User login
Mitigating risk of asthma emergencies during respiratory season
Respiratory illness, cold weather, and fluctuating temperatures can all exacerbate asthma symptoms, leading to potentially serious health complications. Understanding how to mitigate these risks is crucial for maintaining respiratory health and ensuring a safe and healthy season.
As schools across the US have just ended their fall semester, students of all ages will spend their time off away from school. Respiratory season is among us, and children with asthma are at risk for severe asthma exacerbation from viruses that may lead to hospitalization. Since students will soon return for their spring semester, it is important to be reminded of asthma care during respiratory season.
Ten percent of school-aged children in the US have a diagnosis of asthma, with a higher prevalence in lower socioeconomic populations. In a classroom of 30 students, three students carry an asthma diagnosis. Of these children, the National Institutes of Health (NIH) reports 60% will experience asthma exacerbations. These exacerbations not only cause patients with asthma to have a total of 13.8 million absences annually but also lead to approximately 767,000 emergency department visits and 74,000 hospitalizations on an annual basis.1
As we consider these statistics, safe asthma care during respiratory season requires preparation and a proactive approach. Partnering with families and school personnel will increase the likelihood that students will have a safe return for their next semester.
Patients with asthma are at higher risk for complications from respiratory illnesses such as COVID-19, influenza, respiratory syncytial virus (RSV), and streptococcal pneumonia viruses. While RSV vaccination is not widely available yet, vaccination is recommended as early as possible for influenza and COVID-19, as well as consideration for streptococcal pneumonia for patients with severe asthma. Vaccination for all family members should also be considered by the health care team. The health care team should regularly check in with families of patients with asthma to ensure they are educated about the importance of vaccinations and opportunities for immunization.2
Most children with asthma submit their asthma action plan to their school at the beginning of the year. It is important for families to be reminded that if there is a change to their asthma action plan, the updated plan should be discussed and reviewed with school personnel who are responsible for medication administration. Health care providers often will partner with schools and families to create a 504 plan. Many families may not be familiar with this plan and how to request one. Within the state of Illinois, for example, some school districts require 504 plans and others do not. It is derived from Section 504 of the Americans with Disabilities Act and is a contract outlining a child’s asthma care while at school. Families should be reminded that these 504 plans need to be updated at least once a school year.3
Asthma guidelines recommend all children with asthma have access to quick relief medications.4 While this guideline exists, we are reminded by families that their child oftentimes has difficulty obtaining their medication while at school. Despite stock albuterol programs considered by the NIH as being a safe, practical, and potentially lifesaving option for children with asthma, schools across the country are slow to adopt this practice.1 Families often express financial concern about accessing these medications, mainly due to insurance quantity limitations for either single maintenance and reliever therapy intervention or short-acting β2-agonist therapy.
While self-carry is an option in all 50 states and the District of Columbia, parents report poor memory and reliability of their child to administer their medication appropriately. Parents report their children have a poor understanding of time and may administer medication too frequently, or they lack the necessary dexterity to properly administer an inhaler. The correct use of inhalation devices and adherence to prescribed therapy are key aspects in achieving better clinical control and improved quality of life. Parents express fear associated with children having access but poor direct supervision when using their quick relief medication.5 Families need a minimum of two quick relief inhalers (one for home and one for school)—or even three in a co-parenting situation.
Stock albuterol programs mitigate the risk of quick relief medication accessibility. Families may have been required to leave a quick relief inhaler with the school nurse when school started last fall. Despite medication being available from a stock program or supplied from a family, medication expiration dates should be monitored to ensure the medication is available when needed.1 It is important to remind families to track the expiration of medication and request a refill from their asthma provider for replacement at school if a stock albuterol program is not available.
Mitigating the risk of asthma emergencies during respiratory season requires a proactive approach. By partnering with families and schools through vaccination, updating asthma action plans, creating 504 plans, and working to ensure quick relief medication is available, providers and families can work together to decrease the risk of asthma emergencies during respiratory season. Taking these steps can lead to a safer and healthier respiratory season for all.
Emily Simmons, MSN, APN, CPNP-PC, and Alexandra Kacena, MSN, APN, CPNP-PC, are advanced practice provider colleagues at Ann & Robert H. Lurie Children’s Hospital of Chicago, Division of Pulmonary & Sleep Medicine. Partnering with one of the attending pulmonologists, they provide evidence-based, state-of-the-art care to high-risk patients with severe asthma, both within the hospital and in a mobile asthma clinic setting.
References:
1. Lowe AA, Gerald JK, Clemens CJ, Stern DA, Gerald LB. Managing respiratory emergencies at school: a county-wide stock inhaler program. J Allergy Clin Immunol. 2021;148(2):420-427.e5. Preprint. Posted online February 10, 2021. doi: 10.1016/j.jaci.2021.01.028
2. 5 Reasons Why Children With Asthma Need Important Vaccines for the Back-to-School Season. Asthma and Allergy Foundation of America. https://community.aafa.org/blog/5-reasons-why-children-with-asthma-need-important-vaccines-before-heading-back-to-school
3. Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis. 2016;11:2509-2517. doi: 10.2147/COPD.S114576
4. Volerman A, Lowe AA, Pappalardo AA, etc. Ensuring access to albuterol in schools: from policy to implementation. An official ATS/AANMA/ALA/NASN policy statement. Am J Respir Crit Care Med. 2021;204(5):508-522. doi: 10.1164/rccm.202106-1550ST
5. Volerman A, Kim TY, Sridharan G, et al. A mixed-methods study examining inhaler carry and use among children at school. J Asthma. 2020;57(10):1071-1082. Preprint. Posted online July 16, 2019. doi: 10.1080/02770903.2019.1640729
6. Toups MM, Press VG, Volerman A. National analysis of state health policies on students’ right to self-carry and self-administer asthma inhalers at school. J Sch Health. 2018;88(10):776-784. doi: 10.1111/josh.12681
7. 504 Plans for Asthma. Asthma and Allergy Foundation of America. https://aafa.org/asthma/living-with-asthma/504-plans-for-asthma/
Respiratory illness, cold weather, and fluctuating temperatures can all exacerbate asthma symptoms, leading to potentially serious health complications. Understanding how to mitigate these risks is crucial for maintaining respiratory health and ensuring a safe and healthy season.
As schools across the US have just ended their fall semester, students of all ages will spend their time off away from school. Respiratory season is among us, and children with asthma are at risk for severe asthma exacerbation from viruses that may lead to hospitalization. Since students will soon return for their spring semester, it is important to be reminded of asthma care during respiratory season.
Ten percent of school-aged children in the US have a diagnosis of asthma, with a higher prevalence in lower socioeconomic populations. In a classroom of 30 students, three students carry an asthma diagnosis. Of these children, the National Institutes of Health (NIH) reports 60% will experience asthma exacerbations. These exacerbations not only cause patients with asthma to have a total of 13.8 million absences annually but also lead to approximately 767,000 emergency department visits and 74,000 hospitalizations on an annual basis.1
As we consider these statistics, safe asthma care during respiratory season requires preparation and a proactive approach. Partnering with families and school personnel will increase the likelihood that students will have a safe return for their next semester.
Patients with asthma are at higher risk for complications from respiratory illnesses such as COVID-19, influenza, respiratory syncytial virus (RSV), and streptococcal pneumonia viruses. While RSV vaccination is not widely available yet, vaccination is recommended as early as possible for influenza and COVID-19, as well as consideration for streptococcal pneumonia for patients with severe asthma. Vaccination for all family members should also be considered by the health care team. The health care team should regularly check in with families of patients with asthma to ensure they are educated about the importance of vaccinations and opportunities for immunization.2
Most children with asthma submit their asthma action plan to their school at the beginning of the year. It is important for families to be reminded that if there is a change to their asthma action plan, the updated plan should be discussed and reviewed with school personnel who are responsible for medication administration. Health care providers often will partner with schools and families to create a 504 plan. Many families may not be familiar with this plan and how to request one. Within the state of Illinois, for example, some school districts require 504 plans and others do not. It is derived from Section 504 of the Americans with Disabilities Act and is a contract outlining a child’s asthma care while at school. Families should be reminded that these 504 plans need to be updated at least once a school year.3
Asthma guidelines recommend all children with asthma have access to quick relief medications.4 While this guideline exists, we are reminded by families that their child oftentimes has difficulty obtaining their medication while at school. Despite stock albuterol programs considered by the NIH as being a safe, practical, and potentially lifesaving option for children with asthma, schools across the country are slow to adopt this practice.1 Families often express financial concern about accessing these medications, mainly due to insurance quantity limitations for either single maintenance and reliever therapy intervention or short-acting β2-agonist therapy.
While self-carry is an option in all 50 states and the District of Columbia, parents report poor memory and reliability of their child to administer their medication appropriately. Parents report their children have a poor understanding of time and may administer medication too frequently, or they lack the necessary dexterity to properly administer an inhaler. The correct use of inhalation devices and adherence to prescribed therapy are key aspects in achieving better clinical control and improved quality of life. Parents express fear associated with children having access but poor direct supervision when using their quick relief medication.5 Families need a minimum of two quick relief inhalers (one for home and one for school)—or even three in a co-parenting situation.
Stock albuterol programs mitigate the risk of quick relief medication accessibility. Families may have been required to leave a quick relief inhaler with the school nurse when school started last fall. Despite medication being available from a stock program or supplied from a family, medication expiration dates should be monitored to ensure the medication is available when needed.1 It is important to remind families to track the expiration of medication and request a refill from their asthma provider for replacement at school if a stock albuterol program is not available.
Mitigating the risk of asthma emergencies during respiratory season requires a proactive approach. By partnering with families and schools through vaccination, updating asthma action plans, creating 504 plans, and working to ensure quick relief medication is available, providers and families can work together to decrease the risk of asthma emergencies during respiratory season. Taking these steps can lead to a safer and healthier respiratory season for all.
Emily Simmons, MSN, APN, CPNP-PC, and Alexandra Kacena, MSN, APN, CPNP-PC, are advanced practice provider colleagues at Ann & Robert H. Lurie Children’s Hospital of Chicago, Division of Pulmonary & Sleep Medicine. Partnering with one of the attending pulmonologists, they provide evidence-based, state-of-the-art care to high-risk patients with severe asthma, both within the hospital and in a mobile asthma clinic setting.
References:
1. Lowe AA, Gerald JK, Clemens CJ, Stern DA, Gerald LB. Managing respiratory emergencies at school: a county-wide stock inhaler program. J Allergy Clin Immunol. 2021;148(2):420-427.e5. Preprint. Posted online February 10, 2021. doi: 10.1016/j.jaci.2021.01.028
2. 5 Reasons Why Children With Asthma Need Important Vaccines for the Back-to-School Season. Asthma and Allergy Foundation of America. https://community.aafa.org/blog/5-reasons-why-children-with-asthma-need-important-vaccines-before-heading-back-to-school
3. Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis. 2016;11:2509-2517. doi: 10.2147/COPD.S114576
4. Volerman A, Lowe AA, Pappalardo AA, etc. Ensuring access to albuterol in schools: from policy to implementation. An official ATS/AANMA/ALA/NASN policy statement. Am J Respir Crit Care Med. 2021;204(5):508-522. doi: 10.1164/rccm.202106-1550ST
5. Volerman A, Kim TY, Sridharan G, et al. A mixed-methods study examining inhaler carry and use among children at school. J Asthma. 2020;57(10):1071-1082. Preprint. Posted online July 16, 2019. doi: 10.1080/02770903.2019.1640729
6. Toups MM, Press VG, Volerman A. National analysis of state health policies on students’ right to self-carry and self-administer asthma inhalers at school. J Sch Health. 2018;88(10):776-784. doi: 10.1111/josh.12681
7. 504 Plans for Asthma. Asthma and Allergy Foundation of America. https://aafa.org/asthma/living-with-asthma/504-plans-for-asthma/
Respiratory illness, cold weather, and fluctuating temperatures can all exacerbate asthma symptoms, leading to potentially serious health complications. Understanding how to mitigate these risks is crucial for maintaining respiratory health and ensuring a safe and healthy season.
As schools across the US have just ended their fall semester, students of all ages will spend their time off away from school. Respiratory season is among us, and children with asthma are at risk for severe asthma exacerbation from viruses that may lead to hospitalization. Since students will soon return for their spring semester, it is important to be reminded of asthma care during respiratory season.
Ten percent of school-aged children in the US have a diagnosis of asthma, with a higher prevalence in lower socioeconomic populations. In a classroom of 30 students, three students carry an asthma diagnosis. Of these children, the National Institutes of Health (NIH) reports 60% will experience asthma exacerbations. These exacerbations not only cause patients with asthma to have a total of 13.8 million absences annually but also lead to approximately 767,000 emergency department visits and 74,000 hospitalizations on an annual basis.1
As we consider these statistics, safe asthma care during respiratory season requires preparation and a proactive approach. Partnering with families and school personnel will increase the likelihood that students will have a safe return for their next semester.
Patients with asthma are at higher risk for complications from respiratory illnesses such as COVID-19, influenza, respiratory syncytial virus (RSV), and streptococcal pneumonia viruses. While RSV vaccination is not widely available yet, vaccination is recommended as early as possible for influenza and COVID-19, as well as consideration for streptococcal pneumonia for patients with severe asthma. Vaccination for all family members should also be considered by the health care team. The health care team should regularly check in with families of patients with asthma to ensure they are educated about the importance of vaccinations and opportunities for immunization.2
Most children with asthma submit their asthma action plan to their school at the beginning of the year. It is important for families to be reminded that if there is a change to their asthma action plan, the updated plan should be discussed and reviewed with school personnel who are responsible for medication administration. Health care providers often will partner with schools and families to create a 504 plan. Many families may not be familiar with this plan and how to request one. Within the state of Illinois, for example, some school districts require 504 plans and others do not. It is derived from Section 504 of the Americans with Disabilities Act and is a contract outlining a child’s asthma care while at school. Families should be reminded that these 504 plans need to be updated at least once a school year.3
Asthma guidelines recommend all children with asthma have access to quick relief medications.4 While this guideline exists, we are reminded by families that their child oftentimes has difficulty obtaining their medication while at school. Despite stock albuterol programs considered by the NIH as being a safe, practical, and potentially lifesaving option for children with asthma, schools across the country are slow to adopt this practice.1 Families often express financial concern about accessing these medications, mainly due to insurance quantity limitations for either single maintenance and reliever therapy intervention or short-acting β2-agonist therapy.
While self-carry is an option in all 50 states and the District of Columbia, parents report poor memory and reliability of their child to administer their medication appropriately. Parents report their children have a poor understanding of time and may administer medication too frequently, or they lack the necessary dexterity to properly administer an inhaler. The correct use of inhalation devices and adherence to prescribed therapy are key aspects in achieving better clinical control and improved quality of life. Parents express fear associated with children having access but poor direct supervision when using their quick relief medication.5 Families need a minimum of two quick relief inhalers (one for home and one for school)—or even three in a co-parenting situation.
Stock albuterol programs mitigate the risk of quick relief medication accessibility. Families may have been required to leave a quick relief inhaler with the school nurse when school started last fall. Despite medication being available from a stock program or supplied from a family, medication expiration dates should be monitored to ensure the medication is available when needed.1 It is important to remind families to track the expiration of medication and request a refill from their asthma provider for replacement at school if a stock albuterol program is not available.
Mitigating the risk of asthma emergencies during respiratory season requires a proactive approach. By partnering with families and schools through vaccination, updating asthma action plans, creating 504 plans, and working to ensure quick relief medication is available, providers and families can work together to decrease the risk of asthma emergencies during respiratory season. Taking these steps can lead to a safer and healthier respiratory season for all.
Emily Simmons, MSN, APN, CPNP-PC, and Alexandra Kacena, MSN, APN, CPNP-PC, are advanced practice provider colleagues at Ann & Robert H. Lurie Children’s Hospital of Chicago, Division of Pulmonary & Sleep Medicine. Partnering with one of the attending pulmonologists, they provide evidence-based, state-of-the-art care to high-risk patients with severe asthma, both within the hospital and in a mobile asthma clinic setting.
References:
1. Lowe AA, Gerald JK, Clemens CJ, Stern DA, Gerald LB. Managing respiratory emergencies at school: a county-wide stock inhaler program. J Allergy Clin Immunol. 2021;148(2):420-427.e5. Preprint. Posted online February 10, 2021. doi: 10.1016/j.jaci.2021.01.028
2. 5 Reasons Why Children With Asthma Need Important Vaccines for the Back-to-School Season. Asthma and Allergy Foundation of America. https://community.aafa.org/blog/5-reasons-why-children-with-asthma-need-important-vaccines-before-heading-back-to-school
3. Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis. 2016;11:2509-2517. doi: 10.2147/COPD.S114576
4. Volerman A, Lowe AA, Pappalardo AA, etc. Ensuring access to albuterol in schools: from policy to implementation. An official ATS/AANMA/ALA/NASN policy statement. Am J Respir Crit Care Med. 2021;204(5):508-522. doi: 10.1164/rccm.202106-1550ST
5. Volerman A, Kim TY, Sridharan G, et al. A mixed-methods study examining inhaler carry and use among children at school. J Asthma. 2020;57(10):1071-1082. Preprint. Posted online July 16, 2019. doi: 10.1080/02770903.2019.1640729
6. Toups MM, Press VG, Volerman A. National analysis of state health policies on students’ right to self-carry and self-administer asthma inhalers at school. J Sch Health. 2018;88(10):776-784. doi: 10.1111/josh.12681
7. 504 Plans for Asthma. Asthma and Allergy Foundation of America. https://aafa.org/asthma/living-with-asthma/504-plans-for-asthma/
Top reads from the CHEST journal portfolio
Top reads from the CHEST journal portfolio
Journal CHEST®
Nocturnal Cardiac Arrhythmias in Heart Failure With Obstructive and Central Sleep Apnea
By Christian M. Horvath, MD, and colleagues
Horvath et al’s ancillary analysis to the ADVENT-HF trial highlights a significant association between sleep apnea (OSA and CSA) and increased nocturnal cardiac arrhythmias in heart failure patients with reduced ejection fraction (HFrEF). While ADVENT-HF showed no impact of adaptive servo-ventilation on survival and hospitalization, this subanalysis reveals a higher prevalence of arrhythmias, such as excessive supraventricular ectopic activity and atrial fibrillation/flutter (AF), in these patients. Notably, OSA severity was linked to increased atrial ectopy, though not to persistent arrhythmias like AF, contrasting with prior studies, notably from the Sleep Heart Health Study (Mehra et al, AJRCCM. 2006;173(8)). This suggests a complex interplay between OSA/CSA and AF, perhaps mediated by factors such as sympathetic tone and cardiac remodeling. Clinically, these findings underscore the value of targeted sleep apnea screening in patients with HFrEF and suggest the need for individualized arrhythmia risk profiles. Future research should investigate how additional factors mediate sleep apnea’s arrhythmic impact.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
Improving Spontaneous Breathing Trials With a Respiratory Therapist-Driven Protocol
By Christopher A. Linke, RN, MHI, CSSBB, and colleagues
Use of respiratory therapist (RT)-driven spontaneous breathing trial (SBT) protocols are known to improve patient outcomes related to extubation from mechanical ventilation. The authors of this study asked whether an RT-driven SBT protocol could be consistently implemented and sustained to improve outcomes. This single-site quality improvement (QI) project aimed to standardize and re-establish an RT-driven protocol for screening patients for SBT readiness and administering SBTs to appropriate patients in an academic ICU. One hundred twenty-eight patients representing 759 safety screen weaning assessment opportunities were included over a baseline sample and three plan-do-study-act (PDSA) cycles. A key takeaway from this QI project is that consistent use of an RT-driven SBT protocol results in improved use and documentation of an SBT safety screening and completion of an SBT earlier in the day. Despite multiple obstacles, including staffing and communication challenges and poor understanding of terminology, standardization of an RT-driven SBT protocol is achievable.
– Commentary by Mary Jo Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
Navigational Bronchoscopy vs CT Scan-Guided Transthoracic Needle Biopsy for the Diagnosis of Indeterminate Lung Nodules
By Robert J. Lentz, MD, and colleagues
, which will evaluate navigational bronchoscopy (NB) and CT-guided transthoracic needle biopsy (CT-TTNB) for diagnosing indeterminate pulmonary nodules. Although the results are not yet available, this group’s work highlights an emphasis to develop multicenter randomized controlled trials with multidisciplinary teams and clinical impactful data with a primary outcome of diagnostic accuracy (diagnostic results that remain accurate through 12 months of clinical follow-up). If NB proves to be a noninferior alternative to CT-TTNB, then it may be a safer option with a lower complication rate (particularly for pneumothorax). We look forward to the final results from the trial, and future studies incorporating newer technologies, including robotic bronchoscopy, will be a welcome adjunct as well.
– Commentary by Saadia A. Faiz, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST®
Nocturnal Cardiac Arrhythmias in Heart Failure With Obstructive and Central Sleep Apnea
By Christian M. Horvath, MD, and colleagues
Horvath et al’s ancillary analysis to the ADVENT-HF trial highlights a significant association between sleep apnea (OSA and CSA) and increased nocturnal cardiac arrhythmias in heart failure patients with reduced ejection fraction (HFrEF). While ADVENT-HF showed no impact of adaptive servo-ventilation on survival and hospitalization, this subanalysis reveals a higher prevalence of arrhythmias, such as excessive supraventricular ectopic activity and atrial fibrillation/flutter (AF), in these patients. Notably, OSA severity was linked to increased atrial ectopy, though not to persistent arrhythmias like AF, contrasting with prior studies, notably from the Sleep Heart Health Study (Mehra et al, AJRCCM. 2006;173(8)). This suggests a complex interplay between OSA/CSA and AF, perhaps mediated by factors such as sympathetic tone and cardiac remodeling. Clinically, these findings underscore the value of targeted sleep apnea screening in patients with HFrEF and suggest the need for individualized arrhythmia risk profiles. Future research should investigate how additional factors mediate sleep apnea’s arrhythmic impact.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
Improving Spontaneous Breathing Trials With a Respiratory Therapist-Driven Protocol
By Christopher A. Linke, RN, MHI, CSSBB, and colleagues
Use of respiratory therapist (RT)-driven spontaneous breathing trial (SBT) protocols are known to improve patient outcomes related to extubation from mechanical ventilation. The authors of this study asked whether an RT-driven SBT protocol could be consistently implemented and sustained to improve outcomes. This single-site quality improvement (QI) project aimed to standardize and re-establish an RT-driven protocol for screening patients for SBT readiness and administering SBTs to appropriate patients in an academic ICU. One hundred twenty-eight patients representing 759 safety screen weaning assessment opportunities were included over a baseline sample and three plan-do-study-act (PDSA) cycles. A key takeaway from this QI project is that consistent use of an RT-driven SBT protocol results in improved use and documentation of an SBT safety screening and completion of an SBT earlier in the day. Despite multiple obstacles, including staffing and communication challenges and poor understanding of terminology, standardization of an RT-driven SBT protocol is achievable.
– Commentary by Mary Jo Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
Navigational Bronchoscopy vs CT Scan-Guided Transthoracic Needle Biopsy for the Diagnosis of Indeterminate Lung Nodules
By Robert J. Lentz, MD, and colleagues
, which will evaluate navigational bronchoscopy (NB) and CT-guided transthoracic needle biopsy (CT-TTNB) for diagnosing indeterminate pulmonary nodules. Although the results are not yet available, this group’s work highlights an emphasis to develop multicenter randomized controlled trials with multidisciplinary teams and clinical impactful data with a primary outcome of diagnostic accuracy (diagnostic results that remain accurate through 12 months of clinical follow-up). If NB proves to be a noninferior alternative to CT-TTNB, then it may be a safer option with a lower complication rate (particularly for pneumothorax). We look forward to the final results from the trial, and future studies incorporating newer technologies, including robotic bronchoscopy, will be a welcome adjunct as well.
– Commentary by Saadia A. Faiz, MD, FCCP, Member of the CHEST Physician Editorial Board
Journal CHEST®
Nocturnal Cardiac Arrhythmias in Heart Failure With Obstructive and Central Sleep Apnea
By Christian M. Horvath, MD, and colleagues
Horvath et al’s ancillary analysis to the ADVENT-HF trial highlights a significant association between sleep apnea (OSA and CSA) and increased nocturnal cardiac arrhythmias in heart failure patients with reduced ejection fraction (HFrEF). While ADVENT-HF showed no impact of adaptive servo-ventilation on survival and hospitalization, this subanalysis reveals a higher prevalence of arrhythmias, such as excessive supraventricular ectopic activity and atrial fibrillation/flutter (AF), in these patients. Notably, OSA severity was linked to increased atrial ectopy, though not to persistent arrhythmias like AF, contrasting with prior studies, notably from the Sleep Heart Health Study (Mehra et al, AJRCCM. 2006;173(8)). This suggests a complex interplay between OSA/CSA and AF, perhaps mediated by factors such as sympathetic tone and cardiac remodeling. Clinically, these findings underscore the value of targeted sleep apnea screening in patients with HFrEF and suggest the need for individualized arrhythmia risk profiles. Future research should investigate how additional factors mediate sleep apnea’s arrhythmic impact.
– Commentary by Shyam Subramanian, MD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Critical Care
Improving Spontaneous Breathing Trials With a Respiratory Therapist-Driven Protocol
By Christopher A. Linke, RN, MHI, CSSBB, and colleagues
Use of respiratory therapist (RT)-driven spontaneous breathing trial (SBT) protocols are known to improve patient outcomes related to extubation from mechanical ventilation. The authors of this study asked whether an RT-driven SBT protocol could be consistently implemented and sustained to improve outcomes. This single-site quality improvement (QI) project aimed to standardize and re-establish an RT-driven protocol for screening patients for SBT readiness and administering SBTs to appropriate patients in an academic ICU. One hundred twenty-eight patients representing 759 safety screen weaning assessment opportunities were included over a baseline sample and three plan-do-study-act (PDSA) cycles. A key takeaway from this QI project is that consistent use of an RT-driven SBT protocol results in improved use and documentation of an SBT safety screening and completion of an SBT earlier in the day. Despite multiple obstacles, including staffing and communication challenges and poor understanding of terminology, standardization of an RT-driven SBT protocol is achievable.
– Commentary by Mary Jo Farmer, MD, PhD, FCCP, Member of the CHEST Physician Editorial Board
CHEST® Pulmonary
Navigational Bronchoscopy vs CT Scan-Guided Transthoracic Needle Biopsy for the Diagnosis of Indeterminate Lung Nodules
By Robert J. Lentz, MD, and colleagues
, which will evaluate navigational bronchoscopy (NB) and CT-guided transthoracic needle biopsy (CT-TTNB) for diagnosing indeterminate pulmonary nodules. Although the results are not yet available, this group’s work highlights an emphasis to develop multicenter randomized controlled trials with multidisciplinary teams and clinical impactful data with a primary outcome of diagnostic accuracy (diagnostic results that remain accurate through 12 months of clinical follow-up). If NB proves to be a noninferior alternative to CT-TTNB, then it may be a safer option with a lower complication rate (particularly for pneumothorax). We look forward to the final results from the trial, and future studies incorporating newer technologies, including robotic bronchoscopy, will be a welcome adjunct as well.
– Commentary by Saadia A. Faiz, MD, FCCP, Member of the CHEST Physician Editorial Board
Top reads from the CHEST journal portfolio
Top reads from the CHEST journal portfolio
Council of Networks: Reflecting on the success of 2024
I have had the privilege of being the Chair of the Council of Networks this past year, and the engagement of the Chairs, Vice-Chairs, and steering committee members has contributed to a very successful CHEST 2024. Highlights from the meeting include the depth and breadth of 22 Experience CHEST sessions, which were held in the Exhibit Hall and gave trainees and early career faculty the opportunity to submit and present concise teaching on a topic. This year, many of these presentations were devoted to topics of diversity and inclusion.
Our program this year also honored Network Rising Stars at the Network Open Forums. These individuals were early career members who were nominated for their active engagement within CHEST and the Networks. The Networks also hosted a fun and engaging mixer, where members came together and had the opportunity to meet Network leadership, catch up with old friends, and sample a variety of Boston cuisine. I personally had the opportunity to meet several junior faculty who were excited to become involved in the Networks.
One of the initiatives we are working on is developing a robust mentoring program for fellows who are involved in the Networks and Sections. The pieces were put in place over the summer, and we will be gauging success of the program in the spring.
For those of you who have yet to join a Network, we would love for you to be involved. To see the current leadership of each Network, check out their pages on chesnet.org. You can log in to your CHEST account and join as many Networks as you want.
I have had the privilege of being the Chair of the Council of Networks this past year, and the engagement of the Chairs, Vice-Chairs, and steering committee members has contributed to a very successful CHEST 2024. Highlights from the meeting include the depth and breadth of 22 Experience CHEST sessions, which were held in the Exhibit Hall and gave trainees and early career faculty the opportunity to submit and present concise teaching on a topic. This year, many of these presentations were devoted to topics of diversity and inclusion.
Our program this year also honored Network Rising Stars at the Network Open Forums. These individuals were early career members who were nominated for their active engagement within CHEST and the Networks. The Networks also hosted a fun and engaging mixer, where members came together and had the opportunity to meet Network leadership, catch up with old friends, and sample a variety of Boston cuisine. I personally had the opportunity to meet several junior faculty who were excited to become involved in the Networks.
One of the initiatives we are working on is developing a robust mentoring program for fellows who are involved in the Networks and Sections. The pieces were put in place over the summer, and we will be gauging success of the program in the spring.
For those of you who have yet to join a Network, we would love for you to be involved. To see the current leadership of each Network, check out their pages on chesnet.org. You can log in to your CHEST account and join as many Networks as you want.
I have had the privilege of being the Chair of the Council of Networks this past year, and the engagement of the Chairs, Vice-Chairs, and steering committee members has contributed to a very successful CHEST 2024. Highlights from the meeting include the depth and breadth of 22 Experience CHEST sessions, which were held in the Exhibit Hall and gave trainees and early career faculty the opportunity to submit and present concise teaching on a topic. This year, many of these presentations were devoted to topics of diversity and inclusion.
Our program this year also honored Network Rising Stars at the Network Open Forums. These individuals were early career members who were nominated for their active engagement within CHEST and the Networks. The Networks also hosted a fun and engaging mixer, where members came together and had the opportunity to meet Network leadership, catch up with old friends, and sample a variety of Boston cuisine. I personally had the opportunity to meet several junior faculty who were excited to become involved in the Networks.
One of the initiatives we are working on is developing a robust mentoring program for fellows who are involved in the Networks and Sections. The pieces were put in place over the summer, and we will be gauging success of the program in the spring.
For those of you who have yet to join a Network, we would love for you to be involved. To see the current leadership of each Network, check out their pages on chesnet.org. You can log in to your CHEST account and join as many Networks as you want.
A visible impact
In 2023, CHEST’s philanthropic approach evolved to align with the organizational mission and elevate the value placed on giving. This was a pivotal transformation allowing CHEST to broaden its scope and deepen its impact, ensuring that every contribution continues to make a meaningful difference. 2024 was the first full year since the transition, and Bob Musacchio, PhD, CEO of CHEST, and Bob De Marco, MD, FCCP, Chair of the CHEST Board of Advisors, sat down to reflect on the year of CHEST philanthropy.
It’s been a full year since the transition to CHEST philanthropy; from your perspective, how has that transition gone so far?
Bob De Marco, MD, FCCP: It’s been a real pleasure to watch the evolution over the past year. The pillars that we defined to support our giving strategy resonated with a lot of past donors and also helped to engage new donors. Through clinical research, community impact, and dedication to education, we know exactly where our focus should be, allowing us to have the strongest impact while ensuring that donors know exactly where their gifts are going.
Bob Musacchio, PhD: Another benefit to the redefined strategy was its clear integration with the CHEST organization. In the past year, CHEST added social responsibility as one of the organizational pillars, which clarified the commitment to both philanthropy and advocacy. By aligning every element of philanthropy with the existing CHEST mission, we are able to expand our reach exponentially.
Let’s talk about an example of impact you’ve seen in the past year.
De Marco: When the original CHEST Foundation merged with CHEST, we established a new priority that continues to drive our mission: bridging gaps, breaking barriers, and improving health care interactions to enhance patient outcomes and overall health. This commitment is reflected in initiatives like Bridging Specialties® and the First 5 Minutes®—both of which you can learn more about on the CHEST website.
We’ve also entered into the second year of our partnership grant with the Association of Pulmonary and Critical Care Medicine Program Directors, which supports a fellow pursuing pulmonary and critical care medicine. This award recognizes the value of a diverse community in advancing medical education in pulmonary and critical care medicine. It provides an Accreditation Council for Graduate Medical Education fellow-in-training with the support, training, and mentorship needed to pursue a career in medical education and eventually serve as a mentor to future trainees.
Musacchio: I’d like to highlight the growth we’ve seen in our Community Impact grants. Following the shift, the impact grants now follow a participatory grantmaking model that empowers local organizations embedded within their communities to solve problems with the unique insights and solutions that only they can provide. This new strategy includes supporting our Community Connections partners, which are highlighted during the annual meeting. In Boston for CHEST 2024, we partnered with three local organizations—Boston Health Care for the Homeless Program, We Got Us, and the Tufts Community Health Workers Engaging in Integrated Care and Community Action Programs Inter-City collaboration—as our Community Connections to financially support their causes and to highlight their work throughout our meeting. Through partnership, we can strengthen our impact and empower communities to prioritize and improve respiratory well-being, and I look forward to continuing to grow this program in Chicago for CHEST 2025.
What’s next for CHEST philanthropy? Any closing thoughts for CHEST Physician® readers?
De Marco: The future is limitless for CHEST philanthropy. The more funding we receive, the more we can distribute to deserving projects. This includes expanding support to additional disease states, funding the next wave of travel grants, and giving more to support the research and clinical innovations that will shape the future of chest medicine . What I’d love to see is more CHEST members engaging with CHEST philanthropy. We invite you to connect with us—CHEST’s philanthropy team—to discuss how your continued investment can drive even greater impact or ask any questions you may have about the program. We’d welcome the opportunity to talk with you!
Also, if you’re thinking about giving before the end of the year, please know that every gift, new or increased, will be matched dollar for dollar through December 31.
To each and every one of you: Thank you for being a part of the CHEST community—and for your generosity and dedication.
Musacchio: I echo Dr. De Marco’s sentiment and want to reiterate that whether you’re a seasoned donor or considering your first gift, you can play a vital role in shaping the future of our field. Every gift—large or small—moves us forward and strengthens the community we all value. Thank you, and have a happy and healthy holiday season.
MAKE A GIFT TODAY
In 2023, CHEST’s philanthropic approach evolved to align with the organizational mission and elevate the value placed on giving. This was a pivotal transformation allowing CHEST to broaden its scope and deepen its impact, ensuring that every contribution continues to make a meaningful difference. 2024 was the first full year since the transition, and Bob Musacchio, PhD, CEO of CHEST, and Bob De Marco, MD, FCCP, Chair of the CHEST Board of Advisors, sat down to reflect on the year of CHEST philanthropy.
It’s been a full year since the transition to CHEST philanthropy; from your perspective, how has that transition gone so far?
Bob De Marco, MD, FCCP: It’s been a real pleasure to watch the evolution over the past year. The pillars that we defined to support our giving strategy resonated with a lot of past donors and also helped to engage new donors. Through clinical research, community impact, and dedication to education, we know exactly where our focus should be, allowing us to have the strongest impact while ensuring that donors know exactly where their gifts are going.
Bob Musacchio, PhD: Another benefit to the redefined strategy was its clear integration with the CHEST organization. In the past year, CHEST added social responsibility as one of the organizational pillars, which clarified the commitment to both philanthropy and advocacy. By aligning every element of philanthropy with the existing CHEST mission, we are able to expand our reach exponentially.
Let’s talk about an example of impact you’ve seen in the past year.
De Marco: When the original CHEST Foundation merged with CHEST, we established a new priority that continues to drive our mission: bridging gaps, breaking barriers, and improving health care interactions to enhance patient outcomes and overall health. This commitment is reflected in initiatives like Bridging Specialties® and the First 5 Minutes®—both of which you can learn more about on the CHEST website.
We’ve also entered into the second year of our partnership grant with the Association of Pulmonary and Critical Care Medicine Program Directors, which supports a fellow pursuing pulmonary and critical care medicine. This award recognizes the value of a diverse community in advancing medical education in pulmonary and critical care medicine. It provides an Accreditation Council for Graduate Medical Education fellow-in-training with the support, training, and mentorship needed to pursue a career in medical education and eventually serve as a mentor to future trainees.
Musacchio: I’d like to highlight the growth we’ve seen in our Community Impact grants. Following the shift, the impact grants now follow a participatory grantmaking model that empowers local organizations embedded within their communities to solve problems with the unique insights and solutions that only they can provide. This new strategy includes supporting our Community Connections partners, which are highlighted during the annual meeting. In Boston for CHEST 2024, we partnered with three local organizations—Boston Health Care for the Homeless Program, We Got Us, and the Tufts Community Health Workers Engaging in Integrated Care and Community Action Programs Inter-City collaboration—as our Community Connections to financially support their causes and to highlight their work throughout our meeting. Through partnership, we can strengthen our impact and empower communities to prioritize and improve respiratory well-being, and I look forward to continuing to grow this program in Chicago for CHEST 2025.
What’s next for CHEST philanthropy? Any closing thoughts for CHEST Physician® readers?
De Marco: The future is limitless for CHEST philanthropy. The more funding we receive, the more we can distribute to deserving projects. This includes expanding support to additional disease states, funding the next wave of travel grants, and giving more to support the research and clinical innovations that will shape the future of chest medicine . What I’d love to see is more CHEST members engaging with CHEST philanthropy. We invite you to connect with us—CHEST’s philanthropy team—to discuss how your continued investment can drive even greater impact or ask any questions you may have about the program. We’d welcome the opportunity to talk with you!
Also, if you’re thinking about giving before the end of the year, please know that every gift, new or increased, will be matched dollar for dollar through December 31.
To each and every one of you: Thank you for being a part of the CHEST community—and for your generosity and dedication.
Musacchio: I echo Dr. De Marco’s sentiment and want to reiterate that whether you’re a seasoned donor or considering your first gift, you can play a vital role in shaping the future of our field. Every gift—large or small—moves us forward and strengthens the community we all value. Thank you, and have a happy and healthy holiday season.
MAKE A GIFT TODAY
In 2023, CHEST’s philanthropic approach evolved to align with the organizational mission and elevate the value placed on giving. This was a pivotal transformation allowing CHEST to broaden its scope and deepen its impact, ensuring that every contribution continues to make a meaningful difference. 2024 was the first full year since the transition, and Bob Musacchio, PhD, CEO of CHEST, and Bob De Marco, MD, FCCP, Chair of the CHEST Board of Advisors, sat down to reflect on the year of CHEST philanthropy.
It’s been a full year since the transition to CHEST philanthropy; from your perspective, how has that transition gone so far?
Bob De Marco, MD, FCCP: It’s been a real pleasure to watch the evolution over the past year. The pillars that we defined to support our giving strategy resonated with a lot of past donors and also helped to engage new donors. Through clinical research, community impact, and dedication to education, we know exactly where our focus should be, allowing us to have the strongest impact while ensuring that donors know exactly where their gifts are going.
Bob Musacchio, PhD: Another benefit to the redefined strategy was its clear integration with the CHEST organization. In the past year, CHEST added social responsibility as one of the organizational pillars, which clarified the commitment to both philanthropy and advocacy. By aligning every element of philanthropy with the existing CHEST mission, we are able to expand our reach exponentially.
Let’s talk about an example of impact you’ve seen in the past year.
De Marco: When the original CHEST Foundation merged with CHEST, we established a new priority that continues to drive our mission: bridging gaps, breaking barriers, and improving health care interactions to enhance patient outcomes and overall health. This commitment is reflected in initiatives like Bridging Specialties® and the First 5 Minutes®—both of which you can learn more about on the CHEST website.
We’ve also entered into the second year of our partnership grant with the Association of Pulmonary and Critical Care Medicine Program Directors, which supports a fellow pursuing pulmonary and critical care medicine. This award recognizes the value of a diverse community in advancing medical education in pulmonary and critical care medicine. It provides an Accreditation Council for Graduate Medical Education fellow-in-training with the support, training, and mentorship needed to pursue a career in medical education and eventually serve as a mentor to future trainees.
Musacchio: I’d like to highlight the growth we’ve seen in our Community Impact grants. Following the shift, the impact grants now follow a participatory grantmaking model that empowers local organizations embedded within their communities to solve problems with the unique insights and solutions that only they can provide. This new strategy includes supporting our Community Connections partners, which are highlighted during the annual meeting. In Boston for CHEST 2024, we partnered with three local organizations—Boston Health Care for the Homeless Program, We Got Us, and the Tufts Community Health Workers Engaging in Integrated Care and Community Action Programs Inter-City collaboration—as our Community Connections to financially support their causes and to highlight their work throughout our meeting. Through partnership, we can strengthen our impact and empower communities to prioritize and improve respiratory well-being, and I look forward to continuing to grow this program in Chicago for CHEST 2025.
What’s next for CHEST philanthropy? Any closing thoughts for CHEST Physician® readers?
De Marco: The future is limitless for CHEST philanthropy. The more funding we receive, the more we can distribute to deserving projects. This includes expanding support to additional disease states, funding the next wave of travel grants, and giving more to support the research and clinical innovations that will shape the future of chest medicine . What I’d love to see is more CHEST members engaging with CHEST philanthropy. We invite you to connect with us—CHEST’s philanthropy team—to discuss how your continued investment can drive even greater impact or ask any questions you may have about the program. We’d welcome the opportunity to talk with you!
Also, if you’re thinking about giving before the end of the year, please know that every gift, new or increased, will be matched dollar for dollar through December 31.
To each and every one of you: Thank you for being a part of the CHEST community—and for your generosity and dedication.
Musacchio: I echo Dr. De Marco’s sentiment and want to reiterate that whether you’re a seasoned donor or considering your first gift, you can play a vital role in shaping the future of our field. Every gift—large or small—moves us forward and strengthens the community we all value. Thank you, and have a happy and healthy holiday season.
MAKE A GIFT TODAY
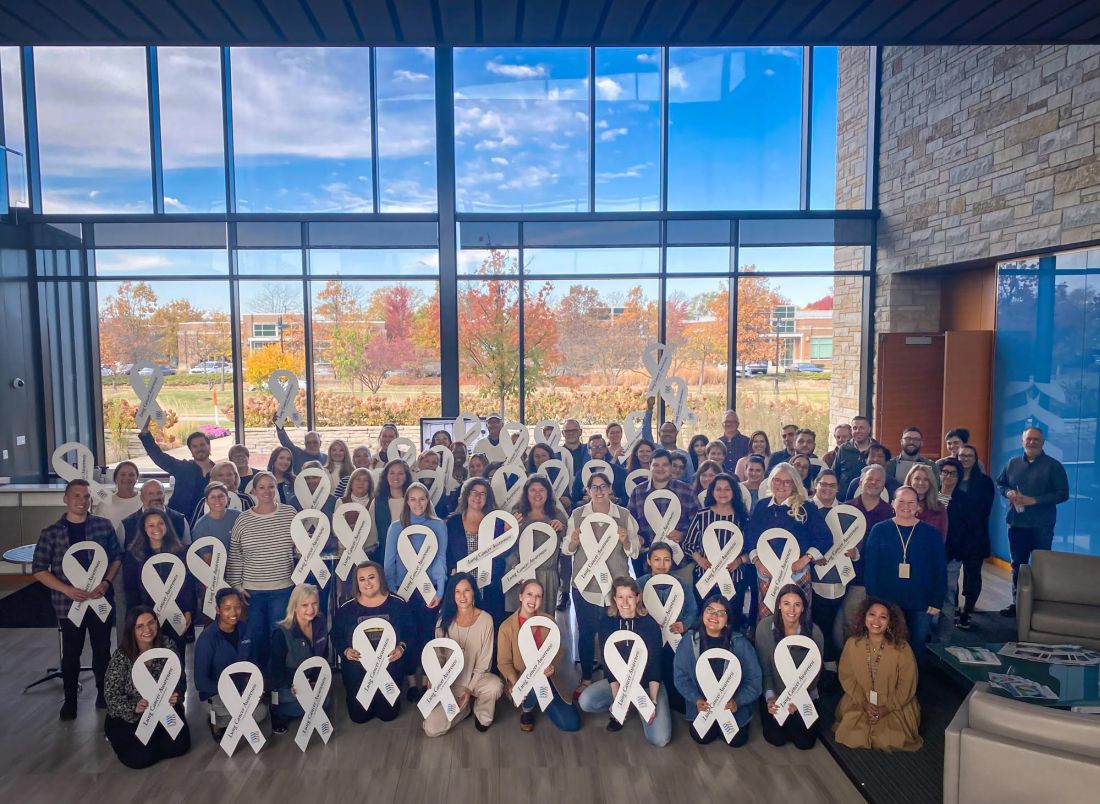
White ribbons around CHEST HQ raise awareness for lung cancer screening and early detection
During the month of November, CHEST displayed white ribbons around its headquarters in Glenview, Illinois, to raise awareness for lung cancer screening and early detection.
According to the World Health Organization, lung cancer kills more people yearly than breast, colon, and prostate cancers combined, and there are 2.1 million lung cancer cases worldwide.
“Lung Cancer Awareness Month was an opportunity for us to shine the spotlight on a disease that is impacting the lives of so many,” said Robert Musacchio, PhD, CEO of CHEST. “As a society of 22,000 respiratory professionals, we continuously provide the latest resources to our members, including the latest guidelines for lung cancer screening. Leveraging the awareness month, we wanted to spread the message throughout our local community that the best way to combat lung cancer is through early screening and detection.”
To identify and diagnose lung cancer in its earlier stages, it is recommended to seek lung cancer screening with a low-dose tomography scan (also known as low-dose CT or LDCT scan). Individuals who meet the below criteria are considered to be at high risk for developing lung cancer and should be screened:
- 50 to 80 years of age;
- have a 20 pack-year history of smoking (one pack a day for 20 years, two packs a day for 10 years, etc.); or
- currently smoke or have quit within the last 15 years.
To secure the ribbons, CHEST worked with an organization called the White Ribbon Project, which promotes awareness about lung cancer by changing public perception of the disease. Started by lung cancer survivor Heidi Onda and her husband, Pierre Onda, MD, the white ribbon initiative has spurred a movement to build community, reframe education, increase awareness, and remove the stigma against lung cancer.
“We are grateful for the advocacy and support of the American College of Chest Physicians in raising awareness for lung cancer,” Ms. Onda said. “We believe as a team of survivors, caregivers, those who have lost loved ones, advocates, the medical and science communities, industry representatives, advocacy organizations, legislators, and cancer centers that we can change the public perception of lung cancer. Anyone with lungs can get lung cancer, no one deserves it, and awareness and early detection of the disease are crucial.”
During the month of November, CHEST displayed white ribbons around its headquarters in Glenview, Illinois, to raise awareness for lung cancer screening and early detection.
According to the World Health Organization, lung cancer kills more people yearly than breast, colon, and prostate cancers combined, and there are 2.1 million lung cancer cases worldwide.
“Lung Cancer Awareness Month was an opportunity for us to shine the spotlight on a disease that is impacting the lives of so many,” said Robert Musacchio, PhD, CEO of CHEST. “As a society of 22,000 respiratory professionals, we continuously provide the latest resources to our members, including the latest guidelines for lung cancer screening. Leveraging the awareness month, we wanted to spread the message throughout our local community that the best way to combat lung cancer is through early screening and detection.”
To identify and diagnose lung cancer in its earlier stages, it is recommended to seek lung cancer screening with a low-dose tomography scan (also known as low-dose CT or LDCT scan). Individuals who meet the below criteria are considered to be at high risk for developing lung cancer and should be screened:
- 50 to 80 years of age;
- have a 20 pack-year history of smoking (one pack a day for 20 years, two packs a day for 10 years, etc.); or
- currently smoke or have quit within the last 15 years.
To secure the ribbons, CHEST worked with an organization called the White Ribbon Project, which promotes awareness about lung cancer by changing public perception of the disease. Started by lung cancer survivor Heidi Onda and her husband, Pierre Onda, MD, the white ribbon initiative has spurred a movement to build community, reframe education, increase awareness, and remove the stigma against lung cancer.
“We are grateful for the advocacy and support of the American College of Chest Physicians in raising awareness for lung cancer,” Ms. Onda said. “We believe as a team of survivors, caregivers, those who have lost loved ones, advocates, the medical and science communities, industry representatives, advocacy organizations, legislators, and cancer centers that we can change the public perception of lung cancer. Anyone with lungs can get lung cancer, no one deserves it, and awareness and early detection of the disease are crucial.”
During the month of November, CHEST displayed white ribbons around its headquarters in Glenview, Illinois, to raise awareness for lung cancer screening and early detection.
According to the World Health Organization, lung cancer kills more people yearly than breast, colon, and prostate cancers combined, and there are 2.1 million lung cancer cases worldwide.
“Lung Cancer Awareness Month was an opportunity for us to shine the spotlight on a disease that is impacting the lives of so many,” said Robert Musacchio, PhD, CEO of CHEST. “As a society of 22,000 respiratory professionals, we continuously provide the latest resources to our members, including the latest guidelines for lung cancer screening. Leveraging the awareness month, we wanted to spread the message throughout our local community that the best way to combat lung cancer is through early screening and detection.”
To identify and diagnose lung cancer in its earlier stages, it is recommended to seek lung cancer screening with a low-dose tomography scan (also known as low-dose CT or LDCT scan). Individuals who meet the below criteria are considered to be at high risk for developing lung cancer and should be screened:
- 50 to 80 years of age;
- have a 20 pack-year history of smoking (one pack a day for 20 years, two packs a day for 10 years, etc.); or
- currently smoke or have quit within the last 15 years.
To secure the ribbons, CHEST worked with an organization called the White Ribbon Project, which promotes awareness about lung cancer by changing public perception of the disease. Started by lung cancer survivor Heidi Onda and her husband, Pierre Onda, MD, the white ribbon initiative has spurred a movement to build community, reframe education, increase awareness, and remove the stigma against lung cancer.
“We are grateful for the advocacy and support of the American College of Chest Physicians in raising awareness for lung cancer,” Ms. Onda said. “We believe as a team of survivors, caregivers, those who have lost loved ones, advocates, the medical and science communities, industry representatives, advocacy organizations, legislators, and cancer centers that we can change the public perception of lung cancer. Anyone with lungs can get lung cancer, no one deserves it, and awareness and early detection of the disease are crucial.”
Get to know Incoming CHEST President, John A. Howington, MD, MBA, FCCP
Starting January 1, 2025, current President-Elect, John A. Howington, MD, MBA, FCCP, will become the new President of CHEST.
Before Dr. Howington steps into the role of President, he spoke with CHEST for a glimpse into his aspirations for 2025.
What would you like to accomplish as President of CHEST?
First, I want to express my gratitude for the honor and privilege of serving as the 87th President of CHEST. The organization is well-served by a high functioning Board of Regents and an incredible staff. My primary goal is to build on the success and momentum of the presidential years of Dr. Buckley and Dr. Addrizzo-Harris. Their annual meetings were a huge success, and the energy and enthusiasm of our members are palpable.
I feel very strongly that great things are ahead of us in the fields of pulmonary medicine and critical care. The CHEST organization will continue to focus on our mission to crush lung disease and stay true to our values of community, inclusivity, innovation, advocacy, and integrity. With 2025 marking the 90th anniversary of the college, I very much look forward to sharing the impact of the organization and showcasing what is yet to come.
We will continue to collaborate with sister societies and like-minded industry partners to improve the quality of patient care and support clinicians in our field. Specifically, I look forward to continuing the momentum we’ve seen in early identification of lung cancer and increasing cure rates. Working as a team of interventional pulmonologists, respiratory therapists, advanced practice providers, thoracic surgeons, and more, we can make a real impact on what it means to be diagnosed with lung cancer.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
CHEST’s greatest strength is the people involved with the organization. There is such a wonderful culture of inclusivity and innovation cultivated by the outstanding staff, committed volunteers, and expert faculty leaders. We have focused on continuous board development for the last eight years and are seeing the benefits in the strategic and innovative steps the Board of Regents have taken to better serve our members and patients. It’s an honor to step into the role of leading such an extraordinary group.
What are some of the challenges facing CHEST, and how will you address them?
While not unique to CHEST, stress and burnout remain an issue in the field of health care. Clinicians are asked to do more with limited resources to provide high-quality care to an increasing number of patients with widely varying needs. We will continue to focus on providing guidance on best practices in the field of chest medicine and sharing innovations that reduce the burdens of health care delivery. To help alleviate the stress put on clinicians, we want to do our part to help remove anything that stands between a clinician and their ability to provide the best care for patients.
What do you ask of members to support you during your presidency?
What I would ask of our members is that they reach out to connect. I want to both celebrate your wins in the field and work with your suggestions to improve CHEST. Making the organization stronger is a collaborative effort, and every voice matters. My email starting January 1 is president@chestnet.org, and if you need some writing inspiration, I’ve got some suggested prompts:
- Share with me a recent personal success or that of a colleague; we want to help spread the word.
- What do you find most rewarding in your practice?
- What’s a recurring challenge you face in practice?
- What is CHEST getting right? Where can we improve?
I look forward to hearing from you.
Warmest regards,
John A. Howington, MD, MBA, FCCP
Starting January 1, 2025, current President-Elect, John A. Howington, MD, MBA, FCCP, will become the new President of CHEST.
Before Dr. Howington steps into the role of President, he spoke with CHEST for a glimpse into his aspirations for 2025.
What would you like to accomplish as President of CHEST?
First, I want to express my gratitude for the honor and privilege of serving as the 87th President of CHEST. The organization is well-served by a high functioning Board of Regents and an incredible staff. My primary goal is to build on the success and momentum of the presidential years of Dr. Buckley and Dr. Addrizzo-Harris. Their annual meetings were a huge success, and the energy and enthusiasm of our members are palpable.
I feel very strongly that great things are ahead of us in the fields of pulmonary medicine and critical care. The CHEST organization will continue to focus on our mission to crush lung disease and stay true to our values of community, inclusivity, innovation, advocacy, and integrity. With 2025 marking the 90th anniversary of the college, I very much look forward to sharing the impact of the organization and showcasing what is yet to come.
We will continue to collaborate with sister societies and like-minded industry partners to improve the quality of patient care and support clinicians in our field. Specifically, I look forward to continuing the momentum we’ve seen in early identification of lung cancer and increasing cure rates. Working as a team of interventional pulmonologists, respiratory therapists, advanced practice providers, thoracic surgeons, and more, we can make a real impact on what it means to be diagnosed with lung cancer.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
CHEST’s greatest strength is the people involved with the organization. There is such a wonderful culture of inclusivity and innovation cultivated by the outstanding staff, committed volunteers, and expert faculty leaders. We have focused on continuous board development for the last eight years and are seeing the benefits in the strategic and innovative steps the Board of Regents have taken to better serve our members and patients. It’s an honor to step into the role of leading such an extraordinary group.
What are some of the challenges facing CHEST, and how will you address them?
While not unique to CHEST, stress and burnout remain an issue in the field of health care. Clinicians are asked to do more with limited resources to provide high-quality care to an increasing number of patients with widely varying needs. We will continue to focus on providing guidance on best practices in the field of chest medicine and sharing innovations that reduce the burdens of health care delivery. To help alleviate the stress put on clinicians, we want to do our part to help remove anything that stands between a clinician and their ability to provide the best care for patients.
What do you ask of members to support you during your presidency?
What I would ask of our members is that they reach out to connect. I want to both celebrate your wins in the field and work with your suggestions to improve CHEST. Making the organization stronger is a collaborative effort, and every voice matters. My email starting January 1 is president@chestnet.org, and if you need some writing inspiration, I’ve got some suggested prompts:
- Share with me a recent personal success or that of a colleague; we want to help spread the word.
- What do you find most rewarding in your practice?
- What’s a recurring challenge you face in practice?
- What is CHEST getting right? Where can we improve?
I look forward to hearing from you.
Warmest regards,
John A. Howington, MD, MBA, FCCP
Starting January 1, 2025, current President-Elect, John A. Howington, MD, MBA, FCCP, will become the new President of CHEST.
Before Dr. Howington steps into the role of President, he spoke with CHEST for a glimpse into his aspirations for 2025.
What would you like to accomplish as President of CHEST?
First, I want to express my gratitude for the honor and privilege of serving as the 87th President of CHEST. The organization is well-served by a high functioning Board of Regents and an incredible staff. My primary goal is to build on the success and momentum of the presidential years of Dr. Buckley and Dr. Addrizzo-Harris. Their annual meetings were a huge success, and the energy and enthusiasm of our members are palpable.
I feel very strongly that great things are ahead of us in the fields of pulmonary medicine and critical care. The CHEST organization will continue to focus on our mission to crush lung disease and stay true to our values of community, inclusivity, innovation, advocacy, and integrity. With 2025 marking the 90th anniversary of the college, I very much look forward to sharing the impact of the organization and showcasing what is yet to come.
We will continue to collaborate with sister societies and like-minded industry partners to improve the quality of patient care and support clinicians in our field. Specifically, I look forward to continuing the momentum we’ve seen in early identification of lung cancer and increasing cure rates. Working as a team of interventional pulmonologists, respiratory therapists, advanced practice providers, thoracic surgeons, and more, we can make a real impact on what it means to be diagnosed with lung cancer.
What do you consider to be CHEST’s greatest strength, and how will you build upon this during your presidency?
CHEST’s greatest strength is the people involved with the organization. There is such a wonderful culture of inclusivity and innovation cultivated by the outstanding staff, committed volunteers, and expert faculty leaders. We have focused on continuous board development for the last eight years and are seeing the benefits in the strategic and innovative steps the Board of Regents have taken to better serve our members and patients. It’s an honor to step into the role of leading such an extraordinary group.
What are some of the challenges facing CHEST, and how will you address them?
While not unique to CHEST, stress and burnout remain an issue in the field of health care. Clinicians are asked to do more with limited resources to provide high-quality care to an increasing number of patients with widely varying needs. We will continue to focus on providing guidance on best practices in the field of chest medicine and sharing innovations that reduce the burdens of health care delivery. To help alleviate the stress put on clinicians, we want to do our part to help remove anything that stands between a clinician and their ability to provide the best care for patients.
What do you ask of members to support you during your presidency?
What I would ask of our members is that they reach out to connect. I want to both celebrate your wins in the field and work with your suggestions to improve CHEST. Making the organization stronger is a collaborative effort, and every voice matters. My email starting January 1 is president@chestnet.org, and if you need some writing inspiration, I’ve got some suggested prompts:
- Share with me a recent personal success or that of a colleague; we want to help spread the word.
- What do you find most rewarding in your practice?
- What’s a recurring challenge you face in practice?
- What is CHEST getting right? Where can we improve?
I look forward to hearing from you.
Warmest regards,
John A. Howington, MD, MBA, FCCP
RBC transfusion guidelines in critical care: Making the case for a restrictive approach
In the high-stakes environment of the intensive care unit (ICU), red blood cell (RBC) transfusions are a common intervention. With approximately 25% of critically ill patients in the US receiving RBC transfusions, optimizing the approach to transfusion is vital not only for patient safety but also for resource management. For the bedside clinician and health care systems, this presents both an opportunity and a challenge: to recalibrate transfusion practices while maintaining the highest standards of patient care.
Why a restrictive strategy?
Historically, transfusions were administered to optimize oxygen delivery to organs in the presence of anemia. However, studies have highlighted the risks associated with transfusions, such as transfusion-related lung injury, circulatory overload, and increased nosocomial infections. These risks are particularly pronounced in critically ill patients, who are often more vulnerable to complications from any additional physiological burden.
The restrictive approach—typically recommended at a hemoglobin threshold of 7 to 8 g/dL—has been shown to be the safer alternative for most ICU patients, as highlighted in recently published clinical guidelines. The data supporting this approach suggest that a restrictive transfusion strategy not only spares patients unnecessary transfusions but also aligns with cost-effective and resource-efficient health care practices.
Key recommendations
For ICU providers, this guideline presents specific recommendations based on a patient’s condition:
• General critical illness: The restrictive approach is preferred over a permissive one, with no adverse effect on ICU mortality, one-year survival, or adverse events. In other words, lower Hgb thresholds do not correlate with poorer outcomes in most critically ill patients.
• Acute gastrointestinal bleeding: Evidence favors a restrictive approach, associated with reduced rebleeding risk and short-term mortality. Studies show a significantly lower incidence of transfusion reactions and costs without compromising patient safety.
• Acute coronary syndrome (ACS): A more cautious approach is advised here. In cases of ACS, a restrictive RBC transfusion strategy could potentially increase the risk of cardiac death. It is recommended to avoid a restrictive approach, as it remains unclear whether there is a gradient effect—where risk progressively increases below a hemoglobin level of 10 g/dL—or a threshold effect at 10 g/dL. In other words, the data does not clarify if a hemoglobin level of 9 g/dL is as safe as 10 g/dL. An individualized transfusion approach, considering patient symptoms and other physiological markers, is recommended.
• Post-cardiac surgery: For postoperative patients, a restrictive strategy is suggested, as it conserves RBCs without impacting outcomes such as mortality or length of hospital stay.
• Isolated troponin elevation: In cases of elevated troponin without evidence of cardiac ischemia, transfusion decisions should consider additional patient-specific variables, with a restrictive approach as the baseline.
• Septic shock: RBC transfusions as part of a resuscitation bundle were not analyzed, as isolating the impact of RBC transfusions from other bundle elements was not feasible. However, with no clear benefit and similar adverse effects, neither strategy proved clinically superior. Nonetheless, a restrictive approach conserves RBC units, thereby saving resources and reducing costs.
The economics of restriction
Beyond clinical benefits, a restrictive approach conserves precious health care resources. With the cost of a single RBC unit hovering around $200—and significantly higher once administrative and logistic expenses are accounted for—reducing unnecessary transfusions translates into substantial savings. For a health care system already strained by limited blood supply and rising demand, a 40% reduction in transfusions across ICUs could alleviate supply pressures and contribute to more equitable resource distribution.
Easier said than done
Adopting a restrictive transfusion policy is not without challenges. Clinicians are trained to act decisively in critical situations, and, often, the instinct is to do more rather than less. However, studies indicate that with proper education, awareness, and decision-support systems, a restrictive policy is both feasible and effective. Institutions may consider behavior modification strategies, such as standardized transfusion order sets and decision-support tools within electronic medical records, to aid in adjusting transfusion practices.
Call to action
The message is clear: For most critically ill patients, a restrictive RBC transfusion strategy is not only safe but optimal. For ICU teams, this calls for a proactive shift in approach. It is a call to scrutinize transfusion triggers and lean toward a judicious, evidence-based approach.
While cases like ACS may require a different approach, the evidence strongly supports that, under most circumstances, less is more. Embracing this approach requires careful consideration, yet the potential benefits for patient safety and health care sustainability are compelling.
As critical care professionals, let us lead the way in refining transfusion practices to uphold patient safety, optimize resources, and adapt to evidence-based guidelines.
ACCESS THE FULL GUIDELINE
In the high-stakes environment of the intensive care unit (ICU), red blood cell (RBC) transfusions are a common intervention. With approximately 25% of critically ill patients in the US receiving RBC transfusions, optimizing the approach to transfusion is vital not only for patient safety but also for resource management. For the bedside clinician and health care systems, this presents both an opportunity and a challenge: to recalibrate transfusion practices while maintaining the highest standards of patient care.
Why a restrictive strategy?
Historically, transfusions were administered to optimize oxygen delivery to organs in the presence of anemia. However, studies have highlighted the risks associated with transfusions, such as transfusion-related lung injury, circulatory overload, and increased nosocomial infections. These risks are particularly pronounced in critically ill patients, who are often more vulnerable to complications from any additional physiological burden.
The restrictive approach—typically recommended at a hemoglobin threshold of 7 to 8 g/dL—has been shown to be the safer alternative for most ICU patients, as highlighted in recently published clinical guidelines. The data supporting this approach suggest that a restrictive transfusion strategy not only spares patients unnecessary transfusions but also aligns with cost-effective and resource-efficient health care practices.
Key recommendations
For ICU providers, this guideline presents specific recommendations based on a patient’s condition:
• General critical illness: The restrictive approach is preferred over a permissive one, with no adverse effect on ICU mortality, one-year survival, or adverse events. In other words, lower Hgb thresholds do not correlate with poorer outcomes in most critically ill patients.
• Acute gastrointestinal bleeding: Evidence favors a restrictive approach, associated with reduced rebleeding risk and short-term mortality. Studies show a significantly lower incidence of transfusion reactions and costs without compromising patient safety.
• Acute coronary syndrome (ACS): A more cautious approach is advised here. In cases of ACS, a restrictive RBC transfusion strategy could potentially increase the risk of cardiac death. It is recommended to avoid a restrictive approach, as it remains unclear whether there is a gradient effect—where risk progressively increases below a hemoglobin level of 10 g/dL—or a threshold effect at 10 g/dL. In other words, the data does not clarify if a hemoglobin level of 9 g/dL is as safe as 10 g/dL. An individualized transfusion approach, considering patient symptoms and other physiological markers, is recommended.
• Post-cardiac surgery: For postoperative patients, a restrictive strategy is suggested, as it conserves RBCs without impacting outcomes such as mortality or length of hospital stay.
• Isolated troponin elevation: In cases of elevated troponin without evidence of cardiac ischemia, transfusion decisions should consider additional patient-specific variables, with a restrictive approach as the baseline.
• Septic shock: RBC transfusions as part of a resuscitation bundle were not analyzed, as isolating the impact of RBC transfusions from other bundle elements was not feasible. However, with no clear benefit and similar adverse effects, neither strategy proved clinically superior. Nonetheless, a restrictive approach conserves RBC units, thereby saving resources and reducing costs.
The economics of restriction
Beyond clinical benefits, a restrictive approach conserves precious health care resources. With the cost of a single RBC unit hovering around $200—and significantly higher once administrative and logistic expenses are accounted for—reducing unnecessary transfusions translates into substantial savings. For a health care system already strained by limited blood supply and rising demand, a 40% reduction in transfusions across ICUs could alleviate supply pressures and contribute to more equitable resource distribution.
Easier said than done
Adopting a restrictive transfusion policy is not without challenges. Clinicians are trained to act decisively in critical situations, and, often, the instinct is to do more rather than less. However, studies indicate that with proper education, awareness, and decision-support systems, a restrictive policy is both feasible and effective. Institutions may consider behavior modification strategies, such as standardized transfusion order sets and decision-support tools within electronic medical records, to aid in adjusting transfusion practices.
Call to action
The message is clear: For most critically ill patients, a restrictive RBC transfusion strategy is not only safe but optimal. For ICU teams, this calls for a proactive shift in approach. It is a call to scrutinize transfusion triggers and lean toward a judicious, evidence-based approach.
While cases like ACS may require a different approach, the evidence strongly supports that, under most circumstances, less is more. Embracing this approach requires careful consideration, yet the potential benefits for patient safety and health care sustainability are compelling.
As critical care professionals, let us lead the way in refining transfusion practices to uphold patient safety, optimize resources, and adapt to evidence-based guidelines.
ACCESS THE FULL GUIDELINE
In the high-stakes environment of the intensive care unit (ICU), red blood cell (RBC) transfusions are a common intervention. With approximately 25% of critically ill patients in the US receiving RBC transfusions, optimizing the approach to transfusion is vital not only for patient safety but also for resource management. For the bedside clinician and health care systems, this presents both an opportunity and a challenge: to recalibrate transfusion practices while maintaining the highest standards of patient care.
Why a restrictive strategy?
Historically, transfusions were administered to optimize oxygen delivery to organs in the presence of anemia. However, studies have highlighted the risks associated with transfusions, such as transfusion-related lung injury, circulatory overload, and increased nosocomial infections. These risks are particularly pronounced in critically ill patients, who are often more vulnerable to complications from any additional physiological burden.
The restrictive approach—typically recommended at a hemoglobin threshold of 7 to 8 g/dL—has been shown to be the safer alternative for most ICU patients, as highlighted in recently published clinical guidelines. The data supporting this approach suggest that a restrictive transfusion strategy not only spares patients unnecessary transfusions but also aligns with cost-effective and resource-efficient health care practices.
Key recommendations
For ICU providers, this guideline presents specific recommendations based on a patient’s condition:
• General critical illness: The restrictive approach is preferred over a permissive one, with no adverse effect on ICU mortality, one-year survival, or adverse events. In other words, lower Hgb thresholds do not correlate with poorer outcomes in most critically ill patients.
• Acute gastrointestinal bleeding: Evidence favors a restrictive approach, associated with reduced rebleeding risk and short-term mortality. Studies show a significantly lower incidence of transfusion reactions and costs without compromising patient safety.
• Acute coronary syndrome (ACS): A more cautious approach is advised here. In cases of ACS, a restrictive RBC transfusion strategy could potentially increase the risk of cardiac death. It is recommended to avoid a restrictive approach, as it remains unclear whether there is a gradient effect—where risk progressively increases below a hemoglobin level of 10 g/dL—or a threshold effect at 10 g/dL. In other words, the data does not clarify if a hemoglobin level of 9 g/dL is as safe as 10 g/dL. An individualized transfusion approach, considering patient symptoms and other physiological markers, is recommended.
• Post-cardiac surgery: For postoperative patients, a restrictive strategy is suggested, as it conserves RBCs without impacting outcomes such as mortality or length of hospital stay.
• Isolated troponin elevation: In cases of elevated troponin without evidence of cardiac ischemia, transfusion decisions should consider additional patient-specific variables, with a restrictive approach as the baseline.
• Septic shock: RBC transfusions as part of a resuscitation bundle were not analyzed, as isolating the impact of RBC transfusions from other bundle elements was not feasible. However, with no clear benefit and similar adverse effects, neither strategy proved clinically superior. Nonetheless, a restrictive approach conserves RBC units, thereby saving resources and reducing costs.
The economics of restriction
Beyond clinical benefits, a restrictive approach conserves precious health care resources. With the cost of a single RBC unit hovering around $200—and significantly higher once administrative and logistic expenses are accounted for—reducing unnecessary transfusions translates into substantial savings. For a health care system already strained by limited blood supply and rising demand, a 40% reduction in transfusions across ICUs could alleviate supply pressures and contribute to more equitable resource distribution.
Easier said than done
Adopting a restrictive transfusion policy is not without challenges. Clinicians are trained to act decisively in critical situations, and, often, the instinct is to do more rather than less. However, studies indicate that with proper education, awareness, and decision-support systems, a restrictive policy is both feasible and effective. Institutions may consider behavior modification strategies, such as standardized transfusion order sets and decision-support tools within electronic medical records, to aid in adjusting transfusion practices.
Call to action
The message is clear: For most critically ill patients, a restrictive RBC transfusion strategy is not only safe but optimal. For ICU teams, this calls for a proactive shift in approach. It is a call to scrutinize transfusion triggers and lean toward a judicious, evidence-based approach.
While cases like ACS may require a different approach, the evidence strongly supports that, under most circumstances, less is more. Embracing this approach requires careful consideration, yet the potential benefits for patient safety and health care sustainability are compelling.
As critical care professionals, let us lead the way in refining transfusion practices to uphold patient safety, optimize resources, and adapt to evidence-based guidelines.
ACCESS THE FULL GUIDELINE
Revival of the aspiration vs chest tube debate for PSP
Thoracic Oncology and Chest Procedures Network
Pleural Disease Section
Considerable heterogeneity exists in the management of primary spontaneous pneumothorax (PSP). American and European guidelines have been grappling with this question for decades: What is the best way to manage PSP? A 2023 randomized, controlled trial (Marx et al. AJRCCM) sought to answer this.
The study recruited 379 adults aged 18 to 55 years between 2009 and 2015, with complete and first PSP in 31 French hospitals. One hundred eighty-nine patients initially received simple aspiration and 190 received chest tube drainage. The aspiration device was removed if a chest radiograph (CXR) following 30 minutes of aspiration showed lung apposition, with suction repeated up to one time with incomplete re-expansion. The chest tubes were large-bore (16-F or 20-F) and removed 72 hours postprocedure if the CXR showed complete lung re-expansion.
Simple aspiration was statistically inferior to chest tube drainage (29% vs 18%). However, first-line simple aspiration resulted in shorter length of stay, less subcutaneous emphysema, site infection, pain, and one-year recurrence.
Since most first-time PSP occurs in younger, healthier adults, simple aspiration could still be considered as it is better tolerated than large-bore chest tubes. However, with more frequent use of small-bore (≤14-F) catheters, ambulatory drainage could also be a suitable option in carefully selected patients. Additionally, inpatient chest tubes do not need to remain in place for 72 hours, as was this study’s protocol. Society guidelines will need to weigh in on the latest high-quality evidence available for final recommendations.
Thoracic Oncology and Chest Procedures Network
Pleural Disease Section
Considerable heterogeneity exists in the management of primary spontaneous pneumothorax (PSP). American and European guidelines have been grappling with this question for decades: What is the best way to manage PSP? A 2023 randomized, controlled trial (Marx et al. AJRCCM) sought to answer this.
The study recruited 379 adults aged 18 to 55 years between 2009 and 2015, with complete and first PSP in 31 French hospitals. One hundred eighty-nine patients initially received simple aspiration and 190 received chest tube drainage. The aspiration device was removed if a chest radiograph (CXR) following 30 minutes of aspiration showed lung apposition, with suction repeated up to one time with incomplete re-expansion. The chest tubes were large-bore (16-F or 20-F) and removed 72 hours postprocedure if the CXR showed complete lung re-expansion.
Simple aspiration was statistically inferior to chest tube drainage (29% vs 18%). However, first-line simple aspiration resulted in shorter length of stay, less subcutaneous emphysema, site infection, pain, and one-year recurrence.
Since most first-time PSP occurs in younger, healthier adults, simple aspiration could still be considered as it is better tolerated than large-bore chest tubes. However, with more frequent use of small-bore (≤14-F) catheters, ambulatory drainage could also be a suitable option in carefully selected patients. Additionally, inpatient chest tubes do not need to remain in place for 72 hours, as was this study’s protocol. Society guidelines will need to weigh in on the latest high-quality evidence available for final recommendations.
Thoracic Oncology and Chest Procedures Network
Pleural Disease Section
Considerable heterogeneity exists in the management of primary spontaneous pneumothorax (PSP). American and European guidelines have been grappling with this question for decades: What is the best way to manage PSP? A 2023 randomized, controlled trial (Marx et al. AJRCCM) sought to answer this.
The study recruited 379 adults aged 18 to 55 years between 2009 and 2015, with complete and first PSP in 31 French hospitals. One hundred eighty-nine patients initially received simple aspiration and 190 received chest tube drainage. The aspiration device was removed if a chest radiograph (CXR) following 30 minutes of aspiration showed lung apposition, with suction repeated up to one time with incomplete re-expansion. The chest tubes were large-bore (16-F or 20-F) and removed 72 hours postprocedure if the CXR showed complete lung re-expansion.
Simple aspiration was statistically inferior to chest tube drainage (29% vs 18%). However, first-line simple aspiration resulted in shorter length of stay, less subcutaneous emphysema, site infection, pain, and one-year recurrence.
Since most first-time PSP occurs in younger, healthier adults, simple aspiration could still be considered as it is better tolerated than large-bore chest tubes. However, with more frequent use of small-bore (≤14-F) catheters, ambulatory drainage could also be a suitable option in carefully selected patients. Additionally, inpatient chest tubes do not need to remain in place for 72 hours, as was this study’s protocol. Society guidelines will need to weigh in on the latest high-quality evidence available for final recommendations.
AI applications in pediatric pulmonary, sleep, and critical care medicine
Airways Disorders Network
Pediatric Chest Medicine Section
Artificial intelligence (AI) refers to the science and engineering of making intelligent machines that mimic human cognitive functions, such as learning and problem solving.1 Asthma exacerbations in young children were detected reliably by AI-aided stethoscope alone.2 Inhaler use has been successfully tracked using active and passive patient input to cloud-based dashboards.3 Asthma specialists can potentially use this knowledge to intervene in real time or more frequent intervals than the current episodic care.
Sleep trackers using commercial-grade sensors can provide useful information about sleep hygiene, sleep duration, and nocturnal awakenings. An increasing number of “wearables” and “nearables” that utilize AI algorithms to evaluate sleep duration and quality are FDA approved. AI-based scoring of polysomnography data can improve the efficiency of a sleep laboratory. Big data analysis of CPAP compliance in children led to identification of actionable items that can be targeted to improve patient outcomes.4
The use of AI models in clinical decision support can result in fewer false alerts and missed patients due to increased model accuracy. Additionally, large language model tools can automatically generate comprehensive progress notes incorporating relevant electronic medical records data, thereby reducing physician charting time.
These case uses highlight the potential to improve workflow efficiency and clinical outcomes in pediatric pulmonary and critical care by incorporating AI tools in medical decision-making and management.
References
1. McCarthy JF, Marx KA, Hoffman PE, et al. Applications of machine learning and high-dimensional visualization in cancer detection, diagnosis, and management. Ann N Y Acad Sci. 2004;1020:239-262.
2. Emeryk A, Derom E, Janeczek K, et al. Home monitoring of asthma exacerbations in children and adults with use of an AI-aided stethoscope. Ann Fam Med. 2023;21(6):517-525.
3. Jaimini U, Thirunarayan K, Kalra M, Venkataraman R, Kadariya D, Sheth A. How is my child’s asthma?” Digital phenotype and actionable insights for pediatric asthma. JMIR Pediatr Parent. 2018;1(2):e11988.
4. Bhattacharjee R, Benjafield AV, Armitstead J, et al. Adherence in children using positive airway pressure therapy: a big-data analysis [published correction appears in Lancet Digit Health. 2020 Sep;2(9):e455.]. Lancet Digit Health. 2020;2(2):e94-e101.
Airways Disorders Network
Pediatric Chest Medicine Section
Artificial intelligence (AI) refers to the science and engineering of making intelligent machines that mimic human cognitive functions, such as learning and problem solving.1 Asthma exacerbations in young children were detected reliably by AI-aided stethoscope alone.2 Inhaler use has been successfully tracked using active and passive patient input to cloud-based dashboards.3 Asthma specialists can potentially use this knowledge to intervene in real time or more frequent intervals than the current episodic care.
Sleep trackers using commercial-grade sensors can provide useful information about sleep hygiene, sleep duration, and nocturnal awakenings. An increasing number of “wearables” and “nearables” that utilize AI algorithms to evaluate sleep duration and quality are FDA approved. AI-based scoring of polysomnography data can improve the efficiency of a sleep laboratory. Big data analysis of CPAP compliance in children led to identification of actionable items that can be targeted to improve patient outcomes.4
The use of AI models in clinical decision support can result in fewer false alerts and missed patients due to increased model accuracy. Additionally, large language model tools can automatically generate comprehensive progress notes incorporating relevant electronic medical records data, thereby reducing physician charting time.
These case uses highlight the potential to improve workflow efficiency and clinical outcomes in pediatric pulmonary and critical care by incorporating AI tools in medical decision-making and management.
References
1. McCarthy JF, Marx KA, Hoffman PE, et al. Applications of machine learning and high-dimensional visualization in cancer detection, diagnosis, and management. Ann N Y Acad Sci. 2004;1020:239-262.
2. Emeryk A, Derom E, Janeczek K, et al. Home monitoring of asthma exacerbations in children and adults with use of an AI-aided stethoscope. Ann Fam Med. 2023;21(6):517-525.
3. Jaimini U, Thirunarayan K, Kalra M, Venkataraman R, Kadariya D, Sheth A. How is my child’s asthma?” Digital phenotype and actionable insights for pediatric asthma. JMIR Pediatr Parent. 2018;1(2):e11988.
4. Bhattacharjee R, Benjafield AV, Armitstead J, et al. Adherence in children using positive airway pressure therapy: a big-data analysis [published correction appears in Lancet Digit Health. 2020 Sep;2(9):e455.]. Lancet Digit Health. 2020;2(2):e94-e101.
Airways Disorders Network
Pediatric Chest Medicine Section
Artificial intelligence (AI) refers to the science and engineering of making intelligent machines that mimic human cognitive functions, such as learning and problem solving.1 Asthma exacerbations in young children were detected reliably by AI-aided stethoscope alone.2 Inhaler use has been successfully tracked using active and passive patient input to cloud-based dashboards.3 Asthma specialists can potentially use this knowledge to intervene in real time or more frequent intervals than the current episodic care.
Sleep trackers using commercial-grade sensors can provide useful information about sleep hygiene, sleep duration, and nocturnal awakenings. An increasing number of “wearables” and “nearables” that utilize AI algorithms to evaluate sleep duration and quality are FDA approved. AI-based scoring of polysomnography data can improve the efficiency of a sleep laboratory. Big data analysis of CPAP compliance in children led to identification of actionable items that can be targeted to improve patient outcomes.4
The use of AI models in clinical decision support can result in fewer false alerts and missed patients due to increased model accuracy. Additionally, large language model tools can automatically generate comprehensive progress notes incorporating relevant electronic medical records data, thereby reducing physician charting time.
These case uses highlight the potential to improve workflow efficiency and clinical outcomes in pediatric pulmonary and critical care by incorporating AI tools in medical decision-making and management.
References
1. McCarthy JF, Marx KA, Hoffman PE, et al. Applications of machine learning and high-dimensional visualization in cancer detection, diagnosis, and management. Ann N Y Acad Sci. 2004;1020:239-262.
2. Emeryk A, Derom E, Janeczek K, et al. Home monitoring of asthma exacerbations in children and adults with use of an AI-aided stethoscope. Ann Fam Med. 2023;21(6):517-525.
3. Jaimini U, Thirunarayan K, Kalra M, Venkataraman R, Kadariya D, Sheth A. How is my child’s asthma?” Digital phenotype and actionable insights for pediatric asthma. JMIR Pediatr Parent. 2018;1(2):e11988.
4. Bhattacharjee R, Benjafield AV, Armitstead J, et al. Adherence in children using positive airway pressure therapy: a big-data analysis [published correction appears in Lancet Digit Health. 2020 Sep;2(9):e455.]. Lancet Digit Health. 2020;2(2):e94-e101.
Mechanical power: A missing piece in lung-protective ventilation?
Critical Care Network
Mechanical Ventilation and Airways Management Section
The ARDSNet trial demonstrated the importance of low tidal volume ventilation in patients with ARDS, and we have learned to monitor parameters such as plateau pressure and driving pressure (DP) to ensure lung-protective ventilation. What role does the higher respiratory rate play? There is growing evidence that respiratory rate may play an important part in the pathogenesis of ventilator-induced lung injury (VILI) and the dynamic effect of both rate and static pressures needs to be evaluated.
The concept of mechanical power (MP) was formalized in 2016 by Gattinoni, et al and defined as the product of respiratory rate and total inflation energy gained per breath.1 Calculations have been developed for both volume-controlled and pressure-controlled ventilation, including elements such as respiratory rate and PEEP. Studies have shown that increased MP is associated with ICU and hospital mortality, even at low tidal volumes.2 The use of MP remains limited in clinical practice due to its dynamic nature and difficulty of calculating in routine clinical practice but may be a feasible addition to the continuous monitoring outputs on a ventilator. Additional prospective studies are also needed to define the optimal threshold of MP and to compare monitoring strategies using MP vs DP.
References
1. Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567-1575.
2. Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914-1922.
Critical Care Network
Mechanical Ventilation and Airways Management Section
The ARDSNet trial demonstrated the importance of low tidal volume ventilation in patients with ARDS, and we have learned to monitor parameters such as plateau pressure and driving pressure (DP) to ensure lung-protective ventilation. What role does the higher respiratory rate play? There is growing evidence that respiratory rate may play an important part in the pathogenesis of ventilator-induced lung injury (VILI) and the dynamic effect of both rate and static pressures needs to be evaluated.
The concept of mechanical power (MP) was formalized in 2016 by Gattinoni, et al and defined as the product of respiratory rate and total inflation energy gained per breath.1 Calculations have been developed for both volume-controlled and pressure-controlled ventilation, including elements such as respiratory rate and PEEP. Studies have shown that increased MP is associated with ICU and hospital mortality, even at low tidal volumes.2 The use of MP remains limited in clinical practice due to its dynamic nature and difficulty of calculating in routine clinical practice but may be a feasible addition to the continuous monitoring outputs on a ventilator. Additional prospective studies are also needed to define the optimal threshold of MP and to compare monitoring strategies using MP vs DP.
References
1. Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567-1575.
2. Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914-1922.
Critical Care Network
Mechanical Ventilation and Airways Management Section
The ARDSNet trial demonstrated the importance of low tidal volume ventilation in patients with ARDS, and we have learned to monitor parameters such as plateau pressure and driving pressure (DP) to ensure lung-protective ventilation. What role does the higher respiratory rate play? There is growing evidence that respiratory rate may play an important part in the pathogenesis of ventilator-induced lung injury (VILI) and the dynamic effect of both rate and static pressures needs to be evaluated.
The concept of mechanical power (MP) was formalized in 2016 by Gattinoni, et al and defined as the product of respiratory rate and total inflation energy gained per breath.1 Calculations have been developed for both volume-controlled and pressure-controlled ventilation, including elements such as respiratory rate and PEEP. Studies have shown that increased MP is associated with ICU and hospital mortality, even at low tidal volumes.2 The use of MP remains limited in clinical practice due to its dynamic nature and difficulty of calculating in routine clinical practice but may be a feasible addition to the continuous monitoring outputs on a ventilator. Additional prospective studies are also needed to define the optimal threshold of MP and to compare monitoring strategies using MP vs DP.
References
1. Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567-1575.
2. Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914-1922.
















