User login
Key ways to differentiate a benign from a malignant adnexal mass
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
Click here to register for PAGS 2014 December 4 to 6 at the Bellagio in Las Vegas
More from PAGS 2013:
Lichen sclerosis: My approach to treatment
Michael Baggish, MD
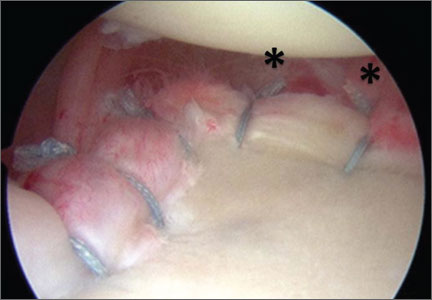
Arthroscopic Anterior Shoulder Stabilization With Percutaneous Assistance and Posteroinferior Capsular Plication
Volar Plate Capsulodesis for Metacarpophalangeal Hyperextension With Basal Joint Arthritis
En Bloc Joystick Reduction of a Comminuted Intra-articular Distal Radius Fracture: A Technical Trick
A Perspective on the Evolution of Distal Radius Fracture Treatment
The treatment for distal radius fractures has changed significantly over time. Initially, distal radius fractures were treated as relatively innocuous injuries that befell the elderly and the comparatively inactive, and casts were the mainstay of treatment. However, closer scrutiny of the clinical results revealed a myriad of problems with these treatments, including “cast disease,” stiffness, inability to hold skeletal position, and soft-tissue compromise that affected the overall function of the wrist and hand.
Additional techniques to improve results included the “pins and plaster” technique, with the introduction of 2 pins in the radius and metacarpals to retard collapse of the fracture while in the cast. This was in some sense an early version of external fixation, with pins giving support to the unstable wrist and the body of the cast serving as the external support. There was further evolution of the adaptation of early versions of external fixation used for the lower extremity towards the treatment of the distal radius. For example, when I was a resident at Massachusetts General Hospital, we routinely applied femoral distractors as external fixation devices for selected distal radius fractures. This was a time when more specific anatomic devices and implants were not yet available.
External fixation evolved,1 and distal radius–specific systems, with enhanced ability to adjust and achieve reduction, became available in the late 1980s. At the same time, distal radius fracture plating evolved from simple “stamped metal” plates with screws that merely fit in the screw holes, to more highly engineered implants with screws that engaged the plate at a fixed angle, much like the blade plate
technology used for lower extremity fractures.2 Over time, the volar fixed-angle plating system supplanted the other treatments and emerged as a popular treatment method.
Use of Kirschner wires or simple pins has been promoted in the past for treatment of distal radius fractures. In France, Kapandji3 described the use of “intra-focal
pinning.” In this technique, smooth Kirschner wires are introduced in the fracture site itself, and then using leverage so that the pins act like “crowbars,” the distal fragment that is malpositioned becomes adjusted into a more anatomic position.3 Kapandji’s treatment can be very effective in achieving reduction; however, as there is no fixation into the distal fragment, this technique has limitations in maintaining the reduction until healing has occurred. Interfragmentary pinning from the dorsal radial and dorsal ulnar aspects were nicely described by Clancey.4 I have found great utility in combining the Kapandji intra-focal techniques to achieve reduction with Clancey pin fixation or distal radius plating to maintain reduction.
I was intrigued with the article by Drs. Siegall and Ziran, “En Bloc Joystick Reduction of a Comminuted Intraarticular Distal Radius Fracture: A Technical Trick,” in this month’s issue of The American Journal of Orthopedics. In their technique, the authors introduced a series of parallel pins or screws below the articular surface from radius to ulna in parallel fashion to provide provisional fixation for the intra-articular components of their complex fracture. Once having done so, they felt more secure in manipulating the distal radius component en bloc; in fact, they used strapping to provide distal traction on the external protruding portion of the pins to help achieve and maintain reduction for their definitive fixation. Drs. Siegall and Ziran describe the use of either Kirschner wires or plating to provide definitive fixation. In the example cited, they performed (via an open method) both the scaffolding and plating without the need of an assistant to hold or maintain the reduction during the osteosynthesis. I can envision adapting the technique they describe to percutaneous treatments for placement of the scaffolding pins, and even the Kapandji/Clancey pins under fluoroscopic guidance or arthroscopeassisted placement.
Despite the popularity and utility of volar fixed-angle plating techniques to treat distal radius fractures, there remain certain situations in which these techniques are faced with challenges. Certainly one of them is the more complex intra-articular fracture with multiple components, or in the very distal fracture patterns in which there is limited bone for the surgeon to use in providing distal screw fixation in the plating systems. Additionally, the nascent malunion presents some challenges as well in terms of performing a “takedown” of the partially healed fracture without destroying the soft, partially healed distal bone that contains the all-important articular component. These are the instances where supplemental techniques such as the one described by Drs. Siegall and Ziran, as well as the
Kapandji and Clancey techniques, have their greatest utility and appeal. Despite one’s wishes and best efforts, some distal radius fractures are not easily reconstructable. In these cases, use of external fixation or temporary arthrodesis
dorsal plating with subsequent plate removal5,6 can be the best reconstructive option and a great “bailout.” The prepared surgeon should have these supplemental techniques in their armamentarium to be able to adapt to the conditions that present themselves in the operating room and to do the best job they can for the patient.
References
1. Agee JM. External fixation. Technical advances based upon multiplanar
ligamentotaxis. Orthop Clin North Am. 1993;24(2):265-274.
2. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable
distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96-102.
3. Kapandji A. Internal fixation by double intrafocal plate. Functional treatment
of non articular fractures of the lower end of the radius (author’s transl) [in French]. Ann Chir. 1976;30(11-12):903-908.
4. Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J Bone Joint Surg Am. 1984;66(7):1008-1014.
5. Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2(4):248-252.
6. Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87(5):945-954.
The treatment for distal radius fractures has changed significantly over time. Initially, distal radius fractures were treated as relatively innocuous injuries that befell the elderly and the comparatively inactive, and casts were the mainstay of treatment. However, closer scrutiny of the clinical results revealed a myriad of problems with these treatments, including “cast disease,” stiffness, inability to hold skeletal position, and soft-tissue compromise that affected the overall function of the wrist and hand.
Additional techniques to improve results included the “pins and plaster” technique, with the introduction of 2 pins in the radius and metacarpals to retard collapse of the fracture while in the cast. This was in some sense an early version of external fixation, with pins giving support to the unstable wrist and the body of the cast serving as the external support. There was further evolution of the adaptation of early versions of external fixation used for the lower extremity towards the treatment of the distal radius. For example, when I was a resident at Massachusetts General Hospital, we routinely applied femoral distractors as external fixation devices for selected distal radius fractures. This was a time when more specific anatomic devices and implants were not yet available.
External fixation evolved,1 and distal radius–specific systems, with enhanced ability to adjust and achieve reduction, became available in the late 1980s. At the same time, distal radius fracture plating evolved from simple “stamped metal” plates with screws that merely fit in the screw holes, to more highly engineered implants with screws that engaged the plate at a fixed angle, much like the blade plate
technology used for lower extremity fractures.2 Over time, the volar fixed-angle plating system supplanted the other treatments and emerged as a popular treatment method.
Use of Kirschner wires or simple pins has been promoted in the past for treatment of distal radius fractures. In France, Kapandji3 described the use of “intra-focal
pinning.” In this technique, smooth Kirschner wires are introduced in the fracture site itself, and then using leverage so that the pins act like “crowbars,” the distal fragment that is malpositioned becomes adjusted into a more anatomic position.3 Kapandji’s treatment can be very effective in achieving reduction; however, as there is no fixation into the distal fragment, this technique has limitations in maintaining the reduction until healing has occurred. Interfragmentary pinning from the dorsal radial and dorsal ulnar aspects were nicely described by Clancey.4 I have found great utility in combining the Kapandji intra-focal techniques to achieve reduction with Clancey pin fixation or distal radius plating to maintain reduction.
I was intrigued with the article by Drs. Siegall and Ziran, “En Bloc Joystick Reduction of a Comminuted Intraarticular Distal Radius Fracture: A Technical Trick,” in this month’s issue of The American Journal of Orthopedics. In their technique, the authors introduced a series of parallel pins or screws below the articular surface from radius to ulna in parallel fashion to provide provisional fixation for the intra-articular components of their complex fracture. Once having done so, they felt more secure in manipulating the distal radius component en bloc; in fact, they used strapping to provide distal traction on the external protruding portion of the pins to help achieve and maintain reduction for their definitive fixation. Drs. Siegall and Ziran describe the use of either Kirschner wires or plating to provide definitive fixation. In the example cited, they performed (via an open method) both the scaffolding and plating without the need of an assistant to hold or maintain the reduction during the osteosynthesis. I can envision adapting the technique they describe to percutaneous treatments for placement of the scaffolding pins, and even the Kapandji/Clancey pins under fluoroscopic guidance or arthroscopeassisted placement.
Despite the popularity and utility of volar fixed-angle plating techniques to treat distal radius fractures, there remain certain situations in which these techniques are faced with challenges. Certainly one of them is the more complex intra-articular fracture with multiple components, or in the very distal fracture patterns in which there is limited bone for the surgeon to use in providing distal screw fixation in the plating systems. Additionally, the nascent malunion presents some challenges as well in terms of performing a “takedown” of the partially healed fracture without destroying the soft, partially healed distal bone that contains the all-important articular component. These are the instances where supplemental techniques such as the one described by Drs. Siegall and Ziran, as well as the
Kapandji and Clancey techniques, have their greatest utility and appeal. Despite one’s wishes and best efforts, some distal radius fractures are not easily reconstructable. In these cases, use of external fixation or temporary arthrodesis
dorsal plating with subsequent plate removal5,6 can be the best reconstructive option and a great “bailout.” The prepared surgeon should have these supplemental techniques in their armamentarium to be able to adapt to the conditions that present themselves in the operating room and to do the best job they can for the patient.
References
1. Agee JM. External fixation. Technical advances based upon multiplanar
ligamentotaxis. Orthop Clin North Am. 1993;24(2):265-274.
2. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable
distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96-102.
3. Kapandji A. Internal fixation by double intrafocal plate. Functional treatment
of non articular fractures of the lower end of the radius (author’s transl) [in French]. Ann Chir. 1976;30(11-12):903-908.
4. Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J Bone Joint Surg Am. 1984;66(7):1008-1014.
5. Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2(4):248-252.
6. Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87(5):945-954.
The treatment for distal radius fractures has changed significantly over time. Initially, distal radius fractures were treated as relatively innocuous injuries that befell the elderly and the comparatively inactive, and casts were the mainstay of treatment. However, closer scrutiny of the clinical results revealed a myriad of problems with these treatments, including “cast disease,” stiffness, inability to hold skeletal position, and soft-tissue compromise that affected the overall function of the wrist and hand.
Additional techniques to improve results included the “pins and plaster” technique, with the introduction of 2 pins in the radius and metacarpals to retard collapse of the fracture while in the cast. This was in some sense an early version of external fixation, with pins giving support to the unstable wrist and the body of the cast serving as the external support. There was further evolution of the adaptation of early versions of external fixation used for the lower extremity towards the treatment of the distal radius. For example, when I was a resident at Massachusetts General Hospital, we routinely applied femoral distractors as external fixation devices for selected distal radius fractures. This was a time when more specific anatomic devices and implants were not yet available.
External fixation evolved,1 and distal radius–specific systems, with enhanced ability to adjust and achieve reduction, became available in the late 1980s. At the same time, distal radius fracture plating evolved from simple “stamped metal” plates with screws that merely fit in the screw holes, to more highly engineered implants with screws that engaged the plate at a fixed angle, much like the blade plate
technology used for lower extremity fractures.2 Over time, the volar fixed-angle plating system supplanted the other treatments and emerged as a popular treatment method.
Use of Kirschner wires or simple pins has been promoted in the past for treatment of distal radius fractures. In France, Kapandji3 described the use of “intra-focal
pinning.” In this technique, smooth Kirschner wires are introduced in the fracture site itself, and then using leverage so that the pins act like “crowbars,” the distal fragment that is malpositioned becomes adjusted into a more anatomic position.3 Kapandji’s treatment can be very effective in achieving reduction; however, as there is no fixation into the distal fragment, this technique has limitations in maintaining the reduction until healing has occurred. Interfragmentary pinning from the dorsal radial and dorsal ulnar aspects were nicely described by Clancey.4 I have found great utility in combining the Kapandji intra-focal techniques to achieve reduction with Clancey pin fixation or distal radius plating to maintain reduction.
I was intrigued with the article by Drs. Siegall and Ziran, “En Bloc Joystick Reduction of a Comminuted Intraarticular Distal Radius Fracture: A Technical Trick,” in this month’s issue of The American Journal of Orthopedics. In their technique, the authors introduced a series of parallel pins or screws below the articular surface from radius to ulna in parallel fashion to provide provisional fixation for the intra-articular components of their complex fracture. Once having done so, they felt more secure in manipulating the distal radius component en bloc; in fact, they used strapping to provide distal traction on the external protruding portion of the pins to help achieve and maintain reduction for their definitive fixation. Drs. Siegall and Ziran describe the use of either Kirschner wires or plating to provide definitive fixation. In the example cited, they performed (via an open method) both the scaffolding and plating without the need of an assistant to hold or maintain the reduction during the osteosynthesis. I can envision adapting the technique they describe to percutaneous treatments for placement of the scaffolding pins, and even the Kapandji/Clancey pins under fluoroscopic guidance or arthroscopeassisted placement.
Despite the popularity and utility of volar fixed-angle plating techniques to treat distal radius fractures, there remain certain situations in which these techniques are faced with challenges. Certainly one of them is the more complex intra-articular fracture with multiple components, or in the very distal fracture patterns in which there is limited bone for the surgeon to use in providing distal screw fixation in the plating systems. Additionally, the nascent malunion presents some challenges as well in terms of performing a “takedown” of the partially healed fracture without destroying the soft, partially healed distal bone that contains the all-important articular component. These are the instances where supplemental techniques such as the one described by Drs. Siegall and Ziran, as well as the
Kapandji and Clancey techniques, have their greatest utility and appeal. Despite one’s wishes and best efforts, some distal radius fractures are not easily reconstructable. In these cases, use of external fixation or temporary arthrodesis
dorsal plating with subsequent plate removal5,6 can be the best reconstructive option and a great “bailout.” The prepared surgeon should have these supplemental techniques in their armamentarium to be able to adapt to the conditions that present themselves in the operating room and to do the best job they can for the patient.
References
1. Agee JM. External fixation. Technical advances based upon multiplanar
ligamentotaxis. Orthop Clin North Am. 1993;24(2):265-274.
2. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable
distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29(1):96-102.
3. Kapandji A. Internal fixation by double intrafocal plate. Functional treatment
of non articular fractures of the lower end of the radius (author’s transl) [in French]. Ann Chir. 1976;30(11-12):903-908.
4. Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J Bone Joint Surg Am. 1984;66(7):1008-1014.
5. Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2(4):248-252.
6. Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87(5):945-954.
Drug could prevent thrombocytopenia in MM

in the bone marrow
Researchers say they’ve identified a previously unknown but crucial component of the platelet production process.
And this discovery could help spare multiple myeloma (MM) patients from thrombocytopenia induced by the proteasome inhibitor bortezomib.
The researchers found that proteasome inhibition blocked platelet production in vitro and in vivo.
But fasudil, a Rho kinase inhibitor that is approved for use outside the US, restored platelet counts.
The researchers believe these findings, published in The Journal of Clinical Investigation, could translate to MM patients.
“A low platelet count is a big issue for people who receive bortezomib for this cancer,” said study author Andrew S. Weyrich, PhD, of the University of Utah in Salt Lake City.
“When platelet levels drop too low, it can mean interrupting treatment to allow the platelet count to recover. Fasudil potentially could help keep platelet counts normal while multiple myeloma patients receive bortezomib.”
Dr Weyrich and his colleagues found that bortezomib-induced proteasome inhibition prevented the production of proplatelets in both human and mouse megakaryocytes.
Megakaryocytes isolated from mice lacking PSMC1, an essential subunit of the 26S proteasome, also failed to produce proplatelets.
Further study revealed that the megakaryocytes’ inability to generate platelets was caused by the hyperactivation of RhoA, a protein that helps megakaryocytes maintain the proper shape to produce platelets.
When the researchers inhibited RhoA or its downstream target, Rho-associated protein kinase, in vitro, they were able to restore megakaryocyte proplatelet formation in the setting of proteasome inhibition.
Likewise, the Rho kinase inhibitor fasudil restored platelet counts in adult mice that had thrombocytopenia induced by proteasome inhibition.
Fasudil is approved in Japan and elsewhere to treat cerebral vasospasms, or constricted arteries that arise as a complication of brain aneurysms.
The drug is under investigation in US clinical trials for treating high blood pressure, diabetic macular edema, and other health issues.
There are no trials investigating fasudil’s effects on thrombocytopenia, but Dr Weyrich and his colleagues hope their study might change that. And if clinical trials produce favorable results, fasudil might be made available for MM patients much faster than a new drug.
“If the Food and Drug Administration did approve fasudil for use by multiple myeloma patients, it could, in principle, be moved to the clinic relatively fast in the United States,” Dr Weyrich said. ![]()

in the bone marrow
Researchers say they’ve identified a previously unknown but crucial component of the platelet production process.
And this discovery could help spare multiple myeloma (MM) patients from thrombocytopenia induced by the proteasome inhibitor bortezomib.
The researchers found that proteasome inhibition blocked platelet production in vitro and in vivo.
But fasudil, a Rho kinase inhibitor that is approved for use outside the US, restored platelet counts.
The researchers believe these findings, published in The Journal of Clinical Investigation, could translate to MM patients.
“A low platelet count is a big issue for people who receive bortezomib for this cancer,” said study author Andrew S. Weyrich, PhD, of the University of Utah in Salt Lake City.
“When platelet levels drop too low, it can mean interrupting treatment to allow the platelet count to recover. Fasudil potentially could help keep platelet counts normal while multiple myeloma patients receive bortezomib.”
Dr Weyrich and his colleagues found that bortezomib-induced proteasome inhibition prevented the production of proplatelets in both human and mouse megakaryocytes.
Megakaryocytes isolated from mice lacking PSMC1, an essential subunit of the 26S proteasome, also failed to produce proplatelets.
Further study revealed that the megakaryocytes’ inability to generate platelets was caused by the hyperactivation of RhoA, a protein that helps megakaryocytes maintain the proper shape to produce platelets.
When the researchers inhibited RhoA or its downstream target, Rho-associated protein kinase, in vitro, they were able to restore megakaryocyte proplatelet formation in the setting of proteasome inhibition.
Likewise, the Rho kinase inhibitor fasudil restored platelet counts in adult mice that had thrombocytopenia induced by proteasome inhibition.
Fasudil is approved in Japan and elsewhere to treat cerebral vasospasms, or constricted arteries that arise as a complication of brain aneurysms.
The drug is under investigation in US clinical trials for treating high blood pressure, diabetic macular edema, and other health issues.
There are no trials investigating fasudil’s effects on thrombocytopenia, but Dr Weyrich and his colleagues hope their study might change that. And if clinical trials produce favorable results, fasudil might be made available for MM patients much faster than a new drug.
“If the Food and Drug Administration did approve fasudil for use by multiple myeloma patients, it could, in principle, be moved to the clinic relatively fast in the United States,” Dr Weyrich said. ![]()

in the bone marrow
Researchers say they’ve identified a previously unknown but crucial component of the platelet production process.
And this discovery could help spare multiple myeloma (MM) patients from thrombocytopenia induced by the proteasome inhibitor bortezomib.
The researchers found that proteasome inhibition blocked platelet production in vitro and in vivo.
But fasudil, a Rho kinase inhibitor that is approved for use outside the US, restored platelet counts.
The researchers believe these findings, published in The Journal of Clinical Investigation, could translate to MM patients.
“A low platelet count is a big issue for people who receive bortezomib for this cancer,” said study author Andrew S. Weyrich, PhD, of the University of Utah in Salt Lake City.
“When platelet levels drop too low, it can mean interrupting treatment to allow the platelet count to recover. Fasudil potentially could help keep platelet counts normal while multiple myeloma patients receive bortezomib.”
Dr Weyrich and his colleagues found that bortezomib-induced proteasome inhibition prevented the production of proplatelets in both human and mouse megakaryocytes.
Megakaryocytes isolated from mice lacking PSMC1, an essential subunit of the 26S proteasome, also failed to produce proplatelets.
Further study revealed that the megakaryocytes’ inability to generate platelets was caused by the hyperactivation of RhoA, a protein that helps megakaryocytes maintain the proper shape to produce platelets.
When the researchers inhibited RhoA or its downstream target, Rho-associated protein kinase, in vitro, they were able to restore megakaryocyte proplatelet formation in the setting of proteasome inhibition.
Likewise, the Rho kinase inhibitor fasudil restored platelet counts in adult mice that had thrombocytopenia induced by proteasome inhibition.
Fasudil is approved in Japan and elsewhere to treat cerebral vasospasms, or constricted arteries that arise as a complication of brain aneurysms.
The drug is under investigation in US clinical trials for treating high blood pressure, diabetic macular edema, and other health issues.
There are no trials investigating fasudil’s effects on thrombocytopenia, but Dr Weyrich and his colleagues hope their study might change that. And if clinical trials produce favorable results, fasudil might be made available for MM patients much faster than a new drug.
“If the Food and Drug Administration did approve fasudil for use by multiple myeloma patients, it could, in principle, be moved to the clinic relatively fast in the United States,” Dr Weyrich said. ![]()
Healthy habits can cut risk of metabolic syndrome in childhood cancer survivors

patient and her father
Credit: Rhoda Baer
Following a healthy lifestyle can decrease the risk of metabolic syndrome in childhood cancer survivors, according to a study published in Cancer.
Unfortunately, only about a quarter of the survivors studied actually practiced healthy lifestyle habits, such as engaging in moderate physical activity; eating the recommended daily serving of fruits, vegetables, and complex carbohydrates; and consuming red meat, alcohol, and sodium in moderation.
Childhood cancer survivors are known to have an increased risk of developing metabolic syndrome.
The syndrome is actually a number of conditions—high blood pressure, increased body fat, and abnormal cholesterol and glucose levels—that, when they occur together, increase a person’s risk of heart disease, stroke, and diabetes.
Kirsten Ness, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues wanted to determine if lifestyle habits might affect the risk of metabolic syndrome among childhood cancer survivors.
So the team analyzed 1598 survivors who were cancer-free for at least 10 years. They had a median age of 32.7 years (range, 18.9 to 60).
The analysis showed that failure to follow healthy lifestyle guidelines roughly doubled the survivors’ risk of developing metabolic syndrome. Women had a 2.4-times greater risk, and men had a 2.2-times greater risk of the syndrome if they did not follow the guidelines.
Metabolic syndrome was present in 31.8% of the participants—32.5% of males and 31% of females.
The researchers considered a subject to have metabolic syndrome if he had or received treatment for 3 or more of the following:
- Abdominal obesity (waist circumference of > 102 cm in males and > 88 cm in females)
- Triglycerides ≥ 150 mg/dL
- High-density lipoprotein cholesterol (< 40 mg/dL in males and < 50 mg/dL in females)
- Hypertension (systolic pressure ≥ 130 mm Hg or diastolic pressure ≥ 85 mm Hg)
- Fasting plasma glucose ≥ 100 mg/dL.
Questionnaires and tests helped the researchers assess whether participants followed healthy lifestyle recommendations issued by the World Cancer Research Fund and American Institute for Cancer Research.
The recommendations include:
- Having a body mass index of 25 or lower
- Engaging in moderate physical activity for 150 minutes each week
- Eating 5 or more servings of fruits and vegetables each day
- Consuming 400 g or more of complex carbohydrates daily
- Eating less than 80 g of red meat each day
- Consuming less than 2400 mg of sodium each day
- Low daily alcohol consumption (less than 14 g for females and less than 28 g for males).
Subjects who met at least 4 of these 7 criteria were classified as following the guidelines. And 27% of the participants—25.2% of males and 28.8% of females—were classified as such.
“These findings are important because they indicate that adults who were treated for cancer as children have the opportunity to influence their own health outcomes,” Dr Ness said.
“[A]dopting a lifestyle that includes maintaining a healthy body weight, regular physical activity, and a diet that includes fruits and vegetables and that limits refined sugars, excessive alcohol, red meat, and salt has potential to prevent development of metabolic syndrome.” ![]()

patient and her father
Credit: Rhoda Baer
Following a healthy lifestyle can decrease the risk of metabolic syndrome in childhood cancer survivors, according to a study published in Cancer.
Unfortunately, only about a quarter of the survivors studied actually practiced healthy lifestyle habits, such as engaging in moderate physical activity; eating the recommended daily serving of fruits, vegetables, and complex carbohydrates; and consuming red meat, alcohol, and sodium in moderation.
Childhood cancer survivors are known to have an increased risk of developing metabolic syndrome.
The syndrome is actually a number of conditions—high blood pressure, increased body fat, and abnormal cholesterol and glucose levels—that, when they occur together, increase a person’s risk of heart disease, stroke, and diabetes.
Kirsten Ness, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues wanted to determine if lifestyle habits might affect the risk of metabolic syndrome among childhood cancer survivors.
So the team analyzed 1598 survivors who were cancer-free for at least 10 years. They had a median age of 32.7 years (range, 18.9 to 60).
The analysis showed that failure to follow healthy lifestyle guidelines roughly doubled the survivors’ risk of developing metabolic syndrome. Women had a 2.4-times greater risk, and men had a 2.2-times greater risk of the syndrome if they did not follow the guidelines.
Metabolic syndrome was present in 31.8% of the participants—32.5% of males and 31% of females.
The researchers considered a subject to have metabolic syndrome if he had or received treatment for 3 or more of the following:
- Abdominal obesity (waist circumference of > 102 cm in males and > 88 cm in females)
- Triglycerides ≥ 150 mg/dL
- High-density lipoprotein cholesterol (< 40 mg/dL in males and < 50 mg/dL in females)
- Hypertension (systolic pressure ≥ 130 mm Hg or diastolic pressure ≥ 85 mm Hg)
- Fasting plasma glucose ≥ 100 mg/dL.
Questionnaires and tests helped the researchers assess whether participants followed healthy lifestyle recommendations issued by the World Cancer Research Fund and American Institute for Cancer Research.
The recommendations include:
- Having a body mass index of 25 or lower
- Engaging in moderate physical activity for 150 minutes each week
- Eating 5 or more servings of fruits and vegetables each day
- Consuming 400 g or more of complex carbohydrates daily
- Eating less than 80 g of red meat each day
- Consuming less than 2400 mg of sodium each day
- Low daily alcohol consumption (less than 14 g for females and less than 28 g for males).
Subjects who met at least 4 of these 7 criteria were classified as following the guidelines. And 27% of the participants—25.2% of males and 28.8% of females—were classified as such.
“These findings are important because they indicate that adults who were treated for cancer as children have the opportunity to influence their own health outcomes,” Dr Ness said.
“[A]dopting a lifestyle that includes maintaining a healthy body weight, regular physical activity, and a diet that includes fruits and vegetables and that limits refined sugars, excessive alcohol, red meat, and salt has potential to prevent development of metabolic syndrome.” ![]()

patient and her father
Credit: Rhoda Baer
Following a healthy lifestyle can decrease the risk of metabolic syndrome in childhood cancer survivors, according to a study published in Cancer.
Unfortunately, only about a quarter of the survivors studied actually practiced healthy lifestyle habits, such as engaging in moderate physical activity; eating the recommended daily serving of fruits, vegetables, and complex carbohydrates; and consuming red meat, alcohol, and sodium in moderation.
Childhood cancer survivors are known to have an increased risk of developing metabolic syndrome.
The syndrome is actually a number of conditions—high blood pressure, increased body fat, and abnormal cholesterol and glucose levels—that, when they occur together, increase a person’s risk of heart disease, stroke, and diabetes.
Kirsten Ness, PhD, of St Jude Children’s Research Hospital in Memphis, Tennessee, and her colleagues wanted to determine if lifestyle habits might affect the risk of metabolic syndrome among childhood cancer survivors.
So the team analyzed 1598 survivors who were cancer-free for at least 10 years. They had a median age of 32.7 years (range, 18.9 to 60).
The analysis showed that failure to follow healthy lifestyle guidelines roughly doubled the survivors’ risk of developing metabolic syndrome. Women had a 2.4-times greater risk, and men had a 2.2-times greater risk of the syndrome if they did not follow the guidelines.
Metabolic syndrome was present in 31.8% of the participants—32.5% of males and 31% of females.
The researchers considered a subject to have metabolic syndrome if he had or received treatment for 3 or more of the following:
- Abdominal obesity (waist circumference of > 102 cm in males and > 88 cm in females)
- Triglycerides ≥ 150 mg/dL
- High-density lipoprotein cholesterol (< 40 mg/dL in males and < 50 mg/dL in females)
- Hypertension (systolic pressure ≥ 130 mm Hg or diastolic pressure ≥ 85 mm Hg)
- Fasting plasma glucose ≥ 100 mg/dL.
Questionnaires and tests helped the researchers assess whether participants followed healthy lifestyle recommendations issued by the World Cancer Research Fund and American Institute for Cancer Research.
The recommendations include:
- Having a body mass index of 25 or lower
- Engaging in moderate physical activity for 150 minutes each week
- Eating 5 or more servings of fruits and vegetables each day
- Consuming 400 g or more of complex carbohydrates daily
- Eating less than 80 g of red meat each day
- Consuming less than 2400 mg of sodium each day
- Low daily alcohol consumption (less than 14 g for females and less than 28 g for males).
Subjects who met at least 4 of these 7 criteria were classified as following the guidelines. And 27% of the participants—25.2% of males and 28.8% of females—were classified as such.
“These findings are important because they indicate that adults who were treated for cancer as children have the opportunity to influence their own health outcomes,” Dr Ness said.
“[A]dopting a lifestyle that includes maintaining a healthy body weight, regular physical activity, and a diet that includes fruits and vegetables and that limits refined sugars, excessive alcohol, red meat, and salt has potential to prevent development of metabolic syndrome.” ![]()
Malaria infection trial a game-changer, group says

Credit: Ute Frevert
and Margaret Shear
Investigators have reported success in the first clinical trial demonstrating controlled malaria infection in an African nation.
The study established that a product containing Plasmodium falciparum sporozoites can be used to safely infect volunteers with malaria in controlled lab conditions in a malaria-endemic country.
This represents a significant milestone in the search for new malaria drugs and vaccines, according to the investigators.
“We are extremely excited by the good results of this malaria challenge test, which opens up unprecedented opportunity for evaluation of new malaria drugs and vaccines in Africa,” said Salim Abdullah, PhD, of the Ifakara Health Institute Bagamoyo Research and Training Centre in Tanzania, where the study took place.
Dr Abdullah and his colleagues reported the results in the American Journal of Tropical Medicine and Hygiene. A related editorial is also available.
The researchers tested sporozoites that were grown in mosquitoes in the lab and then packaged in a purified, aseptic form acceptable for clinical trials. The product is known as PfSPZ Challenge and is owned by Sanaria, Inc., a privately held company in Rockville, Maryland.
Prior to this innovation, the ability to challenge a vaccine’s effectiveness required deliberately infecting vaccinated volunteers with malaria by exposing them to mosquito bites in an insectary.
Few such malaria insectaries exist, and due to the resources needed, these are limited to a handful in the US and Europe, far from the countries where malaria takes its toll.
This clinical trial established that injecting volunteers with cryopreserved, aseptic parasites can safely and effectively infect adult volunteers with P falciparum malaria in a malaria-endemic country.
“This innovation is a game-changer for malaria research and development in Africa,” said study author Stephen L. Hoffman, MD, of Sanaria, Inc. “This is about making available within Africa the same research tools to study malaria that we have in the USA and Europe.”
To test PfSPZ Challenge, the investigators recruited a group of 30 Tanzanian men, residents of Dar es Salaam, who had minimal exposure to malaria during the previous 5 years.
The volunteers were injected intradermally with 10,000 sporozoites (n=12), 25,000 sporozoites (n=11), or normal saline (n=6). Investigators and subjects were blinded to the intervention.
The investigators then compared the infection rate to that of volunteers who participated in a similar study in The Netherlands a few years ago.
After about 2 weeks, all but 2 of the 23 Tanzanian volunteers injected with sporozoites developed active infections, a rate similar to the Dutch volunteers.
Once active infection was established, the volunteers were immediately treated for malaria and cleared of parasites.
None of the volunteers developed serious side effects related to the study. Mild side effects included low-grade fever, headaches, and fatigue.
“This is a real step forward for developing a vaccine against malaria, which has killed more human beings throughout history than any other single cause,” said study author Christopher Plowe, MD, MPH, of the University of Maryland in Baltimore.
“The ability to safely administer malaria parasites by injection rather than by mosquito bite makes it possible to test new malaria vaccines, as well as drugs, anywhere in the world.” ![]()

Credit: Ute Frevert
and Margaret Shear
Investigators have reported success in the first clinical trial demonstrating controlled malaria infection in an African nation.
The study established that a product containing Plasmodium falciparum sporozoites can be used to safely infect volunteers with malaria in controlled lab conditions in a malaria-endemic country.
This represents a significant milestone in the search for new malaria drugs and vaccines, according to the investigators.
“We are extremely excited by the good results of this malaria challenge test, which opens up unprecedented opportunity for evaluation of new malaria drugs and vaccines in Africa,” said Salim Abdullah, PhD, of the Ifakara Health Institute Bagamoyo Research and Training Centre in Tanzania, where the study took place.
Dr Abdullah and his colleagues reported the results in the American Journal of Tropical Medicine and Hygiene. A related editorial is also available.
The researchers tested sporozoites that were grown in mosquitoes in the lab and then packaged in a purified, aseptic form acceptable for clinical trials. The product is known as PfSPZ Challenge and is owned by Sanaria, Inc., a privately held company in Rockville, Maryland.
Prior to this innovation, the ability to challenge a vaccine’s effectiveness required deliberately infecting vaccinated volunteers with malaria by exposing them to mosquito bites in an insectary.
Few such malaria insectaries exist, and due to the resources needed, these are limited to a handful in the US and Europe, far from the countries where malaria takes its toll.
This clinical trial established that injecting volunteers with cryopreserved, aseptic parasites can safely and effectively infect adult volunteers with P falciparum malaria in a malaria-endemic country.
“This innovation is a game-changer for malaria research and development in Africa,” said study author Stephen L. Hoffman, MD, of Sanaria, Inc. “This is about making available within Africa the same research tools to study malaria that we have in the USA and Europe.”
To test PfSPZ Challenge, the investigators recruited a group of 30 Tanzanian men, residents of Dar es Salaam, who had minimal exposure to malaria during the previous 5 years.
The volunteers were injected intradermally with 10,000 sporozoites (n=12), 25,000 sporozoites (n=11), or normal saline (n=6). Investigators and subjects were blinded to the intervention.
The investigators then compared the infection rate to that of volunteers who participated in a similar study in The Netherlands a few years ago.
After about 2 weeks, all but 2 of the 23 Tanzanian volunteers injected with sporozoites developed active infections, a rate similar to the Dutch volunteers.
Once active infection was established, the volunteers were immediately treated for malaria and cleared of parasites.
None of the volunteers developed serious side effects related to the study. Mild side effects included low-grade fever, headaches, and fatigue.
“This is a real step forward for developing a vaccine against malaria, which has killed more human beings throughout history than any other single cause,” said study author Christopher Plowe, MD, MPH, of the University of Maryland in Baltimore.
“The ability to safely administer malaria parasites by injection rather than by mosquito bite makes it possible to test new malaria vaccines, as well as drugs, anywhere in the world.” ![]()

Credit: Ute Frevert
and Margaret Shear
Investigators have reported success in the first clinical trial demonstrating controlled malaria infection in an African nation.
The study established that a product containing Plasmodium falciparum sporozoites can be used to safely infect volunteers with malaria in controlled lab conditions in a malaria-endemic country.
This represents a significant milestone in the search for new malaria drugs and vaccines, according to the investigators.
“We are extremely excited by the good results of this malaria challenge test, which opens up unprecedented opportunity for evaluation of new malaria drugs and vaccines in Africa,” said Salim Abdullah, PhD, of the Ifakara Health Institute Bagamoyo Research and Training Centre in Tanzania, where the study took place.
Dr Abdullah and his colleagues reported the results in the American Journal of Tropical Medicine and Hygiene. A related editorial is also available.
The researchers tested sporozoites that were grown in mosquitoes in the lab and then packaged in a purified, aseptic form acceptable for clinical trials. The product is known as PfSPZ Challenge and is owned by Sanaria, Inc., a privately held company in Rockville, Maryland.
Prior to this innovation, the ability to challenge a vaccine’s effectiveness required deliberately infecting vaccinated volunteers with malaria by exposing them to mosquito bites in an insectary.
Few such malaria insectaries exist, and due to the resources needed, these are limited to a handful in the US and Europe, far from the countries where malaria takes its toll.
This clinical trial established that injecting volunteers with cryopreserved, aseptic parasites can safely and effectively infect adult volunteers with P falciparum malaria in a malaria-endemic country.
“This innovation is a game-changer for malaria research and development in Africa,” said study author Stephen L. Hoffman, MD, of Sanaria, Inc. “This is about making available within Africa the same research tools to study malaria that we have in the USA and Europe.”
To test PfSPZ Challenge, the investigators recruited a group of 30 Tanzanian men, residents of Dar es Salaam, who had minimal exposure to malaria during the previous 5 years.
The volunteers were injected intradermally with 10,000 sporozoites (n=12), 25,000 sporozoites (n=11), or normal saline (n=6). Investigators and subjects were blinded to the intervention.
The investigators then compared the infection rate to that of volunteers who participated in a similar study in The Netherlands a few years ago.
After about 2 weeks, all but 2 of the 23 Tanzanian volunteers injected with sporozoites developed active infections, a rate similar to the Dutch volunteers.
Once active infection was established, the volunteers were immediately treated for malaria and cleared of parasites.
None of the volunteers developed serious side effects related to the study. Mild side effects included low-grade fever, headaches, and fatigue.
“This is a real step forward for developing a vaccine against malaria, which has killed more human beings throughout history than any other single cause,” said study author Christopher Plowe, MD, MPH, of the University of Maryland in Baltimore.
“The ability to safely administer malaria parasites by injection rather than by mosquito bite makes it possible to test new malaria vaccines, as well as drugs, anywhere in the world.” ![]()
FDA expands approved use of ibrutinib in CLL

Credit: Steven Harbour
The US Food and Drug Administration (FDA) has expanded the approved use of ibrutinib (Imbruvica) in patients with chronic lymphocytic leukemia (CLL).
The agency previously granted the drug accelerated approval to treat CLL patients who had received at least 1 prior therapy.
Now, the FDA has granted ibrutinib full approval for that indication and expanded the drug’s approved use to include previously treated and untreated CLL patients with 17p deletion.
The FDA’s decision to grant ibrutinib accelerated approval in CLL was based on the drug’s ability to elicit responses in previously treated patients.
Recent trial results have shown the drug can improve survival rates in CLL, which signifies a clinical benefit and allows the FDA to grant ibrutinib full approval.
Ibrutinib in CLL: Trial results
The expanded approval for ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib in development
Ibrutinib is being studied alone and in combination with other treatments in several hematologic malignancies, including CLL, mantle cell lymphoma (MCL), Waldenstrom’s macroglobulinemia, diffuse large B-cell lymphoma, follicular lymphoma, and multiple myeloma.
Before the FDA granted ibrutinib accelerated approval in CLL, the agency granted the drug accelerated approval for use in previously treated MCL patients. Studies to verify ibrutinib’s clinical benefit in MCL are ongoing.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has recommended marketing authorization for ibrutinib to treat adults with relapsed or refractory MCL.
The committee has also recommended the drug for adults with CLL who have received at least 1 prior therapy and CLL patients with 17p deletion or TP53 mutation who cannot receive chemo-immunotherapy.
Ibrutinib is already approved in Israel for the treatment of adults with MCL who have received at least 1 prior therapy.
Ibrutinib is under development by Janssen Biotech and Pharmacyclics, Inc. The companies co-market ibrutinib in the US, but Janssen markets (or will market) ibrutinib in the rest of the world. ![]()

Credit: Steven Harbour
The US Food and Drug Administration (FDA) has expanded the approved use of ibrutinib (Imbruvica) in patients with chronic lymphocytic leukemia (CLL).
The agency previously granted the drug accelerated approval to treat CLL patients who had received at least 1 prior therapy.
Now, the FDA has granted ibrutinib full approval for that indication and expanded the drug’s approved use to include previously treated and untreated CLL patients with 17p deletion.
The FDA’s decision to grant ibrutinib accelerated approval in CLL was based on the drug’s ability to elicit responses in previously treated patients.
Recent trial results have shown the drug can improve survival rates in CLL, which signifies a clinical benefit and allows the FDA to grant ibrutinib full approval.
Ibrutinib in CLL: Trial results
The expanded approval for ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib in development
Ibrutinib is being studied alone and in combination with other treatments in several hematologic malignancies, including CLL, mantle cell lymphoma (MCL), Waldenstrom’s macroglobulinemia, diffuse large B-cell lymphoma, follicular lymphoma, and multiple myeloma.
Before the FDA granted ibrutinib accelerated approval in CLL, the agency granted the drug accelerated approval for use in previously treated MCL patients. Studies to verify ibrutinib’s clinical benefit in MCL are ongoing.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has recommended marketing authorization for ibrutinib to treat adults with relapsed or refractory MCL.
The committee has also recommended the drug for adults with CLL who have received at least 1 prior therapy and CLL patients with 17p deletion or TP53 mutation who cannot receive chemo-immunotherapy.
Ibrutinib is already approved in Israel for the treatment of adults with MCL who have received at least 1 prior therapy.
Ibrutinib is under development by Janssen Biotech and Pharmacyclics, Inc. The companies co-market ibrutinib in the US, but Janssen markets (or will market) ibrutinib in the rest of the world. ![]()

Credit: Steven Harbour
The US Food and Drug Administration (FDA) has expanded the approved use of ibrutinib (Imbruvica) in patients with chronic lymphocytic leukemia (CLL).
The agency previously granted the drug accelerated approval to treat CLL patients who had received at least 1 prior therapy.
Now, the FDA has granted ibrutinib full approval for that indication and expanded the drug’s approved use to include previously treated and untreated CLL patients with 17p deletion.
The FDA’s decision to grant ibrutinib accelerated approval in CLL was based on the drug’s ability to elicit responses in previously treated patients.
Recent trial results have shown the drug can improve survival rates in CLL, which signifies a clinical benefit and allows the FDA to grant ibrutinib full approval.
Ibrutinib in CLL: Trial results
The expanded approval for ibrutinib is based on results of the phase 3 RESONATE trial, which were presented at this year’s ASCO and EHA meetings.
The trial included 391 previously treated patients, 127 of whom had 17p deletion. Patients were randomized to receive ibrutinib or the anti-CD20 monoclonal antibody ofatumumab until disease progression or unacceptable toxicity.
The trial was stopped early after a pre-planned interim analysis showed that ibrutinib-treated patients experienced a 78% reduction in the risk of disease progression or death.
At the time of interim analysis, the patients’ median time on study was 9.4 months. The best overall response among evaluable patients was 78% in the ibrutinib arm and 11% in the ofatumumab arm.
Ibrutinib significantly prolonged progression-free and overall survival. The median progression-free survival was 8.1 months in the ofatumumab arm and was not reached in the ibrutinib arm (P<0.0001). The median overall survival was not reached in either arm, but the hazard ratio was 0.434 (P=0.0049).
Of the 127 patients with 17p deletion, those treated with ibrutinib experienced a 75% reduction in the risk of disease progression or death.
Adverse events occurred in 99% of patients in the ibrutinib arm and 98% of those in the ofatumumab arm. Grade 3/4 events occurred in 51% and 39%, respectively.
Atrial fibrillation, bleeding-related events, diarrhea, and arthralgia were more common in the ibrutinib arm. Infusion-related reactions, peripheral sensory neuropathy, urticaria, night sweats, and pruritus were more common in the ofatumumab arm.
Ibrutinib in development
Ibrutinib is being studied alone and in combination with other treatments in several hematologic malignancies, including CLL, mantle cell lymphoma (MCL), Waldenstrom’s macroglobulinemia, diffuse large B-cell lymphoma, follicular lymphoma, and multiple myeloma.
Before the FDA granted ibrutinib accelerated approval in CLL, the agency granted the drug accelerated approval for use in previously treated MCL patients. Studies to verify ibrutinib’s clinical benefit in MCL are ongoing.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has recommended marketing authorization for ibrutinib to treat adults with relapsed or refractory MCL.
The committee has also recommended the drug for adults with CLL who have received at least 1 prior therapy and CLL patients with 17p deletion or TP53 mutation who cannot receive chemo-immunotherapy.
Ibrutinib is already approved in Israel for the treatment of adults with MCL who have received at least 1 prior therapy.
Ibrutinib is under development by Janssen Biotech and Pharmacyclics, Inc. The companies co-market ibrutinib in the US, but Janssen markets (or will market) ibrutinib in the rest of the world. ![]()
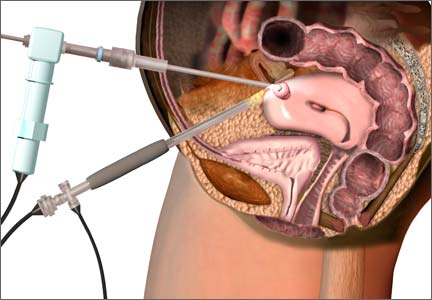
Post–FDA hearing: Will open power morcellation of uterine tissue remain an option during hysterectomy and myomectomy?
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy has been in the limelight in 2014—particularly morcellation performed in an “open” fashion (without use of a protective bag). Concerns about the dispersion of tissue throughout the peritoneal cavity—including the risk of disseminating tissue from leiomyosarcoma, a rare but deadly cancer—have drawn statements from the American College of Obstetricians and Gynecologists (ACOG), the AAGL, the US Food and Drug Administration (FDA), and others, cautioning against the use of open power morcellation in women with a known or suspected malignancy.
In July 2014, the FDA convened a two-day hearing of the Obstetrics and Gynecology Devices Panel (one of the panels in its Medical Devices Advisory Committee) to consider whether power morcellation should remain an option and, if so, what restrictions or labeling might be recommended.
In advance of the FDA hearing, OBG Management invited two experts in women’s health to explore the options more deeply and address the future of minimally invasive surgery (MIS): Ray A. Wertheim, MD, Director of the AAGL Center of Excellence Minimally Invasive Gynecology Program at Inova Fair Oaks Hospital in Fairfax, Virginia, and Harry Reich, MD, widely known as the first surgeon to perform laparoscopic hysterectomy, among other achievements. Both Dr. Wertheim and Dr. Reich were members of the AAGL Tissue Extraction Task Force.
In this Q&A, Dr. Wertheim and Dr. Reich discuss:
- options for tissue extraction going forward
- the importance of continuing to offer minimally invasive surgical approaches
- the need to educate surgeons about the safest approaches to tissue extraction.
Both surgeons believe that power morcellation should remain an option for selected cases, although neither performs the technique himself. Both surgeons also believe that minimally invasive approaches to hysterectomy and myomectomy are here to stay and should continue to be used whenever possible.
AAGL convened an impartial expert panel
OBG Management: Dr. Wertheim, could you tell us a little about the AAGL position statement on the use of power morcellation for uterine tissue extraction at hysterectomy or myomectomy, since you were on the task force that researched and wrote it?1
Dr. Wertheim: AAGL convened its task force to conduct a critical appraisal of the existing evidence related to the practice of uterine extraction in the setting of hysterectomy and myomectomy. Areas in need of further investigation also were identified.
The task force consisted of experts who had no conflicts, were not allowed to discuss or review findings with anyone, and were not reimbursed for their time. Our review is the most complete report to date, more comprehensive than the current reports from the FDA, ACOG, the Society of Gynecologic Oncology (SGO), and the American Urogynecologic Society (AUGS).
Interestingly, AAGL, ACOG, SGO, and AUGS all reached the same conclusion: All existing methods of tissue extraction have benefits and risks that must be balanced.
OBG Management: How did the AAGL Task Force assess the evidence?
Dr. Wertheim: The quality of evidence and strength of recommendations were assessed using US Preventive Services Task Force guidelines. There are very few good data on the issue of power morcellation for uterine tissue extraction, especially in regard to leiomyosarcoma. One needs to be careful making recommendations without good data.
Related article: First large study on risk of cancer spread using power morcellation. Janelle Yates (News for your Practice; August 2014)
At this time, we do not believe there is a single method of tissue extraction that can protect all patients. Therefore, all current methods should remain available. We believe that an understanding of the issues will allow surgeons, hospitals, and patients to make the appropriate informed choices regarding tissue extraction for individual patients undergoing uterine surgery.
AAGL recommendations on the use of power morcellationIn its position statement, the AAGL Tissue Extraction Task Force made the following main points, recommending that surgeons:
Further research also is needed to determine how best to diagnose sarcomas preoperatively, the task force noted. The full report is available on the AAGL Web site.1 —Ray A. Wertheim, MD |
How to manage tissue extraction going forward
OBG Management: Regardless of the FDA’s final decision, what should the gynecologic specialty be doing to avoid disseminating uterine tissue in the peritoneal cavity, particularly leiomyosarcoma?
Dr. Wertheim: MIS is a wonderful advancement in women’s health care. All surgical specialties are moving toward MIS. Our challenge is to perform it as safely as possible, given the data and instrumentation available.
In regard to leiomyosarcoma, because we lack the ability to accurately make the diagnosis preoperatively, we’ve identified risk factors that should be taken into consideration. They include advanced age, a history of radiation or tamoxifen use, black race, hereditary leiomyomatosis, renal cell carcinoma syndrome, and survival of childhood retinoblastoma.
At this time, we have specimen-retrieval bags that can be used with power morcellation. However, it takes skill to be able to place a large specimen inside a bag without injuring surrounding organs due to limited visibility.
Education, at the hospital and national level, is in the works
OBG Management: How should we go about educating surgeons about MIS alternatives to open power morcellation?
Dr. Wertheim: In my hospital, we are mentoring surgeons to help them gain the new skills needed. In addition, I plan to give a grand rounds presentation on tissue extraction for hospitals in northern Virginia and also would like to offer a course in the near future. I’m also hoping that we’ll be able to offer courses around the country before the annual AAGL meeting this November.
At the annual AAGL meeting, the subject will be discussed at length, with an emphasis on identifying risk factors and conducting appropriate preoperative testing, with workshops likely to teach the skills needed to perform these surgeries as safely as possible.
Why a return to reliance on laparotomy would be unwise
OBG Management: Given all the concerns expressed recently about open power morcellation, do you think some surgeons will revert to abdominal hysterectomy rather than rely on MIS? Would such a move be safer than power morcellation?
Dr. Wertheim: That would be a disaster for women. Very reliable data have shown that MIS is safer than open surgery, with much quicker recovery. Almost all of my patients are discharged within 3 hours after surgery, and most no longer require pain medications other than nonsteroidal anti-inflammatory drugs by postoperative day 2. They’re usually back to work within 2 weeks.
We have worked long and hard to develop skills and instrumentation required to perform MIS safely—but nothing replaces good judgment. In some cases, laparotomy or conversion to a laparotomy may be indicated.
New instrumentation is needed and is being developed. In the meantime, my personal bias is to rule out risk factors for malignancy and continue to morcellate with a scalpel, preferably inside a bag. After all, we know that with open power morcellation, fragments and cells are usually left behind regardless of inspection and irrigation. These fragments may cause leiomyomatosis, endometriosis, bowel obstruction, sepsis, and possible dissemination of tumor fragments. Moreover, morcellation into small fragments complicates the pathologist’s ability to give an accurate report. The use of open power morcellation also subjects the patient to a risk of damage to surrounding organs—usually due to the surgeon’s inexperience.
As I have said before, our challenge is to perform these surgeries using the safest techniques possible, given the current data and instrumentation.
OBG Management: Dr. Reich, you have a unique perspective on this issue, because you pioneered laparoscopic hysterectomy. How has uterine tissue extraction evolved since then? Do you think open power morcellation should remain an option?
Dr. Reich: Uterine tissue extraction has not evolved. The terms “laparoscopic hysterectomy” and “total laparoscopic hysterectomy” imply vaginal extraction using a scalpel, not abdominal extraction using a morcellator. Unfortunately there is no substitute for hard work using a #10 blade on a long handle and special vaginal retraction tools.
In 1983, I made a decision to stop performing laparotomy for all gynecologic procedures, including hysterectomy, myomectomy, urology, oncology, abscesses, extensive adhesions, and rectovaginal endometriosis. I was an accomplished vaginal surgeon at that time, as well as a one-handed laparoscopic surgeon, operating while looking through the scope with one eye.
Interest in a laparoscopic approach to hysterectomy began with my presentations about laparoscopic hysterectomy in January 1988. At that time I had over 10 years of experience doing what is now called laparoscopic-assisted vaginal hysterectomy.
I wrote extensively about specimen removal using a scalpel before electronic power morcellators were available. Since then, I have asked those using power morcellators to stop calling their operation a laparoscopic hysterectomy, as it has more in common with an abdominal-extraction hysterectomy.
I have never advocated removing the uterus using power morcellators, and I still believe that most specimens can be removed vaginally without the spray of pieces of the specimen around the peritoneal cavity that occurs with power morcellation. This goes for hysterectomy involving a large uterus, myomectomy through a culdotomy incision, and removal of the uterine fundus after supracervical hysterectomy. (It is irresponsible to use expensive power morcellation to remove small supracervical hysterectomy specimens.) It is time to get back to learning and teaching vaginal morcellation, although I readily admit it is time consuming.
Nevertheless, I believe power morcellation should remain an option. Recent laparoscopic fellowship trainees know only this technique, which is still better than a return to mutilation by laparotomy.
Gynecology is a frustrating profession—30 years of MIS as a sideshow. General surgery has rapidly adopted a laparoscopic approach to most operations, after gynecologists taught them. Today most gynecologists do not do advanced laparoscopic surgery and would love to get back to open incision laparotomy for their operations. We cannot go back.
OBG Management: Dr. Wertheim and Dr. Reich, do your personal views of the morcellation issue differ at all from the official views of professional societies?
Dr. Wertheim: Yes. However, before I share them, I’d like to emphasize that the views I’m about to express are mine and mine only, not those of the AAGL or its task force.
The issue of uterine extraction is a highly emotional and political issue, about which there are few good data.
Abundant Level 1 data strongly support a vaginal or laparoscopic approach for benign hysterectomy when possible. ACOG and AAGL have issued position papers supporting these approaches for benign hysterectomies. Gynecologic surgeons and other surgical specialists have embraced MIS because it is safer, offers faster recovery, produces less postoperative pain, and has fewer complications than open surgery. However, AAGL has maintained for several years that morcellation is contraindicated in cases where uterine malignancy is either known or suspected.
The dilemma with open power morcellation is that even with our best diagnostic tools, the rare uterine sarcoma cannot always be definitively ruled out preoperatively. Endometrial cancer usually can be diagnosed before surgery. However, rare subtypes such as sarcomas are more difficult to reliably diagnose preoperatively, and risk factors for uterine sarcomas are not nearly as well understood as those for endometrial cancer.
I do agree with the FDA’s cautionary statement on April 17, which pointedly prohibits power morcellation for women with suspected precancer or known cancer of the gynecologic organs.2 However, the AAGL Task Force critically reviewed about 120 articles, including the studies assessed by the FDA. Concerns arose regarding the FDA’s interpretation of the data. Due to a number of deficiencies in these studies, some of the conclusions of the FDA may not be completely accurate. The studies analyzed by the FDA were not stratified by risk factors for sarcoma and were not necessarily performed in a setting of reproductive-aged women with presumed fibroids.
Dr. Reich: Here are my personal views about the sarcoma problem and I am sure they differ from the official views:
- Laparoscopic hysterectomy should always mean vaginal extraction unless a less disfiguring site can be discovered; power morcellation implies minilaparotomy and should be renamed to reflect that fact.
- Power morcellation must be differentiated from vaginal and minilaparotomy scalpel morcellation, especially in the media. Vaginal hysterectomy has entailed vaginal scalpel morcellation with successful outcomes for more than 100 years.
- Remember that most gynecologic cancers are approached using the laparoscope today. This certainly includes cervical and endometrial cancer and some ovarian cancers. (For example, one of my neighbors is a 25-year survivor of laparoscopically treated bilateral ovarian cancer who refused laparotomy!)
- I have removed sarcomas by vaginal morcellation during laparoscopic hysterectomy and laparoscopic myomectomy with no late sequelae. In fact, most cervical cancer surgery is done by laparoscopic surgery today. And even an open laparotomy hysterectomy can spread a sarcoma.
- The current morcellation debate arose when a single case of disseminated leiomyosarcoma became highly publicized. It involved a prominent physician whose leiomyosarcoma was unknown to her initial surgeon, and the malignancy was upstaged after the use of power morcellation during hysterectomy. After this case was covered in the media, other cases began to be reported in the lay press as well, some of which predated the publicized case. The truth is, regrettably, that sarcomas carry poor prognoses even when specimens are removed intact. And we don’t know much about the sarcoma that started this debate. Was it mild or aggressive? How many mitotic figures were there per high-powered field? And what was found macroscopicallyand microscopically at the subsequent laparotomy? We on the AAGL Task Force do not know the answers to these questions, although at least some of these variables are reported in other published cases. And because this case is likely to have a powerful effect on MIS in our country and the rest of the world, it is my opinion that we need to know these details.
What is your preferred surgical approach?
OBG Management: Do you perform open power morcellation in selected patients?
Dr. Wertheim: Even though I have performed morcellation with a scalpel transvaginally or through a mini-laparotomy incision for many years, I have never used open power morcellation because of the risk of leaving behind benign or malignant tissue fragments. Morcellation with a scalpel is easily learned and can be performed as quickly as power morcellation. Morcellation with a scalpel produces much larger pieces than with power morcellation. This probably markedly decreases the loss of fragments. I cannot make a definitive statement regarding cell loss, however. Until we have improved instrumentation and are better able to make a preoperative diagnosis of sarcoma, I’m going to rule out risk factors identified by the AAGL Task Force, do the appropriate work-up, and continue to morcellate with a scalpel, placing the specimen in a bag, if technically possible.
Dr. Reich: As I mentioned, I am a vaginal scalpel morcellator. I tried power morcellation when it first was developed but was never a fan. The same techniques used for vaginal extraction using a coring maneuver can be used abdominally through the umbilicus or a 1- or 2-cm trocar site.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
1. The Tissue Extraction Task Force, AAGL. AAGL Position Statement: Morcellation during uterine tissue extraction. http://www.aagl.org/wp-content/uploads/2014/05/Tissue_Extraction_TFR.pdf. Accessed June 13, 2014.
2. US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy. FDA Safety Communication. http://www.fda.gov
/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed June 13, 2014.
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy has been in the limelight in 2014—particularly morcellation performed in an “open” fashion (without use of a protective bag). Concerns about the dispersion of tissue throughout the peritoneal cavity—including the risk of disseminating tissue from leiomyosarcoma, a rare but deadly cancer—have drawn statements from the American College of Obstetricians and Gynecologists (ACOG), the AAGL, the US Food and Drug Administration (FDA), and others, cautioning against the use of open power morcellation in women with a known or suspected malignancy.
In July 2014, the FDA convened a two-day hearing of the Obstetrics and Gynecology Devices Panel (one of the panels in its Medical Devices Advisory Committee) to consider whether power morcellation should remain an option and, if so, what restrictions or labeling might be recommended.
In advance of the FDA hearing, OBG Management invited two experts in women’s health to explore the options more deeply and address the future of minimally invasive surgery (MIS): Ray A. Wertheim, MD, Director of the AAGL Center of Excellence Minimally Invasive Gynecology Program at Inova Fair Oaks Hospital in Fairfax, Virginia, and Harry Reich, MD, widely known as the first surgeon to perform laparoscopic hysterectomy, among other achievements. Both Dr. Wertheim and Dr. Reich were members of the AAGL Tissue Extraction Task Force.
In this Q&A, Dr. Wertheim and Dr. Reich discuss:
- options for tissue extraction going forward
- the importance of continuing to offer minimally invasive surgical approaches
- the need to educate surgeons about the safest approaches to tissue extraction.
Both surgeons believe that power morcellation should remain an option for selected cases, although neither performs the technique himself. Both surgeons also believe that minimally invasive approaches to hysterectomy and myomectomy are here to stay and should continue to be used whenever possible.
AAGL convened an impartial expert panel
OBG Management: Dr. Wertheim, could you tell us a little about the AAGL position statement on the use of power morcellation for uterine tissue extraction at hysterectomy or myomectomy, since you were on the task force that researched and wrote it?1
Dr. Wertheim: AAGL convened its task force to conduct a critical appraisal of the existing evidence related to the practice of uterine extraction in the setting of hysterectomy and myomectomy. Areas in need of further investigation also were identified.
The task force consisted of experts who had no conflicts, were not allowed to discuss or review findings with anyone, and were not reimbursed for their time. Our review is the most complete report to date, more comprehensive than the current reports from the FDA, ACOG, the Society of Gynecologic Oncology (SGO), and the American Urogynecologic Society (AUGS).
Interestingly, AAGL, ACOG, SGO, and AUGS all reached the same conclusion: All existing methods of tissue extraction have benefits and risks that must be balanced.
OBG Management: How did the AAGL Task Force assess the evidence?
Dr. Wertheim: The quality of evidence and strength of recommendations were assessed using US Preventive Services Task Force guidelines. There are very few good data on the issue of power morcellation for uterine tissue extraction, especially in regard to leiomyosarcoma. One needs to be careful making recommendations without good data.
Related article: First large study on risk of cancer spread using power morcellation. Janelle Yates (News for your Practice; August 2014)
At this time, we do not believe there is a single method of tissue extraction that can protect all patients. Therefore, all current methods should remain available. We believe that an understanding of the issues will allow surgeons, hospitals, and patients to make the appropriate informed choices regarding tissue extraction for individual patients undergoing uterine surgery.
AAGL recommendations on the use of power morcellationIn its position statement, the AAGL Tissue Extraction Task Force made the following main points, recommending that surgeons:
Further research also is needed to determine how best to diagnose sarcomas preoperatively, the task force noted. The full report is available on the AAGL Web site.1 —Ray A. Wertheim, MD |
How to manage tissue extraction going forward
OBG Management: Regardless of the FDA’s final decision, what should the gynecologic specialty be doing to avoid disseminating uterine tissue in the peritoneal cavity, particularly leiomyosarcoma?
Dr. Wertheim: MIS is a wonderful advancement in women’s health care. All surgical specialties are moving toward MIS. Our challenge is to perform it as safely as possible, given the data and instrumentation available.
In regard to leiomyosarcoma, because we lack the ability to accurately make the diagnosis preoperatively, we’ve identified risk factors that should be taken into consideration. They include advanced age, a history of radiation or tamoxifen use, black race, hereditary leiomyomatosis, renal cell carcinoma syndrome, and survival of childhood retinoblastoma.
At this time, we have specimen-retrieval bags that can be used with power morcellation. However, it takes skill to be able to place a large specimen inside a bag without injuring surrounding organs due to limited visibility.
Education, at the hospital and national level, is in the works
OBG Management: How should we go about educating surgeons about MIS alternatives to open power morcellation?
Dr. Wertheim: In my hospital, we are mentoring surgeons to help them gain the new skills needed. In addition, I plan to give a grand rounds presentation on tissue extraction for hospitals in northern Virginia and also would like to offer a course in the near future. I’m also hoping that we’ll be able to offer courses around the country before the annual AAGL meeting this November.
At the annual AAGL meeting, the subject will be discussed at length, with an emphasis on identifying risk factors and conducting appropriate preoperative testing, with workshops likely to teach the skills needed to perform these surgeries as safely as possible.
Why a return to reliance on laparotomy would be unwise
OBG Management: Given all the concerns expressed recently about open power morcellation, do you think some surgeons will revert to abdominal hysterectomy rather than rely on MIS? Would such a move be safer than power morcellation?
Dr. Wertheim: That would be a disaster for women. Very reliable data have shown that MIS is safer than open surgery, with much quicker recovery. Almost all of my patients are discharged within 3 hours after surgery, and most no longer require pain medications other than nonsteroidal anti-inflammatory drugs by postoperative day 2. They’re usually back to work within 2 weeks.
We have worked long and hard to develop skills and instrumentation required to perform MIS safely—but nothing replaces good judgment. In some cases, laparotomy or conversion to a laparotomy may be indicated.
New instrumentation is needed and is being developed. In the meantime, my personal bias is to rule out risk factors for malignancy and continue to morcellate with a scalpel, preferably inside a bag. After all, we know that with open power morcellation, fragments and cells are usually left behind regardless of inspection and irrigation. These fragments may cause leiomyomatosis, endometriosis, bowel obstruction, sepsis, and possible dissemination of tumor fragments. Moreover, morcellation into small fragments complicates the pathologist’s ability to give an accurate report. The use of open power morcellation also subjects the patient to a risk of damage to surrounding organs—usually due to the surgeon’s inexperience.
As I have said before, our challenge is to perform these surgeries using the safest techniques possible, given the current data and instrumentation.
OBG Management: Dr. Reich, you have a unique perspective on this issue, because you pioneered laparoscopic hysterectomy. How has uterine tissue extraction evolved since then? Do you think open power morcellation should remain an option?
Dr. Reich: Uterine tissue extraction has not evolved. The terms “laparoscopic hysterectomy” and “total laparoscopic hysterectomy” imply vaginal extraction using a scalpel, not abdominal extraction using a morcellator. Unfortunately there is no substitute for hard work using a #10 blade on a long handle and special vaginal retraction tools.
In 1983, I made a decision to stop performing laparotomy for all gynecologic procedures, including hysterectomy, myomectomy, urology, oncology, abscesses, extensive adhesions, and rectovaginal endometriosis. I was an accomplished vaginal surgeon at that time, as well as a one-handed laparoscopic surgeon, operating while looking through the scope with one eye.
Interest in a laparoscopic approach to hysterectomy began with my presentations about laparoscopic hysterectomy in January 1988. At that time I had over 10 years of experience doing what is now called laparoscopic-assisted vaginal hysterectomy.
I wrote extensively about specimen removal using a scalpel before electronic power morcellators were available. Since then, I have asked those using power morcellators to stop calling their operation a laparoscopic hysterectomy, as it has more in common with an abdominal-extraction hysterectomy.
I have never advocated removing the uterus using power morcellators, and I still believe that most specimens can be removed vaginally without the spray of pieces of the specimen around the peritoneal cavity that occurs with power morcellation. This goes for hysterectomy involving a large uterus, myomectomy through a culdotomy incision, and removal of the uterine fundus after supracervical hysterectomy. (It is irresponsible to use expensive power morcellation to remove small supracervical hysterectomy specimens.) It is time to get back to learning and teaching vaginal morcellation, although I readily admit it is time consuming.
Nevertheless, I believe power morcellation should remain an option. Recent laparoscopic fellowship trainees know only this technique, which is still better than a return to mutilation by laparotomy.
Gynecology is a frustrating profession—30 years of MIS as a sideshow. General surgery has rapidly adopted a laparoscopic approach to most operations, after gynecologists taught them. Today most gynecologists do not do advanced laparoscopic surgery and would love to get back to open incision laparotomy for their operations. We cannot go back.
OBG Management: Dr. Wertheim and Dr. Reich, do your personal views of the morcellation issue differ at all from the official views of professional societies?
Dr. Wertheim: Yes. However, before I share them, I’d like to emphasize that the views I’m about to express are mine and mine only, not those of the AAGL or its task force.
The issue of uterine extraction is a highly emotional and political issue, about which there are few good data.
Abundant Level 1 data strongly support a vaginal or laparoscopic approach for benign hysterectomy when possible. ACOG and AAGL have issued position papers supporting these approaches for benign hysterectomies. Gynecologic surgeons and other surgical specialists have embraced MIS because it is safer, offers faster recovery, produces less postoperative pain, and has fewer complications than open surgery. However, AAGL has maintained for several years that morcellation is contraindicated in cases where uterine malignancy is either known or suspected.
The dilemma with open power morcellation is that even with our best diagnostic tools, the rare uterine sarcoma cannot always be definitively ruled out preoperatively. Endometrial cancer usually can be diagnosed before surgery. However, rare subtypes such as sarcomas are more difficult to reliably diagnose preoperatively, and risk factors for uterine sarcomas are not nearly as well understood as those for endometrial cancer.
I do agree with the FDA’s cautionary statement on April 17, which pointedly prohibits power morcellation for women with suspected precancer or known cancer of the gynecologic organs.2 However, the AAGL Task Force critically reviewed about 120 articles, including the studies assessed by the FDA. Concerns arose regarding the FDA’s interpretation of the data. Due to a number of deficiencies in these studies, some of the conclusions of the FDA may not be completely accurate. The studies analyzed by the FDA were not stratified by risk factors for sarcoma and were not necessarily performed in a setting of reproductive-aged women with presumed fibroids.
Dr. Reich: Here are my personal views about the sarcoma problem and I am sure they differ from the official views:
- Laparoscopic hysterectomy should always mean vaginal extraction unless a less disfiguring site can be discovered; power morcellation implies minilaparotomy and should be renamed to reflect that fact.
- Power morcellation must be differentiated from vaginal and minilaparotomy scalpel morcellation, especially in the media. Vaginal hysterectomy has entailed vaginal scalpel morcellation with successful outcomes for more than 100 years.
- Remember that most gynecologic cancers are approached using the laparoscope today. This certainly includes cervical and endometrial cancer and some ovarian cancers. (For example, one of my neighbors is a 25-year survivor of laparoscopically treated bilateral ovarian cancer who refused laparotomy!)
- I have removed sarcomas by vaginal morcellation during laparoscopic hysterectomy and laparoscopic myomectomy with no late sequelae. In fact, most cervical cancer surgery is done by laparoscopic surgery today. And even an open laparotomy hysterectomy can spread a sarcoma.
- The current morcellation debate arose when a single case of disseminated leiomyosarcoma became highly publicized. It involved a prominent physician whose leiomyosarcoma was unknown to her initial surgeon, and the malignancy was upstaged after the use of power morcellation during hysterectomy. After this case was covered in the media, other cases began to be reported in the lay press as well, some of which predated the publicized case. The truth is, regrettably, that sarcomas carry poor prognoses even when specimens are removed intact. And we don’t know much about the sarcoma that started this debate. Was it mild or aggressive? How many mitotic figures were there per high-powered field? And what was found macroscopicallyand microscopically at the subsequent laparotomy? We on the AAGL Task Force do not know the answers to these questions, although at least some of these variables are reported in other published cases. And because this case is likely to have a powerful effect on MIS in our country and the rest of the world, it is my opinion that we need to know these details.
What is your preferred surgical approach?
OBG Management: Do you perform open power morcellation in selected patients?
Dr. Wertheim: Even though I have performed morcellation with a scalpel transvaginally or through a mini-laparotomy incision for many years, I have never used open power morcellation because of the risk of leaving behind benign or malignant tissue fragments. Morcellation with a scalpel is easily learned and can be performed as quickly as power morcellation. Morcellation with a scalpel produces much larger pieces than with power morcellation. This probably markedly decreases the loss of fragments. I cannot make a definitive statement regarding cell loss, however. Until we have improved instrumentation and are better able to make a preoperative diagnosis of sarcoma, I’m going to rule out risk factors identified by the AAGL Task Force, do the appropriate work-up, and continue to morcellate with a scalpel, placing the specimen in a bag, if technically possible.
Dr. Reich: As I mentioned, I am a vaginal scalpel morcellator. I tried power morcellation when it first was developed but was never a fan. The same techniques used for vaginal extraction using a coring maneuver can be used abdominally through the umbilicus or a 1- or 2-cm trocar site.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
The use of power morcellation to remove the uterus or uterine tumors during hysterectomy and myomectomy has been in the limelight in 2014—particularly morcellation performed in an “open” fashion (without use of a protective bag). Concerns about the dispersion of tissue throughout the peritoneal cavity—including the risk of disseminating tissue from leiomyosarcoma, a rare but deadly cancer—have drawn statements from the American College of Obstetricians and Gynecologists (ACOG), the AAGL, the US Food and Drug Administration (FDA), and others, cautioning against the use of open power morcellation in women with a known or suspected malignancy.
In July 2014, the FDA convened a two-day hearing of the Obstetrics and Gynecology Devices Panel (one of the panels in its Medical Devices Advisory Committee) to consider whether power morcellation should remain an option and, if so, what restrictions or labeling might be recommended.
In advance of the FDA hearing, OBG Management invited two experts in women’s health to explore the options more deeply and address the future of minimally invasive surgery (MIS): Ray A. Wertheim, MD, Director of the AAGL Center of Excellence Minimally Invasive Gynecology Program at Inova Fair Oaks Hospital in Fairfax, Virginia, and Harry Reich, MD, widely known as the first surgeon to perform laparoscopic hysterectomy, among other achievements. Both Dr. Wertheim and Dr. Reich were members of the AAGL Tissue Extraction Task Force.
In this Q&A, Dr. Wertheim and Dr. Reich discuss:
- options for tissue extraction going forward
- the importance of continuing to offer minimally invasive surgical approaches
- the need to educate surgeons about the safest approaches to tissue extraction.
Both surgeons believe that power morcellation should remain an option for selected cases, although neither performs the technique himself. Both surgeons also believe that minimally invasive approaches to hysterectomy and myomectomy are here to stay and should continue to be used whenever possible.
AAGL convened an impartial expert panel
OBG Management: Dr. Wertheim, could you tell us a little about the AAGL position statement on the use of power morcellation for uterine tissue extraction at hysterectomy or myomectomy, since you were on the task force that researched and wrote it?1
Dr. Wertheim: AAGL convened its task force to conduct a critical appraisal of the existing evidence related to the practice of uterine extraction in the setting of hysterectomy and myomectomy. Areas in need of further investigation also were identified.
The task force consisted of experts who had no conflicts, were not allowed to discuss or review findings with anyone, and were not reimbursed for their time. Our review is the most complete report to date, more comprehensive than the current reports from the FDA, ACOG, the Society of Gynecologic Oncology (SGO), and the American Urogynecologic Society (AUGS).
Interestingly, AAGL, ACOG, SGO, and AUGS all reached the same conclusion: All existing methods of tissue extraction have benefits and risks that must be balanced.
OBG Management: How did the AAGL Task Force assess the evidence?
Dr. Wertheim: The quality of evidence and strength of recommendations were assessed using US Preventive Services Task Force guidelines. There are very few good data on the issue of power morcellation for uterine tissue extraction, especially in regard to leiomyosarcoma. One needs to be careful making recommendations without good data.
Related article: First large study on risk of cancer spread using power morcellation. Janelle Yates (News for your Practice; August 2014)
At this time, we do not believe there is a single method of tissue extraction that can protect all patients. Therefore, all current methods should remain available. We believe that an understanding of the issues will allow surgeons, hospitals, and patients to make the appropriate informed choices regarding tissue extraction for individual patients undergoing uterine surgery.
AAGL recommendations on the use of power morcellationIn its position statement, the AAGL Tissue Extraction Task Force made the following main points, recommending that surgeons:
Further research also is needed to determine how best to diagnose sarcomas preoperatively, the task force noted. The full report is available on the AAGL Web site.1 —Ray A. Wertheim, MD |
How to manage tissue extraction going forward
OBG Management: Regardless of the FDA’s final decision, what should the gynecologic specialty be doing to avoid disseminating uterine tissue in the peritoneal cavity, particularly leiomyosarcoma?
Dr. Wertheim: MIS is a wonderful advancement in women’s health care. All surgical specialties are moving toward MIS. Our challenge is to perform it as safely as possible, given the data and instrumentation available.
In regard to leiomyosarcoma, because we lack the ability to accurately make the diagnosis preoperatively, we’ve identified risk factors that should be taken into consideration. They include advanced age, a history of radiation or tamoxifen use, black race, hereditary leiomyomatosis, renal cell carcinoma syndrome, and survival of childhood retinoblastoma.
At this time, we have specimen-retrieval bags that can be used with power morcellation. However, it takes skill to be able to place a large specimen inside a bag without injuring surrounding organs due to limited visibility.
Education, at the hospital and national level, is in the works
OBG Management: How should we go about educating surgeons about MIS alternatives to open power morcellation?
Dr. Wertheim: In my hospital, we are mentoring surgeons to help them gain the new skills needed. In addition, I plan to give a grand rounds presentation on tissue extraction for hospitals in northern Virginia and also would like to offer a course in the near future. I’m also hoping that we’ll be able to offer courses around the country before the annual AAGL meeting this November.
At the annual AAGL meeting, the subject will be discussed at length, with an emphasis on identifying risk factors and conducting appropriate preoperative testing, with workshops likely to teach the skills needed to perform these surgeries as safely as possible.
Why a return to reliance on laparotomy would be unwise
OBG Management: Given all the concerns expressed recently about open power morcellation, do you think some surgeons will revert to abdominal hysterectomy rather than rely on MIS? Would such a move be safer than power morcellation?
Dr. Wertheim: That would be a disaster for women. Very reliable data have shown that MIS is safer than open surgery, with much quicker recovery. Almost all of my patients are discharged within 3 hours after surgery, and most no longer require pain medications other than nonsteroidal anti-inflammatory drugs by postoperative day 2. They’re usually back to work within 2 weeks.
We have worked long and hard to develop skills and instrumentation required to perform MIS safely—but nothing replaces good judgment. In some cases, laparotomy or conversion to a laparotomy may be indicated.
New instrumentation is needed and is being developed. In the meantime, my personal bias is to rule out risk factors for malignancy and continue to morcellate with a scalpel, preferably inside a bag. After all, we know that with open power morcellation, fragments and cells are usually left behind regardless of inspection and irrigation. These fragments may cause leiomyomatosis, endometriosis, bowel obstruction, sepsis, and possible dissemination of tumor fragments. Moreover, morcellation into small fragments complicates the pathologist’s ability to give an accurate report. The use of open power morcellation also subjects the patient to a risk of damage to surrounding organs—usually due to the surgeon’s inexperience.
As I have said before, our challenge is to perform these surgeries using the safest techniques possible, given the current data and instrumentation.
OBG Management: Dr. Reich, you have a unique perspective on this issue, because you pioneered laparoscopic hysterectomy. How has uterine tissue extraction evolved since then? Do you think open power morcellation should remain an option?
Dr. Reich: Uterine tissue extraction has not evolved. The terms “laparoscopic hysterectomy” and “total laparoscopic hysterectomy” imply vaginal extraction using a scalpel, not abdominal extraction using a morcellator. Unfortunately there is no substitute for hard work using a #10 blade on a long handle and special vaginal retraction tools.
In 1983, I made a decision to stop performing laparotomy for all gynecologic procedures, including hysterectomy, myomectomy, urology, oncology, abscesses, extensive adhesions, and rectovaginal endometriosis. I was an accomplished vaginal surgeon at that time, as well as a one-handed laparoscopic surgeon, operating while looking through the scope with one eye.
Interest in a laparoscopic approach to hysterectomy began with my presentations about laparoscopic hysterectomy in January 1988. At that time I had over 10 years of experience doing what is now called laparoscopic-assisted vaginal hysterectomy.
I wrote extensively about specimen removal using a scalpel before electronic power morcellators were available. Since then, I have asked those using power morcellators to stop calling their operation a laparoscopic hysterectomy, as it has more in common with an abdominal-extraction hysterectomy.
I have never advocated removing the uterus using power morcellators, and I still believe that most specimens can be removed vaginally without the spray of pieces of the specimen around the peritoneal cavity that occurs with power morcellation. This goes for hysterectomy involving a large uterus, myomectomy through a culdotomy incision, and removal of the uterine fundus after supracervical hysterectomy. (It is irresponsible to use expensive power morcellation to remove small supracervical hysterectomy specimens.) It is time to get back to learning and teaching vaginal morcellation, although I readily admit it is time consuming.
Nevertheless, I believe power morcellation should remain an option. Recent laparoscopic fellowship trainees know only this technique, which is still better than a return to mutilation by laparotomy.
Gynecology is a frustrating profession—30 years of MIS as a sideshow. General surgery has rapidly adopted a laparoscopic approach to most operations, after gynecologists taught them. Today most gynecologists do not do advanced laparoscopic surgery and would love to get back to open incision laparotomy for their operations. We cannot go back.
OBG Management: Dr. Wertheim and Dr. Reich, do your personal views of the morcellation issue differ at all from the official views of professional societies?
Dr. Wertheim: Yes. However, before I share them, I’d like to emphasize that the views I’m about to express are mine and mine only, not those of the AAGL or its task force.
The issue of uterine extraction is a highly emotional and political issue, about which there are few good data.
Abundant Level 1 data strongly support a vaginal or laparoscopic approach for benign hysterectomy when possible. ACOG and AAGL have issued position papers supporting these approaches for benign hysterectomies. Gynecologic surgeons and other surgical specialists have embraced MIS because it is safer, offers faster recovery, produces less postoperative pain, and has fewer complications than open surgery. However, AAGL has maintained for several years that morcellation is contraindicated in cases where uterine malignancy is either known or suspected.
The dilemma with open power morcellation is that even with our best diagnostic tools, the rare uterine sarcoma cannot always be definitively ruled out preoperatively. Endometrial cancer usually can be diagnosed before surgery. However, rare subtypes such as sarcomas are more difficult to reliably diagnose preoperatively, and risk factors for uterine sarcomas are not nearly as well understood as those for endometrial cancer.
I do agree with the FDA’s cautionary statement on April 17, which pointedly prohibits power morcellation for women with suspected precancer or known cancer of the gynecologic organs.2 However, the AAGL Task Force critically reviewed about 120 articles, including the studies assessed by the FDA. Concerns arose regarding the FDA’s interpretation of the data. Due to a number of deficiencies in these studies, some of the conclusions of the FDA may not be completely accurate. The studies analyzed by the FDA were not stratified by risk factors for sarcoma and were not necessarily performed in a setting of reproductive-aged women with presumed fibroids.
Dr. Reich: Here are my personal views about the sarcoma problem and I am sure they differ from the official views:
- Laparoscopic hysterectomy should always mean vaginal extraction unless a less disfiguring site can be discovered; power morcellation implies minilaparotomy and should be renamed to reflect that fact.
- Power morcellation must be differentiated from vaginal and minilaparotomy scalpel morcellation, especially in the media. Vaginal hysterectomy has entailed vaginal scalpel morcellation with successful outcomes for more than 100 years.
- Remember that most gynecologic cancers are approached using the laparoscope today. This certainly includes cervical and endometrial cancer and some ovarian cancers. (For example, one of my neighbors is a 25-year survivor of laparoscopically treated bilateral ovarian cancer who refused laparotomy!)
- I have removed sarcomas by vaginal morcellation during laparoscopic hysterectomy and laparoscopic myomectomy with no late sequelae. In fact, most cervical cancer surgery is done by laparoscopic surgery today. And even an open laparotomy hysterectomy can spread a sarcoma.
- The current morcellation debate arose when a single case of disseminated leiomyosarcoma became highly publicized. It involved a prominent physician whose leiomyosarcoma was unknown to her initial surgeon, and the malignancy was upstaged after the use of power morcellation during hysterectomy. After this case was covered in the media, other cases began to be reported in the lay press as well, some of which predated the publicized case. The truth is, regrettably, that sarcomas carry poor prognoses even when specimens are removed intact. And we don’t know much about the sarcoma that started this debate. Was it mild or aggressive? How many mitotic figures were there per high-powered field? And what was found macroscopicallyand microscopically at the subsequent laparotomy? We on the AAGL Task Force do not know the answers to these questions, although at least some of these variables are reported in other published cases. And because this case is likely to have a powerful effect on MIS in our country and the rest of the world, it is my opinion that we need to know these details.
What is your preferred surgical approach?
OBG Management: Do you perform open power morcellation in selected patients?
Dr. Wertheim: Even though I have performed morcellation with a scalpel transvaginally or through a mini-laparotomy incision for many years, I have never used open power morcellation because of the risk of leaving behind benign or malignant tissue fragments. Morcellation with a scalpel is easily learned and can be performed as quickly as power morcellation. Morcellation with a scalpel produces much larger pieces than with power morcellation. This probably markedly decreases the loss of fragments. I cannot make a definitive statement regarding cell loss, however. Until we have improved instrumentation and are better able to make a preoperative diagnosis of sarcoma, I’m going to rule out risk factors identified by the AAGL Task Force, do the appropriate work-up, and continue to morcellate with a scalpel, placing the specimen in a bag, if technically possible.
Dr. Reich: As I mentioned, I am a vaginal scalpel morcellator. I tried power morcellation when it first was developed but was never a fan. The same techniques used for vaginal extraction using a coring maneuver can be used abdominally through the umbilicus or a 1- or 2-cm trocar site.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
1. The Tissue Extraction Task Force, AAGL. AAGL Position Statement: Morcellation during uterine tissue extraction. http://www.aagl.org/wp-content/uploads/2014/05/Tissue_Extraction_TFR.pdf. Accessed June 13, 2014.
2. US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy. FDA Safety Communication. http://www.fda.gov
/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed June 13, 2014.
1. The Tissue Extraction Task Force, AAGL. AAGL Position Statement: Morcellation during uterine tissue extraction. http://www.aagl.org/wp-content/uploads/2014/05/Tissue_Extraction_TFR.pdf. Accessed June 13, 2014.
2. US Food and Drug Administration. Laparoscopic uterine power morcellation in hysterectomy and myomectomy. FDA Safety Communication. http://www.fda.gov
/medicaldevices/safety/alertsandnotices/ucm393576.htm. Published April 17, 2014. Accessed June 13, 2014.
Visit the Morcellation Topic Collection Page for additional articles, videos, and audiocasts.