User login
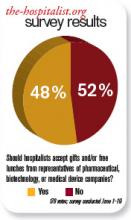
Should hospitalists accept gifts from pharmaceutical, medical device, and biotech companies?
Recent discussions on conflicts of interest in medical publications underscore the significance of the important yet fragile relationship between the pharmaceutical industry and healthcare professionals. Among these is an examination of how academic departments can maintain a relationship with the industry.1 This study suggests that if appropriate boundaries are established between industry and academia, it is possible to collaborate. However, part of the policy in this investigation included “elimination of industry-supplied meals, gifts, and favors.”2
The Institute of Medicine’s “Conflict of Interest in Medical Research, Education, and Practice” included groundbreaking recommendations.3 Among them was a call for professionals to adopt a policy that prohibits “the acceptance of items of material value from pharmaceutical, medical device, and biotechnology companies, except in specified situations.”3
Our nation has been embroiled in a healthcare debate. Questions of right versus privilege, access versus affordability, and, of course, the perpetual political overlay have monopolized most of the discourse. Some contend that healthcare reform will redefine the current relationship between pharma and physicians . . . and not a moment too soon.
Lest there be ambiguity, though, the medical profession remains a noble vocation. This notwithstanding, until 2002, physicians freely participated in golf outings, received athletic tickets, and dined at five-star restaurants. But after the pharmaceutical industry smartly adopted voluntary guidelines that restrict gifting to doctors, we are left with drug samples and, of course, the “free lunch.” Certainly, pharma can claim it has made significant contributions to furthering medical education and research. Many could argue the tangible negative effects that would follow if the funding suddenly were absent.
But let’s not kid ourselves: There is a good reason the pharmaceutical industry spends more than $12 billion per year on marketing to doctors.4 In 2006, Rep. Henry Waxman (D-Calif.) said, “It is obvious that drug companies provide these free lunches so their sales reps can get the doctor’s ear and influence the prescribing practices.”2 Most doctors would never admit any such influence. It would be, however, disingenuous for any practicing physician to say there is none.
A randomized trial conducted by Adair et al concluded the “access to drug samples in clinic influences resident prescribing decisions. This could affect resident education and increase drug costs for patients.”5 An earlier study by Chew et al concluded “the availability of drug samples led physicians to dispense and subsequently prescribe drugs that differ from their preferred drug choice. Physicians most often report using drug samples to avoid cost to the patient.”6
Sure, local culture drives some prescribing practice, but one must be mindful of the reality that the pharmaceutical industry has significant influence. Plus, free drug samples help patients in the short term. Once the samples are gone, an expensive prescription for that new drug will follow. It’s another win for the industry and another loss for the patient and the healthcare system.
Many studies have shown that gifting exerts influence, even if doctors are unwilling to admit it. But patients and doctors alike would like to state with clarity of conscience that the medication prescribed is only based on clinical evidence, not influence. TH
Dr. Pyke is a hospitalist at Geisinger Wyoming Valley Medical Systems in Mountain Top, Pa.
References
- Dubovsky SL, Kaye DL, Pristach CA, DelRegno P, Pessar L, Stiles K. Can academic departments maintain industry relationships while promoting physician professionalism? Acad Med. 2010;85(1):68-73.
- Salganik MW, Hopkins JS, Rockoff JD. Medical salesmen prescribe lunches. Catering trade feeds on rep-doctor meals. The Baltimore Sun. July 29, 2006.
- Institute of Medicine Conflict of Interest in Medical Research, Education and Practice Full Recommendations. 4-28-09.
- Wolfe SM. Why do American drug companies spend more than $12 billion a year pushing drugs? Is it education or promotion? J Gen Intern Med. 2007;11(10):637-639.
- Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118(8):881-884.
- Chew LD, O’Young TS, Hazlet TK, Bradley KA, Maynard C, Lessler DS. A physician survey of the effect of drug sample availability on physicians’ behavior. J Gen Intern Med. 2000;15(7):478-483.
Recent discussions on conflicts of interest in medical publications underscore the significance of the important yet fragile relationship between the pharmaceutical industry and healthcare professionals. Among these is an examination of how academic departments can maintain a relationship with the industry.1 This study suggests that if appropriate boundaries are established between industry and academia, it is possible to collaborate. However, part of the policy in this investigation included “elimination of industry-supplied meals, gifts, and favors.”2
The Institute of Medicine’s “Conflict of Interest in Medical Research, Education, and Practice” included groundbreaking recommendations.3 Among them was a call for professionals to adopt a policy that prohibits “the acceptance of items of material value from pharmaceutical, medical device, and biotechnology companies, except in specified situations.”3
Our nation has been embroiled in a healthcare debate. Questions of right versus privilege, access versus affordability, and, of course, the perpetual political overlay have monopolized most of the discourse. Some contend that healthcare reform will redefine the current relationship between pharma and physicians . . . and not a moment too soon.
Lest there be ambiguity, though, the medical profession remains a noble vocation. This notwithstanding, until 2002, physicians freely participated in golf outings, received athletic tickets, and dined at five-star restaurants. But after the pharmaceutical industry smartly adopted voluntary guidelines that restrict gifting to doctors, we are left with drug samples and, of course, the “free lunch.” Certainly, pharma can claim it has made significant contributions to furthering medical education and research. Many could argue the tangible negative effects that would follow if the funding suddenly were absent.
But let’s not kid ourselves: There is a good reason the pharmaceutical industry spends more than $12 billion per year on marketing to doctors.4 In 2006, Rep. Henry Waxman (D-Calif.) said, “It is obvious that drug companies provide these free lunches so their sales reps can get the doctor’s ear and influence the prescribing practices.”2 Most doctors would never admit any such influence. It would be, however, disingenuous for any practicing physician to say there is none.
A randomized trial conducted by Adair et al concluded the “access to drug samples in clinic influences resident prescribing decisions. This could affect resident education and increase drug costs for patients.”5 An earlier study by Chew et al concluded “the availability of drug samples led physicians to dispense and subsequently prescribe drugs that differ from their preferred drug choice. Physicians most often report using drug samples to avoid cost to the patient.”6
Sure, local culture drives some prescribing practice, but one must be mindful of the reality that the pharmaceutical industry has significant influence. Plus, free drug samples help patients in the short term. Once the samples are gone, an expensive prescription for that new drug will follow. It’s another win for the industry and another loss for the patient and the healthcare system.
Many studies have shown that gifting exerts influence, even if doctors are unwilling to admit it. But patients and doctors alike would like to state with clarity of conscience that the medication prescribed is only based on clinical evidence, not influence. TH
Dr. Pyke is a hospitalist at Geisinger Wyoming Valley Medical Systems in Mountain Top, Pa.
References
- Dubovsky SL, Kaye DL, Pristach CA, DelRegno P, Pessar L, Stiles K. Can academic departments maintain industry relationships while promoting physician professionalism? Acad Med. 2010;85(1):68-73.
- Salganik MW, Hopkins JS, Rockoff JD. Medical salesmen prescribe lunches. Catering trade feeds on rep-doctor meals. The Baltimore Sun. July 29, 2006.
- Institute of Medicine Conflict of Interest in Medical Research, Education and Practice Full Recommendations. 4-28-09.
- Wolfe SM. Why do American drug companies spend more than $12 billion a year pushing drugs? Is it education or promotion? J Gen Intern Med. 2007;11(10):637-639.
- Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118(8):881-884.
- Chew LD, O’Young TS, Hazlet TK, Bradley KA, Maynard C, Lessler DS. A physician survey of the effect of drug sample availability on physicians’ behavior. J Gen Intern Med. 2000;15(7):478-483.
Recent discussions on conflicts of interest in medical publications underscore the significance of the important yet fragile relationship between the pharmaceutical industry and healthcare professionals. Among these is an examination of how academic departments can maintain a relationship with the industry.1 This study suggests that if appropriate boundaries are established between industry and academia, it is possible to collaborate. However, part of the policy in this investigation included “elimination of industry-supplied meals, gifts, and favors.”2
The Institute of Medicine’s “Conflict of Interest in Medical Research, Education, and Practice” included groundbreaking recommendations.3 Among them was a call for professionals to adopt a policy that prohibits “the acceptance of items of material value from pharmaceutical, medical device, and biotechnology companies, except in specified situations.”3
Our nation has been embroiled in a healthcare debate. Questions of right versus privilege, access versus affordability, and, of course, the perpetual political overlay have monopolized most of the discourse. Some contend that healthcare reform will redefine the current relationship between pharma and physicians . . . and not a moment too soon.
Lest there be ambiguity, though, the medical profession remains a noble vocation. This notwithstanding, until 2002, physicians freely participated in golf outings, received athletic tickets, and dined at five-star restaurants. But after the pharmaceutical industry smartly adopted voluntary guidelines that restrict gifting to doctors, we are left with drug samples and, of course, the “free lunch.” Certainly, pharma can claim it has made significant contributions to furthering medical education and research. Many could argue the tangible negative effects that would follow if the funding suddenly were absent.
But let’s not kid ourselves: There is a good reason the pharmaceutical industry spends more than $12 billion per year on marketing to doctors.4 In 2006, Rep. Henry Waxman (D-Calif.) said, “It is obvious that drug companies provide these free lunches so their sales reps can get the doctor’s ear and influence the prescribing practices.”2 Most doctors would never admit any such influence. It would be, however, disingenuous for any practicing physician to say there is none.
A randomized trial conducted by Adair et al concluded the “access to drug samples in clinic influences resident prescribing decisions. This could affect resident education and increase drug costs for patients.”5 An earlier study by Chew et al concluded “the availability of drug samples led physicians to dispense and subsequently prescribe drugs that differ from their preferred drug choice. Physicians most often report using drug samples to avoid cost to the patient.”6
Sure, local culture drives some prescribing practice, but one must be mindful of the reality that the pharmaceutical industry has significant influence. Plus, free drug samples help patients in the short term. Once the samples are gone, an expensive prescription for that new drug will follow. It’s another win for the industry and another loss for the patient and the healthcare system.
Many studies have shown that gifting exerts influence, even if doctors are unwilling to admit it. But patients and doctors alike would like to state with clarity of conscience that the medication prescribed is only based on clinical evidence, not influence. TH
Dr. Pyke is a hospitalist at Geisinger Wyoming Valley Medical Systems in Mountain Top, Pa.
References
- Dubovsky SL, Kaye DL, Pristach CA, DelRegno P, Pessar L, Stiles K. Can academic departments maintain industry relationships while promoting physician professionalism? Acad Med. 2010;85(1):68-73.
- Salganik MW, Hopkins JS, Rockoff JD. Medical salesmen prescribe lunches. Catering trade feeds on rep-doctor meals. The Baltimore Sun. July 29, 2006.
- Institute of Medicine Conflict of Interest in Medical Research, Education and Practice Full Recommendations. 4-28-09.
- Wolfe SM. Why do American drug companies spend more than $12 billion a year pushing drugs? Is it education or promotion? J Gen Intern Med. 2007;11(10):637-639.
- Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118(8):881-884.
- Chew LD, O’Young TS, Hazlet TK, Bradley KA, Maynard C, Lessler DS. A physician survey of the effect of drug sample availability on physicians’ behavior. J Gen Intern Med. 2000;15(7):478-483.
Should hospitalists accept gifts from pharmaceutical, medical device, and biotech companies?
The pharmaceutical industry is big business, and its goal is to make money. If the industry can convince physicians to prescribe its medicines, then it makes more money.
Although pharmaceutical representatives brief physicians on new medications in an effort to encourage the use of their brand-name products, they also provide substantive information on the drugs that serves an educational purpose.
In the past, pharmaceutical companies—along with the medical device and biotechnology industries—showered physicians with expensive gifts, raising ethical questions about physicians’ obligation to the drug companies. Fair enough. These excessive practices were identified and curtailed—to my knowledge—some years ago.
Watchdog groups, however, have continued to call into question every suggestion of “being in the pay” of big pharma. Everything from a plastic pen to a piece of pizza is suspect. There is considerable concern that practicing clinicians are influenced by the smallest gesture, while many large medical institutions continue to accept pharmaceutical-company-funded research grants. If big-pharma investment in research does not corrupt institutions, why is it assumed that carrying a pharmaceutical pen has such a pernicious effect on clinicians?
As a corollary to this question, does anyone really want to discontinue these important research studies just because they are funded by industry dollars?
Listening to drug representatives—even being seen in the vicinity—raises the eyebrows of purists. Do we really want physicians completely divorced from all pharmaceutical company education and communication? Do we feel there is zero benefit to hearing about new medications from the company’s viewpoint?
If physicians completely shut out the representatives, it would be expected that pharmaceutical companies would direct their efforts elsewhere—most likely, to consumers. Is that a better and healthier scenario?
Clearly, there is potential for abuse in pharmaceutical gifts to physicians. The practice should be controlled and monitored. The suspicions raised by purist groups that physicians’ prescribing habits are unalterably biased after a five-minute pharmaceutical representative detail and a chicken sandwich is hyperbole. The voice of reason is silenced in the midst of the inquisition.
In the academic setting, fear of being accused of “bought bias” has physicians clearing their pockets of tainted pens and checking their desks for corrupting paraphernalia. The positive aspects of pharma-sponsored programs and medical lectures are lost for fear of appearing to be complicit with drug companies.
The Aristotelian Golden Mean is superior to extreme positions, and I submit that the best road is the center. Listen to what the drug company representatives have to say, just like you listen to a car salesman: You can learn from both—as long as you research the data and form your own opinion. TH
Dr. Brezina is a hospitalist at Durham Regional Hospital in North Carolina.
The pharmaceutical industry is big business, and its goal is to make money. If the industry can convince physicians to prescribe its medicines, then it makes more money.
Although pharmaceutical representatives brief physicians on new medications in an effort to encourage the use of their brand-name products, they also provide substantive information on the drugs that serves an educational purpose.
In the past, pharmaceutical companies—along with the medical device and biotechnology industries—showered physicians with expensive gifts, raising ethical questions about physicians’ obligation to the drug companies. Fair enough. These excessive practices were identified and curtailed—to my knowledge—some years ago.
Watchdog groups, however, have continued to call into question every suggestion of “being in the pay” of big pharma. Everything from a plastic pen to a piece of pizza is suspect. There is considerable concern that practicing clinicians are influenced by the smallest gesture, while many large medical institutions continue to accept pharmaceutical-company-funded research grants. If big-pharma investment in research does not corrupt institutions, why is it assumed that carrying a pharmaceutical pen has such a pernicious effect on clinicians?
As a corollary to this question, does anyone really want to discontinue these important research studies just because they are funded by industry dollars?
Listening to drug representatives—even being seen in the vicinity—raises the eyebrows of purists. Do we really want physicians completely divorced from all pharmaceutical company education and communication? Do we feel there is zero benefit to hearing about new medications from the company’s viewpoint?
If physicians completely shut out the representatives, it would be expected that pharmaceutical companies would direct their efforts elsewhere—most likely, to consumers. Is that a better and healthier scenario?
Clearly, there is potential for abuse in pharmaceutical gifts to physicians. The practice should be controlled and monitored. The suspicions raised by purist groups that physicians’ prescribing habits are unalterably biased after a five-minute pharmaceutical representative detail and a chicken sandwich is hyperbole. The voice of reason is silenced in the midst of the inquisition.
In the academic setting, fear of being accused of “bought bias” has physicians clearing their pockets of tainted pens and checking their desks for corrupting paraphernalia. The positive aspects of pharma-sponsored programs and medical lectures are lost for fear of appearing to be complicit with drug companies.
The Aristotelian Golden Mean is superior to extreme positions, and I submit that the best road is the center. Listen to what the drug company representatives have to say, just like you listen to a car salesman: You can learn from both—as long as you research the data and form your own opinion. TH
Dr. Brezina is a hospitalist at Durham Regional Hospital in North Carolina.
The pharmaceutical industry is big business, and its goal is to make money. If the industry can convince physicians to prescribe its medicines, then it makes more money.
Although pharmaceutical representatives brief physicians on new medications in an effort to encourage the use of their brand-name products, they also provide substantive information on the drugs that serves an educational purpose.
In the past, pharmaceutical companies—along with the medical device and biotechnology industries—showered physicians with expensive gifts, raising ethical questions about physicians’ obligation to the drug companies. Fair enough. These excessive practices were identified and curtailed—to my knowledge—some years ago.
Watchdog groups, however, have continued to call into question every suggestion of “being in the pay” of big pharma. Everything from a plastic pen to a piece of pizza is suspect. There is considerable concern that practicing clinicians are influenced by the smallest gesture, while many large medical institutions continue to accept pharmaceutical-company-funded research grants. If big-pharma investment in research does not corrupt institutions, why is it assumed that carrying a pharmaceutical pen has such a pernicious effect on clinicians?
As a corollary to this question, does anyone really want to discontinue these important research studies just because they are funded by industry dollars?
Listening to drug representatives—even being seen in the vicinity—raises the eyebrows of purists. Do we really want physicians completely divorced from all pharmaceutical company education and communication? Do we feel there is zero benefit to hearing about new medications from the company’s viewpoint?
If physicians completely shut out the representatives, it would be expected that pharmaceutical companies would direct their efforts elsewhere—most likely, to consumers. Is that a better and healthier scenario?
Clearly, there is potential for abuse in pharmaceutical gifts to physicians. The practice should be controlled and monitored. The suspicions raised by purist groups that physicians’ prescribing habits are unalterably biased after a five-minute pharmaceutical representative detail and a chicken sandwich is hyperbole. The voice of reason is silenced in the midst of the inquisition.
In the academic setting, fear of being accused of “bought bias” has physicians clearing their pockets of tainted pens and checking their desks for corrupting paraphernalia. The positive aspects of pharma-sponsored programs and medical lectures are lost for fear of appearing to be complicit with drug companies.
The Aristotelian Golden Mean is superior to extreme positions, and I submit that the best road is the center. Listen to what the drug company representatives have to say, just like you listen to a car salesman: You can learn from both—as long as you research the data and form your own opinion. TH
Dr. Brezina is a hospitalist at Durham Regional Hospital in North Carolina.
Playground Politics
Baseball, kick the can, Russian roulette—pick your game. Chances are good that it has worked its way into a metaphor to illustrate the infuriating, perplexing, and altogether frustrating inability of Congress to step up to the plate and pass a long-term fix to the broken sustainable growth rate (SGR) formula used to determine Medicare reimbursement rates.
On June 24, legislators avoided catastrophe by temporarily rescinding a 21.3% rate cut that went into effect June 1. The after-the-fact patch meant that some Medicare claims had to be reprocessed to recoup the full value, creating an administrative mess. The accompanying 2.2% rate increase expires Nov. 30. The reimbursement cut could reach nearly 30% next year unless Congress intervenes again.
“Obviously, there’s a lot of frustration around the issue, especially on the membership side,” says Ron Greeno, MD, FACP, SFHM, a member of SHM’s Public Policy and Leadership committees, and chief medical officer for Brentwood, Tenn.-based Cogent Healthcare. For hospitalists in many small private practices, he says, a major percentage of income comes from Medicare. “It’s a tremendous headache,” he says of the uncertainty. “It’s very hard to plan for. You’re trying to budget and you don’t know what the policy is going to be literally from week to week.”
The Blame Game
Despite the widespread sentiment among doctors that a permanent reimbursement rate fix should have been included in the healthcare reform legislation, skittishness over the price tag led legislators to drop it from the package. Based on last fall’s estimates, the total cost of a reform bill that scrapped the SGR would have ballooned by roughly $250 billion over 10 years, which would have threatened the bill’s passage.
But Congress has since been unable to pass a permanent fix as standalone legislation amid mounting concern over the national debt, and the price of inaction continues to rise. On April 30, the Congressional Budget Office (CBO) estimated that the cost of jettisoning the SGR formula and freezing rates at current levels had grown to $276 billion over 10 years.
Any serious consideration of lasting alternatives has now been pushed back to the lame-duck session, after the midterm elections. The can has been kicked down the road so many times, Dr. Greeno and others say, that most Congressional members have boot marks all over them. “So now you have a bigger problem at a more crucial time, when money is tighter than ever in a poor economy,” Dr. Greeno says. “And I just think it’s been a failure of our politicians.”
Other healthcare industry leaders have been just as critical. “Delaying the problem is not a solution,” said AMA President Cecil B. Wilson, MD, in a prepared statement after Congress passed the latest six-month reprieve in June. “It doesn’t solve the Medicare mess Congress has created with a long series of short-term Medicare patches over the last decade—including four to avert the 2010 cut alone.”
AMA-sponsored print ads have reminded legislators that delaying a fix until 2013 will again increase its cost, to $396 billion over 10 years. And the association’s June press release asserted that “Congress is playing a dangerous game of Russian roulette with seniors’ healthcare.”
Perhaps a game of “chicken” would be more apt.
Republicans have dared Democrats to spend the billions for a more lasting solution—in the absence of any cuts elsewhere in the healthcare delivery system—and be labeled as fiscally irresponsible. In turn, Democrats have dared Republicans to let the rate cut take effect and be labeled heartless as Medicare beneficiaries lose access to their healthcare providers.
Both parties blinked, resorting to almost unanimous short-term fixes that have allowed legislators to save face while putting off politically risky votes until after the November elections.
Lynne M. Allen, MN, ARNP, who works as a part-time hospitalist in hematology-oncology at 188-bed Kadlec Regional Medical Center in Richland, Wash., says she and other colleagues were initially hopeful that the Obama administration would make Congress work together to find a lasting solution. “There’s a sense of frustration because instead of that happening from our legislators, they’re playing a lot of games with the funding,” says Allen, a member of Team Hospitalist. “They’re not willing to step up to the plate, as they say, and make a decision that will allow us to go forward smoothly.”
The result, Allen says, has been a “roller-coaster ride” of uncertainty over reimbursements. Because Washington’s Tri-Cities region has a relatively high percentage of patients with private insurance, her hospital is somewhat cushioned from a precipitous drop in Medicare fees. But if CMS is ever forced to cut back on its rates, she fully expects private insurers to follow the same downward track.
Practical Concerns
Barbara Hartley, MD, a part-time hospitalist at 22-bed Benson Hospital in Benson, Ariz., says the town’s healthcare facility is somewhat protected from potential Medicare rate cuts through its official status as a Critical Access Hospital. Instead of being reimbursed through diagnosis-related group (DRG) codes, the rural hospital is repaid by Medicare for its total cost per day per patient.
The arrangement is a stable one at the moment, but not enough to dispel Dr. Hartley’s uneasy question: If the economy worsens, will Medicare be able to retain its commitment to rural hospitals? If not, the pain might be felt acutely in communities like Benson, where Dr. Hartley estimates that as much as 75% of the hospital’s in-patient business is through either Medicare or a Medicare Advantage plan.
Kirk Mathews, CEO of St. Louis-based Inpatient Management Inc. and a member of SHM’s Public Policy and Practice Management committees, says Medicare rate cuts also could significantly reduce the leverage of hospitalists during contract negotiations.
“Even if we’re employed by the hospital, but our professional fees that the hospital can recoup for our services are dramatically affected, it will affect how those future contracts go,” Mathews says. “We might be insulated temporarily by the strength of our current contract. But if the formula—however that works out—dramatically impacts the hospitalist reimbursement on the professional fee side, the hospital will feel that, and then hospitalists will eventually feel that as well.” In other words, it could strengthen the bargaining hand of the hospital at the expense of the hospitalist. “Therein lies the long-term threat,” he points out.
Independent Solution?
Some of the authority over physician payments might eventually be depoliticized via language in the reform legislation that empowers a new entity, the Independent Payment Advisory Board, to create policy on such critical monetary issues as reimbursement rates. Congress could still override the board’s policy decisions, but only if the Congressional alternative saves just as much money.
In the meantime, the money for a fix still has to come from somewhere, and no consensus has emerged. Advocates likewise refuse to coalesce around any single alternative. Some experts favor a new formula based on the Medicare economic index, which measures inflation in healthcare delivery costs. But the CBO estimates that per-beneficiary spending under such a formula would be 30% more by 2016 than under the current formula. Other proposals call for temporarily increasing rates, then reverting to annual GDP growth, plus a bit more to cover physician costs.
No matter how the crisis is resolved, experts say, doctors almost certainly will have to make do with less. “When healthcare reform is finally fully implemented, there are going to be less dollars to pay for more services. It’s inevitable,” Mathews says. “And whether it takes the form of SGR or some other form, I’m afraid physicians are going to have to get used to having less money in the pool of money that’s allocated to pay providers.”
It could be a whole new ballgame. TH
Bryn Nelson, PhD, is a freelance medical writer based in Seattle.
Baseball, kick the can, Russian roulette—pick your game. Chances are good that it has worked its way into a metaphor to illustrate the infuriating, perplexing, and altogether frustrating inability of Congress to step up to the plate and pass a long-term fix to the broken sustainable growth rate (SGR) formula used to determine Medicare reimbursement rates.
On June 24, legislators avoided catastrophe by temporarily rescinding a 21.3% rate cut that went into effect June 1. The after-the-fact patch meant that some Medicare claims had to be reprocessed to recoup the full value, creating an administrative mess. The accompanying 2.2% rate increase expires Nov. 30. The reimbursement cut could reach nearly 30% next year unless Congress intervenes again.
“Obviously, there’s a lot of frustration around the issue, especially on the membership side,” says Ron Greeno, MD, FACP, SFHM, a member of SHM’s Public Policy and Leadership committees, and chief medical officer for Brentwood, Tenn.-based Cogent Healthcare. For hospitalists in many small private practices, he says, a major percentage of income comes from Medicare. “It’s a tremendous headache,” he says of the uncertainty. “It’s very hard to plan for. You’re trying to budget and you don’t know what the policy is going to be literally from week to week.”
The Blame Game
Despite the widespread sentiment among doctors that a permanent reimbursement rate fix should have been included in the healthcare reform legislation, skittishness over the price tag led legislators to drop it from the package. Based on last fall’s estimates, the total cost of a reform bill that scrapped the SGR would have ballooned by roughly $250 billion over 10 years, which would have threatened the bill’s passage.
But Congress has since been unable to pass a permanent fix as standalone legislation amid mounting concern over the national debt, and the price of inaction continues to rise. On April 30, the Congressional Budget Office (CBO) estimated that the cost of jettisoning the SGR formula and freezing rates at current levels had grown to $276 billion over 10 years.
Any serious consideration of lasting alternatives has now been pushed back to the lame-duck session, after the midterm elections. The can has been kicked down the road so many times, Dr. Greeno and others say, that most Congressional members have boot marks all over them. “So now you have a bigger problem at a more crucial time, when money is tighter than ever in a poor economy,” Dr. Greeno says. “And I just think it’s been a failure of our politicians.”
Other healthcare industry leaders have been just as critical. “Delaying the problem is not a solution,” said AMA President Cecil B. Wilson, MD, in a prepared statement after Congress passed the latest six-month reprieve in June. “It doesn’t solve the Medicare mess Congress has created with a long series of short-term Medicare patches over the last decade—including four to avert the 2010 cut alone.”
AMA-sponsored print ads have reminded legislators that delaying a fix until 2013 will again increase its cost, to $396 billion over 10 years. And the association’s June press release asserted that “Congress is playing a dangerous game of Russian roulette with seniors’ healthcare.”
Perhaps a game of “chicken” would be more apt.
Republicans have dared Democrats to spend the billions for a more lasting solution—in the absence of any cuts elsewhere in the healthcare delivery system—and be labeled as fiscally irresponsible. In turn, Democrats have dared Republicans to let the rate cut take effect and be labeled heartless as Medicare beneficiaries lose access to their healthcare providers.
Both parties blinked, resorting to almost unanimous short-term fixes that have allowed legislators to save face while putting off politically risky votes until after the November elections.
Lynne M. Allen, MN, ARNP, who works as a part-time hospitalist in hematology-oncology at 188-bed Kadlec Regional Medical Center in Richland, Wash., says she and other colleagues were initially hopeful that the Obama administration would make Congress work together to find a lasting solution. “There’s a sense of frustration because instead of that happening from our legislators, they’re playing a lot of games with the funding,” says Allen, a member of Team Hospitalist. “They’re not willing to step up to the plate, as they say, and make a decision that will allow us to go forward smoothly.”
The result, Allen says, has been a “roller-coaster ride” of uncertainty over reimbursements. Because Washington’s Tri-Cities region has a relatively high percentage of patients with private insurance, her hospital is somewhat cushioned from a precipitous drop in Medicare fees. But if CMS is ever forced to cut back on its rates, she fully expects private insurers to follow the same downward track.
Practical Concerns
Barbara Hartley, MD, a part-time hospitalist at 22-bed Benson Hospital in Benson, Ariz., says the town’s healthcare facility is somewhat protected from potential Medicare rate cuts through its official status as a Critical Access Hospital. Instead of being reimbursed through diagnosis-related group (DRG) codes, the rural hospital is repaid by Medicare for its total cost per day per patient.
The arrangement is a stable one at the moment, but not enough to dispel Dr. Hartley’s uneasy question: If the economy worsens, will Medicare be able to retain its commitment to rural hospitals? If not, the pain might be felt acutely in communities like Benson, where Dr. Hartley estimates that as much as 75% of the hospital’s in-patient business is through either Medicare or a Medicare Advantage plan.
Kirk Mathews, CEO of St. Louis-based Inpatient Management Inc. and a member of SHM’s Public Policy and Practice Management committees, says Medicare rate cuts also could significantly reduce the leverage of hospitalists during contract negotiations.
“Even if we’re employed by the hospital, but our professional fees that the hospital can recoup for our services are dramatically affected, it will affect how those future contracts go,” Mathews says. “We might be insulated temporarily by the strength of our current contract. But if the formula—however that works out—dramatically impacts the hospitalist reimbursement on the professional fee side, the hospital will feel that, and then hospitalists will eventually feel that as well.” In other words, it could strengthen the bargaining hand of the hospital at the expense of the hospitalist. “Therein lies the long-term threat,” he points out.
Independent Solution?
Some of the authority over physician payments might eventually be depoliticized via language in the reform legislation that empowers a new entity, the Independent Payment Advisory Board, to create policy on such critical monetary issues as reimbursement rates. Congress could still override the board’s policy decisions, but only if the Congressional alternative saves just as much money.
In the meantime, the money for a fix still has to come from somewhere, and no consensus has emerged. Advocates likewise refuse to coalesce around any single alternative. Some experts favor a new formula based on the Medicare economic index, which measures inflation in healthcare delivery costs. But the CBO estimates that per-beneficiary spending under such a formula would be 30% more by 2016 than under the current formula. Other proposals call for temporarily increasing rates, then reverting to annual GDP growth, plus a bit more to cover physician costs.
No matter how the crisis is resolved, experts say, doctors almost certainly will have to make do with less. “When healthcare reform is finally fully implemented, there are going to be less dollars to pay for more services. It’s inevitable,” Mathews says. “And whether it takes the form of SGR or some other form, I’m afraid physicians are going to have to get used to having less money in the pool of money that’s allocated to pay providers.”
It could be a whole new ballgame. TH
Bryn Nelson, PhD, is a freelance medical writer based in Seattle.
Baseball, kick the can, Russian roulette—pick your game. Chances are good that it has worked its way into a metaphor to illustrate the infuriating, perplexing, and altogether frustrating inability of Congress to step up to the plate and pass a long-term fix to the broken sustainable growth rate (SGR) formula used to determine Medicare reimbursement rates.
On June 24, legislators avoided catastrophe by temporarily rescinding a 21.3% rate cut that went into effect June 1. The after-the-fact patch meant that some Medicare claims had to be reprocessed to recoup the full value, creating an administrative mess. The accompanying 2.2% rate increase expires Nov. 30. The reimbursement cut could reach nearly 30% next year unless Congress intervenes again.
“Obviously, there’s a lot of frustration around the issue, especially on the membership side,” says Ron Greeno, MD, FACP, SFHM, a member of SHM’s Public Policy and Leadership committees, and chief medical officer for Brentwood, Tenn.-based Cogent Healthcare. For hospitalists in many small private practices, he says, a major percentage of income comes from Medicare. “It’s a tremendous headache,” he says of the uncertainty. “It’s very hard to plan for. You’re trying to budget and you don’t know what the policy is going to be literally from week to week.”
The Blame Game
Despite the widespread sentiment among doctors that a permanent reimbursement rate fix should have been included in the healthcare reform legislation, skittishness over the price tag led legislators to drop it from the package. Based on last fall’s estimates, the total cost of a reform bill that scrapped the SGR would have ballooned by roughly $250 billion over 10 years, which would have threatened the bill’s passage.
But Congress has since been unable to pass a permanent fix as standalone legislation amid mounting concern over the national debt, and the price of inaction continues to rise. On April 30, the Congressional Budget Office (CBO) estimated that the cost of jettisoning the SGR formula and freezing rates at current levels had grown to $276 billion over 10 years.
Any serious consideration of lasting alternatives has now been pushed back to the lame-duck session, after the midterm elections. The can has been kicked down the road so many times, Dr. Greeno and others say, that most Congressional members have boot marks all over them. “So now you have a bigger problem at a more crucial time, when money is tighter than ever in a poor economy,” Dr. Greeno says. “And I just think it’s been a failure of our politicians.”
Other healthcare industry leaders have been just as critical. “Delaying the problem is not a solution,” said AMA President Cecil B. Wilson, MD, in a prepared statement after Congress passed the latest six-month reprieve in June. “It doesn’t solve the Medicare mess Congress has created with a long series of short-term Medicare patches over the last decade—including four to avert the 2010 cut alone.”
AMA-sponsored print ads have reminded legislators that delaying a fix until 2013 will again increase its cost, to $396 billion over 10 years. And the association’s June press release asserted that “Congress is playing a dangerous game of Russian roulette with seniors’ healthcare.”
Perhaps a game of “chicken” would be more apt.
Republicans have dared Democrats to spend the billions for a more lasting solution—in the absence of any cuts elsewhere in the healthcare delivery system—and be labeled as fiscally irresponsible. In turn, Democrats have dared Republicans to let the rate cut take effect and be labeled heartless as Medicare beneficiaries lose access to their healthcare providers.
Both parties blinked, resorting to almost unanimous short-term fixes that have allowed legislators to save face while putting off politically risky votes until after the November elections.
Lynne M. Allen, MN, ARNP, who works as a part-time hospitalist in hematology-oncology at 188-bed Kadlec Regional Medical Center in Richland, Wash., says she and other colleagues were initially hopeful that the Obama administration would make Congress work together to find a lasting solution. “There’s a sense of frustration because instead of that happening from our legislators, they’re playing a lot of games with the funding,” says Allen, a member of Team Hospitalist. “They’re not willing to step up to the plate, as they say, and make a decision that will allow us to go forward smoothly.”
The result, Allen says, has been a “roller-coaster ride” of uncertainty over reimbursements. Because Washington’s Tri-Cities region has a relatively high percentage of patients with private insurance, her hospital is somewhat cushioned from a precipitous drop in Medicare fees. But if CMS is ever forced to cut back on its rates, she fully expects private insurers to follow the same downward track.
Practical Concerns
Barbara Hartley, MD, a part-time hospitalist at 22-bed Benson Hospital in Benson, Ariz., says the town’s healthcare facility is somewhat protected from potential Medicare rate cuts through its official status as a Critical Access Hospital. Instead of being reimbursed through diagnosis-related group (DRG) codes, the rural hospital is repaid by Medicare for its total cost per day per patient.
The arrangement is a stable one at the moment, but not enough to dispel Dr. Hartley’s uneasy question: If the economy worsens, will Medicare be able to retain its commitment to rural hospitals? If not, the pain might be felt acutely in communities like Benson, where Dr. Hartley estimates that as much as 75% of the hospital’s in-patient business is through either Medicare or a Medicare Advantage plan.
Kirk Mathews, CEO of St. Louis-based Inpatient Management Inc. and a member of SHM’s Public Policy and Practice Management committees, says Medicare rate cuts also could significantly reduce the leverage of hospitalists during contract negotiations.
“Even if we’re employed by the hospital, but our professional fees that the hospital can recoup for our services are dramatically affected, it will affect how those future contracts go,” Mathews says. “We might be insulated temporarily by the strength of our current contract. But if the formula—however that works out—dramatically impacts the hospitalist reimbursement on the professional fee side, the hospital will feel that, and then hospitalists will eventually feel that as well.” In other words, it could strengthen the bargaining hand of the hospital at the expense of the hospitalist. “Therein lies the long-term threat,” he points out.
Independent Solution?
Some of the authority over physician payments might eventually be depoliticized via language in the reform legislation that empowers a new entity, the Independent Payment Advisory Board, to create policy on such critical monetary issues as reimbursement rates. Congress could still override the board’s policy decisions, but only if the Congressional alternative saves just as much money.
In the meantime, the money for a fix still has to come from somewhere, and no consensus has emerged. Advocates likewise refuse to coalesce around any single alternative. Some experts favor a new formula based on the Medicare economic index, which measures inflation in healthcare delivery costs. But the CBO estimates that per-beneficiary spending under such a formula would be 30% more by 2016 than under the current formula. Other proposals call for temporarily increasing rates, then reverting to annual GDP growth, plus a bit more to cover physician costs.
No matter how the crisis is resolved, experts say, doctors almost certainly will have to make do with less. “When healthcare reform is finally fully implemented, there are going to be less dollars to pay for more services. It’s inevitable,” Mathews says. “And whether it takes the form of SGR or some other form, I’m afraid physicians are going to have to get used to having less money in the pool of money that’s allocated to pay providers.”
It could be a whole new ballgame. TH
Bryn Nelson, PhD, is a freelance medical writer based in Seattle.
Rule Proposes Electronic Prescription of Controlled Substances, Doesn’t Scrap Pen-and-Paper Method
Is it true that the Drug Enforcement Administration (DEA) is going to allow doctors to prescribe controlled drugs electronically?
Will I still be able to prescribe on my prescription pads, or is this big government forcing me to use a computer for prescriptions?
J. Hockenstein, DO
Des Moines, Iowa
Dr. Hospitalist responds: On March 31, the DEA published in the Federal Register an interim final rule regarding the “electronic prescription for controlled substances.” (View the entire rule at www.gpoaccess.gov/fr.) The DEA is seeking comment on the proposed rule for the next 60 days. Some of us might remember that the DEA proposed a similar rule for electronic prescribing in June 2008, but that rule did not meet the security requirements already in place at federal healthcare facilities.
Under the current system, providers can create prescriptions electronically, but the prescription has to be printed on paper. The new rule proposes a system of true electronic prescribing; data can be transmitted electronically from the hospital or doctor’s office to the pharmacy without the use of a printer or fax.
This proposed rule does not eliminate the traditional method of paper and pen for prescriptions but allows providers the voluntary option of prescribing controlled substances electronically. This proposed rule also allows pharmacies to receive, dispense, and archive these electronic prescriptions.
For those providers who choose to prescribe electronically, there will be specific requirements to prevent diversion and maintain privacy. Providers must utilize software that meets the rule’s specific requirements. For example, the software system will require a two-step process to authenticate the prescribing provider. These measures might include a password, a token, or the use of biometric identifier (e.g., fingerprint or handprint). For some of us, this might sound space-aged, but such biometric systems are commonplace in other industries. For example, I provided my fingerprint as part of the test center security system when I checked in for my American Board of Internal Medicine (ABIM) recertification examination.
There are several other issues with the proposed rule that one should consider. The new proposal does not affect the existing rule regarding emergency prescriptions. The current law allows physicians to prescribe a Schedule II controlled substance by telephone and the pharmacist to dispense this substance, provided that the amount being dispensed is limited to what is reasonably required during the emergency time period and that the provider provides a hard copy of the prescription to the pharmacist within seven days of the telephone prescription. Under the proposed rule, providers will still be able to prescribe Schedule II substances by telephone under emergency situations but will have the option of providing an electronic copy of the prescription, rather than a paper one, within seven days.
There are other components of the proposed rule that could change your practice. The rule clearly states that an electronic prescription cannot be changed after transmission and that any change to the content of the prescription will render it invalid. This might be important in a handful of situations. For example, if the provider electronically prescribes a brand-name drug, the pharmacist would not be able to make a generic substitution.
Another component of the proposed rule is that it precludes the printing of an electronic prescription, which already has been transmitted and precludes the electronic transmission of a prescription that already has been printed. This situation might arise if the electronic prescription did not transmit due to a computer problem. The provider would not be able to print or fax a copy of the electronic prescription.
The proposed rule has the potential to reduce medical errors, reduce prescription forgeries, and help providers and hospitals integrate their medical records. True electronic prescribing is long overdue. In the future, I envision hospitalists prescribing from their handheld devices.
The key to success, like any computerized system, will be the ability to keep the system running and continuously maintaining and upgrading security measures. For more information regarding electronic prescriptions for controlled substances, visit www.DEAdiversion.usdoj.gov. TH
Is it true that the Drug Enforcement Administration (DEA) is going to allow doctors to prescribe controlled drugs electronically?
Will I still be able to prescribe on my prescription pads, or is this big government forcing me to use a computer for prescriptions?
J. Hockenstein, DO
Des Moines, Iowa
Dr. Hospitalist responds: On March 31, the DEA published in the Federal Register an interim final rule regarding the “electronic prescription for controlled substances.” (View the entire rule at www.gpoaccess.gov/fr.) The DEA is seeking comment on the proposed rule for the next 60 days. Some of us might remember that the DEA proposed a similar rule for electronic prescribing in June 2008, but that rule did not meet the security requirements already in place at federal healthcare facilities.
Under the current system, providers can create prescriptions electronically, but the prescription has to be printed on paper. The new rule proposes a system of true electronic prescribing; data can be transmitted electronically from the hospital or doctor’s office to the pharmacy without the use of a printer or fax.
This proposed rule does not eliminate the traditional method of paper and pen for prescriptions but allows providers the voluntary option of prescribing controlled substances electronically. This proposed rule also allows pharmacies to receive, dispense, and archive these electronic prescriptions.
For those providers who choose to prescribe electronically, there will be specific requirements to prevent diversion and maintain privacy. Providers must utilize software that meets the rule’s specific requirements. For example, the software system will require a two-step process to authenticate the prescribing provider. These measures might include a password, a token, or the use of biometric identifier (e.g., fingerprint or handprint). For some of us, this might sound space-aged, but such biometric systems are commonplace in other industries. For example, I provided my fingerprint as part of the test center security system when I checked in for my American Board of Internal Medicine (ABIM) recertification examination.
There are several other issues with the proposed rule that one should consider. The new proposal does not affect the existing rule regarding emergency prescriptions. The current law allows physicians to prescribe a Schedule II controlled substance by telephone and the pharmacist to dispense this substance, provided that the amount being dispensed is limited to what is reasonably required during the emergency time period and that the provider provides a hard copy of the prescription to the pharmacist within seven days of the telephone prescription. Under the proposed rule, providers will still be able to prescribe Schedule II substances by telephone under emergency situations but will have the option of providing an electronic copy of the prescription, rather than a paper one, within seven days.
There are other components of the proposed rule that could change your practice. The rule clearly states that an electronic prescription cannot be changed after transmission and that any change to the content of the prescription will render it invalid. This might be important in a handful of situations. For example, if the provider electronically prescribes a brand-name drug, the pharmacist would not be able to make a generic substitution.
Another component of the proposed rule is that it precludes the printing of an electronic prescription, which already has been transmitted and precludes the electronic transmission of a prescription that already has been printed. This situation might arise if the electronic prescription did not transmit due to a computer problem. The provider would not be able to print or fax a copy of the electronic prescription.
The proposed rule has the potential to reduce medical errors, reduce prescription forgeries, and help providers and hospitals integrate their medical records. True electronic prescribing is long overdue. In the future, I envision hospitalists prescribing from their handheld devices.
The key to success, like any computerized system, will be the ability to keep the system running and continuously maintaining and upgrading security measures. For more information regarding electronic prescriptions for controlled substances, visit www.DEAdiversion.usdoj.gov. TH
Is it true that the Drug Enforcement Administration (DEA) is going to allow doctors to prescribe controlled drugs electronically?
Will I still be able to prescribe on my prescription pads, or is this big government forcing me to use a computer for prescriptions?
J. Hockenstein, DO
Des Moines, Iowa
Dr. Hospitalist responds: On March 31, the DEA published in the Federal Register an interim final rule regarding the “electronic prescription for controlled substances.” (View the entire rule at www.gpoaccess.gov/fr.) The DEA is seeking comment on the proposed rule for the next 60 days. Some of us might remember that the DEA proposed a similar rule for electronic prescribing in June 2008, but that rule did not meet the security requirements already in place at federal healthcare facilities.
Under the current system, providers can create prescriptions electronically, but the prescription has to be printed on paper. The new rule proposes a system of true electronic prescribing; data can be transmitted electronically from the hospital or doctor’s office to the pharmacy without the use of a printer or fax.
This proposed rule does not eliminate the traditional method of paper and pen for prescriptions but allows providers the voluntary option of prescribing controlled substances electronically. This proposed rule also allows pharmacies to receive, dispense, and archive these electronic prescriptions.
For those providers who choose to prescribe electronically, there will be specific requirements to prevent diversion and maintain privacy. Providers must utilize software that meets the rule’s specific requirements. For example, the software system will require a two-step process to authenticate the prescribing provider. These measures might include a password, a token, or the use of biometric identifier (e.g., fingerprint or handprint). For some of us, this might sound space-aged, but such biometric systems are commonplace in other industries. For example, I provided my fingerprint as part of the test center security system when I checked in for my American Board of Internal Medicine (ABIM) recertification examination.
There are several other issues with the proposed rule that one should consider. The new proposal does not affect the existing rule regarding emergency prescriptions. The current law allows physicians to prescribe a Schedule II controlled substance by telephone and the pharmacist to dispense this substance, provided that the amount being dispensed is limited to what is reasonably required during the emergency time period and that the provider provides a hard copy of the prescription to the pharmacist within seven days of the telephone prescription. Under the proposed rule, providers will still be able to prescribe Schedule II substances by telephone under emergency situations but will have the option of providing an electronic copy of the prescription, rather than a paper one, within seven days.
There are other components of the proposed rule that could change your practice. The rule clearly states that an electronic prescription cannot be changed after transmission and that any change to the content of the prescription will render it invalid. This might be important in a handful of situations. For example, if the provider electronically prescribes a brand-name drug, the pharmacist would not be able to make a generic substitution.
Another component of the proposed rule is that it precludes the printing of an electronic prescription, which already has been transmitted and precludes the electronic transmission of a prescription that already has been printed. This situation might arise if the electronic prescription did not transmit due to a computer problem. The provider would not be able to print or fax a copy of the electronic prescription.
The proposed rule has the potential to reduce medical errors, reduce prescription forgeries, and help providers and hospitals integrate their medical records. True electronic prescribing is long overdue. In the future, I envision hospitalists prescribing from their handheld devices.
The key to success, like any computerized system, will be the ability to keep the system running and continuously maintaining and upgrading security measures. For more information regarding electronic prescriptions for controlled substances, visit www.DEAdiversion.usdoj.gov. TH
Focused Practice in Hospital Medicine Worth the Additional Cost
Focused Practice in Hospital Medicine Worth the Additional Cost
Why are we being required to fork over an extra $380 for the Focused Practice in Hospital Medicine MOC? This feels like the icing on the cake of already a major ripoff.
Dr. Ragan
Grass Valley, Calif.
Dr. Hospitalist responds: Thank you for your frank reaction to the much-anticipated American Board of Internal Medicine (ABIM) Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) program. As you noted, an additional fee is required to participate in this recertification program.
To my knowledge, any and all fees associated with recertification are paid to ABIM. No other organization benefits from the added cost, so your question might be more appropriately addressed to ABIM (see “Focused Practice in Hospital Medicine,” May 2010, p. 1). But because you asked the question, I am happy to respond with my thoughts.
Participation in the FPHM MOC program is not mandatory. I am not aware of any organization that is requiring hospitalists to participate. I don’t expect that your lack of participation will affect your ability to obtain hospital privileges. Like any new MOC program, I would expect some up-front administrative costs associated with developing and administering the practice-improvement modules and the secure examination.
It’s up to you and others to decide whether this added recognition is worth the cost. I can tell you that I have made the decision to participate. I fully expect to be part of the inaugural class of ABIM diplomates with this added recognition by the end of the year.
What went into my own decision to participate? I can tell you that I am a practicing hospitalist who makes a salary typical of most hospitalists. I am frugal with my money and certainly do not view the added cost as an insignificant amount of money. Like most hospitalists, I am not only busy with my professional life, but I have plenty of family commitments as well.
I expect the exam will be rigorous, and the requirements of the practice-improvement modules will be demanding. I would not want it any other way. In the fast-changing healthcare environment, I believe that hospitalists will be challenged to think about what it means to care for a hospitalized patient. To succeed in the future, hospitalists will be expected to not only participate, but also lead QI efforts at their institutions. The FPHM MOC will distinguish me as a hospitalist with added qualifications in the field of QI.
So how about it, Dr. Ragan? Will you join me?
What Certification Requirements Should a Hospitalist Program Have for Its Physicians?
I hope you can help me with some questions I have concerning starting a hospitalist program at my medical center. Are there certain requirements (e.g., board certification in internal medicine, ACLS, etc.) that need to be met, or is that up to the facility? The physician interested in the position is board-certified in infectious disease. Any direction you can give me on this would be greatly appreciated.
Marisa Sellers,
Medical Staff Coordinator,
Hartselle Medical Center,
Hartselle, Ala.
Dr. Hospitalist responds: Congratulations on your medical center’s decision to establish a hospitalist program. Over the past decade, HM has been the fastest-growing field in all of American medicine. The majority of the country’s acute-care hospitals have hospitalists on staff.
Approximately 85% of the country’s hospitalists received training in internal medicine. Most of the other hospitalists received training in pediatrics or family medicine. While most hospitalists are general internists, some also have additional subspecialty training, which seems to be the case of the physician at your medical center. As you know, different medical facilities have different requirements of their medical staff. At the acute-care hospital where I work clinically, maintenance of board certification is required of all medical staff. I know that is not the case for all hospitals, yet I’m not aware of any hospitals with hospitalist-specific medical staff requirements.
Most of the hospitalists who are internists will be either board-eligible or board-certified with the American Board of Internal Medicine (ABIM). You should be aware that ABIM has developed a new program, the Recognition of Focused Practice (RFP) in Hospital Medicine. As part of this maintenance of certification (MOC) program, ABIM diplomates will have the opportunity to take the first ABIM Hospital Medicine examination in October. For more information about this exam, ABIM’s rationale for recognizing a focused practice in HM, and any other questions about this program, please visit the ABIM Web site at www.abim.org/news/news/focused-
practice-hospital-medicine-qa.aspx.
I have heard from hospitalists trained as family physicians who are interested in RFP as hospitalists. It is my understanding that the American Board of Family Medicine is studying the ABIM program and working to develop a similar program for hospitalists with family medicine board certifications.
Regarding your question about hospitalists and the American Heart Association’s advanced cardiac life support (ACLS) training and certification: While I think it is a great idea for hospitalists to receive this training and maintain this certification, I am not aware of any mandate for hospitalists to be uniformly ACLS-certified. I think this is an issue the medical staff at your medical center will have to decide; basically, what is in the best interests of your patients?
Focused Practice in Hospital Medicine Worth the Additional Cost
Why are we being required to fork over an extra $380 for the Focused Practice in Hospital Medicine MOC? This feels like the icing on the cake of already a major ripoff.
Dr. Ragan
Grass Valley, Calif.
Dr. Hospitalist responds: Thank you for your frank reaction to the much-anticipated American Board of Internal Medicine (ABIM) Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) program. As you noted, an additional fee is required to participate in this recertification program.
To my knowledge, any and all fees associated with recertification are paid to ABIM. No other organization benefits from the added cost, so your question might be more appropriately addressed to ABIM (see “Focused Practice in Hospital Medicine,” May 2010, p. 1). But because you asked the question, I am happy to respond with my thoughts.
Participation in the FPHM MOC program is not mandatory. I am not aware of any organization that is requiring hospitalists to participate. I don’t expect that your lack of participation will affect your ability to obtain hospital privileges. Like any new MOC program, I would expect some up-front administrative costs associated with developing and administering the practice-improvement modules and the secure examination.
It’s up to you and others to decide whether this added recognition is worth the cost. I can tell you that I have made the decision to participate. I fully expect to be part of the inaugural class of ABIM diplomates with this added recognition by the end of the year.
What went into my own decision to participate? I can tell you that I am a practicing hospitalist who makes a salary typical of most hospitalists. I am frugal with my money and certainly do not view the added cost as an insignificant amount of money. Like most hospitalists, I am not only busy with my professional life, but I have plenty of family commitments as well.
I expect the exam will be rigorous, and the requirements of the practice-improvement modules will be demanding. I would not want it any other way. In the fast-changing healthcare environment, I believe that hospitalists will be challenged to think about what it means to care for a hospitalized patient. To succeed in the future, hospitalists will be expected to not only participate, but also lead QI efforts at their institutions. The FPHM MOC will distinguish me as a hospitalist with added qualifications in the field of QI.
So how about it, Dr. Ragan? Will you join me?
What Certification Requirements Should a Hospitalist Program Have for Its Physicians?
I hope you can help me with some questions I have concerning starting a hospitalist program at my medical center. Are there certain requirements (e.g., board certification in internal medicine, ACLS, etc.) that need to be met, or is that up to the facility? The physician interested in the position is board-certified in infectious disease. Any direction you can give me on this would be greatly appreciated.
Marisa Sellers,
Medical Staff Coordinator,
Hartselle Medical Center,
Hartselle, Ala.
Dr. Hospitalist responds: Congratulations on your medical center’s decision to establish a hospitalist program. Over the past decade, HM has been the fastest-growing field in all of American medicine. The majority of the country’s acute-care hospitals have hospitalists on staff.
Approximately 85% of the country’s hospitalists received training in internal medicine. Most of the other hospitalists received training in pediatrics or family medicine. While most hospitalists are general internists, some also have additional subspecialty training, which seems to be the case of the physician at your medical center. As you know, different medical facilities have different requirements of their medical staff. At the acute-care hospital where I work clinically, maintenance of board certification is required of all medical staff. I know that is not the case for all hospitals, yet I’m not aware of any hospitals with hospitalist-specific medical staff requirements.
Most of the hospitalists who are internists will be either board-eligible or board-certified with the American Board of Internal Medicine (ABIM). You should be aware that ABIM has developed a new program, the Recognition of Focused Practice (RFP) in Hospital Medicine. As part of this maintenance of certification (MOC) program, ABIM diplomates will have the opportunity to take the first ABIM Hospital Medicine examination in October. For more information about this exam, ABIM’s rationale for recognizing a focused practice in HM, and any other questions about this program, please visit the ABIM Web site at www.abim.org/news/news/focused-
practice-hospital-medicine-qa.aspx.
I have heard from hospitalists trained as family physicians who are interested in RFP as hospitalists. It is my understanding that the American Board of Family Medicine is studying the ABIM program and working to develop a similar program for hospitalists with family medicine board certifications.
Regarding your question about hospitalists and the American Heart Association’s advanced cardiac life support (ACLS) training and certification: While I think it is a great idea for hospitalists to receive this training and maintain this certification, I am not aware of any mandate for hospitalists to be uniformly ACLS-certified. I think this is an issue the medical staff at your medical center will have to decide; basically, what is in the best interests of your patients?
Focused Practice in Hospital Medicine Worth the Additional Cost
Why are we being required to fork over an extra $380 for the Focused Practice in Hospital Medicine MOC? This feels like the icing on the cake of already a major ripoff.
Dr. Ragan
Grass Valley, Calif.
Dr. Hospitalist responds: Thank you for your frank reaction to the much-anticipated American Board of Internal Medicine (ABIM) Focused Practice in Hospital Medicine (FPHM) Maintenance of Certification (MOC) program. As you noted, an additional fee is required to participate in this recertification program.
To my knowledge, any and all fees associated with recertification are paid to ABIM. No other organization benefits from the added cost, so your question might be more appropriately addressed to ABIM (see “Focused Practice in Hospital Medicine,” May 2010, p. 1). But because you asked the question, I am happy to respond with my thoughts.
Participation in the FPHM MOC program is not mandatory. I am not aware of any organization that is requiring hospitalists to participate. I don’t expect that your lack of participation will affect your ability to obtain hospital privileges. Like any new MOC program, I would expect some up-front administrative costs associated with developing and administering the practice-improvement modules and the secure examination.
It’s up to you and others to decide whether this added recognition is worth the cost. I can tell you that I have made the decision to participate. I fully expect to be part of the inaugural class of ABIM diplomates with this added recognition by the end of the year.
What went into my own decision to participate? I can tell you that I am a practicing hospitalist who makes a salary typical of most hospitalists. I am frugal with my money and certainly do not view the added cost as an insignificant amount of money. Like most hospitalists, I am not only busy with my professional life, but I have plenty of family commitments as well.
I expect the exam will be rigorous, and the requirements of the practice-improvement modules will be demanding. I would not want it any other way. In the fast-changing healthcare environment, I believe that hospitalists will be challenged to think about what it means to care for a hospitalized patient. To succeed in the future, hospitalists will be expected to not only participate, but also lead QI efforts at their institutions. The FPHM MOC will distinguish me as a hospitalist with added qualifications in the field of QI.
So how about it, Dr. Ragan? Will you join me?
What Certification Requirements Should a Hospitalist Program Have for Its Physicians?
I hope you can help me with some questions I have concerning starting a hospitalist program at my medical center. Are there certain requirements (e.g., board certification in internal medicine, ACLS, etc.) that need to be met, or is that up to the facility? The physician interested in the position is board-certified in infectious disease. Any direction you can give me on this would be greatly appreciated.
Marisa Sellers,
Medical Staff Coordinator,
Hartselle Medical Center,
Hartselle, Ala.
Dr. Hospitalist responds: Congratulations on your medical center’s decision to establish a hospitalist program. Over the past decade, HM has been the fastest-growing field in all of American medicine. The majority of the country’s acute-care hospitals have hospitalists on staff.
Approximately 85% of the country’s hospitalists received training in internal medicine. Most of the other hospitalists received training in pediatrics or family medicine. While most hospitalists are general internists, some also have additional subspecialty training, which seems to be the case of the physician at your medical center. As you know, different medical facilities have different requirements of their medical staff. At the acute-care hospital where I work clinically, maintenance of board certification is required of all medical staff. I know that is not the case for all hospitals, yet I’m not aware of any hospitals with hospitalist-specific medical staff requirements.
Most of the hospitalists who are internists will be either board-eligible or board-certified with the American Board of Internal Medicine (ABIM). You should be aware that ABIM has developed a new program, the Recognition of Focused Practice (RFP) in Hospital Medicine. As part of this maintenance of certification (MOC) program, ABIM diplomates will have the opportunity to take the first ABIM Hospital Medicine examination in October. For more information about this exam, ABIM’s rationale for recognizing a focused practice in HM, and any other questions about this program, please visit the ABIM Web site at www.abim.org/news/news/focused-
practice-hospital-medicine-qa.aspx.
I have heard from hospitalists trained as family physicians who are interested in RFP as hospitalists. It is my understanding that the American Board of Family Medicine is studying the ABIM program and working to develop a similar program for hospitalists with family medicine board certifications.
Regarding your question about hospitalists and the American Heart Association’s advanced cardiac life support (ACLS) training and certification: While I think it is a great idea for hospitalists to receive this training and maintain this certification, I am not aware of any mandate for hospitalists to be uniformly ACLS-certified. I think this is an issue the medical staff at your medical center will have to decide; basically, what is in the best interests of your patients?
What I Learned
As I write, I’m fighting the jet stream from Washington, D.C., to Denver, midflight on my return from HM10. I’m 30,000 feet above the ground—literally and figuratively—my mind spinning with the thoughts, ideas, and memories from the largest gathering of hospitalists ever. In the end, 2,500 hospitalists descended on our nation’s capital. Shrouded by the din of healthcare reform, we discussed, deliberated, and discovered what’s new in the clinical, political, and programmatic world of HM. Out of this churn, I learned a lot. Here’s but a small sample.
Smart People = Smart Solutions
I learned that if you put really smart people in a room and give them a problem to grapple with, they come up with really smart solutions. At the inaugural Academic Hospital Medicine Leadership Summit, 100 of the brightest, most influential academic hospitalists convened to tackle the problems facing our field.
The output was an amazing crop of inventive ideas aimed at taming the vexing issues surrounding clinical sustainability, academic viability, and career satisfaction. SHM leadership has heard the cry and promises to work closely with the academic community to transform these smart solutions into future initiatives.
Hospitalists Support Healthcare Reform, Should Collude with Hospitals
I learned that most of us support the recently passed healthcare reform legislation, with a few notable dissenters. In response to a question from the chair of SHM’s Public Policy Committee, the vast majority of attendees at the opening plenary session raised their hands affirmatively in response to the question of whether they support the reform bill. Meanwhile, nearly everyone in the crowd felt it is important that SHM have an opinion regarding the legislation and continue to work closely with Congress to ensure its implementation helps our most important constituent—our patients.
Finally, I learned that Ron Greeno, CMO of Brentwood, Tenn.-based Cogent Healthcare, believes that the development of accountable-care organizations might lead hospitalists to align with hospitals to keep costs down. In fact, he saw this as a welcome, intended consequence. In his opinion, this “collusion” promises to raise the quality of care and reduce waste in the system—a statement that was met with applause from the plenary crowd.
The Healthcare Paradox
I learned that blogs save lives. Paul Levy, CEO of Beth Israel Deaconess Medical Center in Boston, roused the crowd during his keynote address by relating the power of transparency. Bothered by the paradox that the medical profession, comprising the most well-intentioned people in the world, could kill so many people through errors (ranked the No. 4 public health hazard in the U.S.), Levy decided to make his hospital’s struggles public.
On his blog, Running a Hospital (runningahospital.blogspot.com), he took the extraordinary step of publically documenting the rates of harm caused at his medical center for the world to see. Additionally, he set audacious goals to reduce the amount of harm to zero. He encouraged hospital staff to raise issues of safety and efficiency as a way to avoid the workarounds—shortcuts—that ultimately increase variability and reduce quality without addressing the core problem.
In response, the staff swarms the problem to rapidly improve the process and ultimately return the system back to homeostasis. The results of this effort can be viewed at Levy’s hospital’s website (www.bidmc.org/QualityandSafety.aspx).
Which Hill Will You Climb?
I learned that leadership is the ability to help people address problems that make the world better. At a much-anticipated presentation, Peter Pronovost, MD, of Johns Hopkins Hospital in Baltimore related a transformative story from his youth. At a summer camp, each boy was assigned to one of three groups and tasked with climbing a seemingly insurmountable hill. The first camp counselor pummeled the group with overbearing directions, directives, and derision, and in the end the group failed to conquer the hill. The second counselor took a more relaxed approach, giving the group essentially no direction. They, too, failed.
The final counselor offered nothing but the inspiration of how marvelous the view from the top of the hill would be and how they’d all have to pull together and work as a team if they wanted to attain that greatness. Dr. Pronovost was in this last group, and has been summiting insurmountable peaks ever since.
You likely are familiar with Dr. Pronovost’s work on ICU line infections. He elaborated on how he accomplished a rate of zero line infections, first at his hospital and then throughout the entire state of Michigan. The key was an inspiring vision and, once again, removal of workarounds. After compiling a checklist of the five most crucial components of line placement and management, Hopkins personnel discovered they were only compliant with the checklist 30% of the time—mostly due to shortcuts caused by inefficient systems that placed supplies too far from the clinical-care setting. After removing those barriers, the compliance rate went to 70%. It was only after empowering the nursing staff to stop physicians from proceeding with line placement unless the checklist was followed that the team was able to achieve 100% compliance.
Today, patients in the Johns Hopkins cardiovascular unit have not suffered a line infection for 87 consecutive weeks. That’s a hill worth climbing.
Saving Lives and Canine Castaways
I learned that the SHM annual meeting is attracting the highest echelon of clinical speakers. Whether it was Dr. Pronovost speaking about line infections, Dr. Greg Fonarow discussing congestive heart failure, or Dr. John Bartlett presenting on Clostrium difficile infections, HM10 featured world-class speakers.
For example, Dr. Bartlett’s work has defined the C. diff field, and the opportunity to hear him was incredible. I learned from him that severe C. diff infections are on the rise and that recurrences are tougher than ever to treat. I also learned that there are mixed data on whether nurses can detect C. diff based on stool smell alone; that up to 10% of dogs carry C. diff (out of the bed, Hogan and Grady!); and that stool transplants are becoming a quality- and quantity-of-life-saving treatment for those with severe bouts of recurrent C. diff.
To quote Dr. Bartlett, “pathophysiologically, it’s a dream; aesthetically, it sucks.”
Homeward Bound
Finally, I learned that every year, SHM feels more and more like my second family, with the annual meeting its family reunion. I saw tons of friends, made dozens more, and look forward to next year in Dallas.
Mostly, however, I was reminded of the emotional tug of being away from home, the emotive power of a few e-mailed photos of your kids, and how great if feels to turn off your electronic devices and return your folding tray and seat back to the upright and locked position. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
As I write, I’m fighting the jet stream from Washington, D.C., to Denver, midflight on my return from HM10. I’m 30,000 feet above the ground—literally and figuratively—my mind spinning with the thoughts, ideas, and memories from the largest gathering of hospitalists ever. In the end, 2,500 hospitalists descended on our nation’s capital. Shrouded by the din of healthcare reform, we discussed, deliberated, and discovered what’s new in the clinical, political, and programmatic world of HM. Out of this churn, I learned a lot. Here’s but a small sample.
Smart People = Smart Solutions
I learned that if you put really smart people in a room and give them a problem to grapple with, they come up with really smart solutions. At the inaugural Academic Hospital Medicine Leadership Summit, 100 of the brightest, most influential academic hospitalists convened to tackle the problems facing our field.
The output was an amazing crop of inventive ideas aimed at taming the vexing issues surrounding clinical sustainability, academic viability, and career satisfaction. SHM leadership has heard the cry and promises to work closely with the academic community to transform these smart solutions into future initiatives.
Hospitalists Support Healthcare Reform, Should Collude with Hospitals
I learned that most of us support the recently passed healthcare reform legislation, with a few notable dissenters. In response to a question from the chair of SHM’s Public Policy Committee, the vast majority of attendees at the opening plenary session raised their hands affirmatively in response to the question of whether they support the reform bill. Meanwhile, nearly everyone in the crowd felt it is important that SHM have an opinion regarding the legislation and continue to work closely with Congress to ensure its implementation helps our most important constituent—our patients.
Finally, I learned that Ron Greeno, CMO of Brentwood, Tenn.-based Cogent Healthcare, believes that the development of accountable-care organizations might lead hospitalists to align with hospitals to keep costs down. In fact, he saw this as a welcome, intended consequence. In his opinion, this “collusion” promises to raise the quality of care and reduce waste in the system—a statement that was met with applause from the plenary crowd.
The Healthcare Paradox
I learned that blogs save lives. Paul Levy, CEO of Beth Israel Deaconess Medical Center in Boston, roused the crowd during his keynote address by relating the power of transparency. Bothered by the paradox that the medical profession, comprising the most well-intentioned people in the world, could kill so many people through errors (ranked the No. 4 public health hazard in the U.S.), Levy decided to make his hospital’s struggles public.
On his blog, Running a Hospital (runningahospital.blogspot.com), he took the extraordinary step of publically documenting the rates of harm caused at his medical center for the world to see. Additionally, he set audacious goals to reduce the amount of harm to zero. He encouraged hospital staff to raise issues of safety and efficiency as a way to avoid the workarounds—shortcuts—that ultimately increase variability and reduce quality without addressing the core problem.
In response, the staff swarms the problem to rapidly improve the process and ultimately return the system back to homeostasis. The results of this effort can be viewed at Levy’s hospital’s website (www.bidmc.org/QualityandSafety.aspx).
Which Hill Will You Climb?
I learned that leadership is the ability to help people address problems that make the world better. At a much-anticipated presentation, Peter Pronovost, MD, of Johns Hopkins Hospital in Baltimore related a transformative story from his youth. At a summer camp, each boy was assigned to one of three groups and tasked with climbing a seemingly insurmountable hill. The first camp counselor pummeled the group with overbearing directions, directives, and derision, and in the end the group failed to conquer the hill. The second counselor took a more relaxed approach, giving the group essentially no direction. They, too, failed.
The final counselor offered nothing but the inspiration of how marvelous the view from the top of the hill would be and how they’d all have to pull together and work as a team if they wanted to attain that greatness. Dr. Pronovost was in this last group, and has been summiting insurmountable peaks ever since.
You likely are familiar with Dr. Pronovost’s work on ICU line infections. He elaborated on how he accomplished a rate of zero line infections, first at his hospital and then throughout the entire state of Michigan. The key was an inspiring vision and, once again, removal of workarounds. After compiling a checklist of the five most crucial components of line placement and management, Hopkins personnel discovered they were only compliant with the checklist 30% of the time—mostly due to shortcuts caused by inefficient systems that placed supplies too far from the clinical-care setting. After removing those barriers, the compliance rate went to 70%. It was only after empowering the nursing staff to stop physicians from proceeding with line placement unless the checklist was followed that the team was able to achieve 100% compliance.
Today, patients in the Johns Hopkins cardiovascular unit have not suffered a line infection for 87 consecutive weeks. That’s a hill worth climbing.
Saving Lives and Canine Castaways
I learned that the SHM annual meeting is attracting the highest echelon of clinical speakers. Whether it was Dr. Pronovost speaking about line infections, Dr. Greg Fonarow discussing congestive heart failure, or Dr. John Bartlett presenting on Clostrium difficile infections, HM10 featured world-class speakers.
For example, Dr. Bartlett’s work has defined the C. diff field, and the opportunity to hear him was incredible. I learned from him that severe C. diff infections are on the rise and that recurrences are tougher than ever to treat. I also learned that there are mixed data on whether nurses can detect C. diff based on stool smell alone; that up to 10% of dogs carry C. diff (out of the bed, Hogan and Grady!); and that stool transplants are becoming a quality- and quantity-of-life-saving treatment for those with severe bouts of recurrent C. diff.
To quote Dr. Bartlett, “pathophysiologically, it’s a dream; aesthetically, it sucks.”
Homeward Bound
Finally, I learned that every year, SHM feels more and more like my second family, with the annual meeting its family reunion. I saw tons of friends, made dozens more, and look forward to next year in Dallas.
Mostly, however, I was reminded of the emotional tug of being away from home, the emotive power of a few e-mailed photos of your kids, and how great if feels to turn off your electronic devices and return your folding tray and seat back to the upright and locked position. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
As I write, I’m fighting the jet stream from Washington, D.C., to Denver, midflight on my return from HM10. I’m 30,000 feet above the ground—literally and figuratively—my mind spinning with the thoughts, ideas, and memories from the largest gathering of hospitalists ever. In the end, 2,500 hospitalists descended on our nation’s capital. Shrouded by the din of healthcare reform, we discussed, deliberated, and discovered what’s new in the clinical, political, and programmatic world of HM. Out of this churn, I learned a lot. Here’s but a small sample.
Smart People = Smart Solutions
I learned that if you put really smart people in a room and give them a problem to grapple with, they come up with really smart solutions. At the inaugural Academic Hospital Medicine Leadership Summit, 100 of the brightest, most influential academic hospitalists convened to tackle the problems facing our field.
The output was an amazing crop of inventive ideas aimed at taming the vexing issues surrounding clinical sustainability, academic viability, and career satisfaction. SHM leadership has heard the cry and promises to work closely with the academic community to transform these smart solutions into future initiatives.
Hospitalists Support Healthcare Reform, Should Collude with Hospitals
I learned that most of us support the recently passed healthcare reform legislation, with a few notable dissenters. In response to a question from the chair of SHM’s Public Policy Committee, the vast majority of attendees at the opening plenary session raised their hands affirmatively in response to the question of whether they support the reform bill. Meanwhile, nearly everyone in the crowd felt it is important that SHM have an opinion regarding the legislation and continue to work closely with Congress to ensure its implementation helps our most important constituent—our patients.
Finally, I learned that Ron Greeno, CMO of Brentwood, Tenn.-based Cogent Healthcare, believes that the development of accountable-care organizations might lead hospitalists to align with hospitals to keep costs down. In fact, he saw this as a welcome, intended consequence. In his opinion, this “collusion” promises to raise the quality of care and reduce waste in the system—a statement that was met with applause from the plenary crowd.
The Healthcare Paradox
I learned that blogs save lives. Paul Levy, CEO of Beth Israel Deaconess Medical Center in Boston, roused the crowd during his keynote address by relating the power of transparency. Bothered by the paradox that the medical profession, comprising the most well-intentioned people in the world, could kill so many people through errors (ranked the No. 4 public health hazard in the U.S.), Levy decided to make his hospital’s struggles public.
On his blog, Running a Hospital (runningahospital.blogspot.com), he took the extraordinary step of publically documenting the rates of harm caused at his medical center for the world to see. Additionally, he set audacious goals to reduce the amount of harm to zero. He encouraged hospital staff to raise issues of safety and efficiency as a way to avoid the workarounds—shortcuts—that ultimately increase variability and reduce quality without addressing the core problem.
In response, the staff swarms the problem to rapidly improve the process and ultimately return the system back to homeostasis. The results of this effort can be viewed at Levy’s hospital’s website (www.bidmc.org/QualityandSafety.aspx).
Which Hill Will You Climb?
I learned that leadership is the ability to help people address problems that make the world better. At a much-anticipated presentation, Peter Pronovost, MD, of Johns Hopkins Hospital in Baltimore related a transformative story from his youth. At a summer camp, each boy was assigned to one of three groups and tasked with climbing a seemingly insurmountable hill. The first camp counselor pummeled the group with overbearing directions, directives, and derision, and in the end the group failed to conquer the hill. The second counselor took a more relaxed approach, giving the group essentially no direction. They, too, failed.
The final counselor offered nothing but the inspiration of how marvelous the view from the top of the hill would be and how they’d all have to pull together and work as a team if they wanted to attain that greatness. Dr. Pronovost was in this last group, and has been summiting insurmountable peaks ever since.
You likely are familiar with Dr. Pronovost’s work on ICU line infections. He elaborated on how he accomplished a rate of zero line infections, first at his hospital and then throughout the entire state of Michigan. The key was an inspiring vision and, once again, removal of workarounds. After compiling a checklist of the five most crucial components of line placement and management, Hopkins personnel discovered they were only compliant with the checklist 30% of the time—mostly due to shortcuts caused by inefficient systems that placed supplies too far from the clinical-care setting. After removing those barriers, the compliance rate went to 70%. It was only after empowering the nursing staff to stop physicians from proceeding with line placement unless the checklist was followed that the team was able to achieve 100% compliance.
Today, patients in the Johns Hopkins cardiovascular unit have not suffered a line infection for 87 consecutive weeks. That’s a hill worth climbing.
Saving Lives and Canine Castaways
I learned that the SHM annual meeting is attracting the highest echelon of clinical speakers. Whether it was Dr. Pronovost speaking about line infections, Dr. Greg Fonarow discussing congestive heart failure, or Dr. John Bartlett presenting on Clostrium difficile infections, HM10 featured world-class speakers.
For example, Dr. Bartlett’s work has defined the C. diff field, and the opportunity to hear him was incredible. I learned from him that severe C. diff infections are on the rise and that recurrences are tougher than ever to treat. I also learned that there are mixed data on whether nurses can detect C. diff based on stool smell alone; that up to 10% of dogs carry C. diff (out of the bed, Hogan and Grady!); and that stool transplants are becoming a quality- and quantity-of-life-saving treatment for those with severe bouts of recurrent C. diff.
To quote Dr. Bartlett, “pathophysiologically, it’s a dream; aesthetically, it sucks.”
Homeward Bound
Finally, I learned that every year, SHM feels more and more like my second family, with the annual meeting its family reunion. I saw tons of friends, made dozens more, and look forward to next year in Dallas.
Mostly, however, I was reminded of the emotional tug of being away from home, the emotive power of a few e-mailed photos of your kids, and how great if feels to turn off your electronic devices and return your folding tray and seat back to the upright and locked position. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Attention to Detail
Hospitalists will be essential players in helping their institutions prepare for the Recovery Audit Contractor (RAC) program, now being rolled out nationwide by the Centers for Medicare & Medicaid Services (CMS). The program is part of CMS’ arsenal to ferret out improper payments and prevent fraud, waste, and abuse in the Medicare system.
All providers who bill Medicare fee-for-service are fair game for an RAC audit, which scrutinizes medical records to validate diagnosis-related groups (DRGs), coding, and the necessity of care provided by hospitals. Hospitalists are being asked to document their diagnosis and treatment decisions more precisely and thoroughly than ever, ensuring that DRG coding is appropriate, medical necessity is watertight, and hospitals are defended from costly overpayment recovery.
Specificity of documentation is the hospitalist’s most potent weapon against this new layer of federal audits.
In a three-year demonstration of the RAC program that ended in March 2008, one-third of all medical records audited resulted in an overpayment finding and collection. RACs collected more than $900 million in overpayments and returned nearly $38 million in underpayments. One-third of provider appeals (physician, hospital, and other providers) were successful during the demo program, according to a June 2008 CMS evaluation report. (Download a copy of the report at www.cms.hhs.gov/RAC/Downloads/RAC_Demonstration_Evaluation_Report.pdf.)
How the Audits Work

Listen to an interview with Dr. Pinson
Out of concern that the Medicare Trust Fund might not be adequately protected against improper payments by existing error detection and prevention efforts, Congress directed CMS to use RACs to identify and recoup Medicare overpayments under Section 306 of the Medicare Modernization Act of 2003, and directed CMS to make the program permanent by 2010 under Section 302 of the Tax Relief and Health Care Act of 2006. According to CMS, RACs were implemented so that physicians and other providers could avoid submitting claims that do not comply with Medicare rules, CMS could lower its error rate, and taxpayers and future Medicare beneficiaries would be protected.1
CMS has contracted with four regional RACs for the national program, and each will use proprietary auditing software to review paid claims from Medicare Part A and Part B providers to ensure that they meet Medicare’s statutory, regulatory, and policy requirements and regulations.
The RACs use automated review for claims that clearly contain errors that resulted in improper payments (e.g., claims for duplicate or uncovered services, claims that violate a written Medicare policy or sanctioned coding guideline), in which case the RAC notifies the provider of the overpayment. For cases in which there is a high probability—but not certainty—that the claim contains an overpayment, the RAC requests medical records from the provider (including imaged medical records on CD or DVD) to conduct a complex review and make a determination as to whether payment of the claim was correct, or whether there was an over- or underpayment.
CMS uses a Web-based data warehouse to ensure that RACs do not review claims that have previously been reviewed by another entity, such as a Medicare carrier, fiscal intermediary, the Office of Inspector General, or a quality-improvement organization (QIO).
The four regional RACs are ramping up their claim review activities in all states, says Connie Leonard, director of CMS’ Division of Recovery Audit Operations. When overpayments are confirmed, the RACs issue letters demanding providers to repay their Medicare carrier or intermediary within 30 days. For confirmed underpayments, RACs inform the provider’s Medicare contractor or fiscal intermediary, which then forwards the additional payment, Leonard says.
Providers can repay an overpayment by check or installment plan on or before 30 days after receiving the RAC demand letter. The Medicare contractors use recoupment—reducing present or future Medicare payments—on day 41. Providers who wish to dispute overpayment charges can take their case through the usual Medicare claims appeal process. RACs also offer a “discussion period”—from the date the provider gets a “Detailed Review Results” letter until the date of recoupment—to discuss with the RAC an improper payment determination outside the normal appeal process, Leonard says.

—Kathy DeVault, RHIA, CCS, CCS-P, manager, Professional Practice Resources, American Health Information Management Association, Chicago
If providers disagree with the RAC’s determination, Leonard says, they should either 1) pay by check by day 30 and file for appeal by day 120 of the demand letter; 2) allow recoupment on day 41 and file for appeal by day 120; 3) stop the recoupment by filing an appeal by day 30; or 4) request an extended payment plan and appeal by day 120.
Some physicians in the demonstration project regarded the third-party RAC companies as “bounty hunters” operating without sufficient CMS oversight, imposing undue administrative burdens on physician practices, and lacking the clinical expertise to adjudicate claims appropriately, according to Michael Schweitz, MD, a rheumatologist from West Palm Beach, Fla., who testified before a Congressional committee in 2008 about RAC activities.
In response, CMS has modified the program (see “Refinements in Permanent RAC Program,” p. 8) in several ways to address those flaws and ensure a fair and smooth auditing process, Leonard says. (Listen to an audio interview with Ms. Leonard)
All About the Details
Because RACs focus on coding and documentation that fails to support DRG designations, hospitalists who focus on accurate and precise documentation that can be coded properly will greatly help their hospitals defend against RAC audits, as well as yield better payment and improved quality scores, says Richard D. Pinson, MD, FACP, CCS, principal of HCQ Consulting in Nashville, Tenn. Pinson will present “Documentation Tips Your Hospital Will Love You For” at HM10 in Washington, D.C., this month. A video/audio download of the presentation will be available on SHM’s Web site in May.
“Coding rules and terminology often don’t match what we’re used to writing in the record, so hospitalists need to learn what these connections are and use them in their medical record documentation,” Pinson says. “This is a core skill for hospitalists: being able to translate clinical terminology into the correct coding terminology for hospitals and coders.”
For example, if a hospitalist sees that a pre-operative patient has severe congestive heart failure, that condition cannot be coded as a complication of the patient’s care or considered as such in the DRG assignment, Pinson explains. If the hospitalist says the patient has an acute exacerbation of systolic heart failure, then that is a major comorbidity and ought to be documented as such. The average value of a major comorbidity in a surgical case could be as much as $20,000 per case, Pinson notes. If the DRG assignment included acute exacerbation but the medical chart only said severe congestive heart failure, the hospital would face recoupment of payment from an RAC audit.
“If we’re inconsistent or ambiguous in how we apply our terms, we can end up inadvertently upcoding. The key is: Learn to use the right terms that correspond to the right codes, based on what your patient actually has, and then be consistent throughout the record in your use of those terms,” Pinson says. For example, “we may admit a patient and say at the very beginning that the patient probably has aspiration pneumonia. We then treat the patient for aspiration pneumonia but leave it out of the discharge summary. The coder may code aspiration pneumonia, but the RAC auditor may point out that it was only mentioned in the patient’s record once, as possible, and may recoup any payment for treatment beyond simple pneumonia.”
Level of care and symptom-based DRG designations are red flags for RAC recovery, Pinson says. When the auditor sees a DRG based on symptoms rather than diagnoses (e.g., chest pain, syncope, transient ischemic attack, dehydration) and it is billed as inpatient status instead of observation status, that’s a target. Those symptoms, he says, often don’t meet the medical necessity criteria for inpatient status.
Pinson advises hospitalists to ask their institution’s case-management department, or hire an external consultant, to abstract key criteria for patient status designation, and to consider starting a patient as observation status until a precise diagnosis can be made that warrants hospital admission. Hospitalists should then describe the patient’s situation more precisely in the medical record as a diagnosis, not just as symptoms—e.g., syncope suspected due to cardiac arrhythmia, or chest pain suspected to be angina.
“For inpatient billing, those uncertain diagnoses, described that way, count as if they were established conditions. They don’t go into symptom DRGs,” Pinson says. “If you’re doing these things to protect the validity of you hospital’s billing, you’ll be protecting yourself at the same time, and it’s unlikely that RACs will single you out at all for auditing.”
Hospitalists can be valuable participants on their institutions’ RAC response team, providing clinical clarification on cases and helping to draft appeal letters.
There are several other red flags that RACs zero in on and hospitalists should watch out for, says Kathy DeVault, RHIA, CCS, CCS-P, manager of Professional Practice Resources for the American Health Information Management Association (AHIMA). Specificity in the medical record makes all the difference. For example, by identifying incorrect coding for excisional debridement (removal of infected tissue), RACs collected nearly $18 million in overpayments in fiscal-year 2006 because medical record documentation omitted such details as the word “excisional” (e.g., sharp debridement coded as excisional debridement), whether it was performed in the operating room or not, instruments used, the extent and depth of the procedure, and if the cutting of tissue was outside or beyond the wound margin.
DeVault warns that “RACs are targeting confusion between septicemia and urosepsis.” According to CMS, if the hospital reports a patient’s principal diagnosis as septicemia (03.89) but the medical record indicates the diagnosis of urosepsis, the RAC will bump the diagnosis code down to urinary tract infection (599.0), a lower-payment DRG, and demand recoupment.1
Urosepsis does not have a specific ICD-9-CM diagnosis code, and defaults to a simple UTI code, as referenced in ICD-9-CM. Unless the physician states in his or her documentation that the patient’s condition was systemic sepsis or septicemia, urosepsis would be coded as a UTI. RACS also denied some respiratory-failure claims for incorrect sequencing of principal diagnosis (e.g., respiratory failure vs. sepsis). The American Hospital Association has issued a regulatory advisory about these issues (web.mhanet.com/userdocs/articles/RAC/AHA_RAC_Coding Advisory_071608.pdf).
DeVault highlights three additional RAC targets that might impact HM:
- Documentation for transbronchial biopsy (a surgical DRG) in which the medical record only shows pathology of bronchus tissue (which RACs regard as nonsurgical);
- Failure to document the severity of a patient’s anemia as such to meet the medical necessity requirement of a blood transfusion (e.g., a chronic blood loss anemia or a pernicious anemia); and
- Documentation of treatments performed by intensivists in an ICU. By the time a patient’s attending physician sees their patient out of the ICU, DeVault says, their acute renal failure could be turned around but the attending might not document what happened in the ICU. The intensivist must see to it that the documentation allows the appropriate DRG assignment for the level of care the patient received.
AHIMA has published a 65-page RAC Audit Toolkit that describes the audit process, outlines preparations and procedures, and offers concrete guidance for appeals. Download a copy at www.ahima.org/infocenter/documents/RACToolkitFINAL.pdf. TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- The Medicare Recovery Audit Contractor (RAC) program: an evaluation of the 3-year demonstration. CMS Web site. Available at: www.cms.hhs.gov/RAC/Downloads/RACEvaluationReport.pdf. Accessed March 3, 2010.
Hospitalists will be essential players in helping their institutions prepare for the Recovery Audit Contractor (RAC) program, now being rolled out nationwide by the Centers for Medicare & Medicaid Services (CMS). The program is part of CMS’ arsenal to ferret out improper payments and prevent fraud, waste, and abuse in the Medicare system.
All providers who bill Medicare fee-for-service are fair game for an RAC audit, which scrutinizes medical records to validate diagnosis-related groups (DRGs), coding, and the necessity of care provided by hospitals. Hospitalists are being asked to document their diagnosis and treatment decisions more precisely and thoroughly than ever, ensuring that DRG coding is appropriate, medical necessity is watertight, and hospitals are defended from costly overpayment recovery.
Specificity of documentation is the hospitalist’s most potent weapon against this new layer of federal audits.
In a three-year demonstration of the RAC program that ended in March 2008, one-third of all medical records audited resulted in an overpayment finding and collection. RACs collected more than $900 million in overpayments and returned nearly $38 million in underpayments. One-third of provider appeals (physician, hospital, and other providers) were successful during the demo program, according to a June 2008 CMS evaluation report. (Download a copy of the report at www.cms.hhs.gov/RAC/Downloads/RAC_Demonstration_Evaluation_Report.pdf.)
How the Audits Work

Listen to an interview with Dr. Pinson
Out of concern that the Medicare Trust Fund might not be adequately protected against improper payments by existing error detection and prevention efforts, Congress directed CMS to use RACs to identify and recoup Medicare overpayments under Section 306 of the Medicare Modernization Act of 2003, and directed CMS to make the program permanent by 2010 under Section 302 of the Tax Relief and Health Care Act of 2006. According to CMS, RACs were implemented so that physicians and other providers could avoid submitting claims that do not comply with Medicare rules, CMS could lower its error rate, and taxpayers and future Medicare beneficiaries would be protected.1
CMS has contracted with four regional RACs for the national program, and each will use proprietary auditing software to review paid claims from Medicare Part A and Part B providers to ensure that they meet Medicare’s statutory, regulatory, and policy requirements and regulations.
The RACs use automated review for claims that clearly contain errors that resulted in improper payments (e.g., claims for duplicate or uncovered services, claims that violate a written Medicare policy or sanctioned coding guideline), in which case the RAC notifies the provider of the overpayment. For cases in which there is a high probability—but not certainty—that the claim contains an overpayment, the RAC requests medical records from the provider (including imaged medical records on CD or DVD) to conduct a complex review and make a determination as to whether payment of the claim was correct, or whether there was an over- or underpayment.
CMS uses a Web-based data warehouse to ensure that RACs do not review claims that have previously been reviewed by another entity, such as a Medicare carrier, fiscal intermediary, the Office of Inspector General, or a quality-improvement organization (QIO).
The four regional RACs are ramping up their claim review activities in all states, says Connie Leonard, director of CMS’ Division of Recovery Audit Operations. When overpayments are confirmed, the RACs issue letters demanding providers to repay their Medicare carrier or intermediary within 30 days. For confirmed underpayments, RACs inform the provider’s Medicare contractor or fiscal intermediary, which then forwards the additional payment, Leonard says.
Providers can repay an overpayment by check or installment plan on or before 30 days after receiving the RAC demand letter. The Medicare contractors use recoupment—reducing present or future Medicare payments—on day 41. Providers who wish to dispute overpayment charges can take their case through the usual Medicare claims appeal process. RACs also offer a “discussion period”—from the date the provider gets a “Detailed Review Results” letter until the date of recoupment—to discuss with the RAC an improper payment determination outside the normal appeal process, Leonard says.

—Kathy DeVault, RHIA, CCS, CCS-P, manager, Professional Practice Resources, American Health Information Management Association, Chicago
If providers disagree with the RAC’s determination, Leonard says, they should either 1) pay by check by day 30 and file for appeal by day 120 of the demand letter; 2) allow recoupment on day 41 and file for appeal by day 120; 3) stop the recoupment by filing an appeal by day 30; or 4) request an extended payment plan and appeal by day 120.
Some physicians in the demonstration project regarded the third-party RAC companies as “bounty hunters” operating without sufficient CMS oversight, imposing undue administrative burdens on physician practices, and lacking the clinical expertise to adjudicate claims appropriately, according to Michael Schweitz, MD, a rheumatologist from West Palm Beach, Fla., who testified before a Congressional committee in 2008 about RAC activities.
In response, CMS has modified the program (see “Refinements in Permanent RAC Program,” p. 8) in several ways to address those flaws and ensure a fair and smooth auditing process, Leonard says. (Listen to an audio interview with Ms. Leonard)
All About the Details
Because RACs focus on coding and documentation that fails to support DRG designations, hospitalists who focus on accurate and precise documentation that can be coded properly will greatly help their hospitals defend against RAC audits, as well as yield better payment and improved quality scores, says Richard D. Pinson, MD, FACP, CCS, principal of HCQ Consulting in Nashville, Tenn. Pinson will present “Documentation Tips Your Hospital Will Love You For” at HM10 in Washington, D.C., this month. A video/audio download of the presentation will be available on SHM’s Web site in May.
“Coding rules and terminology often don’t match what we’re used to writing in the record, so hospitalists need to learn what these connections are and use them in their medical record documentation,” Pinson says. “This is a core skill for hospitalists: being able to translate clinical terminology into the correct coding terminology for hospitals and coders.”
For example, if a hospitalist sees that a pre-operative patient has severe congestive heart failure, that condition cannot be coded as a complication of the patient’s care or considered as such in the DRG assignment, Pinson explains. If the hospitalist says the patient has an acute exacerbation of systolic heart failure, then that is a major comorbidity and ought to be documented as such. The average value of a major comorbidity in a surgical case could be as much as $20,000 per case, Pinson notes. If the DRG assignment included acute exacerbation but the medical chart only said severe congestive heart failure, the hospital would face recoupment of payment from an RAC audit.
“If we’re inconsistent or ambiguous in how we apply our terms, we can end up inadvertently upcoding. The key is: Learn to use the right terms that correspond to the right codes, based on what your patient actually has, and then be consistent throughout the record in your use of those terms,” Pinson says. For example, “we may admit a patient and say at the very beginning that the patient probably has aspiration pneumonia. We then treat the patient for aspiration pneumonia but leave it out of the discharge summary. The coder may code aspiration pneumonia, but the RAC auditor may point out that it was only mentioned in the patient’s record once, as possible, and may recoup any payment for treatment beyond simple pneumonia.”
Level of care and symptom-based DRG designations are red flags for RAC recovery, Pinson says. When the auditor sees a DRG based on symptoms rather than diagnoses (e.g., chest pain, syncope, transient ischemic attack, dehydration) and it is billed as inpatient status instead of observation status, that’s a target. Those symptoms, he says, often don’t meet the medical necessity criteria for inpatient status.
Pinson advises hospitalists to ask their institution’s case-management department, or hire an external consultant, to abstract key criteria for patient status designation, and to consider starting a patient as observation status until a precise diagnosis can be made that warrants hospital admission. Hospitalists should then describe the patient’s situation more precisely in the medical record as a diagnosis, not just as symptoms—e.g., syncope suspected due to cardiac arrhythmia, or chest pain suspected to be angina.
“For inpatient billing, those uncertain diagnoses, described that way, count as if they were established conditions. They don’t go into symptom DRGs,” Pinson says. “If you’re doing these things to protect the validity of you hospital’s billing, you’ll be protecting yourself at the same time, and it’s unlikely that RACs will single you out at all for auditing.”
Hospitalists can be valuable participants on their institutions’ RAC response team, providing clinical clarification on cases and helping to draft appeal letters.
There are several other red flags that RACs zero in on and hospitalists should watch out for, says Kathy DeVault, RHIA, CCS, CCS-P, manager of Professional Practice Resources for the American Health Information Management Association (AHIMA). Specificity in the medical record makes all the difference. For example, by identifying incorrect coding for excisional debridement (removal of infected tissue), RACs collected nearly $18 million in overpayments in fiscal-year 2006 because medical record documentation omitted such details as the word “excisional” (e.g., sharp debridement coded as excisional debridement), whether it was performed in the operating room or not, instruments used, the extent and depth of the procedure, and if the cutting of tissue was outside or beyond the wound margin.
DeVault warns that “RACs are targeting confusion between septicemia and urosepsis.” According to CMS, if the hospital reports a patient’s principal diagnosis as septicemia (03.89) but the medical record indicates the diagnosis of urosepsis, the RAC will bump the diagnosis code down to urinary tract infection (599.0), a lower-payment DRG, and demand recoupment.1
Urosepsis does not have a specific ICD-9-CM diagnosis code, and defaults to a simple UTI code, as referenced in ICD-9-CM. Unless the physician states in his or her documentation that the patient’s condition was systemic sepsis or septicemia, urosepsis would be coded as a UTI. RACS also denied some respiratory-failure claims for incorrect sequencing of principal diagnosis (e.g., respiratory failure vs. sepsis). The American Hospital Association has issued a regulatory advisory about these issues (web.mhanet.com/userdocs/articles/RAC/AHA_RAC_Coding Advisory_071608.pdf).
DeVault highlights three additional RAC targets that might impact HM:
- Documentation for transbronchial biopsy (a surgical DRG) in which the medical record only shows pathology of bronchus tissue (which RACs regard as nonsurgical);
- Failure to document the severity of a patient’s anemia as such to meet the medical necessity requirement of a blood transfusion (e.g., a chronic blood loss anemia or a pernicious anemia); and
- Documentation of treatments performed by intensivists in an ICU. By the time a patient’s attending physician sees their patient out of the ICU, DeVault says, their acute renal failure could be turned around but the attending might not document what happened in the ICU. The intensivist must see to it that the documentation allows the appropriate DRG assignment for the level of care the patient received.
AHIMA has published a 65-page RAC Audit Toolkit that describes the audit process, outlines preparations and procedures, and offers concrete guidance for appeals. Download a copy at www.ahima.org/infocenter/documents/RACToolkitFINAL.pdf. TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- The Medicare Recovery Audit Contractor (RAC) program: an evaluation of the 3-year demonstration. CMS Web site. Available at: www.cms.hhs.gov/RAC/Downloads/RACEvaluationReport.pdf. Accessed March 3, 2010.
Hospitalists will be essential players in helping their institutions prepare for the Recovery Audit Contractor (RAC) program, now being rolled out nationwide by the Centers for Medicare & Medicaid Services (CMS). The program is part of CMS’ arsenal to ferret out improper payments and prevent fraud, waste, and abuse in the Medicare system.
All providers who bill Medicare fee-for-service are fair game for an RAC audit, which scrutinizes medical records to validate diagnosis-related groups (DRGs), coding, and the necessity of care provided by hospitals. Hospitalists are being asked to document their diagnosis and treatment decisions more precisely and thoroughly than ever, ensuring that DRG coding is appropriate, medical necessity is watertight, and hospitals are defended from costly overpayment recovery.
Specificity of documentation is the hospitalist’s most potent weapon against this new layer of federal audits.
In a three-year demonstration of the RAC program that ended in March 2008, one-third of all medical records audited resulted in an overpayment finding and collection. RACs collected more than $900 million in overpayments and returned nearly $38 million in underpayments. One-third of provider appeals (physician, hospital, and other providers) were successful during the demo program, according to a June 2008 CMS evaluation report. (Download a copy of the report at www.cms.hhs.gov/RAC/Downloads/RAC_Demonstration_Evaluation_Report.pdf.)
How the Audits Work

Listen to an interview with Dr. Pinson
Out of concern that the Medicare Trust Fund might not be adequately protected against improper payments by existing error detection and prevention efforts, Congress directed CMS to use RACs to identify and recoup Medicare overpayments under Section 306 of the Medicare Modernization Act of 2003, and directed CMS to make the program permanent by 2010 under Section 302 of the Tax Relief and Health Care Act of 2006. According to CMS, RACs were implemented so that physicians and other providers could avoid submitting claims that do not comply with Medicare rules, CMS could lower its error rate, and taxpayers and future Medicare beneficiaries would be protected.1
CMS has contracted with four regional RACs for the national program, and each will use proprietary auditing software to review paid claims from Medicare Part A and Part B providers to ensure that they meet Medicare’s statutory, regulatory, and policy requirements and regulations.
The RACs use automated review for claims that clearly contain errors that resulted in improper payments (e.g., claims for duplicate or uncovered services, claims that violate a written Medicare policy or sanctioned coding guideline), in which case the RAC notifies the provider of the overpayment. For cases in which there is a high probability—but not certainty—that the claim contains an overpayment, the RAC requests medical records from the provider (including imaged medical records on CD or DVD) to conduct a complex review and make a determination as to whether payment of the claim was correct, or whether there was an over- or underpayment.
CMS uses a Web-based data warehouse to ensure that RACs do not review claims that have previously been reviewed by another entity, such as a Medicare carrier, fiscal intermediary, the Office of Inspector General, or a quality-improvement organization (QIO).
The four regional RACs are ramping up their claim review activities in all states, says Connie Leonard, director of CMS’ Division of Recovery Audit Operations. When overpayments are confirmed, the RACs issue letters demanding providers to repay their Medicare carrier or intermediary within 30 days. For confirmed underpayments, RACs inform the provider’s Medicare contractor or fiscal intermediary, which then forwards the additional payment, Leonard says.
Providers can repay an overpayment by check or installment plan on or before 30 days after receiving the RAC demand letter. The Medicare contractors use recoupment—reducing present or future Medicare payments—on day 41. Providers who wish to dispute overpayment charges can take their case through the usual Medicare claims appeal process. RACs also offer a “discussion period”—from the date the provider gets a “Detailed Review Results” letter until the date of recoupment—to discuss with the RAC an improper payment determination outside the normal appeal process, Leonard says.

—Kathy DeVault, RHIA, CCS, CCS-P, manager, Professional Practice Resources, American Health Information Management Association, Chicago
If providers disagree with the RAC’s determination, Leonard says, they should either 1) pay by check by day 30 and file for appeal by day 120 of the demand letter; 2) allow recoupment on day 41 and file for appeal by day 120; 3) stop the recoupment by filing an appeal by day 30; or 4) request an extended payment plan and appeal by day 120.
Some physicians in the demonstration project regarded the third-party RAC companies as “bounty hunters” operating without sufficient CMS oversight, imposing undue administrative burdens on physician practices, and lacking the clinical expertise to adjudicate claims appropriately, according to Michael Schweitz, MD, a rheumatologist from West Palm Beach, Fla., who testified before a Congressional committee in 2008 about RAC activities.
In response, CMS has modified the program (see “Refinements in Permanent RAC Program,” p. 8) in several ways to address those flaws and ensure a fair and smooth auditing process, Leonard says. (Listen to an audio interview with Ms. Leonard)
All About the Details
Because RACs focus on coding and documentation that fails to support DRG designations, hospitalists who focus on accurate and precise documentation that can be coded properly will greatly help their hospitals defend against RAC audits, as well as yield better payment and improved quality scores, says Richard D. Pinson, MD, FACP, CCS, principal of HCQ Consulting in Nashville, Tenn. Pinson will present “Documentation Tips Your Hospital Will Love You For” at HM10 in Washington, D.C., this month. A video/audio download of the presentation will be available on SHM’s Web site in May.
“Coding rules and terminology often don’t match what we’re used to writing in the record, so hospitalists need to learn what these connections are and use them in their medical record documentation,” Pinson says. “This is a core skill for hospitalists: being able to translate clinical terminology into the correct coding terminology for hospitals and coders.”
For example, if a hospitalist sees that a pre-operative patient has severe congestive heart failure, that condition cannot be coded as a complication of the patient’s care or considered as such in the DRG assignment, Pinson explains. If the hospitalist says the patient has an acute exacerbation of systolic heart failure, then that is a major comorbidity and ought to be documented as such. The average value of a major comorbidity in a surgical case could be as much as $20,000 per case, Pinson notes. If the DRG assignment included acute exacerbation but the medical chart only said severe congestive heart failure, the hospital would face recoupment of payment from an RAC audit.
“If we’re inconsistent or ambiguous in how we apply our terms, we can end up inadvertently upcoding. The key is: Learn to use the right terms that correspond to the right codes, based on what your patient actually has, and then be consistent throughout the record in your use of those terms,” Pinson says. For example, “we may admit a patient and say at the very beginning that the patient probably has aspiration pneumonia. We then treat the patient for aspiration pneumonia but leave it out of the discharge summary. The coder may code aspiration pneumonia, but the RAC auditor may point out that it was only mentioned in the patient’s record once, as possible, and may recoup any payment for treatment beyond simple pneumonia.”
Level of care and symptom-based DRG designations are red flags for RAC recovery, Pinson says. When the auditor sees a DRG based on symptoms rather than diagnoses (e.g., chest pain, syncope, transient ischemic attack, dehydration) and it is billed as inpatient status instead of observation status, that’s a target. Those symptoms, he says, often don’t meet the medical necessity criteria for inpatient status.
Pinson advises hospitalists to ask their institution’s case-management department, or hire an external consultant, to abstract key criteria for patient status designation, and to consider starting a patient as observation status until a precise diagnosis can be made that warrants hospital admission. Hospitalists should then describe the patient’s situation more precisely in the medical record as a diagnosis, not just as symptoms—e.g., syncope suspected due to cardiac arrhythmia, or chest pain suspected to be angina.
“For inpatient billing, those uncertain diagnoses, described that way, count as if they were established conditions. They don’t go into symptom DRGs,” Pinson says. “If you’re doing these things to protect the validity of you hospital’s billing, you’ll be protecting yourself at the same time, and it’s unlikely that RACs will single you out at all for auditing.”
Hospitalists can be valuable participants on their institutions’ RAC response team, providing clinical clarification on cases and helping to draft appeal letters.
There are several other red flags that RACs zero in on and hospitalists should watch out for, says Kathy DeVault, RHIA, CCS, CCS-P, manager of Professional Practice Resources for the American Health Information Management Association (AHIMA). Specificity in the medical record makes all the difference. For example, by identifying incorrect coding for excisional debridement (removal of infected tissue), RACs collected nearly $18 million in overpayments in fiscal-year 2006 because medical record documentation omitted such details as the word “excisional” (e.g., sharp debridement coded as excisional debridement), whether it was performed in the operating room or not, instruments used, the extent and depth of the procedure, and if the cutting of tissue was outside or beyond the wound margin.
DeVault warns that “RACs are targeting confusion between septicemia and urosepsis.” According to CMS, if the hospital reports a patient’s principal diagnosis as septicemia (03.89) but the medical record indicates the diagnosis of urosepsis, the RAC will bump the diagnosis code down to urinary tract infection (599.0), a lower-payment DRG, and demand recoupment.1
Urosepsis does not have a specific ICD-9-CM diagnosis code, and defaults to a simple UTI code, as referenced in ICD-9-CM. Unless the physician states in his or her documentation that the patient’s condition was systemic sepsis or septicemia, urosepsis would be coded as a UTI. RACS also denied some respiratory-failure claims for incorrect sequencing of principal diagnosis (e.g., respiratory failure vs. sepsis). The American Hospital Association has issued a regulatory advisory about these issues (web.mhanet.com/userdocs/articles/RAC/AHA_RAC_Coding Advisory_071608.pdf).
DeVault highlights three additional RAC targets that might impact HM:
- Documentation for transbronchial biopsy (a surgical DRG) in which the medical record only shows pathology of bronchus tissue (which RACs regard as nonsurgical);
- Failure to document the severity of a patient’s anemia as such to meet the medical necessity requirement of a blood transfusion (e.g., a chronic blood loss anemia or a pernicious anemia); and
- Documentation of treatments performed by intensivists in an ICU. By the time a patient’s attending physician sees their patient out of the ICU, DeVault says, their acute renal failure could be turned around but the attending might not document what happened in the ICU. The intensivist must see to it that the documentation allows the appropriate DRG assignment for the level of care the patient received.
AHIMA has published a 65-page RAC Audit Toolkit that describes the audit process, outlines preparations and procedures, and offers concrete guidance for appeals. Download a copy at www.ahima.org/infocenter/documents/RACToolkitFINAL.pdf. TH
Chris Guadagnino is a freelance medical writer based in Philadelphia.
Reference
- The Medicare Recovery Audit Contractor (RAC) program: an evaluation of the 3-year demonstration. CMS Web site. Available at: www.cms.hhs.gov/RAC/Downloads/RACEvaluationReport.pdf. Accessed March 3, 2010.
Massachusetts Update
Massachusetts Update
With the ongoing debate about healthcare reform, I’m curious to know how it worked out in Massachusetts. Didn’t they give everyone health insurance several years ago?
R. McCoy, MD
Birmingham, Ala.
Dr. Hospitalist responds: In 2006, Massachusetts legislators took the same approach to healthcare insurance as they do to auto insurance: require everyone to purchase a plan. If you can’t afford to purchase health insurance, the state provides you insurance through a state-subsidized plan. The state covers individuals earning up to 100% of the federal poverty level (FPL) and partially subsidizes coverage for those earning up to 300% of the FPL.
So how did Massachusetts come up with the money to pay for healthcare insurance for all of its residents? The state traditionally utilized money from a “free-care pool” to partially reimburse hospitals and community health centers for the care provided to indigents. The money in the free-care pool was generated from state and federal taxes, and from assessments on hospitals and healthcare insurance providers. With expanded insurance coverage, Massachusetts estimated that the cost of healthcare delivered to the uninsured would decrease, and the free-care pool could offset the remaining costs of insuring those below the FPL.
Starting in 2007, residents of Massachusetts were required to demonstrate proof of health insurance on their state income tax returns. The state levied penalties on those who failed to obtain coverage. The legislation also required insurers’ family plans to cover young adults up to age 25 or at least two years after they were no longer dependent on their parents. Additionally, businesses with 10 or more employees had to contribute a reasonable amount to their employees’ health insurance premiums or risk a financial penalty.
The Massachusetts health plan has produced both intended and unintended consequences. The plan was successful in its primary goal of insuring its citizens. By the end of 2008, 97% of Massachusetts’ residents were covered. But the system has not increased access to providers because of a shortage of primary-care physicians (PCPs). (Critics also point out that the plan has done nothing to increase the numbers of PCPs in the state.)
Another unexpected outcome is that healthcare costs have increased. The initial expectation was that increasing the percentage of insured individuals would lower overall costs. However, this has not been realized. In fact, the reallocation of funds from the free-care pool has birthed other problems. The state’s “safety net” hospitals—which traditionally have served urban, low-income populations—have experienced financial hardships.
These unexpected findings have not deterred Massachusetts from further efforts to address healthcare reform. In 2008, a special commission was charged with recommendations for a “common payment methodology” that would apply to both public and private payors. The goal is to slow the growth of healthcare costs without adversely affecting the quality of care.
The commission issued its recommendations in July 2009 (www.mass.gov). It suggested “Massachusetts has among the highest healthcare costs in the U.S. … and based on recent history, are projected to grow faster than for the U.S. as a whole.” In its report, the commission was critical of the present fee-for-service reimbursement model and stated that the model was the primary reason for escalating healthcare costs.
The commission noted the fee-for-service model rewards providers for providing more, but not better, care and also encourages providers to provide more-costly services without regard to evidence-based guidelines or a patient’s need. The commission recommended that “global payments with adjustments to reward provision of accessible and high-quality care become the predominant form of payment to providers in Massachusetts.” For the record, the legislature has not acted on the commission recommendations. TH
IMAGE SOURCE: AMANE KANEKO
Massachusetts Update
With the ongoing debate about healthcare reform, I’m curious to know how it worked out in Massachusetts. Didn’t they give everyone health insurance several years ago?
R. McCoy, MD
Birmingham, Ala.
Dr. Hospitalist responds: In 2006, Massachusetts legislators took the same approach to healthcare insurance as they do to auto insurance: require everyone to purchase a plan. If you can’t afford to purchase health insurance, the state provides you insurance through a state-subsidized plan. The state covers individuals earning up to 100% of the federal poverty level (FPL) and partially subsidizes coverage for those earning up to 300% of the FPL.
So how did Massachusetts come up with the money to pay for healthcare insurance for all of its residents? The state traditionally utilized money from a “free-care pool” to partially reimburse hospitals and community health centers for the care provided to indigents. The money in the free-care pool was generated from state and federal taxes, and from assessments on hospitals and healthcare insurance providers. With expanded insurance coverage, Massachusetts estimated that the cost of healthcare delivered to the uninsured would decrease, and the free-care pool could offset the remaining costs of insuring those below the FPL.
Starting in 2007, residents of Massachusetts were required to demonstrate proof of health insurance on their state income tax returns. The state levied penalties on those who failed to obtain coverage. The legislation also required insurers’ family plans to cover young adults up to age 25 or at least two years after they were no longer dependent on their parents. Additionally, businesses with 10 or more employees had to contribute a reasonable amount to their employees’ health insurance premiums or risk a financial penalty.
The Massachusetts health plan has produced both intended and unintended consequences. The plan was successful in its primary goal of insuring its citizens. By the end of 2008, 97% of Massachusetts’ residents were covered. But the system has not increased access to providers because of a shortage of primary-care physicians (PCPs). (Critics also point out that the plan has done nothing to increase the numbers of PCPs in the state.)
Another unexpected outcome is that healthcare costs have increased. The initial expectation was that increasing the percentage of insured individuals would lower overall costs. However, this has not been realized. In fact, the reallocation of funds from the free-care pool has birthed other problems. The state’s “safety net” hospitals—which traditionally have served urban, low-income populations—have experienced financial hardships.
These unexpected findings have not deterred Massachusetts from further efforts to address healthcare reform. In 2008, a special commission was charged with recommendations for a “common payment methodology” that would apply to both public and private payors. The goal is to slow the growth of healthcare costs without adversely affecting the quality of care.
The commission issued its recommendations in July 2009 (www.mass.gov). It suggested “Massachusetts has among the highest healthcare costs in the U.S. … and based on recent history, are projected to grow faster than for the U.S. as a whole.” In its report, the commission was critical of the present fee-for-service reimbursement model and stated that the model was the primary reason for escalating healthcare costs.
The commission noted the fee-for-service model rewards providers for providing more, but not better, care and also encourages providers to provide more-costly services without regard to evidence-based guidelines or a patient’s need. The commission recommended that “global payments with adjustments to reward provision of accessible and high-quality care become the predominant form of payment to providers in Massachusetts.” For the record, the legislature has not acted on the commission recommendations. TH
IMAGE SOURCE: AMANE KANEKO
Massachusetts Update
With the ongoing debate about healthcare reform, I’m curious to know how it worked out in Massachusetts. Didn’t they give everyone health insurance several years ago?
R. McCoy, MD
Birmingham, Ala.
Dr. Hospitalist responds: In 2006, Massachusetts legislators took the same approach to healthcare insurance as they do to auto insurance: require everyone to purchase a plan. If you can’t afford to purchase health insurance, the state provides you insurance through a state-subsidized plan. The state covers individuals earning up to 100% of the federal poverty level (FPL) and partially subsidizes coverage for those earning up to 300% of the FPL.
So how did Massachusetts come up with the money to pay for healthcare insurance for all of its residents? The state traditionally utilized money from a “free-care pool” to partially reimburse hospitals and community health centers for the care provided to indigents. The money in the free-care pool was generated from state and federal taxes, and from assessments on hospitals and healthcare insurance providers. With expanded insurance coverage, Massachusetts estimated that the cost of healthcare delivered to the uninsured would decrease, and the free-care pool could offset the remaining costs of insuring those below the FPL.
Starting in 2007, residents of Massachusetts were required to demonstrate proof of health insurance on their state income tax returns. The state levied penalties on those who failed to obtain coverage. The legislation also required insurers’ family plans to cover young adults up to age 25 or at least two years after they were no longer dependent on their parents. Additionally, businesses with 10 or more employees had to contribute a reasonable amount to their employees’ health insurance premiums or risk a financial penalty.
The Massachusetts health plan has produced both intended and unintended consequences. The plan was successful in its primary goal of insuring its citizens. By the end of 2008, 97% of Massachusetts’ residents were covered. But the system has not increased access to providers because of a shortage of primary-care physicians (PCPs). (Critics also point out that the plan has done nothing to increase the numbers of PCPs in the state.)
Another unexpected outcome is that healthcare costs have increased. The initial expectation was that increasing the percentage of insured individuals would lower overall costs. However, this has not been realized. In fact, the reallocation of funds from the free-care pool has birthed other problems. The state’s “safety net” hospitals—which traditionally have served urban, low-income populations—have experienced financial hardships.
These unexpected findings have not deterred Massachusetts from further efforts to address healthcare reform. In 2008, a special commission was charged with recommendations for a “common payment methodology” that would apply to both public and private payors. The goal is to slow the growth of healthcare costs without adversely affecting the quality of care.
The commission issued its recommendations in July 2009 (www.mass.gov). It suggested “Massachusetts has among the highest healthcare costs in the U.S. … and based on recent history, are projected to grow faster than for the U.S. as a whole.” In its report, the commission was critical of the present fee-for-service reimbursement model and stated that the model was the primary reason for escalating healthcare costs.
The commission noted the fee-for-service model rewards providers for providing more, but not better, care and also encourages providers to provide more-costly services without regard to evidence-based guidelines or a patient’s need. The commission recommended that “global payments with adjustments to reward provision of accessible and high-quality care become the predominant form of payment to providers in Massachusetts.” For the record, the legislature has not acted on the commission recommendations. TH
IMAGE SOURCE: AMANE KANEKO
Healthcare = Team Sport
While most of the focus has been on D.C. and the trillions of dollars to be spent on healthcare reform, HM has grown substantially in the last decade without any significant payment reform or new regulation. This is all the more incredible because the rise of HM has involved two institutions not synonymous with accepting or adapting to change: physicians and hospitals.
In the coming years, hospitals face important challenges, including their fiscal survival, public trust, workforce shortages, difficulty deciding whether their physicians are partners or competitors, and figuring out what to do about all this patient safety and performance improvement hubbub.
Although 2010’s version of healthcare reform will be about increasing access (see “An Imperfect Solution,” January 2010, p. 44), there are still the seeds planted to address the next two pillars of reform: reducing cost and rewarding performance. Together, they create the value proposition in healthcare. All this will make the coming decade one in which the hospital as an institution will need to evolve and adapt if it is to survive.
What is Quality?
As we enter a transitional phase, in some ways, we aren’t even clear on just what quality healthcare is:
- Is quality defined as a payment issue? We see this in discussions of not paying for “never events” or denying payment for readmissions.
- Is quality about being more satisfied? This is found in emphasis on the surveys of patient and family satisfaction that drive hospital CEO compensation and bonuses, as well as in efforts to improve staff retention or in recognition by business, insurers, and government.
- Is quality just checking things off on a clipboard? We all see the endless list of quality measures and increasing documentation that providers have told their patients to stop smoking or get a flu shot, but is that really the quality we are seeking in healthcare?
- Is quality just avoiding embarrassment? Is the best driver of performance improvement outraged hospital trustees wielding printouts comparing hospitals?
We do know that in some ways, the discussion at most of our hospitals has shifted from “Is quality important?” to “How do we do it?” And in this discussion, HM and SHM have taken a leading role in the “solutions” to the problem. Our innovative programs help reduce unnecessary DVTs, improve glycemic control, and refine the discharge process (see Project BOOST) for better patient/family satisfaction, reduced ED visits, and reduced readmissions.
New Ways to Deliver Care
The hospital of the future—I’m talking 2020—will not be defined by bricks and walls. The hospital stay will not end with a patient in a wheelchair being helped into their car. We already know that most patients don’t leave the hospital cured, but are discharged when they are not sick enough to need to stay recumbent in the most expensive hotel in the city. Often these patients are in midcourse of an acute illness, frequently imposed on top of chronic dysfunctions.
While the patient as the true “medical home” for their health and illness have always borne the potholes of slipped handoffs and information transfer deficits, hospitalists now have a clear view of the precarious nature of post-discharge care. Bundling and payment reform, designed to reward coordination of care and the reduction of readmissions to the ED, might be a revenue-driven boost to our ill-designed healthcare system, but the hospital, with the help of their hospitalists, can take the lead in fixing these problems. And we don’t have to wait for payment reform.
The good news is we aren’t alone in our efforts to change the culture, even the mission, of our hospitals. In a time of healthcarewide workforce shortages, there are increasing demands for direct inpatient care, coupled with the added time needed to document current performance and train and implement needed improvements. The only way to meet all of the volume and performance demands is with process change. We need a different way to deliver care to hospitalized patients.
All-Star Teams
High-performing organizations are composed of high-performance teams and a set of operating principles that create a widespread culture of motivated individuals who are focused on metrics, are execution-driven, and are committed to continual improvement and rapid adaptation.
The characteristics of high-performance teams are that they:
- Self-correct and reallocate resources;
- Have clear roles and responsibilities;
- Have clear, valued, and shared visions;
- Have strong team leadership;
- Develop a strong sense of “collective” trust and confidence; and
- Manage and optimize performance outcomes.
SHM has taken the lead at a national level in helping to organize the Hospital Care Collaborative (HCC), which is made up of CEOs and leaders in nursing, pharmacy, case management, social workers, and respiratory therapy. The HCC has published a set of “Common Principles” (see “Common Principles for the Hospital Care Collaborative”) and is planning to develop practical strategies for building high-performance teams at our nation’s hospitals.
SHM recently received support from Ortho-McNeil and has created a partnership with the American Hospital Association, American Organization of Nurse Executives, and American College of Physician Executives to develop principles and strategies to implement high-performance teams and to use this as a springboard to look at hospital care in the broadest sense (including transfers with medical home and accountable-care organizations). To start, SHM has convened a blue-ribbon group of hospital CMOs, CQOs, nursing executives, and other leaders in the hospital C-suite. Former SHM president Pat Cawley, MD, MBA, FHM, assistant professor and executive medical officer at the Medical University of South Carolina in Charleston, will chair this effort.
In these two initiatives, SHM and national hospital leaders are providing direction and innovation at two entry points—the C-suite and executive team—as well as on the front lines with the other healthcare professionals who care for our nation’s hospitalized patients.
More to Come
HM has had an interesting decade, growing to more than 30,000 hospitalists now practicing in 75% of our nation’s hospitals. We’ve taken on comanagement and are providing real success as change agents. But the decade to come will see the reinvention of our nation’s hospitals and distinct changes in workflow and responsibilities. We are moving from care based on the unit of the visit or the procedure to episodes of care. We are moving from a system that rewards just doing something to one that rewards doing the correct thing and doing it well. We are moving our hospitals from a swap meet where each physician has a booth and everyone supports those individual efforts to an institution with a culture that is patient-centered, based on quality measurement and performance, and provides care delivered by teams of health professionals working in concert.
This is a world that hospitalists can thrive in and, with your help and direction, SHM will provide the tools along the way. TH
Dr. Wellikson is CEO of SHM.
While most of the focus has been on D.C. and the trillions of dollars to be spent on healthcare reform, HM has grown substantially in the last decade without any significant payment reform or new regulation. This is all the more incredible because the rise of HM has involved two institutions not synonymous with accepting or adapting to change: physicians and hospitals.
In the coming years, hospitals face important challenges, including their fiscal survival, public trust, workforce shortages, difficulty deciding whether their physicians are partners or competitors, and figuring out what to do about all this patient safety and performance improvement hubbub.
Although 2010’s version of healthcare reform will be about increasing access (see “An Imperfect Solution,” January 2010, p. 44), there are still the seeds planted to address the next two pillars of reform: reducing cost and rewarding performance. Together, they create the value proposition in healthcare. All this will make the coming decade one in which the hospital as an institution will need to evolve and adapt if it is to survive.
What is Quality?
As we enter a transitional phase, in some ways, we aren’t even clear on just what quality healthcare is:
- Is quality defined as a payment issue? We see this in discussions of not paying for “never events” or denying payment for readmissions.
- Is quality about being more satisfied? This is found in emphasis on the surveys of patient and family satisfaction that drive hospital CEO compensation and bonuses, as well as in efforts to improve staff retention or in recognition by business, insurers, and government.
- Is quality just checking things off on a clipboard? We all see the endless list of quality measures and increasing documentation that providers have told their patients to stop smoking or get a flu shot, but is that really the quality we are seeking in healthcare?
- Is quality just avoiding embarrassment? Is the best driver of performance improvement outraged hospital trustees wielding printouts comparing hospitals?
We do know that in some ways, the discussion at most of our hospitals has shifted from “Is quality important?” to “How do we do it?” And in this discussion, HM and SHM have taken a leading role in the “solutions” to the problem. Our innovative programs help reduce unnecessary DVTs, improve glycemic control, and refine the discharge process (see Project BOOST) for better patient/family satisfaction, reduced ED visits, and reduced readmissions.
New Ways to Deliver Care
The hospital of the future—I’m talking 2020—will not be defined by bricks and walls. The hospital stay will not end with a patient in a wheelchair being helped into their car. We already know that most patients don’t leave the hospital cured, but are discharged when they are not sick enough to need to stay recumbent in the most expensive hotel in the city. Often these patients are in midcourse of an acute illness, frequently imposed on top of chronic dysfunctions.
While the patient as the true “medical home” for their health and illness have always borne the potholes of slipped handoffs and information transfer deficits, hospitalists now have a clear view of the precarious nature of post-discharge care. Bundling and payment reform, designed to reward coordination of care and the reduction of readmissions to the ED, might be a revenue-driven boost to our ill-designed healthcare system, but the hospital, with the help of their hospitalists, can take the lead in fixing these problems. And we don’t have to wait for payment reform.
The good news is we aren’t alone in our efforts to change the culture, even the mission, of our hospitals. In a time of healthcarewide workforce shortages, there are increasing demands for direct inpatient care, coupled with the added time needed to document current performance and train and implement needed improvements. The only way to meet all of the volume and performance demands is with process change. We need a different way to deliver care to hospitalized patients.
All-Star Teams
High-performing organizations are composed of high-performance teams and a set of operating principles that create a widespread culture of motivated individuals who are focused on metrics, are execution-driven, and are committed to continual improvement and rapid adaptation.
The characteristics of high-performance teams are that they:
- Self-correct and reallocate resources;
- Have clear roles and responsibilities;
- Have clear, valued, and shared visions;
- Have strong team leadership;
- Develop a strong sense of “collective” trust and confidence; and
- Manage and optimize performance outcomes.
SHM has taken the lead at a national level in helping to organize the Hospital Care Collaborative (HCC), which is made up of CEOs and leaders in nursing, pharmacy, case management, social workers, and respiratory therapy. The HCC has published a set of “Common Principles” (see “Common Principles for the Hospital Care Collaborative”) and is planning to develop practical strategies for building high-performance teams at our nation’s hospitals.
SHM recently received support from Ortho-McNeil and has created a partnership with the American Hospital Association, American Organization of Nurse Executives, and American College of Physician Executives to develop principles and strategies to implement high-performance teams and to use this as a springboard to look at hospital care in the broadest sense (including transfers with medical home and accountable-care organizations). To start, SHM has convened a blue-ribbon group of hospital CMOs, CQOs, nursing executives, and other leaders in the hospital C-suite. Former SHM president Pat Cawley, MD, MBA, FHM, assistant professor and executive medical officer at the Medical University of South Carolina in Charleston, will chair this effort.
In these two initiatives, SHM and national hospital leaders are providing direction and innovation at two entry points—the C-suite and executive team—as well as on the front lines with the other healthcare professionals who care for our nation’s hospitalized patients.
More to Come
HM has had an interesting decade, growing to more than 30,000 hospitalists now practicing in 75% of our nation’s hospitals. We’ve taken on comanagement and are providing real success as change agents. But the decade to come will see the reinvention of our nation’s hospitals and distinct changes in workflow and responsibilities. We are moving from care based on the unit of the visit or the procedure to episodes of care. We are moving from a system that rewards just doing something to one that rewards doing the correct thing and doing it well. We are moving our hospitals from a swap meet where each physician has a booth and everyone supports those individual efforts to an institution with a culture that is patient-centered, based on quality measurement and performance, and provides care delivered by teams of health professionals working in concert.
This is a world that hospitalists can thrive in and, with your help and direction, SHM will provide the tools along the way. TH
Dr. Wellikson is CEO of SHM.
While most of the focus has been on D.C. and the trillions of dollars to be spent on healthcare reform, HM has grown substantially in the last decade without any significant payment reform or new regulation. This is all the more incredible because the rise of HM has involved two institutions not synonymous with accepting or adapting to change: physicians and hospitals.
In the coming years, hospitals face important challenges, including their fiscal survival, public trust, workforce shortages, difficulty deciding whether their physicians are partners or competitors, and figuring out what to do about all this patient safety and performance improvement hubbub.
Although 2010’s version of healthcare reform will be about increasing access (see “An Imperfect Solution,” January 2010, p. 44), there are still the seeds planted to address the next two pillars of reform: reducing cost and rewarding performance. Together, they create the value proposition in healthcare. All this will make the coming decade one in which the hospital as an institution will need to evolve and adapt if it is to survive.
What is Quality?
As we enter a transitional phase, in some ways, we aren’t even clear on just what quality healthcare is:
- Is quality defined as a payment issue? We see this in discussions of not paying for “never events” or denying payment for readmissions.
- Is quality about being more satisfied? This is found in emphasis on the surveys of patient and family satisfaction that drive hospital CEO compensation and bonuses, as well as in efforts to improve staff retention or in recognition by business, insurers, and government.
- Is quality just checking things off on a clipboard? We all see the endless list of quality measures and increasing documentation that providers have told their patients to stop smoking or get a flu shot, but is that really the quality we are seeking in healthcare?
- Is quality just avoiding embarrassment? Is the best driver of performance improvement outraged hospital trustees wielding printouts comparing hospitals?
We do know that in some ways, the discussion at most of our hospitals has shifted from “Is quality important?” to “How do we do it?” And in this discussion, HM and SHM have taken a leading role in the “solutions” to the problem. Our innovative programs help reduce unnecessary DVTs, improve glycemic control, and refine the discharge process (see Project BOOST) for better patient/family satisfaction, reduced ED visits, and reduced readmissions.
New Ways to Deliver Care
The hospital of the future—I’m talking 2020—will not be defined by bricks and walls. The hospital stay will not end with a patient in a wheelchair being helped into their car. We already know that most patients don’t leave the hospital cured, but are discharged when they are not sick enough to need to stay recumbent in the most expensive hotel in the city. Often these patients are in midcourse of an acute illness, frequently imposed on top of chronic dysfunctions.
While the patient as the true “medical home” for their health and illness have always borne the potholes of slipped handoffs and information transfer deficits, hospitalists now have a clear view of the precarious nature of post-discharge care. Bundling and payment reform, designed to reward coordination of care and the reduction of readmissions to the ED, might be a revenue-driven boost to our ill-designed healthcare system, but the hospital, with the help of their hospitalists, can take the lead in fixing these problems. And we don’t have to wait for payment reform.
The good news is we aren’t alone in our efforts to change the culture, even the mission, of our hospitals. In a time of healthcarewide workforce shortages, there are increasing demands for direct inpatient care, coupled with the added time needed to document current performance and train and implement needed improvements. The only way to meet all of the volume and performance demands is with process change. We need a different way to deliver care to hospitalized patients.
All-Star Teams
High-performing organizations are composed of high-performance teams and a set of operating principles that create a widespread culture of motivated individuals who are focused on metrics, are execution-driven, and are committed to continual improvement and rapid adaptation.
The characteristics of high-performance teams are that they:
- Self-correct and reallocate resources;
- Have clear roles and responsibilities;
- Have clear, valued, and shared visions;
- Have strong team leadership;
- Develop a strong sense of “collective” trust and confidence; and
- Manage and optimize performance outcomes.
SHM has taken the lead at a national level in helping to organize the Hospital Care Collaborative (HCC), which is made up of CEOs and leaders in nursing, pharmacy, case management, social workers, and respiratory therapy. The HCC has published a set of “Common Principles” (see “Common Principles for the Hospital Care Collaborative”) and is planning to develop practical strategies for building high-performance teams at our nation’s hospitals.
SHM recently received support from Ortho-McNeil and has created a partnership with the American Hospital Association, American Organization of Nurse Executives, and American College of Physician Executives to develop principles and strategies to implement high-performance teams and to use this as a springboard to look at hospital care in the broadest sense (including transfers with medical home and accountable-care organizations). To start, SHM has convened a blue-ribbon group of hospital CMOs, CQOs, nursing executives, and other leaders in the hospital C-suite. Former SHM president Pat Cawley, MD, MBA, FHM, assistant professor and executive medical officer at the Medical University of South Carolina in Charleston, will chair this effort.
In these two initiatives, SHM and national hospital leaders are providing direction and innovation at two entry points—the C-suite and executive team—as well as on the front lines with the other healthcare professionals who care for our nation’s hospitalized patients.
More to Come
HM has had an interesting decade, growing to more than 30,000 hospitalists now practicing in 75% of our nation’s hospitals. We’ve taken on comanagement and are providing real success as change agents. But the decade to come will see the reinvention of our nation’s hospitals and distinct changes in workflow and responsibilities. We are moving from care based on the unit of the visit or the procedure to episodes of care. We are moving from a system that rewards just doing something to one that rewards doing the correct thing and doing it well. We are moving our hospitals from a swap meet where each physician has a booth and everyone supports those individual efforts to an institution with a culture that is patient-centered, based on quality measurement and performance, and provides care delivered by teams of health professionals working in concert.
This is a world that hospitalists can thrive in and, with your help and direction, SHM will provide the tools along the way. TH
Dr. Wellikson is CEO of SHM.
Patient Privacy Upgrade
Just when you thought you had heard the last about the Health Insurance Portability and Accountability Act (HIPAA), the Department of Health and Human Services (HHS) has promulgated new rules for notifying individuals when their protected health information has been breached. These “breach notification” regulations implement provisions of the Health Information Technology for Economic and Clinical Health (HITECH) Act, passed as part of the American Recovery and Reinvestment Act (ARRA) of 2009. The regulations became effective in September.
The regulations require covered entities (health plans, healthcare clearing houses, and healthcare providers) to promptly notify individuals affected by a breach, as well as the HHS secretary and the media in cases in which a breach affects more than 500 individuals. Breaches affecting fewer than 500 individuals must be reported to HHS annually. Notably, breaches will be posted on the HHS Web site. The regulations also require business associates to notify covered entities with whom they work of breaches.
All Breaches Not Equal
Any impermissible acquisition, access, use, or disclosure of unsecured protected health information that compromises the security or privacy of the information triggers the new breach notification requirement. Health information is unsecured only if it is not encrypted or destroyed. Security or privacy is compromised when a breach poses a significant risk of financial, reputational, or other harm. To determine whether a significant risk of harm exists, a covered entity must document a fact-based assessment of the risk involved, including evaluation of:
- What happened to the information (e.g., Was a laptop stolen and never recovered or lost but subsequently found? Was an unauthorized access intentional or accidental?);
- The nature of the information (e.g., Did the information contain Social Security numbers and other data that could lead to identity theft? Did the information involve sensitive health information?);
- Steps that could mitigate the potential harm (e.g., call the recipient and request destruction of the information and confirmation); and
- The number of individual identifiers present in the information (e.g., Did the information have name, birth date, and Social Security number, or only a medical record number?).
Consequently, breaches that do not involve information that can be used to identify a specific individual are not reportable. Moreover, inadvertent breaches to other covered entities pose a low risk of harm. For example, if medical records are inadvertently faxed to the wrong pharmacy or other healthcare provider, there is low risk of harm because the recipient is independently required to comply with HIPAA.
Additionally, the regulations expressly exclude the following events from the definition of a breach:
- Unintentional, good-faith access by an employee or agent if the information has not been redisclosed. An example would be mail sent to or opened by the wrong staff member;
- Inadvertent disclosures among persons otherwise authorized to access protected health information within the same entity, provided the information is not redisclosed; and
- When an unauthorized recipient could not have retained the information (e.g., paperwork given to the wrong patient but returned immediately without being read).
In each of the examples above, a covered entity does not need to provide breach notification because a breach has not occurred under the regulations.
Notification Requirements
Unless law enforcement makes a written request for a covered entity to delay notification, covered entities must provide written notice to each individual affected by a breach as soon as possible but no later than 60 calendar days from discovery of the breach. Importantly, a covered entity is liable for appropriate notification if they know, or should know, of a breach. Moreover, the knowledge of an employee is imputed to an employer. Further, business associates must notify covered entities of any breaches. Thus, policies and procedures should include training of a covered entity’s workforce and ensuring business associates’ compliance.
While there is not a prescribed form for notice, the regulations do require some specific elements, including:
- Description of the breach and the dates, if known;
- Description of the protected health information involved;
- Steps the affected individual should take to protect themselves (e.g., cancel credit cards);
- Description of the steps being taken by the covered entity; and
- Contact information to obtain more information, which must include a toll-free telephone number, e-mail or postal address, or Web site.
If 10 or more individuals are involved for which the entity does not have adequate contact information, notice can be accomplished by a conspicuous posting on the entity’s Web site for at least 90 days, or a posting in print or broadcast media. In either case, an active toll-free telephone number where individuals can find out if they were affected must be available for 90 days.
If a breach involves more than 500 people from any one state, notification must include prominent media outlets. Moreover, the covered entity must notify the HHS secretary at the time notice is provided to affected individuals. Breaches involving fewer than 500 individuals must be reported annually through the Office of Civil Rights Web site.
Sanctions and Penalties
HHS is required to audit, investigate, and impose civil monetary penalties for offenses resulting from willful neglect. Fortunately, HHS has indicated that it will not be imposing sanctions for unintentional violations of the notification requirements until March. This gives providers some time to implement the necessary processes. Nonetheless, it is important to implement compliance processes now, as the penalties for noncompliance can be severe. Under the new law, penalties are tiered based on knowledge, and are capped at $1.5 million annually.
For more information about HIPAA, visit www.hhs.gov/ocr/privacy. TH
Patrick T. O’Rourke works in the Office of University Counsel at the University of Colorado Denver. Kari Hershey is a public relations consultant with Budman & Hershey, LLC, in Denver.
Just when you thought you had heard the last about the Health Insurance Portability and Accountability Act (HIPAA), the Department of Health and Human Services (HHS) has promulgated new rules for notifying individuals when their protected health information has been breached. These “breach notification” regulations implement provisions of the Health Information Technology for Economic and Clinical Health (HITECH) Act, passed as part of the American Recovery and Reinvestment Act (ARRA) of 2009. The regulations became effective in September.
The regulations require covered entities (health plans, healthcare clearing houses, and healthcare providers) to promptly notify individuals affected by a breach, as well as the HHS secretary and the media in cases in which a breach affects more than 500 individuals. Breaches affecting fewer than 500 individuals must be reported to HHS annually. Notably, breaches will be posted on the HHS Web site. The regulations also require business associates to notify covered entities with whom they work of breaches.
All Breaches Not Equal
Any impermissible acquisition, access, use, or disclosure of unsecured protected health information that compromises the security or privacy of the information triggers the new breach notification requirement. Health information is unsecured only if it is not encrypted or destroyed. Security or privacy is compromised when a breach poses a significant risk of financial, reputational, or other harm. To determine whether a significant risk of harm exists, a covered entity must document a fact-based assessment of the risk involved, including evaluation of:
- What happened to the information (e.g., Was a laptop stolen and never recovered or lost but subsequently found? Was an unauthorized access intentional or accidental?);
- The nature of the information (e.g., Did the information contain Social Security numbers and other data that could lead to identity theft? Did the information involve sensitive health information?);
- Steps that could mitigate the potential harm (e.g., call the recipient and request destruction of the information and confirmation); and
- The number of individual identifiers present in the information (e.g., Did the information have name, birth date, and Social Security number, or only a medical record number?).
Consequently, breaches that do not involve information that can be used to identify a specific individual are not reportable. Moreover, inadvertent breaches to other covered entities pose a low risk of harm. For example, if medical records are inadvertently faxed to the wrong pharmacy or other healthcare provider, there is low risk of harm because the recipient is independently required to comply with HIPAA.
Additionally, the regulations expressly exclude the following events from the definition of a breach:
- Unintentional, good-faith access by an employee or agent if the information has not been redisclosed. An example would be mail sent to or opened by the wrong staff member;
- Inadvertent disclosures among persons otherwise authorized to access protected health information within the same entity, provided the information is not redisclosed; and
- When an unauthorized recipient could not have retained the information (e.g., paperwork given to the wrong patient but returned immediately without being read).
In each of the examples above, a covered entity does not need to provide breach notification because a breach has not occurred under the regulations.
Notification Requirements
Unless law enforcement makes a written request for a covered entity to delay notification, covered entities must provide written notice to each individual affected by a breach as soon as possible but no later than 60 calendar days from discovery of the breach. Importantly, a covered entity is liable for appropriate notification if they know, or should know, of a breach. Moreover, the knowledge of an employee is imputed to an employer. Further, business associates must notify covered entities of any breaches. Thus, policies and procedures should include training of a covered entity’s workforce and ensuring business associates’ compliance.
While there is not a prescribed form for notice, the regulations do require some specific elements, including:
- Description of the breach and the dates, if known;
- Description of the protected health information involved;
- Steps the affected individual should take to protect themselves (e.g., cancel credit cards);
- Description of the steps being taken by the covered entity; and
- Contact information to obtain more information, which must include a toll-free telephone number, e-mail or postal address, or Web site.
If 10 or more individuals are involved for which the entity does not have adequate contact information, notice can be accomplished by a conspicuous posting on the entity’s Web site for at least 90 days, or a posting in print or broadcast media. In either case, an active toll-free telephone number where individuals can find out if they were affected must be available for 90 days.
If a breach involves more than 500 people from any one state, notification must include prominent media outlets. Moreover, the covered entity must notify the HHS secretary at the time notice is provided to affected individuals. Breaches involving fewer than 500 individuals must be reported annually through the Office of Civil Rights Web site.
Sanctions and Penalties
HHS is required to audit, investigate, and impose civil monetary penalties for offenses resulting from willful neglect. Fortunately, HHS has indicated that it will not be imposing sanctions for unintentional violations of the notification requirements until March. This gives providers some time to implement the necessary processes. Nonetheless, it is important to implement compliance processes now, as the penalties for noncompliance can be severe. Under the new law, penalties are tiered based on knowledge, and are capped at $1.5 million annually.
For more information about HIPAA, visit www.hhs.gov/ocr/privacy. TH
Patrick T. O’Rourke works in the Office of University Counsel at the University of Colorado Denver. Kari Hershey is a public relations consultant with Budman & Hershey, LLC, in Denver.
Just when you thought you had heard the last about the Health Insurance Portability and Accountability Act (HIPAA), the Department of Health and Human Services (HHS) has promulgated new rules for notifying individuals when their protected health information has been breached. These “breach notification” regulations implement provisions of the Health Information Technology for Economic and Clinical Health (HITECH) Act, passed as part of the American Recovery and Reinvestment Act (ARRA) of 2009. The regulations became effective in September.
The regulations require covered entities (health plans, healthcare clearing houses, and healthcare providers) to promptly notify individuals affected by a breach, as well as the HHS secretary and the media in cases in which a breach affects more than 500 individuals. Breaches affecting fewer than 500 individuals must be reported to HHS annually. Notably, breaches will be posted on the HHS Web site. The regulations also require business associates to notify covered entities with whom they work of breaches.
All Breaches Not Equal
Any impermissible acquisition, access, use, or disclosure of unsecured protected health information that compromises the security or privacy of the information triggers the new breach notification requirement. Health information is unsecured only if it is not encrypted or destroyed. Security or privacy is compromised when a breach poses a significant risk of financial, reputational, or other harm. To determine whether a significant risk of harm exists, a covered entity must document a fact-based assessment of the risk involved, including evaluation of:
- What happened to the information (e.g., Was a laptop stolen and never recovered or lost but subsequently found? Was an unauthorized access intentional or accidental?);
- The nature of the information (e.g., Did the information contain Social Security numbers and other data that could lead to identity theft? Did the information involve sensitive health information?);
- Steps that could mitigate the potential harm (e.g., call the recipient and request destruction of the information and confirmation); and
- The number of individual identifiers present in the information (e.g., Did the information have name, birth date, and Social Security number, or only a medical record number?).
Consequently, breaches that do not involve information that can be used to identify a specific individual are not reportable. Moreover, inadvertent breaches to other covered entities pose a low risk of harm. For example, if medical records are inadvertently faxed to the wrong pharmacy or other healthcare provider, there is low risk of harm because the recipient is independently required to comply with HIPAA.
Additionally, the regulations expressly exclude the following events from the definition of a breach:
- Unintentional, good-faith access by an employee or agent if the information has not been redisclosed. An example would be mail sent to or opened by the wrong staff member;
- Inadvertent disclosures among persons otherwise authorized to access protected health information within the same entity, provided the information is not redisclosed; and
- When an unauthorized recipient could not have retained the information (e.g., paperwork given to the wrong patient but returned immediately without being read).
In each of the examples above, a covered entity does not need to provide breach notification because a breach has not occurred under the regulations.
Notification Requirements
Unless law enforcement makes a written request for a covered entity to delay notification, covered entities must provide written notice to each individual affected by a breach as soon as possible but no later than 60 calendar days from discovery of the breach. Importantly, a covered entity is liable for appropriate notification if they know, or should know, of a breach. Moreover, the knowledge of an employee is imputed to an employer. Further, business associates must notify covered entities of any breaches. Thus, policies and procedures should include training of a covered entity’s workforce and ensuring business associates’ compliance.
While there is not a prescribed form for notice, the regulations do require some specific elements, including:
- Description of the breach and the dates, if known;
- Description of the protected health information involved;
- Steps the affected individual should take to protect themselves (e.g., cancel credit cards);
- Description of the steps being taken by the covered entity; and
- Contact information to obtain more information, which must include a toll-free telephone number, e-mail or postal address, or Web site.
If 10 or more individuals are involved for which the entity does not have adequate contact information, notice can be accomplished by a conspicuous posting on the entity’s Web site for at least 90 days, or a posting in print or broadcast media. In either case, an active toll-free telephone number where individuals can find out if they were affected must be available for 90 days.
If a breach involves more than 500 people from any one state, notification must include prominent media outlets. Moreover, the covered entity must notify the HHS secretary at the time notice is provided to affected individuals. Breaches involving fewer than 500 individuals must be reported annually through the Office of Civil Rights Web site.
Sanctions and Penalties
HHS is required to audit, investigate, and impose civil monetary penalties for offenses resulting from willful neglect. Fortunately, HHS has indicated that it will not be imposing sanctions for unintentional violations of the notification requirements until March. This gives providers some time to implement the necessary processes. Nonetheless, it is important to implement compliance processes now, as the penalties for noncompliance can be severe. Under the new law, penalties are tiered based on knowledge, and are capped at $1.5 million annually.
For more information about HIPAA, visit www.hhs.gov/ocr/privacy. TH
Patrick T. O’Rourke works in the Office of University Counsel at the University of Colorado Denver. Kari Hershey is a public relations consultant with Budman & Hershey, LLC, in Denver.