User login
Delayed diagnosis of breast cancer: $15M award
Delayed diagnosis of breast cancer: $15M award
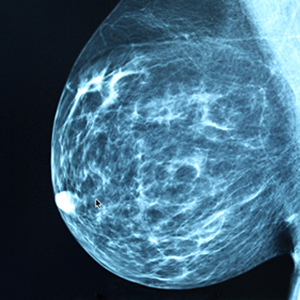
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Sexual harassment and medicine
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
Sexual harassment hit a peak of cultural awareness over the past year. Will medicine be the next field to experience a reckoning?
In 2017, Time magazine’s Person of the Year Award went to the Silence Breakers who spoke out against sexual assault and harassment.1 The exposure of predatory behavior exhibited by once-celebrated movie producers, newscasters, and actors has given rise to a powerful change. The #MeToo movement has risen to support survivors and end sexual violence.
Just like show business, other industries have rich histories of discrimination and power. Think Wall Street, Silicon Valley, hospitality services, and the list goes on and on.2 But what about medicine? To answer this question, this article aims to:
- review the dilemma
- explore our duty to our patients and each other
- discuss solutions to address the problem.
Sexual harassment: A brief history
Decades ago, Anita Hill accused U.S. Supreme Court nominee Clarence Thomas, her boss at the U.S. Department of Education and the Equal Employment Opportunity Commission (EEOC), of sexual harassment.3
The year was 1991, and President George H. W. Bush had nominated Thomas, a federal Circuit Judge, to succeed retiring Associate Supreme Court Justice Thurgood Marshall. With Thomas’s good character presented as a primary qualification, he appeared to be a sure thing.
Continue to: That was until an FBI interview...
That was until an FBI interview of Hill was leaked to the press. Hill asserted that Thomas had sexually harassed her while he was her supervisor at the Department of Education and the EEOC.4 Heavily scrutinized for her choice to follow Thomas to a second job after he had already allegedly harassed her, Hill was in a conundrum shared by many women—putting up with abuse in exchange for a reputable position and the opportunity to fulfill a career ambition.
Hill is a trailblazer for women yearning to speak the truth, and she brought national attention to sexual harassment in the early 1990s. On December 16, 2017, the Commission on Sexual Harassment and Advancing Equality in the Workplace was formed. Hill was selected to lead the charge against sexual harassment in the entertainment industry.5
A forensic assessment of harassment
Hill’s courageous story is one of many touched upon in the 2016 book Because of Sex.6 Author Gillian Thomas, a senior staff attorney with the American Civil Liberties Union’s Women’s Rights Project, explores how Title VII of the Civil Rights Act of 1964 made it illegal to discriminate “because of sex.”
The field of forensic psychiatry has long been attentive to themes of sexual harassment and discrimination. The American Academy of Psychiatry and Law has a robust list of landmark cases thought to be especially important and significant for forensic psychiatry.7 This list includes cases brought forth by tenacious, yet ordinary women who used the law to advocate, and some have taken their fight all the way to the Supreme Court. Let’s consider 2 such cases:
Meritor Savings Bank, FSB v Vinson (1986).8 This was a U.S. labor law case. Michelle Vinson rose through the ranks at Meritor Savings Bank, only to be fired for excessive sick leave. She filed a Title VII suit against the bank. Vinson alleged that the bank was liable for sexual harassment perpetrated by its employee and vice president, Sidney Taylor. Vinson claimed that there had been 40 to 50 sexual encounters over 4 years, ranging from fondling to indecent exposure to rape. Vinson asserted that she never reported these events for fear of losing her job. The Supreme Court, in a 9-to-0 decision, recognized sexual harassment as a violation of Title VII of the Civil Rights Act of 1964.
Continue to: Harris v Forklift Systems, Inc. (1993)
Harris v Forklift Systems, Inc. (1993).9 Teresa Harris, a manager at Forklift Systems, Inc., claimed that the company’s president frequently directed offensive remarks at her that were sexual and discriminatory. The Supreme Court clarified the definition of a “hostile” or “abusive” work environment under Title VII of the Civil Rights Act of 1964. Associate Justice Sandra Day O’Connor was joined by a unanimous majority opinion in agreement with Harris.
Physicians are not immune
Clinicians are affected by sexual harassment, too. We have a duty to protect our patients, colleagues, and ourselves. Psychiatrists in particular often are on the frontlines of helping victims process their trauma.10
But will the field of medicine also face a reckoning when it comes to perpetrating harassment? It seems likely that the medical field would be ripe with harassment when you consider its history of male domination and a hierarchical structure with strong power differentials—not to mention the late nights, exhaustion, easy access to beds, and late-night encounters where inhibitions may be lowered.11
A shocking number of female doctors are sexually harassed. Thirty percent of the top female clinician-researchers have experienced blatant sexual harassment on the job, according to a survey of 573 men and 493 women who received career development awards from the National Institutes of Health in 2006 to 2009.12 In this survey, harassment covered the scope of sexist remarks or behavior, unwanted sexual advances, bribery, threats, and coercion. The majority of those affected said the experience undermined their confidence as professionals, and many said the harassment negatively affected their career advancement.12
Continue to: But what about the progress women have made...
But what about the progress women have made in medicine? Women are surpassing men in terms of admittance to medical school. Last year, for the first time, women accounted for more than half of the enrollees in U.S. medical schools, according to the Association of American Medical Colleges.13 Yet there has been a stalling in terms of change when it comes to harassment.12 Women may be more vulnerable to harassment, both when they’re perceived as weak and when they’re so strong that they challenge traditional hierarchies.
Perpetuating the problem is the trouble with reporting sexual harassment. Victims do not fare well in our society. Even in the #MeToo era, reporting such behavior is far from straightforward.11 Women fear that reporting any harassment will make them a target. Think of Anita Hill—her testimony against Clarence Thomas during his confirmation hearings for the Supreme Court showed that women who report sexual harassment experience marginalization, retaliation, stigmatization, and worse.
The result is that medical professionals tend to suppress the recognition of harassment. We make excuses for it, blame ourselves, or just take it on the chin and move on. There’s also confusion regarding what constitutes harassment. As doctors, especially psychiatrists, we hear harrowing stories. It’s reasonable to downplay our own experiences. Turning everyone into a victim of sexual harassment could detract from the stories of women who were raped, molested, and severely taken advantage of. There is a reasonable fear that diluting their message could be further damaging.14
Time for action
The field of medicine needs to do better in terms of education, support, anticipation, prevention, and reaction to harassment. We have the awareness. Now, we need action.
Continue to: One way to change any culture...
One way to change any culture of harassment or discrimination would be the advancement of more female physicians into leadership positions. The Association of American Medical Colleges has reported that fewer women than men hold faculty positions and full professorships.15,16 There’s also a striking imbalance among fields of medicine practiced by men and women, with more women seen in pediatrics, obstetrics, and gynecology as opposed to surgery. Advancement into policy-setting echelons of medicine is essential for change. Sexual harassment can be a silent problem that will be corrected only when institutions and leaders put it on the forefront of discussions.17
Another possible solution would be to shift problem-solving from punishment to prevention. Many institutions set expectations about intolerance of sexual harassment and conduct occasional lectures about it. However, enforcing protocols and safeguards that support and enforce policy are difficult on the ground level. In any event, punishment alone won’t change a culture.17
Working with students until they are comfortable disclosing details of incidents can be helpful. For example, the University of Wisconsin-Madison employs an ombuds to help with this process.18 All institutions should encourage reporting along confidential pathways and have multiple ways to report.17 Tracking complaints, even seemingly minor infractions, can help identify patterns of behavior and anticipate future incidents.
Some solutions seem obvious, such as informal and retaliation-free reporting that allows institutions to track perpetrators’ behavior; mandatory training that includes bystander training; and disciplining and monitoring transgressors and terminating their employment when appropriate—something along the lines of a zero-tolerance policy. There needs to be more research on the prevalence, severity, and outcomes of sexual harassment, and subsequent investigations, along with research into evidence-based prevention and intervention strategies.17
Continue to: Although this article focuses...
Although this article focuses on harassment of women, men are equally important to this conversation because they, too, can be victims. Men also can serve a pivotal role in mentoring and championing their female counterparts as they strive for advancement, equality, and respect.
The task ahead is large, and this discussion is not over.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
1. Felsenthal E. TIME’s 2017 Person of the Year: the Silence Breakers. TIME. http://time.com/magazine/us/5055335/december-18th-2017-vol-190-no-25-u-s/. Published December 18, 2017. Accessed April 23, 2018.
2. Hiltzik M. Los Angeles Times. Will medicine be the next field to face a sexual harassment reckoning? http://www.latimes.com/business/hiltzik/la-fi-hiltzik-medicine-harassment-20180110-story.html. Published January 10, 2018. Accessed April 23, 2018.
3. Thompson K. For Anita Hill, the Clarence Thomas hearings haven’t really ended. The Washington Post. https://www.washingtonpost.com/politics/for-anita-hill-the-clarence-thomas-hearings-havent-really-ended/2011/10/05/gIQAy2b5QL_story.html. Published October 6, 2011. Accessed April 23, 2018.
4. Toobin J. Good versus evil. In: Toobin J. The nine: inside the secret world of the Supreme Court. New York, NY: Doubleday; 2007:30-32.
5. Barnes B. Motion picture academy finds no merit to accusations against its president. https://www.nytimes.com/2018/03/28/business/media/john-bailey-sexual-harassment-academy.html. The New York Times. Published March 28, 2018. Accessed April 23, 2018.
6. Thomas G. Because of sex: one law, ten cases, and fifty years that changed American women’s lives at work. New York, NY: Picador; 2016.
7. Landmark cases 2014. American Academy of Psychiatry and Law. http://www.aapl.org/landmark_list.htm. 2014. Accessed April 22, 2018.
8. Meritor Savings Bank v Vinson, 477 US 57 (1986).
9. Harris v Forklift Systems, Inc., 114 S Ct 367 (1993).
10. Okwerekwu JA. #MeToo: so many of my patients have a story. And absorbing them is taking its toll. STAT. https://www.scribd.com/article/367482959/Me-Too-So-Many-Of-My-Patients-Have-A-Story-And-Absorbing-Them-Is-Taking-Its-Toll. Published December 18, 2017. Accessed April 23, 2018.
11. Jagsi R. Sexual harassment in medicine—#MeToo. N Engl J Med. 2018;378:209-211.
12. Jagsi R, Griffith KA, Jones R. et al. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120-2121.
13. AAMCNEWS. More women than men enrolled in U.S. medical schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed May 4, 2018.
14. Miller D. #MeToo: does it help? Clinical Psychiatry News. https://www.mdedge.com/psychiatry/article/150148/depression/metoo-does-it-help. Published October 24, 2017. Accessed April 23, 2018.
15. Chang S, Morahan PS, Magrane D, et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt). 2016;25(7):687-696.
16. Lautenberger DM, Dandar, VM, Raezer CL, et al. The state of women in academic medicine: the pipeline and pathways to leadership, 2013-2014. AAMC. https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Published 2014. Accessed May 4, 2018.
17. Jablow M. Zero tolerance: combating sexual harassment in academic medicine. AAMCNews. https://news.aamc.org/diversity/article/combating-sexual-harassment-academic-medicine. Published April 4, 2017. Accessed April 23, 2018.
18. University of Wisconsin-Madison, the School of Medicine and Public Health. UW-Madison Policy on Sexual Harassment and Sexual Violence. https://compliance.wiscweb.wisc.edu/wp-content/uploads/sites/102/2018/01/UW-Madison-Policy-on-Sexual-Harassment-And-Sexual-Violence-January-2018.pdf. Published January 2018. Accessed April 22, 2018.
Lessons from a daunting malpractice event
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
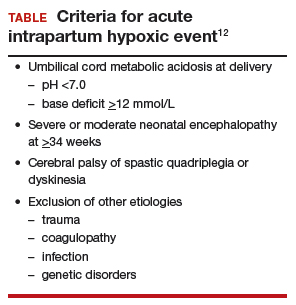
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
CASE Failure to perform cesarean delivery1–4
A 19-year-old woman (G1P0) received prenatal care at a federally funded health center. Her pregnancy was normal without complications. She presented to the hospital after spontaneous rupture of membranes (SROM). The on-call ObGyn employed by the clinic was offsite when the mother was admitted.
The mother signed a standard consent form for vaginal and cesarean deliveries and any other surgical procedure required during the course of giving birth.
The ObGyn ordered low-dose oxytocin to augment labor in light of her SROM. Oxytocin was started at 9:46
Upon delivery, the infant was flaccid and not breathing. His Apgar scores were 2, 3, and 6 at 1, 5, and 10 minutes, respectively, and the cord pH was 7. The neonatal intensive care (NICU) team provided aggressive resuscitation.
At the time of trial, the 18-month-old boy was being fed through a percutaneous endoscopic gastrostomy tube and had a tracheostomy that required periodic suctioning. The child was not able to stand, crawl, or support himself, and will require 24-hour nursing care for the rest of his life.
LAWSUIT. The parents filed a lawsuit in federal court for damages under the Federal Tort Claims Act (see “Notes about this case,”). The mother claimed that she had requested a cesarean delivery early in labor when FHR tracings showed fetal distress, and again prior to vacuum extraction; the ObGyn refused both times.
The ObGyn claimed that when he noted a category III tracing, he recommended cesarean delivery, but the patient refused. He recorded the refusal in the chart some time later, after he had noted the neonate’s appearance.
The parents’ expert testified that restarting oxytocin and using vacuum extraction multiple times were dangerous and gross deviations from acceptable practice. Prolonged and repetitive use of the vacuum extractor caused a large subgaleal hematoma that decreased blood flow to the fetal brain, resulting in irreversible central nervous system (CNS) damage secondary to hypoxic ischemic encephalopathy. An emergency cesarean delivery should have been performed at the first sign of fetal distress.
The defense expert pointed out that the ObGyn discussed the need for cesarean delivery with the patient when fetal distress occurred and that the ObGyn was bedside and monitoring the fetus and the mother. Although the mother consented to a cesarean delivery at time of admission, she refused to allow the procedure.
The labor and delivery (L&D) nurse corroborated the mother’s story that a cesarean delivery was not offered by the ObGyn, and when the patient asked for a cesarean delivery, he refused. The nurse stated that the note added to the records by the ObGyn about the mother’s refusal was a lie. If the mother had refused a cesarean, the nurse would have documented the refusal by completing a Refusal of Treatment form that would have been faxed to the risk manager. No such form was required because nothing was ever offered that the mother refused.
The nurse also testified that during the course of the latter part of labor, the ObGyn left the room several times to assist other patients, deliver another baby, and make an 8-minute phone call to his stockbroker. She reported that the ObGyn was out of the room when delivery occurred.
WHAT’S THE VERDICT?
Read about the verdict and medical considerations.
WHAT’S THE VERDICT?
The medical care and the federal-court bench trial held in front of a judge (not a jury) occurred in Florida. The verdict suggests that the ObGyn breached the standard of care by not offering or proceeding with a cesarean delivery and this management resulted in the child’s injuries. The court awarded damages in the amount of $33,813,495.91, including $29,413,495.91 for the infant; $3,300,000.00 for the plaintiff; and $1,100,000.00 for her spouse.4
Medical considerations
Refusal of medical care
Although it appears that in this case the patient did not actually refuse medical care (cesarean delivery), the case does raise the question of refusal. Refusal of medical care has been addressed by the American College of Obstetricians and Gynecologists (ACOG) predicated upon care that supports maternal and fetal wellbeing.5 There may be a fine balance between safeguarding the pregnant woman’s autonomy and optimization of fetal wellbeing. “Forced compliance,” on the other hand, is the alternative to respecting refusal of treatment. Ethical issues come into play: patient rights; respect for autonomy; violations of bodily integrity; power differentials; and gender equality.5 The use of coercion is “not only ethically impermissible but also medically inadvisable secondary to the realities of prognostic uncertainty and the limitations of medical knowledge.”5 There is an obligation to elicit the patient’s reasoning and lived experience. Perhaps most importantly, as clinicians working to achieve a resolution, consideration of the following is appropriate5:
- reliability and validity of evidence-based medicine
- severity of the prospective outcome
- degree of risk or burden placed on the patient
- patient understanding of the gravity of the situation and risks
- degree of urgency.
Much of this boils down to the obligation to discuss “risks and benefits of treatment, alternatives and consequences of refusing treatment.”6
Complications from vacuum-assisted vaginal delivery
Ghidini and associates, in a multicenter retrospective study, evaluated complications relating to vacuum-assisted delivery. They listed major primary outcomes of subgaleal hemorrhage, skull fracture, and intracranial bleeding, and minor primary outcomes of cephalohematoma, scalp laceration, and extensive skin abrasions. Secondary outcomes included a 5-minute Apgar score of <7, umbilical artery pH of <7.10, shoulder dystocia, and NICU admission.7
A retrospective study from Sweden assessing all vacuum deliveries over a 2-year period compared the use of the Kiwi OmniCup (Clinical Innovations) to use of the Malmström metal cup (Medela). No statistical differences in maternal or neonatal outcomes as well as failure rates were noted. However, the duration of the procedure was longer and the requirement for fundal pressure was higher with the Malmström device.8
Subgaleal hemorrhage. Ghidini and colleagues reported a heightened incidence of head injury related to the duration of vacuum application and birth weight.7 Specifically, vacuum delivery devices increase the risk of subgaleal hemorrhage. Blood can accumulate between the scalp’s epicranial aponeurosis and the periosteum and potentially can extend forward to the orbital margins, backward to the nuchal ridge, and laterally to the temporal fascia. As much as 260 mL of blood can get into this subaponeurotic space in term babies.9 Up to one-quarter of babies who require NICU admission for this condition die.10 This injury seldom occurs with forceps.
Shoulder dystocia. In a meta-analysisfrom Italy, the vacuum extractor was associated with increased risk of shoulder dystocia compared with spontaneous vaginal delivery.11
Intrapartum hypoxia. In 2003, the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy defined an acute intrapartum hypoxic event (TABLE).12
Cerebral palsy (CP) is defined as “a chronic neuromuscular disability characterized by aberrant control of movement or posture appearing early in life and not the result of recognized progressive disease.”13,14
The Collaborative Perinatal Project concluded that birth trauma plays a minimal role in development of CP.15 Arrested labor, use of oxytocin, or prolonged labor did not play a role. CP can develop following significant cerebral or posterior fossa hemorrhage in term infants.16
Perinatal asphyxia is a poor and imprecise term and use of the expression should be abandoned. Overall, 90% of children with CP do not have birth asphyxia as the underlying etiology.14
Prognostic assessment can be made, in part, by using the Sarnat classification system (classification scale for hypoxic-ischemic encephalopathy of the newborn) or an electroencephalogram to stratify the severity of neonatal encephalopathy.12 Such tests are not stand-alone but a segment of assessment. At this point “a better understanding of the processes leading to neonatal encephalopathy and associated outcomes” appear to be required to understand and associate outcomes.12 “More accurate and reliable tools (are required) for prognostic forecasting.”12
Hypoxic-ischemic encephalopathy involves multisystem organ failure including renal, hepatic, hematologic, cardiac, gastrointestinal, and metabolic abnormalities. There is no correlation between the degree of CNS injury and level of other organ abnormalities.12
Differential diagnosis
When events such as those described in this case occur, develop a differential diagnosis by considering the following12:
- uterine rupture
- severe placental abruption
- umbilical cord prolapse
- amniotic fluid embolus
- maternal cardiovascular collapse
- fetal exsanguination.
Read about the legal considerations.
Legal considerations
Although ObGyns are among the specialties most likely to experience malpractice claims,17 a verdict of more than $33 million is unusual.18 Despite the failure of adequate care, and the enormous damages, the ObGyn involved probably will not be responsible for paying the verdict (see “Notes about this case”). The case presents a number of important lessons and reminders for anyone practicing obstetrics.
A procedural comment
The case in this article arose under the Federal Tort Claims Act (FTCA).1 Most government entities have sovereign immunity, meaning that they can be sued only with their consent. In the FTCA, the federal government consented to being sued for the acts of its employees. This right has a number of limitations and some technical procedures, but at its core, it permits the United States to be sued as though it was a private individual.2 Private individuals can be sued for the acts of the agents (including employees).
Although the FTCA is a federal law, and these cases are tried in federal court, the substantive law of the state applies. This case occurred in Florida, so Florida tort law, defenses, and limitation on claims applied here also. Had the events occurred in Iowa, Iowa law would have applied.
In FTCA cases, the United States is the defendant (generally it is the government, not the employee who is the defendant).3 In this case, the ObGyn was employed by a federal government entity to provide delivery services. As a result, the United States was the primary defendant, had the obligation to defend the suit, and will almost certainly be obligated to pay the verdict.
The case facts
Although this description is based on an actual case, the facts were taken from the opinion of the trial court, legal summaries and press reports and not from the full case documents.4-7 We could not independently assess the accuracy of the facts, but for the purpose of this discussion, we have assumed the facts to be correct. The government has apparently filed an appeal in the Eleventh Circuit.
References
- Federal Tort Claims Act. Vol 28 U.S.C. Pt.VI Ch.171 and 28 U.S.C. § 1346(b).
- About the Federal Tort Claims Act (FTCA). Health Resources & Services Administration: Health Center Program. https://bphc.hrsa.gov/ftca/about/index.html. Accessed May 16, 2018.
- Dowell MA, Scott CD. Federally Qualified Health Center Federal Tort Claims Act Insurance Coverage. Health Law. 2015;5:31-43.
- Chang D. Miami doctor's call to broker during baby's delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed January 11, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17-18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
Very large verdict
The extraordinary size of this verdict ($33 million without any punitive damages) is a reminder that in obstetrics, mistakes can have catastrophic consequences and very high costs.19 This fact is reflected in malpractice insurance rates.
A substantial amount of this case’s award will provide around-the-clock care for the child. This verdict was not the result of a runaway jury—it was a judge’s decision. It is also noteworthy to report that a small percentage of physicians (1%) appear responsible for a significant number (about one-third) of paid claims.20
Although the size of the verdict is unusual, the case is a fairly straightforward negligence tort. The judge found that the ObGyn had breached the duty of care for his patient. The actions that fell below the standard of care included restarting the oxytocin, using the Kiwi vacuum device 3 times, and failing to perform a cesarean delivery in light of obvious fetal distress. That negligence caused injury to the infant (and his parents).21 The judge determined that the 4 elements of negligence were present: 1) duty of care, 2) breach of that duty, 3) injury, and 4) a causal link between the breach of duty and the injury. The failure to adhere to good practice standards practically defines breach of duty.22
Multitasking
One important lesson is that multitasking, absence, and inattention can look terrible when things go wrong. Known as “hindsight bias,” the awareness that there was a disastrous result makes it easier to attribute the outcome to small mistakes that otherwise might seem trivial. This ObGyn was in and out of the room during a difficult labor. Perhaps that was understandable if it were unavoidable because of another delivery, but being absent frequently and not present for the delivery now looks very significant.23 And, of course, the 8-minute phone call to the stockbroker shines as a heartless, self-centered act of inattention.
Manipulating the record
Another lesson of this case: Do not manipulate the record. The ObGyn recorded that the patient had refused the cesarean delivery he recommended. Had that been the truth, it would have substantially improved his case. But apparently it was not the truth. Although there was circumstantial evidence (the charting of the patient’s refusal only after the newborn’s condition was obvious, failure to complete appropriate hospital forms), the most damning evidence was the direct testimony of the L&D nurse. She reported that, contrary to what the ObGyn put in the chart, the patient requested a cesarean delivery. In truth, it was the ObGyn who had refused.
A physician who is dishonest with charting—making false statements or going back or “correcting” a chart later—loses credibility and the presumption of acting in good faith. That is disastrous for the physician.24
A hidden lesson
Another lesson, more human than legal, is that it matters how patients are treated when things go wrong. According to press reports, the parents felt that the ObGyn had not recognized that he had made any errors, did not apologize, and had even blamed the mother for the outcome. It does not require graduate work in psychology to expect that this approach would make the parents angry enough to pursue legal action. True regret, respect, and apologies are not panaceas, but they are important.25 Who gets sued and why is a key question that is part of a larger risk management plan. In this case, the magnitude of the injuries made a suit very likely, which is not the case with all bad outcomes.26 Honest communication with patients in the face of bad results remains the goal.27
Pulling it all together
Clinicians must always remain cognizant that the patient comes first and of the importance of working as a team with nursing staff and other allied health professionals. Excellent communication and support staff interaction in good times and bad can make a difference in patient outcomes and, indeed, in medical malpractice verdicts.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
- Chang D. Miami doctor’s call to broker during baby’s delivery leads to $33.8 million judgment. Miami Herald. http://www.miamiherald.com/news/health-care/article147506019.html. Published April 28, 2017. Accessed May 16, 2018.
- Teller SE. $33.8 Million judgment reached in malpractice lawsuit. Legal Reader. https://www.legalreader.com/33-8-million-judgment-reached/. Published May 2017. Accessed May 16, 2018.
- Laska L. Medical Malpractice: Verdicts, Settlements, & Experts. 2017;33(11):17−18.
- Dixon v. U.S. Civil Action No. 15-23502-Civ-Scola. LEAGLE.com. https://www.leagle.com/decision/infdco20170501s18. Published April 28, 2017. Accessed May 8, 2018.
- American College of Obstetricians and Gynecologists Committee on Ethics. Committee Opinion No. 664: Refusal of medically recommended treatment during pregnancy. Obstet Gynecol. 2016;126(6):e175−e182.
- American College of Obstetricians and Gynecologists. Professional liability and risk management an essential guide for obstetrician-gynecologist. 3rd ed. Washington, DC: 2014.
- Ghidini A, Stewart D, Pezzullo J, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017;295(1):67−73.
- Turkmen S. Maternal and neonatal outcomes in vacuum-assisted delivery with the Kiwi OmniCup and Malmstrom metal cup. J Obstet Gynaecol Res. 2015;41(2):207−213.
- Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452−1453.
- Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32(3):228−232.
- Dall’Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and metanalysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;201:62−68.
- American College of Obstetricians and Gynecologists Task Force on Neonatal Encephalopathy. Neonatal Encephalopathy and Neurologic Outcomes. 2nd ed. Washington, DC: 2014.
- Nelson K, Ellenberg J. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981;68:36−44.
- ACOG Technical Bulletin No. 163: Fetal and neonatal neurologic injury. Int J. Gynaecol Obstet. 1993;41(1):97−101.
- Nelson K, Ellenberg J. Antecedents of cerebral palsy. I. Univariate analysis of risks. Am J Dis Child. 1985;139(10):1031−1038.
- Fenichel GM, Webster D, Wong WK. Intracranial hemorrhage in the term newborn. Arch Neurol. 1984;41(1):30−34.
- Peckham C. Medscape Malpractice Report 2015: Why Ob/Gyns Get Sued. Medscape. https://www.medscape.com/features/slideshow/malpractice-report-2015/obgyn#page=1. Published January 2016. Accessed May 16, 2018.
- Bixenstine PJ, Shore AD, Mehtsun WT, Ibrahim AM, Freischlag JA, Makary MA. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014;36(4):43−53.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: Targeting the most injurious neonatal adverse events. J Healthc Risk Manag. 2015;34(4):20−27.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and characteristics of physicians prone to malpractice claims. N Engl J Med. 2016;374(4):354−362.
- Levine AS. Legal 101: Tort law and medical malpractice for physicians. Contemp OBGYN. http://www.contem poraryobgyn.net/obstetrics-gynecology-womens-health/legal-101-tort-law-and-medical-malpractice-physicians. Published July 17, 2015. Accessed May 8, 2018.
- Smith SR, Sanfilippo JS. Applied Business Law. In: Sanfilippo JS, Bieber EJ, Javitch DG, Siegrist RB, eds. MBA for Healthcare. New York, NY: Oxford University Press; 2016:91−126.
- Glaser LM, Alvi FA, Milad MP. Trends in malpractice claims for obstetric and gynecologic procedures, 2005 through 2014. Am J Obstet Gynecol. 2017;217(3):340.e1–e6.
- Seegert L. Malpractice pitfalls: 5 strategies to reduce lawsuit threats. Medical Econ. http://www.medicaleconomics.com/medical-economics-blog/5-strategies-reduce-malpractice-lawsuit-threats. Published November 10, 2016. Accessed May 8, 2018.
- Peckham C. Malpractice and medicine: who gets sued and why? Medscape. http://www.medscape.com/viewarticle/855229. Published December 8, 2015. Accessed May 16, 2018.
- McMichael B. The failure of ‘sorry’: an empirical evaluation of apology laws, health care, and medical malpractice. Social Science Research Network. https://papers.ssrn.com/abstract=3020352. Published August 16, 2017. Accessed May 16, 2018.
- Carranza L, Lyerly AD, Lipira L, Prouty CD, Loren D, Gallagher TH. Delivering the truth: challenges and opportunities for error disclosure in obstetrics. Obstet Gynecol. 2014;123(3):656−659.
Did unsafe oxytocin dose cause uterine rupture? $3.5M settlement
Did unsafe oxytocin dose cause uterine rupture? $3.5M settlement
When a mother presented to the hospital in labor, the on-call ObGyn ordered oxytocin with the dosage to be increased by 2 mU/min until she was receiving 30 mU/min or until an adequate contraction pattern was achieved and maintained. Over the next few hours, the labor and delivery nurse increased the dosage of the infusion several times.
As the patient began to push, a trickle of bright red blood was seen coming from her vagina and the baby's heart tones were temporarily lost. When the fetal heart tones were restored, his heart rate was approximately 50 bpm. After vaginal delivery was attempted using vacuum extraction and forceps, an emergency cesarean delivery was performed, leading to the finding that the mother's uterus had ruptured.
The baby suffered a permanent brain injury due to hypoxic-ischemic encephalopathy.
PATIENT'S CLAIM: The mother sued the hospital and on-call ObGyn. She alleged that the health care providers breached the standard of care by negligently increasing and maintaining the oxytocin at unsafe levels, which caused the mother's uterus to be overworked and eventually rupture. The rupture led to the child's hypoxia. An expert ObGyn noted that the patient's contractions were adequate by the time the oxytocin dose reached 14 mU/min, but the dosage continued to be increased.
DEFENDANTS' DEFENSE: The case was settled during the trial.
VERDICT: A $3.5 million Kansas settlement was reached.
When did the bowel injury occur?
One day after undergoing a hysterectomy, a woman went to the emergency department (ED) because she was feeling ill. She received a diagnosis of a pulmonary embolism for which she was given anticoagulant medications. The patient's symptoms persisted. Computed tomography (CT) imaging showed a bowel injury, and, 17 days after the initial surgery, an emergency laparotomy was performed.
PATIENT'S CLAIM: The patient sued the surgeon and the hospital. The hospital settled before the trial and the case continued against the surgeon.
The patient's early symptoms after surgery were evidence of a bowel injury, but imaging was not undertaken for several days. If the imaging had been undertaken earlier, the bowel injury would have been detected before it caused a rectovaginal fistula. An expert pathologist testified that the microscopic findings he detected postlaparotomy could only exist if a bowel perforation had been there for a significant period of time before the fistula developed. The patient's experts argued that the injury was not a "free perforation," but had been contained by her body, preventing the spread of the infection.
DEFENDANTS' DEFENSE: The surgeon maintained that the injury did not occur during the hysterectomy but developed in the days just before it was discovered. Over time, a collection of infected fluid at the vaginal cuff eroded into the bowel above it, creating an entryway for stool to pass through. Continuous leakage from the bowel for 17 days (the length of time between development of symptoms and discovery of the bowel injury) would have likely resulted in the patient's death.
VERDICT: A Missouri defense verdict was returned.
Did improper delivery techniques caused brachial plexus injury? $950,000 settlement
In April, a woman began receiving prenatal care for her 7th pregnancy. Her history of maternal obesity and diabetes mellitus, physical examinations, and tests suggested that she was at increased risk for having a macrosomic baby and encountering shoulder dystocia during vaginal delivery.
At 37 weeks' gestation, the mother was admitted to the hospital for induction of labor. Shoulder dystocia was encountered during delivery. At birth, the baby weighed 9 lb 10 oz and her right arm was limp. She was found to have a right brachial plexus injury involving C5‒C8 nerve roots and muscles. Two nerve root avulsions were evident on MRI and visualized by the surgeon during an extensive nerve graft operation. Arm function and range of motion improved after surgery, but the child has not recovered normal use of her arm.
PARENTS' CLAIM: Under the standard of care, the ObGyn was required to obtain informed consent, including a discussion of the risks of vaginal delivery (shoulder dystocia and brachial plexus injury), and the option of cesarean delivery. The patient claimed that the ObGyn neither obtained informed consent nor discussed these risks with her.
The labor and delivery nurse reported that the ObGyn told her, before delivery, that he was expecting a large baby and, perhaps, shoulder dystocia.
The ObGyn deviated from the standard of care by applying more than gentle traction to the fetal head while the shoulder was still impacted. The injury to the baby's right brachial plexus resulted from excessive lateral traction used by the ObGyn. The injury would not have occurred if a cesarean delivery had been performed. The mechanism of maternal forces injuring a brachial plexus nerve has never been visualized by any physician and is an unproven hypothesis.
PHYSICIAN'S DEFENSE: The ObGyn reported using standard maneuvers to deliver the baby. He applied traction on the fetal head 3 times: once after McRoberts maneuver, once after suprapubic pressure, and once after delivery of the posterior arm. He dictated into his notes that "We had to be careful to avoid excessive tractive forces." He claimed that shoulder dystocia is an unpredictable and unpreventable obstetric emergency, and that the injury was caused by the maternal forces of labor.
VERDICT: A $950,000 Virginia settlement was reached.
Wrongful death claim
On March 13, a 76-year-old woman went to her primary care physician's office because of a vaginal discharge. A nurse practitioner (NP) diagnosed a urinary tract infection (UTI) and prescribed cefixime (Suprax). Four days later, the patient began to experience severe diarrhea and blamed the medication. At a follow-up visit on March 20, the NP switched the patient to sulfamethoxazole-trimethoprim (Bactrim).
The following day, the patient was found unresponsive on her bathroom floor and was taken to the ED. It was determined that she had Clostridium difficile colitis (C difficile) and was admitted to the hospital. She developed acute renal failure, metabolic acidosis, hypovolemia, hypotension, and tachycardia. When she went into cardiac arrest, attempts to resuscitate her failed. She died on March 22.
ESTATE'S CLAIM: The estate sued the NP, claiming that the patient's symptoms did not meet the criteria for a UTI. If appropriate tests had been performed, the correct diagnosis would have been made and she could have received potentially life-saving treatment.
DEFENDANTS' DEFENSE: The NP claimed there was no negligence. Her diagnosis and treatment of the patient's condition were appropriate in all respects. The development of C difficile is a risk of any antibiotic.
VERDICT: An Indiana defense verdict was returned.
Nuchal cord: Undisclosed settlement
During delivery, the labor and delivery nurses lost the fetal heart-rate (FHR) monitor tracing, resulting in their being unaware of increasing signs of fetal intolerance to labor. The nurses continued to administer oxytocin to induce labor.
At birth, a nuchal cord was identified. The baby was born without signs of life but was successfully resuscitated by hospital staff.
The baby was found to have sustained severe brain damage as a result of profound fetal hypoxia. The child will require 24-hour nursing and supportive care for as long as she lives.
PARENTS' CLAIM: The nurses and ObGyn breached the standard of care resulting in her child's severe brain damage. The hospital nurses failed to continuously monitor the FHR. Profound brain damage was preventable in this case.
DEFENDANTS' DEFENSE: The nurses continuously monitored by listening to sounds coming out of the bedside monitor even though no taping of FHR was occurring on the central monitors or FHR monitor strip. A nuchal cord is an unforeseeable medical emergency; nothing different could have been done to change the outcome.
VERDICT: An undisclosed Texas settlement was reached.
Surgical needle left near bladder
The patient underwent a hysterectomy on July 9. Because of an injury sustained during the operation, bladder repair surgery was performed on July 19. After that surgery, she reported bleeding and urinary incontinence. Results of a computed tomography (CT) scan showed that the bladder repair was not successful, a vesicovaginal fistula had developed, and a 13-mm C-shaped needle was found near her bladder. A third operation to remove the needle from her abdomen took place on August 16.
PATIENT'S CLAIM: The needle left behind after the second surgery caused a fistula to develop. The patient suffered mental and emotional distress from knowing the needle was in her abdomen. Foreign objects left in a patient during surgery are strong evidence of negligence.
DEFENDANTS' DEFENSE: The primary defense claim was the absence of causation--any negligence did not cause the injury. Defense experts testified that the needle was on top of the bladder and did move anywhere to cause damage. The patient developed a vesicovaginal fistula due to complications from the bladder repair operation and not from the needle. In addition, there was testimony that the third surgery was unnecessary because the needle would eventually flush out of the abdomen without causing damage.
VERDICT: A Michigan defense verdict was returned.
Claims cancer diagnosis was delayed
On October 1, 2008, a woman saw her family physician (FP) for routine care. Blood work results showed an elevated white blood cell (WBC) count. The patient claimed that the FP did not inform her of these test results.
One year later, the patient went to an urgent care facility where blood work was performed; the results showed a high WBC count. After a work-up, the patient was given a presumptive diagnosis of mantel cell lymphoma. By December 9, she had undergone the first round of chemotherapy. Subsequent tests revealed that the presumptive diagnosis was incorrect; she actually had low-grade lymphoproliferative disorder.
In lieu of this new diagnosis, the medical team offered the patient the option of discontinuing chemotherapy. She decided, however, to continue the treatment. Chemotherapy was followed by 2 years of rituximab/hyaluronidase human maintenance therapy.
PATIENT'S CLAIM: The patient presented her case to a medical review board. The course of treatment (chemotherapy plus maintenance therapy) left her with permanent heart damage and an elevated risk of developing secondary cancer.
The patient claimed that none of this would have happened if her FP had informed her of the October 2008 test results and recommended appropriate follow-up studies. The results of those studies would have given her the correct diagnosis and allowed her to receive prompt, proper treatment. The medical review board responded unanimously that the FP's conduct constituted a breach of the standard of care, but concluded that the breach was not a factor in the patient's damages.
The patient filed suit against the FP. An expert in internal medicine commented that, based on the 2008 WBC count, the tests should have been repeated and the patient should have been referred to a hematologist/oncologist. Failure to do so increased the patient's risk of developing cancer in the future.
DEFENDANTS' DEFENSE: The FP denied any breach of standard of care. According to her notes, she had shared test results with the patient on November 26 and recommended following up with repeat blood work. The FP blamed the patient for failing to follow-up as recommended.
VERDICT: An Indiana defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Did unsafe oxytocin dose cause uterine rupture? $3.5M settlement
When a mother presented to the hospital in labor, the on-call ObGyn ordered oxytocin with the dosage to be increased by 2 mU/min until she was receiving 30 mU/min or until an adequate contraction pattern was achieved and maintained. Over the next few hours, the labor and delivery nurse increased the dosage of the infusion several times.
As the patient began to push, a trickle of bright red blood was seen coming from her vagina and the baby's heart tones were temporarily lost. When the fetal heart tones were restored, his heart rate was approximately 50 bpm. After vaginal delivery was attempted using vacuum extraction and forceps, an emergency cesarean delivery was performed, leading to the finding that the mother's uterus had ruptured.
The baby suffered a permanent brain injury due to hypoxic-ischemic encephalopathy.
PATIENT'S CLAIM: The mother sued the hospital and on-call ObGyn. She alleged that the health care providers breached the standard of care by negligently increasing and maintaining the oxytocin at unsafe levels, which caused the mother's uterus to be overworked and eventually rupture. The rupture led to the child's hypoxia. An expert ObGyn noted that the patient's contractions were adequate by the time the oxytocin dose reached 14 mU/min, but the dosage continued to be increased.
DEFENDANTS' DEFENSE: The case was settled during the trial.
VERDICT: A $3.5 million Kansas settlement was reached.
When did the bowel injury occur?
One day after undergoing a hysterectomy, a woman went to the emergency department (ED) because she was feeling ill. She received a diagnosis of a pulmonary embolism for which she was given anticoagulant medications. The patient's symptoms persisted. Computed tomography (CT) imaging showed a bowel injury, and, 17 days after the initial surgery, an emergency laparotomy was performed.
PATIENT'S CLAIM: The patient sued the surgeon and the hospital. The hospital settled before the trial and the case continued against the surgeon.
The patient's early symptoms after surgery were evidence of a bowel injury, but imaging was not undertaken for several days. If the imaging had been undertaken earlier, the bowel injury would have been detected before it caused a rectovaginal fistula. An expert pathologist testified that the microscopic findings he detected postlaparotomy could only exist if a bowel perforation had been there for a significant period of time before the fistula developed. The patient's experts argued that the injury was not a "free perforation," but had been contained by her body, preventing the spread of the infection.
DEFENDANTS' DEFENSE: The surgeon maintained that the injury did not occur during the hysterectomy but developed in the days just before it was discovered. Over time, a collection of infected fluid at the vaginal cuff eroded into the bowel above it, creating an entryway for stool to pass through. Continuous leakage from the bowel for 17 days (the length of time between development of symptoms and discovery of the bowel injury) would have likely resulted in the patient's death.
VERDICT: A Missouri defense verdict was returned.
Did improper delivery techniques caused brachial plexus injury? $950,000 settlement
In April, a woman began receiving prenatal care for her 7th pregnancy. Her history of maternal obesity and diabetes mellitus, physical examinations, and tests suggested that she was at increased risk for having a macrosomic baby and encountering shoulder dystocia during vaginal delivery.
At 37 weeks' gestation, the mother was admitted to the hospital for induction of labor. Shoulder dystocia was encountered during delivery. At birth, the baby weighed 9 lb 10 oz and her right arm was limp. She was found to have a right brachial plexus injury involving C5‒C8 nerve roots and muscles. Two nerve root avulsions were evident on MRI and visualized by the surgeon during an extensive nerve graft operation. Arm function and range of motion improved after surgery, but the child has not recovered normal use of her arm.
PARENTS' CLAIM: Under the standard of care, the ObGyn was required to obtain informed consent, including a discussion of the risks of vaginal delivery (shoulder dystocia and brachial plexus injury), and the option of cesarean delivery. The patient claimed that the ObGyn neither obtained informed consent nor discussed these risks with her.
The labor and delivery nurse reported that the ObGyn told her, before delivery, that he was expecting a large baby and, perhaps, shoulder dystocia.
The ObGyn deviated from the standard of care by applying more than gentle traction to the fetal head while the shoulder was still impacted. The injury to the baby's right brachial plexus resulted from excessive lateral traction used by the ObGyn. The injury would not have occurred if a cesarean delivery had been performed. The mechanism of maternal forces injuring a brachial plexus nerve has never been visualized by any physician and is an unproven hypothesis.
PHYSICIAN'S DEFENSE: The ObGyn reported using standard maneuvers to deliver the baby. He applied traction on the fetal head 3 times: once after McRoberts maneuver, once after suprapubic pressure, and once after delivery of the posterior arm. He dictated into his notes that "We had to be careful to avoid excessive tractive forces." He claimed that shoulder dystocia is an unpredictable and unpreventable obstetric emergency, and that the injury was caused by the maternal forces of labor.
VERDICT: A $950,000 Virginia settlement was reached.
Wrongful death claim
On March 13, a 76-year-old woman went to her primary care physician's office because of a vaginal discharge. A nurse practitioner (NP) diagnosed a urinary tract infection (UTI) and prescribed cefixime (Suprax). Four days later, the patient began to experience severe diarrhea and blamed the medication. At a follow-up visit on March 20, the NP switched the patient to sulfamethoxazole-trimethoprim (Bactrim).
The following day, the patient was found unresponsive on her bathroom floor and was taken to the ED. It was determined that she had Clostridium difficile colitis (C difficile) and was admitted to the hospital. She developed acute renal failure, metabolic acidosis, hypovolemia, hypotension, and tachycardia. When she went into cardiac arrest, attempts to resuscitate her failed. She died on March 22.
ESTATE'S CLAIM: The estate sued the NP, claiming that the patient's symptoms did not meet the criteria for a UTI. If appropriate tests had been performed, the correct diagnosis would have been made and she could have received potentially life-saving treatment.
DEFENDANTS' DEFENSE: The NP claimed there was no negligence. Her diagnosis and treatment of the patient's condition were appropriate in all respects. The development of C difficile is a risk of any antibiotic.
VERDICT: An Indiana defense verdict was returned.
Nuchal cord: Undisclosed settlement
During delivery, the labor and delivery nurses lost the fetal heart-rate (FHR) monitor tracing, resulting in their being unaware of increasing signs of fetal intolerance to labor. The nurses continued to administer oxytocin to induce labor.
At birth, a nuchal cord was identified. The baby was born without signs of life but was successfully resuscitated by hospital staff.
The baby was found to have sustained severe brain damage as a result of profound fetal hypoxia. The child will require 24-hour nursing and supportive care for as long as she lives.
PARENTS' CLAIM: The nurses and ObGyn breached the standard of care resulting in her child's severe brain damage. The hospital nurses failed to continuously monitor the FHR. Profound brain damage was preventable in this case.
DEFENDANTS' DEFENSE: The nurses continuously monitored by listening to sounds coming out of the bedside monitor even though no taping of FHR was occurring on the central monitors or FHR monitor strip. A nuchal cord is an unforeseeable medical emergency; nothing different could have been done to change the outcome.
VERDICT: An undisclosed Texas settlement was reached.
Surgical needle left near bladder
The patient underwent a hysterectomy on July 9. Because of an injury sustained during the operation, bladder repair surgery was performed on July 19. After that surgery, she reported bleeding and urinary incontinence. Results of a computed tomography (CT) scan showed that the bladder repair was not successful, a vesicovaginal fistula had developed, and a 13-mm C-shaped needle was found near her bladder. A third operation to remove the needle from her abdomen took place on August 16.
PATIENT'S CLAIM: The needle left behind after the second surgery caused a fistula to develop. The patient suffered mental and emotional distress from knowing the needle was in her abdomen. Foreign objects left in a patient during surgery are strong evidence of negligence.
DEFENDANTS' DEFENSE: The primary defense claim was the absence of causation--any negligence did not cause the injury. Defense experts testified that the needle was on top of the bladder and did move anywhere to cause damage. The patient developed a vesicovaginal fistula due to complications from the bladder repair operation and not from the needle. In addition, there was testimony that the third surgery was unnecessary because the needle would eventually flush out of the abdomen without causing damage.
VERDICT: A Michigan defense verdict was returned.
Claims cancer diagnosis was delayed
On October 1, 2008, a woman saw her family physician (FP) for routine care. Blood work results showed an elevated white blood cell (WBC) count. The patient claimed that the FP did not inform her of these test results.
One year later, the patient went to an urgent care facility where blood work was performed; the results showed a high WBC count. After a work-up, the patient was given a presumptive diagnosis of mantel cell lymphoma. By December 9, she had undergone the first round of chemotherapy. Subsequent tests revealed that the presumptive diagnosis was incorrect; she actually had low-grade lymphoproliferative disorder.
In lieu of this new diagnosis, the medical team offered the patient the option of discontinuing chemotherapy. She decided, however, to continue the treatment. Chemotherapy was followed by 2 years of rituximab/hyaluronidase human maintenance therapy.
PATIENT'S CLAIM: The patient presented her case to a medical review board. The course of treatment (chemotherapy plus maintenance therapy) left her with permanent heart damage and an elevated risk of developing secondary cancer.
The patient claimed that none of this would have happened if her FP had informed her of the October 2008 test results and recommended appropriate follow-up studies. The results of those studies would have given her the correct diagnosis and allowed her to receive prompt, proper treatment. The medical review board responded unanimously that the FP's conduct constituted a breach of the standard of care, but concluded that the breach was not a factor in the patient's damages.
The patient filed suit against the FP. An expert in internal medicine commented that, based on the 2008 WBC count, the tests should have been repeated and the patient should have been referred to a hematologist/oncologist. Failure to do so increased the patient's risk of developing cancer in the future.
DEFENDANTS' DEFENSE: The FP denied any breach of standard of care. According to her notes, she had shared test results with the patient on November 26 and recommended following up with repeat blood work. The FP blamed the patient for failing to follow-up as recommended.
VERDICT: An Indiana defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Did unsafe oxytocin dose cause uterine rupture? $3.5M settlement
When a mother presented to the hospital in labor, the on-call ObGyn ordered oxytocin with the dosage to be increased by 2 mU/min until she was receiving 30 mU/min or until an adequate contraction pattern was achieved and maintained. Over the next few hours, the labor and delivery nurse increased the dosage of the infusion several times.
As the patient began to push, a trickle of bright red blood was seen coming from her vagina and the baby's heart tones were temporarily lost. When the fetal heart tones were restored, his heart rate was approximately 50 bpm. After vaginal delivery was attempted using vacuum extraction and forceps, an emergency cesarean delivery was performed, leading to the finding that the mother's uterus had ruptured.
The baby suffered a permanent brain injury due to hypoxic-ischemic encephalopathy.
PATIENT'S CLAIM: The mother sued the hospital and on-call ObGyn. She alleged that the health care providers breached the standard of care by negligently increasing and maintaining the oxytocin at unsafe levels, which caused the mother's uterus to be overworked and eventually rupture. The rupture led to the child's hypoxia. An expert ObGyn noted that the patient's contractions were adequate by the time the oxytocin dose reached 14 mU/min, but the dosage continued to be increased.
DEFENDANTS' DEFENSE: The case was settled during the trial.
VERDICT: A $3.5 million Kansas settlement was reached.
When did the bowel injury occur?
One day after undergoing a hysterectomy, a woman went to the emergency department (ED) because she was feeling ill. She received a diagnosis of a pulmonary embolism for which she was given anticoagulant medications. The patient's symptoms persisted. Computed tomography (CT) imaging showed a bowel injury, and, 17 days after the initial surgery, an emergency laparotomy was performed.
PATIENT'S CLAIM: The patient sued the surgeon and the hospital. The hospital settled before the trial and the case continued against the surgeon.
The patient's early symptoms after surgery were evidence of a bowel injury, but imaging was not undertaken for several days. If the imaging had been undertaken earlier, the bowel injury would have been detected before it caused a rectovaginal fistula. An expert pathologist testified that the microscopic findings he detected postlaparotomy could only exist if a bowel perforation had been there for a significant period of time before the fistula developed. The patient's experts argued that the injury was not a "free perforation," but had been contained by her body, preventing the spread of the infection.
DEFENDANTS' DEFENSE: The surgeon maintained that the injury did not occur during the hysterectomy but developed in the days just before it was discovered. Over time, a collection of infected fluid at the vaginal cuff eroded into the bowel above it, creating an entryway for stool to pass through. Continuous leakage from the bowel for 17 days (the length of time between development of symptoms and discovery of the bowel injury) would have likely resulted in the patient's death.
VERDICT: A Missouri defense verdict was returned.
Did improper delivery techniques caused brachial plexus injury? $950,000 settlement
In April, a woman began receiving prenatal care for her 7th pregnancy. Her history of maternal obesity and diabetes mellitus, physical examinations, and tests suggested that she was at increased risk for having a macrosomic baby and encountering shoulder dystocia during vaginal delivery.
At 37 weeks' gestation, the mother was admitted to the hospital for induction of labor. Shoulder dystocia was encountered during delivery. At birth, the baby weighed 9 lb 10 oz and her right arm was limp. She was found to have a right brachial plexus injury involving C5‒C8 nerve roots and muscles. Two nerve root avulsions were evident on MRI and visualized by the surgeon during an extensive nerve graft operation. Arm function and range of motion improved after surgery, but the child has not recovered normal use of her arm.
PARENTS' CLAIM: Under the standard of care, the ObGyn was required to obtain informed consent, including a discussion of the risks of vaginal delivery (shoulder dystocia and brachial plexus injury), and the option of cesarean delivery. The patient claimed that the ObGyn neither obtained informed consent nor discussed these risks with her.
The labor and delivery nurse reported that the ObGyn told her, before delivery, that he was expecting a large baby and, perhaps, shoulder dystocia.
The ObGyn deviated from the standard of care by applying more than gentle traction to the fetal head while the shoulder was still impacted. The injury to the baby's right brachial plexus resulted from excessive lateral traction used by the ObGyn. The injury would not have occurred if a cesarean delivery had been performed. The mechanism of maternal forces injuring a brachial plexus nerve has never been visualized by any physician and is an unproven hypothesis.
PHYSICIAN'S DEFENSE: The ObGyn reported using standard maneuvers to deliver the baby. He applied traction on the fetal head 3 times: once after McRoberts maneuver, once after suprapubic pressure, and once after delivery of the posterior arm. He dictated into his notes that "We had to be careful to avoid excessive tractive forces." He claimed that shoulder dystocia is an unpredictable and unpreventable obstetric emergency, and that the injury was caused by the maternal forces of labor.
VERDICT: A $950,000 Virginia settlement was reached.
Wrongful death claim
On March 13, a 76-year-old woman went to her primary care physician's office because of a vaginal discharge. A nurse practitioner (NP) diagnosed a urinary tract infection (UTI) and prescribed cefixime (Suprax). Four days later, the patient began to experience severe diarrhea and blamed the medication. At a follow-up visit on March 20, the NP switched the patient to sulfamethoxazole-trimethoprim (Bactrim).
The following day, the patient was found unresponsive on her bathroom floor and was taken to the ED. It was determined that she had Clostridium difficile colitis (C difficile) and was admitted to the hospital. She developed acute renal failure, metabolic acidosis, hypovolemia, hypotension, and tachycardia. When she went into cardiac arrest, attempts to resuscitate her failed. She died on March 22.
ESTATE'S CLAIM: The estate sued the NP, claiming that the patient's symptoms did not meet the criteria for a UTI. If appropriate tests had been performed, the correct diagnosis would have been made and she could have received potentially life-saving treatment.
DEFENDANTS' DEFENSE: The NP claimed there was no negligence. Her diagnosis and treatment of the patient's condition were appropriate in all respects. The development of C difficile is a risk of any antibiotic.
VERDICT: An Indiana defense verdict was returned.
Nuchal cord: Undisclosed settlement
During delivery, the labor and delivery nurses lost the fetal heart-rate (FHR) monitor tracing, resulting in their being unaware of increasing signs of fetal intolerance to labor. The nurses continued to administer oxytocin to induce labor.
At birth, a nuchal cord was identified. The baby was born without signs of life but was successfully resuscitated by hospital staff.
The baby was found to have sustained severe brain damage as a result of profound fetal hypoxia. The child will require 24-hour nursing and supportive care for as long as she lives.
PARENTS' CLAIM: The nurses and ObGyn breached the standard of care resulting in her child's severe brain damage. The hospital nurses failed to continuously monitor the FHR. Profound brain damage was preventable in this case.
DEFENDANTS' DEFENSE: The nurses continuously monitored by listening to sounds coming out of the bedside monitor even though no taping of FHR was occurring on the central monitors or FHR monitor strip. A nuchal cord is an unforeseeable medical emergency; nothing different could have been done to change the outcome.
VERDICT: An undisclosed Texas settlement was reached.
Surgical needle left near bladder
The patient underwent a hysterectomy on July 9. Because of an injury sustained during the operation, bladder repair surgery was performed on July 19. After that surgery, she reported bleeding and urinary incontinence. Results of a computed tomography (CT) scan showed that the bladder repair was not successful, a vesicovaginal fistula had developed, and a 13-mm C-shaped needle was found near her bladder. A third operation to remove the needle from her abdomen took place on August 16.
PATIENT'S CLAIM: The needle left behind after the second surgery caused a fistula to develop. The patient suffered mental and emotional distress from knowing the needle was in her abdomen. Foreign objects left in a patient during surgery are strong evidence of negligence.
DEFENDANTS' DEFENSE: The primary defense claim was the absence of causation--any negligence did not cause the injury. Defense experts testified that the needle was on top of the bladder and did move anywhere to cause damage. The patient developed a vesicovaginal fistula due to complications from the bladder repair operation and not from the needle. In addition, there was testimony that the third surgery was unnecessary because the needle would eventually flush out of the abdomen without causing damage.
VERDICT: A Michigan defense verdict was returned.
Claims cancer diagnosis was delayed
On October 1, 2008, a woman saw her family physician (FP) for routine care. Blood work results showed an elevated white blood cell (WBC) count. The patient claimed that the FP did not inform her of these test results.
One year later, the patient went to an urgent care facility where blood work was performed; the results showed a high WBC count. After a work-up, the patient was given a presumptive diagnosis of mantel cell lymphoma. By December 9, she had undergone the first round of chemotherapy. Subsequent tests revealed that the presumptive diagnosis was incorrect; she actually had low-grade lymphoproliferative disorder.
In lieu of this new diagnosis, the medical team offered the patient the option of discontinuing chemotherapy. She decided, however, to continue the treatment. Chemotherapy was followed by 2 years of rituximab/hyaluronidase human maintenance therapy.
PATIENT'S CLAIM: The patient presented her case to a medical review board. The course of treatment (chemotherapy plus maintenance therapy) left her with permanent heart damage and an elevated risk of developing secondary cancer.
The patient claimed that none of this would have happened if her FP had informed her of the October 2008 test results and recommended appropriate follow-up studies. The results of those studies would have given her the correct diagnosis and allowed her to receive prompt, proper treatment. The medical review board responded unanimously that the FP's conduct constituted a breach of the standard of care, but concluded that the breach was not a factor in the patient's damages.
The patient filed suit against the FP. An expert in internal medicine commented that, based on the 2008 WBC count, the tests should have been repeated and the patient should have been referred to a hematologist/oncologist. Failure to do so increased the patient's risk of developing cancer in the future.
DEFENDANTS' DEFENSE: The FP denied any breach of standard of care. According to her notes, she had shared test results with the patient on November 26 and recommended following up with repeat blood work. The FP blamed the patient for failing to follow-up as recommended.
VERDICT: An Indiana defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Chief complaint: Homicidal. Assessing violence risk
Mr. F, age 35, is homeless and has a history of cocaine and alcohol use disorders. He is admitted voluntarily to the psychiatric unit because he has homicidal thoughts toward Ms. S, who works in the shelter where he has been staying. Mr. F reports that he is thinking of killing Ms. S if he is discharged because she has been rude to him. He states that he has access to several firearms, but he will not disclose the location. He has been diagnosed with unspecified depressive disorder and exhibited antisocial personality disorder traits. He is being treated with sertraline. However, his mood appears to be relatively stable, except for occasional angry verbal outbursts. The outbursts have been related to intrusive peers or staff turning the television off for group meetings. Mr. F has been joking with peers, eating well, and sleeping appropriately. He reports no suicidal thoughts and has not been physically violent on the unit. However, Mr. F has had a history of violence since his teenage years. He has been incarcerated twice for assault and once for drug possession.
How would you approach assessing and managing Mr. F’s risk for violence?
We all have encountered a patient similar to Mr. F on the psychiatric unit or in the emergency department—a patient who makes violent threats and appears angry, intimidating, manipulative, and/or demanding, despite exhibiting no evidence of mania or psychosis. This patient often has a history of substance abuse and a lifelong pattern of viewing violence as an acceptable way of addressing life’s problems. Many psychiatrists suspect that more time on the inpatient unit is unlikely to reduce this patient’s risk of violence. Why? Because the violence risk does not stem from a treatable mental illness. Further, psychiatrists may be apprehensive about this patient’s potential for violence after discharge and their liability in the event of a bad outcome. No one wants their name associated with a headline that reads “Psychiatrist discharged man less than 24 hours before he killed 3 people.”
The purported relationship between mental illness and violence often is sensationalized in the media. However, research reveals that the vast majority of violence is in fact not due to symptoms of mental illness.1,2 A common clinical challenge in psychiatry involves evaluating individuals at elevated risk of violence and determining how to address their risk factors for violence. When the risk is primarily due to psychosis and can be reduced with antipsychotic medication, the job is easy. But how should we proceed when the risk stems from factors other than mental illness?
This article
Violence and mental illness: A tenuous link
Violence is a major public health concern in the United States. Although in recent years the rates of homicide and aggravated assault have decreased dramatically, there are approximately 16,000 homicides annually in the United States, and more than 1.6 million injuries from assaults treated in emergency departments each year.3 Homicide continues to be one of the leading causes of death among teenagers and young adults.4
The most effective methods of preventing widespread violence are public health approaches, such as parent- and family-focused programs, early childhood education, programs in school, and public policy changes.3 However, as psychiatrists, we are routinely asked to assess the risk of violence for an individual patient and devise strategies to mitigate violence risk.
Continue to: Although certain mental illnesses...
Although certain mental illnesses increase the relative risk of violence (compared with people without mental illness),5,6 recent studies suggest that mental illness plays only a “minor role in explaining violence in populations.”7 It is estimated that as little as 4% of the violence in the United States can be attributed to mental illness.1 According to a 1998 meta-analysis of 48 studies of criminal recidivism, the risk factors for violent recidivism were “almost identical” among offenders who had a mental disorder and those who did not.8
Approaches to assessing violence risk
Psychiatrists can assess the risk of future violence via 3 broad approaches.9,10
Unaided clinical judgment is when a mental health professional estimates violence risk based on his or her own experience and intuition, with knowledge of violence risk factors, but without the use of structured tools.
Actuarial tools are statistical models that use formulae to show relationships between data (risk factors) and outcomes (violence).10,11
Continue to: Structured professional judgment
Structured professional judgment is a hybrid of unaided clinical judgment and actuarial methods. Structured professional judgment tools help the evaluator identify empirically established risk factors. Once the information is collected, it is combined with clinical judgment in decision making.9,10 There are now more than 200 structured tools available for assessing violence risk in criminal justice and forensic mental health populations.12
Clinical judgment, although commonly used in practice, is less accurate than actuarial tools or structured professional judgment.10,11 In general, risk assessment tools offer moderate levels of accuracy in categorizing people at low risk vs high risk.5,13 The tools have better ability to accurately categorize individuals at low risk, compared with high risk, where false positives are common.12,14
Two types of risk factors
Risk factors for violence are commonly categorized as static or dynamic factors. Static factors are historical factors that cannot be changed with intervention (eg, age, sex, history of abuse). Dynamic factors can be changed with intervention (eg, substance abuse).15
Static risk factors. The best predictor of future violence is past violent behavior.5,16,17 Violence risk increases with each prior episode of violence.5 Prior arrests for any crime, especially if the individual was a juvenile at the time of arrest for his or her first violent offense, increase future violence risk.5 Other important static violence risk factors include demographic factors such as age, sex, and socioeconomic status. Swanson et al6 reviewed a large pool of data (approximately 10,000 respondents) from the Epidemiologic Catchment Area survey. Being young, male, and of low socioeconomic status were all associated with violence in the community.6 The highest-risk age group for violence is age 15 to 24.5 Males perpetrate violence in the community at a rate 10 times that of females.18 However, among individuals with severe mental illness, men and women have similar rates of violence.19,20 Unstable employment,21 less education,22 low intelligence,16 and a history of a significant head injury5 also are risk factors for violence.5
Continue to: Being abused as a child...
Being abused as a child, witnessing violence in the home,5,16 and growing up with an unstable parental situation (eg, parental loss or separation) has been linked to violence.16,23,24 Early disruptive behavior in childhood (eg, fighting, lying and stealing, truancy, and school problems) increases violence risk.21,23
Personality factors are important static risk factors for violence. Antisocial personality disorder is the most common personality disorder linked with violence.17 Several studies consistently show psychopathy to be a strong predictor of both violence and criminal behavior.5,25 A psychopath is a person who lacks empathy and close relationships, behaves impulsively, has superficially charming qualities, and is primarily interested in self-gratification.26 Harris et al27 studied 169 released forensic patients and found that 77% of the psychopaths (according to Psychopathy Checklist-Revised [PCL-R] scores) violently recidivated. In contrast, only 21% of the non-psychopaths violently recidivated.27
Other personality factors associated with violence include a predisposition toward feelings of anger and hatred (as opposed to empathy, anxiety, or guilt, which may reduce risk), hostile attributional biases (a tendency to interpret benign behavior of others as intentionally antagonistic), violent fantasies, poor anger control, and impulsivity.5 Although personality factors tend to be longstanding and more difficult to modify, in the outpatient setting, therapeutic efforts can be made to modify hostile attribution biases, poor anger control, and impulsive behavior.
Dynamic risk factors. Substance abuse is strongly associated with violence.6,17 The prevalence of violence is 12 times greater among individuals with alcohol use disorder and 16 times greater among individuals with other substance use disorders, compared with those with no such diagnoses.5,6
Continue to: Steadman et al...
Steadman et al28 compared 1,136 adult patients with mental disorders discharged from psychiatric hospitals with 519 individuals living in the same neighborhoods as the hospitalized patients. They found that the prevalence of violence among discharged patients without substance abuse was “statistically indistinguishable” from the prevalence of violence among community members, in the same neighborhood, who did not have symptoms of substance abuse.28 Swanson et al6 found that the combination of a mental disorder plus an alcohol or substance use disorder substantially increased the risk of violence.
Other dynamic risk factors for violence include mental illness symptoms such as psychosis, especially threat/control-override delusions, where the individual believes that they are being threatened or controlled by an external force.17
Contextual factors to consider in violence risk assessments include current stressors, lack of social support, availability of weapons, access to drugs and alcohol, and the presence of similar circumstances that led to violent behavior in the past.5
How to assess the risk of targeted violence
Targeted violence is a predatory act of violence intentionally committed against a preselected person, group of people, or place.29 Due to the low base rates of these incidents, targeted violence is difficult to study.7,30 These risk assessments require a more specialized approach.
Continue to: In their 1999 article...
In their 1999 article, Borum et al30 discussed threat assessment strategies utilized by the U.S. Secret Service and recommended investigating “pathways of ideas and behaviors that may lead to violent action.” Borum et al30 summarized 3 fundamental principles of threat assessment (Table 130).
What to do when violence risk is not due to mental illness
Based on the information in Mr. F’s case scenario, it is likely that his homicidal ideation is not due to mental illness. Despite this, several risk factors for violence are present. Where do we go from here?
Scott and Resnick17 recommend considering the concept of dangerousness as 5 components (Table 217). When this model of dangerousness is applied to Mr. F’s case, one can see that the magnitude of the harm is great because of threatened homicide. With regard to the imminence of the harm, it would help to clarify whether Mr. F plans to kill Ms. S immediately after discharge, or sometime in the next few months. Is his threat contingent on further provocations by Ms. S? Alternatively, does he intend to kill her for past grievances, regardless of further perceived insults?
Next, the frequency of a behavior relates to how often Mr. F has been aggressive in the past. The severity of his past aggression is also important. What is the most violent act he has ever done? Situational factors in this case include Mr. F’s access to weapons, financial problems, housing problems, and access to drugs and alcohol.17 Mr. F should be asked about what situations previously provoked his violent behavior. Consider how similar the present conditions are to past conditions to which Mr. F responded violently.5 The likelihood that a homicide will occur should take into account Mr. F’s risk factors for violence, as well as the seriousness of his intent to cause harm.
Continue to: Consider using a structured tool...
Consider using a structured tool, such as the Classification of Violence Risk, to help identify Mr. F’s risk factors for violence, or some other formal method to ensure that the proper data are collected. Violence risk assessments are more accurate when structured risk assessment tools are used, compared with clinical judgment alone.
It is important to review collateral sources of information. In Mr. F’s case, useful collateral sources may include his criminal docket (usually available online), past medical records, information from the shelter where he lives, and, potentially, friends or family.
Because Mr. F is making threats of targeted violence, be sure to ask about attack-related behaviors (Table 130).
Regarding the seriousness of Mr. F’s intent to cause harm, it may be helpful to ask him the following questions:
- How likely are you to carry out this act of violence?
- Do you have a plan? Have you taken any steps toward this plan?
- Do you see other, nonviolent solutions to this problem?
- What do you hope that we can do for you to help with this problem?
Continue to: Mr. F's answers...
Mr. F’s answers may suggest the possibility of a hidden agenda. Some patients express homicidal thoughts in order to stay in the hospital. If Mr. F expresses threats that are contingent on discharge and declines to engage in problem-solving discussions, this would cast doubt on the genuineness of his threat. However, doubt about the genuineness of the threat alone is not sufficient to simply discharge Mr. F. Assessment of his intent needs to be considered with other relevant risk factors, risk reduction strategies, and any Tarasoff duties that may apply.
In addition to risk factors, consider mitigating factors. For example, does Mr. F express concern over prison time as a reason to not engage in violence? It would be more ominous if Mr. F says that he does not care if he goes to prison because life is lousy being homeless and unemployed. At this point, an estimation can be made regarding whether Mr. F is a low-, moderate-, or high-risk of violence.
The next step is to organize Mr. F’s risk factors into static (historical) and dynamic (subject to intervention) factors. This will be helpful in formulating a strategy to manage risk because continued hospitalization can only address dynamic risk factors. Often in these cases, the static risk factors are far more numerous than the dynamic risk factors.
Once the data are collected and organized, the final step is to devise a risk management strategy. Some interventions, such as substance use treatment, will be straightforward. A mood-stabilizing medication could be considered, if clinically appropriate, to help reduce aggression and irritability.31 Efforts should be made to eliminate Mr. F’s access to firearms; however, in this case, it sounds unlikely that he will cooperate with those efforts. Ultimately, you may find yourself with a list of risk factors that are unlikely to be altered with further hospitalization, particularly if Mr. F’s homicidal thoughts and intent are due to antisocial personality traits.
Continue to: In that case...
In that case, the most important step will be to carry out your duty to warn/protect others prior to Mr. F’s discharge. Most states either require or permit mental health professionals to take reasonable steps to protect victims from violence when certain conditions are present, such as an explicit threat or identifiable victim (see Related Resources).
Once dynamic risk factors have been addressed, and duty to warn/protect is carried out, if there is no further clinical indication for hospitalization, it would be appropriate to discharge Mr. F. Continued homicidal threats stemming from antisocial personality traits, in the absence of a treatable mental illness (or other modifiable risk factors for violence that can be actively addressed), is not a reason for continued hospitalization. It may be useful to obtain a second opinion from a colleague in such scenarios. A second opinion may offer additional risk management ideas. In the event of a bad outcome, this will also help to show that the decision to discharge the patient was not taken lightly.
The psychiatrist should document a thoughtful risk assessment, the strategies that were implemented to reduce risk, the details of the warning, and the reasoning why continued hospitalization was not indicated (Table 3).
CASE CONTINUED
Decision to discharge
In Mr. F’s case, the treating psychiatrist determined that Mr. F’s risk of violence toward Ms. S was moderate. The psychiatrist identified several static risk factors for violence that raised Mr. F’s risk, but also noted that Mr. F’s threats were likely a manipulative effort to prolong his hospital stay. The psychiatrist carried out his duty to protect by notifying police and Ms. S of the nature of the threat prior to Mr. F’s discharge. The unit social worker helped Mr. F schedule an intake appointment for a substance use disorder treatment facility. Mr. F ultimately stated that he no longer experienced homicidal ideas once a bed was secured for him in a substance use treatment program. The psychiatrist carefully documented Mr. F’s risk assessment and the reasons why Mr. F’s risk would not be significantly altered by further inpatient hospitalization. Mr. F was discharged, and Ms. S remained unharmed.
Continue to: Bottom Line
Bottom Line
Use a structured approach to identify risk factors for violence. Address dynamic risk factors, including access to weapons. Carry out the duty to warn/protect if applicable. Document your decisions and actions carefully, and then discharge the patient if clinically indicated. Do not be “held hostage” by a patient’s homicidal ideation.
Related Resources
- Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
- Douglas KS, Hart SD, Webster CD, et al. HCR-20V3: Assessing risk of violence–user guide. Burnaby, Canada: Mental Health, Law, and Policy Institute, Simon Fraser University; 2013.
- National Conference of State Legislatures. Mental health professionals’ duty to warn. http://www.ncsl.org/research/health/mental-health-professionals-duty-to-warn.aspx. Published September 28, 2015.
Drug Brand Names
Sertraline • Zoloft
1. Skeem J, Kennealy P, Monahan J, et al. Psychosis uncommonly and inconsistently precedes violence among high-risk individuals. Clin Psychol Sci. 2016;4(1):40-49.
2. McGinty E, Frattaroli S, Appelbaum PS, et al. Using research evidence to reframe the policy debate around mental illness and guns: process and recommendations. Am J Public Health. 2014;104(11):e22-e26.
3. Sumner SA, Mercy JA, Dahlberg LL, et al. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478-488.
4. Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016;65(5):1-96.
5. Borum R, Swartz M, Swanson J. Assessing and managing violence risk in clinical practice. J Prac Psychiatry Behav Health. 1996;2(4):205-215.
6. Swanson JW, Holzer CE 3rd, Ganju VK, et al. Violence and psychiatric disorder in the community: Evidence from the epidemiologic catchment area surveys. Hosp Community Psychiatry. 1990;41(7):761-770.
7. Swanson JW. Explaining rare acts of violence: the limits of evidence from population research. Psychiatr Serv. 2011;62(11):1369-1371.
8. Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123(2):123-142.
9. Monahan J. The inclusion of biological risk factors in violence risk assessments. In: Singh I, Sinnott-Armstrong W, Savulescu J, eds. Bioprediction, biomarkers, and bad behavior: scientific, legal, and ethical implications. New York, NY: Oxford University Press; 2014:57-76.
10. Murray J, Thomson ME. Clinical judgement in violence risk assessment. Eur J Psychol. 2010;6(1):128-149.
11. Mossman D. Violence risk: is clinical judgment enough? Current Psychiatry. 2008;7(6):66-72.
12. Douglas T, Pugh J, Singh I, et al. Risk assessment tools in criminal justice and forensic psychiatry: the need for better data. Eur Psychiatry. 2017;42:134-137.
13. Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
14. Fazel S, Singh J, Doll H, et al. Use of risk assessment instruments to predict violence and antisocial behaviour in 73 samples involving 24 827 people: systematic review and meta-analysis. BMJ. 2012;345:e4692. doi: 10.1136/bmj.e4692.
15. National Collaborating Centre for Mental Health (UK). Violence and aggression: short- term management in mental health, health, and community settings: updated edition. London: British Psychological Society; 2015. NICE Guideline, No 10.
16. Klassen D, O’Connor WA. Predicting violence in schizophrenic and non-schizophrenic patients: a prospective study. J Community Psychol. 1988;16(2):217-227.
17. Scott C, Resnick P. Clinical assessment of aggression and violence. In: Rosner R, Scott C, eds. Principles and practice of forensic psychiatry, 3rd ed. Boca Raton, FL: CRC Press; 2017:623-631.
18. Tardiff K, Sweillam A. Assault, suicide, and mental illness. Arch Gen Psychiatry. 1980;37(2):164-169.
19. Lidz CW, Mulvey EP, Gardner W. The accuracy of predictions of violence to others. JAMA. 1993;269(8):1007-1011.
20. Newhill CE, Mulvey EP, Lidz CW. Characteristics of violence in the community by female patients seen in a psychiatric emergency service. Psychiatric Serv. 1995;46(8):785-789.
21. Mulvey E, Lidz C. Clinical considerations in the prediction of dangerousness in mental patients. Clin Psychol Rev. 1984;4(4):379-401.
22. Link BG, Andrews H, Cullen FT. The violent and illegal behavior of mental patients reconsidered. Am Sociol Rev. 1992;57(3):275-292.
23. Harris GT, Rice ME, Quinsey VL. Violent recidivism of mentally disordered offenders: the development of a statistical prediction instrument. Crim Justice and Behav. 1993;20(4):315-335.
24. Klassen D, O’Connor W. Demographic and case history variables in risk assessment. In: Monahan J, Steadman H, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:229-257.
25. Hart SD, Hare RD, Forth AE. Psychopathy as a risk marker for violence: development and validation of a screening version of the revised Psychopathy Checklist. In: Monahan J, Steadman HJ, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:81-98.
26. Cleckley H. The mask of sanity. St. Louis, MO: Mosby; 1941.
27. Harris GT, Rice ME, Cormier CA. Psychopathy and violent recidivism. Law Hum Behav. 1991;15(6):625-637.
28. Steadman HJ, Mulvey EP, Monahan J. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393-401.
29. Meloy JR, White SG, Hart S. Workplace assessment of targeted violence risk: the development and reliability of the WAVR-21. J Forensic Sci. 2013;58(5):1353-1358.
30. Borum R, Fein R, Vossekuil B, et al. Threat assessment: defining an approach for evaluating risk of targeted violence. Behav Sci Law. 1999;17(3):323-337.
31. Tyrer P, Bateman AW. Drug treatment for personality disorders. Adv Psychiatr Treat. 2004;10(5):389-398.
Mr. F, age 35, is homeless and has a history of cocaine and alcohol use disorders. He is admitted voluntarily to the psychiatric unit because he has homicidal thoughts toward Ms. S, who works in the shelter where he has been staying. Mr. F reports that he is thinking of killing Ms. S if he is discharged because she has been rude to him. He states that he has access to several firearms, but he will not disclose the location. He has been diagnosed with unspecified depressive disorder and exhibited antisocial personality disorder traits. He is being treated with sertraline. However, his mood appears to be relatively stable, except for occasional angry verbal outbursts. The outbursts have been related to intrusive peers or staff turning the television off for group meetings. Mr. F has been joking with peers, eating well, and sleeping appropriately. He reports no suicidal thoughts and has not been physically violent on the unit. However, Mr. F has had a history of violence since his teenage years. He has been incarcerated twice for assault and once for drug possession.
How would you approach assessing and managing Mr. F’s risk for violence?
We all have encountered a patient similar to Mr. F on the psychiatric unit or in the emergency department—a patient who makes violent threats and appears angry, intimidating, manipulative, and/or demanding, despite exhibiting no evidence of mania or psychosis. This patient often has a history of substance abuse and a lifelong pattern of viewing violence as an acceptable way of addressing life’s problems. Many psychiatrists suspect that more time on the inpatient unit is unlikely to reduce this patient’s risk of violence. Why? Because the violence risk does not stem from a treatable mental illness. Further, psychiatrists may be apprehensive about this patient’s potential for violence after discharge and their liability in the event of a bad outcome. No one wants their name associated with a headline that reads “Psychiatrist discharged man less than 24 hours before he killed 3 people.”
The purported relationship between mental illness and violence often is sensationalized in the media. However, research reveals that the vast majority of violence is in fact not due to symptoms of mental illness.1,2 A common clinical challenge in psychiatry involves evaluating individuals at elevated risk of violence and determining how to address their risk factors for violence. When the risk is primarily due to psychosis and can be reduced with antipsychotic medication, the job is easy. But how should we proceed when the risk stems from factors other than mental illness?
This article
Violence and mental illness: A tenuous link
Violence is a major public health concern in the United States. Although in recent years the rates of homicide and aggravated assault have decreased dramatically, there are approximately 16,000 homicides annually in the United States, and more than 1.6 million injuries from assaults treated in emergency departments each year.3 Homicide continues to be one of the leading causes of death among teenagers and young adults.4
The most effective methods of preventing widespread violence are public health approaches, such as parent- and family-focused programs, early childhood education, programs in school, and public policy changes.3 However, as psychiatrists, we are routinely asked to assess the risk of violence for an individual patient and devise strategies to mitigate violence risk.
Continue to: Although certain mental illnesses...
Although certain mental illnesses increase the relative risk of violence (compared with people without mental illness),5,6 recent studies suggest that mental illness plays only a “minor role in explaining violence in populations.”7 It is estimated that as little as 4% of the violence in the United States can be attributed to mental illness.1 According to a 1998 meta-analysis of 48 studies of criminal recidivism, the risk factors for violent recidivism were “almost identical” among offenders who had a mental disorder and those who did not.8
Approaches to assessing violence risk
Psychiatrists can assess the risk of future violence via 3 broad approaches.9,10
Unaided clinical judgment is when a mental health professional estimates violence risk based on his or her own experience and intuition, with knowledge of violence risk factors, but without the use of structured tools.
Actuarial tools are statistical models that use formulae to show relationships between data (risk factors) and outcomes (violence).10,11
Continue to: Structured professional judgment
Structured professional judgment is a hybrid of unaided clinical judgment and actuarial methods. Structured professional judgment tools help the evaluator identify empirically established risk factors. Once the information is collected, it is combined with clinical judgment in decision making.9,10 There are now more than 200 structured tools available for assessing violence risk in criminal justice and forensic mental health populations.12
Clinical judgment, although commonly used in practice, is less accurate than actuarial tools or structured professional judgment.10,11 In general, risk assessment tools offer moderate levels of accuracy in categorizing people at low risk vs high risk.5,13 The tools have better ability to accurately categorize individuals at low risk, compared with high risk, where false positives are common.12,14
Two types of risk factors
Risk factors for violence are commonly categorized as static or dynamic factors. Static factors are historical factors that cannot be changed with intervention (eg, age, sex, history of abuse). Dynamic factors can be changed with intervention (eg, substance abuse).15
Static risk factors. The best predictor of future violence is past violent behavior.5,16,17 Violence risk increases with each prior episode of violence.5 Prior arrests for any crime, especially if the individual was a juvenile at the time of arrest for his or her first violent offense, increase future violence risk.5 Other important static violence risk factors include demographic factors such as age, sex, and socioeconomic status. Swanson et al6 reviewed a large pool of data (approximately 10,000 respondents) from the Epidemiologic Catchment Area survey. Being young, male, and of low socioeconomic status were all associated with violence in the community.6 The highest-risk age group for violence is age 15 to 24.5 Males perpetrate violence in the community at a rate 10 times that of females.18 However, among individuals with severe mental illness, men and women have similar rates of violence.19,20 Unstable employment,21 less education,22 low intelligence,16 and a history of a significant head injury5 also are risk factors for violence.5
Continue to: Being abused as a child...
Being abused as a child, witnessing violence in the home,5,16 and growing up with an unstable parental situation (eg, parental loss or separation) has been linked to violence.16,23,24 Early disruptive behavior in childhood (eg, fighting, lying and stealing, truancy, and school problems) increases violence risk.21,23
Personality factors are important static risk factors for violence. Antisocial personality disorder is the most common personality disorder linked with violence.17 Several studies consistently show psychopathy to be a strong predictor of both violence and criminal behavior.5,25 A psychopath is a person who lacks empathy and close relationships, behaves impulsively, has superficially charming qualities, and is primarily interested in self-gratification.26 Harris et al27 studied 169 released forensic patients and found that 77% of the psychopaths (according to Psychopathy Checklist-Revised [PCL-R] scores) violently recidivated. In contrast, only 21% of the non-psychopaths violently recidivated.27
Other personality factors associated with violence include a predisposition toward feelings of anger and hatred (as opposed to empathy, anxiety, or guilt, which may reduce risk), hostile attributional biases (a tendency to interpret benign behavior of others as intentionally antagonistic), violent fantasies, poor anger control, and impulsivity.5 Although personality factors tend to be longstanding and more difficult to modify, in the outpatient setting, therapeutic efforts can be made to modify hostile attribution biases, poor anger control, and impulsive behavior.
Dynamic risk factors. Substance abuse is strongly associated with violence.6,17 The prevalence of violence is 12 times greater among individuals with alcohol use disorder and 16 times greater among individuals with other substance use disorders, compared with those with no such diagnoses.5,6
Continue to: Steadman et al...
Steadman et al28 compared 1,136 adult patients with mental disorders discharged from psychiatric hospitals with 519 individuals living in the same neighborhoods as the hospitalized patients. They found that the prevalence of violence among discharged patients without substance abuse was “statistically indistinguishable” from the prevalence of violence among community members, in the same neighborhood, who did not have symptoms of substance abuse.28 Swanson et al6 found that the combination of a mental disorder plus an alcohol or substance use disorder substantially increased the risk of violence.
Other dynamic risk factors for violence include mental illness symptoms such as psychosis, especially threat/control-override delusions, where the individual believes that they are being threatened or controlled by an external force.17
Contextual factors to consider in violence risk assessments include current stressors, lack of social support, availability of weapons, access to drugs and alcohol, and the presence of similar circumstances that led to violent behavior in the past.5
How to assess the risk of targeted violence
Targeted violence is a predatory act of violence intentionally committed against a preselected person, group of people, or place.29 Due to the low base rates of these incidents, targeted violence is difficult to study.7,30 These risk assessments require a more specialized approach.
Continue to: In their 1999 article...
In their 1999 article, Borum et al30 discussed threat assessment strategies utilized by the U.S. Secret Service and recommended investigating “pathways of ideas and behaviors that may lead to violent action.” Borum et al30 summarized 3 fundamental principles of threat assessment (Table 130).
What to do when violence risk is not due to mental illness
Based on the information in Mr. F’s case scenario, it is likely that his homicidal ideation is not due to mental illness. Despite this, several risk factors for violence are present. Where do we go from here?
Scott and Resnick17 recommend considering the concept of dangerousness as 5 components (Table 217). When this model of dangerousness is applied to Mr. F’s case, one can see that the magnitude of the harm is great because of threatened homicide. With regard to the imminence of the harm, it would help to clarify whether Mr. F plans to kill Ms. S immediately after discharge, or sometime in the next few months. Is his threat contingent on further provocations by Ms. S? Alternatively, does he intend to kill her for past grievances, regardless of further perceived insults?
Next, the frequency of a behavior relates to how often Mr. F has been aggressive in the past. The severity of his past aggression is also important. What is the most violent act he has ever done? Situational factors in this case include Mr. F’s access to weapons, financial problems, housing problems, and access to drugs and alcohol.17 Mr. F should be asked about what situations previously provoked his violent behavior. Consider how similar the present conditions are to past conditions to which Mr. F responded violently.5 The likelihood that a homicide will occur should take into account Mr. F’s risk factors for violence, as well as the seriousness of his intent to cause harm.
Continue to: Consider using a structured tool...
Consider using a structured tool, such as the Classification of Violence Risk, to help identify Mr. F’s risk factors for violence, or some other formal method to ensure that the proper data are collected. Violence risk assessments are more accurate when structured risk assessment tools are used, compared with clinical judgment alone.
It is important to review collateral sources of information. In Mr. F’s case, useful collateral sources may include his criminal docket (usually available online), past medical records, information from the shelter where he lives, and, potentially, friends or family.
Because Mr. F is making threats of targeted violence, be sure to ask about attack-related behaviors (Table 130).
Regarding the seriousness of Mr. F’s intent to cause harm, it may be helpful to ask him the following questions:
- How likely are you to carry out this act of violence?
- Do you have a plan? Have you taken any steps toward this plan?
- Do you see other, nonviolent solutions to this problem?
- What do you hope that we can do for you to help with this problem?
Continue to: Mr. F's answers...
Mr. F’s answers may suggest the possibility of a hidden agenda. Some patients express homicidal thoughts in order to stay in the hospital. If Mr. F expresses threats that are contingent on discharge and declines to engage in problem-solving discussions, this would cast doubt on the genuineness of his threat. However, doubt about the genuineness of the threat alone is not sufficient to simply discharge Mr. F. Assessment of his intent needs to be considered with other relevant risk factors, risk reduction strategies, and any Tarasoff duties that may apply.
In addition to risk factors, consider mitigating factors. For example, does Mr. F express concern over prison time as a reason to not engage in violence? It would be more ominous if Mr. F says that he does not care if he goes to prison because life is lousy being homeless and unemployed. At this point, an estimation can be made regarding whether Mr. F is a low-, moderate-, or high-risk of violence.
The next step is to organize Mr. F’s risk factors into static (historical) and dynamic (subject to intervention) factors. This will be helpful in formulating a strategy to manage risk because continued hospitalization can only address dynamic risk factors. Often in these cases, the static risk factors are far more numerous than the dynamic risk factors.
Once the data are collected and organized, the final step is to devise a risk management strategy. Some interventions, such as substance use treatment, will be straightforward. A mood-stabilizing medication could be considered, if clinically appropriate, to help reduce aggression and irritability.31 Efforts should be made to eliminate Mr. F’s access to firearms; however, in this case, it sounds unlikely that he will cooperate with those efforts. Ultimately, you may find yourself with a list of risk factors that are unlikely to be altered with further hospitalization, particularly if Mr. F’s homicidal thoughts and intent are due to antisocial personality traits.
Continue to: In that case...
In that case, the most important step will be to carry out your duty to warn/protect others prior to Mr. F’s discharge. Most states either require or permit mental health professionals to take reasonable steps to protect victims from violence when certain conditions are present, such as an explicit threat or identifiable victim (see Related Resources).
Once dynamic risk factors have been addressed, and duty to warn/protect is carried out, if there is no further clinical indication for hospitalization, it would be appropriate to discharge Mr. F. Continued homicidal threats stemming from antisocial personality traits, in the absence of a treatable mental illness (or other modifiable risk factors for violence that can be actively addressed), is not a reason for continued hospitalization. It may be useful to obtain a second opinion from a colleague in such scenarios. A second opinion may offer additional risk management ideas. In the event of a bad outcome, this will also help to show that the decision to discharge the patient was not taken lightly.
The psychiatrist should document a thoughtful risk assessment, the strategies that were implemented to reduce risk, the details of the warning, and the reasoning why continued hospitalization was not indicated (Table 3).
CASE CONTINUED
Decision to discharge
In Mr. F’s case, the treating psychiatrist determined that Mr. F’s risk of violence toward Ms. S was moderate. The psychiatrist identified several static risk factors for violence that raised Mr. F’s risk, but also noted that Mr. F’s threats were likely a manipulative effort to prolong his hospital stay. The psychiatrist carried out his duty to protect by notifying police and Ms. S of the nature of the threat prior to Mr. F’s discharge. The unit social worker helped Mr. F schedule an intake appointment for a substance use disorder treatment facility. Mr. F ultimately stated that he no longer experienced homicidal ideas once a bed was secured for him in a substance use treatment program. The psychiatrist carefully documented Mr. F’s risk assessment and the reasons why Mr. F’s risk would not be significantly altered by further inpatient hospitalization. Mr. F was discharged, and Ms. S remained unharmed.
Continue to: Bottom Line
Bottom Line
Use a structured approach to identify risk factors for violence. Address dynamic risk factors, including access to weapons. Carry out the duty to warn/protect if applicable. Document your decisions and actions carefully, and then discharge the patient if clinically indicated. Do not be “held hostage” by a patient’s homicidal ideation.
Related Resources
- Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
- Douglas KS, Hart SD, Webster CD, et al. HCR-20V3: Assessing risk of violence–user guide. Burnaby, Canada: Mental Health, Law, and Policy Institute, Simon Fraser University; 2013.
- National Conference of State Legislatures. Mental health professionals’ duty to warn. http://www.ncsl.org/research/health/mental-health-professionals-duty-to-warn.aspx. Published September 28, 2015.
Drug Brand Names
Sertraline • Zoloft
Mr. F, age 35, is homeless and has a history of cocaine and alcohol use disorders. He is admitted voluntarily to the psychiatric unit because he has homicidal thoughts toward Ms. S, who works in the shelter where he has been staying. Mr. F reports that he is thinking of killing Ms. S if he is discharged because she has been rude to him. He states that he has access to several firearms, but he will not disclose the location. He has been diagnosed with unspecified depressive disorder and exhibited antisocial personality disorder traits. He is being treated with sertraline. However, his mood appears to be relatively stable, except for occasional angry verbal outbursts. The outbursts have been related to intrusive peers or staff turning the television off for group meetings. Mr. F has been joking with peers, eating well, and sleeping appropriately. He reports no suicidal thoughts and has not been physically violent on the unit. However, Mr. F has had a history of violence since his teenage years. He has been incarcerated twice for assault and once for drug possession.
How would you approach assessing and managing Mr. F’s risk for violence?
We all have encountered a patient similar to Mr. F on the psychiatric unit or in the emergency department—a patient who makes violent threats and appears angry, intimidating, manipulative, and/or demanding, despite exhibiting no evidence of mania or psychosis. This patient often has a history of substance abuse and a lifelong pattern of viewing violence as an acceptable way of addressing life’s problems. Many psychiatrists suspect that more time on the inpatient unit is unlikely to reduce this patient’s risk of violence. Why? Because the violence risk does not stem from a treatable mental illness. Further, psychiatrists may be apprehensive about this patient’s potential for violence after discharge and their liability in the event of a bad outcome. No one wants their name associated with a headline that reads “Psychiatrist discharged man less than 24 hours before he killed 3 people.”
The purported relationship between mental illness and violence often is sensationalized in the media. However, research reveals that the vast majority of violence is in fact not due to symptoms of mental illness.1,2 A common clinical challenge in psychiatry involves evaluating individuals at elevated risk of violence and determining how to address their risk factors for violence. When the risk is primarily due to psychosis and can be reduced with antipsychotic medication, the job is easy. But how should we proceed when the risk stems from factors other than mental illness?
This article
Violence and mental illness: A tenuous link
Violence is a major public health concern in the United States. Although in recent years the rates of homicide and aggravated assault have decreased dramatically, there are approximately 16,000 homicides annually in the United States, and more than 1.6 million injuries from assaults treated in emergency departments each year.3 Homicide continues to be one of the leading causes of death among teenagers and young adults.4
The most effective methods of preventing widespread violence are public health approaches, such as parent- and family-focused programs, early childhood education, programs in school, and public policy changes.3 However, as psychiatrists, we are routinely asked to assess the risk of violence for an individual patient and devise strategies to mitigate violence risk.
Continue to: Although certain mental illnesses...
Although certain mental illnesses increase the relative risk of violence (compared with people without mental illness),5,6 recent studies suggest that mental illness plays only a “minor role in explaining violence in populations.”7 It is estimated that as little as 4% of the violence in the United States can be attributed to mental illness.1 According to a 1998 meta-analysis of 48 studies of criminal recidivism, the risk factors for violent recidivism were “almost identical” among offenders who had a mental disorder and those who did not.8
Approaches to assessing violence risk
Psychiatrists can assess the risk of future violence via 3 broad approaches.9,10
Unaided clinical judgment is when a mental health professional estimates violence risk based on his or her own experience and intuition, with knowledge of violence risk factors, but without the use of structured tools.
Actuarial tools are statistical models that use formulae to show relationships between data (risk factors) and outcomes (violence).10,11
Continue to: Structured professional judgment
Structured professional judgment is a hybrid of unaided clinical judgment and actuarial methods. Structured professional judgment tools help the evaluator identify empirically established risk factors. Once the information is collected, it is combined with clinical judgment in decision making.9,10 There are now more than 200 structured tools available for assessing violence risk in criminal justice and forensic mental health populations.12
Clinical judgment, although commonly used in practice, is less accurate than actuarial tools or structured professional judgment.10,11 In general, risk assessment tools offer moderate levels of accuracy in categorizing people at low risk vs high risk.5,13 The tools have better ability to accurately categorize individuals at low risk, compared with high risk, where false positives are common.12,14
Two types of risk factors
Risk factors for violence are commonly categorized as static or dynamic factors. Static factors are historical factors that cannot be changed with intervention (eg, age, sex, history of abuse). Dynamic factors can be changed with intervention (eg, substance abuse).15
Static risk factors. The best predictor of future violence is past violent behavior.5,16,17 Violence risk increases with each prior episode of violence.5 Prior arrests for any crime, especially if the individual was a juvenile at the time of arrest for his or her first violent offense, increase future violence risk.5 Other important static violence risk factors include demographic factors such as age, sex, and socioeconomic status. Swanson et al6 reviewed a large pool of data (approximately 10,000 respondents) from the Epidemiologic Catchment Area survey. Being young, male, and of low socioeconomic status were all associated with violence in the community.6 The highest-risk age group for violence is age 15 to 24.5 Males perpetrate violence in the community at a rate 10 times that of females.18 However, among individuals with severe mental illness, men and women have similar rates of violence.19,20 Unstable employment,21 less education,22 low intelligence,16 and a history of a significant head injury5 also are risk factors for violence.5
Continue to: Being abused as a child...
Being abused as a child, witnessing violence in the home,5,16 and growing up with an unstable parental situation (eg, parental loss or separation) has been linked to violence.16,23,24 Early disruptive behavior in childhood (eg, fighting, lying and stealing, truancy, and school problems) increases violence risk.21,23
Personality factors are important static risk factors for violence. Antisocial personality disorder is the most common personality disorder linked with violence.17 Several studies consistently show psychopathy to be a strong predictor of both violence and criminal behavior.5,25 A psychopath is a person who lacks empathy and close relationships, behaves impulsively, has superficially charming qualities, and is primarily interested in self-gratification.26 Harris et al27 studied 169 released forensic patients and found that 77% of the psychopaths (according to Psychopathy Checklist-Revised [PCL-R] scores) violently recidivated. In contrast, only 21% of the non-psychopaths violently recidivated.27
Other personality factors associated with violence include a predisposition toward feelings of anger and hatred (as opposed to empathy, anxiety, or guilt, which may reduce risk), hostile attributional biases (a tendency to interpret benign behavior of others as intentionally antagonistic), violent fantasies, poor anger control, and impulsivity.5 Although personality factors tend to be longstanding and more difficult to modify, in the outpatient setting, therapeutic efforts can be made to modify hostile attribution biases, poor anger control, and impulsive behavior.
Dynamic risk factors. Substance abuse is strongly associated with violence.6,17 The prevalence of violence is 12 times greater among individuals with alcohol use disorder and 16 times greater among individuals with other substance use disorders, compared with those with no such diagnoses.5,6
Continue to: Steadman et al...
Steadman et al28 compared 1,136 adult patients with mental disorders discharged from psychiatric hospitals with 519 individuals living in the same neighborhoods as the hospitalized patients. They found that the prevalence of violence among discharged patients without substance abuse was “statistically indistinguishable” from the prevalence of violence among community members, in the same neighborhood, who did not have symptoms of substance abuse.28 Swanson et al6 found that the combination of a mental disorder plus an alcohol or substance use disorder substantially increased the risk of violence.
Other dynamic risk factors for violence include mental illness symptoms such as psychosis, especially threat/control-override delusions, where the individual believes that they are being threatened or controlled by an external force.17
Contextual factors to consider in violence risk assessments include current stressors, lack of social support, availability of weapons, access to drugs and alcohol, and the presence of similar circumstances that led to violent behavior in the past.5
How to assess the risk of targeted violence
Targeted violence is a predatory act of violence intentionally committed against a preselected person, group of people, or place.29 Due to the low base rates of these incidents, targeted violence is difficult to study.7,30 These risk assessments require a more specialized approach.
Continue to: In their 1999 article...
In their 1999 article, Borum et al30 discussed threat assessment strategies utilized by the U.S. Secret Service and recommended investigating “pathways of ideas and behaviors that may lead to violent action.” Borum et al30 summarized 3 fundamental principles of threat assessment (Table 130).
What to do when violence risk is not due to mental illness
Based on the information in Mr. F’s case scenario, it is likely that his homicidal ideation is not due to mental illness. Despite this, several risk factors for violence are present. Where do we go from here?
Scott and Resnick17 recommend considering the concept of dangerousness as 5 components (Table 217). When this model of dangerousness is applied to Mr. F’s case, one can see that the magnitude of the harm is great because of threatened homicide. With regard to the imminence of the harm, it would help to clarify whether Mr. F plans to kill Ms. S immediately after discharge, or sometime in the next few months. Is his threat contingent on further provocations by Ms. S? Alternatively, does he intend to kill her for past grievances, regardless of further perceived insults?
Next, the frequency of a behavior relates to how often Mr. F has been aggressive in the past. The severity of his past aggression is also important. What is the most violent act he has ever done? Situational factors in this case include Mr. F’s access to weapons, financial problems, housing problems, and access to drugs and alcohol.17 Mr. F should be asked about what situations previously provoked his violent behavior. Consider how similar the present conditions are to past conditions to which Mr. F responded violently.5 The likelihood that a homicide will occur should take into account Mr. F’s risk factors for violence, as well as the seriousness of his intent to cause harm.
Continue to: Consider using a structured tool...
Consider using a structured tool, such as the Classification of Violence Risk, to help identify Mr. F’s risk factors for violence, or some other formal method to ensure that the proper data are collected. Violence risk assessments are more accurate when structured risk assessment tools are used, compared with clinical judgment alone.
It is important to review collateral sources of information. In Mr. F’s case, useful collateral sources may include his criminal docket (usually available online), past medical records, information from the shelter where he lives, and, potentially, friends or family.
Because Mr. F is making threats of targeted violence, be sure to ask about attack-related behaviors (Table 130).
Regarding the seriousness of Mr. F’s intent to cause harm, it may be helpful to ask him the following questions:
- How likely are you to carry out this act of violence?
- Do you have a plan? Have you taken any steps toward this plan?
- Do you see other, nonviolent solutions to this problem?
- What do you hope that we can do for you to help with this problem?
Continue to: Mr. F's answers...
Mr. F’s answers may suggest the possibility of a hidden agenda. Some patients express homicidal thoughts in order to stay in the hospital. If Mr. F expresses threats that are contingent on discharge and declines to engage in problem-solving discussions, this would cast doubt on the genuineness of his threat. However, doubt about the genuineness of the threat alone is not sufficient to simply discharge Mr. F. Assessment of his intent needs to be considered with other relevant risk factors, risk reduction strategies, and any Tarasoff duties that may apply.
In addition to risk factors, consider mitigating factors. For example, does Mr. F express concern over prison time as a reason to not engage in violence? It would be more ominous if Mr. F says that he does not care if he goes to prison because life is lousy being homeless and unemployed. At this point, an estimation can be made regarding whether Mr. F is a low-, moderate-, or high-risk of violence.
The next step is to organize Mr. F’s risk factors into static (historical) and dynamic (subject to intervention) factors. This will be helpful in formulating a strategy to manage risk because continued hospitalization can only address dynamic risk factors. Often in these cases, the static risk factors are far more numerous than the dynamic risk factors.
Once the data are collected and organized, the final step is to devise a risk management strategy. Some interventions, such as substance use treatment, will be straightforward. A mood-stabilizing medication could be considered, if clinically appropriate, to help reduce aggression and irritability.31 Efforts should be made to eliminate Mr. F’s access to firearms; however, in this case, it sounds unlikely that he will cooperate with those efforts. Ultimately, you may find yourself with a list of risk factors that are unlikely to be altered with further hospitalization, particularly if Mr. F’s homicidal thoughts and intent are due to antisocial personality traits.
Continue to: In that case...
In that case, the most important step will be to carry out your duty to warn/protect others prior to Mr. F’s discharge. Most states either require or permit mental health professionals to take reasonable steps to protect victims from violence when certain conditions are present, such as an explicit threat or identifiable victim (see Related Resources).
Once dynamic risk factors have been addressed, and duty to warn/protect is carried out, if there is no further clinical indication for hospitalization, it would be appropriate to discharge Mr. F. Continued homicidal threats stemming from antisocial personality traits, in the absence of a treatable mental illness (or other modifiable risk factors for violence that can be actively addressed), is not a reason for continued hospitalization. It may be useful to obtain a second opinion from a colleague in such scenarios. A second opinion may offer additional risk management ideas. In the event of a bad outcome, this will also help to show that the decision to discharge the patient was not taken lightly.
The psychiatrist should document a thoughtful risk assessment, the strategies that were implemented to reduce risk, the details of the warning, and the reasoning why continued hospitalization was not indicated (Table 3).
CASE CONTINUED
Decision to discharge
In Mr. F’s case, the treating psychiatrist determined that Mr. F’s risk of violence toward Ms. S was moderate. The psychiatrist identified several static risk factors for violence that raised Mr. F’s risk, but also noted that Mr. F’s threats were likely a manipulative effort to prolong his hospital stay. The psychiatrist carried out his duty to protect by notifying police and Ms. S of the nature of the threat prior to Mr. F’s discharge. The unit social worker helped Mr. F schedule an intake appointment for a substance use disorder treatment facility. Mr. F ultimately stated that he no longer experienced homicidal ideas once a bed was secured for him in a substance use treatment program. The psychiatrist carefully documented Mr. F’s risk assessment and the reasons why Mr. F’s risk would not be significantly altered by further inpatient hospitalization. Mr. F was discharged, and Ms. S remained unharmed.
Continue to: Bottom Line
Bottom Line
Use a structured approach to identify risk factors for violence. Address dynamic risk factors, including access to weapons. Carry out the duty to warn/protect if applicable. Document your decisions and actions carefully, and then discharge the patient if clinically indicated. Do not be “held hostage” by a patient’s homicidal ideation.
Related Resources
- Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
- Douglas KS, Hart SD, Webster CD, et al. HCR-20V3: Assessing risk of violence–user guide. Burnaby, Canada: Mental Health, Law, and Policy Institute, Simon Fraser University; 2013.
- National Conference of State Legislatures. Mental health professionals’ duty to warn. http://www.ncsl.org/research/health/mental-health-professionals-duty-to-warn.aspx. Published September 28, 2015.
Drug Brand Names
Sertraline • Zoloft
1. Skeem J, Kennealy P, Monahan J, et al. Psychosis uncommonly and inconsistently precedes violence among high-risk individuals. Clin Psychol Sci. 2016;4(1):40-49.
2. McGinty E, Frattaroli S, Appelbaum PS, et al. Using research evidence to reframe the policy debate around mental illness and guns: process and recommendations. Am J Public Health. 2014;104(11):e22-e26.
3. Sumner SA, Mercy JA, Dahlberg LL, et al. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478-488.
4. Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016;65(5):1-96.
5. Borum R, Swartz M, Swanson J. Assessing and managing violence risk in clinical practice. J Prac Psychiatry Behav Health. 1996;2(4):205-215.
6. Swanson JW, Holzer CE 3rd, Ganju VK, et al. Violence and psychiatric disorder in the community: Evidence from the epidemiologic catchment area surveys. Hosp Community Psychiatry. 1990;41(7):761-770.
7. Swanson JW. Explaining rare acts of violence: the limits of evidence from population research. Psychiatr Serv. 2011;62(11):1369-1371.
8. Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123(2):123-142.
9. Monahan J. The inclusion of biological risk factors in violence risk assessments. In: Singh I, Sinnott-Armstrong W, Savulescu J, eds. Bioprediction, biomarkers, and bad behavior: scientific, legal, and ethical implications. New York, NY: Oxford University Press; 2014:57-76.
10. Murray J, Thomson ME. Clinical judgement in violence risk assessment. Eur J Psychol. 2010;6(1):128-149.
11. Mossman D. Violence risk: is clinical judgment enough? Current Psychiatry. 2008;7(6):66-72.
12. Douglas T, Pugh J, Singh I, et al. Risk assessment tools in criminal justice and forensic psychiatry: the need for better data. Eur Psychiatry. 2017;42:134-137.
13. Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
14. Fazel S, Singh J, Doll H, et al. Use of risk assessment instruments to predict violence and antisocial behaviour in 73 samples involving 24 827 people: systematic review and meta-analysis. BMJ. 2012;345:e4692. doi: 10.1136/bmj.e4692.
15. National Collaborating Centre for Mental Health (UK). Violence and aggression: short- term management in mental health, health, and community settings: updated edition. London: British Psychological Society; 2015. NICE Guideline, No 10.
16. Klassen D, O’Connor WA. Predicting violence in schizophrenic and non-schizophrenic patients: a prospective study. J Community Psychol. 1988;16(2):217-227.
17. Scott C, Resnick P. Clinical assessment of aggression and violence. In: Rosner R, Scott C, eds. Principles and practice of forensic psychiatry, 3rd ed. Boca Raton, FL: CRC Press; 2017:623-631.
18. Tardiff K, Sweillam A. Assault, suicide, and mental illness. Arch Gen Psychiatry. 1980;37(2):164-169.
19. Lidz CW, Mulvey EP, Gardner W. The accuracy of predictions of violence to others. JAMA. 1993;269(8):1007-1011.
20. Newhill CE, Mulvey EP, Lidz CW. Characteristics of violence in the community by female patients seen in a psychiatric emergency service. Psychiatric Serv. 1995;46(8):785-789.
21. Mulvey E, Lidz C. Clinical considerations in the prediction of dangerousness in mental patients. Clin Psychol Rev. 1984;4(4):379-401.
22. Link BG, Andrews H, Cullen FT. The violent and illegal behavior of mental patients reconsidered. Am Sociol Rev. 1992;57(3):275-292.
23. Harris GT, Rice ME, Quinsey VL. Violent recidivism of mentally disordered offenders: the development of a statistical prediction instrument. Crim Justice and Behav. 1993;20(4):315-335.
24. Klassen D, O’Connor W. Demographic and case history variables in risk assessment. In: Monahan J, Steadman H, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:229-257.
25. Hart SD, Hare RD, Forth AE. Psychopathy as a risk marker for violence: development and validation of a screening version of the revised Psychopathy Checklist. In: Monahan J, Steadman HJ, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:81-98.
26. Cleckley H. The mask of sanity. St. Louis, MO: Mosby; 1941.
27. Harris GT, Rice ME, Cormier CA. Psychopathy and violent recidivism. Law Hum Behav. 1991;15(6):625-637.
28. Steadman HJ, Mulvey EP, Monahan J. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393-401.
29. Meloy JR, White SG, Hart S. Workplace assessment of targeted violence risk: the development and reliability of the WAVR-21. J Forensic Sci. 2013;58(5):1353-1358.
30. Borum R, Fein R, Vossekuil B, et al. Threat assessment: defining an approach for evaluating risk of targeted violence. Behav Sci Law. 1999;17(3):323-337.
31. Tyrer P, Bateman AW. Drug treatment for personality disorders. Adv Psychiatr Treat. 2004;10(5):389-398.
1. Skeem J, Kennealy P, Monahan J, et al. Psychosis uncommonly and inconsistently precedes violence among high-risk individuals. Clin Psychol Sci. 2016;4(1):40-49.
2. McGinty E, Frattaroli S, Appelbaum PS, et al. Using research evidence to reframe the policy debate around mental illness and guns: process and recommendations. Am J Public Health. 2014;104(11):e22-e26.
3. Sumner SA, Mercy JA, Dahlberg LL, et al. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478-488.
4. Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep. 2016;65(5):1-96.
5. Borum R, Swartz M, Swanson J. Assessing and managing violence risk in clinical practice. J Prac Psychiatry Behav Health. 1996;2(4):205-215.
6. Swanson JW, Holzer CE 3rd, Ganju VK, et al. Violence and psychiatric disorder in the community: Evidence from the epidemiologic catchment area surveys. Hosp Community Psychiatry. 1990;41(7):761-770.
7. Swanson JW. Explaining rare acts of violence: the limits of evidence from population research. Psychiatr Serv. 2011;62(11):1369-1371.
8. Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychol Bull. 1998;123(2):123-142.
9. Monahan J. The inclusion of biological risk factors in violence risk assessments. In: Singh I, Sinnott-Armstrong W, Savulescu J, eds. Bioprediction, biomarkers, and bad behavior: scientific, legal, and ethical implications. New York, NY: Oxford University Press; 2014:57-76.
10. Murray J, Thomson ME. Clinical judgement in violence risk assessment. Eur J Psychol. 2010;6(1):128-149.
11. Mossman D. Violence risk: is clinical judgment enough? Current Psychiatry. 2008;7(6):66-72.
12. Douglas T, Pugh J, Singh I, et al. Risk assessment tools in criminal justice and forensic psychiatry: the need for better data. Eur Psychiatry. 2017;42:134-137.
13. Dolan M, Doyle M. Violence risk prediction. Clinical and actuarial measures and the role of the psychopathy checklist. Br J Psychiatry. 2000;177:303-311.
14. Fazel S, Singh J, Doll H, et al. Use of risk assessment instruments to predict violence and antisocial behaviour in 73 samples involving 24 827 people: systematic review and meta-analysis. BMJ. 2012;345:e4692. doi: 10.1136/bmj.e4692.
15. National Collaborating Centre for Mental Health (UK). Violence and aggression: short- term management in mental health, health, and community settings: updated edition. London: British Psychological Society; 2015. NICE Guideline, No 10.
16. Klassen D, O’Connor WA. Predicting violence in schizophrenic and non-schizophrenic patients: a prospective study. J Community Psychol. 1988;16(2):217-227.
17. Scott C, Resnick P. Clinical assessment of aggression and violence. In: Rosner R, Scott C, eds. Principles and practice of forensic psychiatry, 3rd ed. Boca Raton, FL: CRC Press; 2017:623-631.
18. Tardiff K, Sweillam A. Assault, suicide, and mental illness. Arch Gen Psychiatry. 1980;37(2):164-169.
19. Lidz CW, Mulvey EP, Gardner W. The accuracy of predictions of violence to others. JAMA. 1993;269(8):1007-1011.
20. Newhill CE, Mulvey EP, Lidz CW. Characteristics of violence in the community by female patients seen in a psychiatric emergency service. Psychiatric Serv. 1995;46(8):785-789.
21. Mulvey E, Lidz C. Clinical considerations in the prediction of dangerousness in mental patients. Clin Psychol Rev. 1984;4(4):379-401.
22. Link BG, Andrews H, Cullen FT. The violent and illegal behavior of mental patients reconsidered. Am Sociol Rev. 1992;57(3):275-292.
23. Harris GT, Rice ME, Quinsey VL. Violent recidivism of mentally disordered offenders: the development of a statistical prediction instrument. Crim Justice and Behav. 1993;20(4):315-335.
24. Klassen D, O’Connor W. Demographic and case history variables in risk assessment. In: Monahan J, Steadman H, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:229-257.
25. Hart SD, Hare RD, Forth AE. Psychopathy as a risk marker for violence: development and validation of a screening version of the revised Psychopathy Checklist. In: Monahan J, Steadman HJ, eds. Violence and mental disorder: developments in risk assessment. Chicago, IL: University of Chicago Press; 1994:81-98.
26. Cleckley H. The mask of sanity. St. Louis, MO: Mosby; 1941.
27. Harris GT, Rice ME, Cormier CA. Psychopathy and violent recidivism. Law Hum Behav. 1991;15(6):625-637.
28. Steadman HJ, Mulvey EP, Monahan J. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393-401.
29. Meloy JR, White SG, Hart S. Workplace assessment of targeted violence risk: the development and reliability of the WAVR-21. J Forensic Sci. 2013;58(5):1353-1358.
30. Borum R, Fein R, Vossekuil B, et al. Threat assessment: defining an approach for evaluating risk of targeted violence. Behav Sci Law. 1999;17(3):323-337.
31. Tyrer P, Bateman AW. Drug treatment for personality disorders. Adv Psychiatr Treat. 2004;10(5):389-398.
Fetal pathology exam performed without consent: $500,000 verdict
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Fetal pathology exam performed without consent: $500,000 verdict
At 12 to 15 weeks' gestation, a fetus was found to have died. An ObGyn stimulated uterine contractions with misoprostol and the fetus was delivered.
The parents requested chromosomal testing to determine the cause of death. The ObGyn took samples of the baby's skin near the umbilical cord and from the placenta. He told the parents that the tests might come back as inconclusive, and that it may be necessary to take further samples. The couple was also told that, under hospital policy, the fetus must go to the pathology department before being taken to a funeral home. The parents told the ObGyn that they did not want further samples taken for any reason, and that nothing else should be done to their child before funeral preparations. The placenta, umbilical cord, and fetus were placed in 2 separate containers. The container with the placenta and umbilical cord had an anatomic pathology requisition form, indicating that a surgical pathology exam was to be performed. The container with the fetus did not have a requisition form. When the father accompanied the nurse who carried the containers to the pathology department, he told a general technologist that no additional tissue samples were to be taken from the fetus.
The next day, the pathologist made an incision on the fetus' left side and took a sample to create a slide for microscopic analysis. The parents discovered the incision at the funeral home.
PARENTS' CLAIM: The parents sued the hospital and pathologist. The pathologist was negligent in performing a surgical pathology examination without consent. The hospital had a duty to communicate the parents' desires to the pathologist.
According to hospital protocol, the nurse who attended the delivery was to fill out the proper forms and ensure that they were available to the pathologist. The container with the fetus should have had its own requisition form that instructed the pathologist to not perform any further testing. Every specimen that goes to pathology should have a requisition form, per guidelines from the College of American Pathologists (CAP). Without a form, the pathologist should not do anything with the sample.
The parents' verbal instructions not to take additional samples from the fetus were never relayed to the pathologist.
DEFENDANTS' DEFENSE: The hospital and pathologist denied negligence. A single requisition form was appropriate; the containers' labeling and the form made it clear that the placenta, umbilical cord, and fetus were from the same patient. CAP guidelines do not require separate forms. The remains were in the gross room at pathology, which is where specimens are taken for review and analysis. Therefore, the pathologist assumed he was to perform a standard pathology exam on both containers. The technologist with whom the father had spoken met the accepted standard of care.
VERDICT: A $500,000 Maine verdict was returned. The pathologist (through insurance) and the hospital equally shared payment of the award.
When should delivery have occurred? $4M verdict
Concerned that her fetus had stopped moving, a mother presented to the ED. Results of fetal heart-rate (FHR) monitoring ordered by the attending ObGyn (Dr. A) were nonreassuring. A second ObGyn (Dr. B) ordered a fetal biophysical profile (BPP); the score was 2 points. Although a low score usually results in immediate delivery, Dr. B consulted a maternal-fetal medicine (MFM) specialist. After another fetal BPP scored 8 points, the mother was discharged.
The next day, the mother called her ObGyn (Dr. C), who told her to immediately come to his office. A fetal BPP scored 4 points, with nonreassuring fetal heart sounds.
The mother was transported to the hospital for emergency cesarean delivery. At birth, the baby was blue, not breathing, and had meconium in his lungs. After 6 minutes' resuscitation, he began breathing. The child has an hypoxic brain injury.
PARENTS' CLAIM: Based on the nonreassuring FHR readings when the mother first reported lack of fetal movement, and a BPP of 2 points, an immediate cesarean delivery should have been performed. If the child had been delivered in a timely manner, he would have escaped a brain injury. At the very least, the mother should have been kept in the hospital for monitoring.
DEFENDANTS' DEFENSE: Drs. A and B and the hospital claimed that the child did not have a hypoxic injury; he had gastroschisis.
VERDICT: A $4,098,266 New York verdict was returned.
Second twin's birth delayed; brain damage: $1.5M settlement
A 35-year-old woman was 30 weeks' pregnant with twins when she was admitted to a hospital at high risk. At 36 weeks' gestation, she went into labor. A resident called the ObGyn to report that the patient was ready to deliver and waiting to push. The ObGyn advised that he was tied up in another procedure and for the mother to wait until he could get there.
Forty minutes later, the ObGyn arrived and the mother was allowed to push. A first-year resident delivered the first twin without incident. The second twin shifted from a cephalic presentation to a double foot- ling breech presentation and his FHR reflected severe bradycardia. Under the supervision of the ObGyn, a fourth-year resident managed the delivery, which took 28 minutes. The second twin's Apgar scores were low. He was intubated and transferred to a children's hospital for brain cooling.
PARENTS' CLAIM: Although excellent care following the birth reduced the degree of brain damage, the delay caused by the ObGyn's late arrival was responsible for the child's injuries.
PHYSICIAN'S DEFENSE: In pretrial findings, a panel of physicians reported that the child did not have a qualifying injury. However, the case settled before the trial began.
VERDICT: A $1.5 million Virginia settlement was reached.
Pregnant mother prepares for child's congenital heart disorder
A mother was told that her fetus had tricuspid atresia, a congenital defect. The mother and pediatric cardiologist developed a treatment plan to perform a balloon heart procedure at birth then transfer the baby to a specialized hospital.
After birth at a local hospital, the child was also found to have a lung disorder. He was promptly placed on a respirator. The hospital's pediatric cardiologist decided that the baby was too fragile to undergo the balloon procedure, and that the procedure could wait until the child was more stable. The baby died on his third day of life.
The neonatologists involved in treating the baby determined that the cause of death was tricuspid atresia. A pathologist reported that the death was due to a combination of congenital heart and lung disorders.
ESTATE'S CLAIM: The hospital team was sued for not following the prenatal plan. The baby's condition was serious but survivable if treated properly.
DEFENDANTS' DEFENSE: The hospital team made the correct decision to stabilize the baby's lung conditions before performing the balloon repair. The baby died because both his heart and lungs were compromised. The child's chance of survival was very small.
VERDICT: A Mississippi defense verdict was returned.
Severe uterine atony and PPH: hysterectomy
A 35-year-old woman at 41 weeks' gestation was admitted to the hospital in active labor at 5:45 am on July 26. At 2:45 pm, an ObGyn noted that she was 8+ cm dilated, 90% effaced, and that the baby's head was at -1 station. At 6:00 pm, the membranes were artificially ruptured. At 7:45 pm, examination revealed no change in her cervix. The ObGyn reviewed the options with the mother, including offering an epidural and cesarean delivery. At 8:30 pm, an intrauterine pressure catheter was placed. The ObGyn noted an inadequate labor pattern and ordered augmentation with oxytocin. On July 27 at 12:50 am, examination revealed that the cervix was completely dilated and the baby's head was at +1 station. At 2:30 am, oxytocin was infusing at 12 mU/m. At 2:30 am, the patient began to push. By 4:30 am, oxytocin was running at 14 mU/m and the patient continued to push. At 5:00 am, the ObGyn noted no further progression of labor and recommended a cesarean delivery, but the mother wanted to push a little longer. At 6:00 am, with no further progress, the decision was made to perform cesarean delivery. At 6:40 am, the patient was transferred to the operating room and delivery occurred at 7:08 am. The baby weighed 9.5 lb.
The mother's uterus was closed and hemostasis was reached. However, uterine atony was persistent and did not respond to multiple doses of medication or uterine massage. Persistent atony led to postpartum hemorrhaging (PPH). The ObGyn used conservative methods to control the hemorrhage, including medications and sutures. He then called for assistance from another ObGyn, and performed ligation of the utero-ovarian ligaments and additional suturing, which had no effect on the bleeding. They attempted an ovarian artery ligation and placed additional sutures, but the PPH continued. The ObGyn recommended a hysterectomy to the patient and her husband, who agreed. A supracervical hysterectomy was performed. During the procedure, the left ovary tore and was removed.
PARENTS' CLAIM: The patient and her husband spoke at trial of their intention to have more than one child. They sued the ObGyn, her practice, and the hospital. The ObGyn was negligent in allowing labor to continue for too long, for using oxytocin to stimulate contractions, and for allowing the patient to push for several hours, given that the baby was large. Oxytocin stimulation for so many hours without labor progression created an unacceptably high risk of uterine atony. This led to a nonreversible atonic state after delivery, which caused the patient to lose her uterus, left ovary, and her ability to reproduce.
DEFENDANTS' DEFENSE: The ObGyn was not negligent. The ObGyn met the standard of care in the management of labor and delivery. She was attentive, present at appropriate intervals, and there was no point at which a different decision should have been made. The ObGyn allowed the patient to have input in the decision-making process, as long as the ObGyn was comfortable that the decision was not compromising the safety of mother and baby. The length of labor and size of the fetus increased the risk of atony. However, in most cases, this does not occur; it can occur without those risk factors. PPH is a serious but frequently unavoidable complication of childbirth. The ObGyn's management was appropriate and prevented the patient's death.
VERDICT: A Pennsylvania defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Failure to find cancer earlier; patient dies: $4.69M verdict
Failure to find cancer earlier; patient dies: $4.69M verdict
On July 19, a 26-year-old woman presented to the emergency department (ED) with abnormal vaginal bleeding 3 months after giving birth. She was found to have endometrial thickening and an elevated ß human chorionic gonadotropin level. An ObGyn (Dr. A) assumed that the patient was having a miscarriage and sent her home.
On July 30, when the patient returned to the ED with continued bleeding, lesions on her cervix and urethra were discovered. A second ObGyn, Dr. B, addressed the bleeding, removed the lesion, and ordered testing. On August 17, the patient saw a third ObGyn (Dr. C), who did not conduct an examination.
Days later, the patient suffered a brain hemorrhage that was suspicious for hemorrhagic metastasis. After that, stage IV choriocarcinoma was identified. Although she underwent chemotherapy, the patient died 18 months later.
ESTATE'S CLAIM: All 3 ObGyns failed to take a proper history, conduct adequate examinations, and order appropriate testing. Even at stage IV, 75% of patients with choriocarcinoma survive past 5 years. The stroke rendered chemotherapy less effective and substantially contributed to the patient's death. Failure to diagnose the cancer before the stroke allowed the disease to progress beyond the point at which the patient's life could be saved.
DEFENDANTS' DEFENSE: The ObGyns and hospital claimed that appropriate care was provided and that they were not negligent in failing to consider the diagnosis of a very rare form of cancer.
VERDICT: A $4.69 million New Jersey verdict was returned, with all 3 physicians held partially liable.
Hot speculum burns patient: $547,090 award
A 54-year-old woman underwent a hysterectomy performed at a government-operated hospital. After she was anesthetized and unconscious, a second-year resident took a speculum that had been placed in the sterile field by a nurse, and inserted it in the patient's vagina.
When the patient awoke from surgery, she discovered significant burns to her vaginal area, perineum, anus, and buttocks.
PATIENT'S CLAIM: The speculum had just been removed from the autoclave and was very hot. The patient incurred substantial medical bills to treat her injuries and was unable to work for several months. She sued the hospital and resident, alleging error by the nurse in placing the hot speculum in the sterile field without cooling it or advising the resident that it was still hot. The resident was blamed for using the speculum without confirming that it was hot.
DEFENDANTS' DEFENSE: The resident claimed that she reasonably relied on the nurse to not place a hot instrument in the surgical field without first cooling it. The hospital, representing the nurse, denied fault, blaming the resident for not checking the speculum.
VERDICT: A $547,090 Louisiana verdict was awarded by a judge against the resident and the hospital, but it was halved by comparative fault to $273,545.
Surgeon's breast exam insufficient: $375,000 verdict
After a woman in her early 40s found a lump in her left breast, she underwent a radiographic study, which a radiologist interpreted as showing a 3-mm cyst. Without performing additional tests, a general surgeon immediately scheduled her for surgery.
On May 17, the radiologist performed an ultrasound-guided needle-localized biopsy and found a nodule. The patient was immediately sent to the operating room where the surgeon performed a segmental resection of the nodule.
On May 24, the patient presented to the surgeon's office for a postoperative visit. She told the nurse that the palpable mass was still there. The nurse examined the mass, told the patient that the incision was healing nicely, and suggested follow-up in a month.
Four months later, the patient sought a second opinion. On September 15, she underwent a diagnostic mammogram, ultrasound, and biopsy. The biopsy was positive for invasive ductal carcinoma. On September 30, magnetic resonance imaging and a second biopsy further confirmed the diagnosis. On November 2, she underwent a segmental mastectomy with sentinel lymph node biopsy. The pathology report noted a 3-cm invasive ductal carcinoma with necrosis. The patient underwent chemotherapy and radiation treatment.
PATIENT'S CLAIM: She sued the general surgeon, radiologist, and surgical center, alleging that her breast cancer went undiagnosed. Prior to trial, the radiologist and surgical center were dismissed from the case.
The surgeon failed to perform a thorough physical examination and nodal evaluation of the left breast and axilla. His substandard methods to diagnose and treat the patient's breast cancer delayed proper treatment and significantly altered the outcome.
PHYSICIAN'S CLAIM: The surgeon's treatment met the standard of care. The outcome and treatment were not significantly changed by the delay.
VERDICT: A $375,000 Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Failure to find cancer earlier; patient dies: $4.69M verdict
On July 19, a 26-year-old woman presented to the emergency department (ED) with abnormal vaginal bleeding 3 months after giving birth. She was found to have endometrial thickening and an elevated ß human chorionic gonadotropin level. An ObGyn (Dr. A) assumed that the patient was having a miscarriage and sent her home.
On July 30, when the patient returned to the ED with continued bleeding, lesions on her cervix and urethra were discovered. A second ObGyn, Dr. B, addressed the bleeding, removed the lesion, and ordered testing. On August 17, the patient saw a third ObGyn (Dr. C), who did not conduct an examination.
Days later, the patient suffered a brain hemorrhage that was suspicious for hemorrhagic metastasis. After that, stage IV choriocarcinoma was identified. Although she underwent chemotherapy, the patient died 18 months later.
ESTATE'S CLAIM: All 3 ObGyns failed to take a proper history, conduct adequate examinations, and order appropriate testing. Even at stage IV, 75% of patients with choriocarcinoma survive past 5 years. The stroke rendered chemotherapy less effective and substantially contributed to the patient's death. Failure to diagnose the cancer before the stroke allowed the disease to progress beyond the point at which the patient's life could be saved.
DEFENDANTS' DEFENSE: The ObGyns and hospital claimed that appropriate care was provided and that they were not negligent in failing to consider the diagnosis of a very rare form of cancer.
VERDICT: A $4.69 million New Jersey verdict was returned, with all 3 physicians held partially liable.
Hot speculum burns patient: $547,090 award
A 54-year-old woman underwent a hysterectomy performed at a government-operated hospital. After she was anesthetized and unconscious, a second-year resident took a speculum that had been placed in the sterile field by a nurse, and inserted it in the patient's vagina.
When the patient awoke from surgery, she discovered significant burns to her vaginal area, perineum, anus, and buttocks.
PATIENT'S CLAIM: The speculum had just been removed from the autoclave and was very hot. The patient incurred substantial medical bills to treat her injuries and was unable to work for several months. She sued the hospital and resident, alleging error by the nurse in placing the hot speculum in the sterile field without cooling it or advising the resident that it was still hot. The resident was blamed for using the speculum without confirming that it was hot.
DEFENDANTS' DEFENSE: The resident claimed that she reasonably relied on the nurse to not place a hot instrument in the surgical field without first cooling it. The hospital, representing the nurse, denied fault, blaming the resident for not checking the speculum.
VERDICT: A $547,090 Louisiana verdict was awarded by a judge against the resident and the hospital, but it was halved by comparative fault to $273,545.
Surgeon's breast exam insufficient: $375,000 verdict
After a woman in her early 40s found a lump in her left breast, she underwent a radiographic study, which a radiologist interpreted as showing a 3-mm cyst. Without performing additional tests, a general surgeon immediately scheduled her for surgery.
On May 17, the radiologist performed an ultrasound-guided needle-localized biopsy and found a nodule. The patient was immediately sent to the operating room where the surgeon performed a segmental resection of the nodule.
On May 24, the patient presented to the surgeon's office for a postoperative visit. She told the nurse that the palpable mass was still there. The nurse examined the mass, told the patient that the incision was healing nicely, and suggested follow-up in a month.
Four months later, the patient sought a second opinion. On September 15, she underwent a diagnostic mammogram, ultrasound, and biopsy. The biopsy was positive for invasive ductal carcinoma. On September 30, magnetic resonance imaging and a second biopsy further confirmed the diagnosis. On November 2, she underwent a segmental mastectomy with sentinel lymph node biopsy. The pathology report noted a 3-cm invasive ductal carcinoma with necrosis. The patient underwent chemotherapy and radiation treatment.
PATIENT'S CLAIM: She sued the general surgeon, radiologist, and surgical center, alleging that her breast cancer went undiagnosed. Prior to trial, the radiologist and surgical center were dismissed from the case.
The surgeon failed to perform a thorough physical examination and nodal evaluation of the left breast and axilla. His substandard methods to diagnose and treat the patient's breast cancer delayed proper treatment and significantly altered the outcome.
PHYSICIAN'S CLAIM: The surgeon's treatment met the standard of care. The outcome and treatment were not significantly changed by the delay.
VERDICT: A $375,000 Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Failure to find cancer earlier; patient dies: $4.69M verdict
On July 19, a 26-year-old woman presented to the emergency department (ED) with abnormal vaginal bleeding 3 months after giving birth. She was found to have endometrial thickening and an elevated ß human chorionic gonadotropin level. An ObGyn (Dr. A) assumed that the patient was having a miscarriage and sent her home.
On July 30, when the patient returned to the ED with continued bleeding, lesions on her cervix and urethra were discovered. A second ObGyn, Dr. B, addressed the bleeding, removed the lesion, and ordered testing. On August 17, the patient saw a third ObGyn (Dr. C), who did not conduct an examination.
Days later, the patient suffered a brain hemorrhage that was suspicious for hemorrhagic metastasis. After that, stage IV choriocarcinoma was identified. Although she underwent chemotherapy, the patient died 18 months later.
ESTATE'S CLAIM: All 3 ObGyns failed to take a proper history, conduct adequate examinations, and order appropriate testing. Even at stage IV, 75% of patients with choriocarcinoma survive past 5 years. The stroke rendered chemotherapy less effective and substantially contributed to the patient's death. Failure to diagnose the cancer before the stroke allowed the disease to progress beyond the point at which the patient's life could be saved.
DEFENDANTS' DEFENSE: The ObGyns and hospital claimed that appropriate care was provided and that they were not negligent in failing to consider the diagnosis of a very rare form of cancer.
VERDICT: A $4.69 million New Jersey verdict was returned, with all 3 physicians held partially liable.
Hot speculum burns patient: $547,090 award
A 54-year-old woman underwent a hysterectomy performed at a government-operated hospital. After she was anesthetized and unconscious, a second-year resident took a speculum that had been placed in the sterile field by a nurse, and inserted it in the patient's vagina.
When the patient awoke from surgery, she discovered significant burns to her vaginal area, perineum, anus, and buttocks.
PATIENT'S CLAIM: The speculum had just been removed from the autoclave and was very hot. The patient incurred substantial medical bills to treat her injuries and was unable to work for several months. She sued the hospital and resident, alleging error by the nurse in placing the hot speculum in the sterile field without cooling it or advising the resident that it was still hot. The resident was blamed for using the speculum without confirming that it was hot.
DEFENDANTS' DEFENSE: The resident claimed that she reasonably relied on the nurse to not place a hot instrument in the surgical field without first cooling it. The hospital, representing the nurse, denied fault, blaming the resident for not checking the speculum.
VERDICT: A $547,090 Louisiana verdict was awarded by a judge against the resident and the hospital, but it was halved by comparative fault to $273,545.
Surgeon's breast exam insufficient: $375,000 verdict
After a woman in her early 40s found a lump in her left breast, she underwent a radiographic study, which a radiologist interpreted as showing a 3-mm cyst. Without performing additional tests, a general surgeon immediately scheduled her for surgery.
On May 17, the radiologist performed an ultrasound-guided needle-localized biopsy and found a nodule. The patient was immediately sent to the operating room where the surgeon performed a segmental resection of the nodule.
On May 24, the patient presented to the surgeon's office for a postoperative visit. She told the nurse that the palpable mass was still there. The nurse examined the mass, told the patient that the incision was healing nicely, and suggested follow-up in a month.
Four months later, the patient sought a second opinion. On September 15, she underwent a diagnostic mammogram, ultrasound, and biopsy. The biopsy was positive for invasive ductal carcinoma. On September 30, magnetic resonance imaging and a second biopsy further confirmed the diagnosis. On November 2, she underwent a segmental mastectomy with sentinel lymph node biopsy. The pathology report noted a 3-cm invasive ductal carcinoma with necrosis. The patient underwent chemotherapy and radiation treatment.
PATIENT'S CLAIM: She sued the general surgeon, radiologist, and surgical center, alleging that her breast cancer went undiagnosed. Prior to trial, the radiologist and surgical center were dismissed from the case.
The surgeon failed to perform a thorough physical examination and nodal evaluation of the left breast and axilla. His substandard methods to diagnose and treat the patient's breast cancer delayed proper treatment and significantly altered the outcome.
PHYSICIAN'S CLAIM: The surgeon's treatment met the standard of care. The outcome and treatment were not significantly changed by the delay.
VERDICT: A $375,000 Pennsylvania verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.