User login
GAD-M produces high ORR in treatment-naïve ENKTL
LUGANO, SWITZERLAND—A 4-drug regimen has demonstrated efficacy in a phase 2 trial of patients with treatment-naïve extranodal natural killer/T-cell lymphoma (ENKTL).
Treatment with gemcitabine, PEG-asparaginase, dexamethasone, and methotrexate (GAD-M) produced a 94% overall response rate (ORR) and an 83% complete response (CR) rate in this trial.
Responses and survival rates were higher in patients with stage I/II disease, who also received radiotherapy, than in patients with stage III/IV disease.
Grade 1/2 toxicities were frequent, but there were few grade 3/4 non-hematologic toxicities. One patient died of treatment-related toxicity.
Zhiming Li, of Sun Yet-sen University Cancer Center in Guangzhou, China, presented these results at the 14th International Conference on Malignant Lymphoma (ICML).
Patients and treatment
The trial enrolled 41 patients with treatment-naïve ENKTL, and 36 of them were evaluable.
The patients’ median age was 45 (range, 18-75), and 30.6% were female. Most patients (86.1%) had stage I/II disease, 13.9% had an ECOG performance status of 2 or greater, and 41.7% had an IPI score of 2 or greater.
The GAD-M regimen consisted of:
- Gemcitabine given at 1000 mg/m2 via intravenous drip on days 1 and 8
- PEG-asparaginase given at 2500 U/m2 intramuscularly on day 1
- Dexamethasone given at 20 mg via intravenous drip on days 1 to 3
- Methotrexate given at 3000 mg/m2 via continuous, 12-hour infusion on day 1.
The regimen was repeated every 3 weeks.
For patients with stage I/II disease, 2 to 4 cycles of the GAD-M regimen was followed by extensive involved-field radiotherapy and an additional 2 to 4 cycles. For patients with stage III/IV disease, GAD-M was repeated for 6 cycles.
Response and survival
The ORR was 94.4%, both after 2 cycles of GAD-M and after 6 cycles. The CR rate was 50% after 2 cycles and 83.3% after 6 cycles.
In patients with stage I/II disease, the ORR was 100% after 2 cycles and 6 cycles. The CR rate was 54.8% after 2 cycles and 90.3% after 6 cycles.
In patients with stage III/IV disease, the ORR was 60% after 2 cycles and 6 cycles. The CR rate was 20% after 2 cycles and 40% after 6 cycles.
At median follow-up of 23.3 months, the estimated 3-year progression-free survival (PFS) was 72.1%, and the overall survival (OS) was 76.3%.
For patients with stage I/II disease, the PFS was 77.3%, and the OS was 79.3%. For patients with stage III/IV disease, the PFS was 40%, and the OS was 60%.
Safety
Hematologic adverse events (AEs) included anemia (97.2% total, 52.8% grade 3/4), leukocytopenia (94.4%, 27.8% grade 3/4), neutropenia (88.9%, 5.6% grade 3), and thrombocytopenia (47.2%, 13.9% grade 3/4).
Non-hematologic AEs included hypoalbuminemia (100%, 5.6% grade 3), increased transaminases (88.9%, 5.6% grade 3), hyperbilirubinemia (52.8%, 11.1% grade 3), decreased fibrinogen (19.4%, 11.1% grade 4), vomiting (13.9%, 2.8% grade 5), increased creatinine (8.3%, 2.8% grade 3), and abdominal pain (5.6% grade 1).
The grade 5 treatment-related AE occurred in a 61-year-old man. He died of electrolyte disorders caused by severe vomiting. ![]()
LUGANO, SWITZERLAND—A 4-drug regimen has demonstrated efficacy in a phase 2 trial of patients with treatment-naïve extranodal natural killer/T-cell lymphoma (ENKTL).
Treatment with gemcitabine, PEG-asparaginase, dexamethasone, and methotrexate (GAD-M) produced a 94% overall response rate (ORR) and an 83% complete response (CR) rate in this trial.
Responses and survival rates were higher in patients with stage I/II disease, who also received radiotherapy, than in patients with stage III/IV disease.
Grade 1/2 toxicities were frequent, but there were few grade 3/4 non-hematologic toxicities. One patient died of treatment-related toxicity.
Zhiming Li, of Sun Yet-sen University Cancer Center in Guangzhou, China, presented these results at the 14th International Conference on Malignant Lymphoma (ICML).
Patients and treatment
The trial enrolled 41 patients with treatment-naïve ENKTL, and 36 of them were evaluable.
The patients’ median age was 45 (range, 18-75), and 30.6% were female. Most patients (86.1%) had stage I/II disease, 13.9% had an ECOG performance status of 2 or greater, and 41.7% had an IPI score of 2 or greater.
The GAD-M regimen consisted of:
- Gemcitabine given at 1000 mg/m2 via intravenous drip on days 1 and 8
- PEG-asparaginase given at 2500 U/m2 intramuscularly on day 1
- Dexamethasone given at 20 mg via intravenous drip on days 1 to 3
- Methotrexate given at 3000 mg/m2 via continuous, 12-hour infusion on day 1.
The regimen was repeated every 3 weeks.
For patients with stage I/II disease, 2 to 4 cycles of the GAD-M regimen was followed by extensive involved-field radiotherapy and an additional 2 to 4 cycles. For patients with stage III/IV disease, GAD-M was repeated for 6 cycles.
Response and survival
The ORR was 94.4%, both after 2 cycles of GAD-M and after 6 cycles. The CR rate was 50% after 2 cycles and 83.3% after 6 cycles.
In patients with stage I/II disease, the ORR was 100% after 2 cycles and 6 cycles. The CR rate was 54.8% after 2 cycles and 90.3% after 6 cycles.
In patients with stage III/IV disease, the ORR was 60% after 2 cycles and 6 cycles. The CR rate was 20% after 2 cycles and 40% after 6 cycles.
At median follow-up of 23.3 months, the estimated 3-year progression-free survival (PFS) was 72.1%, and the overall survival (OS) was 76.3%.
For patients with stage I/II disease, the PFS was 77.3%, and the OS was 79.3%. For patients with stage III/IV disease, the PFS was 40%, and the OS was 60%.
Safety
Hematologic adverse events (AEs) included anemia (97.2% total, 52.8% grade 3/4), leukocytopenia (94.4%, 27.8% grade 3/4), neutropenia (88.9%, 5.6% grade 3), and thrombocytopenia (47.2%, 13.9% grade 3/4).
Non-hematologic AEs included hypoalbuminemia (100%, 5.6% grade 3), increased transaminases (88.9%, 5.6% grade 3), hyperbilirubinemia (52.8%, 11.1% grade 3), decreased fibrinogen (19.4%, 11.1% grade 4), vomiting (13.9%, 2.8% grade 5), increased creatinine (8.3%, 2.8% grade 3), and abdominal pain (5.6% grade 1).
The grade 5 treatment-related AE occurred in a 61-year-old man. He died of electrolyte disorders caused by severe vomiting. ![]()
LUGANO, SWITZERLAND—A 4-drug regimen has demonstrated efficacy in a phase 2 trial of patients with treatment-naïve extranodal natural killer/T-cell lymphoma (ENKTL).
Treatment with gemcitabine, PEG-asparaginase, dexamethasone, and methotrexate (GAD-M) produced a 94% overall response rate (ORR) and an 83% complete response (CR) rate in this trial.
Responses and survival rates were higher in patients with stage I/II disease, who also received radiotherapy, than in patients with stage III/IV disease.
Grade 1/2 toxicities were frequent, but there were few grade 3/4 non-hematologic toxicities. One patient died of treatment-related toxicity.
Zhiming Li, of Sun Yet-sen University Cancer Center in Guangzhou, China, presented these results at the 14th International Conference on Malignant Lymphoma (ICML).
Patients and treatment
The trial enrolled 41 patients with treatment-naïve ENKTL, and 36 of them were evaluable.
The patients’ median age was 45 (range, 18-75), and 30.6% were female. Most patients (86.1%) had stage I/II disease, 13.9% had an ECOG performance status of 2 or greater, and 41.7% had an IPI score of 2 or greater.
The GAD-M regimen consisted of:
- Gemcitabine given at 1000 mg/m2 via intravenous drip on days 1 and 8
- PEG-asparaginase given at 2500 U/m2 intramuscularly on day 1
- Dexamethasone given at 20 mg via intravenous drip on days 1 to 3
- Methotrexate given at 3000 mg/m2 via continuous, 12-hour infusion on day 1.
The regimen was repeated every 3 weeks.
For patients with stage I/II disease, 2 to 4 cycles of the GAD-M regimen was followed by extensive involved-field radiotherapy and an additional 2 to 4 cycles. For patients with stage III/IV disease, GAD-M was repeated for 6 cycles.
Response and survival
The ORR was 94.4%, both after 2 cycles of GAD-M and after 6 cycles. The CR rate was 50% after 2 cycles and 83.3% after 6 cycles.
In patients with stage I/II disease, the ORR was 100% after 2 cycles and 6 cycles. The CR rate was 54.8% after 2 cycles and 90.3% after 6 cycles.
In patients with stage III/IV disease, the ORR was 60% after 2 cycles and 6 cycles. The CR rate was 20% after 2 cycles and 40% after 6 cycles.
At median follow-up of 23.3 months, the estimated 3-year progression-free survival (PFS) was 72.1%, and the overall survival (OS) was 76.3%.
For patients with stage I/II disease, the PFS was 77.3%, and the OS was 79.3%. For patients with stage III/IV disease, the PFS was 40%, and the OS was 60%.
Safety
Hematologic adverse events (AEs) included anemia (97.2% total, 52.8% grade 3/4), leukocytopenia (94.4%, 27.8% grade 3/4), neutropenia (88.9%, 5.6% grade 3), and thrombocytopenia (47.2%, 13.9% grade 3/4).
Non-hematologic AEs included hypoalbuminemia (100%, 5.6% grade 3), increased transaminases (88.9%, 5.6% grade 3), hyperbilirubinemia (52.8%, 11.1% grade 3), decreased fibrinogen (19.4%, 11.1% grade 4), vomiting (13.9%, 2.8% grade 5), increased creatinine (8.3%, 2.8% grade 3), and abdominal pain (5.6% grade 1).
The grade 5 treatment-related AE occurred in a 61-year-old man. He died of electrolyte disorders caused by severe vomiting. ![]()
Mutations linked to Fanconi anemia
New research suggests that mutations in the RFWD3 gene cause Fanconi anemia (FA).
Investigators detected mutations in the RFWD3 gene in a child with FA and confirmed the relationship between the mutations and the disorder via functional studies in cell and animal models.
The team described this research in The Journal of Clinical Oncology.
Previously, there was knowledge of 21 genes involved in FA.
“The discovery of new genes is essential not only for genetic diagnosis and advice, but also for the development of new therapies,” said study author Jordi Surrallés, PhD, of the Hospital de la Santa Creu i Sant Pau and Universitat Autonoma de Barcelona in Spain.
“The RFWD3 protein is one of the few deficient proteins in patients with Fanconi anemia in which we can see a clear enzymatic activity (ubiquitin ligase), which opens the door to massive drug screenings. In this sense, my group has already worked on several screenings of thousands of therapeutic molecules with the aim of repositioning a drug for this disease.” ![]()
New research suggests that mutations in the RFWD3 gene cause Fanconi anemia (FA).
Investigators detected mutations in the RFWD3 gene in a child with FA and confirmed the relationship between the mutations and the disorder via functional studies in cell and animal models.
The team described this research in The Journal of Clinical Oncology.
Previously, there was knowledge of 21 genes involved in FA.
“The discovery of new genes is essential not only for genetic diagnosis and advice, but also for the development of new therapies,” said study author Jordi Surrallés, PhD, of the Hospital de la Santa Creu i Sant Pau and Universitat Autonoma de Barcelona in Spain.
“The RFWD3 protein is one of the few deficient proteins in patients with Fanconi anemia in which we can see a clear enzymatic activity (ubiquitin ligase), which opens the door to massive drug screenings. In this sense, my group has already worked on several screenings of thousands of therapeutic molecules with the aim of repositioning a drug for this disease.” ![]()
New research suggests that mutations in the RFWD3 gene cause Fanconi anemia (FA).
Investigators detected mutations in the RFWD3 gene in a child with FA and confirmed the relationship between the mutations and the disorder via functional studies in cell and animal models.
The team described this research in The Journal of Clinical Oncology.
Previously, there was knowledge of 21 genes involved in FA.
“The discovery of new genes is essential not only for genetic diagnosis and advice, but also for the development of new therapies,” said study author Jordi Surrallés, PhD, of the Hospital de la Santa Creu i Sant Pau and Universitat Autonoma de Barcelona in Spain.
“The RFWD3 protein is one of the few deficient proteins in patients with Fanconi anemia in which we can see a clear enzymatic activity (ubiquitin ligase), which opens the door to massive drug screenings. In this sense, my group has already worked on several screenings of thousands of therapeutic molecules with the aim of repositioning a drug for this disease.” ![]()
Studies support testing for iron deficiency in young women
A pair of studies suggest physicians should consider testing female adolescents for iron deficiency within a few years of starting menses.
Women are typically tested for anemia in their teens, with a quick and affordable hemoglobin test.
However, iron deficiency can develop years before anemia and can be missed by hemoglobin testing alone.
Blood tests for iron deficiency without anemia are more costly and more difficult to obtain than hemoglobin testing for anemia.
Deepa Sekhar, MD, of Penn State College of Medicine in Hershey, Pennsylvania, and her colleagues set out to determine risk factors for iron deficiency without anemia in order to pinpoint which women could benefit most from the more costly testing.
The results of the researchers’ 2 studies were published in PLOS ONE and The Journal of Pediatrics.
PLOS ONE study
The researchers evaluated data from 6216 females, ages 12 to 49, who took part in the National Health and Nutrition Examination Survey (NHANES) between 2003 and 2010. As part of the survey, participants were tested for both iron deficiency and anemia.
Eight percent of all subjects (n=494) had iron deficiency.
Nine percent (n=250) of non-anemic younger women (ages 12-21) had iron deficiency, as did 7% (n=244) of older women (ages 22-49) who were not anemic.
The researchers looked at potential risk factors for iron deficiency, including the age when women started menstruating, as well as their race/ethnicity, poverty status, food insecurity, tobacco or nicotine use, dietary information, body mass index, and physical activity.
All of these factors have been associated with iron-deficiency anemia in women in prior studies.
In this study, there was only 1 risk factor significantly associated with iron deficiency without anemia.
Young women (ages 12-21) who had been menstruating for more than 3 years had a significantly higher risk of iron deficiency without anemia (risk ratio=3.18).
The Journal of Pediatrics study
In this study, the researchers looked at whether a questionnaire could better predict iron status.
The questionnaire included questions on depression, poor attention, and daytime sleepiness, all of which have been associated with iron deficiency or iron-deficiency anemia, but were not captured in the prior NHANES analyses.
This questionnaire was compared to the 4 questions assessing iron-deficiency anemia risk in the Bright Futures Adolescent Previsit Questionnaire, a survey recommended for physician use by the American Academy of Pediatrics.
Ninety-six female adolescents participated in this study. Eighteen percent of them (n=17) had iron deficiency, and 5% (n=5) had iron-deficiency anemia.
Both the Bright Futures questions and the researchers’ risk assessment questionnaire poorly predicted ferritin and hemoglobin values in these subjects.
Mean differences in depression, poor attention, food insecurity, daytime sleepiness, and body mass index percentile were not significantly associated with ferritin or hemoglobin.
Conclusions
The results of these 2 studies suggest that risk factors and assessments cannot accurately determine which young women should receive testing for iron deficiency, although results from the first study might be used to determine when testing should occur.
“I think we need to establish the optimal timing for an objective assessment of adolescent iron deficiency and anemia,” Dr Sekhar said.
She believes the appropriate age may be 16 years old, when most females will have been menstruating for at least 3 years.
Further research will be needed to determine which blood test for iron deficiency without anemia is accurate, cost-efficient, and practical for routine doctor’s office use.
This test should be given with hemoglobin testing to catch all young women on the spectrum of iron deficiency, Dr Sekhar said. ![]()
A pair of studies suggest physicians should consider testing female adolescents for iron deficiency within a few years of starting menses.
Women are typically tested for anemia in their teens, with a quick and affordable hemoglobin test.
However, iron deficiency can develop years before anemia and can be missed by hemoglobin testing alone.
Blood tests for iron deficiency without anemia are more costly and more difficult to obtain than hemoglobin testing for anemia.
Deepa Sekhar, MD, of Penn State College of Medicine in Hershey, Pennsylvania, and her colleagues set out to determine risk factors for iron deficiency without anemia in order to pinpoint which women could benefit most from the more costly testing.
The results of the researchers’ 2 studies were published in PLOS ONE and The Journal of Pediatrics.
PLOS ONE study
The researchers evaluated data from 6216 females, ages 12 to 49, who took part in the National Health and Nutrition Examination Survey (NHANES) between 2003 and 2010. As part of the survey, participants were tested for both iron deficiency and anemia.
Eight percent of all subjects (n=494) had iron deficiency.
Nine percent (n=250) of non-anemic younger women (ages 12-21) had iron deficiency, as did 7% (n=244) of older women (ages 22-49) who were not anemic.
The researchers looked at potential risk factors for iron deficiency, including the age when women started menstruating, as well as their race/ethnicity, poverty status, food insecurity, tobacco or nicotine use, dietary information, body mass index, and physical activity.
All of these factors have been associated with iron-deficiency anemia in women in prior studies.
In this study, there was only 1 risk factor significantly associated with iron deficiency without anemia.
Young women (ages 12-21) who had been menstruating for more than 3 years had a significantly higher risk of iron deficiency without anemia (risk ratio=3.18).
The Journal of Pediatrics study
In this study, the researchers looked at whether a questionnaire could better predict iron status.
The questionnaire included questions on depression, poor attention, and daytime sleepiness, all of which have been associated with iron deficiency or iron-deficiency anemia, but were not captured in the prior NHANES analyses.
This questionnaire was compared to the 4 questions assessing iron-deficiency anemia risk in the Bright Futures Adolescent Previsit Questionnaire, a survey recommended for physician use by the American Academy of Pediatrics.
Ninety-six female adolescents participated in this study. Eighteen percent of them (n=17) had iron deficiency, and 5% (n=5) had iron-deficiency anemia.
Both the Bright Futures questions and the researchers’ risk assessment questionnaire poorly predicted ferritin and hemoglobin values in these subjects.
Mean differences in depression, poor attention, food insecurity, daytime sleepiness, and body mass index percentile were not significantly associated with ferritin or hemoglobin.
Conclusions
The results of these 2 studies suggest that risk factors and assessments cannot accurately determine which young women should receive testing for iron deficiency, although results from the first study might be used to determine when testing should occur.
“I think we need to establish the optimal timing for an objective assessment of adolescent iron deficiency and anemia,” Dr Sekhar said.
She believes the appropriate age may be 16 years old, when most females will have been menstruating for at least 3 years.
Further research will be needed to determine which blood test for iron deficiency without anemia is accurate, cost-efficient, and practical for routine doctor’s office use.
This test should be given with hemoglobin testing to catch all young women on the spectrum of iron deficiency, Dr Sekhar said. ![]()
A pair of studies suggest physicians should consider testing female adolescents for iron deficiency within a few years of starting menses.
Women are typically tested for anemia in their teens, with a quick and affordable hemoglobin test.
However, iron deficiency can develop years before anemia and can be missed by hemoglobin testing alone.
Blood tests for iron deficiency without anemia are more costly and more difficult to obtain than hemoglobin testing for anemia.
Deepa Sekhar, MD, of Penn State College of Medicine in Hershey, Pennsylvania, and her colleagues set out to determine risk factors for iron deficiency without anemia in order to pinpoint which women could benefit most from the more costly testing.
The results of the researchers’ 2 studies were published in PLOS ONE and The Journal of Pediatrics.
PLOS ONE study
The researchers evaluated data from 6216 females, ages 12 to 49, who took part in the National Health and Nutrition Examination Survey (NHANES) between 2003 and 2010. As part of the survey, participants were tested for both iron deficiency and anemia.
Eight percent of all subjects (n=494) had iron deficiency.
Nine percent (n=250) of non-anemic younger women (ages 12-21) had iron deficiency, as did 7% (n=244) of older women (ages 22-49) who were not anemic.
The researchers looked at potential risk factors for iron deficiency, including the age when women started menstruating, as well as their race/ethnicity, poverty status, food insecurity, tobacco or nicotine use, dietary information, body mass index, and physical activity.
All of these factors have been associated with iron-deficiency anemia in women in prior studies.
In this study, there was only 1 risk factor significantly associated with iron deficiency without anemia.
Young women (ages 12-21) who had been menstruating for more than 3 years had a significantly higher risk of iron deficiency without anemia (risk ratio=3.18).
The Journal of Pediatrics study
In this study, the researchers looked at whether a questionnaire could better predict iron status.
The questionnaire included questions on depression, poor attention, and daytime sleepiness, all of which have been associated with iron deficiency or iron-deficiency anemia, but were not captured in the prior NHANES analyses.
This questionnaire was compared to the 4 questions assessing iron-deficiency anemia risk in the Bright Futures Adolescent Previsit Questionnaire, a survey recommended for physician use by the American Academy of Pediatrics.
Ninety-six female adolescents participated in this study. Eighteen percent of them (n=17) had iron deficiency, and 5% (n=5) had iron-deficiency anemia.
Both the Bright Futures questions and the researchers’ risk assessment questionnaire poorly predicted ferritin and hemoglobin values in these subjects.
Mean differences in depression, poor attention, food insecurity, daytime sleepiness, and body mass index percentile were not significantly associated with ferritin or hemoglobin.
Conclusions
The results of these 2 studies suggest that risk factors and assessments cannot accurately determine which young women should receive testing for iron deficiency, although results from the first study might be used to determine when testing should occur.
“I think we need to establish the optimal timing for an objective assessment of adolescent iron deficiency and anemia,” Dr Sekhar said.
She believes the appropriate age may be 16 years old, when most females will have been menstruating for at least 3 years.
Further research will be needed to determine which blood test for iron deficiency without anemia is accurate, cost-efficient, and practical for routine doctor’s office use.
This test should be given with hemoglobin testing to catch all young women on the spectrum of iron deficiency, Dr Sekhar said. ![]()
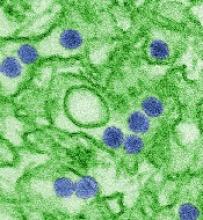
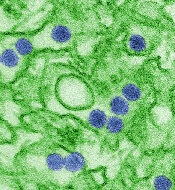
Vaccines protect unborn mice from Zika infection
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.” ![]()
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.” ![]()
Researchers have reported that 2 different vaccines can protect mice from Zika virus-induced congenital disease.
Female mice that were vaccinated before pregnancy and infected with Zika virus while pregnant bore pups that showed no trace of the virus.
These results, published in Cell, offer the first evidence that a vaccine administered prior to pregnancy can protect fetuses from Zika infection and resulting injury.
“There are several vaccines in human trials right now, but, to date, none of them has been shown to protect during pregnancy,” said Michael S. Diamond, MD, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We tested 2 different vaccines, and they both provided substantial protection.”
Last year, Dr Diamond and his colleagues developed a mouse model of Zika infection that mimics the effects of the infection in pregnant women.
Using this model, the researchers evaluated the ability of 2 vaccines to protect fetuses whose mothers were infected during pregnancy.
One of the vaccines is a messenger RNA (mRNA) vaccine, developed by Moderna Therapeutics, that is currently in safety testing in men and women who are not pregnant.
The other is a live-attenuated vaccine, developed by the University of Texas Medical Branch, that is being tested in animals.
For this study, groups of 18 to 20 female mice were vaccinated with one of the vaccines or a placebo, and some animals received a second dose of the same vaccine or placebo a month later.
Three weeks later, the researchers measured antibody levels in the mice’s blood as a measure of the strength of their immune response.
Both vaccines elicited very high levels of neutralizing antibodies against Zika, while the placebos did not.
After the mice became pregnant, they were infected with Zika on the sixth day of pregnancy, to mimic the experience of a woman bitten by a Zika-carrying mosquito early in pregnancy.
One week after infection, the researchers measured the amount of virus in the mothers and fetuses.
With both vaccines, fetuses and placentas from vaccinated mice contained very low levels of Zika’s genetic material.
For the mRNA vaccine, more than half of the placentas and fetuses had no detectable viral genetic material at all.
The live-attenuated vaccine was even more effective. In 78% of the placentas and 83% of the fetuses, no viral genetic material was found.
“The amount of viral genetic material in the placentas and fetuses from the vaccinated females was just above the limit of detection,” Dr Diamond said. “It’s not totally clear whether it was infectious virus or just remnants of viruses that had already been killed.”
In contrast, the amount of detectable viral material in the placentas and fetuses of unvaccinated mice was hundreds to thousands of times higher.
The researchers repeated the experiment with different mice so they could evaluate the pups at birth.
None of the mothers in the placebo group made it to term. The mothers became seriously ill, many of the fetuses showed high levels of infection and died in utero, and the placentas showed severe damage.
In contrast, the vaccinated mothers remained healthy, all of their pups were born without obvious signs of injury, and the newborn pups had no measurable Zika virus in their heads.
“In general, most doctors don’t want to vaccinate during pregnancy on the outside chance that the immune response itself could harm the fetus,” Dr Diamond said. “But if you’re in an area where Zika is circulating, you might vaccinate during pregnancy because the risk of Zika infection is worse than some theoretical risk of immune-mediated damage.”
The researchers did not assess whether the vaccines are safe and effective for use during pregnancy.
Such studies couldn’t really be done in mice, Dr Diamond explained, because mouse pregnancies only last 19 days. That doesn’t allow enough time for a protective immune response to develop before the pups are born.
Additionally, this study did not address the question of whether the vaccines work when pregnant women are infected with Zika through sexual contact. It is possible that Zika virus in semen can travel to the uterus and then to the fetus without passing through the bloodstream.
“The question is, ‘Would the immunity still hold up if the virus does not pass through the bloodstream?’“ Dr Diamond said. “We think it will hold up, but that has to be tested.” ![]()
PD-1 inhibitors treat resistant gray zone lymphoma
Three case reports published in The New England Journal of Medicine describe the successful use of PD-1 inhibitors in gray zone lymphoma.
Two patients who had failed treatment with DA-EPOCH-R (dose-adjusted etoposide, doxorubicin, and cyclophosphamide with vincristine, prednisone, and rituximab) ultimately responded to treatment with pembrolizumab.
Another patient—who had previously received 2 chemotherapy regimens, monotherapy with brentuximab vedotin, and radiation—responded to treatment with nivolumab.
Pembrolizumab treatment
An 18-year-old woman with mediastinal gray-zone lymphoma initially had a partial response to DA-EPOCH-R. However, she progressed 6 weeks after salvage radiotherapy.
She went on to receive pembrolizumab, had a complete metabolic response, and proceeded to allogeneic transplant after 235 days of treatment.
A 76-year-old man with mediastinal gray-zone lymphoma also had a partial response to DA-EPOCH-R but later progressed.
He proceeded to pembrolizumab and had a complete metabolic response. He was still in remission on day 381 of treatment.
Nivolumab treatment
The patient who received nivolumab is Bobbie Flexer, an 80-year-old retired mathematics professor.
“For me, trying nivolumab was a binary choice: I could try the drug or I could give up,” Flexer said.
She had initially achieved a complete metabolic response to DA-EPOCH-R, but her disease progressed after 6 cycles of treatment.
“Given Bobbie’s age and her resistance to chemotherapy, it was difficult to simply increase her dose,” said Flexer’s oncologist, Manali Kamdar, MD, of the University of Colorado School of Medicine in Aurora.
“Bobbie’s tumor biopsy expressed a protein called CD30, and so we started her on brentuximab, which targets these CD30 cells. Unfortunately, Bobbie’s disease progressed through multiple cycles of brentuximab. Subsequently, we switched her to another combined chemotherapy—namely, gemcitabine with oxaliplatin [plus rituximab].”
When that regimen and mediastinal radiation both proved unsuccessful, Dr Kamdar started Flexer on nivolumab.
“Within one dose, she was in less pain, and she looked much better,” Dr Kamdar said.
A PET scan after 6 doses showed that Flexer’s disease was in complete remission, and she was still in remission on day 161 of treatment.
She did experience adverse effects, including 2 bouts of pneumonitis, which were successfully treated with prednisone.
Flexer also experienced an uptick in pancreas enzymes that caused high blood glucose levels. She is learning to treat that side effect with insulin. And dietitians helped her manage expected gut-related side effects of nivolumab.
To Dr Kamdar, Flexer’s case was striking enough to warrant submitting a report to NEJM.
Coincidentally, the journal had just received 2 similar case reports from the National Institutes of Health, in which researchers had used pembrolizumab to target gray zone lymphoma in a nearly identical way.
Together, these cases suggest a new strategy for treating gray zone lymphoma. ![]()
Three case reports published in The New England Journal of Medicine describe the successful use of PD-1 inhibitors in gray zone lymphoma.
Two patients who had failed treatment with DA-EPOCH-R (dose-adjusted etoposide, doxorubicin, and cyclophosphamide with vincristine, prednisone, and rituximab) ultimately responded to treatment with pembrolizumab.
Another patient—who had previously received 2 chemotherapy regimens, monotherapy with brentuximab vedotin, and radiation—responded to treatment with nivolumab.
Pembrolizumab treatment
An 18-year-old woman with mediastinal gray-zone lymphoma initially had a partial response to DA-EPOCH-R. However, she progressed 6 weeks after salvage radiotherapy.
She went on to receive pembrolizumab, had a complete metabolic response, and proceeded to allogeneic transplant after 235 days of treatment.
A 76-year-old man with mediastinal gray-zone lymphoma also had a partial response to DA-EPOCH-R but later progressed.
He proceeded to pembrolizumab and had a complete metabolic response. He was still in remission on day 381 of treatment.
Nivolumab treatment
The patient who received nivolumab is Bobbie Flexer, an 80-year-old retired mathematics professor.
“For me, trying nivolumab was a binary choice: I could try the drug or I could give up,” Flexer said.
She had initially achieved a complete metabolic response to DA-EPOCH-R, but her disease progressed after 6 cycles of treatment.
“Given Bobbie’s age and her resistance to chemotherapy, it was difficult to simply increase her dose,” said Flexer’s oncologist, Manali Kamdar, MD, of the University of Colorado School of Medicine in Aurora.
“Bobbie’s tumor biopsy expressed a protein called CD30, and so we started her on brentuximab, which targets these CD30 cells. Unfortunately, Bobbie’s disease progressed through multiple cycles of brentuximab. Subsequently, we switched her to another combined chemotherapy—namely, gemcitabine with oxaliplatin [plus rituximab].”
When that regimen and mediastinal radiation both proved unsuccessful, Dr Kamdar started Flexer on nivolumab.
“Within one dose, she was in less pain, and she looked much better,” Dr Kamdar said.
A PET scan after 6 doses showed that Flexer’s disease was in complete remission, and she was still in remission on day 161 of treatment.
She did experience adverse effects, including 2 bouts of pneumonitis, which were successfully treated with prednisone.
Flexer also experienced an uptick in pancreas enzymes that caused high blood glucose levels. She is learning to treat that side effect with insulin. And dietitians helped her manage expected gut-related side effects of nivolumab.
To Dr Kamdar, Flexer’s case was striking enough to warrant submitting a report to NEJM.
Coincidentally, the journal had just received 2 similar case reports from the National Institutes of Health, in which researchers had used pembrolizumab to target gray zone lymphoma in a nearly identical way.
Together, these cases suggest a new strategy for treating gray zone lymphoma. ![]()
Three case reports published in The New England Journal of Medicine describe the successful use of PD-1 inhibitors in gray zone lymphoma.
Two patients who had failed treatment with DA-EPOCH-R (dose-adjusted etoposide, doxorubicin, and cyclophosphamide with vincristine, prednisone, and rituximab) ultimately responded to treatment with pembrolizumab.
Another patient—who had previously received 2 chemotherapy regimens, monotherapy with brentuximab vedotin, and radiation—responded to treatment with nivolumab.
Pembrolizumab treatment
An 18-year-old woman with mediastinal gray-zone lymphoma initially had a partial response to DA-EPOCH-R. However, she progressed 6 weeks after salvage radiotherapy.
She went on to receive pembrolizumab, had a complete metabolic response, and proceeded to allogeneic transplant after 235 days of treatment.
A 76-year-old man with mediastinal gray-zone lymphoma also had a partial response to DA-EPOCH-R but later progressed.
He proceeded to pembrolizumab and had a complete metabolic response. He was still in remission on day 381 of treatment.
Nivolumab treatment
The patient who received nivolumab is Bobbie Flexer, an 80-year-old retired mathematics professor.
“For me, trying nivolumab was a binary choice: I could try the drug or I could give up,” Flexer said.
She had initially achieved a complete metabolic response to DA-EPOCH-R, but her disease progressed after 6 cycles of treatment.
“Given Bobbie’s age and her resistance to chemotherapy, it was difficult to simply increase her dose,” said Flexer’s oncologist, Manali Kamdar, MD, of the University of Colorado School of Medicine in Aurora.
“Bobbie’s tumor biopsy expressed a protein called CD30, and so we started her on brentuximab, which targets these CD30 cells. Unfortunately, Bobbie’s disease progressed through multiple cycles of brentuximab. Subsequently, we switched her to another combined chemotherapy—namely, gemcitabine with oxaliplatin [plus rituximab].”
When that regimen and mediastinal radiation both proved unsuccessful, Dr Kamdar started Flexer on nivolumab.
“Within one dose, she was in less pain, and she looked much better,” Dr Kamdar said.
A PET scan after 6 doses showed that Flexer’s disease was in complete remission, and she was still in remission on day 161 of treatment.
She did experience adverse effects, including 2 bouts of pneumonitis, which were successfully treated with prednisone.
Flexer also experienced an uptick in pancreas enzymes that caused high blood glucose levels. She is learning to treat that side effect with insulin. And dietitians helped her manage expected gut-related side effects of nivolumab.
To Dr Kamdar, Flexer’s case was striking enough to warrant submitting a report to NEJM.
Coincidentally, the journal had just received 2 similar case reports from the National Institutes of Health, in which researchers had used pembrolizumab to target gray zone lymphoma in a nearly identical way.
Together, these cases suggest a new strategy for treating gray zone lymphoma. ![]()
Gene therapy maintains normal FVIII levels long-term
BERLIN—New research suggests the investigational gene therapy BMN 270 can allow patients with severe hemophilia A to maintain normal factor VIII (FVIII) levels for over a year.
In a phase 1/2 study, patients who received the highest dose of BMN 270 had median and mean FVIII levels that were consistently within the normal range from week 20 to week 52 and beyond.
The highest dose of BMN 270 reduced the mean annual FVIII infusions by 94% and the mean annualized bleed rate (ABR) by 97%, when compared to prophylaxis.
BMN 270 was also considered well tolerated, and none of the patients developed FVIII inhibitors.
The most common adverse event (AE) in this study was alanine aminotransferase (ALT) elevations. In fact, the increase in ALT levels exceeded a pre-specified threshold, which resulted in the study being placed on hold last year.
However, the hold was ultimately lifted. All cases of ALT increase were non-serious, and all patients with ALT increases have either stopped receiving corticosteroids or are being tapered off of them.
John Pasi, PhD, of Barts and the London School of Medicine and Dentistry in London, UK, presented these results as a late-breaking abstract at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The research was sponsored by BioMarin.
In this phase 1/2 study, 15 patients with severe hemophilia A (FVIII activity levels less than 1%) received a single dose of BMN 270.
Seven patients received a dose of 6e13 vg/kg, 6 received 4e13 vg/kg, and 2 were treated at lower doses as part of dose-escalation and did not achieve therapeutic efficacy.
Safety
Overall, BMN 270 was considered well tolerated across all doses. None of the patients developed inhibitors to FVIII, and none of them withdrew from the study.
The most common AEs across all dose cohorts were ALT elevations (n=10, 67%), arthralgia (n=7, 47%), and back pain, fatigue, and headache (n=5, 33% each).
All ALT increases were non-serious, of limited duration (lasting 0.4 to 7 weeks), and grade 1 in severity. All 7 patients at the 6e13 vg/kg dose remain off of corticosteroids, with no lasting significant impact on FVIII expression and normal ALT levels.
Three of the 6 patients in the 4e13 vg/kg dose cohort received corticosteroids for ALT increases. One has successfully tapered off corticosteroids, and 2 are still tapering off of them.
Two patients reported serious AEs during the study.
One patient was hospitalized for observation after developing grade 2 pyrexia with myalgia and headache within 24 hours of receiving BMN 270 (4e13 vg/kg dose). The event resolved within 48 hours following treatment with paracetamol. The event was considered related to BMN 270.
The other serious AE—planned total knee replacement for chronic arthropathy—was not related to BMN 270.
FVIII levels: 6e13 vg/kg
For patients in the 6e13 vg/kg dose cohort, median and mean FVIII levels from week 20 through 52 have been consistently within the normal levels post-treatment. At 1 year after dosing, the median and mean FVIII levels continue to be above 50%.
Table 1: FVIII levels (%) of 6e13 vg/kg dose patients by visit (n=7)
| Week*
|
20 | 24 | 28 | 32 | 36 | 40 | 44 | 48 | 52 |
| 6e13 vg/kg dose | |||||||||
| N** | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 |
| Median
FVIII level*** (%) |
97 | 101 | 122 | 99 | 99 | 111 | 105 | 105 | 89 |
| Mean
FVIII level*** (%) |
118 | 129 | 123 | 122 | 116 | 124 | 122 | 106 | 104 |
| Range
(low, high) |
(12, 254) | (12, 227) | (15, 257) | (26, 316) | (31, 273) | (17, 264) | (20,242) | (23,196) | (20, 218) |
* Weeks were windowed by +/- 2 weeks
** For week 32, one patient had no FVIII reading
***Bolded numbers are in the normal range of FVIII as defined by the World Federation of Hemophilia
FVIII levels: 4e13 vg/kg
For the 4e13 vg/kg dose cohort, the median and mean FVIII levels from week 8 to 24 are in the mild level. Three of these subjects, who have been observed for 24 weeks, are at the upper end of mild.
Table 2: FVIII levels (%) of 4e13 vg/kg dose patients* by visit (n=6)
| Week*
|
4 | 8 | 12 | 16 | 20 | 24 |
|
4e13 vg/kg dose |
||||||
| N | 6 | 6 | 6 | 3 | 3 | 3 |
| Median
FVIII level** (%) |
4 | 15 | 21 | 35 | 37 | 33 |
| Mean
FVIII level** (%) |
5 | 13 | 19 | 33 | 38 | 33 |
| Range
(low, high) |
(2,10) | (3,21) | (6,32) | (28,38) | (31,45) | (24,41) |
*Weeks were windowed by +/- 2 weeks
** Bolded numbers are in the mild range of FVIII as defined by the World Federation of Hemophilia
ABR and FVIII infusions
Six of the 7 patients in the 6e13 vg/kg cohort were on pre-study prophylaxis.
After these patients received a single dose BMN270 and reached a FVIII level above 5%, the mean ABR was reduced by 97%, from 16.3 to 0.5. The median ABR for these patients was reduced from 16.5 to 0.
The mean annualized FVIII infusions were reduced by 94%, from 136.7 to 8.5. And the median annualized FVIII infusions were reduced from 138.5 to 0.
All 6 patients in the 4e13 vg/kg dose cohort were on pre-study prophylaxis.
The mean ABR was reduced from 12.2 pre-study to 0 after they reached an FVIII level above 5%. The median ABR for these patients was reduced from 8.0 to 0.
The mean annualized FVIII infusions were reduced from 144.2 to 0. The median annualized FVIII infusions were reduced from 155.5 to 0.
“Patients at the 2 highest doses have stopped prophylactic treatment and, to date, bleeds have effectively been eliminated,” Dr Pasi noted.
Based on these results, BioMarin is planning a phase 3 registrational study of BMN 270. The study will likely include fewer than 100 patients and collect data for no longer than a year after a single dose of BMN 270, with subsequent long-term follow-up.
The company is moving the 6e13 vg/kg dose forward but will consider doing an additional study with the 4e13 vg/kg dose at a later date. ![]()
BERLIN—New research suggests the investigational gene therapy BMN 270 can allow patients with severe hemophilia A to maintain normal factor VIII (FVIII) levels for over a year.
In a phase 1/2 study, patients who received the highest dose of BMN 270 had median and mean FVIII levels that were consistently within the normal range from week 20 to week 52 and beyond.
The highest dose of BMN 270 reduced the mean annual FVIII infusions by 94% and the mean annualized bleed rate (ABR) by 97%, when compared to prophylaxis.
BMN 270 was also considered well tolerated, and none of the patients developed FVIII inhibitors.
The most common adverse event (AE) in this study was alanine aminotransferase (ALT) elevations. In fact, the increase in ALT levels exceeded a pre-specified threshold, which resulted in the study being placed on hold last year.
However, the hold was ultimately lifted. All cases of ALT increase were non-serious, and all patients with ALT increases have either stopped receiving corticosteroids or are being tapered off of them.
John Pasi, PhD, of Barts and the London School of Medicine and Dentistry in London, UK, presented these results as a late-breaking abstract at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The research was sponsored by BioMarin.
In this phase 1/2 study, 15 patients with severe hemophilia A (FVIII activity levels less than 1%) received a single dose of BMN 270.
Seven patients received a dose of 6e13 vg/kg, 6 received 4e13 vg/kg, and 2 were treated at lower doses as part of dose-escalation and did not achieve therapeutic efficacy.
Safety
Overall, BMN 270 was considered well tolerated across all doses. None of the patients developed inhibitors to FVIII, and none of them withdrew from the study.
The most common AEs across all dose cohorts were ALT elevations (n=10, 67%), arthralgia (n=7, 47%), and back pain, fatigue, and headache (n=5, 33% each).
All ALT increases were non-serious, of limited duration (lasting 0.4 to 7 weeks), and grade 1 in severity. All 7 patients at the 6e13 vg/kg dose remain off of corticosteroids, with no lasting significant impact on FVIII expression and normal ALT levels.
Three of the 6 patients in the 4e13 vg/kg dose cohort received corticosteroids for ALT increases. One has successfully tapered off corticosteroids, and 2 are still tapering off of them.
Two patients reported serious AEs during the study.
One patient was hospitalized for observation after developing grade 2 pyrexia with myalgia and headache within 24 hours of receiving BMN 270 (4e13 vg/kg dose). The event resolved within 48 hours following treatment with paracetamol. The event was considered related to BMN 270.
The other serious AE—planned total knee replacement for chronic arthropathy—was not related to BMN 270.
FVIII levels: 6e13 vg/kg
For patients in the 6e13 vg/kg dose cohort, median and mean FVIII levels from week 20 through 52 have been consistently within the normal levels post-treatment. At 1 year after dosing, the median and mean FVIII levels continue to be above 50%.
Table 1: FVIII levels (%) of 6e13 vg/kg dose patients by visit (n=7)
| Week*
|
20 | 24 | 28 | 32 | 36 | 40 | 44 | 48 | 52 |
| 6e13 vg/kg dose | |||||||||
| N** | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 |
| Median
FVIII level*** (%) |
97 | 101 | 122 | 99 | 99 | 111 | 105 | 105 | 89 |
| Mean
FVIII level*** (%) |
118 | 129 | 123 | 122 | 116 | 124 | 122 | 106 | 104 |
| Range
(low, high) |
(12, 254) | (12, 227) | (15, 257) | (26, 316) | (31, 273) | (17, 264) | (20,242) | (23,196) | (20, 218) |
* Weeks were windowed by +/- 2 weeks
** For week 32, one patient had no FVIII reading
***Bolded numbers are in the normal range of FVIII as defined by the World Federation of Hemophilia
FVIII levels: 4e13 vg/kg
For the 4e13 vg/kg dose cohort, the median and mean FVIII levels from week 8 to 24 are in the mild level. Three of these subjects, who have been observed for 24 weeks, are at the upper end of mild.
Table 2: FVIII levels (%) of 4e13 vg/kg dose patients* by visit (n=6)
| Week*
|
4 | 8 | 12 | 16 | 20 | 24 |
|
4e13 vg/kg dose |
||||||
| N | 6 | 6 | 6 | 3 | 3 | 3 |
| Median
FVIII level** (%) |
4 | 15 | 21 | 35 | 37 | 33 |
| Mean
FVIII level** (%) |
5 | 13 | 19 | 33 | 38 | 33 |
| Range
(low, high) |
(2,10) | (3,21) | (6,32) | (28,38) | (31,45) | (24,41) |
*Weeks were windowed by +/- 2 weeks
** Bolded numbers are in the mild range of FVIII as defined by the World Federation of Hemophilia
ABR and FVIII infusions
Six of the 7 patients in the 6e13 vg/kg cohort were on pre-study prophylaxis.
After these patients received a single dose BMN270 and reached a FVIII level above 5%, the mean ABR was reduced by 97%, from 16.3 to 0.5. The median ABR for these patients was reduced from 16.5 to 0.
The mean annualized FVIII infusions were reduced by 94%, from 136.7 to 8.5. And the median annualized FVIII infusions were reduced from 138.5 to 0.
All 6 patients in the 4e13 vg/kg dose cohort were on pre-study prophylaxis.
The mean ABR was reduced from 12.2 pre-study to 0 after they reached an FVIII level above 5%. The median ABR for these patients was reduced from 8.0 to 0.
The mean annualized FVIII infusions were reduced from 144.2 to 0. The median annualized FVIII infusions were reduced from 155.5 to 0.
“Patients at the 2 highest doses have stopped prophylactic treatment and, to date, bleeds have effectively been eliminated,” Dr Pasi noted.
Based on these results, BioMarin is planning a phase 3 registrational study of BMN 270. The study will likely include fewer than 100 patients and collect data for no longer than a year after a single dose of BMN 270, with subsequent long-term follow-up.
The company is moving the 6e13 vg/kg dose forward but will consider doing an additional study with the 4e13 vg/kg dose at a later date. ![]()
BERLIN—New research suggests the investigational gene therapy BMN 270 can allow patients with severe hemophilia A to maintain normal factor VIII (FVIII) levels for over a year.
In a phase 1/2 study, patients who received the highest dose of BMN 270 had median and mean FVIII levels that were consistently within the normal range from week 20 to week 52 and beyond.
The highest dose of BMN 270 reduced the mean annual FVIII infusions by 94% and the mean annualized bleed rate (ABR) by 97%, when compared to prophylaxis.
BMN 270 was also considered well tolerated, and none of the patients developed FVIII inhibitors.
The most common adverse event (AE) in this study was alanine aminotransferase (ALT) elevations. In fact, the increase in ALT levels exceeded a pre-specified threshold, which resulted in the study being placed on hold last year.
However, the hold was ultimately lifted. All cases of ALT increase were non-serious, and all patients with ALT increases have either stopped receiving corticosteroids or are being tapered off of them.
John Pasi, PhD, of Barts and the London School of Medicine and Dentistry in London, UK, presented these results as a late-breaking abstract at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The research was sponsored by BioMarin.
In this phase 1/2 study, 15 patients with severe hemophilia A (FVIII activity levels less than 1%) received a single dose of BMN 270.
Seven patients received a dose of 6e13 vg/kg, 6 received 4e13 vg/kg, and 2 were treated at lower doses as part of dose-escalation and did not achieve therapeutic efficacy.
Safety
Overall, BMN 270 was considered well tolerated across all doses. None of the patients developed inhibitors to FVIII, and none of them withdrew from the study.
The most common AEs across all dose cohorts were ALT elevations (n=10, 67%), arthralgia (n=7, 47%), and back pain, fatigue, and headache (n=5, 33% each).
All ALT increases were non-serious, of limited duration (lasting 0.4 to 7 weeks), and grade 1 in severity. All 7 patients at the 6e13 vg/kg dose remain off of corticosteroids, with no lasting significant impact on FVIII expression and normal ALT levels.
Three of the 6 patients in the 4e13 vg/kg dose cohort received corticosteroids for ALT increases. One has successfully tapered off corticosteroids, and 2 are still tapering off of them.
Two patients reported serious AEs during the study.
One patient was hospitalized for observation after developing grade 2 pyrexia with myalgia and headache within 24 hours of receiving BMN 270 (4e13 vg/kg dose). The event resolved within 48 hours following treatment with paracetamol. The event was considered related to BMN 270.
The other serious AE—planned total knee replacement for chronic arthropathy—was not related to BMN 270.
FVIII levels: 6e13 vg/kg
For patients in the 6e13 vg/kg dose cohort, median and mean FVIII levels from week 20 through 52 have been consistently within the normal levels post-treatment. At 1 year after dosing, the median and mean FVIII levels continue to be above 50%.
Table 1: FVIII levels (%) of 6e13 vg/kg dose patients by visit (n=7)
| Week*
|
20 | 24 | 28 | 32 | 36 | 40 | 44 | 48 | 52 |
| 6e13 vg/kg dose | |||||||||
| N** | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 |
| Median
FVIII level*** (%) |
97 | 101 | 122 | 99 | 99 | 111 | 105 | 105 | 89 |
| Mean
FVIII level*** (%) |
118 | 129 | 123 | 122 | 116 | 124 | 122 | 106 | 104 |
| Range
(low, high) |
(12, 254) | (12, 227) | (15, 257) | (26, 316) | (31, 273) | (17, 264) | (20,242) | (23,196) | (20, 218) |
* Weeks were windowed by +/- 2 weeks
** For week 32, one patient had no FVIII reading
***Bolded numbers are in the normal range of FVIII as defined by the World Federation of Hemophilia
FVIII levels: 4e13 vg/kg
For the 4e13 vg/kg dose cohort, the median and mean FVIII levels from week 8 to 24 are in the mild level. Three of these subjects, who have been observed for 24 weeks, are at the upper end of mild.
Table 2: FVIII levels (%) of 4e13 vg/kg dose patients* by visit (n=6)
| Week*
|
4 | 8 | 12 | 16 | 20 | 24 |
|
4e13 vg/kg dose |
||||||
| N | 6 | 6 | 6 | 3 | 3 | 3 |
| Median
FVIII level** (%) |
4 | 15 | 21 | 35 | 37 | 33 |
| Mean
FVIII level** (%) |
5 | 13 | 19 | 33 | 38 | 33 |
| Range
(low, high) |
(2,10) | (3,21) | (6,32) | (28,38) | (31,45) | (24,41) |
*Weeks were windowed by +/- 2 weeks
** Bolded numbers are in the mild range of FVIII as defined by the World Federation of Hemophilia
ABR and FVIII infusions
Six of the 7 patients in the 6e13 vg/kg cohort were on pre-study prophylaxis.
After these patients received a single dose BMN270 and reached a FVIII level above 5%, the mean ABR was reduced by 97%, from 16.3 to 0.5. The median ABR for these patients was reduced from 16.5 to 0.
The mean annualized FVIII infusions were reduced by 94%, from 136.7 to 8.5. And the median annualized FVIII infusions were reduced from 138.5 to 0.
All 6 patients in the 4e13 vg/kg dose cohort were on pre-study prophylaxis.
The mean ABR was reduced from 12.2 pre-study to 0 after they reached an FVIII level above 5%. The median ABR for these patients was reduced from 8.0 to 0.
The mean annualized FVIII infusions were reduced from 144.2 to 0. The median annualized FVIII infusions were reduced from 155.5 to 0.
“Patients at the 2 highest doses have stopped prophylactic treatment and, to date, bleeds have effectively been eliminated,” Dr Pasi noted.
Based on these results, BioMarin is planning a phase 3 registrational study of BMN 270. The study will likely include fewer than 100 patients and collect data for no longer than a year after a single dose of BMN 270, with subsequent long-term follow-up.
The company is moving the 6e13 vg/kg dose forward but will consider doing an additional study with the 4e13 vg/kg dose at a later date. ![]()
CTL019 produces responses in rel/ref DLBCL
The chimeric antigen receptor (CAR) T-cell therapy CTL019 produced a high response rate in a phase 2 trial of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to researchers.
An interim analysis of the JULIET trial revealed a 3-month overall response rate (ORR) of 45%.
Thirty-seven percent of patients had a complete response (CR), and all of the patients who were in CR at 3 months were still in CR at the data cutoff point.
This confirms the high response rates and durable responses observed in a previous single-center trial*, said JULIET investigator Gilles Salles, MD, PhD, of Hospices Civils de Lyon in Lyon, France.
Dr Salles presented results from JULIET at the 22nd Congress of the European Hematology Association (EHA) in Madrid, Spain (abstract LB2604).
The results were also presented at the 14th International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland (abstract 007).
The study was sponsored by Novartis.
Patients
JULIET enrolled 141 patients age 18 and older with relapsed/refractory DLBCL.
Forty-three patients discontinued the study before receiving CTL019—28 due to progressive disease (including 16 deaths), 9 due to an inability to manufacture CTL019, 2 due to adverse events, 1 due to investigator decision, 1 due to study withdrawal, and 1 due to protocol deviation.
Eighty-five patients were infused. The remaining 13 patients were pending infusion at the data cutoff—December 20, 2016.
The median age of the 85 infused patients was 56 (range, 24-75). Ninety-six percent of patients had DLBCL not otherwise specified. Fifty-one percent had germinal center B-cell type DLBCL.
Fifty-four percent of patients had an ECOG performance status of 0, and 46% had a status of 1. Fifty-three percent of patients had stage IV disease, and 8% had bone marrow involvement.
Forty percent of patients had 2 prior lines of antineoplastic therapy, 29% had 3, and 31% had 4 to 7 prior lines.
Forty-one percent of patients were refractory to their last therapy, and 59% had relapsed after their last therapy. Fifty-one percent of patients had prior autologous stem cell transplant.
Treatment
Seventy-six patients (89%) received bridging chemotherapy to prevent disease progression during CTL019 manufacturing. This treatment was completed 2 to 14 days prior to CTL019 infusion.
The median CTL019 cell dose was 3.1 x 108 (range, 0.1-6.0 x 108).
Response
Fifty-one patients were evaluated for response. The median time from infusion to data cutoff was 3.7 months.
The best ORR was 59%, with a CR rate of 43% and a partial response rate of 16%. Twelve percent of patients had stable disease, and 24% progressed.
At 3 months, the ORR was 45%. The CR rate was 37%, and the partial response rate was 8%.
“All patients in CR at 3 months remained in CR at follow-up, and the median duration of response was not reached,” Dr Salles noted.
None of the responders went on to receive a transplant.
Safety
All 85 patients were evaluated for safety. Adverse events of special interest, occurring within 8 weeks of CTL019 infusion, were:
- Cytokine release syndrome—57% all grades, 17% grade 3, 9% grade 4
- Infections—27% all grades, 12% grade 3, 1% grade 4
- Cytopenias not resolved by day 28—26% all grades, 13% grade 3, 8% grade 4
- Neurologic events—21% all grades, 9% grade 3, 4% grade 4
- Febrile neutropenia—14% all grades, 13% grade 3, 1% grade 4
- Tumor lysis syndrome—1% grade 3.
“Adverse events were reversible and effectively managed at the different centers by appropriately trained study personnel,” Dr Salles noted. “There were no CTL019-related deaths and no cerebral edema.” ![]()
The chimeric antigen receptor (CAR) T-cell therapy CTL019 produced a high response rate in a phase 2 trial of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to researchers.
An interim analysis of the JULIET trial revealed a 3-month overall response rate (ORR) of 45%.
Thirty-seven percent of patients had a complete response (CR), and all of the patients who were in CR at 3 months were still in CR at the data cutoff point.
This confirms the high response rates and durable responses observed in a previous single-center trial*, said JULIET investigator Gilles Salles, MD, PhD, of Hospices Civils de Lyon in Lyon, France.
Dr Salles presented results from JULIET at the 22nd Congress of the European Hematology Association (EHA) in Madrid, Spain (abstract LB2604).
The results were also presented at the 14th International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland (abstract 007).
The study was sponsored by Novartis.
Patients
JULIET enrolled 141 patients age 18 and older with relapsed/refractory DLBCL.
Forty-three patients discontinued the study before receiving CTL019—28 due to progressive disease (including 16 deaths), 9 due to an inability to manufacture CTL019, 2 due to adverse events, 1 due to investigator decision, 1 due to study withdrawal, and 1 due to protocol deviation.
Eighty-five patients were infused. The remaining 13 patients were pending infusion at the data cutoff—December 20, 2016.
The median age of the 85 infused patients was 56 (range, 24-75). Ninety-six percent of patients had DLBCL not otherwise specified. Fifty-one percent had germinal center B-cell type DLBCL.
Fifty-four percent of patients had an ECOG performance status of 0, and 46% had a status of 1. Fifty-three percent of patients had stage IV disease, and 8% had bone marrow involvement.
Forty percent of patients had 2 prior lines of antineoplastic therapy, 29% had 3, and 31% had 4 to 7 prior lines.
Forty-one percent of patients were refractory to their last therapy, and 59% had relapsed after their last therapy. Fifty-one percent of patients had prior autologous stem cell transplant.
Treatment
Seventy-six patients (89%) received bridging chemotherapy to prevent disease progression during CTL019 manufacturing. This treatment was completed 2 to 14 days prior to CTL019 infusion.
The median CTL019 cell dose was 3.1 x 108 (range, 0.1-6.0 x 108).
Response
Fifty-one patients were evaluated for response. The median time from infusion to data cutoff was 3.7 months.
The best ORR was 59%, with a CR rate of 43% and a partial response rate of 16%. Twelve percent of patients had stable disease, and 24% progressed.
At 3 months, the ORR was 45%. The CR rate was 37%, and the partial response rate was 8%.
“All patients in CR at 3 months remained in CR at follow-up, and the median duration of response was not reached,” Dr Salles noted.
None of the responders went on to receive a transplant.
Safety
All 85 patients were evaluated for safety. Adverse events of special interest, occurring within 8 weeks of CTL019 infusion, were:
- Cytokine release syndrome—57% all grades, 17% grade 3, 9% grade 4
- Infections—27% all grades, 12% grade 3, 1% grade 4
- Cytopenias not resolved by day 28—26% all grades, 13% grade 3, 8% grade 4
- Neurologic events—21% all grades, 9% grade 3, 4% grade 4
- Febrile neutropenia—14% all grades, 13% grade 3, 1% grade 4
- Tumor lysis syndrome—1% grade 3.
“Adverse events were reversible and effectively managed at the different centers by appropriately trained study personnel,” Dr Salles noted. “There were no CTL019-related deaths and no cerebral edema.” ![]()
The chimeric antigen receptor (CAR) T-cell therapy CTL019 produced a high response rate in a phase 2 trial of adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to researchers.
An interim analysis of the JULIET trial revealed a 3-month overall response rate (ORR) of 45%.
Thirty-seven percent of patients had a complete response (CR), and all of the patients who were in CR at 3 months were still in CR at the data cutoff point.
This confirms the high response rates and durable responses observed in a previous single-center trial*, said JULIET investigator Gilles Salles, MD, PhD, of Hospices Civils de Lyon in Lyon, France.
Dr Salles presented results from JULIET at the 22nd Congress of the European Hematology Association (EHA) in Madrid, Spain (abstract LB2604).
The results were also presented at the 14th International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland (abstract 007).
The study was sponsored by Novartis.
Patients
JULIET enrolled 141 patients age 18 and older with relapsed/refractory DLBCL.
Forty-three patients discontinued the study before receiving CTL019—28 due to progressive disease (including 16 deaths), 9 due to an inability to manufacture CTL019, 2 due to adverse events, 1 due to investigator decision, 1 due to study withdrawal, and 1 due to protocol deviation.
Eighty-five patients were infused. The remaining 13 patients were pending infusion at the data cutoff—December 20, 2016.
The median age of the 85 infused patients was 56 (range, 24-75). Ninety-six percent of patients had DLBCL not otherwise specified. Fifty-one percent had germinal center B-cell type DLBCL.
Fifty-four percent of patients had an ECOG performance status of 0, and 46% had a status of 1. Fifty-three percent of patients had stage IV disease, and 8% had bone marrow involvement.
Forty percent of patients had 2 prior lines of antineoplastic therapy, 29% had 3, and 31% had 4 to 7 prior lines.
Forty-one percent of patients were refractory to their last therapy, and 59% had relapsed after their last therapy. Fifty-one percent of patients had prior autologous stem cell transplant.
Treatment
Seventy-six patients (89%) received bridging chemotherapy to prevent disease progression during CTL019 manufacturing. This treatment was completed 2 to 14 days prior to CTL019 infusion.
The median CTL019 cell dose was 3.1 x 108 (range, 0.1-6.0 x 108).
Response
Fifty-one patients were evaluated for response. The median time from infusion to data cutoff was 3.7 months.
The best ORR was 59%, with a CR rate of 43% and a partial response rate of 16%. Twelve percent of patients had stable disease, and 24% progressed.
At 3 months, the ORR was 45%. The CR rate was 37%, and the partial response rate was 8%.
“All patients in CR at 3 months remained in CR at follow-up, and the median duration of response was not reached,” Dr Salles noted.
None of the responders went on to receive a transplant.
Safety
All 85 patients were evaluated for safety. Adverse events of special interest, occurring within 8 weeks of CTL019 infusion, were:
- Cytokine release syndrome—57% all grades, 17% grade 3, 9% grade 4
- Infections—27% all grades, 12% grade 3, 1% grade 4
- Cytopenias not resolved by day 28—26% all grades, 13% grade 3, 8% grade 4
- Neurologic events—21% all grades, 9% grade 3, 4% grade 4
- Febrile neutropenia—14% all grades, 13% grade 3, 1% grade 4
- Tumor lysis syndrome—1% grade 3.
“Adverse events were reversible and effectively managed at the different centers by appropriately trained study personnel,” Dr Salles noted. “There were no CTL019-related deaths and no cerebral edema.”
De-escalation may improve success of TKI cessation
MADRID—Results of the DESTINY trial suggest that chronic myeloid leukemia (CML) patients may improve their chances of successfully stopping treatment with tyrosine kinase inhibitors (TKIs) by first reducing the dose they receive.
CML patients in deep molecular response (MR4) at study entry had a low rate of recurrence when they first de-escalated their TKI dose—receiving half the standard dose—for a year and then completely stopped receiving TKI treatment for a year.
The 2-year recurrence-free survival (RFS) rate was 77%, which is better than the RFS in any comparable study to date, according to Richard Clark, MD, of the University of Liverpool in Liverpool, UK, and his colleagues.
Dr Clark presented results from DESTINY at the 22nd Congress of the European Hematology Association (EHA) as abstract S423.
DESTINY included 174 CML patients (98 male, 76 female) in stable major molecular response (MMR).
At study entry, patients had received imatinib (n=148), nilotinib (n=16), or dasatinib (n=10) for a median duration of 6.8 years.
For the first 12 months of the study, patients had their TKI dose reduced to half the standard dose. So they received imatinib at 200 mg daily, dasatinib at 50 mg daily, or nilotinib at 200 mg twice daily. After that, patients stopped treatment completely.
After the first 12 months, molecular recurrence was lower in patients with stable MR4 at study entry than in patients who were not in MR4 (but still in MMR)—2.4% (3/125) and 18.4% (9/49), respectively (P<0.001).
During the following 12 months, in which patients had completely stopped TKI treatment, there were 26 recurrences and 4 withdrawals among the remaining 117 patients who were in MR4 at baseline, as well as 20 recurrences and 4 withdrawals among the 36 patients not in MR4.
So the RFS was 77% among patients in MR4 at baseline and 39% among the patients not in MR4 (P<0.001).
The researchers said the probability of RFS was unrelated to patients’ age, gender, performance status, or the prior TKI they received (imatinib vs second-generation TKI).
All patients with recurrence ultimately returned to deep remissions when they resumed their TKI treatment.
“TKI de-escalation is safe for most CML patients with stable and excellent responses to TKI therapy after some years of treatment and is associated with improvement in symptoms,” Dr Clark said.
“Overall, our findings are better than any other studies worldwide and imply that our unique, gradual withdrawal of treatment might be important. We don’t yet understand why our results are so good, but this is a happy problem to have.”
MADRID—Results of the DESTINY trial suggest that chronic myeloid leukemia (CML) patients may improve their chances of successfully stopping treatment with tyrosine kinase inhibitors (TKIs) by first reducing the dose they receive.
CML patients in deep molecular response (MR4) at study entry had a low rate of recurrence when they first de-escalated their TKI dose—receiving half the standard dose—for a year and then completely stopped receiving TKI treatment for a year.
The 2-year recurrence-free survival (RFS) rate was 77%, which is better than the RFS in any comparable study to date, according to Richard Clark, MD, of the University of Liverpool in Liverpool, UK, and his colleagues.
Dr Clark presented results from DESTINY at the 22nd Congress of the European Hematology Association (EHA) as abstract S423.
DESTINY included 174 CML patients (98 male, 76 female) in stable major molecular response (MMR).
At study entry, patients had received imatinib (n=148), nilotinib (n=16), or dasatinib (n=10) for a median duration of 6.8 years.
For the first 12 months of the study, patients had their TKI dose reduced to half the standard dose. So they received imatinib at 200 mg daily, dasatinib at 50 mg daily, or nilotinib at 200 mg twice daily. After that, patients stopped treatment completely.
After the first 12 months, molecular recurrence was lower in patients with stable MR4 at study entry than in patients who were not in MR4 (but still in MMR)—2.4% (3/125) and 18.4% (9/49), respectively (P<0.001).
During the following 12 months, in which patients had completely stopped TKI treatment, there were 26 recurrences and 4 withdrawals among the remaining 117 patients who were in MR4 at baseline, as well as 20 recurrences and 4 withdrawals among the 36 patients not in MR4.
So the RFS was 77% among patients in MR4 at baseline and 39% among the patients not in MR4 (P<0.001).
The researchers said the probability of RFS was unrelated to patients’ age, gender, performance status, or the prior TKI they received (imatinib vs second-generation TKI).
All patients with recurrence ultimately returned to deep remissions when they resumed their TKI treatment.
“TKI de-escalation is safe for most CML patients with stable and excellent responses to TKI therapy after some years of treatment and is associated with improvement in symptoms,” Dr Clark said.
“Overall, our findings are better than any other studies worldwide and imply that our unique, gradual withdrawal of treatment might be important. We don’t yet understand why our results are so good, but this is a happy problem to have.”
MADRID—Results of the DESTINY trial suggest that chronic myeloid leukemia (CML) patients may improve their chances of successfully stopping treatment with tyrosine kinase inhibitors (TKIs) by first reducing the dose they receive.
CML patients in deep molecular response (MR4) at study entry had a low rate of recurrence when they first de-escalated their TKI dose—receiving half the standard dose—for a year and then completely stopped receiving TKI treatment for a year.
The 2-year recurrence-free survival (RFS) rate was 77%, which is better than the RFS in any comparable study to date, according to Richard Clark, MD, of the University of Liverpool in Liverpool, UK, and his colleagues.
Dr Clark presented results from DESTINY at the 22nd Congress of the European Hematology Association (EHA) as abstract S423.
DESTINY included 174 CML patients (98 male, 76 female) in stable major molecular response (MMR).
At study entry, patients had received imatinib (n=148), nilotinib (n=16), or dasatinib (n=10) for a median duration of 6.8 years.
For the first 12 months of the study, patients had their TKI dose reduced to half the standard dose. So they received imatinib at 200 mg daily, dasatinib at 50 mg daily, or nilotinib at 200 mg twice daily. After that, patients stopped treatment completely.
After the first 12 months, molecular recurrence was lower in patients with stable MR4 at study entry than in patients who were not in MR4 (but still in MMR)—2.4% (3/125) and 18.4% (9/49), respectively (P<0.001).
During the following 12 months, in which patients had completely stopped TKI treatment, there were 26 recurrences and 4 withdrawals among the remaining 117 patients who were in MR4 at baseline, as well as 20 recurrences and 4 withdrawals among the 36 patients not in MR4.
So the RFS was 77% among patients in MR4 at baseline and 39% among the patients not in MR4 (P<0.001).
The researchers said the probability of RFS was unrelated to patients’ age, gender, performance status, or the prior TKI they received (imatinib vs second-generation TKI).
All patients with recurrence ultimately returned to deep remissions when they resumed their TKI treatment.
“TKI de-escalation is safe for most CML patients with stable and excellent responses to TKI therapy after some years of treatment and is associated with improvement in symptoms,” Dr Clark said.
“Overall, our findings are better than any other studies worldwide and imply that our unique, gradual withdrawal of treatment might be important. We don’t yet understand why our results are so good, but this is a happy problem to have.”
Blinatumomab granted full approval to treat rel/ref BCP-ALL
The US Food and Drug Administration (FDA) has approved the supplemental biologics license application (sBLA) for blinatumomab (Blincyto®).
The aim of the sBLA was to expand the indication for blinatumomab to include all patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL) and to convert blinatumomab’s accelerated approval to a full approval.
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed or refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Now, the FDA has granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA also recently approved the sBLA for blinatumomab to be infused over 7 days with preservative, adding to the previously approved administration options for infusion over 24 and 48 hours (preservative-free).
The blinatumomab intravenous bag for a 7-day infusion contains Bacteriostatic 0.9% Sodium Chloride, USP (containing 0.9% benzyl alcohol), which permits continuous intravenous infusion of blinatumomab at 28 mcg/day or 15 mcg/m²/day for a total of 7 days.
The 7-day infusion is not recommended for patients weighing less than 22 kg due to the risk of serious and sometimes fatal adverse events associated with benzyl alcohol in pediatric patients. See the full prescribing information for details.
The prescribing information for blinatumomab includes a boxed warning detailing the risk of cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a Risk Evaluation and Mitigation Strategy program in the US intended to inform healthcare providers about these risks.
Blinatumomab is marketed by Amgen.
Trial results
With this sBLA, Amgen sought to make blinatumomab available as a treatment for patients with Ph+ relapsed/refractory BCP-ALL (as well as Ph-).
To this end, the application included data from the ALCANTARA study, which were published in the Journal of Clinical Oncology.
In this trial, researchers evaluated blinatumomab in adults with Ph+ relapsed/refractory BCP-ALL who had failed treatment with at least 1 tyrosine kinase inhibitor.
Thirty-six percent of patients achieved a complete response or complete response with partial hematologic recovery within the first 2 cycles of blinatumomab treatment. Of these patients, 88% were minimal residual disease-negative.
The most frequent adverse events (AEs) in this trial were pyrexia (58%), neurologic events (47%), febrile neutropenia (40%), and headache (31%). Three patients had grade 1/2 cytokine release syndrome, and 3 patients had grade 3 neurologic AEs.
The sBLA also included overall survival (OS) data from the phase 3 TOWER trial, which was intended to support the conversion of blinatumomab’s accelerated approval to a full approval.
Results from the TOWER trial were published in NEJM.
In this study, researchers compared blinatumomab to standard of care (SOC) chemotherapy (4 different regimens) in adults with Ph- relapsed/refractory BCP-ALL.
Blinatumomab produced higher response rates and nearly doubled OS compared to SOC. The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm. The hazard ratio for death was 0.71 (P=0.012).
The incidence of grade 3 or higher AEs was higher in the SOC arm, but the incidence of serious AEs was higher in the blinatumomab arm.
The US Food and Drug Administration (FDA) has approved the supplemental biologics license application (sBLA) for blinatumomab (Blincyto®).
The aim of the sBLA was to expand the indication for blinatumomab to include all patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL) and to convert blinatumomab’s accelerated approval to a full approval.
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed or refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Now, the FDA has granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA also recently approved the sBLA for blinatumomab to be infused over 7 days with preservative, adding to the previously approved administration options for infusion over 24 and 48 hours (preservative-free).
The blinatumomab intravenous bag for a 7-day infusion contains Bacteriostatic 0.9% Sodium Chloride, USP (containing 0.9% benzyl alcohol), which permits continuous intravenous infusion of blinatumomab at 28 mcg/day or 15 mcg/m²/day for a total of 7 days.
The 7-day infusion is not recommended for patients weighing less than 22 kg due to the risk of serious and sometimes fatal adverse events associated with benzyl alcohol in pediatric patients. See the full prescribing information for details.
The prescribing information for blinatumomab includes a boxed warning detailing the risk of cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a Risk Evaluation and Mitigation Strategy program in the US intended to inform healthcare providers about these risks.
Blinatumomab is marketed by Amgen.
Trial results
With this sBLA, Amgen sought to make blinatumomab available as a treatment for patients with Ph+ relapsed/refractory BCP-ALL (as well as Ph-).
To this end, the application included data from the ALCANTARA study, which were published in the Journal of Clinical Oncology.
In this trial, researchers evaluated blinatumomab in adults with Ph+ relapsed/refractory BCP-ALL who had failed treatment with at least 1 tyrosine kinase inhibitor.
Thirty-six percent of patients achieved a complete response or complete response with partial hematologic recovery within the first 2 cycles of blinatumomab treatment. Of these patients, 88% were minimal residual disease-negative.
The most frequent adverse events (AEs) in this trial were pyrexia (58%), neurologic events (47%), febrile neutropenia (40%), and headache (31%). Three patients had grade 1/2 cytokine release syndrome, and 3 patients had grade 3 neurologic AEs.
The sBLA also included overall survival (OS) data from the phase 3 TOWER trial, which was intended to support the conversion of blinatumomab’s accelerated approval to a full approval.
Results from the TOWER trial were published in NEJM.
In this study, researchers compared blinatumomab to standard of care (SOC) chemotherapy (4 different regimens) in adults with Ph- relapsed/refractory BCP-ALL.
Blinatumomab produced higher response rates and nearly doubled OS compared to SOC. The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm. The hazard ratio for death was 0.71 (P=0.012).
The incidence of grade 3 or higher AEs was higher in the SOC arm, but the incidence of serious AEs was higher in the blinatumomab arm.
The US Food and Drug Administration (FDA) has approved the supplemental biologics license application (sBLA) for blinatumomab (Blincyto®).
The aim of the sBLA was to expand the indication for blinatumomab to include all patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (BCP-ALL) and to convert blinatumomab’s accelerated approval to a full approval.
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed or refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Now, the FDA has granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA also recently approved the sBLA for blinatumomab to be infused over 7 days with preservative, adding to the previously approved administration options for infusion over 24 and 48 hours (preservative-free).
The blinatumomab intravenous bag for a 7-day infusion contains Bacteriostatic 0.9% Sodium Chloride, USP (containing 0.9% benzyl alcohol), which permits continuous intravenous infusion of blinatumomab at 28 mcg/day or 15 mcg/m²/day for a total of 7 days.
The 7-day infusion is not recommended for patients weighing less than 22 kg due to the risk of serious and sometimes fatal adverse events associated with benzyl alcohol in pediatric patients. See the full prescribing information for details.
The prescribing information for blinatumomab includes a boxed warning detailing the risk of cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a Risk Evaluation and Mitigation Strategy program in the US intended to inform healthcare providers about these risks.
Blinatumomab is marketed by Amgen.
Trial results
With this sBLA, Amgen sought to make blinatumomab available as a treatment for patients with Ph+ relapsed/refractory BCP-ALL (as well as Ph-).
To this end, the application included data from the ALCANTARA study, which were published in the Journal of Clinical Oncology.
In this trial, researchers evaluated blinatumomab in adults with Ph+ relapsed/refractory BCP-ALL who had failed treatment with at least 1 tyrosine kinase inhibitor.
Thirty-six percent of patients achieved a complete response or complete response with partial hematologic recovery within the first 2 cycles of blinatumomab treatment. Of these patients, 88% were minimal residual disease-negative.
The most frequent adverse events (AEs) in this trial were pyrexia (58%), neurologic events (47%), febrile neutropenia (40%), and headache (31%). Three patients had grade 1/2 cytokine release syndrome, and 3 patients had grade 3 neurologic AEs.
The sBLA also included overall survival (OS) data from the phase 3 TOWER trial, which was intended to support the conversion of blinatumomab’s accelerated approval to a full approval.
Results from the TOWER trial were published in NEJM.
In this study, researchers compared blinatumomab to standard of care (SOC) chemotherapy (4 different regimens) in adults with Ph- relapsed/refractory BCP-ALL.
Blinatumomab produced higher response rates and nearly doubled OS compared to SOC. The median OS was 7.7 months in the blinatumomab arm and 4 months in the SOC arm. The hazard ratio for death was 0.71 (P=0.012).
The incidence of grade 3 or higher AEs was higher in the SOC arm, but the incidence of serious AEs was higher in the blinatumomab arm.
ODAC recommends approval of CTL019 in rel/ref ALL
The US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) has unanimously recommended approval for the chimeric antigen receptor (CAR) T-cell therapy CTL019 (tisagenlecleucel).
The committee voted 10 to 0 in favor of approving CTL019 for the treatment of pediatric and young adult patients (ages 3 to 25) with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA will consider this vote as it reviews the biologics license application (BLA) for CTL019, but the agency is not obligated to follow the ODAC’s recommendation.
The BLA for CTL019 is supported by results from 3 trials.
This includes a pilot study, which was presented at the 2015 ASH Annual Meeting; the phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting; and the phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
ELIANA enrolled 88 patients with relapsed/refractory B-cell ALL, and 68 of them received CTL019.
Nine patients did not receive CTL019 due to death or adverse events, 7 patients were affected by manufacturing failures, and 4 patients were pending infusion at last follow-up.
Most of the infused patients (n=65) received lymphodepleting chemotherapy prior to CTL019 (single dose). The median dose was 3.0 × 106 (range, 0.2-5.4 × 106) transduced CTL019 cells/kg.
Sixty-three patients were evaluable for efficacy.
The overall response rate—complete response (CR) plus CR with incomplete hematologic recovery (CRi)—was 83% (52/63). All patients with CR/CRis were minimal residual disease-negative in the bone marrow.
Sixty-eight patients were evaluated for safety.
Serious adverse events occurred in 69% of patients. These included life-threatening cytokine release syndrome (CRS) and hemophagocytic lymphohistiocytosis, neurological events that occurred with CRS or after CRS was resolved, coagulopathies with CRS, and life-threatening infections.
Seventy-eight percent of patients had CRS—21% with grade 3 and 27% with grade 4 CRS. There were no deaths from CRS.
Forty-four percent of patients had neurological toxicities—15% grade 3 or higher. These included encephalopathy, delirium, hallucinations, somnolence, cognitive disorder, seizure, depressed level of consciousness, mental status changes, dysphagia, muscular weakness, and dysarthria.
Severe infectious complications occurred in 26% of patients, and 3 patients died of such complications.
Eleven patients died after receiving CTL019—7 due to ALL, 1 from cerebral hemorrhage, 1 from encephalitis, 1 from a respiratory tract infection, and 1 from systemic mycosis.
The US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) has unanimously recommended approval for the chimeric antigen receptor (CAR) T-cell therapy CTL019 (tisagenlecleucel).
The committee voted 10 to 0 in favor of approving CTL019 for the treatment of pediatric and young adult patients (ages 3 to 25) with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA will consider this vote as it reviews the biologics license application (BLA) for CTL019, but the agency is not obligated to follow the ODAC’s recommendation.
The BLA for CTL019 is supported by results from 3 trials.
This includes a pilot study, which was presented at the 2015 ASH Annual Meeting; the phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting; and the phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
ELIANA enrolled 88 patients with relapsed/refractory B-cell ALL, and 68 of them received CTL019.
Nine patients did not receive CTL019 due to death or adverse events, 7 patients were affected by manufacturing failures, and 4 patients were pending infusion at last follow-up.
Most of the infused patients (n=65) received lymphodepleting chemotherapy prior to CTL019 (single dose). The median dose was 3.0 × 106 (range, 0.2-5.4 × 106) transduced CTL019 cells/kg.
Sixty-three patients were evaluable for efficacy.
The overall response rate—complete response (CR) plus CR with incomplete hematologic recovery (CRi)—was 83% (52/63). All patients with CR/CRis were minimal residual disease-negative in the bone marrow.
Sixty-eight patients were evaluated for safety.
Serious adverse events occurred in 69% of patients. These included life-threatening cytokine release syndrome (CRS) and hemophagocytic lymphohistiocytosis, neurological events that occurred with CRS or after CRS was resolved, coagulopathies with CRS, and life-threatening infections.
Seventy-eight percent of patients had CRS—21% with grade 3 and 27% with grade 4 CRS. There were no deaths from CRS.
Forty-four percent of patients had neurological toxicities—15% grade 3 or higher. These included encephalopathy, delirium, hallucinations, somnolence, cognitive disorder, seizure, depressed level of consciousness, mental status changes, dysphagia, muscular weakness, and dysarthria.
Severe infectious complications occurred in 26% of patients, and 3 patients died of such complications.
Eleven patients died after receiving CTL019—7 due to ALL, 1 from cerebral hemorrhage, 1 from encephalitis, 1 from a respiratory tract infection, and 1 from systemic mycosis.
The US Food and Drug Administration’s (FDA) Oncologic Drugs Advisory Committee (ODAC) has unanimously recommended approval for the chimeric antigen receptor (CAR) T-cell therapy CTL019 (tisagenlecleucel).
The committee voted 10 to 0 in favor of approving CTL019 for the treatment of pediatric and young adult patients (ages 3 to 25) with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL).
The FDA will consider this vote as it reviews the biologics license application (BLA) for CTL019, but the agency is not obligated to follow the ODAC’s recommendation.
The BLA for CTL019 is supported by results from 3 trials.
This includes a pilot study, which was presented at the 2015 ASH Annual Meeting; the phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting; and the phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
ELIANA enrolled 88 patients with relapsed/refractory B-cell ALL, and 68 of them received CTL019.
Nine patients did not receive CTL019 due to death or adverse events, 7 patients were affected by manufacturing failures, and 4 patients were pending infusion at last follow-up.
Most of the infused patients (n=65) received lymphodepleting chemotherapy prior to CTL019 (single dose). The median dose was 3.0 × 106 (range, 0.2-5.4 × 106) transduced CTL019 cells/kg.
Sixty-three patients were evaluable for efficacy.
The overall response rate—complete response (CR) plus CR with incomplete hematologic recovery (CRi)—was 83% (52/63). All patients with CR/CRis were minimal residual disease-negative in the bone marrow.
Sixty-eight patients were evaluated for safety.
Serious adverse events occurred in 69% of patients. These included life-threatening cytokine release syndrome (CRS) and hemophagocytic lymphohistiocytosis, neurological events that occurred with CRS or after CRS was resolved, coagulopathies with CRS, and life-threatening infections.
Seventy-eight percent of patients had CRS—21% with grade 3 and 27% with grade 4 CRS. There were no deaths from CRS.
Forty-four percent of patients had neurological toxicities—15% grade 3 or higher. These included encephalopathy, delirium, hallucinations, somnolence, cognitive disorder, seizure, depressed level of consciousness, mental status changes, dysphagia, muscular weakness, and dysarthria.
Severe infectious complications occurred in 26% of patients, and 3 patients died of such complications.
Eleven patients died after receiving CTL019—7 due to ALL, 1 from cerebral hemorrhage, 1 from encephalitis, 1 from a respiratory tract infection, and 1 from systemic mycosis.