User login
The Hospitalist only
In the Literature
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
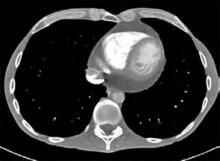
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Performance Measures and Outcomes for Heart Patients
Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70
As our population ages, more emphasis will be placed on issues surrounding efficient and evidence-based care. Heart failure, which accounted for 3.6 million hospitalizations in 2003 and has an overall prevalence of 5 million, will be at the forefront of public policy. As pay for performance (P4P) and standards of care become increasingly prevalent, the medical community will need to scrutinize the standards by which we are measured.
The American College of Cardiology and the American Heart Association (ACC/AHA) developed guidelines for the treatment and care of patients with heart failure. These measures include heart failure discharge instructions, evaluation of left ventricle (LV) function, angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor antagonist (ARB) for LV dysfunction, adult smoking cessation counseling, and anticoagulation at discharge for patients with atrial fibrillation. Adherence to these performance measures should be based on evidence.
The authors’ goal was to determine the validity of these guidelines. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry allowed for the documentation and follow-up of patients adhering to the heart failure guidelines as set forth by the ACC/AHA. The study assessed the relationship between these guidelines and clinical outcomes, including 60- to 90-day mortality and a composite end point of mortality or rehospitalization.
In this study the OPTIMIZE-HF registry was used as the source of prospective data collection. Ten percent of eligible patients were randomly selected from the registry between March 2003 and December 2004 from 91 hospitals. Eligibility for the OPTIMIZE-HF registry included patients 18 and older admitted for worsening heart failure or significant heart failure during their hospital stay. The performance measure of discharge instruction, smoking cessation, and anticoagulation were measured for all eligible patients. Patients with an ejection fraction of 40% or less, or moderate to severe systolic function, were included for the ACE inhibitor/ARB performance measure. One measure not included was treatment with beta-blockers at discharge. The authors included beta-blockers at discharge with metrics similar to those described for ACE/ARB criteria.
The conformity rates and process-outcome links were then determined for the performance measures and beta-blocker treatment as it related to 60- to 90-day mortality/rehospitalization.
The study focused on a random follow-up cohort of 5,791 patients from 91 hospitals. This was similar to the OPTIMIZE-HF cohort of 48,612 patients in 259 hospitals. Demographically, the average cohort’s age was 72, 51% male and 78% white, with 42% of patients diagnosed with ischemic heart disease and 43% with diabetes mellitus. These results were similar to the demographics of the overall OPTIMIZE-HF registry.
Of the eligible patients in the follow-up cohort, 66% (4,010) received complete discharge instructions. Eighty-nine percent of eligible patients (4,664) had their left ventricular function evaluated. For those patients with documented left ventricular systolic dysfunction (2,181), 83% were given an ACE inhibitor or ARB at discharge. Patients who had a diagnosis of atrial fibrillation were discharged with anticoagulation at a rate of 53%, and 72% of patients were counseled on smoking cessation. As compared with ACE inhibitors/ARB, similar results (84%) were seen for beta-blockers at discharge.
Only two of the five ACC/AHA performance measures were predictive of decreasing morbidity and mortality/rehospitalization in unadjusted analysis: patients discharged on ACE inhibitors/ARBs (odds ratio, 0.51; 95% CI 0.34–0.78; P- .002) and smoking cessation counseling. Beta-blockers, not a formal part of the ACC/AHA guidelines, were also a predictor of lower risk of both mortality and rehospitalization (odds ratio, 0.73; 95% CI, 0.55-0.96; P-0.02)
The OPTIMIZE-HF cohort analysis allowed for an opportunity to determine the degree of conformity for the ACC/AHA performance measures. The ACE inhibitors or ARB use at discharge was shown in the OPTIMIZE-HF cohort to have a relative reduction in one-year post discharge mortality by 17% (risk reduction, 0.83; 95% CI, 0.79-0.88) and a trend to lower 60- to 90-days post-discharge mortality and rehospitalization. Although smoking cessation had an early positive correlation, outcomes did not reach statistical significance. The measure of discharge instruction in the current study did not show a benefit on early mortality/rehospitalization in 60- to 90-days post discharge. It is unclear from this study if discharge instructions given to patients were either rushed or discussed in a comprehensive manner. This factor will need clarification and further research.
The measures of discharge instructions, smoking cessation, LV assessment, and anticoagulation for atrial fibrillation have not been examined as effective performance measures prior to this study. These measures were unable to show an independent decrease in 60- to 90-day mortality and rehospitalization.
Patients discharged with beta-blockers showed an association between lower mortality and rehospitalization. This association was found to be stronger than any of the formal ACC/AHA current performance measures.
The ACC/AHA guidelines are becoming standards of care for reporting to agencies such as Centers for Medicare and Medicaid Services or other P4P programs. To allow for improvement of quality, JCAHO and ACC/AHA designed the above criteria to act as a guide for the post discharge care of coronary heart failure patients. Because these criteria are the measures by which hospitals need to report, it will be necessary for data to show validity and a link between the clinical performance measures and improved outcomes.
Of the five measures stated, only ACE inhibitors/ARB at discharge was associated with a decrease in mortality/rehospitalization. Beta-blockers, currently not a performance measure, also showed this trend. Increased scrutiny needs to be part of the criteria for which hospitals and practitioners are being held accountable, and further research validating their effectiveness is warranted.
Risk Indexes for COPD
Niewoehner DE, Lockhnygina Y, Rice K, et al. Risk indexes for exacerbations and hospitalizations due to COPD. Chest. 2007 Jan;131(1):20-28.
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality in the U.S. and continues to increase its numbers annually.
The cornerstone of COPD diagnosis and key predictor of prognosis is a low level of lung function. Another important predictor of morbidity, mortality, and progression of disease is COPD exacerbations.
Unfortunately, the definition of an exacerbation is varied, ranging from an increase in symptoms to COPD-related hospitalizations and death.1 Therefore, prevention of COPD exacerbations is an important management goal. This study focuses on setting a risk model as a clinical management tool, similar to what exists for cardiovascular events or community acquired pneumonia. No previous study has attempted to identify risk factors for exacerbations using prospective data collection and a clearly stated definition of exacerbation.
The study was a parallel-group, randomized, double-blind, placebo-controlled trial in patients with moderate to severe COPD conducted at 26 Veterans Affairs medical centers in the United States. Subjects were 40 or older, with a cigarette smoking history of 10 packs a year or more, a clinical diagnosis of COPD, and a forced expiratory volume [FEV] of 60% or less predicted and 70% or less of the forced vital capacity [FVC].1 Patients were allocated to receive one capsule of tiotropium (18 mg) or placebo for six months.
Of the 1,829 patients selected, 914 were assigned to the tiotropium arm. Patients kept a daily diary, and the investigators collected data by monthly telephone interviews and by site visits at three and six months with spirometry evaluation. They evaluated the association between baseline characteristics, concomitant medications and the study drug and the time to first COPD exacerbation and the time to first hospitalization due to exacerbation. The authors defined an exacerbation as a complex of respiratory symptoms of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days requiring treatment with antibiotics and/or systemic corticosteroids and/or hospital admission.
The investigators found that a statistically significant greater risk for both COPD exacerbations and hospitalizations is associated with being of older age, being a noncurrent smoker, having poorer lung function, using home oxygen, visiting the clinic or emergency department more often, either scheduled or unscheduled, being hospitalized for COPD in the prior year, using either antibiotics or systemic steroids for COPD more often in the prior year, and using short-acting beta agonist, inhaled or oral corticosteroid at a baseline rate.
On the other hand, a statistically significant greater risk of only COPD exacerbation was seen in white patients, with presence of productive cough, longer duration of COPD, use of long-acting beta agonist or theophylline at baseline, and presence of any gastrointestinal or hepatobiliary disease. Lower body-mass index and the presence of cardiovascular comorbidity were associated with statistically significant greater risk for only hospitalization due to COPD.
The investigators also confirmed the previous suggestion that chronic cough is an independent predictor of exacerbation. Interestingly, they found that any cardiovascular comorbidity is a strong and independent predictor of hospitalizations due to COPD. It is unclear if cardiovascular disease truly predisposes subjects to COPD hospitalizations or merely represents a misdiagnosis because both diseases have similar symptoms.
Current smokers were identified as having lower risk of exacerbation and hospitalization, probably due to the “healthy smoker” theory—that deteriorating lung function causes the patient to quit smoking.
This study is the first to gather information about predictors of COPD exacerbations in a prospective fashion using a clear definition of exacerbation. The authors developed a model to assess the risk of COPD exacerbations and hospitalizations due to exacerbations in patients with moderate to severe COPD. Moreover, this model can easily be applied to individual patients and reproduced with simple spirometry and a series of questions.
Though this trial had a reasonable level of statistical significance, it is important to mention that the trial was conducted within a single health system (Veterans Affairs medical centers), there were few women in the study, and the eligibility criteria were very specific.
References
- Mannino DM, Watt G, Hole D, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J. 2006 Mar;27(3):627-643.
Glucose Management in Hospitalized Patients
Leahy JL. Insulin Management of diabetic patients on general medical and surgical floors. Endocr Pract. Jul/Aug 2006;12(Suppl3):86-89.
Although the rationale behind the science for tight control of blood sugar in subsets of hospitalized patient populations is without debate when it comes to the majority of general ward patients, the management of hyperglycemia becomes more of an art. Increasingly we recognize the effect of the relationship between improving glucose management and improving clinical outcomes.
Guidelines for inpatient targeted blood glucose levels exist, but hospitals are moving toward a more individualized approach to subcutaneous insulin protocols for their patients, thus moving beyond the passive sliding scale era.
Institution of an insulin protocol at one such hospital, the University of Vermont, highlights such an approach. The ongoing internal nonrandomized study exemplifies a two-tiered approach initially aimed at expanding the house physician comfort zone to change the culture of hyperglycemic management beyond simply avoiding hypoglycemia to one of an active and—per our current standards—aggressive individualized insulin protocol.
It seems the author envisions a gradual process allowing initial flexibility within the protocol, increasing the intensity of dosing as comfort zones expand. Throughout the process, the principles of determining a patient’s weight-based daily insulin needs are maintained, taking into consideration factors like comorbidities, severity of illness, amount of oral intake, steroid usage, and age. Then, the insulin regimen is physiologically (basal/bolus, basal, continuous) administered according to the route (i.e., total parenteral nutrition) and timing of their nutritional intake.
Adjustments being made to insulin regimens are based on fasting, pre-meal and bedtime glucose as well as the novel approach of bolus insulin after meals with short-acting insulin (i.e., lispro).
Unfortunately although the protocol does perhaps yield itself to being looked at more stringently—in terms of cost effectiveness, improved length of hospital stay, and improved clinical outcomes—the outcome studied here was primarily one of hospitalwide education in advancing the understanding and culture of aggressive individualized insulin protocols. These can often be even more statistically difficult to quantify. As self-reported, improvements were made.
One of the most important aspects of this paper is that it draws attention to the paucity of evidence for improved clinical and monetary outcomes supporting the aggressive hospital management of hyperglycemia in the non-acutely ill patient. Often, the guiding principle is to avoid hypoglycemia. Detailing the specific protocols of one such approach serves as an example for the motivated reader.
Early Switch from IV to Oral Antibiotic in Severe CAP
Oosterheert JJ, Bonten JM, Schneider MME, et al. Effectiveness of early switch from intravenous to oral antibiotics in severe community acquired pneumonia; multicentre randomised trial. BMJ. 2006 Dec 9; 333:1193.
Community acquired pneumonia (CAP) is a common and potentially fatal infection with high healthcare costs. When patients are first admitted to hospitals, antibiotics are usually given intravenously to provide optimal concentrations in the tissues.
The duration of intravenous treatment is an important determinant of length of hospital stay (LOS). The concept of early transition from intravenous to oral antibiotic in the treatment of CAP has been evaluated before, but only in mild to moderately severe disease—and rarely in randomized trials.
This multicenter random controlled trial from five teaching hospitals and two medical centers in the Netherlands enrolled 302 patients in non-intensive care units with severe CAP. The primary outcome was clinical cure and secondary outcome was LOS. The inclusion criteria were adults 18 or older with severe CAP; mean pneumonia severity index of IV-V, new progressive infiltrate on chest X-ray, plus at least two other criteria (cough, sputum production, rectal temperature >38o C or <36.1o C, auscultative findings consistent with pneumonia, leukocytes >109 WBC/L or >15% bands, positive cultures of blob or pleural fluids, CRP three times greater times upper limit of normal).
Exclusion criteria included the need for mechanical ventilation, cystic fibrosis, a history of colonization with gram-negative bacteria due to structural damage to the respiratory tract, malfunction of the digestive tract, life expectancy of less than one month because of underlying disease, infections other than pneumonia that needed antibiotic treatment, and severe immunosuppression (neutropenia [<0.5 109 neutrophils/liter] or a CD4 count< 200/mm3).
Treatment failure was defined as death, still in hospital at day 28 of the study, or clinical deterioration (increase in temperature after initial improvement or the need for mechanical ventilation, switch back to intravenous antibiotics, or readmission for pulmonary reinfection after discharge).
Clinical cure was defined as discharged in good health without signs and symptoms of pneumonia and no treatment failure during follow-up.
The control group comprised 150 subjects who were to receive a standard course of seven days’ intravenous treatment. Meanwhile, 152 subjects were randomized to the early switch group. Baseline characteristics were similar in both groups. More than 80% of patients were in pneumonia severity class IV or V. Most patients received empirical monotherapy with amoxicillin or amoxicillin plus clavulanic acid (n=174; 58%) or a cephalosporin (n=59; 20%), which is in line with Dutch prescribing policies.
The most frequently identified microorganism was S pneumoniae (n=76; 25%). Atypical pathogens were detected in 33 patients (11%). Before day three, 37 patients (12%) were excluded from analysis, leaving 132 patients for analysis in the intervention group and 133 in the control group.
Reasons for exclusion included when the initial diagnosis of CAP was replaced by another diagnosis (n=9), consent was withdrawn (n=11), the protocol was violated (n=4), the patient was admitted to an intensive-care unit for mechanical ventilation (n=6), and the patient died (n=7). After three days of intravenous treatment, 108 of 132 patients (81%) in the intervention group were switched to oral treatment, of whom 102 (94%) received amoxicillin plus clavulanic acid (500+125 mg every eight hours).
In the control group, five patients did not receive intravenous antibiotics for all seven days because of phlebitis associated with intravenous treatment; none of them needed treatment for line-related sepsis. Overall duration of antibiotic treatment was 10.1 days in the intervention group and 9.3 days in the control group (mean difference 0.8 days, 95% confidence interval -0.6 to 2.0).
The duration of intravenous treatment was significantly shorter in the intervention group (mean 3.6 [SD 1.5] versus 7.0 [2.0] days, mean difference 3.4, 2.8 to 3.9). Average time to meet the discharge criteria was 5.2 (2.9) days in the intervention group and 5.7 (3.1) days in the control group (0.5 days -0.3 to 1.2) Total length of hospital stay was 9.6 (5.0) and 11.5 (4.9) days for patients in the intervention group and control group (1.9 days 0.6 to 3.2).
The authors’ findings provide strong evidence that early transition from intravenous to oral antibiotic is also viable in patients with highly graded Pneumonia Severity Index (PSI) CAP, not only in mild to moderately severe disease. This leads to reduced LOS, cost, and possibly reduced risk of line infections and increased patient satisfaction for early discharge.
Note: This study was done with patients suffering straightforward, uncomplicated CAP. The investigators’ findings cannot be applied to patients with other comorbidities like diabetes, COPD, heart failure, or sickle cell, which might require more days on intravenous antibiotic. One might also wonder what impact would have been seen had 37 patients not dropped off, and if another class of oral antibiotic such as quinolones had been used.
Last, the study sample showed S pneumoniae identified in 25% of cases and atypical pathogens to be 11%. What then are the majority of pathogens identified 64% of the time? This would have been another key factor that might have had a great effect on the result.
Although a larger sampling and further risk stratification (to include patients with other comorbidities) are needed, this study makes a valid point for early transition to oral antibiotics in highly graded, uncomplicated CAP. TH
Hard Work Pays Off
This is the second in a series on the four pillars of career satisfaction. Part 1 appeared on p. 14 in the June issue of The Hospitalist.
How can hospitalists work long days often packed from beginning to end and still remain happy with their jobs? One answer can be found in “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org), a comprehensive document by SHM’s Career Satisfaction Task Force (CSTF). This white paper can be used by hospitalists and hospital medicine practices as a toolkit for improving job satisfaction. It outlines the four pillars of career satisfaction.
The Second Pillar: Workload/Schedule
The workload/schedule pillar refers to the type, volume, and intensity of a hospitalist’s work as well as time pressures, variability of work, and number of interruptions. A hospitalist schedule must take all these factors into consideration.
CSTF Co-Chairperson Winthrop Whitcomb, MD, Mercy Medical Center, Springfield, Mass., maintains that this pillar is supported by the other three—autonomy/control, reward/recognition, and community/environment—but most closely with reward/recognition.
“There needs to be a reward system in place no matter what the workload,” says Dr. Whitcomb. “You can’t really talk about workload without addressing rewards. It’s human nature that in order to work hard, you need to be rewarded in some meaningful way.”
But many people—not just physicians but workers from all fields—may have separate concerns about heavy workload and just rewards.
An Example of Workload Issues
You probably know from your own experience as a hospitalist how workload can affect career satisfaction. Here is a fictional example of a hospitalist struggling with an increased patient load:
The director of my community-based hospital medicine program has mandated that each hospitalist see 15 to 20 patients each weekday, and 20 to 30 patients a day over weekends. I know this workload is too heavy to allow good quality of care. Under the pressure of seeing my quota of patients, I’m afraid I might make a mistake or miss something.
“There are physicians out there who can and do handle this type of workload, and they do it happily and well,” Dr. Whitcomb points out. “But this is only true if there is an appropriate reward system in place, and there clearly needs to be a good support system in order to provide quality of care” under this example.
CSTF says this individual should take the following steps:
Step 1: Go on a fact-finding mission. Find out whether hospitalist workload, responsibilities, and schedule at this facility are the norm. “[The hospitalist] should get an idea of what’s happening at other hospital medicine groups; he should understand the national picture,” says Dr. Whitcomb. “He might then realize that hospitalists in his group are only working 187 days a year, and that over a course of a year they’re not really working any harder than others who work more days,” says Dr. Whitcomb. “This might get him thinking a little bit differently about the workload.”
Step 2: Undertake organizational strategies. A hospitalist can find out how he or she has a voice in workload issues.“Figure out how hospitalists are represented in the structure of the group,” advises Dr. Whitcomb. “If a director is mandating how much [hospitalists] work, there has to be some mechanism for the physicians to be able to provide feedback. This often takes the shape of a compensation committee; this group is not just about compensation but about budget and sustainability for both the hospital and the hospitalists.” Physician representation—having a say in workload and schedule—is important to maintain a good balance within a hospital medicine program.
Step 3: Consider recommendations to ease workload. “You can try to change the workload through justifying adding staff or through putting systems in place that allow you to see more patients,” says Dr. Whitcomb. But what if the hospitalist considers or takes these steps and still finds his patient load to be unsustainable long term? “In terms of feeling like you’re not able to provide safe care,” says Dr. Whitcomb, “once you’ve suggested changes to the leadership and no changes are made, this may become a deal-breaker.”
Workload Leans on Other Pillars
The interesting thing about the workload/schedule pillar of job satisfaction is that, if you are unhappy with your workload, the other three pillars can sustain you and make you generally satisfied.
Dr. Whitcomb points to a 2002 article published in the Journal of Health and Social Behavior.1 The study examined a national survey of hospitalists and found that job burnout and intent to remain in the career are more meaningfully associated with favorable “community” relations than with negative experiences such as reduced autonomy.
“Workload is not a predictor of burnout as long as the other three pillars are intact,” summarizes Dr. Whitcomb.
Jane Jerrard has written for The Hospitalist since 2005.
Reference
- Hoff T, Whitcomb WF, Nelson JR. Thriving and surviving in a new medical career: the case of hospitalist physicians. J Health Social Behav. 2002 Mar;43(1):72-91
This is the second in a series on the four pillars of career satisfaction. Part 1 appeared on p. 14 in the June issue of The Hospitalist.
How can hospitalists work long days often packed from beginning to end and still remain happy with their jobs? One answer can be found in “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org), a comprehensive document by SHM’s Career Satisfaction Task Force (CSTF). This white paper can be used by hospitalists and hospital medicine practices as a toolkit for improving job satisfaction. It outlines the four pillars of career satisfaction.
The Second Pillar: Workload/Schedule
The workload/schedule pillar refers to the type, volume, and intensity of a hospitalist’s work as well as time pressures, variability of work, and number of interruptions. A hospitalist schedule must take all these factors into consideration.
CSTF Co-Chairperson Winthrop Whitcomb, MD, Mercy Medical Center, Springfield, Mass., maintains that this pillar is supported by the other three—autonomy/control, reward/recognition, and community/environment—but most closely with reward/recognition.
“There needs to be a reward system in place no matter what the workload,” says Dr. Whitcomb. “You can’t really talk about workload without addressing rewards. It’s human nature that in order to work hard, you need to be rewarded in some meaningful way.”
But many people—not just physicians but workers from all fields—may have separate concerns about heavy workload and just rewards.
An Example of Workload Issues
You probably know from your own experience as a hospitalist how workload can affect career satisfaction. Here is a fictional example of a hospitalist struggling with an increased patient load:
The director of my community-based hospital medicine program has mandated that each hospitalist see 15 to 20 patients each weekday, and 20 to 30 patients a day over weekends. I know this workload is too heavy to allow good quality of care. Under the pressure of seeing my quota of patients, I’m afraid I might make a mistake or miss something.
“There are physicians out there who can and do handle this type of workload, and they do it happily and well,” Dr. Whitcomb points out. “But this is only true if there is an appropriate reward system in place, and there clearly needs to be a good support system in order to provide quality of care” under this example.
CSTF says this individual should take the following steps:
Step 1: Go on a fact-finding mission. Find out whether hospitalist workload, responsibilities, and schedule at this facility are the norm. “[The hospitalist] should get an idea of what’s happening at other hospital medicine groups; he should understand the national picture,” says Dr. Whitcomb. “He might then realize that hospitalists in his group are only working 187 days a year, and that over a course of a year they’re not really working any harder than others who work more days,” says Dr. Whitcomb. “This might get him thinking a little bit differently about the workload.”
Step 2: Undertake organizational strategies. A hospitalist can find out how he or she has a voice in workload issues.“Figure out how hospitalists are represented in the structure of the group,” advises Dr. Whitcomb. “If a director is mandating how much [hospitalists] work, there has to be some mechanism for the physicians to be able to provide feedback. This often takes the shape of a compensation committee; this group is not just about compensation but about budget and sustainability for both the hospital and the hospitalists.” Physician representation—having a say in workload and schedule—is important to maintain a good balance within a hospital medicine program.
Step 3: Consider recommendations to ease workload. “You can try to change the workload through justifying adding staff or through putting systems in place that allow you to see more patients,” says Dr. Whitcomb. But what if the hospitalist considers or takes these steps and still finds his patient load to be unsustainable long term? “In terms of feeling like you’re not able to provide safe care,” says Dr. Whitcomb, “once you’ve suggested changes to the leadership and no changes are made, this may become a deal-breaker.”
Workload Leans on Other Pillars
The interesting thing about the workload/schedule pillar of job satisfaction is that, if you are unhappy with your workload, the other three pillars can sustain you and make you generally satisfied.
Dr. Whitcomb points to a 2002 article published in the Journal of Health and Social Behavior.1 The study examined a national survey of hospitalists and found that job burnout and intent to remain in the career are more meaningfully associated with favorable “community” relations than with negative experiences such as reduced autonomy.
“Workload is not a predictor of burnout as long as the other three pillars are intact,” summarizes Dr. Whitcomb.
Jane Jerrard has written for The Hospitalist since 2005.
Reference
- Hoff T, Whitcomb WF, Nelson JR. Thriving and surviving in a new medical career: the case of hospitalist physicians. J Health Social Behav. 2002 Mar;43(1):72-91
This is the second in a series on the four pillars of career satisfaction. Part 1 appeared on p. 14 in the June issue of The Hospitalist.
How can hospitalists work long days often packed from beginning to end and still remain happy with their jobs? One answer can be found in “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org), a comprehensive document by SHM’s Career Satisfaction Task Force (CSTF). This white paper can be used by hospitalists and hospital medicine practices as a toolkit for improving job satisfaction. It outlines the four pillars of career satisfaction.
The Second Pillar: Workload/Schedule
The workload/schedule pillar refers to the type, volume, and intensity of a hospitalist’s work as well as time pressures, variability of work, and number of interruptions. A hospitalist schedule must take all these factors into consideration.
CSTF Co-Chairperson Winthrop Whitcomb, MD, Mercy Medical Center, Springfield, Mass., maintains that this pillar is supported by the other three—autonomy/control, reward/recognition, and community/environment—but most closely with reward/recognition.
“There needs to be a reward system in place no matter what the workload,” says Dr. Whitcomb. “You can’t really talk about workload without addressing rewards. It’s human nature that in order to work hard, you need to be rewarded in some meaningful way.”
But many people—not just physicians but workers from all fields—may have separate concerns about heavy workload and just rewards.
An Example of Workload Issues
You probably know from your own experience as a hospitalist how workload can affect career satisfaction. Here is a fictional example of a hospitalist struggling with an increased patient load:
The director of my community-based hospital medicine program has mandated that each hospitalist see 15 to 20 patients each weekday, and 20 to 30 patients a day over weekends. I know this workload is too heavy to allow good quality of care. Under the pressure of seeing my quota of patients, I’m afraid I might make a mistake or miss something.
“There are physicians out there who can and do handle this type of workload, and they do it happily and well,” Dr. Whitcomb points out. “But this is only true if there is an appropriate reward system in place, and there clearly needs to be a good support system in order to provide quality of care” under this example.
CSTF says this individual should take the following steps:
Step 1: Go on a fact-finding mission. Find out whether hospitalist workload, responsibilities, and schedule at this facility are the norm. “[The hospitalist] should get an idea of what’s happening at other hospital medicine groups; he should understand the national picture,” says Dr. Whitcomb. “He might then realize that hospitalists in his group are only working 187 days a year, and that over a course of a year they’re not really working any harder than others who work more days,” says Dr. Whitcomb. “This might get him thinking a little bit differently about the workload.”
Step 2: Undertake organizational strategies. A hospitalist can find out how he or she has a voice in workload issues.“Figure out how hospitalists are represented in the structure of the group,” advises Dr. Whitcomb. “If a director is mandating how much [hospitalists] work, there has to be some mechanism for the physicians to be able to provide feedback. This often takes the shape of a compensation committee; this group is not just about compensation but about budget and sustainability for both the hospital and the hospitalists.” Physician representation—having a say in workload and schedule—is important to maintain a good balance within a hospital medicine program.
Step 3: Consider recommendations to ease workload. “You can try to change the workload through justifying adding staff or through putting systems in place that allow you to see more patients,” says Dr. Whitcomb. But what if the hospitalist considers or takes these steps and still finds his patient load to be unsustainable long term? “In terms of feeling like you’re not able to provide safe care,” says Dr. Whitcomb, “once you’ve suggested changes to the leadership and no changes are made, this may become a deal-breaker.”
Workload Leans on Other Pillars
The interesting thing about the workload/schedule pillar of job satisfaction is that, if you are unhappy with your workload, the other three pillars can sustain you and make you generally satisfied.
Dr. Whitcomb points to a 2002 article published in the Journal of Health and Social Behavior.1 The study examined a national survey of hospitalists and found that job burnout and intent to remain in the career are more meaningfully associated with favorable “community” relations than with negative experiences such as reduced autonomy.
“Workload is not a predictor of burnout as long as the other three pillars are intact,” summarizes Dr. Whitcomb.
Jane Jerrard has written for The Hospitalist since 2005.
Reference
- Hoff T, Whitcomb WF, Nelson JR. Thriving and surviving in a new medical career: the case of hospitalist physicians. J Health Social Behav. 2002 Mar;43(1):72-91
How to Hire and Use Clerical Staff
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
For the first few years of my career I was my own secretary. The hospitalist group I was part of ranged in size from two to nine doctors, and each of us handled all our own telephone correspondence and paperwork without clerical help. If you looked up our “office” phone number in the hospital’s physician directory you would find each individual’s pager number.
As a result, each of us got many pages every day regarding routine administrative issues such as hospital medical records, death certificates, and billing questions. Sometimes I felt as though I were answering nearly as many calls via pager as the hospital operator. And the pages about important clinical issues were mixed with all these routine inquiries.
While doing without clerical support in a hospitalist practice can help keep your overhead really low (ours was always well under 10%), it is not an efficient way to operate. A nonclinical support person is nearly always worthwhile. But, while the group I was part of made the mistake of trying to do without such a person (a problem we eventually fixed), a number of groups make the opposite mistake and hire too much clerical help, making it difficult or impossible to justify the cost.
Think carefully about clerical support positions. Unfortunately, in many practices in which the hospitalists are employees of the hospital, the doctors may not be engaged in deciding the optimal role and staffing (number of fulltime employees, or FTEs) for this position. To the doctors, it feels as though this person doesn’t cost them anything (in many cases the doctors aren’t paying for it directly, the hospital is), so they might not spend a lot of time thinking about whether they’re really getting good value for the money. But the doctors are in a much better position than other hospital administrators to know whether that position optimally supports the practice.
The amount of staffing and precise job descriptions will vary tremendously from one practice to another. I want to offer some general guidelines worth consideration by nearly all practices. This discussion is not about support personnel, such as case managers dedicated to the hospitalist practice, midlevel providers, or other clinical support staff. This discussion is really about the front-office support staff for your practice.
How Many to Hire?
My experience suggests a hospitalist practice should have about one FTE of clerical support for every five to 15 FTE hospitalists. The optimal staffing for a particular practice will vary depending on the person’s precise responsibilities. A practice that operates at more than one site (e.g., one hospitalist group covers two hospitals) will usually need more support than one that operates in one hospital.
Practices smaller than five or six FTE hospitalists often need less than full-time support. They might work well using part-time clerical support from an existing member of the hospital’s staff, such as someone in administration or the medical staff office. In many cases this might mean the person has one incoming phone line dedicated to hospitalist calls and another dedicated to the other activity. Depending on which line rings, he/she answers by saying, “hospitalist office,” or “medical staff office.” Usually it is best for the person to be responsible for both activities all day long and not divide his/her time into working for the hospitalists only until noon, then spending the rest of each day supporting the other activity. Until the group I am currently part of grew to eight FTE hospitalists, our clerical support person had a full-time job—half of which was devoted to supporting our practice and the other half to supporting the hospital’s Institutional Review Board (IRB).
Define the Job
There are a number of common ways for a support person to contribute to the practice, which I have grouped into several broad categories:
Handle telephone correspondence. This person should answer all calls to the practice’s main office number. Most practices will have a separate number for billing inquiries, and clinical calls from the hospital’s nursing staff are usually paged directly to the doctor by a nurse. But that still leaves a lot of calls that will go to the support person, such as administrative questions about the practice, calls from former patients (who have been discharged) and families, pharmacies (e.g., asking about refills), funeral homes, and others.
Some practices use a “triage pager” system in which all calls about new referrals to the practice (e.g., from ED doctors, referring PCPs, surgeons requesting consults) always go to the triage pager—day or night. Usually the individual doctors take turns carrying and responding to the triage pager, and after hearing about a referral to the practice they will call the doctor who is up next for new patients and pass the information along. In a large practice, that pager can generate a huge number of daytime calls, making it difficult or impossible for the person holding the triage pager to also care for patients.
Some practices have found that the practice clerical support person can take all those calls during the daytime Monday through Friday and pass them along to the appropriate hospitalist. The clerical person would typically get only the patient name and location and the referring doctor’s name and contact information, then page it to the hospitalist next in line for a new referral. That hospitalist would then call back the referring physician to get more clinical information. That relieves a member of the practice from taking all the calls. And, it puts the referring physician directly in contact with the hospitalist who will see the patient, rather than a triage doctor who won’t be caring for the patient. This should mean a better handoff.
Handle paper correspondence. This person can sort all the faxes, mail, and medical records that come to the practice, and put them in each doctor’s mail box in the office. He/she might initiate work on some forms. For example, upon arrival of a form to certify medical necessity for a piece of equipment (e.g., home oxygen ordered on a patient recently discharged) he might open the envelope, complete as much of the form as possible, attach the relevant records from the hospital stay, and leave all this for the doctor to sign.
Another potentially critical function is to request and pursue outside clinical records requested by one of the hospitalists. For example, a hospitalist admits Ms. Smith at 1 a.m. and realizes it will be helpful to get previous creatinine values from the PCP’s office and the report of a prior cardiac cath from an outside hospital. The hospitalist could simply record a voice mail (at 1 a.m., while seeing the patient) requesting that the practice assistant track down these things the next morning. That might include ensuring an appropriate release-of-information form is signed by the patient and faxed to the outside facility. When the records arrive, the assistant would place them on the patient’s chart (and, if necessary, page the hospitalist to report that the records have arrived).
Support billing functions. Practices use many strategies to ensure good documentation, coding, charge capture, and billing. The assistant might play an important role in this process. For example, the doctors might first report all charge data to the practice assistant who reviews it to make sure there are no conflicting charges (e.g., two doctors bill the same service to a patient on the same day) and no missing charges (e.g., a doctor forgot to submit a charge for one day of a patient’s stay). The assistant can be the principle connection between the doctors and the billing service and might be the first person to troubleshoot problems encountered by the billing service (e.g., getting additional documentation, figuring out which doctor can best address an ICD-9 code that lacks a fifth digit).
Perform general practice administrative functions. The assistant can keep track of when each doctor needs to renew his or her state license, DEA certificate, ACLS certificate, as well as keep track of total hours of CME (e.g., know how many more CME hours each doctor needs this year for state licensing requirements). He/she could also assist in various human resource functions such as ensuring each doctor responds during the open-enrollment period for benefits each year.
In some practices it is appropriate for the assistant to create the physician work schedule for the next month, quarter, or year, and serve as the main point of contact for any schedule change the doctor’s need to make. However, for groups that use a complicated scheduling system, the doctors will often need to take an active role in its creation. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is a co-founder and past-president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
In the Literature
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH
Thrombocytopenia Reaction to Vancomycin
Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced immune thrombocytopenia. N Engl J Med. 2007 Mar 1;356(9):904-910
The use of vancomycin has grown exponentially in the past 20 years.1 Physicians have become increasingly aware of its major side effects, such as red man syndrome, hypersensitivity, neutropenia, and nephrotoxicity. But there have been only a few case reports of thrombocytopenia associated with this drug. This article looked at cases of thrombocytopenia in patients referred for clinical suspicion of vancomycin-induced thrombocytopenia.
From 2001-2005, serum samples were sent to the Platelet and Neutrophil Immunology Laboratory at the BloodCenter of Wisconsin in Milwaukee for testing for vancomycin-dependent antibodies from several sites. Clinical information regarding these patients was obtained from their referring physicians and one of the authors. Platelet reactive antibodies were detected by flow cytometry.
IgG and IgM vancomycin-dependent antibodies were detected in 34 patients. It was found that platelets dropped an average of 93% from pretreatment levels, and the average nadir occurred on day eight. The mean platelet count was 13,600. After vancomycin was discontinued, the platelet count returned to normal in all patients except for the three who died. The average time for resolution of thrombocytopenia was 7.5 days.
Unlike other drug-induced thrombocytopenia, these cases of thrombocytopenia associated with vancomycin appear to be more prone to significant hemorrhage. In this group 34% were found to have had severe hemorrhage defined in this study as florid petechial hemorrhages, ecchymoses, and oozing form the buccal mucosa. Three patients who had renal insufficiency were found to be profoundly thrombocytopenic for a longer duration, presumably due to delayed clearance of vancomycin in this setting.
Based on this study, it appears thrombocytopenia is a significant adverse reaction that can be attributed to vancomycin. Unlike other drug-induced thrombocytopenias, it appears to be associated with a higher likelihood of significant hemorrhage, as well.
Thrombocytopenia is a common occurrence in the acutely ill hospitalized patient and has been linked to increased hospital mortality and increased length of stay.2 Many drugs and diseases that hospitalists treat are associated with thrombocytopenia. The indications for usage of vancomycin continues to grow with the increasing number of patients with prosthetic devices and intravascular access, and the increasing prevalence of MRSA. This study raises awareness of a significant side effect that can be associated with vancomycin.
References
- Ena J, Dick RW, Jones RN, et al. The epidemiology of intravenous vancomycin usage in a university hospital: a 10-year study. JAMA. 1993 Feb 3;269(5):598-602. Comment in JAMA. 1993 Sep 22-29;270(12):1426.
- Crowther MA, Cook DJ, Meade M, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005 Dec;20(4):248-253.
Can the mBRS Stratify Pts Admitted for Nonvariceal Upper GI Bleeds?
Romagnuolo J, Barkun AN, Enns R, et al. Simple clinical predictors may obviate urgent endoscopy in selected patients with nonvariceal upper gastrointestinal tract bleeding. Arch Intern Med. 2007 Feb 12;167(3):265-270.
Nonvariceal upper gastrointestinal bleeding is one of the top 10 admission diagnoses based on reviews of diagnosis-related groups. Patients with low-risk lesions on endoscopy, such as ulcers with a clean base, esophagitis, gastritis, duodenitis, or Mallory-Weiss tears, are felt to have less than a 5% chance of recurrent bleeding. In some instances, these patients can be treated successfully and discharged to home.1
Unfortunately, endoscopy is not always available—especially late at night and on weekends. It would be helpful to have a clinical prediction rule to identify patients at low risk for bleeding who could be safely discharged to get endoscopy within a few days.
In the study, 1,869 patients who had undergone upper endoscopy for upper gastrointestinal bleeding were entered into a Canadian national Registry for Upper GI Bleeding and Endoscopy (RUGBE). A modified Blatchford risk score (mBRS) was calculated to see if it could predict the presence of high-risk stigmata of bleeding, rebleeding rates, and mortality.
This mBRS was also compared with another scoring system—the Rockall score. The mBRS uses clinical and laboratory data to risk assess nonvariceal bleeding. The variables included in the scoring system include hemoglobin, systolic blood pressure, heart rate, melena, liver disease, and heart failure. High-risk endoscopic stigmata were defined as adherent clot after irrigation, a bleeding, oozing or spurting vessel, or a nonbleeding visible vessel. Rebleeding was defined as hematemesis, melena, or a bloody nasogastric aspirate in the presence of shock or a decrease in hemoglobin of 2 g/dL or more.
Patients who had a modified Blatchford risk score of <1 were found to have a lower likelihood of high-risk stigmata on endoscopy and were at a low risk for rebleeding (5%). Patients who had high-risk stigmata on endoscopy but an mBRS score of <1 were also found to have low rebleeding rates. The mBRS seemed to a better predictor than the Rockall score for high-risk stigmata and for rebleeding rates.
Patients with nonvariceal upper gastrointestinal tract bleeding may be identified as low risk for re-bleeding if they are normotensive, not tachycardic, not anemic, and do not have active melena, liver disease, or heart failure. It is conceivable that if endoscopy were not available, these patients could be sent home on high-dose proton pump inhibitor and asked to return for outpatient upper endoscopy within a few days.
The study certainly raises interesting questions. Whether it is acceptable practice to discharge a “low-risk” patient with an upper gastrointestinal hemorrhage on a high-dose proton pump inhibitor with good social support and close outpatient follow-up, but without diagnostic endoscopy is still unclear.
The study is limited by the fact that it is a retrospective analysis; however, it does examine a large cohort of patients. The authors acknowledge this, and this work could lead to a prospective randomized trial that would help answer this question. In the meantime, the mBRS may be a helpful tool to help risk stratify patients admitted for nonvariceal upper gastrointestinal bleeding.
References
- Cipolletta L, Bianco M, Rotondano G, et al. Outpatient management for low-risk nonvariceal upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 2002;55(1):1-5.
Lumbar Puncture to Reduce Adverse Events
Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006 Oct 25;296(16):2012-2022.
Lumbar punctures (LPs) remain a common diagnostic test performed by physicians to rule out meningitis. This procedure may be associated with adverse events, with headache and backache the most commonly reported. This systematic review and meta-analysis sought to review the evidence regarding diagnostic lumbar puncture techniques that might reduce the risk of adverse events, and to examine the accuracy of cerebrospinal fluid (CSF) analysis in the diagnosis of bacterial meningitis.
Studies were identified through searches of the Cochrane Library (www3.interscience.wiley.com/cgi-bin/mrwhome/106568753/AboutCochrane.html), MEDLINE from 1966 to January 2006, and EMBASE from 1980 to January 2006 (without language restrictions) to identify relevant studies. Bibliographies of retrieved articles were also used as data sources.
Randomized controlled trials of patients 18 or older undergoing lumbar puncture testing interventions to facilitate a successful diagnostic procedure or reduce adverse events were identified and selected. As a secondary outcome, trials that assessed the accuracy of CSF biochemical analysis for the diagnosis of bacterial meningitis were also identified and included. Trials that studied spinal anesthesia or myelography were excluded.
Study appraisals for quality (randomization, blinding, and outcome assessment) and data extraction were performed by two investigators independently. Fifteen randomized trials of interventions to reduce adverse events met criteria for inclusion, and four studies of the diagnostic test characteristics of CSF analysis met criteria and were included.
Meta-analysis with a random effects model of five studies (total of 587 patients) comparing atraumatic needles with standard needles yielded a nonsignificant decrease in the odds of headache with an atraumatic needle (absolute risk reduction [ARR], 12.3%; 95% confidence interval [CI], –1.72% to 26.2%). A single study of reinsertion of the stylet before needle removal (600 patients) showed a decreased risk of headache (ARR, 11.3%; 95% CI, 6.50%-16.2%). Meta-analysis of four studies (717 patients) revealed a nonsignificant decrease in headache in patients mobilized after LP (ARR 2.9%; 95% CI, –3.4 to 9.3%).
Data from the diagnostic test studies yielded the following likelihood ratios for diagnosing bacterial meningitis: A CSF–blood glucose ratio of 0.4 or less with a likelihood ratio of 18 (95% CI, 12-27); CSF white blood cell count of 500/µL or higher with a likelihood ratio of 15 (95% CI, 10-22); and CSF lactate level of >31.53 mg/dL with a likelihood ration of 21 (95% CI, 14-32) in accurately diagnosed bacterial meningitis.
These data support the reinsertion of the stylet before needle removal to reduce the risk of headache after lumbar puncture and that patients do not require bed rest after diagnostic lumbar puncture. Biochemical analyses, including CSF-blood glucose ratio, CSF leukocyte count and lactate level are useful in diagnosing bacterial meningitis.
This Rational Clinical Examination systematic review and meta-analysis provides a nice review of the available data on optimizing diagnostic lumbar puncture technique to reduce adverse events. It is somewhat remarkable so little has changed in our knowledge about this long-standing diagnostic procedure. Post-lumbar puncture headaches remain a challenge that may affect patient satisfaction as well as hospital (or observation unit) course particularly for patients who do not have evidence of bacterial meningitis once the analysis is complete.
This review seems to provide some useful answers for physicians performing lumbar puncture, who should consider selecting a small gauge needle and reinserting the stylet prior to removal. Future studies of other maneuvers to reduce post-procedure adverse events should be considered for the question of atraumatic needles, which may be technically more difficult to use. The review confirms and helps quantify the utility of CSF biochemical analysis in the diagnosis of bacterial meningitis.
Who’s Performing Procedures?
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Ann Intern Med. 2007 Mar 6;146(5):355-360. Comment in Ann Intern Med. 2007 Mar 6; 146(5):392-393.
Prior surveys of physicians documented that general internists performed a variety and significant number of procedures in their practice. Much has changed since those prior assessments, including physician training, practice settings, availability of subspecialists, and regulatory requirements that have altered physician’s practice with regard to procedures. This study sought to reassess the volume and variety of procedures performed by general internists compared with the prior survey of 1986. The final sample included 990 completed surveys from general internists from 1,389 returned questionnaires for a successful completion rate of 39.6%.
The median number of different procedures performed in practice decreased from 16 in 1986 to seven in 2004. Internists who practiced in smaller hospitals or smaller towns reported performing almost twice as many procedures as physicians in the largest hospitals and cities. Hours spent in the care of hospitalized patients were also associated with an increased number of different procedures—in particular mechanical ventilation, central venous catheter placement, and thoracentesis. For all but one of the 34 procedures common to both surveys, fewer general internists performed them in 2004 compared with 1986. Remarkably, for 22 of the 34 procedures, a greater than 50% reduction in the proportion of respondents who performed the procedure was noted.
In the 1986 survey, the majority of internists performed all but one of the six procedures required by the American Board of Internal Medicine (ABIM) for certification (abdominal paracentesis, arterial puncture for blood gases, central venous catheter placement, joint aspiration, lumbar puncture, and thoracentesis). Except for joint aspiration, in 2004 these required procedures were performed by 25% or fewer of the respondents.
The 2004 survey demonstrated a striking reduction in the number of different procedures performed by general internists, and a decrease in the proportion of internists who do most procedures. These reductions may stem from a variety of changes in physician practices, including the emergence of hospitalists, availability of subspecialty physicians and proceduralists, and changes in technology and regulatory environments.
Regardless of the forces behind these changes, internal medicine residents’ training in procedures should be re-examined.
Many of those in academic hospital medicine have noted a decline in procedures performed by general internists at large academic centers. This study affirms this trend overall and in particular for physicians in large urban settings or in the largest hospitals. The emergence of hospital medicine may have played a role in reducing the procedures performed by primary care (outpatient) physicians who now spend less time caring for medically ill hospitalized patients.
Residency programs now must consider how to incorporate procedure skills and training to align with the needs of internists. The rising interest in careers in hospital medicine (as opposed to outpatient primary care) necessitates a new approach and individualized plans for gaining procedural skills to match career goals and practice settings. The new ABIM policy acknowledges this greater variability in the procedures performed by internists in practice, and takes steps to more closely align procedure requirements and core manual skills with physician practice.
These changes and new flexibility in requirements provide another opportunity for academic hospital medicine programs to provide leadership, and help shape the training of inpatient physicians. TH
Enchondromatosis
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
Patient history: A 53-year-old female admits with a history of multiple orthopedic, dermatologic, and plastic-surgical procedures. The physical exam is notable for multiple cutaneous hemangiomas.
Salient findings: The images show old fracture deformities of the left fibular shaft and proximal tibia as well as a deformity of the distal femur. The patient has had a left total knee arthroplasty. There are multiple lucent lesions involving the left second, fourth, and fifth rays, with bone deformities. Findings are consistent with multiple chondromas. There is no evidence for malignant degeneration.
Patient population and natural history of disease: Enchondromatosis is a condition of multiple benign ectopic rests of cartilage growing within intramedullary bone, forming lucent lesions and bone expansion on radiographs. The enchondromas can deform and shorten a limb and can predispose the patient to a pathologic fracture. Enchondromas account for 12%-14% of benign bone neoplasms. When associated with cutaneous and visceral hemangiomas, the condition is called Maffucci’s syndrome.
Most patients with Maffucci’s syndrome will develop malignant transformation of at least one enchondroma into a chondrosarcoma (malignant cartilage tumor). Enchondromatosis without hemangiomas is known as Ollier’s disease; about 25% of patients with Ollier’s disease will develop chondrosarcoma by age 40. Both Maffucci’s syndrome and Ollier’s disease are nonhereditary. Metachondromatosis, a condition characterized by multiple enchondromas, is an autosomal dominant condition uniquely associated with osteochondromas.
Management: The physician who evaluates a patient with Maffucci’s syndrome must have a high suspicion for pathologic fracture and malignant degeneration. All bone pain and swelling should be evaluated with plain radiographs. Bone expansion, cortical breakthrough, soft-tissue mass, and deep endosteal scalloping of the cortex are indicative of malignant transformation. These findings are unreliable in the smaller bones of the hands, however, and features of low-grade chondrosarcoma are often indistinguishable from benign enchondromas. Even in the absence of worrisome features on plain radiographs, if clinical suspicion is high, a CT scan and/or an MRI should be performed for further evaluation. Biopsy is often indicated on clinical findings, despite imaging characteristics. Hemangiomas can undergo rapid expansion and are often treated with surgery.
Take-home points:
- Enchondromas are the most common primary neoplasm of the bones in the hand and are benign;
- There is an increased risk of malignant transformation of enchondromas in patients with Ollier’s disease or Maffucci’s syndrome; and
- Biopsy of a lesion may be indicated if clinical suspicion for malignancy is high. TH
Helena Summers is a radiology resident and Erik Summers is a hospitalist at the Mayo Clinic College of Medicine in Rochester, Minn.
Bibliography
- Sun TC, Swee RG, Shives TC, et al. Chondrosarcoma in Maffucci’s syndrome. J Bone Joint Surg Am. 1985 Oct;67(8):1214-1219.
- Schwartz HS, Zimmerman NB, Simon MA, et al. The malignant potential of enchondromatosis. J Bone Joint Surg Am. 1987 Feb;69(2):269-274.
- Chew FS, Maldjian C. Enchondroma and enchondromatosis. emedicine. June 10, 2005. Available at: www.emedicine.com/radio/topic247.htm. Last accessed on March 14, 2007.
The Anorectic Heart
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Patient history: A 40-year-old male with a history of anorexia, depression, and recent weight loss presents for a general medical evaluation prompted by his concerned father. A computed tomography (CT) scan of his chest shows a moderate amount of pneumomediastinum (PM) extending superiorly into the tissues of the neck. He also has a moderate-size pericardial effusion. The patient denies symptoms of chest pain, shortness of breath, nausea, vomiting, or recreational drug use. Specifically, the patient admits to a depressed mood, but denies any vomiting, retching, or auto-destructive behavior. He has no history or evidence of underlying pulmonary disease.
Other notable findings consistent with the patient’s eating disorder are a body mass index (BMI) of 15, leukopenia, hyponatremia, bradycardia, and low blood pressure. A subsequent gastrograffin esophagram shows no obvious leaks or abnormalities. The patient is admitted to the hospital, allowed nothing by mouth, and placed on intravenous piperacillin and tazobactam, and nutrition. A transthoracic echocardiogram to evaluate the pericardial effusion on the first hospital day shows early tamponade physiology. Repeat evaluation two days later shows mild right atrial collapse but no evidence of hemodynamic compromise. Inpatient psychiatry consultation is obtained regarding his depression and eating disorder. On the fifth hospital day, a repeat CT scan shows moderate improvement of the PM. The patient is discharged home with outpatient follow-up.
Discussion: PM is defined as free air or gas in the mediastinum and is an uncommon finding. The etiology is usually from the airway, esophagus, or external trauma/surgery. Spontaneous PM occurs in the absence of an apparent identifiable cause and can exist in isolation or in conjunction with pneumothorax and soft-tissue emphysema. Elevated intraalveolar pressures related to mechanical ventilation or activities involving Valsalva maneuvers, along with pre-existing lung disease, account for the majority of pulmonary-related PM.1 Esophageal tear or rupture is another, less common cause of PM. Several case reports of PM in patients with anorexia nervosa exist, and some experts have postulated that one possible mechanism is vomiting or some other auto-destructive behavior.2-4 Loss of pulmonary connective tissue related to prolonged starvation leading to spontaneous pneumothorax and PM has also been postulated using rat models.5
The most common symptoms associated with PM are chest pain, voice change, and cough. In rare cases, PM can lead to decreased cardiac output. Common triggers of spontaneous PM, such as cough, physical exercise, and drug abuse, have been reported. A high percentage of patients with spontaneous PM have underlying pulmonary disease, including asthma and COPD.1 PM in conjunction with Boerhaave’s syndrome may have a mortality rate as high as 50% to 70%. In patients with anorexia nervosa, PM is often seen in conjunction with other advanced findings, including pancytopenia, electrolyte disturbances, bradycardia, and hypotension.
The age and gender of the patient are atypical for anorexia nervosa, although he does indeed have a restrictive eating disorder. The PM and pericardial effusion are additive unique findings that likely relate to his malnourished state and possible auto-destructive behavior.
Management: Spontaneous PM has been managed in a variety of ways, ranging from outpatient radiographic follow-up to close, inpatient monitoring. Identifying the etiology and monitoring for further progression or complications is important. For patients in whom esophageal tear or microperforation is suspected, early surgical consultation is recommended. An acceptable algorithm for patients with suspected esophageal perforation after endoscopy is to begin with a contrast CT scan of the neck and chest with oral contrast or to use a water-soluble contrast (gastrograffin) esophagram followed by a barium swallow if the water-soluble study is negative.6,7 When imaging reveals no leakage, the PM can be followed radiographically—typically after 48 hours and thereafter slowly advancing the diet. TH
Mackram Eleid, MD, works in the Division of Internal Medicine at the Mayo Clinic Arizona (Scottsdale/Phoenix). Joseph Charles, MD, FACP, is an assistant professor of Medicine and division education coordinator in the Mayo Clinic Hospital Arizona, Scottsdale/Phoenix.
References
- Campillo-Soto A, Coll-Salinas A, Soria-Aledo V, et al. [Spontaneous pneumomediastinum: descriptive study of our experience with 36 cases.] [in Spanish] Arch Bronconeumol. 2005;41:528-531.
- Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft-tissue emphysema without esophageal lesion. Int J Eat Disord. 2005 Nov;38(3):281-284.
- Brooks AP, Martyn C. Pneumomediastinum in anorexia nervosa. Br Med J. 1979;1:125.
- Chatfield WR, Bowditch JD, Forrest CA. Spontaneous pneumomediastinum complicating anorexia nervosa. Br Med J. 1979 Jan 13;1(6156):200-201.
- Sahebjami H, MacGee J. Changes in connective tissue composition of the lung in starvation and refeeding. Am Rev Respir Dis. 1983;128:644-647.
- Dodds WJ, Stewart ET, Vlymen WJ. Appropriate contrast media for the evaluation of esophageal disruption. Radiology. 1982 Jul;144(2):439-441.
- Ghahremani GG. Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993 Nov;31(6):1219-1234.
Get Control
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
This is the first in a series of articles on the four pillars of career satisfaction in hospital medicine.
How do you feel about the hours, compensation, responsibilities, and stresses of your present position? Do you think your job is sustainable—that is, would you be happy to continue your current work for years to come?
Many of today’s hospitalists might not answer the last question with a resounding “yes” because of one or more common factors that lead to chronic dissatisfaction with their careers.
In 2005, SHM formed the Career Satisfaction Task Force (CSTF) to combat this dissatisfaction, charging it with a three-pronged mission: to identify working conditions in hospital medicine that promote success and wellness; to provide resources to enhance career satisfaction; and to promote research into hospitalist career satisfaction and burnout.
“Originally, we were concerned with burnout in hospital medicine,” says CSTF co-chair Sylvia C. W. McKean, MD, FACP, medical director at Brigham and Women's Hospital/Faulkner Hospitalist Service and associate professor of medicine, Harvard Medical School, Boston. “The task force was charged to examine the factors that lead to a long, satisfactory career in hospital medicine.”
New White Paper Available
After reviewing the literature on physician burnout and general career satisfaction, the CSTF created a comprehensive document, “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available at www.hospitalmedicine.org), which can be used by hospitalists and hospital medicine practices as a toolkit for improving or ensuring job satisfaction.
The white paper outlines the four pillars of career satisfaction: autonomy/control, workload/schedule, reward/recognition, and community/environment. It includes a Job Fit self-evaluation questionnaire and other tools and advice that can be used to gather information and take steps to improve problems identified by the survey.
While the information in the white paper can best be used to improve an entire hospital medicine program, individual hospitalists can also benefit from it. The paper clearly states that an individual hospitalist has the power to influence change within his or her job, perhaps by majority rule. They can find a niche of expertise within their practice; pursue continuing medical education opportunities to promote their areas of expertise; nurture networks with peers; and find a mentor and regularly seek advice.
The First Pillar: Autonomy/Control
Control, or autonomy, refers to the need to be able to affect the key factors that influence job performance. For example, do you have control over when, how, and how quickly you perform a specific task? Do you have some say in task assignment and policies? What about the availability of support staff, supplies, and materials?
“Doctors expect to have control in their jobs, control over the tasks they do, how and when they do those tasks,” says CSTF member Tosha Wetterneck, MD, University of Wisconsin Hospital/Clinics in Madison. “This control helps them cope with stress; take that control away, and they can’t cope as well.”
Autonomy is a problem in hospital medicine because the field is still new and not widely understood. Consequently, hospitalists may end up responsible for additional duties and hours—especially on weekends—that other physicians dump on them.
“In some hospitals, the only doctors who can’t cap [their workloads] are the hospitalists,” reports Dr. McKean.
The best way to ensure you’re comfortable with the autonomy offered by your position is to be aware of what you want—and what you get—when you take your job.
“An individual hospitalist always has a choice of taking a job with the clear understanding of what they’ll have control over,” says Dr. Wetterneck. “However, you have to understand what you as a person need to have control over. You don’t want to get yourself into a position where you don’t have control over the specific areas that matter the most to you.”
An Example of Autonomy
To help clarify how lack of autonomy can make career satisfaction plummet, here is a fictional example of a hospitalist who suddenly lost control in her job:
“I love working in hospital medicine and take my job very seriously. However, two months ago my hospital medicine group assumed responsibility for care of neurosurgical patients, and all hospitalists are now required to provide care to these patients. I find this upsetting—I feel like this is one more step in relegating my colleagues and I to the status of ‘super-residents’ who are responsible for everything that other physicians don’t want to do. I want to have control over which type of patients I see.”
According to the CSTF research, this individual should take the following steps:
Step 1: Assess the situation in the manner outlined in the white paper. The hospitalist should:
- Use the Job Fit questionnaire to profile the control elements of the hospitalist practice;
- Become familiar with the hospital’s leadership and committee structure;
- Understand key payer issues that might affect inpatient care; and
- Review her job description.
After reviewing the role personal autonomy plays within her practice, the hospitalist must consider whether she’s in a position to request a change of duties, or whether her new responsibilities are non-negotiable.
“There are different facets of control,” says Dr. Wetterneck. “Some could make the argument that a hospitalist doesn’t have the skills to take care of neurosurgical patients, that this is out of the realm of reasonable expectations for the job. Others might say that there is reasonable expectation, as long as the hospitalists would get extra learning and extra support from other [subspecialists] that they’d be available for consult.”
Regardless of where you stand on the argument of reasonable expectation of a hospitalist’s responsibilities, what if a new job task simply rubs you the wrong way—to the point where you no longer enjoy your work?
“If it’s truly an issue of ‘I don’t want to do this,’ then it becomes an issue of your fit with your group,” Dr. Wetterneck continues. “If everyone in the group is doing it and you don’t want to, then you need to understand how important this control is for you. Is it important enough to change jobs?”
Step 2: If the answer to that last question is “Yes,” this hospitalist should keep autonomy in mind as she begins a job search. The white paper includes questions to ask herself and her potential employers to ensure she has control in her next position. The diversity of hospitalist responsibilities works in her favor—assuming she’s willing to move to another part of the country.
“You can list all the things that make you happy in a job, and you can probably find every single thing on your list in a hospitalist job somewhere in the U.S.,” speculates Dr. Wetterneck.
Next Month
A discussion of the workload/schedule pillar, which refers to the type, volume, and intensity of a hospitalist's work.
The Only Constant
Working in hospital medicine practically guarantees your job will continually change. Whether it’s a change in responsibilities like the example above, the steady growth of your practice, or even a change in leadership or ownership, hospitalists must go with the flow.
“I definitely think that the job requires a certain amount of flexibility,” says Dr. Wetterneck. “Hospitalists have to understand that their job role will continue to change over time. Therefore, people have to really understand what’s important to them.”
The cost of lack of autonomy—or other job stressors—can be severe.
“If a change [in your job] throws you out of control, this can lead to stress,” Dr. Wetterneck points out. “We know from recent studies that stress has an impact on your health, specifically on cardiovascular disease and mortality.” TH
Jane Jerrard has written for The Hospitalist since 2005.
Capitol Gains
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Nine members of SHM’s Public Policy Committee (PPC), accompanied by several SHM staff members, paid a visit to Capitol Hill early this year.
The group spent Feb. 28 calling on senators, representatives, and congressional staff, as they participated in meetings similar to those included in SHM’s Legislative Advocacy Day, held during the 2006 Annual Meeting. In fact, many of the PPC members had second meetings with legislative staff they had met last May.
“We had already broken some ground with Legislative Day, so some people were familiar with us,” says Ron Angus, MD, Department of Medicine, Presbyterian Hospital of Dallas. “We had a little more time to talk about the issues.”
During their meetings, “We emphasized the different roles that SHM can play, and we tried to get a feel for what it means to have a Democrat-led Congress,” says Jack Percelay, MD, MPH, FAAP, Virtua Health, Ridgewood, N.J.
SHM’s senior adviser for advocacy and government affairs, Laura Allendorf, pronounces it “a very productive day.”
Building on a Foundation
The PPC visits were successful partly because this was the second time SHM had visited representatives, allowing the hospitalists to build on their introductory meetings and spend more time discussing issues and offering help. The committee hopes to continue this trend.
“In the long term, we want to see if we can meet with the same people more frequently,” explains Dr. Angus. Allendorf agrees, saying, “The more often we’re up there, the better.”
There may be many more visits or communications. “I think we’re building something long-term, and it’s going to take a while to do that,” says Dr. Angus. “As we get more comfortable talking to these folks, we’ll work on getting them to contact us when issues first come up. Our goal is to be there at the beginning of the process, rather than the end, when it’s too late to have much impact.”
Another reason the February visits were deemed a success involves whom the PPC met with.
“These meetings were more productive because we were meeting with key staff, people on key committees,” recounts Allendorf. “And [participants] had more visits during the day—each had between five and eight. We made a point to meet with committee staff, staff for key committees, including the House Ways and Means Health Subcommittee, the Senate Finance Committee, the Senate Committee on Appropriations, and the Senate Committee on Health, Education, Labor, and Pensions. We met with committee aides hired to handle special issues like Medicare Part B.”
Targeting these influential offices—particularly the powerful Ways and Means Committee—should have greater impact on healthcare legislation and funding.
Making Inroads with Ways and Means
The entire group ended the day in a meeting with Rep. Shelley Berkley, D-Nev., and her health legislative aide Jeff Davis. Berkley serves on the House Ways and Means Committee and is perceived as “physician-friendly.” Her husband is a nephrologist, and Allendorf describes the lawmaker as “very knowledgeable about the issues” in healthcare. “She’s now in a position to do something; she’ll be a major player,” predicts Allendorf.
“We met with Berkley for five or 10 minutes, then had a roundtable with Jeff Davis from her office,” says Dr. Angus. “We talked about increased funding for AHRQ [Agency for Healthcare Research and Quality] and coordinating quality initiatives being brought to bear in hospitals. We tried to emphasize that when you talk about quality in hospitals, you’re talking about hospitalists.”
With her majority role on a key committee, Berkley is one example of the newly empowered Democrats in office—Democrats who may make a difference in pushing through SHM-sponsored legislation.
Democratic Differences?
Did the PPC members notice a difference since May, with the change of majority party in Congress?
“I could feel it,” says Dr. Angus. “There’s been a huge sea change. Those who felt unempowered last year now feel that there’s a clean slate.”
Dr. Percelay saw a difference in priorities among healthcare issues. “In general, the access issue is much more prominent,” he says. “There’s a sense that we need to do something about healthcare expenses and access for everyone. There’s a recognition of big-picture issues—by both Democrats and Republicans—that we aren’t providing coverage for everyone, and we’re spending too much on it.”
Future Advocacy
The PPC counts its Capitol Hill visit a success. Members want to broaden the influence of SHM and hospitalists by enlisting the help of others.
“We want to identify members who are interested in public policy who live in key areas—areas served by legislators on key committees,” explains Dr. Percelay, “so that they can lobby from a local perspective.” Dr. Angus adds, “Ideally, they’ll interact with their national officials when they’re in their local offices. Also, we’d like members to keep an eye on state and local issues.”
Allendorf points out that these members can be identified and reached though SHM’s online Legislative Action Center at capwiz.com/hospitalmedicine/home. If you receive an e-mail asking you to contact one of your representatives regarding a specific issue, you can take part in the advocacy efforts.
In other plans, says Dr. Angus, “We hope to construct some body of resources that hospitalists who go to D.C. on their own can use to go up to the Hill with information in hand and talk to their Congress people.”
PPC members understand they have their work cut out for them when it comes to increasing awareness of SHM and hospitalists on Capitol Hill.
“This is a long-term investment process,” Dr. Percelay says. “We’re learning as an organization how to conduct our public policy efforts. We’re at the beginning stages of meeting with these people and letting them know what hospitalists can do.” TH
Jane Jerrard writes “Public Policy” for The Hospitalist.
Key Keynotes
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
The 10-year anniversary of SHM was an occasion not for looking back on the first decade of the organization, but for looking ahead.
In addition to seven tracks of educational sessions and ample opportunities for networking, SHM’s 10th Annual Meeting, held May 23-25 in Dallas, provided opportunities to get a big-picture glimpse into the future of hospital medicine, in the form of some eye-opening plenary sessions.
Coming Soon: Hospital Medicine Certification
Annual Meeting attendees heard from Robert M. Wachter, MD, and past-SHM President Mary Jo Gorman, MD, MBA, on “Certification in Hospital Medicine: What Does This Mean to Hospitalists? To Employers? To Patients?” The two outlined how the American Board of Internal Medicine (ABIM) is developing a Focused Recognition for Hospital Medicine through its Maintenance of Certification (MOC) system.
Dr. Wachter, who chairs the ABIM Committee on Hospital Medicine Focused Recognition, explained that the focused recognition would give hospitalists a formal credential that recognizes hospital medicine as a distinct field within internal medicine. This is the first time ABIM has offered focused recognition for any subset of internal medicine—and, if approved, the first time the umbrella organization, the American Board of Medical Specialties (ABMS), will offer a focused recognition for a subset of any specialty.
“This is a brand new idea,” stressed Dr. Wachter. “One of the exciting things—the challenging things—is that this is a first step toward the broader issue of how to certify based on experience rather than just training.”
A Look at Digital Medicine
Informally known as the “health technology czar,” David J. Brailer, MD, PhD, served as the first national coordinator for Health Information Technology, at the Department of Health and Human Services until he resigned in April 2006. He is vice chairman of the American Health Information Community, and based on his plenary session “Health Care’s Digital Era: Implications for Hospitalists,” he is obviously familiar with hospital medicine.
“Hospitalists and health IT are co-factors in the same equation of change in healthcare,” said Dr. Brailer. “I can’t see how one can exist without the other.”
He went on to explain that hospitals must lead the way for digital medicine, as they are the institutions with the most opportunity for cost reductions in healthcare, the most opportunity for error reduction (“I’m not saying hospitals have the most errors, but that the corporatized process allows them to reduce errors that occur there,” he clarified), and the best site for innovation to move to a virtual model such as e-ICUs and new tele-specialties.
“And who can we turn to who ‘gets it,’ who can make all this happen?” asked Dr. Brailer of the innovations. “It won’t be the cardiologists, or the emergency department doctors. The obvious answer is that it will be the hospitalists.”
He warned that in order for hospitalists to be change agents, they must first take on the role of leaders of other doctors in inpatient care. “Some [hospitalists] don’t want to take on this role; others are already doing it,” he said. “I think that doctors need this leadership and I can’t think of a better group to do it than hospitalists. They’re going to have to step up to the plate on this.”
Dr. Brailer listed big issues coming up for hospitals, predicting that they will become “the hub of chronic-care management, leaders in adopting state-of-the-art technology, and leaders in quality improvement. Hospitalists are attached to each of these.” He explained that in chronic-care management, patients with chronic illnesses are cared for in a continuum-based way. Currently, inpatient care is the anchor not just for treatment, but for monitoring weight or assessing daily function levels. With chronic-care management, doctors can monitor patients without having them come into the office or the hospital.
“Primary-care doctors won’t be able to perform this off-site monitoring; they don’t have the time or the infrastructure,” explained Dr. Brailer. “But this is exactly what hospitals already do. Electronic monitoring is a real opportunity for them—and for hospitalists—to expand their care offerings.”
In spite of this expansion, he warned that hospitals will be in danger if they don’t change with the times. “The world is moving away from hospital-based care and toward [patient]-centered care,” he stated. “This is apparent in the current push for portability of patient-care information, and in today’s healthcare transparency issues. These are not hospital-friendly measures; in fact, they threaten hospitals to some degree. I hope that these trends will challenge hospitals to question how changes apply to them.”
Dr. Brailer ended with an update on public policy regarding healthcare—not a pretty picture from his insider’s view.
“Not much will happen in the next two years,” he predicted. “The FDA will pass the Prescription Drug User Fee program, and SCHIP [State Children’s Health Insurance Program] will pass in Washington D.C. I don’t think anything else will make it through the thicket of everything else going on.”
He also warned that regardless of who the next president of the U.S. is, nothing much will happen with healthcare reform. “It’s a high-priority item, but not high enough to warrant significant attention,” he said. “In the long term, it will get major attention, but probably only as a result of a catastrophe.”
Factors That Will Shape Our Future
On Friday morning, attendees heard from Jonathan B. Perlin, MD, PhD, MSHA, former under secretary for health at the Veterans Affairs, and currently the chief medical officer and senior vice-president of quality for Hospital Corporation of America (HCA) in Nashville, Tenn.—the nation’s largest hospital group.
In presenting, “Healthcare 2015: Challenges and Opportunities in the Decade Ahead,” Dr. Perlin threaded together the factors that will drive healthcare to a new level in the next eight years: the health needs of the population, including aging and the complications of diabetes, the increased requirements for delivering value, the economic pressures, and the technological changes and decentralization of healthcare delivery. Dr. Perlin, a leader in healthcare transformation and health information technology who has been termed a “clinical futurist,” pointed out that the result of these factors will be a transformation from an industrial to an information age model of healthcare.
Dr. Perlin traced the path being shaped by these challenges and opportunities, explaining that the economics of healthcare are creating pressure on the environment and disrupting the status quo. “Costs are increasing rapidly,” he stated. “It’s pretty clear that we’ve already hit some statutory alarms in the Medicare trust fund. Estimates now indicate that the trust fund will be bankrupt by 2018; we can either limit what we do or we can find better value in delivery of care.”
Response to economic pressure by Medicare and private insurers, said Dr. Perlin, provides a construct for change.
“The private sector, the government, and employers are all saying that we’re not going to buy units of healthcare services any more, we’re going to buy outcomes,” stressed Dr. Perlin. “The result is that performance becomes a gate function for even doing business in the new world.”
Toying with modest incentives in current pay-for-performance models will soon be trumped. “Medicare is changing from an incentive for simply reporting [with the current “Reporting Hospital Quality Data for Annual Payment Update” program] to value-based purchasing,” Dr. Perlin pointed out. Similarly, private insurers are differentiating performance levels and using lower co-pays to direct patients to better performers and high co-pays to redirect patients away from lower performers.
To participate in this new world of value-based purchasing and what Dr. Perlin termed “tiering and steering,” the healthcare industry must reorganize ways that it has traditionally provided care. Pen and paper are replaced by electronic health records. A locus of care is replaced by an interoperable, coordinated cooperative information network.
“The patient is the point of care in the new system, whether supported by glucometers that feed data into a central system,” said Dr. Perlin, “or a heart failure patient is tracked after discharge with a digital scale … or whether it is a hospitalist who reaches into the traditional healthcare setting with remote monitoring to provide round-the-clock support to a critically ill patient.”
In addition to providing enhanced safety, quality, continuity, and efficiency, new systems like these will provide central information sources, powerful in providing real-time, clinical decision-support, as well as generating new knowledge about disease, treatment and service delivery. The tremendous data available will reveal previously unnoticed patterns and provide more support for evidence-based care.
“Medicare and private insurers are focusing more on evidence-based care and are increasingly ambivalent about decisions not supported by evidence,” observed Dr. Perlin.
His view of the near future of healthcare was followed later that day with another plenary session that mulled how hospital medicine might look a decade from now.
Now It’s Time to Say Goodbye …
Dr. Wachter traditionally closes each Annual Meeting with a review of how far the young field of hospital medicine has come.
But at the 10th Annual Meeting, Dr. Wachter chose not to look back but to peer into his crystal ball. His presentation, “The Hospitalist Movement Two Decades Later: A Letter from the Future,” took the form of a letter from his future self, written in 2017, to SHM CEO Larry Wellikson, MD, as each man settles into a long-term care facility.
Dr. Wachter outlined the major forces starting to affect hospital medicine and imagined where they would lead us. And he couldn’t resist one glimpse back in time: “Think about the change we’ve seen already,” he marveled. “There’s no field in modern medical history that’s grown this quickly. We’re both leading the way and riding the waves.”
Dr. Wachter admitted his initial estimates for phenomenal growth of the field are already surpassed. “We originally projected that there would be 20,000 or 30,000 hospitalists,” he said. “Well, we’re already over 20,000. Now I’m thinking the final number will be around 50,000 or 60,000.”
He attributed part of that growth to several changes, including the additional responsibility of hospitalists for caring for surgical patients—something he sees as eventually becoming the norm. Another factor is the role hospitalists play in replacing residents in teaching hospitals, an area that has seen unplanned growth.
And finally, Dr. Wachter speculated that the quality measures movement will also boost the ranks of hospitalists. “We’re already seeing tremendous pressure on hospitalists to help their hospitals achieve success in pay-for-performance programs and in publicly reported measures,” he said. “This type of responsibility was originally considered a nice add-on for using hospitalists, but now it’s getting to be a crucial part. There’s a building expectation that hospitalists will guarantee superb performance.”
Dr. Wachter also touched on how information technology might change hospital medicine. “IT will definitely have an impact, in some exciting ways, and in other ways that have not been thought through,” he warned. “For example, consultation may be very different.” For example, a hospitalist in 2017 may be able to use a video link at a patient’s bedside to consult with one of 100 cardiologists around the country or around the world.
Following Dr. Wachter’s view of the future, Sylvia C. McKean, MD, had the last word at the meeting. As the chair in charge of next year’s Annual Meeting in San Diego, she presented the wrap-up on Friday afternoon, covering “What Have We Learned.”
Looking back on the previous three days, Dr. McKean pronounced, “The future is now.” Pointing to the number of meeting sessions, abstracts and poster presentations that emphasized recent innovations in hospital medicine, she said, “The Annual Meeting helps us find our expertise as hospitalists.” The Annual Meeting, along with SHM’s published Core Competencies helps define the role that hospitalists play in patient-centered care and in patient safety.
Dr. McKean thanked Chad Whelan, chair of the Annual Meeting Committee, for all his work, and said she was looking forward to 2008.
SHM Elects New Members to Board of Directors
Two new members announced; one member re-elected
SHM is pleased to announce the election of Joseph Li, MD, and Mahalakshmi Halasyamani, MD, and the re-election of Patrick Cawley, MD, to its board of directors for terms that began at the SHM Annual Meeting May 23-25 in Dallas.
“One of the strengths that keeps SHM on the cutting edge is the infusion of new talent on the board. SHM is fortunate to have a continued source of hospitalist leaders who willingly share their time and talents to help SHM shape and grow the hospital medicine specialty,” says Larry Wellikson, MD, CEO of SHM.
Each of the newly elected SHM board members comes from distinguished programs and institutions.
Dr. Li is the director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and an assistant professor of medicine at the Harvard Medical School. He has been an active member of SHM, serving on the Education and Annual Meeting Committees, as well as the Procedures Task Force. Dr. Li earned his bachelor’s degree in pharmacy at the University of Oklahoma College of Pharmacy and his medical degree at the University of Oklahoma College of Medicine. He completed his residency at the Beth Israel Deaconess Medical Center.
Dr. Cawley is executive medical director at the Medical University Hospital of South Carolina. Prior to this, he was chief of staff at Conway Medical Center, S.C. He has served on the SHM board of directors since 2004 and is its treasurer. As an active member of SHM, he serves on the Public Policy Committee, Leadership Task Force, and on the advisory board for the Practice Management and Coding Courses. Dr. Cawley earned his bachelor’s degree in biology and chemistry from the University of Scranton (Penn.) and his medical degree from Georgetown University School of Medicine in Wash., D.C. He completed his residency at the Duke University Medical Center in Durham, N.C.
Dr. Halasyamani is the medical director of the heart failure program at Saint Joseph Mercy Hospital in Ann Arbor, Mich. Before that, she served as director of academic internal medicine inpatient services. She is also a clinical instructor of internal medicine at the University of Michigan and associate chair of the department of internal medicine at Saint Joseph Mercy Hospital. Dr. Halasyamani earned her bachelor’s degree in English and chemistry from Saint Louis University (Mo.) and her medical degree from Harvard Medical School, Boston. She completed her residency at Brigham and Women’s Hospital.
Congratulations to the newest members of the SHM Board of Directors.
What's Your Diagnosis?
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.
An 84-year-old white female, a former smoker with a medical history significant for coronary artery disease, chronic renal insufficiency, hypertension, and hyperlipidemia, presented to our hospital with two weeks of progressively worsening lower-back pain.
A detailed review of systems was negative for other symptoms. The patient was normotensive with stable vital signs. A physical examination found a 4 cm nontender, pulsatile mass above umbilicus, but a neurovascular exam of her lower extremities was normal. Laboratory testing revealed an elevated serum creatinine of 4.8 mg/dL (0.8-1.2 mg/dL). An abdominal computed tomography (CT) scan without contrast was performed. (See figure 1, below). TH
What should be your next appropriate
a) Obtain additional imaging studies
b) Initiate intravenous beta-blocker therapy to keep systolic blood pressure < 90 mm Hg
c) Initiate intravenous heparin therapy
d) Observation
e) Perform surgery emergently
Discussion
The answer is “d”: Observation. A CT scan of the abdomen without contrast shows a calcified abdominal aorta with aneurysmal dilatation measuring 4.4 cm in greatest diameter. No dissection or aneurysmal rupture is seen.
The abdominal aorta is the most common site for an arterial aneurysm, occurring below the origin of renal vessels in majority of cases. A diameter greater than 3.0 cm is considered aneurysmal.1 The prevalence increases markedly in individuals older than 60.2 Known risk factors include age, smoking, gender, atherosclerosis, hypertension, and family history of abdominal aneurysm.
The vast majority of the individuals with abdominal aortic aneurysms are asymptomatic. Abdominal or back pain is the most common complain in symptomatic patients. Often, patients have a ruptured aneurysm on presentation, along with pain in the abdomen, back or groin, hypotension with a tender, pulsatile abdominal mass seen on physical examination. In addition to history and examination, several imaging modalities are utilized for diagnosis. Most aneurysms are picked up incidentally on imaging studies performed for other purposes. Abdominal ultrasonography, CT scan, magnetic resonance imaging/magnetic resonance angiography and angiography are all used for diagnosis.
The size of the aneurysm is important when making management decisions. Risk of rupture increases dramatically for aneurysm diameter greater than 5-5.5 cm.3 Elective repair is generally indicated for asymptomatic aneurysms this size because mortality for emergency repair in case of rupture is extremely high. For asymptomatic aneurysms between 3.0-5.5 cm in diameter, the choice between surgery and surveillance depends on the patient’s preference, co-morbidities, presence of risk factors and the risk of surgery. For surveillance, monitor with ultrasound or CT scan every six to 24 months.1 Smoking cessation and treatment of hypertension and hyperlipidemia are important in medical management. Surgical repair is done either by the traditional transabdominal route or retroperitoneal approach. Endovascular stent grafts have also been introduced more recently. Symptomatic aneurysms require repair, regardless of the diameter.
Our patient had several risk factors, including age, smoking, hypertension, and atherosclerosis for developing an abdominal aortic aneurysm. After discussion of findings and management options, patient did not elect to undergo surgical repair. Smoking cessation, continued medical therapy for risk factors and surveillance was advised on discharge. TH
Drs. Aijaz and Newman practice at the Department of Medicine, Mayo Graduate School of Medical Education, Mayo Clinic, Rochester, Minn.
References
- Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006 Mar 21;113(11):e463-654.
- Singh K, Bønaa KH, Jacobsen BK, Bjørk L, Solberg S. Prevalence of and risk factors for abdominal aortic aneurysms in a population-based study: The Tromso Study. Am J Epidemiol. 2001 Aug 1;154(3): 236-244.
- Powell JT, Greenhalgh RM. Clinical practice. Small abdominal aortic aneurysms. N Engl J Med. 2003 May 8;348(19):1895-1901.