User login
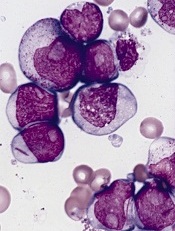
Minimal residual disease could signify worse outcomes in acute myeloid leukemia treatment
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
Although peripheral count recovery and minimal residual disease level following induction therapy are linked, each is an independent prognostic factor for relapse and overall survival in patients with acute myeloid leukemia, investigators say in a report published online March 2 in Journal of Clinical Oncology. “Information about these post-treatment factors is likely more important than information about several traditional pretreatment prognostic factors and should play a major – and perhaps the dominant – role in planning postinduction therapy,” wrote Dr. Xueyan Chen and her associates.
The investigators retrospectively analyzed data from 245 adults with newly diagnosed, relapsed, or refractory acute myeloid leukemia (AML) who achieved either complete remission (CR), complete remission with incomplete platelet recovery (CRp), or complete remission with incomplete blood count recovery (CRi), after induction therapy. The 71% of patients who achieved CR had minimal residual disease (MRD) less frequently and had lower levels of MRD than the 19.6% of patients achieving CRp and 9.4% achieving CRi, suggesting that failure of blood count recovery may result from inadequate treatment of AML.
Read the entire article here: http://jco.ascopubs.org/content/early/2015/02/26/JCO.2014.58.3518
FDA puts drug on fast track to treat secondary AML

The US Food and Drug Administration (FDA) has granted fast track designation for CPX-351, a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle, to treat elderly patients with secondary acute myeloid leukemia (AML).
In a phase 2 study of elderly AML patients, there was no significant difference in response or survival rates between patients who received CPX-351 and those who received cytarabine and daunorubicin.
However, CPX-351 conferred a significant response benefit among patients with poor cytogenetics and a significant survival benefit in patients with secondary AML.
“We are pleased that FDA has granted fast track status for CPX-351 for the treatment of elderly patients with secondary AML,” said Scott Jackson, Chief Executive Officer of Celator Pharmaceuticals, the company developing CPX-351.
“Our ongoing phase 3 study in these patients has completed enrollment, and we expect induction response rate data to be available in the second quarter of this year, and to have overall survival data, the primary endpoint of the study, in the first quarter of 2016.”
“If our phase 3 study comparing CPX-351 to the current standard of care is successful, the fast track designation may provide an added benefit of facilitating the [new drug application] review process.”
The FDA established the fast track designation process to expedite the review of drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation allows a drug’s developer to submit sections of a new drug application (NDA) on a rolling basis, so the FDA can review portions of the NDA as they are received instead of waiting for the entire NDA submission. A fast-track-designated product could be eligible for priority review if supported by clinical data at the time of NDA submission.
Phase 2 trial
In an article published in Blood last April, researchers reported results with CPX-351 in elderly patients with newly diagnosed AML. The study enrolled 126 patients who were 60 to 75 years of age.
They were randomized to receive CPX-351 (n=85) or “control” treatment consisting of cytarabine and daunorubicin (n=41). The treatment groups were well-balanced for disease and patient characteristics at baseline.
Overall, the response rate was 66.7% in the CPX-351 arm and 51.2% in the control arm (P=0.07). Among patients with adverse cytogenetics, the response rates were 77.3% and 38.5%, respectively (P=0.03). And among patients with secondary AML, response rates were 57.6% and 31.6%, respectively (P=0.06).
The median overall survival was 14.7 months in the CPX-351 arm and 12.9 months in the control arm. The median event-free survival was 6.5 months and 2.0 months, respectively. These differences were not statistically significant.
However, secondary AML patients treated with CPX-351 had significantly better overall survival than secondary AML patients in the control arm. The median overall survival was 12.1 months and 6.1 months, respectively (P=0.01). The median event-free survival was 4.5 months and 1.3 months, respectively (P=0.08).
Common adverse events included febrile neutropenia, infection, rash, diarrhea, nausea, edema, and constipation. There were minimal differences between the treatment arms in the incidence of these events.
The median time to neutrophil recovery was longer in the CPX-351 arm than in the control arm—36 days and 32 days, respectively. And the same was true for platelet recovery—37 days and 28 days, respectively.
Patients in the CPX-351 arm had a higher incidence of grade 3-4 infection than controls—70.6% and 43.9%, respectively—but not infection-related deaths—3.5% and 7.3%, respectively.
By day 60, 4.7% of patients in the CPX-351 arm and 14.6% of patients in the control arm had died. All of these deaths occurred in high-risk patients, particularly those with secondary AML. ![]()

The US Food and Drug Administration (FDA) has granted fast track designation for CPX-351, a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle, to treat elderly patients with secondary acute myeloid leukemia (AML).
In a phase 2 study of elderly AML patients, there was no significant difference in response or survival rates between patients who received CPX-351 and those who received cytarabine and daunorubicin.
However, CPX-351 conferred a significant response benefit among patients with poor cytogenetics and a significant survival benefit in patients with secondary AML.
“We are pleased that FDA has granted fast track status for CPX-351 for the treatment of elderly patients with secondary AML,” said Scott Jackson, Chief Executive Officer of Celator Pharmaceuticals, the company developing CPX-351.
“Our ongoing phase 3 study in these patients has completed enrollment, and we expect induction response rate data to be available in the second quarter of this year, and to have overall survival data, the primary endpoint of the study, in the first quarter of 2016.”
“If our phase 3 study comparing CPX-351 to the current standard of care is successful, the fast track designation may provide an added benefit of facilitating the [new drug application] review process.”
The FDA established the fast track designation process to expedite the review of drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation allows a drug’s developer to submit sections of a new drug application (NDA) on a rolling basis, so the FDA can review portions of the NDA as they are received instead of waiting for the entire NDA submission. A fast-track-designated product could be eligible for priority review if supported by clinical data at the time of NDA submission.
Phase 2 trial
In an article published in Blood last April, researchers reported results with CPX-351 in elderly patients with newly diagnosed AML. The study enrolled 126 patients who were 60 to 75 years of age.
They were randomized to receive CPX-351 (n=85) or “control” treatment consisting of cytarabine and daunorubicin (n=41). The treatment groups were well-balanced for disease and patient characteristics at baseline.
Overall, the response rate was 66.7% in the CPX-351 arm and 51.2% in the control arm (P=0.07). Among patients with adverse cytogenetics, the response rates were 77.3% and 38.5%, respectively (P=0.03). And among patients with secondary AML, response rates were 57.6% and 31.6%, respectively (P=0.06).
The median overall survival was 14.7 months in the CPX-351 arm and 12.9 months in the control arm. The median event-free survival was 6.5 months and 2.0 months, respectively. These differences were not statistically significant.
However, secondary AML patients treated with CPX-351 had significantly better overall survival than secondary AML patients in the control arm. The median overall survival was 12.1 months and 6.1 months, respectively (P=0.01). The median event-free survival was 4.5 months and 1.3 months, respectively (P=0.08).
Common adverse events included febrile neutropenia, infection, rash, diarrhea, nausea, edema, and constipation. There were minimal differences between the treatment arms in the incidence of these events.
The median time to neutrophil recovery was longer in the CPX-351 arm than in the control arm—36 days and 32 days, respectively. And the same was true for platelet recovery—37 days and 28 days, respectively.
Patients in the CPX-351 arm had a higher incidence of grade 3-4 infection than controls—70.6% and 43.9%, respectively—but not infection-related deaths—3.5% and 7.3%, respectively.
By day 60, 4.7% of patients in the CPX-351 arm and 14.6% of patients in the control arm had died. All of these deaths occurred in high-risk patients, particularly those with secondary AML. ![]()

The US Food and Drug Administration (FDA) has granted fast track designation for CPX-351, a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle, to treat elderly patients with secondary acute myeloid leukemia (AML).
In a phase 2 study of elderly AML patients, there was no significant difference in response or survival rates between patients who received CPX-351 and those who received cytarabine and daunorubicin.
However, CPX-351 conferred a significant response benefit among patients with poor cytogenetics and a significant survival benefit in patients with secondary AML.
“We are pleased that FDA has granted fast track status for CPX-351 for the treatment of elderly patients with secondary AML,” said Scott Jackson, Chief Executive Officer of Celator Pharmaceuticals, the company developing CPX-351.
“Our ongoing phase 3 study in these patients has completed enrollment, and we expect induction response rate data to be available in the second quarter of this year, and to have overall survival data, the primary endpoint of the study, in the first quarter of 2016.”
“If our phase 3 study comparing CPX-351 to the current standard of care is successful, the fast track designation may provide an added benefit of facilitating the [new drug application] review process.”
The FDA established the fast track designation process to expedite the review of drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation allows a drug’s developer to submit sections of a new drug application (NDA) on a rolling basis, so the FDA can review portions of the NDA as they are received instead of waiting for the entire NDA submission. A fast-track-designated product could be eligible for priority review if supported by clinical data at the time of NDA submission.
Phase 2 trial
In an article published in Blood last April, researchers reported results with CPX-351 in elderly patients with newly diagnosed AML. The study enrolled 126 patients who were 60 to 75 years of age.
They were randomized to receive CPX-351 (n=85) or “control” treatment consisting of cytarabine and daunorubicin (n=41). The treatment groups were well-balanced for disease and patient characteristics at baseline.
Overall, the response rate was 66.7% in the CPX-351 arm and 51.2% in the control arm (P=0.07). Among patients with adverse cytogenetics, the response rates were 77.3% and 38.5%, respectively (P=0.03). And among patients with secondary AML, response rates were 57.6% and 31.6%, respectively (P=0.06).
The median overall survival was 14.7 months in the CPX-351 arm and 12.9 months in the control arm. The median event-free survival was 6.5 months and 2.0 months, respectively. These differences were not statistically significant.
However, secondary AML patients treated with CPX-351 had significantly better overall survival than secondary AML patients in the control arm. The median overall survival was 12.1 months and 6.1 months, respectively (P=0.01). The median event-free survival was 4.5 months and 1.3 months, respectively (P=0.08).
Common adverse events included febrile neutropenia, infection, rash, diarrhea, nausea, edema, and constipation. There were minimal differences between the treatment arms in the incidence of these events.
The median time to neutrophil recovery was longer in the CPX-351 arm than in the control arm—36 days and 32 days, respectively. And the same was true for platelet recovery—37 days and 28 days, respectively.
Patients in the CPX-351 arm had a higher incidence of grade 3-4 infection than controls—70.6% and 43.9%, respectively—but not infection-related deaths—3.5% and 7.3%, respectively.
By day 60, 4.7% of patients in the CPX-351 arm and 14.6% of patients in the control arm had died. All of these deaths occurred in high-risk patients, particularly those with secondary AML. ![]()
Drug can increase survival in poor-risk AML

In a phase 2 trial, an investigational drug conferred a significant improvement in survival when used as salvage therapy in poor-risk patients with acute myeloid leukemia (AML).
On the other hand, the drug did not provide any significant improvements over control treatment (investigator’s choice) in the entire population of AML patients in first relapse.
The drug, CPX-351, is a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle.
Researchers reported these results with CPX-351 in Cancer. The study was funded by Celator Pharmaceuticals, the company developing CPX-351, and the Leukemia and Lymphoma Society.
“Patients with first-relapse AML have generally a poor prognosis, with a limited likelihood of response following salvage treatment,” said study author Jorge Cortes, MD, of the MD Anderson Cancer Center in Houston, Texas.
“This is particularly true for patients classified by the EPI [European Prognostic Index] as poor-risk upon entering the trial.”
For this trial, Dr Cortes and his colleagues evaluated 125 patients, ages 18 to 65, from 35 centers in the US, Canada, and Europe. Patients had AML in first relapse after an initial complete remission lasting a month or longer.
They were stratified per the EPI into favorable-, intermediate-, and poor-risk groups based on the duration of their first complete remission, cytogenetics, age, and transplant history. Most patients (68%) were in the poor-risk group.
Patients were randomized 2:1 to receive CPX-351 (100 units/m2 on days 1, 3, and 5 by 90-minute infusion) or the investigators’ choice of first salvage chemotherapy. The control treatment was usually based on cytarabine and an anthracycline, often with one or more additional agents.
Patient characteristics were largely well-balanced between the treatment arms. However, the CPX-351 group had a younger median age (52 years vs 56 years), more patients with secondary AML (12.3% vs 6.8%), and a higher rate of prior transplant (27.2% vs 15.9%).
Response and survival
Response rates were higher in the CPX-351 arm than in the control arm. The rates of complete response were 37% and 31.8%, respectively. And the rates of complete response with incomplete count recovery were 12.3% and 9.1%, respectively.
However, there was no significant difference in event-free survival (EFS) or overall survival (OS) between the treatment arms.
The median EFS was 4 months in the CPX-351 arm and 1.4 months in the control arm (hazard ratio[HR]=0.66, P=0.08). And the median OS was 8.5 months and 6.3 months, respectively (HR=0.75, P=0.19).
In the poor-risk population, there was no significant improvement in EFS with CPX-351, but there was a significant improvement in OS.
The median EFS was 1.8 months in the CPX-351 arm and 1.2 months in the control arm (HR=0.63, P=0.08). And the median OS was 6.5 months and 4.2 months, respectively (HR=0.55, P=0.02).
Safety and early mortality
The early mortality rate was similar between the treatment arms at 30 days—7.4% in the CPX-351 arm and 4.5% in the control arm—and at 60 days—14.8% and 15.9%, respectively. However, at 90 days, deaths were more frequent in the control arm—21.4% and 37.9%.
Patients in the CPX-351 arm had slower neutrophil recovery than those in the control arm—42 days and 34 days, respectively. The same was true for platelet recovery—45 days and 35 days, respectively.
Delayed hematologic recovery was associated with more infection-related events, such as febrile neutropenia, bacteremia, pneumonia, sepsis, urinary tract infection, pyrexia, and cellulitis.
The researchers believe these results, along with the previously published results from a phase 2 trial of CPX-351 in patients newly diagnosed with AML, support the phase 3 study of CPX-351 as a first-line therapy in older patients with high-risk (secondary) AML.
“We were very pleased to see promising response rates in this difficult-to-treat population,” Dr Cortes said. “And we eagerly await results from Celator’s pivotal phase 3 study of CPX-351, which could fulfill a considerable unmet need in AML.” ![]()

In a phase 2 trial, an investigational drug conferred a significant improvement in survival when used as salvage therapy in poor-risk patients with acute myeloid leukemia (AML).
On the other hand, the drug did not provide any significant improvements over control treatment (investigator’s choice) in the entire population of AML patients in first relapse.
The drug, CPX-351, is a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle.
Researchers reported these results with CPX-351 in Cancer. The study was funded by Celator Pharmaceuticals, the company developing CPX-351, and the Leukemia and Lymphoma Society.
“Patients with first-relapse AML have generally a poor prognosis, with a limited likelihood of response following salvage treatment,” said study author Jorge Cortes, MD, of the MD Anderson Cancer Center in Houston, Texas.
“This is particularly true for patients classified by the EPI [European Prognostic Index] as poor-risk upon entering the trial.”
For this trial, Dr Cortes and his colleagues evaluated 125 patients, ages 18 to 65, from 35 centers in the US, Canada, and Europe. Patients had AML in first relapse after an initial complete remission lasting a month or longer.
They were stratified per the EPI into favorable-, intermediate-, and poor-risk groups based on the duration of their first complete remission, cytogenetics, age, and transplant history. Most patients (68%) were in the poor-risk group.
Patients were randomized 2:1 to receive CPX-351 (100 units/m2 on days 1, 3, and 5 by 90-minute infusion) or the investigators’ choice of first salvage chemotherapy. The control treatment was usually based on cytarabine and an anthracycline, often with one or more additional agents.
Patient characteristics were largely well-balanced between the treatment arms. However, the CPX-351 group had a younger median age (52 years vs 56 years), more patients with secondary AML (12.3% vs 6.8%), and a higher rate of prior transplant (27.2% vs 15.9%).
Response and survival
Response rates were higher in the CPX-351 arm than in the control arm. The rates of complete response were 37% and 31.8%, respectively. And the rates of complete response with incomplete count recovery were 12.3% and 9.1%, respectively.
However, there was no significant difference in event-free survival (EFS) or overall survival (OS) between the treatment arms.
The median EFS was 4 months in the CPX-351 arm and 1.4 months in the control arm (hazard ratio[HR]=0.66, P=0.08). And the median OS was 8.5 months and 6.3 months, respectively (HR=0.75, P=0.19).
In the poor-risk population, there was no significant improvement in EFS with CPX-351, but there was a significant improvement in OS.
The median EFS was 1.8 months in the CPX-351 arm and 1.2 months in the control arm (HR=0.63, P=0.08). And the median OS was 6.5 months and 4.2 months, respectively (HR=0.55, P=0.02).
Safety and early mortality
The early mortality rate was similar between the treatment arms at 30 days—7.4% in the CPX-351 arm and 4.5% in the control arm—and at 60 days—14.8% and 15.9%, respectively. However, at 90 days, deaths were more frequent in the control arm—21.4% and 37.9%.
Patients in the CPX-351 arm had slower neutrophil recovery than those in the control arm—42 days and 34 days, respectively. The same was true for platelet recovery—45 days and 35 days, respectively.
Delayed hematologic recovery was associated with more infection-related events, such as febrile neutropenia, bacteremia, pneumonia, sepsis, urinary tract infection, pyrexia, and cellulitis.
The researchers believe these results, along with the previously published results from a phase 2 trial of CPX-351 in patients newly diagnosed with AML, support the phase 3 study of CPX-351 as a first-line therapy in older patients with high-risk (secondary) AML.
“We were very pleased to see promising response rates in this difficult-to-treat population,” Dr Cortes said. “And we eagerly await results from Celator’s pivotal phase 3 study of CPX-351, which could fulfill a considerable unmet need in AML.” ![]()

In a phase 2 trial, an investigational drug conferred a significant improvement in survival when used as salvage therapy in poor-risk patients with acute myeloid leukemia (AML).
On the other hand, the drug did not provide any significant improvements over control treatment (investigator’s choice) in the entire population of AML patients in first relapse.
The drug, CPX-351, is a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle.
Researchers reported these results with CPX-351 in Cancer. The study was funded by Celator Pharmaceuticals, the company developing CPX-351, and the Leukemia and Lymphoma Society.
“Patients with first-relapse AML have generally a poor prognosis, with a limited likelihood of response following salvage treatment,” said study author Jorge Cortes, MD, of the MD Anderson Cancer Center in Houston, Texas.
“This is particularly true for patients classified by the EPI [European Prognostic Index] as poor-risk upon entering the trial.”
For this trial, Dr Cortes and his colleagues evaluated 125 patients, ages 18 to 65, from 35 centers in the US, Canada, and Europe. Patients had AML in first relapse after an initial complete remission lasting a month or longer.
They were stratified per the EPI into favorable-, intermediate-, and poor-risk groups based on the duration of their first complete remission, cytogenetics, age, and transplant history. Most patients (68%) were in the poor-risk group.
Patients were randomized 2:1 to receive CPX-351 (100 units/m2 on days 1, 3, and 5 by 90-minute infusion) or the investigators’ choice of first salvage chemotherapy. The control treatment was usually based on cytarabine and an anthracycline, often with one or more additional agents.
Patient characteristics were largely well-balanced between the treatment arms. However, the CPX-351 group had a younger median age (52 years vs 56 years), more patients with secondary AML (12.3% vs 6.8%), and a higher rate of prior transplant (27.2% vs 15.9%).
Response and survival
Response rates were higher in the CPX-351 arm than in the control arm. The rates of complete response were 37% and 31.8%, respectively. And the rates of complete response with incomplete count recovery were 12.3% and 9.1%, respectively.
However, there was no significant difference in event-free survival (EFS) or overall survival (OS) between the treatment arms.
The median EFS was 4 months in the CPX-351 arm and 1.4 months in the control arm (hazard ratio[HR]=0.66, P=0.08). And the median OS was 8.5 months and 6.3 months, respectively (HR=0.75, P=0.19).
In the poor-risk population, there was no significant improvement in EFS with CPX-351, but there was a significant improvement in OS.
The median EFS was 1.8 months in the CPX-351 arm and 1.2 months in the control arm (HR=0.63, P=0.08). And the median OS was 6.5 months and 4.2 months, respectively (HR=0.55, P=0.02).
Safety and early mortality
The early mortality rate was similar between the treatment arms at 30 days—7.4% in the CPX-351 arm and 4.5% in the control arm—and at 60 days—14.8% and 15.9%, respectively. However, at 90 days, deaths were more frequent in the control arm—21.4% and 37.9%.
Patients in the CPX-351 arm had slower neutrophil recovery than those in the control arm—42 days and 34 days, respectively. The same was true for platelet recovery—45 days and 35 days, respectively.
Delayed hematologic recovery was associated with more infection-related events, such as febrile neutropenia, bacteremia, pneumonia, sepsis, urinary tract infection, pyrexia, and cellulitis.
The researchers believe these results, along with the previously published results from a phase 2 trial of CPX-351 in patients newly diagnosed with AML, support the phase 3 study of CPX-351 as a first-line therapy in older patients with high-risk (secondary) AML.
“We were very pleased to see promising response rates in this difficult-to-treat population,” Dr Cortes said. “And we eagerly await results from Celator’s pivotal phase 3 study of CPX-351, which could fulfill a considerable unmet need in AML.” ![]()
Study reveals potential strategy to treat AML

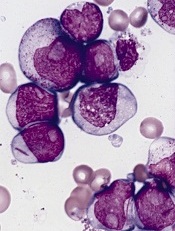
Credit: Lance Liotta
Researchers have discovered that interactions between two molecules—STAT3 and PRL-3—may provide a therapeutic target for acute myeloid leukemia (AML).
The team found evidence to suggest that the STAT3-PRL-3 regulatory loop contributes to the development of AML.
Chng Wee Joo, MB ChB, PhD, of the National University Cancer Institute in Singapore, and his colleagues reported these findings in Experimental Hematology.
The researchers discovered that STAT3, a transcription factor, binds and promotes the production of PRL-3 in cells. A decrease in STAT3 levels led to a corresponding decrease in the levels of PRL-3 and diminished the malignant properties of leukemic cells.
The team therefore concluded that a disruption of this regulatory loop may offer an attractive anti-AML therapeutic strategy. Furthermore, PRL-3 has the potential to be used as a biomarker in personalized therapy for AML patients.
The group was the first to report that the PRL-3 protein is overexpressed in 47% of bone marrow samples from AML patients. In addition, cellular levels of STAT3 were found to be elevated in about 50% of AML cases.
The researchers created a core STAT3 signature by analyzing datasets in the scientific literature. And they found that STAT3 core signature was significantly enriched in AML cases with high PRL-3 expression.
“Earlier studies on PRL-3 have been conducted in other cancers, but only in recent years has attention been turned to the significance of PRL-3 in blood cancer,” Dr Chng said.
“Previously, the mechanism by which PRL-3 is regulated in AML has also not been fully elucidated. This study reveals a novel connection between these two important oncogenes for the first time and also shows that the STAT3-PRL-3 regulatory loop contributes to the pathogenesis of AML.”
The researchers are now looking into methods to target the STAT3-PRL-3 pathway in AML, which could open up new avenues to treat AML patients with high expression of PRL-3 and offer an attractive anti-leukemia therapeutic strategy. ![]()

Credit: Lance Liotta
Researchers have discovered that interactions between two molecules—STAT3 and PRL-3—may provide a therapeutic target for acute myeloid leukemia (AML).
The team found evidence to suggest that the STAT3-PRL-3 regulatory loop contributes to the development of AML.
Chng Wee Joo, MB ChB, PhD, of the National University Cancer Institute in Singapore, and his colleagues reported these findings in Experimental Hematology.
The researchers discovered that STAT3, a transcription factor, binds and promotes the production of PRL-3 in cells. A decrease in STAT3 levels led to a corresponding decrease in the levels of PRL-3 and diminished the malignant properties of leukemic cells.
The team therefore concluded that a disruption of this regulatory loop may offer an attractive anti-AML therapeutic strategy. Furthermore, PRL-3 has the potential to be used as a biomarker in personalized therapy for AML patients.
The group was the first to report that the PRL-3 protein is overexpressed in 47% of bone marrow samples from AML patients. In addition, cellular levels of STAT3 were found to be elevated in about 50% of AML cases.
The researchers created a core STAT3 signature by analyzing datasets in the scientific literature. And they found that STAT3 core signature was significantly enriched in AML cases with high PRL-3 expression.
“Earlier studies on PRL-3 have been conducted in other cancers, but only in recent years has attention been turned to the significance of PRL-3 in blood cancer,” Dr Chng said.
“Previously, the mechanism by which PRL-3 is regulated in AML has also not been fully elucidated. This study reveals a novel connection between these two important oncogenes for the first time and also shows that the STAT3-PRL-3 regulatory loop contributes to the pathogenesis of AML.”
The researchers are now looking into methods to target the STAT3-PRL-3 pathway in AML, which could open up new avenues to treat AML patients with high expression of PRL-3 and offer an attractive anti-leukemia therapeutic strategy. ![]()

Credit: Lance Liotta
Researchers have discovered that interactions between two molecules—STAT3 and PRL-3—may provide a therapeutic target for acute myeloid leukemia (AML).
The team found evidence to suggest that the STAT3-PRL-3 regulatory loop contributes to the development of AML.
Chng Wee Joo, MB ChB, PhD, of the National University Cancer Institute in Singapore, and his colleagues reported these findings in Experimental Hematology.
The researchers discovered that STAT3, a transcription factor, binds and promotes the production of PRL-3 in cells. A decrease in STAT3 levels led to a corresponding decrease in the levels of PRL-3 and diminished the malignant properties of leukemic cells.
The team therefore concluded that a disruption of this regulatory loop may offer an attractive anti-AML therapeutic strategy. Furthermore, PRL-3 has the potential to be used as a biomarker in personalized therapy for AML patients.
The group was the first to report that the PRL-3 protein is overexpressed in 47% of bone marrow samples from AML patients. In addition, cellular levels of STAT3 were found to be elevated in about 50% of AML cases.
The researchers created a core STAT3 signature by analyzing datasets in the scientific literature. And they found that STAT3 core signature was significantly enriched in AML cases with high PRL-3 expression.
“Earlier studies on PRL-3 have been conducted in other cancers, but only in recent years has attention been turned to the significance of PRL-3 in blood cancer,” Dr Chng said.
“Previously, the mechanism by which PRL-3 is regulated in AML has also not been fully elucidated. This study reveals a novel connection between these two important oncogenes for the first time and also shows that the STAT3-PRL-3 regulatory loop contributes to the pathogenesis of AML.”
The researchers are now looking into methods to target the STAT3-PRL-3 pathway in AML, which could open up new avenues to treat AML patients with high expression of PRL-3 and offer an attractive anti-leukemia therapeutic strategy. ![]()
FDA panel backs approval of filgrastim biosimilar
SILVER SPRING, MD. – With the unanimous support of a Food and Drug Administration advisory panel and a favorable review by the agency, a “biosimilar” version of filgrastim, the recombinant granulocyte colony-stimulating factor marketed as Neupogen, will likely become the first biosimilar product to be approved in the United States.
At a meeting on Jan. 7, the FDA’s Oncologic Drugs Advisory Committee voted 14-0 that the filgrastim biosimilar should be approved for the five indications approved for Neupogen in the United States, based on “the totality of the evidence,” which includes pharmacokinetic, pharmacodynamic, immunogenicity, and clinical data. With little debate, they agreed that other than minor differences in clinically inactive components, the biosimilar, currently referred to as “EP2006,” was “highly similar” to the reference product, and that there were “no clinically meaningful differences” between EP2006 and Neupogen – the components of the definition of biosimilarity.
The meeting was considered historic, since this is the first biosimilar to be reviewed by an FDA advisory panel, and if approved, will be the first biosimilar to become available as a result of the Biologics Price Competition and Innovation Act of 2009, which was passed as part of the Affordable Care Act, creating “an abbreviated licensure pathway for biological products shown to be ‘biosimilar’ or ‘interchangeable’ with an FDA-licensed biological product,” according to the FDA.
Neupogen was approved by the FDA in 1991 and is marketed by Amgen. If approved, EP2006 would be the first biosimilar product to be approved in the United States, and, like generic drugs, is expected to provide a cheaper version of Neupogen. Sandoz, the generic pharmaceuticals arm of Novartis, plans to market the biosimilar as Zarxio in the United States. The filgrastim biosimilar was approved in 2009 in the European Union, where it is marketed as Zarzio, and it is now approved in more than 60 countries, with more than 7.5 million days of exposure, according to Sandoz.
Between 2009 and 2012, the use of filgrastim increased by 30% in Europe, and the biosimilar is now the most commonly prescribed version of filgrastim in Europe. The cost of filgrastim dropped substantially after approval because of the competition, company officials said.
EP2006 will be available in prefilled syringes containing 300 mcg/0.5 mL or 480 mcg/0.8 mL administered subcutaneously or intravenously, the same strengths as U.S.-approved Neupogen. For approval, Sandoz submitted eight studies, including two studies comparing EP2006 to U.S.-approved Neupogen conducted specifically for the U.S. approval, one of 28 healthy volunteers and another of 218 women with breast cancer, treated with myelosuppressive chemotherapy, evaluating the pharmacokinetics (PK), pharmacodynamics (PD), safety, and immunogenicity (the breast cancer study also evaluated safety and efficacy). The remaining studies included studies in healthy volunteers and breast cancer patients, comparing the biosimilar to European-approved Neupogen, or single-arm studies.
At the meeting, Sigrid Balser, Ph.D., of the global clinical development department at Sandoz, said that in the U.S. study of healthy volunteers, there was a “high degree of similarity” between EP2006 and Neupogen in terms of the PD and PK results, and the absolute neutrophil count (ANC) and CD34+ cell responses. In the U.S. study of breast cancer patients, EP2006 and Neupogen were equivalent in terms of efficacy over the first chemotherapy cycle and had a similar safety profile over six chemotherapy cycles. There were no signs of immunogenicity associated with the biosimilar in the U.S. or European studies in patients with breast cancer or healthy volunteers.
Outside of the United States, more than 3,800 patients have been treated with Zarzio for various indications, including chemotherapy-induced neutropenia, hematopoietic stem cell mobilization, and severe chronic neutropenia, and have been monitored as part of postmarketing trials or routine pharmacovigilance. To date, there have been no signals of any differences in the safety profile of the filgrastim biosimilar, compared with Neupogen;no cases of immunogenicity; and safety and effectiveness has been “confirmed in clinical practice,” Dr. Balser added.
Based on the data, the FDA reviewers concluded that EP2006 is “highly similar to U.S.-licensed Neupogen, and that there are no clinically meaningful difference between the two products,” said Dr. Albert Deisseroth, medical officer and team leader in the division of hematology products, in the FDA’s office of hematology and oncology products.
“Clinically, they appear to really function pretty equally in terms of what you’re asking them to do,” said the panel chair, Dr. Deborah Armstrong, professor of oncology at Johns Hopkins University, Baltimore. The extensive use of the filgrastim biosimilar in other parts of the world provided evidence of “robust safety and efficacy,” which contributed to her support for approval, she added.
Cost is not allowed to be discussed during FDA panel meetings, and Sandoz did not specify any possible price of the biosimilar, but this issue was the “elephant in the room,” as one panelist pointed out. However, Dr. Louis Weiner, chairman of the department of oncology and director of the Lombardi Comprehensive Cancer Center at Georgetown University in Washington, who spoke on behalf of Sandoz at the meeting, said that the availability of the filgrastim biosimilar has “enormous promise in reducing cost and expanding access” to this treatment. Although it has “unquestioned clinical value,” he said that granulocyte colony-stimulating factor therapy is underused.
The five indications approved for Neupogen are to decrease the incidence of infection‚ as manifested by febrile neutropenia in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever; for reducing the time to neutrophil recovery and the duration of fever, following induction or consolidation chemotherapy treatment of adults with acute myeloid leukemia; to reduce the duration of neutropenia and neutropenia-related clinical sequelae; for the mobilization of hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis; and for chronic administration to reduce the incidence and duration of sequelae of neutropenia in symptomatic patients with congenital‚ cyclic‚ or idiopathic neutropenia.
The FDA usually follows the recommendations of its advisory panels. Panelists were cleared of potential conflicts of interest related to the topic of the meeting. In some cases, a panelist may be given a waiver but not at this meeting. Dr. Weiner’s disclosure included being a consultant to Sandoz.
SILVER SPRING, MD. – With the unanimous support of a Food and Drug Administration advisory panel and a favorable review by the agency, a “biosimilar” version of filgrastim, the recombinant granulocyte colony-stimulating factor marketed as Neupogen, will likely become the first biosimilar product to be approved in the United States.
At a meeting on Jan. 7, the FDA’s Oncologic Drugs Advisory Committee voted 14-0 that the filgrastim biosimilar should be approved for the five indications approved for Neupogen in the United States, based on “the totality of the evidence,” which includes pharmacokinetic, pharmacodynamic, immunogenicity, and clinical data. With little debate, they agreed that other than minor differences in clinically inactive components, the biosimilar, currently referred to as “EP2006,” was “highly similar” to the reference product, and that there were “no clinically meaningful differences” between EP2006 and Neupogen – the components of the definition of biosimilarity.
The meeting was considered historic, since this is the first biosimilar to be reviewed by an FDA advisory panel, and if approved, will be the first biosimilar to become available as a result of the Biologics Price Competition and Innovation Act of 2009, which was passed as part of the Affordable Care Act, creating “an abbreviated licensure pathway for biological products shown to be ‘biosimilar’ or ‘interchangeable’ with an FDA-licensed biological product,” according to the FDA.
Neupogen was approved by the FDA in 1991 and is marketed by Amgen. If approved, EP2006 would be the first biosimilar product to be approved in the United States, and, like generic drugs, is expected to provide a cheaper version of Neupogen. Sandoz, the generic pharmaceuticals arm of Novartis, plans to market the biosimilar as Zarxio in the United States. The filgrastim biosimilar was approved in 2009 in the European Union, where it is marketed as Zarzio, and it is now approved in more than 60 countries, with more than 7.5 million days of exposure, according to Sandoz.
Between 2009 and 2012, the use of filgrastim increased by 30% in Europe, and the biosimilar is now the most commonly prescribed version of filgrastim in Europe. The cost of filgrastim dropped substantially after approval because of the competition, company officials said.
EP2006 will be available in prefilled syringes containing 300 mcg/0.5 mL or 480 mcg/0.8 mL administered subcutaneously or intravenously, the same strengths as U.S.-approved Neupogen. For approval, Sandoz submitted eight studies, including two studies comparing EP2006 to U.S.-approved Neupogen conducted specifically for the U.S. approval, one of 28 healthy volunteers and another of 218 women with breast cancer, treated with myelosuppressive chemotherapy, evaluating the pharmacokinetics (PK), pharmacodynamics (PD), safety, and immunogenicity (the breast cancer study also evaluated safety and efficacy). The remaining studies included studies in healthy volunteers and breast cancer patients, comparing the biosimilar to European-approved Neupogen, or single-arm studies.
At the meeting, Sigrid Balser, Ph.D., of the global clinical development department at Sandoz, said that in the U.S. study of healthy volunteers, there was a “high degree of similarity” between EP2006 and Neupogen in terms of the PD and PK results, and the absolute neutrophil count (ANC) and CD34+ cell responses. In the U.S. study of breast cancer patients, EP2006 and Neupogen were equivalent in terms of efficacy over the first chemotherapy cycle and had a similar safety profile over six chemotherapy cycles. There were no signs of immunogenicity associated with the biosimilar in the U.S. or European studies in patients with breast cancer or healthy volunteers.
Outside of the United States, more than 3,800 patients have been treated with Zarzio for various indications, including chemotherapy-induced neutropenia, hematopoietic stem cell mobilization, and severe chronic neutropenia, and have been monitored as part of postmarketing trials or routine pharmacovigilance. To date, there have been no signals of any differences in the safety profile of the filgrastim biosimilar, compared with Neupogen;no cases of immunogenicity; and safety and effectiveness has been “confirmed in clinical practice,” Dr. Balser added.
Based on the data, the FDA reviewers concluded that EP2006 is “highly similar to U.S.-licensed Neupogen, and that there are no clinically meaningful difference between the two products,” said Dr. Albert Deisseroth, medical officer and team leader in the division of hematology products, in the FDA’s office of hematology and oncology products.
“Clinically, they appear to really function pretty equally in terms of what you’re asking them to do,” said the panel chair, Dr. Deborah Armstrong, professor of oncology at Johns Hopkins University, Baltimore. The extensive use of the filgrastim biosimilar in other parts of the world provided evidence of “robust safety and efficacy,” which contributed to her support for approval, she added.
Cost is not allowed to be discussed during FDA panel meetings, and Sandoz did not specify any possible price of the biosimilar, but this issue was the “elephant in the room,” as one panelist pointed out. However, Dr. Louis Weiner, chairman of the department of oncology and director of the Lombardi Comprehensive Cancer Center at Georgetown University in Washington, who spoke on behalf of Sandoz at the meeting, said that the availability of the filgrastim biosimilar has “enormous promise in reducing cost and expanding access” to this treatment. Although it has “unquestioned clinical value,” he said that granulocyte colony-stimulating factor therapy is underused.
The five indications approved for Neupogen are to decrease the incidence of infection‚ as manifested by febrile neutropenia in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever; for reducing the time to neutrophil recovery and the duration of fever, following induction or consolidation chemotherapy treatment of adults with acute myeloid leukemia; to reduce the duration of neutropenia and neutropenia-related clinical sequelae; for the mobilization of hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis; and for chronic administration to reduce the incidence and duration of sequelae of neutropenia in symptomatic patients with congenital‚ cyclic‚ or idiopathic neutropenia.
The FDA usually follows the recommendations of its advisory panels. Panelists were cleared of potential conflicts of interest related to the topic of the meeting. In some cases, a panelist may be given a waiver but not at this meeting. Dr. Weiner’s disclosure included being a consultant to Sandoz.
SILVER SPRING, MD. – With the unanimous support of a Food and Drug Administration advisory panel and a favorable review by the agency, a “biosimilar” version of filgrastim, the recombinant granulocyte colony-stimulating factor marketed as Neupogen, will likely become the first biosimilar product to be approved in the United States.
At a meeting on Jan. 7, the FDA’s Oncologic Drugs Advisory Committee voted 14-0 that the filgrastim biosimilar should be approved for the five indications approved for Neupogen in the United States, based on “the totality of the evidence,” which includes pharmacokinetic, pharmacodynamic, immunogenicity, and clinical data. With little debate, they agreed that other than minor differences in clinically inactive components, the biosimilar, currently referred to as “EP2006,” was “highly similar” to the reference product, and that there were “no clinically meaningful differences” between EP2006 and Neupogen – the components of the definition of biosimilarity.
The meeting was considered historic, since this is the first biosimilar to be reviewed by an FDA advisory panel, and if approved, will be the first biosimilar to become available as a result of the Biologics Price Competition and Innovation Act of 2009, which was passed as part of the Affordable Care Act, creating “an abbreviated licensure pathway for biological products shown to be ‘biosimilar’ or ‘interchangeable’ with an FDA-licensed biological product,” according to the FDA.
Neupogen was approved by the FDA in 1991 and is marketed by Amgen. If approved, EP2006 would be the first biosimilar product to be approved in the United States, and, like generic drugs, is expected to provide a cheaper version of Neupogen. Sandoz, the generic pharmaceuticals arm of Novartis, plans to market the biosimilar as Zarxio in the United States. The filgrastim biosimilar was approved in 2009 in the European Union, where it is marketed as Zarzio, and it is now approved in more than 60 countries, with more than 7.5 million days of exposure, according to Sandoz.
Between 2009 and 2012, the use of filgrastim increased by 30% in Europe, and the biosimilar is now the most commonly prescribed version of filgrastim in Europe. The cost of filgrastim dropped substantially after approval because of the competition, company officials said.
EP2006 will be available in prefilled syringes containing 300 mcg/0.5 mL or 480 mcg/0.8 mL administered subcutaneously or intravenously, the same strengths as U.S.-approved Neupogen. For approval, Sandoz submitted eight studies, including two studies comparing EP2006 to U.S.-approved Neupogen conducted specifically for the U.S. approval, one of 28 healthy volunteers and another of 218 women with breast cancer, treated with myelosuppressive chemotherapy, evaluating the pharmacokinetics (PK), pharmacodynamics (PD), safety, and immunogenicity (the breast cancer study also evaluated safety and efficacy). The remaining studies included studies in healthy volunteers and breast cancer patients, comparing the biosimilar to European-approved Neupogen, or single-arm studies.
At the meeting, Sigrid Balser, Ph.D., of the global clinical development department at Sandoz, said that in the U.S. study of healthy volunteers, there was a “high degree of similarity” between EP2006 and Neupogen in terms of the PD and PK results, and the absolute neutrophil count (ANC) and CD34+ cell responses. In the U.S. study of breast cancer patients, EP2006 and Neupogen were equivalent in terms of efficacy over the first chemotherapy cycle and had a similar safety profile over six chemotherapy cycles. There were no signs of immunogenicity associated with the biosimilar in the U.S. or European studies in patients with breast cancer or healthy volunteers.
Outside of the United States, more than 3,800 patients have been treated with Zarzio for various indications, including chemotherapy-induced neutropenia, hematopoietic stem cell mobilization, and severe chronic neutropenia, and have been monitored as part of postmarketing trials or routine pharmacovigilance. To date, there have been no signals of any differences in the safety profile of the filgrastim biosimilar, compared with Neupogen;no cases of immunogenicity; and safety and effectiveness has been “confirmed in clinical practice,” Dr. Balser added.
Based on the data, the FDA reviewers concluded that EP2006 is “highly similar to U.S.-licensed Neupogen, and that there are no clinically meaningful difference between the two products,” said Dr. Albert Deisseroth, medical officer and team leader in the division of hematology products, in the FDA’s office of hematology and oncology products.
“Clinically, they appear to really function pretty equally in terms of what you’re asking them to do,” said the panel chair, Dr. Deborah Armstrong, professor of oncology at Johns Hopkins University, Baltimore. The extensive use of the filgrastim biosimilar in other parts of the world provided evidence of “robust safety and efficacy,” which contributed to her support for approval, she added.
Cost is not allowed to be discussed during FDA panel meetings, and Sandoz did not specify any possible price of the biosimilar, but this issue was the “elephant in the room,” as one panelist pointed out. However, Dr. Louis Weiner, chairman of the department of oncology and director of the Lombardi Comprehensive Cancer Center at Georgetown University in Washington, who spoke on behalf of Sandoz at the meeting, said that the availability of the filgrastim biosimilar has “enormous promise in reducing cost and expanding access” to this treatment. Although it has “unquestioned clinical value,” he said that granulocyte colony-stimulating factor therapy is underused.
The five indications approved for Neupogen are to decrease the incidence of infection‚ as manifested by febrile neutropenia in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever; for reducing the time to neutrophil recovery and the duration of fever, following induction or consolidation chemotherapy treatment of adults with acute myeloid leukemia; to reduce the duration of neutropenia and neutropenia-related clinical sequelae; for the mobilization of hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis; and for chronic administration to reduce the incidence and duration of sequelae of neutropenia in symptomatic patients with congenital‚ cyclic‚ or idiopathic neutropenia.
The FDA usually follows the recommendations of its advisory panels. Panelists were cleared of potential conflicts of interest related to the topic of the meeting. In some cases, a panelist may be given a waiver but not at this meeting. Dr. Weiner’s disclosure included being a consultant to Sandoz.
AT AN FDA ADVISORY COMMITTEE MEETING
Certain cancers primarily result from ‘bad luck’
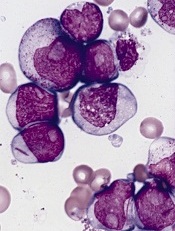
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates. ![]()
Study confirms IDH2 as therapeutic target in AML, MDS

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.

in the Moscone Center
SAN FRANCISCO—The first-in-human study of AG-221 has confirmed IDH2 as a therapeutic target in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), according to investigators.
From the first dose of therapy, the high plasma level observed in patients “translates into a drastic decrease in 2-HG,” said Eytan M. Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Mutations in IDH1 and IDH2 result in the accumulation of the oncometabolite 2-HG. And high levels of 2-HG prompt epigenetic changes to the cell, resulting in impaired cellular differentiation.
“By cycle 1, day 15, at all dose levels, there was fantastic inhibition of 2-HG,” Dr Stein said. “Indeed, this drastic inhibition of 2-HG led to profound clinical benefit.”
He presented interim results of the phase 1 study of AG-221 at the 2014 ASH Annual Meeting (abstract 115).*
The investigators have treated 73 patients with advanced IDH2-mutation-positive hematologic malignancies since the study began in September 2013.
Patients were a median age of 67 years (range, 33-90), and 74% had IDH2 R140 mutations. Most had relapsed/refractory AML (n=55), and the rest had MDS (n=6), untreated AML (n=5), chronic myelomonocytic leukemia (n=5), and myeloid sarcoma (n=1).
Patients received AG-221 as a single agent orally, once or twice a day, continuously, in 28-day cycles. Four dose-expansion cohorts at 100 mg each day were added last October.
To date, the maximum tolerated dose has not been reached, with the highest cumulative daily dose being 300 mg. Investigators observed a single dose-limiting toxicity in 1 patient: grade 5 hypoxia with fungal pneumonia and septic shock.
As of the data cutoff on October 1, 2014, 38 patients were still on therapy, and 35 had discontinued. Five patients withdrew after achieving complete remission (CR) in order to pursue allogeneic transplant.
Dr Stein pointed out that although the median number of prior chemotherapy regimens for the entire cohort was 2, “all of the patients who went on study were predicted to have dismal outcomes with conventional therapy.”
Safety
The therapy was well tolerated, with the most common adverse events (AEs) overall being typical for patients with advanced AML: nausea (23%), pyrexia (19%), and diarrhea (17%).
The majority of serious AEs were disease-related and unrelated to the study drug, Dr Stein said. Thirteen patients experienced 21 serious AEs that were possibly or probably related to treatment.
Investigators observed treatment-related leukocytosis in 3 patients, “but we think that is a differentiating effect of the study drug,” Dr Stein said.
He also pointed out that there was no increase in AEs with increased dose of the drug.
Of the 11 deaths reported, 9 were unrelated to the drug, and 2—sepsis/hypoxia and atrial flutter—were possibly related. The 30-day and 60-day all-cause mortality rates were 4.1% and 13.7%, respectively.
Efficacy
Of the 45 patients who were treated for at least 1 cycle and were evaluable for efficacy, 15 achieved a CR (n=6) or a CR with incomplete blood count recovery. The overall response rate is 56% (25/45).
“Responses appear durable,” Dr Stein commented, “and 90% of responders have had a response duration of at least 3 months, with the earliest patients on study having had durable responses for over 6 months.”
Many of the durable responses are partial remissions, he noted.
Seventeen patients have stable disease, and many of these patients remain on study. Two patients had progressive disease.
“Patients with stable disease have remained on study for a similar amount of time as the responders,” Dr Stein said, “suggesting that, despite the lack of a formal partial remission, many patients are deriving clinical benefit from study treatment.”
This study was sponsored by Agios Pharmaceuticals Inc., the company developing AG-221 in collaboration with Celgene.
Previous results from this study were presented at the 2014 EHA Annual Congress. Based on those results, AG-221 received fast track designation from the US Food and Drug Administration. ![]()
*Data in the presentation were updated from the abstract.
VALOR: Baby step forward or misstep in AML?
SAN FRANCISCO – Adding vosaroxin to cytarabine chemotherapy increased overall survival in first relapsed or refractory acute myeloid leukemia in the phase III VALOR study.
The difference in this primary endpoint, however, failed to achieve statistically significance (median 7.5 months vs. 6.1 months; P = .06), lead study author Dr. Farhad Ravandi reported at the annual meeting of the American Society of Hematology.
More patients receiving vosaroxin (Qinprezo) and cytarabine than cytarabine alone achieved complete remission (CR) (30.1% vs. 16.3%; P < .0001).
The benefit was significant across all subgroups (age at least 60 years, refractory disease, early and late relapse), except in those aged younger than 60 years, he said.
Vosaroxin is an investigational, first-in-class anticancer quinolone derivative that was granted fast track designation by the Food and Drug Administration in 2011 for the potential treatment of relapsed or refractory acute myeloid leukemia (AML) in combination with cytarabine.
Despite missing its primary endpoint, Dr. Ravandi argued during a press briefing that VALOR was a positive trial and that the survival benefit with combination vosaroxin was “highly significant.” He described relapsed/refractory AML as the equivalent of metastatic cancer, with patients presenting with disease “all over their body, right from day 1.”
“In solid tumors, we are excited about a 1- or 2-month survival improvement and I don’t see why we shouldn’t be excited in AML as well,” said Dr. Ravandi of the University of Texas M.D. Anderson Cancer Center in Houston.
He suggested that the bar has been set high in AML because about 40% of patients are cured and that great leaps forward remain rare. “We should not discount the small steps forward in treating our patients and providing better treatment options,” he said.
Press briefing moderator Dr. David Steensma of the Dana-Farber Cancer Institute, Boston, agreed that change is often incremental in AML but countered that the magnitude of benefit wasn’t great.
“AML is a really difficult population, no question about it, but there’s also no question that seven and a half months is pretty crummy and we need to do better than that,” Dr. Steensma said.
VALOR randomly assigned 711 adult patients from 124 sites in 15 countries to IV cytarabine 1 g/m² on days 1-5 plus placebo or IV vosaroxin 90 mg/m² on days 1 and 4 for induction and 70 mg/m² for subsequent cycles. Patients had AML refractory to initial induction therapy or were in first relapse, defined as relapse within 90 days to 24 months after first CR or CR with incomplete platelet recovery.
In all, 30.1% of patients in the vosaroxin group and 29% in the placebo group underwent allogeneic stem cell transplantation (ASCT). In those younger than 60 years, rates were 46.2% and 45.4%.
When stratified by age, there was a significant overall survival benefit with the vosaroxin combination for patients aged 60 years and older, who accounted for two-thirds of the study population (median 7.1 months vs. 5.0 months; hazard ratio, 0.75; P = .003), Dr. Ravandi said.
There was no survival advantage in patients younger than 60 years (median 9.1 months vs. 7.9 months; HR, 1.08, P = .60).
In a preplanned analysis censored for ASCT, median overall survival was significantly better in patients receiving the vosaroxin combination versus cytarabine alone (6.7 months vs. 5.3 months; HR, 0.83; P = .02).
“The benefit may be underestimated by the high rate of [ASCT], particularly in the younger patients,” Dr. Ravandi concluded during the formal presentation of the late-breaking abstract. “These data support the use of vosaroxin in combination with cytarabine as a new standard for salvage therapy in older patients with relapsed or refractory AML.”
During the discussion following the presentation, session comoderator Dr. Jonathan Friedberg of the University of Rochester Medical Center in Rochester, N.Y., asked, “How do you reconcile the observation that the patients you wanted to get to transplant got there, and yet you’re blaming the transplant for poor outcomes?”
Dr. Ravandi responded that transplantation is an issue in all AML studies and that a much larger study would have been needed to show a survival difference regardless of transplant status.
Treatment-related adverse events were more common in patients on vosaroxin and were mostly infection related. Stomatitis was identified as a dose-limiting toxicity in previous studies and occurred at any grade in 49% of vosaroxin patients and 19% of controls and at grade 3/4 in 15% and 3%.
Other notable grade 3/4 events were febrile neutropenia (47% vs. 33%) and thrombocytopenia (24% vs. 25%). This increase in toxicity did not translate into worse all-cause mortality at either 30 or 60 days, Dr. Ravandi said.
Sunesis Pharmaceuticals funded the study. Dr. Ravandi and several coauthors reported financial ties with Sunesis. Dr Steensma reported financial ties with several companies. Dr. Friedberg reported no disclosures.
SAN FRANCISCO – Adding vosaroxin to cytarabine chemotherapy increased overall survival in first relapsed or refractory acute myeloid leukemia in the phase III VALOR study.
The difference in this primary endpoint, however, failed to achieve statistically significance (median 7.5 months vs. 6.1 months; P = .06), lead study author Dr. Farhad Ravandi reported at the annual meeting of the American Society of Hematology.
More patients receiving vosaroxin (Qinprezo) and cytarabine than cytarabine alone achieved complete remission (CR) (30.1% vs. 16.3%; P < .0001).
The benefit was significant across all subgroups (age at least 60 years, refractory disease, early and late relapse), except in those aged younger than 60 years, he said.
Vosaroxin is an investigational, first-in-class anticancer quinolone derivative that was granted fast track designation by the Food and Drug Administration in 2011 for the potential treatment of relapsed or refractory acute myeloid leukemia (AML) in combination with cytarabine.
Despite missing its primary endpoint, Dr. Ravandi argued during a press briefing that VALOR was a positive trial and that the survival benefit with combination vosaroxin was “highly significant.” He described relapsed/refractory AML as the equivalent of metastatic cancer, with patients presenting with disease “all over their body, right from day 1.”
“In solid tumors, we are excited about a 1- or 2-month survival improvement and I don’t see why we shouldn’t be excited in AML as well,” said Dr. Ravandi of the University of Texas M.D. Anderson Cancer Center in Houston.
He suggested that the bar has been set high in AML because about 40% of patients are cured and that great leaps forward remain rare. “We should not discount the small steps forward in treating our patients and providing better treatment options,” he said.
Press briefing moderator Dr. David Steensma of the Dana-Farber Cancer Institute, Boston, agreed that change is often incremental in AML but countered that the magnitude of benefit wasn’t great.
“AML is a really difficult population, no question about it, but there’s also no question that seven and a half months is pretty crummy and we need to do better than that,” Dr. Steensma said.
VALOR randomly assigned 711 adult patients from 124 sites in 15 countries to IV cytarabine 1 g/m² on days 1-5 plus placebo or IV vosaroxin 90 mg/m² on days 1 and 4 for induction and 70 mg/m² for subsequent cycles. Patients had AML refractory to initial induction therapy or were in first relapse, defined as relapse within 90 days to 24 months after first CR or CR with incomplete platelet recovery.
In all, 30.1% of patients in the vosaroxin group and 29% in the placebo group underwent allogeneic stem cell transplantation (ASCT). In those younger than 60 years, rates were 46.2% and 45.4%.
When stratified by age, there was a significant overall survival benefit with the vosaroxin combination for patients aged 60 years and older, who accounted for two-thirds of the study population (median 7.1 months vs. 5.0 months; hazard ratio, 0.75; P = .003), Dr. Ravandi said.
There was no survival advantage in patients younger than 60 years (median 9.1 months vs. 7.9 months; HR, 1.08, P = .60).
In a preplanned analysis censored for ASCT, median overall survival was significantly better in patients receiving the vosaroxin combination versus cytarabine alone (6.7 months vs. 5.3 months; HR, 0.83; P = .02).
“The benefit may be underestimated by the high rate of [ASCT], particularly in the younger patients,” Dr. Ravandi concluded during the formal presentation of the late-breaking abstract. “These data support the use of vosaroxin in combination with cytarabine as a new standard for salvage therapy in older patients with relapsed or refractory AML.”
During the discussion following the presentation, session comoderator Dr. Jonathan Friedberg of the University of Rochester Medical Center in Rochester, N.Y., asked, “How do you reconcile the observation that the patients you wanted to get to transplant got there, and yet you’re blaming the transplant for poor outcomes?”
Dr. Ravandi responded that transplantation is an issue in all AML studies and that a much larger study would have been needed to show a survival difference regardless of transplant status.
Treatment-related adverse events were more common in patients on vosaroxin and were mostly infection related. Stomatitis was identified as a dose-limiting toxicity in previous studies and occurred at any grade in 49% of vosaroxin patients and 19% of controls and at grade 3/4 in 15% and 3%.
Other notable grade 3/4 events were febrile neutropenia (47% vs. 33%) and thrombocytopenia (24% vs. 25%). This increase in toxicity did not translate into worse all-cause mortality at either 30 or 60 days, Dr. Ravandi said.
Sunesis Pharmaceuticals funded the study. Dr. Ravandi and several coauthors reported financial ties with Sunesis. Dr Steensma reported financial ties with several companies. Dr. Friedberg reported no disclosures.
SAN FRANCISCO – Adding vosaroxin to cytarabine chemotherapy increased overall survival in first relapsed or refractory acute myeloid leukemia in the phase III VALOR study.
The difference in this primary endpoint, however, failed to achieve statistically significance (median 7.5 months vs. 6.1 months; P = .06), lead study author Dr. Farhad Ravandi reported at the annual meeting of the American Society of Hematology.
More patients receiving vosaroxin (Qinprezo) and cytarabine than cytarabine alone achieved complete remission (CR) (30.1% vs. 16.3%; P < .0001).
The benefit was significant across all subgroups (age at least 60 years, refractory disease, early and late relapse), except in those aged younger than 60 years, he said.
Vosaroxin is an investigational, first-in-class anticancer quinolone derivative that was granted fast track designation by the Food and Drug Administration in 2011 for the potential treatment of relapsed or refractory acute myeloid leukemia (AML) in combination with cytarabine.
Despite missing its primary endpoint, Dr. Ravandi argued during a press briefing that VALOR was a positive trial and that the survival benefit with combination vosaroxin was “highly significant.” He described relapsed/refractory AML as the equivalent of metastatic cancer, with patients presenting with disease “all over their body, right from day 1.”
“In solid tumors, we are excited about a 1- or 2-month survival improvement and I don’t see why we shouldn’t be excited in AML as well,” said Dr. Ravandi of the University of Texas M.D. Anderson Cancer Center in Houston.
He suggested that the bar has been set high in AML because about 40% of patients are cured and that great leaps forward remain rare. “We should not discount the small steps forward in treating our patients and providing better treatment options,” he said.
Press briefing moderator Dr. David Steensma of the Dana-Farber Cancer Institute, Boston, agreed that change is often incremental in AML but countered that the magnitude of benefit wasn’t great.
“AML is a really difficult population, no question about it, but there’s also no question that seven and a half months is pretty crummy and we need to do better than that,” Dr. Steensma said.
VALOR randomly assigned 711 adult patients from 124 sites in 15 countries to IV cytarabine 1 g/m² on days 1-5 plus placebo or IV vosaroxin 90 mg/m² on days 1 and 4 for induction and 70 mg/m² for subsequent cycles. Patients had AML refractory to initial induction therapy or were in first relapse, defined as relapse within 90 days to 24 months after first CR or CR with incomplete platelet recovery.
In all, 30.1% of patients in the vosaroxin group and 29% in the placebo group underwent allogeneic stem cell transplantation (ASCT). In those younger than 60 years, rates were 46.2% and 45.4%.
When stratified by age, there was a significant overall survival benefit with the vosaroxin combination for patients aged 60 years and older, who accounted for two-thirds of the study population (median 7.1 months vs. 5.0 months; hazard ratio, 0.75; P = .003), Dr. Ravandi said.
There was no survival advantage in patients younger than 60 years (median 9.1 months vs. 7.9 months; HR, 1.08, P = .60).
In a preplanned analysis censored for ASCT, median overall survival was significantly better in patients receiving the vosaroxin combination versus cytarabine alone (6.7 months vs. 5.3 months; HR, 0.83; P = .02).
“The benefit may be underestimated by the high rate of [ASCT], particularly in the younger patients,” Dr. Ravandi concluded during the formal presentation of the late-breaking abstract. “These data support the use of vosaroxin in combination with cytarabine as a new standard for salvage therapy in older patients with relapsed or refractory AML.”
During the discussion following the presentation, session comoderator Dr. Jonathan Friedberg of the University of Rochester Medical Center in Rochester, N.Y., asked, “How do you reconcile the observation that the patients you wanted to get to transplant got there, and yet you’re blaming the transplant for poor outcomes?”
Dr. Ravandi responded that transplantation is an issue in all AML studies and that a much larger study would have been needed to show a survival difference regardless of transplant status.
Treatment-related adverse events were more common in patients on vosaroxin and were mostly infection related. Stomatitis was identified as a dose-limiting toxicity in previous studies and occurred at any grade in 49% of vosaroxin patients and 19% of controls and at grade 3/4 in 15% and 3%.
Other notable grade 3/4 events were febrile neutropenia (47% vs. 33%) and thrombocytopenia (24% vs. 25%). This increase in toxicity did not translate into worse all-cause mortality at either 30 or 60 days, Dr. Ravandi said.
Sunesis Pharmaceuticals funded the study. Dr. Ravandi and several coauthors reported financial ties with Sunesis. Dr Steensma reported financial ties with several companies. Dr. Friedberg reported no disclosures.
AT ASH 2014
Key clinical point: Vosaroxin plus cytarabine failed to significantly improve overall survival in relapsed or refractory AML, but may offer older patients a new option.
Major finding: Median overall survival was 7.5 months for vosaroxin plus cytarabine vs. 6.1 months for cytarabine alone (HR, 0.865; P = .06).
Data source: Randomized, phase III trial in 711 patients with first relapsed or refractory acute myeloid leukemia.
Disclosures: Sunesis Pharmaceuticals funded the study. Dr. Ravandi and several coauthors reported financial ties with Sunesis. Dr Steensma reported financial ties with several companies. Dr. Friedberg reported no disclosures.
Discovery could help predict, prevent therapy-related AML

Credit: Rhoda Baer
A new study challenges the view that cancer treatment is a direct cause of therapy-related acute myeloid leukemia (AML).
The research suggests that mutations in p53 can accumulate in hematopoietic stem cells (HSCs) as a person ages, years before a cancer diagnosis.
If and when cancer develops, these mutated cells are more resistant to treatment and multiply at an accelerated pace after exposure to chemotherapy or radiation therapy, which can then lead to AML.
The findings, reported in Nature, open up new avenues for research to predict which patients are at risk of developing therapy-related AML and to find ways to prevent it.
“Until now, we’ve really understood very little about therapy-related AML and why it is so difficult to treat,” said study author Daniel Link, MD, of Washington University in St Louis, Missouri.
“This gives us some important clues for further studies aimed at treatment and prevention.”
Dr Link and his colleagues began this research by sequencing the genomes of 22 patients with therapy-related AML. The patients had similar numbers and types of mutations in their leukemia cells as other patients who developed AML without prior exposure to chemotherapy or radiation, an indication that cancer treatment does not cause widespread DNA damage.
“This is contrary to what physicians and scientists have long accepted as fact,” said study author Richard K. Wilson, PhD, of The Genome Institute at Washington University.
“It led us to consider a novel hypothesis: p53 mutations accumulate randomly as part of the aging process and are present in blood stem cells long before a patient is diagnosed with therapy-related AML.”
When therapy-related AML occurs, it typically develops 1 to 5 years after treatment with chemotherapy or radiation. Its incidence varies by cancer type. For example, 10% of lymphoma patients who relapse after chemotherapy go on to develop therapy-related AML, compared to 0.1% of breast cancer patients.
The researchers knew that patients with therapy-related AML are more likely than other AML patients to have a high rate of p53 mutations in their blood cells.
But the team was surprised to find that nearly 50% of 19 healthy subjects (aged 68 to 89 with no history of cancer or chemotherapy) had mutations in one copy of p53, an indicator that many people acquire mutations in this gene as they age.
The finding encouraged the researchers to dig further. They scoured the US to find bone marrow samples from patients with therapy-related AML that had been stored before the patients developed leukemia.
“We wanted to know whether we could go back in time—before a patient is diagnosed with therapy-related AML—to find the exact p53 mutation that caused them to develop leukemia years later,” Dr Link said.
The researchers found 7 bone marrow samples that fit the criteria. In 4 samples, they detected specific mutations in p53 that were present at very low rates in blood cells or bone marrow 3 to 6 years before the patients developed AML.
In the 3 cases in which p53 mutations could not be found, the researchers said it’s possible the mutations were present but at rates too low to be detected, or it may be that other age-related mutations contributed to the onset of therapy-related AML.
In related work in mice, the team showed that chemotherapy causes HSCs with mutations in p53 to divide rapidly, which gives them a competitive advantage. But that was not the case in HSCs with both copies of the gene intact.
The researchers suspect the early accumulation of p53 mutations in HSCs likely contributes to the frequent chromosomal and genetic abnormalities seen in patients with therapy-related AML and their poor responses to chemotherapy. The team believes other age-related mutations may be involved in the disease as well.
“We’re already conducting follow-up studies to look for other age-related mutations that may be at play in therapy-related AML,” Dr Link said. “As individuals, we’re not genetically homogeneous throughout our lives. Our DNA is constantly changing as we age, and we know this plays an important role in the development of cancer.”
“With advanced genomics, we can investigate the interplay between aging and the random accumulation of mutations, as a means to improve the diagnosis, treatment, and prevention of cancer.” ![]()

Credit: Rhoda Baer
A new study challenges the view that cancer treatment is a direct cause of therapy-related acute myeloid leukemia (AML).
The research suggests that mutations in p53 can accumulate in hematopoietic stem cells (HSCs) as a person ages, years before a cancer diagnosis.
If and when cancer develops, these mutated cells are more resistant to treatment and multiply at an accelerated pace after exposure to chemotherapy or radiation therapy, which can then lead to AML.
The findings, reported in Nature, open up new avenues for research to predict which patients are at risk of developing therapy-related AML and to find ways to prevent it.
“Until now, we’ve really understood very little about therapy-related AML and why it is so difficult to treat,” said study author Daniel Link, MD, of Washington University in St Louis, Missouri.
“This gives us some important clues for further studies aimed at treatment and prevention.”
Dr Link and his colleagues began this research by sequencing the genomes of 22 patients with therapy-related AML. The patients had similar numbers and types of mutations in their leukemia cells as other patients who developed AML without prior exposure to chemotherapy or radiation, an indication that cancer treatment does not cause widespread DNA damage.
“This is contrary to what physicians and scientists have long accepted as fact,” said study author Richard K. Wilson, PhD, of The Genome Institute at Washington University.
“It led us to consider a novel hypothesis: p53 mutations accumulate randomly as part of the aging process and are present in blood stem cells long before a patient is diagnosed with therapy-related AML.”
When therapy-related AML occurs, it typically develops 1 to 5 years after treatment with chemotherapy or radiation. Its incidence varies by cancer type. For example, 10% of lymphoma patients who relapse after chemotherapy go on to develop therapy-related AML, compared to 0.1% of breast cancer patients.
The researchers knew that patients with therapy-related AML are more likely than other AML patients to have a high rate of p53 mutations in their blood cells.
But the team was surprised to find that nearly 50% of 19 healthy subjects (aged 68 to 89 with no history of cancer or chemotherapy) had mutations in one copy of p53, an indicator that many people acquire mutations in this gene as they age.
The finding encouraged the researchers to dig further. They scoured the US to find bone marrow samples from patients with therapy-related AML that had been stored before the patients developed leukemia.
“We wanted to know whether we could go back in time—before a patient is diagnosed with therapy-related AML—to find the exact p53 mutation that caused them to develop leukemia years later,” Dr Link said.
The researchers found 7 bone marrow samples that fit the criteria. In 4 samples, they detected specific mutations in p53 that were present at very low rates in blood cells or bone marrow 3 to 6 years before the patients developed AML.
In the 3 cases in which p53 mutations could not be found, the researchers said it’s possible the mutations were present but at rates too low to be detected, or it may be that other age-related mutations contributed to the onset of therapy-related AML.
In related work in mice, the team showed that chemotherapy causes HSCs with mutations in p53 to divide rapidly, which gives them a competitive advantage. But that was not the case in HSCs with both copies of the gene intact.
The researchers suspect the early accumulation of p53 mutations in HSCs likely contributes to the frequent chromosomal and genetic abnormalities seen in patients with therapy-related AML and their poor responses to chemotherapy. The team believes other age-related mutations may be involved in the disease as well.
“We’re already conducting follow-up studies to look for other age-related mutations that may be at play in therapy-related AML,” Dr Link said. “As individuals, we’re not genetically homogeneous throughout our lives. Our DNA is constantly changing as we age, and we know this plays an important role in the development of cancer.”
“With advanced genomics, we can investigate the interplay between aging and the random accumulation of mutations, as a means to improve the diagnosis, treatment, and prevention of cancer.” ![]()

Credit: Rhoda Baer
A new study challenges the view that cancer treatment is a direct cause of therapy-related acute myeloid leukemia (AML).
The research suggests that mutations in p53 can accumulate in hematopoietic stem cells (HSCs) as a person ages, years before a cancer diagnosis.
If and when cancer develops, these mutated cells are more resistant to treatment and multiply at an accelerated pace after exposure to chemotherapy or radiation therapy, which can then lead to AML.
The findings, reported in Nature, open up new avenues for research to predict which patients are at risk of developing therapy-related AML and to find ways to prevent it.
“Until now, we’ve really understood very little about therapy-related AML and why it is so difficult to treat,” said study author Daniel Link, MD, of Washington University in St Louis, Missouri.
“This gives us some important clues for further studies aimed at treatment and prevention.”
Dr Link and his colleagues began this research by sequencing the genomes of 22 patients with therapy-related AML. The patients had similar numbers and types of mutations in their leukemia cells as other patients who developed AML without prior exposure to chemotherapy or radiation, an indication that cancer treatment does not cause widespread DNA damage.
“This is contrary to what physicians and scientists have long accepted as fact,” said study author Richard K. Wilson, PhD, of The Genome Institute at Washington University.
“It led us to consider a novel hypothesis: p53 mutations accumulate randomly as part of the aging process and are present in blood stem cells long before a patient is diagnosed with therapy-related AML.”
When therapy-related AML occurs, it typically develops 1 to 5 years after treatment with chemotherapy or radiation. Its incidence varies by cancer type. For example, 10% of lymphoma patients who relapse after chemotherapy go on to develop therapy-related AML, compared to 0.1% of breast cancer patients.
The researchers knew that patients with therapy-related AML are more likely than other AML patients to have a high rate of p53 mutations in their blood cells.
But the team was surprised to find that nearly 50% of 19 healthy subjects (aged 68 to 89 with no history of cancer or chemotherapy) had mutations in one copy of p53, an indicator that many people acquire mutations in this gene as they age.
The finding encouraged the researchers to dig further. They scoured the US to find bone marrow samples from patients with therapy-related AML that had been stored before the patients developed leukemia.
“We wanted to know whether we could go back in time—before a patient is diagnosed with therapy-related AML—to find the exact p53 mutation that caused them to develop leukemia years later,” Dr Link said.
The researchers found 7 bone marrow samples that fit the criteria. In 4 samples, they detected specific mutations in p53 that were present at very low rates in blood cells or bone marrow 3 to 6 years before the patients developed AML.
In the 3 cases in which p53 mutations could not be found, the researchers said it’s possible the mutations were present but at rates too low to be detected, or it may be that other age-related mutations contributed to the onset of therapy-related AML.
In related work in mice, the team showed that chemotherapy causes HSCs with mutations in p53 to divide rapidly, which gives them a competitive advantage. But that was not the case in HSCs with both copies of the gene intact.
The researchers suspect the early accumulation of p53 mutations in HSCs likely contributes to the frequent chromosomal and genetic abnormalities seen in patients with therapy-related AML and their poor responses to chemotherapy. The team believes other age-related mutations may be involved in the disease as well.
“We’re already conducting follow-up studies to look for other age-related mutations that may be at play in therapy-related AML,” Dr Link said. “As individuals, we’re not genetically homogeneous throughout our lives. Our DNA is constantly changing as we age, and we know this plays an important role in the development of cancer.”
“With advanced genomics, we can investigate the interplay between aging and the random accumulation of mutations, as a means to improve the diagnosis, treatment, and prevention of cancer.” ![]()
First randomized evidence for kinase inhibitor use in AML

Photo courtesy of ASH
SAN FRANCISCO—Researchers have presented the first randomized evidence that kinase inhibitors are effective in the treatment of acute myeloid leukemia
(AML).
The multikinase inhibitor sorafenib improved event-free and relapse-free survival in younger patients.
“Interestingly, at this point in time, we can see no clear overall survival benefit for patients treated in the sorafenib arm,” said trial investigator Christoph Röllig, MD, of the Universitätsklinikum Dresden in Germany.
Dr Röllig, representing the Study Alliance Leukemia, presented data on sorafenib from the SORAML trial during the plenary session of the 2014 ASH Annual Meeting (abstract 6). Some funding for this trial was provided by Bayer Healthcare, the company developing sorafenib.
Dr Röllig explained that support for sorafenib’s clinical efficacy in AML was based primarily on case series and a few early phase clinical and nonrandomized
trials.
An earlier randomized study with sorafenib in older AML patients showed no beneficial antileukemic effect with the addition of the agent, and the treatment was associated with significant morbidity.
However, because the biology of AML and drug tolerance are different in younger people, the Study Alliance Leukemia decided to test the drug in a younger
patient population.
They randomized 276 newly diagnosed AML patients aged 60 years or younger to receive 2 cycles of induction chemotherapy with an anthracycline and cytarabine plus either sorafenib or placebo.
The sorafenib dose was 800 mg per day orally. All patients received at least one dose of study medication, forming the statistical analysis set.
Once in complete remission, intermediate-risk patients with a family donor and high-risk patients with a matched donor went on to stem cell transplant.
All other patients proceeded to high-dose cytarabine-based consolidation treatment plus sorafenib or placebo followed by 1 year of maintenance treatment with sorafenib or placebo.
The primary endpoint was event-free survival (EFS). An event was defined as primary treatment failure, relapse, or death.
Patients in each arm were a median age of 50 years, 17% were FLT3-ITD positive, and 33% were NPM1 mutated.
The complete response (CR) rate was 60% in the sorafenib arm and 59% in the placebo arm. Patients with FLT3-ITD mutation achieved a 57% CR rate with sorafenib and a 52% CR rate with placebo.
After a median follow-up of 3 years, investigators observed “significant prolongation of event-free survival in the sorafenib arm,” Dr Röllig said.
Patients on the sorafenib arm had a median EFS of 40% compared with 22% on the placebo arm, or 21 months compared with 9 months (P=0.013).
Patients were censored at the time of transplant. However, uncensored results were very similar, Dr Röllig noted, “with an even greater advantage for sorafenib.”
Fifty-six percent of sorafenib-treated patients were relapse-free and alive after 3 years, compared with 38% of patients on placebo (P=0.017).
The 3-year overall survival was 63% in the sorafenib arm and 56% in the placebo arm (P=0.382).
An exploratory analysis of FLT3-ITD patients revealed that 1-year EFS for sorafenib-treated patients was 54%, and, for placebo-treated patients, it was 50%.
“The reasons for potential efficacy of sorafenib in this mainly FLT3-ITD-negative population must remain speculative,” Dr Röllig said. “We can speculate that the inhibition of other kinases apart from FLT3 might be responsible for the efficacy of this drug in this patient population.”
Sorafenib significantly increased the risk of grade 3 or greater hand-foot syndrome (P<0.001), diarrhea (P=0.001), bleeding (P=0.016), rash (P=0.045), liver toxicity (P=0.048), and fever (P=0.035).
Dr Röllig indicated a confirmatory trial would be desirable in order to establish sorafenib in the AML treatment armamentarium. ![]()

Photo courtesy of ASH
SAN FRANCISCO—Researchers have presented the first randomized evidence that kinase inhibitors are effective in the treatment of acute myeloid leukemia
(AML).
The multikinase inhibitor sorafenib improved event-free and relapse-free survival in younger patients.
“Interestingly, at this point in time, we can see no clear overall survival benefit for patients treated in the sorafenib arm,” said trial investigator Christoph Röllig, MD, of the Universitätsklinikum Dresden in Germany.
Dr Röllig, representing the Study Alliance Leukemia, presented data on sorafenib from the SORAML trial during the plenary session of the 2014 ASH Annual Meeting (abstract 6). Some funding for this trial was provided by Bayer Healthcare, the company developing sorafenib.
Dr Röllig explained that support for sorafenib’s clinical efficacy in AML was based primarily on case series and a few early phase clinical and nonrandomized
trials.
An earlier randomized study with sorafenib in older AML patients showed no beneficial antileukemic effect with the addition of the agent, and the treatment was associated with significant morbidity.
However, because the biology of AML and drug tolerance are different in younger people, the Study Alliance Leukemia decided to test the drug in a younger
patient population.
They randomized 276 newly diagnosed AML patients aged 60 years or younger to receive 2 cycles of induction chemotherapy with an anthracycline and cytarabine plus either sorafenib or placebo.
The sorafenib dose was 800 mg per day orally. All patients received at least one dose of study medication, forming the statistical analysis set.
Once in complete remission, intermediate-risk patients with a family donor and high-risk patients with a matched donor went on to stem cell transplant.
All other patients proceeded to high-dose cytarabine-based consolidation treatment plus sorafenib or placebo followed by 1 year of maintenance treatment with sorafenib or placebo.
The primary endpoint was event-free survival (EFS). An event was defined as primary treatment failure, relapse, or death.
Patients in each arm were a median age of 50 years, 17% were FLT3-ITD positive, and 33% were NPM1 mutated.
The complete response (CR) rate was 60% in the sorafenib arm and 59% in the placebo arm. Patients with FLT3-ITD mutation achieved a 57% CR rate with sorafenib and a 52% CR rate with placebo.
After a median follow-up of 3 years, investigators observed “significant prolongation of event-free survival in the sorafenib arm,” Dr Röllig said.
Patients on the sorafenib arm had a median EFS of 40% compared with 22% on the placebo arm, or 21 months compared with 9 months (P=0.013).
Patients were censored at the time of transplant. However, uncensored results were very similar, Dr Röllig noted, “with an even greater advantage for sorafenib.”
Fifty-six percent of sorafenib-treated patients were relapse-free and alive after 3 years, compared with 38% of patients on placebo (P=0.017).
The 3-year overall survival was 63% in the sorafenib arm and 56% in the placebo arm (P=0.382).
An exploratory analysis of FLT3-ITD patients revealed that 1-year EFS for sorafenib-treated patients was 54%, and, for placebo-treated patients, it was 50%.
“The reasons for potential efficacy of sorafenib in this mainly FLT3-ITD-negative population must remain speculative,” Dr Röllig said. “We can speculate that the inhibition of other kinases apart from FLT3 might be responsible for the efficacy of this drug in this patient population.”
Sorafenib significantly increased the risk of grade 3 or greater hand-foot syndrome (P<0.001), diarrhea (P=0.001), bleeding (P=0.016), rash (P=0.045), liver toxicity (P=0.048), and fever (P=0.035).
Dr Röllig indicated a confirmatory trial would be desirable in order to establish sorafenib in the AML treatment armamentarium. ![]()

Photo courtesy of ASH
SAN FRANCISCO—Researchers have presented the first randomized evidence that kinase inhibitors are effective in the treatment of acute myeloid leukemia
(AML).
The multikinase inhibitor sorafenib improved event-free and relapse-free survival in younger patients.
“Interestingly, at this point in time, we can see no clear overall survival benefit for patients treated in the sorafenib arm,” said trial investigator Christoph Röllig, MD, of the Universitätsklinikum Dresden in Germany.
Dr Röllig, representing the Study Alliance Leukemia, presented data on sorafenib from the SORAML trial during the plenary session of the 2014 ASH Annual Meeting (abstract 6). Some funding for this trial was provided by Bayer Healthcare, the company developing sorafenib.
Dr Röllig explained that support for sorafenib’s clinical efficacy in AML was based primarily on case series and a few early phase clinical and nonrandomized
trials.
An earlier randomized study with sorafenib in older AML patients showed no beneficial antileukemic effect with the addition of the agent, and the treatment was associated with significant morbidity.
However, because the biology of AML and drug tolerance are different in younger people, the Study Alliance Leukemia decided to test the drug in a younger
patient population.
They randomized 276 newly diagnosed AML patients aged 60 years or younger to receive 2 cycles of induction chemotherapy with an anthracycline and cytarabine plus either sorafenib or placebo.
The sorafenib dose was 800 mg per day orally. All patients received at least one dose of study medication, forming the statistical analysis set.
Once in complete remission, intermediate-risk patients with a family donor and high-risk patients with a matched donor went on to stem cell transplant.
All other patients proceeded to high-dose cytarabine-based consolidation treatment plus sorafenib or placebo followed by 1 year of maintenance treatment with sorafenib or placebo.
The primary endpoint was event-free survival (EFS). An event was defined as primary treatment failure, relapse, or death.
Patients in each arm were a median age of 50 years, 17% were FLT3-ITD positive, and 33% were NPM1 mutated.
The complete response (CR) rate was 60% in the sorafenib arm and 59% in the placebo arm. Patients with FLT3-ITD mutation achieved a 57% CR rate with sorafenib and a 52% CR rate with placebo.
After a median follow-up of 3 years, investigators observed “significant prolongation of event-free survival in the sorafenib arm,” Dr Röllig said.
Patients on the sorafenib arm had a median EFS of 40% compared with 22% on the placebo arm, or 21 months compared with 9 months (P=0.013).
Patients were censored at the time of transplant. However, uncensored results were very similar, Dr Röllig noted, “with an even greater advantage for sorafenib.”
Fifty-six percent of sorafenib-treated patients were relapse-free and alive after 3 years, compared with 38% of patients on placebo (P=0.017).
The 3-year overall survival was 63% in the sorafenib arm and 56% in the placebo arm (P=0.382).
An exploratory analysis of FLT3-ITD patients revealed that 1-year EFS for sorafenib-treated patients was 54%, and, for placebo-treated patients, it was 50%.
“The reasons for potential efficacy of sorafenib in this mainly FLT3-ITD-negative population must remain speculative,” Dr Röllig said. “We can speculate that the inhibition of other kinases apart from FLT3 might be responsible for the efficacy of this drug in this patient population.”
Sorafenib significantly increased the risk of grade 3 or greater hand-foot syndrome (P<0.001), diarrhea (P=0.001), bleeding (P=0.016), rash (P=0.045), liver toxicity (P=0.048), and fever (P=0.035).
Dr Röllig indicated a confirmatory trial would be desirable in order to establish sorafenib in the AML treatment armamentarium. ![]()