User login
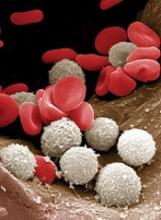
Bacterial infection inhibits hematopoiesis
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.” ![]()
Therapy shows promise for PUPs with severe hemophilia A
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study. ![]()
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study. ![]()
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study. ![]()
Addition of daratumumab improves PFS in MM, company says
Interim results of a phase 3 study suggest adding daratumumab to a 3-drug regimen can improve progression-free survival (PFS) in patients with newly diagnosed multiple myeloma (MM).
In the phase 3 ALCYONE study, researchers are comparing daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) to VMP alone in patients with newly diagnosed MM who are not considered candidates for autologous stem cell transplant.
Genmab A/S recently announced interim results from this trial and said additional data are expected to be submitted for presentation at an upcoming medical conference and for publication in a peer-reviewed journal.
The ALCYONE trial enrolled 706 patients who were randomized to receive 9 cycles of daratumumab plus VMP or VMP alone.
In the daratumumab arm, patients received 16 mg/kg of daratumumab once weekly for 6 weeks (cycle 1; 1 cycle = 42 days), followed by once every 3 weeks (cycles 2-9). After that, patients continued to receive 16 mg/kg of daratumumab once every 4 weeks until disease progression.
At the pre-planned interim analysis, the study’s primary endpoint was met. Treatment with daratumumab reduced the risk of disease progression or death by 50% when compared to VMP alone (hazard ratio=0.50; 95% CI 0.38-0.65; P<0.0001).
The median PFS has not been reached in the daratumumab arm but was an estimated 18.1 months for patients who received VMP alone.
Genmab said that, overall, the safety profile of daratumumab in combination with VMP is consistent with the known safety profile of the VMP regimen and the known safety profile of daratumumab.
Based on these results, an independent data monitoring committee recommended the data be unblinded. All patients will continue to be monitored for safety and overall survival.
Janssen Biotech, Inc., which licensed daratumumab from Genmab in 2012, said it will discuss with health authorities the potential for a regulatory submission for daratumumab in combination with VMP as a treatment for newly diagnosed MM.
Daratumumab is already approved in the US (as DARZALEX®) for use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat MM patients who have received at least 1 prior therapy.
Daratumumab is also approved for use in combination with pomalidomide and dexamethasone to treat MM patients who have received at least 2 prior therapies, including lenalidomide and a proteasome inhibitor (PI).
And daratumumab is approved as monotherapy for MM patients who have received at least 3 prior lines of therapy, including a PI and an immunomodulatory agent, or who are double-refractory to a PI and an immunomodulatory agent. ![]()
Interim results of a phase 3 study suggest adding daratumumab to a 3-drug regimen can improve progression-free survival (PFS) in patients with newly diagnosed multiple myeloma (MM).
In the phase 3 ALCYONE study, researchers are comparing daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) to VMP alone in patients with newly diagnosed MM who are not considered candidates for autologous stem cell transplant.
Genmab A/S recently announced interim results from this trial and said additional data are expected to be submitted for presentation at an upcoming medical conference and for publication in a peer-reviewed journal.
The ALCYONE trial enrolled 706 patients who were randomized to receive 9 cycles of daratumumab plus VMP or VMP alone.
In the daratumumab arm, patients received 16 mg/kg of daratumumab once weekly for 6 weeks (cycle 1; 1 cycle = 42 days), followed by once every 3 weeks (cycles 2-9). After that, patients continued to receive 16 mg/kg of daratumumab once every 4 weeks until disease progression.
At the pre-planned interim analysis, the study’s primary endpoint was met. Treatment with daratumumab reduced the risk of disease progression or death by 50% when compared to VMP alone (hazard ratio=0.50; 95% CI 0.38-0.65; P<0.0001).
The median PFS has not been reached in the daratumumab arm but was an estimated 18.1 months for patients who received VMP alone.
Genmab said that, overall, the safety profile of daratumumab in combination with VMP is consistent with the known safety profile of the VMP regimen and the known safety profile of daratumumab.
Based on these results, an independent data monitoring committee recommended the data be unblinded. All patients will continue to be monitored for safety and overall survival.
Janssen Biotech, Inc., which licensed daratumumab from Genmab in 2012, said it will discuss with health authorities the potential for a regulatory submission for daratumumab in combination with VMP as a treatment for newly diagnosed MM.
Daratumumab is already approved in the US (as DARZALEX®) for use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat MM patients who have received at least 1 prior therapy.
Daratumumab is also approved for use in combination with pomalidomide and dexamethasone to treat MM patients who have received at least 2 prior therapies, including lenalidomide and a proteasome inhibitor (PI).
And daratumumab is approved as monotherapy for MM patients who have received at least 3 prior lines of therapy, including a PI and an immunomodulatory agent, or who are double-refractory to a PI and an immunomodulatory agent. ![]()
Interim results of a phase 3 study suggest adding daratumumab to a 3-drug regimen can improve progression-free survival (PFS) in patients with newly diagnosed multiple myeloma (MM).
In the phase 3 ALCYONE study, researchers are comparing daratumumab in combination with bortezomib, melphalan, and prednisone (VMP) to VMP alone in patients with newly diagnosed MM who are not considered candidates for autologous stem cell transplant.
Genmab A/S recently announced interim results from this trial and said additional data are expected to be submitted for presentation at an upcoming medical conference and for publication in a peer-reviewed journal.
The ALCYONE trial enrolled 706 patients who were randomized to receive 9 cycles of daratumumab plus VMP or VMP alone.
In the daratumumab arm, patients received 16 mg/kg of daratumumab once weekly for 6 weeks (cycle 1; 1 cycle = 42 days), followed by once every 3 weeks (cycles 2-9). After that, patients continued to receive 16 mg/kg of daratumumab once every 4 weeks until disease progression.
At the pre-planned interim analysis, the study’s primary endpoint was met. Treatment with daratumumab reduced the risk of disease progression or death by 50% when compared to VMP alone (hazard ratio=0.50; 95% CI 0.38-0.65; P<0.0001).
The median PFS has not been reached in the daratumumab arm but was an estimated 18.1 months for patients who received VMP alone.
Genmab said that, overall, the safety profile of daratumumab in combination with VMP is consistent with the known safety profile of the VMP regimen and the known safety profile of daratumumab.
Based on these results, an independent data monitoring committee recommended the data be unblinded. All patients will continue to be monitored for safety and overall survival.
Janssen Biotech, Inc., which licensed daratumumab from Genmab in 2012, said it will discuss with health authorities the potential for a regulatory submission for daratumumab in combination with VMP as a treatment for newly diagnosed MM.
Daratumumab is already approved in the US (as DARZALEX®) for use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, to treat MM patients who have received at least 1 prior therapy.
Daratumumab is also approved for use in combination with pomalidomide and dexamethasone to treat MM patients who have received at least 2 prior therapies, including lenalidomide and a proteasome inhibitor (PI).
And daratumumab is approved as monotherapy for MM patients who have received at least 3 prior lines of therapy, including a PI and an immunomodulatory agent, or who are double-refractory to a PI and an immunomodulatory agent. ![]()
Drug granted breakthrough designation for CTCL
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to mogamulizumab for the treatment of adults with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4. It is being developed by Kyowa Hakko Kirin Co., Ltd.
The breakthrough designation for mogamulizumab in CTCL is based on data from the phase 3 MAVORIC study, the largest randomized trial in CTCL.
In MAVORIC, researchers are comparing mogamulizumab and vorinostat in patients with CTCL (both mycosis fungoides and Sézary syndrome) who have failed at least 1 prior systemic treatment.
In April, Kyowa Hakko Kirin announced results from this trial, which showed that patients treated with mogamulizumab have significantly better progression-free survival than patients treated with vorinostat. The company also said mogamulizumab has a tolerable safety profile.
Kyowa Hakko Kirin has not provided any data from MAVORIC but is working with investigators on the future presentation and publication of results from this trial.
Results of a phase 1/2 study of mogamulizumab in previously treated CTCL patients were published in Blood in March 2015.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to mogamulizumab for the treatment of adults with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4. It is being developed by Kyowa Hakko Kirin Co., Ltd.
The breakthrough designation for mogamulizumab in CTCL is based on data from the phase 3 MAVORIC study, the largest randomized trial in CTCL.
In MAVORIC, researchers are comparing mogamulizumab and vorinostat in patients with CTCL (both mycosis fungoides and Sézary syndrome) who have failed at least 1 prior systemic treatment.
In April, Kyowa Hakko Kirin announced results from this trial, which showed that patients treated with mogamulizumab have significantly better progression-free survival than patients treated with vorinostat. The company also said mogamulizumab has a tolerable safety profile.
Kyowa Hakko Kirin has not provided any data from MAVORIC but is working with investigators on the future presentation and publication of results from this trial.
Results of a phase 1/2 study of mogamulizumab in previously treated CTCL patients were published in Blood in March 2015.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to mogamulizumab for the treatment of adults with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4. It is being developed by Kyowa Hakko Kirin Co., Ltd.
The breakthrough designation for mogamulizumab in CTCL is based on data from the phase 3 MAVORIC study, the largest randomized trial in CTCL.
In MAVORIC, researchers are comparing mogamulizumab and vorinostat in patients with CTCL (both mycosis fungoides and Sézary syndrome) who have failed at least 1 prior systemic treatment.
In April, Kyowa Hakko Kirin announced results from this trial, which showed that patients treated with mogamulizumab have significantly better progression-free survival than patients treated with vorinostat. The company also said mogamulizumab has a tolerable safety profile.
Kyowa Hakko Kirin has not provided any data from MAVORIC but is working with investigators on the future presentation and publication of results from this trial.
Results of a phase 1/2 study of mogamulizumab in previously treated CTCL patients were published in Blood in March 2015.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
Researchers estimate risk of death from BIA-ALCL
The risk of death from breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) is less than 1 in a million, according to a study published in Aesthetic Surgery Journal.
Researchers analyzed data on breast implants and estimated the risk of death from BIA-ALCL to be 0.4 micromorts for a woman with bilateral, textured implants.
One micromort means a person’s risk of dying is 1 in a million. For context, a person who drives a car for 1 hour per day is said to have a micromort of 2, which is 5 times the BIA-ALCL micromort.
The researchers noted that there are no documented cases of BIA-ALCL in patients who have only received smooth-surface breast implants. Therefore, the risk of death from BIA-ALCL in a woman with smooth breast implants is “essentially 0.”
“We conducted this micromort study to bring real-life perspective for all existing and potential breast augmentation patients who might have reservations about implants based on the recent media coverage indicating that breast implants can be fatal—a sensationalized take on a very rare and very treatable condition,” said study author William P. Adams, Jr, MD, a professor in the Department of Plastic Surgery at the University of Texas Southwestern in Dallas.
“This analysis resonates with patients. They get it when you explain to a patient that their micromort risk from skiing for 1 day is 2 times higher than the micromort risk of having a textured breast implant for their lifetime—or that traveling 8 hours by car carries a 40-times higher micromort risk than having 2 textured breast implants for their lifetime.”
Dr Adams and his co-author analyzed data from the International Society of Aesthetic Plastic Surgery, the American Society of Plastic Surgeons, the American Society for Aesthetic Plastic Surgery, and the Austrian Breast Implant Register, as well as studies by Allergan and Sientra.
This led to a “conservative estimate” that approximately 30 million patients have textured breast implants worldwide (not including breast reconstructions).
This figure and the report of 12 deaths from BIA-ALCL worldwide suggest the risk of death from BIA-ALCL is 0.4 micromorts per patient (with 2 textured implants) or 0.2 micromorts per textured implant.
“The findings of this study are very important for patient education,” said study author David A. Sieber, MD, a plastic surgeon in private practice in San Francisco, California.
“The clear lymphoproliferative nature of BIA-ALCL, along with the calculated risks associated with its diagnosis, should be used for discussion during new consultations or at the time of presentation for evaluation of delayed-onset seromas.” ![]()
The risk of death from breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) is less than 1 in a million, according to a study published in Aesthetic Surgery Journal.
Researchers analyzed data on breast implants and estimated the risk of death from BIA-ALCL to be 0.4 micromorts for a woman with bilateral, textured implants.
One micromort means a person’s risk of dying is 1 in a million. For context, a person who drives a car for 1 hour per day is said to have a micromort of 2, which is 5 times the BIA-ALCL micromort.
The researchers noted that there are no documented cases of BIA-ALCL in patients who have only received smooth-surface breast implants. Therefore, the risk of death from BIA-ALCL in a woman with smooth breast implants is “essentially 0.”
“We conducted this micromort study to bring real-life perspective for all existing and potential breast augmentation patients who might have reservations about implants based on the recent media coverage indicating that breast implants can be fatal—a sensationalized take on a very rare and very treatable condition,” said study author William P. Adams, Jr, MD, a professor in the Department of Plastic Surgery at the University of Texas Southwestern in Dallas.
“This analysis resonates with patients. They get it when you explain to a patient that their micromort risk from skiing for 1 day is 2 times higher than the micromort risk of having a textured breast implant for their lifetime—or that traveling 8 hours by car carries a 40-times higher micromort risk than having 2 textured breast implants for their lifetime.”
Dr Adams and his co-author analyzed data from the International Society of Aesthetic Plastic Surgery, the American Society of Plastic Surgeons, the American Society for Aesthetic Plastic Surgery, and the Austrian Breast Implant Register, as well as studies by Allergan and Sientra.
This led to a “conservative estimate” that approximately 30 million patients have textured breast implants worldwide (not including breast reconstructions).
This figure and the report of 12 deaths from BIA-ALCL worldwide suggest the risk of death from BIA-ALCL is 0.4 micromorts per patient (with 2 textured implants) or 0.2 micromorts per textured implant.
“The findings of this study are very important for patient education,” said study author David A. Sieber, MD, a plastic surgeon in private practice in San Francisco, California.
“The clear lymphoproliferative nature of BIA-ALCL, along with the calculated risks associated with its diagnosis, should be used for discussion during new consultations or at the time of presentation for evaluation of delayed-onset seromas.” ![]()
The risk of death from breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) is less than 1 in a million, according to a study published in Aesthetic Surgery Journal.
Researchers analyzed data on breast implants and estimated the risk of death from BIA-ALCL to be 0.4 micromorts for a woman with bilateral, textured implants.
One micromort means a person’s risk of dying is 1 in a million. For context, a person who drives a car for 1 hour per day is said to have a micromort of 2, which is 5 times the BIA-ALCL micromort.
The researchers noted that there are no documented cases of BIA-ALCL in patients who have only received smooth-surface breast implants. Therefore, the risk of death from BIA-ALCL in a woman with smooth breast implants is “essentially 0.”
“We conducted this micromort study to bring real-life perspective for all existing and potential breast augmentation patients who might have reservations about implants based on the recent media coverage indicating that breast implants can be fatal—a sensationalized take on a very rare and very treatable condition,” said study author William P. Adams, Jr, MD, a professor in the Department of Plastic Surgery at the University of Texas Southwestern in Dallas.
“This analysis resonates with patients. They get it when you explain to a patient that their micromort risk from skiing for 1 day is 2 times higher than the micromort risk of having a textured breast implant for their lifetime—or that traveling 8 hours by car carries a 40-times higher micromort risk than having 2 textured breast implants for their lifetime.”
Dr Adams and his co-author analyzed data from the International Society of Aesthetic Plastic Surgery, the American Society of Plastic Surgeons, the American Society for Aesthetic Plastic Surgery, and the Austrian Breast Implant Register, as well as studies by Allergan and Sientra.
This led to a “conservative estimate” that approximately 30 million patients have textured breast implants worldwide (not including breast reconstructions).
This figure and the report of 12 deaths from BIA-ALCL worldwide suggest the risk of death from BIA-ALCL is 0.4 micromorts per patient (with 2 textured implants) or 0.2 micromorts per textured implant.
“The findings of this study are very important for patient education,” said study author David A. Sieber, MD, a plastic surgeon in private practice in San Francisco, California.
“The clear lymphoproliferative nature of BIA-ALCL, along with the calculated risks associated with its diagnosis, should be used for discussion during new consultations or at the time of presentation for evaluation of delayed-onset seromas.” ![]()
Watching von Willebrand factor in action
Researchers have gained “important mechanistic insights” into how von Willebrand factor (VWF) controls bleeding, according to an article published in Nature Communications.
Fluorescence imaging and microfluidic tools allowed the researchers to capture images of individual VWF molecules on camera while manipulating the molecules with life-like mechanical forces emulating natural blood flow.
This revealed that VWF undergoes a 2-step, shape-shifting transformation to activate blood clotting.
This transformation is triggered when VWF senses certain changes in blood flow that are indicative of injury.
“Under normal circumstances, VWF molecules are compact and globular in shape,” said study author Hongxia Fu, PhD, of Boston Children’s Hospital in Massachusetts.
“But we found that, when blood flow rate increases, VWF rapidly elongates, stretching out more and more in response to higher shear stress.”
However, elongating is not sufficient to activate blood clotting. It’s only when the tensile forces generated in the elongated VWF hit critical levels that the shape-shifter’s transformation becomes complete.
The tensile forces activate “sticky” sites along VWF, allowing it to adhere to circulating platelets.
Normally, the rush of blood needed to reach these critically high tensile forces can only occur at sites of injury inside blood vessels. This specificity enables VWF to sense blood loss and activate rapidly and locally, without activating elsewhere in the body.
“This experiment really represents a new platform for seeing and measuring what’s happening in the blood on a molecular level,” said study author Wesley P. Wong, PhD, of Boston Children’s Hospital.
“Through the use of novel microfluidic technologies that allow us to mimic the body’s vasculature in combination with single-molecule imaging techniques, we are finally able to capture striking images that uncover the mystery of nature’s forces at work in our bodies.”
Yan Jiang, PhD, of Boston Children’s Hospital, said the new findings could inspire smart drugs that are designed to treat obstructive clotting, like deep vein thrombosis, at only diseased areas of the body.
“When you’re putting a generic drug into the circulatory system, it’s taking effect everywhere, even in places that can cause detriment,” Dr Jiang said. “But what if we could design a smart drug that can mimic the 2-step shape-shifting of VWF and only takes effect in areas where clotting is likely to occur?” ![]()
Researchers have gained “important mechanistic insights” into how von Willebrand factor (VWF) controls bleeding, according to an article published in Nature Communications.
Fluorescence imaging and microfluidic tools allowed the researchers to capture images of individual VWF molecules on camera while manipulating the molecules with life-like mechanical forces emulating natural blood flow.
This revealed that VWF undergoes a 2-step, shape-shifting transformation to activate blood clotting.
This transformation is triggered when VWF senses certain changes in blood flow that are indicative of injury.
“Under normal circumstances, VWF molecules are compact and globular in shape,” said study author Hongxia Fu, PhD, of Boston Children’s Hospital in Massachusetts.
“But we found that, when blood flow rate increases, VWF rapidly elongates, stretching out more and more in response to higher shear stress.”
However, elongating is not sufficient to activate blood clotting. It’s only when the tensile forces generated in the elongated VWF hit critical levels that the shape-shifter’s transformation becomes complete.
The tensile forces activate “sticky” sites along VWF, allowing it to adhere to circulating platelets.
Normally, the rush of blood needed to reach these critically high tensile forces can only occur at sites of injury inside blood vessels. This specificity enables VWF to sense blood loss and activate rapidly and locally, without activating elsewhere in the body.
“This experiment really represents a new platform for seeing and measuring what’s happening in the blood on a molecular level,” said study author Wesley P. Wong, PhD, of Boston Children’s Hospital.
“Through the use of novel microfluidic technologies that allow us to mimic the body’s vasculature in combination with single-molecule imaging techniques, we are finally able to capture striking images that uncover the mystery of nature’s forces at work in our bodies.”
Yan Jiang, PhD, of Boston Children’s Hospital, said the new findings could inspire smart drugs that are designed to treat obstructive clotting, like deep vein thrombosis, at only diseased areas of the body.
“When you’re putting a generic drug into the circulatory system, it’s taking effect everywhere, even in places that can cause detriment,” Dr Jiang said. “But what if we could design a smart drug that can mimic the 2-step shape-shifting of VWF and only takes effect in areas where clotting is likely to occur?” ![]()
Researchers have gained “important mechanistic insights” into how von Willebrand factor (VWF) controls bleeding, according to an article published in Nature Communications.
Fluorescence imaging and microfluidic tools allowed the researchers to capture images of individual VWF molecules on camera while manipulating the molecules with life-like mechanical forces emulating natural blood flow.
This revealed that VWF undergoes a 2-step, shape-shifting transformation to activate blood clotting.
This transformation is triggered when VWF senses certain changes in blood flow that are indicative of injury.
“Under normal circumstances, VWF molecules are compact and globular in shape,” said study author Hongxia Fu, PhD, of Boston Children’s Hospital in Massachusetts.
“But we found that, when blood flow rate increases, VWF rapidly elongates, stretching out more and more in response to higher shear stress.”
However, elongating is not sufficient to activate blood clotting. It’s only when the tensile forces generated in the elongated VWF hit critical levels that the shape-shifter’s transformation becomes complete.
The tensile forces activate “sticky” sites along VWF, allowing it to adhere to circulating platelets.
Normally, the rush of blood needed to reach these critically high tensile forces can only occur at sites of injury inside blood vessels. This specificity enables VWF to sense blood loss and activate rapidly and locally, without activating elsewhere in the body.
“This experiment really represents a new platform for seeing and measuring what’s happening in the blood on a molecular level,” said study author Wesley P. Wong, PhD, of Boston Children’s Hospital.
“Through the use of novel microfluidic technologies that allow us to mimic the body’s vasculature in combination with single-molecule imaging techniques, we are finally able to capture striking images that uncover the mystery of nature’s forces at work in our bodies.”
Yan Jiang, PhD, of Boston Children’s Hospital, said the new findings could inspire smart drugs that are designed to treat obstructive clotting, like deep vein thrombosis, at only diseased areas of the body.
“When you’re putting a generic drug into the circulatory system, it’s taking effect everywhere, even in places that can cause detriment,” Dr Jiang said. “But what if we could design a smart drug that can mimic the 2-step shape-shifting of VWF and only takes effect in areas where clotting is likely to occur?” ![]()
FDA grants priority review to BLA for emicizumab
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for emicizumab.
The BLA is for emicizumab as once-weekly prophylaxis for adults, adolescents, and children with hemophilia A and factor VIII inhibitors.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the BLA for emicizumab by February 23, 2018.
About emicizumab
Emicizumab (formerly ACE910) is an investigational, bispecific monoclonal antibody designed to bring together factors IXa and X, proteins required to activate the natural coagulation cascade and restore the blood clotting process.
The drug is administered by subcutaneous injection of a ready-to-use solution. It was created by Chugai Pharmaceutical Co., Ltd. and is being co-developed by Chugai, Roche, and Genentech.
The BLA for emicizumab is based on results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
HAVEN 1 is a randomized, phase 3 study in which researchers evaluated the efficacy, safety, and pharmacokinetics of emicizumab prophylaxis compared to on-demand bypassing agents (BPAs; no prophylaxis) in adults and adolescents (12 years of age and older) with hemophilia A and inhibitors to factor VIII.
The study included 109 patients who were previously treated with BPAs on-demand or as prophylaxis.
There was a significant reduction in treated bleeds of 87% (risk rate=0.13, P<0.0001) with emicizumab compared with no prophylaxis.
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced thromboembolic events (TEs), and 3 had thrombotic microangiopathy (TMA) while receiving emicizumab prophylaxis and more than 100 u/kg/day of the BPA activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
HAVEN 2 is a single-arm, phase 3 study in which researchers are evaluating the efficacy, safety, and pharmacokinetics of once-weekly emicizumab in children (younger than 12 years of age) with hemophilia A and inhibitors to factor VIII who require treatment with BPAs.
The interim analysis included 19 children. After a median observation time of 12 weeks, 1 of the 19 children had a treated bleed. There were no reported joint or muscle bleeds.
The most common adverse events were mild injection site reactions and nasopharyngitis. No TEs or TMA events were observed. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for emicizumab.
The BLA is for emicizumab as once-weekly prophylaxis for adults, adolescents, and children with hemophilia A and factor VIII inhibitors.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the BLA for emicizumab by February 23, 2018.
About emicizumab
Emicizumab (formerly ACE910) is an investigational, bispecific monoclonal antibody designed to bring together factors IXa and X, proteins required to activate the natural coagulation cascade and restore the blood clotting process.
The drug is administered by subcutaneous injection of a ready-to-use solution. It was created by Chugai Pharmaceutical Co., Ltd. and is being co-developed by Chugai, Roche, and Genentech.
The BLA for emicizumab is based on results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
HAVEN 1 is a randomized, phase 3 study in which researchers evaluated the efficacy, safety, and pharmacokinetics of emicizumab prophylaxis compared to on-demand bypassing agents (BPAs; no prophylaxis) in adults and adolescents (12 years of age and older) with hemophilia A and inhibitors to factor VIII.
The study included 109 patients who were previously treated with BPAs on-demand or as prophylaxis.
There was a significant reduction in treated bleeds of 87% (risk rate=0.13, P<0.0001) with emicizumab compared with no prophylaxis.
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced thromboembolic events (TEs), and 3 had thrombotic microangiopathy (TMA) while receiving emicizumab prophylaxis and more than 100 u/kg/day of the BPA activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
HAVEN 2 is a single-arm, phase 3 study in which researchers are evaluating the efficacy, safety, and pharmacokinetics of once-weekly emicizumab in children (younger than 12 years of age) with hemophilia A and inhibitors to factor VIII who require treatment with BPAs.
The interim analysis included 19 children. After a median observation time of 12 weeks, 1 of the 19 children had a treated bleed. There were no reported joint or muscle bleeds.
The most common adverse events were mild injection site reactions and nasopharyngitis. No TEs or TMA events were observed. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for emicizumab.
The BLA is for emicizumab as once-weekly prophylaxis for adults, adolescents, and children with hemophilia A and factor VIII inhibitors.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the BLA for emicizumab by February 23, 2018.
About emicizumab
Emicizumab (formerly ACE910) is an investigational, bispecific monoclonal antibody designed to bring together factors IXa and X, proteins required to activate the natural coagulation cascade and restore the blood clotting process.
The drug is administered by subcutaneous injection of a ready-to-use solution. It was created by Chugai Pharmaceutical Co., Ltd. and is being co-developed by Chugai, Roche, and Genentech.
The BLA for emicizumab is based on results from a pair of phase 3 studies—HAVEN 1 and HAVEN 2.
Results from HAVEN 1 were published in NEJM and presented at the 26th ISTH Congress in July. Interim results from HAVEN 2 were presented at ISTH as well.
HAVEN 1
HAVEN 1 is a randomized, phase 3 study in which researchers evaluated the efficacy, safety, and pharmacokinetics of emicizumab prophylaxis compared to on-demand bypassing agents (BPAs; no prophylaxis) in adults and adolescents (12 years of age and older) with hemophilia A and inhibitors to factor VIII.
The study included 109 patients who were previously treated with BPAs on-demand or as prophylaxis.
There was a significant reduction in treated bleeds of 87% (risk rate=0.13, P<0.0001) with emicizumab compared with no prophylaxis.
Adverse events occurring in at least 5% of patients treated with emicizumab were local injection site reactions, headache, fatigue, upper respiratory tract infection, and arthralgia.
Two patients experienced thromboembolic events (TEs), and 3 had thrombotic microangiopathy (TMA) while receiving emicizumab prophylaxis and more than 100 u/kg/day of the BPA activated prothrombin complex concentrate, on average, for 24 hours or more before the event. Two of these patients had also received recombinant factor VIIa.
Neither TE required anticoagulation therapy, and 1 patient restarted emicizumab. The cases of TMA observed were transient, and 1 patient restarted emicizumab.
HAVEN 2
HAVEN 2 is a single-arm, phase 3 study in which researchers are evaluating the efficacy, safety, and pharmacokinetics of once-weekly emicizumab in children (younger than 12 years of age) with hemophilia A and inhibitors to factor VIII who require treatment with BPAs.
The interim analysis included 19 children. After a median observation time of 12 weeks, 1 of the 19 children had a treated bleed. There were no reported joint or muscle bleeds.
The most common adverse events were mild injection site reactions and nasopharyngitis. No TEs or TMA events were observed.
High healthcare costs follow CCSs into adulthood
New research suggests survivors of childhood cancer can incur high out-of-pocket medical costs into adulthood and may forgo healthcare to lessen this financial burden.
The study showed that childhood cancer survivors (CCSs) were more likely than non-CCSs to have out-of-pocket medical costs that were at least 10% of their annual income.
And these high costs were associated with delaying care or skipping it altogether.
These findings were published in the Journal of Clinical Oncology.
“Survivors who reported spending a higher percentage of their income on out-of-pocket medical costs were not only more likely to report financial burden, they also were at risk for undertaking behaviors potentially detrimental to their health in order to save money,” said study author Ryan Nipp, MD, of Massachusetts General Hospital Cancer Center in Boston.
“While studies have identified associations between financial burden and patients’ treatment outcomes, quality of life, and even survival among adults with cancer, as far as we know, this is the first to report these associations in survivors of childhood cancer.”
For this research, Dr Nipp and his colleagues surveyed participants in the Childhood Cancer Survivor Study. This included adults who had been treated for childhood cancers between 1970 and 1986 along with a control group of siblings not affected by cancer.
In 2011 and 2012, participants were asked to provide information about their health insurance, the out-of-pocket healthcare costs they paid during the previous year, and sociodemographic information such as annual income and employment status.
The researchers also asked participants whether medical costs posed a financial burden and, if so, what measures they had taken to deal with that burden.
Study population
The researchers received complete responses from 580 CCSs and 173 of their siblings without a history of cancer. The most common cancer diagnosis was leukemia (33%), followed by Hodgkin lymphoma (14%), while non-Hodgkin lymphoma was less common (7%).
CCSs were a mean of 30.2 years from diagnosis. Use of chemotherapy (77%), radiation (66%), and surgery (81%) were common. Few patients had cancer recurrence (13%) or second cancers (5%).
There was no significant difference between CCSs and their siblings with regard to age at the time of the survey (P=0.071), household income (P=0.053), education (P=0.345), health insurance status (P=0.317), or having at least 1 hospitalization in the past year (P=0.270).
However, CCSs were significantly more likely than siblings to have chronic health conditions (P<0.001). Forty percent of CCSs had severe or life-threatening chronic conditions, compared to 17% of siblings.
Seventy-six percent of CCSs and 80% of siblings were employed. Twenty-nine percent of CCSs and 39% of siblings had household incomes exceeding $100,000. Twelve percent of CCSs and 5% of siblings had household incomes below $20,000.
Ninety-one percent of CCSs and 93% of siblings were insured. Most subjects in both groups (81% and 87%, respectively) had employer-sponsored insurance.
Results
CCSs were significantly more likely than their siblings to have out-of-pocket medical costs that were at least 10% of their annual income—10% and 3%, respectively (P<0.001).
Among CCSs, those with higher out-of-pocket costs (≥10% vs <10% of income) were more likely to have household incomes below $50,000 (odds ratio [OR]=5.5) and to report being hospitalized in the past year (OR=2.3).
CCSs with a higher percentage of their income spent on out-of-pocket costs were also more likely to:
- Have problems paying their medical bills (OR=8.8)
- Report inability to pay for basic costs of living such as food, heat, or rent (OR=6.1)
- Defer healthcare for a medical problem (OR=3.1)
- Skip a test, treatment, or follow-up (OR=2.1)
- Consider filing for bankruptcy (OR=6.4).
“A more comprehensive understanding of the relationship between high out-of-pocket medical costs and the adverse effects of increased financial burden on cancer survivors could be instrumental in helping us identify those at risk for higher costs to help us address their financial challenges and improve health outcomes,” Dr Nipp said.
“It could also help inform policy changes to help meet the unique needs of cancer survivors and improve our understanding of how both higher costs and resulting financial burden influence patients’ approach to their medical care and decision-making.”
New research suggests survivors of childhood cancer can incur high out-of-pocket medical costs into adulthood and may forgo healthcare to lessen this financial burden.
The study showed that childhood cancer survivors (CCSs) were more likely than non-CCSs to have out-of-pocket medical costs that were at least 10% of their annual income.
And these high costs were associated with delaying care or skipping it altogether.
These findings were published in the Journal of Clinical Oncology.
“Survivors who reported spending a higher percentage of their income on out-of-pocket medical costs were not only more likely to report financial burden, they also were at risk for undertaking behaviors potentially detrimental to their health in order to save money,” said study author Ryan Nipp, MD, of Massachusetts General Hospital Cancer Center in Boston.
“While studies have identified associations between financial burden and patients’ treatment outcomes, quality of life, and even survival among adults with cancer, as far as we know, this is the first to report these associations in survivors of childhood cancer.”
For this research, Dr Nipp and his colleagues surveyed participants in the Childhood Cancer Survivor Study. This included adults who had been treated for childhood cancers between 1970 and 1986 along with a control group of siblings not affected by cancer.
In 2011 and 2012, participants were asked to provide information about their health insurance, the out-of-pocket healthcare costs they paid during the previous year, and sociodemographic information such as annual income and employment status.
The researchers also asked participants whether medical costs posed a financial burden and, if so, what measures they had taken to deal with that burden.
Study population
The researchers received complete responses from 580 CCSs and 173 of their siblings without a history of cancer. The most common cancer diagnosis was leukemia (33%), followed by Hodgkin lymphoma (14%), while non-Hodgkin lymphoma was less common (7%).
CCSs were a mean of 30.2 years from diagnosis. Use of chemotherapy (77%), radiation (66%), and surgery (81%) were common. Few patients had cancer recurrence (13%) or second cancers (5%).
There was no significant difference between CCSs and their siblings with regard to age at the time of the survey (P=0.071), household income (P=0.053), education (P=0.345), health insurance status (P=0.317), or having at least 1 hospitalization in the past year (P=0.270).
However, CCSs were significantly more likely than siblings to have chronic health conditions (P<0.001). Forty percent of CCSs had severe or life-threatening chronic conditions, compared to 17% of siblings.
Seventy-six percent of CCSs and 80% of siblings were employed. Twenty-nine percent of CCSs and 39% of siblings had household incomes exceeding $100,000. Twelve percent of CCSs and 5% of siblings had household incomes below $20,000.
Ninety-one percent of CCSs and 93% of siblings were insured. Most subjects in both groups (81% and 87%, respectively) had employer-sponsored insurance.
Results
CCSs were significantly more likely than their siblings to have out-of-pocket medical costs that were at least 10% of their annual income—10% and 3%, respectively (P<0.001).
Among CCSs, those with higher out-of-pocket costs (≥10% vs <10% of income) were more likely to have household incomes below $50,000 (odds ratio [OR]=5.5) and to report being hospitalized in the past year (OR=2.3).
CCSs with a higher percentage of their income spent on out-of-pocket costs were also more likely to:
- Have problems paying their medical bills (OR=8.8)
- Report inability to pay for basic costs of living such as food, heat, or rent (OR=6.1)
- Defer healthcare for a medical problem (OR=3.1)
- Skip a test, treatment, or follow-up (OR=2.1)
- Consider filing for bankruptcy (OR=6.4).
“A more comprehensive understanding of the relationship between high out-of-pocket medical costs and the adverse effects of increased financial burden on cancer survivors could be instrumental in helping us identify those at risk for higher costs to help us address their financial challenges and improve health outcomes,” Dr Nipp said.
“It could also help inform policy changes to help meet the unique needs of cancer survivors and improve our understanding of how both higher costs and resulting financial burden influence patients’ approach to their medical care and decision-making.”
New research suggests survivors of childhood cancer can incur high out-of-pocket medical costs into adulthood and may forgo healthcare to lessen this financial burden.
The study showed that childhood cancer survivors (CCSs) were more likely than non-CCSs to have out-of-pocket medical costs that were at least 10% of their annual income.
And these high costs were associated with delaying care or skipping it altogether.
These findings were published in the Journal of Clinical Oncology.
“Survivors who reported spending a higher percentage of their income on out-of-pocket medical costs were not only more likely to report financial burden, they also were at risk for undertaking behaviors potentially detrimental to their health in order to save money,” said study author Ryan Nipp, MD, of Massachusetts General Hospital Cancer Center in Boston.
“While studies have identified associations between financial burden and patients’ treatment outcomes, quality of life, and even survival among adults with cancer, as far as we know, this is the first to report these associations in survivors of childhood cancer.”
For this research, Dr Nipp and his colleagues surveyed participants in the Childhood Cancer Survivor Study. This included adults who had been treated for childhood cancers between 1970 and 1986 along with a control group of siblings not affected by cancer.
In 2011 and 2012, participants were asked to provide information about their health insurance, the out-of-pocket healthcare costs they paid during the previous year, and sociodemographic information such as annual income and employment status.
The researchers also asked participants whether medical costs posed a financial burden and, if so, what measures they had taken to deal with that burden.
Study population
The researchers received complete responses from 580 CCSs and 173 of their siblings without a history of cancer. The most common cancer diagnosis was leukemia (33%), followed by Hodgkin lymphoma (14%), while non-Hodgkin lymphoma was less common (7%).
CCSs were a mean of 30.2 years from diagnosis. Use of chemotherapy (77%), radiation (66%), and surgery (81%) were common. Few patients had cancer recurrence (13%) or second cancers (5%).
There was no significant difference between CCSs and their siblings with regard to age at the time of the survey (P=0.071), household income (P=0.053), education (P=0.345), health insurance status (P=0.317), or having at least 1 hospitalization in the past year (P=0.270).
However, CCSs were significantly more likely than siblings to have chronic health conditions (P<0.001). Forty percent of CCSs had severe or life-threatening chronic conditions, compared to 17% of siblings.
Seventy-six percent of CCSs and 80% of siblings were employed. Twenty-nine percent of CCSs and 39% of siblings had household incomes exceeding $100,000. Twelve percent of CCSs and 5% of siblings had household incomes below $20,000.
Ninety-one percent of CCSs and 93% of siblings were insured. Most subjects in both groups (81% and 87%, respectively) had employer-sponsored insurance.
Results
CCSs were significantly more likely than their siblings to have out-of-pocket medical costs that were at least 10% of their annual income—10% and 3%, respectively (P<0.001).
Among CCSs, those with higher out-of-pocket costs (≥10% vs <10% of income) were more likely to have household incomes below $50,000 (odds ratio [OR]=5.5) and to report being hospitalized in the past year (OR=2.3).
CCSs with a higher percentage of their income spent on out-of-pocket costs were also more likely to:
- Have problems paying their medical bills (OR=8.8)
- Report inability to pay for basic costs of living such as food, heat, or rent (OR=6.1)
- Defer healthcare for a medical problem (OR=3.1)
- Skip a test, treatment, or follow-up (OR=2.1)
- Consider filing for bankruptcy (OR=6.4).
“A more comprehensive understanding of the relationship between high out-of-pocket medical costs and the adverse effects of increased financial burden on cancer survivors could be instrumental in helping us identify those at risk for higher costs to help us address their financial challenges and improve health outcomes,” Dr Nipp said.
“It could also help inform policy changes to help meet the unique needs of cancer survivors and improve our understanding of how both higher costs and resulting financial burden influence patients’ approach to their medical care and decision-making.”
Vitamin C regulates HSCs, curbs AML development
Researchers have described a molecular mechanism that could help explain the link between low vitamin C (ascorbate) levels and acute myeloid leukemia (AML).
The team found that mice with low levels of ascorbate in their blood experience a notable increase in hematopoietic stem cell (HSC) frequency and function.
This, in turn, accelerates AML development, partly by inhibiting the tumor suppressor Tet2.
Sean Morrison, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported these findings in Nature.
“We have known for a while that people with lower levels of ascorbate (vitamin C) are at increased cancer risk, but we haven’t fully understood why,” Dr Morrison said. “Our research provides part of the explanation, at least for the blood-forming system.”
Dr Morrison and his colleagues developed a technique for analyzing the metabolic profiles of rare cell populations and used it to compare HSCs to restricted hematopoietic progenitors.
The researchers found that each hematopoietic cell type had a “distinct metabolic signature,” and both human and mouse HSCs had “unusually high” levels of ascorbate, which decreased as the cells differentiated.
To determine if ascorbate is important for HSC function, the team studied mice that lacked gulonolactone oxidase (Gulo), an enzyme mice use to synthesize their own ascorbate. Loss of the enzyme requires Gulo-deficient mice to obtain ascorbate exclusively through their diet like humans do.
So when the researchers fed the mice a standard diet, which contains little ascorbate, the animals’ ascorbate levels were depleted.
The team expected ascorbate depletion might lead to loss of HSC function, but they found the opposite was true. HSCs actually gained function, and this increased the incidence of AML in the mice.
This increase is partly tied to how ascorbate affects Tet2. The researchers found that ascorbate depletion can limit Tet2 function in tissues in a way that increases the risk of AML.
In addition, ascorbate depletion cooperated with Flt3 internal tandem duplication mutations to accelerate leukemogenesis. But the researchers were able to suppress leukemogenesis by feeding animals higher levels of ascorbate.
“Stem cells use ascorbate to regulate the abundance of certain chemical modifications on DNA, which are part of the epigenome,” said study author Michalis Agathocleous, PhD, of the University of Texas Southwestern Medical Center.
“So when stem cells don’t receive enough vitamin C, the epigenome can become damaged in a way that increases stem cell function but also increases the risk of leukemia.”
The researchers said further studies are needed to better understand the potential clinical implications of these findings.
However, the findings may have implications for older patients with clonal hematopoiesis. This condition increases a person’s risk of developing leukemia, but it is not well understood why certain patients develop leukemia and others do not. The results of this study might offer an explanation.
“One of the most common mutations in patients with clonal hematopoiesis is a loss of one copy of TET2,” Dr Morrison said. “Our results suggest patients with clonal hematopoiesis and a TET2 mutation should be particularly careful to get 100% of their daily vitamin C requirement. Because these patients only have one good copy of TET2 left, they need to maximize the residual TET2 tumor-suppressor activity to protect themselves from cancer.”
Researchers have described a molecular mechanism that could help explain the link between low vitamin C (ascorbate) levels and acute myeloid leukemia (AML).
The team found that mice with low levels of ascorbate in their blood experience a notable increase in hematopoietic stem cell (HSC) frequency and function.
This, in turn, accelerates AML development, partly by inhibiting the tumor suppressor Tet2.
Sean Morrison, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported these findings in Nature.
“We have known for a while that people with lower levels of ascorbate (vitamin C) are at increased cancer risk, but we haven’t fully understood why,” Dr Morrison said. “Our research provides part of the explanation, at least for the blood-forming system.”
Dr Morrison and his colleagues developed a technique for analyzing the metabolic profiles of rare cell populations and used it to compare HSCs to restricted hematopoietic progenitors.
The researchers found that each hematopoietic cell type had a “distinct metabolic signature,” and both human and mouse HSCs had “unusually high” levels of ascorbate, which decreased as the cells differentiated.
To determine if ascorbate is important for HSC function, the team studied mice that lacked gulonolactone oxidase (Gulo), an enzyme mice use to synthesize their own ascorbate. Loss of the enzyme requires Gulo-deficient mice to obtain ascorbate exclusively through their diet like humans do.
So when the researchers fed the mice a standard diet, which contains little ascorbate, the animals’ ascorbate levels were depleted.
The team expected ascorbate depletion might lead to loss of HSC function, but they found the opposite was true. HSCs actually gained function, and this increased the incidence of AML in the mice.
This increase is partly tied to how ascorbate affects Tet2. The researchers found that ascorbate depletion can limit Tet2 function in tissues in a way that increases the risk of AML.
In addition, ascorbate depletion cooperated with Flt3 internal tandem duplication mutations to accelerate leukemogenesis. But the researchers were able to suppress leukemogenesis by feeding animals higher levels of ascorbate.
“Stem cells use ascorbate to regulate the abundance of certain chemical modifications on DNA, which are part of the epigenome,” said study author Michalis Agathocleous, PhD, of the University of Texas Southwestern Medical Center.
“So when stem cells don’t receive enough vitamin C, the epigenome can become damaged in a way that increases stem cell function but also increases the risk of leukemia.”
The researchers said further studies are needed to better understand the potential clinical implications of these findings.
However, the findings may have implications for older patients with clonal hematopoiesis. This condition increases a person’s risk of developing leukemia, but it is not well understood why certain patients develop leukemia and others do not. The results of this study might offer an explanation.
“One of the most common mutations in patients with clonal hematopoiesis is a loss of one copy of TET2,” Dr Morrison said. “Our results suggest patients with clonal hematopoiesis and a TET2 mutation should be particularly careful to get 100% of their daily vitamin C requirement. Because these patients only have one good copy of TET2 left, they need to maximize the residual TET2 tumor-suppressor activity to protect themselves from cancer.”
Researchers have described a molecular mechanism that could help explain the link between low vitamin C (ascorbate) levels and acute myeloid leukemia (AML).
The team found that mice with low levels of ascorbate in their blood experience a notable increase in hematopoietic stem cell (HSC) frequency and function.
This, in turn, accelerates AML development, partly by inhibiting the tumor suppressor Tet2.
Sean Morrison, PhD, of the University of Texas Southwestern Medical Center in Dallas, and his colleagues reported these findings in Nature.
“We have known for a while that people with lower levels of ascorbate (vitamin C) are at increased cancer risk, but we haven’t fully understood why,” Dr Morrison said. “Our research provides part of the explanation, at least for the blood-forming system.”
Dr Morrison and his colleagues developed a technique for analyzing the metabolic profiles of rare cell populations and used it to compare HSCs to restricted hematopoietic progenitors.
The researchers found that each hematopoietic cell type had a “distinct metabolic signature,” and both human and mouse HSCs had “unusually high” levels of ascorbate, which decreased as the cells differentiated.
To determine if ascorbate is important for HSC function, the team studied mice that lacked gulonolactone oxidase (Gulo), an enzyme mice use to synthesize their own ascorbate. Loss of the enzyme requires Gulo-deficient mice to obtain ascorbate exclusively through their diet like humans do.
So when the researchers fed the mice a standard diet, which contains little ascorbate, the animals’ ascorbate levels were depleted.
The team expected ascorbate depletion might lead to loss of HSC function, but they found the opposite was true. HSCs actually gained function, and this increased the incidence of AML in the mice.
This increase is partly tied to how ascorbate affects Tet2. The researchers found that ascorbate depletion can limit Tet2 function in tissues in a way that increases the risk of AML.
In addition, ascorbate depletion cooperated with Flt3 internal tandem duplication mutations to accelerate leukemogenesis. But the researchers were able to suppress leukemogenesis by feeding animals higher levels of ascorbate.
“Stem cells use ascorbate to regulate the abundance of certain chemical modifications on DNA, which are part of the epigenome,” said study author Michalis Agathocleous, PhD, of the University of Texas Southwestern Medical Center.
“So when stem cells don’t receive enough vitamin C, the epigenome can become damaged in a way that increases stem cell function but also increases the risk of leukemia.”
The researchers said further studies are needed to better understand the potential clinical implications of these findings.
However, the findings may have implications for older patients with clonal hematopoiesis. This condition increases a person’s risk of developing leukemia, but it is not well understood why certain patients develop leukemia and others do not. The results of this study might offer an explanation.
“One of the most common mutations in patients with clonal hematopoiesis is a loss of one copy of TET2,” Dr Morrison said. “Our results suggest patients with clonal hematopoiesis and a TET2 mutation should be particularly careful to get 100% of their daily vitamin C requirement. Because these patients only have one good copy of TET2 left, they need to maximize the residual TET2 tumor-suppressor activity to protect themselves from cancer.”
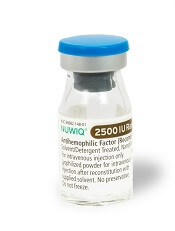
FDA approves new strengths of hemophilia therapy
The US Food and Drug Administration (FDA) has approved new product strengths for the factor VIII therapy simoctocog alfa (NUWIQ®).
Simoctocog alfa is the first B-domain-deleted recombinant factor VIII product derived from a human cell line—not chemically modified or fused with another protein—designed to treat hemophilia A.
Simoctocog alfa is FDA-approved to treat adults and children with hemophilia A. This includes on-demand treatment and control of bleeding episodes, routine prophylaxis to reduce the frequency of bleeding episodes, and perioperative management of bleeding.
Now, the FDA has approved single-dose simoctocog alfa vial strengths of 2500, 3000, and 4000 International Units (IU), which will be available for order in the US starting September 2017.
These new vial strengths will be provided in addition to the already available strengths of 250, 500, 1000, and 2000 IU.
“The new vial options will benefit patients, physicians, and healthcare professionals by providing greater treatment flexibility and convenience,” said Flemming Nielsen, president of Octapharma USA, makers of simoctocog alfa.
According to Octapharma, the additional vial strengths offer benefits beyond potentially reducing the number of vials used per patient. The new vial sizes may benefit heavier patients who could use fewer product vials and, in some cases, just one vial.
More vial options will increase dosing flexibility by allowing physicians to select various vial combinations to align closer to the prescribed dose. The new vial sizes could be particularly beneficial to patients using a pharmacokinetic (PK)-guided, personalized prophylaxis approach.
Results of Octapharma’s clinical trial on the PK-guided dosing with simoctocog alfa were published in Haemophilia in April.
This study, known as GENA-21 or NuPreviq, enrolled 66 previously treated adults with severe hemophilia A. Patients were originally started on infusions 3 times a week or every other day. Subsequent dosing intervals were then determined based on individual PK data.
The median dosing interval with PK-guided prophylaxis was 3.5 days, and 57% of patients were able to decrease infusions to twice-weekly or less.
The median weekly prophylaxis dose was reduced by 7.2%, from 100.0 IU kg−1 with standard prophylaxis to 92.8 IU kg−1 during the last 2 months of personalized prophylaxis.
For all bleeds, the mean annualized bleeding rate (ABR) during personalized prophylaxis was 1.45, and the median was 0 (interquartile range, [IQR]: 0, 1.9).
For spontaneous bleeds, the mean ABR was 0.79, and the median was 0 (IQR: 0, 0). For joint bleeds, the mean ABR was 0.91, and the median was 0 (IQR: 0, 0).
None of the patients developed FVIII inhibitors. There were no treatment-related serious or severe adverse events, clinically significant abnormalities in laboratory parameters, or cases of thromboembolism.
The ongoing trial GENA-21b is designed to confirm the results of GENA-21.
The US Food and Drug Administration (FDA) has approved new product strengths for the factor VIII therapy simoctocog alfa (NUWIQ®).
Simoctocog alfa is the first B-domain-deleted recombinant factor VIII product derived from a human cell line—not chemically modified or fused with another protein—designed to treat hemophilia A.
Simoctocog alfa is FDA-approved to treat adults and children with hemophilia A. This includes on-demand treatment and control of bleeding episodes, routine prophylaxis to reduce the frequency of bleeding episodes, and perioperative management of bleeding.
Now, the FDA has approved single-dose simoctocog alfa vial strengths of 2500, 3000, and 4000 International Units (IU), which will be available for order in the US starting September 2017.
These new vial strengths will be provided in addition to the already available strengths of 250, 500, 1000, and 2000 IU.
“The new vial options will benefit patients, physicians, and healthcare professionals by providing greater treatment flexibility and convenience,” said Flemming Nielsen, president of Octapharma USA, makers of simoctocog alfa.
According to Octapharma, the additional vial strengths offer benefits beyond potentially reducing the number of vials used per patient. The new vial sizes may benefit heavier patients who could use fewer product vials and, in some cases, just one vial.
More vial options will increase dosing flexibility by allowing physicians to select various vial combinations to align closer to the prescribed dose. The new vial sizes could be particularly beneficial to patients using a pharmacokinetic (PK)-guided, personalized prophylaxis approach.
Results of Octapharma’s clinical trial on the PK-guided dosing with simoctocog alfa were published in Haemophilia in April.
This study, known as GENA-21 or NuPreviq, enrolled 66 previously treated adults with severe hemophilia A. Patients were originally started on infusions 3 times a week or every other day. Subsequent dosing intervals were then determined based on individual PK data.
The median dosing interval with PK-guided prophylaxis was 3.5 days, and 57% of patients were able to decrease infusions to twice-weekly or less.
The median weekly prophylaxis dose was reduced by 7.2%, from 100.0 IU kg−1 with standard prophylaxis to 92.8 IU kg−1 during the last 2 months of personalized prophylaxis.
For all bleeds, the mean annualized bleeding rate (ABR) during personalized prophylaxis was 1.45, and the median was 0 (interquartile range, [IQR]: 0, 1.9).
For spontaneous bleeds, the mean ABR was 0.79, and the median was 0 (IQR: 0, 0). For joint bleeds, the mean ABR was 0.91, and the median was 0 (IQR: 0, 0).
None of the patients developed FVIII inhibitors. There were no treatment-related serious or severe adverse events, clinically significant abnormalities in laboratory parameters, or cases of thromboembolism.
The ongoing trial GENA-21b is designed to confirm the results of GENA-21.
The US Food and Drug Administration (FDA) has approved new product strengths for the factor VIII therapy simoctocog alfa (NUWIQ®).
Simoctocog alfa is the first B-domain-deleted recombinant factor VIII product derived from a human cell line—not chemically modified or fused with another protein—designed to treat hemophilia A.
Simoctocog alfa is FDA-approved to treat adults and children with hemophilia A. This includes on-demand treatment and control of bleeding episodes, routine prophylaxis to reduce the frequency of bleeding episodes, and perioperative management of bleeding.
Now, the FDA has approved single-dose simoctocog alfa vial strengths of 2500, 3000, and 4000 International Units (IU), which will be available for order in the US starting September 2017.
These new vial strengths will be provided in addition to the already available strengths of 250, 500, 1000, and 2000 IU.
“The new vial options will benefit patients, physicians, and healthcare professionals by providing greater treatment flexibility and convenience,” said Flemming Nielsen, president of Octapharma USA, makers of simoctocog alfa.
According to Octapharma, the additional vial strengths offer benefits beyond potentially reducing the number of vials used per patient. The new vial sizes may benefit heavier patients who could use fewer product vials and, in some cases, just one vial.
More vial options will increase dosing flexibility by allowing physicians to select various vial combinations to align closer to the prescribed dose. The new vial sizes could be particularly beneficial to patients using a pharmacokinetic (PK)-guided, personalized prophylaxis approach.
Results of Octapharma’s clinical trial on the PK-guided dosing with simoctocog alfa were published in Haemophilia in April.
This study, known as GENA-21 or NuPreviq, enrolled 66 previously treated adults with severe hemophilia A. Patients were originally started on infusions 3 times a week or every other day. Subsequent dosing intervals were then determined based on individual PK data.
The median dosing interval with PK-guided prophylaxis was 3.5 days, and 57% of patients were able to decrease infusions to twice-weekly or less.
The median weekly prophylaxis dose was reduced by 7.2%, from 100.0 IU kg−1 with standard prophylaxis to 92.8 IU kg−1 during the last 2 months of personalized prophylaxis.
For all bleeds, the mean annualized bleeding rate (ABR) during personalized prophylaxis was 1.45, and the median was 0 (interquartile range, [IQR]: 0, 1.9).
For spontaneous bleeds, the mean ABR was 0.79, and the median was 0 (IQR: 0, 0). For joint bleeds, the mean ABR was 0.91, and the median was 0 (IQR: 0, 0).
None of the patients developed FVIII inhibitors. There were no treatment-related serious or severe adverse events, clinically significant abnormalities in laboratory parameters, or cases of thromboembolism.
The ongoing trial GENA-21b is designed to confirm the results of GENA-21.