-DHAP (rituximab, dexamethasone, high-dose cytarabine, and cisplatin) in August 2014, followed by autologous stem cell transplantation in October of that year. The patient started nivolumab maintenance therapy in February 2015 but started experiencing neurological symptoms that eventually led to ending nivolumab treatment in September 2015.
The patient’s lymphoma relapsed in June 2016. “The disabling neurological symptoms and his personal situation, however, worsened the patient’s depressive symptoms so severely that he went abroad to commit assisted suicide,” wrote Dr. Strik and his colleagues.
The authors proposed the term “immune checkpoint inhibitor–associated CNS autoimmune disorder (ICICAD)” to describe the inflammatory condition described in the case report.
They declared no conflicts of interest related to the case report and did not receive grant support for conducting the research described in it.
FROM THE EUROPEAN JOURNAL OF CANCER
Key clinical point: Autoimmune encephalitis may be a potential complication of checkpoint inhibitor therapy.
Major finding: A patient with B-cell non-Hodgkin lymphoma presented with double vision, ataxia, impaired speech, and mild cognitive dysfunction following treatment with nivolumab. Examination of a brain lesion showed a T cell–dominated inflammatory process thought to be autoimmune in origin.
Data source: A case report of a 53-year-old man with B-cell non-Hodgkin lymphoma (B-NHL) who received nivolumab maintenance treatment.
Disclosures: The authors declared no conflicts of interest and did not receive grant support for the research.
Rituximab improves salvage in elderly B-cell lymphoma patients
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
In elderly patients with aggressive B-cell lymphomas who experience treatment failure after CHOP or rituximab-CHOP (R-CHOP), the outcomes of subsequent salvage therapy were improved when rituximab was included, results of a retrospective analysis suggest.
“Survival after rituximab-containing salvage therapy was better in all patient groups, supporting the repeated administration of rituximab to all patients needing salvage therapy,” wrote investigator Bertram Glass, MD, of the department of hematology and stem cell transplantation at Helios Klinikum Berlin-Buch, Berlin, and his coauthors (Ann Oncol. 2017 Oct 6. doi: 10.1093/annonc/mdx556).
Dr. Glass and colleagues reviewed data from the randomized RICOVER-60 trial, which included 1,222 patients aged 61-80 years with aggressive B-cell lymphomas who received CHOP or R-CHOP for six or eight cycles. Based on survival outcomes, six cycles of R-CHOP every 2 weeks should be the preferred regimen, investigators wrote when the study results were published in 2008 (Lancet Oncol. 2008;9[2]:105-16. doi: 10.1016/S1470-2045(08)70002-0).
Of 1,222 patients in the RICOVER-60 trial, 301 (24.6%) had treatment failure, of whom 297 could be included in the present analysis.
Rituximab, included in salvage therapy for 57.4% of those evaluable patients, was found to improve the 2-year survival rate from 20.7% to 46.8% (P less than .001), Dr. Glass and his coinvestigators reported.
The benefit of rituximab in the salvage setting was apparent regardless of whether patients received R-CHOP or CHOP as part of their initial therapy in RICOVER-60, they added.
Among patients who had received CHOP as first-line therapy, 2-year overall survival was 49.6% for those who received rituximab in the salvage setting, compared with 19.1% for those who did not (P less than .001), according to the published data. Likewise, in the initial R-CHOP group, 2-year overall survival was 33.1% for rituximab in salvage and 22.5% for no rituximab in salvage (P = .034).
The investigators also looked for differences in prognosis according to specific patient characteristics, including presence of MYC rearrangements and MYC expression by immunohistochemistry.
In patients with MYC translocation at diagnosis, use of rituximab reduced risk of initial treatment failure from 58.8% to 26.3%, according to the investigators. After treatment failure, patients who initially received CHOP had significantly improved 2-year survival if they had MYC translocations or negative MYC immunohistochemistry, though no such association was found for patients who initially received R-CHOP, they wrote.
Dr. Glass and colleagues concluded that new treatment strategies are needed.
“Overall, the outcome of second-line treatment of elderly patients with refractory and relapsed aggressive B-cell lymphoma is disappointing and worse than in younger patients regardless of the modality chosen,” they wrote. “New drugs and treatment modalities with the potential to change the dismal outlook for elderly patients with aggressive B-cell lymphomas are eagerly awaited.”
Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
FROM ANNALS OF ONCOLOGY
Key clinical point: Rituximab improved salvage therapy for elderly patients with aggressive-B-cell lymphoma who relapsed after CHOP or R-CHOP.
Major finding: Rituximab as part of a salvage regimen improved the 2-year survival rate from 20.7% to 46.8% (P less than .001).
Data source: Retrospective analysis including 297 elderly patients in the RICOVER-60 trial who had progressive, persistent, or relapsed lymphoma.
Disclosures: Dr. Glass and several coauthors reported honoraria, research funding, and consultancies with Roche.
FDA approves second CAR-T therapy
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
A second chimeric antigen receptor (CAR) T-cell therapy has gained FDA approval, this time for the treatment of large B-cell lymphoma in adults.
“Today marks another milestone in the development of a whole new scientific paradigm for the treatment of serious diseases,” FDA Commissioner Scott Gottlieb, MD, said in a statement. “This approval demonstrates the continued momentum of this promising new area of medicine, and we’re committed to supporting and helping expedite the development of these products.”
Approval was based on ZUMA-1, a multicenter clinical trial of 101 adults with refractory or relapsed large B-cell lymphoma. Almost three-quarters (72%) of patients responded, including 51% who achieved complete remission.
CAR-T therapy can cause severe, life-threatening side effects, most notably cytokine release syndrome (CRS) and neurologic toxicities, for which axicabtagene ciloleucel will carry a boxed warning and will come with a risk evaluation and mitigation strategy (REMS), according to the FDA.
The list price for a single treatment of axicabtagene ciloleucel is $373,000, according to the manufacturer.
“We will soon release a comprehensive policy to address how we plan to support the development of cell-based regenerative medicine,” Dr. Gottlieb said in a statement. “That policy will also clarify how we will apply our expedited programs to breakthrough products that use CAR-T cells and other gene therapies. We remain committed to supporting the efficient development of safe and effective treatments that leverage these new scientific platforms.”
Axicabtagene ciloleucel was developed by Kite Pharma, which was acquired recently by Gilead Sciences.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
Obinutuzumab edges out rituximab for PFS in follicular lymphoma
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
Should obinutuzumab replace rituximab as the standard antibody in the treatment of patients receiving chemoimmunotherapy regimens for follicular lymphoma? Results from this trial would suggest that there might be no advantage for an obinutuzumab-containing chemoimmunotherapy regimen if maintenance treatment was not planned. Even with maintenance therapy, there is no evidence from this trial of an overall survival benefit with obinutuzumab. These findings, combined with the higher rate of toxic effects and, presumably, the higher cost of obinutuzumab, raise important questions regarding the advantage of its use. This issue is complicated further because it is possible that giving rituximab at a dose of 1,000 mg might reduce or eliminate any difference in progression-free survival – that is, if the difference is primarily a dose effect.
When the data on minimal residual disease are made available, the case in favor of obinutuzumab may appear to be more compelling if indeed a higher proportion of patients who received obinutuzumab have minimal residual disease status at some point in treatment and remain in remission longer than those who received rituximab. At the moment, the competition between these agents looks too close to call.
These comments are excerpted from an editorial (N Engl J Med. 2017 Oct 5;377;14:1389-90) by James O. Armitage, MD, University of Nebraska, Omaha, and Dan L. Longo, MD, Dana-Farber Cancer Institute, Boston. Dr. Armitage reported personal fees from Conatus, Samus Therapeutics, and Tesaro. Dr. Longo reported no relevant disclosures. He is deputy editor of The New England Journal of Medicine.
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
In a head-to-head trial of anti-CD20 monoclonal antibodies in first-line therapy for follicular lymphoma, obinutuzumab-based chemotherapy was associated with slightly but significantly better progression-free survival than rituximab-based therapy, but at the cost of higher toxicities, including severe adverse events.
Among 1,202 patients with follicular lymphoma followed for a median of 34.5 months, the estimated 3-year rate of progression-free survival (PFS) for patients randomized to obinutuzumab-based chemotherapy and maintenance was 80%, compared with 73.3% for patients randomized to rituximab chemotherapy and maintenance. Response rates and overall survival were similar between the treatment groups, Robert Marcus, MB, BS, of King’s College Hospital, London, and his coinvestigators reported in the GALLIUM trial.
They acknowledged, however, that there were substantial differences between the treatment groups in the cumulative doses of obinutuzumab (Gazyva) and rituximab (Rituxan and others), which could have affected the relative efficacy of each regimen.
In addition, while patients were randomly assigned to one monoclonal antibody or the other, the choice of chemotherapy regimens, while standardized, was left to the discretion of investigators at each treatment site, another factor that might have influenced outcomes.
The investigators reported the results of a preplanned interim efficacy analysis. They compared obinutuzumab or rituximab plus chemotherapy in patients with indolent non-Hodgkin lymphoma, but the trial was powered to detect a PFS difference only in patients with follicular lymphoma. Patients who had a clinical response to induction therapy went on to maintenance therapy with the same monoclonal antibody.
In all, 1,202 patients with follicular lymphoma were enrolled and randomized, 601 in each arm, to receive induction with either intravenous obinutuzumab 1,000 mg on days 1, 8, and 15 of cycle 1 and on day 1 of subsequent cycles, or rituximab 375 mg/m2 on day 1 of each cycle for six or eight cycles, depending on the accompanying chemotherapy regimen. The regimens used were either CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), CVP (cyclophosphamide, vincristine, and prednisone), or bendamustine.
Patients with partial or complete responses were then maintained on the same monoclonal antibody they had received during induction, either obinutuzumab 1,000 mg or rituximab 375 mg/m2 every 2 months for 2 years, or until disease progression. Patients were not allowed to be crossed over to the other maintenance therapy.
Patients with stable disease after induction continued to be followed, but did not receive maintenance therapy.
The interim analysis was performed after 245 of 370 anticipated events (disease progression, relapse, or death) had occurred. At that time, the independent data and safety monitoring committee recommended full analysis of the trial data, and the sponsor agreed.
After a median follow-up of 34.5 months, an intention-to-treat analysis showed that the investigator-assessed, estimated 3-year rate of PFS was 80.0% in the obinutuzumab arm, compared with 73.3%; in the rituximab arm. This translated into a hazard ratio (HR) for progression, relapse, or death of 0.66 (P = .001). An independent review committee calculated a HR favoring obinutuzumab of 0.71 (P = .01).
Estimated 3-year overall survival rates were not significantly different at 94% and 92.1%, respectively.
Overall response rates were similar between the groups, at 88.5% with obinutuzumab group and 86.9% with rituximab, a difference that was not significant.
Obinutuzumab was associated with a higher rate of prespecified events of special interest, including infections, cardiac events, second neoplasms, infusion-related events, neutropenia, and thrombocytopenia.
Adverse events deemed to be related to the antibodies occurred in 59.3% of patients on obinutuzumab, and 48.9% of patients on rituximab.
There were more frequent grade 3 or 4 adverse events and deaths with obinutuzumab, occurring in 74.6% of patients vs. 67.8% on rituximab. Fatal adverse events occurred in 4% and 3.4% of patients, respectively.
A total of 81 patients died during the trial, including 35 in the obinutuzumab group and 46 in the rituximab group.
F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Obinutuzumab-based chemotherapy and maintenance was associated with better progression-free survival, but not overall survival, compared with rituximab-based chemotherapy and maintenance.
Major finding: Three-year progression-free survival was 80% with obinutuzumab, vs. 73.3% with rituximab.
Data source: Interim analysis of a randomized phase 3, open-label trial of 1,202 patients with follicular lymphoma.
Disclosures: F. Hoffmann–La Roche supported the trial. Dr. Marcus disclosed consulting fees and lecture fees from Takeda Pharmaceuticals and travel support, consulting fees, and lecture fees from Roche. The majority of coauthors disclosed similar relationships.
VCR regimen showed efficacy in mantle cell and indolent lymphomas
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
The combination of bortezomib, cladribine, and rituximab (VCR) was an effective treatment regimen for patients with CD20-positive mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), based on results of a recent phase 2, open-label study.
The overall response rate was 92% in the single-center, 24-patient study. The 2-year progression-free survival (PFS) was 82% and 54%, respectively, for MCL and iNHL patients; PFS was 80% for treatment-naive patients and 57% for those with refractory/recalcitrant disease, according to Soham D. Puvvada, MD, of the University of Arizona Cancer Center in Tucson, and her associates.
Two-year overall survival was 91% for MCL and 69% for iNHL patients. Median time to progression was 34.5 months, and median PFS had not been reached at 2 years, according to the researchers.
While the study (NCT00980395) was small and limited by its single-center design, the VCR combination “has encouraging activity in both MCL and iNHL and could be compared to standard therapies in future studies,” the researchers wrote. “For MCL in particular, we believe a noninferiority comparison to standard therapies would be justified by our results.”
Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia, data show.
“Although hematological toxicity can be an issue, the regimen provides an alternative option in transplant ineligible relapsed/refractory MCL and iNHL,” wrote Dr. Puvvada and her colleagues. The study was published in Clinical Lymphoma, Myeloma & Leukemia (doi: 10.1016/j.clml.2017.09.001).
The researchers studied the combination of bortezomib, the proteasome inhibitor initially approved for relapsed/refractory MCL, cladribine, which has shown activity and promising response rates in patients with indolent lymphomas, and rituximab in patients with CD20-positive mantle cell or indolent lymphoma.
Patients with follicular lymphomas were eligible to be included in the study if they had received at least one previous line of therapy. All other participants could be treatment naive or have relapsed after previous treatment.
Of the 24 patients enrolled, 11 had MCL, 5 had follicular lymphoma, 4 had marginal zone lymphoma, 3 had lymphoplasmacytic lymphoma, and 1 had small lymphocytic lymphoma.
The VCR regimen, given every 28 days for no more than six cycles, included rituximab at 375 mg/m2 given intravenously on day 1 of each cycle, cladribine 4 mg/m2 given intravenously over 2 hours on days 1 through 5, and bortezomib 1.3 mg/m2 given intravenously on days 1 and 4. Patients received a median of five cycles of therapy.
Adverse events of grade 3 or greater occurred in 14 patients (58%); 8 patients had leukopenia, 6 had thrombocytopenia, 5 had fatigue, and 5 had neutropenia, which included febrile neutropenia in 3 patients.
With a median follow-up of 38.5 months, overall response rate for VCR was 96%. Complete responses occurred in 8 of 23 evaluable patients (35%) and partial responses in 14 more patients (61%).
FROM LYMPHOMA, MYELOMA & LEUKEMIA
Key clinical point:
Major finding: The overall response rate was 92%, with a 2-year PFS of 82% and 54% for patients with mantle cell lymphoma (MCL) and indolent non-Hodgkin’s lymphoma (iNHL), respectively. Adverse events were most commonly hematologic, and three patients experienced febrile neutropenia.
Data source: A phase 2, open-label study including 24 patients with mantle cell or indolent lymphomas.
Disclosures: No disclosures were reported in the accepted manuscript.
Adding bortezomib to R-CHOP didn’t improve survival in diffuse large B-cell lymphoma
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
, findings from the phase-2 PYRAMID trial showed.
When the proteasome inhibitor bortezomib was combined with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously untreated non–germinal center B-cell–like (non-GCB) DLBCL, a significant improvement in progression-free survival (PFS) was not observed.
There also was no increase in 2-year PFS among patients treated with the combination of bortezomib plus R-CHOP (VR-CHOP), according to findings from the open-label, randomized study published in the Journal of Clinical Oncology (2017 Sep 1. doi: 10.1200/JCO.2017.73.2784).
“A potential reason for the lack of benefit with VR-CHOP was that only two doses of bortezomib were given per 21-day cycle, whereas the standard schedule for bortezomib in multiple myeloma is four doses per cycle on days 1, 4, 8, and 11,” wrote John P. Leonard, MD, of Weill Cornell Medicine and New York Presbyterian Hospital, New York, and his colleagues. “In this study, treatment duration was limited to six 21-day cycles of R-CHOP.”
The authors noted that previous research has demonstrated the feasibility of using VR-CHOP and similar immunochemotherapy regimens in DLBCL. In the current PYRAMID (Personalized Lymphoma Therapy: Randomized Study of Proteasome Inhibition in Non-GCB DLBCL) phase 2 trial, VR-CHOP was compared with R-CHOP in 206 patients with previously untreated non-GCB DLBCL who were selected by real-time subtyping conducted or confirmed at a central laboratory that used the Hans algorithm.
The cohort was randomized to receive six 21-day cycles of standard R-CHOP alone or R-CHOP plus bortezomib 1.3 mg/m2 intravenously on days 1 and 4, and the primary endpoint was PFS.
The hazard ratio (HR) for PFS was 0.73 (90% confidence interval, 0.43-1.24) and favored VR-CHOP (P = .611), while the median PFS was not reached in either group. At 2 years, PFS was 77.6% with R-CHOP, versus 82.0% with VR-CHOP.
Among patients with high-intermediate/high International Prognostic Index (IPI) risk, those rates were 65.1% with R-CHOP, versus 72.4% with VR-CHOP (HR, 0.67; 90% CI, 0.34-1.29; P = .606). For those patients at low/low-intermediate IPI risk, the rates were 90.0% for R-CHOP, versus 88.9% for VR-CHOP (HR, 0.85; 90% CI, 0.35-2.10; P = .958).
The overall response rate was 98% for R-CHOP patients and 96% for VR-CHOP, with complete response rates of 49% and 56%, respectively.
Time to progression rates at 2 years were 79.8% for R-CHOP, versus 83.0% with VR-CHOP (HR, 0.79; 90% CI, 0.45-1.37; P = .767). While median overall survival was not reached in either arm, the HR for the entire cohort was 0.75 (90% CI, 0.38-1.45; P = .763). Two-year overall survival was 88.4% and 93.0%, respectively.
In the high-intermediate/high IPI score group, 2-year overall survival was 79.2% with R-CHOP, versus 92.1% with VR-CHOP (HR, 0.62; 90% CI, 0.25-1.42; P = .638), and for those with low/low-intermediate IPI risk scores, 97.7% versus 93.8% (HR, 1.02; 90% CI, 0.34-3.27; P = .999).
Millennium Pharmaceuticals supported the study. Dr. Leonard and several of the coauthors reported relationships with industry.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Bortezomib combined with R-CHOP did not improve outcomes significantly in diffuse large B-cell lymphoma.
Major finding: Two-year progression-free survival was 77.6% with R-CHOP, compared with 82.0% with VR-CHOP, a nonsignificant difference.
Data source: An open-label, randomized, phase 2 trial that compared VR-CHOP to R-CHOP in 206 patients with previously untreated non-GCB DLBCL.
Disclosures: Millennium Pharmaceuticals funded the study. Dr. Leonard and several of the coauthors reported relationships with industry.
FDA grants accelerated approval to copanlisib for relapsed follicular lymphoma
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
The Food and Drug Administration has granted accelerated approval to copanlisib (Aliqopa) for the treatment of adults with relapsed follicular lymphoma who have received at least two prior treatments.
Approval of the kinase inhibitor was based on an overall response rate of 59% in a single-arm trial of 104 patients with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. These patients had a complete or partial response for a median 12.2 months.
“For patients with relapsed follicular lymphoma, the cancer often comes back even after multiple treatments,” Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research said in the press release. “Options are limited for these patients and today’s approval provides an additional choice for treatment, filling an unmet need for them,” he said.
Biosimilar matches rituximab in large follicular lymphoma trial
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
MADRID – The biosimilar GP2013 met the criteria for therapeutic equivalence to rituximab in a large comparator trial of previously untreated patients with aggressive follicular lymphoma.
Based on results presented at the European Society for Medical Oncology Congress, “there is absolutely no difference in the objective response rates for GP2013 and rituximab,” the primary endpoint of the trial, reported Wojciech Jurczak, MD, PhD, head of lymphoma, department of hematology, Jagiellonian University, Krakow, Poland.
Dr. Jurczak characterized the double-blind, randomized phase 3 trial ASSIST_FL (NCT01419665) as the “largest biosimilar trial in hematology.” For the study, 629 patients with previously untreated, advanced-stage follicular lymphoma were randomized to GP2013 and the conventional regimen of cyclophosphamide, vincristine, and prednisone (G-CVP) or rituximab and the same three-agent regimen (R-CVP). Each regimen was given for eight cycles followed by maintenance monotherapy with the assigned monoclonal antibody for up to 2 years.
The primary endpoint, objective response rate (ORR), was 87.1% and 87.5% for G-CVP and R-CVP, respectively. There were no differences in ORR among the subgroups evaluated, which included patients aged 60 years and older vs. younger patients, presence or absence of bulky disease, high or low FLIPI (Follicular Lymphoma International Prognostic Index) score, gender, and the geographic region where treatment was given.
Safety was a secondary endpoint evaluated at the end of eight cycles and again after a year of maintenance therapy. The proportion of patients with any adverse event and the proportion with grade 3 or greater adverse events were not statistically different at any time point. There were also no significant differences in any of the other secondary endpoints evaluated, which included pharmacokinetic, pharmacodynamic, and immune measures.
The results are consistent with those of a related randomized bioequivalence trial comparing GP2013 and rituximab in 312 patients with rheumatoid arthritis (Ann Rheum Dis. 2017;76:1598-1602). The primary endpoint in that trial was area-under-the-curve serum concentration time.
The two studies are mutually reinforcing, and “the ASSIST_FL trial ends the story. We have the totality of evidence that GP2013 can be considered a biosimilar,” said Dr. Jurczak, who anticipates “major price differences” for this agent relative to rituximab.
“We may, based on the results of the follicular lymphoma trial, use the biosimilar in all registered indications for rituximab,” said Dr. Jurczak. This is also the conclusion of the European Medicine Agency, which approved this agent in June 2017 for all rituximab indications.
In explaining the process for approval of biosimilars, Dr. Jurczak emphasized that demonstrating bioequivalence is not the same as the approval process for a new therapeutic agent, for which regulatory agents require a demonstration of efficacy on a meaningful clinical endpoint, such as progression-free survival. For biosimilars, it is not necessary to show clinical benefits. Biosimilars must demonstrate the same biological activity, and ORR is considered an acceptable measure.
The ESMO-invited discussant, Michele Ghielmini, MD, PhD, medical director at the Oncology Institute of Southern Switzerland, Bellinzona, agreed. “We can reasonably speculate that (when rituximab and the biosimilar are associated with the same) response rate, they will lead to the same clinical benefits.”
AT ESMO 2017
Key clinical point:
Major finding: The objective response rates were 87.1% and 87.5% for G-CVP and R-CVP.
Data source: Double-blind, multicenter randomized trial of 629 patients with previously untreated, advanced-stage follicular lymphoma.
Disclosures: Dr. Jurczak reported financial relationships with Sandoz.
FDA grants Priority Review to Gazyva for follicular lymphoma
Gazyva (obinutuzumab) has been granted a Priority Review by the Food and Drug Administration for the treatment of previously untreated follicular lymphoma, according to a press release from Genentech.
FDA approval was based on results from the GALLIUM study, a phase 3 trial comparing Gazyva to Rituxan (rituximab). Patients who received Gazyva plus chemotherapy followed by Gazyva therapy alone for 2 years had a 32% improvement in progression-free survival during the 41.1 month follow-up period, compared with the patient group who received Rituxan plus chemotherapy followed by 2 years of Rituxan therapy alone. Median progression-free survival has not been reached in either arm of the study.
The most common adverse events that occurred more often in the Gazyva arm of the study were low white blood cell count, infections, infusion-related reactions, low platelet count, new tumors, and cardiac events.
“Based on the GALLIUM study, Gazyva-based treatment significantly improved progression-free survival over the current standard of care, and we are committed to bringing this potential new option to patients as soon as possible,” Dr. Sandra Horning, chief medical officer and head of Genentech’s Global Product Development said in the press release.
The FDA is expected to make a decision on approval under Priority Review by Dec. 23, 2017.
Find the full press release on the Genentech website.
Gazyva (obinutuzumab) has been granted a Priority Review by the Food and Drug Administration for the treatment of previously untreated follicular lymphoma, according to a press release from Genentech.
FDA approval was based on results from the GALLIUM study, a phase 3 trial comparing Gazyva to Rituxan (rituximab). Patients who received Gazyva plus chemotherapy followed by Gazyva therapy alone for 2 years had a 32% improvement in progression-free survival during the 41.1 month follow-up period, compared with the patient group who received Rituxan plus chemotherapy followed by 2 years of Rituxan therapy alone. Median progression-free survival has not been reached in either arm of the study.
The most common adverse events that occurred more often in the Gazyva arm of the study were low white blood cell count, infections, infusion-related reactions, low platelet count, new tumors, and cardiac events.
“Based on the GALLIUM study, Gazyva-based treatment significantly improved progression-free survival over the current standard of care, and we are committed to bringing this potential new option to patients as soon as possible,” Dr. Sandra Horning, chief medical officer and head of Genentech’s Global Product Development said in the press release.
The FDA is expected to make a decision on approval under Priority Review by Dec. 23, 2017.
Find the full press release on the Genentech website.
Gazyva (obinutuzumab) has been granted a Priority Review by the Food and Drug Administration for the treatment of previously untreated follicular lymphoma, according to a press release from Genentech.
FDA approval was based on results from the GALLIUM study, a phase 3 trial comparing Gazyva to Rituxan (rituximab). Patients who received Gazyva plus chemotherapy followed by Gazyva therapy alone for 2 years had a 32% improvement in progression-free survival during the 41.1 month follow-up period, compared with the patient group who received Rituxan plus chemotherapy followed by 2 years of Rituxan therapy alone. Median progression-free survival has not been reached in either arm of the study.
The most common adverse events that occurred more often in the Gazyva arm of the study were low white blood cell count, infections, infusion-related reactions, low platelet count, new tumors, and cardiac events.
“Based on the GALLIUM study, Gazyva-based treatment significantly improved progression-free survival over the current standard of care, and we are committed to bringing this potential new option to patients as soon as possible,” Dr. Sandra Horning, chief medical officer and head of Genentech’s Global Product Development said in the press release.
The FDA is expected to make a decision on approval under Priority Review by Dec. 23, 2017.
Find the full press release on the Genentech website.
Obinutuzumab-CHOP not superior to rituximab-CHOP in new DLBCL
Obinutuzumab with CHOP therapy did not improve progression-free survival, compared with rituximab plus CHOP, in patients with previously untreated diffuse large B-cell lymphoma (DLBCL), according to results from a phase 3 trial published in the Journal of Clinical Oncology. (2017 Aug 10. doi: 10.1200/JCO.2017.73.3402)
The findings suggest that obinutuzumab, a glycoengineered, type II, anti-CD20 monoclonal antibody, might not offer a benefit over standard treatment with rituximab, an anti-CD20 monoclonal antibody, when used with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
A total of 1,418 patients were enrolled at 207 centers in 29 countries in the GOYA trial and were randomly assigned to one regimen or the other. The mean duration of exposure to the drugs was 25 weeks for both. The progression-free survival was 69.6% for obinutuzumab-CHOP – also known as G-CHOP – and 66.9% for rituximab-CHOP, not a statistically significant difference, wrote Umberto Vitolo, MD, of University-Hospital Città della Salute e della Scienza, Torino, Italy, and his fellow investigators.
The rate of adverse events was similar between the two groups. The lack of superiority of obinutuzumab comes after findings of its superiority in untreated follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL). The investigators suggested that this may be a sign that obinutuzumab’s efficacy is best seen in less aggressive disease types.
“Given the advantages of G-based therapy in patients with FL and CLL, the lack of benefit of G-CHOP in patients with DLBCL in the GOYA study was unexpected, and the reasons for it are unclear,” they wrote. “This lack of benefit might simply have resulted from the differences in biologic and clinical profiles between indolent lymphoproliferative diseases, such as FL and CLL, and aggressive ones, such as DLBCL.”
The study was sponsored by F. Hoffman-La Roche, the manufacturer of the two drugs, and had support from Fondazione Italiana Linfomi.
Obinutuzumab with CHOP therapy did not improve progression-free survival, compared with rituximab plus CHOP, in patients with previously untreated diffuse large B-cell lymphoma (DLBCL), according to results from a phase 3 trial published in the Journal of Clinical Oncology. (2017 Aug 10. doi: 10.1200/JCO.2017.73.3402)
The findings suggest that obinutuzumab, a glycoengineered, type II, anti-CD20 monoclonal antibody, might not offer a benefit over standard treatment with rituximab, an anti-CD20 monoclonal antibody, when used with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
A total of 1,418 patients were enrolled at 207 centers in 29 countries in the GOYA trial and were randomly assigned to one regimen or the other. The mean duration of exposure to the drugs was 25 weeks for both. The progression-free survival was 69.6% for obinutuzumab-CHOP – also known as G-CHOP – and 66.9% for rituximab-CHOP, not a statistically significant difference, wrote Umberto Vitolo, MD, of University-Hospital Città della Salute e della Scienza, Torino, Italy, and his fellow investigators.
The rate of adverse events was similar between the two groups. The lack of superiority of obinutuzumab comes after findings of its superiority in untreated follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL). The investigators suggested that this may be a sign that obinutuzumab’s efficacy is best seen in less aggressive disease types.
“Given the advantages of G-based therapy in patients with FL and CLL, the lack of benefit of G-CHOP in patients with DLBCL in the GOYA study was unexpected, and the reasons for it are unclear,” they wrote. “This lack of benefit might simply have resulted from the differences in biologic and clinical profiles between indolent lymphoproliferative diseases, such as FL and CLL, and aggressive ones, such as DLBCL.”
The study was sponsored by F. Hoffman-La Roche, the manufacturer of the two drugs, and had support from Fondazione Italiana Linfomi.
Obinutuzumab with CHOP therapy did not improve progression-free survival, compared with rituximab plus CHOP, in patients with previously untreated diffuse large B-cell lymphoma (DLBCL), according to results from a phase 3 trial published in the Journal of Clinical Oncology. (2017 Aug 10. doi: 10.1200/JCO.2017.73.3402)
The findings suggest that obinutuzumab, a glycoengineered, type II, anti-CD20 monoclonal antibody, might not offer a benefit over standard treatment with rituximab, an anti-CD20 monoclonal antibody, when used with CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
A total of 1,418 patients were enrolled at 207 centers in 29 countries in the GOYA trial and were randomly assigned to one regimen or the other. The mean duration of exposure to the drugs was 25 weeks for both. The progression-free survival was 69.6% for obinutuzumab-CHOP – also known as G-CHOP – and 66.9% for rituximab-CHOP, not a statistically significant difference, wrote Umberto Vitolo, MD, of University-Hospital Città della Salute e della Scienza, Torino, Italy, and his fellow investigators.
The rate of adverse events was similar between the two groups. The lack of superiority of obinutuzumab comes after findings of its superiority in untreated follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL). The investigators suggested that this may be a sign that obinutuzumab’s efficacy is best seen in less aggressive disease types.
“Given the advantages of G-based therapy in patients with FL and CLL, the lack of benefit of G-CHOP in patients with DLBCL in the GOYA study was unexpected, and the reasons for it are unclear,” they wrote. “This lack of benefit might simply have resulted from the differences in biologic and clinical profiles between indolent lymphoproliferative diseases, such as FL and CLL, and aggressive ones, such as DLBCL.”
The study was sponsored by F. Hoffman-La Roche, the manufacturer of the two drugs, and had support from Fondazione Italiana Linfomi.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Obinutuzumab with CHOP therapy did not improve progression-free survival for diffuse large B-cell lymphoma, compared with standard treatment with rituximab used with CHOP.
Major finding: The estimated PFS was 69.6% for obinutuzumab-CHOP and 66.9% for rituximab-CHOP, an insignificant difference.
Data source: A randomized phase 3 trial of 1,418 patients at 207 centers in 29 countries.
Disclosures: The study was sponsored by F. Hoffman-La Roche, the manufacturer of the two drugs, and had support from Fondazione Italiana Linfomi..