User login
FDA lifts clinical hold on AML trials
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on 3 trials of vadastuximab talirine (SGN-CD33A), an antibody-drug conjugate targeting CD33, in acute myeloid leukemia (AML).
Last December, 1 trial was placed on full clinical hold (enrollment was halted and no further dosing of subjects was allowed), and 2 were placed on partial hold (enrollment was halted, but existing patients could continue treatment with re-consent).
All 3 of the holds were due to the potential risk of hepatotoxicity in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) before or after treatment with vadastuximab talirine.
In particular, the holds were in response to 6 cases of hepatotoxicity, including several cases of veno-occlusive disease (VOD), with 4 fatal events.
At the time the holds were announced, Seattle Genetics, Inc., the company developing vadastuximab talirine, said it was working with the FDA to determine whether there is an association between hepatotoxicity and treatment with the drug.
The company analyzed data from more than 350 patients treated with vadastuximab talirine and found no such association.
The rate of VOD they observed was “within the background rate of VOD in AML patients receiving allo-transplant,” according to Clay B. Siegall, PhD, president, chief executive officer, and chairman of the board at Seattle Genetics.
Dr Siegall said the company would not disclose the exact rate of VOD in these trials.
Resuming trials
As Seattle Genetics found no evidence to suggest that vadastuximab talirine increased the risk of hepatotoxicity, the FDA lifted the clinical holds on all 3 trials. The 2 trials placed on partial hold will continue, but the trial placed on full hold will not.
One of the trials that will continue is a phase 1 study of vadastuximab talirine alone and in combination with hypomethylating agents in both newly diagnosed and relapsed AML patients.
The other trial is a phase 1 study of vadastuximab talirine in combination with 7+3 chemotherapy in newly diagnosed, younger AML patients. (Results from this trial were presented at the 2016 ASH Annual Meeting.)
Cancelled trial
The trial that will not resume is a phase 1/2 study of vadastuximab talirine monotherapy pre- and post-allogeneic HSCT in patients with relapsed, chemo-resistant AML.
Seattle Genetics said it will not continue with this trial because of the challenges of developing therapies in this specific setting.
“It’s a very small group of patients, and we’re going to focus on the 3 biggest groups of patients [older and younger patients newly diagnosed with AML and patients with myelodysplastic syndromes] so we can really impact AML in the biggest way,” Dr Siegall said.
He noted that this decision does not prevent patients from undergoing HSCT after receiving vadastuximab talirine.
In the phase 1/2 trial, patients received vadastuximab talirine directly before HSCT, a practice that will not continue. However, patients can undergo HSCT as long as the transplant doesn’t occur immediately after treatment with vadastuximab talirine.
Moving forward
Two other trials of vadastuximab talirine were not affected by the clinical holds and have continued to enroll patients.
One is CASCADE, a randomized, phase 3 trial of vadastuximab talirine as front-line therapy in older AML patients. The other is a phase 1/2 trial of vadastuximab talirine as front-line therapy in patients with myelodysplastic syndromes.
Seattle Genetics is also planning to begin a randomized, phase 2 trial comparing 7+3 chemotherapy alone to 7+3 in combination with vadastuximab talirine in younger patients with previously untreated AML. The company plans to start the trial later this year.
Going forward, additional risk mitigation measures will be implemented in all vadastuximab talirine studies, including revised eligibility criteria and stopping rules for VOD.
Specifically, trials will not be stopped if the incidence of VOD is considered within the normal range, and an adjudication committee consisting of 2 experts will be tasked with verifying reports of VOD.
In addition, patients with liver cirrhosis due to alcohol abuse are no longer eligible for trials of vadastuximab talirine. ![]()
Long-term safety, efficacy of hemophilia B therapy
Interim results from the B-YOND trial suggest prophylactic treatment with a recombinant factor IX Fc fusion protein (rFIXFc) can provide long-term safety and efficacy, according to researchers.
B-YOND is an extension study for adults and adolescents who completed the B-LONG study and children who completed the Kids B-LONG study.
In both trials, researchers tested rFIXFc in patients with hemophilia B.
The median duration of rFIXFc treatment has surpassed 3 years for the adults and adolescents enrolled in B-YOND and exceeded 1.5 years for children in this trial.
Researchers said the median annualized bleeding rates (ABRs) have been low in these patients, and none of the patients have developed inhibitors.
“The interim data from B-YOND confirm the safety profile of [rFIXFc] and show that adult, adolescent, and pediatric subjects maintained low annual bleed rates with prophylactic dosing of [rFIXFc] every 1 to 2 weeks,” said principal investigator John Pasi, MD, PhD, of Barts and the London School of Medicine and Dentistry in London, UK.
“These results come from the longest-term study of an extended half-life therapy for hemophilia B and provide physicians across the globe with important insights and information about the treatment of hemophilia B.”
The results were published in Thrombosis and Haemostasis.
The research was sponsored by Bioverativ Therapeutics Inc., the company developing rFIXFc (also known as eftrenonacog alfa and by the brand name Alprolix) in collaboration with Sobi. rFIXFc is approved to treat hemophilia B in the US, European Union, and other countries.
Treatment
B-YOND has enrolled 116 patients with hemophilia B who completed B-LONG (n=93) or Kids B-LONG (n=23). The patients were placed in 1 of 4 treatment groups (but could change at any point):
- Weekly prophylaxis—20 to 100 IU/kg every 7 days (50 adults/adolescents, 19 children)
- Individualized prophylaxis—100 IU/kg every 8 to 16 days (30 adults/adolescents, 5 children)
- Modified prophylaxis, which was defined as further dosing personalization to optimize prophylaxis (13 adults/adolescents, 1 child)
- Episodic treatment, which was available only to adults and adolescents (n=15).
In the weekly prophylaxis group, the median dosing interval was 7.0 days for adults, adolescents, and children. The average weekly prophylactic dose was 49.5 IU/kg in adults/adolescents, 64.4 IU/kg in kids younger than 6, and 63.1 IU/kg in kids ages 6 to 11.
In the individualized prophylaxis group, the median dosing interval was 13.7 days for adults and adolescents and 10.0 days in pediatric patients (ages 6 to 11 only). The average weekly prophylactic dose was 50.2 IU/kg in adults/adolescents, and 66.6 IU/kg in kids ages 6 to 11.
In the modified prophylaxis group, the median dosing interval was 6.9 days for adults and adolescents and 4.1 days in the single pediatric patient (who was older than 6). The average weekly prophylactic dose was 61.7 IU/kg in adults/adolescents and 157.9 IU/kg in the pediatric patient.
From the start of B-LONG to the B-YOND interim data cut, adults/adolescents had a median of 39.5 months of cumulative rFIXFc treatment and a median of 162 cumulative exposure days.
From the start of Kids B-LONG to the data cut, pediatric patients had a median of 21.9 months of cumulative rFIXFc treatment and a median of 94 cumulative exposure days.
ABRs
As of the interim data cut, the overall median ABR was 2.3 for adults/adolescents in both the weekly and individualized prophylaxis groups.
The median ABR was 2.4 for adults/adolescents in the modified prophylaxis group and 11.3 for those receiving on-demand treatment.
Among children under age 6 (n=9), the median ABR in the weekly prophylaxis group was 0. (None of the younger children had individualized or modified prophylaxis.)
For children ages 6 to 11, the median ABR was 2.7 in the weekly prophylaxis group (n=10) and 2.4 in the individualized prophylaxis group (n=5). The patient in the modified prophylaxis group had an ABR of 3.1.
Safety
The researchers said rFIXFc was well-tolerated, and the adverse events (AEs) reported were typical of the population studied.
AEs were reported in 75.9% of patients. The most common were headache (n=14, 12.1%) and common cold (n=13, 11.2%), and the majority of AEs were considered unrelated to rFIXFc.
Three adult/adolescent patients experienced AEs during B-YOND that were considered treatment-related, including noncardiac chest pain, hematuria, and obstructive uropathy. All 3 events resolved.
One patient experienced breath odor during B-LONG that was considered treatment-related. And 1 patient reported decreased appetite during Kids B-LONG that was considered treatment-related. Neither of these events resolved.
There were 39 serious AEs in 23 patients (19.8%). All but 1 of these events were considered unrelated to rFIXFc.
The treatment-related serious AE was renal colic in a patient originally enrolled in the B-LONG study. The patient had a medical history of previous clot colic. The event resolved and did not lead to study discontinuation.
There have been no reports of serious allergic reactions or anaphylaxis associated with rFIXFc, no vascular thrombotic events, and no deaths. ![]()
Interim results from the B-YOND trial suggest prophylactic treatment with a recombinant factor IX Fc fusion protein (rFIXFc) can provide long-term safety and efficacy, according to researchers.
B-YOND is an extension study for adults and adolescents who completed the B-LONG study and children who completed the Kids B-LONG study.
In both trials, researchers tested rFIXFc in patients with hemophilia B.
The median duration of rFIXFc treatment has surpassed 3 years for the adults and adolescents enrolled in B-YOND and exceeded 1.5 years for children in this trial.
Researchers said the median annualized bleeding rates (ABRs) have been low in these patients, and none of the patients have developed inhibitors.
“The interim data from B-YOND confirm the safety profile of [rFIXFc] and show that adult, adolescent, and pediatric subjects maintained low annual bleed rates with prophylactic dosing of [rFIXFc] every 1 to 2 weeks,” said principal investigator John Pasi, MD, PhD, of Barts and the London School of Medicine and Dentistry in London, UK.
“These results come from the longest-term study of an extended half-life therapy for hemophilia B and provide physicians across the globe with important insights and information about the treatment of hemophilia B.”
The results were published in Thrombosis and Haemostasis.
The research was sponsored by Bioverativ Therapeutics Inc., the company developing rFIXFc (also known as eftrenonacog alfa and by the brand name Alprolix) in collaboration with Sobi. rFIXFc is approved to treat hemophilia B in the US, European Union, and other countries.
Treatment
B-YOND has enrolled 116 patients with hemophilia B who completed B-LONG (n=93) or Kids B-LONG (n=23). The patients were placed in 1 of 4 treatment groups (but could change at any point):
- Weekly prophylaxis—20 to 100 IU/kg every 7 days (50 adults/adolescents, 19 children)
- Individualized prophylaxis—100 IU/kg every 8 to 16 days (30 adults/adolescents, 5 children)
- Modified prophylaxis, which was defined as further dosing personalization to optimize prophylaxis (13 adults/adolescents, 1 child)
- Episodic treatment, which was available only to adults and adolescents (n=15).
In the weekly prophylaxis group, the median dosing interval was 7.0 days for adults, adolescents, and children. The average weekly prophylactic dose was 49.5 IU/kg in adults/adolescents, 64.4 IU/kg in kids younger than 6, and 63.1 IU/kg in kids ages 6 to 11.
In the individualized prophylaxis group, the median dosing interval was 13.7 days for adults and adolescents and 10.0 days in pediatric patients (ages 6 to 11 only). The average weekly prophylactic dose was 50.2 IU/kg in adults/adolescents, and 66.6 IU/kg in kids ages 6 to 11.
In the modified prophylaxis group, the median dosing interval was 6.9 days for adults and adolescents and 4.1 days in the single pediatric patient (who was older than 6). The average weekly prophylactic dose was 61.7 IU/kg in adults/adolescents and 157.9 IU/kg in the pediatric patient.
From the start of B-LONG to the B-YOND interim data cut, adults/adolescents had a median of 39.5 months of cumulative rFIXFc treatment and a median of 162 cumulative exposure days.
From the start of Kids B-LONG to the data cut, pediatric patients had a median of 21.9 months of cumulative rFIXFc treatment and a median of 94 cumulative exposure days.
ABRs
As of the interim data cut, the overall median ABR was 2.3 for adults/adolescents in both the weekly and individualized prophylaxis groups.
The median ABR was 2.4 for adults/adolescents in the modified prophylaxis group and 11.3 for those receiving on-demand treatment.
Among children under age 6 (n=9), the median ABR in the weekly prophylaxis group was 0. (None of the younger children had individualized or modified prophylaxis.)
For children ages 6 to 11, the median ABR was 2.7 in the weekly prophylaxis group (n=10) and 2.4 in the individualized prophylaxis group (n=5). The patient in the modified prophylaxis group had an ABR of 3.1.
Safety
The researchers said rFIXFc was well-tolerated, and the adverse events (AEs) reported were typical of the population studied.
AEs were reported in 75.9% of patients. The most common were headache (n=14, 12.1%) and common cold (n=13, 11.2%), and the majority of AEs were considered unrelated to rFIXFc.
Three adult/adolescent patients experienced AEs during B-YOND that were considered treatment-related, including noncardiac chest pain, hematuria, and obstructive uropathy. All 3 events resolved.
One patient experienced breath odor during B-LONG that was considered treatment-related. And 1 patient reported decreased appetite during Kids B-LONG that was considered treatment-related. Neither of these events resolved.
There were 39 serious AEs in 23 patients (19.8%). All but 1 of these events were considered unrelated to rFIXFc.
The treatment-related serious AE was renal colic in a patient originally enrolled in the B-LONG study. The patient had a medical history of previous clot colic. The event resolved and did not lead to study discontinuation.
There have been no reports of serious allergic reactions or anaphylaxis associated with rFIXFc, no vascular thrombotic events, and no deaths. ![]()
Interim results from the B-YOND trial suggest prophylactic treatment with a recombinant factor IX Fc fusion protein (rFIXFc) can provide long-term safety and efficacy, according to researchers.
B-YOND is an extension study for adults and adolescents who completed the B-LONG study and children who completed the Kids B-LONG study.
In both trials, researchers tested rFIXFc in patients with hemophilia B.
The median duration of rFIXFc treatment has surpassed 3 years for the adults and adolescents enrolled in B-YOND and exceeded 1.5 years for children in this trial.
Researchers said the median annualized bleeding rates (ABRs) have been low in these patients, and none of the patients have developed inhibitors.
“The interim data from B-YOND confirm the safety profile of [rFIXFc] and show that adult, adolescent, and pediatric subjects maintained low annual bleed rates with prophylactic dosing of [rFIXFc] every 1 to 2 weeks,” said principal investigator John Pasi, MD, PhD, of Barts and the London School of Medicine and Dentistry in London, UK.
“These results come from the longest-term study of an extended half-life therapy for hemophilia B and provide physicians across the globe with important insights and information about the treatment of hemophilia B.”
The results were published in Thrombosis and Haemostasis.
The research was sponsored by Bioverativ Therapeutics Inc., the company developing rFIXFc (also known as eftrenonacog alfa and by the brand name Alprolix) in collaboration with Sobi. rFIXFc is approved to treat hemophilia B in the US, European Union, and other countries.
Treatment
B-YOND has enrolled 116 patients with hemophilia B who completed B-LONG (n=93) or Kids B-LONG (n=23). The patients were placed in 1 of 4 treatment groups (but could change at any point):
- Weekly prophylaxis—20 to 100 IU/kg every 7 days (50 adults/adolescents, 19 children)
- Individualized prophylaxis—100 IU/kg every 8 to 16 days (30 adults/adolescents, 5 children)
- Modified prophylaxis, which was defined as further dosing personalization to optimize prophylaxis (13 adults/adolescents, 1 child)
- Episodic treatment, which was available only to adults and adolescents (n=15).
In the weekly prophylaxis group, the median dosing interval was 7.0 days for adults, adolescents, and children. The average weekly prophylactic dose was 49.5 IU/kg in adults/adolescents, 64.4 IU/kg in kids younger than 6, and 63.1 IU/kg in kids ages 6 to 11.
In the individualized prophylaxis group, the median dosing interval was 13.7 days for adults and adolescents and 10.0 days in pediatric patients (ages 6 to 11 only). The average weekly prophylactic dose was 50.2 IU/kg in adults/adolescents, and 66.6 IU/kg in kids ages 6 to 11.
In the modified prophylaxis group, the median dosing interval was 6.9 days for adults and adolescents and 4.1 days in the single pediatric patient (who was older than 6). The average weekly prophylactic dose was 61.7 IU/kg in adults/adolescents and 157.9 IU/kg in the pediatric patient.
From the start of B-LONG to the B-YOND interim data cut, adults/adolescents had a median of 39.5 months of cumulative rFIXFc treatment and a median of 162 cumulative exposure days.
From the start of Kids B-LONG to the data cut, pediatric patients had a median of 21.9 months of cumulative rFIXFc treatment and a median of 94 cumulative exposure days.
ABRs
As of the interim data cut, the overall median ABR was 2.3 for adults/adolescents in both the weekly and individualized prophylaxis groups.
The median ABR was 2.4 for adults/adolescents in the modified prophylaxis group and 11.3 for those receiving on-demand treatment.
Among children under age 6 (n=9), the median ABR in the weekly prophylaxis group was 0. (None of the younger children had individualized or modified prophylaxis.)
For children ages 6 to 11, the median ABR was 2.7 in the weekly prophylaxis group (n=10) and 2.4 in the individualized prophylaxis group (n=5). The patient in the modified prophylaxis group had an ABR of 3.1.
Safety
The researchers said rFIXFc was well-tolerated, and the adverse events (AEs) reported were typical of the population studied.
AEs were reported in 75.9% of patients. The most common were headache (n=14, 12.1%) and common cold (n=13, 11.2%), and the majority of AEs were considered unrelated to rFIXFc.
Three adult/adolescent patients experienced AEs during B-YOND that were considered treatment-related, including noncardiac chest pain, hematuria, and obstructive uropathy. All 3 events resolved.
One patient experienced breath odor during B-LONG that was considered treatment-related. And 1 patient reported decreased appetite during Kids B-LONG that was considered treatment-related. Neither of these events resolved.
There were 39 serious AEs in 23 patients (19.8%). All but 1 of these events were considered unrelated to rFIXFc.
The treatment-related serious AE was renal colic in a patient originally enrolled in the B-LONG study. The patient had a medical history of previous clot colic. The event resolved and did not lead to study discontinuation.
There have been no reports of serious allergic reactions or anaphylaxis associated with rFIXFc, no vascular thrombotic events, and no deaths. ![]()
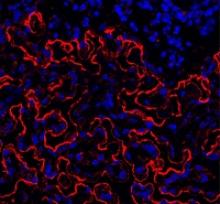
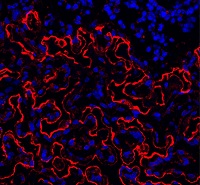
Group reports rejuvenation of aging HSCs
Preclinical research suggests osteopontin, a protein made by osteoblasts, plays a role in hematopoietic stem cell (HSC) aging.
Experiments in mice revealed that, with age, there is a reduction in the expression of osteopontin in the bone marrow stroma.
A lack of osteopontin induced young HSCs to “act” older, while treating older HSCs with recombinant osteopontin restored youthful properties.
Hartmut Geiger, PhD, of the University of Ulm in Germany, and his colleagues reported these findings in EMBO.
“We show that the place where HSCs form in the bone marrow loses osteopontin upon aging, but if you give back the missing protein to the blood-forming cells, they suddenly rejuvenate and act younger,” Dr Geiger said.
“Our study points to exciting, novel ways to have a better immune system and possibly less blood cancer upon aging by therapeutically targeting the place where blood stem cells form.”
The researchers conducted a number of experiments to test the formation and vitality of cells in and near the bone marrow microenvironment.
The team looked at the formation of endosteum stroma cells in aging mice and monitored levels of osteopontin and other proteins linked to distinct cells in the bone marrow during the aging process.
The researchers said they observed reduced production of osteoblasts and other stroma cells in the endosteum of older mice. They also saw decreased osteopontin levels in the bone marrow of older animals, which was associated with reduced vigor and function of HSCs.
The team followed up these experiments by transplanting bone marrow cells from older mice (19 to 21 months) into young mice (8 to 10 weeks).
The researchers also transplanted aged HSCs from older mice into younger mice, and the team treated aged HSCs with a recombinant form of the osteopontin protein.
Transplantation into the younger animals caused HSCs to behave in a younger, more vital manner, the researchers said. This meant smaller numbers of HSCs with greater potential for forming different blood cells, which included larger populations of B and T cells and decreased production of myeloid cells.
The researchers also saw aged HSCs treated with recombinant osteopontin regain their youthful characteristics and capacity to form different blood cell types. Also observed was diminished signaling of Cdc42, a protein previously shown to cause aging in HSCs.
Osteopontin levels are not only low in the bone marrow niche but also in the blood upon aging. As a follow-up to the current study, the researchers are investigating the possibility of using osteopontin replacement therapy in mice to counter the influence of an aging niche directly in the animals. ![]()
Preclinical research suggests osteopontin, a protein made by osteoblasts, plays a role in hematopoietic stem cell (HSC) aging.
Experiments in mice revealed that, with age, there is a reduction in the expression of osteopontin in the bone marrow stroma.
A lack of osteopontin induced young HSCs to “act” older, while treating older HSCs with recombinant osteopontin restored youthful properties.
Hartmut Geiger, PhD, of the University of Ulm in Germany, and his colleagues reported these findings in EMBO.
“We show that the place where HSCs form in the bone marrow loses osteopontin upon aging, but if you give back the missing protein to the blood-forming cells, they suddenly rejuvenate and act younger,” Dr Geiger said.
“Our study points to exciting, novel ways to have a better immune system and possibly less blood cancer upon aging by therapeutically targeting the place where blood stem cells form.”
The researchers conducted a number of experiments to test the formation and vitality of cells in and near the bone marrow microenvironment.
The team looked at the formation of endosteum stroma cells in aging mice and monitored levels of osteopontin and other proteins linked to distinct cells in the bone marrow during the aging process.
The researchers said they observed reduced production of osteoblasts and other stroma cells in the endosteum of older mice. They also saw decreased osteopontin levels in the bone marrow of older animals, which was associated with reduced vigor and function of HSCs.
The team followed up these experiments by transplanting bone marrow cells from older mice (19 to 21 months) into young mice (8 to 10 weeks).
The researchers also transplanted aged HSCs from older mice into younger mice, and the team treated aged HSCs with a recombinant form of the osteopontin protein.
Transplantation into the younger animals caused HSCs to behave in a younger, more vital manner, the researchers said. This meant smaller numbers of HSCs with greater potential for forming different blood cells, which included larger populations of B and T cells and decreased production of myeloid cells.
The researchers also saw aged HSCs treated with recombinant osteopontin regain their youthful characteristics and capacity to form different blood cell types. Also observed was diminished signaling of Cdc42, a protein previously shown to cause aging in HSCs.
Osteopontin levels are not only low in the bone marrow niche but also in the blood upon aging. As a follow-up to the current study, the researchers are investigating the possibility of using osteopontin replacement therapy in mice to counter the influence of an aging niche directly in the animals. ![]()
Preclinical research suggests osteopontin, a protein made by osteoblasts, plays a role in hematopoietic stem cell (HSC) aging.
Experiments in mice revealed that, with age, there is a reduction in the expression of osteopontin in the bone marrow stroma.
A lack of osteopontin induced young HSCs to “act” older, while treating older HSCs with recombinant osteopontin restored youthful properties.
Hartmut Geiger, PhD, of the University of Ulm in Germany, and his colleagues reported these findings in EMBO.
“We show that the place where HSCs form in the bone marrow loses osteopontin upon aging, but if you give back the missing protein to the blood-forming cells, they suddenly rejuvenate and act younger,” Dr Geiger said.
“Our study points to exciting, novel ways to have a better immune system and possibly less blood cancer upon aging by therapeutically targeting the place where blood stem cells form.”
The researchers conducted a number of experiments to test the formation and vitality of cells in and near the bone marrow microenvironment.
The team looked at the formation of endosteum stroma cells in aging mice and monitored levels of osteopontin and other proteins linked to distinct cells in the bone marrow during the aging process.
The researchers said they observed reduced production of osteoblasts and other stroma cells in the endosteum of older mice. They also saw decreased osteopontin levels in the bone marrow of older animals, which was associated with reduced vigor and function of HSCs.
The team followed up these experiments by transplanting bone marrow cells from older mice (19 to 21 months) into young mice (8 to 10 weeks).
The researchers also transplanted aged HSCs from older mice into younger mice, and the team treated aged HSCs with a recombinant form of the osteopontin protein.
Transplantation into the younger animals caused HSCs to behave in a younger, more vital manner, the researchers said. This meant smaller numbers of HSCs with greater potential for forming different blood cells, which included larger populations of B and T cells and decreased production of myeloid cells.
The researchers also saw aged HSCs treated with recombinant osteopontin regain their youthful characteristics and capacity to form different blood cell types. Also observed was diminished signaling of Cdc42, a protein previously shown to cause aging in HSCs.
Osteopontin levels are not only low in the bone marrow niche but also in the blood upon aging. As a follow-up to the current study, the researchers are investigating the possibility of using osteopontin replacement therapy in mice to counter the influence of an aging niche directly in the animals. ![]()
Cell-free DNA mutational analysis in AITL
SAN FRANCISCO—An exploratory study suggests cell-free DNA from peripheral blood may be a viable alternative to tumor DNA for mutational profiling in angioimmunoblastic T-cell lymphoma (AITL).
Investigators sequenced cell-free DNA and tumor DNA collected from 13 patients with AITL and found that, in 85% of cases, there was concordance between the tumor mutational profile and the cell-free DNA mutational profile.
“The cell-free DNA mutational analysis seems to mirror the mutational analysis of the tumor in the majority of cases,” said Neha Mehta-Shah, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“This may be particularly interesting when we don’t have very much tumor DNA available for sequencing, as occurs frequently in this patient population.”
Dr Mehta-Shah presented these findings at the 9th Annual T-cell Lymphoma Forum.
She said the primary objective of this study was to evaluate whether somatic mutation analysis of cell-free DNA for IDH2 correlates with tumor mutational profiling for IDH2.
The secondary objective was to evaluate whether somatic mutational analysis of cell-free DNA mirrors the mutational profile of the tumor.
So Dr Mehta-Shah and her colleagues sequenced various samples from 14 patients with AITL (4 who were newly diagnosed and 10 with relapsed disease).
The investigators compared cell-free DNA obtained from peripheral blood samples with genomic DNA obtained from primary tumor biopsies and with DNA from peripheral blood mononuclear cells (for germline comparison). One of the 14 patients didn’t have tumor tissue available, so 13 patients were included in the analysis.
The team performed targeted next-generation sequencing using Memorial Sloan Kettering Cancer Center’s IMPACT platform, which sequences 410 genes known to be recurrently mutated in cancer.
The investigators observed concordance between the tumor mutational profile and the cell-free DNA profile in 85% of cases (11/13).
Identical alterations in TET2, RHOA, IDH2, DNMT3A, and ROS1 were detected in cell-free DNA from peripheral blood and tumor genomic DNA, with a similar variant allele frequency.
On the other hand, mutational analysis of cell-free DNA obtained from urine samples from 2 of the patients did not correlate with somatic mutations from tumor DNA.
This research also revealed that some samples had multiple mutations in TET2, which are indicative of subclonal populations.
And sequential samples from 2 patients, collected at the start of salvage therapy and at subsequent relapse, showed the disappearance of mutations in RHOA, TET2, and IDH2. This observation has been attributed to clonal evolution and/or changes in overall disease burden. ![]()
SAN FRANCISCO—An exploratory study suggests cell-free DNA from peripheral blood may be a viable alternative to tumor DNA for mutational profiling in angioimmunoblastic T-cell lymphoma (AITL).
Investigators sequenced cell-free DNA and tumor DNA collected from 13 patients with AITL and found that, in 85% of cases, there was concordance between the tumor mutational profile and the cell-free DNA mutational profile.
“The cell-free DNA mutational analysis seems to mirror the mutational analysis of the tumor in the majority of cases,” said Neha Mehta-Shah, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“This may be particularly interesting when we don’t have very much tumor DNA available for sequencing, as occurs frequently in this patient population.”
Dr Mehta-Shah presented these findings at the 9th Annual T-cell Lymphoma Forum.
She said the primary objective of this study was to evaluate whether somatic mutation analysis of cell-free DNA for IDH2 correlates with tumor mutational profiling for IDH2.
The secondary objective was to evaluate whether somatic mutational analysis of cell-free DNA mirrors the mutational profile of the tumor.
So Dr Mehta-Shah and her colleagues sequenced various samples from 14 patients with AITL (4 who were newly diagnosed and 10 with relapsed disease).
The investigators compared cell-free DNA obtained from peripheral blood samples with genomic DNA obtained from primary tumor biopsies and with DNA from peripheral blood mononuclear cells (for germline comparison). One of the 14 patients didn’t have tumor tissue available, so 13 patients were included in the analysis.
The team performed targeted next-generation sequencing using Memorial Sloan Kettering Cancer Center’s IMPACT platform, which sequences 410 genes known to be recurrently mutated in cancer.
The investigators observed concordance between the tumor mutational profile and the cell-free DNA profile in 85% of cases (11/13).
Identical alterations in TET2, RHOA, IDH2, DNMT3A, and ROS1 were detected in cell-free DNA from peripheral blood and tumor genomic DNA, with a similar variant allele frequency.
On the other hand, mutational analysis of cell-free DNA obtained from urine samples from 2 of the patients did not correlate with somatic mutations from tumor DNA.
This research also revealed that some samples had multiple mutations in TET2, which are indicative of subclonal populations.
And sequential samples from 2 patients, collected at the start of salvage therapy and at subsequent relapse, showed the disappearance of mutations in RHOA, TET2, and IDH2. This observation has been attributed to clonal evolution and/or changes in overall disease burden. ![]()
SAN FRANCISCO—An exploratory study suggests cell-free DNA from peripheral blood may be a viable alternative to tumor DNA for mutational profiling in angioimmunoblastic T-cell lymphoma (AITL).
Investigators sequenced cell-free DNA and tumor DNA collected from 13 patients with AITL and found that, in 85% of cases, there was concordance between the tumor mutational profile and the cell-free DNA mutational profile.
“The cell-free DNA mutational analysis seems to mirror the mutational analysis of the tumor in the majority of cases,” said Neha Mehta-Shah, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“This may be particularly interesting when we don’t have very much tumor DNA available for sequencing, as occurs frequently in this patient population.”
Dr Mehta-Shah presented these findings at the 9th Annual T-cell Lymphoma Forum.
She said the primary objective of this study was to evaluate whether somatic mutation analysis of cell-free DNA for IDH2 correlates with tumor mutational profiling for IDH2.
The secondary objective was to evaluate whether somatic mutational analysis of cell-free DNA mirrors the mutational profile of the tumor.
So Dr Mehta-Shah and her colleagues sequenced various samples from 14 patients with AITL (4 who were newly diagnosed and 10 with relapsed disease).
The investigators compared cell-free DNA obtained from peripheral blood samples with genomic DNA obtained from primary tumor biopsies and with DNA from peripheral blood mononuclear cells (for germline comparison). One of the 14 patients didn’t have tumor tissue available, so 13 patients were included in the analysis.
The team performed targeted next-generation sequencing using Memorial Sloan Kettering Cancer Center’s IMPACT platform, which sequences 410 genes known to be recurrently mutated in cancer.
The investigators observed concordance between the tumor mutational profile and the cell-free DNA profile in 85% of cases (11/13).
Identical alterations in TET2, RHOA, IDH2, DNMT3A, and ROS1 were detected in cell-free DNA from peripheral blood and tumor genomic DNA, with a similar variant allele frequency.
On the other hand, mutational analysis of cell-free DNA obtained from urine samples from 2 of the patients did not correlate with somatic mutations from tumor DNA.
This research also revealed that some samples had multiple mutations in TET2, which are indicative of subclonal populations.
And sequential samples from 2 patients, collected at the start of salvage therapy and at subsequent relapse, showed the disappearance of mutations in RHOA, TET2, and IDH2. This observation has been attributed to clonal evolution and/or changes in overall disease burden. ![]()
MSC product granted fast track designation
The US Food and Drug Administration (FDA) has granted fast track designation to a mesenchymal stem cell (MSC) product, MSC-100-IV, as a treatment for children with steroid-refractory acute graft-vs-host disease (aGVHD).
MSC-100-IV consists of human MSCs derived from donor bone marrow and expanded in culture.
Fast track designation has the potential to shorten the time to FDA approval for MSC-100-IV through priority review, which reduces the FDA review process from 10 months to 6 months.
The designation also allows for a rolling review process, whereby completed sections of the Biologics License Application can be submitted for FDA review as they become available, instead of waiting for all sections to be completed.
In addition, fast track designation provides product developers with opportunities for more frequent meetings and written communications with the FDA.
MSC-100-IV is being developed by Mesoblast Limited in partnership with Mallinckrodt Pharmaceuticals.
Trial results
The application for fast track designation for MSC-100-IV was supported by a trial of 241 pediatric patients with steroid-refractory aGVHD. Results from this trial were presented at the 2016 BMT Tandem Meetings.
Patients initially received 2 million MSCs/kg twice a week for 4 weeks, at least 3 days apart. If they achieved a partial or mixed response (improvement in one organ with deterioration in another) at the day-28 assessment, patients then received 2 million MSCs/kg once a week for 4 weeks.
The patients received a total of 2434 infusions—a median of 11 (range, 1-24)—and had a median treatment duration of 46 days (range, 1-186).
Fifty-seven percent of patients (n=138) had at least 1 serious adverse event. About 5% (n=11) were considered treatment-related, and 1.7% (n=4) led to study discontinuation. There was 1 infusion reaction.
The overall response rate at day 28 was 65%, and the complete response rate was 14%. Responses were observed for all aGVHD grades and did not differ by baseline organ involvement.
Day 100 survival was significantly better in children who achieved a response at day 28—82%, compared to 39% for non-responders (P<0.0001).
In November 2016, Mesoblast reported success in an ongoing, phase 3 registration trial of MSC-100-IV in 60 children with steroid-refractory aGVHD.
The company said the trial was successful in a pre-specified interim futility analysis using the primary endpoint of day-28 overall response. Enrollment in this trial is expected to be complete in mid-2017. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to a mesenchymal stem cell (MSC) product, MSC-100-IV, as a treatment for children with steroid-refractory acute graft-vs-host disease (aGVHD).
MSC-100-IV consists of human MSCs derived from donor bone marrow and expanded in culture.
Fast track designation has the potential to shorten the time to FDA approval for MSC-100-IV through priority review, which reduces the FDA review process from 10 months to 6 months.
The designation also allows for a rolling review process, whereby completed sections of the Biologics License Application can be submitted for FDA review as they become available, instead of waiting for all sections to be completed.
In addition, fast track designation provides product developers with opportunities for more frequent meetings and written communications with the FDA.
MSC-100-IV is being developed by Mesoblast Limited in partnership with Mallinckrodt Pharmaceuticals.
Trial results
The application for fast track designation for MSC-100-IV was supported by a trial of 241 pediatric patients with steroid-refractory aGVHD. Results from this trial were presented at the 2016 BMT Tandem Meetings.
Patients initially received 2 million MSCs/kg twice a week for 4 weeks, at least 3 days apart. If they achieved a partial or mixed response (improvement in one organ with deterioration in another) at the day-28 assessment, patients then received 2 million MSCs/kg once a week for 4 weeks.
The patients received a total of 2434 infusions—a median of 11 (range, 1-24)—and had a median treatment duration of 46 days (range, 1-186).
Fifty-seven percent of patients (n=138) had at least 1 serious adverse event. About 5% (n=11) were considered treatment-related, and 1.7% (n=4) led to study discontinuation. There was 1 infusion reaction.
The overall response rate at day 28 was 65%, and the complete response rate was 14%. Responses were observed for all aGVHD grades and did not differ by baseline organ involvement.
Day 100 survival was significantly better in children who achieved a response at day 28—82%, compared to 39% for non-responders (P<0.0001).
In November 2016, Mesoblast reported success in an ongoing, phase 3 registration trial of MSC-100-IV in 60 children with steroid-refractory aGVHD.
The company said the trial was successful in a pre-specified interim futility analysis using the primary endpoint of day-28 overall response. Enrollment in this trial is expected to be complete in mid-2017. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to a mesenchymal stem cell (MSC) product, MSC-100-IV, as a treatment for children with steroid-refractory acute graft-vs-host disease (aGVHD).
MSC-100-IV consists of human MSCs derived from donor bone marrow and expanded in culture.
Fast track designation has the potential to shorten the time to FDA approval for MSC-100-IV through priority review, which reduces the FDA review process from 10 months to 6 months.
The designation also allows for a rolling review process, whereby completed sections of the Biologics License Application can be submitted for FDA review as they become available, instead of waiting for all sections to be completed.
In addition, fast track designation provides product developers with opportunities for more frequent meetings and written communications with the FDA.
MSC-100-IV is being developed by Mesoblast Limited in partnership with Mallinckrodt Pharmaceuticals.
Trial results
The application for fast track designation for MSC-100-IV was supported by a trial of 241 pediatric patients with steroid-refractory aGVHD. Results from this trial were presented at the 2016 BMT Tandem Meetings.
Patients initially received 2 million MSCs/kg twice a week for 4 weeks, at least 3 days apart. If they achieved a partial or mixed response (improvement in one organ with deterioration in another) at the day-28 assessment, patients then received 2 million MSCs/kg once a week for 4 weeks.
The patients received a total of 2434 infusions—a median of 11 (range, 1-24)—and had a median treatment duration of 46 days (range, 1-186).
Fifty-seven percent of patients (n=138) had at least 1 serious adverse event. About 5% (n=11) were considered treatment-related, and 1.7% (n=4) led to study discontinuation. There was 1 infusion reaction.
The overall response rate at day 28 was 65%, and the complete response rate was 14%. Responses were observed for all aGVHD grades and did not differ by baseline organ involvement.
Day 100 survival was significantly better in children who achieved a response at day 28—82%, compared to 39% for non-responders (P<0.0001).
In November 2016, Mesoblast reported success in an ongoing, phase 3 registration trial of MSC-100-IV in 60 children with steroid-refractory aGVHD.
The company said the trial was successful in a pre-specified interim futility analysis using the primary endpoint of day-28 overall response. Enrollment in this trial is expected to be complete in mid-2017. ![]()
Survey: Patients largely unaware of docs’ industry ties
A survey of nearly 2000 people suggests many Americans may not know if their physician receives industry payments.
A majority of the individuals surveyed were treated by a doctor who received some form of industry payment in the last year, but few of the patients were aware of these payments.
In fact, more than half of the patients did not know that accepting industry payments is something physicians may do.
“The findings suggest that although physicians who accept industry payments are in the minority, they are caring for a very substantial portion of America’s adult patient population,” said Genevieve Pham-Kanter, PhD, of Drexel University’s Dornsife School of Public Health in Philadelphia, Pennsylvania.
She and her colleagues reported these findings in the Journal of General Internal Medicine.
Since 2013, the Sunshine Act, part of the Patient Protection and Affordable Care Act, has required pharmaceutical and medical device manufacturers to report gifts and payments they make to healthcare providers. This information is publicly available on the Centers for Medicare and Medicaid Services’ Open Payments website.
Dr Pham-Kanter and her colleagues conducted their survey shortly before the first release of the Open Payments data in September 2014. However, payment data were already publicly available in certain states, nationwide via the Pro Publica website, and through disclosures made by pharmaceutical and medical device firms themselves (who had been required to release payment information as part of legal settlements or did so voluntarily).
Survey results
The researchers conducted their online survey in 3542 adults. Respondents were asked whether they were aware of industry payments and to name the physicians they had seen most frequently in the previous year.
Physician names were then linked to the Open Payment data to ascertain how often patients saw doctors who accepted industry payments.
There were 1987 respondents who could be matched to a specific physician. Sixty-five percent of these individuals had visited a physician who accepted an industry payment in the last 12 months, but only 5% of the respondents actually knew if their doctors received industry payments.
Forty-five percent of respondents said they knew about the practice of doctors receiving industry payments, and 12% said information about such payments was publicly available.
“These findings tell us that if you thought that your doctor was not receiving any money from industry, you’re most likely mistaken,” Dr Pham-Kanter said. “Patients should be aware of the incentives that their physicians face that may lead them to not always act in their patients’ best interest.”
In Open Payments, all physicians averaged $193 in yearly payments and gifts. But when measuring only the doctors visited by participants in the survey, the median payment amount over the last year was $510, more than 2.5 times the US average.
“We may be lulled into thinking this isn’t a big deal because the average payment amount across all doctors is low,” Dr Pham-Kanter said. “But that obscures the fact that most people are seeing doctors who receive the largest payments.”
“Drug companies have long known that even small gifts to physicians can be influential,” added study author Michelle Mello, JD, PhD, of Stanford University School of Medicine and Stanford Law School in California. “And research validates the notion that they tend to induce feelings of reciprocity.” ![]()
A survey of nearly 2000 people suggests many Americans may not know if their physician receives industry payments.
A majority of the individuals surveyed were treated by a doctor who received some form of industry payment in the last year, but few of the patients were aware of these payments.
In fact, more than half of the patients did not know that accepting industry payments is something physicians may do.
“The findings suggest that although physicians who accept industry payments are in the minority, they are caring for a very substantial portion of America’s adult patient population,” said Genevieve Pham-Kanter, PhD, of Drexel University’s Dornsife School of Public Health in Philadelphia, Pennsylvania.
She and her colleagues reported these findings in the Journal of General Internal Medicine.
Since 2013, the Sunshine Act, part of the Patient Protection and Affordable Care Act, has required pharmaceutical and medical device manufacturers to report gifts and payments they make to healthcare providers. This information is publicly available on the Centers for Medicare and Medicaid Services’ Open Payments website.
Dr Pham-Kanter and her colleagues conducted their survey shortly before the first release of the Open Payments data in September 2014. However, payment data were already publicly available in certain states, nationwide via the Pro Publica website, and through disclosures made by pharmaceutical and medical device firms themselves (who had been required to release payment information as part of legal settlements or did so voluntarily).
Survey results
The researchers conducted their online survey in 3542 adults. Respondents were asked whether they were aware of industry payments and to name the physicians they had seen most frequently in the previous year.
Physician names were then linked to the Open Payment data to ascertain how often patients saw doctors who accepted industry payments.
There were 1987 respondents who could be matched to a specific physician. Sixty-five percent of these individuals had visited a physician who accepted an industry payment in the last 12 months, but only 5% of the respondents actually knew if their doctors received industry payments.
Forty-five percent of respondents said they knew about the practice of doctors receiving industry payments, and 12% said information about such payments was publicly available.
“These findings tell us that if you thought that your doctor was not receiving any money from industry, you’re most likely mistaken,” Dr Pham-Kanter said. “Patients should be aware of the incentives that their physicians face that may lead them to not always act in their patients’ best interest.”
In Open Payments, all physicians averaged $193 in yearly payments and gifts. But when measuring only the doctors visited by participants in the survey, the median payment amount over the last year was $510, more than 2.5 times the US average.
“We may be lulled into thinking this isn’t a big deal because the average payment amount across all doctors is low,” Dr Pham-Kanter said. “But that obscures the fact that most people are seeing doctors who receive the largest payments.”
“Drug companies have long known that even small gifts to physicians can be influential,” added study author Michelle Mello, JD, PhD, of Stanford University School of Medicine and Stanford Law School in California. “And research validates the notion that they tend to induce feelings of reciprocity.” ![]()
A survey of nearly 2000 people suggests many Americans may not know if their physician receives industry payments.
A majority of the individuals surveyed were treated by a doctor who received some form of industry payment in the last year, but few of the patients were aware of these payments.
In fact, more than half of the patients did not know that accepting industry payments is something physicians may do.
“The findings suggest that although physicians who accept industry payments are in the minority, they are caring for a very substantial portion of America’s adult patient population,” said Genevieve Pham-Kanter, PhD, of Drexel University’s Dornsife School of Public Health in Philadelphia, Pennsylvania.
She and her colleagues reported these findings in the Journal of General Internal Medicine.
Since 2013, the Sunshine Act, part of the Patient Protection and Affordable Care Act, has required pharmaceutical and medical device manufacturers to report gifts and payments they make to healthcare providers. This information is publicly available on the Centers for Medicare and Medicaid Services’ Open Payments website.
Dr Pham-Kanter and her colleagues conducted their survey shortly before the first release of the Open Payments data in September 2014. However, payment data were already publicly available in certain states, nationwide via the Pro Publica website, and through disclosures made by pharmaceutical and medical device firms themselves (who had been required to release payment information as part of legal settlements or did so voluntarily).
Survey results
The researchers conducted their online survey in 3542 adults. Respondents were asked whether they were aware of industry payments and to name the physicians they had seen most frequently in the previous year.
Physician names were then linked to the Open Payment data to ascertain how often patients saw doctors who accepted industry payments.
There were 1987 respondents who could be matched to a specific physician. Sixty-five percent of these individuals had visited a physician who accepted an industry payment in the last 12 months, but only 5% of the respondents actually knew if their doctors received industry payments.
Forty-five percent of respondents said they knew about the practice of doctors receiving industry payments, and 12% said information about such payments was publicly available.
“These findings tell us that if you thought that your doctor was not receiving any money from industry, you’re most likely mistaken,” Dr Pham-Kanter said. “Patients should be aware of the incentives that their physicians face that may lead them to not always act in their patients’ best interest.”
In Open Payments, all physicians averaged $193 in yearly payments and gifts. But when measuring only the doctors visited by participants in the survey, the median payment amount over the last year was $510, more than 2.5 times the US average.
“We may be lulled into thinking this isn’t a big deal because the average payment amount across all doctors is low,” Dr Pham-Kanter said. “But that obscures the fact that most people are seeing doctors who receive the largest payments.”
“Drug companies have long known that even small gifts to physicians can be influential,” added study author Michelle Mello, JD, PhD, of Stanford University School of Medicine and Stanford Law School in California. “And research validates the notion that they tend to induce feelings of reciprocity.” ![]()
Genetic variants linked to HSCT outcomes in ALL
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.” ![]()
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.” ![]()
ORLANDO, FL—Results of a genome-wide association study suggest that several genetic variants are associated with outcomes of allogeneic hematopoietic stem cell transplant (HSCT) in patients with acute lymphoblastic leukemia (ALL).
Investigators identified several single-nucleotide polymorphisms (SNPs) in ALL patients and their unrelated donors that were associated with disease-related death or progression-free survival (PFS) within 1 year of HSCT.
“We believe that these findings will lead to a better understanding of the biology of this disease,” said investigator Theresa Hahn, PhD, of Roswell Park Cancer Institute in Buffalo, New York.
“Additionally, we expect that this work will eventually help clinical teams to identify unrelated donors with genotypes that yield better survival in transplant patients and enhance the chances for successful blood and marrow transplants.”
Dr Hahn presented this work as a “Best Abstract” at the 2017 BMT Tandem Meetings (abstract 1).
For this study, she and her colleagues analyzed data on patients treated at more than 150 US transplant centers between 2000 and 2011. The investigators evaluated data on more than 3000 patients with acute leukemias or myelodysplastic syndromes, but Dr Hahn only presented findings in the ALL patients and their donors.
The patients and donors were divided into 2 cohorts. Cohort 1 included 483 ALL patients who underwent HSCT from 2000 to 2008 and 466 unrelated donors who were a 10/10 HLA match for the patients.
Cohort 2 included 94 ALL patients who received a transplant from a 10/10 HLA-matched donor between 2009 and 2011 or from an 8/8 HLA-matched donor between 2000 and 2011. There were 92 donors in this cohort.
The investigators sequenced blood samples from the recipients and donors to identify SNPs. The SNPs were then measured for association with disease-related death and PFS using Cox proportional hazards models adjusted for recipient age, disease status at HSCT (early, intermediate, or advanced), graft source (blood or marrow), and year of transplant.
SNPs in donors
The top 2 SNPs in donors that were associated with a significant increase in disease-related death were:
- rs79503405 in LRP2 on chromosome 2.
- rs77618918 in ASIC2 on chromosome 17.
Dr Hahn noted that rs79503405 is in complete linkage disequilibrium (r2=1.0) with a genotyped missense variant (rs17848149) and a synonymous coding variant (rs35114151) in LRP2.
She also pointed out that the other top SNP (rs77618918) associated with disease-related death is not in linkage disequilibrium with other SNPs of functional importance, so the significance of this SNP is unknown.
There were no SNPs in donors that were significantly associated with PFS.
SNPs in recipients
In HSCT recipients, there were 3 linked variants in NRG1 on chromosome 8 (rs79853417, rs6990973, and rs145488394) that were significantly associated with disease-related death.
Another SNP (rs60640657) on chromosome 2 (CTNNA3/LOC101928961/LRRTM3) was also significantly associated with ALL-related death.
In addition, Dr Hahn and her colleagues found that 1 region in recipient genomes contains multiple variants (rs113263921 and others) associated with PFS. The SNPs are located on chromosome 3 in MLH1 and TRANK1.
“The donor and recipient genetic variants contributed independently to death due to ALL,” Dr Hahn said in closing. “Genetic variants for PFS do not overlap with death due to ALL, and this is probably due to the inclusion of both non-fatal disease progression as well as transplant-related mortality in the definition of PFS.”
“Constitutional genetic variants in recipients and donors increase the risk of death due to ALL, and they warrant further study into the impact of these genes on disease and transplant-related biology.”
Combo prolongs OS in relapsed/refractory MM
NEW DEHLI—A 2-drug combination previously shown to prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM) can prolong overall survival (OS) as well, according to researchers.
Updated results of the phase 3 ENDEAVOR trial showed that patients who received treatment with carfilzomib and dexamethasone had a 7.6-month benefit in median OS when compared to patients who received bortezomib and dexamethasone.
Previous results from this trial showed a 9.3-month benefit in median PFS with carfilzomib and dexamethasone.
“Based on these data, we now know that [carfilzomib] not only significantly extended progression-free survival compared to [bortezomib] but also overall survival, making it a clinically meaningful advance in the treatment of relapsed or refractory multiple myeloma,” said Meletios A. Dimopoulos, MD, of the University of Athens in Greece.
Dr Dimopoulos presented OS results from ENDEAVOR at the 16th International Myeloma Workshop. The trial was funded by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen.
ENDEAVOR included 929 MM patients who had received 1 to 3 prior treatment regimens. The patients were randomized to receive carfilzomib and low-dose dexamethasone (n=464) or bortezomib and low-dose dexamethasone (n=465) until disease progression.
Baseline characteristics were similar between the treatment arms.
Detailed patient and treatment characteristics, as well as response and PFS data, have been previously reported.
OS and safety
The median OS was 47.6 months in the carfilzomib arm and 40.0 months in the bortezomib arm. All-cause mortality was significantly lower with the carfilzomib combination than the bortezomib combination (hazard ratio [HR]=0.791, 1-sided P=0.0100).
Researchers said there was an OS benefit with the carfilzomib combination whether or not patients received prior treatment with bortezomib and regardless of patients’ age, ECOG performance status at baseline, cytogenetic risk group, or the number of previous therapies they received.
The HR was 0.75 (carfilzomib vs bortezomib) for patients with no prior bortezomib and 0.84 for patients who received prior bortezomib. The HR was 0.85 for patients younger than 65, 0.71 for those ages 65 to 74, and 0.84 for patients age 75 and older.
The HR was 0.81 for patients with an ECOG status of 0, 0.80 for those with a status of 1, and 0.50 for those with a status of 2. The HR was 0.83 for patients with high-risk cytogenetics and 0.85 for those with standard-risk cytogenetics.
The HR was 0.83 for patients with 1 prior line of therapy and 0.76 for those with 2 to 3 prior lines of therapy.
The researchers said safety results in this analysis were comparable with previously reported results. The incidence of grade 3 or higher adverse events was 81.4% in the carfilzomib arm and 71.1% in the bortezomib arm.
The most common adverse events of any grade (in the carfilzomib and bortezomib arms, respectively) were anemia (42.5% and 28.3%), diarrhea (36.3% and 40.6%), pyrexia (32.4% and 15.4%), dyspnea (32.2% and 13.6%), fatigue (32.2% and 30.7%), and hypertension (32.2% and 9.9%).
NEW DEHLI—A 2-drug combination previously shown to prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM) can prolong overall survival (OS) as well, according to researchers.
Updated results of the phase 3 ENDEAVOR trial showed that patients who received treatment with carfilzomib and dexamethasone had a 7.6-month benefit in median OS when compared to patients who received bortezomib and dexamethasone.
Previous results from this trial showed a 9.3-month benefit in median PFS with carfilzomib and dexamethasone.
“Based on these data, we now know that [carfilzomib] not only significantly extended progression-free survival compared to [bortezomib] but also overall survival, making it a clinically meaningful advance in the treatment of relapsed or refractory multiple myeloma,” said Meletios A. Dimopoulos, MD, of the University of Athens in Greece.
Dr Dimopoulos presented OS results from ENDEAVOR at the 16th International Myeloma Workshop. The trial was funded by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen.
ENDEAVOR included 929 MM patients who had received 1 to 3 prior treatment regimens. The patients were randomized to receive carfilzomib and low-dose dexamethasone (n=464) or bortezomib and low-dose dexamethasone (n=465) until disease progression.
Baseline characteristics were similar between the treatment arms.
Detailed patient and treatment characteristics, as well as response and PFS data, have been previously reported.
OS and safety
The median OS was 47.6 months in the carfilzomib arm and 40.0 months in the bortezomib arm. All-cause mortality was significantly lower with the carfilzomib combination than the bortezomib combination (hazard ratio [HR]=0.791, 1-sided P=0.0100).
Researchers said there was an OS benefit with the carfilzomib combination whether or not patients received prior treatment with bortezomib and regardless of patients’ age, ECOG performance status at baseline, cytogenetic risk group, or the number of previous therapies they received.
The HR was 0.75 (carfilzomib vs bortezomib) for patients with no prior bortezomib and 0.84 for patients who received prior bortezomib. The HR was 0.85 for patients younger than 65, 0.71 for those ages 65 to 74, and 0.84 for patients age 75 and older.
The HR was 0.81 for patients with an ECOG status of 0, 0.80 for those with a status of 1, and 0.50 for those with a status of 2. The HR was 0.83 for patients with high-risk cytogenetics and 0.85 for those with standard-risk cytogenetics.
The HR was 0.83 for patients with 1 prior line of therapy and 0.76 for those with 2 to 3 prior lines of therapy.
The researchers said safety results in this analysis were comparable with previously reported results. The incidence of grade 3 or higher adverse events was 81.4% in the carfilzomib arm and 71.1% in the bortezomib arm.
The most common adverse events of any grade (in the carfilzomib and bortezomib arms, respectively) were anemia (42.5% and 28.3%), diarrhea (36.3% and 40.6%), pyrexia (32.4% and 15.4%), dyspnea (32.2% and 13.6%), fatigue (32.2% and 30.7%), and hypertension (32.2% and 9.9%).
NEW DEHLI—A 2-drug combination previously shown to prolong progression-free survival (PFS) in patients with relapsed/refractory multiple myeloma (MM) can prolong overall survival (OS) as well, according to researchers.
Updated results of the phase 3 ENDEAVOR trial showed that patients who received treatment with carfilzomib and dexamethasone had a 7.6-month benefit in median OS when compared to patients who received bortezomib and dexamethasone.
Previous results from this trial showed a 9.3-month benefit in median PFS with carfilzomib and dexamethasone.
“Based on these data, we now know that [carfilzomib] not only significantly extended progression-free survival compared to [bortezomib] but also overall survival, making it a clinically meaningful advance in the treatment of relapsed or refractory multiple myeloma,” said Meletios A. Dimopoulos, MD, of the University of Athens in Greece.
Dr Dimopoulos presented OS results from ENDEAVOR at the 16th International Myeloma Workshop. The trial was funded by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen.
ENDEAVOR included 929 MM patients who had received 1 to 3 prior treatment regimens. The patients were randomized to receive carfilzomib and low-dose dexamethasone (n=464) or bortezomib and low-dose dexamethasone (n=465) until disease progression.
Baseline characteristics were similar between the treatment arms.
Detailed patient and treatment characteristics, as well as response and PFS data, have been previously reported.
OS and safety
The median OS was 47.6 months in the carfilzomib arm and 40.0 months in the bortezomib arm. All-cause mortality was significantly lower with the carfilzomib combination than the bortezomib combination (hazard ratio [HR]=0.791, 1-sided P=0.0100).
Researchers said there was an OS benefit with the carfilzomib combination whether or not patients received prior treatment with bortezomib and regardless of patients’ age, ECOG performance status at baseline, cytogenetic risk group, or the number of previous therapies they received.
The HR was 0.75 (carfilzomib vs bortezomib) for patients with no prior bortezomib and 0.84 for patients who received prior bortezomib. The HR was 0.85 for patients younger than 65, 0.71 for those ages 65 to 74, and 0.84 for patients age 75 and older.
The HR was 0.81 for patients with an ECOG status of 0, 0.80 for those with a status of 1, and 0.50 for those with a status of 2. The HR was 0.83 for patients with high-risk cytogenetics and 0.85 for those with standard-risk cytogenetics.
The HR was 0.83 for patients with 1 prior line of therapy and 0.76 for those with 2 to 3 prior lines of therapy.
The researchers said safety results in this analysis were comparable with previously reported results. The incidence of grade 3 or higher adverse events was 81.4% in the carfilzomib arm and 71.1% in the bortezomib arm.
The most common adverse events of any grade (in the carfilzomib and bortezomib arms, respectively) were anemia (42.5% and 28.3%), diarrhea (36.3% and 40.6%), pyrexia (32.4% and 15.4%), dyspnea (32.2% and 13.6%), fatigue (32.2% and 30.7%), and hypertension (32.2% and 9.9%).
Chlormethine gel approved to treat mycosis fungoides
The European Commission has granted marketing authorization for chlormethine gel (Ledaga®) as a treatment for adults with mycosis fungoides (MF), but the product is not expected to be available until next year.
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Hybrid medicines have a different strength, are administered differently, or have a different indication from the reference medicine.
Ledaga contains the same active substance as Caryolysine—chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells—but Ledaga is a gel intended for cutaneous use.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to fulfill a list of post-approval measures for the product proposed by the European Medicines Agency’s Committee for Medicinal Products for Human Use.
Subject to fulfilling the agreed commitments and achieving market access in various countries, a potential first European launch of Ledaga is not expected before January 2018. When it is launched, Ledaga will be available as a 160 μg/g gel.
Phase 2 study
The authorization of hybrid medicines depends partly on the results of tests on the reference medicine and partly on new data from clinical trials.
The marketing authorization for Ledaga is based, in part, on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 MF patients who were randomized 1:1 to receive topical treatment with 0.02% chlormethine gel (Ledaga) or compounded control—0.02% chlormethine compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, skin pain), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment.
The European Commission has granted marketing authorization for chlormethine gel (Ledaga®) as a treatment for adults with mycosis fungoides (MF), but the product is not expected to be available until next year.
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Hybrid medicines have a different strength, are administered differently, or have a different indication from the reference medicine.
Ledaga contains the same active substance as Caryolysine—chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells—but Ledaga is a gel intended for cutaneous use.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to fulfill a list of post-approval measures for the product proposed by the European Medicines Agency’s Committee for Medicinal Products for Human Use.
Subject to fulfilling the agreed commitments and achieving market access in various countries, a potential first European launch of Ledaga is not expected before January 2018. When it is launched, Ledaga will be available as a 160 μg/g gel.
Phase 2 study
The authorization of hybrid medicines depends partly on the results of tests on the reference medicine and partly on new data from clinical trials.
The marketing authorization for Ledaga is based, in part, on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 MF patients who were randomized 1:1 to receive topical treatment with 0.02% chlormethine gel (Ledaga) or compounded control—0.02% chlormethine compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, skin pain), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment.
The European Commission has granted marketing authorization for chlormethine gel (Ledaga®) as a treatment for adults with mycosis fungoides (MF), but the product is not expected to be available until next year.
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Hybrid medicines have a different strength, are administered differently, or have a different indication from the reference medicine.
Ledaga contains the same active substance as Caryolysine—chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells—but Ledaga is a gel intended for cutaneous use.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to fulfill a list of post-approval measures for the product proposed by the European Medicines Agency’s Committee for Medicinal Products for Human Use.
Subject to fulfilling the agreed commitments and achieving market access in various countries, a potential first European launch of Ledaga is not expected before January 2018. When it is launched, Ledaga will be available as a 160 μg/g gel.
Phase 2 study
The authorization of hybrid medicines depends partly on the results of tests on the reference medicine and partly on new data from clinical trials.
The marketing authorization for Ledaga is based, in part, on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 MF patients who were randomized 1:1 to receive topical treatment with 0.02% chlormethine gel (Ledaga) or compounded control—0.02% chlormethine compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, skin pain), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment.
Pathogenesis of breast-implant-associated ALCL
SAN FRANCISCO—A small study suggests an abnormal immune response characterized by the production of interleukin-13 (IL-13) underlies the pathogenesis of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The immune response appears to be directed toward bacterial antigens on the surface of the breast implants.
Marshall E. Kadin, MD, of Roger Williams Medical Center in Providence, Rhode Island, presented these findings at the 9th Annual T-cell Lymphoma Forum.
Dr Kadin noted that BIA-ALCL is a rare type of CD30+ T-cell ALCL that has been reported in more than 200 women worldwide.
Although a cause-and-effect relationship between breast implants and BIA-ALCL has been suggested, the underlying pathogenesis of this malignancy is unclear.
A bacterial biofilm containing gram-negative bacilli has been detected in breast implants from patients with BIA-ALCL.
Therefore, Dr Kadin and his colleagues hypothesized that an immune response toward the bacterial antigens may mediate the pathogenesis of BIA-ALCL.
The researchers studied 13 clinical samples of breast implant capsules and regional lymph nodes from 4 patients with BIA-ALCL, 7 patients with systemic ALCL, and 1 patient with peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS).
Immunohistochemistry was used to determine the presence of IL-13, IL-4, GATA3, and immunoglobulin E (IgE) in these samples.
All clinical samples of anaplastic cells from breast implant capsules tested positive for the presence of IL-13 (13/13). GATA3 was expressed in most anaplastic cell samples (12/13), and IL-4 expression was found in some anaplastic cell samples (6/13). IL-13 and GATA3 expression were observed in some intra-capsular small lymphocytes.
While IL-13 was also detected in BIA-ALCL cell lines, it was not found in 4 of the 7 systemic ALCL cases or the PTCL-NOS case.
Dr Kadin said the lack of IL-13 receptor expression in BIA-ALCL cell lines suggests that IL-13 is not an autocrine growth factor for BIA-ALCL, and its expression is most likely associated with an allergic immune response.
IL-13 is known to induce immunoglobulin class switching in plasma cells to produce IgE. H&E and Giemsa staining of the BIA-ALCL tumor tissue and involved regional lymph nodes revealed IgE and eosinophils on the surface of mast cells and follicular dendritic cells.
Taken together, these data point to an allergic reaction in breast implant capsules of BIA-ALCL.
Dr Kadin was hopeful that these findings could be extrapolated to prevent BIA-ALCL by identifying individuals at higher risk for developing the disease.
The next step for this research is to decipher the role of bacterial antigens in mediating the immune response and whether women who develop BIA-ALCL have a significant increase in other atopic conditions.
SAN FRANCISCO—A small study suggests an abnormal immune response characterized by the production of interleukin-13 (IL-13) underlies the pathogenesis of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The immune response appears to be directed toward bacterial antigens on the surface of the breast implants.
Marshall E. Kadin, MD, of Roger Williams Medical Center in Providence, Rhode Island, presented these findings at the 9th Annual T-cell Lymphoma Forum.
Dr Kadin noted that BIA-ALCL is a rare type of CD30+ T-cell ALCL that has been reported in more than 200 women worldwide.
Although a cause-and-effect relationship between breast implants and BIA-ALCL has been suggested, the underlying pathogenesis of this malignancy is unclear.
A bacterial biofilm containing gram-negative bacilli has been detected in breast implants from patients with BIA-ALCL.
Therefore, Dr Kadin and his colleagues hypothesized that an immune response toward the bacterial antigens may mediate the pathogenesis of BIA-ALCL.
The researchers studied 13 clinical samples of breast implant capsules and regional lymph nodes from 4 patients with BIA-ALCL, 7 patients with systemic ALCL, and 1 patient with peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS).
Immunohistochemistry was used to determine the presence of IL-13, IL-4, GATA3, and immunoglobulin E (IgE) in these samples.
All clinical samples of anaplastic cells from breast implant capsules tested positive for the presence of IL-13 (13/13). GATA3 was expressed in most anaplastic cell samples (12/13), and IL-4 expression was found in some anaplastic cell samples (6/13). IL-13 and GATA3 expression were observed in some intra-capsular small lymphocytes.
While IL-13 was also detected in BIA-ALCL cell lines, it was not found in 4 of the 7 systemic ALCL cases or the PTCL-NOS case.
Dr Kadin said the lack of IL-13 receptor expression in BIA-ALCL cell lines suggests that IL-13 is not an autocrine growth factor for BIA-ALCL, and its expression is most likely associated with an allergic immune response.
IL-13 is known to induce immunoglobulin class switching in plasma cells to produce IgE. H&E and Giemsa staining of the BIA-ALCL tumor tissue and involved regional lymph nodes revealed IgE and eosinophils on the surface of mast cells and follicular dendritic cells.
Taken together, these data point to an allergic reaction in breast implant capsules of BIA-ALCL.
Dr Kadin was hopeful that these findings could be extrapolated to prevent BIA-ALCL by identifying individuals at higher risk for developing the disease.
The next step for this research is to decipher the role of bacterial antigens in mediating the immune response and whether women who develop BIA-ALCL have a significant increase in other atopic conditions.
SAN FRANCISCO—A small study suggests an abnormal immune response characterized by the production of interleukin-13 (IL-13) underlies the pathogenesis of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The immune response appears to be directed toward bacterial antigens on the surface of the breast implants.
Marshall E. Kadin, MD, of Roger Williams Medical Center in Providence, Rhode Island, presented these findings at the 9th Annual T-cell Lymphoma Forum.
Dr Kadin noted that BIA-ALCL is a rare type of CD30+ T-cell ALCL that has been reported in more than 200 women worldwide.
Although a cause-and-effect relationship between breast implants and BIA-ALCL has been suggested, the underlying pathogenesis of this malignancy is unclear.
A bacterial biofilm containing gram-negative bacilli has been detected in breast implants from patients with BIA-ALCL.
Therefore, Dr Kadin and his colleagues hypothesized that an immune response toward the bacterial antigens may mediate the pathogenesis of BIA-ALCL.
The researchers studied 13 clinical samples of breast implant capsules and regional lymph nodes from 4 patients with BIA-ALCL, 7 patients with systemic ALCL, and 1 patient with peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS).
Immunohistochemistry was used to determine the presence of IL-13, IL-4, GATA3, and immunoglobulin E (IgE) in these samples.
All clinical samples of anaplastic cells from breast implant capsules tested positive for the presence of IL-13 (13/13). GATA3 was expressed in most anaplastic cell samples (12/13), and IL-4 expression was found in some anaplastic cell samples (6/13). IL-13 and GATA3 expression were observed in some intra-capsular small lymphocytes.
While IL-13 was also detected in BIA-ALCL cell lines, it was not found in 4 of the 7 systemic ALCL cases or the PTCL-NOS case.
Dr Kadin said the lack of IL-13 receptor expression in BIA-ALCL cell lines suggests that IL-13 is not an autocrine growth factor for BIA-ALCL, and its expression is most likely associated with an allergic immune response.
IL-13 is known to induce immunoglobulin class switching in plasma cells to produce IgE. H&E and Giemsa staining of the BIA-ALCL tumor tissue and involved regional lymph nodes revealed IgE and eosinophils on the surface of mast cells and follicular dendritic cells.
Taken together, these data point to an allergic reaction in breast implant capsules of BIA-ALCL.
Dr Kadin was hopeful that these findings could be extrapolated to prevent BIA-ALCL by identifying individuals at higher risk for developing the disease.
The next step for this research is to decipher the role of bacterial antigens in mediating the immune response and whether women who develop BIA-ALCL have a significant increase in other atopic conditions.