User login
CAR T cells elicit durable, potent responses in kids with EM relapse of ALL
CHICAGO—Outcomes for pediatric patients with relapsed acute lymphoblastic leukemia (ALL) are dismal, with the probability of event-free survival ranging from 15% to 70% after a first relapse to 15% to 20% after a second relapse.
“So novel therapies are obviously urgently needed,” Mala Kiran Talekar, MD, of the Children's Hospital of Philadelphia in Pennsylvania, affirmed. “And herein comes the role of CAR T cells as a breakthrough therapy for relapsed/refractory pediatric ALL.”
She presented the outcome of chimeric antigen receptor (CAR) T-cell therapy in pediatric patients with non-CNS extramedullary (EM) relapse at the ASCO 2017 Annual meeting as abstract 10507.
The investigators had drawn the patient population for this analysis from 2 CAR studies, CTL019 and CTL119.
CTL019, which had already been completed, employed a murine CAR, and CTL119 is ongoing and uses a humanized CAR.
Of the 60 patients enrolled in CTL019, 56 (93%) achieved a complete response (CR) at day 28, and 100% had a CNS remission. Their 12-month overall survival (OS) was 79%.
“[K]eep in mind, when the study first started,” Dr Talekar said, “the patient population that had been referred to us was patients who had suffered a second or greater relapse or had been refractory to forms of treatment available to them, and the majority had been refractory to multiple therapies.”
The humanized CAR study, CTL119, is divided into 2 cohorts—one with CAR-naïve patients (n=22) and the other a CAR-retreatment arm (n=15) with patients who had received previous CAR therapy and relapsed.
Dr Talekar explained that the humanized CAR was made with the intention of decreasing rejection or loss of persistence of the T cells related to murine antigenicity.
Nine patients (60%) in the CAR-retreatment arm achieved a CR at day 28, and at 6 months, 78% experienced relapse-free survival (RFS) with a median follow-up of 12 months.
All of the CAR-naïve patients achieved CR at day 28, with 86% achieving RFS at 6 months, with a median follow-up of 10 months.
ALL with EM involvement
The investigators identified 10 pediatric patients treated in the murine (n=6) or humanized (n=4) trials who had received CAR therapy for isolated extramedullary disease or for combined bone marrow extramedullary (BM/EM) relapse of ALL.
They defined EM relapse as involvement of a non-CNS site confirmed by imaging with or without pathology within 12 months of CAR T-cell infusion. After infusion, patients had diagnostic imaging performed at 1, 3, 6, 9, and 12 months.
Of the 10 patients, 5 had active EM involvement at the time of infusion, 2 had isolated EM relapse—1 with parotid and multifocal bony lesions and 1 with testis and sinus lesions—and 5 had multiple sites of EM relapse.
The patients had 2 to 4 prior ALL relapses, 2 had prior local radiation to the EM site, and all 10 had received prior bone marrow transplants.
Three patients had an MLL rearrangement, 1 had hypodiploid ALL, and 1 had trisomy 21.
Nine of the 10 patients achieved MRD-negative CR at day 28.
One patient was not evaluable because his disease progressed within 2 weeks of CAR therapy in both the bone marrow and EM site. He died 6 weeks after the infusion.
Five patients evaluated by serial imaging had objective responses. Two had no evidence of EM disease by day 28, 2 had resolution by 3 months, and 1 had continued decrease in the size of her uterine mass at 3 and 6 months. She underwent hysterectomy at 8 months with no evidence of disease on pathology.
Four patients with a prior history of skin or testicular involvement had no evidence of disease by exam at day 28.
Three of the 9 patients relapsed with CD19+ disease. One had skin/medullary involvement and died at 38 months after CAR T-cell infusion. And 2 had medullary disease: 1 died at 17 months and 1 is alive at 28 months.
The remaining 6 patients are alive and well at a median follow-up of 10 months (range, 3 – 16 months) without recurrence of disease.
The investigators therefore concluded that single agent CAR T-cell immunotherapy can induce potent and durable response in patients with EM relapse of their ALL. ![]()
CHICAGO—Outcomes for pediatric patients with relapsed acute lymphoblastic leukemia (ALL) are dismal, with the probability of event-free survival ranging from 15% to 70% after a first relapse to 15% to 20% after a second relapse.
“So novel therapies are obviously urgently needed,” Mala Kiran Talekar, MD, of the Children's Hospital of Philadelphia in Pennsylvania, affirmed. “And herein comes the role of CAR T cells as a breakthrough therapy for relapsed/refractory pediatric ALL.”
She presented the outcome of chimeric antigen receptor (CAR) T-cell therapy in pediatric patients with non-CNS extramedullary (EM) relapse at the ASCO 2017 Annual meeting as abstract 10507.
The investigators had drawn the patient population for this analysis from 2 CAR studies, CTL019 and CTL119.
CTL019, which had already been completed, employed a murine CAR, and CTL119 is ongoing and uses a humanized CAR.
Of the 60 patients enrolled in CTL019, 56 (93%) achieved a complete response (CR) at day 28, and 100% had a CNS remission. Their 12-month overall survival (OS) was 79%.
“[K]eep in mind, when the study first started,” Dr Talekar said, “the patient population that had been referred to us was patients who had suffered a second or greater relapse or had been refractory to forms of treatment available to them, and the majority had been refractory to multiple therapies.”
The humanized CAR study, CTL119, is divided into 2 cohorts—one with CAR-naïve patients (n=22) and the other a CAR-retreatment arm (n=15) with patients who had received previous CAR therapy and relapsed.
Dr Talekar explained that the humanized CAR was made with the intention of decreasing rejection or loss of persistence of the T cells related to murine antigenicity.
Nine patients (60%) in the CAR-retreatment arm achieved a CR at day 28, and at 6 months, 78% experienced relapse-free survival (RFS) with a median follow-up of 12 months.
All of the CAR-naïve patients achieved CR at day 28, with 86% achieving RFS at 6 months, with a median follow-up of 10 months.
ALL with EM involvement
The investigators identified 10 pediatric patients treated in the murine (n=6) or humanized (n=4) trials who had received CAR therapy for isolated extramedullary disease or for combined bone marrow extramedullary (BM/EM) relapse of ALL.
They defined EM relapse as involvement of a non-CNS site confirmed by imaging with or without pathology within 12 months of CAR T-cell infusion. After infusion, patients had diagnostic imaging performed at 1, 3, 6, 9, and 12 months.
Of the 10 patients, 5 had active EM involvement at the time of infusion, 2 had isolated EM relapse—1 with parotid and multifocal bony lesions and 1 with testis and sinus lesions—and 5 had multiple sites of EM relapse.
The patients had 2 to 4 prior ALL relapses, 2 had prior local radiation to the EM site, and all 10 had received prior bone marrow transplants.
Three patients had an MLL rearrangement, 1 had hypodiploid ALL, and 1 had trisomy 21.
Nine of the 10 patients achieved MRD-negative CR at day 28.
One patient was not evaluable because his disease progressed within 2 weeks of CAR therapy in both the bone marrow and EM site. He died 6 weeks after the infusion.
Five patients evaluated by serial imaging had objective responses. Two had no evidence of EM disease by day 28, 2 had resolution by 3 months, and 1 had continued decrease in the size of her uterine mass at 3 and 6 months. She underwent hysterectomy at 8 months with no evidence of disease on pathology.
Four patients with a prior history of skin or testicular involvement had no evidence of disease by exam at day 28.
Three of the 9 patients relapsed with CD19+ disease. One had skin/medullary involvement and died at 38 months after CAR T-cell infusion. And 2 had medullary disease: 1 died at 17 months and 1 is alive at 28 months.
The remaining 6 patients are alive and well at a median follow-up of 10 months (range, 3 – 16 months) without recurrence of disease.
The investigators therefore concluded that single agent CAR T-cell immunotherapy can induce potent and durable response in patients with EM relapse of their ALL. ![]()
CHICAGO—Outcomes for pediatric patients with relapsed acute lymphoblastic leukemia (ALL) are dismal, with the probability of event-free survival ranging from 15% to 70% after a first relapse to 15% to 20% after a second relapse.
“So novel therapies are obviously urgently needed,” Mala Kiran Talekar, MD, of the Children's Hospital of Philadelphia in Pennsylvania, affirmed. “And herein comes the role of CAR T cells as a breakthrough therapy for relapsed/refractory pediatric ALL.”
She presented the outcome of chimeric antigen receptor (CAR) T-cell therapy in pediatric patients with non-CNS extramedullary (EM) relapse at the ASCO 2017 Annual meeting as abstract 10507.
The investigators had drawn the patient population for this analysis from 2 CAR studies, CTL019 and CTL119.
CTL019, which had already been completed, employed a murine CAR, and CTL119 is ongoing and uses a humanized CAR.
Of the 60 patients enrolled in CTL019, 56 (93%) achieved a complete response (CR) at day 28, and 100% had a CNS remission. Their 12-month overall survival (OS) was 79%.
“[K]eep in mind, when the study first started,” Dr Talekar said, “the patient population that had been referred to us was patients who had suffered a second or greater relapse or had been refractory to forms of treatment available to them, and the majority had been refractory to multiple therapies.”
The humanized CAR study, CTL119, is divided into 2 cohorts—one with CAR-naïve patients (n=22) and the other a CAR-retreatment arm (n=15) with patients who had received previous CAR therapy and relapsed.
Dr Talekar explained that the humanized CAR was made with the intention of decreasing rejection or loss of persistence of the T cells related to murine antigenicity.
Nine patients (60%) in the CAR-retreatment arm achieved a CR at day 28, and at 6 months, 78% experienced relapse-free survival (RFS) with a median follow-up of 12 months.
All of the CAR-naïve patients achieved CR at day 28, with 86% achieving RFS at 6 months, with a median follow-up of 10 months.
ALL with EM involvement
The investigators identified 10 pediatric patients treated in the murine (n=6) or humanized (n=4) trials who had received CAR therapy for isolated extramedullary disease or for combined bone marrow extramedullary (BM/EM) relapse of ALL.
They defined EM relapse as involvement of a non-CNS site confirmed by imaging with or without pathology within 12 months of CAR T-cell infusion. After infusion, patients had diagnostic imaging performed at 1, 3, 6, 9, and 12 months.
Of the 10 patients, 5 had active EM involvement at the time of infusion, 2 had isolated EM relapse—1 with parotid and multifocal bony lesions and 1 with testis and sinus lesions—and 5 had multiple sites of EM relapse.
The patients had 2 to 4 prior ALL relapses, 2 had prior local radiation to the EM site, and all 10 had received prior bone marrow transplants.
Three patients had an MLL rearrangement, 1 had hypodiploid ALL, and 1 had trisomy 21.
Nine of the 10 patients achieved MRD-negative CR at day 28.
One patient was not evaluable because his disease progressed within 2 weeks of CAR therapy in both the bone marrow and EM site. He died 6 weeks after the infusion.
Five patients evaluated by serial imaging had objective responses. Two had no evidence of EM disease by day 28, 2 had resolution by 3 months, and 1 had continued decrease in the size of her uterine mass at 3 and 6 months. She underwent hysterectomy at 8 months with no evidence of disease on pathology.
Four patients with a prior history of skin or testicular involvement had no evidence of disease by exam at day 28.
Three of the 9 patients relapsed with CD19+ disease. One had skin/medullary involvement and died at 38 months after CAR T-cell infusion. And 2 had medullary disease: 1 died at 17 months and 1 is alive at 28 months.
The remaining 6 patients are alive and well at a median follow-up of 10 months (range, 3 – 16 months) without recurrence of disease.
The investigators therefore concluded that single agent CAR T-cell immunotherapy can induce potent and durable response in patients with EM relapse of their ALL. ![]()
Azacitidine alone comparable to AZA combos for most MDS patients
A 3-arm phase 2 study of azacitidine alone or in combination with lenalidomide or vorinostat in patients with higher-risk myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) has shown the combination therapies to have similar overall response rates (ORR) to azacitidine monotherapy. Based on these findings, investigators did not choose either combination arm for phase 3 testing of overall survival.
However, patients with CMML treated with the azacitidine-lenalidomide combination had twice the ORR compared with azacitidine monotherapy, they reported.
And patients with certain mutations, such as DNMT3A, BCOR, and NRAS, had higher overall response rates, although only those with the DNMT3A mutation were significant.
Mikkael A. Sekeres, MD, of the Cleveland Clinic in Cleveland, Ohio, and colleagues reported these findings in the Journal of Clinical Oncology on behalf of the North American Intergroup Study SWOG S117.
Doses of azacitidine were the same for monotherapy and combination arms: 75 mg/m2/day intravenously or subcutaneously on days 1 to 7 of a 28-day cycle.
Patients in the lenalidomide arm received 10 mg/day orally of that drug on days 1 to 21, and patients in the vorinostat arm received 300 mg twice daily orally on days 3 to 9.
Patient characteristics
Patients had MDS of IPSS Intermediate-2 or higher or bone marrow blasts 5% or greater. Patients with CMML had fewer than 20% blasts.
The investigators randomized 277 patients to receive either azacitidine alone (n=92), azacitidine plus lenalidomide (n=93), or azacitidine plus vorinostat (n=92).
Patients were a median age of 70 years (range, 28 to 93). Eighty-five patients (31%) were female, 53 (19%) had CMML, and 18 (6%) had treatment-related MDS. More than half the patients were transfusion-dependent at baseline.
Baseline characteristics were similar across the 3 arms. The investigators noted that the baseline characteristics were also similar across the 90 centers participating in the study, whether they were an MDS Center of Excellence or a high-volume center.
Adverse events
For the most part, therapy-related adverse events were similar across the arms.
Rates of grade 3 or higher febrile neutropenia and infection and infestations were similar for all 3 cohorts: 89% for azaciditine monotherapy, 91% for the lenalidomide combination, and 91% for the vorinostat combination.
However, the vorinostat arm had more grade 3 or higher gastrointestinal toxicities (14 patients, 15%) compared with the monotherapy arm (4 patients, 4%), P=0.02.
And patients receiving lenalidomide experienced more grade 3 or higher rash (14 patients, 16%) compared with patients receiving monotherapy (3 patients, 3%), P=0.005.
Patients in the combination arms stopped therapy at significantly higher rates than the monotherapy arm. Eight percent of patients receiving monotherapy stopped treatment compared with 20% in the lenalidomide arm and 21% in the vorinostat arm.
Patients in the combination arms also had more dose modifications not specified in the protocol than those in the monotherapy arm. Twenty-four percent receiving azacitidine monotherapy had non-protocol defined dose modifications, compared with 43% in the lenalidomide arm and 42% in the vorinostat arm.
Responses
The ORR for the entire study population was 38%.
Patients in the monotherapy arm had an ORR of 38%, those in the lenalidomide arm, 49%, and those in the vorinostate arm, 27%. Neither arm achieved significance compared with the monotherapy arm.
Patients who were treatment-naïve in the lenalidomide arm had a somewhat improved ORR compared with monotherapy, P=0.08.
The median duration of response for all cohorts was 15 months: 10 months for monotherapy, 14 months for lenalidomide, and 18 months for vorinostat.
Patients who were able to remain on therapy for 6 months or more in the lenalidomide arm achieved a higher ORR of 87% compared with monotherapy (62%, P=0.01). However, there was no difference in response duration with longer therapy.
The median overall survival (OS) was 17 months for all patients, 15 months for patients in the monotherapy group, 19 months for those in the lenalidomide arm, and 17 months for those in the vorinostat group.
CMML patients had similar OS across treatment arms, with the median not yet reached for patients in the monotherapy arm.
Subgroup responses
Patients with CMML in the lenalidomide arm had a significantly higher ORR than CMML patients in the monotherapy arm, 68% and 28%, respectively (P=0.02).
Median duration of response for CMML patients was 19 months, with no differences between the arms.
The investigators observed no differences in ORR for therapy-related MDS, IPSS subgroups, transfusion-dependent patients, or allogeneic transplant rates.
However, they noted ORR was better for patients with chromosome 5 abnormality regardless of treatment arm than for those without the abnormality (odds ratio, 2.17, P=0.008).
One hundred thirteen patients had mutational data available. They had a median number of 2 mutations (range, 0 to 7), with the most common being ASXL1 (n = 31), TET2 (n = 26), SRSF2 (n = 23), TP53 (n = 22), RUNX1 (n = 21), and U2AF1 (n = 19).
Patients with DNMT3A mutation had a significantly higher ORR than for patients without mutations, 67% and 34%, respectively P=0.025).
Patients with BCOR and NRAS mutations had numerically higher, but non-significant, ORR than non-mutated patients. Patients with BCOR mutation had a 57% ORR compared with 34% for non-mutated patients (P=0.23). Patients with NRAS mutation had a 60% ORR compared with 36% for non-mutated patients (P=0.28).
Patients with mutations in TET2 (P = .046) and TP53 (P = .003) had a worse response duration than those without mutations.
Response duration was significantly better with fewer mutations. For 2 or more mutations, the hazard ration was 6.86 versus no mutations (P=0.01).
The investigators believed under-dosing may have compromised response and survival in the combination arms. They suggested that studies focused on the subgroups that seemed to benefit from the combinations should be conducted. ![]()
A 3-arm phase 2 study of azacitidine alone or in combination with lenalidomide or vorinostat in patients with higher-risk myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) has shown the combination therapies to have similar overall response rates (ORR) to azacitidine monotherapy. Based on these findings, investigators did not choose either combination arm for phase 3 testing of overall survival.
However, patients with CMML treated with the azacitidine-lenalidomide combination had twice the ORR compared with azacitidine monotherapy, they reported.
And patients with certain mutations, such as DNMT3A, BCOR, and NRAS, had higher overall response rates, although only those with the DNMT3A mutation were significant.
Mikkael A. Sekeres, MD, of the Cleveland Clinic in Cleveland, Ohio, and colleagues reported these findings in the Journal of Clinical Oncology on behalf of the North American Intergroup Study SWOG S117.
Doses of azacitidine were the same for monotherapy and combination arms: 75 mg/m2/day intravenously or subcutaneously on days 1 to 7 of a 28-day cycle.
Patients in the lenalidomide arm received 10 mg/day orally of that drug on days 1 to 21, and patients in the vorinostat arm received 300 mg twice daily orally on days 3 to 9.
Patient characteristics
Patients had MDS of IPSS Intermediate-2 or higher or bone marrow blasts 5% or greater. Patients with CMML had fewer than 20% blasts.
The investigators randomized 277 patients to receive either azacitidine alone (n=92), azacitidine plus lenalidomide (n=93), or azacitidine plus vorinostat (n=92).
Patients were a median age of 70 years (range, 28 to 93). Eighty-five patients (31%) were female, 53 (19%) had CMML, and 18 (6%) had treatment-related MDS. More than half the patients were transfusion-dependent at baseline.
Baseline characteristics were similar across the 3 arms. The investigators noted that the baseline characteristics were also similar across the 90 centers participating in the study, whether they were an MDS Center of Excellence or a high-volume center.
Adverse events
For the most part, therapy-related adverse events were similar across the arms.
Rates of grade 3 or higher febrile neutropenia and infection and infestations were similar for all 3 cohorts: 89% for azaciditine monotherapy, 91% for the lenalidomide combination, and 91% for the vorinostat combination.
However, the vorinostat arm had more grade 3 or higher gastrointestinal toxicities (14 patients, 15%) compared with the monotherapy arm (4 patients, 4%), P=0.02.
And patients receiving lenalidomide experienced more grade 3 or higher rash (14 patients, 16%) compared with patients receiving monotherapy (3 patients, 3%), P=0.005.
Patients in the combination arms stopped therapy at significantly higher rates than the monotherapy arm. Eight percent of patients receiving monotherapy stopped treatment compared with 20% in the lenalidomide arm and 21% in the vorinostat arm.
Patients in the combination arms also had more dose modifications not specified in the protocol than those in the monotherapy arm. Twenty-four percent receiving azacitidine monotherapy had non-protocol defined dose modifications, compared with 43% in the lenalidomide arm and 42% in the vorinostat arm.
Responses
The ORR for the entire study population was 38%.
Patients in the monotherapy arm had an ORR of 38%, those in the lenalidomide arm, 49%, and those in the vorinostate arm, 27%. Neither arm achieved significance compared with the monotherapy arm.
Patients who were treatment-naïve in the lenalidomide arm had a somewhat improved ORR compared with monotherapy, P=0.08.
The median duration of response for all cohorts was 15 months: 10 months for monotherapy, 14 months for lenalidomide, and 18 months for vorinostat.
Patients who were able to remain on therapy for 6 months or more in the lenalidomide arm achieved a higher ORR of 87% compared with monotherapy (62%, P=0.01). However, there was no difference in response duration with longer therapy.
The median overall survival (OS) was 17 months for all patients, 15 months for patients in the monotherapy group, 19 months for those in the lenalidomide arm, and 17 months for those in the vorinostat group.
CMML patients had similar OS across treatment arms, with the median not yet reached for patients in the monotherapy arm.
Subgroup responses
Patients with CMML in the lenalidomide arm had a significantly higher ORR than CMML patients in the monotherapy arm, 68% and 28%, respectively (P=0.02).
Median duration of response for CMML patients was 19 months, with no differences between the arms.
The investigators observed no differences in ORR for therapy-related MDS, IPSS subgroups, transfusion-dependent patients, or allogeneic transplant rates.
However, they noted ORR was better for patients with chromosome 5 abnormality regardless of treatment arm than for those without the abnormality (odds ratio, 2.17, P=0.008).
One hundred thirteen patients had mutational data available. They had a median number of 2 mutations (range, 0 to 7), with the most common being ASXL1 (n = 31), TET2 (n = 26), SRSF2 (n = 23), TP53 (n = 22), RUNX1 (n = 21), and U2AF1 (n = 19).
Patients with DNMT3A mutation had a significantly higher ORR than for patients without mutations, 67% and 34%, respectively P=0.025).
Patients with BCOR and NRAS mutations had numerically higher, but non-significant, ORR than non-mutated patients. Patients with BCOR mutation had a 57% ORR compared with 34% for non-mutated patients (P=0.23). Patients with NRAS mutation had a 60% ORR compared with 36% for non-mutated patients (P=0.28).
Patients with mutations in TET2 (P = .046) and TP53 (P = .003) had a worse response duration than those without mutations.
Response duration was significantly better with fewer mutations. For 2 or more mutations, the hazard ration was 6.86 versus no mutations (P=0.01).
The investigators believed under-dosing may have compromised response and survival in the combination arms. They suggested that studies focused on the subgroups that seemed to benefit from the combinations should be conducted. ![]()
A 3-arm phase 2 study of azacitidine alone or in combination with lenalidomide or vorinostat in patients with higher-risk myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) has shown the combination therapies to have similar overall response rates (ORR) to azacitidine monotherapy. Based on these findings, investigators did not choose either combination arm for phase 3 testing of overall survival.
However, patients with CMML treated with the azacitidine-lenalidomide combination had twice the ORR compared with azacitidine monotherapy, they reported.
And patients with certain mutations, such as DNMT3A, BCOR, and NRAS, had higher overall response rates, although only those with the DNMT3A mutation were significant.
Mikkael A. Sekeres, MD, of the Cleveland Clinic in Cleveland, Ohio, and colleagues reported these findings in the Journal of Clinical Oncology on behalf of the North American Intergroup Study SWOG S117.
Doses of azacitidine were the same for monotherapy and combination arms: 75 mg/m2/day intravenously or subcutaneously on days 1 to 7 of a 28-day cycle.
Patients in the lenalidomide arm received 10 mg/day orally of that drug on days 1 to 21, and patients in the vorinostat arm received 300 mg twice daily orally on days 3 to 9.
Patient characteristics
Patients had MDS of IPSS Intermediate-2 or higher or bone marrow blasts 5% or greater. Patients with CMML had fewer than 20% blasts.
The investigators randomized 277 patients to receive either azacitidine alone (n=92), azacitidine plus lenalidomide (n=93), or azacitidine plus vorinostat (n=92).
Patients were a median age of 70 years (range, 28 to 93). Eighty-five patients (31%) were female, 53 (19%) had CMML, and 18 (6%) had treatment-related MDS. More than half the patients were transfusion-dependent at baseline.
Baseline characteristics were similar across the 3 arms. The investigators noted that the baseline characteristics were also similar across the 90 centers participating in the study, whether they were an MDS Center of Excellence or a high-volume center.
Adverse events
For the most part, therapy-related adverse events were similar across the arms.
Rates of grade 3 or higher febrile neutropenia and infection and infestations were similar for all 3 cohorts: 89% for azaciditine monotherapy, 91% for the lenalidomide combination, and 91% for the vorinostat combination.
However, the vorinostat arm had more grade 3 or higher gastrointestinal toxicities (14 patients, 15%) compared with the monotherapy arm (4 patients, 4%), P=0.02.
And patients receiving lenalidomide experienced more grade 3 or higher rash (14 patients, 16%) compared with patients receiving monotherapy (3 patients, 3%), P=0.005.
Patients in the combination arms stopped therapy at significantly higher rates than the monotherapy arm. Eight percent of patients receiving monotherapy stopped treatment compared with 20% in the lenalidomide arm and 21% in the vorinostat arm.
Patients in the combination arms also had more dose modifications not specified in the protocol than those in the monotherapy arm. Twenty-four percent receiving azacitidine monotherapy had non-protocol defined dose modifications, compared with 43% in the lenalidomide arm and 42% in the vorinostat arm.
Responses
The ORR for the entire study population was 38%.
Patients in the monotherapy arm had an ORR of 38%, those in the lenalidomide arm, 49%, and those in the vorinostate arm, 27%. Neither arm achieved significance compared with the monotherapy arm.
Patients who were treatment-naïve in the lenalidomide arm had a somewhat improved ORR compared with monotherapy, P=0.08.
The median duration of response for all cohorts was 15 months: 10 months for monotherapy, 14 months for lenalidomide, and 18 months for vorinostat.
Patients who were able to remain on therapy for 6 months or more in the lenalidomide arm achieved a higher ORR of 87% compared with monotherapy (62%, P=0.01). However, there was no difference in response duration with longer therapy.
The median overall survival (OS) was 17 months for all patients, 15 months for patients in the monotherapy group, 19 months for those in the lenalidomide arm, and 17 months for those in the vorinostat group.
CMML patients had similar OS across treatment arms, with the median not yet reached for patients in the monotherapy arm.
Subgroup responses
Patients with CMML in the lenalidomide arm had a significantly higher ORR than CMML patients in the monotherapy arm, 68% and 28%, respectively (P=0.02).
Median duration of response for CMML patients was 19 months, with no differences between the arms.
The investigators observed no differences in ORR for therapy-related MDS, IPSS subgroups, transfusion-dependent patients, or allogeneic transplant rates.
However, they noted ORR was better for patients with chromosome 5 abnormality regardless of treatment arm than for those without the abnormality (odds ratio, 2.17, P=0.008).
One hundred thirteen patients had mutational data available. They had a median number of 2 mutations (range, 0 to 7), with the most common being ASXL1 (n = 31), TET2 (n = 26), SRSF2 (n = 23), TP53 (n = 22), RUNX1 (n = 21), and U2AF1 (n = 19).
Patients with DNMT3A mutation had a significantly higher ORR than for patients without mutations, 67% and 34%, respectively P=0.025).
Patients with BCOR and NRAS mutations had numerically higher, but non-significant, ORR than non-mutated patients. Patients with BCOR mutation had a 57% ORR compared with 34% for non-mutated patients (P=0.23). Patients with NRAS mutation had a 60% ORR compared with 36% for non-mutated patients (P=0.28).
Patients with mutations in TET2 (P = .046) and TP53 (P = .003) had a worse response duration than those without mutations.
Response duration was significantly better with fewer mutations. For 2 or more mutations, the hazard ration was 6.86 versus no mutations (P=0.01).
The investigators believed under-dosing may have compromised response and survival in the combination arms. They suggested that studies focused on the subgroups that seemed to benefit from the combinations should be conducted. ![]()
Severe health conditions decrease among childhood cancer survivors
CHICAGO—The 15-year cumulative incidence of severe health conditions for survivors of childhood cancer has decreased over the past 30 years, from 12.7% for those diagnosed in the 1970s to 10.1% and 8.9% for those diagnosed in the 1980s and 1990s, respectively. And the decreases were greatest for patients with Wilms’ tumor and Hodgkin lymphoma (HL), followed by patients with astrocytoma, non-Hodgkin lymphoma (NHL), and acute lymphoblastic leukemia (ALL).
Investigators of the Childhood Cancer Survivor Study (CCSS) undertook a retrospective cohort analysis of children aged 0 – 14 years diagnosed with cancer between 1970 and 1999. Their goal was to determine whether cancer therapy modifications have maintained cure rates while decreasing the risk of late effects of therapy.
Todd M. Gibson, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, presented the findings at the 2017 annual meeting of the American Society for Clinical Oncology (ASCO) as abstract LBA10500.
Researchers analyzed data from 23,600 childhood cancer survivors in the CCSS who were alive 5 years after diagnosis. The patients had leukemia, lymphoma, CNS malignancies, Wilms tumor, neuroblastoma, or soft-tissue/bone sarcoma.
Dr Gibson noted that while 83% of children with a malignancy achieve a 5-year survival, more than half develop at least one severe, disabling, life-threatening health condition by age 50.
The survivors were a median age at last follow-up of 28 years (range, 5-63) and the median time since diagnosis was 21 years (range, 5-43).
The investigators found significant decreases in severe health conditions in 6 diagnostic groups:
- Wilms tumor, decreased from 13% to 5% (P<0.0001)
- HL, decreased from 18% to 11% (P<0.0001)
- Astrocytoma, decreased from 15% to 9% (P=0.004)
- NHL, decreased from 10% to 6% (P=0.04)
- ALL, decreased from 9% to 7% (P=0.002)
- Ewings sarcoma, decreased from 19% to 10% (P=0.01)
They found no reductions in subsequent severe health conditions among survivors of neuroblastoma, acute myeloid leukemia (AML), soft tissue sarcoma, or osteosarcoma.
The investigators believe the decreases were driven mainly by a reduced incidence of endocrine conditions, subsequent malignant neoplasms, gastrointestinal and neurological conditions, but not cardiac or pulmonary conditions.
They also analyzed the reduction in treatment intensities by decade for different diseases and found they correlated with the reduced incidence of serious chronic health conditions by 15 years after diagnosis.
The National Institutes of Health funded the study.
CHICAGO—The 15-year cumulative incidence of severe health conditions for survivors of childhood cancer has decreased over the past 30 years, from 12.7% for those diagnosed in the 1970s to 10.1% and 8.9% for those diagnosed in the 1980s and 1990s, respectively. And the decreases were greatest for patients with Wilms’ tumor and Hodgkin lymphoma (HL), followed by patients with astrocytoma, non-Hodgkin lymphoma (NHL), and acute lymphoblastic leukemia (ALL).
Investigators of the Childhood Cancer Survivor Study (CCSS) undertook a retrospective cohort analysis of children aged 0 – 14 years diagnosed with cancer between 1970 and 1999. Their goal was to determine whether cancer therapy modifications have maintained cure rates while decreasing the risk of late effects of therapy.
Todd M. Gibson, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, presented the findings at the 2017 annual meeting of the American Society for Clinical Oncology (ASCO) as abstract LBA10500.
Researchers analyzed data from 23,600 childhood cancer survivors in the CCSS who were alive 5 years after diagnosis. The patients had leukemia, lymphoma, CNS malignancies, Wilms tumor, neuroblastoma, or soft-tissue/bone sarcoma.
Dr Gibson noted that while 83% of children with a malignancy achieve a 5-year survival, more than half develop at least one severe, disabling, life-threatening health condition by age 50.
The survivors were a median age at last follow-up of 28 years (range, 5-63) and the median time since diagnosis was 21 years (range, 5-43).
The investigators found significant decreases in severe health conditions in 6 diagnostic groups:
- Wilms tumor, decreased from 13% to 5% (P<0.0001)
- HL, decreased from 18% to 11% (P<0.0001)
- Astrocytoma, decreased from 15% to 9% (P=0.004)
- NHL, decreased from 10% to 6% (P=0.04)
- ALL, decreased from 9% to 7% (P=0.002)
- Ewings sarcoma, decreased from 19% to 10% (P=0.01)
They found no reductions in subsequent severe health conditions among survivors of neuroblastoma, acute myeloid leukemia (AML), soft tissue sarcoma, or osteosarcoma.
The investigators believe the decreases were driven mainly by a reduced incidence of endocrine conditions, subsequent malignant neoplasms, gastrointestinal and neurological conditions, but not cardiac or pulmonary conditions.
They also analyzed the reduction in treatment intensities by decade for different diseases and found they correlated with the reduced incidence of serious chronic health conditions by 15 years after diagnosis.
The National Institutes of Health funded the study.
CHICAGO—The 15-year cumulative incidence of severe health conditions for survivors of childhood cancer has decreased over the past 30 years, from 12.7% for those diagnosed in the 1970s to 10.1% and 8.9% for those diagnosed in the 1980s and 1990s, respectively. And the decreases were greatest for patients with Wilms’ tumor and Hodgkin lymphoma (HL), followed by patients with astrocytoma, non-Hodgkin lymphoma (NHL), and acute lymphoblastic leukemia (ALL).
Investigators of the Childhood Cancer Survivor Study (CCSS) undertook a retrospective cohort analysis of children aged 0 – 14 years diagnosed with cancer between 1970 and 1999. Their goal was to determine whether cancer therapy modifications have maintained cure rates while decreasing the risk of late effects of therapy.
Todd M. Gibson, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, presented the findings at the 2017 annual meeting of the American Society for Clinical Oncology (ASCO) as abstract LBA10500.
Researchers analyzed data from 23,600 childhood cancer survivors in the CCSS who were alive 5 years after diagnosis. The patients had leukemia, lymphoma, CNS malignancies, Wilms tumor, neuroblastoma, or soft-tissue/bone sarcoma.
Dr Gibson noted that while 83% of children with a malignancy achieve a 5-year survival, more than half develop at least one severe, disabling, life-threatening health condition by age 50.
The survivors were a median age at last follow-up of 28 years (range, 5-63) and the median time since diagnosis was 21 years (range, 5-43).
The investigators found significant decreases in severe health conditions in 6 diagnostic groups:
- Wilms tumor, decreased from 13% to 5% (P<0.0001)
- HL, decreased from 18% to 11% (P<0.0001)
- Astrocytoma, decreased from 15% to 9% (P=0.004)
- NHL, decreased from 10% to 6% (P=0.04)
- ALL, decreased from 9% to 7% (P=0.002)
- Ewings sarcoma, decreased from 19% to 10% (P=0.01)
They found no reductions in subsequent severe health conditions among survivors of neuroblastoma, acute myeloid leukemia (AML), soft tissue sarcoma, or osteosarcoma.
The investigators believe the decreases were driven mainly by a reduced incidence of endocrine conditions, subsequent malignant neoplasms, gastrointestinal and neurological conditions, but not cardiac or pulmonary conditions.
They also analyzed the reduction in treatment intensities by decade for different diseases and found they correlated with the reduced incidence of serious chronic health conditions by 15 years after diagnosis.
The National Institutes of Health funded the study.
Differences emerge in new guidelines for managing FN in kids
A multidisciplinary, international panel of experts has updated earlier clinical practice guidelines on managing fever and neutropenia (FN) in children with cancer and in those undergoing hematopoietic stem cell transplantation (HSCT). And while most of the recommendations remained unchanged from the 2012 guidelines, a few key differences emerged. The changes included addition of a 4th generation cephalosporin for empirical antifungal therapy and refinements in risk stratification for invasive fungal disease (IFD), among others.
The new guidelines were published by The International Pediatric Fever and Neutropenia Guideline Panel in the Journal of Clinical Oncology.
The recommendations were organized into 3 major sections: initial presentation, ongoing management, and empirical antifungal therapy. The guidelines panel followed procedures previously validated for creating evidence-based guidelines and used the Appraisal of Guidelines for Research & Evaluation II instrument as a framework.
For the initial presentation of FN, the panel increased the quality of evidence from low to moderate in the recommendation to obtain peripheral blood cultures concurrent with central venous catheter cultures.
In the treatment of FN, the panel added a 4th-generation cephalosporin as empirical therapy in high-risk FN.
The panel refined the IFD risk factors and decreased the quality of evidence from moderate to low. Children with acute myeloid leukemia (AML), high-risk acute lymphoblastic leukemia (ALL), relapsed acute leukemia, those undergoing allogeneic HSCT, those with prolonged neutropenia, and those receiving high-dose corticosteroids are at high risk of IFD. All others should be categorized as IFD low risk.
The panel suggested serum galactomannan not be used to guide empirical antifungal management for prolonged FN lasting 96 hours or more in high-risk IFD patients. GM does not rule out non-Aspergillus molds, and therefore high negative values provide less useful predictions. Previously, the use of galactomannan was a weak recommendation.
The panel added a new recommendation against using fungal polymerase chain reaction (PCR) testing in blood. They explained PCR testing provides poor positive predictive values and negative predictive values are not sufficiently high to be clinically useful. Also, PCR testing is not yet standardized.
Another new recommendation is the addition of imaging of the abdomen in patients without localizing signs or symptoms. Even though the ideal imaging modality is not known, ultrasound is readily available, not associated with radiation exposure, and usually does not require sedation. For these reasons, the panel said it is preferable to computed tomography or magnetic resonance imaging.
The panel also changed a previously weak recommendation to administer empirical therapy for IFD low-risk patients with prolonged FN to a weak recommendation against administering therapy for these patients.
The panel's recommendations and their rationale can be found in the JCO article.
The guidelines update was supported by meeting grants from the Canadian Institutes of Health Research and the Garron Comprehensive Cancer Centre. ![]()
A multidisciplinary, international panel of experts has updated earlier clinical practice guidelines on managing fever and neutropenia (FN) in children with cancer and in those undergoing hematopoietic stem cell transplantation (HSCT). And while most of the recommendations remained unchanged from the 2012 guidelines, a few key differences emerged. The changes included addition of a 4th generation cephalosporin for empirical antifungal therapy and refinements in risk stratification for invasive fungal disease (IFD), among others.
The new guidelines were published by The International Pediatric Fever and Neutropenia Guideline Panel in the Journal of Clinical Oncology.
The recommendations were organized into 3 major sections: initial presentation, ongoing management, and empirical antifungal therapy. The guidelines panel followed procedures previously validated for creating evidence-based guidelines and used the Appraisal of Guidelines for Research & Evaluation II instrument as a framework.
For the initial presentation of FN, the panel increased the quality of evidence from low to moderate in the recommendation to obtain peripheral blood cultures concurrent with central venous catheter cultures.
In the treatment of FN, the panel added a 4th-generation cephalosporin as empirical therapy in high-risk FN.
The panel refined the IFD risk factors and decreased the quality of evidence from moderate to low. Children with acute myeloid leukemia (AML), high-risk acute lymphoblastic leukemia (ALL), relapsed acute leukemia, those undergoing allogeneic HSCT, those with prolonged neutropenia, and those receiving high-dose corticosteroids are at high risk of IFD. All others should be categorized as IFD low risk.
The panel suggested serum galactomannan not be used to guide empirical antifungal management for prolonged FN lasting 96 hours or more in high-risk IFD patients. GM does not rule out non-Aspergillus molds, and therefore high negative values provide less useful predictions. Previously, the use of galactomannan was a weak recommendation.
The panel added a new recommendation against using fungal polymerase chain reaction (PCR) testing in blood. They explained PCR testing provides poor positive predictive values and negative predictive values are not sufficiently high to be clinically useful. Also, PCR testing is not yet standardized.
Another new recommendation is the addition of imaging of the abdomen in patients without localizing signs or symptoms. Even though the ideal imaging modality is not known, ultrasound is readily available, not associated with radiation exposure, and usually does not require sedation. For these reasons, the panel said it is preferable to computed tomography or magnetic resonance imaging.
The panel also changed a previously weak recommendation to administer empirical therapy for IFD low-risk patients with prolonged FN to a weak recommendation against administering therapy for these patients.
The panel's recommendations and their rationale can be found in the JCO article.
The guidelines update was supported by meeting grants from the Canadian Institutes of Health Research and the Garron Comprehensive Cancer Centre. ![]()
A multidisciplinary, international panel of experts has updated earlier clinical practice guidelines on managing fever and neutropenia (FN) in children with cancer and in those undergoing hematopoietic stem cell transplantation (HSCT). And while most of the recommendations remained unchanged from the 2012 guidelines, a few key differences emerged. The changes included addition of a 4th generation cephalosporin for empirical antifungal therapy and refinements in risk stratification for invasive fungal disease (IFD), among others.
The new guidelines were published by The International Pediatric Fever and Neutropenia Guideline Panel in the Journal of Clinical Oncology.
The recommendations were organized into 3 major sections: initial presentation, ongoing management, and empirical antifungal therapy. The guidelines panel followed procedures previously validated for creating evidence-based guidelines and used the Appraisal of Guidelines for Research & Evaluation II instrument as a framework.
For the initial presentation of FN, the panel increased the quality of evidence from low to moderate in the recommendation to obtain peripheral blood cultures concurrent with central venous catheter cultures.
In the treatment of FN, the panel added a 4th-generation cephalosporin as empirical therapy in high-risk FN.
The panel refined the IFD risk factors and decreased the quality of evidence from moderate to low. Children with acute myeloid leukemia (AML), high-risk acute lymphoblastic leukemia (ALL), relapsed acute leukemia, those undergoing allogeneic HSCT, those with prolonged neutropenia, and those receiving high-dose corticosteroids are at high risk of IFD. All others should be categorized as IFD low risk.
The panel suggested serum galactomannan not be used to guide empirical antifungal management for prolonged FN lasting 96 hours or more in high-risk IFD patients. GM does not rule out non-Aspergillus molds, and therefore high negative values provide less useful predictions. Previously, the use of galactomannan was a weak recommendation.
The panel added a new recommendation against using fungal polymerase chain reaction (PCR) testing in blood. They explained PCR testing provides poor positive predictive values and negative predictive values are not sufficiently high to be clinically useful. Also, PCR testing is not yet standardized.
Another new recommendation is the addition of imaging of the abdomen in patients without localizing signs or symptoms. Even though the ideal imaging modality is not known, ultrasound is readily available, not associated with radiation exposure, and usually does not require sedation. For these reasons, the panel said it is preferable to computed tomography or magnetic resonance imaging.
The panel also changed a previously weak recommendation to administer empirical therapy for IFD low-risk patients with prolonged FN to a weak recommendation against administering therapy for these patients.
The panel's recommendations and their rationale can be found in the JCO article.
The guidelines update was supported by meeting grants from the Canadian Institutes of Health Research and the Garron Comprehensive Cancer Centre. ![]()
MRD beats CR in prognostic value for MM, team confirms
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
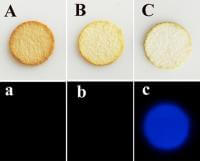
Malaria drug could help identify bloodstains
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
Preventing thrombosis without increasing bleeding risk
It may be possible to disrupt thrombosis without increasing the risk of bleeding, according to preclinical research published in Nature Communications.
“We have found a new thrombosis target that does not increase bleeding risk,” said study author Daniel I. Simon, MD, of University Hospitals Cleveland Medical Center in Cleveland, Ohio.
“Our discovery indicates that you can identify a new pathway and target that mediates blood clotting but does not affect our body’s natural processes to stop bleeding.”
The new pathway centers around a pair of protein receptors. One—Mac-1—is found on the surface of leukocytes recruited to sites of blood vessel injury, and the other—GPIbα—resides on the surface of platelets.
When the receptors interact, they trigger cascades of signals that amplify both inflammation and clotting.
The researchers found that genetically engineered mice, either without the Mac-1 receptor or with a mutant form of the receptor, could not bind GPIbα on platelets. As a result, the mice had delayed clot formation in response to artery injury.
However, these mice had similar platelet counts, platelet activation, plasma coagulation activity, and bleeding time as wild-type mice.
Additional experiments in mice showed that an antibody targeting Mac-1:GPIba inhibits thrombus formation.
And glucosamine, a small-molecule inhibitor of Mac-1:GPIba binding, inhibits thrombus formation without increasing bleeding risk.
Mice exposed to glucosamine were still able to successfully stop minor bleeding, like tail cuts, and maintain normal coagulation and platelet function.
The researchers believe these findings could lead to the development of better antithrombotic agents, as “the interaction between leukocyte Mac-1 and platelet GPIba is positioned as a novel and targetable mediator of thrombosis but not hemostasis.”
“Current anticlotting drugs and antiplatelet agents are effective in reducing heart attack and stroke but are associated with increased bleeding and transfusion,” Dr Simon said. “We have learned that bleeding and transfusion complications are equally as bad from a prognosis standpoint as heart attack or stroke.” ![]()
It may be possible to disrupt thrombosis without increasing the risk of bleeding, according to preclinical research published in Nature Communications.
“We have found a new thrombosis target that does not increase bleeding risk,” said study author Daniel I. Simon, MD, of University Hospitals Cleveland Medical Center in Cleveland, Ohio.
“Our discovery indicates that you can identify a new pathway and target that mediates blood clotting but does not affect our body’s natural processes to stop bleeding.”
The new pathway centers around a pair of protein receptors. One—Mac-1—is found on the surface of leukocytes recruited to sites of blood vessel injury, and the other—GPIbα—resides on the surface of platelets.
When the receptors interact, they trigger cascades of signals that amplify both inflammation and clotting.
The researchers found that genetically engineered mice, either without the Mac-1 receptor or with a mutant form of the receptor, could not bind GPIbα on platelets. As a result, the mice had delayed clot formation in response to artery injury.
However, these mice had similar platelet counts, platelet activation, plasma coagulation activity, and bleeding time as wild-type mice.
Additional experiments in mice showed that an antibody targeting Mac-1:GPIba inhibits thrombus formation.
And glucosamine, a small-molecule inhibitor of Mac-1:GPIba binding, inhibits thrombus formation without increasing bleeding risk.
Mice exposed to glucosamine were still able to successfully stop minor bleeding, like tail cuts, and maintain normal coagulation and platelet function.
The researchers believe these findings could lead to the development of better antithrombotic agents, as “the interaction between leukocyte Mac-1 and platelet GPIba is positioned as a novel and targetable mediator of thrombosis but not hemostasis.”
“Current anticlotting drugs and antiplatelet agents are effective in reducing heart attack and stroke but are associated with increased bleeding and transfusion,” Dr Simon said. “We have learned that bleeding and transfusion complications are equally as bad from a prognosis standpoint as heart attack or stroke.” ![]()
It may be possible to disrupt thrombosis without increasing the risk of bleeding, according to preclinical research published in Nature Communications.
“We have found a new thrombosis target that does not increase bleeding risk,” said study author Daniel I. Simon, MD, of University Hospitals Cleveland Medical Center in Cleveland, Ohio.
“Our discovery indicates that you can identify a new pathway and target that mediates blood clotting but does not affect our body’s natural processes to stop bleeding.”
The new pathway centers around a pair of protein receptors. One—Mac-1—is found on the surface of leukocytes recruited to sites of blood vessel injury, and the other—GPIbα—resides on the surface of platelets.
When the receptors interact, they trigger cascades of signals that amplify both inflammation and clotting.
The researchers found that genetically engineered mice, either without the Mac-1 receptor or with a mutant form of the receptor, could not bind GPIbα on platelets. As a result, the mice had delayed clot formation in response to artery injury.
However, these mice had similar platelet counts, platelet activation, plasma coagulation activity, and bleeding time as wild-type mice.
Additional experiments in mice showed that an antibody targeting Mac-1:GPIba inhibits thrombus formation.
And glucosamine, a small-molecule inhibitor of Mac-1:GPIba binding, inhibits thrombus formation without increasing bleeding risk.
Mice exposed to glucosamine were still able to successfully stop minor bleeding, like tail cuts, and maintain normal coagulation and platelet function.
The researchers believe these findings could lead to the development of better antithrombotic agents, as “the interaction between leukocyte Mac-1 and platelet GPIba is positioned as a novel and targetable mediator of thrombosis but not hemostasis.”
“Current anticlotting drugs and antiplatelet agents are effective in reducing heart attack and stroke but are associated with increased bleeding and transfusion,” Dr Simon said. “We have learned that bleeding and transfusion complications are equally as bad from a prognosis standpoint as heart attack or stroke.” ![]()
Gene plays key role in iron homeostasis
A gene known to prevent autoimmune diseases is a key regulator in iron uptake, according to research published in Cell Reports.
“We found previously that, when mice lack the gene Regnase-1, they suffer from severe autoimmune diseases and anemia,” said study author Masanori Yoshinaga, MD, of Kyoto University in Japan.
“At first, we assumed that anemia was a secondary effect, but, after detailed analysis, we found that the 2 symptoms develop independently.”
Continued study of mice with a Regnase-1 mutation revealed a functional defect in the principal site for iron absorption in the body, the duodenum.
“The next step was to find the role of Regnase-1 in iron-uptake maintenance,” Dr Yoshinaga said. “We started by looking at the most important iron-uptake gene, Transferrin Receptor 1, or TfR1.”
“Our results showed that Regnase-1 degrades the mRNA of TfR1, thereby inhibiting the synthesis of the TfR1 protein and, additionally, that it likely regulates other important iron-controlling genes.”
“Further analysis of Regnase-1 in iron-related homeostasis may provide insight into the mechanisms causing anemia and other iron-related disorders, perhaps eventually leading to new methods of treatment,” said study author Osamu Takeuchi, MD, PhD, of Kyoto University. ![]()
A gene known to prevent autoimmune diseases is a key regulator in iron uptake, according to research published in Cell Reports.
“We found previously that, when mice lack the gene Regnase-1, they suffer from severe autoimmune diseases and anemia,” said study author Masanori Yoshinaga, MD, of Kyoto University in Japan.
“At first, we assumed that anemia was a secondary effect, but, after detailed analysis, we found that the 2 symptoms develop independently.”
Continued study of mice with a Regnase-1 mutation revealed a functional defect in the principal site for iron absorption in the body, the duodenum.
“The next step was to find the role of Regnase-1 in iron-uptake maintenance,” Dr Yoshinaga said. “We started by looking at the most important iron-uptake gene, Transferrin Receptor 1, or TfR1.”
“Our results showed that Regnase-1 degrades the mRNA of TfR1, thereby inhibiting the synthesis of the TfR1 protein and, additionally, that it likely regulates other important iron-controlling genes.”
“Further analysis of Regnase-1 in iron-related homeostasis may provide insight into the mechanisms causing anemia and other iron-related disorders, perhaps eventually leading to new methods of treatment,” said study author Osamu Takeuchi, MD, PhD, of Kyoto University. ![]()
A gene known to prevent autoimmune diseases is a key regulator in iron uptake, according to research published in Cell Reports.
“We found previously that, when mice lack the gene Regnase-1, they suffer from severe autoimmune diseases and anemia,” said study author Masanori Yoshinaga, MD, of Kyoto University in Japan.
“At first, we assumed that anemia was a secondary effect, but, after detailed analysis, we found that the 2 symptoms develop independently.”
Continued study of mice with a Regnase-1 mutation revealed a functional defect in the principal site for iron absorption in the body, the duodenum.
“The next step was to find the role of Regnase-1 in iron-uptake maintenance,” Dr Yoshinaga said. “We started by looking at the most important iron-uptake gene, Transferrin Receptor 1, or TfR1.”
“Our results showed that Regnase-1 degrades the mRNA of TfR1, thereby inhibiting the synthesis of the TfR1 protein and, additionally, that it likely regulates other important iron-controlling genes.”
“Further analysis of Regnase-1 in iron-related homeostasis may provide insight into the mechanisms causing anemia and other iron-related disorders, perhaps eventually leading to new methods of treatment,” said study author Osamu Takeuchi, MD, PhD, of Kyoto University. ![]()
EMA recommends orphan designation for hemophilia B product
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has issued a positive opinion recommending orphan designation for CB 2679d/ISU304 for the treatment of hemophilia B.
CB 2679d is a coagulation factor IX variant that has demonstrated, in preclinical studies, the potential to normalize factor IX levels via a daily subcutaneous injection.
The product is being developed by Catalyst Biosciences and ISU Abxis. ISU Abxis plans to initiate a phase 1/2 study of CB 2679d in individuals with severe hemophilia B this month in South Korea.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has issued a positive opinion recommending orphan designation for CB 2679d/ISU304 for the treatment of hemophilia B.
CB 2679d is a coagulation factor IX variant that has demonstrated, in preclinical studies, the potential to normalize factor IX levels via a daily subcutaneous injection.
The product is being developed by Catalyst Biosciences and ISU Abxis. ISU Abxis plans to initiate a phase 1/2 study of CB 2679d in individuals with severe hemophilia B this month in South Korea.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission. ![]()
The European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products has issued a positive opinion recommending orphan designation for CB 2679d/ISU304 for the treatment of hemophilia B.
CB 2679d is a coagulation factor IX variant that has demonstrated, in preclinical studies, the potential to normalize factor IX levels via a daily subcutaneous injection.
The product is being developed by Catalyst Biosciences and ISU Abxis. ISU Abxis plans to initiate a phase 1/2 study of CB 2679d in individuals with severe hemophilia B this month in South Korea.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The commission typically makes a decision within 30 days of the submission.
Indian govt. waited months to report Zika cases
The Indian government waited months to report its first cases of Zika virus to the World Health Organization (WHO), according to a statement from the agency.
The WHO said that, on May 15, Ministry of Health and Family Welfare-Government of India reported 3 laboratory-confirmed cases of Zika virus disease in the Bapunagar area of the Ahmedabad district in Gujarat, India.
The first of these cases was originally discovered in November 2016, and the other 2 were discovered in January 2017 and February 2017, respectively.
Chief Secretary of Gujarat State J. N. Singh told The Times of India that “the government consciously did not go public with the cases.”
However, B.J. Medical College (BJMC), where the cases were discovered, reported them to the National Institute of Virology, Pune, which informed the Indian Council of Medical Research and the Union government “as per protocol,” according to Singh.
Soumya Swaminathan, director-general of the Indian Council of Medical Research, told Scroll.in that the discovery of Zika at BJMC prompted increased surveillance for the virus in Ahmedabad. However, because no additional cases of Zika were found, the government felt no need to inform the public.
The same Scroll.in article reported that Bapunagar residents are angry but not surprised the government did not inform the public of the Zika cases. In fact, there is a theory that the government failed to disclose the Zika cases out of fear that the news would disrupt the Vibrant Gujarat Summit, a conference for investors taking place in Gandhinagar.
However, the mayor of Ahmedabad, Gautam Shah, denied this, as well as any knowledge of the Zika cases prior to the WHO’s disclosure. And Shankar Chaudhary, Gujarat’s health minister, said the government complied with WHO guidelines on reporting Zika cases.
Case details
Singh told The Times of India that all 3 Zika patients “are well and have shown no complications till now.”
According to the WHO, the first Zika case was a 34-year-old female who delivered a “clinically well baby” at BJMC in Ahmedabad on November 9, 2016. She developed a low-grade fever after delivery while still in the hospital. She had no history of fever during pregnancy and no history of travel for the past 3 months.
The Viral Research & Diagnostic Laboratory at BJMC found the patient was positive for Zika virus. Subsequent testing at the National Institute of Virology, Pune, confirmed this finding.
The second case of Zika virus was detected during antenatal clinic surveillance. Between January 6 and 12 of this year, 111 blood samples were collected in the antenatal clinic at BJMC.
One of these samples, from a 22-year-old pregnant female, tested positive for Zika. According to Singh, this patient also delivered a healthy baby.
The third case of Zika was detected via acute febrile illness surveillance. Between February 10 and 16 of this year, 93 blood samples were collected from patients treated for febrile illness treated at BJMC. And a 64-year-old male who had febrile illness for 8 days tested positive for Zika.
The WHO said these findings suggest low-level transmission of Zika virus, but new cases may occur in the future. The agency recommended strengthening surveillance in the area.
The WHO did not recommend any travel or trade restriction to India based on these Zika cases. And the agency noted that several steps have been taken to inform the public of the risk of Zika in India and prevent an outbreak in the country.
The Indian government waited months to report its first cases of Zika virus to the World Health Organization (WHO), according to a statement from the agency.
The WHO said that, on May 15, Ministry of Health and Family Welfare-Government of India reported 3 laboratory-confirmed cases of Zika virus disease in the Bapunagar area of the Ahmedabad district in Gujarat, India.
The first of these cases was originally discovered in November 2016, and the other 2 were discovered in January 2017 and February 2017, respectively.
Chief Secretary of Gujarat State J. N. Singh told The Times of India that “the government consciously did not go public with the cases.”
However, B.J. Medical College (BJMC), where the cases were discovered, reported them to the National Institute of Virology, Pune, which informed the Indian Council of Medical Research and the Union government “as per protocol,” according to Singh.
Soumya Swaminathan, director-general of the Indian Council of Medical Research, told Scroll.in that the discovery of Zika at BJMC prompted increased surveillance for the virus in Ahmedabad. However, because no additional cases of Zika were found, the government felt no need to inform the public.
The same Scroll.in article reported that Bapunagar residents are angry but not surprised the government did not inform the public of the Zika cases. In fact, there is a theory that the government failed to disclose the Zika cases out of fear that the news would disrupt the Vibrant Gujarat Summit, a conference for investors taking place in Gandhinagar.
However, the mayor of Ahmedabad, Gautam Shah, denied this, as well as any knowledge of the Zika cases prior to the WHO’s disclosure. And Shankar Chaudhary, Gujarat’s health minister, said the government complied with WHO guidelines on reporting Zika cases.
Case details
Singh told The Times of India that all 3 Zika patients “are well and have shown no complications till now.”
According to the WHO, the first Zika case was a 34-year-old female who delivered a “clinically well baby” at BJMC in Ahmedabad on November 9, 2016. She developed a low-grade fever after delivery while still in the hospital. She had no history of fever during pregnancy and no history of travel for the past 3 months.
The Viral Research & Diagnostic Laboratory at BJMC found the patient was positive for Zika virus. Subsequent testing at the National Institute of Virology, Pune, confirmed this finding.
The second case of Zika virus was detected during antenatal clinic surveillance. Between January 6 and 12 of this year, 111 blood samples were collected in the antenatal clinic at BJMC.
One of these samples, from a 22-year-old pregnant female, tested positive for Zika. According to Singh, this patient also delivered a healthy baby.
The third case of Zika was detected via acute febrile illness surveillance. Between February 10 and 16 of this year, 93 blood samples were collected from patients treated for febrile illness treated at BJMC. And a 64-year-old male who had febrile illness for 8 days tested positive for Zika.
The WHO said these findings suggest low-level transmission of Zika virus, but new cases may occur in the future. The agency recommended strengthening surveillance in the area.
The WHO did not recommend any travel or trade restriction to India based on these Zika cases. And the agency noted that several steps have been taken to inform the public of the risk of Zika in India and prevent an outbreak in the country.
The Indian government waited months to report its first cases of Zika virus to the World Health Organization (WHO), according to a statement from the agency.
The WHO said that, on May 15, Ministry of Health and Family Welfare-Government of India reported 3 laboratory-confirmed cases of Zika virus disease in the Bapunagar area of the Ahmedabad district in Gujarat, India.
The first of these cases was originally discovered in November 2016, and the other 2 were discovered in January 2017 and February 2017, respectively.
Chief Secretary of Gujarat State J. N. Singh told The Times of India that “the government consciously did not go public with the cases.”
However, B.J. Medical College (BJMC), where the cases were discovered, reported them to the National Institute of Virology, Pune, which informed the Indian Council of Medical Research and the Union government “as per protocol,” according to Singh.
Soumya Swaminathan, director-general of the Indian Council of Medical Research, told Scroll.in that the discovery of Zika at BJMC prompted increased surveillance for the virus in Ahmedabad. However, because no additional cases of Zika were found, the government felt no need to inform the public.
The same Scroll.in article reported that Bapunagar residents are angry but not surprised the government did not inform the public of the Zika cases. In fact, there is a theory that the government failed to disclose the Zika cases out of fear that the news would disrupt the Vibrant Gujarat Summit, a conference for investors taking place in Gandhinagar.
However, the mayor of Ahmedabad, Gautam Shah, denied this, as well as any knowledge of the Zika cases prior to the WHO’s disclosure. And Shankar Chaudhary, Gujarat’s health minister, said the government complied with WHO guidelines on reporting Zika cases.
Case details
Singh told The Times of India that all 3 Zika patients “are well and have shown no complications till now.”
According to the WHO, the first Zika case was a 34-year-old female who delivered a “clinically well baby” at BJMC in Ahmedabad on November 9, 2016. She developed a low-grade fever after delivery while still in the hospital. She had no history of fever during pregnancy and no history of travel for the past 3 months.
The Viral Research & Diagnostic Laboratory at BJMC found the patient was positive for Zika virus. Subsequent testing at the National Institute of Virology, Pune, confirmed this finding.
The second case of Zika virus was detected during antenatal clinic surveillance. Between January 6 and 12 of this year, 111 blood samples were collected in the antenatal clinic at BJMC.
One of these samples, from a 22-year-old pregnant female, tested positive for Zika. According to Singh, this patient also delivered a healthy baby.
The third case of Zika was detected via acute febrile illness surveillance. Between February 10 and 16 of this year, 93 blood samples were collected from patients treated for febrile illness treated at BJMC. And a 64-year-old male who had febrile illness for 8 days tested positive for Zika.
The WHO said these findings suggest low-level transmission of Zika virus, but new cases may occur in the future. The agency recommended strengthening surveillance in the area.
The WHO did not recommend any travel or trade restriction to India based on these Zika cases. And the agency noted that several steps have been taken to inform the public of the risk of Zika in India and prevent an outbreak in the country.