User login
Dextromethorphan/quinidine for pseudobulbar affect
In October 2010, the FDA approved a combination of dextromethorphan (DM) and quinidine for the treatment of pseudobulbar affect (PBA)—also called pathological laughing and crying, affective lability, emotional dyscontrol, emotional incontinence, and involuntary emotional expression disorder—in patients with neurologic disorders and brain injuries (Table). Despite receiving an approvable letter in 2006, the compound was not approved at that time because of concerns about the arrhythmogenic potential of quinidine, which prolongs the QT interval. The manufacturer conducted another study using one-third of the previous quinidine dose, which ameliorated this concern and led to approval.
Clinical implications
PBA is manifested by involuntary labile, shallow affect with sudden and unpredictable laughing, crying, or other emotional displays that are not appropriate to the social setting and may not be congruent with the patient’s prevailing mood.1 Episodes are often paroxysmal and cannot be interrupted voluntarily.2 PBA seems to be caused by a loss of descending cortical control of brainstem motor nuclei and possibly the cerebellum, disrupting inhibitory mechanisms and resulting in inappropriate and involuntary emotional display.3 Several studies have demonstrated involvement of subcortical areas, particularly the anterior limb of the internal capsule and the bulbar area. The patho-physiology of PBA may involve excessive release of glutamate by injured neurons, disrupting systems for motor control of emotional expression.4,5
Table
Dextromethorphan/quinidine: Fast facts
| Brand name: Nuedexta |
| Indication: Pseudobulbar affect |
| Approval date: October 29, 2010 |
| Availability date: First quarter of 2011 |
| Manufacturer: Avanir |
| Dosage forms: Dextromethorphan, 20 mg, plus quinidine, 10 mg |
| Starting dose: 1 capsule per day |
| Target dose: 2 capsules per day |
PBA is most common in diseases that interfere bilaterally with the corticohypothalamic and corticobulbar tracts that control voluntary and involuntary faciorespiratory mechanisms. However, PBA occurs in unilateral disease as well. The reported prevalence of PBA is:
- 49% in amyotrophic lateral sclerosis (ALS)
- 18% to 39% in Alzheimer’s disease
- 11% to 34% in stroke
- 10% to 11% in multiple sclerosis (MS) and traumatic brain injury.6,7
PBA also has been reported in patients with Parkinson’s disease, brain tumors, Wilson’s disease, syphilitic pseudobulbar palsy, and various encephalitides.1 An estimated 880,000 U.S. patients exhibit PBA.8
Previously, there was no FDA-approved treatment for PBA. However, small controlled trials suggest that selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs)— usually in doses lower than those used to treat depression—may effectively reduce symptoms within 2 to 3 days.1 Although dopaminergic agents such as levodopa and amantadine have shown benefit in open trials, results of controlled studies using objective measurements have not been positive.
How it works
DM is a serotonergic substance that also is an agonist of 1-sigma receptors and a low-affinity, uncompetitive antagonist of N-methyl-d-aspartate (NMDA) receptors, which are important in glutamate signaling, through binding at the phencyclidine site on the NMDA complex.7,9 The 1-sigma receptor was thought to be an opioid receptor subtype, but unlike opioid receptors it is not blocked by narcotic antagonists and does not have an endogenous ligand. However, the 1-sigma receptor does modulate activity of opioid mu receptors in addition to altering dopamine release and possibly reducing glutamate release.9 Sigma receptors are densely distributed in the limbic system and in systems related to motor control of affective expression and seem to be involved in learning, responses to stress, mood regulation, and drug dependence.1 Because DM preferentially binds to brain regions that regulate emotional expression,10 it could normalize glutaminergic neurotransmission and other relevant systems in these regions.1 However, DM’s exact mechanism of action is unknown.
Quinidine is a sodium channel antagonist usually used as a type Ia antiarrhythmic.5 DM is subject to extensive first-pass metabolism by cytochrome P (CYP) 450 2D6 to dextrorphan, which after being glucuronidated cannot cross the blood-brain barrier. In doses 10 to 25 times lower than those used to treat cardiac arrhythmias, quinidine inhibits 2D6 and increases DM bioavailability.10 DM blood levels increase linearly with dose following coadministration with quinidine but are undetectable in most patients given DM alone.7,9
Efficacy and tolerability
A combination of DM and quinidine (DMQ) reduced Center for Neurologic Study-Lability Scale (CNC-LS) scores and the number of daily PBA episodes in 3 randomized trials.5,7,10 Visit this article at CurrentPsychiatry.com for a table summarizing these studies.
An 85-day randomized, double-blind, placebo-controlled study of 150 patients with PBA associated with MS found that DM, 30 mg, plus quinidine, 30 mg, (DMQ 30-30) was twice as effective as placebo within a week in reducing CNC-LS scores.10 DMQ 30-30 patients also had approximately half as many episodes of inappropriate laughing, crying, or combined laughing and crying and a 2-fold greater decrease in pain intensity.10 Twenty-one percent of DMQ 30-30 patients experienced complete remission—no PBA episodes—compared with 7% of placebo patients. There were no significant differences in QT prolongation between DMQ 30-30 and placebo.
A 3-arm, double-blind, 28-day, phase III multicenter trial of 140 ALS patients with PBA compared DM monotherapy, quinidine monotherapy, and DMQ 30-30.5 Compared with either drug alone, DMQ 30-30 showed greater reduction of CNC-LS scores, as well as improved quality of life and quality of relationships scores, with equal benefit in poor and extensive DM metabolizers. However, the control conditions may not have been adequate. Quinidine alone would not be expected to have an effect on PBA, and the DM dose, which was the same in combination and monotherapy, may have been too low to be effective by itself. In support of this hypothesis, the DM plasma level was 18 times higher in patients taking DMQ 30-30 than those taking DM monotherapy.
In a manufacturer-sponsored, multicenter, 12-week randomized trial, 326 patients with ALS or MS and clinically significant PBA were randomly assigned to DM, 30 mg, plus quinidine, 10 mg (DMQ 30-10), DM, 20 mg, plus quinidine, 10 mg (DMQ 20-10), or placebo, each administered twice daily.7 Patients with comorbid psychiatric disorders or significant depressive symptoms were excluded. Although daily PBA episodes decreased in all groups, the daily rate of PBA episodes was 47% lower for patients taking DMQ 30-10, and 49% lower with DMQ 20-10 compared with placebo (both P < .001). The mean decrease in the number of daily PBA episodes was 3.9 to 4.1 with active treatment and 3.0 with placebo. Side effects were more common with active drug than placebo and included dizziness, nausea, diarrhea, and urinary tract infection. There were no serious adverse cardiac events and no active drug recipients showed a QTc interval >480 msec or a change from baseline >60 msec.11 Discontinuation rates in this study were lower than in studies of DMQ 30-30. In an open-label extension of 253 patients who completed the double-blind phase and were assigned to DMQ 30-10 for 12 weeks, the incidence of treatment-related adverse events was 28%, with a 5.5% rate of serious adverse events.12
Safety
Because the 10 mg dose of quinidine in the approved formulation of DMQ is 10 times lower than the antiarrhythmic dose, substantial ECG changes and adverse cardiac effects with DMQ have not been reported. The most common side effects of DM are nausea, somnolence, dizziness, and headache. Thrombocytopenia, QT prolongation, hepatotoxicity, allergic reactions, and anticholinergic side effects can occur.
In high doses and combined with other substances, DM has been used as a recreational drug. When taken in high doses, adverse effects include nausea, vomiting, malaise, dilated pupils, difficulty urinating, increased urination frequency, fever, tachycardia, loss of appetite, shakiness, seizures, and potentially coma and death. DMQ may have a greater potential for serious adverse effects than DM alone because quinidine increases DM bioavailability and blood levels. The abuse potential of DMQ is not clear.
Psychosis has been reported with higher DM doses. The psychotomimetic effects of phencyclidine (PCP) are related to binding to the PCP site on the NMDA receptor complex—to which DM also binds—with reduced glutamate signaling in information processing systems. Therefore, caution is indicated when prescribing DM to patients with psychosis.
Because DM, a CYP2D6 substrate, is combined with quinidine, a 2D6 inhibitor, administering DMQ with other 2D6 inhibitors could lead to toxicity. When DMQ is combined with SSRIs and similar agents, the serotonergic properties of DM could result in serotonin syndrome, which could be fatal if DM is combined with monoamine oxidase inhibitors.10 Combinations of DM and acetaminophen and antihistamines can be dangerous at higher doses.10 Because quinidine is metabolized by CYP3A, inhibitors of this enzyme such as ketoconazole, nefazodone, and grapefruit juice should be avoided. Similarly, inhibition of CYP2D6 by quinidine could raise levels of coadministered 2D6 substrates.
Contraindications. DMQ is contraindicated in patients with:
- heart failure
- prolonged QT interval
- congenital long QT interval
- history of torsades de pointes
- complete atrioventricular (AV) block without implanted pacemakers.13
DMQ also is contraindicated in patients at high risk for complete AV block.13
Dosing
DMQ is available as a capsule containing DM, 20 mg, and quinidine, 10 mg. The recommended starting dose is 1 capsule by mouth for 7 days, then 1 capsule every 12 hours.
Although DMQ is convenient, its advantage over starting with DM alone and adding a small dose of a non-serotonergic 2D6 inhibitor if DM is not effective remains to be demonstrated. In view of the unknown potential for abuse and toxicity as well as the cost of the proprietary drug ($3,000 to $5,000 a year), it would seem prudent to consider using an SSRI or a TCA first.8 These medications also act on 1-sigma receptors,14,15 which may account in part for their reported benefit.
Related Resource
- Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
Drug Brand Names
- Amantadine • Symmetrel
- Dextromethorphan/quinidine •Nefazodone
- Ketoconazole • Nizoral
- Levodopa • Sinemet
- Neudexta • Serzone
- Quinidine • Quinidex
Disclosures
Dr. Dubovsky receives research support from Biogen Idec, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Otsuka, the Peter and Elizabeth C. Tower Foundation, and Pfizer, Inc.
Dr. Tan reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 2
Dextromethorphan/quinidine for PBA: Evidence shows efficacy
| Study | Patients | Dosages | Results |
|---|---|---|---|
| Panitch et al, 200610; 85-day, randomized, double-blind, placebo-controlled | 150 MS patients with PBA | DMQ 30-30 or placebo, given twice a day | DMQ 30-30 was associated with greater reductions in CNC-LS scores, fewer PBA episodes, improvement in QOL and QOR, and decrease in pain intensity |
| Pope, 20065; 3-arm, double-blind, 28-day phase III multicenter trial | 140 ALS patients with PBA | DMQ 30-30, DM, 30 mg, or quinidine, 30 mg, given twice daily | DMQ 30-30 was associated with greater decreases in CNC-LS scores and number of laughing and crying episodes and improvements in QOL and QOR compared with DM or quinidine alone |
| Pioro et al, 20107; 12-week, randomized, double-blind, placebo-controlled trial | 326 ALS and MS patients with clinically significant PBA | DMQ 30-10, DMQ 20-10, or placebo, given twice daily | CNC-LS scores decreased in all groups but the daily rate of PBA episodes was 47% lower for DMQ 30-10 and 49% lower for DMQ 20-10 compared with placebo |
| ALS: amyotrophic lateral sclerosis; CNC-LS: Center for Neurologic Study-Lability Scale; DM: dextromethorphan; DMQ 20-10: dextromethorphan, 20 mg, plus quinidine, 10 mg; DMQ 30-10: dextromethorphan, 30 mg, plus quinidine, 10 mg; DMQ 30-30: dextromethorphan, 30 mg, plus quinidine, 30 mg; MS: multiple sclerosis; PBA: pseudobulbar affect; QOL: quality of life; QOR: quality of relationships | |||
1. Schiffer R, Pope LE. Review of pseudobulbar affect including a novel and potential therapy. J Neuropsychiatry Clin Neurosci. 2005;17:447-454.
2. Rosen HJ, Cummings J. A real reason for patients with pseudobulbar affect to smile. Ann Neurol. 2007;61:92-96.
3. Miller A. Pseudobulbar affect in multiple sclerosis: toward the development of innovative therapeutic strategies. J Neurol Sci. 2006;245:153-159.
4. Mattson MP. Excitotoxic and excitoprotective mechanisms: abundant targets for the prevention and treatment of neurodegenerative disorders. Neuromolecular Med. 2003;3:65-94.
5. Pope LE. AVP-923 as a novel treatment for pseudobulbar affect in ALS. Progress in Neurotherapeutics and Neuropsychopharmacology. 2006;1:91-104.
6. Arciniegas DB. A clinical overview of pseudobulbar affect. Am J Geriatr Pharmacother. 2005;3(suppl A):4-8.
7. Pioro EP, Brooks BR, Cummings J, et al. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68:693-702.
8. Johnston SC, Hauser SL. Marketing and drug costs: who is laughing and crying? Ann Neurol. 2007;61:11A-12A.
9. Brooks BR, Thisted RA, Appel SH, et al and. the AVP-923 ALS Study Group. Treatment of pseudobulbar affect with dextromethorphan/quinidine: a randomized trial. Neurology. 2004;63:1364-1370.
10. Panitch HS, Thisted RA, Smith RA, et al. and the Psuedobulbar Affect in Multiple Sclerosis Study Group. Randomized, controlled trial of dextromethorphan/ quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol. 2006;59:780-787.
11. Kaye R, Pratt C. Summary of cardiac safety from a randomized, placebo-controlled, trial of dextromethorphan/ quinidine (STAR) for treatment of pseudobulbar affect. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
12. Pioro EP, Brooks BR, Cummings J, et al. Safety and tolerability of dextromethorphan/quinidine for pseudobulbar affect in a 12-week, open-label extension study. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
13. Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
14. Narita N, Hashimoto K, Tomitaka S, et al. Interactions of selective serotonin reuptake inhibitors with subtypes of sigma receptors in rat brain. Eur J Pharmacol. 1996;307(1):117-119.
15. Dhir A, Kulkarni SK. Involvement of sigma-1 receptor modulation in the antidepressant action of venlafaxine. Neurosci Lett. 2007;420(3):204-208.
In October 2010, the FDA approved a combination of dextromethorphan (DM) and quinidine for the treatment of pseudobulbar affect (PBA)—also called pathological laughing and crying, affective lability, emotional dyscontrol, emotional incontinence, and involuntary emotional expression disorder—in patients with neurologic disorders and brain injuries (Table). Despite receiving an approvable letter in 2006, the compound was not approved at that time because of concerns about the arrhythmogenic potential of quinidine, which prolongs the QT interval. The manufacturer conducted another study using one-third of the previous quinidine dose, which ameliorated this concern and led to approval.
Clinical implications
PBA is manifested by involuntary labile, shallow affect with sudden and unpredictable laughing, crying, or other emotional displays that are not appropriate to the social setting and may not be congruent with the patient’s prevailing mood.1 Episodes are often paroxysmal and cannot be interrupted voluntarily.2 PBA seems to be caused by a loss of descending cortical control of brainstem motor nuclei and possibly the cerebellum, disrupting inhibitory mechanisms and resulting in inappropriate and involuntary emotional display.3 Several studies have demonstrated involvement of subcortical areas, particularly the anterior limb of the internal capsule and the bulbar area. The patho-physiology of PBA may involve excessive release of glutamate by injured neurons, disrupting systems for motor control of emotional expression.4,5
Table
Dextromethorphan/quinidine: Fast facts
| Brand name: Nuedexta |
| Indication: Pseudobulbar affect |
| Approval date: October 29, 2010 |
| Availability date: First quarter of 2011 |
| Manufacturer: Avanir |
| Dosage forms: Dextromethorphan, 20 mg, plus quinidine, 10 mg |
| Starting dose: 1 capsule per day |
| Target dose: 2 capsules per day |
PBA is most common in diseases that interfere bilaterally with the corticohypothalamic and corticobulbar tracts that control voluntary and involuntary faciorespiratory mechanisms. However, PBA occurs in unilateral disease as well. The reported prevalence of PBA is:
- 49% in amyotrophic lateral sclerosis (ALS)
- 18% to 39% in Alzheimer’s disease
- 11% to 34% in stroke
- 10% to 11% in multiple sclerosis (MS) and traumatic brain injury.6,7
PBA also has been reported in patients with Parkinson’s disease, brain tumors, Wilson’s disease, syphilitic pseudobulbar palsy, and various encephalitides.1 An estimated 880,000 U.S. patients exhibit PBA.8
Previously, there was no FDA-approved treatment for PBA. However, small controlled trials suggest that selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs)— usually in doses lower than those used to treat depression—may effectively reduce symptoms within 2 to 3 days.1 Although dopaminergic agents such as levodopa and amantadine have shown benefit in open trials, results of controlled studies using objective measurements have not been positive.
How it works
DM is a serotonergic substance that also is an agonist of 1-sigma receptors and a low-affinity, uncompetitive antagonist of N-methyl-d-aspartate (NMDA) receptors, which are important in glutamate signaling, through binding at the phencyclidine site on the NMDA complex.7,9 The 1-sigma receptor was thought to be an opioid receptor subtype, but unlike opioid receptors it is not blocked by narcotic antagonists and does not have an endogenous ligand. However, the 1-sigma receptor does modulate activity of opioid mu receptors in addition to altering dopamine release and possibly reducing glutamate release.9 Sigma receptors are densely distributed in the limbic system and in systems related to motor control of affective expression and seem to be involved in learning, responses to stress, mood regulation, and drug dependence.1 Because DM preferentially binds to brain regions that regulate emotional expression,10 it could normalize glutaminergic neurotransmission and other relevant systems in these regions.1 However, DM’s exact mechanism of action is unknown.
Quinidine is a sodium channel antagonist usually used as a type Ia antiarrhythmic.5 DM is subject to extensive first-pass metabolism by cytochrome P (CYP) 450 2D6 to dextrorphan, which after being glucuronidated cannot cross the blood-brain barrier. In doses 10 to 25 times lower than those used to treat cardiac arrhythmias, quinidine inhibits 2D6 and increases DM bioavailability.10 DM blood levels increase linearly with dose following coadministration with quinidine but are undetectable in most patients given DM alone.7,9
Efficacy and tolerability
A combination of DM and quinidine (DMQ) reduced Center for Neurologic Study-Lability Scale (CNC-LS) scores and the number of daily PBA episodes in 3 randomized trials.5,7,10 Visit this article at CurrentPsychiatry.com for a table summarizing these studies.
An 85-day randomized, double-blind, placebo-controlled study of 150 patients with PBA associated with MS found that DM, 30 mg, plus quinidine, 30 mg, (DMQ 30-30) was twice as effective as placebo within a week in reducing CNC-LS scores.10 DMQ 30-30 patients also had approximately half as many episodes of inappropriate laughing, crying, or combined laughing and crying and a 2-fold greater decrease in pain intensity.10 Twenty-one percent of DMQ 30-30 patients experienced complete remission—no PBA episodes—compared with 7% of placebo patients. There were no significant differences in QT prolongation between DMQ 30-30 and placebo.
A 3-arm, double-blind, 28-day, phase III multicenter trial of 140 ALS patients with PBA compared DM monotherapy, quinidine monotherapy, and DMQ 30-30.5 Compared with either drug alone, DMQ 30-30 showed greater reduction of CNC-LS scores, as well as improved quality of life and quality of relationships scores, with equal benefit in poor and extensive DM metabolizers. However, the control conditions may not have been adequate. Quinidine alone would not be expected to have an effect on PBA, and the DM dose, which was the same in combination and monotherapy, may have been too low to be effective by itself. In support of this hypothesis, the DM plasma level was 18 times higher in patients taking DMQ 30-30 than those taking DM monotherapy.
In a manufacturer-sponsored, multicenter, 12-week randomized trial, 326 patients with ALS or MS and clinically significant PBA were randomly assigned to DM, 30 mg, plus quinidine, 10 mg (DMQ 30-10), DM, 20 mg, plus quinidine, 10 mg (DMQ 20-10), or placebo, each administered twice daily.7 Patients with comorbid psychiatric disorders or significant depressive symptoms were excluded. Although daily PBA episodes decreased in all groups, the daily rate of PBA episodes was 47% lower for patients taking DMQ 30-10, and 49% lower with DMQ 20-10 compared with placebo (both P < .001). The mean decrease in the number of daily PBA episodes was 3.9 to 4.1 with active treatment and 3.0 with placebo. Side effects were more common with active drug than placebo and included dizziness, nausea, diarrhea, and urinary tract infection. There were no serious adverse cardiac events and no active drug recipients showed a QTc interval >480 msec or a change from baseline >60 msec.11 Discontinuation rates in this study were lower than in studies of DMQ 30-30. In an open-label extension of 253 patients who completed the double-blind phase and were assigned to DMQ 30-10 for 12 weeks, the incidence of treatment-related adverse events was 28%, with a 5.5% rate of serious adverse events.12
Safety
Because the 10 mg dose of quinidine in the approved formulation of DMQ is 10 times lower than the antiarrhythmic dose, substantial ECG changes and adverse cardiac effects with DMQ have not been reported. The most common side effects of DM are nausea, somnolence, dizziness, and headache. Thrombocytopenia, QT prolongation, hepatotoxicity, allergic reactions, and anticholinergic side effects can occur.
In high doses and combined with other substances, DM has been used as a recreational drug. When taken in high doses, adverse effects include nausea, vomiting, malaise, dilated pupils, difficulty urinating, increased urination frequency, fever, tachycardia, loss of appetite, shakiness, seizures, and potentially coma and death. DMQ may have a greater potential for serious adverse effects than DM alone because quinidine increases DM bioavailability and blood levels. The abuse potential of DMQ is not clear.
Psychosis has been reported with higher DM doses. The psychotomimetic effects of phencyclidine (PCP) are related to binding to the PCP site on the NMDA receptor complex—to which DM also binds—with reduced glutamate signaling in information processing systems. Therefore, caution is indicated when prescribing DM to patients with psychosis.
Because DM, a CYP2D6 substrate, is combined with quinidine, a 2D6 inhibitor, administering DMQ with other 2D6 inhibitors could lead to toxicity. When DMQ is combined with SSRIs and similar agents, the serotonergic properties of DM could result in serotonin syndrome, which could be fatal if DM is combined with monoamine oxidase inhibitors.10 Combinations of DM and acetaminophen and antihistamines can be dangerous at higher doses.10 Because quinidine is metabolized by CYP3A, inhibitors of this enzyme such as ketoconazole, nefazodone, and grapefruit juice should be avoided. Similarly, inhibition of CYP2D6 by quinidine could raise levels of coadministered 2D6 substrates.
Contraindications. DMQ is contraindicated in patients with:
- heart failure
- prolonged QT interval
- congenital long QT interval
- history of torsades de pointes
- complete atrioventricular (AV) block without implanted pacemakers.13
DMQ also is contraindicated in patients at high risk for complete AV block.13
Dosing
DMQ is available as a capsule containing DM, 20 mg, and quinidine, 10 mg. The recommended starting dose is 1 capsule by mouth for 7 days, then 1 capsule every 12 hours.
Although DMQ is convenient, its advantage over starting with DM alone and adding a small dose of a non-serotonergic 2D6 inhibitor if DM is not effective remains to be demonstrated. In view of the unknown potential for abuse and toxicity as well as the cost of the proprietary drug ($3,000 to $5,000 a year), it would seem prudent to consider using an SSRI or a TCA first.8 These medications also act on 1-sigma receptors,14,15 which may account in part for their reported benefit.
Related Resource
- Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
Drug Brand Names
- Amantadine • Symmetrel
- Dextromethorphan/quinidine •Nefazodone
- Ketoconazole • Nizoral
- Levodopa • Sinemet
- Neudexta • Serzone
- Quinidine • Quinidex
Disclosures
Dr. Dubovsky receives research support from Biogen Idec, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Otsuka, the Peter and Elizabeth C. Tower Foundation, and Pfizer, Inc.
Dr. Tan reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 2
Dextromethorphan/quinidine for PBA: Evidence shows efficacy
| Study | Patients | Dosages | Results |
|---|---|---|---|
| Panitch et al, 200610; 85-day, randomized, double-blind, placebo-controlled | 150 MS patients with PBA | DMQ 30-30 or placebo, given twice a day | DMQ 30-30 was associated with greater reductions in CNC-LS scores, fewer PBA episodes, improvement in QOL and QOR, and decrease in pain intensity |
| Pope, 20065; 3-arm, double-blind, 28-day phase III multicenter trial | 140 ALS patients with PBA | DMQ 30-30, DM, 30 mg, or quinidine, 30 mg, given twice daily | DMQ 30-30 was associated with greater decreases in CNC-LS scores and number of laughing and crying episodes and improvements in QOL and QOR compared with DM or quinidine alone |
| Pioro et al, 20107; 12-week, randomized, double-blind, placebo-controlled trial | 326 ALS and MS patients with clinically significant PBA | DMQ 30-10, DMQ 20-10, or placebo, given twice daily | CNC-LS scores decreased in all groups but the daily rate of PBA episodes was 47% lower for DMQ 30-10 and 49% lower for DMQ 20-10 compared with placebo |
| ALS: amyotrophic lateral sclerosis; CNC-LS: Center for Neurologic Study-Lability Scale; DM: dextromethorphan; DMQ 20-10: dextromethorphan, 20 mg, plus quinidine, 10 mg; DMQ 30-10: dextromethorphan, 30 mg, plus quinidine, 10 mg; DMQ 30-30: dextromethorphan, 30 mg, plus quinidine, 30 mg; MS: multiple sclerosis; PBA: pseudobulbar affect; QOL: quality of life; QOR: quality of relationships | |||
In October 2010, the FDA approved a combination of dextromethorphan (DM) and quinidine for the treatment of pseudobulbar affect (PBA)—also called pathological laughing and crying, affective lability, emotional dyscontrol, emotional incontinence, and involuntary emotional expression disorder—in patients with neurologic disorders and brain injuries (Table). Despite receiving an approvable letter in 2006, the compound was not approved at that time because of concerns about the arrhythmogenic potential of quinidine, which prolongs the QT interval. The manufacturer conducted another study using one-third of the previous quinidine dose, which ameliorated this concern and led to approval.
Clinical implications
PBA is manifested by involuntary labile, shallow affect with sudden and unpredictable laughing, crying, or other emotional displays that are not appropriate to the social setting and may not be congruent with the patient’s prevailing mood.1 Episodes are often paroxysmal and cannot be interrupted voluntarily.2 PBA seems to be caused by a loss of descending cortical control of brainstem motor nuclei and possibly the cerebellum, disrupting inhibitory mechanisms and resulting in inappropriate and involuntary emotional display.3 Several studies have demonstrated involvement of subcortical areas, particularly the anterior limb of the internal capsule and the bulbar area. The patho-physiology of PBA may involve excessive release of glutamate by injured neurons, disrupting systems for motor control of emotional expression.4,5
Table
Dextromethorphan/quinidine: Fast facts
| Brand name: Nuedexta |
| Indication: Pseudobulbar affect |
| Approval date: October 29, 2010 |
| Availability date: First quarter of 2011 |
| Manufacturer: Avanir |
| Dosage forms: Dextromethorphan, 20 mg, plus quinidine, 10 mg |
| Starting dose: 1 capsule per day |
| Target dose: 2 capsules per day |
PBA is most common in diseases that interfere bilaterally with the corticohypothalamic and corticobulbar tracts that control voluntary and involuntary faciorespiratory mechanisms. However, PBA occurs in unilateral disease as well. The reported prevalence of PBA is:
- 49% in amyotrophic lateral sclerosis (ALS)
- 18% to 39% in Alzheimer’s disease
- 11% to 34% in stroke
- 10% to 11% in multiple sclerosis (MS) and traumatic brain injury.6,7
PBA also has been reported in patients with Parkinson’s disease, brain tumors, Wilson’s disease, syphilitic pseudobulbar palsy, and various encephalitides.1 An estimated 880,000 U.S. patients exhibit PBA.8
Previously, there was no FDA-approved treatment for PBA. However, small controlled trials suggest that selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs)— usually in doses lower than those used to treat depression—may effectively reduce symptoms within 2 to 3 days.1 Although dopaminergic agents such as levodopa and amantadine have shown benefit in open trials, results of controlled studies using objective measurements have not been positive.
How it works
DM is a serotonergic substance that also is an agonist of 1-sigma receptors and a low-affinity, uncompetitive antagonist of N-methyl-d-aspartate (NMDA) receptors, which are important in glutamate signaling, through binding at the phencyclidine site on the NMDA complex.7,9 The 1-sigma receptor was thought to be an opioid receptor subtype, but unlike opioid receptors it is not blocked by narcotic antagonists and does not have an endogenous ligand. However, the 1-sigma receptor does modulate activity of opioid mu receptors in addition to altering dopamine release and possibly reducing glutamate release.9 Sigma receptors are densely distributed in the limbic system and in systems related to motor control of affective expression and seem to be involved in learning, responses to stress, mood regulation, and drug dependence.1 Because DM preferentially binds to brain regions that regulate emotional expression,10 it could normalize glutaminergic neurotransmission and other relevant systems in these regions.1 However, DM’s exact mechanism of action is unknown.
Quinidine is a sodium channel antagonist usually used as a type Ia antiarrhythmic.5 DM is subject to extensive first-pass metabolism by cytochrome P (CYP) 450 2D6 to dextrorphan, which after being glucuronidated cannot cross the blood-brain barrier. In doses 10 to 25 times lower than those used to treat cardiac arrhythmias, quinidine inhibits 2D6 and increases DM bioavailability.10 DM blood levels increase linearly with dose following coadministration with quinidine but are undetectable in most patients given DM alone.7,9
Efficacy and tolerability
A combination of DM and quinidine (DMQ) reduced Center for Neurologic Study-Lability Scale (CNC-LS) scores and the number of daily PBA episodes in 3 randomized trials.5,7,10 Visit this article at CurrentPsychiatry.com for a table summarizing these studies.
An 85-day randomized, double-blind, placebo-controlled study of 150 patients with PBA associated with MS found that DM, 30 mg, plus quinidine, 30 mg, (DMQ 30-30) was twice as effective as placebo within a week in reducing CNC-LS scores.10 DMQ 30-30 patients also had approximately half as many episodes of inappropriate laughing, crying, or combined laughing and crying and a 2-fold greater decrease in pain intensity.10 Twenty-one percent of DMQ 30-30 patients experienced complete remission—no PBA episodes—compared with 7% of placebo patients. There were no significant differences in QT prolongation between DMQ 30-30 and placebo.
A 3-arm, double-blind, 28-day, phase III multicenter trial of 140 ALS patients with PBA compared DM monotherapy, quinidine monotherapy, and DMQ 30-30.5 Compared with either drug alone, DMQ 30-30 showed greater reduction of CNC-LS scores, as well as improved quality of life and quality of relationships scores, with equal benefit in poor and extensive DM metabolizers. However, the control conditions may not have been adequate. Quinidine alone would not be expected to have an effect on PBA, and the DM dose, which was the same in combination and monotherapy, may have been too low to be effective by itself. In support of this hypothesis, the DM plasma level was 18 times higher in patients taking DMQ 30-30 than those taking DM monotherapy.
In a manufacturer-sponsored, multicenter, 12-week randomized trial, 326 patients with ALS or MS and clinically significant PBA were randomly assigned to DM, 30 mg, plus quinidine, 10 mg (DMQ 30-10), DM, 20 mg, plus quinidine, 10 mg (DMQ 20-10), or placebo, each administered twice daily.7 Patients with comorbid psychiatric disorders or significant depressive symptoms were excluded. Although daily PBA episodes decreased in all groups, the daily rate of PBA episodes was 47% lower for patients taking DMQ 30-10, and 49% lower with DMQ 20-10 compared with placebo (both P < .001). The mean decrease in the number of daily PBA episodes was 3.9 to 4.1 with active treatment and 3.0 with placebo. Side effects were more common with active drug than placebo and included dizziness, nausea, diarrhea, and urinary tract infection. There were no serious adverse cardiac events and no active drug recipients showed a QTc interval >480 msec or a change from baseline >60 msec.11 Discontinuation rates in this study were lower than in studies of DMQ 30-30. In an open-label extension of 253 patients who completed the double-blind phase and were assigned to DMQ 30-10 for 12 weeks, the incidence of treatment-related adverse events was 28%, with a 5.5% rate of serious adverse events.12
Safety
Because the 10 mg dose of quinidine in the approved formulation of DMQ is 10 times lower than the antiarrhythmic dose, substantial ECG changes and adverse cardiac effects with DMQ have not been reported. The most common side effects of DM are nausea, somnolence, dizziness, and headache. Thrombocytopenia, QT prolongation, hepatotoxicity, allergic reactions, and anticholinergic side effects can occur.
In high doses and combined with other substances, DM has been used as a recreational drug. When taken in high doses, adverse effects include nausea, vomiting, malaise, dilated pupils, difficulty urinating, increased urination frequency, fever, tachycardia, loss of appetite, shakiness, seizures, and potentially coma and death. DMQ may have a greater potential for serious adverse effects than DM alone because quinidine increases DM bioavailability and blood levels. The abuse potential of DMQ is not clear.
Psychosis has been reported with higher DM doses. The psychotomimetic effects of phencyclidine (PCP) are related to binding to the PCP site on the NMDA receptor complex—to which DM also binds—with reduced glutamate signaling in information processing systems. Therefore, caution is indicated when prescribing DM to patients with psychosis.
Because DM, a CYP2D6 substrate, is combined with quinidine, a 2D6 inhibitor, administering DMQ with other 2D6 inhibitors could lead to toxicity. When DMQ is combined with SSRIs and similar agents, the serotonergic properties of DM could result in serotonin syndrome, which could be fatal if DM is combined with monoamine oxidase inhibitors.10 Combinations of DM and acetaminophen and antihistamines can be dangerous at higher doses.10 Because quinidine is metabolized by CYP3A, inhibitors of this enzyme such as ketoconazole, nefazodone, and grapefruit juice should be avoided. Similarly, inhibition of CYP2D6 by quinidine could raise levels of coadministered 2D6 substrates.
Contraindications. DMQ is contraindicated in patients with:
- heart failure
- prolonged QT interval
- congenital long QT interval
- history of torsades de pointes
- complete atrioventricular (AV) block without implanted pacemakers.13
DMQ also is contraindicated in patients at high risk for complete AV block.13
Dosing
DMQ is available as a capsule containing DM, 20 mg, and quinidine, 10 mg. The recommended starting dose is 1 capsule by mouth for 7 days, then 1 capsule every 12 hours.
Although DMQ is convenient, its advantage over starting with DM alone and adding a small dose of a non-serotonergic 2D6 inhibitor if DM is not effective remains to be demonstrated. In view of the unknown potential for abuse and toxicity as well as the cost of the proprietary drug ($3,000 to $5,000 a year), it would seem prudent to consider using an SSRI or a TCA first.8 These medications also act on 1-sigma receptors,14,15 which may account in part for their reported benefit.
Related Resource
- Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
Drug Brand Names
- Amantadine • Symmetrel
- Dextromethorphan/quinidine •Nefazodone
- Ketoconazole • Nizoral
- Levodopa • Sinemet
- Neudexta • Serzone
- Quinidine • Quinidex
Disclosures
Dr. Dubovsky receives research support from Biogen Idec, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Otsuka, the Peter and Elizabeth C. Tower Foundation, and Pfizer, Inc.
Dr. Tan reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Table 2
Dextromethorphan/quinidine for PBA: Evidence shows efficacy
| Study | Patients | Dosages | Results |
|---|---|---|---|
| Panitch et al, 200610; 85-day, randomized, double-blind, placebo-controlled | 150 MS patients with PBA | DMQ 30-30 or placebo, given twice a day | DMQ 30-30 was associated with greater reductions in CNC-LS scores, fewer PBA episodes, improvement in QOL and QOR, and decrease in pain intensity |
| Pope, 20065; 3-arm, double-blind, 28-day phase III multicenter trial | 140 ALS patients with PBA | DMQ 30-30, DM, 30 mg, or quinidine, 30 mg, given twice daily | DMQ 30-30 was associated with greater decreases in CNC-LS scores and number of laughing and crying episodes and improvements in QOL and QOR compared with DM or quinidine alone |
| Pioro et al, 20107; 12-week, randomized, double-blind, placebo-controlled trial | 326 ALS and MS patients with clinically significant PBA | DMQ 30-10, DMQ 20-10, or placebo, given twice daily | CNC-LS scores decreased in all groups but the daily rate of PBA episodes was 47% lower for DMQ 30-10 and 49% lower for DMQ 20-10 compared with placebo |
| ALS: amyotrophic lateral sclerosis; CNC-LS: Center for Neurologic Study-Lability Scale; DM: dextromethorphan; DMQ 20-10: dextromethorphan, 20 mg, plus quinidine, 10 mg; DMQ 30-10: dextromethorphan, 30 mg, plus quinidine, 10 mg; DMQ 30-30: dextromethorphan, 30 mg, plus quinidine, 30 mg; MS: multiple sclerosis; PBA: pseudobulbar affect; QOL: quality of life; QOR: quality of relationships | |||
1. Schiffer R, Pope LE. Review of pseudobulbar affect including a novel and potential therapy. J Neuropsychiatry Clin Neurosci. 2005;17:447-454.
2. Rosen HJ, Cummings J. A real reason for patients with pseudobulbar affect to smile. Ann Neurol. 2007;61:92-96.
3. Miller A. Pseudobulbar affect in multiple sclerosis: toward the development of innovative therapeutic strategies. J Neurol Sci. 2006;245:153-159.
4. Mattson MP. Excitotoxic and excitoprotective mechanisms: abundant targets for the prevention and treatment of neurodegenerative disorders. Neuromolecular Med. 2003;3:65-94.
5. Pope LE. AVP-923 as a novel treatment for pseudobulbar affect in ALS. Progress in Neurotherapeutics and Neuropsychopharmacology. 2006;1:91-104.
6. Arciniegas DB. A clinical overview of pseudobulbar affect. Am J Geriatr Pharmacother. 2005;3(suppl A):4-8.
7. Pioro EP, Brooks BR, Cummings J, et al. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68:693-702.
8. Johnston SC, Hauser SL. Marketing and drug costs: who is laughing and crying? Ann Neurol. 2007;61:11A-12A.
9. Brooks BR, Thisted RA, Appel SH, et al and. the AVP-923 ALS Study Group. Treatment of pseudobulbar affect with dextromethorphan/quinidine: a randomized trial. Neurology. 2004;63:1364-1370.
10. Panitch HS, Thisted RA, Smith RA, et al. and the Psuedobulbar Affect in Multiple Sclerosis Study Group. Randomized, controlled trial of dextromethorphan/ quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol. 2006;59:780-787.
11. Kaye R, Pratt C. Summary of cardiac safety from a randomized, placebo-controlled, trial of dextromethorphan/ quinidine (STAR) for treatment of pseudobulbar affect. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
12. Pioro EP, Brooks BR, Cummings J, et al. Safety and tolerability of dextromethorphan/quinidine for pseudobulbar affect in a 12-week, open-label extension study. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
13. Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
14. Narita N, Hashimoto K, Tomitaka S, et al. Interactions of selective serotonin reuptake inhibitors with subtypes of sigma receptors in rat brain. Eur J Pharmacol. 1996;307(1):117-119.
15. Dhir A, Kulkarni SK. Involvement of sigma-1 receptor modulation in the antidepressant action of venlafaxine. Neurosci Lett. 2007;420(3):204-208.
1. Schiffer R, Pope LE. Review of pseudobulbar affect including a novel and potential therapy. J Neuropsychiatry Clin Neurosci. 2005;17:447-454.
2. Rosen HJ, Cummings J. A real reason for patients with pseudobulbar affect to smile. Ann Neurol. 2007;61:92-96.
3. Miller A. Pseudobulbar affect in multiple sclerosis: toward the development of innovative therapeutic strategies. J Neurol Sci. 2006;245:153-159.
4. Mattson MP. Excitotoxic and excitoprotective mechanisms: abundant targets for the prevention and treatment of neurodegenerative disorders. Neuromolecular Med. 2003;3:65-94.
5. Pope LE. AVP-923 as a novel treatment for pseudobulbar affect in ALS. Progress in Neurotherapeutics and Neuropsychopharmacology. 2006;1:91-104.
6. Arciniegas DB. A clinical overview of pseudobulbar affect. Am J Geriatr Pharmacother. 2005;3(suppl A):4-8.
7. Pioro EP, Brooks BR, Cummings J, et al. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68:693-702.
8. Johnston SC, Hauser SL. Marketing and drug costs: who is laughing and crying? Ann Neurol. 2007;61:11A-12A.
9. Brooks BR, Thisted RA, Appel SH, et al and. the AVP-923 ALS Study Group. Treatment of pseudobulbar affect with dextromethorphan/quinidine: a randomized trial. Neurology. 2004;63:1364-1370.
10. Panitch HS, Thisted RA, Smith RA, et al. and the Psuedobulbar Affect in Multiple Sclerosis Study Group. Randomized, controlled trial of dextromethorphan/ quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol. 2006;59:780-787.
11. Kaye R, Pratt C. Summary of cardiac safety from a randomized, placebo-controlled, trial of dextromethorphan/ quinidine (STAR) for treatment of pseudobulbar affect. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
12. Pioro EP, Brooks BR, Cummings J, et al. Safety and tolerability of dextromethorphan/quinidine for pseudobulbar affect in a 12-week, open-label extension study. Paper presented at: Annual Meeting of the American Academy of Neurology; April 15, 2010; Toronto, Ontario, Canada.
13. Neudexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals; 2010.
14. Narita N, Hashimoto K, Tomitaka S, et al. Interactions of selective serotonin reuptake inhibitors with subtypes of sigma receptors in rat brain. Eur J Pharmacol. 1996;307(1):117-119.
15. Dhir A, Kulkarni SK. Involvement of sigma-1 receptor modulation in the antidepressant action of venlafaxine. Neurosci Lett. 2007;420(3):204-208.
Lurasidone for schizophrenia
In October 2010, the FDA approved lurasidone for the acute treatment of schizophrenia at a dose of 40 or 80 mg/d administered once daily with food (Table 1).
Table 1
Lurasidone: Fast facts
| Brand name: Latuda |
| Indication: Schizophrenia in adults |
| Approval date: October 28, 2010 |
| Availability date: February 2011 |
| Manufacturer: Sunovion Pharmaceuticals, Inc. |
| Dosing forms: 40 mg and 80 mg tablets |
| Recommended dosage: Starting dose: 40 mg/d. Maximum dose: 80 mg/d |
How it works
Although the drug’s exact mechanism of action is not known, it is thought that lurasidone’s antipsychotic properties are related to its antagonism at serotonin 2A (5-HT2A) and dopamine D2 receptors.1
Similar to most other atypical antipsychotics, lurasidone has high binding affinity for 5-HT2A and D2. Lurasidone has also high binding affinity for 5-HT7, 5-HT1A, and α2C-adrenergic receptors, low affinity for α-1 receptors, and virtually no affinity for H1 and M1 receptors (Table 2). Activity on 5-HT7, 5-HT1A, and α2C-adrenergic receptors is believed to enhance cognition, and 5-HT7 is being studied for a potential role in mood regulation and sensory processing.2,3 Lurasidone’s low activity on α-1, H1, and M1 receptors suggests a low risk of orthostatic hypotension, H1-mediated sedation and weight gain, and H1- and M1-mediated cognitive blunting.
Pharmacokinetics
Lurasidone is absorbed in the gastrointestinal tract. It reaches maximum concentration (Cmax) in 1 to 3 hours. Cmax doubles when lurasidone is administered with food (≥350 calories), but absorption is independent of the meal’s fat content.4 After absorption, the drug is highly bound (99%) to serum proteins (albumin and α-1-glycoprotein). The elimination half-life is 18 hours and steady-state concentration is reached within 7 days.1 Lurasidone is eliminated predominantly through cytochrome P450 (CYP) 3A4 metabolism in the liver.
Efficacy
Lurasidone’s efficacy for treatment of acute schizophrenia was established in four 6-week, randomized placebo-controlled clinical trials.1 The patients were adults (mean age: 38.8; range: 18 to 72) who met DSM-IVTR criteria for schizophrenia, didn’t abuse drugs or alcohol, and had not taken any investigational drug for ≥1 month. Symptoms were measured on the Positive and Negative Syndrome Scale (PANSS); Brief Psychiatric Rating Scale as derived from the PANSS (BPRSd); and the Clinical Global Impressions-Severity scale (CGI-S).
In the first clinical trial, 145 patients were randomized to lurasidone, 40 mg/d or 120 mg/d, or placebo. Treatment with either dose of lurasidone was superior to treatment with placebo on the BPRSd (Least Squares Mean [LSM] difference from placebo in change from baseline: -5.6 on lurasidone 40 mg/d, -6.7 on lurasidone 120 mg/d) and CGI-S.1,5
The second trial randomized 180 patients to lurasidone, 80 mg/d, or placebo. Lurasidone, 80 mg/d, was superior to placebo as measured on the BPRSd (LSM difference from placebo in change from baseline: -4.7 on lurasidone 80 mg/d) and CGI-S.1,6
The third trial randomized 489 patients to lurasidone, 40 mg/d, 80 mg/d, 120 mg/d, or placebo. All lurasidone arms were superior to placebo on PANSS (LSM difference from placebo in change from baseline: -2.1 on 40 mg/d, -6.4 on 80 mg/d, and -3.5 on 120 mg/d) and CGI-S scores. This study also showed that lurasidone appears to have a rapid onset of action (day 3 to 4) and provides sustained improvement of symptoms.1
In the fourth trial, 473 individuals were randomized to lurasidone, 40 mg/d or 120 mg/d, olanzapine, 15 mg/d, or placebo. Olanzapine and both dosages of lurasidone were superior to placebo in improving PANSS scores (LSM difference from placebo in change from baseline: -9.7 on lurasidone 40 mg/d, -7.5 on lurasidone 120 mg/d, and -12.6 on olanzapine 15 mg/d) and CGI-S.1,7 Both doses of lurasidone were not superior to olanzapine but had less negative impact on lipid profile, weight gain, and glycemia.
Tolerability
Tolerability information is extracted from a clinical study database consisting of 2,096 patients with schizophrenia who participated in premarketing clinical trials and were exposed to single or multiple doses of lurasidone, 20 mg, 40 mg, 80 mg, or 120 mg.1 Overall, lurasidone was well tolerated. The rate of discontinuation from clinical trials because of adverse effects was 9.4% for lurasidone vs 5.9% for placebo. Somnolence, akathisia, nausea, parkinsonism, and agitation were the most commonly reported adverse reactions; somnolence and akathisia appear dose-related. Other adverse effects associated with lurasidone were nausea, vomiting, dyspepsia, dystonia, dizziness, insomnia, agitation, and anxiety (Table 2).
Metabolic changes (hyperlipidemia, hyperglycemia, and increased body weight) associated with cardiovascular risk in patients treated with atypical antipsychotics were studied in short-term placebo-controlled trials. Lurasidone is considered to be weight-neutral and does not have significant effects on serum lipids or glucose.2 As is the case with other D2 antagonists, lurasidone is associated with increased prolactin, which appears to be greater in females and is dose-dependent. Lurasidone is not associated with significant QTc prolongation, seizures, transaminases increase, or changes in serum chemistry, hematology, or urinalysis.
Table 2
Lurasidone receptor binding profile and receptor-related effects
| Ki (nM)* | Effects associated with activity on the receptor | |
|---|---|---|
| D2 | 0.994 | Antipsychotic effects. Akathisia (15%), parkinsonism (11%), dystonia (5%), hyperprolactinemia (8.3% for women, 1.9% for men) |
| 5-HT2A | 0.47 | Antipsychotic effects. Improves extrapyramidal symptoms |
| 5-HT7 | 0.495 | Antipsychotic effects. Improves cognition, mood |
| 5-HT1A | 6.38 | Improves cognition, mood. Nausea (12%), vomiting (8%) |
| α-1 | 48 | Orthostatic hypotension (5%), sedation (22%) |
| α-2C | 10.8 | Improves cognition |
| H1 | >1000 | No significant adverse effects mediated through H1 receptor because of low binding affinity |
| M1 | >1000 | No significant adverse effects mediated through M1 receptor because of low binding affinity |
| *Ki dissociation constant; the lower the number, the higher affinity of the compound for the receptor Source: Adapted from reference 1, expert opinion, and lurasidone data on file, 2008 | ||
Contraindications
Lurasidone is contraindicated in patients with known sensitivity to lurasidone hydrochloride. Because of the risk for pharmacokinetic drug-drug interactions, lurasidone is contraindicated for patients who are taking strong CYP3A4 inhibitors (eg, ketoconazole) or inducers (eg, rifampin).
Similar to other medications in its class, lurasidone carries a “black-box” warning of increased mortality in elderly patients with dementia-related psychosis and it is not FDA-approved for treating this condition. Animal teratogenicity studies using lurasidone, 25 mg/kg/d and 50 mg/kg/d, did not show adverse effects during organogenesis, and lurasidone is classified as pregnancy category B (animal studies failed to demonstrate risk to the fetus and there are no adequate and well-controlled studies in pregnant women, or animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester). The use of lurasidone in geriatric and pediatric populations was not studied.1
Dosing
Lurasidone is manufactured as 40 mg and 80 mg tablets. The recommended starting dose is 40 mg/d and the maximum recommended dose is 80 mg/d.1 In clinical trials, lurasidone, 120 mg/d, was associated with increased incidence of adverse effects without added benefit.
Lurasidone doesn’t require initial dose titration and should be given with food that provides ≥350 calories to improve medication absorption. Dose adjustment is recommended for use in patients with moderate or severe renal or hepatic impairment and when coadministered with CYP3A4 moderate inhibitors; the dose in these patients should not exceed 40 mg/d.
Related Resource
- Citrome L. Lurasidone for schizophrenia: a review of the efficacy and safety profile for this newly approved second-generation antipsychotic. Int J Clin Pract. 2010 Epub ahead of print.
Drug Brand Names
- Ketoconazole • Nizoral
- Lurasidone • Latuda
- Olanzapine • Zyprexa
- Rifampin • Rifadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc.; 2010.
2. Meyer JM, Loebel AD, Schweizer E. Lurasidone: a new drug in development for schizophrenia. Expert Opin Investig Drugs. 2009;18(11):1715-1726.
3. Terry AV, Jr, Buccafusco JJ, Wilson C. Cognitive dysfunction in neuropsychiatric, disorders: selected serotonin receptor subtypes as therapeutic targets. Behav Brain Res. 2008;195(1):30-38.
4. Preskorn SH, Yu-Yuan CH, Sarubbi D, et al. Lurasidone pharmacokinetics: Assessment of potential for drug-drug interaction. Abstract presented at: The American College of Neuropsychopharmacology 49th Annual Meeting; December 5-9, 2010; Miami Beach, FL.
5. Loebel A, Cucchiaro J, Ogasa M, et al. Lurasidone for schizophrenia: symptomatic remission during short-term treatment. Abstract presented at: 162nd Annual Meeting of American Psychiatric Association; May 16-21, 2009; San Francisco, CA. Abstract NR1-054.
6. Nakamura M, Ogasa M, Guarino J, et al. Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial. J Clin Psychiatry. 2009;70(6):829-836.
7. Meltzer H, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of acute schizophrenia: results of the double-blind, placebo-controlled, PEARL 2 trial. Abstract presented at: 48th Annual Meeting of American College of Neuropsychopharmacology; December 6-10, 2009; Hollywood, FL. Abstract 76.
In October 2010, the FDA approved lurasidone for the acute treatment of schizophrenia at a dose of 40 or 80 mg/d administered once daily with food (Table 1).
Table 1
Lurasidone: Fast facts
| Brand name: Latuda |
| Indication: Schizophrenia in adults |
| Approval date: October 28, 2010 |
| Availability date: February 2011 |
| Manufacturer: Sunovion Pharmaceuticals, Inc. |
| Dosing forms: 40 mg and 80 mg tablets |
| Recommended dosage: Starting dose: 40 mg/d. Maximum dose: 80 mg/d |
How it works
Although the drug’s exact mechanism of action is not known, it is thought that lurasidone’s antipsychotic properties are related to its antagonism at serotonin 2A (5-HT2A) and dopamine D2 receptors.1
Similar to most other atypical antipsychotics, lurasidone has high binding affinity for 5-HT2A and D2. Lurasidone has also high binding affinity for 5-HT7, 5-HT1A, and α2C-adrenergic receptors, low affinity for α-1 receptors, and virtually no affinity for H1 and M1 receptors (Table 2). Activity on 5-HT7, 5-HT1A, and α2C-adrenergic receptors is believed to enhance cognition, and 5-HT7 is being studied for a potential role in mood regulation and sensory processing.2,3 Lurasidone’s low activity on α-1, H1, and M1 receptors suggests a low risk of orthostatic hypotension, H1-mediated sedation and weight gain, and H1- and M1-mediated cognitive blunting.
Pharmacokinetics
Lurasidone is absorbed in the gastrointestinal tract. It reaches maximum concentration (Cmax) in 1 to 3 hours. Cmax doubles when lurasidone is administered with food (≥350 calories), but absorption is independent of the meal’s fat content.4 After absorption, the drug is highly bound (99%) to serum proteins (albumin and α-1-glycoprotein). The elimination half-life is 18 hours and steady-state concentration is reached within 7 days.1 Lurasidone is eliminated predominantly through cytochrome P450 (CYP) 3A4 metabolism in the liver.
Efficacy
Lurasidone’s efficacy for treatment of acute schizophrenia was established in four 6-week, randomized placebo-controlled clinical trials.1 The patients were adults (mean age: 38.8; range: 18 to 72) who met DSM-IVTR criteria for schizophrenia, didn’t abuse drugs or alcohol, and had not taken any investigational drug for ≥1 month. Symptoms were measured on the Positive and Negative Syndrome Scale (PANSS); Brief Psychiatric Rating Scale as derived from the PANSS (BPRSd); and the Clinical Global Impressions-Severity scale (CGI-S).
In the first clinical trial, 145 patients were randomized to lurasidone, 40 mg/d or 120 mg/d, or placebo. Treatment with either dose of lurasidone was superior to treatment with placebo on the BPRSd (Least Squares Mean [LSM] difference from placebo in change from baseline: -5.6 on lurasidone 40 mg/d, -6.7 on lurasidone 120 mg/d) and CGI-S.1,5
The second trial randomized 180 patients to lurasidone, 80 mg/d, or placebo. Lurasidone, 80 mg/d, was superior to placebo as measured on the BPRSd (LSM difference from placebo in change from baseline: -4.7 on lurasidone 80 mg/d) and CGI-S.1,6
The third trial randomized 489 patients to lurasidone, 40 mg/d, 80 mg/d, 120 mg/d, or placebo. All lurasidone arms were superior to placebo on PANSS (LSM difference from placebo in change from baseline: -2.1 on 40 mg/d, -6.4 on 80 mg/d, and -3.5 on 120 mg/d) and CGI-S scores. This study also showed that lurasidone appears to have a rapid onset of action (day 3 to 4) and provides sustained improvement of symptoms.1
In the fourth trial, 473 individuals were randomized to lurasidone, 40 mg/d or 120 mg/d, olanzapine, 15 mg/d, or placebo. Olanzapine and both dosages of lurasidone were superior to placebo in improving PANSS scores (LSM difference from placebo in change from baseline: -9.7 on lurasidone 40 mg/d, -7.5 on lurasidone 120 mg/d, and -12.6 on olanzapine 15 mg/d) and CGI-S.1,7 Both doses of lurasidone were not superior to olanzapine but had less negative impact on lipid profile, weight gain, and glycemia.
Tolerability
Tolerability information is extracted from a clinical study database consisting of 2,096 patients with schizophrenia who participated in premarketing clinical trials and were exposed to single or multiple doses of lurasidone, 20 mg, 40 mg, 80 mg, or 120 mg.1 Overall, lurasidone was well tolerated. The rate of discontinuation from clinical trials because of adverse effects was 9.4% for lurasidone vs 5.9% for placebo. Somnolence, akathisia, nausea, parkinsonism, and agitation were the most commonly reported adverse reactions; somnolence and akathisia appear dose-related. Other adverse effects associated with lurasidone were nausea, vomiting, dyspepsia, dystonia, dizziness, insomnia, agitation, and anxiety (Table 2).
Metabolic changes (hyperlipidemia, hyperglycemia, and increased body weight) associated with cardiovascular risk in patients treated with atypical antipsychotics were studied in short-term placebo-controlled trials. Lurasidone is considered to be weight-neutral and does not have significant effects on serum lipids or glucose.2 As is the case with other D2 antagonists, lurasidone is associated with increased prolactin, which appears to be greater in females and is dose-dependent. Lurasidone is not associated with significant QTc prolongation, seizures, transaminases increase, or changes in serum chemistry, hematology, or urinalysis.
Table 2
Lurasidone receptor binding profile and receptor-related effects
| Ki (nM)* | Effects associated with activity on the receptor | |
|---|---|---|
| D2 | 0.994 | Antipsychotic effects. Akathisia (15%), parkinsonism (11%), dystonia (5%), hyperprolactinemia (8.3% for women, 1.9% for men) |
| 5-HT2A | 0.47 | Antipsychotic effects. Improves extrapyramidal symptoms |
| 5-HT7 | 0.495 | Antipsychotic effects. Improves cognition, mood |
| 5-HT1A | 6.38 | Improves cognition, mood. Nausea (12%), vomiting (8%) |
| α-1 | 48 | Orthostatic hypotension (5%), sedation (22%) |
| α-2C | 10.8 | Improves cognition |
| H1 | >1000 | No significant adverse effects mediated through H1 receptor because of low binding affinity |
| M1 | >1000 | No significant adverse effects mediated through M1 receptor because of low binding affinity |
| *Ki dissociation constant; the lower the number, the higher affinity of the compound for the receptor Source: Adapted from reference 1, expert opinion, and lurasidone data on file, 2008 | ||
Contraindications
Lurasidone is contraindicated in patients with known sensitivity to lurasidone hydrochloride. Because of the risk for pharmacokinetic drug-drug interactions, lurasidone is contraindicated for patients who are taking strong CYP3A4 inhibitors (eg, ketoconazole) or inducers (eg, rifampin).
Similar to other medications in its class, lurasidone carries a “black-box” warning of increased mortality in elderly patients with dementia-related psychosis and it is not FDA-approved for treating this condition. Animal teratogenicity studies using lurasidone, 25 mg/kg/d and 50 mg/kg/d, did not show adverse effects during organogenesis, and lurasidone is classified as pregnancy category B (animal studies failed to demonstrate risk to the fetus and there are no adequate and well-controlled studies in pregnant women, or animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester). The use of lurasidone in geriatric and pediatric populations was not studied.1
Dosing
Lurasidone is manufactured as 40 mg and 80 mg tablets. The recommended starting dose is 40 mg/d and the maximum recommended dose is 80 mg/d.1 In clinical trials, lurasidone, 120 mg/d, was associated with increased incidence of adverse effects without added benefit.
Lurasidone doesn’t require initial dose titration and should be given with food that provides ≥350 calories to improve medication absorption. Dose adjustment is recommended for use in patients with moderate or severe renal or hepatic impairment and when coadministered with CYP3A4 moderate inhibitors; the dose in these patients should not exceed 40 mg/d.
Related Resource
- Citrome L. Lurasidone for schizophrenia: a review of the efficacy and safety profile for this newly approved second-generation antipsychotic. Int J Clin Pract. 2010 Epub ahead of print.
Drug Brand Names
- Ketoconazole • Nizoral
- Lurasidone • Latuda
- Olanzapine • Zyprexa
- Rifampin • Rifadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
In October 2010, the FDA approved lurasidone for the acute treatment of schizophrenia at a dose of 40 or 80 mg/d administered once daily with food (Table 1).
Table 1
Lurasidone: Fast facts
| Brand name: Latuda |
| Indication: Schizophrenia in adults |
| Approval date: October 28, 2010 |
| Availability date: February 2011 |
| Manufacturer: Sunovion Pharmaceuticals, Inc. |
| Dosing forms: 40 mg and 80 mg tablets |
| Recommended dosage: Starting dose: 40 mg/d. Maximum dose: 80 mg/d |
How it works
Although the drug’s exact mechanism of action is not known, it is thought that lurasidone’s antipsychotic properties are related to its antagonism at serotonin 2A (5-HT2A) and dopamine D2 receptors.1
Similar to most other atypical antipsychotics, lurasidone has high binding affinity for 5-HT2A and D2. Lurasidone has also high binding affinity for 5-HT7, 5-HT1A, and α2C-adrenergic receptors, low affinity for α-1 receptors, and virtually no affinity for H1 and M1 receptors (Table 2). Activity on 5-HT7, 5-HT1A, and α2C-adrenergic receptors is believed to enhance cognition, and 5-HT7 is being studied for a potential role in mood regulation and sensory processing.2,3 Lurasidone’s low activity on α-1, H1, and M1 receptors suggests a low risk of orthostatic hypotension, H1-mediated sedation and weight gain, and H1- and M1-mediated cognitive blunting.
Pharmacokinetics
Lurasidone is absorbed in the gastrointestinal tract. It reaches maximum concentration (Cmax) in 1 to 3 hours. Cmax doubles when lurasidone is administered with food (≥350 calories), but absorption is independent of the meal’s fat content.4 After absorption, the drug is highly bound (99%) to serum proteins (albumin and α-1-glycoprotein). The elimination half-life is 18 hours and steady-state concentration is reached within 7 days.1 Lurasidone is eliminated predominantly through cytochrome P450 (CYP) 3A4 metabolism in the liver.
Efficacy
Lurasidone’s efficacy for treatment of acute schizophrenia was established in four 6-week, randomized placebo-controlled clinical trials.1 The patients were adults (mean age: 38.8; range: 18 to 72) who met DSM-IVTR criteria for schizophrenia, didn’t abuse drugs or alcohol, and had not taken any investigational drug for ≥1 month. Symptoms were measured on the Positive and Negative Syndrome Scale (PANSS); Brief Psychiatric Rating Scale as derived from the PANSS (BPRSd); and the Clinical Global Impressions-Severity scale (CGI-S).
In the first clinical trial, 145 patients were randomized to lurasidone, 40 mg/d or 120 mg/d, or placebo. Treatment with either dose of lurasidone was superior to treatment with placebo on the BPRSd (Least Squares Mean [LSM] difference from placebo in change from baseline: -5.6 on lurasidone 40 mg/d, -6.7 on lurasidone 120 mg/d) and CGI-S.1,5
The second trial randomized 180 patients to lurasidone, 80 mg/d, or placebo. Lurasidone, 80 mg/d, was superior to placebo as measured on the BPRSd (LSM difference from placebo in change from baseline: -4.7 on lurasidone 80 mg/d) and CGI-S.1,6
The third trial randomized 489 patients to lurasidone, 40 mg/d, 80 mg/d, 120 mg/d, or placebo. All lurasidone arms were superior to placebo on PANSS (LSM difference from placebo in change from baseline: -2.1 on 40 mg/d, -6.4 on 80 mg/d, and -3.5 on 120 mg/d) and CGI-S scores. This study also showed that lurasidone appears to have a rapid onset of action (day 3 to 4) and provides sustained improvement of symptoms.1
In the fourth trial, 473 individuals were randomized to lurasidone, 40 mg/d or 120 mg/d, olanzapine, 15 mg/d, or placebo. Olanzapine and both dosages of lurasidone were superior to placebo in improving PANSS scores (LSM difference from placebo in change from baseline: -9.7 on lurasidone 40 mg/d, -7.5 on lurasidone 120 mg/d, and -12.6 on olanzapine 15 mg/d) and CGI-S.1,7 Both doses of lurasidone were not superior to olanzapine but had less negative impact on lipid profile, weight gain, and glycemia.
Tolerability
Tolerability information is extracted from a clinical study database consisting of 2,096 patients with schizophrenia who participated in premarketing clinical trials and were exposed to single or multiple doses of lurasidone, 20 mg, 40 mg, 80 mg, or 120 mg.1 Overall, lurasidone was well tolerated. The rate of discontinuation from clinical trials because of adverse effects was 9.4% for lurasidone vs 5.9% for placebo. Somnolence, akathisia, nausea, parkinsonism, and agitation were the most commonly reported adverse reactions; somnolence and akathisia appear dose-related. Other adverse effects associated with lurasidone were nausea, vomiting, dyspepsia, dystonia, dizziness, insomnia, agitation, and anxiety (Table 2).
Metabolic changes (hyperlipidemia, hyperglycemia, and increased body weight) associated with cardiovascular risk in patients treated with atypical antipsychotics were studied in short-term placebo-controlled trials. Lurasidone is considered to be weight-neutral and does not have significant effects on serum lipids or glucose.2 As is the case with other D2 antagonists, lurasidone is associated with increased prolactin, which appears to be greater in females and is dose-dependent. Lurasidone is not associated with significant QTc prolongation, seizures, transaminases increase, or changes in serum chemistry, hematology, or urinalysis.
Table 2
Lurasidone receptor binding profile and receptor-related effects
| Ki (nM)* | Effects associated with activity on the receptor | |
|---|---|---|
| D2 | 0.994 | Antipsychotic effects. Akathisia (15%), parkinsonism (11%), dystonia (5%), hyperprolactinemia (8.3% for women, 1.9% for men) |
| 5-HT2A | 0.47 | Antipsychotic effects. Improves extrapyramidal symptoms |
| 5-HT7 | 0.495 | Antipsychotic effects. Improves cognition, mood |
| 5-HT1A | 6.38 | Improves cognition, mood. Nausea (12%), vomiting (8%) |
| α-1 | 48 | Orthostatic hypotension (5%), sedation (22%) |
| α-2C | 10.8 | Improves cognition |
| H1 | >1000 | No significant adverse effects mediated through H1 receptor because of low binding affinity |
| M1 | >1000 | No significant adverse effects mediated through M1 receptor because of low binding affinity |
| *Ki dissociation constant; the lower the number, the higher affinity of the compound for the receptor Source: Adapted from reference 1, expert opinion, and lurasidone data on file, 2008 | ||
Contraindications
Lurasidone is contraindicated in patients with known sensitivity to lurasidone hydrochloride. Because of the risk for pharmacokinetic drug-drug interactions, lurasidone is contraindicated for patients who are taking strong CYP3A4 inhibitors (eg, ketoconazole) or inducers (eg, rifampin).
Similar to other medications in its class, lurasidone carries a “black-box” warning of increased mortality in elderly patients with dementia-related psychosis and it is not FDA-approved for treating this condition. Animal teratogenicity studies using lurasidone, 25 mg/kg/d and 50 mg/kg/d, did not show adverse effects during organogenesis, and lurasidone is classified as pregnancy category B (animal studies failed to demonstrate risk to the fetus and there are no adequate and well-controlled studies in pregnant women, or animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester). The use of lurasidone in geriatric and pediatric populations was not studied.1
Dosing
Lurasidone is manufactured as 40 mg and 80 mg tablets. The recommended starting dose is 40 mg/d and the maximum recommended dose is 80 mg/d.1 In clinical trials, lurasidone, 120 mg/d, was associated with increased incidence of adverse effects without added benefit.
Lurasidone doesn’t require initial dose titration and should be given with food that provides ≥350 calories to improve medication absorption. Dose adjustment is recommended for use in patients with moderate or severe renal or hepatic impairment and when coadministered with CYP3A4 moderate inhibitors; the dose in these patients should not exceed 40 mg/d.
Related Resource
- Citrome L. Lurasidone for schizophrenia: a review of the efficacy and safety profile for this newly approved second-generation antipsychotic. Int J Clin Pract. 2010 Epub ahead of print.
Drug Brand Names
- Ketoconazole • Nizoral
- Lurasidone • Latuda
- Olanzapine • Zyprexa
- Rifampin • Rifadin
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc.; 2010.
2. Meyer JM, Loebel AD, Schweizer E. Lurasidone: a new drug in development for schizophrenia. Expert Opin Investig Drugs. 2009;18(11):1715-1726.
3. Terry AV, Jr, Buccafusco JJ, Wilson C. Cognitive dysfunction in neuropsychiatric, disorders: selected serotonin receptor subtypes as therapeutic targets. Behav Brain Res. 2008;195(1):30-38.
4. Preskorn SH, Yu-Yuan CH, Sarubbi D, et al. Lurasidone pharmacokinetics: Assessment of potential for drug-drug interaction. Abstract presented at: The American College of Neuropsychopharmacology 49th Annual Meeting; December 5-9, 2010; Miami Beach, FL.
5. Loebel A, Cucchiaro J, Ogasa M, et al. Lurasidone for schizophrenia: symptomatic remission during short-term treatment. Abstract presented at: 162nd Annual Meeting of American Psychiatric Association; May 16-21, 2009; San Francisco, CA. Abstract NR1-054.
6. Nakamura M, Ogasa M, Guarino J, et al. Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial. J Clin Psychiatry. 2009;70(6):829-836.
7. Meltzer H, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of acute schizophrenia: results of the double-blind, placebo-controlled, PEARL 2 trial. Abstract presented at: 48th Annual Meeting of American College of Neuropsychopharmacology; December 6-10, 2009; Hollywood, FL. Abstract 76.
1. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc.; 2010.
2. Meyer JM, Loebel AD, Schweizer E. Lurasidone: a new drug in development for schizophrenia. Expert Opin Investig Drugs. 2009;18(11):1715-1726.
3. Terry AV, Jr, Buccafusco JJ, Wilson C. Cognitive dysfunction in neuropsychiatric, disorders: selected serotonin receptor subtypes as therapeutic targets. Behav Brain Res. 2008;195(1):30-38.
4. Preskorn SH, Yu-Yuan CH, Sarubbi D, et al. Lurasidone pharmacokinetics: Assessment of potential for drug-drug interaction. Abstract presented at: The American College of Neuropsychopharmacology 49th Annual Meeting; December 5-9, 2010; Miami Beach, FL.
5. Loebel A, Cucchiaro J, Ogasa M, et al. Lurasidone for schizophrenia: symptomatic remission during short-term treatment. Abstract presented at: 162nd Annual Meeting of American Psychiatric Association; May 16-21, 2009; San Francisco, CA. Abstract NR1-054.
6. Nakamura M, Ogasa M, Guarino J, et al. Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial. J Clin Psychiatry. 2009;70(6):829-836.
7. Meltzer H, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of acute schizophrenia: results of the double-blind, placebo-controlled, PEARL 2 trial. Abstract presented at: 48th Annual Meeting of American College of Neuropsychopharmacology; December 6-10, 2009; Hollywood, FL. Abstract 76.
Trazodone extended release for major depressive disorder
Extended-release (ER) trazodone—FDA-approved in February 2010—improves symptoms of major depressive disorder (MDD) and allows once-daily dosing (Table 1). Trazodone immediate release (IR) was developed in 1960 and approved by the FDA for treatment of MDD in December 1981. Trazodone IR is now mainly prescribed off-label as a hypnotic at lower-than-antidepressant doses, such as 50 to 100 mg/d at bedtime. The dose needed to achieve antidepressant effect is believed to be ≥300 mg/d. Use of the IR formulation for treating depression has been limited by the need for 3-times-a-day dosing and daytime sedation associated with peaks in serum concentration.
Table 1
Trazodone extended release: Fast facts
| Brand name: Oleptro |
| Class: Triazolopyridine-derived antidepressant |
| Indication: Major depressive disorder |
| Approval date: February 2, 2010 |
| Availability date: August 10, 2010 |
| Manufacturer: Labopharm, Inc. |
| Dosage forms: 150 mg and 300 mg bisectable tablets |
| Starting dose: 150 mg at bedtime |
| Target dose: 300 mg/d; maximum dose 375 mg/d |
Clinical implications
Trazodone ER was designed to eliminate the peaks and troughs in serum concentration seen with trazodone IR. It was hypothesized that by reducing the maximum concentration (Cmax) peaks, trazodone ER would permit higher doses to be better tolerated and help patients to more easily reach target antidepressant doses (≥300 mg/d). Trazodone ER’s once-daily dosing also may increase patient adherence.
How it works
The exact mechanism of action through which trazodone treats depression is not completely understood, but is likely related to enhancing serotonergic activity in the CNS. Trazodone is a triazolopyridine antidepressant, inhibits the serotonin transporter, and is a 5-HT2A and 5-HT2C antagonist. This is why it is sometimes referred as a serotonin antagonist/reuptake inhibitor, but regulatory agencies do not accept this class name. Trazodone is an antagonist at both histamine (H1) and α1-adrenergic receptors, which may mediate trazodone’s sedating properties (H1) and hypotensive (α1-adrenergic) effects.
The ER formulation employs a cross-linked, high-amylose starch excipient that provides controlled release of trazodone over an extended period.
Pharmacokinetics
Trazodone ER has linear pharmacokinetics in doses from 75 to 375 mg. Trazodone ER, 300 mg/d, provides a steady-state exposure equivalent to 100 mg of trazodone IR given 3 times daily, while having a lower Cmax. A high-fat meal can increase Cmax of trazodone ER by 1.9-fold. Trazodone is extensively biotransformed in the liver via the cytochrome P450 (CYP) 3A4 pathway and its metabolites are eliminated within 72 hours. Elimination is predominantly renal, with 70% to 75% of an oral dose being recovered in the urine within 72 hours.1 This formulation maintains its controlled-release properties if bisected.
Because trazodone is a substrate of the CYP3A4 enzyme, its metabolism can be inhibited by CYP3A4 inhibitors. Exercise caution when coadministering medications that cause CYP3A4 inhibition with trazodone ER. The effect of short-term administration of ritonavir (4 doses of 200 mg) on the pharmacokinetics of a single dose of trazodone (50 mg) has been studied in 10 healthy subjects.2 The Cmax of trazodone increased by 34%, area under the curve increased 2.4-fold, half-life increased by 2.2-fold, and clearance decreased by 52%. There is no difference in the half-life between the IR and ER formulations because the ER formulation influences only the release kinetics of the drug, not the half-life of the medication.
Efficacy
Efficacy of trazodone for MDD initially was established in trials conducted with trazodone IR.3-10 The efficacy of the ER formulation was established in a multi-center randomized, double-blind, placebo-controlled trial with 412 patients (age 18 to 80). Patients who met DSM-IV criteria for MDD were randomly assigned to trazodone ER (n=206) or placebo (n=206) for 8 weeks.11 This study showed a statistically significant difference between trazodone ER and placebo after 8 weeks of treatment on the primary outcome measure, which was a change in score on the 17-item Hamilton Depression Rating scale (HAMD-17). HAM-D-17 scores decreased 11.4 points in the trazodone ER group and 9.3 points in the placebo group (P=.012 in the modified intent to treat [ITT] population; P=.009 in the completer analysis). This difference was seen from week 1 and throughout the study. Efficacy of trazodone ER was further supported by statistically significant differences between the drug and placebo in 7 of 13 secondary efficacy endpoints in both the modified ITT and per protocol (PP) populations (HAM-D-17 mood item, mean Montgomery-Åsberg Depression Rating Scale [MADRS] total score, mean Clinical Global Impressions Severity of Illness [CGI-S] score, percentage of HAM-D-17 responders, and 3 quality of sleep items [overall quality of sleep, trouble falling asleep, and awakening during the night]). Overall effect sizes for the HAM-D-17 were -0.26 (modified ITT-last observation carried forward [LOCF] dataset) and -0.33 (PP/observed cases [OC] dataset). The effect sizes in MADRS scores were -0.22 and -0.29 for the modified ITT-LOCF and the PP/OC analyses, respectively.12
Sleep measures. In the study sample >90% of patients had insomnia at baseline (defined as a score ≥2 in any HAM-D-17 sleep item or sum of all 3 sleep items of ≥4). Patients receiving trazodone ER had significant improvement in all 3 HAM-D-17 sleep items. Subjects reported improvement in the overall quality of sleep and awakening during the night after the first week of treatment. Investigators found no significant interaction between improvements in core symptoms of depression and baseline MADRS reduced sleep item or early changes in the HAM-D-17 sleep items. This suggests that the antidepressant effect of trazodone ER was independent of severity of sleep difficulties at baseline and of improvement in insomnia during the study.12
Researchers observed improvement in suicidal ideation on MADRS (item 10) and HAM-D-17 (item 3) after 8 weeks of treatment (effect size -0.2 favoring trazodone ER over placebo).12
In 2 European comparative, randomized, double-blind trials, trazodone prolonged release showed similar antidepressant efficacy as paroxetine4 and setraline5 as measured by HAM-D, MADRS, and CGI-S. This prolonged release formulation made in Europe is not the same technology as the ER formulation recently approved by the FDA.
Tolerability
In the pivotal registration study, trazodone ER was well tolerated at a mean dose of 310 mg/d.11 Twenty-five patients (12.4%) in the trazodone ER group discontinued the drug because of side effects. The most common side effects leading to discontinuation in the active treatment group were dizziness (n=7), sedation (n=5), and somnolence (n=3).11 The most frequent adverse events reported at any study time point were headache (33%), somnolence (31%), dry mouth (25%), dizziness (25%), nausea (21%), sedation (17%), and fatigue (15%) (Table 2).11 In general, these adverse events were mild to moderate and short-lived; most side effects resolved within the first 2 to 3 weeks of treatment with trazodone ER.11
Sexual side effects—delayed ejaculation, delayed time to orgasm, or orgasmic blockade—are common with many anti-depressants. In the pivotal registration study, the incidence of sexual side effects was low (4.9% with trazodone ER vs 2.5% with placebo).11 This is much lower than the rates typically found with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, which range from 17% to 41%.13,14 This benefit is thought to be mediated through 5-HT2A and 5-HT2C antagonism. Priapism has been reported in trazodone IR at rates ranging from 1 in 1,000 to 1 in 10,000 and does not appear to be dose-related.15 The rate of priapism in persons using agents for erectile dysfunction ranges from .05% to 6%.15 No case of priapism was seen in the trazodone ER study; however, with its sample size of 412 patients this study was not powered to adequately detect this adverse event.11
There was no significant weight gain difference between the active drug and placebo groups over 8 weeks of treatment.
Safety. Trazodone ER should not be used within 14 days of taking a monoamine oxidase inhibitor.1 Trazodone carries a pregnancy category C, meaning that it should be used only if the potential benefit justifies potential risk to the fetus. In animal studies, trazodone has been shown to cause increased fetal resorption and congenital anomalities with doses up to 50 times the maximum human dose (375 mg/d). Trazo-done may be secreted in breast milk. The drug is best avoided in patients with recent myocardial infarction.
Table 2
Trazodone extended release treatment-emergent adverse events*
| Trazodone ER (n=202) | Placebo (n=204) | |
|---|---|---|
| Headache | 67 (33%) | 55 (27%) |
| Somnolence | 63 (31%) | 32 (16%) |
| Dry mouth | 51 (25%) | 26 (13%) |
| Dizziness | 50 (25%) | 25 (12%) |
| Nausea | 42 (21%) | 26 (13%) |
| Sedation | 34 (17%) | 7 (3%) |
| Fatigue | 30 (15%) | 17 (8%) |
| Diarrhea | 19 (9%) | 23 (11%) |
| Constipation | 16 (8%) | 4 (2%) |
| Back pain | 11 (5%) | 7 (3%) |
| Blurred vision | 11 (5%) | 0 (0%) |
| *Reported by ≥5% of patients Source: Reference 11 | ||
Dosing
The recommended starting dose is 150 mg/d at bedtime. The dose may be increased by 75 mg/d every 3 days, but the maximum dose should not exceed 375 mg/d.1 Trazodone ER is available in 150 mg or 300 mg bisectable tablets. Breaking the tablets in half does not affect the controlled release, but they should not be chewed or crushed.
Related Resource
- Extended-release trazodone (Oleptro) prescribing information. www.oleptro.com/images/9379.pdf.
Drug Brand Names
- Paroxetine • Paxil
- Ritonavir • Norvir
- Sertraline • Zoloft
- Trazodone • Desyrel
- Trazodone extended-release • Oleptro
Disclosures
Dr. Hidalgo receives grant/research support from AstraZeneca, CeNeRx Biopharma, Centers for Disease Control and Prevention, Dainippon Sumitomo Pharma America, Inc., Eli Lilly and Company, Forest Laboratories, Indevus Pharmaceuticals, Janssen Pharmaceuticals, Labopharm, Otsuka, Pfizer, Inc., Repligen Corp., Sanofi-Synthelabo, Sepracor, and the University of South Florida, and is consultant to the MAPI Institute.
Dr. Sheehan has received grant funding support from, been affiliated with, or received honoraria and travel expenses related to lectures/presentations or consultant activities from the following organizations: Abbott Laboratories,1,2,3 Ad Hoc Committee, Treatment Drug and Assessment Research Review,1 Alexza,1 Alza Pharmaceuticals, Palo Alto, CA,1 the American Medical Association,2 American Psychiatric Association Task Force on Benzodiazepine Dependency,1 American Psychiatric Association Task Force on Treatments of Psychiatric Disorders,1 American Psychiatric Association Working Group to Revise DSM III Anxiety Disorders Section,1 Anclote Foundation,2 Anxiety Disorders Resource Center,1 Anxiety Drug Efficacy Case, the FDA,1 Applied Health Outcomes/Xcenda,1 AstraZeneca,1,2,3 Avera Pharmaceuticals,1,2 Boehringer Ingelheim,3 Boots Pharmaceuticals,3 Bristol-Myers Squibb,1,2,3 Burroughs Wellcome,2,3 Cephalon,1 Charter Hospitals,3 Ciba Geigy,3 Committee (RRC) of the National Institute for Mental Health on Anxiety and Phobic Disorder Projects,1 Connecticut and Ohio Academies of Family Physicians,1 Cortex Pharmaceutical,1 Council on Anxiety Disorders,1 CPC Coliseum Medical Center,1 Cypress Bioscience,1 Dista Products Company,3 Division of Drugs and Technology, American Medical Association,1 Eisai,1,2 Eli Lilly and Company,2,3 Excerpta Medica Asia,3 Faxmed, Inc.,1 Forest Laboratories,1,2 Glaxo Pharmaceuticals,3 GlaxoSmithKline,1,2,3 Glaxo-Wellcome,2 Hospital Corporation of America,3 Humana,3 ICI,3 INC Research,1 International Clinical Research (ICR),2 International Society for CNS Drug Development (ISCDD),1 Janssen Pharmaceuticals,1,2,3 Jazz Pharmaceuticals,1,2 Kali-Duphar,2,3 Labopharm,1 Layton Bioscience,1 Lilly Research Laboratories,1 Lundbeck, Denmark,1 Marion Merrell Dow,3 McNeil Pharmaceuticals,3 Mead Johnson,2,3 Medical Outcome Systems,4 MediciNova,1,2 Merck Sharp & Dohme,2,3 National Anxiety Awareness Program,1 National Anxiety Foundation,1 National Depressive and Manic Depressive Association,1 National Institute on Drug Abuse,2 National Institute of Health,2 Neuronetics,1 Novartis Pharmaceuticals Corp.,2 Novo Nordisk,3 Organon,1,3 Orion Pharma,1 Parexel International Corporation,1 Parke-Davis,2,3 Pfizer, Inc.,1,2,3 Pharmacia,1 Pharmacia and Upjohn,1,3 Philadelphia College of Pharmacy and Science,1 Pierre Fabre, France,1 Quintiles,2 Rhone Laboratories,3 Rhone-Poulenc Rorer Pharmaceuticals,3 Roche,1 Roerig,3 Sandoz Pharmaceuticals,2,3 sanofi-aventis,1,2,3 Sanofi-Synthelabo Recherche,1,2 Schering Corporation,3 Sepracor,1 Shire Laboratories, Inc.,1 SmithKline Beecham,1,2,3 Solvay Pharmaceuticals,1,3 Takeda Pharmaceuticals,1 Tampa General Hospital,1 University of South Florida Psychiatry Center,2 University of South Florida College of Medicine, TAP Pharmaceuticals,2,3 Targacept,1 Tampa General Hospital-University Psychiatry Center,3 Tikvah Therapeutics,1 Titan Pharmaceuticals,1 United Bioscience,2 The Upjohn Company,1,2,3 U.S. Congress-House of Representatives Committee,1 University of South Florida Friends of Research in Psychiatry, Board of Trustees,1 Warner Chilcott,2,3 World Health Organization,1 Worldwide Clinical Trials,2 Wyeth-Ayerst,1,2,3 ZARS,1 and Zeneca Pharmaceuticals.1
1: Consultant; 2: Grant/Research Support; 3: Lectures/ Presentations; 4: Stock Holder
1. Oleptro [package insert]. Dublin, Ireland: Labopharm Europe Limited; 2010.
2. Greenblatt DJ, von Moltke LL, Harmatz JS, et al. Short-term exposure to low-dose ritonavir impairs clearance and enhances adverse effects of trazodone. J Clin Pharmacol. 2003;43(4):414-422.
3. Beasley CM, Jr, Dornseif BE, Pultz JA, et al. Fluoxetine versus trazodone: efficacy and activating-sedating effects. J Clin Psychiatry. 1991;52:294-299.
4. Kasper S, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and paroxetine in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2005;21:1139-1146.
5. Munizza C, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and sertraline in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2006;22:1703-1713.
6. Cunningham LA, Borison RL, Carman JS, et al. A comparison of venlafaxine, trazodone, and placebo in major depression. J Clin Pyschopharmacol. 1994;14:99-106.
7. Weisler RH, Johnston JA, Lineberry CG, et al. Comparison of bupropion and trazodone in the treatment of major depression. J Clin Psychopharmacol. 1994;14:170-179.
8. Feighner JP. Trazodone, a triazolopyridine derivative, in primary depressive disorder. J Clin Psychiatry. 1980;41:250-255.
9. Rickels K, Case WG. Trazodone in depressed outpatients. Am J Psychiatry. 1982;139:803-806.
10. Perry PJ, Garvey MJ, Kelly MW, et al. A comparative trial of fluoxetine versus trazodone in outpatients with major depression. J Clin Psychiatry. 1989;50:290-294.
11. Sheehan DV, Croft HA, Gossen ER, et al. Extended-release trazodone in major depressive disorder: a randomized, double-blind, placebo-controlled study. Psychiatry (Edgmont). 2009;6(5):20-33.
12. Sheehan DV, Rozova A, Gossen ER, et al. The efficacy and tolerability of once-daily controlled-release trazodone for depressed mood, anxiety, insomnia, and suicidality in major depressive disorder. Psychopharmacol Bull. 2009;42(4):5-22.
13. Hu XH, Bull SA, Hunkeler EM, et al. Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression: patient report versus physician estimate. J Clin Psychiatry. 2004;65(7):959-965.
14. Landén M, Högberg P, Thase ME. Incidence of sexual side effects in refractory depression during treatment with citalopram or paroxetine. J Clin Psychiatry. 2005;66(1):100-106.
15. Thompson JW, Jr, Ware MR, Blashfield RK. Psychotropic medications and priapism: a comprehensive review. J Clin Psychiatry. 1990;51:430-433.
Extended-release (ER) trazodone—FDA-approved in February 2010—improves symptoms of major depressive disorder (MDD) and allows once-daily dosing (Table 1). Trazodone immediate release (IR) was developed in 1960 and approved by the FDA for treatment of MDD in December 1981. Trazodone IR is now mainly prescribed off-label as a hypnotic at lower-than-antidepressant doses, such as 50 to 100 mg/d at bedtime. The dose needed to achieve antidepressant effect is believed to be ≥300 mg/d. Use of the IR formulation for treating depression has been limited by the need for 3-times-a-day dosing and daytime sedation associated with peaks in serum concentration.
Table 1
Trazodone extended release: Fast facts
| Brand name: Oleptro |
| Class: Triazolopyridine-derived antidepressant |
| Indication: Major depressive disorder |
| Approval date: February 2, 2010 |
| Availability date: August 10, 2010 |
| Manufacturer: Labopharm, Inc. |
| Dosage forms: 150 mg and 300 mg bisectable tablets |
| Starting dose: 150 mg at bedtime |
| Target dose: 300 mg/d; maximum dose 375 mg/d |
Clinical implications
Trazodone ER was designed to eliminate the peaks and troughs in serum concentration seen with trazodone IR. It was hypothesized that by reducing the maximum concentration (Cmax) peaks, trazodone ER would permit higher doses to be better tolerated and help patients to more easily reach target antidepressant doses (≥300 mg/d). Trazodone ER’s once-daily dosing also may increase patient adherence.
How it works
The exact mechanism of action through which trazodone treats depression is not completely understood, but is likely related to enhancing serotonergic activity in the CNS. Trazodone is a triazolopyridine antidepressant, inhibits the serotonin transporter, and is a 5-HT2A and 5-HT2C antagonist. This is why it is sometimes referred as a serotonin antagonist/reuptake inhibitor, but regulatory agencies do not accept this class name. Trazodone is an antagonist at both histamine (H1) and α1-adrenergic receptors, which may mediate trazodone’s sedating properties (H1) and hypotensive (α1-adrenergic) effects.
The ER formulation employs a cross-linked, high-amylose starch excipient that provides controlled release of trazodone over an extended period.
Pharmacokinetics
Trazodone ER has linear pharmacokinetics in doses from 75 to 375 mg. Trazodone ER, 300 mg/d, provides a steady-state exposure equivalent to 100 mg of trazodone IR given 3 times daily, while having a lower Cmax. A high-fat meal can increase Cmax of trazodone ER by 1.9-fold. Trazodone is extensively biotransformed in the liver via the cytochrome P450 (CYP) 3A4 pathway and its metabolites are eliminated within 72 hours. Elimination is predominantly renal, with 70% to 75% of an oral dose being recovered in the urine within 72 hours.1 This formulation maintains its controlled-release properties if bisected.
Because trazodone is a substrate of the CYP3A4 enzyme, its metabolism can be inhibited by CYP3A4 inhibitors. Exercise caution when coadministering medications that cause CYP3A4 inhibition with trazodone ER. The effect of short-term administration of ritonavir (4 doses of 200 mg) on the pharmacokinetics of a single dose of trazodone (50 mg) has been studied in 10 healthy subjects.2 The Cmax of trazodone increased by 34%, area under the curve increased 2.4-fold, half-life increased by 2.2-fold, and clearance decreased by 52%. There is no difference in the half-life between the IR and ER formulations because the ER formulation influences only the release kinetics of the drug, not the half-life of the medication.
Efficacy
Efficacy of trazodone for MDD initially was established in trials conducted with trazodone IR.3-10 The efficacy of the ER formulation was established in a multi-center randomized, double-blind, placebo-controlled trial with 412 patients (age 18 to 80). Patients who met DSM-IV criteria for MDD were randomly assigned to trazodone ER (n=206) or placebo (n=206) for 8 weeks.11 This study showed a statistically significant difference between trazodone ER and placebo after 8 weeks of treatment on the primary outcome measure, which was a change in score on the 17-item Hamilton Depression Rating scale (HAMD-17). HAM-D-17 scores decreased 11.4 points in the trazodone ER group and 9.3 points in the placebo group (P=.012 in the modified intent to treat [ITT] population; P=.009 in the completer analysis). This difference was seen from week 1 and throughout the study. Efficacy of trazodone ER was further supported by statistically significant differences between the drug and placebo in 7 of 13 secondary efficacy endpoints in both the modified ITT and per protocol (PP) populations (HAM-D-17 mood item, mean Montgomery-Åsberg Depression Rating Scale [MADRS] total score, mean Clinical Global Impressions Severity of Illness [CGI-S] score, percentage of HAM-D-17 responders, and 3 quality of sleep items [overall quality of sleep, trouble falling asleep, and awakening during the night]). Overall effect sizes for the HAM-D-17 were -0.26 (modified ITT-last observation carried forward [LOCF] dataset) and -0.33 (PP/observed cases [OC] dataset). The effect sizes in MADRS scores were -0.22 and -0.29 for the modified ITT-LOCF and the PP/OC analyses, respectively.12
Sleep measures. In the study sample >90% of patients had insomnia at baseline (defined as a score ≥2 in any HAM-D-17 sleep item or sum of all 3 sleep items of ≥4). Patients receiving trazodone ER had significant improvement in all 3 HAM-D-17 sleep items. Subjects reported improvement in the overall quality of sleep and awakening during the night after the first week of treatment. Investigators found no significant interaction between improvements in core symptoms of depression and baseline MADRS reduced sleep item or early changes in the HAM-D-17 sleep items. This suggests that the antidepressant effect of trazodone ER was independent of severity of sleep difficulties at baseline and of improvement in insomnia during the study.12
Researchers observed improvement in suicidal ideation on MADRS (item 10) and HAM-D-17 (item 3) after 8 weeks of treatment (effect size -0.2 favoring trazodone ER over placebo).12
In 2 European comparative, randomized, double-blind trials, trazodone prolonged release showed similar antidepressant efficacy as paroxetine4 and setraline5 as measured by HAM-D, MADRS, and CGI-S. This prolonged release formulation made in Europe is not the same technology as the ER formulation recently approved by the FDA.
Tolerability
In the pivotal registration study, trazodone ER was well tolerated at a mean dose of 310 mg/d.11 Twenty-five patients (12.4%) in the trazodone ER group discontinued the drug because of side effects. The most common side effects leading to discontinuation in the active treatment group were dizziness (n=7), sedation (n=5), and somnolence (n=3).11 The most frequent adverse events reported at any study time point were headache (33%), somnolence (31%), dry mouth (25%), dizziness (25%), nausea (21%), sedation (17%), and fatigue (15%) (Table 2).11 In general, these adverse events were mild to moderate and short-lived; most side effects resolved within the first 2 to 3 weeks of treatment with trazodone ER.11
Sexual side effects—delayed ejaculation, delayed time to orgasm, or orgasmic blockade—are common with many anti-depressants. In the pivotal registration study, the incidence of sexual side effects was low (4.9% with trazodone ER vs 2.5% with placebo).11 This is much lower than the rates typically found with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, which range from 17% to 41%.13,14 This benefit is thought to be mediated through 5-HT2A and 5-HT2C antagonism. Priapism has been reported in trazodone IR at rates ranging from 1 in 1,000 to 1 in 10,000 and does not appear to be dose-related.15 The rate of priapism in persons using agents for erectile dysfunction ranges from .05% to 6%.15 No case of priapism was seen in the trazodone ER study; however, with its sample size of 412 patients this study was not powered to adequately detect this adverse event.11
There was no significant weight gain difference between the active drug and placebo groups over 8 weeks of treatment.
Safety. Trazodone ER should not be used within 14 days of taking a monoamine oxidase inhibitor.1 Trazodone carries a pregnancy category C, meaning that it should be used only if the potential benefit justifies potential risk to the fetus. In animal studies, trazodone has been shown to cause increased fetal resorption and congenital anomalities with doses up to 50 times the maximum human dose (375 mg/d). Trazo-done may be secreted in breast milk. The drug is best avoided in patients with recent myocardial infarction.
Table 2
Trazodone extended release treatment-emergent adverse events*
| Trazodone ER (n=202) | Placebo (n=204) | |
|---|---|---|
| Headache | 67 (33%) | 55 (27%) |
| Somnolence | 63 (31%) | 32 (16%) |
| Dry mouth | 51 (25%) | 26 (13%) |
| Dizziness | 50 (25%) | 25 (12%) |
| Nausea | 42 (21%) | 26 (13%) |
| Sedation | 34 (17%) | 7 (3%) |
| Fatigue | 30 (15%) | 17 (8%) |
| Diarrhea | 19 (9%) | 23 (11%) |
| Constipation | 16 (8%) | 4 (2%) |
| Back pain | 11 (5%) | 7 (3%) |
| Blurred vision | 11 (5%) | 0 (0%) |
| *Reported by ≥5% of patients Source: Reference 11 | ||
Dosing
The recommended starting dose is 150 mg/d at bedtime. The dose may be increased by 75 mg/d every 3 days, but the maximum dose should not exceed 375 mg/d.1 Trazodone ER is available in 150 mg or 300 mg bisectable tablets. Breaking the tablets in half does not affect the controlled release, but they should not be chewed or crushed.
Related Resource
- Extended-release trazodone (Oleptro) prescribing information. www.oleptro.com/images/9379.pdf.
Drug Brand Names
- Paroxetine • Paxil
- Ritonavir • Norvir
- Sertraline • Zoloft
- Trazodone • Desyrel
- Trazodone extended-release • Oleptro
Disclosures
Dr. Hidalgo receives grant/research support from AstraZeneca, CeNeRx Biopharma, Centers for Disease Control and Prevention, Dainippon Sumitomo Pharma America, Inc., Eli Lilly and Company, Forest Laboratories, Indevus Pharmaceuticals, Janssen Pharmaceuticals, Labopharm, Otsuka, Pfizer, Inc., Repligen Corp., Sanofi-Synthelabo, Sepracor, and the University of South Florida, and is consultant to the MAPI Institute.
Dr. Sheehan has received grant funding support from, been affiliated with, or received honoraria and travel expenses related to lectures/presentations or consultant activities from the following organizations: Abbott Laboratories,1,2,3 Ad Hoc Committee, Treatment Drug and Assessment Research Review,1 Alexza,1 Alza Pharmaceuticals, Palo Alto, CA,1 the American Medical Association,2 American Psychiatric Association Task Force on Benzodiazepine Dependency,1 American Psychiatric Association Task Force on Treatments of Psychiatric Disorders,1 American Psychiatric Association Working Group to Revise DSM III Anxiety Disorders Section,1 Anclote Foundation,2 Anxiety Disorders Resource Center,1 Anxiety Drug Efficacy Case, the FDA,1 Applied Health Outcomes/Xcenda,1 AstraZeneca,1,2,3 Avera Pharmaceuticals,1,2 Boehringer Ingelheim,3 Boots Pharmaceuticals,3 Bristol-Myers Squibb,1,2,3 Burroughs Wellcome,2,3 Cephalon,1 Charter Hospitals,3 Ciba Geigy,3 Committee (RRC) of the National Institute for Mental Health on Anxiety and Phobic Disorder Projects,1 Connecticut and Ohio Academies of Family Physicians,1 Cortex Pharmaceutical,1 Council on Anxiety Disorders,1 CPC Coliseum Medical Center,1 Cypress Bioscience,1 Dista Products Company,3 Division of Drugs and Technology, American Medical Association,1 Eisai,1,2 Eli Lilly and Company,2,3 Excerpta Medica Asia,3 Faxmed, Inc.,1 Forest Laboratories,1,2 Glaxo Pharmaceuticals,3 GlaxoSmithKline,1,2,3 Glaxo-Wellcome,2 Hospital Corporation of America,3 Humana,3 ICI,3 INC Research,1 International Clinical Research (ICR),2 International Society for CNS Drug Development (ISCDD),1 Janssen Pharmaceuticals,1,2,3 Jazz Pharmaceuticals,1,2 Kali-Duphar,2,3 Labopharm,1 Layton Bioscience,1 Lilly Research Laboratories,1 Lundbeck, Denmark,1 Marion Merrell Dow,3 McNeil Pharmaceuticals,3 Mead Johnson,2,3 Medical Outcome Systems,4 MediciNova,1,2 Merck Sharp & Dohme,2,3 National Anxiety Awareness Program,1 National Anxiety Foundation,1 National Depressive and Manic Depressive Association,1 National Institute on Drug Abuse,2 National Institute of Health,2 Neuronetics,1 Novartis Pharmaceuticals Corp.,2 Novo Nordisk,3 Organon,1,3 Orion Pharma,1 Parexel International Corporation,1 Parke-Davis,2,3 Pfizer, Inc.,1,2,3 Pharmacia,1 Pharmacia and Upjohn,1,3 Philadelphia College of Pharmacy and Science,1 Pierre Fabre, France,1 Quintiles,2 Rhone Laboratories,3 Rhone-Poulenc Rorer Pharmaceuticals,3 Roche,1 Roerig,3 Sandoz Pharmaceuticals,2,3 sanofi-aventis,1,2,3 Sanofi-Synthelabo Recherche,1,2 Schering Corporation,3 Sepracor,1 Shire Laboratories, Inc.,1 SmithKline Beecham,1,2,3 Solvay Pharmaceuticals,1,3 Takeda Pharmaceuticals,1 Tampa General Hospital,1 University of South Florida Psychiatry Center,2 University of South Florida College of Medicine, TAP Pharmaceuticals,2,3 Targacept,1 Tampa General Hospital-University Psychiatry Center,3 Tikvah Therapeutics,1 Titan Pharmaceuticals,1 United Bioscience,2 The Upjohn Company,1,2,3 U.S. Congress-House of Representatives Committee,1 University of South Florida Friends of Research in Psychiatry, Board of Trustees,1 Warner Chilcott,2,3 World Health Organization,1 Worldwide Clinical Trials,2 Wyeth-Ayerst,1,2,3 ZARS,1 and Zeneca Pharmaceuticals.1
1: Consultant; 2: Grant/Research Support; 3: Lectures/ Presentations; 4: Stock Holder
Extended-release (ER) trazodone—FDA-approved in February 2010—improves symptoms of major depressive disorder (MDD) and allows once-daily dosing (Table 1). Trazodone immediate release (IR) was developed in 1960 and approved by the FDA for treatment of MDD in December 1981. Trazodone IR is now mainly prescribed off-label as a hypnotic at lower-than-antidepressant doses, such as 50 to 100 mg/d at bedtime. The dose needed to achieve antidepressant effect is believed to be ≥300 mg/d. Use of the IR formulation for treating depression has been limited by the need for 3-times-a-day dosing and daytime sedation associated with peaks in serum concentration.
Table 1
Trazodone extended release: Fast facts
| Brand name: Oleptro |
| Class: Triazolopyridine-derived antidepressant |
| Indication: Major depressive disorder |
| Approval date: February 2, 2010 |
| Availability date: August 10, 2010 |
| Manufacturer: Labopharm, Inc. |
| Dosage forms: 150 mg and 300 mg bisectable tablets |
| Starting dose: 150 mg at bedtime |
| Target dose: 300 mg/d; maximum dose 375 mg/d |
Clinical implications
Trazodone ER was designed to eliminate the peaks and troughs in serum concentration seen with trazodone IR. It was hypothesized that by reducing the maximum concentration (Cmax) peaks, trazodone ER would permit higher doses to be better tolerated and help patients to more easily reach target antidepressant doses (≥300 mg/d). Trazodone ER’s once-daily dosing also may increase patient adherence.
How it works
The exact mechanism of action through which trazodone treats depression is not completely understood, but is likely related to enhancing serotonergic activity in the CNS. Trazodone is a triazolopyridine antidepressant, inhibits the serotonin transporter, and is a 5-HT2A and 5-HT2C antagonist. This is why it is sometimes referred as a serotonin antagonist/reuptake inhibitor, but regulatory agencies do not accept this class name. Trazodone is an antagonist at both histamine (H1) and α1-adrenergic receptors, which may mediate trazodone’s sedating properties (H1) and hypotensive (α1-adrenergic) effects.
The ER formulation employs a cross-linked, high-amylose starch excipient that provides controlled release of trazodone over an extended period.
Pharmacokinetics
Trazodone ER has linear pharmacokinetics in doses from 75 to 375 mg. Trazodone ER, 300 mg/d, provides a steady-state exposure equivalent to 100 mg of trazodone IR given 3 times daily, while having a lower Cmax. A high-fat meal can increase Cmax of trazodone ER by 1.9-fold. Trazodone is extensively biotransformed in the liver via the cytochrome P450 (CYP) 3A4 pathway and its metabolites are eliminated within 72 hours. Elimination is predominantly renal, with 70% to 75% of an oral dose being recovered in the urine within 72 hours.1 This formulation maintains its controlled-release properties if bisected.
Because trazodone is a substrate of the CYP3A4 enzyme, its metabolism can be inhibited by CYP3A4 inhibitors. Exercise caution when coadministering medications that cause CYP3A4 inhibition with trazodone ER. The effect of short-term administration of ritonavir (4 doses of 200 mg) on the pharmacokinetics of a single dose of trazodone (50 mg) has been studied in 10 healthy subjects.2 The Cmax of trazodone increased by 34%, area under the curve increased 2.4-fold, half-life increased by 2.2-fold, and clearance decreased by 52%. There is no difference in the half-life between the IR and ER formulations because the ER formulation influences only the release kinetics of the drug, not the half-life of the medication.
Efficacy
Efficacy of trazodone for MDD initially was established in trials conducted with trazodone IR.3-10 The efficacy of the ER formulation was established in a multi-center randomized, double-blind, placebo-controlled trial with 412 patients (age 18 to 80). Patients who met DSM-IV criteria for MDD were randomly assigned to trazodone ER (n=206) or placebo (n=206) for 8 weeks.11 This study showed a statistically significant difference between trazodone ER and placebo after 8 weeks of treatment on the primary outcome measure, which was a change in score on the 17-item Hamilton Depression Rating scale (HAMD-17). HAM-D-17 scores decreased 11.4 points in the trazodone ER group and 9.3 points in the placebo group (P=.012 in the modified intent to treat [ITT] population; P=.009 in the completer analysis). This difference was seen from week 1 and throughout the study. Efficacy of trazodone ER was further supported by statistically significant differences between the drug and placebo in 7 of 13 secondary efficacy endpoints in both the modified ITT and per protocol (PP) populations (HAM-D-17 mood item, mean Montgomery-Åsberg Depression Rating Scale [MADRS] total score, mean Clinical Global Impressions Severity of Illness [CGI-S] score, percentage of HAM-D-17 responders, and 3 quality of sleep items [overall quality of sleep, trouble falling asleep, and awakening during the night]). Overall effect sizes for the HAM-D-17 were -0.26 (modified ITT-last observation carried forward [LOCF] dataset) and -0.33 (PP/observed cases [OC] dataset). The effect sizes in MADRS scores were -0.22 and -0.29 for the modified ITT-LOCF and the PP/OC analyses, respectively.12
Sleep measures. In the study sample >90% of patients had insomnia at baseline (defined as a score ≥2 in any HAM-D-17 sleep item or sum of all 3 sleep items of ≥4). Patients receiving trazodone ER had significant improvement in all 3 HAM-D-17 sleep items. Subjects reported improvement in the overall quality of sleep and awakening during the night after the first week of treatment. Investigators found no significant interaction between improvements in core symptoms of depression and baseline MADRS reduced sleep item or early changes in the HAM-D-17 sleep items. This suggests that the antidepressant effect of trazodone ER was independent of severity of sleep difficulties at baseline and of improvement in insomnia during the study.12
Researchers observed improvement in suicidal ideation on MADRS (item 10) and HAM-D-17 (item 3) after 8 weeks of treatment (effect size -0.2 favoring trazodone ER over placebo).12
In 2 European comparative, randomized, double-blind trials, trazodone prolonged release showed similar antidepressant efficacy as paroxetine4 and setraline5 as measured by HAM-D, MADRS, and CGI-S. This prolonged release formulation made in Europe is not the same technology as the ER formulation recently approved by the FDA.
Tolerability
In the pivotal registration study, trazodone ER was well tolerated at a mean dose of 310 mg/d.11 Twenty-five patients (12.4%) in the trazodone ER group discontinued the drug because of side effects. The most common side effects leading to discontinuation in the active treatment group were dizziness (n=7), sedation (n=5), and somnolence (n=3).11 The most frequent adverse events reported at any study time point were headache (33%), somnolence (31%), dry mouth (25%), dizziness (25%), nausea (21%), sedation (17%), and fatigue (15%) (Table 2).11 In general, these adverse events were mild to moderate and short-lived; most side effects resolved within the first 2 to 3 weeks of treatment with trazodone ER.11
Sexual side effects—delayed ejaculation, delayed time to orgasm, or orgasmic blockade—are common with many anti-depressants. In the pivotal registration study, the incidence of sexual side effects was low (4.9% with trazodone ER vs 2.5% with placebo).11 This is much lower than the rates typically found with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, which range from 17% to 41%.13,14 This benefit is thought to be mediated through 5-HT2A and 5-HT2C antagonism. Priapism has been reported in trazodone IR at rates ranging from 1 in 1,000 to 1 in 10,000 and does not appear to be dose-related.15 The rate of priapism in persons using agents for erectile dysfunction ranges from .05% to 6%.15 No case of priapism was seen in the trazodone ER study; however, with its sample size of 412 patients this study was not powered to adequately detect this adverse event.11
There was no significant weight gain difference between the active drug and placebo groups over 8 weeks of treatment.
Safety. Trazodone ER should not be used within 14 days of taking a monoamine oxidase inhibitor.1 Trazodone carries a pregnancy category C, meaning that it should be used only if the potential benefit justifies potential risk to the fetus. In animal studies, trazodone has been shown to cause increased fetal resorption and congenital anomalities with doses up to 50 times the maximum human dose (375 mg/d). Trazo-done may be secreted in breast milk. The drug is best avoided in patients with recent myocardial infarction.
Table 2
Trazodone extended release treatment-emergent adverse events*
| Trazodone ER (n=202) | Placebo (n=204) | |
|---|---|---|
| Headache | 67 (33%) | 55 (27%) |
| Somnolence | 63 (31%) | 32 (16%) |
| Dry mouth | 51 (25%) | 26 (13%) |
| Dizziness | 50 (25%) | 25 (12%) |
| Nausea | 42 (21%) | 26 (13%) |
| Sedation | 34 (17%) | 7 (3%) |
| Fatigue | 30 (15%) | 17 (8%) |
| Diarrhea | 19 (9%) | 23 (11%) |
| Constipation | 16 (8%) | 4 (2%) |
| Back pain | 11 (5%) | 7 (3%) |
| Blurred vision | 11 (5%) | 0 (0%) |
| *Reported by ≥5% of patients Source: Reference 11 | ||
Dosing
The recommended starting dose is 150 mg/d at bedtime. The dose may be increased by 75 mg/d every 3 days, but the maximum dose should not exceed 375 mg/d.1 Trazodone ER is available in 150 mg or 300 mg bisectable tablets. Breaking the tablets in half does not affect the controlled release, but they should not be chewed or crushed.
Related Resource
- Extended-release trazodone (Oleptro) prescribing information. www.oleptro.com/images/9379.pdf.
Drug Brand Names
- Paroxetine • Paxil
- Ritonavir • Norvir
- Sertraline • Zoloft
- Trazodone • Desyrel
- Trazodone extended-release • Oleptro
Disclosures
Dr. Hidalgo receives grant/research support from AstraZeneca, CeNeRx Biopharma, Centers for Disease Control and Prevention, Dainippon Sumitomo Pharma America, Inc., Eli Lilly and Company, Forest Laboratories, Indevus Pharmaceuticals, Janssen Pharmaceuticals, Labopharm, Otsuka, Pfizer, Inc., Repligen Corp., Sanofi-Synthelabo, Sepracor, and the University of South Florida, and is consultant to the MAPI Institute.
Dr. Sheehan has received grant funding support from, been affiliated with, or received honoraria and travel expenses related to lectures/presentations or consultant activities from the following organizations: Abbott Laboratories,1,2,3 Ad Hoc Committee, Treatment Drug and Assessment Research Review,1 Alexza,1 Alza Pharmaceuticals, Palo Alto, CA,1 the American Medical Association,2 American Psychiatric Association Task Force on Benzodiazepine Dependency,1 American Psychiatric Association Task Force on Treatments of Psychiatric Disorders,1 American Psychiatric Association Working Group to Revise DSM III Anxiety Disorders Section,1 Anclote Foundation,2 Anxiety Disorders Resource Center,1 Anxiety Drug Efficacy Case, the FDA,1 Applied Health Outcomes/Xcenda,1 AstraZeneca,1,2,3 Avera Pharmaceuticals,1,2 Boehringer Ingelheim,3 Boots Pharmaceuticals,3 Bristol-Myers Squibb,1,2,3 Burroughs Wellcome,2,3 Cephalon,1 Charter Hospitals,3 Ciba Geigy,3 Committee (RRC) of the National Institute for Mental Health on Anxiety and Phobic Disorder Projects,1 Connecticut and Ohio Academies of Family Physicians,1 Cortex Pharmaceutical,1 Council on Anxiety Disorders,1 CPC Coliseum Medical Center,1 Cypress Bioscience,1 Dista Products Company,3 Division of Drugs and Technology, American Medical Association,1 Eisai,1,2 Eli Lilly and Company,2,3 Excerpta Medica Asia,3 Faxmed, Inc.,1 Forest Laboratories,1,2 Glaxo Pharmaceuticals,3 GlaxoSmithKline,1,2,3 Glaxo-Wellcome,2 Hospital Corporation of America,3 Humana,3 ICI,3 INC Research,1 International Clinical Research (ICR),2 International Society for CNS Drug Development (ISCDD),1 Janssen Pharmaceuticals,1,2,3 Jazz Pharmaceuticals,1,2 Kali-Duphar,2,3 Labopharm,1 Layton Bioscience,1 Lilly Research Laboratories,1 Lundbeck, Denmark,1 Marion Merrell Dow,3 McNeil Pharmaceuticals,3 Mead Johnson,2,3 Medical Outcome Systems,4 MediciNova,1,2 Merck Sharp & Dohme,2,3 National Anxiety Awareness Program,1 National Anxiety Foundation,1 National Depressive and Manic Depressive Association,1 National Institute on Drug Abuse,2 National Institute of Health,2 Neuronetics,1 Novartis Pharmaceuticals Corp.,2 Novo Nordisk,3 Organon,1,3 Orion Pharma,1 Parexel International Corporation,1 Parke-Davis,2,3 Pfizer, Inc.,1,2,3 Pharmacia,1 Pharmacia and Upjohn,1,3 Philadelphia College of Pharmacy and Science,1 Pierre Fabre, France,1 Quintiles,2 Rhone Laboratories,3 Rhone-Poulenc Rorer Pharmaceuticals,3 Roche,1 Roerig,3 Sandoz Pharmaceuticals,2,3 sanofi-aventis,1,2,3 Sanofi-Synthelabo Recherche,1,2 Schering Corporation,3 Sepracor,1 Shire Laboratories, Inc.,1 SmithKline Beecham,1,2,3 Solvay Pharmaceuticals,1,3 Takeda Pharmaceuticals,1 Tampa General Hospital,1 University of South Florida Psychiatry Center,2 University of South Florida College of Medicine, TAP Pharmaceuticals,2,3 Targacept,1 Tampa General Hospital-University Psychiatry Center,3 Tikvah Therapeutics,1 Titan Pharmaceuticals,1 United Bioscience,2 The Upjohn Company,1,2,3 U.S. Congress-House of Representatives Committee,1 University of South Florida Friends of Research in Psychiatry, Board of Trustees,1 Warner Chilcott,2,3 World Health Organization,1 Worldwide Clinical Trials,2 Wyeth-Ayerst,1,2,3 ZARS,1 and Zeneca Pharmaceuticals.1
1: Consultant; 2: Grant/Research Support; 3: Lectures/ Presentations; 4: Stock Holder
1. Oleptro [package insert]. Dublin, Ireland: Labopharm Europe Limited; 2010.
2. Greenblatt DJ, von Moltke LL, Harmatz JS, et al. Short-term exposure to low-dose ritonavir impairs clearance and enhances adverse effects of trazodone. J Clin Pharmacol. 2003;43(4):414-422.
3. Beasley CM, Jr, Dornseif BE, Pultz JA, et al. Fluoxetine versus trazodone: efficacy and activating-sedating effects. J Clin Psychiatry. 1991;52:294-299.
4. Kasper S, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and paroxetine in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2005;21:1139-1146.
5. Munizza C, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and sertraline in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2006;22:1703-1713.
6. Cunningham LA, Borison RL, Carman JS, et al. A comparison of venlafaxine, trazodone, and placebo in major depression. J Clin Pyschopharmacol. 1994;14:99-106.
7. Weisler RH, Johnston JA, Lineberry CG, et al. Comparison of bupropion and trazodone in the treatment of major depression. J Clin Psychopharmacol. 1994;14:170-179.
8. Feighner JP. Trazodone, a triazolopyridine derivative, in primary depressive disorder. J Clin Psychiatry. 1980;41:250-255.
9. Rickels K, Case WG. Trazodone in depressed outpatients. Am J Psychiatry. 1982;139:803-806.
10. Perry PJ, Garvey MJ, Kelly MW, et al. A comparative trial of fluoxetine versus trazodone in outpatients with major depression. J Clin Psychiatry. 1989;50:290-294.
11. Sheehan DV, Croft HA, Gossen ER, et al. Extended-release trazodone in major depressive disorder: a randomized, double-blind, placebo-controlled study. Psychiatry (Edgmont). 2009;6(5):20-33.
12. Sheehan DV, Rozova A, Gossen ER, et al. The efficacy and tolerability of once-daily controlled-release trazodone for depressed mood, anxiety, insomnia, and suicidality in major depressive disorder. Psychopharmacol Bull. 2009;42(4):5-22.
13. Hu XH, Bull SA, Hunkeler EM, et al. Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression: patient report versus physician estimate. J Clin Psychiatry. 2004;65(7):959-965.
14. Landén M, Högberg P, Thase ME. Incidence of sexual side effects in refractory depression during treatment with citalopram or paroxetine. J Clin Psychiatry. 2005;66(1):100-106.
15. Thompson JW, Jr, Ware MR, Blashfield RK. Psychotropic medications and priapism: a comprehensive review. J Clin Psychiatry. 1990;51:430-433.
1. Oleptro [package insert]. Dublin, Ireland: Labopharm Europe Limited; 2010.
2. Greenblatt DJ, von Moltke LL, Harmatz JS, et al. Short-term exposure to low-dose ritonavir impairs clearance and enhances adverse effects of trazodone. J Clin Pharmacol. 2003;43(4):414-422.
3. Beasley CM, Jr, Dornseif BE, Pultz JA, et al. Fluoxetine versus trazodone: efficacy and activating-sedating effects. J Clin Psychiatry. 1991;52:294-299.
4. Kasper S, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and paroxetine in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2005;21:1139-1146.
5. Munizza C, Olivieri L, Di Loreto G, et al. A comparative, randomized double blind study of trazodone prolonged-release and sertraline in the treatment of patients with major depressive disorder. Curr Med Res Opin. 2006;22:1703-1713.
6. Cunningham LA, Borison RL, Carman JS, et al. A comparison of venlafaxine, trazodone, and placebo in major depression. J Clin Pyschopharmacol. 1994;14:99-106.
7. Weisler RH, Johnston JA, Lineberry CG, et al. Comparison of bupropion and trazodone in the treatment of major depression. J Clin Psychopharmacol. 1994;14:170-179.
8. Feighner JP. Trazodone, a triazolopyridine derivative, in primary depressive disorder. J Clin Psychiatry. 1980;41:250-255.
9. Rickels K, Case WG. Trazodone in depressed outpatients. Am J Psychiatry. 1982;139:803-806.
10. Perry PJ, Garvey MJ, Kelly MW, et al. A comparative trial of fluoxetine versus trazodone in outpatients with major depression. J Clin Psychiatry. 1989;50:290-294.
11. Sheehan DV, Croft HA, Gossen ER, et al. Extended-release trazodone in major depressive disorder: a randomized, double-blind, placebo-controlled study. Psychiatry (Edgmont). 2009;6(5):20-33.
12. Sheehan DV, Rozova A, Gossen ER, et al. The efficacy and tolerability of once-daily controlled-release trazodone for depressed mood, anxiety, insomnia, and suicidality in major depressive disorder. Psychopharmacol Bull. 2009;42(4):5-22.
13. Hu XH, Bull SA, Hunkeler EM, et al. Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression: patient report versus physician estimate. J Clin Psychiatry. 2004;65(7):959-965.
14. Landén M, Högberg P, Thase ME. Incidence of sexual side effects in refractory depression during treatment with citalopram or paroxetine. J Clin Psychiatry. 2005;66(1):100-106.
15. Thompson JW, Jr, Ware MR, Blashfield RK. Psychotropic medications and priapism: a comprehensive review. J Clin Psychiatry. 1990;51:430-433.
Doxepin for insomnia
Low-dose doxepin—3 mg and 6 mg—has demonstrated efficacy for insomnia characterized by frequent or early-morning awakenings and an inability to return to sleep (Table 1).1 FDA-approved in March 2010, doxepin (3 mg and 6 mg) is only the second insomnia medication not designated as a controlled substance and thus may be of special value in patients with a history of substance abuse.
Table 1
Doxepin: Fast facts
| Brand name: Silenor |
| Indication: Insomnia characterized by difficulty with sleep maintenance |
| Approval date: March 2010 |
| Availability date: September 7, 2010 |
| Manufacturer: Somaxon Pharmaceuticals |
| Dosage forms: 3 mg and 6 mg tablets |
| Recommended dosage: 3 mg or 6 mg once daily within 30 minutes of bedtime |
Clinical implications
Ramelteon, the other hypnotic that is not a controlled substance, is indicated for sleep initiation insomnia (ie, inability to fall asleep). In contrast, low-dose doxepin is for patients with sleep maintenance insomnia, which is waking up frequently or early in the morning and not falling back asleep.1,2 A tricyclic antidepressant first approved in 1969, doxepin has long been available in larger doses (10-, 25-, 50-, 75-, 100-, and 150-mg capsules) to treat depression and anxiety and as a topical preparation (5% cream) for pruritus, but not in dosages <10 mg. An inexpensive generic doxepin oral solution (10 mg/ml) is available and can be titrated to smaller dosages by a dropper. Liquid doxepin costs 10 to 20 cents per dose. A pharmacist can provide a dropper, and patients should mix the medication in 4 ounces of water, milk, or juice; 0.3 ml of liquid doxepin contains 3 mg of active ingredient and 0.6 ml of solution contains 6 mg of doxepin. These other dosage forms of doxepin, however, are not FDA-approved for insomnia. (The retail price of low-dose doxepin was not available when this article went to press.)
How it works
Doxepin’s mechanism of action for treating depression and insomnia remains unknown. The antidepressant effect of doxepin is thought to result from inhibition of serotonin and norepinephrine reuptake at the synaptic cleft. Animal studies have shown anticholinergic and antihistaminergic activity with doxepin.2 Doxepin is a potent histamine antagonist—predominantly at the H1 receptor—and its binding potency to the H1 receptor is approximately 100-times higher than its binding potency for monoamine transporters (serotonin and norepinephrine).2,3 Brain histamine is believed to be 1 of the key elements in maintaining wakefulness, and the activation of the H1 receptor is thought to play an important role in mediating arousal. Blockade of the H1 receptor by doxepin likely plays a role in reducing wakefulness. Typically, therapeutic doses of antidepressants with anti-histaminergic properties, such as doxepin at antidepressant doses, amitriptyline, or desipramine, do not selectively block H1 receptors, but act at cholinergic, serotonergic, adrenergic, histaminergic, and muscarinic receptors, which can cause adverse effects.3 However, low doses of doxepin (1, 3, and 6 mg) can achieve selective H1 blockade.4,5 Patients taking >25 mg/d of doxepin may report clinically significant anticholinergic effects.
Pharmacokinetics
When doxepin, 6 mg, was administered to healthy, fasting patients, time to maximum concentration (Tmax) was 3.5 hours. Peak plasma concentration (Cmax) increased in a dose-related fashion when doxepin was increased from 3 mg to 6 mg. Doxepin, 6 mg, taken with a high-fat meal resulted in area under the curve increase of 41%, Cmax increase of 15%, and almost 3-hour delay in Tmax. Therefore, to prevent a delay in onset of action and to minimize the likelihood of daytime sedation, doxepin should not be taken within 3 hours of a meal.1-3
Doxepin is metabolized primarily by the liver’s cytochrome P450 (CYP) 2C19 and CYP2D6 enzymes; CYP1A2 and CYP2D6 are involved to a lesser extent. If doxepin is coadministered with drugs that inhibit these isoenzymes, such as fluoxetine and paroxetine, doxepin blood levels may increase. Doxepin does not seem to induce CYP isoenzymes. This medication is metabolized by demethylation and oxidation; the primary metabolite is nordoxepin (N-desmethyldoxepin), which later undergoes glucuronide conjugation. The half-life is 15 hours for doxepin and 31 hours for nordoxepin. Doxepin is excreted in urine primarily as glucuronide conjugate.1-3
Coadministration with cimetidine, an inhibitor of CYP isoenzymes, could double the doxepin plasma concentration; therefore, patients taking cimetidine should not exceed 3 mg/d of doxepin.
Efficacy
Doxepin reduced insomnia symptoms in 3 pilot studies at doses of 10, 25, and 50 mg, and in 2 phase III randomized, double-blind, placebo-controlled clinical trials using 1, 3, and 6 mg (Table 2).4,5 Clinical studies lasted up to 3 months.1-3,6-8
In the first phase III trial, 67 patients, age 18 to 64 with chronic primary insomnia, were randomly assigned to placebo or 1 mg, 3 mg, or 6 mg of doxepin for 2 nights. All patients received all treatments, and each treatment was followed by 8 hours of polysomnography (PSG) evaluation in a sleep laboratory.4 In this study, patients taking doxepin at all doses achieved improvement in objective (PSG-defined) and subjective (patient-reported) measures of sleep duration and sleep maintenance. Wake after sleep onset (WASO), total sleep time (TST), and sleep efficiency (SE) improved with all doxepin doses, and wake time during sleep (WTDS)—which was the primary study endpoint—decreased with 3 mg and 6 mg doses, but not with 1 mg or placebo. In addition, PSG indicators of early-morning awakenings (terminal insomnia) were reduced, as shown by an increase in SE during the final third of the night and the 7th and 8th hours of sleep (1, 3, and 6 mg doses) and a reduction in wake time after sleep (WTAS) during the final third of the night (6 mg only). The effects on sleep duration and maintenance were more robust with 3 mg and 6 mg doses. Improved sleep onset was seen only with the 6 mg dose. Next-day alertness was assessed using the Visual Analogue Scale (VAS) for sleepiness, and the Digit-Symbol Substitution Test (DSST) and the Symbol-Copying Task (SCT) for psychomotor function. No statistically significant differences were found among placebo and any of the doxepin doses on the VAS, DSST, or SCT.
Doxepin was well tolerated. Reported adverse events were mild or moderate. Headaches and somnolence were reported by >2% of patients. The incidence of adverse events, including next-day sedation, was similar to that of placebo. Additionally, there were no spontaneous reports of anticholinergic side effects, which are associated with higher doxepin doses.4
The second phase III trial examined safety and efficacy of 1, 3, and 6 mg doxepin in patients age ≥65.5 Seventy-six adults with primary insomnia were randomly assigned to receive placebo or doxepin for 2 nights; all patients received all treatments, and each treatment was followed by an 8-hour PSG. Patients taking any doxepin dose achieved objective and subjective improvement in sleep duration and sleep maintenance, which lasted into the final hours of the night. WTDS (primary study endpoint), WASO, TST, and overall SE improved at all doxepin doses compared with placebo, and WTAS and SE at hours 7 and 8 improved at doxepin doses of 3 mg and 6 mg compared with placebo. These findings suggest that doxepin, 3 mg and 6 mg, can help older insomnia patients with early morning awakenings.
In this study, no statistically significant differences were found among placebo and any doxepin doses on VAS, DSST, or SCT or next-day residual sedation. The incidence of side effects was low and similar to that of placebo. Adverse events were mild or moderate; 1 incident of chest pain was reported, but it was determined not to be of cardiac origin and not related to study drug. There were no spontaneous reports of anticholinergic side effects associated with higher doses of doxepin. There were no reports of memory impairment.5
Table 2
Evidence of effectiveness of doxepin for insomnia
| Study | Subjects | Dosages | Results |
|---|---|---|---|
| Roth et al, 20074; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 67 patients age 18 to 64 with chronic primary insomnia | 1, 3, or 6 mg given once daily at bedtime for 2 nights | Improvement vs placebo in PSG-defined WASO, TST, SE, and SE during the final third of the night. 6-mg dose significantly reduced subjective latency to sleep onset. Safety profile of all 3 doses was comparable to placebo. No difference in residual sedation |
| Scharf et al, 20085; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 76 patients age ≥65 with primary insomnia | 1, 3, or 6 mg at bedtime for 2 nights | Reduction vs placebo in WTDS and WASO at all 3 doses. Increase in TST and SE at all 3 doses. No difference in number of awakenings after sleep onset and latency to persistent sleep at all 3 doses. WTAS was reduced only at 3 and 6 mg doses. Patient-reported WTAS was decreased at all doses. Patient-reported latency to sleep onset decreased only with 6 mg. Safety profile of all 3 doses was comparable to placebo and there were no differences among placebo and all 3 doses doxepin in next-day sleepiness or psychomotor function |
| PSG: polysomnography; SE: sleep efficiency; TST: total sleep time; WASO: wake after sleep onset; WTAS: wake time after sleep; WTDS: wake time during sleep Source: References 4,5 | |||
Tolerability
Clinical studies that evaluated the safety of doxepin lasted up to 3 months. Somnolence/sedation, nausea, and upper respiratory tract infection were reported by >2% of patients taking doxepin and were more common than in patients treated with placebo.1 All reported adverse events were mild to moderate.
Doxepin appears to be better tolerated at hypnotic doses (3 mg and 6 mg) than at antidepressant doses (50 to 300 mg/d), although direct comparative studies are not available.2,4,5 Additionally, psycho-motor function assessed using DSST and SCT and next-day sedation assessed using VAS in patients receiving hypnotic doses of doxepin (1 and 3 mg) were the same as placebo. Two studies noted small-to-modest decreases in DSST, SCT, and VAS when doxepin, 6 mg, was administered.1 Patients taking doxepin at antidepressant doses report significant anticholinergic side effects, including sedation, confusion, urinary retention, constipation, blurred vision, and dry mouth. Hypotension also has been reported at antidepressant doses, and there seems to be a dose-dependant cardiotoxicity, with higher incidence of adverse effects occurring at higher doses of the drug.
Severe toxicity or death from overdose is presumably less likely with hypnotic doses of doxepin than with higher doses, although this has not been systematically explored. If an insomniac overdosed on a 30-day supply of an hypnotic dose (3 or 6 mg), he or she would take only 90 to 180 mg of doxepin, which would be unlikely to cause severe toxicity or death.2-4
Symptoms of withdrawal and rebound insomnia—an increase in WASO compared with baseline after discontinuing the medication—were assessed in a 35-day double-blind study of adults with chronic insomnia.1 There was no evidence of withdrawal syndrome as measured by Tyler’s Symptom Checklist after doxepin 3 mg and 6 mg was discontinued. Discontinuation period-emergent nausea and vomiting was noted in 5% of patients taking 6 mg of doxepin, but not in those taking placebo or 3 mg of doxepin. There was no evidence of rebound insomnia after doxepin 3 mg and 6 mg was discontinued.1
Contraindications
Doxepin is contraindicated in patients with hypersensitivity to doxepin hydrochloride, with severe urinary retention, with narrow angle glaucoma, and who have used monoamine oxidase inhibitors (MAOIs) within the previous 2 weeks. Serious adverse effects, including hypertensive crisis and death, have been reported with coadministration of MAOIs and certain drugs, such as serotonergic antidepressants and some opioids derivatives. There are no reports of concomitant use of doxepin with MAOIs.1
Dosing
In adults, the recommended hypnotic dose for doxepin is 6 mg taken 30 minutes before bedtime. For patients age ≥65, the recommended starting hypnotic dose is 3 mg 30 minutes before bedtime, which can be increased to 6 mg if indicated.1
Related Resources
- Doghramji K, Grewal R, Markov D. Evaluation and management of insomnia in the psychiatric setting. Focus. 2009;8(4):441-454.
- Psychiatric Clinics of North America. December 2006. All articles in this issue address sleep disorders encountered in psychiatric practice.
- National Sleep Foundation. www.sleepfoundation.org.
Drug Brand Names
- Amitriptyline • Elavil
- Cimetidine • Tagamet
- Desipramine • Norpramin
- Doxepin (3 mg and 6 mg) • Silenor
- Doxepin (10 to 150 mg, oral) • Sinequan
- Doxepin cream • Prudoxin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Ramelteon • Rozerem
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Silenor [package insert]. San Diego, CA: Somaxon; 2010.
2. Goforth HW. Low-dose doxepin for the treatment of insomnia: emerging data. Expert Opin Pharmacother. 2009;10(10):1649-1655.
3. Stahl SM. Selective histamine H1 antagonism: novel hypnotic and pharmacologic actions challenge classical notions of antihistamines. CNS Spectr. 2008;13(12):1027-1038.
4. Roth T, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in adults with primary insomnia. Sleep. 2007;30(11):1555-1561.
5. Scharf M, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in elderly patients with primary insomnia: a randomized, double-blind, placebo-controlled crossover study. J Clin Psychiatry. 2008;69:1557-1564.
6. Hajak G, Rodenbeck A, Adler L, et al. Nocturnal melatonin secretion and sleep after doxepin administration in chronic primary insomnia. Pharmacopsychiatry. 1996;29:187-192.
7. Hajak G, Rodenbeck A, Voderholzer U, et al. Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study. J Clin Psychiatry. 2001;62:453-463.
8. Rodenbeck A, Cohrs S, Jordan W, et al. The sleep-improving effects of doxepin are paralleled by a normalized plasma cortisol secretion in primary insomnia. A placebo-controlled, double-blind, randomized, cross-over study followed by an open treatment for 3 weeks. Psychopharmacology. 2003;170:423-428.
Low-dose doxepin—3 mg and 6 mg—has demonstrated efficacy for insomnia characterized by frequent or early-morning awakenings and an inability to return to sleep (Table 1).1 FDA-approved in March 2010, doxepin (3 mg and 6 mg) is only the second insomnia medication not designated as a controlled substance and thus may be of special value in patients with a history of substance abuse.
Table 1
Doxepin: Fast facts
| Brand name: Silenor |
| Indication: Insomnia characterized by difficulty with sleep maintenance |
| Approval date: March 2010 |
| Availability date: September 7, 2010 |
| Manufacturer: Somaxon Pharmaceuticals |
| Dosage forms: 3 mg and 6 mg tablets |
| Recommended dosage: 3 mg or 6 mg once daily within 30 minutes of bedtime |
Clinical implications
Ramelteon, the other hypnotic that is not a controlled substance, is indicated for sleep initiation insomnia (ie, inability to fall asleep). In contrast, low-dose doxepin is for patients with sleep maintenance insomnia, which is waking up frequently or early in the morning and not falling back asleep.1,2 A tricyclic antidepressant first approved in 1969, doxepin has long been available in larger doses (10-, 25-, 50-, 75-, 100-, and 150-mg capsules) to treat depression and anxiety and as a topical preparation (5% cream) for pruritus, but not in dosages <10 mg. An inexpensive generic doxepin oral solution (10 mg/ml) is available and can be titrated to smaller dosages by a dropper. Liquid doxepin costs 10 to 20 cents per dose. A pharmacist can provide a dropper, and patients should mix the medication in 4 ounces of water, milk, or juice; 0.3 ml of liquid doxepin contains 3 mg of active ingredient and 0.6 ml of solution contains 6 mg of doxepin. These other dosage forms of doxepin, however, are not FDA-approved for insomnia. (The retail price of low-dose doxepin was not available when this article went to press.)
How it works
Doxepin’s mechanism of action for treating depression and insomnia remains unknown. The antidepressant effect of doxepin is thought to result from inhibition of serotonin and norepinephrine reuptake at the synaptic cleft. Animal studies have shown anticholinergic and antihistaminergic activity with doxepin.2 Doxepin is a potent histamine antagonist—predominantly at the H1 receptor—and its binding potency to the H1 receptor is approximately 100-times higher than its binding potency for monoamine transporters (serotonin and norepinephrine).2,3 Brain histamine is believed to be 1 of the key elements in maintaining wakefulness, and the activation of the H1 receptor is thought to play an important role in mediating arousal. Blockade of the H1 receptor by doxepin likely plays a role in reducing wakefulness. Typically, therapeutic doses of antidepressants with anti-histaminergic properties, such as doxepin at antidepressant doses, amitriptyline, or desipramine, do not selectively block H1 receptors, but act at cholinergic, serotonergic, adrenergic, histaminergic, and muscarinic receptors, which can cause adverse effects.3 However, low doses of doxepin (1, 3, and 6 mg) can achieve selective H1 blockade.4,5 Patients taking >25 mg/d of doxepin may report clinically significant anticholinergic effects.
Pharmacokinetics
When doxepin, 6 mg, was administered to healthy, fasting patients, time to maximum concentration (Tmax) was 3.5 hours. Peak plasma concentration (Cmax) increased in a dose-related fashion when doxepin was increased from 3 mg to 6 mg. Doxepin, 6 mg, taken with a high-fat meal resulted in area under the curve increase of 41%, Cmax increase of 15%, and almost 3-hour delay in Tmax. Therefore, to prevent a delay in onset of action and to minimize the likelihood of daytime sedation, doxepin should not be taken within 3 hours of a meal.1-3
Doxepin is metabolized primarily by the liver’s cytochrome P450 (CYP) 2C19 and CYP2D6 enzymes; CYP1A2 and CYP2D6 are involved to a lesser extent. If doxepin is coadministered with drugs that inhibit these isoenzymes, such as fluoxetine and paroxetine, doxepin blood levels may increase. Doxepin does not seem to induce CYP isoenzymes. This medication is metabolized by demethylation and oxidation; the primary metabolite is nordoxepin (N-desmethyldoxepin), which later undergoes glucuronide conjugation. The half-life is 15 hours for doxepin and 31 hours for nordoxepin. Doxepin is excreted in urine primarily as glucuronide conjugate.1-3
Coadministration with cimetidine, an inhibitor of CYP isoenzymes, could double the doxepin plasma concentration; therefore, patients taking cimetidine should not exceed 3 mg/d of doxepin.
Efficacy
Doxepin reduced insomnia symptoms in 3 pilot studies at doses of 10, 25, and 50 mg, and in 2 phase III randomized, double-blind, placebo-controlled clinical trials using 1, 3, and 6 mg (Table 2).4,5 Clinical studies lasted up to 3 months.1-3,6-8
In the first phase III trial, 67 patients, age 18 to 64 with chronic primary insomnia, were randomly assigned to placebo or 1 mg, 3 mg, or 6 mg of doxepin for 2 nights. All patients received all treatments, and each treatment was followed by 8 hours of polysomnography (PSG) evaluation in a sleep laboratory.4 In this study, patients taking doxepin at all doses achieved improvement in objective (PSG-defined) and subjective (patient-reported) measures of sleep duration and sleep maintenance. Wake after sleep onset (WASO), total sleep time (TST), and sleep efficiency (SE) improved with all doxepin doses, and wake time during sleep (WTDS)—which was the primary study endpoint—decreased with 3 mg and 6 mg doses, but not with 1 mg or placebo. In addition, PSG indicators of early-morning awakenings (terminal insomnia) were reduced, as shown by an increase in SE during the final third of the night and the 7th and 8th hours of sleep (1, 3, and 6 mg doses) and a reduction in wake time after sleep (WTAS) during the final third of the night (6 mg only). The effects on sleep duration and maintenance were more robust with 3 mg and 6 mg doses. Improved sleep onset was seen only with the 6 mg dose. Next-day alertness was assessed using the Visual Analogue Scale (VAS) for sleepiness, and the Digit-Symbol Substitution Test (DSST) and the Symbol-Copying Task (SCT) for psychomotor function. No statistically significant differences were found among placebo and any of the doxepin doses on the VAS, DSST, or SCT.
Doxepin was well tolerated. Reported adverse events were mild or moderate. Headaches and somnolence were reported by >2% of patients. The incidence of adverse events, including next-day sedation, was similar to that of placebo. Additionally, there were no spontaneous reports of anticholinergic side effects, which are associated with higher doxepin doses.4
The second phase III trial examined safety and efficacy of 1, 3, and 6 mg doxepin in patients age ≥65.5 Seventy-six adults with primary insomnia were randomly assigned to receive placebo or doxepin for 2 nights; all patients received all treatments, and each treatment was followed by an 8-hour PSG. Patients taking any doxepin dose achieved objective and subjective improvement in sleep duration and sleep maintenance, which lasted into the final hours of the night. WTDS (primary study endpoint), WASO, TST, and overall SE improved at all doxepin doses compared with placebo, and WTAS and SE at hours 7 and 8 improved at doxepin doses of 3 mg and 6 mg compared with placebo. These findings suggest that doxepin, 3 mg and 6 mg, can help older insomnia patients with early morning awakenings.
In this study, no statistically significant differences were found among placebo and any doxepin doses on VAS, DSST, or SCT or next-day residual sedation. The incidence of side effects was low and similar to that of placebo. Adverse events were mild or moderate; 1 incident of chest pain was reported, but it was determined not to be of cardiac origin and not related to study drug. There were no spontaneous reports of anticholinergic side effects associated with higher doses of doxepin. There were no reports of memory impairment.5
Table 2
Evidence of effectiveness of doxepin for insomnia
| Study | Subjects | Dosages | Results |
|---|---|---|---|
| Roth et al, 20074; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 67 patients age 18 to 64 with chronic primary insomnia | 1, 3, or 6 mg given once daily at bedtime for 2 nights | Improvement vs placebo in PSG-defined WASO, TST, SE, and SE during the final third of the night. 6-mg dose significantly reduced subjective latency to sleep onset. Safety profile of all 3 doses was comparable to placebo. No difference in residual sedation |
| Scharf et al, 20085; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 76 patients age ≥65 with primary insomnia | 1, 3, or 6 mg at bedtime for 2 nights | Reduction vs placebo in WTDS and WASO at all 3 doses. Increase in TST and SE at all 3 doses. No difference in number of awakenings after sleep onset and latency to persistent sleep at all 3 doses. WTAS was reduced only at 3 and 6 mg doses. Patient-reported WTAS was decreased at all doses. Patient-reported latency to sleep onset decreased only with 6 mg. Safety profile of all 3 doses was comparable to placebo and there were no differences among placebo and all 3 doses doxepin in next-day sleepiness or psychomotor function |
| PSG: polysomnography; SE: sleep efficiency; TST: total sleep time; WASO: wake after sleep onset; WTAS: wake time after sleep; WTDS: wake time during sleep Source: References 4,5 | |||
Tolerability
Clinical studies that evaluated the safety of doxepin lasted up to 3 months. Somnolence/sedation, nausea, and upper respiratory tract infection were reported by >2% of patients taking doxepin and were more common than in patients treated with placebo.1 All reported adverse events were mild to moderate.
Doxepin appears to be better tolerated at hypnotic doses (3 mg and 6 mg) than at antidepressant doses (50 to 300 mg/d), although direct comparative studies are not available.2,4,5 Additionally, psycho-motor function assessed using DSST and SCT and next-day sedation assessed using VAS in patients receiving hypnotic doses of doxepin (1 and 3 mg) were the same as placebo. Two studies noted small-to-modest decreases in DSST, SCT, and VAS when doxepin, 6 mg, was administered.1 Patients taking doxepin at antidepressant doses report significant anticholinergic side effects, including sedation, confusion, urinary retention, constipation, blurred vision, and dry mouth. Hypotension also has been reported at antidepressant doses, and there seems to be a dose-dependant cardiotoxicity, with higher incidence of adverse effects occurring at higher doses of the drug.
Severe toxicity or death from overdose is presumably less likely with hypnotic doses of doxepin than with higher doses, although this has not been systematically explored. If an insomniac overdosed on a 30-day supply of an hypnotic dose (3 or 6 mg), he or she would take only 90 to 180 mg of doxepin, which would be unlikely to cause severe toxicity or death.2-4
Symptoms of withdrawal and rebound insomnia—an increase in WASO compared with baseline after discontinuing the medication—were assessed in a 35-day double-blind study of adults with chronic insomnia.1 There was no evidence of withdrawal syndrome as measured by Tyler’s Symptom Checklist after doxepin 3 mg and 6 mg was discontinued. Discontinuation period-emergent nausea and vomiting was noted in 5% of patients taking 6 mg of doxepin, but not in those taking placebo or 3 mg of doxepin. There was no evidence of rebound insomnia after doxepin 3 mg and 6 mg was discontinued.1
Contraindications
Doxepin is contraindicated in patients with hypersensitivity to doxepin hydrochloride, with severe urinary retention, with narrow angle glaucoma, and who have used monoamine oxidase inhibitors (MAOIs) within the previous 2 weeks. Serious adverse effects, including hypertensive crisis and death, have been reported with coadministration of MAOIs and certain drugs, such as serotonergic antidepressants and some opioids derivatives. There are no reports of concomitant use of doxepin with MAOIs.1
Dosing
In adults, the recommended hypnotic dose for doxepin is 6 mg taken 30 minutes before bedtime. For patients age ≥65, the recommended starting hypnotic dose is 3 mg 30 minutes before bedtime, which can be increased to 6 mg if indicated.1
Related Resources
- Doghramji K, Grewal R, Markov D. Evaluation and management of insomnia in the psychiatric setting. Focus. 2009;8(4):441-454.
- Psychiatric Clinics of North America. December 2006. All articles in this issue address sleep disorders encountered in psychiatric practice.
- National Sleep Foundation. www.sleepfoundation.org.
Drug Brand Names
- Amitriptyline • Elavil
- Cimetidine • Tagamet
- Desipramine • Norpramin
- Doxepin (3 mg and 6 mg) • Silenor
- Doxepin (10 to 150 mg, oral) • Sinequan
- Doxepin cream • Prudoxin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Ramelteon • Rozerem
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Low-dose doxepin—3 mg and 6 mg—has demonstrated efficacy for insomnia characterized by frequent or early-morning awakenings and an inability to return to sleep (Table 1).1 FDA-approved in March 2010, doxepin (3 mg and 6 mg) is only the second insomnia medication not designated as a controlled substance and thus may be of special value in patients with a history of substance abuse.
Table 1
Doxepin: Fast facts
| Brand name: Silenor |
| Indication: Insomnia characterized by difficulty with sleep maintenance |
| Approval date: March 2010 |
| Availability date: September 7, 2010 |
| Manufacturer: Somaxon Pharmaceuticals |
| Dosage forms: 3 mg and 6 mg tablets |
| Recommended dosage: 3 mg or 6 mg once daily within 30 minutes of bedtime |
Clinical implications
Ramelteon, the other hypnotic that is not a controlled substance, is indicated for sleep initiation insomnia (ie, inability to fall asleep). In contrast, low-dose doxepin is for patients with sleep maintenance insomnia, which is waking up frequently or early in the morning and not falling back asleep.1,2 A tricyclic antidepressant first approved in 1969, doxepin has long been available in larger doses (10-, 25-, 50-, 75-, 100-, and 150-mg capsules) to treat depression and anxiety and as a topical preparation (5% cream) for pruritus, but not in dosages <10 mg. An inexpensive generic doxepin oral solution (10 mg/ml) is available and can be titrated to smaller dosages by a dropper. Liquid doxepin costs 10 to 20 cents per dose. A pharmacist can provide a dropper, and patients should mix the medication in 4 ounces of water, milk, or juice; 0.3 ml of liquid doxepin contains 3 mg of active ingredient and 0.6 ml of solution contains 6 mg of doxepin. These other dosage forms of doxepin, however, are not FDA-approved for insomnia. (The retail price of low-dose doxepin was not available when this article went to press.)
How it works
Doxepin’s mechanism of action for treating depression and insomnia remains unknown. The antidepressant effect of doxepin is thought to result from inhibition of serotonin and norepinephrine reuptake at the synaptic cleft. Animal studies have shown anticholinergic and antihistaminergic activity with doxepin.2 Doxepin is a potent histamine antagonist—predominantly at the H1 receptor—and its binding potency to the H1 receptor is approximately 100-times higher than its binding potency for monoamine transporters (serotonin and norepinephrine).2,3 Brain histamine is believed to be 1 of the key elements in maintaining wakefulness, and the activation of the H1 receptor is thought to play an important role in mediating arousal. Blockade of the H1 receptor by doxepin likely plays a role in reducing wakefulness. Typically, therapeutic doses of antidepressants with anti-histaminergic properties, such as doxepin at antidepressant doses, amitriptyline, or desipramine, do not selectively block H1 receptors, but act at cholinergic, serotonergic, adrenergic, histaminergic, and muscarinic receptors, which can cause adverse effects.3 However, low doses of doxepin (1, 3, and 6 mg) can achieve selective H1 blockade.4,5 Patients taking >25 mg/d of doxepin may report clinically significant anticholinergic effects.
Pharmacokinetics
When doxepin, 6 mg, was administered to healthy, fasting patients, time to maximum concentration (Tmax) was 3.5 hours. Peak plasma concentration (Cmax) increased in a dose-related fashion when doxepin was increased from 3 mg to 6 mg. Doxepin, 6 mg, taken with a high-fat meal resulted in area under the curve increase of 41%, Cmax increase of 15%, and almost 3-hour delay in Tmax. Therefore, to prevent a delay in onset of action and to minimize the likelihood of daytime sedation, doxepin should not be taken within 3 hours of a meal.1-3
Doxepin is metabolized primarily by the liver’s cytochrome P450 (CYP) 2C19 and CYP2D6 enzymes; CYP1A2 and CYP2D6 are involved to a lesser extent. If doxepin is coadministered with drugs that inhibit these isoenzymes, such as fluoxetine and paroxetine, doxepin blood levels may increase. Doxepin does not seem to induce CYP isoenzymes. This medication is metabolized by demethylation and oxidation; the primary metabolite is nordoxepin (N-desmethyldoxepin), which later undergoes glucuronide conjugation. The half-life is 15 hours for doxepin and 31 hours for nordoxepin. Doxepin is excreted in urine primarily as glucuronide conjugate.1-3
Coadministration with cimetidine, an inhibitor of CYP isoenzymes, could double the doxepin plasma concentration; therefore, patients taking cimetidine should not exceed 3 mg/d of doxepin.
Efficacy
Doxepin reduced insomnia symptoms in 3 pilot studies at doses of 10, 25, and 50 mg, and in 2 phase III randomized, double-blind, placebo-controlled clinical trials using 1, 3, and 6 mg (Table 2).4,5 Clinical studies lasted up to 3 months.1-3,6-8
In the first phase III trial, 67 patients, age 18 to 64 with chronic primary insomnia, were randomly assigned to placebo or 1 mg, 3 mg, or 6 mg of doxepin for 2 nights. All patients received all treatments, and each treatment was followed by 8 hours of polysomnography (PSG) evaluation in a sleep laboratory.4 In this study, patients taking doxepin at all doses achieved improvement in objective (PSG-defined) and subjective (patient-reported) measures of sleep duration and sleep maintenance. Wake after sleep onset (WASO), total sleep time (TST), and sleep efficiency (SE) improved with all doxepin doses, and wake time during sleep (WTDS)—which was the primary study endpoint—decreased with 3 mg and 6 mg doses, but not with 1 mg or placebo. In addition, PSG indicators of early-morning awakenings (terminal insomnia) were reduced, as shown by an increase in SE during the final third of the night and the 7th and 8th hours of sleep (1, 3, and 6 mg doses) and a reduction in wake time after sleep (WTAS) during the final third of the night (6 mg only). The effects on sleep duration and maintenance were more robust with 3 mg and 6 mg doses. Improved sleep onset was seen only with the 6 mg dose. Next-day alertness was assessed using the Visual Analogue Scale (VAS) for sleepiness, and the Digit-Symbol Substitution Test (DSST) and the Symbol-Copying Task (SCT) for psychomotor function. No statistically significant differences were found among placebo and any of the doxepin doses on the VAS, DSST, or SCT.
Doxepin was well tolerated. Reported adverse events were mild or moderate. Headaches and somnolence were reported by >2% of patients. The incidence of adverse events, including next-day sedation, was similar to that of placebo. Additionally, there were no spontaneous reports of anticholinergic side effects, which are associated with higher doxepin doses.4
The second phase III trial examined safety and efficacy of 1, 3, and 6 mg doxepin in patients age ≥65.5 Seventy-six adults with primary insomnia were randomly assigned to receive placebo or doxepin for 2 nights; all patients received all treatments, and each treatment was followed by an 8-hour PSG. Patients taking any doxepin dose achieved objective and subjective improvement in sleep duration and sleep maintenance, which lasted into the final hours of the night. WTDS (primary study endpoint), WASO, TST, and overall SE improved at all doxepin doses compared with placebo, and WTAS and SE at hours 7 and 8 improved at doxepin doses of 3 mg and 6 mg compared with placebo. These findings suggest that doxepin, 3 mg and 6 mg, can help older insomnia patients with early morning awakenings.
In this study, no statistically significant differences were found among placebo and any doxepin doses on VAS, DSST, or SCT or next-day residual sedation. The incidence of side effects was low and similar to that of placebo. Adverse events were mild or moderate; 1 incident of chest pain was reported, but it was determined not to be of cardiac origin and not related to study drug. There were no spontaneous reports of anticholinergic side effects associated with higher doses of doxepin. There were no reports of memory impairment.5
Table 2
Evidence of effectiveness of doxepin for insomnia
| Study | Subjects | Dosages | Results |
|---|---|---|---|
| Roth et al, 20074; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 67 patients age 18 to 64 with chronic primary insomnia | 1, 3, or 6 mg given once daily at bedtime for 2 nights | Improvement vs placebo in PSG-defined WASO, TST, SE, and SE during the final third of the night. 6-mg dose significantly reduced subjective latency to sleep onset. Safety profile of all 3 doses was comparable to placebo. No difference in residual sedation |
| Scharf et al, 20085; phase III, randomized, multi-center, double-blind, placebo-controlled, 4-period crossover, dose-response study | 76 patients age ≥65 with primary insomnia | 1, 3, or 6 mg at bedtime for 2 nights | Reduction vs placebo in WTDS and WASO at all 3 doses. Increase in TST and SE at all 3 doses. No difference in number of awakenings after sleep onset and latency to persistent sleep at all 3 doses. WTAS was reduced only at 3 and 6 mg doses. Patient-reported WTAS was decreased at all doses. Patient-reported latency to sleep onset decreased only with 6 mg. Safety profile of all 3 doses was comparable to placebo and there were no differences among placebo and all 3 doses doxepin in next-day sleepiness or psychomotor function |
| PSG: polysomnography; SE: sleep efficiency; TST: total sleep time; WASO: wake after sleep onset; WTAS: wake time after sleep; WTDS: wake time during sleep Source: References 4,5 | |||
Tolerability
Clinical studies that evaluated the safety of doxepin lasted up to 3 months. Somnolence/sedation, nausea, and upper respiratory tract infection were reported by >2% of patients taking doxepin and were more common than in patients treated with placebo.1 All reported adverse events were mild to moderate.
Doxepin appears to be better tolerated at hypnotic doses (3 mg and 6 mg) than at antidepressant doses (50 to 300 mg/d), although direct comparative studies are not available.2,4,5 Additionally, psycho-motor function assessed using DSST and SCT and next-day sedation assessed using VAS in patients receiving hypnotic doses of doxepin (1 and 3 mg) were the same as placebo. Two studies noted small-to-modest decreases in DSST, SCT, and VAS when doxepin, 6 mg, was administered.1 Patients taking doxepin at antidepressant doses report significant anticholinergic side effects, including sedation, confusion, urinary retention, constipation, blurred vision, and dry mouth. Hypotension also has been reported at antidepressant doses, and there seems to be a dose-dependant cardiotoxicity, with higher incidence of adverse effects occurring at higher doses of the drug.
Severe toxicity or death from overdose is presumably less likely with hypnotic doses of doxepin than with higher doses, although this has not been systematically explored. If an insomniac overdosed on a 30-day supply of an hypnotic dose (3 or 6 mg), he or she would take only 90 to 180 mg of doxepin, which would be unlikely to cause severe toxicity or death.2-4
Symptoms of withdrawal and rebound insomnia—an increase in WASO compared with baseline after discontinuing the medication—were assessed in a 35-day double-blind study of adults with chronic insomnia.1 There was no evidence of withdrawal syndrome as measured by Tyler’s Symptom Checklist after doxepin 3 mg and 6 mg was discontinued. Discontinuation period-emergent nausea and vomiting was noted in 5% of patients taking 6 mg of doxepin, but not in those taking placebo or 3 mg of doxepin. There was no evidence of rebound insomnia after doxepin 3 mg and 6 mg was discontinued.1
Contraindications
Doxepin is contraindicated in patients with hypersensitivity to doxepin hydrochloride, with severe urinary retention, with narrow angle glaucoma, and who have used monoamine oxidase inhibitors (MAOIs) within the previous 2 weeks. Serious adverse effects, including hypertensive crisis and death, have been reported with coadministration of MAOIs and certain drugs, such as serotonergic antidepressants and some opioids derivatives. There are no reports of concomitant use of doxepin with MAOIs.1
Dosing
In adults, the recommended hypnotic dose for doxepin is 6 mg taken 30 minutes before bedtime. For patients age ≥65, the recommended starting hypnotic dose is 3 mg 30 minutes before bedtime, which can be increased to 6 mg if indicated.1
Related Resources
- Doghramji K, Grewal R, Markov D. Evaluation and management of insomnia in the psychiatric setting. Focus. 2009;8(4):441-454.
- Psychiatric Clinics of North America. December 2006. All articles in this issue address sleep disorders encountered in psychiatric practice.
- National Sleep Foundation. www.sleepfoundation.org.
Drug Brand Names
- Amitriptyline • Elavil
- Cimetidine • Tagamet
- Desipramine • Norpramin
- Doxepin (3 mg and 6 mg) • Silenor
- Doxepin (10 to 150 mg, oral) • Sinequan
- Doxepin cream • Prudoxin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Ramelteon • Rozerem
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Silenor [package insert]. San Diego, CA: Somaxon; 2010.
2. Goforth HW. Low-dose doxepin for the treatment of insomnia: emerging data. Expert Opin Pharmacother. 2009;10(10):1649-1655.
3. Stahl SM. Selective histamine H1 antagonism: novel hypnotic and pharmacologic actions challenge classical notions of antihistamines. CNS Spectr. 2008;13(12):1027-1038.
4. Roth T, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in adults with primary insomnia. Sleep. 2007;30(11):1555-1561.
5. Scharf M, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in elderly patients with primary insomnia: a randomized, double-blind, placebo-controlled crossover study. J Clin Psychiatry. 2008;69:1557-1564.
6. Hajak G, Rodenbeck A, Adler L, et al. Nocturnal melatonin secretion and sleep after doxepin administration in chronic primary insomnia. Pharmacopsychiatry. 1996;29:187-192.
7. Hajak G, Rodenbeck A, Voderholzer U, et al. Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study. J Clin Psychiatry. 2001;62:453-463.
8. Rodenbeck A, Cohrs S, Jordan W, et al. The sleep-improving effects of doxepin are paralleled by a normalized plasma cortisol secretion in primary insomnia. A placebo-controlled, double-blind, randomized, cross-over study followed by an open treatment for 3 weeks. Psychopharmacology. 2003;170:423-428.
1. Silenor [package insert]. San Diego, CA: Somaxon; 2010.
2. Goforth HW. Low-dose doxepin for the treatment of insomnia: emerging data. Expert Opin Pharmacother. 2009;10(10):1649-1655.
3. Stahl SM. Selective histamine H1 antagonism: novel hypnotic and pharmacologic actions challenge classical notions of antihistamines. CNS Spectr. 2008;13(12):1027-1038.
4. Roth T, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in adults with primary insomnia. Sleep. 2007;30(11):1555-1561.
5. Scharf M, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in elderly patients with primary insomnia: a randomized, double-blind, placebo-controlled crossover study. J Clin Psychiatry. 2008;69:1557-1564.
6. Hajak G, Rodenbeck A, Adler L, et al. Nocturnal melatonin secretion and sleep after doxepin administration in chronic primary insomnia. Pharmacopsychiatry. 1996;29:187-192.
7. Hajak G, Rodenbeck A, Voderholzer U, et al. Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study. J Clin Psychiatry. 2001;62:453-463.
8. Rodenbeck A, Cohrs S, Jordan W, et al. The sleep-improving effects of doxepin are paralleled by a normalized plasma cortisol secretion in primary insomnia. A placebo-controlled, double-blind, randomized, cross-over study followed by an open treatment for 3 weeks. Psychopharmacology. 2003;170:423-428.
Guanfacine extended release for ADHD
Guanfacine extended release (GXR)—a selective α-2 adrenergic agonist FDA-approved for the treatment of attention-deficit/hyperactivity disorder (ADHD)—has demonstrated efficacy for inattentive and hyperactive/impulsive symptom domains in 2 large trials lasting 8 and 9 weeks.1,2 GXR’s once-daily formulation may increase adherence and deliver consistent control of symptoms across a full day ( Table 1 ).
Table 1
Guanfacine extended release: Fast facts
| Brand name: Intuniv |
| Indication: Attention-deficit/hyperactivity disorder |
| Approval date: September 3, 2009 |
| Availability date: November 2009 |
| Manufacturer: Shire |
| Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets |
| Recommended dosage: 0.05 to 0.12 mg/kg once daily |
Clinical implications
GXR exhibits enhancement of noradrenergic pathways through selective direct receptor action in the prefrontal cortex.3 This mechanism of action is different from that of other FDA-approved ADHD medications. GXR can be used alone or in combination with stimulants or atomoxetine for treating complex ADHD, such as cases accompanied by oppositional features and emotional dysregulation or characterized by partial stimulant response.
How it works
Guanfacine—originally developed as an immediate-release (IR) antihypertensive—reduces sympathetic tone, causing centrally mediated vasodilation and reduced heart rate. Although GXR’s mechanism of action in ADHD is not known, the drug is a selective α-2A receptor agonist thought to directly engage postsynaptic receptors in the prefrontal cortex (PFC), an area of the brain believed to play a major role in attentional and organizational functions that preclinical research has linked to ADHD.3
The postsynaptic α-2A receptor is thought to play a central role in the optimal functioning of the PFC as illustrated by the “inverted U hypothesis of PFC activation.”4 In this model, cyclic adenosine monophosphate (cAMP) levels build within the prefrontal cortical neurons and cause specific ion channels—hyperpolarization-activated cyclic nucleotide gated (HCN) channels—to open on dendritic spines of these neurons.5 Activation of HCN channels effectively reduces membrane resistance, cutting off synaptic inputs and disconnecting PFC network connections. Because α-2A receptors are located in proximity to HCN channels, their stimulation by GXR closes HCN channels, inhibits further production of cAMP, and reestablishes synaptic function and the resulting network connectivity.5 Blockade of α-2A receptors by yohimbine reverses this process, eroding network connectivity, and in monkeys has been demonstrated to impair working memory,6 damage inhibition/impulse control, and produce locomotor hyperactivity.
Direct stimulation by GXR of the postsynaptic α-2A receptors is thought to:
- strengthen working memory
- reduce susceptibility to distraction
- improve attention regulation
- improve behavioral inhibition
- enhance impulse control.7
Pharmacokinetics
GXR offers enhanced pharmaceutics relative to IR guanfacine. IR guanfacine exhibits poor absorption characteristics—peak plasma concentration is achieved too rapidly and then declines precipitously, with considerable inter-individual variation.
GXR’s once-daily formulation is implemented by a proprietary enteric-coated sustained release mechanism8 that is meant to:
- control absorption
- provide a broad but flat plasma concentration profile
- reduce inter-individual variation of guanfacine exposure.
Compared with IR guanfacine, GXR exhibits delayed time of maximum concentration (Tmax) and reduced maximum concentration (Cmax). Therapeutic concentrations can be sustained over longer periods with reduced peak-to-trough fluctuation,8 which tends to improve tolerability and symptom control throughout the day. The convenience of once-daily dosing also may increase adherence.
GXR’s pharmacokinetic characteristics do not change with dose, but high-fat meals will increase absorption of the drug—Cmax increases by 75% and area under the plasma concentration time curve increases by 40%. Because GXR primarily is metabolized through cytochrome P450 (CYP) 3A4, CYP3A4 inhibitors such as ketoconazole will increase guanfacine plasma concentrations and elevate the risk of adverse events such as bradycardia, hypotension, and sedation. Conversely, CYP3A4 inducers such as rifampin will significantly reduce total guanfacine exposure. Coadministration of valproic acid with GXR can result in increased valproic acid levels, producing additive CNS side effects.
Efficacy
GXR reduced both inattentive and hyperactive/impulsive symptoms in 2 phase III, forced-dose, parallel-design, randomized, placebo-controlled trials ( Table 2 ). In the first trial,1 345 children age 6 to 17 received placebo or GXR, 2 mg, 3 mg, or 4 mg once daily for 8 weeks. In the second study,2 324 children age 6 to 17 received placebo or GXR, 1 mg, 2 mg, 3 mg, or 4 mg, once daily for 9 weeks; the 1-mg dose was given only to patients weighing <50 kg (<110 lbs).
In both trials, doses were increased in increments of 1 mg/week, and investigators evaluated participants’ ADHD signs and symptoms once a week using the clinician administered and scored ADHD Rating Scale-IV (ADHD-RS-IV). The primary outcome was change in total ADHD-RS-IV score from baseline to endpoint.
In both trials, patients taking GXR demonstrated statistically signifcant improvements in ADHD-RS-IV score starting 1 to 2 weeks after they began receiving once-daily GXR:
- In the first trial, the mean reduction in ADHD-RS-IV total score at endpoint was –16.7 for GXR compared with –8.9 for placebo (P < .0001).
- In the second, the reduction was –19.6 for GXR and –12.2 for placebo (P=.004).
Placebo-adjusted least squares mean changes from baseline were statistically significant for all GXR doses in the randomized treatment groups in both studies.
Secondary efficacy outcome measures included the Conners’ Parent Rating Scale-Revised: Short Form (CPRS-R) and the Conners’ Teacher Rating Scale-Revised: Short Form (CTRS-R).
Significant improvements were seen on both scales. On the CPRS-R, parents reported significant improvement across a full day (as measured at 6 PM, 8 PM, and 6 AM the next day). On the CTRS-R—which was used only in the first trial—teachers reported significant improvement throughout the school day (as measured at 10 AM and 2 PM).
Treating oppositional symptoms. In a collateral study,9 GXR was evaluated in complex ADHD patients age 6 to 12 who exhibited oppositional symptoms. The primary efficacy measure was change from baseline to endpoint in the oppositional subscale of the Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R:L) score.
All subjects randomized to GXR started on a dose of 1 mg/d—which could be titrated by 1 mg/week during the 5-week, dose-optimization period to a maximum of 4 mg/d—and were maintained at their optimal doses for 3 additional weeks. Among the 217 subjects enrolled, 138 received GXR and 79, placebo.
Least-squares mean reductions from baseline to endpoint in CPRS-R:L oppositional subscale scores were –10.9 in the GXR group compared with –6.8 in the placebo group (P < .001; effect size 0.590). The GXR-treated group showed a significantly greater reduction in ADHD-RS-IV total score from baseline to endpoint compared with the placebo group (–23.8 vs –11.4, respectively, P < .001; effect size 0.916).
Table 2
Randomized, controlled trials supporting GXR’s effectiveness
for treating ADHD symptoms
| Study | Subjects | GXR dosages | Results |
|---|---|---|---|
| Biederman et al, 20087 ; phase III, forced-dose parallel-design | 345 ADHD patients age 6 to 17 | 2, 3, or 4 mg given once daily for 8 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-16.7 vs -8.9) |
| Sallee et al, 20098 ; phase III, forced-dose parallel-design | 324 ADHD patients age 6 to 17 | 1,* 2, 3, or 4 mg given once daily for 9 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-19.6 vs -12.2) |
| Connor et al, 20099 ; collateral study | 217 complex ADHD patients age 6 to 12 with oppositional symptoms | Starting dose 1 mg/d, titrated to a maximum of 4 mg/d for a total of 8 weeks | GXR was associated with significantly lower scores on CPRS-R:L oppositional subscale (-10.9 vs -6.8) and ADHD-RS-IV (-23.8 vs -11.4) compared with placebo |
| *1-mg dose was given only to subjects weighing <50 kg (<110 lbs) | |||
| ADHD: attention-deficit/hyperactivity disorder; ADHD-RS-IV: Attention-Deficit/Hyperactivity Disorder Rating Scale-IV; CPRS-R:L: Conners’ Parent Rating Scale-Revised: Long Form; GXR: guanfacine extended release | |||
Tolerability
In the phase III trials, the most commonly reported drug-related adverse reactions (occurring in ≥2% of patients) were:
- somnolence (38%)
- headache (24%)
- fatigue (14%)
- upper abdominal pain (10%)
- nausea, lethargy, dizziness, hypotension/decreased blood pressure, irritability (6% for each)
- decreased appetite (5%)
- dry mouth (4%)
- constipation (3%).
Many of these adverse reactions appear to be dose-related, particularly somnolence, sedation, abdominal pain, dizziness, and hypotension/decreased blood pressure.
Overall, GXR was well tolerated; clinicians rated most events as mild to moderate. Twelve percent of GXR patients discontinued the clinical studies because of adverse events, compared with 4% in the placebo groups. The most common adverse reactions leading to discontinuation were somnolence/sedation (6%) and fatigue (2%). Less common adverse reactions leading to discontinuation (occurring in 1% of patients) included hypotension/decreased blood pressure, headache, and dizziness.
Open-label safety trial. Sallee et al10 conducted a longer-term, open-label, flexible-dose safety continuation study of 259 GXR-treated patients (mean exposure 10 months), some of whom also received a psychostimulant. Common adverse reactions (occurring in ≥5% of subjects) included somnolence (45%), headache (26%), fatigue (16%), upper abdominal pain (11%), hypotension/decreased blood pressure (10%), vomiting (9%), dizziness (7%), nausea (7%), weight gain (7%), and irritability (6%).10 In a subset of patients, the onset of sedative events typically occurred within the first 3 weeks of GXR treatment and then declined with maintenance to a frequency of approximately 16%. The rates of somnolence, sedation, or fatigue were lowest among patients who also received a psychostimulant ( Figure ).
Distribution of GXR doses before the end of this study was 37% of patients on 4 mg, 33% on 3 mg, 27% on 2 mg, and 3% on 1 mg, suggesting a preference for maintenance doses of 3 to 4 mg/d. The most frequent adverse reactions leading to discontinuation were somnolence (3%), syncopal events (2%), increased weight (2%), depression (2%), and fatigue (2%). Other adverse reactions leading to discontinuation (occurring in approximately 1% of patients) included hypotension/decreased blood pressure, sedation, headache, and lethargy. Serious adverse reactions in the longer-term study in >1 patient included syncope (2%) and convulsion (0.4%).
Figure: Incidence of somnolence, sedation, and fatigue in study patients receiving GXR
with or without psychostimulants
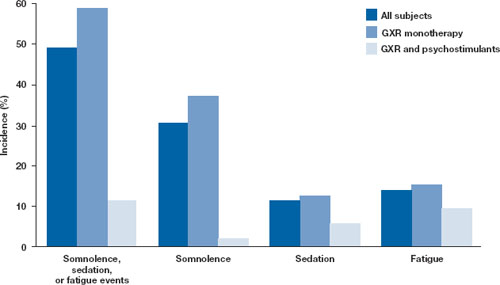
In an open-label continuation study of 259 patients treated with guanfacine extended release (GXR), somnolence, sedation, or fatigue was reported by 49% of subjects overall, 59% of those who received GXR monotherapy, and 11% of those given GXR with a psychostimulant.
GXR: guanfacine extended release
Source: Reprinted with permission from Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226 Safety warnings relating to the likelihood of hypotension, bradycardia, and possible syncope when prescribing GXR should be understood in the context of its pharmacologic action to lower heart rate and blood pressure. In the short-term (8 to 9 weeks) controlled trials, the maximum mean changes from baseline in systolic blood pressure, diastolic blood pressure, and pulse were -5 mm Hg, -3 mm Hg, and -6 bpm, respectively, for all dose groups combined. These changes, which generally occurred 1 week after reaching target doses of 1 to 4 mg/d, were dose-dependent but usually modest and did not cause other symptoms; however, hypotension and bradycardia can occur.
In the longer-term, open-label safety study,10 maximum decreases in systolic and diastolic blood pressure occurred in the first month of treatment; decreases were less pronounced over time. Syncope occurred in 1% of pediatric subjects but was not dose-dependent. Guanfacine IR can increase QT interval but not in a dose-dependent fashion.
Dosing
The approved dose range for GXR is 1 to 4 mg once daily in the morning. Initiate treatment at 1 mg/d, and adjust the dose in increments of no more than 1 mg/week, evaluating the patient weekly. GXR maintenance therapy is frequently in the range of 2 to 4 mg/d.
Because adverse events such as hypotension, bradycardia, and sedation are dose-related, evaluate benefit and risk using mg/kg range approximation. GXR efficacy on a weight-adjusted (mg/kg) basis is consistent across a dosage range of 0.01 to 0.17 mg/kg/d. Clinically relevant improvements are usually observed beginning at doses of 0.05 to 0.08 mg/kg/d. In clinical trials, efficacy increased with increasing weight-adjusted dose (mg/kg), so if GXR is well-tolerated, doses up to 0.12 mg/kg once daily may provide additional benefit up to the maximum of 4 mg/d.
Instruct patients to swallow GXR whole because crushing, chewing, or otherwise breaking the tablet’s enteric coating will markedly enhance guanfacine release.
Abruptly discontinuing GXR is associated with infrequent, transient elevations in blood pressure above the patient’s baseline (ie, rebound). To minimize these effects, GXR should be gradually tapered in decrements of no more than 1 mg every 3 to 7 days. Isolated missed doses of GXR generally are not a problem, but ≥2 consecutive missed doses may warrant reinitiation of the titration schedule.
Related resource
- Guanfacine extended release (Intuniv) prescribing information. www.intuniv.com/documents/INTUNIV_Full_Prescribing_Information.pdf.
Drug brand names
- Atomoxetine • Strattera
- Guanfacine extended release • Intuniv
- Guanfacine immediate release • Tenex
- Ketoconazole • Nizoral
- Rifampin • Rifadin, Rimactane
- Valproic acid • Depakene, Depakote
Disclosure
Dr. Sallee receives grant/research support from the National Institutes of Health. He is a consultant to Otsuka, Nextwave, and Sepracor and a consultant to and speaker for Shire. Dr. Sallee is a consultant to, shareholder of, and member of the board of directors of P2D Inc. and a principal in Satiety Solutions.
1. Biederman J, Melmed RD, Patel A, et al. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121:e73-e84.
2. Sallee F, McGough J, Wigal T, et al. For the SPD503 Study Group Guanfacine extended release in children and adolescents with attention deficit hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48(2):155-165.
3. Arnsten AF, Cai JX, Goldman-Rakic PS. The α-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects: evidence for α-2 receptor subtypes. J Neurosci. 1988;8:4287-4298.
4. Vijayraghavan S, Wang M, Birnbaum SG, et al. Inverted-U dopamine D1 receptor actions on prefrontal neurons engaged in working memory. Nat Neurosci. 2007;10:376-384.
5. Wang M, Ramos BP, Paspalas CD, et al. α 2-A adrenoceptors strengthen working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell. 2007;129:397-410.
6. Li BM, Mei ZT. Delayed-response deficit induced by local injection of the α 2-adrenergic antagonist yohimbine into the dorsolateral prefrontal cortex in young adult monkeys. Behav Neural Biol. 1994;62:134-139.
7. Scahill L, Chappell PB, Kim YS, et al. A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1067-1074.
8. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29:617-625.
9. Connor D, Spencer T, Kratochvil C, et al. Effects of guanfacine extended release on secondary measures in children with attention-deficit/hyperactivity disorder and oppositional symptoms. Abstract presented at: Annual Meeting of the American Psychiatric Association; May 18, 2009; San Francisco, CA.
10. Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226.
Guanfacine extended release (GXR)—a selective α-2 adrenergic agonist FDA-approved for the treatment of attention-deficit/hyperactivity disorder (ADHD)—has demonstrated efficacy for inattentive and hyperactive/impulsive symptom domains in 2 large trials lasting 8 and 9 weeks.1,2 GXR’s once-daily formulation may increase adherence and deliver consistent control of symptoms across a full day ( Table 1 ).
Table 1
Guanfacine extended release: Fast facts
| Brand name: Intuniv |
| Indication: Attention-deficit/hyperactivity disorder |
| Approval date: September 3, 2009 |
| Availability date: November 2009 |
| Manufacturer: Shire |
| Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets |
| Recommended dosage: 0.05 to 0.12 mg/kg once daily |
Clinical implications
GXR exhibits enhancement of noradrenergic pathways through selective direct receptor action in the prefrontal cortex.3 This mechanism of action is different from that of other FDA-approved ADHD medications. GXR can be used alone or in combination with stimulants or atomoxetine for treating complex ADHD, such as cases accompanied by oppositional features and emotional dysregulation or characterized by partial stimulant response.
How it works
Guanfacine—originally developed as an immediate-release (IR) antihypertensive—reduces sympathetic tone, causing centrally mediated vasodilation and reduced heart rate. Although GXR’s mechanism of action in ADHD is not known, the drug is a selective α-2A receptor agonist thought to directly engage postsynaptic receptors in the prefrontal cortex (PFC), an area of the brain believed to play a major role in attentional and organizational functions that preclinical research has linked to ADHD.3
The postsynaptic α-2A receptor is thought to play a central role in the optimal functioning of the PFC as illustrated by the “inverted U hypothesis of PFC activation.”4 In this model, cyclic adenosine monophosphate (cAMP) levels build within the prefrontal cortical neurons and cause specific ion channels—hyperpolarization-activated cyclic nucleotide gated (HCN) channels—to open on dendritic spines of these neurons.5 Activation of HCN channels effectively reduces membrane resistance, cutting off synaptic inputs and disconnecting PFC network connections. Because α-2A receptors are located in proximity to HCN channels, their stimulation by GXR closes HCN channels, inhibits further production of cAMP, and reestablishes synaptic function and the resulting network connectivity.5 Blockade of α-2A receptors by yohimbine reverses this process, eroding network connectivity, and in monkeys has been demonstrated to impair working memory,6 damage inhibition/impulse control, and produce locomotor hyperactivity.
Direct stimulation by GXR of the postsynaptic α-2A receptors is thought to:
- strengthen working memory
- reduce susceptibility to distraction
- improve attention regulation
- improve behavioral inhibition
- enhance impulse control.7
Pharmacokinetics
GXR offers enhanced pharmaceutics relative to IR guanfacine. IR guanfacine exhibits poor absorption characteristics—peak plasma concentration is achieved too rapidly and then declines precipitously, with considerable inter-individual variation.
GXR’s once-daily formulation is implemented by a proprietary enteric-coated sustained release mechanism8 that is meant to:
- control absorption
- provide a broad but flat plasma concentration profile
- reduce inter-individual variation of guanfacine exposure.
Compared with IR guanfacine, GXR exhibits delayed time of maximum concentration (Tmax) and reduced maximum concentration (Cmax). Therapeutic concentrations can be sustained over longer periods with reduced peak-to-trough fluctuation,8 which tends to improve tolerability and symptom control throughout the day. The convenience of once-daily dosing also may increase adherence.
GXR’s pharmacokinetic characteristics do not change with dose, but high-fat meals will increase absorption of the drug—Cmax increases by 75% and area under the plasma concentration time curve increases by 40%. Because GXR primarily is metabolized through cytochrome P450 (CYP) 3A4, CYP3A4 inhibitors such as ketoconazole will increase guanfacine plasma concentrations and elevate the risk of adverse events such as bradycardia, hypotension, and sedation. Conversely, CYP3A4 inducers such as rifampin will significantly reduce total guanfacine exposure. Coadministration of valproic acid with GXR can result in increased valproic acid levels, producing additive CNS side effects.
Efficacy
GXR reduced both inattentive and hyperactive/impulsive symptoms in 2 phase III, forced-dose, parallel-design, randomized, placebo-controlled trials ( Table 2 ). In the first trial,1 345 children age 6 to 17 received placebo or GXR, 2 mg, 3 mg, or 4 mg once daily for 8 weeks. In the second study,2 324 children age 6 to 17 received placebo or GXR, 1 mg, 2 mg, 3 mg, or 4 mg, once daily for 9 weeks; the 1-mg dose was given only to patients weighing <50 kg (<110 lbs).
In both trials, doses were increased in increments of 1 mg/week, and investigators evaluated participants’ ADHD signs and symptoms once a week using the clinician administered and scored ADHD Rating Scale-IV (ADHD-RS-IV). The primary outcome was change in total ADHD-RS-IV score from baseline to endpoint.
In both trials, patients taking GXR demonstrated statistically signifcant improvements in ADHD-RS-IV score starting 1 to 2 weeks after they began receiving once-daily GXR:
- In the first trial, the mean reduction in ADHD-RS-IV total score at endpoint was –16.7 for GXR compared with –8.9 for placebo (P < .0001).
- In the second, the reduction was –19.6 for GXR and –12.2 for placebo (P=.004).
Placebo-adjusted least squares mean changes from baseline were statistically significant for all GXR doses in the randomized treatment groups in both studies.
Secondary efficacy outcome measures included the Conners’ Parent Rating Scale-Revised: Short Form (CPRS-R) and the Conners’ Teacher Rating Scale-Revised: Short Form (CTRS-R).
Significant improvements were seen on both scales. On the CPRS-R, parents reported significant improvement across a full day (as measured at 6 PM, 8 PM, and 6 AM the next day). On the CTRS-R—which was used only in the first trial—teachers reported significant improvement throughout the school day (as measured at 10 AM and 2 PM).
Treating oppositional symptoms. In a collateral study,9 GXR was evaluated in complex ADHD patients age 6 to 12 who exhibited oppositional symptoms. The primary efficacy measure was change from baseline to endpoint in the oppositional subscale of the Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R:L) score.
All subjects randomized to GXR started on a dose of 1 mg/d—which could be titrated by 1 mg/week during the 5-week, dose-optimization period to a maximum of 4 mg/d—and were maintained at their optimal doses for 3 additional weeks. Among the 217 subjects enrolled, 138 received GXR and 79, placebo.
Least-squares mean reductions from baseline to endpoint in CPRS-R:L oppositional subscale scores were –10.9 in the GXR group compared with –6.8 in the placebo group (P < .001; effect size 0.590). The GXR-treated group showed a significantly greater reduction in ADHD-RS-IV total score from baseline to endpoint compared with the placebo group (–23.8 vs –11.4, respectively, P < .001; effect size 0.916).
Table 2
Randomized, controlled trials supporting GXR’s effectiveness
for treating ADHD symptoms
| Study | Subjects | GXR dosages | Results |
|---|---|---|---|
| Biederman et al, 20087 ; phase III, forced-dose parallel-design | 345 ADHD patients age 6 to 17 | 2, 3, or 4 mg given once daily for 8 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-16.7 vs -8.9) |
| Sallee et al, 20098 ; phase III, forced-dose parallel-design | 324 ADHD patients age 6 to 17 | 1,* 2, 3, or 4 mg given once daily for 9 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-19.6 vs -12.2) |
| Connor et al, 20099 ; collateral study | 217 complex ADHD patients age 6 to 12 with oppositional symptoms | Starting dose 1 mg/d, titrated to a maximum of 4 mg/d for a total of 8 weeks | GXR was associated with significantly lower scores on CPRS-R:L oppositional subscale (-10.9 vs -6.8) and ADHD-RS-IV (-23.8 vs -11.4) compared with placebo |
| *1-mg dose was given only to subjects weighing <50 kg (<110 lbs) | |||
| ADHD: attention-deficit/hyperactivity disorder; ADHD-RS-IV: Attention-Deficit/Hyperactivity Disorder Rating Scale-IV; CPRS-R:L: Conners’ Parent Rating Scale-Revised: Long Form; GXR: guanfacine extended release | |||
Tolerability
In the phase III trials, the most commonly reported drug-related adverse reactions (occurring in ≥2% of patients) were:
- somnolence (38%)
- headache (24%)
- fatigue (14%)
- upper abdominal pain (10%)
- nausea, lethargy, dizziness, hypotension/decreased blood pressure, irritability (6% for each)
- decreased appetite (5%)
- dry mouth (4%)
- constipation (3%).
Many of these adverse reactions appear to be dose-related, particularly somnolence, sedation, abdominal pain, dizziness, and hypotension/decreased blood pressure.
Overall, GXR was well tolerated; clinicians rated most events as mild to moderate. Twelve percent of GXR patients discontinued the clinical studies because of adverse events, compared with 4% in the placebo groups. The most common adverse reactions leading to discontinuation were somnolence/sedation (6%) and fatigue (2%). Less common adverse reactions leading to discontinuation (occurring in 1% of patients) included hypotension/decreased blood pressure, headache, and dizziness.
Open-label safety trial. Sallee et al10 conducted a longer-term, open-label, flexible-dose safety continuation study of 259 GXR-treated patients (mean exposure 10 months), some of whom also received a psychostimulant. Common adverse reactions (occurring in ≥5% of subjects) included somnolence (45%), headache (26%), fatigue (16%), upper abdominal pain (11%), hypotension/decreased blood pressure (10%), vomiting (9%), dizziness (7%), nausea (7%), weight gain (7%), and irritability (6%).10 In a subset of patients, the onset of sedative events typically occurred within the first 3 weeks of GXR treatment and then declined with maintenance to a frequency of approximately 16%. The rates of somnolence, sedation, or fatigue were lowest among patients who also received a psychostimulant ( Figure ).
Distribution of GXR doses before the end of this study was 37% of patients on 4 mg, 33% on 3 mg, 27% on 2 mg, and 3% on 1 mg, suggesting a preference for maintenance doses of 3 to 4 mg/d. The most frequent adverse reactions leading to discontinuation were somnolence (3%), syncopal events (2%), increased weight (2%), depression (2%), and fatigue (2%). Other adverse reactions leading to discontinuation (occurring in approximately 1% of patients) included hypotension/decreased blood pressure, sedation, headache, and lethargy. Serious adverse reactions in the longer-term study in >1 patient included syncope (2%) and convulsion (0.4%).
Figure: Incidence of somnolence, sedation, and fatigue in study patients receiving GXR
with or without psychostimulants
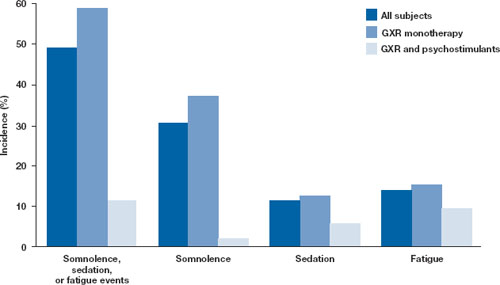
In an open-label continuation study of 259 patients treated with guanfacine extended release (GXR), somnolence, sedation, or fatigue was reported by 49% of subjects overall, 59% of those who received GXR monotherapy, and 11% of those given GXR with a psychostimulant.
GXR: guanfacine extended release
Source: Reprinted with permission from Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226 Safety warnings relating to the likelihood of hypotension, bradycardia, and possible syncope when prescribing GXR should be understood in the context of its pharmacologic action to lower heart rate and blood pressure. In the short-term (8 to 9 weeks) controlled trials, the maximum mean changes from baseline in systolic blood pressure, diastolic blood pressure, and pulse were -5 mm Hg, -3 mm Hg, and -6 bpm, respectively, for all dose groups combined. These changes, which generally occurred 1 week after reaching target doses of 1 to 4 mg/d, were dose-dependent but usually modest and did not cause other symptoms; however, hypotension and bradycardia can occur.
In the longer-term, open-label safety study,10 maximum decreases in systolic and diastolic blood pressure occurred in the first month of treatment; decreases were less pronounced over time. Syncope occurred in 1% of pediatric subjects but was not dose-dependent. Guanfacine IR can increase QT interval but not in a dose-dependent fashion.
Dosing
The approved dose range for GXR is 1 to 4 mg once daily in the morning. Initiate treatment at 1 mg/d, and adjust the dose in increments of no more than 1 mg/week, evaluating the patient weekly. GXR maintenance therapy is frequently in the range of 2 to 4 mg/d.
Because adverse events such as hypotension, bradycardia, and sedation are dose-related, evaluate benefit and risk using mg/kg range approximation. GXR efficacy on a weight-adjusted (mg/kg) basis is consistent across a dosage range of 0.01 to 0.17 mg/kg/d. Clinically relevant improvements are usually observed beginning at doses of 0.05 to 0.08 mg/kg/d. In clinical trials, efficacy increased with increasing weight-adjusted dose (mg/kg), so if GXR is well-tolerated, doses up to 0.12 mg/kg once daily may provide additional benefit up to the maximum of 4 mg/d.
Instruct patients to swallow GXR whole because crushing, chewing, or otherwise breaking the tablet’s enteric coating will markedly enhance guanfacine release.
Abruptly discontinuing GXR is associated with infrequent, transient elevations in blood pressure above the patient’s baseline (ie, rebound). To minimize these effects, GXR should be gradually tapered in decrements of no more than 1 mg every 3 to 7 days. Isolated missed doses of GXR generally are not a problem, but ≥2 consecutive missed doses may warrant reinitiation of the titration schedule.
Related resource
- Guanfacine extended release (Intuniv) prescribing information. www.intuniv.com/documents/INTUNIV_Full_Prescribing_Information.pdf.
Drug brand names
- Atomoxetine • Strattera
- Guanfacine extended release • Intuniv
- Guanfacine immediate release • Tenex
- Ketoconazole • Nizoral
- Rifampin • Rifadin, Rimactane
- Valproic acid • Depakene, Depakote
Disclosure
Dr. Sallee receives grant/research support from the National Institutes of Health. He is a consultant to Otsuka, Nextwave, and Sepracor and a consultant to and speaker for Shire. Dr. Sallee is a consultant to, shareholder of, and member of the board of directors of P2D Inc. and a principal in Satiety Solutions.
Guanfacine extended release (GXR)—a selective α-2 adrenergic agonist FDA-approved for the treatment of attention-deficit/hyperactivity disorder (ADHD)—has demonstrated efficacy for inattentive and hyperactive/impulsive symptom domains in 2 large trials lasting 8 and 9 weeks.1,2 GXR’s once-daily formulation may increase adherence and deliver consistent control of symptoms across a full day ( Table 1 ).
Table 1
Guanfacine extended release: Fast facts
| Brand name: Intuniv |
| Indication: Attention-deficit/hyperactivity disorder |
| Approval date: September 3, 2009 |
| Availability date: November 2009 |
| Manufacturer: Shire |
| Dosing forms: 1-mg, 2-mg, 3-mg, and 4-mg extended-release tablets |
| Recommended dosage: 0.05 to 0.12 mg/kg once daily |
Clinical implications
GXR exhibits enhancement of noradrenergic pathways through selective direct receptor action in the prefrontal cortex.3 This mechanism of action is different from that of other FDA-approved ADHD medications. GXR can be used alone or in combination with stimulants or atomoxetine for treating complex ADHD, such as cases accompanied by oppositional features and emotional dysregulation or characterized by partial stimulant response.
How it works
Guanfacine—originally developed as an immediate-release (IR) antihypertensive—reduces sympathetic tone, causing centrally mediated vasodilation and reduced heart rate. Although GXR’s mechanism of action in ADHD is not known, the drug is a selective α-2A receptor agonist thought to directly engage postsynaptic receptors in the prefrontal cortex (PFC), an area of the brain believed to play a major role in attentional and organizational functions that preclinical research has linked to ADHD.3
The postsynaptic α-2A receptor is thought to play a central role in the optimal functioning of the PFC as illustrated by the “inverted U hypothesis of PFC activation.”4 In this model, cyclic adenosine monophosphate (cAMP) levels build within the prefrontal cortical neurons and cause specific ion channels—hyperpolarization-activated cyclic nucleotide gated (HCN) channels—to open on dendritic spines of these neurons.5 Activation of HCN channels effectively reduces membrane resistance, cutting off synaptic inputs and disconnecting PFC network connections. Because α-2A receptors are located in proximity to HCN channels, their stimulation by GXR closes HCN channels, inhibits further production of cAMP, and reestablishes synaptic function and the resulting network connectivity.5 Blockade of α-2A receptors by yohimbine reverses this process, eroding network connectivity, and in monkeys has been demonstrated to impair working memory,6 damage inhibition/impulse control, and produce locomotor hyperactivity.
Direct stimulation by GXR of the postsynaptic α-2A receptors is thought to:
- strengthen working memory
- reduce susceptibility to distraction
- improve attention regulation
- improve behavioral inhibition
- enhance impulse control.7
Pharmacokinetics
GXR offers enhanced pharmaceutics relative to IR guanfacine. IR guanfacine exhibits poor absorption characteristics—peak plasma concentration is achieved too rapidly and then declines precipitously, with considerable inter-individual variation.
GXR’s once-daily formulation is implemented by a proprietary enteric-coated sustained release mechanism8 that is meant to:
- control absorption
- provide a broad but flat plasma concentration profile
- reduce inter-individual variation of guanfacine exposure.
Compared with IR guanfacine, GXR exhibits delayed time of maximum concentration (Tmax) and reduced maximum concentration (Cmax). Therapeutic concentrations can be sustained over longer periods with reduced peak-to-trough fluctuation,8 which tends to improve tolerability and symptom control throughout the day. The convenience of once-daily dosing also may increase adherence.
GXR’s pharmacokinetic characteristics do not change with dose, but high-fat meals will increase absorption of the drug—Cmax increases by 75% and area under the plasma concentration time curve increases by 40%. Because GXR primarily is metabolized through cytochrome P450 (CYP) 3A4, CYP3A4 inhibitors such as ketoconazole will increase guanfacine plasma concentrations and elevate the risk of adverse events such as bradycardia, hypotension, and sedation. Conversely, CYP3A4 inducers such as rifampin will significantly reduce total guanfacine exposure. Coadministration of valproic acid with GXR can result in increased valproic acid levels, producing additive CNS side effects.
Efficacy
GXR reduced both inattentive and hyperactive/impulsive symptoms in 2 phase III, forced-dose, parallel-design, randomized, placebo-controlled trials ( Table 2 ). In the first trial,1 345 children age 6 to 17 received placebo or GXR, 2 mg, 3 mg, or 4 mg once daily for 8 weeks. In the second study,2 324 children age 6 to 17 received placebo or GXR, 1 mg, 2 mg, 3 mg, or 4 mg, once daily for 9 weeks; the 1-mg dose was given only to patients weighing <50 kg (<110 lbs).
In both trials, doses were increased in increments of 1 mg/week, and investigators evaluated participants’ ADHD signs and symptoms once a week using the clinician administered and scored ADHD Rating Scale-IV (ADHD-RS-IV). The primary outcome was change in total ADHD-RS-IV score from baseline to endpoint.
In both trials, patients taking GXR demonstrated statistically signifcant improvements in ADHD-RS-IV score starting 1 to 2 weeks after they began receiving once-daily GXR:
- In the first trial, the mean reduction in ADHD-RS-IV total score at endpoint was –16.7 for GXR compared with –8.9 for placebo (P < .0001).
- In the second, the reduction was –19.6 for GXR and –12.2 for placebo (P=.004).
Placebo-adjusted least squares mean changes from baseline were statistically significant for all GXR doses in the randomized treatment groups in both studies.
Secondary efficacy outcome measures included the Conners’ Parent Rating Scale-Revised: Short Form (CPRS-R) and the Conners’ Teacher Rating Scale-Revised: Short Form (CTRS-R).
Significant improvements were seen on both scales. On the CPRS-R, parents reported significant improvement across a full day (as measured at 6 PM, 8 PM, and 6 AM the next day). On the CTRS-R—which was used only in the first trial—teachers reported significant improvement throughout the school day (as measured at 10 AM and 2 PM).
Treating oppositional symptoms. In a collateral study,9 GXR was evaluated in complex ADHD patients age 6 to 12 who exhibited oppositional symptoms. The primary efficacy measure was change from baseline to endpoint in the oppositional subscale of the Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R:L) score.
All subjects randomized to GXR started on a dose of 1 mg/d—which could be titrated by 1 mg/week during the 5-week, dose-optimization period to a maximum of 4 mg/d—and were maintained at their optimal doses for 3 additional weeks. Among the 217 subjects enrolled, 138 received GXR and 79, placebo.
Least-squares mean reductions from baseline to endpoint in CPRS-R:L oppositional subscale scores were –10.9 in the GXR group compared with –6.8 in the placebo group (P < .001; effect size 0.590). The GXR-treated group showed a significantly greater reduction in ADHD-RS-IV total score from baseline to endpoint compared with the placebo group (–23.8 vs –11.4, respectively, P < .001; effect size 0.916).
Table 2
Randomized, controlled trials supporting GXR’s effectiveness
for treating ADHD symptoms
| Study | Subjects | GXR dosages | Results |
|---|---|---|---|
| Biederman et al, 20087 ; phase III, forced-dose parallel-design | 345 ADHD patients age 6 to 17 | 2, 3, or 4 mg given once daily for 8 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-16.7 vs -8.9) |
| Sallee et al, 20098 ; phase III, forced-dose parallel-design | 324 ADHD patients age 6 to 17 | 1,* 2, 3, or 4 mg given once daily for 9 weeks | GXR was associated with significantly lower ADHD-RS-IV score compared with placebo (-19.6 vs -12.2) |
| Connor et al, 20099 ; collateral study | 217 complex ADHD patients age 6 to 12 with oppositional symptoms | Starting dose 1 mg/d, titrated to a maximum of 4 mg/d for a total of 8 weeks | GXR was associated with significantly lower scores on CPRS-R:L oppositional subscale (-10.9 vs -6.8) and ADHD-RS-IV (-23.8 vs -11.4) compared with placebo |
| *1-mg dose was given only to subjects weighing <50 kg (<110 lbs) | |||
| ADHD: attention-deficit/hyperactivity disorder; ADHD-RS-IV: Attention-Deficit/Hyperactivity Disorder Rating Scale-IV; CPRS-R:L: Conners’ Parent Rating Scale-Revised: Long Form; GXR: guanfacine extended release | |||
Tolerability
In the phase III trials, the most commonly reported drug-related adverse reactions (occurring in ≥2% of patients) were:
- somnolence (38%)
- headache (24%)
- fatigue (14%)
- upper abdominal pain (10%)
- nausea, lethargy, dizziness, hypotension/decreased blood pressure, irritability (6% for each)
- decreased appetite (5%)
- dry mouth (4%)
- constipation (3%).
Many of these adverse reactions appear to be dose-related, particularly somnolence, sedation, abdominal pain, dizziness, and hypotension/decreased blood pressure.
Overall, GXR was well tolerated; clinicians rated most events as mild to moderate. Twelve percent of GXR patients discontinued the clinical studies because of adverse events, compared with 4% in the placebo groups. The most common adverse reactions leading to discontinuation were somnolence/sedation (6%) and fatigue (2%). Less common adverse reactions leading to discontinuation (occurring in 1% of patients) included hypotension/decreased blood pressure, headache, and dizziness.
Open-label safety trial. Sallee et al10 conducted a longer-term, open-label, flexible-dose safety continuation study of 259 GXR-treated patients (mean exposure 10 months), some of whom also received a psychostimulant. Common adverse reactions (occurring in ≥5% of subjects) included somnolence (45%), headache (26%), fatigue (16%), upper abdominal pain (11%), hypotension/decreased blood pressure (10%), vomiting (9%), dizziness (7%), nausea (7%), weight gain (7%), and irritability (6%).10 In a subset of patients, the onset of sedative events typically occurred within the first 3 weeks of GXR treatment and then declined with maintenance to a frequency of approximately 16%. The rates of somnolence, sedation, or fatigue were lowest among patients who also received a psychostimulant ( Figure ).
Distribution of GXR doses before the end of this study was 37% of patients on 4 mg, 33% on 3 mg, 27% on 2 mg, and 3% on 1 mg, suggesting a preference for maintenance doses of 3 to 4 mg/d. The most frequent adverse reactions leading to discontinuation were somnolence (3%), syncopal events (2%), increased weight (2%), depression (2%), and fatigue (2%). Other adverse reactions leading to discontinuation (occurring in approximately 1% of patients) included hypotension/decreased blood pressure, sedation, headache, and lethargy. Serious adverse reactions in the longer-term study in >1 patient included syncope (2%) and convulsion (0.4%).
Figure: Incidence of somnolence, sedation, and fatigue in study patients receiving GXR
with or without psychostimulants
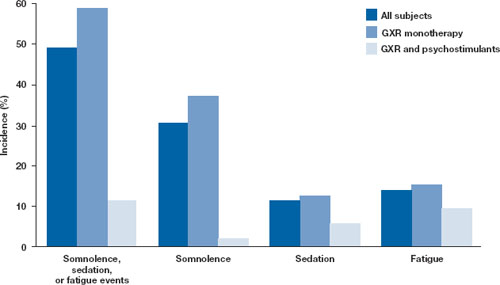
In an open-label continuation study of 259 patients treated with guanfacine extended release (GXR), somnolence, sedation, or fatigue was reported by 49% of subjects overall, 59% of those who received GXR monotherapy, and 11% of those given GXR with a psychostimulant.
GXR: guanfacine extended release
Source: Reprinted with permission from Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226 Safety warnings relating to the likelihood of hypotension, bradycardia, and possible syncope when prescribing GXR should be understood in the context of its pharmacologic action to lower heart rate and blood pressure. In the short-term (8 to 9 weeks) controlled trials, the maximum mean changes from baseline in systolic blood pressure, diastolic blood pressure, and pulse were -5 mm Hg, -3 mm Hg, and -6 bpm, respectively, for all dose groups combined. These changes, which generally occurred 1 week after reaching target doses of 1 to 4 mg/d, were dose-dependent but usually modest and did not cause other symptoms; however, hypotension and bradycardia can occur.
In the longer-term, open-label safety study,10 maximum decreases in systolic and diastolic blood pressure occurred in the first month of treatment; decreases were less pronounced over time. Syncope occurred in 1% of pediatric subjects but was not dose-dependent. Guanfacine IR can increase QT interval but not in a dose-dependent fashion.
Dosing
The approved dose range for GXR is 1 to 4 mg once daily in the morning. Initiate treatment at 1 mg/d, and adjust the dose in increments of no more than 1 mg/week, evaluating the patient weekly. GXR maintenance therapy is frequently in the range of 2 to 4 mg/d.
Because adverse events such as hypotension, bradycardia, and sedation are dose-related, evaluate benefit and risk using mg/kg range approximation. GXR efficacy on a weight-adjusted (mg/kg) basis is consistent across a dosage range of 0.01 to 0.17 mg/kg/d. Clinically relevant improvements are usually observed beginning at doses of 0.05 to 0.08 mg/kg/d. In clinical trials, efficacy increased with increasing weight-adjusted dose (mg/kg), so if GXR is well-tolerated, doses up to 0.12 mg/kg once daily may provide additional benefit up to the maximum of 4 mg/d.
Instruct patients to swallow GXR whole because crushing, chewing, or otherwise breaking the tablet’s enteric coating will markedly enhance guanfacine release.
Abruptly discontinuing GXR is associated with infrequent, transient elevations in blood pressure above the patient’s baseline (ie, rebound). To minimize these effects, GXR should be gradually tapered in decrements of no more than 1 mg every 3 to 7 days. Isolated missed doses of GXR generally are not a problem, but ≥2 consecutive missed doses may warrant reinitiation of the titration schedule.
Related resource
- Guanfacine extended release (Intuniv) prescribing information. www.intuniv.com/documents/INTUNIV_Full_Prescribing_Information.pdf.
Drug brand names
- Atomoxetine • Strattera
- Guanfacine extended release • Intuniv
- Guanfacine immediate release • Tenex
- Ketoconazole • Nizoral
- Rifampin • Rifadin, Rimactane
- Valproic acid • Depakene, Depakote
Disclosure
Dr. Sallee receives grant/research support from the National Institutes of Health. He is a consultant to Otsuka, Nextwave, and Sepracor and a consultant to and speaker for Shire. Dr. Sallee is a consultant to, shareholder of, and member of the board of directors of P2D Inc. and a principal in Satiety Solutions.
1. Biederman J, Melmed RD, Patel A, et al. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121:e73-e84.
2. Sallee F, McGough J, Wigal T, et al. For the SPD503 Study Group Guanfacine extended release in children and adolescents with attention deficit hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48(2):155-165.
3. Arnsten AF, Cai JX, Goldman-Rakic PS. The α-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects: evidence for α-2 receptor subtypes. J Neurosci. 1988;8:4287-4298.
4. Vijayraghavan S, Wang M, Birnbaum SG, et al. Inverted-U dopamine D1 receptor actions on prefrontal neurons engaged in working memory. Nat Neurosci. 2007;10:376-384.
5. Wang M, Ramos BP, Paspalas CD, et al. α 2-A adrenoceptors strengthen working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell. 2007;129:397-410.
6. Li BM, Mei ZT. Delayed-response deficit induced by local injection of the α 2-adrenergic antagonist yohimbine into the dorsolateral prefrontal cortex in young adult monkeys. Behav Neural Biol. 1994;62:134-139.
7. Scahill L, Chappell PB, Kim YS, et al. A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1067-1074.
8. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29:617-625.
9. Connor D, Spencer T, Kratochvil C, et al. Effects of guanfacine extended release on secondary measures in children with attention-deficit/hyperactivity disorder and oppositional symptoms. Abstract presented at: Annual Meeting of the American Psychiatric Association; May 18, 2009; San Francisco, CA.
10. Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226.
1. Biederman J, Melmed RD, Patel A, et al. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121:e73-e84.
2. Sallee F, McGough J, Wigal T, et al. For the SPD503 Study Group Guanfacine extended release in children and adolescents with attention deficit hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48(2):155-165.
3. Arnsten AF, Cai JX, Goldman-Rakic PS. The α-2 adrenergic agonist guanfacine improves memory in aged monkeys without sedative or hypotensive side effects: evidence for α-2 receptor subtypes. J Neurosci. 1988;8:4287-4298.
4. Vijayraghavan S, Wang M, Birnbaum SG, et al. Inverted-U dopamine D1 receptor actions on prefrontal neurons engaged in working memory. Nat Neurosci. 2007;10:376-384.
5. Wang M, Ramos BP, Paspalas CD, et al. α 2-A adrenoceptors strengthen working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell. 2007;129:397-410.
6. Li BM, Mei ZT. Delayed-response deficit induced by local injection of the α 2-adrenergic antagonist yohimbine into the dorsolateral prefrontal cortex in young adult monkeys. Behav Neural Biol. 1994;62:134-139.
7. Scahill L, Chappell PB, Kim YS, et al. A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1067-1074.
8. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29:617-625.
9. Connor D, Spencer T, Kratochvil C, et al. Effects of guanfacine extended release on secondary measures in children with attention-deficit/hyperactivity disorder and oppositional symptoms. Abstract presented at: Annual Meeting of the American Psychiatric Association; May 18, 2009; San Francisco, CA.
10. Sallee FR, Lyne A, Wigal T, et al. Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19(3):215-226.
Asenapine for schizophrenia and bipolar I disorder
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.
Iloperidone for schizophrenia
Iloperidone is a second-generation (atypical) antipsychotic the FDA approved in May 2009 for treating acute schizophrenia in adults (Table 1). Iloperidone is not a derivative (metabolite, isomer, or different formulation) of any other antipsychotic. Clinical trials have shown that iloperidone is efficacious and suggest that for some patients its side-effect profile may be more favorable than that of other antipsychotics.
Table 1
Iloperidone: Fast facts
| Brand name: Fanapt |
| Class: Atypical antipsychotic (serotonin/dopamine antagonist) |
| Indication: Acute schizophrenia in adults |
| Approval date: May 2009 |
| Availability date: Late 2009 |
| Manufacturer: Vanda Pharmaceuticals, Inc. |
| Dosing forms: 1-, 2-, 4-, 6-, 8-, 10-, and 12-mg tablets (nonscored); titration pack of 2×1-mg, 2×2-mg, 2×4-mg, and 2×6-mg tablets |
| Starting dose: 1 mg bid (2 mg total daily dose) |
| Target dose: 12 to 24 mg total daily dose |
Clinical implications
Iloperidone’s binding profile is similar to that of other antipsychotics with relatively stronger affinity for serotonin (5-HT2A) than dopamine (D2) receptors, and its efficacy is roughly comparable to that of other non-clozapine antipsychotics.
Individual patients may respond differently to specific antipsychotics, even when those agents have shown equivalent efficacy in clinical trials. Therefore, a key therapeutic question is the degree of differential efficacy—differences in response at an individual level—among iloperidone and other antipsychotics.
The differential efficacy among iloperidone and other antipsychotics is unknown. Our clinical experience and iloperidone’s unique structure suggest, however, that this agent might be helpful for certain patients who do not fully respond to or are unable to tolerate other antipsychotics.
How iloperidone works
Like other antipsychotics, iloperidone’s efficacy presumably is based on its ability to block [antagonize] dopamine D2 receptors. Its chemical structure is most similar to risperidone, paliperidone, and ziprasidone, but its receptor binding profile is distinguished by a relatively lower affinity for serotonin receptors 5-HT1A and 5-HT2C than ziprasidone, and a relative lack of muscarinic and histaminic antagonist properties (Table 2).
The relatively higher affinity of iloperidone (and its metabolite P95) for the NEα1 receptor correlates with the drug’s propensity to cause orthostatic hypotension during initial up-titration.1 Differences in iloperidone’s receptor binding profile compared with other antipsychotics likely are responsible for its different side-effect profile.2,3
Table 2
Relative receptor binding affinities of 3 atypical antipsychotics*
| Binding affinity | |||
|---|---|---|---|
| Receptor | Risperidone | Ziprasidone | Iloperidone |
| Dopamine D2 | High | High | High |
| Serotonin 5-HT1A | Low | High | Low |
| Serotonin 5-HT2A | High | High | High |
| Serotonin 5-HT2C | Moderate | High | Moderate† |
| Norepinephrine NEα1 | High | Moderate | Moderate‡ |
| Histamine H1 | Moderate | Moderate | Low |
| Muscarinic M1 | Negligible | Negligible | Negligible |
| * Cross-comparison of binding strengths reflects the subjective judgment of the authors. The goal is to demonstrate differences in overall binding patterns, and these estimates should not be considered an exact cross-comparison | |||
| † Published reports of binding affinity of iloperidone show considerable variation for the 5HT2C site | |||
| ‡ One metabolite of iloperidone [P95] does not have CNS activity but has potent alpha-1 antagonism and may contribute to the initial orthostatic hypotension seen in clinical trials | |||
Pharmacokinetics
Iloperidone is administered twice daily and can be taken with or without food. The bioavailability of iloperidone tablets is 96%, and peak plasma concentrations are achieved 2 to 4 hours after ingestion.
Like all antipsychotics except paliperidone, iloperidone is metabolized by the liver’s cytochrome P450 (CYP) system. The enzyme pathways CYP3A4 and CYP2D6 transform iloperidone into 2 metabolites: one with CNS activity (P88) and one that does not cross the blood-brain barrier and is not active in the CNS (P95) but likely has peripheral effects.
Genetic variations in CYP2D6 activity can substantially alter how individual patients metabolize iloperidone. The half-life of iloperidone and its active metabolites differs depending on whether someone is a poor metabolizer (no functional CYP2D6 activity), intermediate metabolizer (reduced CYP2D6 activity), or extensive metabolizer (“normal” CYP2D6 activity). The usual half-life of iloperidone (approximately 18 hours in extensive metabolizers) can be almost 50% longer (>24 hours) in CYP2D6 poor metabolizers.
There are no recommendations to test patients for genetic variants that result in poor metabolism from CYP2D6. Rather, clinicians simply need to be aware that this could be the source of interindividual differences they see in iloperidone tolerability, just as it is for any other medication that is a substrate for the CYP2D6 enzyme system.
Interactions. Medications that inhibit the CYP3A4 or CYP2D6 systems can increase iloperidone plasma level when taken concurrently with iloperidone, even if intrinsic liver metabolism activity is normal. Fluoxetine and paroxetine are potent CYP2D6 inhibitors. Concurrent treatment with either of these selective serotonin reuptake inhibitors could increase iloperidone plasma concentration by 100% or more.4
Similarly, cotreatment with a potent CYP3A4 inhibitor such as ketoconazole (or drinking grapefruit juice) will decrease metabolism and increase plasma concentrations of iloperidone and its active metabolites by about 50%. Smoking status should not influence iloperidone plasma concentration because this drug is not a primary substrate for CYP1A2, the enzyme induced by cigarette smoking.
The bottom line: reduce iloperidone dosage by 50% for patients who are taking a strong CYP2D6 and/or CYP3A4 inhibitor (see Dosing below).
Efficacy
In clinical trials, iloperidone was shown to be efficacious in treating positive and negative symptoms and general psychopathology in acute episodes of schizophrenia. It is important to consider the efficacy studies of iloperidone within the context of the history of its development plan.
Early clinical trials. Most of iloperidone’s phase II and III studies were conducted by Novartis between 1998 and 2002. Initial phase III studies included three 6-week, double-blind, placebo-controlled acute trials comparing a range of iloperidone doses with placebo and an active comparator:5,6
- The first trial compared iloperidone, 4, 8, or 12 mg/d, with placebo or haloperidol, 15 mg/d.
- The second compared iloperidone, 4 to 8 mg/d or 10 to 16 mg/d, with placebo and risperidone, 4 to 8 mg/d.
- The third compared iloperidone, 12 to 16 mg/d or 20 to 24 mg/d, with placebo or risperidone, 6 to 8 mg/d.
These studies totaled 1,066 patients in the iloperidone treatment arms, with target dosages for iloperidone ranging from 4 to 24 mg/d. Iloperidone was more efficacious than placebo for positive, negative, and overall total symptoms on the Positive and Negative Syndrome Scale (PANSS), albeit 4 mg/d and 8 mg/d dosages narrowly missed the .05 significance level.
The haloperidol and risperidone active controls appeared more effective than iloperidone in the original analyses, but these studies were not designed for analysis of comparative efficacy. The protocols for all of these studies used an up-titration schedule for the iloperidone groups that took 1 week to reach steady-state levels, whereas the haloperidol and risperidone groups had a briefer up-titration to target dose.
The interpretation of these studies is complex and a detailed discussion is beyond the scope of this article. However, a post-hoc analysis that included subjects who remained in the study after 2 weeks of double-blind medication showed that iloperidone performed comparably to risperidone7 and haloperidol.8
A new phase III trial. The question remained whether iloperidone was as efficacious as other first-line antipsychotics but had been “penalized” by its slower up-titration schedule and clinical trial design flaws. After acquiring the development rights to iloperidone from Novartis and reviewing prior study designs and results, Vanda Pharmaceuticals designed another phase III study comparing iloperidone with placebo and ziprasidone. Its purpose was to correct for possible design flaws in the previous studies.
Ziprasidone was selected as the active control because of its established efficacy, safety, and twice-daily dosing. In this trial, researchers attempted to match the 2 drugs’ up-titration schedules. Twice-daily doses were given with food as follows:
- iloperidone, 1, 2, 4, 6, 8, 10, and 12 mg (days 1 to 7, respectively)
- ziprasidone, 20 mg (days 1 to 2), 40 mg (days 3 to 4), 60 mg (days 5 to 6), and 80 mg (day 7).
By day 7, target dosages were reached: iloperidone, 24 mg/d, and ziprasidone, 160 mg/d.9
Patients receiving iloperidone showed significantly greater improvement in PANSS total scores at 4 weeks vs those receiving placebo (–12.0, iloperidone; –7.1, placebo; P < .01).9 Patients receiving ziprasidone also achieved significantly greater improvement vs those receiving placebo (–12.3; P < .05 vs placebo).
The iloperidone and ziprasidone groups showed significantly greater improvement from baseline vs placebo in PANSS positive (P) and negative (N) subscale scores. Significantly more patients receiving iloperidone (72%) than placebo (52%) experienced improvement (≥20% reduction from baseline) in PANSS-P scores (P = .005).
Patients receiving iloperidone had a significantly greater reduction in Clinical Global Impression-Severity scale score vs placebo (–0.65 and –0.39, respectively; P = .007), as did patients receiving ziprasidone (–0.67; P = .013).
Iloperidone met all predefined protocol criteria for efficacy vs placebo and had efficacy equal to the highest approved dose of ziprasidone. These results demonstrated that iloperidone has comparable efficacy to ziprasidone and support the validity of the re-analysis of earlier studies showing comparable efficacy between iloperidone and risperidone7 or haloperidol.8 In July 2008 the FDA issued a not approvable letter for iloperidone, requesting further clinical trials because of concerns about the drug’s efficacy compared with risperidone. The FDA approved iloperidone in May 2009 after the manufacturer provided additional data from existing trials that demonstrated comparable efficacy to risperidone.
Long-term efficacy. A double-blind extension study compared patients remaining on blinded iloperidone (4 to 16 mg/d) or haloperidol (5 to 20 mg/d) after completing a 6-week efficacy study.10 The drugs showed equivalent efficacy in preventing relapse over 46 weeks follow-up. Because this study included no placebo group, the FDA does not consider it to be an interpretable relapse prevention study.
Tolerability
Clinicians might consider iloperidone when seeking to switch a patient to an antipsychotic with a potentially lower side-effect burden.6,11 Compared with risperidone, iloperidone has a lower liability for extrapyramidal symptoms (EPS) and does not cause clinically significant prolactin elevation (Table 3).5,7-9 Compared with ziprasidone, iloperidone has a lower EPS and akathisia liability. Somewhat greater weight gain was seen with iloperidone when compared with ziprasidone in a 4-week study (iloperidone, +2.8 kg; ziprasidone, +1.1 kg; placebo, +0.5 kg) but the 2 drugs’ effects on triglycerides and cholesterol were comparable.9
Iloperidone has a similar degree of QTc prolongation as ziprasidone (mean 9 msec at the highest dosage of 12 mg bid). Safety studies including administration of maximal doses of iloperidone with CYP3A4 and CYP2D6 inhibitors showed a mean QTc prolongation of 19 msec without clinically significant problems, and iloperidone has not been associated with serious arrhythmia.4 Iloperidone should not be prescribed to patients with significant cardiac problems or electrolyte disturbances, however, or those taking drugs known to have clinically significant QTc/proarrhythmic properties, such as thioridazine, droperidol, pimozide, or methadone.4
Iloperidone has the same safety concerns associated with other atypical antipsychotics, including tardive dyskinesia and neuroleptic malignant syndrome. Like other atypical antipsychotics, iloperidone carries a warning of increased mortality risk in elderly patients with dementia-related psychosis.
Dose-related side effects include dizziness, orthostatic hypotension, and tachycardia. Dizziness occurred more often at higher doses (20% at 20 to 24 mg/d vs 10% at 10 to 16 mg/d vs 7% in placebo groups). Presumably these side effects are related to NEα1 antagonism and are the basis for the recommended dose-titration schedule described below. Clinical trials do not seem to demonstrate a dose-response relationship for acute EPS or akathisia.
Table 3
Common side effects: Iloperidone vs other antipsychotics*
| Other antipsychotic | Less likely or less severe with iloperidone | More likely or more severe with iloperidone |
|---|---|---|
| Haloperidol4,8 | EPS Akathisia Prolactin elevation | Weight gain Orthostasis |
| Olanzapine | Dyslipidemia Weight gain Sedation | Orthostasis |
| Quetiapine | Dyslipidemia Sedation | EPS |
| Risperidone4,6 | EPS Prolactin elevation Akathisia | None |
| Ziprasidone7 | EPS Akathisia | Weight gain Orthostasis |
| Aripiprazole | Akathisia | Weight gain Orthostasis |
| * Iloperidone has been compared head-to-head with haloperidol, risperidone, and ziprasidone in clinical trials. Other suggested antipsychotic side effect liabilities are based on indirect comparisons | ||
| EPS: extrapyramidal symptoms | ||
The approved dosage range for iloperidone is 12 to 24 mg/d, given as 6 to 12 mg bid. Some trials suggest a dose-response relationship, with 24 mg being more effective than lower target doses.5 Reduce the target dosage of iloperidone by one-half when administering it concomitantly with medications that are strong CYP2D6 or CYP3A4 inhibitors.
Titration schedule. Because iloperidone’s relatively strong NEα1 antagonism creates risk for initial orthostatic hypotension, the drug needs to be titrated to the target dose over 4 to 7 days:
- 1 mg bid at day 1
- 2 mg bid at day 2
- 4 mg bid at day 3
- 6 mg bid at day 4 (for a target dosage of 12 mg/d)
- 8 mg bid at day 5
- 10 mg bid at day 6
- 12 mg bid at day 7 (for a target dosage of 24 mg/d).
Monitor patients for dose adjustments based on clinical status, concomitant use of other medications (including antipsychotics), and tolerability of up-titration.
The need to titrate iloperidone slowly to reach efficacious acute antipsychotic doses may lead to delayed effectiveness compared with antipsychotics that can be started at therapeutic doses. This problem also may be seen with up-titration of other agents with strong NEα1 properties, including chlorpromazine, clozapine, quetiapine, and risperidone, and should be considered when treating patients who need rapid dose escalation.
Related resource
- Iloperidone (Fanapt) prescribing information. www.fanapt.com/fanapt-pi-may09.pdf.
Drug brand names
- Aripiprazole • Abilify
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Droperidol • Inapsine
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Ketoconazole • Nizoral
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Paroxetine • Paxil
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Weiden receives research support from the National Institute of Mental Health and Ortho-McNeil Janssen. He is a consultant to AstraZeneca, Bristol-Myers Squibb/Otsuka America Pharmaceutical, Eli Lilly and Company, Forest, Ortho-McNeil Janssen, Pfizer Inc., Schering-Plough, Vanda, and Wyeth, and a speaker for Ortho-McNeil Janssen and Pfizer Inc.
Dr. Bishop receives research/grant support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil Janssen.
1. Subramanian N, Kalkman HO. Receptor profile of P88-8991 and P95-12113, metabolites of the novel antipsychotic iloperidone. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26(3):553-560.
2. Kalkman HO, Feuerbach D, Lötscher E. Functional characterization of the novel antipsychotic iloperidone at human D2, D3, alpha 2C, 5-HT6, and 5-HT1A receptors. Life Sci. 2003;73(9):1151-1159.
3. Kalkman HO, Subramanian N, Hoyer D. Extended radioligand binding profile of iloperidone: a broad spectrum dopamine/serotonin/norepinephrine receptor antagonist for the management of psychotic disorders. Neuropsychopharmacology. 2001;25(6):904-914.
4. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals Inc; 2009.
5. Potkin SG, Litman RE, Torres R. Efficacy of iloperidone in the treatment of schizophrenia: initial phase 3 studies. J Clin Psychopharmacol. 2008;28(2 suppl 1):S4-S11.
6. Weiden PJ, Cutler AJ, Polymeropoulos MH. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28(2 suppl 1):S12-19.
7. Hamilton J, Wolfgang C, Feeney J, et al. Efficacy of iloperidone is comparable to risperidone in analyses of a placebo- and risperidone-controlled clinical trial for schizophrenia (pp. NR1-033). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
8. Feeney J, Wolfgang C, Polymeropoulos M, et al. The comparative efficacy of iloperidone and haloperidol across four short-term controlled trials (pp. NR1-026). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
9. Cutler AJ, Kalali AH, Weiden PJ, et al. Four-week, double-blind, placebo- and ziprasidone-controlled trial of iloperidone in patients with acute exacerbations of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S20-28.
10. Torres R, Nasrallah H, Baroldi P. Iloperidone versus haloperidol as long-term maintenance treatment for patients with schizophrenia or schizoaffective disorder (pp. NR4-093). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
11. Kane JM, Lauriello J, Laska E, et al. Long-term efficacy and safety of iloperidone: results from 3 clinical trials for the treatment of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S29-S35.
Iloperidone is a second-generation (atypical) antipsychotic the FDA approved in May 2009 for treating acute schizophrenia in adults (Table 1). Iloperidone is not a derivative (metabolite, isomer, or different formulation) of any other antipsychotic. Clinical trials have shown that iloperidone is efficacious and suggest that for some patients its side-effect profile may be more favorable than that of other antipsychotics.
Table 1
Iloperidone: Fast facts
| Brand name: Fanapt |
| Class: Atypical antipsychotic (serotonin/dopamine antagonist) |
| Indication: Acute schizophrenia in adults |
| Approval date: May 2009 |
| Availability date: Late 2009 |
| Manufacturer: Vanda Pharmaceuticals, Inc. |
| Dosing forms: 1-, 2-, 4-, 6-, 8-, 10-, and 12-mg tablets (nonscored); titration pack of 2×1-mg, 2×2-mg, 2×4-mg, and 2×6-mg tablets |
| Starting dose: 1 mg bid (2 mg total daily dose) |
| Target dose: 12 to 24 mg total daily dose |
Clinical implications
Iloperidone’s binding profile is similar to that of other antipsychotics with relatively stronger affinity for serotonin (5-HT2A) than dopamine (D2) receptors, and its efficacy is roughly comparable to that of other non-clozapine antipsychotics.
Individual patients may respond differently to specific antipsychotics, even when those agents have shown equivalent efficacy in clinical trials. Therefore, a key therapeutic question is the degree of differential efficacy—differences in response at an individual level—among iloperidone and other antipsychotics.
The differential efficacy among iloperidone and other antipsychotics is unknown. Our clinical experience and iloperidone’s unique structure suggest, however, that this agent might be helpful for certain patients who do not fully respond to or are unable to tolerate other antipsychotics.
How iloperidone works
Like other antipsychotics, iloperidone’s efficacy presumably is based on its ability to block [antagonize] dopamine D2 receptors. Its chemical structure is most similar to risperidone, paliperidone, and ziprasidone, but its receptor binding profile is distinguished by a relatively lower affinity for serotonin receptors 5-HT1A and 5-HT2C than ziprasidone, and a relative lack of muscarinic and histaminic antagonist properties (Table 2).
The relatively higher affinity of iloperidone (and its metabolite P95) for the NEα1 receptor correlates with the drug’s propensity to cause orthostatic hypotension during initial up-titration.1 Differences in iloperidone’s receptor binding profile compared with other antipsychotics likely are responsible for its different side-effect profile.2,3
Table 2
Relative receptor binding affinities of 3 atypical antipsychotics*
| Binding affinity | |||
|---|---|---|---|
| Receptor | Risperidone | Ziprasidone | Iloperidone |
| Dopamine D2 | High | High | High |
| Serotonin 5-HT1A | Low | High | Low |
| Serotonin 5-HT2A | High | High | High |
| Serotonin 5-HT2C | Moderate | High | Moderate† |
| Norepinephrine NEα1 | High | Moderate | Moderate‡ |
| Histamine H1 | Moderate | Moderate | Low |
| Muscarinic M1 | Negligible | Negligible | Negligible |
| * Cross-comparison of binding strengths reflects the subjective judgment of the authors. The goal is to demonstrate differences in overall binding patterns, and these estimates should not be considered an exact cross-comparison | |||
| † Published reports of binding affinity of iloperidone show considerable variation for the 5HT2C site | |||
| ‡ One metabolite of iloperidone [P95] does not have CNS activity but has potent alpha-1 antagonism and may contribute to the initial orthostatic hypotension seen in clinical trials | |||
Pharmacokinetics
Iloperidone is administered twice daily and can be taken with or without food. The bioavailability of iloperidone tablets is 96%, and peak plasma concentrations are achieved 2 to 4 hours after ingestion.
Like all antipsychotics except paliperidone, iloperidone is metabolized by the liver’s cytochrome P450 (CYP) system. The enzyme pathways CYP3A4 and CYP2D6 transform iloperidone into 2 metabolites: one with CNS activity (P88) and one that does not cross the blood-brain barrier and is not active in the CNS (P95) but likely has peripheral effects.
Genetic variations in CYP2D6 activity can substantially alter how individual patients metabolize iloperidone. The half-life of iloperidone and its active metabolites differs depending on whether someone is a poor metabolizer (no functional CYP2D6 activity), intermediate metabolizer (reduced CYP2D6 activity), or extensive metabolizer (“normal” CYP2D6 activity). The usual half-life of iloperidone (approximately 18 hours in extensive metabolizers) can be almost 50% longer (>24 hours) in CYP2D6 poor metabolizers.
There are no recommendations to test patients for genetic variants that result in poor metabolism from CYP2D6. Rather, clinicians simply need to be aware that this could be the source of interindividual differences they see in iloperidone tolerability, just as it is for any other medication that is a substrate for the CYP2D6 enzyme system.
Interactions. Medications that inhibit the CYP3A4 or CYP2D6 systems can increase iloperidone plasma level when taken concurrently with iloperidone, even if intrinsic liver metabolism activity is normal. Fluoxetine and paroxetine are potent CYP2D6 inhibitors. Concurrent treatment with either of these selective serotonin reuptake inhibitors could increase iloperidone plasma concentration by 100% or more.4
Similarly, cotreatment with a potent CYP3A4 inhibitor such as ketoconazole (or drinking grapefruit juice) will decrease metabolism and increase plasma concentrations of iloperidone and its active metabolites by about 50%. Smoking status should not influence iloperidone plasma concentration because this drug is not a primary substrate for CYP1A2, the enzyme induced by cigarette smoking.
The bottom line: reduce iloperidone dosage by 50% for patients who are taking a strong CYP2D6 and/or CYP3A4 inhibitor (see Dosing below).
Efficacy
In clinical trials, iloperidone was shown to be efficacious in treating positive and negative symptoms and general psychopathology in acute episodes of schizophrenia. It is important to consider the efficacy studies of iloperidone within the context of the history of its development plan.
Early clinical trials. Most of iloperidone’s phase II and III studies were conducted by Novartis between 1998 and 2002. Initial phase III studies included three 6-week, double-blind, placebo-controlled acute trials comparing a range of iloperidone doses with placebo and an active comparator:5,6
- The first trial compared iloperidone, 4, 8, or 12 mg/d, with placebo or haloperidol, 15 mg/d.
- The second compared iloperidone, 4 to 8 mg/d or 10 to 16 mg/d, with placebo and risperidone, 4 to 8 mg/d.
- The third compared iloperidone, 12 to 16 mg/d or 20 to 24 mg/d, with placebo or risperidone, 6 to 8 mg/d.
These studies totaled 1,066 patients in the iloperidone treatment arms, with target dosages for iloperidone ranging from 4 to 24 mg/d. Iloperidone was more efficacious than placebo for positive, negative, and overall total symptoms on the Positive and Negative Syndrome Scale (PANSS), albeit 4 mg/d and 8 mg/d dosages narrowly missed the .05 significance level.
The haloperidol and risperidone active controls appeared more effective than iloperidone in the original analyses, but these studies were not designed for analysis of comparative efficacy. The protocols for all of these studies used an up-titration schedule for the iloperidone groups that took 1 week to reach steady-state levels, whereas the haloperidol and risperidone groups had a briefer up-titration to target dose.
The interpretation of these studies is complex and a detailed discussion is beyond the scope of this article. However, a post-hoc analysis that included subjects who remained in the study after 2 weeks of double-blind medication showed that iloperidone performed comparably to risperidone7 and haloperidol.8
A new phase III trial. The question remained whether iloperidone was as efficacious as other first-line antipsychotics but had been “penalized” by its slower up-titration schedule and clinical trial design flaws. After acquiring the development rights to iloperidone from Novartis and reviewing prior study designs and results, Vanda Pharmaceuticals designed another phase III study comparing iloperidone with placebo and ziprasidone. Its purpose was to correct for possible design flaws in the previous studies.
Ziprasidone was selected as the active control because of its established efficacy, safety, and twice-daily dosing. In this trial, researchers attempted to match the 2 drugs’ up-titration schedules. Twice-daily doses were given with food as follows:
- iloperidone, 1, 2, 4, 6, 8, 10, and 12 mg (days 1 to 7, respectively)
- ziprasidone, 20 mg (days 1 to 2), 40 mg (days 3 to 4), 60 mg (days 5 to 6), and 80 mg (day 7).
By day 7, target dosages were reached: iloperidone, 24 mg/d, and ziprasidone, 160 mg/d.9
Patients receiving iloperidone showed significantly greater improvement in PANSS total scores at 4 weeks vs those receiving placebo (–12.0, iloperidone; –7.1, placebo; P < .01).9 Patients receiving ziprasidone also achieved significantly greater improvement vs those receiving placebo (–12.3; P < .05 vs placebo).
The iloperidone and ziprasidone groups showed significantly greater improvement from baseline vs placebo in PANSS positive (P) and negative (N) subscale scores. Significantly more patients receiving iloperidone (72%) than placebo (52%) experienced improvement (≥20% reduction from baseline) in PANSS-P scores (P = .005).
Patients receiving iloperidone had a significantly greater reduction in Clinical Global Impression-Severity scale score vs placebo (–0.65 and –0.39, respectively; P = .007), as did patients receiving ziprasidone (–0.67; P = .013).
Iloperidone met all predefined protocol criteria for efficacy vs placebo and had efficacy equal to the highest approved dose of ziprasidone. These results demonstrated that iloperidone has comparable efficacy to ziprasidone and support the validity of the re-analysis of earlier studies showing comparable efficacy between iloperidone and risperidone7 or haloperidol.8 In July 2008 the FDA issued a not approvable letter for iloperidone, requesting further clinical trials because of concerns about the drug’s efficacy compared with risperidone. The FDA approved iloperidone in May 2009 after the manufacturer provided additional data from existing trials that demonstrated comparable efficacy to risperidone.
Long-term efficacy. A double-blind extension study compared patients remaining on blinded iloperidone (4 to 16 mg/d) or haloperidol (5 to 20 mg/d) after completing a 6-week efficacy study.10 The drugs showed equivalent efficacy in preventing relapse over 46 weeks follow-up. Because this study included no placebo group, the FDA does not consider it to be an interpretable relapse prevention study.
Tolerability
Clinicians might consider iloperidone when seeking to switch a patient to an antipsychotic with a potentially lower side-effect burden.6,11 Compared with risperidone, iloperidone has a lower liability for extrapyramidal symptoms (EPS) and does not cause clinically significant prolactin elevation (Table 3).5,7-9 Compared with ziprasidone, iloperidone has a lower EPS and akathisia liability. Somewhat greater weight gain was seen with iloperidone when compared with ziprasidone in a 4-week study (iloperidone, +2.8 kg; ziprasidone, +1.1 kg; placebo, +0.5 kg) but the 2 drugs’ effects on triglycerides and cholesterol were comparable.9
Iloperidone has a similar degree of QTc prolongation as ziprasidone (mean 9 msec at the highest dosage of 12 mg bid). Safety studies including administration of maximal doses of iloperidone with CYP3A4 and CYP2D6 inhibitors showed a mean QTc prolongation of 19 msec without clinically significant problems, and iloperidone has not been associated with serious arrhythmia.4 Iloperidone should not be prescribed to patients with significant cardiac problems or electrolyte disturbances, however, or those taking drugs known to have clinically significant QTc/proarrhythmic properties, such as thioridazine, droperidol, pimozide, or methadone.4
Iloperidone has the same safety concerns associated with other atypical antipsychotics, including tardive dyskinesia and neuroleptic malignant syndrome. Like other atypical antipsychotics, iloperidone carries a warning of increased mortality risk in elderly patients with dementia-related psychosis.
Dose-related side effects include dizziness, orthostatic hypotension, and tachycardia. Dizziness occurred more often at higher doses (20% at 20 to 24 mg/d vs 10% at 10 to 16 mg/d vs 7% in placebo groups). Presumably these side effects are related to NEα1 antagonism and are the basis for the recommended dose-titration schedule described below. Clinical trials do not seem to demonstrate a dose-response relationship for acute EPS or akathisia.
Table 3
Common side effects: Iloperidone vs other antipsychotics*
| Other antipsychotic | Less likely or less severe with iloperidone | More likely or more severe with iloperidone |
|---|---|---|
| Haloperidol4,8 | EPS Akathisia Prolactin elevation | Weight gain Orthostasis |
| Olanzapine | Dyslipidemia Weight gain Sedation | Orthostasis |
| Quetiapine | Dyslipidemia Sedation | EPS |
| Risperidone4,6 | EPS Prolactin elevation Akathisia | None |
| Ziprasidone7 | EPS Akathisia | Weight gain Orthostasis |
| Aripiprazole | Akathisia | Weight gain Orthostasis |
| * Iloperidone has been compared head-to-head with haloperidol, risperidone, and ziprasidone in clinical trials. Other suggested antipsychotic side effect liabilities are based on indirect comparisons | ||
| EPS: extrapyramidal symptoms | ||
The approved dosage range for iloperidone is 12 to 24 mg/d, given as 6 to 12 mg bid. Some trials suggest a dose-response relationship, with 24 mg being more effective than lower target doses.5 Reduce the target dosage of iloperidone by one-half when administering it concomitantly with medications that are strong CYP2D6 or CYP3A4 inhibitors.
Titration schedule. Because iloperidone’s relatively strong NEα1 antagonism creates risk for initial orthostatic hypotension, the drug needs to be titrated to the target dose over 4 to 7 days:
- 1 mg bid at day 1
- 2 mg bid at day 2
- 4 mg bid at day 3
- 6 mg bid at day 4 (for a target dosage of 12 mg/d)
- 8 mg bid at day 5
- 10 mg bid at day 6
- 12 mg bid at day 7 (for a target dosage of 24 mg/d).
Monitor patients for dose adjustments based on clinical status, concomitant use of other medications (including antipsychotics), and tolerability of up-titration.
The need to titrate iloperidone slowly to reach efficacious acute antipsychotic doses may lead to delayed effectiveness compared with antipsychotics that can be started at therapeutic doses. This problem also may be seen with up-titration of other agents with strong NEα1 properties, including chlorpromazine, clozapine, quetiapine, and risperidone, and should be considered when treating patients who need rapid dose escalation.
Related resource
- Iloperidone (Fanapt) prescribing information. www.fanapt.com/fanapt-pi-may09.pdf.
Drug brand names
- Aripiprazole • Abilify
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Droperidol • Inapsine
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Ketoconazole • Nizoral
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Paroxetine • Paxil
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Weiden receives research support from the National Institute of Mental Health and Ortho-McNeil Janssen. He is a consultant to AstraZeneca, Bristol-Myers Squibb/Otsuka America Pharmaceutical, Eli Lilly and Company, Forest, Ortho-McNeil Janssen, Pfizer Inc., Schering-Plough, Vanda, and Wyeth, and a speaker for Ortho-McNeil Janssen and Pfizer Inc.
Dr. Bishop receives research/grant support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil Janssen.
Iloperidone is a second-generation (atypical) antipsychotic the FDA approved in May 2009 for treating acute schizophrenia in adults (Table 1). Iloperidone is not a derivative (metabolite, isomer, or different formulation) of any other antipsychotic. Clinical trials have shown that iloperidone is efficacious and suggest that for some patients its side-effect profile may be more favorable than that of other antipsychotics.
Table 1
Iloperidone: Fast facts
| Brand name: Fanapt |
| Class: Atypical antipsychotic (serotonin/dopamine antagonist) |
| Indication: Acute schizophrenia in adults |
| Approval date: May 2009 |
| Availability date: Late 2009 |
| Manufacturer: Vanda Pharmaceuticals, Inc. |
| Dosing forms: 1-, 2-, 4-, 6-, 8-, 10-, and 12-mg tablets (nonscored); titration pack of 2×1-mg, 2×2-mg, 2×4-mg, and 2×6-mg tablets |
| Starting dose: 1 mg bid (2 mg total daily dose) |
| Target dose: 12 to 24 mg total daily dose |
Clinical implications
Iloperidone’s binding profile is similar to that of other antipsychotics with relatively stronger affinity for serotonin (5-HT2A) than dopamine (D2) receptors, and its efficacy is roughly comparable to that of other non-clozapine antipsychotics.
Individual patients may respond differently to specific antipsychotics, even when those agents have shown equivalent efficacy in clinical trials. Therefore, a key therapeutic question is the degree of differential efficacy—differences in response at an individual level—among iloperidone and other antipsychotics.
The differential efficacy among iloperidone and other antipsychotics is unknown. Our clinical experience and iloperidone’s unique structure suggest, however, that this agent might be helpful for certain patients who do not fully respond to or are unable to tolerate other antipsychotics.
How iloperidone works
Like other antipsychotics, iloperidone’s efficacy presumably is based on its ability to block [antagonize] dopamine D2 receptors. Its chemical structure is most similar to risperidone, paliperidone, and ziprasidone, but its receptor binding profile is distinguished by a relatively lower affinity for serotonin receptors 5-HT1A and 5-HT2C than ziprasidone, and a relative lack of muscarinic and histaminic antagonist properties (Table 2).
The relatively higher affinity of iloperidone (and its metabolite P95) for the NEα1 receptor correlates with the drug’s propensity to cause orthostatic hypotension during initial up-titration.1 Differences in iloperidone’s receptor binding profile compared with other antipsychotics likely are responsible for its different side-effect profile.2,3
Table 2
Relative receptor binding affinities of 3 atypical antipsychotics*
| Binding affinity | |||
|---|---|---|---|
| Receptor | Risperidone | Ziprasidone | Iloperidone |
| Dopamine D2 | High | High | High |
| Serotonin 5-HT1A | Low | High | Low |
| Serotonin 5-HT2A | High | High | High |
| Serotonin 5-HT2C | Moderate | High | Moderate† |
| Norepinephrine NEα1 | High | Moderate | Moderate‡ |
| Histamine H1 | Moderate | Moderate | Low |
| Muscarinic M1 | Negligible | Negligible | Negligible |
| * Cross-comparison of binding strengths reflects the subjective judgment of the authors. The goal is to demonstrate differences in overall binding patterns, and these estimates should not be considered an exact cross-comparison | |||
| † Published reports of binding affinity of iloperidone show considerable variation for the 5HT2C site | |||
| ‡ One metabolite of iloperidone [P95] does not have CNS activity but has potent alpha-1 antagonism and may contribute to the initial orthostatic hypotension seen in clinical trials | |||
Pharmacokinetics
Iloperidone is administered twice daily and can be taken with or without food. The bioavailability of iloperidone tablets is 96%, and peak plasma concentrations are achieved 2 to 4 hours after ingestion.
Like all antipsychotics except paliperidone, iloperidone is metabolized by the liver’s cytochrome P450 (CYP) system. The enzyme pathways CYP3A4 and CYP2D6 transform iloperidone into 2 metabolites: one with CNS activity (P88) and one that does not cross the blood-brain barrier and is not active in the CNS (P95) but likely has peripheral effects.
Genetic variations in CYP2D6 activity can substantially alter how individual patients metabolize iloperidone. The half-life of iloperidone and its active metabolites differs depending on whether someone is a poor metabolizer (no functional CYP2D6 activity), intermediate metabolizer (reduced CYP2D6 activity), or extensive metabolizer (“normal” CYP2D6 activity). The usual half-life of iloperidone (approximately 18 hours in extensive metabolizers) can be almost 50% longer (>24 hours) in CYP2D6 poor metabolizers.
There are no recommendations to test patients for genetic variants that result in poor metabolism from CYP2D6. Rather, clinicians simply need to be aware that this could be the source of interindividual differences they see in iloperidone tolerability, just as it is for any other medication that is a substrate for the CYP2D6 enzyme system.
Interactions. Medications that inhibit the CYP3A4 or CYP2D6 systems can increase iloperidone plasma level when taken concurrently with iloperidone, even if intrinsic liver metabolism activity is normal. Fluoxetine and paroxetine are potent CYP2D6 inhibitors. Concurrent treatment with either of these selective serotonin reuptake inhibitors could increase iloperidone plasma concentration by 100% or more.4
Similarly, cotreatment with a potent CYP3A4 inhibitor such as ketoconazole (or drinking grapefruit juice) will decrease metabolism and increase plasma concentrations of iloperidone and its active metabolites by about 50%. Smoking status should not influence iloperidone plasma concentration because this drug is not a primary substrate for CYP1A2, the enzyme induced by cigarette smoking.
The bottom line: reduce iloperidone dosage by 50% for patients who are taking a strong CYP2D6 and/or CYP3A4 inhibitor (see Dosing below).
Efficacy
In clinical trials, iloperidone was shown to be efficacious in treating positive and negative symptoms and general psychopathology in acute episodes of schizophrenia. It is important to consider the efficacy studies of iloperidone within the context of the history of its development plan.
Early clinical trials. Most of iloperidone’s phase II and III studies were conducted by Novartis between 1998 and 2002. Initial phase III studies included three 6-week, double-blind, placebo-controlled acute trials comparing a range of iloperidone doses with placebo and an active comparator:5,6
- The first trial compared iloperidone, 4, 8, or 12 mg/d, with placebo or haloperidol, 15 mg/d.
- The second compared iloperidone, 4 to 8 mg/d or 10 to 16 mg/d, with placebo and risperidone, 4 to 8 mg/d.
- The third compared iloperidone, 12 to 16 mg/d or 20 to 24 mg/d, with placebo or risperidone, 6 to 8 mg/d.
These studies totaled 1,066 patients in the iloperidone treatment arms, with target dosages for iloperidone ranging from 4 to 24 mg/d. Iloperidone was more efficacious than placebo for positive, negative, and overall total symptoms on the Positive and Negative Syndrome Scale (PANSS), albeit 4 mg/d and 8 mg/d dosages narrowly missed the .05 significance level.
The haloperidol and risperidone active controls appeared more effective than iloperidone in the original analyses, but these studies were not designed for analysis of comparative efficacy. The protocols for all of these studies used an up-titration schedule for the iloperidone groups that took 1 week to reach steady-state levels, whereas the haloperidol and risperidone groups had a briefer up-titration to target dose.
The interpretation of these studies is complex and a detailed discussion is beyond the scope of this article. However, a post-hoc analysis that included subjects who remained in the study after 2 weeks of double-blind medication showed that iloperidone performed comparably to risperidone7 and haloperidol.8
A new phase III trial. The question remained whether iloperidone was as efficacious as other first-line antipsychotics but had been “penalized” by its slower up-titration schedule and clinical trial design flaws. After acquiring the development rights to iloperidone from Novartis and reviewing prior study designs and results, Vanda Pharmaceuticals designed another phase III study comparing iloperidone with placebo and ziprasidone. Its purpose was to correct for possible design flaws in the previous studies.
Ziprasidone was selected as the active control because of its established efficacy, safety, and twice-daily dosing. In this trial, researchers attempted to match the 2 drugs’ up-titration schedules. Twice-daily doses were given with food as follows:
- iloperidone, 1, 2, 4, 6, 8, 10, and 12 mg (days 1 to 7, respectively)
- ziprasidone, 20 mg (days 1 to 2), 40 mg (days 3 to 4), 60 mg (days 5 to 6), and 80 mg (day 7).
By day 7, target dosages were reached: iloperidone, 24 mg/d, and ziprasidone, 160 mg/d.9
Patients receiving iloperidone showed significantly greater improvement in PANSS total scores at 4 weeks vs those receiving placebo (–12.0, iloperidone; –7.1, placebo; P < .01).9 Patients receiving ziprasidone also achieved significantly greater improvement vs those receiving placebo (–12.3; P < .05 vs placebo).
The iloperidone and ziprasidone groups showed significantly greater improvement from baseline vs placebo in PANSS positive (P) and negative (N) subscale scores. Significantly more patients receiving iloperidone (72%) than placebo (52%) experienced improvement (≥20% reduction from baseline) in PANSS-P scores (P = .005).
Patients receiving iloperidone had a significantly greater reduction in Clinical Global Impression-Severity scale score vs placebo (–0.65 and –0.39, respectively; P = .007), as did patients receiving ziprasidone (–0.67; P = .013).
Iloperidone met all predefined protocol criteria for efficacy vs placebo and had efficacy equal to the highest approved dose of ziprasidone. These results demonstrated that iloperidone has comparable efficacy to ziprasidone and support the validity of the re-analysis of earlier studies showing comparable efficacy between iloperidone and risperidone7 or haloperidol.8 In July 2008 the FDA issued a not approvable letter for iloperidone, requesting further clinical trials because of concerns about the drug’s efficacy compared with risperidone. The FDA approved iloperidone in May 2009 after the manufacturer provided additional data from existing trials that demonstrated comparable efficacy to risperidone.
Long-term efficacy. A double-blind extension study compared patients remaining on blinded iloperidone (4 to 16 mg/d) or haloperidol (5 to 20 mg/d) after completing a 6-week efficacy study.10 The drugs showed equivalent efficacy in preventing relapse over 46 weeks follow-up. Because this study included no placebo group, the FDA does not consider it to be an interpretable relapse prevention study.
Tolerability
Clinicians might consider iloperidone when seeking to switch a patient to an antipsychotic with a potentially lower side-effect burden.6,11 Compared with risperidone, iloperidone has a lower liability for extrapyramidal symptoms (EPS) and does not cause clinically significant prolactin elevation (Table 3).5,7-9 Compared with ziprasidone, iloperidone has a lower EPS and akathisia liability. Somewhat greater weight gain was seen with iloperidone when compared with ziprasidone in a 4-week study (iloperidone, +2.8 kg; ziprasidone, +1.1 kg; placebo, +0.5 kg) but the 2 drugs’ effects on triglycerides and cholesterol were comparable.9
Iloperidone has a similar degree of QTc prolongation as ziprasidone (mean 9 msec at the highest dosage of 12 mg bid). Safety studies including administration of maximal doses of iloperidone with CYP3A4 and CYP2D6 inhibitors showed a mean QTc prolongation of 19 msec without clinically significant problems, and iloperidone has not been associated with serious arrhythmia.4 Iloperidone should not be prescribed to patients with significant cardiac problems or electrolyte disturbances, however, or those taking drugs known to have clinically significant QTc/proarrhythmic properties, such as thioridazine, droperidol, pimozide, or methadone.4
Iloperidone has the same safety concerns associated with other atypical antipsychotics, including tardive dyskinesia and neuroleptic malignant syndrome. Like other atypical antipsychotics, iloperidone carries a warning of increased mortality risk in elderly patients with dementia-related psychosis.
Dose-related side effects include dizziness, orthostatic hypotension, and tachycardia. Dizziness occurred more often at higher doses (20% at 20 to 24 mg/d vs 10% at 10 to 16 mg/d vs 7% in placebo groups). Presumably these side effects are related to NEα1 antagonism and are the basis for the recommended dose-titration schedule described below. Clinical trials do not seem to demonstrate a dose-response relationship for acute EPS or akathisia.
Table 3
Common side effects: Iloperidone vs other antipsychotics*
| Other antipsychotic | Less likely or less severe with iloperidone | More likely or more severe with iloperidone |
|---|---|---|
| Haloperidol4,8 | EPS Akathisia Prolactin elevation | Weight gain Orthostasis |
| Olanzapine | Dyslipidemia Weight gain Sedation | Orthostasis |
| Quetiapine | Dyslipidemia Sedation | EPS |
| Risperidone4,6 | EPS Prolactin elevation Akathisia | None |
| Ziprasidone7 | EPS Akathisia | Weight gain Orthostasis |
| Aripiprazole | Akathisia | Weight gain Orthostasis |
| * Iloperidone has been compared head-to-head with haloperidol, risperidone, and ziprasidone in clinical trials. Other suggested antipsychotic side effect liabilities are based on indirect comparisons | ||
| EPS: extrapyramidal symptoms | ||
The approved dosage range for iloperidone is 12 to 24 mg/d, given as 6 to 12 mg bid. Some trials suggest a dose-response relationship, with 24 mg being more effective than lower target doses.5 Reduce the target dosage of iloperidone by one-half when administering it concomitantly with medications that are strong CYP2D6 or CYP3A4 inhibitors.
Titration schedule. Because iloperidone’s relatively strong NEα1 antagonism creates risk for initial orthostatic hypotension, the drug needs to be titrated to the target dose over 4 to 7 days:
- 1 mg bid at day 1
- 2 mg bid at day 2
- 4 mg bid at day 3
- 6 mg bid at day 4 (for a target dosage of 12 mg/d)
- 8 mg bid at day 5
- 10 mg bid at day 6
- 12 mg bid at day 7 (for a target dosage of 24 mg/d).
Monitor patients for dose adjustments based on clinical status, concomitant use of other medications (including antipsychotics), and tolerability of up-titration.
The need to titrate iloperidone slowly to reach efficacious acute antipsychotic doses may lead to delayed effectiveness compared with antipsychotics that can be started at therapeutic doses. This problem also may be seen with up-titration of other agents with strong NEα1 properties, including chlorpromazine, clozapine, quetiapine, and risperidone, and should be considered when treating patients who need rapid dose escalation.
Related resource
- Iloperidone (Fanapt) prescribing information. www.fanapt.com/fanapt-pi-may09.pdf.
Drug brand names
- Aripiprazole • Abilify
- Chlorpromazine • Thorazine
- Clozapine • Clozaril
- Droperidol • Inapsine
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Iloperidone • Fanapt
- Ketoconazole • Nizoral
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paliperidone • Invega
- Paroxetine • Paxil
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosures
Dr. Weiden receives research support from the National Institute of Mental Health and Ortho-McNeil Janssen. He is a consultant to AstraZeneca, Bristol-Myers Squibb/Otsuka America Pharmaceutical, Eli Lilly and Company, Forest, Ortho-McNeil Janssen, Pfizer Inc., Schering-Plough, Vanda, and Wyeth, and a speaker for Ortho-McNeil Janssen and Pfizer Inc.
Dr. Bishop receives research/grant support from the National Institute of Mental Health, NARSAD, and Ortho-McNeil Janssen.
1. Subramanian N, Kalkman HO. Receptor profile of P88-8991 and P95-12113, metabolites of the novel antipsychotic iloperidone. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26(3):553-560.
2. Kalkman HO, Feuerbach D, Lötscher E. Functional characterization of the novel antipsychotic iloperidone at human D2, D3, alpha 2C, 5-HT6, and 5-HT1A receptors. Life Sci. 2003;73(9):1151-1159.
3. Kalkman HO, Subramanian N, Hoyer D. Extended radioligand binding profile of iloperidone: a broad spectrum dopamine/serotonin/norepinephrine receptor antagonist for the management of psychotic disorders. Neuropsychopharmacology. 2001;25(6):904-914.
4. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals Inc; 2009.
5. Potkin SG, Litman RE, Torres R. Efficacy of iloperidone in the treatment of schizophrenia: initial phase 3 studies. J Clin Psychopharmacol. 2008;28(2 suppl 1):S4-S11.
6. Weiden PJ, Cutler AJ, Polymeropoulos MH. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28(2 suppl 1):S12-19.
7. Hamilton J, Wolfgang C, Feeney J, et al. Efficacy of iloperidone is comparable to risperidone in analyses of a placebo- and risperidone-controlled clinical trial for schizophrenia (pp. NR1-033). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
8. Feeney J, Wolfgang C, Polymeropoulos M, et al. The comparative efficacy of iloperidone and haloperidol across four short-term controlled trials (pp. NR1-026). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
9. Cutler AJ, Kalali AH, Weiden PJ, et al. Four-week, double-blind, placebo- and ziprasidone-controlled trial of iloperidone in patients with acute exacerbations of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S20-28.
10. Torres R, Nasrallah H, Baroldi P. Iloperidone versus haloperidol as long-term maintenance treatment for patients with schizophrenia or schizoaffective disorder (pp. NR4-093). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
11. Kane JM, Lauriello J, Laska E, et al. Long-term efficacy and safety of iloperidone: results from 3 clinical trials for the treatment of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S29-S35.
1. Subramanian N, Kalkman HO. Receptor profile of P88-8991 and P95-12113, metabolites of the novel antipsychotic iloperidone. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26(3):553-560.
2. Kalkman HO, Feuerbach D, Lötscher E. Functional characterization of the novel antipsychotic iloperidone at human D2, D3, alpha 2C, 5-HT6, and 5-HT1A receptors. Life Sci. 2003;73(9):1151-1159.
3. Kalkman HO, Subramanian N, Hoyer D. Extended radioligand binding profile of iloperidone: a broad spectrum dopamine/serotonin/norepinephrine receptor antagonist for the management of psychotic disorders. Neuropsychopharmacology. 2001;25(6):904-914.
4. Fanapt [package insert]. Rockville, MD: Vanda Pharmaceuticals Inc; 2009.
5. Potkin SG, Litman RE, Torres R. Efficacy of iloperidone in the treatment of schizophrenia: initial phase 3 studies. J Clin Psychopharmacol. 2008;28(2 suppl 1):S4-S11.
6. Weiden PJ, Cutler AJ, Polymeropoulos MH. Safety profile of iloperidone: a pooled analysis of 6-week acute-phase pivotal trials. J Clin Psychopharmacol. 2008;28(2 suppl 1):S12-19.
7. Hamilton J, Wolfgang C, Feeney J, et al. Efficacy of iloperidone is comparable to risperidone in analyses of a placebo- and risperidone-controlled clinical trial for schizophrenia (pp. NR1-033). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
8. Feeney J, Wolfgang C, Polymeropoulos M, et al. The comparative efficacy of iloperidone and haloperidol across four short-term controlled trials (pp. NR1-026). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
9. Cutler AJ, Kalali AH, Weiden PJ, et al. Four-week, double-blind, placebo- and ziprasidone-controlled trial of iloperidone in patients with acute exacerbations of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S20-28.
10. Torres R, Nasrallah H, Baroldi P. Iloperidone versus haloperidol as long-term maintenance treatment for patients with schizophrenia or schizoaffective disorder (pp. NR4-093). Presented at: American Psychiatric Association Annual Meeting; May 16-21, 2009; San Francisco, CA.
11. Kane JM, Lauriello J, Laska E, et al. Long-term efficacy and safety of iloperidone: results from 3 clinical trials for the treatment of schizophrenia. J Clin Psychopharmacol. 2008;28(2 suppl 1):S29-S35.
Transcranial magnetic stimulation for depression
Only 28% to 33% of patients with major depression experience remission after their first antidepressant treatment, according to results of the Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial.1 Therapeutic options include switching to an alternate antidepressant, augmentation with a second antidepressant, psychotherapy, mood stabilizers, or second-generation antipsychotics.
In October 2008, the FDA approved a new option: transcranial magnetic stimulation (NeuroStar TMS Therapy), a neuro-modulation approach indicated for patients with major depressive disorder (MDD) who failed 1 adequate antidepressant trial in the current episode (Table 1).
Table 1
Transcranial magnetic stimulation: Fast facts
| Brand name: NeuroStar TMS Therapy |
| Class: Class II medical device |
| Indication: Treatment of major depressive disorder in adults who failed to achieve satisfactory improvement from 1 prior antidepressant medication at or above the minimal effective dose and duration in the current depressive episode |
| Approval date: October 7, 2008 |
| Availability: Limited number of treatment centers; see www.NeuroStarTMS.com |
| Manufacturer: Neuronetics, Inc. |
| Recommended dose: 75 10-Hz, 4-second trains; 26-second intertrain interval; administered over the left dorsolateral prefrontal cortex; 5 days a week, up to 6 weeks |
How it works
TMS delivers intense intermittent magnetic pulses produced by an electrical charge into a ferromagnetic coil. The intensity of the pulse is similar to that of MRI (1.5 to 2 tesla); however, in MRI the magnetic field is constantly on, whereas in TMS the field is exceptionally brief (milliseconds).
For depression treatment, the coil is usually placed on the scalp over the left dorsolateral prefrontal cortex (DLPFC). Pulses are delivered in a rapid, repetitive train, causing neuronal depolarization in a small area of the cerebral cortex and distal effects in other neurocircuits.
For depression, standard outpatient treatment consists of 5 daily sessions per week for up to 6 weeks. Each session takes approximately 40 minutes, and patients typically return to normal daily activities without difficulty. Initially, NeuroStar TMS will be available in a limited number of treatment centers (see Related Resource).
Intensity of treatment is individualized by adjusting parameters that affect delivery of the magnetic pulses. Motor threshold (MT) is the level of stimulation required to produce movement in a contralateral target muscle, such as the abductor pollicis brevis that causes contraction of the thumb. Once this level is determined, pulses are administered at an intensity relative to the MT (such as 120%). Single TMS pulses are used to find the relevant area of the motor cortex, whereas repetitive pulses are applied over the left DLPFC for therapy.
Frequency of stimulation is measured in cycles per second or hertz (Hz). Stimulation train is the duration during which pulses are administered, and the intertrain interval (ITI) is the time between stimulation trains. Other parameters include site of stimulation and number of treatments per day, week, and course. Recommended treatment levels appear in (Table 2).
Table 2
TMS depression treatment parameters
| Parameter | Definition | Recommended treatment level | |
|---|---|---|---|
| Motor threshold | Level of stimulation required to produce contractions in the contralateral target muscle (abductor pollicis brevis, which causes contraction of the thumb) | 120% | |
| Frequency of stimulation | Measured in cycles per second or hertz (Hz) | 10 Hz | |
| Stimulation train | Duration of the stimulation | 4 seconds | |
| Intertrain interval | Time between stimulation trains | 26 seconds | |
| Site of stimulation | Where in the brain the stimulation will occur | Left dorsolateral prefrontal cortex | |
| Number of treatments | How many times the patient receives stimulation/treatment | 5 days per week for up to 6 weeks | |
| Total stimulation time | Number of stimulations given in a session | 3,000 stimulations per session | |
| TMS: transcranial magnetic stimulation | |||
Efficacy
George et al2 first reported TMS for depression in 1995. Initial small, open-label studies examined a variety of treatment intensities, durations, and stimulation sites. Several sham-controlled studies further refined treatment parameters. These studies generally found TMS efficacious, but questioned the robustness of the clinical effect.
To better assess the antidepressant effect of TMS, studies employed larger samples and more aggressive treatment parameters. Avery et al3 randomized 68 patients to 15 sessions of active or sham TMS over the left DLPFC. Each treatment consisted of 32 10-Hz, 5-second trains at 110% MT with a 25-second ITI. At 1 and 2 weeks after treatment, 31% of subjects in the active treatment group showed a significant decrease in symptoms—defined as ≥50% reduction in Hamilton Depression Rating Scale (HDRS) score—versus 6% in the sham group. In addition, 20% of subjects in the active TMS group achieved remission (defined as HDRS score
The largest trial of TMS monotherapy (N=301) for moderately treatment-resistant major depression was completed in 2007.4 This 3-phase study began with a 4- to 6-week, randomized, double-blind activeversus-sham TMS procedure, followed by 6 weeks of open-label TMS in initial nonresponders. The third phase reintroduced TMS over 6 months as needed to augment maintenance antidepressant medication.
This trial used the most aggressive treatment parameters to date: 75 10-Hz, 4-second trains at 120% MT with a 26-second ITI, delivering 3,000 pulses per treatment over an average of 26 sessions. To maintain an adequate blind, the study utilized sham and active coils with similar appearances, placement, and acoustic properties. The sham coil had an embedded aluminum shield, which limited the magnetic energy reaching the cortex to ≤10% of the active coil. Although there was no assessment of the adequacy of the blind in this trial:
- subjects were naive to TMS in the sham-controlled phase
- TMS operators did not assess efficacy
- TMS operators and subjects did not discuss the treatment experience with the efficacy raters.
Compared with those who received the sham procedure, subjects who received active TMS showed significantly better response rates on the Montgomery-Åsberg Depression Rating Scale (MADRS) at weeks 4 and 6. Similar results were found for the 17- and 24-item HDRS. At 6 weeks, the remission rate (defined as a MADRS score
A post-hoc analysis found that the greatest benefit occurred in patients who had only 1 failed adequate antidepressant trial (effect size=0.83).5
TMS vs ECT. Dowd et al6 summarized 8 published trials that compared TMS with electroconvulsive therapy (ECT) for severe depression:
- 5 reported equivalent efficacy
- 1 found unilateral ECT (UL-ECT) and bilateral ECT (BL-ECT) superior to TMS
- 1 reported UL-ECT superior to TMS
- 1 found UL-ECT plus medication superior to TMS monotherapy in patients with psychosis but comparable in efficacy to TMS in the absence of psychosis.
These results need to be interpreted with caution because of the studies’ diverse designs, nonblinded assessments, and small sample sizes.
Tolerability and safety
The most frequently reported adverse effects of TMS are headache and pain at the site of stimulation. Seizures had been reported in early trials, but the extremely low occurrence has been much lower since Wasserman7 published consensus guidelines on the safe use of TMS in 1996.
Janicak et al8 examined safety data from the 3-phase trial mentioned above, which included >10,000 cumulative treatment sessions. TMS was well-tolerated, with a low discontinuation rate associated with adverse effects: 4.5% in the active treatment group versus 3.4% in the sham TMS procedure group. No deaths, seizures, or cases of treatment-emergent mania occurred. The most commonly reported adverse effects were transient headache and discomfort at the stimulation site. Most patients acclimated to these effects in the first week. No changes were seen in cognitive functioning or auditory thresholds.
As in previous studies, TMS was safely combined with antidepressants in the third phase of this trial; however, patients at risk for seizure or on medications that could lower the seizure threshold were excluded. Thus, risk of seizure may be increased under these conditions. TMS is contraindicated for patients with implanted metallic devices or nonremovable objects in or around the head, except for dental hardware or braces.
- For availability information, contact the manufacturer, Neuronetics, at (877) 6000-7555 or www.NeuroStarTMS.com.
Disclosures
Drs. Dowd, Rado, and Janicak receive research support from and are consultants to Neuronetics, Inc.
Dr. Welch receives research support from Neuronetics, Inc.
1. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163(1):28-40.
2. George MS, Wassermann EM, Williams WA, et al. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport 1995;6(14):1853-6.
3. Avery DH, Holtzheimer PE, III, Fawaz W, et al. A controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depression. Biol Psychiatry 2006;59:187-94.
4. O’Reardon JP, Solvason HB, Janicak PG, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multi-site randomized controlled trial. Biol Psychiatry 2007;62:1208-16.
5. Lisanby SH, Husain MM, Rosenquist PB, et al. Daily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trial. Neuropsychopharmacology Epub 2008 Aug 13.
6. Dowd SM, Janicak PG. Transcranial magnetic stimulation for major depression: part II. Psychopharm Review 2007;42(1):1-8.
7. Wasserman EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5-7, 1996. Electroencephalogr Clin Neurophysiol 1998;108(1):1-16.
8. Janicak PG, O’Reardon JP, Sampson SM, et al. Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction. J Clin Psychiatry 2008;69:222-33.
Only 28% to 33% of patients with major depression experience remission after their first antidepressant treatment, according to results of the Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial.1 Therapeutic options include switching to an alternate antidepressant, augmentation with a second antidepressant, psychotherapy, mood stabilizers, or second-generation antipsychotics.
In October 2008, the FDA approved a new option: transcranial magnetic stimulation (NeuroStar TMS Therapy), a neuro-modulation approach indicated for patients with major depressive disorder (MDD) who failed 1 adequate antidepressant trial in the current episode (Table 1).
Table 1
Transcranial magnetic stimulation: Fast facts
| Brand name: NeuroStar TMS Therapy |
| Class: Class II medical device |
| Indication: Treatment of major depressive disorder in adults who failed to achieve satisfactory improvement from 1 prior antidepressant medication at or above the minimal effective dose and duration in the current depressive episode |
| Approval date: October 7, 2008 |
| Availability: Limited number of treatment centers; see www.NeuroStarTMS.com |
| Manufacturer: Neuronetics, Inc. |
| Recommended dose: 75 10-Hz, 4-second trains; 26-second intertrain interval; administered over the left dorsolateral prefrontal cortex; 5 days a week, up to 6 weeks |
How it works
TMS delivers intense intermittent magnetic pulses produced by an electrical charge into a ferromagnetic coil. The intensity of the pulse is similar to that of MRI (1.5 to 2 tesla); however, in MRI the magnetic field is constantly on, whereas in TMS the field is exceptionally brief (milliseconds).
For depression treatment, the coil is usually placed on the scalp over the left dorsolateral prefrontal cortex (DLPFC). Pulses are delivered in a rapid, repetitive train, causing neuronal depolarization in a small area of the cerebral cortex and distal effects in other neurocircuits.
For depression, standard outpatient treatment consists of 5 daily sessions per week for up to 6 weeks. Each session takes approximately 40 minutes, and patients typically return to normal daily activities without difficulty. Initially, NeuroStar TMS will be available in a limited number of treatment centers (see Related Resource).
Intensity of treatment is individualized by adjusting parameters that affect delivery of the magnetic pulses. Motor threshold (MT) is the level of stimulation required to produce movement in a contralateral target muscle, such as the abductor pollicis brevis that causes contraction of the thumb. Once this level is determined, pulses are administered at an intensity relative to the MT (such as 120%). Single TMS pulses are used to find the relevant area of the motor cortex, whereas repetitive pulses are applied over the left DLPFC for therapy.
Frequency of stimulation is measured in cycles per second or hertz (Hz). Stimulation train is the duration during which pulses are administered, and the intertrain interval (ITI) is the time between stimulation trains. Other parameters include site of stimulation and number of treatments per day, week, and course. Recommended treatment levels appear in (Table 2).
Table 2
TMS depression treatment parameters
| Parameter | Definition | Recommended treatment level | |
|---|---|---|---|
| Motor threshold | Level of stimulation required to produce contractions in the contralateral target muscle (abductor pollicis brevis, which causes contraction of the thumb) | 120% | |
| Frequency of stimulation | Measured in cycles per second or hertz (Hz) | 10 Hz | |
| Stimulation train | Duration of the stimulation | 4 seconds | |
| Intertrain interval | Time between stimulation trains | 26 seconds | |
| Site of stimulation | Where in the brain the stimulation will occur | Left dorsolateral prefrontal cortex | |
| Number of treatments | How many times the patient receives stimulation/treatment | 5 days per week for up to 6 weeks | |
| Total stimulation time | Number of stimulations given in a session | 3,000 stimulations per session | |
| TMS: transcranial magnetic stimulation | |||
Efficacy
George et al2 first reported TMS for depression in 1995. Initial small, open-label studies examined a variety of treatment intensities, durations, and stimulation sites. Several sham-controlled studies further refined treatment parameters. These studies generally found TMS efficacious, but questioned the robustness of the clinical effect.
To better assess the antidepressant effect of TMS, studies employed larger samples and more aggressive treatment parameters. Avery et al3 randomized 68 patients to 15 sessions of active or sham TMS over the left DLPFC. Each treatment consisted of 32 10-Hz, 5-second trains at 110% MT with a 25-second ITI. At 1 and 2 weeks after treatment, 31% of subjects in the active treatment group showed a significant decrease in symptoms—defined as ≥50% reduction in Hamilton Depression Rating Scale (HDRS) score—versus 6% in the sham group. In addition, 20% of subjects in the active TMS group achieved remission (defined as HDRS score
The largest trial of TMS monotherapy (N=301) for moderately treatment-resistant major depression was completed in 2007.4 This 3-phase study began with a 4- to 6-week, randomized, double-blind activeversus-sham TMS procedure, followed by 6 weeks of open-label TMS in initial nonresponders. The third phase reintroduced TMS over 6 months as needed to augment maintenance antidepressant medication.
This trial used the most aggressive treatment parameters to date: 75 10-Hz, 4-second trains at 120% MT with a 26-second ITI, delivering 3,000 pulses per treatment over an average of 26 sessions. To maintain an adequate blind, the study utilized sham and active coils with similar appearances, placement, and acoustic properties. The sham coil had an embedded aluminum shield, which limited the magnetic energy reaching the cortex to ≤10% of the active coil. Although there was no assessment of the adequacy of the blind in this trial:
- subjects were naive to TMS in the sham-controlled phase
- TMS operators did not assess efficacy
- TMS operators and subjects did not discuss the treatment experience with the efficacy raters.
Compared with those who received the sham procedure, subjects who received active TMS showed significantly better response rates on the Montgomery-Åsberg Depression Rating Scale (MADRS) at weeks 4 and 6. Similar results were found for the 17- and 24-item HDRS. At 6 weeks, the remission rate (defined as a MADRS score
A post-hoc analysis found that the greatest benefit occurred in patients who had only 1 failed adequate antidepressant trial (effect size=0.83).5
TMS vs ECT. Dowd et al6 summarized 8 published trials that compared TMS with electroconvulsive therapy (ECT) for severe depression:
- 5 reported equivalent efficacy
- 1 found unilateral ECT (UL-ECT) and bilateral ECT (BL-ECT) superior to TMS
- 1 reported UL-ECT superior to TMS
- 1 found UL-ECT plus medication superior to TMS monotherapy in patients with psychosis but comparable in efficacy to TMS in the absence of psychosis.
These results need to be interpreted with caution because of the studies’ diverse designs, nonblinded assessments, and small sample sizes.
Tolerability and safety
The most frequently reported adverse effects of TMS are headache and pain at the site of stimulation. Seizures had been reported in early trials, but the extremely low occurrence has been much lower since Wasserman7 published consensus guidelines on the safe use of TMS in 1996.
Janicak et al8 examined safety data from the 3-phase trial mentioned above, which included >10,000 cumulative treatment sessions. TMS was well-tolerated, with a low discontinuation rate associated with adverse effects: 4.5% in the active treatment group versus 3.4% in the sham TMS procedure group. No deaths, seizures, or cases of treatment-emergent mania occurred. The most commonly reported adverse effects were transient headache and discomfort at the stimulation site. Most patients acclimated to these effects in the first week. No changes were seen in cognitive functioning or auditory thresholds.
As in previous studies, TMS was safely combined with antidepressants in the third phase of this trial; however, patients at risk for seizure or on medications that could lower the seizure threshold were excluded. Thus, risk of seizure may be increased under these conditions. TMS is contraindicated for patients with implanted metallic devices or nonremovable objects in or around the head, except for dental hardware or braces.
- For availability information, contact the manufacturer, Neuronetics, at (877) 6000-7555 or www.NeuroStarTMS.com.
Disclosures
Drs. Dowd, Rado, and Janicak receive research support from and are consultants to Neuronetics, Inc.
Dr. Welch receives research support from Neuronetics, Inc.
Only 28% to 33% of patients with major depression experience remission after their first antidepressant treatment, according to results of the Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial.1 Therapeutic options include switching to an alternate antidepressant, augmentation with a second antidepressant, psychotherapy, mood stabilizers, or second-generation antipsychotics.
In October 2008, the FDA approved a new option: transcranial magnetic stimulation (NeuroStar TMS Therapy), a neuro-modulation approach indicated for patients with major depressive disorder (MDD) who failed 1 adequate antidepressant trial in the current episode (Table 1).
Table 1
Transcranial magnetic stimulation: Fast facts
| Brand name: NeuroStar TMS Therapy |
| Class: Class II medical device |
| Indication: Treatment of major depressive disorder in adults who failed to achieve satisfactory improvement from 1 prior antidepressant medication at or above the minimal effective dose and duration in the current depressive episode |
| Approval date: October 7, 2008 |
| Availability: Limited number of treatment centers; see www.NeuroStarTMS.com |
| Manufacturer: Neuronetics, Inc. |
| Recommended dose: 75 10-Hz, 4-second trains; 26-second intertrain interval; administered over the left dorsolateral prefrontal cortex; 5 days a week, up to 6 weeks |
How it works
TMS delivers intense intermittent magnetic pulses produced by an electrical charge into a ferromagnetic coil. The intensity of the pulse is similar to that of MRI (1.5 to 2 tesla); however, in MRI the magnetic field is constantly on, whereas in TMS the field is exceptionally brief (milliseconds).
For depression treatment, the coil is usually placed on the scalp over the left dorsolateral prefrontal cortex (DLPFC). Pulses are delivered in a rapid, repetitive train, causing neuronal depolarization in a small area of the cerebral cortex and distal effects in other neurocircuits.
For depression, standard outpatient treatment consists of 5 daily sessions per week for up to 6 weeks. Each session takes approximately 40 minutes, and patients typically return to normal daily activities without difficulty. Initially, NeuroStar TMS will be available in a limited number of treatment centers (see Related Resource).
Intensity of treatment is individualized by adjusting parameters that affect delivery of the magnetic pulses. Motor threshold (MT) is the level of stimulation required to produce movement in a contralateral target muscle, such as the abductor pollicis brevis that causes contraction of the thumb. Once this level is determined, pulses are administered at an intensity relative to the MT (such as 120%). Single TMS pulses are used to find the relevant area of the motor cortex, whereas repetitive pulses are applied over the left DLPFC for therapy.
Frequency of stimulation is measured in cycles per second or hertz (Hz). Stimulation train is the duration during which pulses are administered, and the intertrain interval (ITI) is the time between stimulation trains. Other parameters include site of stimulation and number of treatments per day, week, and course. Recommended treatment levels appear in (Table 2).
Table 2
TMS depression treatment parameters
| Parameter | Definition | Recommended treatment level | |
|---|---|---|---|
| Motor threshold | Level of stimulation required to produce contractions in the contralateral target muscle (abductor pollicis brevis, which causes contraction of the thumb) | 120% | |
| Frequency of stimulation | Measured in cycles per second or hertz (Hz) | 10 Hz | |
| Stimulation train | Duration of the stimulation | 4 seconds | |
| Intertrain interval | Time between stimulation trains | 26 seconds | |
| Site of stimulation | Where in the brain the stimulation will occur | Left dorsolateral prefrontal cortex | |
| Number of treatments | How many times the patient receives stimulation/treatment | 5 days per week for up to 6 weeks | |
| Total stimulation time | Number of stimulations given in a session | 3,000 stimulations per session | |
| TMS: transcranial magnetic stimulation | |||
Efficacy
George et al2 first reported TMS for depression in 1995. Initial small, open-label studies examined a variety of treatment intensities, durations, and stimulation sites. Several sham-controlled studies further refined treatment parameters. These studies generally found TMS efficacious, but questioned the robustness of the clinical effect.
To better assess the antidepressant effect of TMS, studies employed larger samples and more aggressive treatment parameters. Avery et al3 randomized 68 patients to 15 sessions of active or sham TMS over the left DLPFC. Each treatment consisted of 32 10-Hz, 5-second trains at 110% MT with a 25-second ITI. At 1 and 2 weeks after treatment, 31% of subjects in the active treatment group showed a significant decrease in symptoms—defined as ≥50% reduction in Hamilton Depression Rating Scale (HDRS) score—versus 6% in the sham group. In addition, 20% of subjects in the active TMS group achieved remission (defined as HDRS score
The largest trial of TMS monotherapy (N=301) for moderately treatment-resistant major depression was completed in 2007.4 This 3-phase study began with a 4- to 6-week, randomized, double-blind activeversus-sham TMS procedure, followed by 6 weeks of open-label TMS in initial nonresponders. The third phase reintroduced TMS over 6 months as needed to augment maintenance antidepressant medication.
This trial used the most aggressive treatment parameters to date: 75 10-Hz, 4-second trains at 120% MT with a 26-second ITI, delivering 3,000 pulses per treatment over an average of 26 sessions. To maintain an adequate blind, the study utilized sham and active coils with similar appearances, placement, and acoustic properties. The sham coil had an embedded aluminum shield, which limited the magnetic energy reaching the cortex to ≤10% of the active coil. Although there was no assessment of the adequacy of the blind in this trial:
- subjects were naive to TMS in the sham-controlled phase
- TMS operators did not assess efficacy
- TMS operators and subjects did not discuss the treatment experience with the efficacy raters.
Compared with those who received the sham procedure, subjects who received active TMS showed significantly better response rates on the Montgomery-Åsberg Depression Rating Scale (MADRS) at weeks 4 and 6. Similar results were found for the 17- and 24-item HDRS. At 6 weeks, the remission rate (defined as a MADRS score
A post-hoc analysis found that the greatest benefit occurred in patients who had only 1 failed adequate antidepressant trial (effect size=0.83).5
TMS vs ECT. Dowd et al6 summarized 8 published trials that compared TMS with electroconvulsive therapy (ECT) for severe depression:
- 5 reported equivalent efficacy
- 1 found unilateral ECT (UL-ECT) and bilateral ECT (BL-ECT) superior to TMS
- 1 reported UL-ECT superior to TMS
- 1 found UL-ECT plus medication superior to TMS monotherapy in patients with psychosis but comparable in efficacy to TMS in the absence of psychosis.
These results need to be interpreted with caution because of the studies’ diverse designs, nonblinded assessments, and small sample sizes.
Tolerability and safety
The most frequently reported adverse effects of TMS are headache and pain at the site of stimulation. Seizures had been reported in early trials, but the extremely low occurrence has been much lower since Wasserman7 published consensus guidelines on the safe use of TMS in 1996.
Janicak et al8 examined safety data from the 3-phase trial mentioned above, which included >10,000 cumulative treatment sessions. TMS was well-tolerated, with a low discontinuation rate associated with adverse effects: 4.5% in the active treatment group versus 3.4% in the sham TMS procedure group. No deaths, seizures, or cases of treatment-emergent mania occurred. The most commonly reported adverse effects were transient headache and discomfort at the stimulation site. Most patients acclimated to these effects in the first week. No changes were seen in cognitive functioning or auditory thresholds.
As in previous studies, TMS was safely combined with antidepressants in the third phase of this trial; however, patients at risk for seizure or on medications that could lower the seizure threshold were excluded. Thus, risk of seizure may be increased under these conditions. TMS is contraindicated for patients with implanted metallic devices or nonremovable objects in or around the head, except for dental hardware or braces.
- For availability information, contact the manufacturer, Neuronetics, at (877) 6000-7555 or www.NeuroStarTMS.com.
Disclosures
Drs. Dowd, Rado, and Janicak receive research support from and are consultants to Neuronetics, Inc.
Dr. Welch receives research support from Neuronetics, Inc.
1. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163(1):28-40.
2. George MS, Wassermann EM, Williams WA, et al. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport 1995;6(14):1853-6.
3. Avery DH, Holtzheimer PE, III, Fawaz W, et al. A controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depression. Biol Psychiatry 2006;59:187-94.
4. O’Reardon JP, Solvason HB, Janicak PG, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multi-site randomized controlled trial. Biol Psychiatry 2007;62:1208-16.
5. Lisanby SH, Husain MM, Rosenquist PB, et al. Daily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trial. Neuropsychopharmacology Epub 2008 Aug 13.
6. Dowd SM, Janicak PG. Transcranial magnetic stimulation for major depression: part II. Psychopharm Review 2007;42(1):1-8.
7. Wasserman EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5-7, 1996. Electroencephalogr Clin Neurophysiol 1998;108(1):1-16.
8. Janicak PG, O’Reardon JP, Sampson SM, et al. Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction. J Clin Psychiatry 2008;69:222-33.
1. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163(1):28-40.
2. George MS, Wassermann EM, Williams WA, et al. Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport 1995;6(14):1853-6.
3. Avery DH, Holtzheimer PE, III, Fawaz W, et al. A controlled study of repetitive transcranial magnetic stimulation in medication-resistant major depression. Biol Psychiatry 2006;59:187-94.
4. O’Reardon JP, Solvason HB, Janicak PG, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multi-site randomized controlled trial. Biol Psychiatry 2007;62:1208-16.
5. Lisanby SH, Husain MM, Rosenquist PB, et al. Daily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trial. Neuropsychopharmacology Epub 2008 Aug 13.
6. Dowd SM, Janicak PG. Transcranial magnetic stimulation for major depression: part II. Psychopharm Review 2007;42(1):1-8.
7. Wasserman EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5-7, 1996. Electroencephalogr Clin Neurophysiol 1998;108(1):1-16.
8. Janicak PG, O’Reardon JP, Sampson SM, et al. Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction. J Clin Psychiatry 2008;69:222-33.
Extended-release fluvoxamine for social anxiety disorder and OCD
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
Desvenlafaxine for depression
Compared with other antidepressants, desvenlafaxine might have more predictable effects and a lower risk of drug-drug interactions because of the way it is metabolized. The FDA approved this selective serotonin-norepinephrine reuptake inhibitor (SNRI)—a major active metabolite of venlafaxine—for treating major depressive disorder (MDD, Table 1). In clinical trials, desvenlafaxine was more effective than placebo in improving patients’ scores on scales of depressive symptoms and overall improvement.1
Table 1
Desvenlafaxine: Fast facts
| Brand name: Pristiq |
| Class: Serotonin-norepinephrine reuptake inhibitor |
| Indication: Major depressive disorder |
| Approval date: February 2008 |
| Availability date: May 2008 |
| Manufacturer: Wyeth Pharmaceuticals |
| Dosing forms: 50- and 100-mg tablets |
| Recommended dose: 50 to 100 mg/d |
Clinical implications
Unlike other SNRIs (venlafaxine and duloxetine), desvenlafaxine does not depend on cytochrome P450 (CYP) 2D6 for bio-transformation. As a result plasma concentrations vary less among individual patients, which should result in more predictable efficacy and tolerability. In addition, unlike bupropion, duloxetine, fluoxetine, and paroxetine, desvenlafaxine does not affect the functional activity of CYP 2D6. This translates into a lower risk of drug-drug interactions and more predictable effects on coadministered drugs that are cleared by CYP 2D6.
How it works
Serotonin, norepinephrine, and dopamine in the CNS are involved in mood and neurovegetative functions that are disturbed in patients with MDD. Desvenlafaxine selectively inhibits serotonin and norepinephrine reuptake pumps, therefore increasing serotonin and norepinephrine concentration in the synaptic cleft.2 The drug has weak binding affinity for the dopamine transporter and does not cause substantial changes in extracellular dopamine concentration. Decreased presynaptic serotonin and norepinephrine uptake increases the synaptic concentration of these neurotransmitters. These effects are thought to be responsible for desvenlafaxine’s antidepressant efficacy.
Pharmacokinetics
Desvenlafaxine’s single-dose pharmacokinetics are linear and dose-proportional over the recommended 50 to 100 mg/d dosing range. The half-life is approximately 11 hours. Steady-state plasma concentration is achieved in 4 to 5 days with once-daily dosing.
Food does not affect intestinal absorption. Bioavailability after oral administration is 80%, and time to reach maximum concentration (Tmax) is 7.5 hours. Plasma protein binding is 30% and is independent of desvenlafaxine concentration.1
Desvenlafaxine is excreted renally:
- unchanged (45% at 72 hours after administration)
- as desvenlafaxine-glucuronide
- as N-desvenlafaxine-glucuronide.
Desvenlafaxine-glucuronide is the final metabolite of conjugation reaction with glucuronic acid. N-desvenlafaxine-glucuronide is an end product of a 2-step metabolic reaction that starts with oxidation by CYP 3A4 to produce N-desvenlafaxine, which is conjugated with glucuronic acid to create N-desvenlafaxine-glucuronide. As a result of these metabolic and elimination pathways, dosing adjustment is recommended for patients with severe renal impairment or who are taking a CYP 3A4 inhibitor.
Dosing
Desvenlafaxine is available as 50-mg and 100-mg tablets. The recommended dosage is 50 mg/d, and the maximum recommended dosage in patients with hepatic impairment is 100 mg/d.
No dosing adjustment is necessary for patients with moderate renal impairment. The recommend regimen for those with severe renal impairment or end-stage renal disease is 50 mg every other day.
Instruct patients to take desvenlafaxine at approximately the same time each day, with or without food. Tell them not to discontinue the drug abruptly and to immediately report any adverse effects (AEs).
Efficacy
Desvenlafaxine’s antidepressant efficacy was established in four 8-week, randomized, double-blind, placebo-controlled, fixed-dose (50 mg to 400 mg once daily) studies in adult outpatients who met DSM-IV-TR criteria for MDD.1,2,4
In the first study,3 461 patients received desvenlafaxine, 100 mg, 200 mg, or 400 mg, or placebo. In the second study,4 369 patients received 200 mg or 400 mg or placebo. In 2 additional studies, a total of 930 patients received 50 mg or 100 mg or placebo.1
All studies used the 17-item Hamilton Rating Scale for Depression (HAM-D17) to measure depressive symptom improvement and the Clinical Global Impressions-Improvement (CGI-I) scale to measure overall improvement. Desvenlafaxine was more effective than placebo in HAM-D17 score improvement in all 4 studies and in CGI-I score improvement in 3 studies.
In studies comparing 50 mg/d with 100 mg/d, doses >50 mg/d provided no additional benefit. Higher starting fixed doses were associated with more frequent AEs and discontinuation.
Gender or age had no effect on treatment outcome. There was no difference in safety in elderly vs younger patients. Data are insufficient to establish a relationship between race and desvenlafaxine responsiveness. Desvenlafaxine’s safety and effectiveness in children and adolescents was not evaluated, and the drug is not approved for these patients.
Tolerability and safety
Desvenlafaxine’s tolerability is comparable to that of other SNRIs. In premarketing studies, 12% of patients receiving desvenlafaxine (50 mg/d to 400 mg/d) discontinued treatment because of AEs, compared with 3% in the placebo group. The discontinuation rate in patients receiving 100 mg/d was 8.7% compared with 4.1% in patients taking 50 mg/d.
AEs generally occur during the first week of treatment. In the 8-week trials, the most common AEs were nausea and dizziness (Table 2). In a long-term study (up to 9 months), the most common AE was vomiting. Although the recommended starting dose is 50 mg/d, to avoid AEs consider beginning with every-other-day dosing.
Table 2
Desvenlafaxine trials: Rates of adverse effects
| Desvenlafaxine dose | |||
|---|---|---|---|
| Adverse effect | 50 mg/d | 100 mg/d | Placebo |
| Nausea | 22% | 26% | 10% |
| Dizziness | 13% | 10% | 5% |
| Insomnia | 9% | 12% | 6% |
| Hyperhidrosis | 10% | 11% | 4% |
| Constipation | 9% | 9% | 4% |
| Somnolence | 4% | 9% | 4% |
| Decreased appetite | 5% | 8% | 2% |
| Erectile dysfunction | 3% | 6% | 1% |
| Decreased libido | 4% | 5% | 1% |
| Anxiety | 3% | 5% | 2% |
| Source: Reference 1 | |||
Abruptly discontinuing desvenlafaxine can cause withdrawal symptoms, including dizziness, nausea, headache, irritability, insomnia, diarrhea, anxiety, abnormal dreams, fatigue, and hyperhidrosis. The frequency of withdrawal symptoms is higher with longer treatment duration. Gradually reducing the dose by administering 50 mg of desvenlafaxine less often can reduce withdrawal symptoms.
Clinical issues
All SNRIs and selective serotonin reuptake inhibitors (SSRIs) have a “black-box” warning about the potential for clinical worsening and increased suicidality early in treatment. Closely monitor patients for suicidal ideation/behaviors during the first months of treatment and with dose changes.
When taken in the third trimester of pregnancy, SNRIs and SSRIs can cause serious neonatal complications—including respiratory distress, cyanosis, apnea, and seizures—that may require longer hospitalization, respiratory support, or tube feeding for the infant. Carefully consider risks and benefits of third-trimester antidepressant use.5 Desvenlafaxine is excreted in breast milk and may cause AEs in infants who are breast-fed.
In clinical trials, patients taking desvenlafaxine experienced increased cholesterol, triglycerides, and blood pressure. Monitor these parameters closely in patients taking desvenlafaxine, and use the drug with caution in patients with cerebrovascular and cardiovascular disease.
Other concerns in patients taking desvenlafaxine include:
- Antidepressant medications can trigger hypomania or mania in patients with bipolar disorder.
- Patients—particularly those who are elderly or taking diuretics—may develop hyponatremia as a result of syndrome of in-appropriate antidiuretic hormone.
- Patients with an increased risk of glaucoma need to be monitored because of the drug’s effect on blood pressure.
Drug interactions. Coadministering desvenlafaxine with serotonergic medications— such as triptans, other antidepressants, and tramadol—can cause serotonin syndrome, a potentially life-threatening condition characterized by mental status changes, autonomic instability, neuromuscular aberrations, and gastrointestinal symptoms. Concomitant use of desvenlafaxine and blood-thinning medications such as warfarin, aspirin, and nonsteroidal anti-inflammatory drugs may result in abnormal bleeding. Patients taking a potent CYP 3A4 inhibitor such as ketoconazole may have increased desvenlafaxine concentration.
Contraindications
Do not prescribe desvenlafaxine to patients who are:
- hypersensitive to venlafaxine chloride, desvenlafaxine succinate, or any parts of the desvenlafaxine formulation
- taking a monoamine oxidase inhibitor (MAOI), or have discontinued an MAOI within 14 days.
Patients who stop taking desvenlafaxine should wait 7 days before starting an MAOI.
Drug brand names
- Bupropion • Wellbutrin
- Desvenlafaxine • Pristiq
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Ketoconazole • Nizoral
- Paroxetine • Prozac
- Tramadol • Ultram
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Preskorn has in the past year received research/ grant support from and served as a speaker for Wyeth Pharmaceuticals. Previously, he has received research/grant support from or served as a speaker for or consultant to Abbott Laboratories, AstraZeneca, Aventis, Biovail, Boehringer Ingleheim, Bristol-Myers Squibb, Eisai, Eli Lilly and Company, GlaxoSmithKline, Hoffman LaRoche, Janssen, L.P., Johnson & Johnson, Lundbeck, Merck, Novartis, Organon, Otsuka, Pfizer Inc., Solvay, Somerset, Sumitomo, and Yamanouchi.
1. Pristiq [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals; 2008.
2. Deecher DC, Beyer CE, Johnston G, et al. Desvenlafaxine succinate: a new serotonin and norepinephrine reuptake inhibitor. J Pharmacol Exp Ther 2006;318(2):657-65.
3. DeMartinis NA, Yeung PP, Entsuah R, Manley AL. A double-blind, placebo-controlled study of the efficacy and safety of desvenlafaxine succinate in the treatment of major depressive disorder. J Clin Psychiatry 2007;68(5):677-88.
4. Septien-Velez L, Pitrosky B, Padmanabhan SK, et al. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in the treatment of major depressive disorder. Int Clin Psychopharmacol 2007;22(6):338-47.
5. Lennestål R, Källén B. Delivery outcome in relation to maternal use of some recently introduced antidepressants. J Clin Psychopharmacol 2007;27(6):607-13.
Dr. Lincoln is a clinical instructor and Dr. Preskorn is a professor of psychiatry, University of Kansas Medical Center, Wichita. Dr. Preskorn also is the psychopharmacology Section Editor of CURRENT PSYCHIATRY and president and CEO of Clinical Research Institute, Wichita.
Compared with other antidepressants, desvenlafaxine might have more predictable effects and a lower risk of drug-drug interactions because of the way it is metabolized. The FDA approved this selective serotonin-norepinephrine reuptake inhibitor (SNRI)—a major active metabolite of venlafaxine—for treating major depressive disorder (MDD, Table 1). In clinical trials, desvenlafaxine was more effective than placebo in improving patients’ scores on scales of depressive symptoms and overall improvement.1
Table 1
Desvenlafaxine: Fast facts
| Brand name: Pristiq |
| Class: Serotonin-norepinephrine reuptake inhibitor |
| Indication: Major depressive disorder |
| Approval date: February 2008 |
| Availability date: May 2008 |
| Manufacturer: Wyeth Pharmaceuticals |
| Dosing forms: 50- and 100-mg tablets |
| Recommended dose: 50 to 100 mg/d |
Clinical implications
Unlike other SNRIs (venlafaxine and duloxetine), desvenlafaxine does not depend on cytochrome P450 (CYP) 2D6 for bio-transformation. As a result plasma concentrations vary less among individual patients, which should result in more predictable efficacy and tolerability. In addition, unlike bupropion, duloxetine, fluoxetine, and paroxetine, desvenlafaxine does not affect the functional activity of CYP 2D6. This translates into a lower risk of drug-drug interactions and more predictable effects on coadministered drugs that are cleared by CYP 2D6.
How it works
Serotonin, norepinephrine, and dopamine in the CNS are involved in mood and neurovegetative functions that are disturbed in patients with MDD. Desvenlafaxine selectively inhibits serotonin and norepinephrine reuptake pumps, therefore increasing serotonin and norepinephrine concentration in the synaptic cleft.2 The drug has weak binding affinity for the dopamine transporter and does not cause substantial changes in extracellular dopamine concentration. Decreased presynaptic serotonin and norepinephrine uptake increases the synaptic concentration of these neurotransmitters. These effects are thought to be responsible for desvenlafaxine’s antidepressant efficacy.
Pharmacokinetics
Desvenlafaxine’s single-dose pharmacokinetics are linear and dose-proportional over the recommended 50 to 100 mg/d dosing range. The half-life is approximately 11 hours. Steady-state plasma concentration is achieved in 4 to 5 days with once-daily dosing.
Food does not affect intestinal absorption. Bioavailability after oral administration is 80%, and time to reach maximum concentration (Tmax) is 7.5 hours. Plasma protein binding is 30% and is independent of desvenlafaxine concentration.1
Desvenlafaxine is excreted renally:
- unchanged (45% at 72 hours after administration)
- as desvenlafaxine-glucuronide
- as N-desvenlafaxine-glucuronide.
Desvenlafaxine-glucuronide is the final metabolite of conjugation reaction with glucuronic acid. N-desvenlafaxine-glucuronide is an end product of a 2-step metabolic reaction that starts with oxidation by CYP 3A4 to produce N-desvenlafaxine, which is conjugated with glucuronic acid to create N-desvenlafaxine-glucuronide. As a result of these metabolic and elimination pathways, dosing adjustment is recommended for patients with severe renal impairment or who are taking a CYP 3A4 inhibitor.
Dosing
Desvenlafaxine is available as 50-mg and 100-mg tablets. The recommended dosage is 50 mg/d, and the maximum recommended dosage in patients with hepatic impairment is 100 mg/d.
No dosing adjustment is necessary for patients with moderate renal impairment. The recommend regimen for those with severe renal impairment or end-stage renal disease is 50 mg every other day.
Instruct patients to take desvenlafaxine at approximately the same time each day, with or without food. Tell them not to discontinue the drug abruptly and to immediately report any adverse effects (AEs).
Efficacy
Desvenlafaxine’s antidepressant efficacy was established in four 8-week, randomized, double-blind, placebo-controlled, fixed-dose (50 mg to 400 mg once daily) studies in adult outpatients who met DSM-IV-TR criteria for MDD.1,2,4
In the first study,3 461 patients received desvenlafaxine, 100 mg, 200 mg, or 400 mg, or placebo. In the second study,4 369 patients received 200 mg or 400 mg or placebo. In 2 additional studies, a total of 930 patients received 50 mg or 100 mg or placebo.1
All studies used the 17-item Hamilton Rating Scale for Depression (HAM-D17) to measure depressive symptom improvement and the Clinical Global Impressions-Improvement (CGI-I) scale to measure overall improvement. Desvenlafaxine was more effective than placebo in HAM-D17 score improvement in all 4 studies and in CGI-I score improvement in 3 studies.
In studies comparing 50 mg/d with 100 mg/d, doses >50 mg/d provided no additional benefit. Higher starting fixed doses were associated with more frequent AEs and discontinuation.
Gender or age had no effect on treatment outcome. There was no difference in safety in elderly vs younger patients. Data are insufficient to establish a relationship between race and desvenlafaxine responsiveness. Desvenlafaxine’s safety and effectiveness in children and adolescents was not evaluated, and the drug is not approved for these patients.
Tolerability and safety
Desvenlafaxine’s tolerability is comparable to that of other SNRIs. In premarketing studies, 12% of patients receiving desvenlafaxine (50 mg/d to 400 mg/d) discontinued treatment because of AEs, compared with 3% in the placebo group. The discontinuation rate in patients receiving 100 mg/d was 8.7% compared with 4.1% in patients taking 50 mg/d.
AEs generally occur during the first week of treatment. In the 8-week trials, the most common AEs were nausea and dizziness (Table 2). In a long-term study (up to 9 months), the most common AE was vomiting. Although the recommended starting dose is 50 mg/d, to avoid AEs consider beginning with every-other-day dosing.
Table 2
Desvenlafaxine trials: Rates of adverse effects
| Desvenlafaxine dose | |||
|---|---|---|---|
| Adverse effect | 50 mg/d | 100 mg/d | Placebo |
| Nausea | 22% | 26% | 10% |
| Dizziness | 13% | 10% | 5% |
| Insomnia | 9% | 12% | 6% |
| Hyperhidrosis | 10% | 11% | 4% |
| Constipation | 9% | 9% | 4% |
| Somnolence | 4% | 9% | 4% |
| Decreased appetite | 5% | 8% | 2% |
| Erectile dysfunction | 3% | 6% | 1% |
| Decreased libido | 4% | 5% | 1% |
| Anxiety | 3% | 5% | 2% |
| Source: Reference 1 | |||
Abruptly discontinuing desvenlafaxine can cause withdrawal symptoms, including dizziness, nausea, headache, irritability, insomnia, diarrhea, anxiety, abnormal dreams, fatigue, and hyperhidrosis. The frequency of withdrawal symptoms is higher with longer treatment duration. Gradually reducing the dose by administering 50 mg of desvenlafaxine less often can reduce withdrawal symptoms.
Clinical issues
All SNRIs and selective serotonin reuptake inhibitors (SSRIs) have a “black-box” warning about the potential for clinical worsening and increased suicidality early in treatment. Closely monitor patients for suicidal ideation/behaviors during the first months of treatment and with dose changes.
When taken in the third trimester of pregnancy, SNRIs and SSRIs can cause serious neonatal complications—including respiratory distress, cyanosis, apnea, and seizures—that may require longer hospitalization, respiratory support, or tube feeding for the infant. Carefully consider risks and benefits of third-trimester antidepressant use.5 Desvenlafaxine is excreted in breast milk and may cause AEs in infants who are breast-fed.
In clinical trials, patients taking desvenlafaxine experienced increased cholesterol, triglycerides, and blood pressure. Monitor these parameters closely in patients taking desvenlafaxine, and use the drug with caution in patients with cerebrovascular and cardiovascular disease.
Other concerns in patients taking desvenlafaxine include:
- Antidepressant medications can trigger hypomania or mania in patients with bipolar disorder.
- Patients—particularly those who are elderly or taking diuretics—may develop hyponatremia as a result of syndrome of in-appropriate antidiuretic hormone.
- Patients with an increased risk of glaucoma need to be monitored because of the drug’s effect on blood pressure.
Drug interactions. Coadministering desvenlafaxine with serotonergic medications— such as triptans, other antidepressants, and tramadol—can cause serotonin syndrome, a potentially life-threatening condition characterized by mental status changes, autonomic instability, neuromuscular aberrations, and gastrointestinal symptoms. Concomitant use of desvenlafaxine and blood-thinning medications such as warfarin, aspirin, and nonsteroidal anti-inflammatory drugs may result in abnormal bleeding. Patients taking a potent CYP 3A4 inhibitor such as ketoconazole may have increased desvenlafaxine concentration.
Contraindications
Do not prescribe desvenlafaxine to patients who are:
- hypersensitive to venlafaxine chloride, desvenlafaxine succinate, or any parts of the desvenlafaxine formulation
- taking a monoamine oxidase inhibitor (MAOI), or have discontinued an MAOI within 14 days.
Patients who stop taking desvenlafaxine should wait 7 days before starting an MAOI.
Drug brand names
- Bupropion • Wellbutrin
- Desvenlafaxine • Pristiq
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Ketoconazole • Nizoral
- Paroxetine • Prozac
- Tramadol • Ultram
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Preskorn has in the past year received research/ grant support from and served as a speaker for Wyeth Pharmaceuticals. Previously, he has received research/grant support from or served as a speaker for or consultant to Abbott Laboratories, AstraZeneca, Aventis, Biovail, Boehringer Ingleheim, Bristol-Myers Squibb, Eisai, Eli Lilly and Company, GlaxoSmithKline, Hoffman LaRoche, Janssen, L.P., Johnson & Johnson, Lundbeck, Merck, Novartis, Organon, Otsuka, Pfizer Inc., Solvay, Somerset, Sumitomo, and Yamanouchi.
Compared with other antidepressants, desvenlafaxine might have more predictable effects and a lower risk of drug-drug interactions because of the way it is metabolized. The FDA approved this selective serotonin-norepinephrine reuptake inhibitor (SNRI)—a major active metabolite of venlafaxine—for treating major depressive disorder (MDD, Table 1). In clinical trials, desvenlafaxine was more effective than placebo in improving patients’ scores on scales of depressive symptoms and overall improvement.1
Table 1
Desvenlafaxine: Fast facts
| Brand name: Pristiq |
| Class: Serotonin-norepinephrine reuptake inhibitor |
| Indication: Major depressive disorder |
| Approval date: February 2008 |
| Availability date: May 2008 |
| Manufacturer: Wyeth Pharmaceuticals |
| Dosing forms: 50- and 100-mg tablets |
| Recommended dose: 50 to 100 mg/d |
Clinical implications
Unlike other SNRIs (venlafaxine and duloxetine), desvenlafaxine does not depend on cytochrome P450 (CYP) 2D6 for bio-transformation. As a result plasma concentrations vary less among individual patients, which should result in more predictable efficacy and tolerability. In addition, unlike bupropion, duloxetine, fluoxetine, and paroxetine, desvenlafaxine does not affect the functional activity of CYP 2D6. This translates into a lower risk of drug-drug interactions and more predictable effects on coadministered drugs that are cleared by CYP 2D6.
How it works
Serotonin, norepinephrine, and dopamine in the CNS are involved in mood and neurovegetative functions that are disturbed in patients with MDD. Desvenlafaxine selectively inhibits serotonin and norepinephrine reuptake pumps, therefore increasing serotonin and norepinephrine concentration in the synaptic cleft.2 The drug has weak binding affinity for the dopamine transporter and does not cause substantial changes in extracellular dopamine concentration. Decreased presynaptic serotonin and norepinephrine uptake increases the synaptic concentration of these neurotransmitters. These effects are thought to be responsible for desvenlafaxine’s antidepressant efficacy.
Pharmacokinetics
Desvenlafaxine’s single-dose pharmacokinetics are linear and dose-proportional over the recommended 50 to 100 mg/d dosing range. The half-life is approximately 11 hours. Steady-state plasma concentration is achieved in 4 to 5 days with once-daily dosing.
Food does not affect intestinal absorption. Bioavailability after oral administration is 80%, and time to reach maximum concentration (Tmax) is 7.5 hours. Plasma protein binding is 30% and is independent of desvenlafaxine concentration.1
Desvenlafaxine is excreted renally:
- unchanged (45% at 72 hours after administration)
- as desvenlafaxine-glucuronide
- as N-desvenlafaxine-glucuronide.
Desvenlafaxine-glucuronide is the final metabolite of conjugation reaction with glucuronic acid. N-desvenlafaxine-glucuronide is an end product of a 2-step metabolic reaction that starts with oxidation by CYP 3A4 to produce N-desvenlafaxine, which is conjugated with glucuronic acid to create N-desvenlafaxine-glucuronide. As a result of these metabolic and elimination pathways, dosing adjustment is recommended for patients with severe renal impairment or who are taking a CYP 3A4 inhibitor.
Dosing
Desvenlafaxine is available as 50-mg and 100-mg tablets. The recommended dosage is 50 mg/d, and the maximum recommended dosage in patients with hepatic impairment is 100 mg/d.
No dosing adjustment is necessary for patients with moderate renal impairment. The recommend regimen for those with severe renal impairment or end-stage renal disease is 50 mg every other day.
Instruct patients to take desvenlafaxine at approximately the same time each day, with or without food. Tell them not to discontinue the drug abruptly and to immediately report any adverse effects (AEs).
Efficacy
Desvenlafaxine’s antidepressant efficacy was established in four 8-week, randomized, double-blind, placebo-controlled, fixed-dose (50 mg to 400 mg once daily) studies in adult outpatients who met DSM-IV-TR criteria for MDD.1,2,4
In the first study,3 461 patients received desvenlafaxine, 100 mg, 200 mg, or 400 mg, or placebo. In the second study,4 369 patients received 200 mg or 400 mg or placebo. In 2 additional studies, a total of 930 patients received 50 mg or 100 mg or placebo.1
All studies used the 17-item Hamilton Rating Scale for Depression (HAM-D17) to measure depressive symptom improvement and the Clinical Global Impressions-Improvement (CGI-I) scale to measure overall improvement. Desvenlafaxine was more effective than placebo in HAM-D17 score improvement in all 4 studies and in CGI-I score improvement in 3 studies.
In studies comparing 50 mg/d with 100 mg/d, doses >50 mg/d provided no additional benefit. Higher starting fixed doses were associated with more frequent AEs and discontinuation.
Gender or age had no effect on treatment outcome. There was no difference in safety in elderly vs younger patients. Data are insufficient to establish a relationship between race and desvenlafaxine responsiveness. Desvenlafaxine’s safety and effectiveness in children and adolescents was not evaluated, and the drug is not approved for these patients.
Tolerability and safety
Desvenlafaxine’s tolerability is comparable to that of other SNRIs. In premarketing studies, 12% of patients receiving desvenlafaxine (50 mg/d to 400 mg/d) discontinued treatment because of AEs, compared with 3% in the placebo group. The discontinuation rate in patients receiving 100 mg/d was 8.7% compared with 4.1% in patients taking 50 mg/d.
AEs generally occur during the first week of treatment. In the 8-week trials, the most common AEs were nausea and dizziness (Table 2). In a long-term study (up to 9 months), the most common AE was vomiting. Although the recommended starting dose is 50 mg/d, to avoid AEs consider beginning with every-other-day dosing.
Table 2
Desvenlafaxine trials: Rates of adverse effects
| Desvenlafaxine dose | |||
|---|---|---|---|
| Adverse effect | 50 mg/d | 100 mg/d | Placebo |
| Nausea | 22% | 26% | 10% |
| Dizziness | 13% | 10% | 5% |
| Insomnia | 9% | 12% | 6% |
| Hyperhidrosis | 10% | 11% | 4% |
| Constipation | 9% | 9% | 4% |
| Somnolence | 4% | 9% | 4% |
| Decreased appetite | 5% | 8% | 2% |
| Erectile dysfunction | 3% | 6% | 1% |
| Decreased libido | 4% | 5% | 1% |
| Anxiety | 3% | 5% | 2% |
| Source: Reference 1 | |||
Abruptly discontinuing desvenlafaxine can cause withdrawal symptoms, including dizziness, nausea, headache, irritability, insomnia, diarrhea, anxiety, abnormal dreams, fatigue, and hyperhidrosis. The frequency of withdrawal symptoms is higher with longer treatment duration. Gradually reducing the dose by administering 50 mg of desvenlafaxine less often can reduce withdrawal symptoms.
Clinical issues
All SNRIs and selective serotonin reuptake inhibitors (SSRIs) have a “black-box” warning about the potential for clinical worsening and increased suicidality early in treatment. Closely monitor patients for suicidal ideation/behaviors during the first months of treatment and with dose changes.
When taken in the third trimester of pregnancy, SNRIs and SSRIs can cause serious neonatal complications—including respiratory distress, cyanosis, apnea, and seizures—that may require longer hospitalization, respiratory support, or tube feeding for the infant. Carefully consider risks and benefits of third-trimester antidepressant use.5 Desvenlafaxine is excreted in breast milk and may cause AEs in infants who are breast-fed.
In clinical trials, patients taking desvenlafaxine experienced increased cholesterol, triglycerides, and blood pressure. Monitor these parameters closely in patients taking desvenlafaxine, and use the drug with caution in patients with cerebrovascular and cardiovascular disease.
Other concerns in patients taking desvenlafaxine include:
- Antidepressant medications can trigger hypomania or mania in patients with bipolar disorder.
- Patients—particularly those who are elderly or taking diuretics—may develop hyponatremia as a result of syndrome of in-appropriate antidiuretic hormone.
- Patients with an increased risk of glaucoma need to be monitored because of the drug’s effect on blood pressure.
Drug interactions. Coadministering desvenlafaxine with serotonergic medications— such as triptans, other antidepressants, and tramadol—can cause serotonin syndrome, a potentially life-threatening condition characterized by mental status changes, autonomic instability, neuromuscular aberrations, and gastrointestinal symptoms. Concomitant use of desvenlafaxine and blood-thinning medications such as warfarin, aspirin, and nonsteroidal anti-inflammatory drugs may result in abnormal bleeding. Patients taking a potent CYP 3A4 inhibitor such as ketoconazole may have increased desvenlafaxine concentration.
Contraindications
Do not prescribe desvenlafaxine to patients who are:
- hypersensitive to venlafaxine chloride, desvenlafaxine succinate, or any parts of the desvenlafaxine formulation
- taking a monoamine oxidase inhibitor (MAOI), or have discontinued an MAOI within 14 days.
Patients who stop taking desvenlafaxine should wait 7 days before starting an MAOI.
Drug brand names
- Bupropion • Wellbutrin
- Desvenlafaxine • Pristiq
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Ketoconazole • Nizoral
- Paroxetine • Prozac
- Tramadol • Ultram
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Preskorn has in the past year received research/ grant support from and served as a speaker for Wyeth Pharmaceuticals. Previously, he has received research/grant support from or served as a speaker for or consultant to Abbott Laboratories, AstraZeneca, Aventis, Biovail, Boehringer Ingleheim, Bristol-Myers Squibb, Eisai, Eli Lilly and Company, GlaxoSmithKline, Hoffman LaRoche, Janssen, L.P., Johnson & Johnson, Lundbeck, Merck, Novartis, Organon, Otsuka, Pfizer Inc., Solvay, Somerset, Sumitomo, and Yamanouchi.
1. Pristiq [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals; 2008.
2. Deecher DC, Beyer CE, Johnston G, et al. Desvenlafaxine succinate: a new serotonin and norepinephrine reuptake inhibitor. J Pharmacol Exp Ther 2006;318(2):657-65.
3. DeMartinis NA, Yeung PP, Entsuah R, Manley AL. A double-blind, placebo-controlled study of the efficacy and safety of desvenlafaxine succinate in the treatment of major depressive disorder. J Clin Psychiatry 2007;68(5):677-88.
4. Septien-Velez L, Pitrosky B, Padmanabhan SK, et al. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in the treatment of major depressive disorder. Int Clin Psychopharmacol 2007;22(6):338-47.
5. Lennestål R, Källén B. Delivery outcome in relation to maternal use of some recently introduced antidepressants. J Clin Psychopharmacol 2007;27(6):607-13.
Dr. Lincoln is a clinical instructor and Dr. Preskorn is a professor of psychiatry, University of Kansas Medical Center, Wichita. Dr. Preskorn also is the psychopharmacology Section Editor of CURRENT PSYCHIATRY and president and CEO of Clinical Research Institute, Wichita.
1. Pristiq [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals; 2008.
2. Deecher DC, Beyer CE, Johnston G, et al. Desvenlafaxine succinate: a new serotonin and norepinephrine reuptake inhibitor. J Pharmacol Exp Ther 2006;318(2):657-65.
3. DeMartinis NA, Yeung PP, Entsuah R, Manley AL. A double-blind, placebo-controlled study of the efficacy and safety of desvenlafaxine succinate in the treatment of major depressive disorder. J Clin Psychiatry 2007;68(5):677-88.
4. Septien-Velez L, Pitrosky B, Padmanabhan SK, et al. A randomized, double-blind, placebo-controlled trial of desvenlafaxine succinate in the treatment of major depressive disorder. Int Clin Psychopharmacol 2007;22(6):338-47.
5. Lennestål R, Källén B. Delivery outcome in relation to maternal use of some recently introduced antidepressants. J Clin Psychopharmacol 2007;27(6):607-13.
Dr. Lincoln is a clinical instructor and Dr. Preskorn is a professor of psychiatry, University of Kansas Medical Center, Wichita. Dr. Preskorn also is the psychopharmacology Section Editor of CURRENT PSYCHIATRY and president and CEO of Clinical Research Institute, Wichita.